Advanced Cell Cryopreservation Protocols: Optimizing Freezing and Thawing for Enhanced Viability in Biomedical Research
This article provides a comprehensive guide to cell cryopreservation for researchers and drug development professionals.
Advanced Cell Cryopreservation Protocols: Optimizing Freezing and Thawing for Enhanced Viability in Biomedical Research
Abstract
This article provides a comprehensive guide to cell cryopreservation for researchers and drug development professionals. It covers the fundamental principles of cryobiology, detailed step-by-step protocols for freezing and thawing, advanced troubleshooting for common issues, and a comparative analysis of emerging technologies. The content synthesizes current industry practices and recent scientific findings to help optimize cell viability, maintain stemness, and ensure reproducibility in advanced therapies and research applications.
The Science of Cryopreservation: Core Principles and Critical Preparations for Cell Survival
This application note details the critical role of cryopreservation in biomedical research and drug development for preserving genetic integrity and establishing secure backup cell stocks. We provide a consolidated overview of the principles underpinning successful cryopreservation, followed by detailed, actionable protocols for the freezing and thawing of mammalian cells. The note includes standardized methodologies, optimized reagent solutions, and data presentation to ensure experimental reproducibility and maximize post-thaw cell viability and function.
Cryopreservation is a cornerstone technique for the long-term storage of living cells and tissues at ultra-low temperatures, typically below -150°C in liquid nitrogen, effectively halting all metabolic activity [1] [2]. Its importance extends far beyond simple storage; it is an essential strategy for maintaining genetic integrity, preventing phenotypic drift, and creating reliable backup stocks for research reproducibility and biopharmaceutical production [3] [1]. Without cryopreservation, maintaining cell lines in continuous culture leads to significant risks, including genetic instability due to selective pressures, increased chances of microbial contamination, and substantial investments in time and resources [2]. Implementing a robust cell banking system is therefore indispensable for safeguarding valuable cell lines, including primary cells and stem cells, ensuring they remain available with consistent characteristics for future experiments, cell-based assays, and therapeutic applications [3] [4].
Quantitative Data and Analysis
The following tables summarize key quantitative parameters for successful cryopreservation, derived from established best practices.
Table 1: Standard Cryopreservation Parameters for Mammalian Cells
| Parameter | Recommended Range | Rationale & Impact |
|---|---|---|
| Cell Viability Pre-Freeze | >75% [1] | Ensures a healthy population is preserved; lower viability compromises recovery. |
| Cell Concentration | 1x10^6 to 5x10^6 cells/mL [5] [1] | Prevents overcrowding and resource competition; avoids apoptosis from low density. |
| Cooling Rate | -1°C/minute [5] [1] [4] | Allows water to exit cells slowly, minimizing lethal intracellular ice crystallization. |
| Storage Temperature | < -150°C (Liquid Nitrogen) [2] | Halts all biochemical activity, enabling virtually indefinite storage. |
| DMSO Concentration | 10% (v/v) [1] [4] | Common standard; balances cryoprotection with cytotoxicity. |
Table 2: Cryoprotectant Agent (CPA) Comparison
| Cryoprotectant | Type | Common Usage | Key Considerations |
|---|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating [4] | 10% in culture medium or serum [1] | Gold standard; can be cytotoxic and requires rapid post-thaw removal [1]. |
| Glycerol | Penetrating [4] | 10% in culture medium or serum [1] | Slower cell permeability; often used for red blood cells and certain sensitive cells. |
| Trehalose | Non-Penetrating [4] | 20-100mM in combination with other CPAs | Stabilizes membranes; often used in vitrification mixtures to reduce toxicity of PAs [4]. |
Experimental Protocols
Protocol: Cryopreservation of Mammalian Cells
This protocol is adapted from established best practices for freezing adherent and suspension mammalian cell lines [5] [1].
Principle: To preserve cells at a specific passage in a state of suspended animation by using a controlled slow freeze in the presence of cryoprotectants, ensuring high viability and functionality upon thawing.
Materials:
- Healthy, log-phase cells (70-80% confluent for adherent cells) [5]
- Appropriate cell culture medium
- Cryopreservation medium (e.g., 90% FBS + 10% DMSO, or serum-free alternatives) [1]
- Trypsin-EDTA (for adherent cells)
- Phosphate Buffered Saline (PBS)
- Centrifuge tubes
- Programmable freezer or isopropanol freezing chamber (e.g., CoolCell) [1]
- Cryogenic vials
- -80°C Freezer
- Liquid nitrogen storage tank
Methodology:
- Cell Harvesting: For adherent cells, wash with PBS, trypsinize, and neutralize with complete medium. For suspension cells, proceed directly [1].
- Cell Counting and Viability Assessment: Centrifuge the cell suspension (300 x g, 5 min). Resuspend the pellet and perform a cell count and viability assay (e.g., Trypan Blue exclusion). Ensure viability is >75% [5] [1].
- Centrifugation and Resuspension: Centrifuge the required volume of cell suspension again. Aspirate the supernatant completely.
- Freezing Medium Addition: Gently resuspend the cell pellet in pre-chilled freezing medium to achieve a final concentration of 1-5 x 10^6 cells/mL. Keep the tube on wet ice [5].
- Aliquoting: Quickly aliquot 1 mL of the cell suspension into labeled cryovials.
- Controlled-Rate Freezing: Immediately place the cryovials into a pre-cooled isopropanol freezing chamber and transfer it to a -80°C freezer for a minimum of 4 hours (ideally overnight). The chamber ensures a cooling rate of approximately -1°C/minute [5] [1].
- Long-Term Storage: The following day, promptly transfer the cryovials to the vapor phase of a liquid nitrogen storage tank for long-term preservation [5].
Protocol: Thawing and Recovery of Cryopreserved Cells
Principle: To rapidly reanimate frozen cells while minimizing the cytotoxic effects of cryoprotectants like DMSO and osmotic stress, thereby maximizing cell recovery.
Materials:
- Cryovial of frozen cells
- 37°C water bath
- Pre-warmed complete culture medium
- Centrifuge tubes
- Culture vessel
Methodology:
- Rapid Thaw: Retrieve the cryovial from liquid nitrogen storage. Without delay, immerse it in a 37°C water bath with gentle agitation until only a small ice crystal remains (approximately 60-90 seconds). Do not submerge the vial cap [5] [1].
- Decontamination: Wipe the exterior of the vial with 70% ethanol before transferring to a biosafety cabinet.
- Dilution and Cryoprotectant Removal: Gently transfer the thawed cell suspension to a centrifuge tube containing 10 mL of pre-warmed complete medium. This rapid dilution reduces DMSO toxicity [1].
- Centrifugation: Centrifuge the cell suspension at 300 x g for 5 minutes. Discard the supernatant.
- Resuspension and Plating: Gently resuspend the cell pellet in fresh, pre-warmed complete culture medium. Transfer the cells to an appropriate culture vessel and place in a 37°C, 5% CO₂ incubator [1].
- Post-Thaw Assessment: After 24 hours, perform a visual inspection for cell attachment (adherent cells) and a viability count to confirm successful recovery [5].
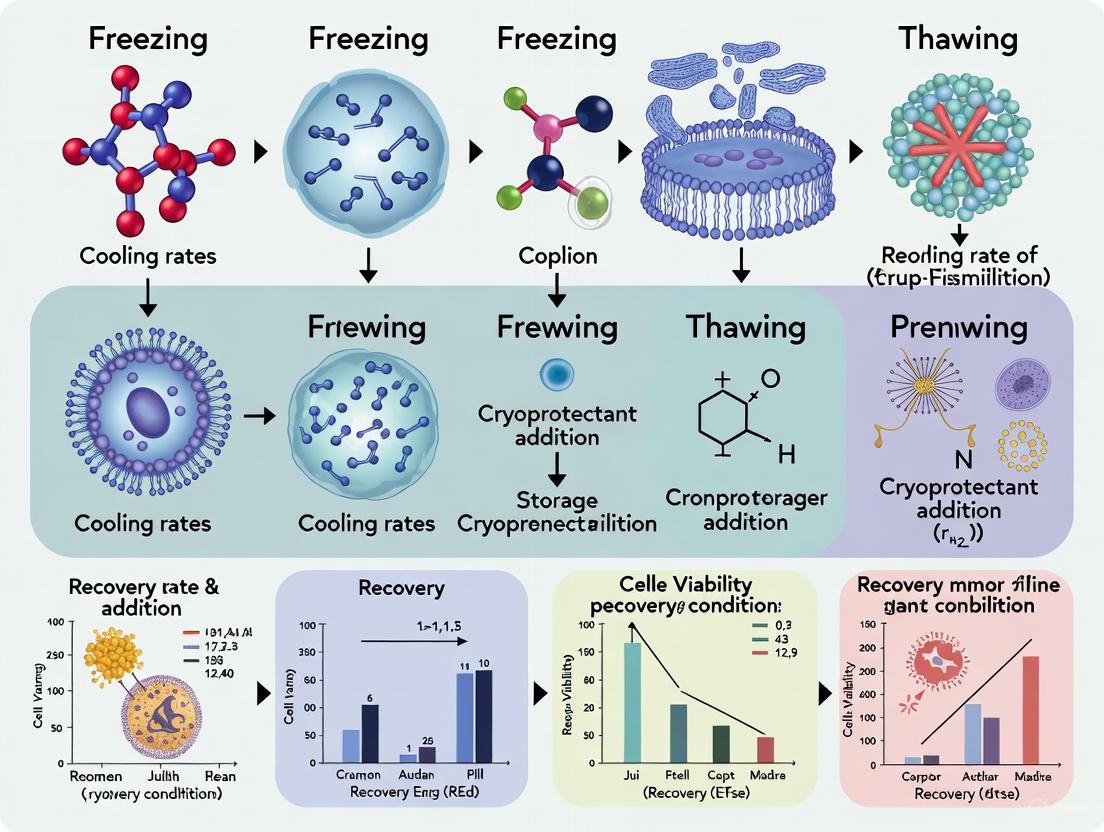
Visualization of Workflows
Cryopreservation Principle: Slow Freezing
Thawing and Recovery Process
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Cell Cryopreservation
| Item | Function & Application |
|---|---|
| Cryoprotective Agents (CPAs) | Protect cells from ice crystal damage and osmotic stress during freeze-thaw. DMSO is the most common penetrating CPA [4]. |
| Serum (e.g., FBS) | Provides proteins and other macromolecules that stabilize cell membranes and reduce ice crystal formation in traditional freezing media [1]. |
| Serum-Free Freezing Media | Chemically defined formulations that eliminate batch-to-batch variability of serum, essential for clinical or regulated applications [1]. |
| Controlled-Rate Freezer | Equipment that ensures a consistent, optimal cooling rate (e.g., -1°C/min), critical for protocol reproducibility and high viability [1] [2]. |
| Isopropanol Freezing Chamber | A passive, cost-effective device that approximates a -1°C/min cooling rate when placed at -80°C, suitable for most cell types [1]. |
| Liquid Nitrogen Storage System | Provides the ultra-low temperatures (<-150°C) required for long-term (years) stable preservation of cell stocks with minimal degradation [5] [2]. |
Cryoprotectants are substances used to protect biological tissue from freezing damage, specifically the formation of ice crystals that can mechanically disrupt cellular membranes and cause lethal increases in solute concentration during the cryopreservation process [4] [6]. The field of cryopreservation began to advance significantly in the mid-20th century when researchers discovered that the addition of cryoprotective agents (CPAs) could dramatically improve cell survival after freezing and thawing [4]. The origins of low-temperature tissue storage research date back to the late 1800s, but the critical breakthrough occurred when glycerol was first successfully used to protect spermatozoa in subfreezing temperatures, followed by the discovery of dimethyl sulfoxide (DMSO) as an effective cryoprotectant in the late 1950s [4] [7].
Cryoprotectants are broadly categorized into two classes: permeating agents (PAs) and non-permeating agents (NPAs). Permeating agents, which include DMSO, glycerol, ethylene glycol, and propylene glycol, are characterized by their relatively small molecular size (typically less than 100 daltons) and amphiphilic nature, allowing them to easily penetrate cell membranes [4]. These agents function primarily by depressing the freezing point of water and promoting vitrification—the formation of an amorphous, glassy solid instead of crystalline ice—through hydrogen bonding with water molecules [4] [6]. Non-permeating agents, such as polyethylene glycol (PEG), sucrose, and trehalose, are typically larger molecules that exert their protective effects extracellularly by inducing vitrification and minimizing osmotic stress [4].
The effectiveness of any cryoprotectant depends on its ability to increase solute concentration within and around cells without exhibiting significant toxicity, a balance that often necessitates using precisely defined concentrations and sometimes mixtures of different cryoprotectants [4] [6]. For decades, cryopreservation protocols relied heavily on fetal bovine serum (FBS) as a medium component, but in recent years, there has been a significant shift toward serum-free formulations due to concerns about variability, contamination risks, and regulatory requirements, particularly for cell-based therapies and biopharmaceutical production [8] [9].
Table 1: Classification of Common Cryoprotectants
| Type | Examples | Molecular Weight | Mechanism of Action | Common Applications |
|---|---|---|---|---|
| Permeating Agents | DMSO, Glycerol, Ethylene Glycol, Propylene Glycol | < 100 Da | Penetrate cell membrane, depress freezing point, promote vitrification | Cell lines, stem cells, sperm, oocytes, embryos [4] |
| Non-Permeating Agents | Trehalose, Sucrose, Raffinose, PEG, PVP | > 100 Da | Remain extracellular, induce vitrification, stabilize membranes | Biopharmaceuticals, sensitive cell types, vitrification mixtures [4] |
Mechanisms of Action and Damage Pathways
Cryoprotectant Mechanisms
Cryoprotectants operate through multiple interconnected mechanisms to protect cells during the freezing and thawing processes. Their primary function is to mitigate the two main theories of freezing damage: (1) the mechanical destruction of cellular membranes by ice crystals, and (2) the lethal increase in solute concentration in the remaining liquid phase as ice forms [4]. Permeating cryoprotectants like DMSO and glycerol readily cross biological membranes and increase the intracellular solute concentration. This depresses the freezing point of water and reduces the amount of water available to form ice crystals, thereby promoting vitrification [4] [6]. The ability of these compounds to form hydrogen bonds with water is crucial to their protective effect, as it interferes with the formation of critical nucleation sites required for crystal formation [4].
DMSO exhibits additional concentration-dependent effects on membrane dynamics. At low concentrations (approximately 5%), it decreases membrane thickness and increases permeability. At standard cryopreservation concentrations (10%), it induces water pore formation in biological membranes, facilitating the replacement of intracellular water with cryoprotectant. However, at high concentrations (40%), it can cause lipid bilayers to disintegrate, demonstrating the narrow window between protection and toxicity [4]. Non-permeating agents operate extracellularly by a similar vitrification mechanism, creating a stable glassy matrix that prevents ice crystal growth and minimizes osmotic shock to cells [4].
Cellular Damage Pathways During Cryopreservation
The journey of cells through cryopreservation exposes them to multiple potential damage pathways that cryoprotectants must address, as illustrated in the diagram below.
Beyond the physical damage from ice crystals, cells face significant challenges from osmotic stress. As extracellular water freezes, solutes become concentrated, creating a hypertonic environment that draws water out of cells, leading to harmful cell shrinkage. During thawing, the reverse process can cause cells to swell and potentially lyse if not properly managed [4]. The cooling and thawing rates are critical factors influencing these damage pathways. Slow cooling rates (approximately 1°C/min) allow sufficient time for water to exit cells before freezing, minimizing intracellular ice formation, but may prolong exposure to concentrated solutes. Rapid cooling can lead to devastating intracellular ice formation [4] [1]. Different cell types require optimized cooling rates; for example, rapid cooling is associated with better outcomes for oocytes and embryonic stem cells, while slow cooling is recommended for hepatocytes and mesenchymal stem cells [4].
Comparative Analysis of DMSO, Glycerol, and Serum-Free Formulations
DMSO (Dimethyl Sulfoxide)
DMSO is one of the most widely used permeating cryoprotectants in research and clinical applications. At the standard concentration of 10% (often corresponding to a 2M solution), DMSO increases the porosity of the cellular membrane, facilitating water movement and helping to prevent the formation of damaging ice crystals by increasing intracellular solute concentration [4]. Its efficacy has been demonstrated across diverse cell types, including stem cells, immune cells, and various primary cells [8] [1].
A key advantage of DMSO is its proven performance in preserving complex tissues. For instance, in a comparative study on human testicular tissue, DMSO at 0.7 mol/l concentration maintained the structure of seminiferous tubules and spermatogonia significantly better than protocols using propanediol or glycerol [10]. However, DMSO is not without limitations. It exhibits concentration-dependent toxicity; at high concentrations, it can disrupt lipid bilayers [4]. Furthermore, concerns have emerged about its potential to induce epigenetic changes and differentiation in certain sensitive cell types, such as stem cells [7]. Clinical side effects, including tonic-clonic seizure and cardiac arrest during infusion of autologous peripheral blood stem cells, have also been reported, though these are often associated with the reinfusion of DMSO-preserved cells rather than the freezing process itself [7].
Glycerol
Glycerol was the first cryoprotectant discovered, successfully used for the cryopreservation of spermatozoa in the late 1940s [4] [6]. It remains a valuable tool, particularly for cell types sensitive to DMSO. Like DMSO, it is a permeating agent that depresses the freezing point and promotes vitrification.
Glycerol's effectiveness can be context-dependent. In a study on rooster semen cryopreservation, DMSO generally performed better than glycerol across various freezing protocols and concentrations [11]. Furthermore, glycerol was found to be severely damaging to the basal compartment of seminiferous tubules in testicular tissue, making it unsuitable for that specific application [10]. Glycerol's permeability varies significantly between cell types, which can sometimes lead to insufficient protection or osmotic damage if not carefully controlled. It is often used as an alternative when DMSO toxicity is a concern or for specific protocols, such as the cryopreservation of certain insect or amphibian cells that naturally produce glycerol as a cryoprotectant [6].
Serum-Free Formulations
The shift toward serum-free cryopreservation media is driven by several critical factors: the need to eliminate batch-to-batch variability inherent in fetal bovine serum (FBS), reduce the risk of contamination by animal-derived pathogens, and align with regulatory standards for clinical applications, particularly in cell therapy and regenerative medicine [8] [9].
Research has demonstrated that well-designed serum-free formulations can match or even surpass the performance of serum-containing media. A 2007 study on vascular cell lines showed that cryopreservation in serum-free solutions specifically formulated for low-temperature storage (Unisol-cryoprotectant vehicle) produced viable cells with retention values up to 75% of unfrozen controls. Crucially, the study concluded that "including serum in the formulation provided no additional benefit to the cells and in some cases actually produced lower cell viability after cryopreservation" [9]. Modern serum-free media are complex, defined solutions that often incorporate a combination of permeating cryoprotectants (like DMSO), non-permeating agents (such as trehalose or sucrose), and other stabilizing components to maintain cell integrity during freeze-thaw cycles [8].
Table 2: Comparative Analysis of DMSO, Glycerol, and Serum-Free Formulations
| Parameter | DMSO | Glycerol | Serum-Free Formulations |
|---|---|---|---|
| Standard Concentration | 5-10% (v/v) [4] [1] | 10% (v/v) [1] | Varies; often includes DMSO + NPAs [8] |
| Mechanism | Permeating agent; induces pore formation [4] | Permeating agent [4] | Combined permeating & non-permeating agents [8] [4] |
| Key Advantages | High efficacy for many cell types; well-established protocols [1] | Lower toxicity for some sensitive cells [1] | Defined composition; reduced variability & contamination risk; regulatory compliance [8] [9] |
| Key Limitations | Potential cytotoxicity; can affect differentiation & epigenetics [7] | Variable permeability; not ideal for all tissues (e.g., testicular) [10] | May require optimization for specific cell types [8] |
| Post-Thaw Viability (Examples) | >90% for MSC in serum-free media [8] | ~71% motility for rooster semen at 15% [11] | Up to 75% viability of unfrozen controls for vascular cells [9] |
| Primary Applications | Stem cells, immune cells, cell therapy, primary cells [8] [1] | Semen (historically), DMSO-sensitive cells [6] [11] | Cell therapy manufacturing, biopharmaceuticals, clinical applications [8] |
Application Notes and Protocols
Standard Mammalian Cell Cryopreservation Protocol
The following protocol outlines a standardized, controlled-rate method for cryopreserving mammalian cells, adaptable to both serum-containing and serum-free media. This protocol is designed to maximize post-thaw viability and functionality for a wide range of adherent and suspension cell types [1].
Principle: Cryopreservation at a controlled cooling rate of -1°C/minute minimizes intracellular ice crystal formation by allowing sufficient water efflux from cells before freezing. The addition of a cryoprotectant (DMSO or glycerol) further protects cells by promoting vitrification [4] [1].
Materials:
- Cryopreservation Media (See Table 1 in Section 4.2 for formulations)
- 1-2 mL sterile cryovials
- Controlled-rate freezing device (e.g., CoolCell or programmable freezer)
- Liquid nitrogen storage tank
- -80°C freezer
Procedure:
- Cell Preparation: Harvest cells during their optimal growth phase (typically logarithmic phase). For adherent cells, wash with PBS, dissociate with trypsin, and neutralize with culture media. For suspension cells, proceed directly to centrifugation [1].
- Viability and Counting: Count cells using a hemocytometer or automated counter. Ensure cell viability is at least 75% before cryopreservation [1].
- Centrifugation: Centrifuge the cell suspension at 300 x g for 5 minutes at room temperature. Carefully aspirate the supernatant [1].
- Resuspension in Cryomedium: Loosen the cell pellet gently. Resuspend cells in pre-chilled cryopreservation media at a density of 1 x 10^6 to 1 x 10^7 cells/mL. Gently mix to ensure a uniform suspension. Note: Cells should not remain in cryomedium containing DMSO at room temperature for more than 10 minutes to minimize toxicity [1].
- Aliquoting: Dispense 1 mL of the cell suspension into each labeled cryovial. Seal the vials tightly.
- Controlled-Rate Freezing: Place the cryovials into a controlled-rate freezing device (e.g., CoolCell) and immediately transfer to a -80°C freezer for 24 hours. The device will ensure a consistent cooling rate of approximately -1°C/minute [1].
- Long-Term Storage: After 24 hours, promptly transfer the cryovials to the vapor or liquid phase of a liquid nitrogen storage system (-135°C to -196°C) for long-term preservation. Avoid prolonged storage at -80°C, as this can reduce viability [1].
Quality Control:
- Post-Thaw Analysis: Always assess the viability and functionality of a representative vial after thawing. This can include trypan blue exclusion for viability, flow cytometry for specific markers, and functional assays (e.g., differentiation potential for stem cells, secretion for production cells) [4].
- Record Keeping: Maintain detailed records including passage number, date frozen, cell density, viability pre-freeze and post-thaw, and the specific cryomedium formulation used.
Formulation-Specific Considerations
Table 3: Cryopreservation Media Formulations for Different Culture Systems
| Culture Type | Freezing Media Formulation | Notes & Considerations |
|---|---|---|
| Cells in FBS-containing Media | 90% FBS + 10% DMSO [1] | Traditional method; provides undefined nutrients and proteins. High protein content may interfere with downstream applications. |
| Cells in Serum-Free Media | 90% conditioned media + 10% DMSO OR Commercial serum-free cryomedium [1] | Conditioned media is the supernatant from the centrifugation step. Commercial serum-free media are optimized for defined components and regulatory compliance [8]. |
| Glycerol-Sensitive Cells | 90% FBS + 10% Glycerol [1] | Glycerol permeates more slowly than DMSO for some cell types; requires careful optimization of equilibration and thawing times. |
| Advanced Serum-Free Formulations | Defined base (e.g., RPMI, DMEM) + 10% DMSO + Non-permeating agents (e.g., trehalose, sucrose) + Synthetic polymers [8] [7] | Designed for high recovery and consistent performance in regulated environments like cell therapy manufacturing [8]. |
Thawing and Recovery Protocol
The thawing process is as critical as freezing for maintaining cell viability. Rapid thawing is essential to minimize the time cells are exposed to the cytotoxic effects of DMSO and to prevent the growth of small, damaging ice crystals (recrystallization) during the phase transition [1].
Procedure:
- Rapid Thaw: Remove the cryovial from liquid nitrogen and immediately place it in a 37°C water bath. Gently agitate the vial until only a small ice crystal remains (approximately 80% thawed). This should take no longer than 1-2 minutes. Do not thaw at room temperature or submerge the vial cap. [1]
- Dilution and Cryoprotectant Removal: Immediately after thawing, decontaminate the vial with 70% ethanol. Using a pipette, gently transfer the cell suspension to a 15 mL conical tube containing 10 mL of pre-warmed complete culture medium. This step rapidly dilutes the cryoprotectant [1].
- Centrifugation: Centrifuge the cell suspension at 300 x g for 5 minutes to pellet the cells and remove the cryoprotectant-containing supernatant [1].
- Resuspension and Culture: Discard the supernatant, gently resuspend the cell pellet in fresh, pre-warmed culture medium, and transfer the cells to an appropriate culture vessel. Place the vessel in a 37°C, 5% CO₂ incubator [1].
- Post-Thaw Assessment: Assess cell viability 24 hours post-thaw to allow for recovery. For sensitive applications (e.g., cell therapy), functional assays should be performed to confirm the retention of critical biological activity [8] [4].
Applications in Research and Drug Development
The selection and optimization of cryoprotectants are pivotal across numerous fields, from basic research to advanced clinical applications. The following workflow outlines the key decision points for selecting and applying cryoprotectants in a research and development pipeline.
