Antibiotic Efficacy Against Mycoplasma pneumoniae: From Macrolide Resistance to Novel Therapeutic Strategies
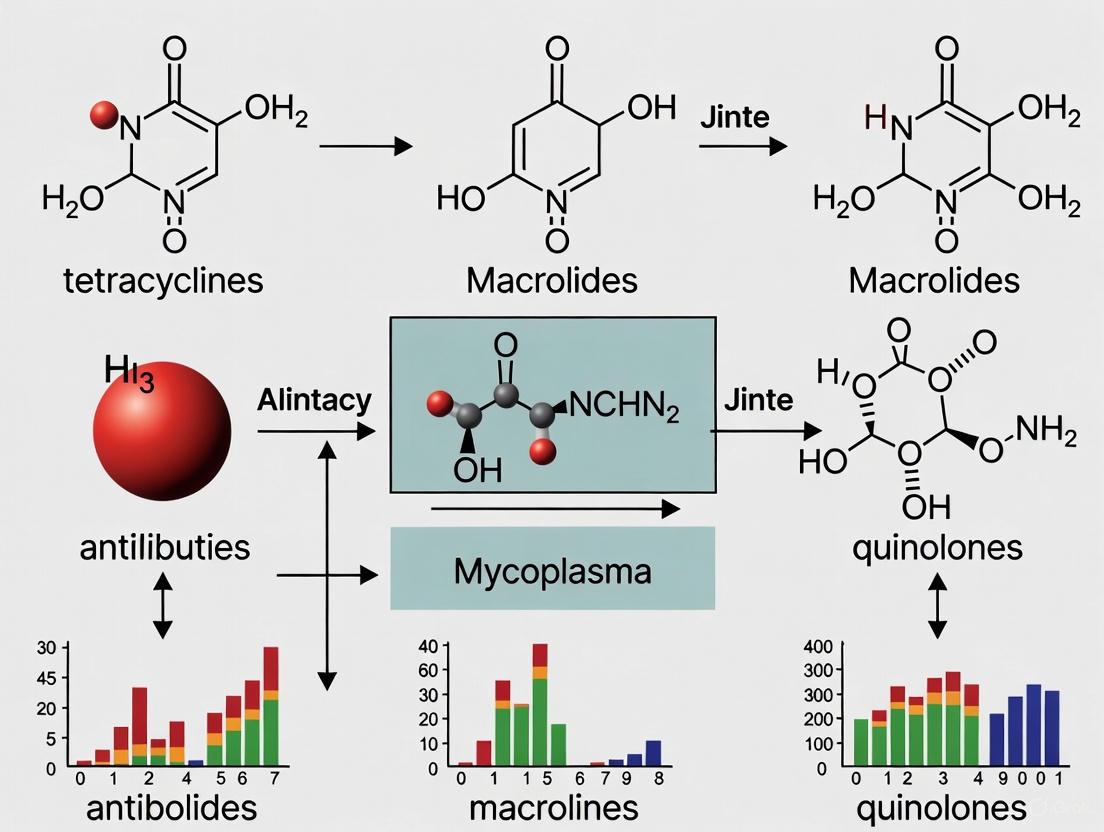
This article synthesizes current research on the efficacy of various antibiotics for eradicating Mycoplasma pneumoniae, with a particular focus on the global challenge of macrolide resistance.
Antibiotic Efficacy Against Mycoplasma pneumoniae: From Macrolide Resistance to Novel Therapeutic Strategies
Abstract
This article synthesizes current research on the efficacy of various antibiotics for eradicating Mycoplasma pneumoniae, with a particular focus on the global challenge of macrolide resistance. It explores foundational mechanisms of antibiotic action and bacterial evasion, evaluates methodological approaches for assessing efficacy in both planktonic and biofilm states, and investigates troubleshooting strategies such as synergistic antibiotic combinations and alternative non-antibiotic modalities. The content further provides a comparative validation of clinical outcomes across different patient populations and antibiotic classes, including macrolides, tetracyclines, and fluoroquinolones. Aimed at researchers and drug development professionals, this review aims to bridge laboratory findings with clinical applications to guide the development of next-generation therapeutic interventions.
Understanding Mycoplasma pneumoniae and the Challenge of Antibiotic Resistance
Mycoplasma pneumoniae stands as a remarkable exception in the bacterial world, representing one of the smallest self-replicating organisms known to science. This pathogen lacks a cell wall—a defining feature of most bacteria—possessing only a triple-layered cell membrane enriched with sterols [1] [2]. This minimalist cellular architecture stems from extensive genomic reduction; its genome spans approximately 816 kilobase pairs containing around 687 genes, reflecting an evolutionary trajectory toward obligate parasitism in the human respiratory tract [1]. This genomic reduction has rendered M. pneumoniae intrinsically resistant to beta-lactam antibiotics that target peptidoglycan synthesis, necessitating alternative therapeutic strategies that inhibit protein synthesis or DNA replication [1] [2].
The clinical significance of M. pneumoniae has been highlighted by its recent global resurgence following the relaxation of COVID-19 pandemic control measures. After a prolonged period of suppression during 2020-2022, outbreaks emerged worldwide in 2023-2024, causing substantial morbidity in both pediatric and adult populations [3] [4]. This resurgence has provided new insights into the epidemiology of this pathogen and renewed focus on the challenges it presents, particularly the growing prevalence of macrolide-resistant M. pneumoniae (MRMP) strains, especially in East Asia where resistance rates exceed 80% [5] [2]. Understanding the unique biology of this wall-less pathogen is thus essential for developing effective countermeasures against infections that range from mild respiratory illness to severe pneumonia requiring hospitalization.
Unique Structural Biology and Pathogenic Mechanisms
The Terminal Organelle: Adhesion and Motility Apparatus
The absence of a cell wall has profound implications for the cellular organization of M. pneumoniae. Instead of rigid peptidoglycan-based structure, this pathogen relies on a sophisticated internal cytoskeleton to maintain structural integrity and facilitate essential pathogenic functions. Central to its virulence is a specialized polar extension known as the terminal organelle (or attachment organelle), which orchestrates both cytoadherence to host epithelia and a unique form of gliding motility [1].
The terminal organelle features a complex bipartite architecture with surface-exposed nap-like proteins that facilitate host-pathogen interactions, and an intricately organized internal structure that generates mechanical force [1]. The adhesion machinery comprises four evolutionarily conserved surface proteins: P1 (MPN141), P90/P40 (encoded by MPN142 as proteolytic cleavage products), and P30 (MPN453). Spatial mapping demonstrates that the P1 adhesin complex, comprising P1 and P90/P40 subunits, localizes at the apical tip forming a rigid membrane anchor, while P30 dynamically associates with the complex periphery to regulate force transduction during gliding motility [1].
Internally, the terminal organelle contains an electron-dense core structure maintained through three specialized components: the terminal button, paired plates, and bowl complex. This core scaffold provides mechanical stability and serves as an assembly platform for the adhesion machinery [1]. The coordinated action of these structures enables M. pneumoniae to adhere to respiratory epithelium, propelling itself via gliding motility to colonize host tissues while evading mucociliary clearance [6].
Cytotoxicity and Immune Evasion Strategies
The pathogenic strategy of M. pneumoniae extends beyond adhesion to active host cell damage and immune system manipulation. Upon attachment to respiratory epithelium, the bacterium releases several cytotoxic molecules, including hydrogen peroxide (H₂O₂) and community-acquired respiratory distress syndrome (CARDS) toxin [1] [2]. These virulence factors work in concert to damage epithelial cells and cilia, disrupting mucociliary clearance and promoting the characteristic tissue damage observed in mycoplasma pneumonia.
The interaction between respiratory epithelial cells and surface lipoproteins of M. pneumoniae stimulates the host immune system through Toll-like receptor (TLR)-2 or TLR-4 pathways, potentially inducing intercellular adhesion molecule receptor synthesis [2]. However, the pathogen employs several immune evasion strategies, including antigenic variation of surface proteins and the formation of biofilm towers that provide enhanced resistance to both antibiotics and host immune effectors [7]. Biofilm formation represents a particularly important adaptation for chronic infection, as these structures show dramatically increased resistance to erythromycin (up to 8,500-128,000 times the minimal inhibitory concentration for planktonic cells) and complement-mediated killing [7].
Antibiotic Efficacy Comparison: Clinical and Experimental Data
Treatment Modalities and Outcomes in Pediatric Pneumonia
The absence of a cell wall in M. pneumoniae fundamentally shapes therapeutic approaches, restricting effective antibiotic classes to those targeting protein synthesis (macrolides, tetracyclines) or DNA replication (fluoroquinolones). The rising prevalence of macrolide-resistant strains has complicated treatment decisions, particularly for pediatric patients where tetracyclines and fluoroquinolones have historically been used with caution due to potential side effects.
A comprehensive 2025 study of 389 children with M. pneumoniae pneumonia (MPP) in South Korea revealed striking patterns in treatment efficacy across different therapeutic approaches. The overall macrolide resistance rate was 89.1%, yet treatment outcomes varied significantly between intervention strategies [5]. The table below summarizes the fever duration and clinical outcomes across different treatment modalities.
Table 1: Comparative Efficacy of Treatment Modalities for Pediatric M. pneumoniae Pneumonia
| Treatment Group | Number of Patients | Total Fever Duration (Days, Median) | Time to Defervescence After Treatment Initiation (Days) | Hospitalization Rate | Macrolide Resistance Rate |
|---|---|---|---|---|---|
| Spontaneous Resolution (SR) | 85 | 5.0 | N/A | 81.4% | Not reported |
| Macrolide Only (ML) | 70 | 7.0 | 2-3 | 84.7% | 72.0% |
| Macrolide with Other Treatments (ML-O) | 148 | 8.0 | 2-3 | 93.9% | 96.7% |
| Second-line Antibiotics and/or Steroids (2nd-A/S) | 86 | 7.0 | 0-2 | 84.7% | 100% |
This real-world data reveals several important patterns. First, a substantial proportion of cases (21.9%) experienced spontaneous resolution without targeted antibiotic therapy, highlighting the self-limiting nature of many M. pneumoniae infections [5]. Second, despite high macrolide resistance rates, macrolide monotherapy remained effective in many patients, with fever resolution occurring within 2-3 days of treatment initiation. Third, the combination of macrolides with other treatments was associated with longer total fever duration and higher hospitalization rates, likely reflecting treatment selection bias for more severe cases [5].
Doxycycline Efficacy in Severe Mycoplasma pneumoniae Pneumonia
For severe or macrolide-unresponsive infections, second-line antibiotics become essential. A 2025 clinical analysis evaluated the efficacy and safety of doxycycline in treating Severe Mycoplasma pneumoniae Pneumonia (SMPP) in children under eight years old, comparing outcomes between a doxycycline treatment group (44 cases) and a macrolide control group (48 cases) [8]. All included children had failed to respond to at least three days of prior macrolide therapy, meeting criteria for macrolide-unresponsive Mycoplasma pneumoniae pneumonia (MUMPP).
Table 2: Doxycycline vs. Macrolide Efficacy in Severe Pediatric M. pneumoniae Pneumonia
| Clinical Parameter | Doxycycline Group (n=44) | Macrolide Group (n=48) | P-value |
|---|---|---|---|
| Cough Relief Time (Days) | 5.4 ± 1.2 | 7.2 ± 1.6 | < 0.05 |
| Pulmonary Rale Resolution Time (Days) | 6.2 ± 1.3 | 8.0 ± 1.7 | < 0.05 |
| Overall Treatment Efficacy Rate | 88.6% | 75.0% | < 0.05 |
| Fever Resolution Time | No significant difference | No significant difference | > 0.05 |
| Hospitalization Duration | No significant difference | No significant difference | > 0.05 |
| Adverse Event Rate | 18.2% | 16.7% | > 0.05 |
The study demonstrated that doxycycline provided significantly faster resolution of key respiratory symptoms compared to continued macrolide therapy, with comparable safety profiles [8]. Notably, no tooth discoloration—a historical concern with tetracycline use in children—was observed in this cohort, supporting recent guidelines that recognize the favorable risk-benefit profile of short-course doxycycline for resistant M. pneumoniae infections in children [8].
Synergistic Antibiotic Combinations Against Biofilm Structures
The formation of biofilm towers by M. pneumoniae represents a significant challenge for antimicrobial therapy, as these structures confer dramatically increased antibiotic resistance. A 2025 investigation explored eradication strategies for these resilient bacterial communities, testing individual antibiotics and combination therapies against pre-formed biofilm structures [7].
Table 3: Antibiotic Efficacy Against M. pneumoniae Biofilm Towers
| Antibiotic/Combination | Minimum Inhibitory Concentration (MIC) for Planktonic Cells | Efficacy Against Biofilm Towers | Mechanism of Action |
|---|---|---|---|
| Erythromycin (Macrolide) | Reference MIC | 8,500-128,000× less effective (high resistance) | Inhibits protein synthesis |
| Doxycycline (Tetracycline) | Comparable to erythromycin for planktonic cells | Moderate efficacy as monotherapy | Inhibits protein synthesis |
| Moxifloxacin (Fluoroquinolone) | Comparable to erythromycin for planktonic cells | Moderate efficacy as monotherapy | Inhibits DNA replication |
| Erythromycin + Doxycycline | N/A | Synergistic effect (FICI* < 0.5) | Dual protein synthesis inhibition |
| Erythromycin + Moxifloxacin | N/A | Synergistic effect (FICI* < 0.5) | Protein synthesis + DNA replication inhibition |
| Doxycycline + Moxifloxacin | N/A | Synergistic effect (FICI* < 0.5) | Protein synthesis + DNA replication inhibition |
*FICI: Fractional Inhibitory Concentration Index
Checkerboard assays revealed that dual combinations of erythromycin, moxifloxacin, and doxycycline acted synergistically against two strains of M. pneumoniae [7]. Although fluoroquinolones and tetracyclines in children are not preferred over macrolides due to potential side effects, this work demonstrates that synergistic interactions among therapeutic agents provide potential clinical paths to substantially reducing or eradicating M. pneumoniae biofilms, thereby decreasing morbidity [7].
Experimental Protocols for Key Investigations
Checkerboard Assay for Synergistic Antibiotic Interactions
The evaluation of antibiotic combinations against M. pneumoniae follows standardized methodologies that enable quantification of synergistic, additive, or antagonistic effects. The checkerboard broth microdilution assay represents a crucial experimental approach for identifying effective combinations against resistant strains or biofilm structures [7].
Protocol:
- Antibiotic Preparation: Prepare stock solutions of test antibiotics (erythromycin, doxycycline, moxifloxacin) at specified concentrations. Erythromycin stock at 25.6 mg/ml in ethanol; moxifloxacin stock at 2.048 mg/ml in ultra-pure water; doxycycline stock at 20 mg/ml in ultra-pure water [7].
- Bacterial Inoculum: Syringe M. pneumoniae stocks through a 26-g needle multiple times, followed by dilution in SP-4 broth to achieve a final inoculum of 1.0 × 10⁴ CFU/ml for antibiotic testing [7].
- Checkerboard Setup: Dilute antibiotics to start with twice the MIC of each antibiotic. Add decreasing concentrations of both antibiotics to each well of a 96-well plate, except for the last row and column containing only one antibiotic [7].
- Inoculation and Incubation: Inoculate M. pneumoniae in all wells and incubate at 37°C until the growth control changes color from red to yellow in SP-4 medium [7].
- FICI Calculation: Determine the Fractional Inhibitory Concentration Index using the formula: FICI = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone). Synergy is defined as FICI ≤ 0.5 [7].
Biofilm Tower Eradication Assay
The evaluation of antimicrobial agents against M. pneumoniae biofilm structures requires specialized methodologies that account for the unique properties of these organized bacterial communities.
Protocol:
- Biofilm Formation: Grow M. pneumoniae wild-type strains M129 and 19294 in SP-4 broth in 24- or 96-well plates at 37°C for extended periods (several days) to allow distinct mound- or dome-shaped biofilm towers to form [7].
- Antimicrobial Exposure: Expose pre-formed biofilm towers to individual antibiotics or combinations at clinically relevant concentrations. Include H₂O₂ as a model for small molecule therapeutics [7].
- Crystal Violet Staining: Perform crystal violet assays to quantify remaining biofilm biomass after treatment. This provides a quantitative measure of biofilm eradication [7].
- Microscopic Validation: Validate crystal violet results using scanning electron microscopy to visually confirm the eradication of biofilm towers, which often reveals more complete clearance than indicated by staining alone [7].
- Viability Assessment: Combine antibiotic treatments with complementary killing mechanisms (e.g., erythromycin with complement) to assess complete eradication of viable bacteria within biofilm structures [7].
Macrolide Resistance Mechanisms and Therapeutic Implications
The growing challenge of macrolide-resistant M. pneumoniae (MRMP) demands thorough understanding of its underlying mechanisms and clinical consequences. Resistance primarily occurs through point mutations in domain V of the 23S rRNA gene, with nucleotide transitions A2063G and A2064G being most common [2]. These alterations structurally modify the macrolide binding site on the 50S ribosomal subunit, reducing drug affinity and rendering conventional treatments ineffective.
The geographic distribution of MRMP shows striking variation, with resistance rates exceeding 80% in East Asian countries like South Korea, China, and Japan, compared to less than 10% in North America and Europe [2]. This disparity likely reflects regional differences in antibiotic prescribing practices and the clonal expansion of resistant strains, particularly sequence type 3 strains that dominate in high-resistance regions [2].
Despite high-level in vitro resistance, the clinical picture is more nuanced. Many children with MRMP infections experience spontaneous resolution without targeted antibiotic therapy, and macrolide treatment often provides symptomatic benefit even when infections involve resistant strains [5] [2]. This apparent paradox may reflect the immunomodulatory properties of macrolides, their activity against co-pathogens, or the self-limiting nature of many M. pneumoniae infections.
The Researcher's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents for M. pneumoniae Investigation
| Reagent/Material | Specification | Research Application | Key Considerations |
|---|---|---|---|
| SP-4 Broth Medium | Complex undefined medium containing peptone, yeast extract, serum components | Primary culture medium for axenic growth | Supports biofilm tower formation; color change indicates metabolic activity |
| Cell Culture Systems | BEAS-2B respiratory epithelial cells | Host-pathogen interaction studies | Enables investigation of adhesion, cytotoxicity, and biofilm formation on living cells |
| PCR Reagents | Primers targeting P1 adhesin gene, 23S rRNA resistance mutations | Detection, quantification, and resistance profiling | Enables differentiation of macrolide-resistant and sensitive strains |
| Antibiotic Stock Solutions | Erythromycin (25.6 mg/ml in ethanol), Doxycycline (20 mg/ml in water), Moxifloxacin (2.048 mg/ml in water) | Antimicrobial efficacy testing | Vehicle controls essential for ethanol-soluble compounds |
| Biofilm Assessment Tools | Crystal violet stain, Scanning electron microscopy equipment | Biofilm formation and eradication quantification | SEM provides superior visualization of biofilm architecture compared to light microscopy |
| Animal Models | Syrian hamsters, mouse pulmonary infection models | In vivo pathogenesis and therapeutic studies | Limited models due to species specificity of human-pathogenic M. pneumoniae |
The unique wall-less biology of Mycoplasma pneumoniae continues to present formidable challenges for clinical management and therapeutic development. The recent global resurgence following the COVID-19 pandemic hiatus has underscored the persistent public health threat posed by this pathogen, while the inexorable spread of macrolide-resistant strains demands innovative treatment approaches [3] [4].
Promising avenues for future investigation include the development of combination therapies that exploit synergistic antibiotic interactions to overcome biofilm-mediated resistance [7]. Additionally, targeting the adhesion and motility apparatus represents an attractive strategy that could prevent initial colonization and interrupt disease progression [1] [6]. As our understanding of the molecular mechanisms underlying M. pneumoniae pathogenesis continues to deepen, particularly the function of the terminal organelle and its role in immune evasion, new opportunities for therapeutic intervention will undoubtedly emerge.
The self-limiting nature of many M. pneumoniae infections, coupled with the growing challenge of antibiotic resistance, suggests that future management strategies may increasingly focus on immunomodulatory approaches rather than purely antimicrobial interventions. Nevertheless, the continued evolution of this minimalist pathogen ensures that it will remain a significant subject of clinical concern and scientific fascination for years to come.
Macrolide-resistant Mycoplasma pneumoniae (MRMP) has emerged as a significant global public health challenge, particularly in the management of community-acquired pneumonia. The epidemiology of MRMP demonstrates stark geographical variations, with notably high resistance rates in East Asia compared to Western nations. This phenomenon is primarily driven by point mutations in the 23S rRNA gene, which reduce macrolide binding affinity and compromise treatment efficacy. The COVID-19 pandemic temporarily disrupted transmission dynamics through non-pharmaceutical interventions, but recent surveillance data indicate a pronounced post-pandemic resurgence of M. pneumoniae infections, including macrolide-resistant strains. Understanding these global patterns is essential for developing targeted surveillance, stewardship programs, and treatment guidelines to address this evolving threat.
Global Prevalence and Regional Distribution
The prevalence of macrolide-resistant M. pneumoniae exhibits dramatic geographical disparities, with the highest burden concentrated in East Asia.
Table 1: Global Prevalence of Macrolide-Resistant M. pneumoniae (MRMP)
| World Health Organization Region | MRMP Prevalence (%) | Key Countries/Regions with Reported Data |
|---|---|---|
| Western Pacific | 53.4% | China, Japan, South Korea |
| South East Asia | 9.8% | Limited data available |
| Americas | 8.4% | United States |
| Europe | 5.1% | Southern Italy, France |
Recent studies from specific regions provide more granular data on resistance patterns:
- Southern Italy (2023-2025): A comprehensive study reported an overall MRMP rate of 7.5%, with the highest prevalence observed in preadolescents aged 10-14 years (12.6%). The majority (96%) of resistant strains harbored the A2063G mutation. [10]
- China: Resistance rates remain exceptionally high. A 2025 study from Xi'an reported that 100% of cultured isolates harbored the A2063G mutation in the 23S rRNA gene, with phenotypic resistance to macrolides observed in 38.6% of cases. [11] Earlier multicenter studies in Chinese adults demonstrated resistance rates as high as 80% against erythromycin and 72% against azithromycin. [12]
- Japan (Osaka): Surveillance data from 2024 indicate a resurgence of MRMP following the COVID-19 pandemic, with resistance rates climbing again to 65.2% after a period of decline during peak intervention periods. [13]
Table 2: Recent Regional Surveillance Data on MRMP
| Region | Time Period | Study Population | Resistance Rate | Predominant Mutation |
|---|---|---|---|---|
| Southern Italy | 2023-2025 | All ages (median: 10 years) | 7.5% | A2063G (96%) |
| Xi'an, China | 2023 | Hospitalized children | 38.6% (phenotypic) | A2063G (100% genotypic) |
| Osaka, Japan | 2024 | Pediatric patients | 65.2% | A2063G |
| Beijing, China | 2011-2017 | Adult patients | 41.7% | A2063G |
Molecular Mechanisms of Macrolide Resistance
The primary mechanism of macrolide resistance in M. pneumoniae involves target site modification through point mutations in domain V of the 23S rRNA gene, which codes for the macrolide binding site on the bacterial ribosome.
Key Genetic Mutations
The most prevalent mutations occur at specific positions in the 23S rRNA gene:
- A2063G transition: This is the most common resistance mutation globally, accounting for approximately 96.8% of resistant strains. This mutation confers high-level resistance to 14- and 15-membered macrolides (erythromycin, azithromycin, clarithromycin) and intermediate resistance to 16-membered macrolides. [14] [9]
- A2064G transition: The second most frequent mutation, representing about 4.8% of cases, also resulting in high-level macrolide resistance. [9]
- Less common mutations: Including A2063C, A2063T, A2067G, and C2617G, which are rarely observed in clinical isolates. [14]
These mutations reduce binding affinity between macrolide antibiotics and the ribosomal target site, preventing inhibition of protein synthesis.
Additional Resistance Mechanisms
While target site mutations represent the primary resistance mechanism, emerging research suggests supplementary pathways:
- Efflux pump mechanisms: A 2025 study from Beijing identified two clinical isolates carrying efflux pump genes (msrA/B and mefA). When exposed to the efflux pump inhibitor reserpine, the minimum inhibitory concentration (MIC) for azithromycin decreased to a quarter of the original values, confirming functional contribution to resistance. [15]
- Ribosomal protein mutations: Mutations in genes encoding ribosomal proteins L4 and L22 have been associated with low-level macrolide resistance in laboratory-selected mutants, though these are rarely reported in clinical isolates. [14]
Diagram Title: Molecular Mechanisms of Macrolide Resistance in M. pneumoniae
Detection Methodologies and Experimental Protocols
Accurate detection of macrolide resistance is crucial for appropriate clinical management and epidemiological surveillance. The following section details standardized laboratory protocols.
Molecular Detection of Resistance Mutations
Protocol: PCR Amplification and Sequencing of 23S rRNA Domain V
- Sample Preparation: Respiratory specimens (nasopharyngeal swabs, bronchoalveolar lavage fluid, or throat swabs) are collected and transported in appropriate medium. Nucleic acids are extracted using commercial kits (e.g., QIAamp DNA Mini kit, STARMag Universal Cartridge kit). [10] [15]
- PCR Amplification: Amplify domain V of the 23S rRNA gene using specific primers. A typical reaction mixture includes DNA template (2-5 µL), PCR reaction mix (40-45 µL), and Taq enzyme (3 µL). Cycling conditions: initial denaturation at 93°C for 2 minutes, followed by 10 cycles of 93°C for 45 seconds, 55°C for 1 minute, then 30 cycles of 93°C for 30 seconds and 55°C for 10 minutes. [12]
- Sequencing and Analysis: PCR products are purified and sequenced using Sanger sequencing. Sequences are aligned with reference strains using software such as BioEdit and MEGA to identify point mutations at positions 2063, 2064, and 2617. [10]
Culture and Phenotypic Susceptibility Testing
Protocol: Broth Microdilution Method for MIC Determination
- Culture Conditions: Inoculate respiratory specimens into PPLO broth medium supplemented with horse serum, yeast extract, and glucose. Incubate at 37°C with 5% CO₂ for 2-3 weeks, monitoring for color change (red to yellow) indicating growth. Subculture positive samples onto solid PPLO agar for colony isolation. [11]
- MIC Testing: Prepare serial dilutions of antimicrobial agents (erythromycin, azithromycin, tetracycline, fluoroquinolones) in microtiter plates. Inoculate wells with standardized bacterial suspension. Incubate plates at 37°C until growth is visible in control wells (typically 24-48 hours). The MIC is defined as the lowest antibiotic concentration that prevents color change. [12] [15]
- Interpretive Criteria: Resistance breakpoints vary by antibiotic: Erythromycin (≥1 µg/mL), Azithromycin (≥1 µg/mL), Tetracycline (≤2 µg/mL), Moxifloxacin (≤0.5 µg/mL). [12]
Diagram Title: MRMP Detection and Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for MRMP Investigation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Culture Media | PPLO Broth, PPLO Agar (Oxoid) | Culture and isolation of M. pneumoniae from clinical specimens; growth indicated by color change with phenol red indicator. [12] [11] |
| Molecular Detection Kits | Allplex Respiratory Panel Assays, PCR Fluorescence Probing Kit (Zhi-Jiang) | Multiplex real-time PCR detection of M. pneumoniae and other respiratory pathogens; includes primer sets for specific target amplification. [10] [12] |
| Nucleic Acid Extraction Kits | QIAamp DNA Mini Kit (Qiagen), STARMag Universal Cartridge Kit (Seegene) | Extraction of high-quality DNA from clinical samples for downstream molecular applications including PCR and sequencing. [10] [15] |
| Antibiotics for Susceptibility Testing | Erythromycin, Azithromycin, Midecamycin, Tetracycline, Moxifloxacin | Reference standards for determining minimum inhibitory concentrations (MICs) using broth microdilution methods. [12] [15] |
| Sequencing Reagents | BioEdit, MEGA software, CLC Sequence Viewer | Analysis of sequence data for identification of resistance-conferring mutations in target genes (23S rRNA). [10] [12] |
| Specialized Equipment | MALDI-TOF MS (QuanTOF I), Real-time PCR systems (ABI Prism 7500) | Genotype identification through mass spectrometry; quantitative PCR for pathogen detection and bacterial load determination. [12] [11] |
Treatment Alternatives and Clinical Management
With rising macrolide resistance, particularly in East Asia, alternative treatment strategies have become increasingly important for effective clinical management.
