Autologous CAR T-Cell Production: A Comprehensive Guide from Foundational Principles to Manufacturing Optimization
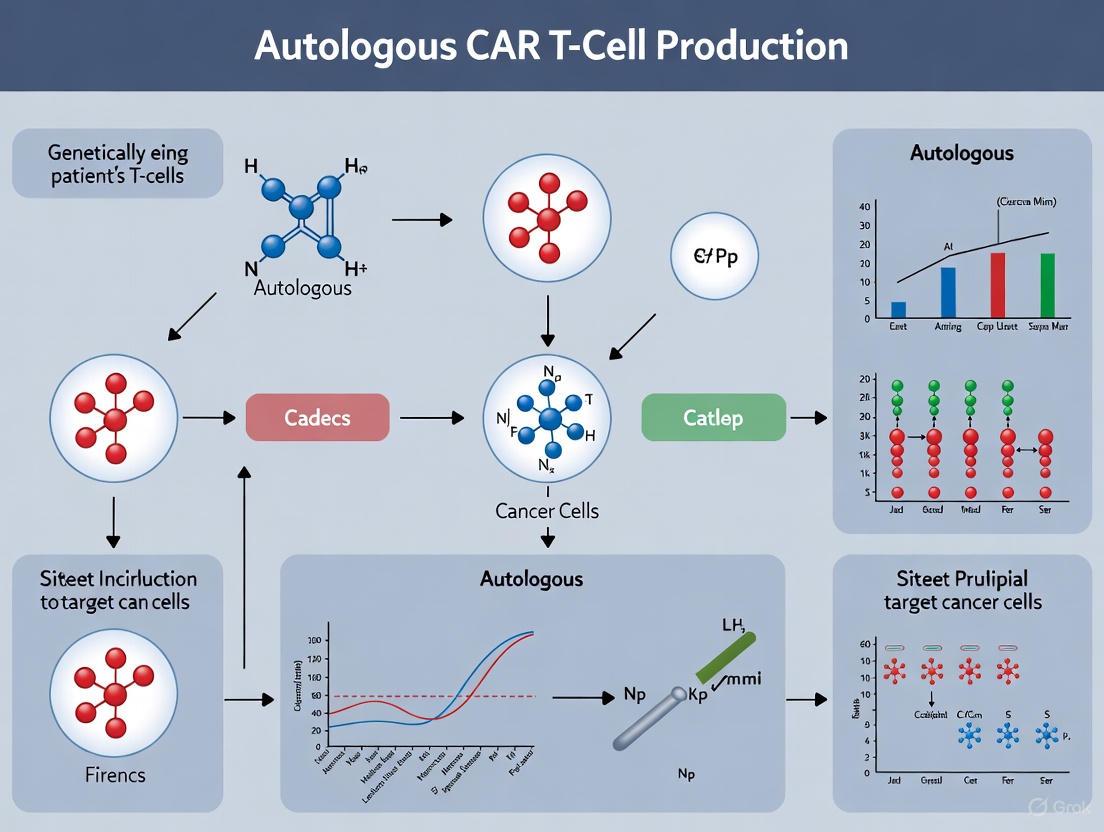
This article provides a detailed examination of autologous chimeric antigen receptor (CAR) T-cell production, a groundbreaking yet complex personalized cancer immunotherapy.
Autologous CAR T-Cell Production: A Comprehensive Guide from Foundational Principles to Manufacturing Optimization
Abstract
This article provides a detailed examination of autologous chimeric antigen receptor (CAR) T-cell production, a groundbreaking yet complex personalized cancer immunotherapy. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology of CAR constructs, from first to fifth generations. The scope encompasses the complete methodological workflow, including cell sourcing, viral and non-viral engineering, and expansion. It critically addresses prevalent manufacturing challenges such as T-cell exhaustion, product variability, and high costs, while presenting optimization and troubleshooting strategies. Finally, the article offers a comparative analysis with emerging allogeneic 'off-the-shelf' approaches, discussing validation techniques and the push for standardized quality controls to ensure product consistency, safety, and efficacy.
The Science Behind the Therapy: Deconstructing CAR T-Cell Biology and Structure
Chimeric Antigen Receptor (CAR) T-cell therapy represents a paradigm shift in cancer treatment, particularly for hematologic malignancies. The core of this technology is the CAR, a synthetic receptor that redirects T cells to recognize and eliminate tumor cells. The evolution of CAR designs, from first to fifth-generation constructs, has been marked by incremental enhancements in signaling domains to improve T-cell activation, persistence, and ability to overcome the immunosuppressive tumor microenvironment. This progression is central to autologous CAR T-cell production research, where the goal is to manufacture a consistent, potent, and durable product from a patient's own T cells. This article details the defining characteristics of each CAR generation and provides standardized protocols for their in-vitro evaluation, serving as a critical resource for researchers and drug development professionals in the field.
The Generational Evolution of CAR Constructs
The table below summarizes the key structural and functional characteristics of each generation of CAR designs.
Table 1: Evolution of CAR Constructs from First to Fifth Generation
| Generation | Signaling Domains | Key Features & Functions | Primary Advantages | Key Limitations |
|---|---|---|---|---|
| First | CD3ζ | Single-chain variable fragment (scFv) linked to CD3ζ chain. | • Proof-of-concept for redirected T-cell cytotoxicity.• Basic antigen-specific activation. | • No costimulatory signaling.• Poor T-cell persistence • Limited expansion in vivo. |
| Second | CD3ζ + 1 Costimulatory (e.g., CD28 or 4-1BB) | Incorporation of one costimulatory domain. | • Enhanced T-cell expansion and cytotoxicity.• Improved persistence (especially with 4-1BB).• Foundation for all approved commercial CAR-T products [1]. | • Susceptibility to immunosuppressive environments.• Potential for T-cell exhaustion. |
| Third | CD3ζ + 2+ Costimulatory (e.g., CD28 + 4-1BB) | Combination of multiple costimulatory signals. | • Synergistic signaling for enhanced effector function.• Potentially greater cytokine production and longevity. | • Increased complexity without a clear consistent clinical advantage over 2nd gen.• Risk of excessive activation. |
| Fourth | CD3ζ + Costimulatory + Cytokine/JAK/STAT domain | "Armored" CARs; constitutive or induced cytokine signaling (e.g., IL-12, IL-15). | • Resistance to immunosuppressive microenvironments (e.g., TGFβ).• Enhanced in-situ proliferation and survival.• Recruitment of innate immune cells. | • Increased risk of on-target, off-tumor toxicity due to cytokine release.• More complex manufacturing and safety profiling. |
| Fifth | CD3ζ + Costimulatory + TGFβ | "Switch" CARs; inducible signaling pathways (e.g., NFAT, JAK/STAT). | • Ability to target solid tumors via multiple antigens.• Fine-tuned control over T-cell activity.• Reduced potential for tonic signaling and exhaustion. | • Highly complex genetic engineering.• Challenges in clinical translation and validation.• Potential for unintended immune reactions. |
All approved CAR T-cell products are second-generation CARs that incorporate either a CD28 or CD137 (4-1BB) costimulatory domain, which are essential for eliciting a clinically relevant immune response [1]. The choice of costimulatory domain can impact the product's performance profile; for instance, CD28 domains are associated with rapid, potent effector function, while 4-1BB domains favor enhanced persistence and memory formation.
Essential Research Reagent Solutions
The following table catalogs critical reagents required for the manufacturing and functional assessment of CAR T cells across different generations.
Table 2: Key Research Reagents for CAR T-Cell Development and Testing
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Viral Vectors | Stable delivery of CAR transgene into T cells. | • Lentiviral or gamma-retroviral vectors are most common. Require extensive safety testing, adding to cost and time [1]. |
| Non-Viral Transfection | Alternative gene delivery method. | • Transposon (e.g., Sleeping Beauty) systems or CRISPR-Cas9 for gene editing. Emerging to overcome limitations of viral vectors [1]. |
| Magnetic Beads | T-cell activation and expansion. | • Dynabeads CD3/CD28 Cell Therapy Systems are widely used for initial T-cell stimulation [2]. Must be GMP-grade. |
| Cell Culture Media | Ex-vivo T-cell expansion. | • Serum-free media formulations are preferred for defined composition and reduced risk of contamination. Often supplemented with cytokines (e.g., IL-2). |
| Cytokines | Promoting T-cell growth and survival. | • IL-2 is commonly used. Research explores others like IL-7, IL-15, and IL-21 to influence T-cell phenotype (e.g., memory vs. effector) [1]. |
| Enrichment Kits | Isolation of specific T-cell subsets. | • Kits for positive/negative selection of CD4+, CD8+, or central memory T cells (e.g., CD62L+). Used to create defined composition products [1]. |
| Flow Cytometry Antibodies | Phenotyping and detecting CAR T cells. | • Anti-CAR antibodies (e.g., FMC63-based for CD19 CARs) or antibodies against safety tags (e.g., truncated EGFR) [3]. Paired with T-cell subset markers (CD3, CD4, CD8, CD45RO, CD62L). |
| qPCR/ddPCR Assays | Quantitative detection of CAR transgene. | • Primers and probes targeting the CAR transgene for kinetic monitoring of expansion and persistence in patient samples [3]. |
Experimental Protocol: In-Vitro Functional Assessment of CAR T Cells
This protocol outlines a standardized methodology for evaluating the cytotoxic function and cytokine release of generated CAR T cells, critical steps in characterizing any CAR construct.
Materials
- CAR T Cells: Generated and expanded per manufacturing protocol.
- Target Cells: Antigen-positive tumor cell line (e.g., Nalm-6 for CD19) and an antigen-negative isogenic control line.
- Culture Medium: Appropriate complete medium (e.g., RPMI-1640 with 10% FBS).
- Equipment: CO₂ incubator, sterile tissue culture hood, centrifuge, multichannel pipettes, flow cytometer, ELISA plate reader.
- Reagents:
- For Cytotoxicity Assay: Lactate Dehydrogenase (LDH) release detection kit OR a flow cytometry-based assay (e.g., CFSE/7-AAD staining).
- For Cytokine Assay: Human IFN-γ and IL-2 ELISA kits or LEGENDplex bead-based array.
Methodologies
A. Cytotoxicity Assay (LDH Release)
This assay measures antigen-specific killing of target cells by CAR T cells.
Day 0: Plate Setup
- Harvest CAR T cells and target cells. Count and resuspend in culture medium.
- In a 96-well U-bottom plate, co-culture CAR T cells with target cells at various Effector:Target (E:T) ratios (e.g., 40:1, 20:1, 10:1, 5:1). Recommended total volume is 200 µL/well.
- Include essential control wells:
- Spontaneous LDH Release: Target cells + medium only.
- Maximum LDH Release: Target cells + lysis solution (from kit).
- Effector Spontaneous Release: CAR T cells + medium only.
- Background Control: Culture medium only.
- Prepare triplicates for each condition.
Day 1: Assay Development
- Centrifuge the plate at 250xg for 4 minutes.
- Carefully transfer 100 µL of supernatant from each well to a new flat-bottom 96-well plate, avoiding disturbance of the cell pellet.
- Add 100 µL of the LDH reaction mixture to each well containing the supernatant. Incubate for 30 minutes in the dark at room temperature.