Cell Therapy Manufacturing: This area demands the highest standards for cryoprotectant selection. Serum-free, xeno-free formulations are essential for regulatory compliance and patient safety. These formulations are designed to preserve not only viability (>90% for mesenchymal stem cells) but also critical therapeutic functions, such as differentiation potential and secretory profile, post-thaw [8]. Consistency is paramount, as variability in cryopreservation can directly impact clinical outcomes.
Biopharmaceutical Production: The production of therapeutic proteins relies on stable, consistent cell banks. Serum-free cryopreservation of production cell lines (e.g., CHO cells) ensures reproducible yields and reduces the risk of batch failures caused by serum variability or contamination. Adopting serum-free media has been reported to increase post-thaw productivity by 15-20% compared to serum-based methods [8].
Regenerative Medicine and Advanced Therapies: Cryopreservation of delicate cell types like induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs) requires specialized protocols to maintain their pluripotent state. Serum-free media are critical here, as serum can introduce uncontrolled differentiation signals. Optimized protocols can achieve viability rates exceeding 90% while preserving pluripotency markers and differentiation capacity, which is essential for tissue engineering and transplantation applications [8].
Research and Biobanking: In academic and industrial research, serum-free cryopreservation minimizes experimental variability, leading to more reliable and reproducible results. For biobanking of clinical samples (e.g., blood, tissue biopsies), serum-free media ensure sample integrity for future diagnostic analysis and eliminate the risk of contamination by animal components, which is critical for downstream genomic or proteomic analyses [8].
The Scientist's Toolkit: Essential Reagents and Materials
Successful cryopreservation relies on a suite of specialized reagents and equipment. The following table details key solutions and tools essential for implementing robust cryopreservation protocols.
Table 4: Essential Research Reagents and Solutions for Cryopreservation
| Tool/Solution | Function/Description | Application Notes |
|---|---|---|
| DMSO (Dimethyl Sulfoxide) | Permeating cryoprotectant; standard concentration 5-10% [4] [1]. | Use high-grade, sterile-filtered DMSO. Hyroscopic; store properly. Add to media just before use to avoid precipitation. |
| Glycerol | Permeating cryoprotectant; standard concentration 10% [1] [6]. | An alternative to DMSO for sensitive cells. Sterilize by autoclaving or filtration. |
| Serum-Free Cryopreservation Media | Defined, animal-origin-free media for clinical & sensitive research applications [8]. | Available from vendors (e.g., Thermo Fisher, STEMCELL Tech). Formulations are often cell type-specific (e.g., for T-cells, MSC). |
| Trehalose | Non-permeating disaccharide cryoprotectant; stabilizes membranes & proteins [4]. | Often used in combination with permeating CPAs to reduce their toxic concentration. |
| Controlled-Rate Freezer (e.g., CoolCell) | Device ensuring consistent cooling rate (~-1°C/min) critical for high viability [1]. | Passive devices (CoolCell) are placed in a -80°C freezer. Active, programmable freezers offer more flexibility. |
| Liquid Nitrogen Storage System | Provides long-term storage at -135°C (vapor) to -196°C (liquid) [1]. | Liquid phase offers lower temperature but risk of explosion if vial seal fails. Vapor phase is safer for routine storage. |
| Cryovials | Specially designed tubes for low-temperature storage; typically 1-2 mL capacity. | Use internally-threaded vials for superior seal and to prevent liquid nitrogen ingress during storage. |
The field of cryopreservation is evolving beyond the conventional use of DMSO and glycerol. Research is increasingly focused on the development of advanced cryoprotectant mixtures that reduce toxicity by combining multiple agents at lower individual concentrations [6] [7]. Furthermore, bio-inspired approaches are gaining traction, such as the use of antifreeze proteins and cryoprotectants like trehalose, which are produced naturally by extremophiles to withstand freezing conditions [6] [7].
Emerging technologies are also poised to transform cryopreservation workflows. Vitrification, the process of solidifying water into a glassy state without ice crystallization, is being advanced for complex tissues and organs using high concentrations of cryoprotectant cocktails [6] [7]. Novel warming techniques, such as inductive heating of magnetic nanoparticles, address the challenge of achieving rapid and uniform warming, which is critical for the success of vitrification [7]. The integration of library-based discovery approaches and materials science is enabling the high-throughput screening and design of new polymeric cryoprotectants and ice-binding inhibitors [7].
The judicious selection and application of cryoprotectants—spanning the established efficacy of DMSO, the utility of glycerol, and the modern advantages of serum-free formulations—are foundational to successful cell preservation. The optimal cryopreservation strategy is not one-size-fits-all; it must be tailored to the specific cell type, application, and regulatory context. As the demand for cell-based therapies and biopharmaceuticals continues to grow, the adoption of defined, serum-free cryopreservation media is expected to become the standard, driven by the imperative for consistency, safety, and regulatory compliance. The future of cryopreservation lies in the intelligent design of next-generation cryoprotectants and protocols that further minimize damage, enhance recovery, and enable the long-term preservation of increasingly complex biological systems.
Within the broader context of cell freezing and thawing protocol research, the steps taken prior to the freezing process are critical determinants of post-thaw cell viability, functionality, and experimental reproducibility. Cryopreservation is not merely a pause button for cells; it is a stressful event that only healthy, optimally prepared cultures can withstand without significant loss. For researchers, scientists, and drug development professionals, establishing robust pre-freeze checkpoints is a non-negotiable standard for ensuring the integrity of cell banks and the reliability of downstream applications, from basic research to cell-based therapies. This application note details the essential pre-freeze assessments—cell health, confluency, and contamination status—providing structured protocols and data to standardize this vital preparatory phase.
Key Pre-Freeze Checkpoints
A successful cryopreservation outcome hinges on verifying three key cellular conditions immediately before freezing. The quantitative targets for these checkpoints are summarized in Table 1.
Table 1: Quantitative Pre-Freeze Checkpoint Targets
| Checkpoint | Optimal Target / Status | Critical Thresholds & Notes |
|---|---|---|
| Cell Health & Growth Phase | Logarithmic (log) growth phase [12] [13] [1] | High viability (>75% [1], ideally >90% [13]) is required. Cells should be passaged 1-2 days before freezing [14] [15]. |
| Cell Confluency | 70-80% for most adherent cells [16] [17] [13] | Avoid overconfluency (>80-100%) to prevent stress, death, and spontaneous differentiation [16] [12] [17]. |
| Contamination Status | Confirmed absence of microbial contamination [12] [13] | Check for media turbidity, unexpected color change, or morphological changes in cells [13]. Conduct mycoplasma testing [13]. |
Checkpoint 1: Cell Health and Growth Phase
Rationale: Cells must be in a robust state of health to survive the rigors of cryopreservation. Harvesting cells during their logarithmic growth phase ensures maximum metabolic activity and health, which is a strong predictor of post-thaw recovery [12] [13] [1]. Cells in this phase are most resilient, while those in the stationary or decline phase have a significantly reduced capacity to withstand freezing stress.
Experimental Protocol: Assessing Growth Phase and Viability
- Method: Perform a cell count and viability assay 1-2 days after the last passaging, immediately before the freezing procedure [14] [15].
- Procedure:
- Harvest Cells: Detach adherent cells using a standard method (e.g., trypsin/EDTA) or collect suspension cells [1].
- Prepare Cell Suspension: Resuspend cells in an appropriate culture medium [1].
- Count and Assess Viability: Mix the cell suspension with Trypan Blue (or an equivalent dye) and load it into a hemocytometer [18] [1]. Viable cells will exclude the dye, while non-viable cells will take it up.
- Calculation: Calculate the total cell count and the percentage of viable cells. Proceed with cryopreservation only if viability exceeds 75% [1], though ideally it should be >90% [13].
Checkpoint 2: Cell Confluency
Rationale: Cell confluency is the percentage of the culture vessel surface area covered by adherent cells [16] [17]. It is a crucial parameter that helps determine the timing for passaging and cryopreservation [16]. Overconfluency can lead to nutrient depletion, contact inhibition, competition for physical space, and even the onset of spontaneous differentiation in sensitive cell types like stem cells and preadipocytes [16] [17]. This state dramatically increases cell stress and death upon thawing [17]. Conversely, freezing cells at too low a confluency can also yield suboptimal results.
Experimental Protocol: Measuring Confluency Method 1: Qualitative Visual Estimation (Common but Subjective)
- Procedure: Visually inspect the cell monolayer under a standard phase-contrast microscope and estimate the percentage of the surface area covered [16] [17].
- Reference Guidelines:
- 50% Confluent: The area covered by cells is roughly equal to the area not covered by cells [17].
- 70-80% Confluent: The surface is mostly covered, but clear gaps between cells are still visible. This is the ideal range for freezing most cell types [16] [17] [13].
- 100% Confluent: The entire surface is covered by cells with no visible gaps between them [17].
Method 2: Automated Image Analysis (Accurate and Reproducible)
- Procedure: Use integrated imaging systems (e.g., EVOS M3000 Imaging System, Olympus CKX53 with confluency software) that capture images and automatically calculate the percentage of area covered by cells using thresholding and edge-detection algorithms [16] [17]. This method eliminates inter-researcher variability.
Checkpoint 3: Contamination Status
Rationale: Cryopreserving a contaminated culture is tantamount to preserving the contaminant, leading to the irreversible loss of the cell line and potential cross-contamination of other stocks. Microbial contamination (e.g., bacteria, fungi, mycoplasma) can deplete nutrients, alter cell metabolism, and induce cell death [16] [13].
Experimental Protocol: Assessing Contamination Status
- Method 1: Visual and Microscopic Inspection
- Method 2: Mycoplasma Testing
- Procedure: Given that mycoplasma contamination is not visible under a standard microscope, it is recommended to implement regular testing using commercially available PCR-based detection kits or enzymatic assays as part of the pre-freeze workflow, especially for master cell banks [13].
- Aseptic Technique: During all handling steps, use proper aseptic technique, including wiping down all containers with 70% ethanol or isopropanol before opening them inside a biosafety cabinet [18] [13].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Pre-Freeze Assessment
| Item | Function & Application |
|---|---|
| Hemocytometer | A specialized slide with a grid for manually counting cells and assessing population density [18]. |
| Trypan Blue | A vital dye used to distinguish between viable and non-viable cells during counting; non-viable cells with compromised membranes take up the blue stain [18] [1]. |
| Phase-Contrast Microscope | Essential for the visual inspection of cell morphology, confluency estimation, and initial checks for gross microbial contamination [16] [17]. |
| Automated Cell Counter | Instrument that automates cell counting and viability analysis, improving speed and reducing subjectivity compared to manual methods. |
| Mycoplasma Detection Kit | A dedicated test (e.g., PCR-based) to identify the presence of mycoplasma, a common and invisible cell culture contaminant [13]. |
| Cell-Freezing Medium | A specialized solution, often containing cryoprotectants like DMSO and FBS, designed to protect cells from freezing damage [14] [13] [1]. |
Integrated Workflow
The following diagram illustrates the logical sequence and decision points for the key pre-freeze checkpoints.
Logical Workflow for Pre-Freeze Checkpoints
The success of modern cell-based therapies, regenerative medicine, and biomedical research hinges on the ability to reliably preserve living cells without compromising their viability or biological function. The fundamental challenge of cryopreservation lies in navigating the complex thermodynamics of water phase changes at sub-zero temperatures. Intracellular ice crystallization is overwhelmingly lethal to cells, causing mechanical destruction of cellular membranes and organelles [19] [4]. Consequently, the core principles of cryopreservation focus on understanding and controlling the transition of water from liquid to solid states—either through crystalline formation or vitrification—to mitigate these damaging effects [20]. This application note examines the thermodynamic principles of glass transition and crystallization, detailing practical protocols designed to prevent intracellular ice formation and ensure high post-thaw cell viability and functionality for research and therapeutic applications.
Theoretical Foundations: Thermodynamics of Freezing
Ice Crystallization and Its Cellular Consequences
During freezing, the formation of ice crystals poses two primary mechanical threats to cells. First, extracellular ice formation mechanically crushes cells and creates osmotic imbalances. Second, intracellular ice crystals physically disrupt organelles and pierce the plasma membrane, which is almost always lethal [19] [4]. The energy dynamics of this process are critical; as water freezes, the latent heat of fusion is released, which can cause a temperature spike if not properly managed during controlled-rate freezing [20].
The nucleation of ice crystals can be described by the critical radius r, the minimum size a crystal nucleus must reach for spontaneous growth to occur. This radius is given by: [r = - {{2\gamma } \over {\Delta {Sv}\Delta T}}] where γ is the interfacial energy per unit area, and ΔSvΔT is the free energy of solidification per unit volume. Consequently, nucleation occurs when the supercooling ΔT satisfies: [\Delta T \ge - {{2\gamma } \over {\Delta {S_v}R}}] where R is the radius of an ice nucleating agent [19]. This relationship demonstrates that larger nucleating agents require smaller supercooling for ice formation to initiate.
The Glass Transition and Vitrification
Vitrification represents a fundamentally different approach to solidification, where water transitions into an amorphous, glass-like state without forming ice crystals. This process is achieved through rapid cooling and/or high concentrations of cryoprotective agents (CPAs), dramatically increasing solution viscosity until molecular motion effectively ceases [20] [4].
The glass transition point is the critical temperature at which this amorphous solid forms, typically ranging between -100°C and -130°C for cryopreservation solutions [21]. Below this temperature, biological time effectively stops, enabling indefinite storage. In contrast, the vitrification point refers to the specific conditions (combining CPA concentration and cooling rate) under which this glassy state is achieved without ice crystallization [21]. For biological samples containing cells or tissues, storage must occur below the glass transition temperature to ensure long-term stability [20].
Table 1: Critical Temperature Transitions in Cryopreservation
| Transition Point | Definition | Typical Temperature Range | Impact on Cells |
|---|---|---|---|
| Nucleation Point | Initial stage of ice crystal formation | -5°C to -10°C [21] | Ice crystals cause mechanical damage and osmotic stress [21] |
| Glass Transition (Tg) | Transition to amorphous glassy state | -100°C to -130°C [21] | Halts biochemical processes; enables long-term storage [20] |
| Vitrification Point | Achieves glassy state without ice formation | Below -120°C [21] | Minimizes cellular damage; maintains viability [21] |
Essential Concepts for Preventing Intracellular Ice
Cryoprotectant Mechanisms
Cryoprotective Agents (CPAs) are essential components of freezing media that protect cells through multiple mechanisms [4]:
- Depressing Ice Nucleation: CPAs lower the freezing point of the solution and reduce the amount of ice formed at any given temperature.
- Promoting Glass Transition: They facilitate the transition to a glassy state at higher temperatures.
- Reducing Cell Shrinkage: By modulating osmotic pressure, CPAs minimize deleterious cell dehydration during slow freezing.
- Stabilizing Membranes and Proteins: Some CPAs directly interact with cellular structures to maintain their integrity.
CPAs are categorized as permeating or non-permeating based on their ability to cross cell membranes. Permeating agents (e.g., DMSO, glycerol) enter cells and protect against intracellular ice formation, while non-permeating agents (e.g., sucrose, trehalose) exert their effects extracellularly, often enabling reduced concentrations of toxic permeating agents [4].
Cooling Rate Optimization
The cooling rate is a critical parameter that determines the balance between intracellular ice formation and osmotic dehydration damage. Different cell types have unique optimal cooling rates based on their membrane permeability and volume [4].
- Slow Cooling (≈1°C/min): Allows water to exit the cell before freezing, minimizing intracellular ice but potentially causing excessive dehydration [13] [4].
- Rapid Cooling (Vitrification): Prevents water efflux, resulting in vitrification rather than ice crystallization, but requires high CPA concentrations [20] [22].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Equipment for Cryopreservation Research
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Permeating Cryoprotectants | Penetrate cell membranes to prevent intracellular ice [4] | DMSO, Glycerol, Ethylene Glycol [4] |
| Non-Permeating Cryoprotectants | Act extracellularly; enable CPA concentration reduction [4] | Sucrose, Trehalose, Polyethylene Glycol (PEG) [4] |
| Optimized Freezing Media | Ready-to-use, defined formulations for specific cell types [13] | CryoStor CS10, mFreSR for pluripotent stem cells [13] |
| Controlled-Rate Freezer | Precisely manages cooling rate (typically -1°C/min) [13] [23] | Liquid nitrogen or electric cryocooling models [20] [23] |
| Passive Cooling Devices | Provides approximate cooling rate when CRF unavailable [13] | Nalgene Mr. Frosty, Corning CoolCell [13] |
| Cryogenic Storage Vials | Secure containment for long-term storage [13] | Internal-threaded vials; sterilized [13] |
| Liquid Nitrogen Storage | Long-term storage below glass transition (-135°C to -196°C) [13] [20] | Liquid or vapor phase nitrogen systems [13] |
Experimental Protocols
Protocol: Controlled-Rate Freezing for Mononuclear Cells
This standardized protocol is optimized for cell types such as Peripheral Blood Mononuclear Cells (PBMCs) and mesenchymal stromal cells, which benefit from slow cooling rates [13] [4].
Materials:
- Cryopreservation medium: CryoStor CS10 or equivalent containing 10% DMSO [13]
- Sterile cryogenic vials
- Controlled-rate freezer or passive freezing container
- Programmable water bath (37°C) or automated thawing device
Method:
- Harvesting and Preparation: Harvest cells during logarithmic growth phase at >80% confluency. Gently centrifuge to pellet cells and remove supernatant [13].
- CPA Addition: Resuspend cell pellet in pre-chilled (4°C) cryopreservation medium to a final concentration of 1x10^6 to 5x10^6 cells/mL. Gently mix to ensure uniform CPA exposure [13].
- Aliquoting: Dispense 1-2 mL of cell suspension into each cryogenic vial. Keep vials on wet ice to maintain temperature stability during CPA exposure [13].
- Controlled-Rate Freezing:
- Using Controlled-Rate Freezer: Place vials in chamber and initiate program:
- Using Passive Container: Place vials in isopropanol freezing container and transfer immediately to -80°C freezer for 18-24 hours [13].
- Long-Term Storage: Transfer vials to liquid nitrogen storage (-135°C to -196°C) for long-term preservation [13].
- Thawing and Assessment: Rapidly thaw vials in 37°C water bath with gentle agitation until only a small ice crystal remains. Immediately transfer to pre-warmed culture medium and assess viability and vitality [13] [21].
Protocol: Vitrification of Sensitive Cell Types
This method is particularly suitable for oocytes, embryos, and induced pluripotent stem cells (iPSCs) that are highly sensitive to CPA toxicity and ice crystal damage [24] [22].
Materials:
- Vitrification solution: Combination of permeating (e.g., DMSO, ethylene glycol) and non-permeating (e.g., sucrose) CPAs [4]
- Open or closed vitrification devices
- Liquid nitrogen for rapid cooling
Method:
- Equilibration: Expose cells to lower concentration CPA solution (e.g., 2-4 M permeating CPA) for 10-15 minutes at room temperature to permit partial dehydration and CPA penetration [4].
- Vitrification Solution Exposure: Transfer cells to high concentration vitrification solution (e.g., 6-8 M total CPAs with sucrose) for <60 seconds at room temperature [4].
- Rapid Cooling: Quickly load cells in minimal volume onto vitrification device and directly plunge into liquid nitrogen, achieving cooling rates >20,000°C/min [4].
- Storage and Thawing: Store in liquid nitrogen. For thawing, rapidly warm and sequentially transfer through decreasing CPA concentrations to remove CPAs and prevent osmotic shock [4].
Quantitative Data for Protocol Optimization
Table 3: Cell-Type Specific Cryopreservation Parameters and Outcomes
| Cell Type | Recommended Cooling Rate | Recommended CPA | Post-Thaw Viability Target | Key Functional Assays |
|---|---|---|---|---|
| Hepatocytes | Slow cooling [4] | 10% DMSO [4] | >80% [25] | Albumin secretion, drug metabolism [4] |
| Pancreatic Islets | Rapid cooling [4] | Vitrification mixtures [4] | >85% [25] | Glucose-stimulated insulin release [4] |
| Stem Cells (MSCs, HSCs) | Slow cooling (-1°C/min) [4] | 10% DMSO [13] [4] | >80% [25] | Differentiation potential, surface markers [21] |
| Oocytes | Rapid cooling (vitrification) [4] | EG/DMSO/sucrose [4] | >90% [24] | Fertilization rates, embryonic development [24] |
| CAR-T Cells | Controlled-rate freezing [23] | DMSO-containing [23] | >80% [25] | Cytokine release, tumor killing [23] |
Workflow and Thermodynamic Pathways
The following diagram illustrates the critical decision points in a cryopreservation protocol based on thermodynamic principles, guiding researchers toward either the crystalline or vitrification pathway.
Diagram 1: Thermodynamic Decision Pathway in Cryopreservation. This workflow outlines the critical branching points where cooling rate and CPA concentration determine whether cells follow the path of crystalline ice formation with dehydration or achieve a vitrified state.
Mastering the thermodynamics of freezing—specifically the interplay between glass transition, ice crystallization, and intracellular ice prevention—is fundamental to advancing cell-based research and therapies. The protocols and principles detailed in this application note provide a framework for optimizing cryopreservation outcomes based on cell-specific requirements. As the field progresses toward more complex cellular products, including engineered tissues and organoids, further refinement of these thermodynamic approaches will be essential. Future developments will likely focus on reducing CPA toxicity through improved vitrification mixtures, standardizing protocols across cell types, and enhancing monitoring techniques during the freezing process to ensure both high viability and preserved cellular functionality post-thaw.
Step-by-Step Protocols: From Log-Phase Harvest to Long-Term Liquid Nitrogen Storage
Within the comprehensive framework of cell freezing and thawing research, the pre-freeze preparation phase is critically important for ensuring high post-thaw viability and functionality. This stage establishes the foundational condition of cells before they undergo the stresses of cryopreservation. Two parameters are paramount: harvesting cells during their logarithmic growth phase (log phase) and resuspending them at an optimal concentration in cryopreservation medium. Neglecting these factors can lead to poor recovery, reduced viability, and experimental inconsistencies, ultimately compromising the value of cryopreserved cell stocks [26] [13]. This application note provides detailed protocols and best practices for these crucial pre-freeze steps, equipping researchers and drug development professionals with the methodologies needed to create high-quality, reproducible cell banks.
The Critical Importance of Log Phase Harvesting
Log phase, also known as the exponential growth phase, represents the period when cells are actively dividing and are at their peak metabolic health. Cells harvested during this period typically have >90% viability and are most resilient to the stresses of cryopreservation, including dissociation, centrifugation, and exposure to cryoprotectants like DMSO [26] [27]. Using log-phase cells for freezing leads to superior attachment and growth post-thaw, faster recovery, and more reliable experimental outcomes.
The primary rationale for this practice is the prevention of genetic drift and phenotypic changes. Continuous passaging of cells beyond their log phase can lead to senescence, genetic drift, and potential transformation, especially in finite cell lines [26]. Cryopreservation acts as a "pause button," suspending cellular metabolism. By freezing cells at their healthiest, their genetic integrity and functionality are preserved for future use. For adherent cultures, this means harvesting at 80-95% confluence, while suspension cultures should be harvested when the cell density is high but before the growth medium is exhausted [13] [28].
Table 1: Indicators of Log Phase for Different Culture Types
| Culture Type | Visual & Metabolic Indicators | Recommended Harvest Point |
|---|---|---|
| Adherent Cells | - Cells are actively dividing and mitotic figures may be visible.- Culture is sub-confluent (not 100% covered).- Medium is not exhausted (normal color).- Cells exhibit characteristic, healthy morphology. | 80-95% confluence [28] |
| Suspension Cells | - Cell density is increasing exponentially.- Culture medium has not shifted significantly in color/pH.- Viability is high (>90%) as determined by trypan blue exclusion. | Before maximum density is reached; while viability is >90% [27] |
Determining Optimal Cell Concentration for Freezing
Resuspending the cell pellet at the correct concentration in freezing medium is equally critical. A concentration that is too low can lead to poor recovery and viability after thawing, as a minimum cell density is often required for effective cell signaling and growth. Conversely, a concentration that is too high can promote undesirable cell clumping and exhaust the cryoprotectant, reducing its protective efficacy [13].
The optimal cell concentration is cell-type dependent. Researchers are advised to test a range of concentrations to determine the ideal density for their specific cell line. The general range for most mammalian cells is between 1x10^3 and 1x10^6 cells/mL, though many common cell types fall within a narrower window [13].
Table 2: General Guidelines for Cell Freezing Concentrations
| Cell Type | Typical Freezing Concentration | Notes & Considerations |
|---|---|---|
| Adherent Cells (general) | 1-5 x 10^6 cells/mL [28] [27] | A common starting point is ~2 x 10^6 cells/mL [28]. |
| Suspension Cells (general) | 5-10 x 10^6 cells/mL [27] | A common starting point is ~5 x 10^6 cells/mL [28]. |
| PBMCs | 5-25 x 10^6 cells/mL [29] | Concentration can be adjusted based on experimental needs and volume constraints. |
| Stem Cells (e.g., hPSCs) | Cell-type specific | Use specialized freezing media and follow vendor-recommended concentrations, which can vary [13]. |
Experimental Protocols
Protocol 1: Harvesting Adherent Cells in Log Phase
This protocol describes the process for harvesting adherent mammalian cells, such as HEK293 or HeLa, prior to cryopreservation.
Research Reagent Solutions & Materials
- Complete Growth Medium: Pre-warmed to 37°C [26].