Alternative Antimicrobial Agents
- Tetracyclines: Doxycycline and minocycline demonstrate excellent activity against MRMP with no reported resistance in clinical isolates. These agents are effective alternatives for older children and adults but are typically avoided in young children due to potential effects on bone and tooth development. [12] [14]
- Fluoroquinolones: Moxifloxacin and levofloxacin maintain efficacy against MRMP and serve as valuable alternatives, particularly for adults. However, their use in children is restricted due to concerns about potential effects on cartilage development. Recent surveillance has detected strains with elevated MICs nearing resistance breakpoints, suggesting emerging resistance may become a future concern. [12] [14]
- 16-membered macrolides: Midecamycin, a 16-membered ring macrolide, has shown promising activity against some azithromycin-resistant strains (MIC90: 16 µg/mL) and may represent a treatment option, particularly for pediatric patients where tetracyclines and fluoroquinolones are contraindicated. [15]
Adjunctive Therapies
For refractory MRMP pneumonia characterized by excessive immune activation, immunomodulatory agents may be beneficial:
- Corticosteroids: Used to dampen excessive inflammatory response and immune-mediated pulmonary injury in severe cases. [14]
- Intravenous Immunoglobulin (IVIG): May be beneficial in modulating host immune responses in severe, refractory cases. [14]
The selection of alternative agents must consider patient age, severity of illness, local resistance patterns, and potential adverse effects, highlighting the importance of antimicrobial stewardship programs to optimize treatment outcomes while minimizing further resistance development.
The global epidemiology of macrolide-resistant M. pneumoniae presents a complex and evolving challenge with significant geographical disparities. The high resistance rates in East Asia compared to Western regions underscore the impact of regional antibiotic practices and surveillance systems. The primary mechanism of resistance involves point mutations in the 23S rRNA gene, with the A2063G transition mutation dominating globally. Advanced molecular techniques combined with traditional culture methods provide comprehensive tools for detection and characterization. As MRMP infections resurge following the COVID-19 pandemic, continued surveillance, judicious antibiotic use, and consideration of alternative treatment approaches will be essential to mitigate the impact of this resistant pathogen on public health worldwide.
Molecular Mechanisms of Resistance: Mutations in the 23S rRNA Gene (A2063G and A2064G) represents a critical area of investigation within antimicrobial resistance research. These specific point mutations within the peptidyl transferase loop of domain V in the 23S ribosomal RNA (rRNA) gene constitute the primary mechanism of macrolide resistance in Mycoplasma pneumoniae [14]. The rising global prevalence of these mutations, particularly in Asian countries where resistance rates approach 80-90%, directly compromises the clinical efficacy of first-line macrolide antibiotics and presents substantial challenges for managing respiratory infections [14] [16]. This guide systematically compares how these mutations impact mycoplasma removal efficacy across different antibiotic classes, providing researchers and drug development professionals with synthesized experimental data and methodologies essential for advancing therapeutic strategies.
Molecular Basis of 23S rRNA Mutations and Macrolide Resistance
Mechanism of Antibiotic Action and Resistance
Macrolide antibiotics, including erythromycin, clarithromycin, and azithromycin, exert their antibacterial effect by binding to the 50S ribosomal subunit. This binding occurs specifically within the nascent peptide exit tunnel of the ribosome, adjacent to the peptidyl transferase center [14]. The binding site predominantly involves domain V of the 23S rRNA, where macrolides physically block the elongation of the growing polypeptide chain, thereby inhibiting bacterial protein synthesis and preventing bacterial replication [17].
The acquisition of macrolide resistance in Mycoplasma pneumoniae occurs almost exclusively through point mutations that modify this binding site [14]. Unlike many other bacterial pathogens that utilize efflux mechanisms or enzymatic modification of antibiotics, M. pneumoniae resistance is primarily mediated through target site modification via mutations in the 23S rRNA gene [14]. The most prevalent mutations involve single nucleotide transitions at positions A2063G and A2064G (Escherichia coli numbering system) within domain V [18]. These nucleotide substitutions induce conformational changes in the ribosome that reduce macrolide binding affinity through steric hindrance and alteration of critical interaction points [19].
Structural Consequences of Mutations
The molecular mechanisms by which A2063G and A2064G mutations confer resistance have been elucidated through structural and biochemical studies. The A2063G transition introduces a guanine residue that possesses an additional exocyclic 2-amino group compared to the wild-type adenine. This amino group sterically hinders optimal positioning of macrolide molecules within the binding pocket, creating physical interference that disrupts drug-ribosome interactions [19]. Similarly, the A2064G mutation introduces comparable steric constraints, though with somewhat different effects on binding affinity.
Computational modeling based on crystallographic data reveals that these mutations cause significant van der Waals overlaps between the rRNA and the macrolide structure [19]. The A2063G mutation produces more substantial steric hindrance than A2064G, correlating with observed higher levels of resistance for the A2063G mutation [14] [20]. When both mutations occur together (double mutation), they act synergistically to create more profound conformational changes in the ribosomal binding site, resulting in even greater resistance levels compared to either single mutation alone [20].
Figure 1: Mechanism of Macrolide Resistance Due to 23S rRNA Mutations. This diagram illustrates how A2063G/A2064G mutations in the 23S rRNA gene prevent macrolide binding to the ribosomal target site, allowing ongoing protein synthesis in resistant strains.
Global Prevalence and Distribution Patterns
The prevalence of macrolide-resistant Mycoplasma pneumoniae (MRMP) harboring A2063G and A2064G mutations demonstrates significant geographical variation, reflecting regional differences in antibiotic usage practices and surveillance systems.
Table 1: Global Prevalence of Macrolide-Resistant Mycoplasma pneumoniae
| Region | Resistance Prevalence (%) | Most Common Mutation | Trend | Key References |
|---|---|---|---|---|
| East Asia | 62-96.4% | A2063G (77%) | Stable at high levels | [16] [20] [21] |
| United States | 2.4-9% | A2063G (>95%) | Increasing post-pandemic | [21] |
| Europe | 5-6% | A2063G (5%) | Stable at low levels | [16] [21] |
| Iran | 0% in studied cohort | Not detected | Not established | [22] |
Recent surveillance data indicates an alarming reemergence of MRMP following the COVID-19 pandemic. A 2025 study from Ohio, USA, documented a significant increase in cases, with resistance rates rising from 0.7% in June 2024 to 4.4% by September 2024 [21]. This represents a substantial increase compared to the pre-pandemic resistance rate of 2.8% reported in the same pediatric population [21]. Similarly, a 2025 systematic review and meta-analysis encompassing 53 studies and 8,960 individuals confirmed the persistently high resistance rates in Asia (62%) compared to Europe (6%) and America (9%) [16] [20].
The A2063G transition is unequivocally the dominant resistance mechanism worldwide, accounting for approximately 67% of resistant cases globally [16]. The A2064G mutation occurs less frequently, with a global pooled prevalence of only 3% [16]. The concurrent presence of both A2063G and A2064G (double mutation) is relatively rare but clinically significant due to its association with more severe disease manifestations and higher levels of resistance [20].
Comparative Antibiotic Efficacy Against Mutated Strains
Macrolides and Their Limitations
Macrolide antibiotics demonstrate markedly reduced efficacy against M. pneumoniae strains harboring A2063G and A2064G mutations. The resistance mechanism profoundly impacts clinical outcomes, as evidenced by treatment failure, prolonged symptomatology, and extended hospitalization.
Table 2: Antibiotic Efficacy Against Mycoplasma pneumoniae with 23S rRNA Mutations
| Antibiotic Class | Example Agents | Mechanism of Action | Efficacy Against Wild-Type Strains | Efficacy Against A2063G/A2064G Mutants | Resistance Mechanism |
|---|---|---|---|---|---|
| Macrolides | Azithromycin, Clarithromycin, Erythromycin | Binds to 23S rRNA, inhibits protein synthesis | High (First-line treatment) | Severely compromised | Target site modification (A2063G/A2064G) |
| Tetracyclines | Doxycycline, Minocycline | Binds to 30S ribosomal subunit | Moderate (Second-line) | Maintained efficacy | No cross-resistance reported |
| Fluoroquinolones | Levofloxacin | Inhibits DNA gyrase and topoisomerase IV | Moderate (Second-line) | Maintained efficacy | No cross-resistance reported |
| Ketolides | Telithromycin | Binds to 23S rRNA with higher affinity | High | Variable, some retained activity | Enhanced ribosomal binding |
Clinical studies directly correlate these mutations with refractory disease courses. Patients infected with MRMP strains experience significantly longer fever duration (HR = 3.72 for all genotypes), extended hospital stays, and increased risk of severe disease progression compared to those with macrolide-sensitive strains [20]. The meta-analysis by Frontiers in Pharmacology (2025) further established that double mutations (A2063G + A2064G) confer more severe clinical outcomes compared to single mutations, including prolonged fever duration (HR = 5.32 versus 3.66) and higher likelihood of severe illness (HR = 7.80 versus 5.89) [20].
Comparative clinical studies between different macrolides have demonstrated variability in treatment outcomes. A 2021 study comparing clarithromycin versus erythromycin for pediatric respiratory mycoplasma infections found superior outcomes with clarithromycin, including higher MP-PCR negative rates (96.23% vs. 75.47%), shorter antipyretic time (2.63 vs. 4.06 days), reduced hospitalization duration (15.14 vs. 20.63 days), and lower incidence of adverse effects [23].
Alternative Antibiotic Classes
For infections with MRMP, tetracyclines (doxycycline, minocycline) and fluoroquinolones (levofloxacin) represent effective alternative therapeutic options as they do not exhibit cross-resistance with macrolides [14]. These antibiotic classes target different bacterial components—tetracyclines bind to the 30S ribosomal subunit while fluoroquinolones inhibit DNA gyrase and topoisomerase IV—allowing them to bypass the resistance conferred by 23S rRNA mutations [14].
Importantly, systematic surveillance has not detected acquired resistance to tetracyclines or fluoroquinolones in MRMP clinical isolates, supporting their utility as second-line agents [14]. However, usage limitations exist for these antibiotic classes in pediatric populations due to potential side effects: tetracyclines are typically avoided in children under 8 years due to tooth discoloration risk, while fluoroquinolones have restrictions in growing children due to cartilage development concerns [14].
Experimental Protocols for Detection and Analysis
Molecular Detection of Resistance Mutations
Protocol 1: PCR Amplification and Sequencing of 23S rRNA Domain V
This method represents the gold standard for detecting A2063G and A2064G mutations with high specificity and reliability.
DNA Extraction: Extract genomic DNA from clinical samples (throat swabs or cultured isolates) using commercial kits such as the High Pure PCR Template Preparation Kit (Roche) [22]. Begin with 200μL of sample and elute in 50-100μL of elution buffer.
PCR Amplification: Prepare 25μL reaction mixtures containing:
- 2.5μL 10X PCR buffer
- 1.5μL MgCl₂ (25mM)
- 0.5μL dNTPs (10mM each)
- 0.5μL each forward and reverse primer (10μM)
- 0.2μL Taq DNA polymerase (5U/μL)
- 2μL DNA template
- 17.3μL nuclease-free water
Primer sequences for 23S rRNA domain V:
- Forward: 5'-TAACTATAACGGTCCTAAGG-3'
- Reverse: 5'-GCTACAACTGGAGCATAAGA-3' [22]
Thermocycling Conditions:
- Initial denaturation: 94°C for 4 minutes
- 35 cycles of:
- Denaturation: 94°C for 45 seconds
- Annealing: 55°C for 45 seconds
- Extension: 72°C for 50 seconds
- Final extension: 72°C for 5 minutes
Product Analysis: Verify amplification by electrophoresis on 1.5% agarose gel; expected product size is 793bp [22].
Sequencing: Purify PCR products using commercial kits and perform Sanger sequencing with the same amplification primers. Analyze sequences using alignment software (e.g., ClustalW2) to identify A2063G and A2064G mutations [22].
Figure 2: Experimental Workflow for Detecting 23S rRNA Mutations. This diagram outlines the key steps in identifying A2063G and A2064G mutations in Mycoplasma pneumoniae clinical isolates, from sample collection to final mutation reporting.
Protocol 2: Broth Microdilution for Minimum Inhibitory Concentration (MIC) Determination
This phenotypic method quantitatively measures macrolide resistance levels.
Bacterial Inoculum Preparation: Grow M. pneumoniae in PPLO broth medium enriched with horse serum and glucose for 5-7 days until color change indicates adequate growth. Standardize inoculum to 1-5×10⁵ CFU/mL [22].
Antibiotic Preparation: Prepare doubling dilutions of clarithromycin (or other macrolides) in enriched PPLO broth in 96-well microtiter plates. Typical concentration range: 0.000125-512 μg/mL [22].
Inoculation and Incubation: Add standardized bacterial inoculum to each well. Include growth control (no antibiotic) and sterility control (no inoculum) wells. Seal plates and incubate at 37°C for 5-7 days under appropriate atmospheric conditions [22].
MIC Determination: Read plates when color change occurs in growth control well. The MIC is defined as the lowest antibiotic concentration that prevents color change (indicating no bacterial growth) [22]. Interpret results according to CLSI breakpoints where available.
Quality Control: Include reference strains with known MIC values (e.g., M. pneumoniae ATCC 29342) with each assay run [22].
Comparative Efficacy Study Design
Protocol 3: Clinical Treatment Response Assessment
This protocol outlines a standardized approach for comparing antibiotic efficacy in clinical settings.
Patient Selection and Grouping: Enroll patients with confirmed M. pneumoniae infection (positive by PCR) and randomize into treatment groups using a random number table. Ensure comparable baseline characteristics between groups (age, gender, illness severity) [23].
Treatment Administration:
Efficacy Evaluation:
Statistical Analysis: Compare outcomes between groups using appropriate statistical tests (chi-square for categorical variables, t-tests for continuous variables) with significance set at p<0.05 [23].
Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating 23S rRNA Mutations
| Reagent/Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| DNA Extraction Kits | High Pure PCR Template Preparation Kit (Roche) | Isolation of high-quality genomic DNA from clinical samples | Efficient removal of PCR inhibitors; suitable for small sample volumes |
| PCR Reagents | Taq DNA polymerase, dNTPs, specific primers for 23S rRNA domain V | Amplification of target resistance region | High fidelity amplification; optimized for GC-rich regions |
| Culture Media | PPLO broth with horse serum and glucose | Propagation of Mycoplasma pneumoniae isolates | Supports fastidious growth of mycoplasma species |
| Antibiotic Standards | Clarithromycin, azithromycin, erythromycin, doxycycline, levofloxacin | MIC determination and resistance profiling | Pharmaceutical grade; precisely quantified potency |
| Sequencing Reagents | BigDye Terminators, cycle sequencing kits | Mutation detection and confirmation | High accuracy base calling; compatible with automated sequencers |
| Reference Strains | M. pneumoniae ATCC 29342 | Quality control in resistance testing | Genotype and phenotype well-characterized |
| Commercial Detection Kits | PCR-RFLP kits, real-time PCR kits with HRM analysis | Rapid screening for A2063G/A2064G mutations | High-throughput capability; reduced turnaround time |
The A2063G and A2064G mutations in the 23S rRNA gene represent a formidable challenge in the management of Mycoplasma pneumoniae infections, rendering first-line macrolide antibiotics increasingly ineffective, particularly in regions with high resistance prevalence. The comprehensive analysis presented in this guide demonstrates that these mutations significantly impair mycoplasma removal efficacy of macrolides, necessitating alternative treatment approaches including tetracyclines and fluoroquinolones that maintain activity against resistant strains. Researchers and drug development professionals must prioritize ongoing surveillance of these mutations, development of rapid diagnostic methods for their detection, and investigation of novel antimicrobial agents that circumvent this resistance mechanism. The experimental protocols and comparative data provided herein offer foundational methodologies for advancing these critical research objectives aimed at addressing the expanding challenge of macrolide-resistant M. pneumoniae.
Biofilm formation represents a fundamental virulence strategy for bacterial pathogens, creating protected communities that exhibit dramatically enhanced antibiotic resistance while simultaneously attenuating virulence factor production to facilitate persistent infections. This review synthesizes current findings on the mechanistic basis of biofilm-mediated resistance, examining the synergistic roles of physical diffusion barriers, metabolic heterogeneity, and persister cell formation. We specifically contextualize these principles within Mycoplasma pneumoniae biofilm research, comparing the efficacy of conventional and novel therapeutic strategies. Quantitative analysis reveals that biofilms can increase antibiotic minimum inhibitory concentrations by several orders of magnitude compared to planktonic cells, presenting formidable challenges for clinical management. Emerging anti-virulence approaches that target quorum sensing systems and biofilm dispersion mechanisms offer promising alternatives to traditional bactericidal strategies, potentially reducing selective pressure for resistance development while effectively disrupting pathogenic communities.
Bacterial biofilms are immobile, three-dimensional aggregates of microorganisms encased in a self-produced extracellular matrix that adhere to biological or inert surfaces [24] [25]. This structured mode of growth represents a primary virulence mechanism for numerous pathogens, enabling persistent colonization and chronic infections that are remarkably refractory to antimicrobial therapy and host immune responses [26]. The biofilm lifecycle progresses through defined stages: initial reversible attachment, irreversible attachment, microcolony formation, maturation, and active dispersal [25]. During maturation, bacteria undergo significant physiological changes and secrete extracellular polymeric substances (EPS) that can constitute over 90% of the biofilm's dry mass, creating a protective microenvironment [24].
The clinical significance of biofilms is substantial, with an estimated 65% of all bacterial infections and nearly 80% of chronic wounds involving biofilm components [24]. These infections contribute significantly to healthcare costs, with recent analyses estimating the global economic impact of biofilms exceeds $280 billion annually [24]. Biofilms pose particular challenges in device-associated infections (catheters, prosthetic joints, pacemakers) and chronic conditions such as cystic fibrosis, where they underlie persistent inflammation and tissue damage despite aggressive antibiotic therapy [25] [26].
Mycoplasma pneumoniae, a common cause of community-acquired respiratory infections, exemplifies the clinical challenges posed by biofilm-forming pathogens. This cell wall-deficient bacterium forms distinctive biofilm towers during prolonged infection, exhibiting dramatically increased resistance to macrolide antibiotics and complement-mediated host defenses [27]. Understanding the interplay between biofilm-mediated antibiotic resistance and virulence attenuation in M. pneumoniae and other pathogens is essential for developing effective therapeutic countermeasures.
Mechanisms of Enhanced Antibiotic Resistance in Biofilms
Biofilms employ multiple concurrent strategies to achieve remarkable levels of antibiotic tolerance, often exhibiting 10 to 1,000-fold increases in minimal inhibitory concentrations (MICs) compared to their planktonic counterparts [26]. These resistance mechanisms operate synergistically to protect the bacterial community, representing a multifaceted defense system that poses significant challenges for antimicrobial therapy.
Physical Barrier Function and Reduced Antimicrobial Penetration
The extracellular matrix serves as a formidable physical barrier that significantly impedes antibiotic penetration through several mechanisms. The matrix composition—including polysaccharides, proteins, extracellular DNA (eDNA), and lipids—creates a dense, negatively charged network that can bind and sequester antimicrobial agents [24] [28]. Positively charged aminoglycosides, for example, readily interact with anionic eDNA components, effectively reducing their diffusion into deeper biofilm layers [25]. Additionally, extracellular enzymes within the matrix, such as β-lactamases, can inactivate antibiotics faster than they can diffuse through the biofilm, creating a protective gradient [24]. The reduced and heterogeneous penetration of antimicrobials results in sub-inhibitory concentrations in the biofilm interior, enabling bacterial survival despite apparently adequate dosing [24].
Metabolic Heterogeneity and Persister Cell Formation
Biofilms develop distinct metabolic microenvironments due to nutrient and oxygen gradients from the periphery to the core. This physiological heterogeneity generates subpopulations with varying growth rates and metabolic activities [24] [25]. Cells in nutrient-depleted zones enter slow-growing or dormant states, reducing their susceptibility to antibiotics that primarily target active cellular processes [24]. The deepest biofilm layers are particularly exposed to nutrient-depleted conditions due to diffusion barriers and consumption by peripheral cells, making these regions hotspots for antibiotic tolerance [24]. Within these heterogeneous populations, specialized "persister" cells exhibit multidrug tolerance without genetic mutation [25] [26]. These dormant variants can survive extreme antibiotic challenges and repopulate the biofilm once antibiotic pressure diminishes, contributing significantly to chronic and recurrent infections [25] [28].
Efflux Pump Regulation and Genetic Adaptation
Efflux pumps, which actively export antibiotics from bacterial cells, demonstrate spatially distinct expression patterns within biofilms [24]. In Pseudomonas aeruginosa biofilms, for instance, specific antibiotic resistance pumps are upregulated in upper regions while showing no change or downregulation in middle sections [24]. This heterogeneous expression creates specialized zones of enhanced antibiotic extrusion. Furthermore, the close proximity of cells within the biofilm matrix facilitates efficient horizontal gene transfer, enabling the dissemination of resistance determinants throughout the community [25]. Bacteria in biofilms can also undergo global transcriptional reprogramming via mechanisms such as the multiple antibiotic resistance (mar) operon in Escherichia coli, which coordinately regulates expression of various genes to establish a multidrug-resistant phenotype [28].
Table 1: Key Mechanisms of Antibiotic Resistance in Biofilms
| Resistance Mechanism | Key Components | Functional Impact | Representative Pathogens |
|---|---|---|---|
| Physical Barrier | EPS matrix, eDNA, polysaccharides | Binds antibiotics, reduces penetration, enzymatic inactivation | Pseudomonas aeruginosa, Staphylococcus aureus |
| Metabolic Heterogeneity | Nutrient/oxygen gradients, slow-growing cells | Reduced susceptibility to growth-dependent antibiotics | Escherichia coli, Mycoplasma pneumoniae |
| Persister Cells | Dormant bacterial subpopulations | Transient multidrug tolerance, biofilm regeneration | S. aureus, P. aeruginosa |
| Efflux Pumps | Membrane transport proteins | Active antibiotic extrusion, zone-specific protection | P. aeruginosa, Klebsiella pneumoniae |
| Genetic Adaptation | Horizontal gene transfer, stress responses | Stable resistance development, community-wide protection | ESKAPE pathogens |
Attenuated Virulence Factor Production in Biofilms
The biofilm lifestyle involves a strategic trade-off between protection and pathogenicity, with many pathogens downregulating virulence factor production during biofilm growth to facilitate long-term persistence. This virulence attenuation represents an adaptive response that minimizes excessive host damage and immune activation while maintaining colonization.
Metabolic Reprogramming in Biofilm Communities
As biofilms mature, nutrient availability becomes limited due to high cell density and diffusion barriers, triggering global metabolic changes that impact virulence gene expression [24] [28]. In M. pneumoniae, biofilm formation is associated with significant attenuation of key virulence factors, including hydrogen peroxide (H₂O₂), hydrogen sulfide (H₂S), and the ADP-ribosylating and vacuolating CARDS toxin [27]. This coordinated downregulation likely reflects resource allocation toward maintenance and matrix production rather than aggressive host damage. Notably, M. pneumoniae biofilm towers show no protection against exogenous H₂O₂ despite reduced endogenous production, suggesting that virulence attenuation is a specific adaptation rather than general metabolic suppression [27].
Quorum Sensing-Mediated Virulence Regulation
Bacteria within biofilms utilize quorum sensing (QS) systems to coordinate gene expression in a population-density-dependent manner [24] [29]. These chemical communication networks precisely regulate the production of virulence factors to optimize host-pathogen interactions. Gram-negative bacteria typically employ acyl-homoserine lactones, while gram-positive species use autoinducing peptides as signaling molecules [24]. In P. aeruginosa, the pqs QS system directly controls the production of elastase, pyocyanin, and other exoproducts [30]. During biofilm development, QS systems can shift from expressing acute virulence factors to promoting persistence traits, balancing the requirements for initial colonization and long-term maintenance [24] [29].
Diagram 1: Quorum sensing regulation of virulence and biofilm formation. Quorum sensing systems coordinate virulence factor production, matrix formation, and persister cell development in response to environmental cues, including host factors and antibiotic exposure. QS inhibitors such as wogonin can disrupt this signaling network.
Mycoplasma pneumoniae Biofilms: A Case Study in Chronic Infection
M. pneumoniae provides a compelling model for understanding the clinical implications of biofilm formation in chronic respiratory infections. This pathogen forms distinctive mound- or dome-shaped biofilm towers during prolonged growth, both axenically and on respiratory epithelial cells [27]. These structures exhibit characteristics highly relevant to chronic disease, including extreme antibiotic resistance and complement evasion.
Antibiotic Resistance Profiles in M. pneumoniae Biofilms
M. pneumoniae biofilms demonstrate staggering levels of macrolide resistance, with biofilm-embedded bacteria surviving erythromycin concentrations up to 512 µg/mL—approximately 8,500-128,000 times the MIC for planktonic cells [27]. This resistance emerges progressively as biofilms mature, suggesting developmental regulation rather than constitutive protection. The resistance spectrum varies among antibiotic classes, with fluoroquinolones and tetracyclines retaining some activity against biofilm-resident bacteria, particularly when used in combination [27].
Table 2: Antibiotic Efficacy Against Mycoplasma pneumoniae Biofilms
| Antibiotic Class | Representative Agent | MIC (Planktonic) | MIC (Biofilm) | Resistance Fold-Increase | Synergistic Combinations |
|---|---|---|---|---|---|
| Macrolides | Erythromycin | 0.004-0.06 µg/mL | 512 µg/mL | 8,500-128,000× | Erythromycin + Moxifloxacin |
| Fluoroquinolones | Moxifloxacin | 0.03-0.25 µg/mL | 4-8 µg/mL | 100-250× | Moxifloxacin + Doxycycline |
| Tetracyclines | Doxycycline | 0.125-0.5 µg/mL | 8-16 µg/mL | 60-130× | Doxycycline + Erythromycin |
| Combination Therapy | Erythromycin + Moxifloxacin | - | - | - | 85-95% biofilm eradication |
Novel Therapeutic Approaches for M. pneumoniae Biofilms
Conventional monotherapy often fails against established M. pneumoniae biofilms, necessitating alternative treatment strategies. Checkerboard assays have revealed strong synergistic interactions between antibiotic classes, with dual combinations of erythromycin, moxifloxacin, and doxycycline achieving substantial eradication of pre-formed biofilm towers [27]. These combinations demonstrate efficacy at clinically achievable concentrations, suggesting potential translational applications. Interestingly, M. pneumoniae biofilms show no enhanced resistance to hydrogen peroxide despite producing this compound as a virulence factor during planktonic growth [27]. This vulnerability to oxidative stress may represent an exploitable therapeutic weakness for biofilm-associated infections.
Experimental Models and Methodologies for Biofilm Research
Robust experimental systems are essential for investigating biofilm biology and evaluating potential therapeutic interventions. Standardized assays and model systems have been developed to quantify biofilm formation, antibiotic resistance, and virulence factor production under controlled conditions.
Biofilm Cultivation and Assessment Techniques
M. pneumoniae biofilm towers are typically cultured in SP-4 broth in 24- or 96-well plates over several days, forming distinct mound- or dome-shaped structures [27]. Crystal violet staining provides a quantitative measure of biofilm biomass, while scanning electron microscopy offers detailed visualization of three-dimensional architecture and cellular organization [27]. For antibiotic susceptibility testing, minimum inhibitory concentration (MIC) assays are conducted according to established guidelines for fastidious microorganisms, with serial dilutions of antimicrobial agents in appropriate growth media [27]. Color change indicators in the growth medium facilitate determination of metabolic activity and growth inhibition endpoints.
Virulence Factor Quantification Methods
The attenuated production of virulence factors in biofilms can be quantified through various specialized assays. Hydrogen peroxide production is measured using colorimetric or fluorometric peroxidase-based assays, while cytotoxic effects on eukaryotic cells can be evaluated through lactate dehydrogenase release assays or direct viability staining [27]. For M. pneumoniae, CARDS toxin production can be assessed through immunological methods or ADP-ribosylating activity measurements. Comparative transcriptomics and proteomics provide comprehensive profiles of gene expression differences between biofilm and planktonic populations, identifying key regulatory switches in virulence pathways [27].
Diagram 2: Experimental workflow for Mycoplasma pneumoniae biofilm research. The methodology involves standardized inoculation procedures, extended incubation to permit biofilm tower development, and multiple assessment techniques to quantify biofilm characteristics, antibiotic resistance, and virulence factor production.
Therapeutic Strategies: Conventional Antibiotics and Anti-Virulence Approaches
The formidable resistance mechanisms employed by biofilms necessitate innovative therapeutic strategies that extend beyond conventional antibiotic monotherapy. Current approaches include optimized antibiotic combinations and emerging anti-virulence compounds that target specific biofilm maintenance pathways.
Antibiotic Combinations with Enhanced Biofilm Activity
Synergistic antibiotic combinations demonstrate significantly improved efficacy against biofilms compared to individual agents. For M. pneumoniae, dual combinations of erythromycin with moxifloxacin, erythromycin with doxycycline, or moxifloxacin with doxycycline achieve 85-95% eradication of pre-formed biofilm towers at clinically relevant concentrations [27]. Similar synergistic interactions have been reported for other bacterial pathogens, including S. aureus and P. aeruginosa, particularly when combining agents with different mechanisms of action and divergent resistance pathways [31]. These combinations appear to target multiple subpopulations within the heterogeneous biofilm community, overcoming the limitations of single-agent therapy.