- Measure the absorbance at 490 nm and 620 nm (reference wavelength) using a plate reader.
Calculation:
- Calculate the percentage of specific cytotoxicity using the formula:
% Cytotoxicity = (Experimental - Effector Spontaneous - Spontaneous) / (Maximum - Spontaneous) * 100
- Calculate the percentage of specific cytotoxicity using the formula:
B. Cytokine Release Assay (ELISA)
This assay quantifies T-cell activation upon antigen engagement by measuring secreted cytokines.
Day 0: Stimulation
- Set up the same co-cultures as for the cytotoxicity assay in a 96-well plate. A 6- to 18-hour incubation is typically sufficient for cytokine detection.
Day 1: Sample Collection and ELISA
- Centrifuge the plate and collect cell-free supernatants. Store at -80°C if not used immediately.
- Perform the ELISA procedure according to the manufacturer's instructions for IFN-γ and IL-2.
- Briefly: Add standards and samples to the pre-coated plate → Incubate → Wash → Add biotinylated detection antibody → Incubate → Wash → Add enzyme-conjugated streptavidin → Incubate → Wash → Add substrate solution → Stop reaction → Read absorbance.
Data Interpretation
- Cytotoxicity: A successful CAR T-cell product will show high, antigen-specific lysis of positive target cells in a dose-dependent manner (increasing with E:T ratio), with minimal lysis of antigen-negative cells.
- Cytokine Release: Significant levels of IFN-γ and IL-2 should be detected only in co-cultures with antigen-positive target cells, confirming specific T-cell activation. The magnitude of release can be correlated with the level of activation.
CAR T-Cell Signaling Pathway and Experimental Workflow
The following diagrams, generated using Graphviz, illustrate the key intracellular signaling of a second-generation CAR and the overall experimental workflow for CAR T-cell evaluation.
Second Generation CAR Signaling
CAR T-Cell Functional Assay Workflow
The therapeutic success of autologous Chimeric Antigen Receptor (CAR) T-cell therapy is fundamentally rooted in the meticulous design of its core structural components. A CAR is a synthetic receptor that reprograms a patient's own T lymphocytes to recognize and eliminate cancerous cells. The efficacy, persistence, and safety of the resulting CAR-T product are directly governed by the function of its constituent domains [4] [5]. Within the context of autologous CAR T-cell production research, optimizing these domains is critical for overcoming challenges such as product variability, T-cell exhaustion, and suboptimal in vivo performance [6]. This Application Note provides a detailed breakdown of the four core modules of a CAR—the single-chain variable fragment (scFv), the hinge, the transmembrane domain, and the intracellular signaling domain—and presents associated experimental protocols for their evaluation and optimization.
The Structural Modules of a CAR
The canonical CAR is a modular fusion protein, comprising an extracellular antigen-recognition domain, typically an scFv; a hinge region that provides flexibility; a hydrophobic transmembrane domain that anchors the receptor; and a complex intracellular signaling domain that initiates T-cell activation [4] [7] [8]. The synergistic function of these modules dictates the overall success of the CAR-T cell product [9].
Single-Chain Variable Fragment (scFv)
The scFv is the antigen-binding domain of the CAR, conferring specificity towards a target tumor-associated antigen (TAA). It is engineered from the variable heavy (VH) and variable light (VL) chains of a monoclonal antibody, connected by a short, flexible peptide linker [4] [7].
Key Design Considerations:
- Affinity and Specificity: The scFv's affinity must be carefully balanced. While high affinity can enhance tumor recognition, it may also lead to on-target, off-tumor toxicity by attacking healthy cells with low antigen expression. An "affinity threshold" often exists for optimal function [5] [8].
- Immunogenicity: Murine-derived scFvs can trigger immune responses in patients, leading to rapid clearance of CAR-T cells and potential anaphylaxis. Humanization or use of fully human scFvs is critical for improving persistence and safety [5].
- Epitope Binding and scFv Aggregation: The location of the target epitope (membrane-distal vs. membrane-proximal) influences CAR efficacy. Furthermore, scFvs with low folding stability can aggregate, leading to tonic signaling and premature T-cell exhaustion [7] [10].
Table 1: Critical Characteristics of the scFv Antigen-Binding Domain
| Characteristic | Impact on CAR-T Function | Optimization Strategy |
|---|---|---|
| Affinity | Determines sensitivity to antigen density; excessive affinity can cause on-target, off-tumor toxicity. | Fine-tune affinity using phage/yeast display; employ low-affinity binders for a higher therapeutic index. |
| Specificity | Defines target recognition and potential cross-reactivity with healthy tissues. | Perform extensive cross-reactivity screens against human tissue arrays. |
| Immunogenicity | Murine sequences can trigger host immune rejection, reducing product persistence. | Humanize scFv sequences or use fully human scFv libraries. |
| Linker Length | Influences scFv valency and off-rate; short linkers can form "diabodies" with higher avidity. | Use (G4S)3 or Whitlow linkers; tailor length based on target epitope accessibility [10]. |
| Target Epitope | Membrane-proximal epitopes may require shorter hinges for optimal access. | Map epitope location and pair with a hinge of appropriate length [5]. |
Hinge Region
The hinge or spacer region is an extracellular structural domain that connects the scFv to the transmembrane domain. Its primary function is to provide flexibility and steric access to the target epitope [4] [7].
Key Design Considerations:
- Length and Flexibility: The optimal length is dependent on the location of the target epitope. Long spacers (e.g., from IgG1) are better for accessing membrane-proximal epitopes, while short spacers (e.g., from CD8α) are sufficient for membrane-distal epitopes [7] [10].
- Domain Origin and FcγR Binding: Hinges derived from immunoglobulins (IgG1, IgG4) can bind to Fcγ receptors (FcγR) on innate immune cells, leading to activation-induced cell death and off-target depletion of CAR-T cells. Fc-silenced mutations (e.g., IgG4 with L235E mutation) or the use of non-Fc receptor-derived hinges (CD8α, CD28) can mitigate this [7] [8].
- Impact on Signaling: The hinge domain can influence CAR clustering and the intensity of activation signaling, effectively regulating the signaling threshold [11] [10].
Table 2: Common Hinge Domains and Their Properties
| Hinge Domain | Length | Key Properties | Clinical/Preclinical Use |
|---|---|---|---|
| CD8α | Short | Low cytokine release; reduced activation-induced cell death (AICD); commonly used. | Yes (e.g., Tisa-cel, Cilta-cel) [10] [8] |
| CD28 | Short/Medium | Can enhance activation and cytokine production; may increase AICD. | Yes (e.g., Axi-cel) [10] |
| IgG1 | Long | Provides long spacer; risk of FcγR binding; requires Fc-silencing mutations. | Preclinical/Some clinical |
| IgG4 (Fc-silenced) | Long | Provides long spacer; reduced FcγR binding after mutation. | Yes (e.g., Brexu-cel) [10] |
Transmembrane Domain
The transmembrane domain (TMD) is a hydrophobic α-helix that anchors the CAR structure within the T-cell membrane. It plays a crucial role in receptor stability and signaling [7] [11].
Key Design Considerations:
- Surface Expression and Stability: The TMD is a major determinant of CAR surface expression levels. Domains from CD28 and CD8α often confer enhanced membrane stability compared to the CD3ζ TMD [11] [8].
- Homodimerization and Interaction with Endogenous Proteins: The CD3ζ TMD can lead to incorporation of the CAR into the endogenous TCR complex, causing ligand-independent signaling. In contrast, CD28 and CD8α TMDs promote CAR homodimerization without significant TCR interaction [7] [11].
- Signal Transduction: The TMD influences the stability of the immunological synapse and the efficiency of signal transduction from the extracellular to the intracellular domain [11].
Intracellular Signaling Domain
The intracellular domain is responsible for initiating T-cell activation and effector functions upon antigen binding. The design of this domain has evolved through several "generations" [4].
First-Generation CARs: Contain only the CD3ζ chain signaling domain, which carries three Immunoreceptor Tyrosine-Based Activation Motifs (ITAMs). These CARs showed limited persistence and efficacy in clinical applications due to the lack of a co-stimulatory signal [4].
Second-Generation CARs: Incorporate one costimulatory domain (e.g., CD28 or 4-1BB) proximal to the CD3ζ domain. This addition provides a critical second signal, dramatically improving T-cell expansion, cytokine secretion, persistence, and cytotoxicity. All currently FDA-approved CAR-T products are second-generation [4] [1].
Third-Generation CARs: Contain two costimulatory domains in tandem (e.g., CD28-41BB or CD28-OX40 combined with CD3ζ). The clinical benefits of this design are still under investigation, as the signaling output is not a simple additive effect [4].
Key Design Considerations:
- Costimulatory Domain Choice: The identity of the costimulatory domain critically shapes the phenotype, metabolism, and persistence of CAR-T cells.
- Signal Strength: The design must balance potent activation with the risk of T-cell exhaustion from excessive or tonic signaling.
Table 3: Comparison of Primary Costimulatory Domains in Second-Generation CARs
| Costimulatory Domain | T Cell Phenotype | Metabolic Profile | Persistence | Kinetics | Example Product |
|---|---|---|---|---|---|
| CD28 | Effector Memory | Aerobic Glycolysis | Shorter | Rapid, intense activation | Axi-cel (Yescarta) [4] [1] |
| 4-1BB (CD137) | Central Memory | Mitochondrial Oxidative Phosphorylation | Longer | Slener, more sustained | Tisa-cel (Kymriah) [4] [1] |
Experimental Protocols for Domain Analysis
This section outlines key methodologies for the functional characterization of CAR domains during the research and development phase.
Protocol: Evaluation of scFv Affinity and Specificity
Objective: To determine the binding affinity (KD) of the isolated scFv and confirm its specificity for the intended target antigen.
Materials:
- Biosensor System: Surface Plasmon Resonance (SPR, e.g., Biacore) or Bio-Layer Interferometry (BLI, e.g., Octet).
- Purified scFv: As a monomeric protein.
- Purified Target Antigen: Recombinant protein, including both the intended target and related proteins for specificity testing.
Method:
- Immobilization: Immobilize the target antigen onto the biosensor chip or biosensor tip.
- Association: Expose the immobilized antigen to a concentration series of the scFv protein and monitor binding in real-time.
- Dissociation: Replace the scFv solution with buffer to monitor dissociation of the bound complex.
- Data Analysis: Fit the resulting association and dissociation curves to a 1:1 binding model to calculate the kinetic rate constants (kon, koff) and the equilibrium dissociation constant (KD = koff/kon).
- Specificity Test: Repeat the assay using off-target proteins to confirm lack of binding.
Interpretation: A low KD (nanomolar range) indicates high affinity. The absence of binding to off-target proteins confirms specificity. This in vitro affinity should be correlated with functional CAR-T cell activity [5].
Protocol: Flow Cytometry-Based Analysis of CAR Surface Expression and Antigen Binding
Objective: To quantify the surface expression level of the full CAR construct and verify its functional antigen-binding capability.
Materials:
- CAR-T Cells: Transduced and expanded.
- Control T Cells: Non-transduced (NTD) or mock-transduced.