- Balanced Salt Solution (e.g., DPBS): Without calcium or magnesium, sterile [26].
- Dissociation Reagent (e.g., Trypsin, TrypLE): Without phenol red, sterile [26] [28].
- Trypan Blue Solution (0.4%): For viability staining and cell counting [27].
- Hemocytometer or Automated Cell Counter [26].
- Centrifuge and Sterile Conical Tubes [26].
Methodology
- Preparation: Visually inspect the culture under a microscope. Confirm that cells are healthy, display normal morphology, and are at 80-95% confluence [28]. Ensure all reagents are pre-warmed and work under sterile conditions in a laminar flow hood.
- Aspiration: Carefully aspirate and discard the spent culture medium from the tissue culture vessel.
- Rinsing: Gently add a sufficient volume of pre-warmed DPBS to wash the cell monolayer. Swirl gently and aspirate the PBS. This step removes residual serum that can inhibit trypsin.
- Dissociation: Add enough pre-warmed dissociation reagent (e.g., TrypLE) to cover the monolayer. Incubate the vessel at 37°C for the time specified for the cell line (typically 2-5 minutes) [28].
- Neutralization: Firmly tap the vessel to dislodge the cells. Under microscopic examination, most cells should be detached and rounded. Add a volume of complete growth medium (containing serum) that is at least equal to the volume of dissociation reagent used to neutralize the reaction.
- Collection: Pipette the cell suspension over the surface of the vessel to collect any remaining cells and transfer the entire suspension to a sterile conical tube.
- Cell Counting: Perform a viable cell count using trypan blue exclusion and a hemocytometer or automated cell counter [26] [27]. Mix 10-20 µL of cell suspension with an equal volume of 0.4% trypan blue. Load onto a hemocytometer and count unstained (viable) and blue-stained (non-viable) cells. Calculate total and viable cell concentration.
Protocol 2: Harvesting Suspension Cells in Log Phase
This protocol is for harvesting non-adherent mammalian cells, such as Jurkat or HL-60 cells.
Research Reagent Solutions & Materials
- Complete Growth Medium [26].
- Trypan Blue Solution (0.4%) [27].
- Hemocytometer or Automated Cell Counter [26].
- Centrifuge and Sterile Conical Tubes [26].
Methodology
- Preparation: Gently mix the suspension culture to ensure a homogeneous cell distribution. Take a small sample for a viability count. Confirm the cells are in log phase by high viability (>90%) and increasing cell density [27].
- Collection: Transfer the entire cell suspension to a sterile conical tube.
- Centrifugation: Centrifuge the tube at 200-400 x g for 5-10 minutes at room temperature to pellet the cells [26] [27].
- Supernatant Removal: Carefully decant or aspirate the supernatant without disturbing the cell pellet.
- Resuspension: Gently tap the tube to loosen the pellet. Resuspend the cells in a small volume of fresh, pre-warmed complete growth medium by pipetting up and down slowly.
- Cell Counting: Perform a viable cell count as described in Protocol 1, Step 7.
Protocol 3: Determining Concentration and Preparing for Freezing
This final protocol covers calculating the required volume of freezing medium and preparing the cell suspension for aliquoting.
Research Reagent Solutions & Materials
- Freezing Medium: Pre-chilled (2-8°C). This can be a commercial, serum-free formulation (e.g., CryoStor) or a lab-made medium (e.g., 90% FBS + 10% DMSO) [26] [28].
- Sterile Cryogenic Vials [26].
- Pipettes and sterile tips.
Methodology
- Centrifugation: Centrifuge the harvested cell suspension (from Protocol 1 or 2) at 200-400 x g for 5-10 minutes [26]. Aspirate the supernatant completely.
- Concentration Calculation: Based on the viable cell count and the target freezing concentration (refer to Table 2), calculate the volume of freezing medium required.
- Volume of Freezing Medium (mL) = Total number of viable cells / Desired concentration (cells/mL)
- Resuspension in Freezing Medium: Gently tap the tube to loosen the cell pellet. Slowly add the calculated, pre-chilled volume of freezing medium to the pellet. Gently resuspend the cells using a pipette to achieve a homogeneous suspension. Work efficiently but avoid creating bubbles.
- Aliquoting: Quickly aliquot the cell suspension into pre-labeled cryogenic vials. Gently mix the main cell suspension frequently during aliquoting to ensure consistency across vials [26].
- Immediate Freezing: Transfer the filled cryovials to a controlled-rate freezing apparatus (e.g., "Mr. Frosty" or a programmable freezer) and place it in a -80°C freezer immediately. Do not delay, as cells are sensitive to extended exposure to cryoprotectants like DMSO at room temperature [29].
The workflow below summarizes the key decision points and steps in the pre-freeze preparation process.
Cryopreservation is a vital process in biological research and clinical applications, enabling the long-term storage of cells while maintaining their viability and functionality. The choice of freezing media is a critical determinant of post-thaw cell recovery and experimental reproducibility. This application note provides a detailed comparison between standard laboratory-prepared formulations and commercial serum-free alternatives, offering evidence-based protocols for researchers and drug development professionals working within the context of cell freezing and thawing optimization.
The transition from traditional serum-containing media to defined serum-free formulations addresses several challenges, including batch-to-batch variability, ethical concerns, and the risk of pathogen transmission associated with fetal bovine serum (FBS) [30] [31]. Commercial serum-free media offer standardized, ready-to-use solutions designed to provide consistent performance across diverse cell types and applications, from basic research to clinical cell therapy manufacturing.
Comparative Analysis: Formulations and Performance
Composition and Characteristics
Table 1: Key Components and Characteristics of Freezing Media Types
| Component/Characteristic | Standard Formulations | Commercial Serum-Free Media |
|---|---|---|
| Base Medium | Culture medium (e.g., RPMI, DMEM) [32] | Proprietary, chemically defined base [33] [13] |
| Protein Source | 10-90% Fetal Bovine Serum (FBS) [32] | Animal-derived protein-free or recombinant human proteins [30] [13] |
| Cryoprotectant | 10% DMSO, sometimes 10% glycerol [32] | Typically 10% DMSO; some with reduced DMSO or alternative agents [30] [34] |
| Regulatory Status | Laboratory-grade, often not suitable for therapeutics | Often manufactured under cGMP for clinical applications [13] |
| Key Advantage | Low cost, lab-specific customization | Defined composition, lot-to-lot consistency, reduced contamination risk [33] [31] |
| Primary Limitation | Serum variability, undefined components, immunogenicity risk | Higher cost, may require cell-specific optimization [33] |
Quantitative Performance Data
Recent comparative studies provide quantitative evidence of the performance of commercial serum-free media against standard FBS-based formulations.
Table 2: Performance Comparison in PBMC Cryopreservation (2-Year Study) [30] [31]
| Freezing Medium | DMSO Concentration | Viability & Functionality | Remarks |
|---|---|---|---|
| FBS (Reference) | 10% | Baseline for comparison | Traditional standard, raises ethical and safety concerns [31] |
| CryoStor CS10 | 10% | High viability and functionality comparable to FBS | Serum-free, effective for long-term (2-year) cryopreservation |
| NutriFreez D10 | 10% | High viability and functionality comparable to FBS | Serum-free, performs well in long-term storage |
| Bambanker D10 | 10% | Comparable viability, diverging T-cell functionality | Serum-free, may require functional validation for immune assays |
| Media with <7.5% DMSO | <7.5% | Significant viability loss | Eliminated from long-term study after initial assessment |
The data demonstrate that serum-free media containing 10% DMSO (CryoStor CS10 and NutriFreez D10) can effectively preserve cell viability and functionality over a two-year period, matching the performance of traditional FBS-supplemented media [30]. This is a significant finding for biobanking and clinical trials requiring long-term sample storage.
Detailed Protocols
Protocol 1: Preparation and Use of Standard Freezing Media
This protocol outlines the procedure for creating and using traditional serum-containing freezing media [32].
Reagents and Materials
- Log-phase cells at >80% confluency and >90% viability [13] [32]
- Complete growth medium (basal medium + serum)
- Fetal Bovine Serum (FBS)
- Cryoprotectant: Dimethyl Sulfoxide (DMSO, cell culture grade) or Glycerol
- Balanced salt solution (e.g., DPBS) without Ca2+/Mg2+ [32]
- Dissociation reagent (e.g., trypsin) for adherent cells [32]
- Sterile conical tubes (15 mL or 50 mL)
- Sterile cryogenic vials
Freezing Medium Formulation
A common standard formulation consists of:
- 50-90% Complete Growth Medium
- 10-50% FBS
- 10% DMSO [32]
Note: DMSO should be added last, and the complete freezing medium should be chilled (2°-8°C) before use to minimize DMSO toxicity [32].
Step-by-Step Procedure
- Harvest Cells: For adherent cells, wash with DPBS and detach using an appropriate dissociation reagent. Gently resuspend the detached cells in complete growth medium [32].
- Count and Centrifuge: Determine total cell count and viability. Centrifuge the cell suspension at approximately 100–400 × g for 5-10 minutes. Aspirate and discard the supernatant carefully [32].
- Resuspend in Freezing Medium: Resuspend the cell pellet in the pre-chilled standard freezing medium to achieve a final concentration typically between 1x10^6 to 1x10^7 cells/mL [13] [32]. Gently mix to ensure a homogeneous cell suspension.
- Aliquot: Dispense the cell suspension into sterile cryogenic vials, typically 1 mL per vial. Mix the suspension gently but frequently during aliquoting to ensure consistent cell density across vials [32].
- Freeze: Place the cryovials in an isopropanol freezing container (e.g., "Mr. Frosty") or an isopropanol-free container (e.g., Corning CoolCell) and immediately transfer to a -80°C freezer for 18-24 hours (or overnight) to achieve a cooling rate of approximately -1°C/minute [13] [32].
- Long-Term Storage: After 24 hours, promptly transfer the cryovials to a liquid nitrogen storage tank for long-term preservation in the vapor phase (below -135°C) [13] [32].
Protocol 2: Application of Commercial Serum-Free Freezing Media
This protocol describes the use of ready-to-use commercial serum-free media, which are increasingly critical for standardized and clinical-grade workflows [13].
Reagents and Materials
- Log-phase cells at >80% confluency and >90% viability [13]
- Commercial serum-free freezing medium (e.g., CryoStor CS10, NutriFreez D10, mFreSR) [30] [13]
- Balanced salt solution (e.g., DPBS)
- Dissociation reagent for adherent cells
- Sterile conical tubes
- Sterile cryogenic vials
Freezing Medium Selection
Select a medium optimized for your specific cell type:
- General Cell Types (PBMCs, etc.): CryoStor CS10 [30] [13]
- Human ES/iPS Cells: mFreSR [13]
- Mesenchymal Stromal Cells (MSCs): MesenCult-ACF Freezing Medium [13]
Step-by-Step Procedure
- Harvest Cells: Harvest cells as described in Protocol 1, Step 1.
- Count and Centrifuge: Determine total cell count and viability. Centrifuge the cell suspension and aspirate the supernatant completely.
- Resuspend in Commercial Medium: Resuspend the cell pellet directly in the pre-chilled, ready-to-use commercial serum-free medium at the manufacturer's recommended cell density (e.g., 1-2x10^6 cells/mL for iPSCs [34]). The medium already contains the optimized cryoprotectant (typically 10% DMSO) and other protective agents [13].
- Aliquot: Dispense the cell suspension into cryogenic vials, mixing gently to maintain homogeneity.
- Freeze: Use a controlled-rate freezing apparatus or a validated freezing container (e.g., CoolCell) placed at -80°C to ensure a consistent cooling rate of -1°C/minute [13].
- Long-Term Storage: Transfer vials to liquid nitrogen for long-term storage within 24 hours.
Workflow and Decision Pathway
The following diagram illustrates the key decision-making process and workflow for selecting and using an appropriate freezing media protocol.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Cryopreservation
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Cryoprotective Agents (CPAs) | Penetrate cell membrane, reduce ice crystal formation | DMSO (10%): Gold standard, intracellular CPA [34] [35]. Glycerol: Alternative intracellular CPA [32]. Handle DMSO with care. |
| Controlled-Rate Freezing Containers | Ensure optimal cooling rate (~-1°C/min) for cell survival | Isopropanol-containing: Nalgene Mr. Frosty [32]. Isopropanol-free: Corning CoolCell [13] [34]. Avoid non-validated homemade devices [34]. |
| Commercial Serum-Free Media | Ready-to-use, defined formulation for specific cell types | CryoStor CS10: General purpose & stem cells [13]. mFreSR: For human ES/iPS cells [13]. NutriFreez D10: Effective for PBMCs [30]. |
| Liquid Nitrogen Storage System | Long-term storage at <-135°C to halt metabolic activity | Store cryovials in the vapor phase of liquid nitrogen to prevent explosion risks associated with liquid phase storage [32] [34]. |
| Cell Detachment Reagents | Gently detach adherent cells for harvesting before freezing | Trypsin or TrypLE Express [32]. Minimize exposure time to maintain high viability. |
| Viability/Cell Counting Assays | Quantify cell count and viability pre-freeze and post-thaw | Trypan Blue exclusion with hemocytometer or automated cell counters (e.g., Countess) [32]. |
The choice between standard formulations and commercial serum-free alternatives for freezing media is a strategic decision that impacts experimental reproducibility, cell viability, and regulatory compliance. While standard FBS-DMSO formulations remain a cost-effective option for basic research, commercial serum-free media provide a robust, defined, and consistent solution ideal for critical applications, long-term biobanking, and clinical development.
Evidence confirms that leading serum-free media can match or exceed the performance of traditional media in preserving cell viability and functionality over extended periods [30]. Adhering to optimized protocols—emphasizing healthy starting cells, controlled-rate freezing, and proper storage conditions—is essential for success, regardless of the media chosen. As the field advances, the trends toward cGMP manufacturing, specialized formulations, and reduced DMSO content will further solidify the role of commercial serum-free media in modern biomedical research and therapeutic development.
Controlled-rate freezing is a cornerstone technique in biomedical research and biopharmaceutical development, essential for the long-term preservation of cell lines, primary cells, and sensitive biological therapeutics. By precisely managing the cooling process, researchers can mitigate the damaging effects of ice crystal formation, maintain cellular viability, and ensure the genetic and functional integrity of biological materials over indefinite storage periods. The standard cooling profile of -1°C per minute has emerged as a gold protocol for a wide variety of mammalian cells, representing a critical parameter that balances the osmotic stress and intracellular ice formation [1] [36]. This application note details the underlying principles, provides definitive protocols, and characterizes the necessary equipment to master this fundamental procedure, framing it within the broader context of cell freezing and thawing protocol research.
Principles and Mechanisms
The fundamental goal of controlled-rate freezing is to navigate the physical phase change of water from liquid to solid in a way that minimizes lethal damage to cellular structures.
The Physics of Cell Damage During Freezing
During uncontrolled freezing, two primary mechanisms cause cell death:
- Intracellular Ice Formation (IIF): If cooling occurs too rapidly, water within the cell does not have sufficient time to exit and forms destructive ice crystals that puncture organelles and the plasma membrane [1].
- Solution Effects (Solute Imbalance): If cooling is too slow, the prolonged exposure to a hypertonic extracellular environment causes excessive cellular dehydration and shrinkage, leading to osmotic stress and protein denaturation [1].
The -1°C/minute cooling rate is optimized to avoid both extremes. It allows enough time for water to osmotically exit the cell, thereby minimizing IIF, but is sufficiently rapid to limit the duration of exposure to damaging solute concentrations [36].
The Role of Cryoprotectants
Cryoprotectant agents (CPAs) like Dimethyl Sulfoxide (DMSO) or glycerol are integral to the process. They function by:
- Reducing the freezing point of the medium.
- Lowering the salt concentration in the residual unfrozen fraction, thus mitigating "solution effects" [1] [26].
- Amortizing the cell membrane and stabilizing proteins [13].
The following diagram illustrates the sequential protective mechanisms enabled by the controlled -1°C/minute rate and cryoprotectants.
Diagram 1: Protective cascade of controlled-rate freezing.
Successful cryopreservation depends on optimizing several interdependent parameters. The table below summarizes these key variables and their typical specifications for standard mammalian cell lines.
Table 1: Key Parameters for Controlled-Rate Freezing Protocols
| Parameter | Standard Specification | Rationale & Impact |
|---|---|---|
| Cooling Rate | -1°C / minute from room temperature to -40°C to -80°C [1] [36] | Balances water efflux (prevents IIF) against exposure time to hypertonic conditions (prevents solute damage) [36]. |
| Cell Viability (Pre-freeze) | >90% (Minimum >75%) [1] [26] | Ensures a healthy population is preserved; low viability compromises post-thaw recovery. |
| Cell Concentration | ~1 x 10^6 cells/mL [1] [13] | Optimal density for survival; too low can lead to poor recovery, too high can cause clumping. |
| Cryoprotectant | 5-10% DMSO or 10% Glycerol [1] [26] | DMSO is most common; Glycerol is alternative for sensitive lines. Cytotoxic at room temperature, requiring rapid handling. |
| Freezing Medium | 90% FBS* + 10% DMSO, or serum-free commercial media (e.g., CryoStor) [1] [26] [13] | *FBS provides extra protein and membrane stabilization. Defined, serum-free media are preferred for regulatory-compliant work. |
| Final Storage Temperature | < -135°C (typically in liquid nitrogen vapor phase) [36] [13] | Halts all metabolic activity. Storage at -80°C is suboptimal and leads to declining viability over weeks/months [1] [36]. |
Equipment and Methodology
Equipment for Achieving Controlled Cooling
Several technologies can achieve the -1°C/minute profile, each with distinct advantages.
Table 2: Comparison of Controlled-Rate Freezing Equipment
| Equipment Type | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Programmable Controlled-Rate Freezer [36] | Uses a pre-programmed cooling profile, often with liquid nitrogen injection. | Highest precision and reproducibility; validatable processes; suitable for sensitive cells and scalable volumes [36]. | High equipment cost; not as accessible for all labs. |
| Passive Cooling Devices (e.g., CoolCell or "Mr. Frosty") [1] [26] | Uses an isopropanol chamber or other insulator to create a predictable cooling rate in a -80°C freezer. | Low-cost, simple, and reliable; requires no electricity; highly accessible [1]. | Limited capacity; cooling rate is fixed and dependent on freezer performance. |
| Liquid Nitrogen-Free Freezers [37] | Uses mechanical refrigeration and precise control systems. | Portable; safe for cleanrooms (no contamination risk from LN2); lower long-term costs [37]. | Limited maximum freezing rate (~-1°C/min); may not be suitable for all cell types [37]. |
Standardized Freezing Protocol for Mammalian Cells
The following step-by-step protocol is applicable to both adherent and suspension mammalian cell lines.
Pre-freeze Preparation:
- Cell Status: Culture cells to mid-log phase growth (>90% viability, >80% confluency for adherent cells) [26] [13].
- Freezing Medium: Prepare fresh, and pre-cool to 2-8°C. A common formulation is 90% FBS + 10% DMSO. Warm to 37°C before use is also recommended by some protocols [1].
- Aseptic Technique: Perform all steps under sterile conditions in a laminar flow hood [13].
Procedure:
- Harvest Cells: For adherent cells, wash with PBS and detach using a standard dissociation reagent like trypsin. For suspension cells, proceed directly [1] [26].
- Neutralize & Count: Resuspend cells in complete growth medium. Determine total cell count and viability using a hemocytometer or automated cell counter with Trypan Blue exclusion [1] [26].
- Pellet and Resuspend: Centrifuge the cell suspension at 300 x g for 5 minutes. Aspirate the supernatant completely. Gently loosen the cell pellet [1].
- Re-suspension in Freezing Medium: Resuspend the cell pellet in the pre-cooled freezing medium to a final concentration of ~1 x 10^6 cells/mL [1] [13]. Mix gently but thoroughly to ensure a homogeneous suspension.
- Aliquoting: Quickly aliquot 1 mL of the cell suspension into labeled, sterile cryovials. Keep vials on ice or in a cooler after aliquoting [1].
- Initiate Freezing: Immediately transfer the cryovials to a pre-equilibrated controlled-rate freezing device.
- Long-Term Storage: Within 24 hours, transfer the cryovials to long-term storage in the vapor phase of liquid nitrogen (< -135°C) [1] [36]. Avoid prolonged storage at -80°C.
Diagram 2: Experimental workflow for cell cryopreservation.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful cryopreservation workflow relies on specific, high-quality materials. The following table lists essential items and their functions.
Table 3: Essential Reagents and Materials for Controlled-Rate Freezing
| Item | Function & Application Notes |
|---|---|
| Cryoprotectant (DMSO/Glycerol) | Penetrating agent that reduces ice crystal formation. Use high-purity, cell culture-tested grade. Handle with care as DMSO facilitates cellular uptake of other molecules [26]. |
| Serum (FBS) or Defined Stabilizer | Provides extracellular osmotic support and helps stabilize the cell membrane. Serum-free, defined cryomedium (e.g., CryoStor) is recommended for regulatory compliance and consistency [13]. |
| Base Growth Medium | Used as a component of the freezing medium to maintain physiological pH and nutrient balance. |
| Cryogenic Vials | Sterile, leak-proof vials designed to withstand extreme temperatures. Internal-threaded vials are preferred to prevent contamination [13]. |
| Controlled-Rate Freezing Device | Apparatus to ensure reproducible -1°C/min cooling. Can be active (programmable freezer) or passive (e.g., CoolCell) [1] [36]. |
| Liquid Nitrogen Storage System | For long-term storage of frozen samples at < -135°C. Vapor phase storage is generally safer than liquid phase to prevent vial explosion and cross-contamination [36]. |
Troubleshooting and Optimization
Even with a standardized protocol, researchers may encounter issues. Common problems and their solutions include:
- Low Post-Thaw Viability:
- Cause: Cells were not in log-phase, pre-freeze viability was low, or cells were held in freezing medium at room temperature for too long (>10 minutes) [1].
- Solution: Ensure cells are healthy and frozen at optimal density. Work quickly after adding freezing medium, keeping vials on ice before freezing.
- Excessive Cell Clumping or Lysis:
- Cause: Freezing rate was too fast or too slow; inappropriate cryoprotectant concentration [1].
- Solution: Verify the cooling rate calibration of your equipment. For sensitive cells, test alternative CPAs like glycerol or optimize DMSO concentration.
- Contamination:
- Cause: Non-sterile technique or compromised freezing medium.
- Solution: Practice strict aseptic technique and use antibiotic-antimycotic agents in culture if appropriate and validated.
Mastering the -1°C/minute cooling profile is a fundamental requirement for reliable and reproducible biopreservation. This controlled process, supported by appropriate cryoprotectants and proper technique, directly safeguards the viability, genetic stability, and functional utility of priceless biological resources. As research advances toward more complex models like organoids and cell therapies, the principles of controlled-rate freezing remain the bedrock upon which successful long-term storage strategies are built.
Cryopreservation is a fundamental technique in biomedical research and drug development, enabling the long-term storage of viable cell lines, primary cells, and stem cells. Within the broader context of cell freezing and thawing protocols, passive freezing methods utilizing isopropanol chambers represent a widely accessible and cost-effective alternative to expensive programmable freezing equipment. These chambers provide a standardized approach to achieving the critical slow cooling rate of approximately -1°C/minute essential for maintaining cell viability during the freezing process [26] [38] [39]. This application note details the methodology, optimization parameters, and practical considerations for implementing isopropanol chamber-based cryopreservation in research and development settings.
Materials and Reagents
Table 1: Essential reagents and equipment for cryopreservation using isopropanol chambers
| Category | Item | Specification/Function |
|---|---|---|
| Cryoprotective Agents | Dimethyl sulfoxide (DMSO) | 10% final concentration in freezing medium; penetrates cells to prevent ice crystal formation [26] [40]. |
| Glycerol | 10% final concentration; an alternative cryoprotectant that does not penetrate cells as readily [26] [41]. | |
| Freezing Medium | Serum-containing Medium | e.g., 90% Fetal Bovine Serum (FBS) + 10% DMSO; provides nutrients and protein for protection [26] [40]. |
| Serum-free Medium | Chemically defined, protein-free formulations with DMSO (e.g., 7.5%-10%) for sensitive cell types [26] [42]. | |
| Equipment | Isopropanol Chamber | Insulated container filled with isopropanol; ensures a slow, controlled cooling rate of ~-1°C/min [26] [40]. |
| Cryogenic Vials | Sterile, leak-proof vials designed for ultra-low temperature storage [26]. | |
| -80°C Freezer | For initial freezing phase with the isopropanol chamber [26]. | |
| Liquid Nitrogen Tank | For long-term storage of frozen vials in the vapor phase (< -135°C) [26]. |
Quantitative Performance Data
Table 2: Comparative analysis of isopropanol chamber performance and limitations
| Parameter | Isopropanol Chamber Performance | Notes and Limitations |
|---|---|---|
| Cooling Rate | Approximately -1°C/minute [26] [38] | The stated rate can vary based on vial position and isopropanol condition [38]. |
| Cell Viability Post-Thaw | Variable; can be suboptimal compared to controlled-rate systems [38] [43] | Highly dependent on protocol consistency and cell type. |
| Reproducibility | Lower than programmable or alcohol-free passive freezers [38] | Performance hindered by variability in isopropanol between freeze runs [38]. |
| Throughput | Limited to one run per day [38] | Requires long wait periods for the isopropanol to equilibrate to room temperature between uses [38]. |
| Key Advantage | Low initial cost and simplicity of use [40] [39] | Provides a more standardized method than homemade Styrofoam boxes [38]. |
Step-by-Step Protocol
Cell Preparation and Harvesting
- Culture Conditions: Use healthy, actively dividing cells in the logarithmic growth phase with at least 90% viability [26]. Passage cells 1-2 days before freezing to ensure robust health [40].