Anti-Virulence and Quorum Sensing Inhibition
Anti-virulence strategies represent a promising alternative to traditional bactericidal approaches by specifically disrupting pathogenicity without imposing strong selective pressure for resistance development [32] [33]. Quorum sensing inhibitors (QSIs) such as wogonin—a flavonoid derived from Agrimonia pilosa—effectively attenuate P. aeruginosa pathogenicity by interfering with the pqs QS system [30]. Treatment with wogonin downregulates QS-related genes, reduces production of elastase, pyocyanin, and proteolytic enzymes, and inhibits biofilm formation while enhancing bacterial clearance in animal models [30]. Other promising QSIs include terrein, parthenolide, and 4-amino-quinolone-based compounds, which similarly disrupt virulence coordination in various pathogens [32].
Table 3: Emerging Anti-Virulence Compounds with Anti-Biofilm Activity
| Compound | Source/Target | Mechanism of Action | Experimental Efficacy |
|---|---|---|---|
| Wogonin | Agrimonia pilosa/pqs QS system | Inhibits PQS signal synthesis, downregulates virulence genes | Reduces biofilm formation, attenuates in vivo pathogenicity |
| Terrein | Fungal metabolite | Inhibits QS, reduces elastase/pyocyanin production | Protects mice and C. elegans from P. aeruginosa infection |
| Parthenolide | Medicinal plant | Reduces pyocyanin, protease, and biofilm production | Inhibits swarming motility, disrupts established biofilms |
| Savirin | Synthetic compound | Targets two-component systems, inhibits RNAIII production | Reduces S. aureus skin infection severity in murine models |
| MEDI4893 | Monoclonal antibody | Neutralizes α-hemolysin toxin | Prevents S. aureus-mediated tissue damage in experimental infections |
The Scientist's Toolkit: Essential Research Reagents for Biofilm Studies
Advanced research on biofilm formation and therapeutic intervention requires specialized reagents and methodological approaches. The following toolkit highlights essential materials for investigating biofilm biology and evaluating potential anti-biofilm strategies.
Table 4: Essential Research Reagents for Biofilm Studies
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Culture Media | SP-4 broth, glucose/citrate media | Biofilm cultivation under defined conditions | Matrix composition varies with carbon source |
| Staining Reagents | Crystal violet, LIVE/DEAD kits | Biofilm biomass and viability quantification | Complementary methods provide different information |
| Antibiotic Standards | Erythromycin, moxifloxacin, doxycycline | MIC determination, combination studies | Clinical formulations vs. research-grade purity |
| QS Inhibitors | Wogonin, synthetic AIP analogs | Anti-virulence mechanism studies | Species-specific QS system differences |
| Matrix Components | DNase I, dispersin B, glycosidases | Matrix disruption studies | Enzyme specificity for different EPS components |
| Analytical Tools | HPLC systems, qPCR instruments | Virulence factor quantification, gene expression | Sensitivity requirements for bacterial metabolites |
Biofilm formation represents a sophisticated virulence strategy that balances enhanced community protection through multilayered antibiotic resistance mechanisms with attenuated virulence factor production to facilitate persistent infection. The case of M. pneumoniae illustrates how these adaptations contribute to chronic respiratory disease and complicate therapeutic interventions. Quantitative analysis reveals that biofilms can increase antibiotic MICs by several orders of magnitude, rendering conventional monotherapy increasingly inadequate. The future of biofilm management lies in combination approaches that integrate optimized antibiotic pairs with targeted anti-virulence agents such as quorum sensing inhibitors. These strategies offer the potential to disrupt pathogenic communities while minimizing selective pressure for resistance development. Further research into the molecular regulation of biofilm development and maintenance will identify additional targets for precisely countering this fundamental bacterial survival strategy.
Mycoplasma pneumoniae is a significant cause of community-acquired pneumonia in both children and adults worldwide. As a wall-less bacterium, it is inherently resistant to beta-lactam antibiotics that target cell wall synthesis, making macrolides—which inhibit bacterial protein synthesis—the cornerstone of treatment [34]. For decades, erythromycin, azithromycin, and clarithromycin have served as first-line therapeutic agents against Mycoplasma infections. However, the rising global prevalence of macrolide-resistant M. pneumoniae (MRMP) strains, particularly in East Asia where resistance rates exceed 80%, presents a substantial clinical challenge [13] [15] [34]. This guide provides a comprehensive comparison of these first-line macrolide agents, focusing on their efficacy against Mycoplasma pneumoniae, mechanisms of action and resistance, and limitations imposed by both bacterial resistance and drug-specific safety profiles. Understanding these aspects is crucial for researchers and drug development professionals working to address the growing threat of antimicrobial resistance.
Macrolide Comparison: Efficacy, Spectrum, and Key Characteristics
The three primary macrolides—azithromycin, clarithromycin, and erythromycin—share a common mechanism of action but differ significantly in their pharmacokinetic properties, antimicrobial spectrum, and clinical applications.
Table 1: Comparative Characteristics of First-line Macrolides
| Feature | Erythromycin | Clarithromycin | Azithromycin |
|---|---|---|---|
| Generation | First | Second | Second (Azalide) |
| Mechanism of Action | Binds 50S ribosomal subunit, inhibits protein synthesis [35] | Binds 50S ribosomal subunit, inhibits protein synthesis [35] | Binds 50S ribosomal subunit, inhibits protein synthesis [35] |
| Anti-Mycoplasma Activity | Effective against sensitive strains [35] | Effective against sensitive strains [35] | Effective against sensitive strains [35] |
| Key Resistance Mechanism | 23S rRNA mutation (e.g., A2063G, A2064G) [15] [34] | 23S rRNA mutation (e.g., A2063G, A2064G) [15] [34] | 23S rRNA mutation (e.g., A2063G, A2064G) [15] [34] |
| Common Formulations | Oral tablets (250/500 mg), Topical (2%), Ophthalmic (0.5%) [35] | Oral tablets (125/250/500 mg), Suspension (125 mg/5mL) [35] | Oral tablets (100-600 mg), IV (500 mg), Suspension [35] |
| Half-life | Short (~1.5 hours) | Intermediate (~5 hours) | Extended (~68 hours) [35] |
| Unique Properties | Motilin agonist; high GI upset [35] [36] | 14-hydroxy metabolite enhances activity [37] | Extensive tissue penetration & long half-life [35] |
Macrolides exert their antibacterial effect by binding to the 50S ribosomal subunit of bacteria, specifically targeting nucleotides in domain V of the 23S rRNA. This binding inhibits protein synthesis by causing premature dissociation of the peptidyl-tRNA complex from the ribosome, ultimately preventing chain elongation [35] [34]. They are considered bacteriostatic antibiotics but can be bactericidal at higher concentrations [35].
While all macrolides are effective against Mycoplasma pneumoniae, their spectrum extends to other atypical pathogens including Legionella species and Chlamydia pneumoniae, making them valuable for empirical treatment of community-acquired pneumonia [35]. Clarithromycin also plays a specific role in Helicobacter pylori eradication regimens [35].
A critical distinction lies in their pharmacokinetic profiles. Azithromycin, with its prolonged half-life and extensive tissue penetration, enables once-daily dosing and shorter treatment courses. In contrast, erythromycin and clarithromycin typically require multiple daily doses [35]. These properties, along with a generally more favorable gastrointestinal tolerance profile, have made azithromycin and clarithromycin preferred over erythromycin in many clinical scenarios [37].
Quantitative Efficacy and Resistance Data
The clinical utility of macrolides is increasingly constrained by the global rise of resistance, particularly in M. pneumoniae, necessitating a clear understanding of quantitative efficacy data.
Table 2: Anti-Mycoplasma pneumoniae Efficacy and Resistance Profiles
| Parameter | Erythromycin | Clarithromycin | Azithromycin | Midecamycin* |
|---|---|---|---|---|
| MIC90 (susceptible strains) | Not specified in sources | Not specified in sources | Not specified in sources | 16 µg/mL [15] |
| Primary Resistance Mechanism | 23S rRNA mutations (A2063G, A2064G) [15] [34] | 23S rRNA mutations (A2063G, A2064G) [15] [34] | 23S rRNA mutations (A2063G, A2064G) [15] [34] | Not specified in sources |
| Regional Resistance Rate (Pediatrics, East Asia) | Up to 80-100% [13] [34] | Up to 80-100% [13] [34] | Up to 80-100% [13] [34] | Not specified in sources |
| Reported Resistance Rate (Adult Study, Beijing) | 41.7% (within cohort) [15] | 41.7% (within cohort) [15] | 41.7% (within cohort) [15] | Not specified in sources |
| Alternative for Resistant Strains | Not recommended | Not recommended | Not recommended | Promising alternative [15] |
Note: Midecamycin is a 16-membered ring macrolide included for comparison as an investigational alternative. MIC90: Minimum Inhibitory Concentration required to inhibit 90% of isolates.
The most critical limitation of macrolide therapy is high-level resistance, primarily mediated by point mutations in the 23S rRNA gene, with A2063G being the most prevalent and consequential substitution [15] [34]. This single mutation significantly alters the drug's binding site, reducing its affinity and rendering the antibiotics ineffective [34].
Epidemiologically, resistance rates show dramatic geographic variation. While generally low in Europe and the Americas (<10%), rates in East Asian countries like Japan, South Korea, and China have soared to 80-100% in recent years [13] [34]. A 2025 study from Osaka, Japan, reported a resistance rate of 72.9% in 2024, indicating a resurgence after a temporary decline during the COVID-19 pandemic [13]. This trend underscores the role of antimicrobial selective pressure and clonal expansion in resistance dissemination [34].
In vitro studies highlight potential alternatives. Midecamycin, a 16-membered-ring macrolide, has demonstrated promising activity against MRMP, with one study reporting an MIC90 of 16 µg/mL, suggesting it may represent a viable therapeutic option, particularly for pediatric populations where tetracyclines and fluoroquinolones are used with caution due to toxicity concerns [15].
Mechanisms of Action and Resistance
A detailed understanding of macrolide mechanisms at the molecular level is fundamental for developing strategies to overcome resistance.
Protein Synthesis Inhibition Pathway
The primary antibacterial action of macrolides involves binding to the bacterial 50S ribosomal subunit. The following diagram illustrates this key mechanism and the major resistance pathway.
Experimental Protocol for Antimicrobial Susceptibility Testing
Research on macrolide efficacy and resistance relies on standardized laboratory methodologies. The following is a typical protocol for determining Minimum Inhibitory Concentration (MIC) against M. pneumoniae.
Objective: To determine the minimum inhibitory concentration (MIC) of macrolide antibiotics against clinical isolates of Mycoplasma pneumoniae.
Materials:
- Mycoplasma pneumoniae isolates: Clinical strains isolated from oropharyngeal swabs [15].
- Reference strain: M. pneumoniae FH (ATCC 15531) as a drug-sensitive control [15].
- Culture media: SP4 broth medium (e.g., OXOID CM0403) [15].
- Antibiotics: Erythromycin, azithromycin, clarithromycin, midecamycin standard powders [15].
- Equipment: Microdilution trays, CO₂ incubator, sterile pipettes.
Methodology:
- Inoculum Preparation: Harvest actively growing M. pneumoniae cultures and adjust turbidity to 10⁴–10⁵ color-changing units (CCU)/mL in SP4 broth [15].
- Antibiotic Dilution: Prepare two-fold serial dilutions of each macrolide in SP4 broth across the microdilution trays, covering a concentration range from 0.001 µg/mL to 256 µg/mL [15].
- Inoculation: Add an equal volume of the standardized inoculum to each well of the microdilution tray.
- Incubation: Incub trays at 37°C under 5% CO₂ conditions [15].
- MIC Determination: Read plates daily. The MIC is defined as the lowest antibiotic concentration that prevents a color change in the phenol red indicator (indicating no bacterial growth) at the time when the growth control wells first show a color change (typically from red to yellow) [15]. Tests should be performed in triplicate for reliability.
- Resistance Breakpoint: Per previous research, a MIC of ≥32 µg/mL is typically used to define resistance for erythromycin, azithromycin, and midecamycin [15].
Limitations Beyond Resistance: Safety and Toxicity
The clinical profile of macrolides is further complicated by a range of non-resistance limitations, particularly concerning adverse effects.
Table 3: Comparative Safety and Toxicity Profiles
| Adverse Effect / Limitation | Erythromycin | Clarithromycin | Azithromycin | Clinical Implications |
|---|---|---|---|---|
| Gastrointestinal (Overall) | Very Common (ROR=3.17) [36] | Common (ROR=2.10) [36] | Common (ROR=2.07) [36] | Motilin agonist effect; causes nausea, vomiting, diarrhea [35] |
| QT Prolongation / Torsades de Pointes | High risk (ROR=4.1) [38] | Moderate risk (ROR=4.5) [38] | Lower risk (ROR=7.4)* [38] | Contraindicated in patients with long QT syndrome; caution with concomitant QT-prolonging drugs [35] |
| Hepatotoxicity | Reported [35] | Not specified in sources | Not specified in sources | Particularly in pregnant women [35] |
| Cardiovascular Toxicity | Valve disorders (ROR=2.3), Ventricular tachyarrhythmias (ROR=3.5) [38] | Valve disorders (ROR=1.8), Ventricular tachyarrhythmias (ROR=3.6) [38] | Heart failure (ROR=1.46), Hypertension (ROR=1.1) [38] | Azithromycin has a distinct CV toxicity profile; requires monitoring [38] |
| Sensorineural Hearing Loss | Reported [35] | Reported [35] | Reported [35] | Often reversible upon discontinuation, but can be permanent [35] |
| Drug-Drug Interactions | Strong CYP3A4 inhibitor [35] | Less interaction potential [35] | Minimal interaction potential [35] | High risk of interaction with carbamazepine, theophylline, terfenadine [35] |
Note: *While azithromycin's ROR for QT prolongation is higher, studies suggest its proarrhythmic potential may be lower than other macrolides due to different patterns of action potential prolongation [38]. ROR = Reporting Odds Ratio from pharmacovigilance studies.
Gastrointestinal toxicity is a class-wide limitation, driven by macrolides' action as motilin receptor agonists that stimulate gastrointestinal motility [35]. A 2025 pharmacovigilance study analyzing FDA Adverse Event Reporting System (FAERS) data found that among pediatric patients, nearly one-third of adverse event reports for oral macrolides involved GI issues, with vomiting, diarrhea, and nausea being most frequent [36]. Erythromycin demonstrated the highest reporting odds ratio (ROR=3.17) for these events [36].
Cardiovascular toxicity, particularly QT interval prolongation and risk of Torsades de Pointes, is a significant concern [35]. A 2025 analysis of the global VigiBase database confirmed that azithromycin, erythromycin, and clarithromycin were all associated with ventricular tachyarrhythmias and TdP/QT prolongation [38]. Importantly, the cardiovascular toxicity profile differs among agents: azithromycin was uniquely associated with increased reports of hypertension and heart failure, distinguishing it from other macrolides [38].
Macrolides also exhibit significant drug-drug interactions, primarily through inhibition of the cytochrome P450 system, especially CYP3A4. Erythromycin is a potent inhibitor, followed by clarithromycin, while azithromycin has minimal effect on these enzymes and consequently fewer interactions [35]. This is a critical consideration in polypharmacy patients.
The Scientist's Toolkit: Essential Research Reagents
Research into macrolide efficacy and resistance requires specialized reagents and methodologies. The following table details key solutions and their applications for scientists in this field.
Table 4: Essential Research Reagents for Macrolide-Mycoplasma Studies
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| SP4 Broth & Agar Media | Culture and propagation of fastidious Mycoplasma pneumoniae isolates [15]. | Contains serum, peptone, and growth factors; color change (phenol red) indicates metabolic activity and growth [15]. |
| Broth Microdilution Trays | Standardized in vitro antimicrobial susceptibility testing (AST) for MIC determination [15]. | Enables two-fold serial dilutions of antibiotics; used with colorimetric readout for M. pneumoniae [15]. |
| PCR Reagents | Amplification of target genes (e.g., 23S rRNA, ribosomal proteins L4/L22) for resistance mutation screening [15]. | Primers specific for M. pneumoniae 23S rRNA domains II and V are essential for identifying A2063G et al. mutations [15]. |
| DNA Sequencing Kits | Sanger sequencing of PCR products to confirm specific resistance-conferring point mutations [15]. | Critical for correlating genotype (mutation) with phenotype (elevated MIC) [15]. |
| Efflux Pump Inhibitors (e.g., Reserpine) | Investigate non-mutational resistance mechanisms in clinical isolates [15]. | Reduction in MIC in the presence of inhibitor suggests active efflux contributes to resistance [15]. |
Erythromycin, azithromycin, and clarithromycin remain foundational agents for treating Mycoplasma pneumoniae infections, but their utility is increasingly constrained by significant limitations. The most pressing challenge is the global emergence and spread of macrolide-resistant strains, driven primarily by stable point mutations in the 23S rRNA target site. This resistance is no longer a theoretical concern but a clinical reality in many parts of the world, with rates exceeding 80% in some endemic regions [13] [34]. Furthermore, class-wide adverse effects, particularly gastrointestinal and cardiac toxicity, along with significant drug-drug interactions, complicate their use, especially in vulnerable populations.
Future research and drug development must focus on several key areas: 1) elucidating the full scope of resistance mechanisms beyond 23S rRNA mutations, including potential efflux pump activity [15]; 2) developing rapid, accurate diagnostic tests to distinguish macrolide-resistant infections at the point of care, enabling tailored therapy; and 3) exploring alternative antibiotic classes, such as the 16-membered ring macrolide midecamycin [15], tetracyclines, and fluoroquinolones, while balancing their efficacy against their own toxicity profiles. For researchers and drug developers, overcoming these limitations is paramount to ensuring effective treatment for Mycoplasma pneumoniae infections in an era of escalating antimicrobial resistance.
Assessing Antibiotic Efficacy: From In Vitro Models to Clinical Trial Endpoints
The Minimum Inhibitory Concentration (MIC) assay stands as the gold standard in clinical and research microbiology for determining the susceptibility of bacterial strains to antimicrobial agents [39]. These assays quantitatively measure the lowest concentration of an antimicrobial required to inhibit the visible growth of a microorganism in vitro [39] [40]. In the context of mycoplasma research—a genus of bacteria lacking a cell wall—accurate MIC determination is particularly crucial. Mycoplasma species are intrinsically resistant to beta-lactam antibiotics and require tailored testing approaches [41] [42]. The data derived from MIC assays directly informs the selection of appropriate antibiotics and helps track the emergence of resistant strains, a growing concern in mycoplasma treatment [42].
Antibacterial agents are broadly classified based on their mode of action: bactericidal agents kill bacteria, while bacteriostatic agents inhibit their growth and replication [40]. This distinction is typically determined in vitro by calculating the Minimum Bactericidal Concentration (MBC) to MIC ratio. An MBC/MIC ratio of ≤4 defines a bactericidal agent, whereas a ratio >4 indicates bacteriostatic activity [40]. However, this classification is not absolute, as some antibiotics exhibit both activities depending on the bacterial species, drug concentration, and infection environment [40]. For instance, linezolid is bacteriostatic against enterococci and MRSA but can be bactericidal against Streptococcus pneumoniae [40]. Understanding this distinction is vital for designing effective therapeutic strategies, especially for severe mycoplasma infections where the host's immune status may influence drug efficacy.
Standardized Methodologies for MIC Determination
Reliable MIC determination requires strict adherence to standardized protocols established by international bodies such as the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [39] [43]. The following sections detail the core methodologies.
Broth Microdilution: The Reference Method
Broth microdilution in cation-adjusted Mueller-Hinton broth (CAMHB) is recognized as the standard reference method for antimicrobial susceptibility testing (AST) [43]. This method involves testing a bacterial inoculum against a series of doubling antibiotic concentrations.
Table 1: Key Components of a Broth Microdilution MIC Assay
| Component | Specification | Purpose |
|---|---|---|
| Growth Medium | Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium that ensures consistent cation concentrations for reproducible antibiotic activity [43]. |
| Inoculum Preparation | Standardized to ~5 x 10⁵ CFU/mL in sterile saline [39] | Achieves a precise, reproducible bacterial density critical for accurate MIC results. |
| Incubation Conditions | 35°C ± 2°C for 16-20 hours (for most bacteria) [39] | Optimal conditions for bacterial growth. Mycoplasma may require longer incubation and specialized media [42]. |
| MIC Interpretation | Visual or automated reading of growth inhibition | The lowest antibiotic concentration showing no visible growth is recorded as the MIC [39]. |
Protocol 2a: Standard Broth Microdilution Method [39]
- Bacterial Strain Preparation: Using a sterile loop, streak the bacterial strain onto an appropriate solid agar medium (e.g., LB agar) and incubate statically overnight at 37°C.
- Overnight Culture: Inoculate a liquid broth medium with several distinct colonies from the agar plate. Incubate for the appropriate duration (e.g., overnight at 37°C with agitation at 220 RPM).
- Inoculum Standardization:
- Gently mix the overnight culture and measure its optical density at 600 nm (OD600).
- Dilute the culture in sterile saline to achieve a final density of approximately 5 x 10⁵ CFU/mL. The required volume can be calculated using the formula:
Volume (μL) of culture = 1000 μL / (10 × OD600 measurement) / (target OD600) - Confirm the inoculum density by performing a serial dilution and colony-forming unit (CFU) enumeration.
- MIC Plate Preparation and Inoculation:
- Prepare a microtiter plate containing a serial two-fold dilution of the antibiotic in CAMHB.
- Add the standardized inoculum to each well of the test plate.
- Include growth control wells (inoculum without antibiotic) and sterility control wells (medium only).
- Incubation and Reading:
- Incub the plate under appropriate conditions (e.g., 37°C for 16-20 hours).
- After incubation, determine the MIC as the lowest antibiotic concentration that completely inhibits visible bacterial growth.
Alternative and Specialized MIC Methods
For specific applications or constraints, other MIC methods are employed:
Protocol 1: Antibiotic Gradient Strips [39] This technique uses plastic strips impregnated with a predefined, continuous antibiotic gradient. The strip is applied to an agar plate seeded with the standardized inoculum. After incubation, an elliptical zone of inhibition forms, and the MIC is read at the point where the ellipse's edge intersects the strip. While convenient, this method is generally more expensive than broth microdilution.
Protocol 2b: Cation-Adjusted Broth for Polymyxins [39] Testing polymyxin antibiotics (e.g., colistin) requires strict use of cation-adjusted media, as divalent cation concentrations can significantly affect their activity. The methodology is otherwise identical to the standard broth microdilution.
Protocol 2c: Low-Volume Broth Microdilution [39] This adaptation uses smaller volumes (e.g., in 96-well plates with 50-100 μL total volume) to conserve precious compounds, such as novel antimicrobial peptides or limited-quantity experimental drugs.
The workflow for these standardized methods is summarized in the diagram below.
Determining Bacteriostatic vs. Bactericidal Activity
While the MIC indicates growth inhibition, it does not distinguish between bacteriostatic and bactericidal effects. This determination requires further analysis using the MBC test or time-kill curves.
Minimum Bactericidal Concentration (MBC) Determination
The MBC is defined as the minimum concentration of antimicrobial required to achieve a ≥99.9% (a 3-log₁₀) reduction in the initial bacterial inoculum [40]. The procedure is as follows:
- Perform MIC Assay: First, conduct a standard broth microdilution MIC assay as described in Protocol 2a.
- Sub-culture from MIC Plate: After reading the MIC, aliquot a small volume (e.g., 10-100 μL) from each well that shows no visible growth, including wells with antibiotic concentrations above the MIC.
- Viable Count Assessment: Spread the aliquots onto non-selective agar plates and incubate them to allow any surviving bacteria to form colonies.
- Calculate MBC: The MBC is the lowest antibiotic concentration from which the sub-culture results in ≤0.1% survival (i.e., a 99.9% kill rate) of the original inoculum. The MBC/MIC ratio is then calculated to classify the antibiotic's action.
Time-Kill Curves
Time-kill assays provide a more dynamic assessment of an antibiotic's bactericidal kinetics [40]. In this method, a bacterial culture is exposed to a fixed concentration of an antibiotic (e.g., at the MIC or multiple multiples of the MIC). Samples are withdrawn at regular intervals over 24 hours, and the viable bacterial count (in CFU/mL) is determined for each time point. The data is plotted as log₁₀ CFU/mL versus time. A bacteriostatic agent is characterized by a curve where the bacterial count remains relatively stable or decreases by less than 3-log₁₀ over 24 hours. In contrast, a bactericidal agent will show a sustained reduction of ≥3-log₁₀ in the bacterial count [40].
Table 2: Classifying Bacteriostatic and Bactericidal Antibiotics
| Bactericidal Agents | Bacteriostatic Agents | Agents with Dual Activity |
|---|---|---|
| Aminoglycosides [40] | Tetracyclines [40] | Linezolid (Bacteriostatic vs. MRSA/VRE; Bactericidal vs. Streptococcus pneumoniae) [40] |
| β-Lactams [40] | Macrolides [40] | Ciprofloxacin (Can be both, depending on mechanism) [40] |
| Fluoroquinolones [40] | Oxazolidinones [40] | Tigecycline (Generally bacteriostatic, but can be bactericidal against some strains) [40] |
| Glycopeptides [40] | Sulfonamides [40] | Chloramphenicol (Bacteriostatic against Enterobacterales; Bactericidal against some pathogens) [40] |
Application in Mycoplasma Research and Antimicrobial Resistance
Mycoplasma species present unique diagnostic and therapeutic challenges due to their lack of a cell wall, slow growth, and specific culture requirements [41] [42]. Standardized MIC testing for mycoplasmas often follows CLSI document M43-A or manufacturer-defined interpretive criteria for tests like the Mycoplasma IST2/IST3 [44] [42].
Recent surveillance studies highlight concerning resistance patterns. A 2025 study from Brazil found high rates of fluoroquinolone resistance in urogenital mycoplasmas, with 75.0% of Mycoplasma hominis and 84.1% of Ureaplasma urealyticum isolates resistant to ciprofloxacin [42]. Levofloxacin resistance was also notable, particularly in co-infections [42]. This underscores the critical need for ongoing susceptibility monitoring to guide empiric therapy.
Molecular methods like metagenomic Next-Generation Sequencing (mNGS) are emerging as powerful tools for detection and resistance profiling. A 2025 study found that mNGS of bronchoalveolar lavage fluid was significantly more sensitive for diagnosing Mycoplasma pneumoniae pneumonia (MPP) than non-invasive tests like nasopharyngeal NAAT (74.1% sensitivity) or serum IgM assays (23.6% sensitivity) [41]. This superior detection capability makes mNGS a valuable reference standard for evaluating simpler diagnostic tests in complex cases.
Essential Research Reagent Solutions
Successful and reproducible MIC and bactericidal testing relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagents for MIC and Bacteriostatic Assays
| Reagent / Material | Function in the Assay | Application Notes |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution; ensures consistent divalent cation levels (Ca²⁺, Mg²⁺) that affect antibiotic activity [43]. | Essential for reliable, reproducible results, especially for testing polymyxins [39]. |
| Prepared MIC Panels | Multi-well plates containing pre-diluted, lyophilized or frozen antibiotics in a serial dilution series. | Saves time, improves accuracy of dilution preparation, and ensures consistency across experiments. |
| Quality Control Strains | Strains with well-defined and stable MIC ranges (e.g., E. coli ATCC 25922) used to validate assay performance [39]. | Must be run regularly according to CLSI/EUCAST guidelines to ensure the entire test system is functioning correctly [45] [39]. |
| Mycoplasma Detection Kits | PCR- or nucleic acid amplification-based kits (e.g., ACROBiosystems OPA-S102) for rapid, sensitive detection of mycoplasma contamination in cell cultures or samples [46]. | Crucial for ensuring cell cultures used in research are not contaminated, which can confound experimental results. |
| Antibiotic Gradient Strips | Pre-made plastic strips for determining MIC on agar surfaces, offering convenience and flexibility [39]. | Useful for testing single isolates or when broth microdilution is not feasible. Higher cost per test. |
Standardized MIC and bactericidal activity assays are foundational to antimicrobial research and clinical microbiology. The rigorous methodologies defined by CLSI and EUCAST, including broth microdilution and MBC determination, provide the critical data needed to characterize antibiotic potency, classify agents as bactericidal or bacteriostatic, and monitor the alarming spread of antimicrobial resistance. This is especially pertinent in mycoplasma research, where unique biological characteristics and rising resistance to fluoroquinolones and other drug classes demand precise and reliable susceptibility data. Adherence to these standardized protocols ensures the generation of accurate, reproducible, and clinically translatable results, which are essential for guiding effective patient therapy and advancing the development of new antibacterial agents.