- Staining Antibodies: Anti-tag antibody (e.g., anti-HA, anti-FLAG) for CAR detection, fluorescently conjugated secondary antibodies.
- Recombinant Antigen: Target antigen fused to a tag (e.g., His-tag, Fc-tag).
- Flow Cytometer.
Method:
- Harvest and Wash: Harvest CAR-T and control cells, wash with FACS buffer (PBS + 2% FBS).
- Staining for CAR Expression:
- Aliquot cells into two tubes.
- Stain one tube with a primary anti-tag antibody and the other with an isotype control antibody.
- Incubate, wash, and then stain with a fluorescent secondary antibody if needed.
- Staining for Antigen Binding:
- Aliquot fresh cells.
- Incubate with the recombinant target antigen protein.
- Wash and then stain with a fluorescent anti-tag antibody that recognizes the tag on the antigen.
- Analysis: Analyze all samples on a flow cytometer. Gate on live, single T cells.
Interpretation: CAR expression is confirmed by a positive shift in fluorescence in the anti-tag stained sample compared to the isotype control. Functional antigen binding is confirmed by a positive shift in the antigen-binding stained sample compared to cells stained with the detection antibody alone. This protocol is adapted from methods described in [11].
Protocol: In Vitro Cytotoxicity Assay (Real-Time Impedance-Based)
Objective: To quantitatively assess the ability of CAR-T cells to kill antigen-expressing tumor cells in real-time.
Materials:
- CAR-T Cells: Effector cells.
- Target Tumor Cells: Antigen-positive and antigen-negative cell lines.
- Real-Time Cell Analyzer: Instrument capable of measuring electrical impedance (e.g., xCelligence RTCA).
Method:
- Seed Target Cells: Seed the target tumor cells into a specialized E-plate and allow them to adhere and proliferate overnight. The instrument will establish a baseline impedance measurement.
- Add Effector Cells: The next day, add CAR-T cells at various Effector:Target (E:T) ratios to the wells. Include wells with non-transduced T cells as a negative control.
- Monitor Impedance: Continuously monitor cell impedance for 24-96 hours. As the CAR-T cells kill the adherent target cells, the cell index (a measure of impedance) will decrease.
- Data Analysis: Calculate percentage cytotoxicity at different time points using the formula provided by the instrument manufacturer, which typically compares the cell index in experimental wells to that in target-cell-only control wells.
Interpretation: Antigen-specific killing is demonstrated by a dose- and time-dependent decrease in impedance only in co-cultures with antigen-positive target cells and CAR-T cells. This method provides kinetic data that endpoint assays cannot [12].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for CAR Domain Research and Development
| Reagent / Tool | Function in R&D | Key Considerations |
|---|---|---|
| scFv Phage/Yeast Display Library | Discovery and affinity maturation of antigen-binding domains. | Enables screening of large naive or immune libraries for high-affinity binders without immune tolerance [5]. |
| Lentiviral/Retroviral Vectors | Stable genetic modification of primary human T cells for CAR expression. | Lentivirus can transduce non-dividing cells; Retrovirus requires T-cell activation. Both require extensive safety testing [6] [1]. |
| Anti-Tag Antibodies (e.g., anti-HA, LdT) | Detection and purification of CAR-positive T cells post-transduction. | Requires incorporation of a small tag (e.g., HA, Strep-tag) into the extracellular hinge region [11] [10]. |
| Recombinant Antigen Protein | Validation of CAR binding specificity and flow cytometry staining. | Should be in a membrane-bound-like conformation; Fc-fusion proteins are common. |
| Magnetic Cell Separation Beads | Isolation of specific T-cell subsets (e.g., CD4+/CD8+) from leukapheresis product. | Allows for defined starting populations and final product composition (e.g., Liso-cel) [6] [1]. |
| Cytokine ELISA/MSD Kits | Quantification of cytokine secretion (e.g., IFN-γ, IL-2) upon antigen-specific activation. | Measures T-cell activation strength and potential for cytokine release syndrome (CRS) [5]. |
The rational design of the scFv, hinge, transmembrane, and signaling domains is paramount to engineering effective and safe autologous CAR-T cell products. As research advances, the interplay between these domains is increasingly recognized as a critical factor, where a change in one module can profoundly affect the function of another [11] [9]. Future directions in autologous CAR-T production research will focus on further optimizing these domains to combat T-cell exhaustion, improve persistence, and enhance efficacy against solid tumors. This includes exploring novel costimulatory domains (e.g., ICOS, OX40), developing fully human and stable non-scFv binders, and engineering hinges and TMDs that precisely tune signaling thresholds [10] [8]. A deep understanding of these core components provides the foundational knowledge required to innovate and advance the next generation of CAR-T cell therapies.
Autologous chimeric antigen receptor T-cell (CAR-T) therapy represents a paradigm shift in cancer treatment, demonstrating remarkable efficacy in treating hematological malignancies. This personalized immunotherapeutic approach involves genetically engineering a patient's own T-cells to express synthetic receptors that redirect them to specifically target and eliminate cancer cells [13]. The clinical success of this technology is embodied by the U.S. Food and Drug Administration (FDA) approval of several autologous CAR-T products, all of which target either the CD19 antigen on B-cell malignancies or the B-cell maturation antigen (BCMA) on multiple myeloma cells [14] [15]. These therapies are characterized by their status as "living drugs," which, upon infusion, can persist, expand, and maintain long-term surveillance within the patient's body [14]. The recent FDA decision to eliminate the Risk Evaluation and Mitigation Strategies (REMS) for these products underscores the medical community's growing experience and confidence in managing their associated risks, such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) [16] [17]. This application note details the approved autologous CAR-T products, their target antigens, and the standardized protocols that underpin their clinical application.
The following table synthesizes key information for the seven autologous CAR-T cell therapies currently approved by the U.S. FDA, providing a clear comparison of their targets, indications, and developers.
Table 1: FDA-Approved Autologous CAR-T Cell Therapies and Their Targets
| Product Name (Generic Name) | Molecular Target | Approved Indication(s) | Developer/Marketer |
|---|---|---|---|
| Kymriah (tisagenlecleucel) [14] [15] | CD19 [14] [15] | Pediatric and young adult B-cell acute lymphoblastic leukemia (ALL); Adult relapsed or refractory large B-cell lymphoma [14] [15] | Novartis [14] [15] |
| Yescarta (axicabtagene ciloleucel) [14] [15] | CD19 [14] [15] | Adult relapsed or refractory large B-cell lymphoma [14] [15] | Kite Pharma (Gilead Sciences) [14] [15] |
| Tecartus (brexucabtagene autoleucel) [14] [15] | CD19 [14] [15] | Adult relapsed or refractory mantle cell lymphoma (MCL) [14] [15] | Kite Pharma (Gilead Sciences) [14] [15] |
| Breyanzi (lisocabtagene maraleucel) [14] [15] | CD19 [14] [15] | Adult relapsed or refractory large B-cell lymphoma [14] [15] | Juno Therapeutics (Bristol-Myers Squibb) [14] [15] |
| Abecma (idecabtagene vicleucel) [14] [15] | BCMA [14] [15] | Adult relapsed or refractory multiple myeloma [14] [15] | bluebird bio & Bristol-Myers Squibb [14] [15] |
| Carvykti (ciltacabtagene autoleucel) [14] [15] | BCMA [14] [15] | Adult relapsed or refractory multiple myeloma [14] [15] | Legend Biotech & Janssen (Johnson & Johnson) [14] [15] |
| Aucatzyl (list of indications may vary) [14] [15] | Not explicitly stated in sources, but implied to be a target for approved autologous therapy | Developed and marketed by Autolus Therapeutics [14] [15] | Autolus Therapeutics [14] [15] |
Core Protocol: Standardized Workflow for Autologous CAR-T Cell Manufacturing
The manufacturing of clinical-grade autologous CAR-T cells is a multi-step process that must adhere to strict current Good Manufacturing Practice (cGMP) guidelines. The following protocol outlines the standard workflow, which can be executed using centralized, decentralized, or point-of-care models [18].
Patient Leukapheresis and T-Cell Collection
- Objective: To collect a sufficient number of the patient's mononuclear cells, including T-cells.
- Procedure:
- Schedule patient leukapheresis prior to initiating lymphodepleting chemotherapy.
- Perform leukapheresis to collect peripheral blood mononuclear cells (PBMCs).
- Transport the apheresis product in a temperature-controlled shipping container to the manufacturing facility.
- Isolate and enrich T-cells from the apheresis product using density gradient centrifugation or magnetic bead-based separation (e.g., Ficoll-Paque PLUS, Miltenyi Biotec MACS Cell Separation Systems).
T-Cell Activation and Genetic Modification
- Objective: To activate the isolated T-cells and introduce the CAR transgene.
- Procedure:
- T-Cell Activation: Resuspend T-cells in culture medium supplemented with cytokines (e.g., IL-2, IL-7, IL-15) and activate using anti-CD3/CD28 antibody-coated beads or soluble agonists.
- Genetic Transduction: Within 24-48 hours of activation, transduce the T-cells with the CAR construct.
- Method: Use gamma-retroviral or lentiviral vectors as the primary gene delivery method [13]. The vector is added to the culture at a predetermined Multiplicity of Infection (MOI).
- Alternative Technologies: Non-viral methods, such as electroporation of transposon/transposase systems (e.g., piggyBac) or mRNA, are also in development [19].
- Incubate cells under standard conditions (37°C, 5% CO2) for transduction.
Ex Vivo Cell Expansion
- Objective: To generate a clinically relevant dose of CAR-T cells.
- Procedure:
- Following transduction, culture the cells in gas-permeable culture bags or closed-system bioreactors.
- Maintain cells in appropriate media (e.g., TexMACS, X-VIVO 15) with necessary cytokines and nutrients.
- Monitor cell density, viability, and phenotype daily. Perform medium exchanges or cell dilutions to maintain optimal growth conditions.
- Continue expansion until the target cell number is achieved, typically over 7-10 days, though next-day processes are emerging [20].
Formulation, Cryopreservation, and Release
- Objective: To prepare the final product for infusion and ensure it meets all release specifications.
- Procedure:
- Harvesting: Collect CAR-T cells from the culture system and wash to remove debris and cytokines.
- Formulation: Resuspend the cell pellet in a cryopreservation medium containing human serum albumin and DMSO.
- Cryopreservation: Fill the final product into infusion bags, cryofreeze using a controlled-rate freezer, and store in the vapor phase of liquid nitrogen.
- Quality Control (QC) Testing: Perform mandatory release testing on aliquots of the product. This includes:
- Sterility: Tests for bacterial and fungal contamination.
- Mycoplasma: PCR or culture-based testing.
- Potency: In vitro co-culture assay to measure specific cytotoxicity against target antigen-expressing cells and IFN-γ release.
- Identity: Flow cytometry confirming CAR expression and T-cell markers.
- Purity and Viability: Absence of undesirable cell populations and high viability (>70-80%).
- Transport: Ship the cryopreserved product back to the treatment center for infusion.
Diagram 1: Autologous CAR-T Cell Manufacturing and Clinical Workflow
The Scientist's Toolkit: Essential Reagents for CAR-T Cell Research
The development and production of CAR-T cells rely on a suite of specialized reagents and equipment. The table below details key components of the research and manufacturing toolkit.