- Harvesting:
- Centrifugation: Pellet cells at approximately 100–400 × g for 5–10 minutes. Aspirate the supernatant completely [26].
Freezing Medium Preparation and Resuspension
- Preparation: Prepare a freezing medium, such as 90% FBS with 10% DMSO, and keep it cold (2°–8°C) until use [26] [40]. Note: Handle DMSO with care as it easily penetrates skin and can carry other compounds with it [26] [40].
- Resuspension: Resuspend the cell pellet in the cold freezing medium at a high density. A typical density for cryopreservation is 1-2 x 10^6 cells/mL [26] [42]. Keep the cell suspension on ice after adding DMSO.
Aliquotting and Freezing with the Isopropanol Chamber
- Aliquotting: Dispense 1 mL aliquots of the cell suspension into labeled cryovials. Mix the cell suspension gently but often to ensure a homogeneous distribution of cells in each vial [26].
- Chamber Setup: Place the cryovials into the isopropanol chamber, ensuring they are properly seated. Important: Check the manufacturer's instructions regarding the required level of isopropanol and replenish if necessary, as its condition affects performance [38].
- Slow Freezing: Transfer the entire chamber to a -80°C freezer for a minimum of 4 hours, or preferably overnight [26] [42] [40]. This allows for a controlled cooling rate of about -1°C per minute.
Long-Term Storage
- After the overnight freezing, quickly transfer the cryovials from the isopropanol chamber to a long-term storage system.
- For maximum stability, store vials in the gas phase of a liquid nitrogen tank (below -135°C) [26]. Storing in the liquid phase carries a risk of explosion [26].
Workflow and Decision Pathway
The following diagram illustrates the complete experimental workflow for cryopreservation using an isopropanol chamber.
Troubleshooting and Optimization
- Low Post-Thaw Viability: Ensure cells are in log phase and highly viable before freezing. Verify that the isopropanol chamber is at room temperature at the start of the procedure and has not been overused, as old isopropanol can degrade performance [38].
- Inconsistent Results Between Vials: This can result from uneven cooling within the chamber. Gently mix the cell suspension frequently during aliquotting to ensure homogeneity, and do not overload the chamber [26] [38].
- Alternative Passive Freezing Methods: For greater reproducibility without the cost of a programmable freezer, consider alcohol-free controlled-rate containers (e.g., CoolCell). These devices use a proprietary insulating foam and a thermal core to provide a consistent -1°C/minute cooling rate without the variability associated with isopropanol [38] [43].
Isopropanol chambers provide a simple and economically viable method for cryopreserving cell cultures, making them particularly suitable for laboratories with limited budgets or those initiating cryopreservation workflows. While users must be aware of limitations regarding reproducibility and potential variability, adhering strictly to the detailed protocol—focusing on cell health, cold freezing medium, correct chamber use, and prompt transfer to long-term storage—can yield successful results. For applications demanding higher reproducibility, such as in cell therapy development or biobanking, alcohol-free passive freezers present a robust and reliable alternative within the spectrum of passive freezing technologies.
Within the broader context of cell freezing and thawing protocol research, the thawing process is a critical, yet often overlooked, determinant of post-preservation cell success. The phase change from a frozen to a liquid state presents significant stresses to biological materials, including the risk of ice recrystallization and osmotic shock [44]. For researchers, scientists, and drug development professionals, the choice of thawing method is not merely a matter of convenience but a key variable impacting cell viability, functional recovery, and experimental reproducibility.
The 37°C water bath has long been the conventional method for rapidly thawing cryopreserved samples, leveraging a high heat transfer rate to minimize the time samples spend in a potentially damaging semi-frozen state [45] [46]. However, challenges such as temperature inconsistency, cross-contamination risk, and operational difficulties in non-laboratory settings have prompted the development of alternatives [47]. Modern dry thawing systems have emerged as a technologically advanced solution, offering a contained and controlled thermal environment. This application note provides a comparative assessment of these two techniques, supported by experimental data and detailed protocols, to guide the selection and optimization of thawing processes in biomedical research and development.
Comparative Analysis of Thawing Methods
A direct comparison of thawing methods is essential for evidence-based protocol selection. The following table summarizes core characteristics of the 37°C water bath and modern dry thawing systems.
Table 1: Fundamental Characteristics of Water Bath vs. Dry Thawing Systems
| Characteristic | 37°C Water Bath | Modern Dry Thawing Systems |
|---|---|---|
| Heating Medium | Liquid water | Solid metal blocks or beads [47] |
| Primary Advantage | Rapid heat transfer, widely available [45] | Contained system, portable, consistent temperature [47] |
| Contamination Risk | Present (if vial is not properly sealed) [47] | Very low [47] |
| Temperature Stability | Requires monitoring; can cool rapidly when cold samples are introduced [47] | Self-contained mechanism maintains consistent temperature [47] |
| Portability & On-site Use | Limited | High; often powered by low-voltage sources (e.g., vehicle socket) [47] |
| Typical Thawing Duration | ~1-2 minutes for 1 mL cryovials [46] [18] | Comparable; e.g., 30 seconds for 0.25 mL straws [47] |
Quantitative Performance Data
Beyond operational features, quantitative post-thaw cell quality metrics are crucial. A recent comparative study on rooster sperm provides robust, head-to-head experimental data on the impact of both methods on key cell quality attributes [47].
Table 2: Quantitative Post-thaw Cell Quality Metrics: Water Bath vs. Dry Thawing [47]
| Sperm Quality Parameter | Water Bath (37°C for 30s) | Dry Thawing System (37°C for 30s) |
|---|---|---|
| Total Motility (%) | 68.14% | 82.38% |
| Progressive Motility (%) | 21.20% | 33.18% |
| Viability (%) | 73.7% | 82.2% |
| Morphological Abnormalities (%) | 35.8% | 23.9% |
| Curvilinear Velocity (VCL, μm/s) | 66.49 | 79.41 |
| Average Path Velocity (VAP, μm/s) | 37.42 | 47.52 |
| Straight-Line Velocity (VSL, μm/s) | 21.59 | 27.18 |
| DNA Integrity - Tail DNA (%) | 81.11% | 77.37% |
| DNA Integrity - Olive Tail Moment | 16.93 | 15.28 |
The data demonstrates that the dry thawing system yielded superior post-thaw quality across nearly all measured parameters, including motility, viability, morphology, and kinematic characteristics [47]. Notably, metrics of DNA integrity also showed reduced damage with the dry thawing method, a critical factor for applications requiring genomic stability [47].
Experimental Protocols
Standardized protocols are vital for reproducibility. Below are detailed methodologies for thawing using both the water bath and a dry thawing system.
Standardized Protocol: 37°C Water Bath Thawing
This protocol is widely applicable to many cell types, including primary cells and stem cells [45] [46] [18].
Materials:
- Pre-warmed complete growth medium (37°C)
- 70% ethanol
- Centrifuge tubes
- Pipettes and serological pipettes
- Water bath accurately calibrated to 37°C
Procedure:
- Preparation: Warm a sufficient volume of complete growth medium in a 37°C water bath. Aseptically prepare a work area and label centrifuge tubes [45] [18].
- Retrieval: Quickly retrieve the cryovial from liquid nitrogen storage. Exercise caution as vials stored in liquid phase can present an explosion risk [45].
- Thawing: Immediately place the sealed cryovial in the 37°C water bath. Gently swirl the vial until only a small ice crystal remains, which typically takes 1–2 minutes. Avoid submerging the vial cap to prevent contamination [45] [46].
- Decontamination: Transfer the vial to the biosafety cabinet and thoroughly wipe the exterior with 70% ethanol [45] [18].
- Dilution: Gently transfer the thawed cell suspension to a centrifuge tube using a pipette. Slowly add pre-warmed medium dropwise (e.g., 10-20 mL) while gently swirling the tube to dilute the cryoprotectant (e.g., DMSO) and mitigate osmotic shock [45] [46].
- Washing: Centrifuge the cell suspension at a cell-appropriate speed (e.g., 200–300 × g) for 5–10 minutes [45] [48]. Carefully decant the supernatant without disturbing the pellet.
- Resuspension & Seeding: Gently resuspend the cell pellet in fresh, pre-warmed complete medium. Seed the cells at a high density into an appropriate culture vessel to optimize recovery [45].
Standardized Protocol: Dry Thawing System
This protocol utilizes a specialized dry thawing device, which employs precisely controlled metal surfaces to thaw samples [47].
Materials:
- Dry thawing system (e.g., portable device with slots for straws/vials)
- Pre-warmed complete growth medium (37°C)
- Other materials (centrifuge tubes, pipettes, etc.) as listed in the water bath protocol
Procedure:
- Setup: Power the dry thawing system and allow it to reach the setpoint temperature (e.g., 37°C). Prepare warm medium and labware aseptically as in the previous protocol [47].
- Loading: Remove the frozen straw (0.25 mL or 0.5 mL) or cryovial from storage and immediately place it into the designated, pre-warmed slot on the dry thawing device [47].
- Thawing: Allow the sample to thaw for the manufacturer-recommended duration (e.g., 30 seconds for 0.25 mL straws). The device maintains a consistent temperature, eliminating the need for swirling [47].
- Post-thaw Processing: Wipe the outside of the straw or vial with 70% ethanol. Proceed with dilution, centrifugation, and seeding as described in Steps 5–7 of the water bath protocol. The dry system eliminates the need for drying wet straws [47].
Workflow Visualization
The following diagram illustrates the key decision points and steps in the thawing process, applicable to both methods.
Diagram 1: Universal Cell Thawing Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Successful cell thawing relies on a suite of essential reagents and materials. The following table details key items and their functions in the post-thaw recovery process.
Table 3: Essential Research Reagent Solutions for Cell Thawing
| Item | Function & Application Notes |
|---|---|
| Complete Growth Medium | Pre-warmed to 37°C. Provides essential nutrients and serum for cell recovery post-thaw. The specific medium (e.g., IMDM, DMEM, RPMI-1640) is cell type-dependent [46] [18]. |
| Cryoprotectant Dilution Medium | Used for the initial dropwise dilution of thawed cells. Often serum-containing medium (e.g., with 10% FBS) or PBS with 2% FBS to stabilize cells and osmotically dilute DMSO [46] [18]. |
| DNase I Solution | Prevents cell clumping caused by DNA released from damaged cells during thawing. Added during the washing step (e.g., 100 µg/mL) [18]. |
| Dimethyl Sulfoxide (DMSO) | The most common penetrating cryoprotectant agent (CPA). Protects cells during freezing but must be thoroughly washed out post-thaw to prevent toxicity [49] [12]. |
| Serum (e.g., FBS) | A common component of freezing and recovery media. Provides proteins and growth factors that stabilize cell membranes and support cell attachment and growth [48] [18]. |
| Phosphate-Buffered Saline (PBS) | A balanced salt solution used for washing cells and for preparing dilution media. Versatile and isotonic for most mammalian cells [48] [18]. |
Post-Thaw Recovery Considerations
The thawing process itself is only the first step; ensuring cell recovery and functionality in the hours and days that follow is paramount. Research indicates that a 24-hour recovery period is often insufficient for a full return to baseline function. Studies on human bone marrow-derived mesenchymal stem cells (hBM-MSCs) show that while cell viability can recover within 24 hours, metabolic activity and adhesion potential may remain impaired beyond this point [48]. Furthermore, the negative impact of cryopreservation can extend to long-term attributes like colony-forming ability and differentiation potential, underscoring the need for comprehensive post-thaw assessment [48].
The following diagram outlines the key factors and checkpoints for evaluating post-thaw recovery.
Diagram 2: Post-Thaw Recovery Assessment Timeline
The selection of a thawing method is a critical step in the cold chain that significantly influences experimental outcomes and the efficacy of cell-based therapies. While the 37°C water bath remains a valid and widely used method, modern dry thawing systems present a compelling alternative with demonstrated advantages in post-thaw cell quality, operational consistency, and reduced contamination risk [47].
The choice between methods should be guided by a comprehensive consideration of the application's requirements. For routine laboratory work with robust cell lines, a properly executed water bath protocol may suffice. However, for sensitive primary cells, stem cells, or in settings where reproducibility, portability, and sterility are paramount—such as in clinical-grade drug development and cell therapy manufacturing—dry thawing systems offer a superior and more controlled solution. By adopting optimized and validated thawing protocols, researchers and developers can significantly enhance cell recovery, ensure data integrity, and advance the reliability of their biological products.
Within the broader context of optimizing cell freezing and thawing protocols, the post-thaw phase presents critical challenges that can significantly undermine cell viability and functionality. The rapid dilution of cryoprotective agents (CPAs), particularly dimethyl sulfoxide (DMSO), induces severe osmotic stress that can trigger apoptosis and mechanical cell damage [50]. Simultaneously, the inherent cytotoxicity of DMSO becomes increasingly problematic as temperatures rise, creating a delicate balance between removing toxic compounds and maintaining osmotic equilibrium [51]. This application note synthesizes current evidence and provides detailed protocols for implementing dilution strategies that minimize these dual threats, ensuring maximal post-thaw cell recovery for research and therapeutic applications.
Theoretical Foundations of Osmotic Injury
Mechanisms of Osmotic Shock
During cryopreservation, cells undergo profound volumetric changes as water and permeating CPAs move across the membrane according to osmotic gradients. The return to isotonic conditions after thawing must be carefully managed to prevent two distinct damage mechanisms:
- Cell Swelling and Lysis: Rapid dilution creates a steep osmotic gradient where water influx dramatically outpaces CPA efflux. This causes cells to swell beyond their volumetric tolerance, potentially resulting in membrane rupture [50] [4]. The excessive cell expansion during the thawing process is a primary contributor to immediate post-thaw mortality.
- Metabolic Disruption: Even without physical rupture, the dramatic volumetric fluctuations can disrupt cytoskeletal organization, organelle positioning, and critical metabolic processes. This sub-lethal damage may manifest as reduced attachment efficiency, delayed proliferation, or impaired functionality in downstream applications [12].
DMSO Cytotoxicity Considerations
While DMSO provides essential cryoprotection, its dose-dependent toxicity becomes particularly problematic during post-thaw handling. Evidence indicates that DMSO exposure should be limited to <30 minutes post-thaw whenever possible, as prolonged contact at elevated temperatures significantly compromises cell viability and function [51]. This creates a complex optimization challenge where practitioners must rapidly reduce DMSO concentration while simultaneously avoiding the osmotic consequences of abrupt concentration changes.
Table 1: Comparative Analysis of Dilution Method Efficacy Across Cell Types
| Cell Type | Dilution Method | CPA Concentration | Viability Outcome | Functional Assessment | Reference Model |
|---|---|---|---|---|---|
| Bovine Spermatozoa | Slow (multi-step) | 7% Glycerol | Significantly higher membrane integrity | Improved HOS test reactivity | [52] |
| Bovine Spermatozoa | Rapid (single-step) | 7% Glycerol | Increased coiled tails indicating damage | Reduced motility over incubation | [52] |
| Cord Blood HPCs | Washout (centrifugation) | 10% DMSO | Superior viability maintained >1h post-thaw | Improved hematopoietic function | [51] |
| Cord Blood HPCs | Dilution only | 10% DMSO | Declining viability after thawing | Reduced progenitor function | [51] |
| HepG2 Cells | Microfluidic control | 1,2-propanediol + Trehalose | 25% higher viability vs. conventional | Maintained metabolic activity | [50] |
Dilution Methodologies: Experimental Protocols
Slow Multi-Step Dilution Protocol
The slow, multi-step dilution method is particularly recommended for sensitive primary cells, stem cells, and any samples cryopreserved with CPA concentrations exceeding 5% [53] [12]. This approach gradually reduces extracellular osmolarity, allowing controlled water influx and CPA efflux that minimizes membrane stress.
Materials Required:
- Pre-warmed complete culture medium (37°C)
- Ice-cold basal medium or PBS with 2% FBS (4°C)
- 50 mL conical centrifuge tubes
- Serological pipettes
- Centrifuge with temperature control
- Automated cell counter or hemocytometer
Procedure:
- Immediately after thawing, transfer the cell suspension to a 50 mL conical tube containing 1 mL of pre-warmed culture medium.
- Gently agitate the tube to ensure initial mixing.
- Every 2 minutes, add equal volumes of pre-warmed medium, mixing gently after each addition until a minimum 1:10 dilution factor is achieved.
- Centrifuge the diluted suspension at 300 × g for 10 minutes at room temperature.
- Carefully aspirate the supernatant without disturbing the pellet.
- Resuspend cells in an appropriate volume of complete medium for counting and downstream applications.
Validation Points:
- Viability Assessment: Compare pre- and post-wash viability using trypan blue exclusion or flow cytometry with viability dyes.
- Functionality Testing: For stem cells, perform colony-forming unit assays; for immune cells, evaluate cytokine production or proliferation capacity.
Microfluidic Dilution Approach
Microfluidic technology represents a sophisticated alternative for minimizing osmotic shock by creating precisely controlled concentration gradients during CPA removal [50]. This method enables continuous processing where cells experience a gradual linear decrease in CPA concentration rather than step changes.
Experimental Setup:
- Fabricate PDMS microfluidic channels using soft lithography techniques [50].
- Bond channels to glass slides using oxygen plasma treatment.
- Connect syringe pumps for controlled injection of cell suspension and dilution medium.
- Design channel geometry to optimize laminar flow and diffusion-based mixing.
Protocol Parameters:
- Flow Rate: 0.5-5 μL/min depending on channel dimensions
- Temperature: Maintain at 4°C throughout process to reduce DMSO toxicity
- Dilution Gradient: Linear decrease from initial CPA concentration to <0.5%
- Collection: Directly into pre-cooled collection tubes
Performance Metrics:
- Post-thaw viability improvements of up to 25% over conventional methods [50]
- Reduced inter-technician variability in cell recovery
- Maintenance of metabolic activity and proliferative capacity
Centrifugation-Based Washout Method
For cell types tolerant of mechanical processing, centrifugation provides an effective means of rapidly removing DMSO while controlling osmotic conditions.
Protocol Variations Based on Cell Type:
- Standard Wash Protocol:
- Dilute thawed cell suspension 1:5 with ice-cold medium containing 2-5% FBS
- Centrifuge at 300 × g for 10 minutes at 4°C
- Aspirate supernatant and resuspend in fresh medium
- Repeat centrifugation if necessary for specific applications
- Dextran-40 Albumin Solution Method (for hematopoietic cells):
Table 2: DMSO Toxicity Timeline and Management Strategies
| Time Post-Thaw | Toxic Effects | Recommended Action | Cell Type Evidence |
|---|---|---|---|
| <30 minutes | Minimal toxicity | Optimal window for dilution | Cord blood HPCs [51] |
| 30-60 minutes | Moderate metabolic disruption | Immediate processing critical | iPSCs [12] |
| >60 minutes | Significant viability loss | Consider specialized rescue protocols | Primary hepatocytes |
| >2 hours | Extensive apoptosis/necrosis | Expect substantial cell loss | Most primary cell types |
Practical Implementation Guide
Decision Framework for Dilution Strategy Selection
The following workflow diagram illustrates the critical decision points for selecting an appropriate dilution strategy based on cell type and experimental constraints:
The Scientist's Toolkit: Essential Reagents and Equipment
Table 3: Key Research Reagent Solutions for Post-Thaw Processing
| Reagent/Equipment | Function | Application Notes | Evidence |
|---|---|---|---|
| Cell culture-grade DMSO | Cryoprotectant | Use at 5-10% final concentration; limit exposure time | [4] [55] |
| Trehalose | Non-permeating CPA | Provides extracellular protection; reduces required DMSO | [50] [4] |
| Dextran-40 with albumin | Wash solution medium | Reduces osmotic stress during centrifugation; for HSCs | [54] |
| DNase I Solution | Prevents clumping | Add 100 μg/mL when cell aggregation occurs post-thaw | [18] |
| Controlled-rate freezer | Temperature management | Ensures consistent cooling rates; improves reproducibility | [12] |
| Microfluidic devices | Precision dilution | Enables gradual CPA removal; minimizes osmotic shock | [50] |
| ThawSTAR CFT2 | Automated thawing | Standardizes thaw rate; reduces technician variability | [18] |
Effective management of post-thaw osmotic stress and DMSO toxicity requires a nuanced approach tailored to specific cell types and experimental requirements. The protocols and data presented herein demonstrate that gradual dilution strategies—whether through multi-step manual methods or advanced microfluidic systems—significantly improve cell recovery by maintaining membrane integrity during the critical transition from cryopreservation to culture conditions. As cryopreservation continues to enable advanced therapeutic applications including stem cell therapies and regenerative medicine, optimized post-thaw handling protocols will remain essential for maximizing cell viability, functionality, and experimental reproducibility.
Solving Common Cryopreservation Challenges: A Guide to Maximizing Viability and Recovery
Achieving high cell viability and functionality after thawing is a critical, yet often challenging, prerequisite for successful research and clinical applications in cell biology and therapy development. The process of cryopreservation subjects living cells to profound physical and chemical stresses. Poor post-thaw outcomes—characterized by low viability, reduced attachment, and diminished function—can derail experiments, compromise drug screening data, and invalidate cell therapy products. This application note systematically addresses the primary factors influencing post-thaw success, focusing on three key investigative areas: the original cell source, the freezing rate, and the conditions of storage. By providing structured diagnostic workflows and detailed experimental protocols, we aim to equip researchers with the tools to identify and rectify the most common failure points in the cryopreservation cascade.
Critical Factors Affecting Post-Thaw Viability
Cell Source and Pre-Freeze Status
The initial quality and handling of the cell culture destined for cryopreservation fundamentally determine its potential to survive freezing and thawing.
- Cell Health and Confluency: Cells should be harvested during their maximum growth phase (log phase) and typically at greater than 80% confluency to ensure optimal recovery [13]. Cells in senescence or decline phase exhibit reduced metabolic activity and are more susceptible to cryo-injuries.
- Microbial Contamination: Undetected contamination, particularly by mycoplasma, can catastrophically reduce post-thaw viability and poses a risk of contaminating other cell stocks [13] [56]. Comprehensive testing for bacteria, fungi, and mycoplasma is essential before banking.
- Genetic Stability: Continuous passaging can lead to genetic drift, which may not only alter the cell's characteristics but also its resilience to cryopreservation stresses. Freezing cells at the lowest possible passage number is recommended [13].
Freezing Rate and Cryoprotectant Toxicity
The rate of temperature descent and the choice of cryoprotective agents (CPAs) are arguably the most technically nuanced aspects of cryopreservation.
- Cooling Rate: A controlled, slow cooling rate of approximately -1°C/minute is considered ideal for a wide range of mammalian cells [13] [1] [4]. This rate allows sufficient time for water to exit the cell, minimizing lethal intracellular ice formation [57] [4]. Excessively slow cooling can expose cells to hypertonic solutions for too long, while overly rapid cooling causes intracellular ice crystals.
- Cryoprotectant Toxicity: While Dimethyl Sulfoxide (DMSO) is the most common penetrating CPA, it is cytotoxic. Exposure of cells to DMSO-containing freezing media at room temperature for more than 10 minutes before freezing can significantly harm viability [1]. The osmotic shock during the addition and removal of CPAs is another major source of cell death [58] [56].
Storage and Thawing Inconsistencies
Failures can occur after the freezing process itself, during storage or at the moment of thawing.
- Storage Temperature Fluctuations: Long-term storage should be at -135°C to -196°C (vapor or liquid phase of nitrogen) to halt all metabolic activity [13] [58]. Storage at -80°C is acceptable only for the short term (less than one month), as transient warming events from freezer door openings can cause ice recrystallization and accelerate cell degradation [13] [58].
- Suboptimal Thawing: The fundamental rule for thawing is "rapid warming and slow freezing" [13]. Slow thawing increases the time cells are exposed to high solute concentrations and allows small, intracellular ice crystals to recrystallize into larger, more damaging ones [1]. Rapid thawing in a 37°C water bath is standard practice.
Table 1: Troubleshooting Guide for Poor Post-Thaw Viability
| Observed Problem | Potential Cause | Diagnostic Experiments | Proposed Solution |
|---|---|---|---|
| Low viability immediately post-thaw | Cryoprotectant toxicity; Intracellular ice formation | Test different DMSO concentrations (5-15%); Compare cooling rates | Reduce DMSO exposure time; Optimize cooling rate toward -1°C/min [1] [4] |
| Poor cell attachment & spreading | Osmotic shock during thawing; Cell damage during pre-freeze handling | Vary post-thaw dilution media (osmolarity); Check pre-freeze viability | Use step-wise CPA removal; Ensure cells are >80% confluent and in log phase pre-freeze [13] [58] |
| High variability between vials | Inconsistent freezing rate; Improper vial storage | Record storage location/temperature history; Validate freezer performance | Use controlled-rate freezer; Store vials in liquid nitrogen vapor phase [13] [58] |
| Loss of specific cell function | Cell-specific sensitivity; Unoptimized cryomedium | Perform functional assays post-thaw; Test specialized, serum-free media | Adopt cell-specific freezing protocols; Use defined, commercial cryomedium [59] [4] |
Experimental Protocols for Diagnosis and Optimization
Protocol: Systematic Freezing Rate Optimization
Objective: To empirically determine the optimal cooling rate for a specific cell type, thereby minimizing intracellular ice formation and solute effects.