Antimicrobial resistance represents one of the most pressing global health challenges, driving the need for innovative therapeutic strategies. Combination therapy using multiple antimicrobial agents has emerged as a promising approach to combat multidrug-resistant pathogens. This comparison guide examines the checkerboard assay methodology as a standardized tool for evaluating antibiotic interactions, supplemented by clinical efficacy data on antibiotic combinations against various pathogens, including Mycoplasma pneumoniae. We present detailed experimental protocols, quantitative interaction assessments, and specialized applications to support researchers and drug development professionals in designing effective combination therapies.
The rise of antimicrobial resistance has transformed combination therapy from a specialized approach into an essential strategy for treating multidrug-resistant infections. Checkerboard assays provide a systematic methodology for quantifying drug interactions through a microdilution technique that tests varying concentrations of two antimicrobial agents in combination [47]. This approach enables researchers to determine whether drug pairs interact synergistically, additively, or antagonistically, information critical for optimizing therapeutic regimens.
Combination therapies are already well-established for specific infections. Helicobacter pylori infections typically employ quadruple therapies combining proton pump inhibitors with metronidazole and either amoxicillin or bismuth and clarithromycin or tetracycline [48]. Similarly, tuberculosis treatment guidelines recommend initial quadruple therapy with ethambutol, isoniazid, pyrazinamide, and rifampin, followed by dual therapy with isoniazid and rifampin [48]. The checkerboard assay serves as a vital tool for identifying new combinations with potential clinical application, especially against pathogens exhibiting resistance to conventional monotherapies.
Checkerboard Assay Methodology
Core Principles and Workflow
The checkerboard assay is a microdilution technique performed in 96-well plates that enables systematic evaluation of two antimicrobial agents in combination [47]. The fundamental principle involves creating a matrix where each well contains a unique combination of drug concentrations, allowing for high-throughput assessment of their interactive effects on bacterial growth.
Experimental Workflow:
Figure 1: Checkerboard assay workflow illustrating key steps from reagent preparation to data interpretation.
Detailed Experimental Protocol
Day 1: Preparation Phase
- Microbial Inoculum Preparation: Select isolated bacterial colonies and inoculate into 10 mL of Mueller-Hinton broth (MHB). Incubate at 35±2°C in an orbital shaker incubator at 200 rpm under aerobic conditions for 18±2 hours until reaching approximately 10⁹ CFU/mL [47].
- Culture Media Preparation: Prepare Mueller-Hinton broth (MHB), cation-adjusted Mueller-Hinton broth (CAMHB), and double-concentrated CAMHB (2×CAMHB) according to manufacturer specifications. Sterilize by autoclaving at 121°C for 15 minutes [47].
- Antimicrobial Stock Solutions: Prepare stock solutions of both antimicrobial agents from powder form using appropriate solvents as recommended by CLSI or EUCAST guidelines. Stock solutions should be prepared at concentrations 4-fold higher than the highest concentration to be tested in the assay [47].
Day 2: Assay Setup
- Plate Preparation: Dispense 100 μL of 2×CAMHB medium into each well of a 96-well microplate using a multichannel pipette [47].
- Drug A Preparation and Dispensing:
- Prepare 1.5 mL of stock solution (SA) in 2×CAMHB medium at 4-fold higher than the highest test concentration.
- Prepare 500 μL of 2× stock solution (2×SA) at 8-fold higher than the highest test concentration.
- Dispense 100 μL of SA into row A from columns 1-11.
- Dispense 100 μL of 2×SA into well A12 [47].
- First Serial Dilution of Drug A: Perform serial dilution of Drug A from row A to G using a multichannel pipette set to 100 μL, discarding excess volume from row G [47].
- Drug B Preparation and Dispensing:
- Prepare 1.0 mL of stock solution (SB) in 2×CAMHB at 4-fold higher than the highest test concentration.
- Dispense 100 μL of SB into each well of column 12.
- Second Serial Dilution of Drug B: Dilute Drug B from column 12 to 2 using a multichannel pipette, discarding excess volume from column 2 [47].
- Plate Inoculation: Prepare bacterial inoculum at 10⁶ CFU/mL in 0.9% NaCl from the Day 1 culture. Add 100 μL to each well, resulting in a final inoculum concentration of 5×10⁵ CFU/mL [47].
- Incubation and Reading: Incubate plates at 35±2°C for 16-20 hours. Measure bacterial growth using optical density at 600 nm or through colony-forming unit (CFU) counts [47].
Research Reagent Solutions
Table 1: Essential reagents and materials for checkerboard assays
| Reagent/Material | Function | Specifications |
|---|---|---|
| Mueller-Hinton Broth (MHB) | Standardized growth medium for antimicrobial testing | Prepared according to CLSI/EUCAST standards [47] |
| Cation-Adjusted MHB (CAMHB) | Enhanced medium for fastidious organisms | Contains supplemental calcium and magnesium ions [47] |
| Sterile 0.9% NaCl | Bacterial suspension and dilution | Provides isotonic environment for bacterial viability [47] |
| 96-well Microplates | Assay platform | Clear, flat-bottom, sterile plates for optical reading [47] |
| Multichannel Pipette | Liquid handling | Enables high-throughput reagent distribution [47] |
| Antimicrobial Stock Solutions | Test compounds | Prepared at appropriate concentrations in recommended solvents [47] |
Data Interpretation and Interaction Classification
Fractional Inhibitory Concentration (FIC) Index Calculation
The FIC index quantifies the interaction between two antimicrobial agents using the formula [49] [50]:
FIC Index = (MIC of drug A in combination / MIC of drug A alone) + (MIC of drug B in combination / MIC of drug B alone)
Where:
- MIC of drug A in combination: The lowest concentration of drug A that inhibits growth when combined with drug B
- MIC of drug A alone: The minimum inhibitory concentration of drug A when tested individually
- MIC of drug B in combination: The lowest concentration of drug B that inhibits growth when combined with drug A
- MIC of drug B alone: The minimum inhibitory concentration of drug B when tested individually
Interaction Classification Based on FIC Index [49] [50]:
- Synergy: FIC Index ≤ 0.5
- Additive/Indifference: FIC Index > 0.5 to ≤ 4
- Antagonism: FIC Index > 4
Figure 2: Decision pathway for classifying drug interactions based on FIC index values.
Advanced Interpretation Methods
More sophisticated approaches to checkerboard assay interpretation incorporate cell viability measurements through colony-forming unit (CFU) counts rather than relying solely on optical density readings. This method provides distinction between bacteriostatic versus bactericidal effects and enables more accurate determination of antibiotic synergy versus antagonism [51]. The percentage of viable organisms analysis (PVOA) and percentage of viable organisms versus visible turbidity (PVOV) calculations offer enhanced sensitivity in detecting synergistic or antagonistic interactions, particularly in polymicrobial communities [51].
Applications in Antimicrobial Research
Combination Therapy Against Resistant Pathogens
Checkerboard assays have identified numerous promising combinations against multidrug-resistant pathogens:
Gram-negative Bacteria:
- Ceftazidime-avibactam + aztreonam against metallo-β-lactamase-producing Enterobacterales [52]
- Colistin + meropenem against carbapenem-resistant Acinetobacter baumannii [52]
- Ceftolozane-tazobactam + amikacin against extensively drug-resistant Pseudomonas aeruginosa [53]
Gram-positive Bacteria:
- Daptomycin + fosfomycin against methicillin-resistant Staphylococcus aureus (MRSA) bacteremia and endocarditis [53]
- Ciprofloxacin + daptomycin and tobramycin + vancomycin against Staphylococcus aureus persister cells [54]
Clinical Efficacy in Mycoplasma Respiratory Infections
Table 2: Clinical comparison of clarithromycin versus erythromycin for pediatric respiratory mycoplasma infection
| Parameter | Clarithromycin Group (n=53) | Erythromycin Group (n=53) | P-value |
|---|---|---|---|
| MP-PCR Negative Rate | 96.23% | 75.47% | 0.001 |
| Total Clinical Effectiveness | 96.23% | 75.47% | 0.001 |
| Hospital Stay (days) | 15.14 ± 2.01 | 20.63 ± 3.15 | 0.001 |
| Antipyretic Time (days) | 2.63 ± 0.57 | 4.06 ± 0.75 | 0.001 |
| Drug Cost (Yuan) | 1654.63 ± 100.21 | 2152.14 ± 163.48 | 0.001 |
| Side Effect Incidence | Significantly lower | Higher | <0.05 |
| Medication Compliance | Significantly higher | Lower | <0.05 |
A 2021 clinical study comparing clarithromycin and erythromycin in 106 children with respiratory mycoplasma infection demonstrated clarithromycin's significant advantages across multiple efficacy parameters [23]. The clarithromycin group showed superior mycoplasma clearance (96.23% vs 75.47% MP-PCR negative rate), shorter hospitalization (15.14 vs 20.63 days), faster fever resolution (2.63 vs 4.06 days), reduced drug costs, and improved safety profile [23].
Antimicrobial Peptide-Antibiotic Combinations
Antimicrobial peptides (AMPs) represent a promising class of therapeutic agents that exhibit synergistic effects when combined with conventional antibiotics [55]. The unique membrane-disrupting mechanisms of AMPs complement the targeted activities of traditional antibiotics:
Mechanisms of AMP-Antibiotic Synergy:
- Increased Membrane Permeability: AMPs like tachyplesin III disrupt bacterial membrane integrity, enhancing penetration of antibiotics like piperacillin-tazobactam into Pseudomonas aeruginosa [55].
- Biofilm Disruption: AMPs including G10KHc facilitate tobramycin penetration through Pseudomonas aeruginosa biofilms [55].
- Resistance Inhibition: Colistin combined with imipenem counteracts resistance development in multidrug-resistant Pseudomonas aeruginosa [55].
- Direct Potentiation: Lactoferrin enhances the efficacy of ciprofloxacin, clarithromycin, and minocycline against periodontal pathogens including Porphyromonas gingivalis [55].
Advanced Applications and Modifications
Polymicrobial Checkerboard Assays
Traditional checkerboard assays face limitations in polymicrobial infections where turbidity measurements cannot differentiate effects on individual community members. An advanced methodology incorporates selective and differential plating to determine viable cell counts for each species within a community [51]. This approach revealed that the clinically recommended ceftazidime-gentamicin combination, while synergistic against Pseudomonas aeruginosa in monoculture, becomes antagonistic in a polymicrobial community also containing Acinetobacter baumannii, Staphylococcus aureus, and Enterococcus faecalis [51].
Time-Kill Kinetic Assays
Checkerboard assays identify synergistic concentrations, while time-kill kinetic studies provide temporal characterization of the killing rate [50]. These assays determine whether combinations are bacteriostatic or bactericidal and measure their effect on bacterial populations throughout the growth cycle [50]. For example, antibiotic combinations tested at 100× MIC against Staphylococcus aureus stationary-phase cells showed a two to six log₁₀ reduction in CFU followed by a plateau, indicating persister cell populations [54].
Collateral Sensitivity Applications
Checkerboard approaches can identify collateral sensitivity interactions, where resistance to one antibiotic increases susceptibility to another [48]. This phenomenon creates evolutionary trade-offs that can be exploited through alternating therapy regimens. For instance, cycling neomycin and ciprofloxacin against Staphylococcus aureus significantly slowed resistance development compared to monotherapy [48]. Similarly, expression of mobile beta-lactamases in Escherichia coli produces robust collateral sensitivity to colistin and azithromycin across phylogenetically unrelated strains [48].
Checkerboard assays remain an essential methodology for systematically evaluating antimicrobial combinations in the era of multidrug resistance. The technique provides quantitative assessment of drug interactions through FIC index calculation, enabling classification of combinations as synergistic, additive, or antagonistic. Recent methodological advancements, including viability plating for polymicrobial communities and integration with time-kill studies, have enhanced the clinical relevance of checkerboard testing.
Clinical studies demonstrate the therapeutic potential of synergistic combinations, particularly against resistant pathogens like Mycoplasma pneumoniae, where clarithromycin shows superior efficacy and safety compared to erythromycin. The ongoing exploration of novel combinations, including antimicrobial peptides with conventional antibiotics and those exploiting collateral sensitivity networks, represents a promising frontier in combating antimicrobial resistance. As resistance mechanisms continue to evolve, checkerboard assays will remain fundamental tools for designing effective combination therapies tailored to specific pathogens and clinical contexts.
Within the critical field of antimicrobial research, robust biofilm eradication models are indispensable for evaluating the efficacy of new therapeutic agents. Biofilms, which are structured microbial communities encased in a protective extracellular polymeric substance (EPS), demonstrate significantly enhanced tolerance to antimicrobial treatments compared to their free-living (planktonic) counterparts [56]. This recalcitrance is a major contributor to persistent and recurrent infections, making biofilms a principal focus in studies concerning microbial pathogenicity and drug development [56]. The efficacy of any potential anti-biofilm compound or antibiotic regimen must be rigorously validated using reliable, reproducible laboratory models that can accurately simulate real-life scenarios [57].
This guide provides a comparative analysis of two foundational techniques in biofilm research: the Crystal Violet (CV) assay and Scanning Electron Microscopy (SEM). The CV assay is a high-throughput, colorimetric method used for the quantitative assessment of total biofilm biomass [58] [57]. In contrast, SEM offers high-resolution, qualitative imaging that reveals the intricate architecture and spatial organization of biofilms [59] [60]. Framed within the context of researching mycoplasma removal efficacy, this article will objectively compare these models, detailing their protocols, applications, and limitations, and provide supporting experimental data to aid researchers in selecting the appropriate tool for their investigative needs.
Understanding Biofilms and the Challenge of Eradication
Biofilm Structure and Development
Biofilm formation is a complex, multi-stage process that begins with the initial attachment of planktonic cells to a surface [56]. Following attachment, the cells aggregate and begin to produce an EPS, becoming irreversibly attached [56]. As the biofilm matures, it develops a complex three-dimensional architecture characterized by microcolonies and water channels, reaching its maximum cell density [56]. The final stage involves the active dispersal of cells from the biofilm to colonize new surfaces [56]. This lifecycle poses a significant challenge for eradication, as cells within the biofilm are protected by the EPS matrix.
Mechanisms of Biofilm Antibiotic Tolerance (BAT)
Bacteria residing within biofilms can be up to a thousand times more tolerant to antimicrobial agents than planktonic cells [56]. This phenomenon, known as Biofilm Antibiotic Tolerance (BAT), is mediated by several innate factors:
- Restricted Penetration: The EPS matrix can act as a physical barrier, limiting the diffusion of antimicrobial agents into the deepest layers of the biofilm [56]. However, the effectiveness of this barrier is variable and depends on the specific antibiotic and biofilm composition.
- Reduced Growth Rate: The internal structure of a biofilm creates microenvironments deprived of oxygen and nutrients. This leads to zones of slow-growing or dormant cells, which are less susceptible to antibiotics that primarily target rapidly dividing cells [56].
- Presence of Persisters: A sub-population of metabolically dormant cells, known as "persisters," exhibits high tolerance to antibiotics and other stressors, contributing to biofilm recurrence after treatment [57].
The Crystal Violet (CV) Assay: A Quantitative Workhorse
Principle and Applications
The Crystal Violet (CV) assay is one of the most widely used methods for the quantitative assessment of biofilm formation. It is a colorimetric technique based on the binding of crystal violet, a triphenylmethane dye, to bacterial cells and polysaccharides within the EPS matrix through ionic interactions [57]. The intensity of the stain, measured via spectrophotometry after elution, serves as a proxy for the total biofilm biomass. Its primary advantages are its simplicity, cost-effectiveness, and high-throughput capability, making it ideal for initial screening of biofilm formation under different conditions or for evaluating the efficacy of anti-biofilm compounds [58] [57]. A significant recent advancement is the development of standardized protocols that calibrate CV absorbance against objective measures like Dry Cell Weight (DCW), thereby converting the assay from a comparative tool to a quantitative method that allows for cross-laboratory comparisons [58].
Detailed Experimental Protocol
Instruments and Reagents: 0.1% (w/v) crystal violet solution; 95% ethanol or 10% acetic acid; 96-well microtiter plates (or other growth formats like culture tubes); spectrophotometer or plate reader; micropipettes [58].
Procedure:
- Biofilm Growth: Inoculate a planktonic culture of the test microorganism into the wells of a 96-well microtiter plate. Incubate under appropriate conditions to allow biofilm formation on the well walls.
- Staining: Remove the planktonic culture and gently wash the wells with water to remove non-adherent cells. Add a 0.1% crystal violet solution to each well and incubate for a predetermined time (e.g., 15-30 minutes).
- Destaining and Washing: Carefully decant the crystal violet solution and gently wash the stained biofilm with water to remove excess, unbound dye. This step is critical, as vigorous pipetting can dislodge the biofilm and increase variability [58].
- Elution: Add a solvent (e.g., 95% ethanol or 10% acetic acid) to the wells to solubilize the crystal violet bound to the biofilm. Research indicates that 10% acetic acid may provide more consistent results with lower variability compared to ethanol, potentially due to ethanol's high volatility and lower effectiveness at solubilizing the dye [58].
- Quantification: Transfer the eluted dye to a new microtiter plate (if necessary) and measure the absorbance at 540 nm using a plate reader. The absorbance values are proportional to the total biofilm biomass.
Table 1: Key Characteristics of the Crystal Violet Assay
| Feature | Description | Implication for Research |
|---|---|---|
| Measured Parameter | Total biofilm biomass (cells + EPS) | Does not distinguish between live cells and matrix components. |
| Throughput | High (96-well plate format) | Ideal for screening large numbers of conditions or compounds. |
| Quantitative Output | Absorbance at 540 nm | Can be correlated to Dry Cell Weight (DCW) for standardization [58]. |
| Key Advantage | Simplicity, cost-effectiveness, and reproducibility within a lab. | Accessible for most laboratories. |
| Key Limitation | Does not provide information on viability or 3D structure. | Should be supplemented with viability assays or imaging. |
Workflow Visualization
The following diagram illustrates the standard workflow for the Crystal Violet assay, from biofilm growth to quantitative analysis.
Scanning Electron Microscopy (SEM): Qualitative Structural Insight
Principle and Applications
Scanning Electron Microscopy (SEM) is a powerful imaging technique that provides high-resolution, topographical information about a sample's surface. In biofilm research, it is used to visualize the complex three-dimensional architecture of biofilms, including microcolonies, water channels, and the texture of the EPS matrix [59]. Conventional SEM requires samples to be observed in a high vacuum, which necessitates extensive preparation including chemical fixation, dehydration, and critical-point drying, often followed by metal coating to prevent charging [60]. These procedures can introduce artifacts, such as shrinkage, potentially distorting the biofilm's native structure.
A significant innovation in this field is the Atmospheric SEM (ASEM), which allows for the observation of samples in an open solution environment through a pressure-resistant silicon nitride (SiN) film [60]. This technology enables the rapid imaging of biofilms—and small, difficult-to-culture organisms like mycoplasmas—in a near-native, hydrated state with a resolution of approximately 8 nm, dramatically reducing preparation time and artifacts [60].
Detailed Experimental Protocol
Instruments and Reagents: SEM microscope (or ASEM for liquid imaging); sample mounting stubs; chemical fixatives (e.g., glutaraldehyde, osmium tetroxide); ethanol or acetone for dehydration; critical point dryer; sputter coater (for conventional SEM) [59] [60].
Procedure for Conventional SEM:
- Fixation: Fix the biofilm sample (grown on a suitable substrate) using a buffered aldehyde solution (e.g., 2.5% glutaraldehyde) to preserve its structure. Post-fixation with osmium tetroxide may be used to enhance contrast.
- Dehydration: Gradually dehydrate the fixed sample using a series of ethanol or acetone solutions (e.g., 30%, 50%, 70%, 90%, 100%) to remove all water.
- Drying: Perform critical-point drying to remove the dehydrating agent without causing the surface tension-induced collapse of the delicate biofilm structures.
- Mounting and Coating: Mount the dried sample on a stub and coat it with a thin layer of conductive material, such as gold or platinum, using a sputter coater.
- Imaging: Place the sample in the SEM vacuum chamber and image using a focused electron beam. Detected secondary or backscattered electrons are used to generate a topographical image.
Procedure for ASEM:
- Sample Preparation: Suspend the cells (e.g., mycoplasmas) in an appropriate buffer.
- Loading: Add the suspension to an ASEM dish, the base of which is the SiN film. The sample can be stained with metal stains for contrast [60].
- Imaging: Directly observe the sample in its liquid state using the inverted SEM beam, which scans from below the dish. This allows for quasi-simultaneous recording with an optical microscope from above [60].
Table 2: Key Characteristics of Scanning Electron Microscopy
| Feature | Conventional SEM | Atmospheric SEM (ASEM) |
|---|---|---|
| Sample State | Dehydrated, fixed, and coated | Hydrated, in solution |
| Preparation Time | Long (hours to days) | Short (minutes) |
| Key Advantage | Very high resolution of surface details. | Observation of near-native structures; dynamic potential. |
| Key Limitation | Extensive preparation can cause artifacts; only end-point analysis. | Lower resolution than high-vacuum SEM; requires specialized equipment. |
| Information Gained | Detailed 3D architecture and texture. | Internal features and specific protein localization in solution [60]. |
Direct Model Comparison and Context in Mycoplasma Research
Side-by-Side Technical Comparison
The choice between CV assay and SEM depends heavily on the research question. The table below provides a direct comparison to guide this decision.
Table 3: Direct Comparison of Biofilm Eradication Models
| Parameter | Crystal Violet (CV) Assay | Scanning Electron Microscopy (SEM) |
|---|---|---|
| Primary Function | Quantitative biomass assessment | Qualitative structural imaging |
| Throughput | High | Low |
| Resolution | N/A (bulk measurement) | High (nanometer scale) |
| Cost | Low | High |
| Technical Skill | Low to Moderate | High |
| Viability Data | No (requires complementary assay) | No (unless viability stains are used) |
| Sample Preparation | Simple staining and washing | Extensive fixation/coating (SEM) or minimal (ASEM) |
| Data Output | Numerical (Absorbance) | Visual (Images) |
| Best Use Case | Screening antibiotic efficacy, growth optimization | Visual confirmation of eradication, structural analysis |
Application in Mycoplasma Research
Mycoplasmas are among the smallest free-living bacteria and lack a cell wall, posing unique challenges for both imaging and eradication [60]. Research into their biofilm-forming capabilities and the efficacy of removal agents is critical, especially with the global resurgence of macrolide-resistant Mycoplasma pneumoniae [3] [21].
- Crystal Violet Assay: This model can be used to screen the effectiveness of various antibiotic classes (macrolides, tetracyclines, fluoroquinolones) against mycoplasma biofilms in a high-throughput manner [3]. For instance, a researcher could use the CV assay to quantify the reduction in biofilm biomass following treatment with sitafloxacin versus minocycline, providing quantitative dose-response data.
- Scanning Electron Microscopy: SEM, particularly ASEM, is exceptionally suited for mycoplasma research due to the organism's sub-micron size (around 200 nm wide), which is below the resolution limit of standard light microscopy [60]. ASEM allows for the rapid imaging of mycoplasmas like M. mobile in solution, visualizing their attachment to surfaces and their distinctive flask-shaped morphology with a protruding "leg" structure [60]. This provides irrefutable visual evidence of whether an antibiotic treatment has disrupted biofilm integrity or detached cells from a surface.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful biofilm research relies on a suite of essential reagents and materials. The following table details key solutions and their functions, particularly for the models discussed.
Table 4: Essential Research Reagents for Biofilm Studies
| Research Reagent / Material | Function in Biofilm Research |
|---|---|
| Crystal Violet Solution (0.1%) | A triphenylmethane dye that binds stoichiometrically to cells and polysaccharides in the EPS matrix, enabling colorimetric quantification of total biofilm biomass [58] [57]. |
| Acetic Acid (10%) or Ethanol (95%) | Solvents used to elute the crystal violet dye from the stained biofilm for subsequent spectrophotometric measurement. Acetic acid may offer superior reproducibility [58]. |
| Microtiter Plates (96-well) | Polystyrene plates providing a standardized, high-throughput platform for growing and analyzing multiple biofilm samples simultaneously under static conditions [57]. |
| Silicon Nitride (SiN) Film Dishes | Specialized dishes used in Atmospheric SEM (ASEM). The electron-transparent SiN film forms the base, allowing the SEM beam to image samples in open solution [60]. |
| DDQ (2,3-dichloro-5,6-dicyano-1,4-benzoquinone) | An oxidizing agent used in analytical chemistry to convert leuco compounds (e.g., leucocrystal violet) back to their colored, charged forms for accurate quantification in complex matrices like fish tissue [61]. |
| Propylsulfonic Acid (PRS) SPE Columns | Solid-phase extraction columns used for sample clean-up to isolate and purify analytes like triphenylmethane dyes from complex biological samples before instrumental analysis [61]. |
Integrated Workflow for Biofilm Eradication Validation
An effective research strategy often involves an integrated approach, using both quantitative and qualitative models to validate findings. The following diagram outlines a logical workflow for comprehensively assessing a potential anti-biofilm treatment, from initial screening to mechanistic insight.
The Crystal Violet assay and Scanning Electron Microscopy represent two pillars of biofilm eradication research, each with distinct and complementary strengths. The CV assay stands out for its quantitative power, high-throughput capability, and cost-effectiveness, making it an indispensable tool for initial screening and dose-response studies. In contrast, SEM provides unparalleled qualitative insight into the three-dimensional architecture of biofilms, offering visual proof of structural disintegration following treatment.
Within the specific context of mycoplasma research, the integration of these models is particularly powerful. The CV assay can efficiently screen the efficacy of various antibiotics against challenging, macrolide-resistant strains [21], while advanced techniques like ASEM can directly visualize the interaction of these minimalistic pathogens with surfaces and therapeutic agents in a near-native state [60]. A robust research program will leverage the strengths of both models—using the CV assay for broad quantification and SEM for deep structural validation—to generate comprehensive and reliable data on the mycoplasma removal efficacy of novel antibiotics and anti-biofilm strategies.
This guide objectively compares the performance of doxycycline and macrolide antibiotics in the treatment of Mycoplasma pneumoniae pneumonia (MPP), with a focus on key clinical and microbiological endpoints. The data is synthesized from recent clinical and laboratory studies to serve researchers and drug development professionals investigating mycoplasma removal efficacy.
Comparative Antibiotic Performance in Severe MPP
The table below summarizes quantitative data from clinical studies comparing doxycycline and macrolide antibiotics in pediatric patients with Severe Mycoplasma pneumoniae Pneumonia (SMPP).
Table 1: Comparison of Clinical Endpoints for Doxycycline vs. Macrolides in Severe MPP
| Clinical Endpoint | Doxycycline Group (n=44) | Macrolide Group (n=48) | Statistical Significance (p-value) | Effect Size (where available) |
|---|---|---|---|---|
| Time to Defervescence (Fever Resolution) | Not significantly different | Not significantly different | p > 0.05 [8] | - |
| Time to Cough Relief | 5.4 ± 1.2 days | 7.2 ± 1.6 days | p < 0.05 [8] | - |
| Time to Pulmonary Rale Resolution | 6.2 ± 1.3 days | 8.0 ± 1.7 days | p < 0.05 [8] | - |
| Overall Treatment Efficacy Rate | 88.6% | 75.0% | p < 0.05 [8] | Relative Risk (RR): 0.68 (95% CI: 0.58–0.79) [8] |
| Adverse Event Rate | 18.2% | 16.7% | p > 0.05 [8] | - |
| Microbiological Efficacy (Biofilm Eradication in vitro) | Effective in synergistic combinations [27] | Highly resistant in biofilm state [27] | - | - |
Detailed Experimental Protocols
Clinical Study Protocol for Antibiotic Efficacy
This protocol outlines the methodology used in the recent clinical comparison of doxycycline and macrolides [8].
- Study Population: 92 pediatric patients under 8 years old hospitalized with Severe Mycoplasma pneumoniae Pneumonia (SMPP), specifically identified as macrolide-unresponsive MPP (MUMPP) after failing at least three days of prior macrolide therapy.
- Diagnostic Criteria: Based on the 2023 Guidelines for the Diagnosis and Treatment of Mycoplasma pneumoniae in Children, including persistent high fever (≥39°C for ≥5 days), respiratory distress, extrapulmonary complications, hypoxemia (pulse oxygen saturation ≤93%), and significant radiographic findings [8].
- Treatment Groups:
- Experimental Group (n=44): Received oral doxycycline at 2 mg/kg every 12 hours for 10 days.
- Control Group (n=48): Continued intravenous macrolide antibiotic therapy.
- Concomitant Treatment: Both groups received standardized supportive care, including glucocorticoids (methylprednisolone), bronchoscopic intervention when necessary, and management of co-infections [8].