Table 2: Key Research Reagent Solutions for Autologous CAR-T Cell Production
| Reagent/Equipment Category | Specific Examples | Function in CAR-T Workflow |
|---|---|---|
| Cell Separation Systems [18] | Miltenyi Biotec CliniMACS Prodigy, Magnetic-Activated Cell Sorting (MACS) reagents | Isolation and enrichment of T-cells from leukapheresis material. |
| Cell Activation Reagents | Anti-CD3/CD28 antibody-coated beads, TransAct | Provides Signal 1 (CD3) and Signal 2 (CD28) for initial T-cell activation prior to genetic modification. |
| Gene Delivery Vectors [13] [19] | Lentiviral vectors, Gamma-retroviral vectors, Transposon Systems (piggyBac) | Stable integration of the CAR transgene into the T-cell genome to confer antigen specificity. |
| Cell Culture Media & Cytokines [18] | TexMACS Medium, X-VIVO 15; Recombinant IL-2, IL-7, IL-15 | Supports the ex vivo expansion and maintenance of T-cells, promoting desired phenotypes like memory subsets. |
| Automated Manufacturing Platforms [18] [20] | Miltenyi Biotec CliniMACS Prodigy, Lonza Cocoon | Automates and standardizes the manufacturing process from cell culture to final formulation in a closed system. |
| Analytical & QC Tools | Flow Cytometry (CAR expression, immunophenotyping), Cytotoxicity Assays (Potency) | Critical for in-process testing and final product release to ensure identity, purity, potency, and safety. |
Antigen Targets and Signaling Pathways in Second-Generation CARs
The clinical success of approved CAR-T products is largely attributed to the use of second-generation CAR designs. These synthetic receptors incorporate a costimulatory domain (e.g., CD28 or 4-1BB) alongside the primary CD3ζ activation signal, which significantly enhances T-cell persistence, expansion, and antitumor efficacy compared to first-generation constructs [13]. The choice of costimulatory domain influences the metabolic and functional profile of the resulting CAR-T cells.
Diagram 2: Second-Generation CAR Structure and Signaling
Recent Regulatory Evolution and Future Perspectives
A significant recent development is the FDA's elimination of the Risk Evaluation and Mitigation Strategies (REMS) for BCMA- and CD19-directed autologous CAR-T cell immunotherapies in June 2025 [17]. This decision reflects the hematology/oncology community's extensive experience and established infrastructure for safely managing these therapies, including toxicities like CRS and ICANS [16]. The removal of the REMS requirements reduces administrative burdens and is expected to improve patient access, particularly in rural areas, while maintaining safety through updated product labeling and post-market surveillance [17].
Future advancements in the field are focused on overcoming current challenges. Key areas of research include:
- Reducing Vein-to-Vein Time: Innovations like semi-automated 24-hour manufacturing processes are being developed to shorten production time, which may improve efficacy by preserving naïve T-cell subsets and accelerate treatment for critically ill patients [20].
- Expanding to Solid Tumors: A major frontier is the application of CAR-T therapy to solid tumors, which requires overcoming obstacles like tumor heterogeneity, immunosuppressive microenvironments, and identifying safe and effective target antigens [21] [13].
- Developing Allogeneic ("Off-the-Shelf") Products: Research is intensifying on allogeneic CAR-T cells derived from healthy donors, which use gene editing (e.g., TALEN, CRISPR) to limit graft-versus-host disease (GvHD) and TCR-mediated immune responses, potentially enabling immediate, scalable treatment [22] [14] [13].
The approved autologous CAR-T cell therapies targeting CD19 and BCMA have firmly established this modality as a pillar of cancer treatment. Continued refinement of manufacturing protocols, coupled with evolving regulatory frameworks and intense research into next-generation technologies, promises to broaden the applicability and accessibility of this powerful therapeutic platform.
Current Landscape and Unmet Needs in Hematologic Malignancies and Solid Tumors
Chimeric Antigen Receptor (CAR) T-cell therapy represents a paradigm shift in cancer treatment, demonstrating unprecedented efficacy in relapsed/refractory hematological malignancies [23] [24]. This adoptive cell therapy involves genetically engineering a patient's own T-cells to express synthetic receptors that target tumor-associated antigens, redirecting immune cells to recognize and eliminate cancer [19] [25]. As of 2025, six autologous CAR-T products have received FDA approval, all targeting antigens in hematologic cancers (CD19 or BCMA) [24] [26]. Despite remarkable success in hematological malignancies, significant challenges remain in extending these successes to solid tumors, which constitute over 90% of all malignancies [27]. This application note delineates the current landscape, unmet needs, and experimental protocols within the context of autologous CAR-T cell production research, providing a comprehensive resource for scientists and drug development professionals.
Current Clinical Landscape of CAR-T Therapy
The CAR-T field has evolved rapidly since the first FDA approvals in 2017. The current clinical landscape is characterized by robust activity in hematologic malignancies with emerging efforts in solid tumors.
Table 1: FDA-Approved Autologous CAR-T Cell Therapies (as of 2025)
| Product Name | Target Antigen | Year Approved | Indications | Costimulatory Domain |
|---|---|---|---|---|
| Kymriah (Tisagenlecleucel) | CD19 | 2017 | ALL, NHL | 4-1BB |
| Yescarta (Axicabtagene ciloleucel) | CD19 | 2017 | NHL, Follicular lymphoma | CD28 |
| Tecartus (Brexucabtagene autoleucel) | CD19 | 2020 | ALL, Mantle cell | CD28 |
| Breyanzi (Lisocabtagene maraleucel) | CD19 | 2021 | NHL | 4-1BB |
| Abecma (Idecabtagene vicleucel) | BCMA | 2021 | Multiple Myeloma | 4-1BB |
| Carvykti (Ciltacabtagene autoleucel) | BCMA | 2022 | Multiple Myeloma | 4-1BB |
The pipeline for CAR-T therapies continues to expand rapidly, with over 300 companies and 300+ pipeline drugs in development as of 2025 [19]. Key developments include next-generation constructs targeting novel antigens such as GPRC5D and FcRH5 for multiple myeloma, and emerging approaches for acute myeloid leukemia (AML) and solid tumors [23] [24].
Unmet Needs and Challenges
Challenges in Hematologic Malignancies
Despite remarkable success, several limitations persist in hematologic applications. Relapse remains a significant concern, with approximately 30-50% of patients experiencing disease recurrence within one year post-infusion [24]. Antigen escape variants, wherein tumor cells downregulate or lose target antigen expression, constitute a primary mechanism of relapse [27]. Additional challenges include restricted patient access due to manufacturing constraints and high costs (approximately $500,000 per infusion), significant toxicities such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS), and limited efficacy in certain hematologic malignancies like AML due to lack of tumor-specific antigens [23] [26].
Challenges in Solid Tumors
The application of CAR-T therapy to solid tumors faces formidable biological and technical hurdles:
- Lack of tumor-specific antigens: Solid tumors typically express tumor-associated antigens (TAAs) rather than tumor-specific antigens (TSAs), increasing the risk of on-target/off-tumor toxicity against healthy tissues expressing these antigens [27].
- Immunosuppressive tumor microenvironment (TME): The TME creates physical and biochemical barriers through immunosuppressive cells (Tregs, MDSCs), cytokines (TGF-β, IL-10), and checkpoint molecules (PD-L1, B7-H3) that inhibit CAR-T function and persistence [27] [28].
- Poor tumor infiltration: Physical barriers including abnormal vasculature, dense extracellular matrix, and high interstitial pressure impede CAR-T cell trafficking and infiltration into tumor sites [28].
- Antigen heterogeneity: Intra-tumoral and inter-tumoral heterogeneity in antigen expression promotes selection of antigen-loss variants and tumor escape [27].
Engineering Strategies and Experimental Protocols
CAR Construct Engineering and Signaling Pathways
CARs are synthetic receptors comprising extracellular antigen-recognition domains (typically scFv), hinge/spacer regions, transmembrane domains, and intracellular signaling domains [24]. The evolution of CAR design has progressed through five generations, each incorporating enhanced functionality.
Table 2: Research Reagent Solutions for CAR Construct Engineering
| Reagent Category | Specific Examples | Function in CAR Engineering | Key Suppliers |
|---|---|---|---|
| Viral Vectors | Lentivirus, Retrovirus, γ-Retrovirus | Stable genomic integration of CAR transgene | Lentigen, Local production [26] |
| Non-Viral Vectors | Transposon (piggyBac), CRISPR/Cas9 | Site-specific integration, reduced mutagenesis | Various |
| CAR Signaling Domains | CD3ζ, CD28, 4-1BB, OX40, ICOS | T-cell activation and costimulation | Gene synthesis companies |
| Cytokine Cassettes | IL-12, IL-15, IL-7, IL-21 | Enhanced persistence, memory formation | Various |
| Safety Switches | EGFRt, iCaspase9 | Controlled elimination of CAR-T cells | Various |
Protocol 4.1.1: Second-Generation CAR Construct Design
- scFv Selection: Clone variable heavy (VH) and light (VL) chains from hybridoma or phage display libraries, connecting via (Gly₄Ser)₃ linkers [24].
- Hinge Domain Selection: Choose appropriate hinge length (CD8α, CD28, or IgG4-Fc) based on target antigen accessibility [27].
- Transmembrane Domain: Fuse hinge to transmembrane domains (typically CD28 or CD8α) for stable membrane anchoring [24].
- Signaling Domains: Clone CD3ζ activation domain with costimulatory domain (CD28 for rapid activation, 4-1BB for enhanced persistence) in tandem [24].
- Vector Cloning: Subclone CAR cassette into lentiviral or retroviral backbone with EF-1α or MND promoters for T-cell expression [26].
Strategies for Solid Tumors
4.2.1 Target Antigen Optimization
Approaches to address antigen heterogeneity and specificity in solid tumors include:
Protocol 4.2.1: Bispecific CAR-T Cell Generation
- CAR Design: Design two separate CAR constructs targeting distinct TAAs (e.g., HER2 and IL13Rα2 for glioblastoma) [27].
- Vector Production: Generate lentiviral vectors for each CAR construct with different selection markers (e.g., NGFR and CD34).
- Sequential Transduction: Isolate T-cells via leukapheresis and activate with CD3/CD28 antibodies. Transduce with first CAR vector, expand for 48-72 hours, then transduce with second CAR vector [27].
- Selection and Expansion: Isque double-positive cells via magnetic sorting and expand in IL-2/IL-15 media for 10-14 days [26].
- Functional Validation: Validate bispecific function through cytotoxicity assays against single-antigen and dual-antigen expressing tumor cells [27].
4.2.2 TME Modulation Strategies
Protocol 4.2.2: Armored CAR-T Cells with TME-Resistant Features
- Cytokine Armoring: Clone IL-12, IL-15, or IL-7 cytokine cassettes into CAR construct via P2A or T2A self-cleaving peptides [28].
- Checkpoint Inhibition: Co-express dominant-negative TGF-β receptor (dnTGFβR) or PD-1/CD28 chimeric switch receptors (CSR) to convert inhibitory signals into activation [28].