Materials:
- Healthy, log-phase cells
- Standard cryopreservation medium (e.g., 90% FBS + 10% DMSO)
- Cryovials
- Controlled-rate freezer (or passive cooling device like CoolCell)
- Liquid nitrogen storage tank
Method:
- Prepare a single, large batch of cells and aliquot into cryovials as per standard procedure.
- Divide the vials into several groups. Subject each group to a different cooling rate. A suggested range is -0.3°C/min, -1°C/min, -3°C/min, and -10°C/min [56] [4].
- Use a controlled-rate freezer for precise control. If using passive devices, note that they are typically designed for a rate of ~-1°C/min at -80°C.
- After freezing, transfer all vials to liquid nitrogen for storage for at least 24 hours.
- Thaw all vials rapidly in a 37°C water bath using a consistent technique.
- Assess post-thaw viability using a dye exclusion method (e.g., Trypan Blue) and a more sensitive assay of health, such as ATP-based viability testing [58], at 0 hours and 24 hours post-thaw to capture delayed-onset cell death.
- The cooling rate yielding the highest viability and functional recovery is optimal for that cell type.
Protocol: Assessing and Mitigating Cryoprotectant Toxicity
Objective: To evaluate the impact of DMSO exposure time and concentration on post-thaw viability and function.
Materials:
- Healthy, log-phase cells
- Basal medium (e.g., culture medium without serum)
- DMSO
- Centrifuge
Method:
- Prepare two freezing media: one with 10% DMSO and another with a lower concentration (e.g., 5-7%) supplemented with a non-penetrating CPA like sucrose or trehalose to maintain osmolarity [4].
- Harvest and concentrate the cells. Divide them into aliquots for each freezing medium condition.
- For each medium, further divide cells into groups with different exposure times (e.g., 1, 5, 10, and 15 minutes at room temperature) before initiating freezing.
- Freeze all samples using the standard (or newly optimized) cooling rate.
- After storage and thawing, measure viability and a key cellular function (e.g., metabolic activity, attachment efficiency, or lineage-specific differentiation potential).
- The data will identify the maximum tolerable DMSO concentration and exposure time for the cells.
The following workflow outlines the logical process for diagnosing the root cause of poor post-thaw viability and guides the researcher toward the appropriate corrective experimental protocols.
The Scientist's Toolkit: Key Reagent Solutions
Selecting the appropriate reagents is fundamental to standardizing and improving cryopreservation outcomes. The transition from lab-made formulations to defined, commercial media can significantly enhance reproducibility, especially for clinical applications.
Table 2: Essential Reagents for Cryopreservation Optimization
| Reagent Category | Specific Examples | Function & Rationale | Application Notes |
|---|---|---|---|
| Defined Cryopreservation Media | CryoStor [13], CELLBANKER [60] | Serum-free, GMP-manufactured solutions designed to minimize cryopreservation-induced apoptosis and provide a consistent, defined environment. | Reduces lot-to-lot variability and safety concerns associated with FBS. Ideal for regulated cell therapy workflows [13] [61]. |
| Cell-Type Specific Media | mFreSR (for ES/iPS cells) [13], MesenCult-ACF (for MSCs) [13] | Formulated to address the unique biological and physical needs of sensitive stem cell types, improving recovery of pluripotent/multipotent state. | Crucial for maintaining the functionality and differentiation potential of stem cells post-thaw [13] [56]. |
| Penetrating Cryoprotectants | Dimethyl Sulfoxide (DMSO), Glycerol [60] [4] | Lowers the freezing point of water, facilitates vitrification, and reduces intracellular ice crystal formation by penetrating the cell. | DMSO is most common but cytotoxic; use at 5-10%. Glycerol is an alternative for DMSO-sensitive cells [1] [4]. |
| Non-Penetrating Cryoprotectants | Sucrose, Trehalose, Hydroxyethyl Starch [60] [4] | Increases extracellular osmolarity, promoting gentle cell dehydration. Helps stabilize cell membranes and reduces the required concentration of toxic penetrating CPAs. | Trehalose is a natural cryoprotectant in freeze-tolerant organisms. Useful in vitrification mixtures [60] [4]. |
| Viability Assay Kits | ATP-based Luminescence Kits, Flow Cytometry Apoptosis Kits | Provides a more sensitive and quantitative measure of cell health and function compared to simple dye exclusion, detecting early apoptosis and metabolic capacity. | Essential for identifying delayed-onset cell death, which can occur 24+ hours post-thaw [58]. |
Diagnosing the root cause of poor post-thaw viability requires a methodical approach that scrutinizes each stage of the cryopreservation workflow. As detailed in this application note, researchers must systematically investigate the triumvirate of cell source, freezing rate, and storage conditions. By employing the diagnostic tables and optimized experimental protocols provided—such as empirically determining the ideal cooling rate and mitigating cryoprotectant toxicity—scientists can transition from troubleshooting failures to proactively designing robust preservation strategies. The adoption of defined, cell type-specific reagents further ensures consistency and quality. Ultimately, mastering these principles is indispensable for generating reliable research data and advancing the development of safe and effective cell-based therapeutics.
Within the critical field of advanced therapy medicinal products (ATMPs), cryopreservation serves as a indispensable process, enabling the long-term storage and viability of vital cell types for research and clinical applications [62] [63]. However, the "one-size-fits-all" approach to freezing and thawing is a primary cause of insufficient cell recovery and functionality, particularly for sensitive cell types like induced pluripotent stem cells (iPSCs), primary cells, and chimeric antigen receptor T-cells (CAR-Ts) [64] [65]. Optimizing cryopreservation protocols is therefore not merely a technical improvement but a fundamental requirement for ensuring the success of downstream experiments and therapies. This application note, framed within a broader thesis on cell freezing and thawing, provides a detailed, evidence-based guide for researchers and drug development professionals to tailor cryopreservation methodologies for these sensitive cells. We synthesize recent findings to present optimized protocols, quantitative data comparisons, and practical workflows designed to maximize post-thaw viability, recovery, and critical functionality.
Unique Cryopreservation Challenges by Cell Type
Sensitive cell types exhibit distinct biological characteristics that dictate specific vulnerabilities during the cryopreservation process. Understanding these differences is the first step toward effective protocol optimization.
Induced Pluripotent Stem Cells (iPSCs): iPSCs are particularly vulnerable to intracellular ice formation due to their large surface area-to-volume ratio [12]. The method of passaging—whether as single cells or aggregates—significantly impacts recovery. Frozen aggregates benefit from preserved cell-cell contacts, leading to faster post-thaw recovery, but suffer from variable cryoprotectant penetration. In contrast, single-cell suspensions allow for precise quality control but require more time to re-form colonies after thawing [12]. Furthermore, iPSCs are highly susceptible to osmotic shock during thawing, and their survival is critically dependent on being cryopreserved during the logarithmic growth phase to ensure maximum health and recovery potential [64] [12].
Primary Cells: Sourced directly from tissue, primary cells retain in vivo physiology but have limited in vitro expansion capacity, making every vial precious [65]. They are more fragile than immortalized lines and exhibit significant donor-to-donor variability, which can introduce batch-to-batch inconsistency [65]. A key challenge is avoiding cryoinjury, which encompasses not just ice crystal damage but also osmotic stress and toxicity from cryoprotective agents (CPAs) [65]. The success of primary cell cryopreservation is highly dependent on pre-freeze quality, requiring high initial viability (≥90%) and confirmation of a mycoplasma-free status [65].
CAR-T Cells and Other Therapeutic Lymphocytes: For cell-based therapeutics like CAR-T cells, the imperative extends beyond simple viability to preserving long-term therapeutic potency and effector function [66] [62]. Studies show that while cryopreserved CAR-T products can lead to complete clinical remissions, fresh products may exhibit higher in vitro anti-tumor reactivity and altered expression of key surface markers like TIM-3 [66]. A major logistical advantage is that cryopreservation of starting materials (e.g., leukapheresis products) decouples manufacturing from patient scheduling, creating a more flexible and resilient supply chain [67] [62]. The focus is on maintaining a high proportion of functional T-cells and critical quality attributes through a standardized freezing process.
Comparative Analysis of Optimal Cryopreservation Conditions
The table below summarizes the optimized cryopreservation parameters for iPSCs, primary cells, and CAR-T cells, based on analysis of recent research data. This provides a quick reference for key variables.
Table 1: Optimized Cryopreservation Parameters for Sensitive Cell Types
| Parameter | iPSCs | Primary Cells (e.g., HDFs) | CAR-T Cells / Leukapheresis |
|---|---|---|---|
| Preferred Cryoprotectant | 10% DMSO in specific freezing medium [12] | FBS + 10% DMSO [68] | CS10 (10% DMSO) or equivalent [67] |
| Cooling Rate | Controlled rate, ~ -1°C/min [12] [13] | Controlled rate, ~ -1°C/min [13] | Controlled rate, time-sensitive protocol (≤120 min to freezing initiation) [67] |
| Optimal Storage Duration | Indefinite at ≤ -135°C [12] | 0-6 months for highest attachment [68] | Long-term viable (years) [67] |
| Post-Thaw Viability Benchmark | Ready for experiments in 4-7 days [64] | >80% [68] | ≥90% [67] |
| Key Consideration | Freeze during log-phase growth as aggregates; prevent osmotic shock during thaw [64] [12] | Pre-freeze viability check (≥90%); use of defined cryomedium [68] [65] | Standardized, automated processing to ensure consistency and high T-cell proportion [67] |
The data reveals several critical trends. First, a controlled cooling rate of approximately -1°C per minute is a universal best practice, achievable via controlled-rate freezers or passive freezing containers [12] [13]. Second, while DMSO remains the dominant cryoprotectant, its specific formulation (e.g., with FBS or in defined commercial media like CryoStor) varies and impacts outcomes [68] [67] [13]. Finally, the definition of "success" differs: for iPSCs, it is timely return to a proliferative state; for primary cells, it is high attachment and viability; and for CAR-T cells, it is the retention of phenotypic profiles and cytotoxic potential [64] [68] [66].
Detailed Experimental Protocols
Optimized Protocol for iPSC Cryopreservation and Thawing
This protocol is designed for iPSCs maintained as aggregates on feeder-free, Matrigel-coated plates [64] [12].
Freezing Protocol:
- Pre-freeze Check: Confirm cells are healthy, in the logarithmic growth phase, and free from microbial contamination (e.g., mycoplasma) before harvesting [64] [13].
- Harvesting: Gently dissociate cells into small aggregates (clumps) using a gentle cell dissociation reagent. Avoid generating a single-cell suspension to preserve cell-cell contacts [12].
- Preparation: Centrifuge the aggregates and resuspend the pellet in a pre-cooled (4°C), DMSO-based freezing medium (e.g., commercial formulations like mFreSR or CryoStor CS10) [12] [13].
- Aliquoting: Quickly aliquot the cell suspension into cryovials at a density of 1x10^3 - 1x10^6 cells/mL [13].
- Controlled-Rate Freezing: Immediately transfer the vials to an isopropanol freezing container (e.g., Mr. Frosty) or a controlled-rate freezer. Place the container in a -80°C freezer for a minimum of 4 hours (or overnight) to ensure a consistent cooling rate of ~ -1°C/min [64] [13].
- Long-Term Storage: After 24 hours, promptly transfer the vials to the vapor phase of a liquid nitrogen tank (≤ -135°C) for long-term storage [12].
Thawing and Recovery Protocol:
- Rapid Thaw: Retrieve a vial from storage and immediately place it in a 37°C water bath with gentle agitation. Thaw quickly until only a small ice crystal remains [64] [13].
- Prevent Osmotic Shock: Gently transfer the thawed cell suspension to a centrifuge tube containing a large volume (e.g., 10 mL) of pre-warmed complete culture medium. This stepwise dilution is critical to gradually reduce the concentration of DMSO and prevent osmotic shock [64] [12].
- Centrifuge and Seed: Centrifuge the cell mixture at a low speed (e.g., 500-1000 x g for 5 minutes) to pellet the cells. Carefully remove the supernatant containing the residual cryoprotectant and resuspend the pellet in fresh, pre-warmed culture medium [64].
- Seed at High Density: Seed the cells as a dense suspension onto a Matrigel-coated plate with 10µM ROCK inhibitor to enhance cell attachment and survival [64].
- Medium Change: After 24 hours, replace the medium with fresh culture medium without ROCK inhibitor to support continued growth and colony formation.
Optimized Protocol for Primary Human Dermal Fibroblast (HDF) Cryopreservation
This protocol is based on comparative studies showing optimal results with FBS + 10% DMSO [68].
Freezing Protocol:
- Culture and Harvest: Culture HDFs until they are 70-80% confluent. Harvest the cells using standard trypsinization methods [68].
- Count and Centrifuge: Perform a cell count to confirm viability is ≥90%. Centrifuge the cell suspension and aspirate the supernatant [65].
- Resuspend in Cryomedium: Resuspend the cell pellet in freezing medium (FBS supplemented with 10% DMSO) at a concentration of ~1x10^6 cells/mL. Prepare the cryomedium fresh and add it to the cell pellet dropwise while gently swirling to ensure mixing [68] [65].
- Aliquot and Freeze: Aliquot the suspension into cryovials. Use a controlled-rate freezing container and place it in a -80°C freezer overnight [68] [13].
- Long-Term Storage: Transfer vials to liquid nitrogen for storage. Data suggests storage duration of 0-6 months yields the highest post-thaw attachment rates [68].
Thawing and Recovery Protocol (Direct vs. Indirect): Research indicates both direct and indirect revival methods can yield viability above 80% for HDFs, with nuanced differences [68].
- Direct Revival: Rapidly thaw the vial and directly seed the entire contents into a culture flask with pre-warmed growth medium. This method is faster and avoids the potential cell loss associated with centrifugation [68].
- Indirect Revival: Rapidly thaw the vial and transfer the cell suspension to a centrifuge tube containing warm medium. Centrifuge (e.g., 5000 rpm for 5 min) to remove the DMSO-containing supernatant before resuspending the pellet in fresh medium and seeding [68]. This method may show significantly higher expression of proliferation markers like Ki67 at longer storage times (e.g., 3 months) [68].
Key Protocol for Cryopreserved Leukapheresis in CAR-T Manufacturing
This protocol outlines the standardized process for using cryopreserved leukapheresis as starting material, which is critical for scalable CAR-T production [67].
Pre-processing and Cryopreservation:
- Centrifugation: Subject the leukapheresis product to a centrifugation step to reduce non-cellular impurities like residual red blood cells and platelets, which can impact post-thaw T-cell viability [67].
- Formulation: Resuspend the cell pellet in a clinical-grade cryoprotectant like CS10 (10% DMSO). The target cell concentration is ~5x10^7 cells/mL [67].
- Time-Sensitive Freezing: The interval from cryoprotectant addition to the initiation of controlled-rate freezing must be strictly limited to ≤ 120 minutes to prevent ice crystal formation [67].
- Controlled-Rate Freezing: Use a validated controlled-rate freezer to freeze the product. Store the bags in the vapor phase of liquid nitrogen [67].
Thawing and Recovery:
- Rapid Thaw: Thaw the leukapheresis bag quickly in a 37°C water bath [67].
- Gentle Handling: Transfer the contents to a larger volume of pre-warmed medium. Avoid harsh pipetting or vortexing to prevent damage to delicate immune cells [63].
- Dilution and Wash: Gently dilute and wash the cells to reduce the concentration of DMSO. Some protocols may include a rest period (overnight incubation) to allow cellular recovery before initiating the CAR-T manufacturing process [63].
Visualization of Workflows
The following diagrams illustrate the core logical workflows for optimizing cryopreservation and the specific thawing process for iPSCs, highlighting critical decision points.
Diagram 1: Critical iPSC thawing workflow to prevent osmotic shock.
Diagram 2: Logical workflow for tailoring cryopreservation protocols.
The Scientist's Toolkit: Essential Reagents and Materials
The table below lists key reagents and materials crucial for implementing the optimized protocols described in this note.
Table 2: Essential Research Reagent Solutions for Cryopreservation
| Reagent/Material | Function & Application | Examples & Notes |
|---|---|---|
| Cryoprotective Agents (CPAs) | Protect cells from ice crystal damage and osmotic stress. | DMSO: Standard penetrating CPA. Commercial Media (CryoStor CS10, mFreSR): Defined, serum-free formulations for specific cell types, ideal for regulated work [68] [13]. |
| Controlled-Rate Freezing Devices | Ensure consistent, optimal cooling rate (~ -1°C/min). | Isopropanol Containers (Mr. Frosty), CoolCell: Passive cooling devices for -80°C freezers. Programmable Freezers: Provide precise, customizable cooling profiles [12] [13]. |
| Cryogenic Storage Vials | Secure, sterile containers for long-term storage. | Use internally-threaded vials to prevent contamination when stored in liquid nitrogen [13]. |
| ROCK Inhibitor (Y-27632) | Enhances survival of single pluripotent stem cells and aggregates post-thaw by inhibiting apoptosis. | Add to culture medium for 24 hours after thawing iPSCs [64]. |
| Liquid Nitrogen Storage System | Provides long-term storage at ≤ -135°C to halt all metabolic activity. | Store in vapor phase to minimize risk of vial explosion and prevent warming above critical glass transition temperatures [12] [62]. |
The path to successful cryopreservation of sensitive cell types is one of deliberate customization. As this application note demonstrates, leveraging cell-type-specific insights—from the log-phase freezing of iPSCs and the validated cryomedium for primary fibroblasts to the time-sensitive processing of leukapheresis for CAR-T manufacturing—is fundamental to achieving high post-thaw viability and functionality. By adhering to the detailed protocols, data, and best practices outlined herein, researchers and clinicians can significantly enhance the reliability and reproducibility of their work with iPSCs, primary cells, and advanced therapeutics. This tailored approach ensures that these valuable cellular resources are not merely preserved, but are fully poised to drive successful research outcomes and clinical applications.
Within the critical field of cell freezing and thawing protocols, the integrity of research and the safety of drug development workflows depend on rigorous contamination control. The process of cryopreservation, while essential for the long-term storage of valuable cell lines and therapeutic products, introduces multiple vectors for potential compromise, from microbial ingress during handling to the physical dangers of ultra-low temperature storage. This application note provides a detailed framework for integrating aseptic laboratory techniques with safe liquid nitrogen storage practices to mitigate these risks. Adherence to the protocols and safety measures outlined herein is fundamental to ensuring cell viability, genetic stability, and the reproducibility of experimental and clinical outcomes in cell-based research and development.
Comprehensive Aseptic Technique in the Cell Culture Laboratory
Core Principles and Work Area Management
Aseptic technique is a collection of procedures designed to create a barrier between microorganisms in the environment and the sterile cell culture [69]. Its implementation is crucial to prevent biological contamination from bacteria, fungi, and viruses, which can sacrifice the integrity of an experiment, waste valuable resources, and lead to the loss of precious cell lines [69].
A major requirement is maintaining a dedicated, sterile work area, most commonly a laminar flow hood or biosafety cabinet [69]. Key practices include:
- Placement and Operation: The hood should be situated in an area free from drafts, doors, windows, and through traffic, and should be left running at all times, only being turned off for extended non-use periods [69].
- Surface Disinfection: The work surface must be uncluttered and thoroughly disinfected with 70% ethanol before and during work, especially after any spillage [69].
- Sterile Handling: Placing caps or covers face down on the work surface and ensuring all bottles, flasks, and plates are wiped with 70% ethanol before introduction to the hood are standard practices [69]. Using a Bunsen burner for flaming is not necessary nor recommended within a modern cell culture hood [69].
Personal Protective Equipment (PPE) and Hygiene
Personnel are a primary source of contamination. Proper PPE and hygiene form an immediate protective barrier [69] [70].
- Essential PPE: Lab coats or gowns, gloves, and safety glasses or a full-face visor are mandatory. For liquid nitrogen handling, thermally insulated cryogenic gloves extending up the forearm are required [71].
- Personal Hygiene: Researchers must wash hands before and after working with cultures. Long hair should be tied back, and one should avoid talking, singing, or whistling when performing sterile procedures [69].
Sterile Handling of Reagents and Cultures
- Liquid Handling: Always use a pipettor with sterile glass or disposable plastic pipettes. Each pipette should be used only once to avoid cross-contamination [69].
- Container Management: Always cap bottles and flasks after use and never leave sterile containers uncovered. Multi-well plates should be sealed with tape or stored in resealable bags [69].
- Reagent Sterility: Commercially prepared reagents and media undergo strict quality control, but they can become contaminated during handling. Always sterilize any lab-prepared solutions using the appropriate procedure and inspect reagents for cloudiness, unusual color, or foul smell before use [69].
Table: Aseptic Technique Checklist for Cell Culture Procedures
| Category | Checkpoint | Completed (Y/N) |
|---|---|---|
| Work Area | Work surface uncluttered and wiped with 70% ethanol. | |
| Cell culture hood is in a low-traffic area and running properly. | ||
| Personal Hygiene | Appropriate PPE (gloves, lab coat) is worn. | |
| Hands are washed; long hair is tied back. | ||
| Reagents & Media | Outside containers wiped with 70% ethanol. | |
| All containers are capped when not in use. | ||
| Reagents are inspected for signs of contamination. | ||
| Handling | Working slowly and deliberately. | |
| Using sterile pipettes only once. | ||
| Caps are placed face-down on the work surface. | ||
| Any spillage is mopped immediately with 70% ethanol. |
The following workflow diagram illustrates the logical sequence of actions for maintaining asepsis during routine cell culture handling, connecting pre-work preparation to specific actions and their contamination control objectives.
Safe Liquid Nitrogen Storage Practices
Hazards of Liquid Nitrogen and Essential Safety Protocols
Liquid nitrogen (LN2), used for long-term storage at -196°C, presents significant hazards that require strict safety protocols to ensure personnel safety and sample integrity [72] [71].
- Extreme Cold and Asphyxiation: LN2 can cause severe cryogenic burns upon contact with skin. Furthermore, as it evaporates, it expands rapidly (1 liter of LN2 produces ~700 liters of gas), displacing oxygen and creating a risk of asphyxiation in poorly ventilated areas [71].
- PPE and Ventilation: Essential PPE for handling LN2 includes a full-face visor, thermally insulated cryogenic gloves, a lab coat, and a splash-proof apron [71]. Work must be conducted in well-ventilated areas equipped with oxygen monitoring systems with alarms set to trigger at 18% oxygen concentration [71].
- The Two-Person Protocol and Training: Never work alone with liquid nitrogen. A two-person "buddy system" is critical, especially during sample transfers or refilling vessels, so one can respond in case of an emergency [71]. Comprehensive, documented training is mandatory for all personnel handling LN2 [71].
Cryogenic Storage and Sample Integrity
For long-term storage, samples must be held at temperatures below the glass transition point to halt all metabolic activity and prevent the damaging formation of intracellular ice crystals [12]. Storage in the vapor phase of liquid nitrogen (typically -150°C to -160°C) is a common practice that mitigates the risk of cross-contamination from liquid nitrogen potentially entering compromised vials, a risk associated with liquid phase storage [12].
Table: Liquid Nitrogen Safety & Storage Overview
| Aspect | Key Parameter | Protocol/Specification |
|---|---|---|
| Personal Protective Equipment (PPE) | Gloves | Thermally insulated, forearm-length |
| Eye/Face Protection | Full-face visor | |
| Body Protection | Lab coat, splash-proof apron | |
| Ventilation & Monitoring | Oxygen Monitor Alarm | Set at 18% O₂ |
| Ventilation Type | Mechanical ventilation system | |
| Personnel Protocols | Buddy System | Mandatory two-person rule |
| Training | Comprehensive, documented mandatory training | |
| Sample Storage | Long-term Temperature | ≤ -135°C (vapor phase LN2 or -150°C freezers) |
| Storage Method | Vapor phase recommended to prevent cross-contamination |
The following diagram outlines the decision-making process and key actions for implementing secure liquid nitrogen storage, from risk assessment to emergency response.
Integrated Protocols for Cryopreservation and Thawing
Cryopreservation Protocol: A Step-by-Step Guide
The following protocol is a generalized guide for freezing cells as cell aggregates or single cells. The goal is a slow, controlled freezing rate of approximately -1°C/minute to minimize intracellular ice crystal formation and cellular dehydration [13] [12].
- Harvesting: Harvest cells during their maximum growth phase (log phase), ideally at >80% confluency, and ensure they are free from microbial contamination [13] [12].
- Centrifugation: Centrifuge the cell suspension to pellet the cells. Carefully remove the supernatant [13].
- Resuspension in Freezing Medium: Resuspend the cell pellet in an appropriate, sterile freezing medium. A common formulation is culture medium containing 10% Dimethyl Sulfoxide (DMSO) as a cryoprotectant, although defined, serum-free commercial media (e.g., CryoStor CS10) are recommended for regulated work [13] [4]. The optimal cell concentration is typically 1x10^3 to 1x10^6 cells/mL [13].
- Aliquoting: Aseptically aliquot the cell suspension into labeled, sterile cryogenic vials. Internal-threaded vials are preferred to prevent contamination [13].
- Controlled-Rate Freezing: Place the cryogenic vials in an isopropanol freezing container (e.g., Nalgene Mr. Frosty) or an isopropanol-free container (e.g., Corning CoolCell) and immediately transfer it to a -80°C freezer for 18-24 hours. This provides the necessary cooling rate [13].
- Long-Term Storage: After 24 hours, promptly transfer the vials to long-term storage in a liquid nitrogen tank, either in the vapor phase (-135°C to -196°C) or the liquid phase (-196°C) [13]. Vapor phase storage is often recommended to prevent cross-contamination [12].