- Primary Endpoints:
- Time to Defervescence: Time from initiation of treatment until body temperature normalized.
- Time to Symptom Resolution: Time until cough and pulmonary rales resolved.
- Overall Treatment Efficacy: Assessed via chest CT scans one week post-treatment initiation and clinical evaluation.
- Safety Monitoring: Adverse events were recorded and compared between groups.
In Vitro Protocol for Synergistic Biofilm Eradication
This protocol describes the laboratory methods used to test antibiotic combinations against M. pneumoniae biofilms [27].
- Bacterial Strains: Mycoplasma pneumoniae wild-type strains M129 and 19294, representing the two major subtypes of the species.
- Biofilm Cultivation: Bacteria were grown in SP-4 broth in 24- or 96-well plates at 37°C for several days to allow for the formation of mature biofilm towers.
- Antibiotic Agents: Erythromycin (ERY), Doxycycline (DOX), and Moxifloxacin (MOX) were prepared in serial twofold dilutions.
- Checkerboard Assays: Used to test for synergistic effects between pairs of antibiotics (ERY+DOX, ERY+MOX, DOX+MOX). Fractional Inhibitory Concentration (FIC) indices were calculated to quantify synergy.
- Biofilm Eradication Assessment:
- Crystal Violet Assay: Provided a quantitative measure of total biofilm biomass remaining after antibiotic treatment.
- Scanning Electron Microscopy (SEM): Used for qualitative, visual confirmation of biofilm structural integrity or eradication.
- H₂O₂ Sensitivity Testing: Biofilm towers were exposed to dilutions of hydrogen peroxide to assess vulnerability to this virulence factor.
Visualizing Research Pathways and Synergistic Effects
Research and Therapeutic Pathways for Severe MPP
Mechanism of Synergistic Biofilm Eradication
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for M. pneumoniae Efficacy Studies
| Reagent / Solution | Function in Experimental Protocol |
|---|---|
| SP-4 Broth | The complex, undefined culture medium required for the axenic growth of Mycoplasma pneumoniae in vitro [27]. |
| M. pneumoniae Strains (M129, 19294) | Wild-type strains representing the two primary subtypes of the species, used to ensure genetic diversity in experimental findings [27]. |
| Antibiotic Stock Solutions (ERY, DOX, MOX) | Prepared, filter-sterilized concentrates for dilution in MIC and synergy testing. Erythromycin is often dissolved in ethanol, while doxycycline and moxifloxacin are in ultra-pure water [27]. |
| Hydrogen Peroxide (H₂O₂) | Used to test the vulnerability of biofilm towers to oxidative stress and virulence factors, revealing a key defensive weakness [27]. |
| Crystal Violet Stain | A quantitative dye-based assay used to measure the total biomass of biofilms remaining after experimental treatment [27]. |
| Methylprednisolone | A glucocorticoid used in conjunction with antibiotics in clinical studies to control the inflammatory response that contributes to severe pulmonary pathology in MPP [62]. |
The efficacy of antibiotic treatments, particularly in specialized fields such as mycoplasma removal research, is fundamentally dependent on precise and sensitive pathogen detection. Traditional culture-based methods, while considered a gold standard, are often hampered by prolonged turnaround times and limited sensitivity, especially for fastidious organisms [63] [64]. These limitations have accelerated the adoption of molecular diagnostics, which provide rapid, accurate, and comprehensive pathogen identification. Among these, Polymerase Chain Reaction (PCR) and Metagenomic Next-Generation Sequencing (mNGS) have emerged as cornerstone technologies. PCR offers high sensitivity and specificity for targeting known pathogens, whereas mNGS delivers a hypothesis-free approach capable of identifying virtually any pathogen from a sample, proving invaluable in cases of polymicrobial or culture-negative infections [64] [65] [66]. The integration of machine learning (ML) into these diagnostic frameworks is further revolutionizing the field by enhancing the interpretation of complex datasets, predicting antibiotic resistance, and ultimately guiding targeted therapeutic strategies. This guide provides a comparative analysis of PCR and mNGS, grounded in recent experimental data, and explores the burgeoning applications of machine learning in clinical microbiology.
Comparative Analysis of PCR and mNGS
The selection between PCR and mNGS is dictated by the clinical or research question at hand. The table below summarizes their core characteristics based on recent comparative studies.
Table 1: Core Characteristics of PCR and mNGS
| Feature | PCR (and targeted assays) | Metagenomic NGS (mNGS) |
|---|---|---|
| Core Principle | Amplification of specific, known DNA/RNA sequences using predefined primers and probes [67]. | Unbiased sequencing of all nucleic acids in a sample; no prior knowledge of pathogens required [64] [68]. |
| Detection Range | Narrow; limited to the specific pathogens targeted by the primer/probe set. | Broad; capable of detecting bacteria, viruses, fungi, and parasites simultaneously [63] [65]. |
| Turnaround Time | Short (a few hours) [64]. | Longer (typically 24-48 hours) [68]. |
| Cost | Relatively low [64]. | High [68] [69]. |
| Sensitivity | High for targeted pathogens [63]. | High, but can be affected by high levels of host DNA [70]. |
| Specificity | High [63]. | Variable; requires careful bioinformatic analysis to distinguish colonization from infection [64]. |
| Key Advantage | Rapid, cost-effective, and highly sensitive for confirming suspected pathogens. | Unbiased detection of novel, rare, and co-infecting pathogens without a prior hypothesis [65]. |
| Main Limitation | Requires a priori suspicion of the causative pathogen. | High cost, complex data interpretation, and risk of detecting contaminants or commensals [64]. |
Diagnostic Performance in Clinical Settings
Recent studies directly comparing these methods highlight their respective strengths. A large 2025 study on Mycobacterium tuberculosis (MTB) detection found a high overall agreement (98.38%) between mNGS and real-time PCR (RT-PCR), with both methods showing sensitivity above 90% and perfect specificity (100%) [63]. The study revealed that concordance was strongly influenced by microbial load, with perfect agreement in samples with low PCR cycle threshold (Ct) values (indicating high bacterial DNA), but lower concordance (76.47%) in samples with higher Ct values (20
In the context of lower respiratory tract infections (LRTIs), mNGS demonstrates a clear advantage in comprehensive pathogen identification. One 2025 study reported a significantly higher positive detection rate for mNGS compared to traditional methods (86.7% vs. 41.8%) [65]. It was particularly valuable for detecting polymicrobial infections and rare pathogens, such as non-tuberculous mycobacteria (NTM) and Legionella, which were frequently missed by other methods [65]. Another 2025 study comparing mNGS to two types of targeted NGS (tNGS) concluded that while capture-based tNGS showed the highest diagnostic accuracy for routine testing, mNGS was superior for detecting rare pathogens due to its unbiased nature [68].
Table 2: Comparative Diagnostic Performance from Recent Studies
| Study Context (Year) | Comparison | Key Performance Findings |
|---|---|---|
| Tuberculosis Detection (2025) [63] | mNGS vs. RT-PCR | Overall Agreement: 98.38%Sensitivity: mNGS 92.31%, RT-PCR 90.38%Specificity: Both 100% |
| Lower Respiratory Tract Infections (2025) [65] | mNGS vs. Traditional Methods (culture, PCR) | Positive Detection Rate: mNGS 86.7% vs. Traditional 41.8%Strength: mNGS identified 29 pathogens missed by traditional methods, including NTM and viruses. |
| Invasive Pulmonary Fungal Infections (2025) [69] | tNGS vs. mNGS vs. Culture | Sensitivity: tNGS 89.7%, mNGS (similar sensitivity), Culture 65.8%Specificity: tNGS 94.2%, Culture 100%Combining NGS with culture significantly improved sensitivity. |
| Periprosthetic Joint Infection (2025) [64] | mNGS vs. Culture | Sensitivity: mNGS significantly higher than culture.Strength: mNGS detected polymicrobial infections at 1.5x the rate of culture. |
Experimental Protocols for Key Studies
Protocol 1: mNGS for Mycobacterium tuberculosis Detection
This protocol is derived from a 2025 study that evaluated mNGS for MTB detection in 556 clinical samples [63].
- Sample Preparation: Bronchoalveolar lavage fluid (BALF), sputum, or other samples are collected. Sample is liquefied and homogenized.
- DNA Extraction: Total DNA is extracted using a commercial kit (e.g., IDSeq Micro DNA Kit). The extraction includes steps to lyse the hardy mycobacterial cell wall.
- Library Preparation: The extracted DNA is fragmented, and adapters are ligated to construct a sequencing library using a transposase method. This step does not involve pathogen-specific primers.
- Sequencing: The library is sequenced on a high-throughput platform (e.g., Illumina NextSeq 550), generating at least 10 million single-end 75bp reads per sample, with a quality score (Q30) of ≥85%.
- Bioinformatic Analysis:
- Quality Control: Low-quality and short sequences (<35 bp) are filtered out using tools like fastp.
- Host Depletion: Sequencing reads aligning to the human reference genome (GRCh38) are removed.
- Pathogen Identification: The remaining non-human reads are aligned against comprehensive microbial genome databases.
- Reporting: A positive MTB detection is reported if the number of reads mapped to the MTB genome exceeds a predefined threshold [63].
Figure 1: The mNGS Workflow for Pathogen Detection. This diagram illustrates the key steps from sample processing to pathogen identification, highlighting the unbiased, hypothesis-free approach.
Protocol 2: Targeted NGS (tNGS) for Fungal Pathogen Detection
This protocol is based on a 2025 study that developed a fungal-specific tNGS (Fi-tNGS) assay for invasive pulmonary fungal infections [69].
- Assay Design: A panel of primers is designed to target specific genomic regions of 64 clinically relevant fungal species.
- Sample Processing: BALF or sputum samples are collected and homogenized. Total nucleic acid (DNA and RNA) is extracted.
- Target Enrichment (Multiplex PCR): The extracted nucleic acids are subjected to a multiplex PCR reaction using the predefined primer pool. This step selectively amplifies the target fungal sequences, enriching them relative to host and other microbial DNA.
- Library Preparation & Sequencing: The amplified products (amplicons) are prepared for sequencing and loaded onto a sequencer (e.g., Illumina MiniSeq). The required sequencing depth is lower than for mNGS due to the targeted enrichment.
- Bioinformatic Analysis:
- Reads are demultiplexed and checked for quality.
- High-quality reads are directly aligned to a database of the targeted fungal sequences.
- Species-level identification is reported based on the aligned reads.
Figure 2: The Targeted NGS (tNGS) Workflow. This method uses a targeted primer panel to enrich for specific pathogens (e.g., fungi), increasing sensitivity and reducing cost and host background compared to mNGS.
The Scientist's Toolkit: Key Research Reagent Solutions
The successful implementation of these advanced detection methods relies on a suite of specialized reagents and tools.
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Example from Literature |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from diverse clinical samples (BALF, tissue, fluid). | QIAamp DNA Mini Kit [67], IDSeq Micro DNA Kit [63], MagPure Pathogen DNA/RNA Kit [68]. |
| Host DNA Depletion Reagents | Critical for mNGS sensitivity; reduces human background to improve microbial signal. | Benzonase and Tween20 [68]. |
| Library Preparation Kits | Prepares fragmented and adapter-ligated DNA libraries for sequencing on NGS platforms. | VAHTS Universal Pro DNA Library Prep Kit [70], Ovation Ultralow System V2 [68]. |
| Targeted Enrichment Panels | Primer or probe sets for tNGS; enables focused, sensitive detection of pathogen groups. | Fi-tNGS primer pool for 64 fungal species [69], Respiratory Pathogen Detection Kit [68]. |
| Positive Control Materials | Validates the entire testing process, from extraction to detection. | Quantified microbial standards (e.g., 500 CFU/mL of C. albicans for LoD) [69]. |
| Bioinformatics Pipelines | Software for quality control, host read removal, and microbial classification. | Fastp, BWA, Bowtie2, KneadData, and custom databases [63] [68] [70]. |
The Role of Machine Learning and Future Directions
Machine learning is poised to address some of the most significant challenges in molecular pathogen detection. Current research focuses on several key applications:
- Differentiating Infection from Colonization: ML models can be trained on mNGS and tNGS datasets, incorporating data such as pathogen read counts, genomic coverage, and clinical metadata (e.g., white blood cell count, imaging) to more accurately predict whether a detected microorganism is a true pathogen or a bystander colonizer [64].
- Predicting Antibiotic Resistance: By analyzing genetic sequences, ML algorithms can help identify known resistance markers and predict phenotypic resistance from genotypic data, potentially overcoming the limitations of culture-based antibiotic susceptibility testing [64]. This is particularly relevant for mycoplasma, where resistance mechanisms like the A2063G mutation in 23S rRNA are well-defined [67].
- Workflow Optimization and Integration: ML can assist in automating and optimizing bioinformatic analysis, reducing turnaround time, and integrating multi-omics data for a holistic view of the host-pathogen interaction. The future of microbial diagnostics lies in the intelligent integration of mNGS and tNGS data, refined by machine learning algorithms, to provide clinicians with actionable insights for personalized antibiotic therapy, directly impacting research on mycoplasma removal efficacy and other antimicrobial strategies.
Overcoming Treatment Failure: Synergistic Combinations and Alternative Modalities
Thesis Context: The escalating global challenge of antimicrobial resistance (AMR) has necessitated a paradigm shift in therapeutic strategies, particularly for pathogens capable of forming biofilms. Among these, Mycoplasma pneumoniae stands out due to its intrinsic resistance to many antibiotic classes—a consequence of its natural lack of a cell wall—and its demonstrated ability to form resilient biofilm structures. These biofilms are a critical virulence factor, strongly associated with chronic and recurrent respiratory infections, as well as extrapulmonary complications. This guide objectively compares the efficacy of combining the macrolide erythromycin with either doxycycline (a tetracycline) or moxifloxacin (a fluoroquinolone) for eradicating M. pneumoniae biofilms. The focus is on presenting supporting experimental data on their synergistic interactions, providing researchers and drug development professionals with a clear comparison of these promising combination strategies.
Comparative Analysis of Combination Efficacy
The following tables summarize key quantitative data from recent studies investigating these antibiotic combinations against Mycoplasma pneumoniae biofilms.
Table 1: Minimum Inhibitory Concentration (MIC) Profiles of Individual Antibiotics This table outlines the baseline susceptibility of M. pneumoniae to the antibiotics in question, highlighting the prevalence of macrolide resistance and the retained susceptibility to other classes. Data is compiled from contemporary clinical isolates [71].
| Antibiotic (Class) | MIC Range (Susceptible Isolates) | MIC Range (Resistant Isolates) | Prevalence of Resistance (Representative Data) |
|---|---|---|---|
| Erythromycin (Macrolide) | ≤0.5 mg/L [71] | 128 - 1024 mg/L [71] | 100% of tested Chinese isolates (2023) [71] |
| Azithromycin (Macrolide) | ≤0.5 mg/L [71] | 4 - 256 mg/L [71] | 100% of tested Chinese isolates (2023) [71] |
| Doxycycline (Tetracycline) | ≤0.125 - 1 mg/L [71] | Not Reported | 0% (All tested isolates susceptible) [71] |
| Moxifloxacin (Fluoroquinolone) | ≤0.125 mg/L [71] | Not Reported | 0% (All tested isolates susceptible) [71] |
Table 2: Synergistic Eradication of Pre-Formed Biofilms This table compares the efficacy of combination therapy against mature M. pneumoniae biofilm "towers," a model for chronic infection. Data is derived from in vitro studies specifically testing these combinations [72] [27].
| Antibiotic Combination | Test Strain(s) | Assay Type | Key Finding on Synergy | Efficacy Against Pre-formed Biofilms |
|---|---|---|---|---|
| Erythromycin + Doxycycline | M. pneumoniae M129 & 19294 [27] | Checkerboard, Crystal Violet, SEM | Synergistic Interaction [72] [27] | Substantial reduction in biofilm biomass; near-complete eradication observed via SEM [27] |
| Erythromycin + Moxifloxacin | M. pneumoniae M129 & 19294 [27] | Checkerboard, Crystal Violet, SEM | Synergistic Interaction [72] [27] | Substantial reduction in biofilm biomass; near-complete eradication observed via SEM [27] |
Detailed Experimental Protocols for Synergy Testing
To ensure reproducibility and provide a clear framework for the presented data, this section details the key methodologies used in the cited research.
Broth Microdilution for Minimum Inhibitory Concentration (MIC)
The MIC is the gold standard for determining the in vitro susceptibility of a microorganism to an antimicrobial agent. The protocol for M. pneumoniae is as follows [71]:
- Bacterial Preparation: M. pneumoniae stocks are syringed and diluted in SP-4 or PPLO broth to achieve a final inoculum of approximately 1.0 x 10⁴ CFU/mL.
- Plate Setup: A 96-well microplate is used. Each antibiotic is serially diluted twofold in the appropriate broth across the plate's rows.
- Inoculation and Incubation: The prepared bacterial inoculum is added to each well. Plates are sealed and incubated at 37°C until a color change (from red to yellow, due to phenol red pH indicator) is observed in the growth control wells, typically taking 6-8 days.
- MIC Determination: The MIC is defined as the lowest concentration of antibiotic that completely inhibits bacterial metabolism, indicated by the absence of a color change in the well [71].
Checkerboard Assay for Synergy Testing
The checkerboard assay is a fundamental technique for quantifying drug interactions.
- Plate Setup: A 96-well plate is used. One antibiotic (e.g., Erythromycin) is diluted along the x-axis, while the second antibiotic (e.g., Doxycycline or Moxifloxacin) is diluted along the y-axis. This creates a matrix with every possible combination of the two drug concentrations [27].
- Inoculation and Analysis: The plate is inoculated with a standardized suspension of M. pneumoniae. After incubation, the Fractional Inhibitory Concentration (FIC) index is calculated for each combination. Synergy is typically defined as an FIC index of ≤0.5 [72] [27].
Biofilm Cultivation and Eradication Assay
Assessing antibiotic action against biofilms requires specific protocols distinct from planktonic cultures.
- Biofilm Formation: M. pneumoniae is inoculated into 24-well or 96-well plates containing SP-4 broth and incubated for an extended period (several days) to allow for the development of mature biofilm towers [27].
- Treatment and Quantification: Pre-formed biofilms are treated with antibiotics, either alone or in combination, at clinically relevant concentrations. The most common method for quantifying remaining biofilm biomass is the crystal violet assay:
- Visual Confirmation: To confirm results from crystal violet staining, Scanning Electron Microscopy (SEM) is employed. This provides high-resolution images that visually confirm the architectural integrity or disintegration of the biofilm structures following treatment [27].
Visualizing the Experimental Workflow
The following diagram illustrates the logical sequence and key decision points in the process of testing synergistic antibiotic combinations for biofilm eradication, as described in the experimental protocols.
Figure 1. Experimental workflow for evaluating synergistic antibiotic combinations against Mycoplasma pneumoniae biofilms, from initial isolation to final confirmation.
The Scientist's Toolkit: Key Research Reagents and Materials
Successfully conducting these experiments requires specific biological materials, reagents, and equipment. The table below lists essential solutions and their functions as used in the cited studies.
Table 3: Essential Research Reagents and Materials
| Item Name | Specific Function / Application in Research | Key Details / Considerations |
|---|---|---|
| SP-4 Broth | Complex culture medium for growing M. pneumoniae; used for MIC and biofilm culture [27]. | Requires supplementation with serum (e.g., Fetal Bovine Serum) as a source of cholesterol [73]. |
| PPLO Broth | Alternative culture medium base; used for antimicrobial susceptibility testing [71]. | Similar to SP-4, requires enrichment with serum and yeast extract for robust growth of mycoplasma [71]. |
| Erythromycin Stock | Macrolide antibiotic; component of synergistic combinations [27]. | Typically dissolved in ethanol (e.g., 25.6 mg/mL stock); filter-sterilized and stored at -20°C [27]. |
| Doxycycline Stock | Tetracycline antibiotic; component of synergistic combinations [27]. | Typically dissolved in ultra-pure water (e.g., 20 mg/mL stock); filter-sterilized and stored at -20°C [27]. |
| Moxifloxacin Stock | Fluoroquinolone antibiotic; component of synergistic combinations [27]. | Typically dissolved in ultra-pure water (e.g., ~2 mg/mL stock); filter-sterilized and stored at -20°C [27]. |
| Crystal Violet Solution | A histological dye used to stain and quantify adherent biofilm biomass [72] [27]. | Applied to fixed biofilms; dissolved in a solvent like ethanol or acetic acid for absorbance measurement. |
| 96-well Microplates | Platform for high-throughput MIC, checkerboard, and biofilm assays [27] [71]. | Polystyrene plates are standard; ensure consistency for biofilm formation studies. |
| M. pneumoniae Strains | Clinical or reference strains for in vitro experiments [27]. | Common strains include M129 (ATCC 29342) and 19294; use of multiple strains is recommended for generalizability [27]. |
The data compellingly demonstrate that combinations of erythromycin with either doxycycline or moxifloxacin exhibit strong synergistic activity against Mycoplasma pneumoniae biofilms in vitro. This synergy is particularly significant given the near-ubiquitous resistance to macrolides like erythromycin when used alone. Both combinations achieved substantial, and in some cases near-complete, eradication of pre-formed biofilms, a feat rarely accomplished with monotherapies. For researchers and drug developers, these findings underscore the potential of revisiting existing antibiotics through the lens of combination therapy. While both combinations are promising, the choice between a doxycycline- or moxifloxacin-based regimen may ultimately hinge on further preclinical and clinical factors, including toxicity profiles—especially relevant for pediatric populations—and the potential for resistance development to the companion drug. This comparative guide provides a foundational dataset and methodological framework for advancing these synergistic strategies toward clinical application.
The treatment of severe and refractory Mycoplasma pneumoniae pneumonia (RMPP) in pediatric patients represents a significant clinical challenge, particularly given the global rise of macrolide-resistant strains. In regions such as East Asia, macrolide-resistant M. pneumoniae (MRMP) rates exceed 80%, necessitating alternative therapeutic strategies [74] [75]. This review objectively compares the efficacy, safety, and application protocols of two principal second-line antibiotic classes—tetracyclines (specifically doxycycline) and fluoroquinolones—for managing pediatric RMPP when first-line macrolide therapy fails.
Comparative Efficacy Data for Second-Line Agents
Table 1: Comparative Efficacy of Doxycycline and Fluoroquinolones in Pediatric MRMP
| Outcome Measure | Doxycycline/Tetracyclines | Fluoroquinolones | Comparative Findings |
|---|---|---|---|
| Treatment Efficacy Rate | 88.6% (doxycycline) [8] | 90% (lascufloxacin) [31] | Comparable high efficacy |
| Fever Resolution Time | −1.5 days vs. macrolides [8] | 1-2 days (levofloxacin) [75] | Doxycycline shows significant reduction |
| Time to Cough Relief | 5.4 ± 1.2 days (significantly faster) [8] | Not specifically reported | Doxycycline demonstrates superior symptom relief |
| Defervescence within 48h | 90% (minocycline) [31] | 90% (lascufloxacin) [31] | Equivalent for minocycline and lascufloxacin |
| Therapeutic Advantage | Superior efficacy vs. macrolides (OR=0.33) [75] | Shortened defervescence vs. macrolides [75] | Both classes effective alternatives |
Table 2: Safety Profiles of Second-Line Agents in Pediatrics
| Safety Parameter | Doxycycline | Fluoroquinolones |
|---|---|---|
| Common Adverse Events | Mild rash, gastrointestinal discomfort (18.2% incidence) [8] | Arthralgia, musculoskeletal events [75] |
| Serious Safety Concerns | Theoretical tooth discoloration (low risk with doxycycline) [75] | Cartilage toxicity concerns, antibiotic resistance [75] |
| Evidence from Studies | No tooth discoloration observed in clinical studies [8] [75] | No significant difference in bone/muscle damage in meta-analysis [75] |
| Clinical Guidelines | Recommended for courses <21 days in children <8 years [75] | Reserved for cases where tetracyclines are contraindicated [75] |
Resistance Mechanisms and Antibiotic Selection
The rising incidence of MRMP stems from point mutations in the 23S rRNA gene, specifically an A-to-G transition at position 2063, which confers high-level macrolide resistance [31]. This resistance pattern has necessitated the development of clear clinical pathways for transitioning to second-line agents.
Experimental Design and Methodologies
Clinical Trial Design for Efficacy Assessment
Recent investigations into second-line agents for RMPP have employed rigorous clinical trial methodologies. The doxycycline efficacy study utilized a comparative group design with 92 pediatric patients divided into doxycycline (44 cases) versus continued macrolide therapy (48 cases) [8]. Participants were children under eight years hospitalized with severe MP pneumonia (SMPP) who had failed to respond to at least three days of prior macrolide therapy, meeting criteria for macrolide-unresponsive MP pneumonia (MUMPP) [8].
The experimental group received oral doxycycline at 2 mg/kg every 12 hours for 10 days, while the control group continued macrolide therapy. Both groups received standardized adjuvant treatments including methylprednisolone (2 mg/kg/day, adjustable to 4-6 mg/kg/day in severe cases), bronchoalveolar lavage when indicated, and supportive care. Primary outcome measures included time to cough relief, pulmonary rale resolution, fever resolution time, hospitalization duration, and overall treatment efficacy rate assessed via chest CT scans one week post-therapy initiation [8].
Diagnostic Criteria and Resistance Monitoring
Table 3: Key Reagents and Diagnostic Tools for MP Research
| Research Tool | Application/Function | Experimental Implementation |
|---|---|---|
| PCR for 23S rRNA | Detection of A2063G mutation conferring macrolide resistance [31] | Identified macrolide-resistant strains with A-to-G transition at position 2063 |
| Mycoplasma Culture | Pathogen isolation and antimicrobial susceptibility testing [75] | Culturing bacterial samples to confirm MP and identify resistance genes |
| Chest CT Imaging | Assessment of pulmonary lesions and treatment efficacy [8] | Performed one week post-therapy to evaluate resolution of consolidation |
| BAL (Bronchoalveolar Lavage) | Sample collection and therapeutic intervention [8] | Performed immediately after excluding contraindications per 2018 Chinese Guidelines |
| Serological Testing | MP antibody detection (four-fold increase convalescent vs. acute) [74] | Confirmed MP diagnosis alongside clinical presentation |
Molecular Analysis of Resistance Mechanisms
Fluoroquinolone resistance studies employed multilocus sequence typing (MLST) and genetic evolutionary analysis of whole-genome sequences from 77 Mycoplasma bovis isolates (2008-2023) to identify resistance mutations [76]. While conducted on M. bovis, these methodologies inform understanding of potential resistance mechanisms in M. pneumoniae.
Researchers amplified and sequenced quinolone resistance-determining regions (QRDRs) of parC and gyrA genes. Molecular dynamic simulations assessed binding energies between mutant proteins and fluoroquinolones, revealing that GyrA S83F/Y and ParC S80R double mutations caused high-level fluoroquinolone resistance by decreasing drug-binding stability [76].
Discussion and Clinical Implications
The accumulating evidence supports doxycycline as the preferred second-line agent for pediatric RMPP due to its demonstrated efficacy, favorable safety profile in young children, and minimal resistance development. Clinical guidelines now reflect this shift, with the Canadian Pediatric Society and American Academy of Pediatrics endorsing doxycycline for courses under 21 days in children younger than eight when indicated [75].
Fluoroquinolones remain valuable alternatives when tetracyclines are contraindicated, though their use should be judicious due to concerns about cartilage toxicity and emerging resistance patterns. The discovery of novel fluoroquinolone resistance mutations, including ParC S80R in Mycoplasma species, underscores the need for ongoing surveillance and prudent antimicrobial stewardship [76].
Future research should focus on optimizing dosing regimens, identifying predictive biomarkers for treatment failure, and developing novel antimicrobial approaches to address the evolving challenge of resistant Mycoplasma pneumoniae infections in pediatric populations.
The rise of antimicrobial resistance (AMR) represents one of the most critical challenges to global public health in the 21st century, with multidrug-resistant (MDR) pathogens contributing to millions of deaths annually [77]. As traditional antibiotics become increasingly ineffective, the scientific community has accelerated research into non-antibiotic antimicrobial strategies. Among these approaches, hydrogen peroxide (H₂O₂) has emerged as a widely used biocide with broad-spectrum activity against bacteria, viruses, fungi, and spores [78]. Its appeal lies in its relatively low toxicity and environmentally friendly breakdown products—water and oxygen [78].
This review examines the efficacy of hydrogen peroxide against bacterial biofilms, which represent a particular challenge in healthcare settings and industrial applications. Biofilms are structured microbial communities encased in a protective extracellular matrix that confers significant resistance to antimicrobial agents—up to 1,000 times more resistant than their planktonic counterparts [77] [78]. We focus specifically on the performance of hydrogen peroxide formulations against biofilms formed by clinically relevant pathogens, with particular emphasis on Gram-negative organisms from the ESKAPEE group that pose significant threats in healthcare environments [79].