- Chemokine Receptor Matching: Engineer CAR-T cells to express chemokine receptors (e.g., CXCR2, CCR4) matching tumor-secreted chemokines to enhance infiltration [28].
- Metabolic Engineering: Overexpress PPAR-γ or SREBP transcription factors to enhance lipid metabolism and resist TME nutrient deprivation [28].
T-cell Subset Selection Protocols
Emerging evidence indicates that specific T-cell subsets confer distinct functional advantages for CAR-T products.
Table 3: T-cell Subsets for CAR-T Manufacturing
| T-cell Subset | Phenotypic Markers | Functional Advantages | Protocol Considerations |
|---|---|---|---|
| CD4+ T-cells | CD3+CD4+ | Enhanced persistence, cytokine production | Isolate via positive selection; infuse at 1:1 ratio with CD8+ CAR-T [28] |
| CD8+CD161+ T-cells | CD3+CD8+CD161+ | Enhanced cytotoxicity, memory features | Isolate via FACS sorting; shows increased granzyme B and perforin [28] |
| γδ T-cells | TCRγδ+ | MHC-independent recognition, lower GVHD risk | Expand with zoledronate (ZOL) pre-treatment [28] |
| NKT cells | CD3+TCRVα24-Jα18+ | Innate-adaptive bridge, improved safety | Culture with IL-15 for enhanced persistence [28] |
| TN/SCM cells | CD45RA+CD45RO-CCR7+CD95+ | Reduced exhaustion, enhanced persistence | Isolate via FACS; demonstrates superior antineoplastic activity [28] |
Protocol 4.3.1: T-cell Subset Isolation and CAR Engineering
- Leukapheresis: Collect peripheral blood mononuclear cells (PBMCs) from patient via standard leukapheresis procedures [26].
- Subset Isolation: Isolate desired T-cell subsets using magnetic-activated cell sorting (MACS) or fluorescence-activated cell sorting (FACS) with specific antibody panels.
- T-cell Activation: Activate isolated T-cells with CD3/CD28 antibodies immobilized on beads or artificial antigen-presenting cells (aAPCs) [26].
- Genetic Modification: Transduce activated T-cells with CAR-encoding lentiviral vectors at MOI 5-10 via spinoculation (centrifugation at 2000xg for 90 minutes at 32°C) [26].
- Ex Vivo Expansion: Culture transduced T-cells in X-VIVO 15 or TexMACs media supplemented with 5-10% human AB serum, IL-2 (100 IU/mL), and IL-15 (10 ng/mL) for 10-14 days [26].
- Quality Control: Perform flow cytometry for CAR expression, sterility testing, and potency assays before infusion.
Autologous CAR-T Manufacturing Workflows
The autologous CAR-T manufacturing process presents significant logistical and technical challenges, with current efforts focused on decentralized production models to enhance accessibility.
Protocol 5.1: Decentralized CAR-T Manufacturing Using Closed Systems
- Point-of-Care Leukapheresis: Perform leukapheresis at treatment center, processing within 6-8 hours of collection [26].
- Closed System Manufacturing: Utilize automated closed systems (e.g., CliniMACS Prodigy, Lonza Cocoon) with single-use disposable kits to minimize contamination risk [26].
- Reduced Vein-to-Vein Time: Implement accelerated protocols (8-12 days vs. standard 2-4 weeks) using fresh cell infusion where possible [26].
- Abbreviated Quality Control: Employ rapid sterility testing (e.g., BacT/ALERT) and flow cytometry for CAR expression to reduce release time [26].
- Clinical studies demonstrate that decentralized manufacturing can reduce vein-to-vein time to 8-11 days with comparable efficacy to commercial products [26].
The landscape of CAR-T cell therapy continues to evolve rapidly, with promising strategies emerging to address current challenges. Key future directions include the development of allogeneic "off-the-shelf" CAR-T products, enhanced safety systems via synthetic biology, combination therapies with checkpoint inhibitors or small molecules, and personalized CAR approaches targeting neoantigens [27] [24] [28]. For solid tumors, innovative approaches such as in vivo CAR-T cell generation and CAR-T cells capable of remodeling the tumor microenvironment represent promising frontiers [28]. The ongoing optimization of autologous CAR-T manufacturing through decentralized models and automated systems will be crucial for improving accessibility and reducing costs, ultimately expanding this transformative therapy to more patients worldwide.
From Vein to Vein: A Step-by-Step Guide to the Autologous CAR T-Cell Manufacturing Workflow
In autologous Chimeric Antigen Receptor (CAR) T-cell production, the quality of the final therapeutic product is inherently linked to the quality of the patient's starting material. Leukapheresis, the procedure used to collect peripheral blood mononuclear cells (PBMCs), provides the essential foundation for manufacturing. The critical quality attributes (CQAs) of the collected PBMCs—including cell composition, viability, and functional potential—significantly impact downstream processes such as T-cell activation, genetic modification, and expansion, ultimately influencing the safety, potency, and efficacy of the resulting CAR T-cell product [6] [29]. This application note details the procedures for leukapheresis collection, PBMC processing, and the analytical assessment of key quality attributes within the context of autologous CAR T-cell research and development.
Leukapheresis as a Starting Material
Leukapheresis vs. Buffy Coat
For CAR T-cell manufacturing, leukapheresis is the standard method for obtaining starting material due to its superior yield and quality compared to buffy coat isolation from whole blood.
Table 1: Comparison of Leukapheresis and Buffy Coat as Starting Material for Cell Therapy
| Attribute | Leukapheresis (Leukopak) | Buffy Coat |
|---|---|---|
| Collection Volume | 100 - 200 mL [30] | ~5 mL (from 500 mL whole blood) [30] |
| PBMC Yield | Up to 8.5 billion cells [30] | Up to ~1 billion cells [30] |
| Cell Composition | Primarily mononuclear cells [30] | Mononuclear cells + granulocytes [30] |
| Purity | Higher PBMC purity, lower granulocyte contamination [30] [31] | Lower purity, requires further purification [30] |
| Standardization | More standardized protocol [30] | Higher variability [30] |
| Best For | Clinical applications, scale-up, manufacturing [30] | Pilot studies, budget-conscious exploratory assays [30] |
Impact of Leukapheresis on Donor Immune Competence
A critical consideration for autologous therapy is whether the leukapheresis procedure itself compromises the donor's immune system. Research indicates that a single 2-liter leukapheresis procedure has no significant impact on a patient's immune cell counts or function. Circulating lymphocytes represent only about 2% of the total body lymphocyte pool, and the immune system rapidly compensates for the collected cells [32]. Studies in cancer patients show no significant change in absolute lymphocyte count (ALC), CD3+, CD4+, or CD8+ cell counts post-procedure, and T-cell function, as measured by IFN-γ ELISPOT response to influenza, remains intact [32].
Donor Considerations and Cell Collection
The health status of the patient donor is a major variable affecting the leukapheresis product. Factors such as advanced age, specific disease types (e.g., B-ALL), and prior therapies (e.g., lymphotoxic drugs) can lead to reduced lymphocyte collection efficiency and negatively impact the initial quality of T cells [29]. Products from heavily pre-treated patients may contain T cells with an increased frequency of exhaustion markers and impaired mitochondrial biogenesis, which can affect the expansion and persistence of the final CAR T-cell product [29]. Therefore, careful donor screening and, when possible, scheduling the leukapheresis procedure after a suitable washout period from certain therapies, is recommended.
PBMC Processing and Cryopreservation
Experimental Protocol: PBMC Isolation from Leukopak
The following protocol, adapted from GCLP guidelines, ensures high-quality PBMC isolation for research and clinical applications [33].
Objective: To isolate and cryopreserve PBMCs from a leukapheresis product within 8 hours of collection, maximizing cell viability, yield, and functionality.
Materials:
- Leukapheresis product (fresh, room temperature)
- Dulbecco's Phosphate Buffered Saline (D-PBS), without Ca2+/Mg2+
- Ficoll-Paque Premium density gradient medium
- Cryopreservation medium: 90% Fetal Bovine Serum (FBS) + 10% DMSO
- Centrifuge, automated cell counter (e.g., Vi-CELL XR), hemacytometer
- Programmable controlled-rate freezer
- Liquid nitrogen vapor phase storage freezer
Procedure:
- Receipt and Initial Assessment: Upon receipt, record the leukapheresis product volume and perform an initial white blood cell (WBC) count using an automated hematology analyzer [33].
- Dilution and Separation:
- Divide the leukapheresis product into manageable equal volumes (e.g., four parts).
- Dilute each part with D-PBS to a total volume of 140 mL [33].
- Carefully overlay the diluted product onto Ficoll-Paque Premium in appropriate centrifuge tubes (e.g., 35 mL of diluted product over 15 mL of Ficoll) [33].
- Centrifuge at 800 × g for 30 minutes at 25°C with the brake off [33].
- PBMC Harvesting and Washing:
- After centrifugation, carefully aspirate and discard the upper plasma/platelet layer.
- Harvest the opaque PBMC interface layer (buffy coat) and transfer it to a new tube.
- Wash the harvested PBMCs with D-PBS by centrifuging at 300 × g for 10 minutes at 25°C. Discard the supernatant. Repeat the wash step a second time [33].
- Cell Counting and Viability Assessment:
- Pool all washed PBMCs into a homogeneous suspension.
- Perform cell count and viability assessment. It is recommended to use multiple platforms (e.g., automated cell counter and manual hemacytometer with trypan blue exclusion) in triplicate to ensure accuracy. Results from different platforms should fall within 20% of the mean to be accepted [33].
- Cryopreservation:
- Adjust the cell concentration to 20 × 10^6 cells/mL using pre-chilled cryopreservation medium (90% FBS / 10% DMSO) [33].
- Aliquot the cell suspension into pre-labeled cryovials and place them on wet ice.
- Transfer vials to a programmed controlled-rate freezer, cooling at a rate of -1°C per minute from 4°C to -90°C [33].
- Immediately transfer the frozen vials to a vapor-phase liquid nitrogen freezer for long-term storage at ≤ -150°C [33].
Diagram 1: PBMC isolation and cryopreservation workflow.
Critical Quality Attributes of Patient PBMCs
The CQAs of the PBMC starting material are predictive of manufacturing success and product performance. Key attributes to monitor are summarized below.
Table 2: Critical Quality Attributes of Patient PBMCs for CAR T-Cell Manufacturing
| Quality Attribute | Description & Impact | Assessment Method |
|---|---|---|
| Viability | Indulates overall cell health. Low viability can lead to poor expansion and product efficacy. | Trypan blue exclusion using automated cell counters (e.g., Vi-CELL BLU) [34]. |
| Cell Count & Total Yield | Determines if sufficient material is available for manufacturing. | Automated hematology analyzers (e.g., Ac*T 5Diff CP) [33]. |
| PBMC Composition & Purity | High granulocyte or monocyte contamination can reduce T-cell expansion and transduction efficiency [29]. | Flow cytometry for CD3+ (T cells), CD19+ (B cells), CD14+ (monocytes), CD16+/CD66b+ (granulocytes). |
| CD4+:CD8+ Ratio | Influences product phenotype and efficacy. A defined ratio (e.g., 1:1) may improve consistency [6]. | Flow cytometry for CD4 and CD8 surface markers. |
| T-cell Phenotype | A higher proportion of naïve (TN) and stem cell memory (TSCM) cells is associated with better expansion and persistence post-infusion [6] [29]. | Flow cytometry for CD45RA, CD45RO, CD62L, CCR7, CD95. |
| Functional Competence | Assesses the baseline capacity of T cells to respond to stimuli. | IFN-γ ELISPOT in response to viral antigens (e.g., flu) [32]. |
| Microbiological Safety | Ensures the starting material is free from microbial contamination. | Sterility testing (e.g., BacT/ALERT) [35]. |
Experimental Protocol: Phenotypic Characterization by Flow Cytometry
Objective: To characterize the immune cell composition and T-cell differentiation state within the PBMC starting material.