Thawing Protocol: A Step-by-Step Guide
The fundamental rule for thawing is "rapid thawing and slow freezing." Rapid thawing minimizes exposure to the damaging effects of cryoprotectant solutes and reduces damage from ice recrystallization [13] [73].
- Rapid Thaw: Remove the vial from liquid nitrogen storage and immediately swirl it in a 37°C water bath until only a small ice crystal remains (~60-90 seconds). Do not submerge the vial's cap [73].
- Decontaminate Vial: Wipe the outside of the vial thoroughly with 70% ethanol to prevent contamination ingress [69] [73].
- Transfer and Dilute: Quickly transfer the cell suspension to a sterile tube containing a large volume (e.g., 10 mL) of pre-warmed thaw medium or complete culture medium. To further minimize osmotic shock, the medium can be added dropwise to the cells [73].
- Centrifuge and Resuspend: Immediately centrifuge the cell suspension at a low speed (e.g., 200-300 x g for 5-10 minutes) to remove the DMSO-containing freezing medium. Carefully decant the supernatant and resuspend the cell pellet in fresh, pre-warmed culture medium [73].
- Culture: Transfer the resuspended cells to an appropriate culture vessel and incubate at 37°C in a 5% CO₂ incubator [73]. Cell attachment and viability can typically be assessed after 24 hours [73].
Troubleshooting Common Contamination and Viability Issues
Table: Common Cryopreservation Problems and Solutions
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Post-Thaw Viability | Suboptimal freezing rate | Use a controlled-rate freezer or validated freezing container [13] [74]. |
| Intracellular ice crystal formation | Ensure cryoprotectant (e.g., DMSO) is present and cells are frozen at -1°C/min [12] [4]. | |
| Microbial Contamination | Breach in aseptic technique during freezing/thawing | Strictly adhere to aseptic protocol; wipe vials with ethanol; work in a BSC [69] [13]. |
| Contaminated liquid nitrogen storage | Store vials in the vapor phase to prevent liquid ingress [12]. | |
| Osmotic Shock | Improper thawing/dilution technique | Rapidly thaw and use a large volume of pre-warmed medium; consider dropwise dilution [12] [73]. |
| Cell Clumping/ Low Yield | Freezing cells at too high a concentration | Optimize cell concentration for your specific cell type [13]. |
| Genetic Drift in Culture | Excessive passaging before freezing | Freeze cells at an early passage and during the log growth phase [13] [12]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for Cryopreservation
| Item | Function/Description | Example Uses |
|---|---|---|
| DMSO (Dimethyl Sulfoxide) | A permeating cryoprotectant agent (CPA) that penetrates cells, depresses the freezing point, and inhibits intracellular ice crystal formation [4]. | Standard cryoprotectant used at 5-10% concentration in freezing media for a wide range of cell types [13] [4]. |
| Defined Cryopreservation Media | Ready-to-use, serum-free media (e.g., CryoStor, mFreSR) providing a controlled, protective environment for freezing and thawing, often compliant with GMP standards [13]. | Essential for sensitive cells (e.g., iPSCs, MSCs) and regulated applications like cell therapy [13]. |
| Controlled-Rate Freezing Containers | Insulated containers (e.g., Nalgene Mr. Frosty, Corning CoolCell) that provide a consistent cooling rate of ~-1°C/min when placed in a -80°C freezer [13]. | Accessible and consistent method for slow freezing of cells without a programmable freezer [13]. |
| Cryogenic Vials | Sterile, leak-proof vials designed to withstand ultra-low temperatures of liquid nitrogen. Internal-threaded vials help prevent contamination [13]. | Safe containment and storage of all frozen cell suspensions. |
| Liquid Nitrogen Storage Systems | Tanks designed for secure storage of cryogenic vials at -135°C to -196°C in either the vapor or liquid phase [72] [71]. | Long-term preservation of cell banks for research and biobanking. |
The transition of advanced therapies from laboratory research to commercial manufacturing introduces profound cryopreservation challenges that extend far beyond the well-established protocols for preserving single vials of research-grade cells. While cryopreservation of cell suspensions is fundamentally successful, scaling up to the large volumes and high cell densities required for allogeneic (off-the-shelf) therapies creates a new paradigm where traditional approaches often fail [75] [76]. The growing cell and gene therapy market, projected to reach USD 96.99 billion by 2035, underscores the urgent industrial need for robust, scalable preservation methods [25].
The core of the challenge lies in the fact that processes optimized for single patient autologous doses do not translate effectively to batches producing tens of thousands of doses [76]. As scale increases, previously minor issues such as cryoprotectant (CPA) toxicity and inconsistent heat transfer become major obstacles to product viability and batch consistency [75] [76]. This application note delineates the principal scaling challenges and provides evidence-based strategies and protocols to overcome them, ensuring the transition from research to commercial manufacturing does not compromise product quality, viability, or therapeutic function.
Key Scaling Challenges and Underlying Principles
Scaling cryopreservation presents multi-faceted challenges that stem from fundamental biophysical and practical principles.
Physical and Biological Barriers
- Increased Diffusion Distances: In large volumes like cryobags or substantial tissue constructs, cells located further from the surface experience delayed exposure to CPAs during loading and to temperature changes during cooling and warming. This creates a heterogeneous population within the same batch, where central cells may be under-protected or experience different freezing kinetics [75].
- Thermal Mass and Heat Transfer: Large volumes have greater thermal mass, making precise control over cooling and warming rates more difficult. Inconsistent cooling can lead to zones of intracellular ice formation (from cooling too quickly) or excessive solute damage (from cooling too slowly) [77] [78].
- CPA Toxicity and Osmotic Stress: Equilibrating a large volume with a permeating CPA like DMSO requires time. Prolonged exposure to liquid CPAs at non-frozen temperatures, necessary to ensure full penetration, can lead to significant toxicity [75] [77]. Conversely, rapid addition or removal of CPAs can cause severe osmotic shock, damaging or destroying cells.
Practical and Regulatory Hurdles
- Process Standardization and Reproducibility: The "gold standard" of 10% DMSO cooled at -1°C/min was developed for specific cell types in small volumes [76]. Its application to diverse, complex cell products (e.g., iPSC-derived NK cells, engineered CAR-T cells) and larger formats is often suboptimal, leading to high variability in post-thaw recovery and function [76].
- Container and Equipment Limitations: The shift from cryovials to cryobags alters the surface-to-volume ratio and heat transfer dynamics. Furthermore, the thick walls of GMP-compliant cryocontainers can further impede heat transfer [75]. Automated fill-finish processes for thousands of vials can extend the room-temperature hold time for cells in CPA, exacerbating toxicity [76].
Table 1: Summary of Primary Scaling Challenges and Their Impacts
| Challenge | Impact on Large Batches | Consequence for Product |
|---|---|---|
| Non-uniform CPA Exposure [75] | Inconsistent protection across the batch | Varying post-thaw viability and function; loss of critical cell subsets |
| Inconsistent Cooling/Warming [78] | Zones of intracellular ice or excessive dehydration | Reduced overall cell recovery and viability |
| Amplified CPA Toxicity [75] [76] | Cumulative damage during fill-finish and equilibration | Loss of cell function, induction of apoptosis, impaired engraftment |
| Container-Driven Limitations [75] | Altered freezing kinetics compared to lab-scale vials | Failure of protocols that were successful at small scale |
Scalable Protocol for Cryopreserving Cell Therapy Products
The following protocol is designed for the cryopreservation of large-volume cell suspensions, such as a harvest from a bioreactor, into multiple cryobags or a single large container. It emphasizes control and scalability, building on foundational principles [5] [13] and incorporating strategies to address scaling challenges [79] [78].
Pre-Freeze Preparation and Optimization
Cell Health and Quality Control:
- Harvest cells during the logarithmic growth phase (e.g., >80% confluency for adherent cells) to ensure maximum health and recovery potential [5].
- Perform thorough pre-freeze analysis: cell count, viability assessment (e.g., Trypan Blue exclusion), and sterility/mycoplasma testing [5] [13]. For therapy-critical functions, include a potency assay.
Cryopreservation Media Selection:
- Use a chemically-defined, serum-free cryopreservation medium (e.g., CryoStor CS10) [13]. This eliminates lot-to-lot variability and regulatory concerns associated with fetal bovine serum (FBS).
- For large batches, empirically determine the lowest effective concentration of DMSO (e.g., 5-10%) to mitigate toxicity during extended processing [76].
Container Selection:
- Select GMP-grade, internally-threaded cryogenic vials or cryobags appropriate for the target volume. Pre-validate the fill volume to ensure optimal surface-to-volume ratio for freezing and thawing.
Controlled-Rate Freezing Process
Cell Concentration and Formulation:
- Centrifuge the harvested cell suspension and resuspend the pellet in pre-chilled (2-8°C) cryopreservation medium to the target concentration. For large batches, a typical range is 1x10^6 to 1x10^7 cells/mL [13]. Avoid excessively high concentrations to prevent cell clumping.
- Maintain the cell suspension on wet ice during the aliquoting process to minimize CPA toxicity [5].
Cooling Profile Optimization:
- Do not rely on passive cooling devices (e.g., Mr. Frosty) for critical large batches. Use a programmable controlled-rate freezer (CRF) [78] [13].
- A foundational cooling profile starts at -1°C/min from 4°C to -40°C, then at -5°C/min to -80°C or below [13]. However, this must be optimized for specific cell types.
- Controlled Ice Nucleation: To minimize supercooling and ensure consistent ice formation across the batch, initiate nucleation (seeding) in the CRF at the sample's freezing point (typically around -5° to -10°C).
Transfer to Long-Term Storage:
Rapid Thawing and Recovery
Rapid Thawing: Thaw the product quickly by immersing the container in a 37°C water bath with gentle agitation until only a small ice crystal remains [5] [13]. This minimizes damaging ice recrystallization.
Dilution and CPA Removal:
- Transfer the thawed contents immediately to a large volume (e.g., 10x the thawed volume) of pre-warmed, complete culture medium [5]. For sensitive cells, add the thawed cell suspension dropwise to the dilution medium to mitigate osmotic shock.
- Centrifuge at a gentle speed to pellet cells and remove the CPA-containing supernatant.
Post-Thaw Assessment:
- Resuspend the cell pellet in fresh culture medium and perform a viability count.
- Beyond simple viability, assess key functional attributes post-thaw, such as expansion potential, phenotype (e.g., CD3+ purity for T cells), differentiation status (e.g., Tn/Tcm proportions), and specific cytotoxic function for cell therapies [80].
The Scientist's Toolkit: Essential Reagents and Equipment
Successful scale-up requires carefully selected tools. The table below details key solutions for developing and implementing a robust large-batch cryopreservation process.
Table 2: Essential Toolkit for Scalable Cryopreservation R&D and GMP Manufacturing
| Tool Category | Example Products/Functions | Role in Scaling |
|---|---|---|
| Defined Cryomedium [13] | CryoStor, BloodStor | Provides a consistent, xeno-free environment; reduces batch variability and regulatory risk compared to lab-made FBS/DMSO mixes. |
| Programmable CRF System [78] | Grant Instruments CRFT, other controlled-rate freezers | Enables precise, reproducible cooling profile optimization at small scale, with direct translation to GMP-grade large-scale freezers. |
| GMP Cryocontainers [75] [13] | Cryobags, internal-threaded cryovials | Designed for large volumes and qualified for GMP processes; critical for ensuring container integrity and patient safety. |
| Automated Thawing | ThawSTAR and similar instruments | Standardizes the thawing process, removing user variability and ensuring consistent, rapid warming critical for large-batch recovery. |
| Automated Handling [79] | Automated fill-finish and CPA addition/removal systems | Reduces operator-dependent variability and processing time, mitigating CPA toxicity during large-batch production. |
Process Optimization and Future Directions
Moving beyond a one-size-fits-all approach is imperative for the next generation of advanced therapies.
Systematic Optimization via DoE
For each new cell product, key cryopreservation parameters must be systematically optimized using a Design of Experiment (DoE) approach [78]. This involves:
- Defining the Variable Space: Cooling rate (e.g., 0.5 to 5°C/min), thawing rate, CPA type and concentration (e.g., 5% to 15% DMSO).
- Selecting Key Metrics: Post-thaw viability, recovery yield, phenotype retention (e.g., stemness markers), and a relevant functional assay (e.g., cytotoxicity, cytokine secretion) [80].
- High-Throughput Screening: Using a platform like a CRFT system to test multiple conditions in parallel with small-volume samples [78].
- Data-Driven Refinement: Using statistical analysis to identify the optimal parameter set that maximizes the selected metrics.
Emerging Strategies and Innovations
- DMSO Reduction and Alternatives: Growing evidence of DMSO-related toxicity in patients and its impact on cell function is driving research into lower DMSO concentrations and DMSO-free formulations using alternative CPAs [76].
- Automation and Closed Systems: The implementation of automated, closed systems for CPA addition/removal, filling, and freezing is key to ensuring reproducibility, scalability, and compliance for allogeneic products [79] [76].
- Vitrification for Tissues: While challenging to scale, ice-free vitrification is a promising avenue for preserving more complex structures like tissue-engineered products and organoids, which are susceptible to damage from extracellular ice [75] [77].
Scaling cryopreservation for advanced therapy manufacturing is a critical, non-trivial endeavor that requires a deliberate and scientific approach. Success hinges on moving beyond empirical, small-scale methods to a fundamentally sound strategy that addresses the unique physical and practical challenges of large volumes and high cell densities. By leveraging defined reagents, precision-controlled equipment, automated systems, and a rigorous, data-driven optimization workflow, developers can create robust, scalable cryopreservation processes. This ensures that the transformative potential of cell and gene therapies is not lost in the transition from the research bench to the patient's bedside.
Evaluating Cryopreservation Success: Viability Assays, Protocol Comparisons, and Industry Trends
The success of cell-based research, clinical applications, and drug development hinges on the reliable cryopreservation and thawing of cellular material. A critical, and often overlooked, component of this process is rigorous post-thaw quality control (QC). Simply confirming cell viability immediately after thawing provides an incomplete and potentially misleading picture of cellular health. A comprehensive QC assessment must evaluate multiple parameters: initial viability, longer-term recovery, preserved specific functions (such as differentiation potential or effector functions), and, for stem cells, the undifferentiated state. This Application Note provides a detailed framework for a multi-faceted QC strategy, offering standardized protocols and analytical tools to ensure that cryopreserved cells meet the high standards required for reproducible and reliable scientific and therapeutic outcomes.
The Critical Pillars of Post-Thaw Assessment
A robust post-thaw QC protocol moves beyond a single time-point viability measurement. It is essential to recognize that cells can undergo delayed-onset apoptosis or experience functional impairment even with high initial viability [81]. Therefore, assessment should be structured around four key pillars, as illustrated in the workflow below.
Quantitative Assays for Viability and Recovery
Accurate quantification of cell survival and yield is the foundation of post-thaw QC. The assays in this section provide critical, quantifiable data for assessing the initial success of the cryopreservation protocol.
Table 1: Core Viability and Recovery Assays
| Assay | Measurement | Typical Output | Key Considerations |
|---|---|---|---|
| Trypan Blue Exclusion [82] [18] | Membrane integrity (immediate viability) | Viability (%) | Quick and inexpensive; can overestimate viability if measured only immediately post-thaw [81]. |
| Flow Cytometry with Viability Dyes (e.g., 7-AAD, AO/PI) [83] | Membrane integrity within a phenotyped population | Viability of specific cell subsets (e.g., % live CD3+ T-cells) | Allows for viability gating on specific populations of interest in heterogeneous samples. |
| Total Cell Recovery Calculation [81] | Yield of live cells post-thaw | Absolute number of live cells recovered | Crucial for avoiding false positives; a sample can have high viability but very low recovery, making it practically useless [81]. |
| Post-Thaw Culture Growth [81] [12] | Recovery over time, apoptosis | Growth curve, confluence, population doubling time | Assesses delayed-onset apoptosis and the capacity for proliferation, providing a more realistic picture of functional recovery. |
Protocol: Standardized Viability and Total Recovery Assessment
This protocol combines trypan blue exclusion with cell counting to provide two essential metrics.
Materials:
Method:
- Thaw and Dilute: Rapidly thaw cells and dilute in pre-warmed medium [14]. To minimize DMSO toxicity, promptly proceed to the next step.
- Wash Cells: Centrifuge the cell suspension at 300 × g for 10 minutes. Carefully remove the supernatant containing the cryoprotectant [18].
- Resuspend and Count: Resuspend the cell pellet in a known volume of PBS with 2% FBS. Remove a 20 µL aliquot of the cell suspension for counting [18].
- Mix with Trypan Blue: Mix the 20 µL cell aliquot with 20 µL of 0.4% Trypan Blue solution (1:1 dilution) [18]. For lower cell numbers, cells can be diluted directly in 20 µL of Trypan Blue [18].
- Count and Calculate:
- Load the mixture onto a hemocytometer and count the clear (viable) and blue (non-viable) cells.
- Viability (%) = [Number of viable cells / (Number of viable + non-viable cells)] × 100.
- Total Cell Recovery = (Total number of viable cells post-thaw / Total number of viable cells frozen) × 100 [81].
Evaluating Cellular Functionality and Phenotype
For most applications, confirming that cells not only survive but also retain their intended biological function is paramount. This is especially critical for immune cells and stem cells.
Functional Assays for Immune Cells
Table 2: Functional Assays for Cryopreserved Immune Cells
| Cell Type | Functional Assay | Readout | Application Example |
|---|---|---|---|
| T-cells [83] | Activation/Stimulation | Cytokine production (e.g., IFN-γ, IL-2) via ELISA or flow cytometry. | QC for CAR-T cell products [83]. |
| Monocytes/Macrophages [82] | Differentiation Capacity | Induction with PMA; assessment of adherent, macrophage-like morphology and CD14/CD11b marker upregulation [82]. | Ensuring THP-1 monocytes can differentiate post-thaw for disease modeling [82]. |
| PBMCs [84] | Proliferative Response | Stimulation with mitogens (e.g., PHA); measurement of proliferation via dye dilution or metabolic activity. | Check for granulocyte contamination, which can suppress T-cell function [84]. |
Protocol: Post-Thaw Differentiation of THP-1 Monocytes into Macrophages
This protocol demonstrates how to verify the functional differentiation capacity of a key immune cell model after cryopreservation [82].
Materials:
- Thawed THP-1 monocytic cells
- RPMI 1640 medium supplemented with 10% FBS
- Phorbol 12-myristate 13-acetate (PMA)
- Tissue culture plates
- Flow cytometry antibodies against CD14 and CD11b
Method:
- Thaw and Recover: Thaw THP-1 cells and wash as described in Section 3.1. Culture the cells in standard growth medium for 24-48 hours to allow recovery.
- Induce Differentiation: Seed the recovered THP-1 cells into tissue culture plates. Treat with 50-100 ng/mL PMA for 48-72 hours.
- Assess Differentiation:
- Morphology: Observe under a microscope. Undifferentiated monocytes are round and non-adherent. Differentiated macrophages will become large, ameboid-shaped, and adherent to the plate [82].
- Surface Markers: Harvest cells and analyze by flow cytometry for the upregulation of macrophage-associated markers CD14 and CD11b. Successful differentiation should show a significant increase in the expression of these markers compared to non-induced controls, matching the profile of non-frozen cells [82].
Confirming Stemness in Pluripotent Stem Cells
For induced pluripotent stem cells (iPSCs) and other stem cells, a critical quality check is the preservation of "stemness"—the undifferentiated state and capacity to differentiate into multiple lineages. A combination of molecular and functional assays is required.
Table 3: Essential Assays for Verifying Stem Cell Pluripotency
| Assay Type | Target | Specific Method | Expected Outcome for Validated iPSCs |
|---|---|---|---|
| Molecular Analysis | Pluripotency Gene Expression | RT-qPCR for OCT4, SOX2, NANOG | High expression levels comparable to pre-freeze controls. |
| Protein Analysis | Pluripotency Marker Expression | Immunocytochemistry (ICC) for OCT4, SOX2, SSEA-4, TRA-1-60 | Strong nuclear (OCT4, SOX2) or surface (SSEA-4) staining in >90% of cells. |
| Functional Assay | In Vitro Differentiation | Embryoid Body (EB) formation & spontaneous differentiation | Capacity to form derivatives of all three germ layers (ectoderm, mesoderm, endoderm). |
Protocol: Immunocytochemical Analysis of Pluripotency Markers
This protocol allows for the visual confirmation of key pluripotency proteins in cultured iPSCs post-thaw.
Materials:
- Thawed and recovered iPSCs grown on Matrigel-coated coverslips
- 4% Paraformaldehyde (PFA) in PBS
- Permeabilization buffer (e.g., 0.1% Triton X-100 in PBS)
- Blocking buffer (e.g., 3% BSA in PBS)
- Primary antibodies: Anti-OCT4, Anti-SOX2, Anti-SSEA-4
- Fluorescently-labeled secondary antibodies
- DAPI nuclear stain
- Fluorescence microscope
Method:
- Culture and Fix: Culture thawed iPSCs for 3-5 days until they reach ~70% confluence. Fix cells with 4% PFA for 15 minutes at room temperature.
- Permeabilize and Block: Permeabilize cells with 0.1% Triton X-100 for 10 minutes, then incubate with blocking buffer for 1 hour to prevent non-specific antibody binding.
- Stain: Incubate with primary antibodies diluted in blocking buffer overnight at 4°C. Wash thoroughly with PBS, then incubate with appropriate secondary antibodies for 1 hour at room temperature in the dark.
- Counterstain and Image: Stain nuclei with DAPI for 5 minutes. After final washes, mount the coverslips and image using a fluorescence microscope. Analyze the percentage of cells positive for the pluripotency markers.
The Scientist's Toolkit: Essential Research Reagents
A successful post-thaw QC pipeline relies on a suite of reliable reagents and tools. The following table details key solutions required for the experiments described in this note.
Table 4: Research Reagent Solutions for Post-Thaw QC
| Reagent / Kit | Function | Application Example |
|---|---|---|
| Cryopreservation Medium (e.g., with DMSO, polyampholytes) [82] [14] | Protects cells from ice crystal damage and osmotic stress during freezing. | CryoStor CS10; or in-house formulations with 5-10% DMSO, with or without macromolecular cryoprotectants like polyampholytes [82] [85]. |
| Viability Stain (Trypan Blue, AO/PI, 7-AAD) [18] [83] | Distinguishes live cells (intact membranes) from dead cells (compromised membranes). | Initial post-thaw viability assessment; 7-AAD is used in flow cytometry to gate out dead cells [83]. |
| Flow Cytometry Antibody Panels | Identifies and characterizes specific cell populations based on surface and intracellular markers. | Confirming CD3+ T-cells in PBMCs [83]; checking CD14/CD11b upregulation in differentiated macrophages [82]. |
| Cell Stimulation Cocktails (e.g., PMA, PHA) | Activates cells to test their functional capacity post-thaw. | PMA for monocyte differentiation [82]; PHA for T-cell proliferation assays [84]. |
| Pluripotency Marker Antibody Panel (e.g., OCT4, SOX2, NANOG, SSEA-4) [86] | Detects key transcription factors and surface proteins indicative of an undifferentiated stem cell state. | Immunocytochemistry and flow cytometry analysis of thawed iPSCs to confirm stemness is retained. |
| Controlled-Rate Freezer / Passive Cooler (e.g., CoolCell) [82] [87] | Ensures a consistent, optimized freezing rate (typically -1°C/min), which is crucial for high viability. | Standardizing the freezing process across experiments to reduce variability and improve post-thaw outcomes. |
Within cell and gene therapy, vaccine production, and biobanking, the cryopreservation workflow is a critical path. The freezing method employed—controlled-rate freezing (CRF) or passive freezing (PF)—directly influences post-thaw cell viability, functionality, and process scalability. CRF, long considered the gold standard, uses programmable freezers to precisely lower sample temperature at a predetermined rate [88]. In contrast, PF, or uncontrolled-rate freezing, involves placing samples in an insulated container within a -80°C mechanical freezer, allowing a non-programmed cooling rate [89]. This application note provides a comparative analysis of both methodologies, framing them within a broader thesis on cell freezing and thawing protocol research. It is designed to equip researchers, scientists, and drug development professionals with structured quantitative data, detailed experimental protocols, and strategic guidance for method selection.
Comparative Performance Data
The choice between CRF and PF involves trade-offs between cell viability, process consistency, and resource allocation. The following table synthesizes key comparative data from recent studies.
Table 1: Comparative Analysis of Controlled-Rate Freezing and Passive Freezing
| Parameter | Controlled-Rate Freezing (CRF) | Passive Freezing (PF) |
|---|---|---|
| Cooling Rate Control | Precise, programmable profiles (e.g., -0.3°C/min to -1.8°C/min for iPSC) [12] | Uncontrolled, depends on insulator and freezer [89] |
| Typical TNC Viability (Post-Thaw) | 74.2% ± 9.9% (HPC study) [89] | 68.4% ± 9.4% (HPC study) [89] |
| Typical CD34+ Viability (Post-Thaw) | 77.1% ± 11.3% (HPC study) [89] | 78.5% ± 8.0% (HPC study) [89] |
| Neutrophil Engraftment (Days) | 12.4 ± 5.0 days (HPC study) [89] | 15.0 ± 7.7 days (HPC study) [89] |
| Platelet Engraftment (Days) | 21.5 ± 9.1 days (HPC study) [89] | 22.3 ± 22.8 days (HPC study) [89] |
| Key Advantage | Maximizes viability for sensitive cells (iPSC, oocytes); ensures lot-to-lot consistency; supports regulatory compliance [88] [12] | A cost-effective alternative for robust cell types like HPCs; simpler operation [89] |
| Primary Disadvantage | High capital equipment cost; requires more specialized training [88] | Higher outcome variability; not ideal for cells sensitive to intracellular ice [20] |
| Regulatory Support | Built-in functionality for GMP & 21 CFR Part 11 (e.g., data traceability, user access levels, electronic logs) [90] [91] | Limited inherent support; relies on manual documentation [90] |
Experimental Protocols
Protocol A: Controlled-Rate Freezing of Cell Suspensions in Vials
This protocol is optimized for sensitive cells such as induced Pluripotent Stem Cells (iPSCs) and is executable on devices like the Thermo Scientific CryoMed series [90] [91].