Hydrogen Peroxide Mechanisms of Action
Hydrogen peroxide exerts its antimicrobial effects primarily through the generation of highly reactive hydroxyl radicals (OH·) via Fenton-type reactions [80] [78]. These radicals attack multiple cellular components, including membrane lipids, DNA, and other essential cell structures [80]. The oxidative damage leads to rapid cell death in susceptible microorganisms.
Against biofilms, hydrogen peroxide demonstrates additional mechanisms of action. In Gram-negative bacteria, internally produced H₂O₂ may play a role in biofilm differentiation and dispersal [80]. For Staphylococci, studies have shown that hydrogen peroxide can reduce the expression of the icaADB cassette, which is involved in polysaccharide intercellular adhesion—a key component of biofilm stability [80]. This multi-target mechanism makes hydrogen peroxide potentially effective against both planktonic and biofilm-associated microorganisms, though with markedly different efficacy levels.
Experimental Approaches for Evaluating Antimicrobial Efficacy
Standard Susceptibility Testing
The minimum inhibitory concentration (MIC) against planktonic cultures is typically determined using broth dilution methods according to established standards [80]. For hydrogen peroxide, these tests generally employ concentration ranges from 100 to 800 ppm (approximately 3-24 mM) against a standardized inoculum of 10⁶ CFU/mL for bacteria [80]. The minimum bactericidal concentration (MBC) is determined by subculturing samples from tubes showing no visible growth.
Biofilm Susceptibility Testing
Evaluating antimicrobial efficacy against biofilms requires specialized methodologies that account for the unique properties of biofilm communities. Common approaches include:
- Biofilm cultivation: Mature biofilms are typically grown on relevant surfaces (e.g., stainless steel, titanium, polymethylmethacrylate) for 24 hours to allow for complete matrix development [81] [78].
- Treatment exposure: Biofilms are exposed to antiseptic solutions for clinically relevant contact times (typically 1-10 minutes) [81].
- Viability assessment: Post-treatment biofilm viability is quantified through colony-forming unit (CFU) counts, metabolic assays, or molecular methods [81] [78].
- Log reduction calculation: The efficacy is expressed as log₁₀ reduction in viable counts compared to untreated controls [80].
Table 1: Key Methodological Parameters for Biofilm Efficacy Studies
| Parameter | Typical Range | References |
|---|---|---|
| Biofilm maturation time | 24 hours | [78] [79] |
| Hydrogen peroxide concentration | 0.5-20 mM (planktonic); up to 200 mM (biofilms) | [78] [79] |
| Exposure time | 1 minute to 24 hours | [78] [79] |
| Temperature | Room temperature (20-25°C) | [78] |
| Neutralization method | Dilution or chemical neutralizers | [78] |
Figure 1: Experimental Workflow for Evaluating Hydrogen Peroxide Efficacy Against Biofilms
Comparative Efficacy of Hydrogen Peroxide Against Biofilms
Efficacy Against Planktonic vs. Biofilm Cells
Multiple studies demonstrate a dramatic reduction in hydrogen peroxide susceptibility when bacteria transition from planktonic to biofilm growth states. Perumal et al. reported that planktonic cultures of clinically important Gram-negative pathogens exhibited MIC values of 0.5-20 mM H₂O₂, regardless of their drug resistance profiles [78] [79]. However, biofilms of the same strains showed up to 266-fold reduced susceptibility to hydrogen peroxide and its commercial formulations [78] [79].
The degree of reduced susceptibility correlated strongly with the biofilm-forming capacity of individual strains, with variation observed between species [79]. This highlights the critical importance of testing antimicrobial efficacy against biofilms rather than extrapolating from planktonic susceptibility data.
Table 2: Comparative Susceptibility of Planktonic vs. Biofilm Cells to Hydrogen Peroxide
| Bacterial Species | Planktonic MIC (mM H₂O₂) | Biofilm Effective Concentration (mM H₂O₂) | Reduction Factor |
|---|---|---|---|
| Acinetobacter spp. | 7-14 | >200 (at 1 min exposure) | >14-28× |
| Klebsiella pneumoniae | 7-14 | >200 (at 1 min exposure) | >14-28× |
| Pseudomonas aeruginosa | 7-14 | >200 (at 1 min exposure) | >14-28× |
| Staphylococcus aureus | 100-300 ppm* | Not reported | - |
| Escherichia coli | 100-300 ppm* | Not reported | - |
*Data from sensitivity testing with H₂O₂ range 100-800 ppm [80]
Formulation Effects on Hydrogen Peroxide Efficacy
Commercial hydrogen peroxide formulations often include additional active ingredients designed to enhance efficacy. Accelerated hydrogen peroxide formulations containing acids demonstrated better performance at short exposure times, while ethanol-containing products required longer contact times to achieve similar effects [78] [79].
A network meta-analysis of irrigation solutions for periprosthetic joint infections found that 10% povidone-iodine (containing approximately 1% available iodine) for 5 minutes exposure achieved the greatest effect against mature biofilms, with hydrogen peroxide-based solutions showing variable performance [81]. This suggests that while hydrogen peroxide has value as an antimicrobial, its efficacy against biofilms may be surpassed by other antiseptic approaches in specific clinical contexts.
Spectrum of Activity and Limitations
Hydrogen peroxide exhibits a broad but incomplete spectrum of antimicrobial activity. One evaluation of hydrogen peroxide against dental unit water line biofilms found it effective against many bacteria including Pseudomonas spp., Streptococcus spp., Staphylococcus spp., and E. coli, with minimum inhibitory concentrations between 100-300 ppm [80]. However, the same study noted no inhibitory effects against Aggregatibacter actinomycetemcomitans, Candida glabrata, Candida parapsilosis, Fusobacterium nucleatum, or Parvimonas micra [80], indicating significant gaps in its coverage.
The Researcher's Toolkit: Essential Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Hydrogen Peroxide Biofilm Studies
| Reagent/Category | Function/Application | Examples/Specific Uses |
|---|---|---|
| Hydrogen Peroxide Formulations | Primary antimicrobial agent tested | Unformulated H₂O₂; accelerated H₂O₂ with silver, ethanol, or acids [78] [79] |
| Biofilm Cultivation Surfaces | Substrate for biofilm growth | Stainless steel, titanium, polymethylmethacrylate [81] [78] |
| Viability Assessment Tools | Quantification of surviving bacteria post-treatment | Colony forming unit (CFU) counts; metabolic assays; PCR-based quantification [82] [81] |
| Detection & Visualization | Observation and quantification of biofilms | Hoechst 33342 DNA staining; confocal microscopy; flow cytometry [83] [82] |
| Comparative Antiseptics | Benchmarking H₂O₂ performance against alternatives | Povidone-iodine (10%, 0.3%); chlorhexidine gluconate [81] |
Hydrogen peroxide remains a valuable tool in the arsenal against microbial contamination, particularly for planktonic microorganisms. However, its efficacy against mature biofilms is significantly compromised, with biofilms exhibiting up to 266-fold reduced susceptibility compared to their planktonic counterparts [78] [79]. This limitation is particularly evident with clinical isolates of multidrug-resistant nosocomial pathogens, raising concerns about the reliance on hydrogen peroxide-based disinfectants alone for biofilm control in healthcare settings [79].
The variable performance of different hydrogen peroxide formulations suggests that product selection should be guided by specific use cases, with accelerated formulations containing acids showing advantages for rapid disinfection and ethanol-based products potentially requiring longer contact times [78]. Researchers and clinicians should consider these limitations when designing disinfection protocols for biofilm-associated pathogens, particularly in the context of implant-associated infections where biofilm eradication is critical for therapeutic success.
Future research should focus on optimizing hydrogen peroxide formulations and delivery systems to enhance biofilm penetration, as well as exploring combination therapies with other antimicrobial agents to overcome the limitations of single-agent approaches.
Comparative Efficacy of Adjunctive Therapies for SevereM. pneumoniaePneumonia
The management of Severe Mycoplasma pneumoniae Pneumonia (SMPP) increasingly relies on adjunctive therapies, primarily corticosteroids and bronchoscopic intervention, to counter the excessive immune response and mechanical complications that characterize severe and refractory cases. The efficacy of these interventions varies based on specific clinical profiles, as summarized in the table below.
Table 1: Efficacy Comparison of Adjunctive Therapies for Severe M. pneumoniae Pneumonia
| Adjunctive Therapy | Reported Efficacy & Key Findings | Patient Population / Context | Key Clinical Outcomes |
|---|---|---|---|
| Corticosteroids [84] [85] [62] | Effective in reducing fever and inflammation; low-dose (e.g., 1-2 mg/kg methylprednisolone) shows similar efficacy to high-dose with a better safety profile [62]. | Children and adults with severe or refractory MP pneumonia; often used with antibiotics [84] [85]. | Shorter fever duration [84] [85]; rapid improvement in clinical symptoms and chest radiographic findings [84]; prevents pulmonary lesions with fewer side effects (e.g., hypertension) at low doses [62]. |
| Bronchoscopic Intervention (BAL) [86] [87] | Highly effective for pulmonary atelectasis in MPP; increases lung recruitment and shortens CRP recovery time [86]. Increases pathogen detection and resolves lung lesions in multilobar consolidation [87]. | Children with MPP complicated by pulmonary atelectasis or multilobar consolidation [86] [87]. | Higher incidence of lung recruitment [86]; shorter lesion-resolution duration on imaging [87]; effective removal of mucus plugs causing obstruction [87]. |
| Corticosteroid-Resistant RMPP [88] | Predictors of resistance: fever duration ≥11 days, lymphocytes ≤32%, CRP ≥48.73 mg/L, LDH ≥545.7 U/L [88]. | Children with Refractory MPP (RMPP) not responding to standard corticosteroid regimens [88]. | Associated with mucus plug formation often requiring bronchoscopy; longer hospitalization and higher complication rates (e.g., pleural effusion) [88]. |
Detailed Experimental Protocols and Methodologies
Corticosteroid Clinical Trial Protocol
A recent multi-center, randomized controlled trial established the protocol for evaluating corticosteroid efficacy in children with SMPP [62].
- Patient Population: Pediatric patients diagnosed with severe MPP. Diagnosis is based on clinical symptoms, radiological confirmation of pneumonia, and serological or PCR-based evidence of M. pneumoniae infection [74] [62].
- Intervention Groups: Patients are randomized into two treatment groups. Both groups receive a standard antibiotic (e.g., azithromycin). One group receives low-dose methylprednisolone, while the other receives high-dose methylprednisolone [62].
- Primary Outcome: The incidence of adverse pulmonary lesions, assessed via chest imaging at six months post-treatment [62].
- Secondary Outcomes: These include the time to defervescence (fever resolution), duration of hospitalization, and the incidence of adverse drug effects such as hypertension [62].
- Statistical Analysis: A statistical comparison of primary and secondary outcomes between the low-dose and high-dose groups determines the optimal dose based on a balance of efficacy and safety [62].
Bronchoscopic Intervention Analysis Protocol
The efficacy of Bronchoalveolar Lavage (BAL) is often demonstrated through retrospective cohort studies with propensity-score matching to minimize bias [86] [87].
- Study Design & Population: Retrospective analysis of children hospitalized with MPP complicated by atelectasis or multilobar consolidation. The cohort is divided into those who underwent bronchoscopy with BAL and those who did not (non-BAL group) [86] [87].
- Matching Procedure: Propensity Score Matching (PSM) is used to balance baseline characteristics (e.g., age, fever duration, severity markers) between the BAL and non-BAL groups, ensuring a fair comparison [86].
- BAL Procedure: A fiberoptic bronchoscope is passed through the vocal cords under sedation. Lidocaine is applied for local anesthesia. The bronchoscope is advanced to the lesion site, and sterile saline at 37°C is instilled in aliquots of 0.5–1.0 mL/kg, followed by immediate suction [86].
- Outcome Measures:
- Radiological Recovery: Two independent, blinded radiologists assess chest images. A reduction in the atelectasis area of more than 50% is considered effective pulmonary recruitment [86].
- Inflammatory Markers: The time for C-reactive protein (CRP) to drop below 8 mg/L is tracked [86].
- Other Clinical Outcomes: Duration of fever, length of hospital stay, and co-infection detection rates are also analyzed [87].
Mechanistic Pathways and Clinical Decision Logic
The rationale for using adjunctive therapies stems from the immunopathogenesis of SMPP. The following diagram illustrates the underlying immune-mediated lung injury and the mechanistic targets of corticosteroids and bronchoscopy.
Diagram 1: Mechanism of SMPP and Adjunctive Therapy Targets. M. pneumoniae infection triggers an excessive host immune response, leading to inflammatory lung damage and mucus plug formation. Corticosteroids target the inflammatory pathway, while bronchoscopy mechanically addresses airway obstruction.
The decision to apply these therapies in a clinical or research setting follows a logical workflow based on patient response and complication profile.
Diagram 2: Clinical Decision Logic for Adjunctive Therapies. This workflow guides the application of corticosteroids and bronchoscopy based on treatment response and complications, including assessment for corticosteroid resistance.
Research Reagent Solutions and Essential Materials
The following table details key reagents and materials essential for conducting research on M. pneumoniae and evaluating therapeutic efficacy, derived from the analyzed experimental protocols.
Table 2: Essential Research Reagents and Materials for M. pneumoniae Investigation
| Reagent/Material | Function in Research | Example Application/Note |
|---|---|---|
| SP-4 Broth | Culture medium for axenic cultivation of M. pneumoniae strains [27]. | Used for maintaining bacterial stocks and in vitro experiments like MIC testing and biofilm assays [27]. |
| Methylprednisolone / Prednisolone | Synthetic glucocorticoid to modulate inflammatory response in vivo. | Dosing is critical; low-dose (1-2 mg/kg) vs. high-dose (5-10 mg/kg) comparisons are relevant for efficacy and safety studies [84] [62]. |
| Fiberoptic Bronchoscope | Medical device for visualizing airways and performing Bronchoalveolar Lavage (BAL). | Key for therapeutic intervention studies on atelectasis and for obtaining deep-lung samples for pathogen analysis [86] [87]. |
| PCR Assays | Detection of M. pneumoniae DNA/RNA in respiratory samples (e.g., nasopharyngeal secretions, BAL fluid) [86] [74]. | Considered a gold standard for active infection diagnosis in clinical research due to high sensitivity and specificity [74] [89]. |
| Serological Assays (IgM ELISA, Latex Agglutination) | Detection of host antibody response to M. pneumoniae infection. | A four-fold increase in antibody titer in paired sera is a common diagnostic criterion in clinical studies [84] [74]. |
| Antibiotics (Macrolides, Tetracyclines, Fluoroquinolones) | Investigational and comparative agents for background therapy in adjunctive therapy trials. | Includes Azithromycin (macrolide), Doxycycline (tetracycline), and Moxifloxacin (fluoroquinolone) for studying resistant strains or combination therapy [31] [27]. |
Mycoplasma pneumoniae is a formidable and common contaminant in cell culture laboratories, capable of inducing chronic infections and compromising experimental integrity. As a bacterium lacking a cell wall, it is intrinsically resistant to conventional antibiotics like β-lactams, making its eradication particularly challenging [8]. Compounding this problem is the widespread emergence of macrolide-resistant M. pneumoniae strains, with resistance rates exceeding 90% in some regions, primarily driven by point mutations in the 23S rRNA gene (A2063G and A2064G) [20]. Furthermore, M. pneumoniae can form structured biofilm towers that exhibit extreme antibiotic resistance, tolerating erythromycin concentrations up to 8,500–128,000 times the minimal inhibitory concentration (MIC) for planktonic cells [27]. These factors necessitate the exploration of alternative eradication strategies. Antimicrobial Photodynamic Therapy (aPDT) using methylene blue represents a promising non-antibiotic approach that utilizes light-activated oxygen species to destroy microbial pathogens, offering a potential solution for decontaminating cell cultures without promoting traditional drug resistance.
Comparative Analysis of Mycoplasma Eradication Strategies
The following table summarizes the efficacy of various interventions against Mycoplasma pneumoniae, based on current research findings.
Table 1: Comparison of Mycoplasma pneumoniae Eradication Strategies
| Strategy | Key Efficacy Findings | Advantages | Limitations/Considerations |
|---|---|---|---|
| Macrolides (e.g., Azithromycin) | - First-line treatment but failing efficacy due to resistance [8].- Resistance mutations (A2063G/A2064G) prolong fever duration and increase severity [20]. | - Historically effective [8]. | - High resistance rates (up to 90% in Asia) [20].- Ineffective against biofilms [27]. |
| Doxycycline (Tetracycline) | - Shorter cough relief time (5.4 ± 1.2 vs. 7.2 ± 1.6 days) and higher treatment efficacy (88.6% vs. 75.0%) vs. macrolides in children [8].- Effective in synergistic combinations against biofilms [27]. | - Effective against macrolide-resistant strains [8].- Low resistance profile [8]. | - Not first-choice in children due to potential side effects [27]. |
| Moxifloxacin (Fluoroquinolone) | - Effective in synergistic combinations with other antibiotics to eradicate pre-formed biofilm towers [27]. | - Potent antimicrobial activity [27]. | - Potential side effects limit use in children [27]. |
| Antibiotic Synergy (e.g., Erythromycin + Doxycycline) | - Checkerboard assays showed synergistic action against two M. pneumoniae strains [27].- Pairs of agents at clinical concentrations showed substantial efficacy against pre-formed biofilms [27]. | - Can overcome biofilm-mediated resistance [27].- Allows use of lower antibiotic concentrations [27]. | - Requires compatibility testing.- Potential for complex side effects. |
| Hydrogen Peroxide (H₂O₂) | - Biofilm towers provided no defense against H₂O₂, which was highly effective in eradication [27]. | - Effective against biofilm state [27].- Simple, small-molecule therapeutic [27]. | - Can be cytotoxic to host cells at high concentrations. |
| aPDT with Methylene Blue (MB) | - MB-mediated aPDT demonstrates strong, dose-dependent photodynamic activity against pathogens [90].- Generates reactive oxygen species (ROS) causing irreversible cell damage [90]. | - Broad-spectrum action regardless of antibiotic resistance pattern [91].- Low potential for microbial resistance [90]. | - Efficacy depends on PS retention, light dosimetry, and oxygen availability [92].- Can be antagonized by certain other PSs in combination [90]. |
Experimental Evidence and Protocols
In Vitro Antibiotic Synergy Testing Against Biofilms
Background: The study by Fahim et al. (2025) investigated methods to eradicate M. pneumoniae biofilm towers, which are highly resistant to single-antibiotic treatments [27].
Methodology:
- Biofilm Growth: M. pneumoniae strains (M129 and 19294) were grown in SP-4 broth in 24- or 96-well plates for several days to form mature biofilm towers [27].
- Checkerboard Assay: Used to test for antibiotic synergy between erythromycin (ERY), doxycycline (DOX), and moxifloxacin (MOX). Antibiotics were diluted in a series of twofold dilutions in SP-4 broth and combined in various concentrations in a 96-well plate inoculated with bacteria [27].
- Crystal Violet Assay: Pre-formed biofilms were treated with antibiotic combinations. After incubation, biofilms were stained with crystal violet to quantify remaining biomass, providing an initial assessment of eradication efficacy [27].
- Scanning Electron Microscopy (SEM): Treated biofilm towers were visualized using SEM to confirm the physical destruction of the biofilm structure, which revealed more complete eradication than crystal violet assays indicated [27].
Key Findings: Dual combinations of ERY, DOX, and MOX acted synergistically. When used at clinically relevant concentrations, these pairs showed substantial efficacy against pre-formed biofilm towers, with SEM confirming widespread destruction [27].
Clinical Evaluation of Doxycycline
Background: A 2025 study evaluated the efficacy and safety of doxycycline for Severe Mycoplasma pneumoniae Pneumonia (SMPP) in children under eight years old, a population where macrolide resistance is a significant concern [8].
Methodology:
- Patient Cohort: 92 pediatric SMPP cases were divided into a doxycycline treatment group (44 cases) and a macrolide control group (48 cases). All patients had not responded to at least three days of prior macrolide therapy [8].
- Treatment Protocol: The doxycycline group received oral doxycycline at 2 mg/kg every 12 hours for 10 days. The control group continued macrolide therapy. Both groups received consistent adjunct treatments, including methylprednisolone and bronchoscopic intervention if needed [8].
- Outcome Measures: Primary endpoints included cough relief time, pulmonary rale resolution time, fever resolution time, hospitalization duration, and overall treatment efficacy rate. Safety was assessed by monitoring adverse events [8].
Key Findings: The doxycycline group showed significantly shorter cough relief time (5.4 ± 1.2 vs. 7.2 ± 1.6 days) and pulmonary rale resolution time (6.2 ± 1.3 vs. 8.0 ± 1.7 days). The overall treatment efficacy rate was higher in the doxycycline group (88.6% vs. 75.0%), with no significant difference in adverse event rates and no tooth discoloration observed [8].
Methylene Blue aPDT Formulation and Testing
Background: The clinical translation of aPDT is often hindered by insufficient photosensitizer retention at the target site. A 2025 study developed a high-viscosity methylene blue formulation to address this challenge [92].
Methodology:
- Formulation Development: MB formulations were prepared with mucoadhesive polymers (Hydroxypropylmethylcellulose, HPMC; Carboxymethylcellulose, CMC) and a surfactant (Sodium Dodecyl Sulfate, SDS) to reduce MB aggregation and enhance viscosity for better retention [92].
- Characterization: The dimer-to-monomer (D/M) ratio was measured via spectrophotometry to optimize the formulation, as monomeric MB is more effective at generating singlet oxygen. pH, viscosity, and stability were also monitored [92].
- Microbial Uptake and In Vitro aPDT: Candida albicans biofilms were used to test MB uptake and the antimicrobial efficacy of the viscous formulation upon irradiation with red light, comparing it to aqueous MB [92].
Key Findings: The optimized formulation (0.005% MB, 0.25% SDS in 0.5% CMC at acidic pH) effectively reduced MB aggregation, maintained stability, and showed comparable antimicrobial efficacy in vitro to aqueous MB, despite lower biofilm uptake, highlighting its potential for clinical applications [92].
Workflow and Mechanism Visualization
Experimental Workflow for aPDT and Antibiotic Evaluation
The following diagram outlines a combined research approach for evaluating aPDT and antibiotic therapies against contaminated cell cultures.
Mechanism of Methylene Blue aPDT
This diagram illustrates the core mechanism of antimicrobial photodynamic therapy at the cellular level.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Mycoplasma Eradication Research
| Reagent / Material | Function/Description | Application Example |
|---|---|---|
| Methylene Blue (MB) | Phenothiazine dye photosensitizer; generates ROS upon light activation [90]. | Primary agent for aPDT protocols against planktonic and biofilm-associated mycoplasma [92]. |
| Doxycycline | Broad-spectrum tetracycline antibiotic; inhibits bacterial protein synthesis [8]. | Control/treatment arm for macrolide-resistant M. pneumoniae; used in synergy studies [8] [27]. |
| Moxifloxacin | Fluoroquinolone antibiotic; inhibits DNA gyrase and topoisomerase IV [27]. | Component of synergistic antibiotic combinations for biofilm eradication [27]. |
| Carboxymethylcellulose (CMC) | Anionic polymer; used as a mucoadhesive agent to increase formulation viscosity and retention [92]. | Key component in viscous MB formulations for improved clinical efficacy in aPDT [92]. |
| Sodium Dodecyl Sulfate (SDS) | Surfactant; reduces MB aggregation, promoting the monomeric form for more efficient singlet oxygen production [92]. | Additive in optimized MB formulations to enhance photodynamic activity [92]. |
| SP-4 Broth | Complex culture medium optimized for the growth of Mycoplasma pneumoniae [27]. | Culturing M. pneumoniae and for forming biofilm towers for in vitro efficacy testing [27]. |
| 660 nm Diode Laser | Light source matching the absorption peak of methylene blue for effective photoactivation [93] [92]. | Standard light source for activating MB in aPDT experiments [93]. |
The fight against mycoplasma contamination in cell cultures requires a multifaceted approach due to the limitations of traditional antibiotics, particularly the rise of resistance and the resilience of biofilms. Doxycycline has proven to be a clinically effective alternative for macrolide-resistant strains, while synergistic antibiotic combinations and hydrogen peroxide show promise in disrupting resistant biofilms in vitro [8] [27]. Antimicrobial Photodynamic Therapy with methylene blue emerges as a compelling non-antibiotic strategy, leveraging reactive oxygen species to inflict broad, multi-target damage on microbial cells with a low likelihood of inducing resistance [90] [91]. Future research should focus on optimizing MB formulations for cell culture applications, standardizing light delivery protocols, and exploring the full potential of aPDT-antibiotic combinations. This integrated arsenal of strategies provides researchers with powerful tools to safeguard the integrity of their cell-based systems.
Comparative Clinical Efficacy and Safety Profiles of Antibiotic Classes
The rising global prevalence of macrolide-resistant Mycoplasma pneumoniae (MRMP) presents a critical challenge in managing respiratory infections. While macrolides remain the first-line treatment for susceptible M. pneumoniae infections, their efficacy against resistant strains is significantly compromised. This comparison guide objectively analyzes clinical outcomes between macrolide monotherapy and the potential for spontaneous resolution in MRMP infections, providing researchers and drug development professionals with evidence-based experimental data and methodologies. The escalating resistance rates, particularly in East Asia where prevalence exceeds 75% in some regions [27] [15], underscore the urgency of understanding therapeutic limitations and bacterial behavior in the absence of effective antibiotic pressure. This evaluation synthesizes current clinical evidence and in vitro research to inform future antibiotic development and treatment strategies for resistant mycoplasma infections.
Comparative Clinical Outcomes Data
Table 1: Documented Clinical Outcomes in Macrolide-Resistant M. pneumoniae (MRMP) Infections
| Outcome Measure | Macrolide Monotherapy in Confirmed MRMP | Spontaneous Resolution (Self-Limiting Course) |
|---|---|---|
| Treatment Failure Rate | 31.6% progress to refractory pneumonia [94] | Limited data on confirmed MRMP; immunocompetent individuals may clear susceptible infections [27] |
| Fever Duration | Prolonged; >6.5 days indicates RMPP risk [94] | Typically shorter in susceptible, uncomplicated cases |
| Microbiological Clearance | Often failed; persistence despite therapy [94] | Possible for susceptible strains post-symptoms [27] |
| Radiological Progression | High rates of consolidation (74.7%) and atelectasis (26.3%) [94] | Not documented for resistant strains |
| Extrapulmonary Complications | 47.4% incidence [94] | Less common in uncomplicated, susceptible infections |
| Hospitalization Requirements | Extended stays; 86.9% hospitalization rate [10] | More common in outpatient settings for susceptible cases |
| Resistance Development | Possible amplification during therapy [95] | Not applicable |
Table 2: Alternative Antibiotic Efficacy Against MRMP
| Antibiotic Class | Example Agents | Efficacy Against MRMP | Key Clinical Findings |
|---|---|---|---|
| Tetracyclines | Doxycycline | High efficacy [8] | Shorter cough relief (5.4±1.2 vs 7.2±1.6 days) and higher efficacy rate (88.6% vs 75.0%) vs macrolides in children [8] |
| Fluoroquinolones | Levofloxacin, Moxifloxacin | High efficacy [96] | Successful in severe MRMP pneumonia failing macrolide therapy; rapid improvement in ICU patients [96] |
| Combination Therapy | Erythromycin + Doxycycline, Moxifloxacin + Doxycycline | Synergistic in vitro [27] [7] | Checkerboard assays show FICI <0.5; virtually eradicates biofilm towers at clinical concentrations [7] |
The clinical data demonstrates that macrolide monotherapy consistently underperforms in MRMP infections, with significant rates of treatment failure and disease progression. The progression to refractory Mycoplasma pneumoniae pneumonia (RMPP) occurs in nearly one-third of pediatric MRMP cases despite macrolide treatment [94]. These patients exhibit more severe pulmonary manifestations, including higher rates of lung consolidation (74.7% vs 42.5%) and atelectasis (26.3% vs 12.5%) compared to those with macrolide-sensitive infections [94].
The literature reveals a critical knowledge gap regarding spontaneous resolution of confirmed MRMP infections. While immunocompetent hosts can clear susceptible M. pneumoniae infections without antimicrobial intervention [27], the natural history of untreated MRMP remains poorly documented. The available evidence suggests that the virulence mechanisms and host immune evasion strategies of resistant strains may complicate spontaneous clearance, particularly given their association with biofilm formation [27] [7].