Materials:
- PBMC sample (fresh or thawed)
- Flow cytometry staining buffer (D-PBS + 2% FBS)
- Antibody panel:
- Lineage: CD3 (FITC), CD19 (PE), CD14 (PerCP-Cy5.5), CD56 (APC) for NK cells
- T-cell Subsets: CD4 (FITC), CD8 (PE)
- T-cell Differentiation: CD45RA (FITC), CD45RO (PE), CCR7 (APC)
- Viability dye (e.g., 7-AAD)
- Flow cytometer
Procedure:
- Cell Staining:
- Aliquot 1 × 10^6 PBMCs into flow cytometry tubes.
- Wash cells with staining buffer by centrifuging at 300 × g for 5 minutes.
- Resuspend cell pellet in 100 µL of staining buffer containing the pre-optimized antibody cocktail and viability dye.
- Incubate for 30 minutes at 4°C in the dark.
- Wash cells twice with staining buffer and resuspend in a fixed volume for acquisition.
- Data Acquisition and Analysis:
- Acquire data on a flow cytometer, collecting a minimum of 50,000 events in the lymphocyte gate.
- Analyze data using flow cytometry analysis software:
- Gate on singlets, then lymphocytes based on FSC-A/SSC-A, then viable cells (7-AAD negative).
- For composition: Report the percentage of CD3+ T cells, CD19+ B cells, CD14+ monocytes, and CD56+ NK cells.
- For T-cell subsets: Report the CD4+:CD8+ ratio.
- For differentiation: Within CD4+ and CD8+ T cells, identify:
- Naïve (TN): CD45RA+ CCR7+
- Central Memory (TCM): CD45RO+ CCR7+
- Effector Memory (TEM): CD45RO+ CCR7-
- Terminally Differentiated Effector (TE): CD45RA+ CCR7-
Diagram 2: PBMC immunophenotyping analysis workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Tools for PBMC Processing and Quality Assessment
| Reagent / Tool | Function | Example / Note |
|---|---|---|
| Leukapheresis System | Automated collection of white blood cells with high PBMC yield. | Spectra Optia Apheresis System [31] [33]. |
| Density Gradient Medium | Separates PBMCs from other blood components based on density. | Ficoll-Paque Premium [31] [33]. |
| Cell Counter & Viability Analyzer | Provides accurate cell count and viability data. | Vi-CELL BLU or similar automated systems based on trypan blue exclusion [33] [34]. |
| Cryopreservation Medium | Protects cells from ice crystal damage during freezing. | Typically 90% FBS + 10% DMSO [33]. |
| Programmable Freezer | Ensures consistent, controlled cooling rate for optimal cell recovery post-thaw. | Freezing at -1°C/min [33]. |
| Flow Cytometry Panels | Characterizes cell composition, subset ratios, and differentiation states. | Antibodies against CD3, CD4, CD8, CD45RA, CD45RO, CCR7, etc. |
| Cell Activation Reagents | Activates T cells prior to genetic modification and expansion. | Anti-CD3/CD28 antibody-coated magnetic beads [34]. |
| Serum-Free Media | Supports T-cell expansion with defined components, reducing batch variability. | GMP-compliant, xeno-free media [34]. |
| Cytokines | Promotes T-cell survival, proliferation, and influences differentiation during culture. | IL-2, IL-7, and IL-15 [34]. |
Concluding Remarks on Implementation
Integrating a rigorous assessment of the leukapheresis starting material is paramount for successful autologous CAR T-cell research and development. The protocols outlined here for PBMC isolation and quality control provide a framework for standardizing processes across an organization. Standardized procedures for leukapheresis collection, PBMC processing, and cryopreservation help minimize pre-analytical variability [33]. Establishing and monitoring donor eligibility criteria is essential to ensure patient safety and the collection of a viable cellular product [33]. Furthermore, implementing a robust panel of release assays that assess the CQAs described ensures that only starting material meeting predefined specifications proceeds to manufacturing, de-risking the entire production pipeline and enhancing the consistency of the final CAR T-cell therapy [35].
Within the framework of autologous CAR T-cell production research, the initial T-cell activation step is a critical determinant of the final product's phenotypic and functional characteristics. This process transitions T cells from a quiescent to a proliferative state, initiating the expansion phase essential for clinical dosing. The choice of activation method directly influences key performance metrics, including transduction efficiency, expansion fold, and the generation of desirable memory T-cell subsets such as T stem cell memory (TSCM). Current research focuses on refining these methods to improve the efficacy and accessibility of CAR T-cell therapies. This article details established and emerging protocols, providing a comparative analysis of their application in manufacturing pipelines.
Biological Basis of T-Cell Activation
Effective T-cell activation is a cornerstone of successful adoptive T-cell therapy, as it initiates the cellular processes necessary for subsequent genetic modification and massive expansion. This process is not a single signal but a carefully orchestrated sequence of molecular events.
Signaling Pathways
T-cell activation is initiated by two primary signals. Signal 1 is delivered through the T-cell receptor (TCR) upon recognition of its specific antigen. In therapeutic manufacturing, this is typically mimicked using antibodies against the CD3 complex, a key component of the TCR. Signal 1 alone is insufficient and can lead to T-cell anergy. A crucial Signal 2, or co-stimulation, is required for full activation, prevention of anergy, and promotion of T-cell survival and proliferation. The CD28 receptor binding to B7 ligands on antigen-presenting cells is a primary co-stimulatory pathway, and in manufacturing, it is commonly triggered using anti-CD28 antibodies [36] [6].
The intracellular signaling cascades downstream of CD3 and CD28 engagement activate key transcription factors, including NFAT (Nuclear Factor of Activated T-cells), NF-κB (Nuclear Factor kappa-light-chain-enhancer of activated B cells), and AP-1 (Activator Protein 1). This leads to the expression of genes critical for T-cell function, such as IL-2, and the upregulation of activation-induced markers on the cell surface [36].
Key Activation Markers for Monitoring
Following successful activation, T cells rapidly alter their surface phenotype. Key markers used to monitor and quantify activation include:
- CD69: An early activation marker, upregulated within hours of stimulation [37] [38].
- CD25 (IL-2Rα): The alpha chain of the IL-2 receptor, upregulated within 24-48 hours, allowing cells to respond to the proliferative signal of IL-2 [38].
- CD134 (OX40) and CD137 (4-1BB): These are later co-stimulatory markers belonging to the TNF receptor family. Their expression, particularly on CD4+ T cells, is often used to identify antigen-specific T-cell responses and is also incorporated into later-generation CAR constructs for enhanced persistence [37] [39].
The following diagram illustrates the core signaling pathway and the subsequent appearance of key surface markers used for detection.
Established Methods for T-Cell Activation
Current Good Manufacturing Practice (GMP)-compliant methods for T-cell activation primarily rely on surface receptor engagement using antibody-based platforms. The two most common approaches are summarized in the table below and detailed in the subsequent sections.
Table 1: Comparison of Established T-Cell Activation Methods
| Method | Mechanism of Action | Key Advantages | Key Limitations | Typical Co-stimulation |
|---|---|---|---|---|
| Anti-CD3/CD28 Magnetic Beads | Synthetic beads coated with antibodies provide Signals 1 & 2. | Closed system; uniform activation; beads can be actively removed post-activation to prevent over-stimulation [40]. | Higher material cost; requires magnetic separation equipment. | Integrated CD28 antibody on bead surface. |
| Soluble Anti-CD3/CD28 Antibodies | Antibodies added directly to culture media. | Simplicity; low cost; no need for bead removal. | Potential for over-activation and exhaustion; less controlled signal strength. | Requires soluble CD28 antibody, often with cross-linking. |
Anti-CD3/CD28 Magnetic Beads
This method utilizes paramagnetic beads covalently coated with antibodies specific for CD3 and CD28. It is the most widely used platform in clinical CAR-T cell manufacturing due to its reproducibility and effectiveness [40] [6].
The beads function as synthetic antigen-presenting cells, providing a surface for TCR cross-linking (via anti-CD3) and simultaneous co-stimulation (via anti-CD28). This robust signal drives T cells into cycle efficiently. A significant technical advancement is the development of detachable beads. Traditional beads are removed via passive decay, but detachable beads allow for active, on-demand removal using a specific release buffer. This provides greater process control, reduces the risk of bead carry-over into the final product, and minimizes T-cell death due to overactivation and exhaustion [40].
The workflow often integrates bead-based activation with other unit operations. For instance, the CTS Detachable Dynabeads can be used with the CTS DynaCellect Magnetic Separation System for one-step T-cell isolation and activation, followed by active bead release, streamlining the manufacturing process [40].
Soluble Agonist Antibodies
This method involves adding soluble anti-CD3 and anti-CD28 antibodies directly to the culture. To enhance signaling, the anti-CD3 antibody is often immobilized on a surface, such as the culture flask, or used in conjunction with cross-linking secondary antibodies. While simpler and more cost-effective than bead-based methods, it offers less control over signal strength and duration. Continuous exposure to soluble agonists can drive T cells toward a more terminally differentiated effector phenotype and increase the risk of activation-induced cell death [41]. Consequently, this method is more common in research-scale experiments than in current GMP manufacturing for commercial therapies.
Advanced and Emerging Activation Methodologies
Innovation in T-cell activation is directed toward shortening manufacturing timelines, improving product consistency, and enhancing the fitness of the resulting T-cell products.
Accelerated and Bead-Free Protocols
Next-generation workflows are challenging the conventional multi-day activation and expansion paradigm. Research from industry leaders demonstrates the feasibility of a 24-hour lentiviral transduction process. This process leverages one-step isolation and activation with detachable CD3/CD28 beads, followed by rapid lentiviral transduction and active bead removal. The resulting CAR-T cells exhibit a more naive and T stem cell memory (TSCM) phenotype, which is associated with improved persistence and anti-tumor activity in vivo, compared to cells from a standard 7-day process [40].
Concurrently, novel bead-free transduction protocols are being developed. These systems eliminate magnetic beads entirely, instead using reagent mixtures like T Cell TransAct to provide the initial activation signal simultaneously with lentiviral vector addition. This approach significantly streamlines production by removing the bead handling and removal steps, reduces costs, and can achieve high transduction efficiencies (60-80%) while maintaining good cell viability [41].