Principle: To minimize intracellular ice crystal formation and cellular dehydration by controlling the cooling rate through critical phase transition temperatures, thereby preserving cell viability and function [12] [20].
The Scientist's Toolkit: Table 2: Essential Reagents and Equipment for Controlled-Rate Freezing
| Item | Function |
|---|---|
| Programmable Controlled-Rate Freezer (e.g., CryoMed CRF) | Precisely controls cooling rate and manages exothermic heat release during phase change [90] [91]. |
| Cryoprotectant Agent (e.g., 10% DMSO) | Penetrates cells, reduces ice crystal formation, and mitigates osmotic shock [12]. |
| Type T Thermocouple | Provides real-time sample temperature monitoring for process validation [90] [91]. |
| Cryogenic Vials | Contain cell suspension for freezing and storage. |
Methodology:
- Preparation: Harvest and concentrate cells in a logarithmic growth phase. Resuspend the cell pellet in a pre-chilled freezing medium containing a cryoprotectant like 10% DMSO [12].
- Loading: Aseptically aliquot the cell suspension into cryovials. Instrument vials with pre-sterilized Type T thermocouples if sample temperature verification is required.
- Programming: Load a validated freezing profile. For many iPSCs, a rate of -1°C/min from +4°C to -40°C to -50°C is effective, followed by a faster ramp (e.g., -10°C/min) to -100°C [12]. The profile should account for the exothermic heat of fusion [20].
- Initiation: Place the instrumented vials in the CRF chamber and start the program.
- Transfer: Upon program completion, immediately transfer vials to a long-term storage system (liquid nitrogen vapor phase or -150°C freezer) to avoid exceeding critical glass transition temperatures [12].
Protocol B: Passive Freezing of Hematopoietic Progenitor Cells (HPCs)
This protocol validates PF as an acceptable method for initial cryopreservation of HPCs prior to long-term storage in liquid nitrogen [89].
Principle: To achieve a cooling rate slow enough to prevent significant intracellular ice formation in robust cell types using an insulated container in a -80°C freezer, providing a simpler and more cost-effective workflow.
The Scientist's Toolkit: Table 3: Essential Reagents and Equipment for Passive Freezing
| Item | Function |
|---|---|
| -80°C Mechanical Freezer | Provides the cold energy sink for the freezing process. |
| Passive Cooling Device (e.g., insulated container, "Mr. Frosty") | Insulates samples to achieve an approximate cooling rate of -1°C to -3°C/min. |
| Cryoprotectant Agent (e.g., DMSO) | Standard agent to protect cells during freezing and thawing. |
Methodology:
- Preparation: Mix the HPC product with a cryoprotectant solution per standard operating procedures.
- Loading: Aseptically fill cryobags or vials with the cell suspension.
- Freezing: Place the filled containers into a passive cooling device that has been pre-conditioned at room temperature. Immediately transfer the entire assembly into a -80°C mechanical freezer.
- Storage: Leave the samples in the freezer for a minimum of 24 hours before transferring them to long-term liquid nitrogen storage [89].
The decision-making process for selecting and optimizing a freezing method is summarized below.
The Impact of Thawing and Storage
The freezing process is only one component of the cold chain. Thawing rates and storage temperatures are equally critical for maintaining cell viability.
Thawing Protocols: The optimal thawing rate is often dependent on the freezing method. Cells frozen via CRF generally benefit from a slow thawing process (e.g., in a 37°C water bath with gentle agitation) to allow for proper rehydration and efflux of cryoprotectant. In contrast, rapid freezing often necessitates rapid thawing to prevent the growth of small, damaging intracellular ice crystals into larger, more destructive ones [20]. For iPSCs, rapid thawing and subsequent steps to prevent osmotic shock are crucial for good cell recovery [12].
Storage Considerations: For long-term storage of viable cells, temperatures below -130°C are required, as biological time effectively stops, preventing degenerative chemical reactions [20]. Storage in the vapor phase of liquid nitrogen (typically -150°C to -160°C) is standard practice to maintain temperatures below the critical extracellular glass transition temperature of -123°C [12].
Regulatory and Integration Considerations
For cell and gene therapy applications, regulatory compliance is paramount. Controlled-rate freezers designed for Good Manufacturing Practice (GMP) environments offer built-in features to support 21 CFR Part 11 requirements [90] [91]. These include:
- Three-level user access control to authorize personnel.
- Electronic audit trails for all freezing runs and system events.
- Data export capabilities (e.g., to USB as PDF) for complete traceability and audit readiness.
Integration with larger automation platforms and Laboratory Information Management Systems (LIMS) via standard protocols like Ethernet or Modbus is also a key capability of modern CRF systems, enhancing overall process control and data integrity [88].
Both controlled-rate and passive freezing have a defined place in modern biomedical research and production. CRF is the unequivocal choice for sensitive, high-value biologics like iPSCs, cell and gene therapies, and critical vaccines, where maximizing viability, ensuring lot-to-lot consistency, and meeting regulatory demands are non-negotiable [88] [90] [12]. For more robust cell types like hematopoietic progenitor cells, where a retrospective study found equivalent engraftment outcomes, passive freezing presents a scientifically valid and resource-efficient alternative [89]. The final decision must be rooted in a critical analysis of the target cell's biology, the required quality and regulatory thresholds, and the total cost of ownership.
Within the critical work of cell culture and biobanking, the thawing of cryopreserved cells is a fundamental yet high-risk procedure. The choice of thawing method directly impacts cell viability, functionality, and the integrity of subsequent experimental data. This application note provides a detailed comparative analysis of the two primary thawing methodologies—conventional water baths and modern dry thawing systems—framed within broader research on cryopreservation protocols. We focus on quantifying contamination risk and temperature consistency, two factors paramount to reproducible science and successful drug development. The protocols and data presented herein are designed to empower researchers in selecting and implementing the optimal thawing strategy for their specific cellular systems.
Background & Core Principles
The Imperative of Rapid Thawing: Unlike the controlled, slow rate required for freezing cells, the thawing process must be rapid. This minimizes the time cells spend in a transitional phase where damaging ice recrystallization can occur and reduces exposure to high concentrations of cryoprotectants like Dimethyl Sulfoxide (DMSO), which can become toxic upon warming [92] [93]. A swift transition from frozen to liquid state is therefore critical for high cell survival rates [12].
Thawing as a Source of Contamination: The thawing process is a vulnerability point for microbial contamination. Traditional water baths, with their warm, stagnant water, are an ideal breeding ground for bacteria and fungi [94] [95]. The risk is exacerbated when the watertight integrity of a cryovial cap is compromised, a phenomenon known as the "wicking effect," which can draw contaminated water into the vial [93].
Temperature Uniformity and Its Impact: Consistent and uniform heat application during thawing is essential. Inconsistent thawing can lead to localized hotspots, potentially denaturing sensitive proteins and compromising the functionality of biological products like Fresh Frozen Plasma (FFP) or delicate primary cells [96] [94]. Ensuring temperature homogeneity is thus a key metric for assessing thawing equipment.
Comparative Analysis: Water Bath vs. Dry Thawing
A systematic comparison of water bath and dry thawing technologies reveals critical differences in performance, risk, and operational efficiency.
Table 1: Key Feature Comparison between Water Bath and Dry Thawing Systems
| Feature | Water Bath | Dry Thawing System |
|---|---|---|
| Contamination Risk | High (direct contact with non-sterile water) [94] [95] | Very Low (closed, dry-thawing environment) [94] [93] |
| Temperature Uniformity | Good with agitation, but can have cold spots [97] | High (engineered for consistent heat transfer) [94] [95] |
| Thawing Speed | Fast (excellent thermal conductivity of water) [93] | Slightly slower, but highly controlled [93] |
| Process Standardization | Low (user-dependent monitoring) | High (programmable, automated cycles) [94] [95] |
| Maintenance Burden | High (regular cleaning, water replacement) [97] | Low (minimal daily upkeep) [94] |
| Throughput | Varies, can be high with large baths | Model-dependent, often designed for multiple simultaneous samples [94] |
Quantitative data reinforces these comparative features. A study on thawing Fresh Frozen Plasma (FFP) provides a direct, data-driven comparison of the two methods.
Table 2: Quantitative Comparison of Thawing Methods for Fresh Frozen Plasma (FFP) Based on a study comparing 37°C water bath vs. Plasmatherm II dry thawer at 45°C [95]
| Parameter | Water Bath | Dry Thawing System | P-value |
|---|---|---|---|
| Mean Thawing Time | 24.3 ± 2.35 minutes | 15 minutes | < 0.0001 |
| Bacterial Contamination | Mixed bacterial growth (e.g., Pseudomonas) observed in water samples | Sterile culture from device surfaces | N/A |
| Coagulation Factors | No significant difference in PT, aPTT, Fibrinogen, or Factor VIII activity between methods post-thaw | > 0.05 |
The data in Table 2 demonstrates that the dry thawing system offered a 36% faster thawing time while completely eliminating the microbial contamination risk associated with the water bath. Critically, both methods preserved the functional quality of the plasma proteins equally well, indicating that the faster, drier method does not compromise product integrity [95].
Detailed Experimental Protocols
Protocol A: Thawing Cells Using a Water Bath
This protocol outlines the standard procedure for thawing cryopreserved cells using a water bath, emphasizing steps to mitigate its inherent risks [18] [92].
Research Reagent Solutions & Materials
- Complete Growth Medium: Pre-warmed to 37°C. Provides essential nutrients for cell recovery.
- Phosphate-Buffered Saline (PBS) with 2% FBS: Used for washing cells to dilute cryoprotectant.
- 70% Ethanol: For decontamin vial exteriors.
- Water Bath: Calibrated and maintained at 37°C.
- Personal Protective Equipment (PPE): Lab coat, gloves, and safety goggles.
Procedure
- Preparation: Pre-warm the complete growth medium in the 37°C water bath. Prepare a centrifuge tube with 10-20 mL of warm medium or PBS with 2% FBS [18] [92].
- Retrieval: Remove the cryovial from liquid nitrogen storage. Handle vials from liquid-phase storage with caution due to explosion risks [92].
- Thawing: Immediately and partially submerge the cryovial in the 37°C water bath. Gently swirl the vial to ensure even thawing and to create convection currents. Keep the cap above the water level to prevent contamination via wicking [92] [93].
- Transfer: Once only a small ice crystal remains (typically 1-2 minutes), remove the vial from the bath and swiftly decontaminate its exterior with 70% ethanol [18] [92].
- Dilution & Washing: Transfer the cell suspension to the prepared centrifuge tube using a sterile pipette. Adding the medium dropwise while gently swirling the tube can help reduce osmotic shock [12].
- Centrifugation: Centrifuge the cell suspension at 200-300 x g for 5-10 minutes to pellet the cells and remove the cryoprotectant-containing supernatant [18] [92].
- Resuspension & Culture: Carefully aspirate the supernatant without disturbing the pellet. Gently resuspend the cells in fresh, pre-warmed complete growth medium and transfer to a culture vessel [92].
Protocol B: Thawing Cells Using a Dry Thawing System
This protocol describes the use of a dedicated dry thawing device, such as the ThawSTAR or a system using the Eppendorf SmartBlock, offering a sterile and consistent alternative [18] [93].
Research Reagent Solutions & Materials
- Complete Growth Medium: Pre-warmed to 37°C.
- Centrifuge Tubes, Serological Pipettes: Sterile, for handling cell suspensions.
- Dry Thawing Device: e.g., ThawSTAR CFT2 Automated Thawing System or Eppendorf ThermoMixer C with SmartBlock cryo thaw [18] [93].
Procedure
- Preparation: Pre-warm the complete growth medium. Place the dry thawing device inside the biosafety cabinet for a fully sterile workflow, if the device is disinfectable [93].
- Retrieval: Remove the cryovial from storage and place it directly into the dry thawing device's block.
- Thawing: Initiate the automated thawing cycle. The device will use conductive heating and often agitation to thaw the vial at a controlled, rapid rate without any liquid [18] [94].
- Completion: The device will signal (e.g., with an alarm) once thawing is complete, preventing overheating [95].
- Dilution & Washing: Proceed as in Protocol A, steps 5-7. Since the vial remains sterile throughout the thawing process, the risk of introducing contamination during transfer is minimized.
The following workflow diagram summarizes the decision-making process and key steps for both thawing methods.
The Scientist's Toolkit
The following table lists key reagents and equipment essential for successful cell thawing, detailing their critical functions in the protocol.
Table 3: Essential Research Reagent Solutions and Materials for Cell Thawing
| Item | Function & Importance |
|---|---|
| Cryoprotective Agent (CPA)(e.g., DMSO) | Permeates cells, depresses freezing point, and inhibits lethal intracellular ice crystal formation during freezing [4] [12]. |
| Complete Growth Medium | Pre-warmed medium provides immediate nutrients and a familiar environment for cells to recover from the stressful thawing process [92]. |
| Serum (e.g., FBS) | Added to medium; provides proteins, growth factors, and other undefined components that support cell attachment and proliferation post-thaw. |
| DNase I Solution | Added if cells clump post-thaw; degrades DNA released from dead cells, which can trap live cells and reduce recovery [18]. |
| Water Bath or Dry Thawing Device | Provides the controlled, rapid heat source required for thawing. The choice directly impacts contamination risk and process consistency [97] [93]. |
| Hemocytometer & Viability Stain(e.g., Trypan Blue) | Allows for accurate cell counting and viability assessment immediately after thawing, which is critical for determining thaw success and seeding density [18]. |
The transition from traditional water baths to controlled dry thawing systems represents a significant advancement in laboratory practice for cell freezing and thawing research. While water baths offer rapid heating and low initial cost, their high contamination risk and variable process control pose substantial threats to experimental reproducibility and valuable biological samples. Dry thawing technology effectively addresses these shortcomings by providing a sterile, standardized, and efficient thawing environment, as evidenced by quantitative data showing faster processing times and elimination of microbial contaminants. For researchers and drug development professionals requiring the highest standards of data integrity, sample security, and operational reliability, investing in dry thawing systems is a scientifically justified and strategically sound decision.
Within the rapidly advancing field of cell and gene therapy, cryopreservation serves as a fundamental pillar, enabling the logistics of cell banking, distribution, and final product administration. The freeze-thaw process, however, introduces significant stressors that can compromise cell viability, potency, and ultimately, therapeutic efficacy. This application note frames contemporary insights on controlled-rate freezing (CRF) and thawing practices within a broader thesis on protocol standardization. As research and development progresses toward clinical application, a deep understanding of the principles governing ice crystal formation, cryoprotectant toxicity, and osmotic stress becomes paramount. The International Society for Cell & Gene Therapy (ISCT) envisions the translation of these therapies into safe, effective treatments through rigorous scientific standardization [98]. This document synthesizes current best practices and experimental protocols to support researchers and drug development professionals in optimizing these critical manufacturing steps, with a special emphasis on data derived from controlled-rate freezer qualification and post-thaw recovery assessment.
Key Survey Findings on Current Industry Practices
Controlled-Rate Freezer (CRF) Qualification and Utilization
Table 1: Key Findings on CRF Qualification and Outcomes
| Survey Parameter | Finding | Experimental Support |
|---|---|---|
| Primary CRF Application | Cryopreservation of PBMCs for subsequent DC generation | [99] |
| Freezing Rate for PBMCs | Approximately -1°C/min | [99] [4] |
| Impact on Cell Yield | Significantly higher cell yields vs. standard IPA freezing | [99] |
| Immature DC Yield | ~50% higher with CRF vs. standard IPA freezing | [99] |
| Functional Outcome | Superior antigen-specific autologous T-cell stimulation | [99] |
The adoption of Controlled-Rate Freezers represents a significant technological advancement over uncontrolled methods like isopropyl alcohol (IPA) "Mr. Frosty" containers. A critical comparative study analyzed the cryopreservation of highly concentrated peripheral blood mononuclear cells (PBMCs) destined for dendritic cell (DC)-based immunotherapy. The findings were revealing: PBMC cryopreservation using an automated CRF, followed by thawing and differentiation, resulted in significantly higher cell yields of both immature and mature DCs. Specifically, immature DC yields and total protein content after using a CRF were comparable to results obtained with freshly prepared PBMCs and exceeded results of standard IPA freezing by approximately 50% [99]. Beyond quantitative recovery, the functional capacity of these cells was enhanced. While phenotypic markers and allogeneic T-cell stimulation were similar, DCs generated from CRF-cryopreserved PBMCs induced a significantly higher antigen-specific IFN-γ release from autologous effector T cells, a key metric for immunotherapeutic efficacy [99].
Thawing Practices and Post-Thaw Recovery Optimization
Table 2: Key Findings on Thawing Practices and Outcomes
| Practice Variable | Recommended Protocol | Impact on Viability |
|---|---|---|
| Thawing Rate | Rapid (37°C water bath, <1 minute) | Minimizes ice recrystallization damage & DMSO exposure [100] [13] |
| Post-Thaw Dilution | Slow, drop-wise addition of pre-warmed medium | Prevents osmotic shock, ensuring gradual rehydration [100] [12] |
| DMSO Removal | Centrifugation at ~200 × g for 5-10 minutes | Effectively removes cytotoxic cryoprotectant [100] |
| Initial Seeding Density | High density at plating | Optimizes cell recovery by supporting cell-cell contact & paracrine signaling [100] [12] |
| Critical Growth Phase | Harvest during logarithmic growth phase | Ensures cells are in a robust, active state pre-freezing, enhancing post-thaw recovery [12] |
The "slow freeze, rapid thaw" principle remains a cornerstone of successful cryopreservation. Rapid thawing in a 37°C water bath is critical to minimize the damaging effects of ice recrystallization [100] [13]. For induced pluripotent stem cells (iPSCs), which are particularly vulnerable, this process should be swift, taking less than one minute until only a small ice crystal remains [100] [12]. The subsequent step—diluting the thawed cell suspension—is equally crucial. To prevent osmotic shock, the dense DMSO-containing cell suspension should be diluted slowly, in a drop-wise manner, into a larger volume of pre-warmed complete growth medium [100] [12]. This allows for a gradual equilibrium of solutes across the cell membrane, preventing lethal water influx. Finally, plating thawed cells at a high density is a widely recommended strategy to optimize recovery, as it facilitates essential cell-cell contacts and secretory factors that support survival and proliferation [100] [12].
Detailed Experimental Protocols
Protocol 1: Controlled-Rate Freezing of PBMCs for Immunotherapy Applications
This protocol, adapted from a peer-reviewed study, details the methodology for achieving superior DC yields and function from cryopreserved PBMCs using a Controlled-Rate Freezer [99].
Materials:
- Biological Material: Leukapheresis product from healthy donors.
- Freezing Medium: 20% Dimethyl Sulfoxide (DMSO), 40% Fetal Calf Serum (FCS), 40% RPMI 1640.
- Equipment: Controlled-Rate Freezer (e.g., Planer Kryo10 SerieII), 1-ml cryopreservation tubes, Liquid nitrogen storage tank.
Methodology:
- PBMC Preparation: Isolate PBMCs from the leukapheresis product using standard density gradient centrifugation.
- Cell Suspension: Resuspend the PBMC pellet in freezing medium at a high concentration of 2 × 10^8 cells/mL.
- Aliquoting: Transfer 1 mL of the cell suspension into each 1-ml cryopreservation tube.
- Controlled-Rate Freezing Program:
- Utilize a computer-assisted CRF.
- The cooling rate should be programmed to approximately -1°C/min down to a final temperature of -80°C.
- This slow, controlled cooling is essential to balance cell dehydration and intracellular ice formation.
- Long-Term Storage: After the program completes, immediately transfer the cryotubes to a liquid nitrogen tank for long-term storage in the vapor phase (<-135°C).
Protocol 2: Thawing and Recovery of Cryopreserved iPSCs
Optimized recovery of sensitive cell types like iPSCs requires careful attention to thawing kinetics and subsequent handling to prevent osmotic shock and support attachment [100] [12].
Materials:
- Cryopreserved Vial: iPSCs frozen as cell aggregates.
- Thawing Medium: Pre-warmed complete growth medium appropriate for the cell line.
- Wash Medium: Pre-warmed basal medium or DMSO-free complete medium.
- Coated Vessels: Tissue culture plates coated with Matrigel or equivalent.
Methodology:
- Rapid Thawing: Retrieve the cryovial from liquid nitrogen and immediately place it in a 37°C water bath. Gently swirl the vial until only a small bit of ice remains (typically <1 minute).
- Decontamination: Transfer the vial to a laminar flow hood and wipe the outside with 70% ethanol.
- Slow Dilution: Using a pipette, transfer the thawed cell suspension drop-wise into a centrifuge tube containing at least 10mL of pre-warmed thawing medium. This slow dilution is critical for preventing osmotic shock.
- Centrifugation: Pellet the cells by centrifugation at approximately 200 × g for 5 minutes.
- DMSO Removal: Aseptically decant the supernatant, which contains the cytotoxic DMSO.
- Resuspension and Seeding: Gently resuspend the cell pellet in fresh, pre-warmed complete growth medium. Plate the cells at a high density onto the pre-coated culture vessel to optimize recovery and support colony formation.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Cryopreservation
| Item | Function/Application | Example & Notes |
|---|---|---|
| Cryoprotectant | Permeates cells, depresses freezing point, inhibits intracellular ice crystal formation. | DMSO is most common (e.g., 10%). Glycerol, ethylene glycol are alternatives. Toxicity requires careful handling [4] [13]. |
| Basal Freezing Medium | Provides base solution for cryoprotectant; can include salts, nutrients. | RPMI 1640, DMEM. Often mixed with serum or serum-free alternatives [99] [101]. |
| Serum/Protein Supplement | Provides extracellular non-permeating cryoprotection, supports membrane stability. | Fetal Bovine/Calf Serum (FBS/FCS). For defined media, use CryoStor CS10 or BloodStor [99] [13]. |
| Defined Freezing Media | Ready-to-use, serum-free formulations for specific cell types; enhances consistency. | mFreSR (for human ES/iPS cells), MesenCult-ACF (for MSCs). Supports GMP compliance [13]. |
| Controlled-Rate Freezing Device | Ensures reproducible, optimal cooling rate (-1°C/min) for maximum viability. | Planer Kryo10 (CRF) or Mr. Frosty/CoolCell (passive containers) [99] [13]. |
| Cryogenic Storage Vials/Bags | Secure, sterile containment for long-term storage at ultra-low temperatures. | Corning Cryogenic Vials; OriGen CryoStore Bags (ideal for small volumes 10-30mL, GMP-compliant) [13] [102]. |
Workflow and Signaling Pathways
The following workflow diagrams the logical sequence and critical decision points for the key cryopreservation and thawing protocols discussed in this note.
Diagram 1: Cryopreservation and Thawing Workflow. This chart outlines the sequential steps for the cryopreservation of cells like PBMCs and the subsequent thawing process, highlighting critical control points such as controlled-rate freezing and slow dilution.
The integration of qualified Controlled-Rate Freezing and optimized thawing practices is not merely a technical improvement but a fundamental requirement for ensuring the quality, potency, and consistency of cellular products in research and clinical development. The data presented underscores that moving beyond uncontrolled freezing methods can yield substantial benefits, including significantly higher cell yields and enhanced functional capacity post-thaw. As the industry advances, the adoption of standardized, well-characterized protocols—buttressed by defined reagents and GMP-compliant materials—will be instrumental in translating promising cell and gene therapies from the research bench to reliable patient treatments. The continued collection of survey data and publication of comparative studies will be vital to further refine these critical manufacturing steps and fulfill the ISCT's vision of improving patients' lives through safe and effective therapies [98].
Within the critical workflows of cell and gene therapy manufacturing, the processes of freezing and thawing present a significant bottleneck where cell viability and product quality can be compromised. The post-thaw recovery of cells is a vital determinant for the success of downstream applications, influencing everything from experimental reproducibility to clinical efficacy [64]. Traditional manual thawing methods are susceptible to variability, posing challenges for standardization and scale-up. Emerging technologies, specifically automated thawing systems and Process Analytical Technology (PAT), are now addressing these challenges by introducing unprecedented levels of control, monitoring, and reproducibility. This application note details the integration of these technologies, providing a structured framework and detailed protocols to enhance cell recovery and process understanding within the broader context of bioprocess optimization and regulatory compliance.
Automated Thawing Systems
Automated thawing systems represent a significant evolution from simple water baths, combining sophisticated hardware and software to deliver precise, reproducible warming of cryopreserved samples. At their core, these systems are designed to transition cells from a frozen state to a viable, suspension-ready condition while minimizing the cellular stress associated with traditional thawing methods [103].
The fundamental hardware components typically include an insulated thawing chamber, precision temperature sensors, and thermal control units that ensure uniform heat distribution. This hardware synergy is critical for achieving rapid thawing, which helps reduce the exposure time to potentially harmful cryoprotectants like DMSO and minimizes damage from ice recrystallization [13]. Furthermore, modern equipment prioritizes materials that meet stringent biocompatibility and sterilization standards, with some systems incorporating integrated sterilization cycles or disposable components to mitigate contamination risks—a paramount concern in cell and gene therapy production [103].