Resistance Mechanisms and Experimental Models
Molecular Basis of Macrolide Resistance
MRMP resistance primarily occurs through point mutations in domain V of the 23S rRNA gene, with A2063G and A2064G substitutions being most prevalent [15] [94] [10]. These mutations reduce macrolide binding affinity by altering the ribosomal target site. Regional variability exists in resistance patterns; Southern Italy reports a 7.5% MRMP prevalence with 96% attributed to A2063G mutation [10], while China documents rates exceeding 80% in some regions [15].
Emerging research indicates efflux pump mechanisms may contribute to resistance in some strains. Two clinical MRMP isolates were found to harbor efflux pump genes msrA/B and mefA, with the efflux pump inhibitor reserpine reducing azithromycin MIC to a quarter of original values [15]. This secondary resistance mechanism warrants consideration in drug development strategies.
Biofilm Formation and Treatment Implications
M. pneumoniae forms biofilm towers during prolonged infection, exhibiting extreme macrolide resistance (up to 512 µg/mL erythromycin, 8,500-128,000×MIC) [27] [7]. These structures demonstrate features consistent with chronic infection, including attenuated virulence factor production (H₂O₂, CARDS toxin) and enhanced complement resistance [7].
Diagram 1: MRMP Infection Pathway Flowchart - This diagram illustrates the progression of M. pneumoniae infections and critical decision points where treatment efficacy diverges based on resistance status.
Experimental Protocols and Methodologies
Broth Microdilution for Antimicrobial Susceptibility Testing
Purpose: Determine minimum inhibitory concentrations (MICs) of antimicrobial agents against M. pneumoniae isolates [15].
Methodology:
- Inoculum Preparation: Suspend M. pneumoniae cells in SP-4 broth to achieve final inoculum of 1.0×10⁴ CFU/mL [7]
- Antibiotic Dilution: Prepare twofold serial dilutions of antibiotics in 96-well plates (erythromycin, azithromycin, doxycycline, moxifloxacin)
- Incubation Conditions: Incubate at 37°C until growth controls show color change from red to yellow (typically 7-14 days)
- MIC Determination: Define MIC as lowest antibiotic concentration preventing color change
- Quality Control: Include drug-sensitive control strain (e.g., FH/ATCC 15531), sterility controls, and vehicle controls
Application: This method enabled researchers to establish that biofilm-associated M. pneumoniae exhibits dramatically increased erythromycin MICs (512 µg/mL versus 0.004-0.064 µg/mL for planktonic cells) [7].
Checkerboard Synergy Assay
Purpose: Evaluate interactive effects of antibiotic combinations against MRMP [7].
Methodology:
- Preparation: Dilute antibiotics to start with twice the MIC of each drug
- Plate Setup: Create decreasing concentrations of both antibiotics in 96-well plate format
- Inoculation: Add M. pneumoniae suspension to all wells except sterility controls
- Incubation: Incubate at 37°C until growth control shows color change
- FICI Calculation: Calculate Fractional Inhibitory Concentration Index using formula: FICI = (MIC drug A in combination/MIC drug A alone) + (MIC drug B in combination/MIC drug B alone)
- Interpretation: Define synergy as FICI <0.5; additive as FICI 0.5-1.0; indifferent as FICI 1.0-4.0; antagonistic as FICI >4.0
Key Findings: This methodology demonstrated that dual combinations of erythromycin, moxifloxacin, and doxycycline act synergistically (FICI <0.5) against both M129 and 19294 M. pneumoniae strains [7].
Biofilm Tower Eradication Assay
Purpose: Assess efficacy of antimicrobial agents against pre-formed M. pneumoniae biofilm towers [27] [7].
Methodology:
- Biofilm Formation: Grow M. pneumoniae in SP-4 broth for extended periods (≥10 days) until dome-shaped biofilm towers develop
- Treatment Application: Expose pre-formed biofilm towers to antimicrobial agents at clinically relevant concentrations
- Viability Assessment:
- Crystal Violet Staining: Quantify remaining biomass after treatment
- Scanning Electron Microscopy: Visualize structural integrity of biofilm towers post-treatment
- Complementary Approaches: Evaluate combinations with hydrogen peroxide (H₂O₂), to which biofilm towers remain sensitive despite erythromycin resistance
Significance: This protocol revealed that synergistic antibiotic combinations can virtually eliminate biofilm towers that are otherwise highly resistant to monotherapy [7].
Research Reagent Solutions
Table 3: Essential Research Materials for MRMP Investigation
| Reagent/Equipment | Specification | Research Application |
|---|---|---|
| SP-4 Broth Medium | Custom formulation with mycoplasma supplements [7] | Optimal axenic growth of M. pneumoniae for biofilm and MIC assays |
| M. pneumoniae Strains | M129 and 19294 subtypes [7] | Represent genetic diversity in resistance and biofilm studies |
| Antimicrobial Standards | Erythromycin, azithromycin, doxycycline, moxifloxacin [15] [7] | MIC determination and synergy studies |
| 96-Well Microplates | Sterile, tissue-culture treated | Broth microdilution and checkerboard assays |
| PCR Reagents | 23S rRNA domain V primers, sequencing reagents [15] [10] | Detection of A2063G, A2064G resistance mutations |
| Cell Culture System | BEAS-2B respiratory tissue culture cells [7] | Biofilm formation studies in host cell context |
| Scanning Electron Microscope | High-resolution imaging capability | Visualization of biofilm tower architecture and disruption |
The comparative analysis unequivocally demonstrates that macrolide monotherapy produces suboptimal outcomes in confirmed MRMP infections, with high treatment failure rates and significant complications. The potential for spontaneous resolution in genuine MRMP cases appears limited, as resistant strains are associated with more severe disease manifestations and complex survival mechanisms including biofilm formation. Promising research directions include synergistic antibiotic combinations that demonstrate efficacy against resistant strains and biofilms in vitro, particularly doxycycline-containing regimens [8] [7]. Future therapeutic development should prioritize approaches that target the unique biological features of MRMP, including its biofilm formation capabilities and resistance mechanisms, to effectively address this growing public health challenge.
Within the broader research on the mycoplasma removal efficacy of different antibiotics, macrolides remain a cornerstone of treatment. The comparison between first-generation macrolides, like erythromycin, and second-generation agents, like clarithromycin, provides critical insights for drug development. This guide objectively compares clarithromycin and erythromycin based on clinical efficacy, safety profiles, pharmacokinetic properties, and patient compliance, with a specific focus on applications in respiratory infections caused by Mycoplasma pneumoniae and other community-acquired pathogens. The analysis is grounded in a synthesis of recent meta-analyses, randomized controlled trials, and pharmacokinetic studies to provide researchers and scientists with a data-driven resource for decision-making.
Comprehensive Comparative Analysis: Data Tables
The following tables summarize the key quantitative comparisons between clarithromycin and erythromycin across multiple domains, from overall clinical efficacy to pharmacokinetic properties.
Table 1: Comparative Clinical Efficacy and Safety in Respiratory Infections
| Parameter | Clarithromycin | Erythromycin | Supporting Evidence (Source) |
|---|---|---|---|
| Clinical Success Rate (CAP, Adults/Adolescents) | Benchmark | RR 0.79 (95% CI, 0.64 to 0.98) vs. clarithromycin [97] | Meta-analysis of 4 RCTs (n=472) [97] |
| Clinical Cure Rate (CAP, Adults/Adolescents) | Benchmark | RR 0.67 (95% CI, 0.48 to 0.92) vs. clarithromycin [97] | Meta-analysis of 4 RCTs [97] |
| Radiological Success Rate (CAP) | Benchmark | RR 0.84 (95% CI, 0.71 to 0.996) vs. clarithromycin [97] | Meta-analysis of 4 RCTs [97] |
| Treatment Discontinuation Due to Adverse Effects | 4% (4/96 patients) [98] | 19% (21/112 patients) [98] | Multicenter, double-blind RCT (n=208) [98] |
| MP-PCR Negative Rate (Pediatric Mycoplasma Infection) | 96.23% (51/53 patients) [23] | 75.47% (40/53 patients) [23] | Randomized clinical trial (n=106) [23] |
Table 2: Pharmacokinetic and Dosing Profile Comparison
| Parameter | Clarithromycin | Erythromycin | Context and Implications |
|---|---|---|---|
| Bioavailability | 55% [99] | ~25% [99] | Clarithromycin's structural modification prevents acid degradation, leading to more predictable absorption [99]. |
| Half-Life (Hours) | 2.6 - 2.7 hrs [99] | 1.5 - 3.0 hrs [99] | Longer half-life supports less frequent dosing, improving compliance. |
| Dosing Frequency | Twice daily [98] | Four times daily [98] | Directly impacts patient compliance and convenience. |
| Food Effect | Absorption and bioavailability may be enhanced [99] | Bioavailability decreased for base and stearate formulations [99] | Affects dosing recommendations and consistency of drug exposure. |
| Tissue Penetration (Lung) | High (e.g., 13.5 mg/kg at 4h post-dose) [99] | Lower than newer macrolides | Superior tissue penetration exceeds MIC90 for many respiratory pathogens [99]. |
Table 3: Pediatric Outcomes and Compliance Metrics
| Parameter | Clarithromycin | Erythromycin | Study Details |
|---|---|---|---|
| Antipyretic Time (Days) | 2.63 ± 0.57 [23] | 4.06 ± 0.75 [23] | Randomized trial in children with respiratory mycoplasma infection (n=106) [23]. |
| Hospital Stay (Days) | 15.14 ± 2.01 [23] | 20.63 ± 3.15 [23] | Same as above [23]. |
| Medication Compliance Rate | Significantly Higher [23] | Significantly Lower [23] | Assessed via Morisky questionnaire; clarithromycin group had lower drug costs [23]. |
| Incidence of GI Side Effects | Significantly Lower [23] | Significantly Higher [23] | Mainly nausea, diarrhea, and abdominal pain [23]. |
Analysis of Key Comparative Studies and Experimental Protocols
Clinical Efficacy in Community-Acquired Pneumonia (CAP)
A 2022 meta-analysis of randomized controlled trials (RCTs) provides high-level evidence comparing the efficacy of these macrolides in adults and adolescents with CAP. The analysis included four RCTs with a total of 472 patients, all comparing erythromycin monotherapy to clarithromycin monotherapy. No studies comparing erythromycin to azithromycin monotherapy were found.
- Methodology: The researchers performed a systematic search of PubMed, EMBASE, Cochrane Library, and clinical trial registries up to November 2021. They used random-effects models to calculate risk ratios (RR) with 95% confidence intervals (CI) for dichotomous outcomes, including clinical success, clinical cure, and radiological success [97] [100].
- Results: The meta-analysis concluded that erythromycin was associated with significantly lower rates of clinical success (RR, 0.79), clinical cure (RR, 0.67), and radiological success (RR, 0.84) compared to clarithromycin. The authors noted that given this inferior efficacy and higher adverse event profile, erythromycin should not be the first-choice macrolide for CAP when clarithromycin (or azithromycin) is available [97].
Safety and Tolerability Profile
A 1991 multicenter, double-blind, randomized trial exemplifies the significant differences in tolerability that have been consistently observed.
- Methodology: This trial randomized 208 adult patients with CAP to receive either clarithromycin (250 mg twice daily) or erythromycin stearate (500 mg four times daily) for 14 days. Efficacy was evaluated in 108 patients, and tolerance was analyzed on an intention-to-treat basis [98].
- Results: While clinical success rates were similar (89% for clarithromycin vs. 98% for erythromycin), the safety outcomes were markedly different. Adverse effects, primarily gastrointestinal (e.g., nausea, diarrhea, abdominal pain), caused discontinuation of treatment in 19% of patients in the erythromycin group compared to only 4% in the clarithromycin group (P < 0.01) [98]. This high rate of treatment-disrupting side effects is a major practical disadvantage for erythromycin.
Efficacy in Pediatric Mycoplasma Respiratory Infections
The utility of clarithromycin in a key indication for macrolides is demonstrated in a 2021 study on pediatric respiratory mycoplasma infection.
- Methodology: 106 children with confirmed infections were randomized to receive either clarithromycin or erythromycin for 14 days. The primary outcome was the multiplex polymerase chain reaction (MP-PCR) negative rate after treatment. Secondary outcomes included clinical efficacy, antipyretic time, hospital stay, drug cost, and medication compliance [23].
- Results: The clarithromycin group showed a significantly higher MP-PCR negative rate (96.23% vs. 75.47%) and overall clinical effectiveness rate. Children receiving clarithromycin also had a shorter fever duration, shorter hospital stays, lower drug costs, and a higher overall medication compliance rate. The incidence of toxic and side effects was significantly lower in the clarithromycin group [23].
Dose-Response Relationship in Experimental Models
Research in animal models provides insights into the potential for optimizing clarithromycin therapy.
- Experimental Protocol: One study investigated the effect of increasing dosages of clarithromycin (10, 25, or 75 mg/kg/day) in a mouse model of M. pneumoniae pneumonia. Mice were inoculated intranasally with M. pneumoniae and then treated subcutaneously with clarithromycin or placebo daily for 12 days [101] [102].
- Outcome Measures and Workflow: The following diagram illustrates the experimental workflow and key outcome measures assessed in this study.
Figure 1. Experimental workflow for evaluating clarithromycin efficacy in a murine M. pneumoniae pneumonia model.
- Findings: The study demonstrated that elevated dosages of clarithromycin resulted in greater antimicrobial efficacy, with significantly reduced quantitative M. pneumoniae cultures. Furthermore, higher doses led to greater improvement in disease severity markers, including reduced lung histopathology scores, bronchoalveolar lavage (BAL) cytokine concentrations, and airway hyperresponsiveness [101]. This dose-dependent effect highlights the compound's potential for optimized therapeutic regimens.
Mechanistic and Pharmacokinetic Insights
The superior clinical performance of clarithromycin is underpinned by its more favorable pharmacokinetic profile.
Table 4: Research Reagent Solutions for Macrolide Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| SP4 Broth and Agar | Culture medium for growing and quantifying Mycoplasma pneumoniae. | Used for inoculum preparation and quantitative culture of bronchoalveolar lavage (BAL) samples in murine models [101]. |
| Bronchoalveolar Lavage (BAL) Fluid | Sampled from the respiratory tract to measure pathogen load and host immune response. | Analysis of quantitative M. pneumoniae culture and cytokine/chemokine concentrations using multiplex bead immunoassays [101]. |
| Multiplex Bead Immunoassays | Simultaneously quantify multiple cytokines, chemokines, and growth factors in biological samples. | Used with the Luminex LabMAP system to profile pulmonary inflammation in response to infection and treatment [101]. |
| Whole-body Plethysmography | Measures respiratory parameters in conscious, unrestrained animals to assess airway function. | Used to monitor airway hyperresponsiveness (Penh value) after methacholine challenge in infected and treated mice [101]. |
- Structural Advantage and Absorption: Clarithromycin is an acid-stable analogue of erythromycin with a methoxy substitution at the C-6 position. This modification prevents its conversion in the stomach to inactive forms, resulting in higher and more reliable bioavailability (55% for clarithromycin vs. ~25% for erythromycin base) [99]. Furthermore, clarithromycin absorption may be enhanced by food, whereas the absorption of some erythromycin formulations is diminished [99].
- Metabolism and Tissue Distribution: A key differentiator is clarithromycin's metabolism to an active metabolite, 14-hydroxy-clarithromycin. This metabolite contributes an additive or synergistic effect against certain pathogens, like Haemophilus influenzae, potentially overcoming the limited activity erythromycin has against this bacterium [99] [100]. Both clarithromycin and its active metabolite achieve high concentrations in respiratory tissues (tonsils, nasal mucosa, lung parenchyma) that significantly exceed the MIC90 for common respiratory pathogens [99]. The following diagram summarizes the key pharmacokinetic advantages of clarithromycin.
Figure 2. Key pharmacokinetic advantages of clarithromycin over erythromycin that underpin its clinical efficacy.
For researchers and drug development professionals investigating antibiotics for respiratory infections, the evidence clearly delineates the positions of clarithromycin and erythromycin. Clarithromycin demonstrates superior efficacy in the treatment of community-acquired pneumonia and pediatric mycoplasma infections, coupled with a significantly more favorable safety and tolerability profile. Its pharmacokinetic advantages—including acid stability, the presence of an active metabolite, excellent tissue penetration, and a longer half-life—provide a mechanistic explanation for these clinical outcomes. Furthermore, the simpler twice-daily dosing regimen of clarithromycin translates into higher patient compliance, a critical factor in treatment success. While erythromycin remains an important historical agent, the body of evidence supports the preference for clarithromycin (and other advanced macrolides) in most clinical scenarios where a macrolide is indicated, particularly within the context of optimizing mycoplasma removal efficacy and overall patient-centered outcomes.
The treatment landscape for Severe Mycoplasma pneumoniae Pneumonia (SMPP) is evolving due to the global rise of macrolide-resistant M. pneumoniae (MRMP) strains. Macrolides have traditionally been the first-line therapy for pediatric SMPP. However, the growing challenge of macrolide resistance has intensified the need for effective alternative treatments, particularly for severe cases. Doxycycline, a tetracycline-class antibiotic, has emerged as a clinically important option. This guide objectively compares the performance of doxycycline against macrolide antibiotics for SMPP, focusing on key efficacy metrics such as symptom resolution times, with supporting data from clinical studies and meta-analyses for researchers and drug development professionals.
Comparative Efficacy Data
Numerous clinical studies have directly compared the efficacy of doxycycline and macrolides in children with SMPP, especially in cases of macrolide-unresponsive or resistant infections. The quantitative data below summarize the key differences in treatment outcomes.
Table 1: Comparison of Primary Clinical Outcomes between Doxycycline and Macrolides in SMPP Treatment
| Clinical Outcome Metric | Doxycycline Group | Macrolide Group | Statistical Significance (p-value) | Source Study Details |
|---|---|---|---|---|
| Cough Relief Time (days) | 5.4 ± 1.2 | 7.2 ± 1.6 | p < 0.05 | Prospective study of 92 children with SMPP [8] |
| Pulmonary Rale Resolution Time (days) | 6.2 ± 1.3 | 8.0 ± 1.7 | p < 0.05 | Prospective study of 92 children with SMPP [8] |
| Overall Treatment Efficacy Rate | 88.6% | 75.0% | p < 0.05 | Prospective study of 92 children with SMPP [8] |
| Time to Defervescence in MRMP (days) | 2 | 5 | p < 0.001 | Retrospective analysis of 145 cases [103] |
| Time to Chest X-ray Improvement in MRMP (days) | 3 | 6 | p < 0.001 | Retrospective analysis of 145 cases [103] |
| Fever Duration after Treatment (days) | Shorter | Longer | p = 0.027 | Analysis of 106 children with MRMP [104] |
| Hospitalization Duration (days) | Shorter | Longer | p = 0.037 | Analysis of 106 children with MRMP [104] |
| Rate of Adverse Events | 18.2% | 16.7% | p > 0.05 (Not Significant) | Primarily mild rash and GI discomfort; no tooth discoloration reported [8] |
A 2025 meta-analysis corroborates these findings, demonstrating that doxycycline was associated with superior treatment efficacy (Risk Ratio: 0.68, 95% CI: 0.58–0.79) and a significantly shorter fever resolution time (mean difference: -1.5 days, 95% CI: -2.3 to -0.7) [8] [105].
Detailed Experimental Protocols
To evaluate and compare the clinical performance of these antibiotics, researchers typically employ structured clinical study designs. The following methodologies are representative of the cited investigations.
Protocol for Prospective Clinical Efficacy and Safety Trial
This protocol outlines a standard design for a head-to-head comparison of doxycycline versus macrolides in a pediatric SMPP population.
- Study Population: Pediatric patients under 8 years old hospitalized with a diagnosis of SMPP according to established guidelines (e.g., 2023 Guidelines for the Diagnosis and Treatment of Mycoplasma pneumoniae in Children). Key diagnostic criteria include persistent high fever (≥39°C) for ≥5 days, respiratory distress, hypoxemia (pulse oxygen saturation ≤93%), and significant radiographic findings [8].
- Inclusion Criteria:
- Failure to respond to at least 3 days of prior macrolide therapy (defining macrolide-unresponsive M. pneumoniae pneumonia, MUMPP).
- No history of allergy to macrolide or tetracycline antibiotics.
- No severe congenital anomalies or primary immunodeficiency [8].
- Group Allocation: Patients are divided into two treatment groups:
- Doxycycline Group: Receives oral doxycycline at 2 mg/kg every 12 hours for 10 days.
- Macrolide Group: Continues treatment with a macrolide antibiotic (e.g., azithromycin) [8].
- Concomitant Treatment: Both groups receive standardized supportive care, which may include glucocorticoids (e.g., methylprednisolone at 2 mg/kg/day) for anti-inflammatory effect, bronchoscopic intervention if needed, and mucus reduction therapy [8].
- Data Collection: Clinical data are extracted from electronic medical records, including:
- Time to resolution of key symptoms (fever, cough, pulmonary rales).
- Duration of hospitalization.
- Chest CT or X-ray improvement one week post-treatment initiation.
- Incidence and type of adverse events [8].
Protocol for Retrospective Analysis of Macrolide-Resistant MP (MRMP)
This methodology is used to assess antibiotic efficacy in the context of confirmed resistance.
- Data Source & Patient Selection: Retrospective analysis of data from children hospitalized with MRMP pneumonia over a defined period (e.g., May 2019 to August 2022). Patients are grouped based on actual treatment received [104].
- Group Definitions:
- DOX Group: Treated with oral doxycycline alone.
- ATD Group: Switched from intravenous azithromycin to oral doxycycline during treatment.
- AZI Group: Treated with intravenous azithromycin alone [104].
- Resistance Determination: Macrolide resistance is confirmed by identifying point mutations (e.g., A2063G transition) in the 23S rRNA gene of M. pneumoniae from nasopharyngeal samples using polymerase chain reaction (PCR) [103].
- Outcome Analysis: Primary outcomes are time to defervescence after treatment initiation and time to radiographic improvement. Statistical adjustments, such as Propensity Score Matching (PSM), are used to minimize confounding factors [104].
Signaling Pathways and Treatment Decision Workflow
The following diagram illustrates the pathogenic mechanisms of M. pneumoniae and the logical workflow for selecting between macrolide and doxycycline therapy, integrating host immune response and bacterial resistance.
SMPP Treatment Pathway
This diagram delineates the two primary pathways in SMPP pathogenesis: direct bacterial damage and excessive host immune response. It also maps the clinical decision algorithm for antibiotic therapy, highlighting the pivot to doxycycline upon treatment failure or known resistance.
The Scientist's Toolkit: Research Reagent Solutions
Research into M. pneumoniae antibiotic efficacy relies on specific reagents and methodological tools. The following table details essential materials and their applications in this field.
Table 2: Key Research Reagents and Materials for M. pneumoniae Antibiotic Studies
| Reagent / Material | Primary Function in Research | Application Example |
|---|---|---|
| Mycoplasma Culture Media (e.g., SP4, Hayflick's medium) | Supports the fastidious growth of M. pneumoniae for in vitro isolation and propagation. | Essential for obtaining clinical isolates from patient samples (e.g., nasopharyngeal swabs, bronchoalveolar lavage fluid) for subsequent antibiotic susceptibility testing [103]. |
| PCR Reagents for 23S rRNA Gene | Amplifies and sequences the target region of the M. pneumoniae genome. | Used for the molecular detection of M. pneumoniae and for identifying macrolide-resistance conferring mutations (e.g., A2063G, A2064G) in domain V of the 23S rRNA gene [103]. |
| Antibiotic MIC Strips/Panels | Determines the minimum inhibitory concentration (MIC) of antibiotics against a bacterial isolate. | Used in phenotypic antimicrobial susceptibility testing (AST) to quantify the resistance level of M. pneumoniae isolates to macrolides, doxycycline, and other antibiotics [106]. |
| Cell Line Models (e.g., human respiratory epithelial cells) | Provides a host-cell environment to study infection dynamics and antibiotic penetration. | Employed in advanced in vitro studies to investigate the intracellular activity of antibiotics and their efficacy in a more physiologically relevant system [107]. |
| ELISA/Kits for Cytokine Profiling | Quantifies levels of specific cytokines and inflammatory markers. | Critical for research on refractory MPP to measure the exaggerated host immune response (e.g., IL-6, IL-8, TNF-α) and to evaluate the effect of adjunctive immunomodulatory therapies like corticosteroids [108]. |
Synthesized evidence from recent clinical studies and meta-analyses robustly indicates that doxycycline is an effective and safe therapeutic alternative to macrolides for children with Severe Mycoplasma pneumoniae Pneumonia, particularly in the context of macrolide resistance. The key differentiator for doxycycline is its consistently demonstrated ability to shorten the resolution time of respiratory symptoms, specifically cough and pulmonary rales, compared to continued macrolide therapy. While both drug classes exhibit similar safety profiles with mostly mild adverse events, doxycycline's superior efficacy in overcoming macrolide resistance makes it a critical tool in the SMPP treatment arsenal. Future research should focus on optimizing the timing of doxycycline initiation and further elucidating its long-term safety profile in younger pediatric populations.
The therapeutic landscape for Mycoplasma pneumoniae pneumonia (MPP) has undergone significant shifts due to the rapid global spread of macrolide-resistant strains, particularly across East Asia. In Japan, despite a temporary decline after peaking in 2012, the prevalence of macrolide-resistant M. pneumoniae has begun increasing again, with current resistance rates reaching 54% according to a recent prospective observational study [31]. This resurgence poses substantial clinical challenges as macrolides, once the standard therapy, increasingly prove ineffective. Consequently, the Japanese Society of Mycoplasmology has recommended minocycline, a tetracycline antibiotic, as the first-choice treatment for macrolide-resistant MPP [31]. However, the emergence of lascufloxacin, a next-generation fluoroquinolone, offers a promising alternative worthy of scientific scrutiny and comparison.
Comparative Efficacy Analysis: Lascufloxacin Versus Minocycline
Clinical Performance in Macrolide-Resistant MPP
A 2025 prospective observational study conducted across 12 facilities affiliated with Kansai Medical University Hospital provides the most direct comparative evidence available. The investigation, which enrolled 93 patients with MPP between January 2024 and January 2025, revealed striking parallels in efficacy between the two therapeutic options [31].
Table 1: Comparative Efficacy of Lascufloxacin vs. Minocycline in M. pneumoniae Pneumonia
| Patient Population | Treatment Group | Defervescence within 48 hours | Antibiotic Change Required |
|---|---|---|---|
| Macrolide-sensitive MPP (n=33) | Lascufloxacin | 91% | None |
| Macrolide-sensitive MPP (n=33) | Minocycline | 90% | None |
| Macrolide-resistant MPP (n=42) | Lascufloxacin | 90% | None |
| Macrolide-resistant MPP (n=42) | Minocycline | 90% | None |
Among the 51 patients (54%) infected with macrolide-resistant M. pneumoniae, all exhibited an A-to-G transition at position 2063 in domain V of the 23S rRNA gene, conferring high-level resistance to macrolides [31]. Despite this resistance profile, both lascufloxacin and minocycline demonstrated exceptional and equivalent performance, achieving equivalent fever resolution without requiring antibiotic regimen changes in any patients.
Minocycline Performance Against Macrolide Standards
A separate 2025 systematic review and meta-analysis encompassing 13 randomized controlled trials provides additional context for minocycline's performance against the macrolide standard, azithromycin [109] [110]. The analysis demonstrated minocycline's superior efficacy on multiple clinical parameters compared to azithromycin.
Table 2: Minocycline vs. Azithromycin Performance for MPP Treatment
| Outcome Measure | Mean Difference/Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|
| Overall Treatment Efficacy | OR = 2.24 | 1.31-3.84 | P=0.003 |
| Hospitalization Duration | MD = 7.57 days | 6.96-8.19 | P<0.001 |
| Fever Duration | MD = 5.90 days | 4.82-6.97 | P<0.001 |
| Cough Resolution Time | MD = 3.15 days | 2.58-3.72 | P<0.001 |
| Adverse Reactions | OR = 0.51 | 0.35-0.74 | P<0.001 |
The meta-analysis confirmed that minocycline not only significantly enhances treatment efficacy for refractory MPP but also promotes faster recovery with a better safety profile than azithromycin [109]. This established efficacy background provides important context for evaluating lascufloxacin as a potential alternative.
Experimental Methodologies and Analytical Approaches
Study Design and Patient Selection
The comparative study between lascufloxacin and minocycline employed a prospective observational design conducted across multiple medical centers to enhance generalizability [31]. Patient enrollment followed strict diagnostic criteria for MPP, confirmed through clinical presentation, radiological evidence, and microbiological testing. Resistance profiling was performed through genetic analysis of the 23S rRNA gene, specifically identifying the A2063G mutation associated with macrolide resistance [31]. This methodological rigor ensures the reliability of the comparative efficacy data.
Microbiological Assessment Techniques
The primary efficacy endpoint measured was defervescence within 48 hours of antibiotic initiation, a clinically meaningful metric reflecting rapid infection control [31]. Additional outcome assessments included the necessity for antibiotic regimen changes, treatment failure rates, and comprehensive safety monitoring. The consistency in outcome measures across both treatment groups enables valid comparative analysis between the two therapeutic approaches.