Optogenetic Control
For high-precision research applications, optogenetic tools offer unprecedented spatiotemporal control over T-cell activation. The Opto-CD28-REACT system is a key example. This platform uses a recombinant protein comprising an anti-CD28 single-chain variable fragment (scFv) fused to a phytochrome-interacting factor (PIF6). This protein binds to the CD28 receptor on non-engineered primary human T cells. Upon illumination with red light (630 nm), PIF6 binds to PhyB tetramer-coated beads, triggering CD28 clustering and signaling. This interaction can be rapidly reversed within minutes by switching to far-red light (780 nm) [36].
When combined with a similar optogenetic tool for the TCR ( opto-CD3ϵ-REACT), this system enables fully reversible, tunable, and independent optical control of both Signal 1 and Signal 2. This allows researchers to dissect the precise contributions of signal timing, duration, and synergy to T-cell fate decisions, providing insights for rational design of future activation strategies [36].
The following workflow diagram compares a traditional process with an advanced, accelerated manufacturing workflow.
Detailed Experimental Protocols
Protocol: T-Cell Activation Using Detachable CD3/CD28 Beads in a 24-Hour Workflow
This protocol is adapted from a published, automated workflow for rapid CAR-T cell manufacturing [40].
Key Reagents and Equipment:
- Quarter Leukopak (starting material)
- CTS Detachable Dynabeads CD3/CD28 (Thermo Fisher Scientific)
- CTS DynaCellect Magnetic Separation System (Thermo Fisher Scientific)
- CTS Rotea Counterflow Centrifugation System (Thermo Fisher Scientific)
- Lentiviral vector (e.g., CD19-CAR, produced using LV-MAX system)
- T-cell culture medium (e.g., TexMACS or X-VIVO 15, supplemented with IL-2)
Procedure:
- Isolation and Activation: Load the leukopak and CTS Detachable Dynabeads onto the CTS DynaCellect System. Perform a one-step procedure to isolate T cells and conjugate them with activation beads.
- Lentiviral Transduction: Harvest the bead-bound T cells and resuspend them in culture medium supplemented with IL-2 (100 IU/mL). Add the lentiviral vector at a low multiplicity of infection (MOI ~2). Incubate the culture for 6-8 hours at 37°C, 5% CO2.
- Active Debeading: Transfer the cell culture back to the CTS DynaCellect System. Add CTS Detachable Dynabeads Release Buffer to actively dissociate and remove the magnetic beads from the T cells.
- Wash and Concentrate: Transfer the bead-free, transduced T cells to the CTS Rotea System. Perform a counterflow centrifugation step to wash the cells and concentrate them to the desired volume for final formulation.
- Formulation: The final cell product can be cryopreserved or administered fresh. Comparative analysis with a 7-day expansion process typically shows a higher proportion of desirable TSCM cells (CD45RA+/CCR7+) in the 24-hour product [40].
Protocol: Simultaneous Activation and Transduction with a Bead-Free Reagent
This protocol outlines a simplified, research-scale method for efficient T-cell engineering without magnetic beads [41].
Key Reagents:
- Human Pan T Cell Isolation Kit (Miltenyi Biotec)
- T Cell TransAct, human (Miltenyi Biotec)
- Lentiviral supernatant (concentrated using Lenti-X Concentrator)
- Primary T-cell culture medium (e.g., RPMI-1640 with 10% FBS and 100 IU/mL IL-2)
Procedure:
- T Cell Isolation: Isolate primary human T cells from PBMCs using a negative selection kit per the manufacturer's instructions.
- Simultaneous Activation/Transduction: Seed the isolated T cells in a culture plate at 1-2 x 10^6 cells/mL. Add T Cell TransAct reagent (at a recommended cell:reagent ratio) and the concentrated lentiviral supernatant directly to the culture simultaneously. Add polybrene (e.g., 5-8 µg/mL) to enhance viral transduction.
- Incubation: Incubate the culture for 24-48 hours at 37°C, 5% CO2. There is no need for spinoculation in this protocol.
- Culture and Expansion: After the initial incubation, carefully remove the culture medium containing the TransAct reagent and lentivirus, and resuspend the cells in fresh culture medium with IL-2. Continue culturing and expanding the cells as needed. Transduction efficiency can be assessed by flow cytometry 72-96 hours post-transduction, typically reaching 60-80% [41].
The Scientist's Toolkit: Essential Reagents and Equipment
Table 2: Key Research Reagent Solutions for T-Cell Activation and Analysis
| Category | Product Example | Function in T-Cell Activation/Expansion |
|---|---|---|
| Activation Reagents | CTS Detachable Dynabeads CD3/CD28 [40] | Provides integrated Signal 1 (CD3) and Signal 2 (CD28) for robust, controllable T-cell activation. Allows for active bead removal. |
| T Cell TransAct [41] | A soluble, bead-free reagent that stimulates T-cell proliferation and activation, ideal for simplified, simultaneous activation/transduction protocols. | |
| Cytokines | Recombinant Human IL-2 [41] | A critical cytokine added to culture media to support T-cell survival, promote proliferation, and prevent activation-induced cell death post-stimulation. |
| Detection Kits | Human Activated T Cell Markers Flow Cytometry Panel [38] | A pre-configured antibody panel (typically CD3, CD4, CD8, CD25, CD69) for simultaneous identification and phenotyping of activated T-cell populations via flow cytometry. |
| Culture Systems | Xuri Cell Expansion System W25 [42] | A wave-motion bioreactor that provides a semi-automated, closed, and scalable system for the expansion of T cells, improving yield and consistency over static culture. |
The initial T-cell activation step is a foundational and highly tunable process in autologous CAR T-cell production. While magnetic beads coated with anti-CD3/CD28 antibodies remain the industry standard for robust and GMP-compliant manufacturing, the field is rapidly evolving. The emergence of accelerated workflows and bead-free activation systems highlights a clear trend toward simplifying processes and enhancing the therapeutic fitness of the final cell product by preserving early memory T-cell phenotypes. Furthermore, sophisticated research tools like optogenetics are providing deep mechanistic insights that will inform the next generation of activation strategies. The continued optimization of this critical first step is paramount to improving the efficacy, safety, and accessibility of CAR T-cell therapies for a broader patient population.
The manufacturing of autologous chimeric antigen receptor (CAR) T-cells represents a cornerstone of modern cancer immunotherapy. A critical determinant in the production workflow is the selection of a gene delivery system, a choice that fundamentally influences the safety, efficacy, cost, and scalability of the resulting cellular therapeutic [43] [6]. Currently, the field is divided between well-established viral vector platforms and emerging non-viral technologies. Viral vectors, particularly lentiviral (LV) and gamma-retroviral (RV) vectors, are characterized by their high transduction efficiency and stable transgene expression, forming the basis for most currently approved CAR T-cell products [43] [44]. In contrast, non-viral systems, primarily the PiggyBac (PB) transposon and CRISPR/Cas9-based genome editing, offer advantages in cargo capacity, cost-effectiveness, and reduced risk of insertional mutagenesis, positioning them as promising alternatives for next-generation therapies [43] [45] [46]. This Application Note provides a structured comparison of these four key genetic engineering platforms within the context of autologous CAR T-cell production, presenting summarized quantitative data, detailed experimental protocols, and essential resource information to guide researchers and drug development professionals.
Comparative Analysis of Engineering Platforms
The selection of a gene delivery system involves trade-offs between efficiency, safety, and practical manufacturing considerations. The table below provides a quantitative comparison of the core characteristics of viral and non-viral platforms.
Table 1: Platform Comparison for CAR T-Cell Engineering
| Feature | Lentiviral (LV) Vector | Retroviral (RV) Vector | PiggyBac (PB) Transposon | CRISPR/Cas9 Knock-in |
|---|---|---|---|---|
| Integration Mechanism | Semi-random integration [43] | Prefers integration into gene promoters [43] | "Cut-and-paste" into TTAA sites [43] [45] | Directed integration via homologous directed repair (HDR) [45] |
| Cargo Capacity | Limited (~8-10 kb) [43] | Limited (~8-10 kb) [43] | Very High (up to 200 kb) [43] [45] | Moderate (depends on delivery method) |
| Transduction/Knock-in Efficiency | High (can reach ~70%) [44] | High [43] | Moderate, but improved with hyperactive mutants [43] [46] | Generally lower than viral; requires optimization [45] |
| Genotoxic Risk | Lower risk compared to RV [43] | Higher risk due to preference for gene promoters [43] | Considered safer, but requires monitoring (e.g., CARTELL trial) [45] | Risk of off-target editing and translocations [45] |
| Manufacturing Cost & Regulation | High cost, stringent regulatory hurdles [43] [45] | High cost, stringent regulatory hurdles [43] | Lower cost, simpler regulatory path [43] [45] | Lower cost, simpler regulatory path [45] |
| Primary Applications | Stable CAR expression in clinical products [6] [44] | Stable CAR expression in clinical products (e.g., Yescarta) [6] | Stable CAR expression with large cargoes [43] [46] | Gene knockout (e.g., PD-1, TCR) and targeted CAR insertion [47] [48] |
The following diagram illustrates the fundamental mechanistic differences in how these platforms integrate genetic material into the T-cell genome, which underlies their distinct safety and performance profiles.
Integration Mechanism Workflow
Detailed Experimental Protocols
Protocol 1: CAR T-Cell Production Using Lentiviral Vector
This protocol is adapted from established methods for clinical-grade CAR T-cell manufacturing [47] [49].
Key Reagents:
- Cells: HEK293T cells (for LV production), Human primary T-cells from leukapheresis.
- Media: RPMI-1640 with 10% FCS (R10) for 293T cells; AIM-V medium with IL-2 and serum replacement for T-cells.
- Plasmids: Transfer plasmid (CAR construct), pTRP gag/pol, pTRP RSV-Rev, pTRP VSVG packaging plasmids.
- Activation: Anti-CD3/CD28 antibodies or beads.
- Special Reagent: BX795 (TBK1/IKKɛ inhibitor) to enhance transduction [49].
Procedure:
- Lentiviral Vector Production (Day -4):
- Plate HEK293T cells in T150 flasks. The next day, transfert cells at 60-70% confluency using a lipofection reagent mixed with the four plasmids.
- Collect the viral supernatant at 24 and 48 hours post-transfection. Pool, concentrate via ultracentrifugation, and resuspend the viral pellet. Aliquot and store at -80°C.
- Determine functional titer (TU/mL) by transducing activated T-cells and measuring CAR+ cells via flow cytometry.
T-Cell Activation and Transduction (Day 0):
- Isolate CD3+ T-cells from PBMCs via negative selection. Activate cells using plate-bound anti-CD3/CD28 antibodies or beads in AIM-V medium supplemented with IL-2 (100 U/mL) and IL-15 (10 ng/mL).
Transduction (Day 1):
- Add the concentrated lentiviral vector and transduction enhancer (e.g., TransPlus) to the activated T-cells. Include BX795 (4 µM) during the transduction to boost efficiency by inhibiting the antiviral response [49].
- After 6 hours, add fresh medium to support cell growth.
Expansion and Harvest (Days 2-14):
- Culture cells, feeding as necessary. Expand cells for 10-14 days, monitoring CAR expression and cell count.
- Harvest and cryopreserve the final CAR T-cell product.
Protocol 2: Multiplexed Genome Engineering using the "One-Shot" CRISPR System
This protocol enables efficient knockout of multiple genes (e.g., TCR, HLA-I, PD-1) concurrently with CAR introduction [48].