The software architecture provides the intelligence for process control, featuring real-time monitoring, comprehensive data logging, and process validation capabilities. Advanced systems are equipped with sensors that can detect process deviations and automatically adjust parameters to maintain optimal thawing conditions. User-friendly interfaces allow technicians to set customized protocols based on cell type and bag or vial volume, with some platforms enabling remote oversight of multiple units [103].
Process Analytical Technology (PAT) in Thawing
Process Analytical Technology (PAT) is a framework encouraged by regulatory agencies to design, analyze, and control manufacturing through timely measurements of critical quality and performance attributes. In the context of thawing processes, PAT moves the paradigm from simple endpoint checks to continuous, dynamic monitoring [104] [105].
PAT tools enable real-time monitoring of critical process parameters (CPPs) during thawing operations. For instance, dielectric spectroscopy can be applied to monitor biological samples by measuring the capacitance of intact cell membranes. This provides valuable information on cell concentration and viability in real-time, allowing for immediate intervention if parameters drift from established setpoints [104]. Similarly, other inline analytical tools can track changes in the physical and biochemical environment of the thawing suspension, providing a holistic view of the process.
The data generated by these tools feed into control strategies that enhance process robustness. By recognizing unfavorable changes in CPPs early, manufacturers can intervene to prevent the loss of valuable production batches [104]. This data-driven approach is integral to a Quality-by-Design (QbD) framework, where the thawing process is no longer a black box but a well-understood and controlled unit operation, thereby mitigating risks to both product quality and patient safety [105].
Integrated Thawing Workflow: Manual vs. Automated
The following diagram contrasts the steps and decision points in manual and automated thawing workflows, highlighting where automation and PAT reduce variability and introduce critical monitoring points.
Application Protocols
Protocol: Automated Thawing of Cell Therapy Products
This protocol is designed for use with automated thawing systems (e.g., ThawSTAR CFT2 or similar) and is applicable to suspension cells, including those used in cell and gene therapies [103] [73].
Materials:
- Pre-programmed automated thawing instrument
- Cryopreserved vial of cells (e.g., iPSCs, PBMCs)
- Pre-warmed Thaw Medium (e.g., CryoStor CS10 or similar)
- Sterile 15 mL or 50 mL conical tube
- Centrifuge
- Appropriate cell culture vessel
Procedure:
- System Preparation: Power on the automated thawing instrument and select the validated protocol corresponding to the cell type and vial volume. The system performs an automatic self-check.
- Loading: Remove the frozen cryovial from liquid nitrogen storage and quickly place it into the designated chamber of the thawing instrument. Ensure the vial is securely seated.
- Initiation: Start the protocol. The instrument will agitate and warm the vial at a controlled, optimized rate. The process is typically complete within 1-2 minutes.
- PAT Monitoring: The system's integrated sensors (e.g., temperature, dielectric spectroscopy) monitor the process in real-time, ensuring the thawing profile remains within validated parameters and logging all data for traceability [103].
- Unloading & Transfer: Immediately upon completion, remove the vial from the instrument. Wipe the exterior with 70% ethanol. Gently loosen the cap to release pressure.
- Dilution & Washing: Transfer the entire thawed cell suspension to a sterile tube containing 10 mL of pre-warmed Thaw Medium. For sensitive cells, add the medium dropwise initially to prevent osmotic shock [64] [73].
- Centrifugation: Pellet the cells by centrifugation at 200-300 × g for 5-10 minutes.
- Resuspension: Carefully aspirate the supernatant, which contains cryoprotectants like DMSO. Gently resuspend the cell pellet in fresh, pre-warmed Growth Medium.
- Seeding: Transfer the cell suspension to a culture vessel and place it in a 37°C, 5% CO₂ incubator.
- Assessment: After 24 hours, assess cell attachment (for adherent cells), viability, and confluence. Change the medium to remove any non-viable cells and debris.
Protocol: Integration of PAT for Thaw Process Monitoring
This protocol outlines the integration of a PAT tool, specifically dielectric spectroscopy, to monitor cell health and concentration during the post-thaw recovery phase.
Materials:
- Bioreactor or culture vessel with PAT ports
- Dielectric spectroscopy probe (e.g., for capacitance measurement)
- Compatible analyzer and data acquisition software
- Cell culture post-thaw
Procedure:
- Calibration: Prior to thawing, calibrate the dielectric spectroscopy probe according to the manufacturer's instructions. This may involve measurements in culture medium alone.
- Probe Installation: Aseptically install the sterilized probe into the culture vessel where the thawed and resuspended cells will be transferred.
- Baseline Measurement: With the fresh culture medium in the vessel, establish a baseline capacitance measurement.
- Initiate Monitoring: After transferring the thawed and washed cells into the vessel, immediately begin continuous monitoring.
- Data Interpretation: Monitor the biocapacitance (often reported as capacitance at a specific frequency, e.g., 10 MHz). A stable or increasing signal indicates a high proportion of cells with intact plasma membranes, correlating with good viability. A declining signal may indicate cell death and membrane rupture [104].
- Process Decision: Use the real-time data to inform subsequent process steps. For example, if the biocapacitance drops precipitously post-thaw, it may trigger a quality investigation or indicate the need for a process adjustment in the next batch.
Data Presentation and Analysis
Quantitative Comparison of Thawing Methods
The following table summarizes key performance metrics for manual versus automated thawing systems, drawing from current technology analyses and cell recovery studies.
Table 1: Performance Comparison of Cell Thawing Methods
| Parameter | Manual Thawing (Water Bath) | Automated Thawing Systems |
|---|---|---|
| Thawing Rate Control | Variable; relies on user technique | Precise and programmable (-1°C/min cooling standard for freezing; rapid, controlled warming for thawing) [13] |
| Post-Thaw Viability | Often variable (e.g., 70-90% for iPSCs) | Highly consistent (e.g., >90% for iPSCs with optimized protocols) [64] |
| Process Data Logging | Manual record-keeping | Automated, real-time data logging (time, temperature) for traceability [103] |
| Contamination Risk | Higher (potential water bath contamination) | Lower (closed or sterile disposable components) [103] |
| Regulatory Compliance | Extensive validation required | Easier validation with built-in audit trails and compliance with GMP/ISO 13485 [103] |
| Typical Cell Recovery Time | 4-7 days (can extend to 2-3 weeks if suboptimal) [64] | Consistent recovery in 4-7 days post-thaw [64] |
Research Reagent Solutions
A successful thawing process relies on a suite of specialized reagents and materials. The table below lists essential components and their critical functions.
Table 2: Essential Materials for Cell Thawing Protocols
| Material | Function | Examples & Notes |
|---|---|---|
| Defined Cryopreservation Medium | Protects cells from ice crystal damage during freeze-thaw; contains cryoprotectants. | CryoStor CS10 [13], mFreSR for pluripotent stem cells [13]. Prefer GMP-manufactured, serum-free formulations. |
| Thawing Medium | Dilutes cryoprotectant post-thaw; provides nutrients and osmotic support. | Often uses standard growth medium without antibiotics initially; some protocols use specialized Thaw Medium 10 [73]. |
| Controlled-Rate Freezing Container | Ensures optimal cooling rate (-1°C/min) during initial freezing step, critical for post-thaw viability. | Nalgene Mr. Frosty (isopropanol-based), Corning CoolCell (isopropanol-free) [13]. |
| Automated Thawing Instrument | Provides reproducible, rapid, and controlled warming of frozen samples. | ThawSTAR CFT2; features include real-time monitoring and validation support [103]. |
| PAT Probe | Monitors critical process parameters like viable cell density in real-time. | Dielectric spectroscopy probe for measuring biocapacitance [104]. |
Discussion and Outlook
The integration of automated thawing systems and PAT marks a significant leap toward robust, closed, and digitally managed bioprocesses. By 2025, the adoption of these technologies is expected to accelerate, driven by regulatory pressures and the compelling need for reproducibility in advanced therapies [103]. The outlook includes innovations such as AI-driven process optimization, where historical thawing data trains algorithms to predict and correct for batch-to-batch variability, and enhanced IoT connectivity for seamless data transfer to centralized manufacturing execution systems (MES) [103].
Persistent challenges include the high initial investment for advanced equipment and the complexity of integrating new systems into established workflows, particularly for smaller facilities [103]. Furthermore, the success of any thawing protocol is profoundly influenced by upstream factors, particularly the freezing process and the cell growth phase before preservation. Cells should be harvested during their maximum growth phase (log phase) and frozen at high confluence (>80%) to ensure the best post-thaw recovery [13] [64].
Future development will focus on creating more modular and scalable thawing solutions that can integrate directly with downstream processing units, creating continuous and highly controlled manufacturing pipelines for cell-based products. As these technologies mature, they will become the standard, ensuring that the critical thawing step no longer represents a vulnerability but a well-controlled and reliable foundation for regenerative medicine.
Conclusion
Mastering cell cryopreservation is a critical competency that underpins reproducibility and success in biomedical research and cell-based therapies. By integrating foundational scientific principles with robust, optimized protocols and rigorous post-thaw validation, researchers can significantly enhance cell viability and functionality. Future advancements will likely focus on standardizing controlled-rate freezer qualification, developing cell-type-specific freezing media, and integrating real-time process monitoring. As the field of advanced therapies progresses, refining these protocols will be paramount for scaling manufacturing, ensuring product consistency, and ultimately improving clinical outcomes.
References
- 1. Learn about cryopreservation of mammalian cell lines for long term... [https://www.abcam.com/en-us/technical-resources/protocols/cryopreservation-of-mammalian-cell-lines]
- 2. How to maintain a cell ? – Single Use Support bank [https://www.susupport.com/blogs/knowledge/how-to-maintain-a-cell-bank]
- 3. Stem cell : preserving banks lines, maintaining cell ... genetic integrity [https://pubmed.ncbi.nlm.nih.gov/21822864/]
- 4. Cryopreservation: An Overview of Principles and Cell-Specific Considerations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995302/]
- 5. and Freezing to Maintain Viability | Corning Cells Thawing Cells [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/top-tips-for-freezing-and-thawing-cells-to-maintain-viability.html]
- 6. Cryoprotectant - Wikipedia [https://en.wikipedia.org/wiki/Cryoprotectant]
- 7. Chemical approaches to cryopreservation | Nature Reviews Chemistry [https://www.nature.com/articles/s41570-022-00407-4]
- 8. - Serum Media in the Real World: 5 Uses You'll... Free Cryopreservation [https://www.linkedin.com/pulse/serum-free-cryopreservation-media-real-world-3mp7e]
- 9. - Serum solutions for free of cryopreservation cells [https://pubmed.ncbi.nlm.nih.gov/17879124/]
- 10. Optimizing cryopreservation of human testicular tissue: comparison of... [https://pubmed.ncbi.nlm.nih.gov/15860503/]
- 11. of conventional and automated Comparison methods on... freezing [https://bnrc.springeropen.com/articles/10.1186/s42269-020-00371-3]
- 12. Improving Cell Recovery: Freezing and Thawing Optimization of Induced Pluripotent Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8909336/]
- 13. Cryopreservation Basics: Protocols and Best Practices for Freezing ... [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 14. How to Freeze and Thaw Cells with Cell Freezing Medium? - CellStore Biotechnology Co., Ltd. [https://www.cellstore-global.com/how-to-freeze-and-thaw-cells-with-cell-freezing-medium.html]
- 15. Freezing and thawing of cell lines protocol. EuroMAbNet [https://www.euromabnet.com/protocols/freezing-thawing.php]
- 16. How to Measure Cell | Life in the Lab Confluency [https://www.thermofisher.com/blog/life-in-the-lab/how-to-measure-cell-confluency/]
- 17. : Why It Matters and 3 Easy Methods Cell Confluency [https://bitesizebio.com/63887/cell-confluency/]
- 18. Cell Thawing Protocol for Frozen Primary Cells | STEMCELL Technologies [https://www.stemcell.com/how-to-thaw-frozen-primary-cells.html]
- 19. Avoidance of crystallization by freeze resistance [https://www.doitpoms.ac.uk/tlplib/biocrystal/avoidance2.php]
- 20. Cryopreservation Freezing Methods and... | Technology Networks [https://www.technologynetworks.com/cell-science/articles/cryopreservation-freezing-methods-and-equipment-292855]
- 21. Why Bother Optimizing Your Cryopreservation Process | Medium [https://medium.com/@RR-BPC/heres-why-cryopreservation-optimization-matters-a67bc2c06c89]
- 22. Cryopreservation - GeeksforGeeks [https://www.geeksforgeeks.org/biology/cryopreservation/]
- 23. Cell Therapy Drug Product Development: Technical Considerations and Challenges - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0022354923003209]
- 24. Cell Freezing Solutions in the Real World: 5 Uses You'll Actually See... [https://www.linkedin.com/pulse/cell-freezing-solutions-real-world-5-uses-youll-actually-lcdie]
- 25. Cell Cryopreservation Market Size & Share | Growth Trends 2025-2037 [https://www.researchnester.com/reports/cell-cryopreservation-market/5636]
- 26. | Thermo Fisher Scientific - US Cell Freezing Protocols [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 27. Freezing and viability staining of cells [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/animal-cell-culture/essential-protocols-for-animal-cell-culture/freezing-and-viability-staining-of-cells]
- 28. Freezing Protocol [https://www.cytion.com/us/Knowledge-Hub/Cell-Culture-Techniques/Freezing-Protocol/]
- 29. This is a protocol on how to best isolate, freeze , and thaw PBMCs. [https://www.mabtech.com/knowledge-hub/isolation-freezing-and-thawing-pbmcs]
- 30. Evaluation of the viability and functionality of human peripheral blood mononuclear cells cryopreserved up to 2 years in animal-protein-free freezing media compared to the FBS-supplemented reference medium - PubMed [https://pubmed.ncbi.nlm.nih.gov/40821813/]
- 31. https://public-pages-files-2025.frontiersin.org/journals/ ... [https://public-pages-files-2025.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1627973/xml]
- 32. Cell Freezing Protocols | Thermo Fisher Scientific - TR [https://www.thermofisher.com/tr/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 33. - Serum Future-proof Strategies: Trends... Free Freezing Media [https://www.datainsightsmarket.com/reports/serum-free-freezing-media-1207262]
- 34. Cryopreservation of Cells: Dos and Don’ts | Corning [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/the-dos-and-donts-of-cryopreservation.html]
- 35. Cell Freezing Market | Global Market Analysis Report - 2035 Media [https://www.futuremarketinsights.com/reports/cell-freezing-media-market]
- 36. The Importance of Controlling the Rate of Freezing [https://www.thermofisher.com/blog/life-in-the-lab/the-importance-of-controlling-the-rate-of-freezing/]
- 37. Liquid Nitrogen vs liquid nitrogen-free Cell | Strex Freezers Cell [https://strexcell.com/blog/liquid-nitrogen-vs-liquid-nitrogen-free-cell-freezers/]
- 38. Freezing Containers for Cell Preservation [https://www.genengnews.com/resources/freezing-containers-for-cell-preservation/]
- 39. Optimal Protocol for Cryopreservation of Cultured Cells | Strex Cell [https://strexcell.com/blog/freeze-protocol-for-cells/]
- 40. and Thawing Freezing in the Lab: 8 Tips and Tricks Cells [https://bitesizebio.com/13684/freezing-and-thawing-mammalian-cells-tutorial/]
- 41. Freezing Cell | Thermo Fisher Scientific - CN Protocols [https://www.thermofisher.cn/cn/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 42. Culturing Human Neural Stem Cells | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/protocols/neurobiology/neurobiology-protocols/immune-response-biomarker-profiling.html]
- 43. Cryopreservation and thawing of cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/23129152/]
- 44. Walking on thin ice: controlled freezing & thawing of pharmaceutical active molecules [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/2677/Walking-on-thin-ice-controlled-freezing-thawing-of-pharmaceutical-active-molec]
- 45. | Thermo Fisher Scientific - TR Thawing Cells [https://www.thermofisher.com/tr/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 46. PBMC Thawing : How to Optimize Protocol Recovery Cell [https://cytologicsbio.com/pbmc-thawing-protocol-how-to-optimize-cell-recovery/]
- 47. Frontiers | Comparative assessment of thawing methods for frozen... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1562053/full]
- 48. Quantitative assessment of the impact of cryopreservation on human bone marrow-derived mesenchymal stem cells: up to 24 h post-thaw and beyond | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02054-2]
- 49. Freezing Medium Containing 5% DMSO Enhances the Cell Viability and Recovery Rate After Cryopreservation of Regulatory T Cell Products ex vivo and in vivo - PubMed [https://pubmed.ncbi.nlm.nih.gov/34926446/]
- 50. Microfluidics for Cryopreservation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2719835/]
- 51. Assessing the toxic effects of DMSO on cord blood to determine exposure time limits and the optimum concentration for cryopreservation - PubMed [https://pubmed.ncbi.nlm.nih.gov/25899864/]
- 52. (PDF) Frozen- thawed bovine spermatozoa diluted by slow or rapid... [https://www.academia.edu/83919351/Frozen_thawed_bovine_spermatozoa_diluted_by_slow_or_rapid_dilution_method_Measurements_on_occurrence_of_osmotic_shock_and_sperm_viability]
- 53. Mammalian Thawing : Methods and Considerations-overview Cells [https://www.linkedin.com/pulse/thawing-mammalian-cells-methods-hadi-hezaveh]
- 54. Post-thaw removal of DMSO does not completely abrogate infusional toxicity or the need for pre-infusion histamine blockade - PubMed [https://pubmed.ncbi.nlm.nih.gov/20426544/]
- 55. DMSO Cell Culture Guide: Unlock Perfect Cell Cryopreservation - sciencespark.blog [https://sciencespark.blog/dmso-cell-culture-cryopreservation-guide]
- 56. Improving Cell Recovery: Freezing and Thawing Optimization of Induced Pluripotent Stem Cells [https://www.mdpi.com/2073-4409/11/5/799]
- 57. Cryopreservation - Wikipedia [https://en.wikipedia.org/wiki/Cryopreservation]
- 58. Impact of Freeze–Thaw Processes on the Quality of Cells [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/365/Impact-of-FreezeThaw-Processes-on-the-Quality-of-Cells]
- 59. Impact of Cryopreservation and Freeze-Thawing on Therapeutic Properties of Mesenchymal Stromal/Stem Cells and Other Common Cellular Therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9045030/]
- 60. Cryopreservation: A Review Article - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9756256/]
- 61. CryoStor® Cryopreservation Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/cell-growth-and-maintenance/cryostor-cryopreservation-protocol]
- 62. Impact of Cryopreservation and Freeze - Thawing on Therapeutic... [https://link.springer.com/article/10.1007/s40778-022-00212-1]
- 63. Cryopreservation in Cell and Gene Therapy: Ensuring High-Viability Cells for Research & Manufacturing [https://cgt.global/cryopreservation-in-cell-and-gene-therapy-ensuring-high-viability-cells-for-research-manufacturing/]
- 64. Improving Cell Recovery: Freezing and Thawing of... Optimization [https://pubmed.ncbi.nlm.nih.gov/35269421/]
- 65. and Recovery of Cryopreservation : Best... | IntechOpen Primary Cells [https://www.intechopen.com/online-first/1231876]
- 66. Impact of cryopreservation on CAR T production and clinical response - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9582437/]
- 67. Cryopreserved leukapheresis enables scalable and distributed CAR-T manufacturing: a multi-platform comparative study | Scientific Reports [https://www.nature.com/articles/s41598-025-14865-5]
- 68. of Optimisation conditions, including storage... cryopreservation [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-024-00516-6]
- 69. Laboratory Aseptic and Safety in Techniques Culture Cell [https://www.thermofisher.com/za/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 70. Processing Aseptic and Control Prevention Contamination [https://laafon.com/aseptic-processing-control/]
- 71. Tips for Secure Liquid Nitrogen Safety Cell Storage [https://www.cytion.com/Knowledge-Hub/Blog/Liquid-Nitrogen-Safety-Tips-for-Secure-Cell-Storage/]
- 72. Container in the Real World... Liquid Nitrogen Cryopreservation [https://www.linkedin.com/pulse/liquid-nitrogen-cryopreservation-container-real-world-5-c8ghe]
- 73. Cell Thawing Protocol [https://bpsbioscience.com/cell-thawing-protocol]
- 74. PBMC Storage - Cryopreservation & Controlled-Rate Freezing [https://researchdonors.co.uk/2025/02/18/the-importance-of-cryopreservation-solutions-and-controlled-rate-freezing-in-pbmc-storage/]
- 75. up Scaling from Cell Suspensions to... | IntechOpen Cryopreservation [https://www.intechopen.com/chapters/84457]
- 76. Current issues & future trends in cryopreservation for advanced therapies [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3053/Current-issues-future-trends-in-cryopreservation-for-advanced-therapies]
- 77. Winter is coming: the future of cryopreservation | BMC Biology [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-021-00976-8]
- 78. Optimizing Cryopreservation Conditions with CRFT: A Scalable... [https://www.grantinstruments.com/posts/optimizing-cryopreservation-conditions-with-crft-a-scalable-approach-from-lab-to-industry]
- 79. Optimizing Cryopreservation for Leukapheresis: Advancing Cell and Gene Therapy Supply Chains - Cryoport Systems [https://www.cryoport.com/optimizing-cryopreservation-for-leukapheresis-advancing-cell-and-gene-therapy-supply-chains/]
- 80. Comparative analysis and process optimization for manufacturing CAR-T using the PiggyBac system derived from cryopreserved versus fresh PBMCs | Scientific Reports [https://www.nature.com/articles/s41598-025-89686-7]
- 81. Post-Thaw Culture and Measurement of Total Cell Recovery Is Crucial in the Evaluation of New Macromolecular Cryoprotectants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7362331/]
- 82. Cryopreservation and post - thaw differentiation of monocytes enabled... [https://pubs.rsc.org/en/content/articlehtml/2025/lp/d5lp00131e]
- 83. Establishment and validation of in-house cryopreserved... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8705121/]
- 84. Optimizing PBMC Viability and Recovery: Updated Best... - CGT Global [https://cgt.global/pbmc-viability-and-recovery/]
- 85. PBMC Cryopreservation Protocol for High Post - thaw Viability [https://cytologicsbio.com/pbmc-cryopreservation-protocol-for-high-post-thaw-viability/]
- 86. EMT & Stemness FAQs [https://www.novusbio.com/support/emt-and-stemness-faqs]
- 87. Freezing Technology: Control of Freezing, Thawing, and Ice Nucleation | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-0716-0783-1_6]
- 88. Programmable Controlled in the Real World: 5 Uses... Rate Freezer [https://www.linkedin.com/pulse/programmable-controlled-rate-freezer-real-ylf5e]
- 89. is equivalent to Passive - freezing for... controlled rate freezing [https://pubmed.ncbi.nlm.nih.gov/40323255/]
- 90. CryoMed Controlled - Rate that Meet 21 CFR Part 11... Freezers [https://www.thermofisher.com/blog/life-in-the-lab/cryomed-controlled-rate-freezers-that-meet-21-cfr-part-11-requirements/]
- 91. New Controlled - Rate Provide Optimal... | Lab Manager Freezers [https://www.labmanager.com/new-controlled-rate-freezers-provide-optimal-sample-protection-and-support-gmp-and-21-cfr-part-11-requirements-24826]
- 92. Frozen Cells | Thermo Fisher Scientific - LU Thawing [https://www.thermofisher.com/lu/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 93. Cell thawing device – Advantages... - Eppendorf Marocco [https://www.eppendorf.com/ma-en/lab-academy/life-science/molecular-biology/cell-thawing-device-advantages-disadvantages/]
- 94. Plasma Thawers. Advantages and differences of dry from... thawing [https://tahat-aksi.com/blog/plasma-thawers-advantages-and-differences-of-dry-thawing-from-water-bath]
- 95. Rapid dry plasma thawing system: An alternative to conventional... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613422/]
- 96. Video: Regulating Temperature in the Lab: Applying Heat [https://www.jove.com/v/5043/regulating-temperature-in-the-lab-applying-heat]
- 97. Addgene: Water Bath Protocol [https://www.addgene.org/protocols/water-bath/]
- 98. Home - International Society for Cell & Gene Therapy [https://www.isctglobal.org/home]
- 99. Controlled-rate freezer cryopreservation of highly concentrated peripheral blood mononuclear cells results in higher cell yields and superior autologous T-cell stimulation for dendritic cell-based immunotherapy - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3493671/]
- 100. | Thermo Fisher Scientific - RU Thawing Cells [https://www.thermofisher.com/ru/ru/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 101. StarrLab - Culture Freeze Thaw Cells [https://sites.google.com/a/umn.edu/starrlab/protocols/cell-work/culture-freeze-thaw-cells]
- 102. Why OriGen Biomedical® CryoStore Freezing ... - OriGen Biomedical [https://www.origen.com/news-and-insights/why-origen-biomedical-cryostore-freezing-bags-are-key-for-small-volume-cryopreservation]
- 103. How Cell And Gene Therapy Thawing Equipment Works — In One... [https://www.linkedin.com/pulse/how-cell-gene-therapy-thawing-equipment-works-qjn4f]
- 104. (PAT) in insect and mammalian Process ... analytical technology cell [https://pubmed.ncbi.nlm.nih.gov/24297424/]
- 105. and Quality-by-Design... | SpringerLink Process Analytical Technology [https://link.springer.com/chapter/10.1007/978-3-319-10320-4_21]