Figure 1: Experimental Workflow for Comparative Antibiotic Efficacy Studies
Impact on Human Microbiota: A Safety Consideration
Lascufloxacin's Ecological Effects
The ecological impact of antibiotic therapy on human microbiota represents a crucial safety consideration in treatment selection. A 2025 investigation specifically examined the temporal effects of lascufloxacin administration on both gut and salivary microbiota in healthy participants and pneumonia patients using next-generation sequencing methodologies [111] [112].
The study administered LSFX (75 mg, once daily, orally) and collected fecal and saliva samples at five time points (Days 0, 3, 7, 14, and 28). Analysis revealed that in healthy participants, α-diversity indices of both gut and salivary microbiota decreased significantly, reaching their lowest values on Day 3 [111]. While the Chao1 index (richness) of gut microbiota recovered by Day 28, the Shannon index (evenness) did not fully recover within the 28-day observation period [112]. The salivary microbiota exhibited more prolonged disruption, with neither richness nor evenness recovering within 28 days [111].
At the taxonomic level, lascufloxacin administration resulted in a decreased abundance of the Lachnospiraceae family in the gut microbiota, and reduced levels of Granulicatella, Streptococcus, Prevotella, Absconditabacteriales (SR1), and Saccharimonadales in the salivary microbiota [112]. Notably, the pneumonia patient group exhibited a different disruption pattern, with α-diversity indices reaching their lowest point on Day 14 after lascufloxacin initiation [111].
Comparative Safety Profiles
While the search results do not provide direct microbiota comparison data for minocycline, the systematic review on minocycline's safety demonstrated a significantly lower adverse reaction rate compared to azithromycin (OR = 0.51; 95% CI: 0.35-0.74; P<0.001) [109]. Common adverse effects monitored included gastrointestinal symptoms (vomiting, abdominal pain, diarrhea), liver dysfunction, and dermatological manifestations such as exanthema and photosensitivity [110].
Figure 2: Lascufloxacin Impact on Human Microbiota
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagents and Methodologies for Antibiotic Efficacy Studies
| Reagent/Methodology | Specific Application | Function in Research |
|---|---|---|
| Next-Generation Sequencing | 16S rRNA analysis [112] | Enables comprehensive assessment of microbial diversity and taxonomic composition in response to antibiotic exposure |
| 23S rRNA Gene Sequencing | A2063G mutation detection [31] | Identifies specific genetic marker conferring macrolide resistance in M. pneumoniae |
| Culture-Based Susceptibility Testing | Minimum Inhibitory Concentration (MIC) determination [31] | Quantifies antibiotic potency against bacterial pathogens and establishes resistance patterns |
| Prospective Observational Design | Multi-center clinical trials [31] | Provides real-world evidence of antibiotic performance across diverse patient populations |
| Meta-Analytical Approaches | Systematic review of RCTs [109] | Synthesizes evidence across multiple studies to establish overall treatment effects |
| Microbiome Diversity Indices | Chao1 (richness), Shannon (evenness) [112] | Quantifies ecological impact of antibiotics on human microbiota |
The compelling efficacy equivalence between lascufloxacin and minocycline for macrolide-resistant MPP, coupled with their distinct ecological and safety profiles, presents clinicians with valuable alternatives for managing this challenging infection. The experimental evidence confirms that both antibiotics achieve nearly identical fever resolution rates (90%) in macrolide-resistant cases without requiring treatment regimen changes [31].
For researchers and drug development professionals, these findings highlight the importance of continuing to investigate non-macrolide options for MPP, particularly as resistance patterns evolve. The methodological approaches outlined – including prospective multi-center designs, molecular resistance profiling, and comprehensive microbiota assessment – provide robust frameworks for future comparative antibiotic studies.
As macrolide resistance continues to spread globally, having multiple effective therapeutic alternatives becomes increasingly crucial for clinical management and resistance containment strategies. Lascufloxacin emerges from these studies as a viable clinical alternative to minocycline, particularly valuable when tetracyclines are contraindicated or when specific pharmacological properties are preferred. Future research directions should include direct head-to-head randomized controlled trials and longer-term follow-up to further elucidate the comparative advantages of each agent in specific patient populations.
The treatment of pediatric infections, particularly community-acquired pneumonia (CAP) caused by Mycoplasma pneumoniae, requires careful antibiotic selection balanced against age-specific safety profiles. Macrolides have traditionally been the first-line therapy for pediatric M. pneumoniae infections, but the global rise of macrolide-resistant M. pneumoniae (MRMP) strains has necessitated increased use of alternative antibiotic classes, namely tetracyclines and fluoroquinolones, in children [75]. This shift presents clinicians with complex risk-benefit decisions, as tetracyclines and fluoroquinolones carry historical safety concerns in pediatric populations, including dental effects and potential musculoskeletal complications [113]. This analysis systematically compares the adverse event profiles of these three antibiotic classes within the context of treating pediatric M. pneumoniae infections, synthesizing current evidence to inform clinical practice and drug development.
Comparative Safety Profiles of Antibiotic Classes
The safety profiles of macrolides, tetracyclines, and fluoroquinolones differ significantly, necessitating careful consideration for pediatric use. The table below summarizes the key adverse events and associated risks for each antibiotic class.
Table 1: Comparative Adverse Event Profiles of Antibiotic Classes in Pediatric Populations
| Antibiotic Class | Most Common Adverse Events | Serious/Rare Adverse Events | Age-Specific Concerns | Risk Level & Evidence |
|---|---|---|---|---|
| Macrolides | Gastrointestinal (nausea, vomiting, diarrhea, abdominal pain) [23] | Hepatic toxicity, QT prolongation | Generally well-tolerated across all pediatric age groups | Low risk; Extensive pediatric use supports safety, though GI effects are common [23] |
| Tetracyclines | Gastrointestinal upset, photosensitivity [113] | Tooth discoloration, enamel hypoplasia, transient bone growth inhibition | Contraindicated in children <8 years due to teeth staining risk; doxycycline carries lower risk than older tetracyclines [75] [113] | Medium risk (with mitigation); Modern evidence suggests short-course doxycycline under age 8 carries minimal dental risk [75] |
| Fluoroquinolones | Gastrointestinal, CNS effects (headache, dizziness) [114] | Musculoskeletal adverse events (arthralgia, tendonitis), peripheral neuropathy, cartilage toxicity (theoretical) | Historically limited due to juvenile animal cartilage damage; human data shows lower risk [113] [114] | Medium risk; Musculoskeletal events are typically transient and reversible; risk is often outweighed by benefit in resistant infections [75] [114] |
Detailed Safety Analysis and Clinical Considerations
Macrolide Safety Profile
Macrolides, including azithromycin and clarithromycin, are generally well-tolerated in children. Gastrointestinal disturbances are the most frequently reported adverse effects. A 2021 study comparing clarithromycin to erythromycin in 106 children with respiratory mycoplasma infection found a significantly lower incidence of toxic side effects, including nausea, diarrhea, and abdominal pain, in the clarithromycin group [23]. This suggests that within the macrolide class, agent-specific tolerability differences exist. Macrolides remain the first-line treatment for suspected M. pneumoniae in children due to their established safety profile, but their efficacy is increasingly compromised by resistance [75].
Tetracycline Safety Profile and Re-evaluation of Historical Concerns
The primary safety concern for tetracyclines in pediatrics is permanent tooth discoloration and enamel hypoplasia resulting from calcium-tetracycline complex deposition in developing teeth and bones [113]. This led to the long-standing contraindication of tetracycline use in children under eight years of age.
However, recent evidence has prompted a re-evaluation of this risk, particularly for doxycycline. Contemporary guidelines from the Canadian Pediatric Society and the American Academy of Pediatrics now support the use of doxycycline for courses of less than 21 days in children under 8 years when indicated, such as for MRMP or Rocky Mountain spotted fever [75]. This shift is supported by pharmacological data showing doxycycline has a lower affinity for calcium compared to older tetracyclines [75]. A retrospective study of 58 children receiving doxycycline for Rocky Mountain spotted fever found no cases of tooth staining or enamel hypoplasia [75].
For children over eight years of age, tetracyclines are considered a highly effective and safe alternative for MRMP. A meta-analysis found treatment with tetracyclines was associated with significantly shorter fever duration and higher therapeutic efficacy compared to macrolides for MRMP [115].
Fluoroquinolone Safety Profile and Risk Mitigation
Fluoroquinolone use in children has been historically restricted due to safety concerns originating from animal studies. Juvenile animals administered fluoroquinolones developed inflammation and destruction of weight-bearing joints, raising concerns about potential cartilage toxicity in children [113] [114].
Subsequent human studies have revealed a more nuanced risk profile. Musculoskeletal adverse events, most commonly arthralgia, are the most frequently reported class-related event. A systematic review of over 16,000 pediatric patients found the risk of an MAE was approximately 1 in 62.5 patients [114]. However, the vast majority of these events were transient and resolved completely with drug discontinuation or medical management, with no documented cases of permanent joint damage in clinical trials [75] [114]. A large meta-analysis of 10 studies found no statistically significant difference in bone and muscle damage between children who received fluoroquinolones and those who did not [75].
Other concerns, such as peripheral neuropathy and central nervous system effects, appear to be rare in pediatric populations, with rates similar to those of comparator antibiotics [114]. Given the risk-benefit profile, current guidelines recommend reserving fluoroquinolones for cases where tetracyclines are not indicated or for infections caused by multidrug-resistant pathogens like Pseudomonas aeruginosa [75] [114].
Efficacy and Safety in Macrolide-Resistant Mycoplasma Pneumoniae
The rising incidence of MRMP has made understanding the safety of second-line agents increasingly important. The following table synthesizes efficacy and key safety outcomes from meta-analyses comparing these antibiotic classes for MRMP.
Table 2: Efficacy and Safety Outcomes for Macrolide-Resistant M. pneumoniae (MRMP) in Children
| Outcome Measure | Tetracyclines vs. Macrolides | Fluoroquinolones vs. Macrolides | Tetracyclines vs. Fluoroquinolones |
|---|---|---|---|
| Therapeutic Efficacy (OR) | OR: 8.80 (95% CI: 3.12-24.82) [115] [116] | Not statistically significantly different at 24 hours (OR: 1.11) [115] | Equally effective; no significant difference in time to defervescence in network meta-analysis [117] |
| Fever Duration (WMD) | WMD: -1.45 days (95% CI: -2.55 to -0.36) [115] [116] | Shorter than macrolides; achieves defervescence within 48h (OR: 2.78) [115] | Not significantly different (Mean difference: -0.40 days) [117] |
| Hospital Stay (WMD) | WMD: -3.33 days (95% CI: -4.32 to -2.35) [115] [116] | Data limited | Data limited |
| Key Safety Findings | Doxycycline for short courses (<21 days) shows minimal dental risk in children <8 yrs [75] | MAEs are typically transient and reversible; serious events are rare [75] [114] | Levofloxacin may be associated with a higher rate of adverse reactions in children compared to other options [117] |
OR: Odds Ratio; WMD: Weighted Mean Difference; CI: Confidence Interval
Experimental Protocols for Pediatric Antibiotic Safety and Efficacy Research
Systematic Review and Meta-Analysis Protocol
Research evaluating the comparative safety and efficacy of antibiotics in children often relies on systematic reviews and meta-analyses of clinical studies, as randomized controlled trials (RCTs) directly comparing these agents in pediatric populations can be limited.
Figure 1: Workflow for Systematic Review and Meta-Analysis in Pediatric Antibiotic Research
Key Methodological Steps:
- Eligibility Criteria: Studies are typically included if they involve pediatric patients (≤18 years) with MRMP infection, compare interventions (tetracyclines, fluoroquinolones) to an active control (macrolides) or each other, and report predefined efficacy and safety outcomes [115] [116].
- Outcome Measures: Primary efficacy outcomes often include time to defervescence (TTD), duration of hospitalization, and clinical success rate. Safety outcomes focus on the incidence of class-specific adverse events, such as musculoskeletal adverse events for fluoroquinolones and dental effects for tetracyclines [115] [117].
- Statistical Analysis: For direct comparisons, pooled odds ratios for dichotomous outcomes and weighted mean differences for continuous outcomes are calculated using random-effects models. Network meta-analyses may be employed to compare multiple agents simultaneously and rank their efficacy and safety [116] [117].
Laboratory Protocols for Mycoplasma pneumoniae Antibiotic Testing
Figure 2: In Vitro Assessment of Antibiotic Efficacy against M. pneumoniae
Detailed Methodology:
- Culture and Inoculum Preparation: M. pneumoniae strains, including clinical isolates and reference strains, are cultured in specific media. The bacterial inoculum is standardized to a concentration of 10^4–10^5 color-changing units per milliliter [116].
- Antibiotic Susceptibility Testing: Antibiotics are prepared in serial two-fold dilutions. The minimum inhibitory concentration is determined as the lowest antibiotic concentration that completely inhibits bacterial growth. For macrolide resistance, genotyping is performed to detect point mutations in the 23S rRNA gene, which are strongly associated with resistance [75] [116].
- Outcome Measures: The primary outcome is the MIC for each antibiotic-strain combination. Efficacy is correlated with clinical outcomes, with higher MICs indicating lower efficacy. This laboratory data provides the mechanistic basis for clinical treatment failure and guides the selection of alternative agents [75].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Pediatric Antibiotic Research
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Pediatric Clinical Isolates | Provides relevant bacterial strains for in vitro testing, reflecting current resistance patterns. | Determining the MIC of doxycycline against macrolide-resistant M. pneumoniae clinical isolates [75]. |
| Cell Culture Media (e.g., SP4) | Supports the growth and propagation of fastidious bacteria like M. pneumoniae. | Culturing M. pneumoniae from patient samples (e.g., throat swabs) for subsequent antibiotic testing [116]. |
| PCR Kits & Primers | Enables detection, quantification, and genotyping of pathogens and resistance markers. | Confirming M. pneumoniae infection via MP-PCR and identifying 23S rRNA mutations conferring macrolide resistance [75] [23]. |
| Antibiotic Reference Standards | Highly purified compounds used as benchmarks for preparing accurate drug dilutions in susceptibility assays. | Creating serial dilutions for MIC testing to compare the potency of different antibiotics [116]. |
| Animal Models (e.g., juvenile rodent) | Used to study antibiotic pharmacokinetics and age-specific toxicities (e.g., cartilage or dental effects). | Investigating the potential for arthropathy with fluoroquinolones or dental staining with tetracyclines in a developing organism [113] [114]. |
The management of pediatric M. pneumoniae infections is evolving due to increasing macrolide resistance. While macrolides remain the safest first-line option for susceptible infections, evidence supports the careful use of tetracyclines and fluoroquinolones in resistant cases. The historical safety concerns for these second-line agents, particularly regarding dental effects with tetracyclines and musculoskeletal events with fluoroquinolones, appear less prohibitive than previously thought when used judiciously. Short-course doxycycline is a viable option for children under eight, and fluoroquinolone-associated arthropathy is typically transient. The decision to use these agents must be individualized, weighing the severity of infection, local resistance patterns, and the specific risk-benefit profile for each patient.
Conclusion
The escalating global prevalence of macrolide-resistant Mycoplasma pneumoniae necessitates a paradigm shift in therapeutic strategy. The evidence conclusively demonstrates that while macrolides remain a cornerstone, their utility is diminishing when used alone, particularly against biofilms. The future of effective mycoplasma eradication lies in a multi-pronged approach: the timely deployment of validated second-line antibiotics like doxycycline and newer fluoroquinolones for severe cases, the strategic use of synergistic antibiotic combinations to overcome biofilm-mediated resistance, and the exploration of adjunctive and non-antibiotic modalities. For researchers and drug developers, critical future directions include the development of rapid point-of-care resistance detection tools, the design of robust clinical trials for optimized combination regimens, and the continued investigation into novel antimicrobial mechanisms that can circumvent existing resistance pathways, thereby ensuring effective treatment options for this persistent pathogen.
References
- 1. Advances in adhesion-related pathogenesis ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1613760/full]
- 2. Growing Threat of Macrolide-Resistant Mycoplasma ... [https://jkms.org/DOIx.php?id=10.3346/jkms.2025.40.e317]
- 3. Resurgence of Mycoplasma pneumoniae infections in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404625/]
- 4. Description of a Current Outbreak of Mycoplasma ... [https://www.mdpi.com/2076-0817/14/1/60]
- 5. Treatment modalities for fever duration in children with ... [https://www.nature.com/articles/s41598-025-99537-0]
- 6. Unraveling the role of distinct cytoskeletal motility structures in ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-04320-w]
- 7. Eradication of Mycoplasma pneumoniae biofilm towers by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12393767/]
- 8. Efficacy and safety of doxycycline for severe Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283874/]
- 9. Global Trends in the Proportion of Macrolide-Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9274321/]
- 10. Prevalence of Macrolide-Resistant Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602751/]
- 11. Antimicrobial susceptibility and molecular characteristics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568347/]
- 12. Macrolide-resistant Mycoplasma pneumoniae prevalence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723809/]
- 13. Macrolide-resistant Mycoplasma pneumoniae infection ... [https://www.sciencedirect.com/science/article/abs/pii/S2212534525000516]
- 14. Mechanism of resistance acquisition and treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5500384/]
- 15. Macrolide resistance in Mycoplasma pneumoniae in adult ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1496521/full]
- 16. Recent Macrolide Resistance Pattern of Mycoplasma ... [https://pubmed.ncbi.nlm.nih.gov/40330176/]
- 17. Mutation in 23S rRNA Responsible for Resistance to 16 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC90283/]
- 18. Mutations in 23S rRNA and Ribosomal Protein L4 Account for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC90022/]
- 19. Molecular Mechanisms by Which rRNA Mutations Confer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1068640/]
- 20. Association between point mutations of macrolide-resistant ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1682167/full]
- 21. Macrolide-Resistant Mycoplasma pneumoniae Infections ... [https://wwwnc.cdc.gov/eid/article/31/3/24-1570_article]
- 22. The Prevalence of 23S rRNA Mutations in ML-Resistant M. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7603257/]
- 23. Efficacy of different antibiotics in treatment of children with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8362522/]
- 24. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 25. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 26. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 27. Eradication of Mycoplasma pneumoniae biofilm towers by ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329571]
- 28. Understanding the Mechanism of Bacterial Biofilms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5427689/]
- 29. Biofilm, resistance, and quorum sensing: The triple threat in ... [https://www.sciencedirect.com/science/article/pii/S2950194625003462]
- 30. Inhibition of Virulence Factors and Biofilm Formation by ... [https://pubmed.ncbi.nlm.nih.gov/34884499/]
- 31. Therapeutic efficacy of lascufloxacin in patients with ... [https://pubmed.ncbi.nlm.nih.gov/40530812/]
- 32. Anti-virulence therapeutic strategies against bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9719373/]
- 33. Anti-virulence strategies to combat bacteria-mediated ... [https://www.nature.com/articles/nrd3013]
- 34. Growing Threat of Macrolide-Resistant Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602143/]
- 35. Macrolides - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK551495/]
- 36. Gastrointestinal safety of oral erythromycin, clarithromycin, ... [https://pubmed.ncbi.nlm.nih.gov/40702206/]
- 37. THE NEWER MACROLIDES: Azithromycin and ... [https://www.sciencedirect.com/science/article/pii/S0891552020306942]
- 38. Cardiovascular Toxicity Profile of Macrolides Investigated ... [https://link.springer.com/article/10.1007/s12012-025-09970-w]
- 39. Antibiotic susceptibility testing using minimum inhibitory concentration... [https://www.nature.com/articles/s44259-024-00051-6?error=cookies_not_supported&code=185a98cf-fbbf-46b3-992d-f5a296d950f0]
- 40. Bactericidal versus bacteriostatic antibacterials: clinical significance... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11695898/]
- 41. Evaluation of non-invasive diagnostic tests for Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518258/]
- 42. Evaluating the Antibiotic Resistance Patterns in ... [https://www.mdpi.com/2674-0710/4/3/12]
- 43. Modification of antimicrobial susceptibility testing methods [https://pubmed.ncbi.nlm.nih.gov/40971802/]
- 44. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria]
- 45. M100 | Performance Standards for Antimicrobial ... [https://clsi.org/shop/standards/m100/]
- 46. Mycoplasma detection and accurate rapid release testing [https://www.news-medical.net/whitepaper/20250922/Mycoplasma-detection-and-the-need-for-accurate-rapid-release-testing.aspx]
- 47. New and simplified method for drug combination studies by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8563647/]
- 48. Drug combinations targeting antibiotic resistance [https://www.nature.com/articles/s44259-024-00047-2]
- 49. Antimicrobial Synergy Testing/Checkerboard Assay [https://antiviral.creative-diagnostics.com/antimicrobial-synergy-testing-checkerboard-assay.html]
- 50. Antimicrobial Synergy Study – Checkerboard Testing [https://emerypharma.com/solutions/cell-microbiology-services/antimicrobial-synergy-study-checkerboard-testing/]
- 51. Development of a Polymicrobial Checkerboard Assay as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376321/]
- 52. Efficacy of Combination Therapies for the Treatment of Multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9027966/]
- 53. Leveraging Laboratory and Clinical Studies to Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671129/]
- 54. Synergistic effect of antibiotic combinations on ... [https://www.sciencedirect.com/science/article/pii/S2590207522000028]
- 55. Synergistic action of antimicrobial peptides and antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11322369/]
- 56. Bacterial Biofilm Eradication Agents: A Current Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6893625/]
- 57. Classical and Modern Models for Biofilm Studies [https://www.mdpi.com/2079-6382/13/12/1228]
- 58. Establishing a quantitative link between crystal violet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477910/]
- 59. Scanning electron microscopy of mycoplasmas adhering to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC551345/]
- 60. Rapid imaging of mycoplasma in solution using ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X11023205]
- 61. LIB 4395 Analyses of Crystal Violet & Brilliant Green [https://www.fda.gov/food/laboratory-methods-food/laboratory-information-bulletin-lib-4395-analyses-crystal-violet-brilliant-green]
- 62. Pediatric investigation study identifies the optimal dose of ... [https://www.eurekalert.org/news-releases/1093221]
- 63. Comparison and evaluation of metagenomic next- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1694179/full]
- 64. The application value and challenges of metagenomic next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528123/]
- 65. Diagnostic value of metagenomic next-generation ... [https://www.nature.com/articles/s41598-025-23695-4]
- 66. Comparison of pathogen detection performance between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375685/]
- 67. Comparison of different detection methods for Mycoplasma ... [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-021-02523-4]
- 68. Comparative diagnostic performance of metagenomic and ... [https://www.nature.com/articles/s41598-025-11834-w]
- 69. An innovative fungal-specific targeted next-generation ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06784-w]
- 70. Comparative analysis of metagenomic next-generation ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03887-8]
- 71. In vitro antimicrobial susceptibility of Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308128/]
- 72. Eradication of Mycoplasma pneumoniae biofilm towers by ... [https://pubmed.ncbi.nlm.nih.gov/40875659/]
- 73. Mycoplasma Biofilms: Characteristics and Control Strategies [https://www.mdpi.com/2076-2607/13/8/1850]
- 74. Evidence‐based guideline for the diagnosis and treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11998179/]
- 75. Resistant Mycoplasma pneumoniae in children - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312865/]
- 76. Emergence of Novel Fluoroquinolone Resistance ... [https://wwwnc.cdc.gov/eid/article/31/8/24-1137_article]
- 77. Harnessing Non-Antibiotic Strategies to Counter Multidrug ... [https://www.mdpi.com/2079-6382/14/1/57]
- 78. Evaluation of the effectiveness of hydrogen-peroxide ... [https://www.sciencedirect.com/science/article/abs/pii/S0195670114001546]
- 79. Evaluation of the effectiveness of hydrogen-peroxide-based ... [https://researchportal.ukhsa.gov.uk/en/publications/evaluation-of-the-effectiveness-of-hydrogen-peroxide-based-disinf/]
- 80. Evaluation of Antimicrobial-Antibiofilm Activity of a Hydrogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2948419/]
- 81. Efficacy of Different Irrigation Solutions on Bacterial Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029087/]
- 82. Evaluation of mycoplasma removal reagents using qPCR ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269718307036]
- 83. A new method for detecting mycoplasma in cell cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270630/]
- 84. Early Corticosteroid Therapy for Mycoplasma pneumoniae ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6572103/]
- 85. Outcomes of Adjunctive Corticosteroid Treatment in ... [https://pubmed.ncbi.nlm.nih.gov/39230949]
- 86. Efficacy of bronchoalveolar lavage in treating mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11982992/]
- 87. The role of flexible bronchoscopy in children with ... [https://pubmed.ncbi.nlm.nih.gov/35459766/]
- 88. The clinical characteristics of corticosteroid-resistant ... [https://www.nature.com/articles/srep39929]
- 89. New Guidelines Released for Pediatric Mycoplasma ... [https://bioengineer.org/new-guidelines-released-for-pediatric-mycoplasma-pneumoniae-infection-insights-from-the-latest-pediatric-investigation-study/]
- 90. The Combined Photosensitizers in Antimicrobial ... [https://www.mdpi.com/1422-0067/26/20/10211]
- 91. Comparison of Antibacterial Activity and Wound Healing in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.673408/full]
- 92. Viscous methylene blue formulation for antimicrobial ... [https://www.nature.com/articles/s41598-025-98568-x]
- 93. Comparative Evaluation of Antimicrobial Photodynamic ... [https://pubmed.ncbi.nlm.nih.gov/40655586/]
- 94. Clinical characteristics and outcomes of macrolide-resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597172/]
- 95. Treatment Outcomes of Mycobacterium avium Complex ... [https://pubmed.ncbi.nlm.nih.gov/40453874/]
- 96. Fulminant Macrolide-Resistant Mycoplasma pneumoniae ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12414137/]
- 97. Efficacy of erythromycin compared to clarithromycin and ... [https://pubmed.ncbi.nlm.nih.gov/35523718/]
- 98. A comparative safety and efficacy study of clarithromycin ... [https://pubmed.ncbi.nlm.nih.gov/1827098/]
- 99. Pharmacokinetic properties of clarithromycin [https://pmc.ncbi.nlm.nih.gov/articles/PMC3250788/]
- 100. Efficacy of erythromycin compared to clarithromycin and ... [https://www.sciencedirect.com/science/article/abs/pii/S1341321X22001349]
- 101. Efficacy of increasing dosages of clarithromycin for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3172041/]
- 102. Efficacy of increasing dosages of clarithromycin for ... [https://scholars.uthscsa.edu/en/publications/efficacy-of-increasing-dosages-of-clarithromycin-for-treatment-of/]
- 103. Clinical Efficacy of Doxycycline for Treatment of Macrolide- ... [https://www.mdpi.com/2079-6382/10/2/192]
- 104. Efficacy of doxycycline therapy for macrolide-resistant ... [https://pubmed.ncbi.nlm.nih.gov/38439015/]
- 105. Efficacy and safety of doxycycline for severe Mycoplasma ... [https://pubmed.ncbi.nlm.nih.gov/40694196/]
- 106. Next-generation rapid phenotypic antimicrobial ... [https://www.nature.com/articles/s41467-024-53930-x]
- 107. The Changing Landscape of Antibiotic Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291801/]
- 108. Rational stepwise approach for Mycoplasma pneumoniae ... [https://www.sciencedirect.com/science/article/pii/S1684118220302474]
- 109. The efficacy and adverse reactions of minocycline against ... [https://pubmed.ncbi.nlm.nih.gov/41158388/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0YBfl48FHBbRC_4eiJ1Dqis0V0NLDy4IFVDmReIo2q1&fc=None&ff=20251030204713&v=2.18.0.post22+67771e2]
- 110. The efficacy and adverse reactions of minocycline against ... [https://jtd.amegroups.org/article/view/105947/html]
- 111. Temporal effects of lascufloxacin on human gut and ... [https://www.sciencedirect.com/science/article/abs/pii/S1341321X2400206X]
- 112. Temporal effects of lascufloxacin on human gut and ... [https://pubmed.ncbi.nlm.nih.gov/39089446/]
- 113. Pediatric Antibiotic Use: A Focused Review of ... [https://www.uspharmacist.com/article/pediatric-antibiotic-use-a-focused-review-of-fluoroquinolones-and-tetracyclines]
- 114. Fluoroquinolone Use In Children [https://pedemmorsels.com/fluoroquinolone-use-in-children/]
- 115. Efficacy of tetracyclines and fluoroquinolones for the ... [https://pubmed.ncbi.nlm.nih.gov/34563128/]
- 116. Efficacy of tetracyclines and fluoroquinolones for the treatment ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06508-7]
- 117. Effectiveness and safety of tetracyclines and quinolones in ... [https://www.sciencedirect.com/science/article/pii/S2589537024001688]