Key Reagents:
- Cells: Human primary T-cells.
- Vector: A single lentiviral vector co-expressing the CAR and multiple gRNAs (e.g., targeting TRAC and B2M).
- Nuclease: Cas9 mRNA or eSpCas9(1.1) mRNA for higher fidelity.
- Equipment: Electroporator.
Procedure:
- T-Cell Activation (Day 0): Activate isolated T-cells as described in Protocol 1.
- Lentiviral Transduction (Day 1): Transduce activated T-cells with the "one-shot" CRISPR/CAR lentiviral vector.
- Electroporation with Cas9 mRNA (Day 3): Three days post-transduction, when CAR and gRNA expression is stable, perform a single electroporation to deliver Cas9 mRNA into the cells.
- Expansion and Validation (Days 4-14):
- Expand cells using standard protocols.
- Analyze knockout efficiency via flow cytometry (e.g., loss of CD3 and HLA-I) and sequence potential off-target sites to validate editing precision.
Protocol 3: CAR T-Cell Generation with PiggyBac Transposon System
This protocol uses a non-viral, plasmid-based system for stable CAR integration [43] [46].
Key Reagents:
- Cells: Human primary T-cells.
- Plasmids: Donor plasmid containing the CAR flanked by PB ITRs, and a helper plasmid expressing the hyperactive PB transposase (e.g., hyPBase).
- Equipment: Electroporator.
Procedure:
- T-Cell Activation (Day 0): Activate T-cells as previously described.
- Electroporation (Day 1): Co-electroporate the activated T-cells with the donor and helper plasmids.
- Expansion and Analysis (Days 2-14):
- Culture and expand cells for 13-15 days.
- Monitor CAR expression over time and evaluate the cytotoxic function of the CD19pbCAR T-cells against target cells (e.g., Raji cells) using a standard cytotoxicity assay [46].
The Scientist's Toolkit: Key Research Reagent Solutions
Successful execution of the protocols relies on high-quality, well-characterized reagents. The following table lists essential materials and their critical functions in the CAR T-cell engineering workflow.
Table 2: Essential Reagents for CAR T-Cell Engineering
| Reagent / Solution | Function / Application | Examples / Notes |
|---|---|---|
| Anti-CD3/CD28 Antibodies/Magnetic Beads | In vitro T-cell activation, mimicking APC interaction [44]. | Clone OKT3 (anti-CD3) and CD28.2 (anti-CD28); Dynabeads for clinical scale. |
| Lentiviral Packaging Plasmids | Production of replication-incompetent lentiviral vectors. | Second-generation systems (psPAX2, pMD2.G) for improved safety [47]. |
| Transposase Plasmids | Catalyzes the integration of the transposon-based CAR from donor plasmid. | Hyperactive PiggyBac transposase (hyPBase, bz-hyPBase) for higher efficiency [43] [46]. |
| CRISPR/Cas9 Components | Targeted genome editing for gene knockout or knock-in. | Cas9 mRNA/protein and chemically modified sgRNAs for reduced toxicity and higher efficiency [47] [48]. |
| Cytokines (IL-2, IL-7, IL-15) | Promotes T-cell survival, proliferation, and influences memory phenotype during ex vivo culture. | IL-7/IL-15 favored for generating stem-cell memory and central memory T-cells [47] [49]. |
| Transduction Enhancers | Increases viral or non-viral gene delivery efficiency. | RetroNectin (for RV); BX795 compound (for LV in T-cells) [49]. |
| Selection Markers | Enriches for successfully engineered cells, critical for low-efficiency systems. | Drug resistance (e.g., puromycin) or surface markers (e.g., truncated EGFR) for positive selection [45]. |
The landscape of genetic engineering for autologous CAR T-cell production is rich with options, each with distinct advantages. Lentiviral vectors remain the gold standard for reliable, high-efficiency transduction in approved therapies, while retroviral vectors carry a higher genotoxic risk. The non-viral landscape is rapidly advancing, with the PiggyBac system offering a high-capacity and cost-effective alternative for stable gene delivery, and CRISPR/Cas9 providing unparalleled precision for multiplex gene knockout and targeted integration. The choice of platform is not mutually exclusive; combining non-viral CRISPR editing with viral CAR delivery is a powerful strategy to produce enhanced allogeneic or autologous products. As the field progresses, the refinement of these protocols, particularly in improving the knock-in efficiency of non-viral systems and ensuring their long-term safety, will be paramount to broadening the accessibility and applicability of CAR T-cell therapies.
The ex vivo expansion of autologous chimeric antigen receptor (CAR) T-cells represents a critical and time-intensive phase in the manufacturing of cell therapies. The primary objective is to generate a sufficient therapeutic dose of functionally competent cells, a process that can typically require 7–14 days [50]. The choice of expansion platform and culture conditions directly influences not only the final cell yield and viability but also critical quality attributes (CQAs) such as T-cell phenotype, potency, and persistence in vivo [12] [6]. This document outlines standardized protocols and application notes for the in vitro expansion of CAR-T cells, providing a framework for process development and optimization within a research setting focused on autologous CAR-T production.
Key Experimental Data and Comparative Analysis
Impact of Perfusion Parameters on CAR-T Cell Expansion
Systematic optimization of perfusion processes in stirred-tank bioreactors can significantly intensify CAR-T cell manufacturing. The following table summarizes quantitative findings from a Design of Experiments (DOE) study investigating critical process parameters (CPPs) [50] [51].
Table 1: Effects of Perfusion Parameters on CAR-T Cell Expansion in Stirred-Tank Bioreactors
| Parameter | Levels Tested | Impact on Fold Expansion | Key Findings |
|---|---|---|---|
| Perfusion Start Time | 48, 72, 96 hours post-inoculation | Significant | Earlier initiation (48h) supported higher viability and prevented nutrient depletion, leading to superior growth [50]. |
| Perfusion Rate | 0.25, 0.5, 1.0 VVD* | Most significant factor (3x greater impact than start time) | Higher rates (1.0 VVD) correlated with increased final cell densities. A minimum of 0.85 VVD was recommended for optimal growth [51]. |
| Donor Variability | 3 healthy donors | Significant | Optimal perfusion ranges differed between donors, highlighting the need for adaptive strategies to address patient-specific variability [50] [51]. |
| Overall Outcome | Optimal: 48h start, 1.0 VVD | 4.5-fold improvement in yield vs. fed-batch | Achieved final cell densities of >21 × 10^6 cells/mL and a 50% reduction in time to reach a representative dose [50]. |
*VVD: Vessel Volumes per Day
Comparison of CAR-T Cell Expansion Platforms
Selecting an appropriate expansion system is fundamental to process scalability, control, and final product quality. The table below compares commonly used platforms.
Table 2: Comparison of Platforms for Clinical-Grade CAR-T Cell Expansion
| Expansion Platform | Key Features | Reported Cell Yields | Advantages | Limitations |
|---|---|---|---|---|
| Stirred-Tank Bioreactor (STR) with Perfusion | Controlled parameters (pH, DO), continuous medium exchange [51]. | >21 × 10^6 cells/mL in 7 days [50] [51]. | High level of process control, scalability, supports high cell densities, homogeneous culture [50] [51]. | Higher complexity and cost, risk of filter fouling, requires optimization of multiple parameters [50]. |
| G-Rex (Gas-Permeable Static Culture) | Gas-permeable membrane at base, allowing unlimited oxygen supply [52]. | 20–30 × 10^6 cells/cm² (e.g., 2–3 × 10^9 cells in a 100 cm² device) [52]. | Simplicity, reduced intervention, physiologic environment, low cost [52]. | Limited process monitoring and control, less homogeneous culture compared to STRs [52]. |
| Rocking-Motion Bioreactor | Rocking mechanism for mixing and gas transfer, single-use bags [53]. | More than twice the yield compared to growth without perfusion [51]. | Good scalability, closed system, simpler than STRs [53]. | Mixing and oxygen transfer can be less uniform than in STRs [51]. |
| Static Culture (Flasks/Bags) | Traditional multi-layer flasks or culture bags [12]. | Varies; generally lower than intensified systems. | Low barrier to entry, simple operation [12]. | Labor-intensive, limited scalability, poor process control and monitoring, high risk of contamination [12]. |
Detailed Experimental Protocols
Protocol 1: Intensified CAR-T Cell Expansion in a Perfused Stirred-Tank Bioreactor
This protocol is adapted from studies demonstrating intensified expansion in xeno-free, serum-free (XF/SF) medium using the Ambr 250 High-Throughput Perfusion system [50] [51].
3.1.1 Workflow Overview
3.1.2 Materials and Reagents
- Cells: Activated and CAR-transduced human T-cells.
- Basal Medium: Xeno-free, serum-free medium (e.g., 4Cell Nutri-T GMP) [50].
- Bioreactor System: Ambr 250 High-Throughput Perfusion system or equivalent small-scale stirred-tank bioreactor with an alternative tangential flow (ATF) perfusion device.
- Analytical Instruments: Hemocytometer or automated cell counter, bioanalyzer for metabolite analysis (glucose, lactate), flow cytometer for immunophenotyping.
3.1.3 Step-by-Step Procedure
- Bioreactor Setup and Inoculation: Prepare the bioreactor according to manufacturer instructions. Set control parameters (temperature: 37°C, dissolved oxygen: 50%, pH: 7.2). Inoculate the bioreactor with CAR-T cells at a density of 0.25 × 10^6 cells/mL in XF/SF medium [50].
- Batch Phase (0 - 48 hours): Allow cells to grow in batch mode. Monitor viable cell density (VCD), viability, and metabolite levels (glucose, lactate, glutamine) daily.
- Perfusion Initiation: At 48 hours post-inoculation, initiate the ATF perfusion system. Set the initial perfusion rate to 1.0 VVD using fresh pre-warmed XF/SF medium [50] [51].
- Continuous Culture and Monitoring (Days 3 - 7):
- Maintain perfusion rate. Adjust based on cell growth and metabolic demands if using an adaptive strategy.
- Record VCD and viability daily.
- Monitor and record key metabolites at least once per day to ensure nutrient levels are maintained and waste products are removed.
- Monitor transmembrane pressure of the ATF filter to detect potential fouling [50].
- Harvest: On day 7, or when the target cell density is reached, terminate the culture. Harvest cells and perform final counts and viability assessment. Expected final densities are >21 × 10^6 cells/mL [51].
3.1.4 Quality Control Assessment
- Viability: Should remain >90% throughout the culture [50] [51].
- Phenotype: Analyze harvested cells by flow cytometry for memory (e.g., naïve, central memory) and exhaustion markers (e.g., PD-1). A predominance of naïve/central memory phenotypes is desirable [50].
- Function: Perform in vitro cytotoxicity and cytokine release assays to confirm effector function [50].
Protocol 2: Rapid CAR-T Cell Manufacturing with Reduced Ex Vivo Culture
This protocol outlines a shortened expansion process designed to preserve favorable T-cell phenotypes by minimizing ex vivo culture time [12].
3.2.1 Workflow Overview
3.2.2 Materials and Reagents
- Starting Material: Patient leukapheresis product.
- Activation Reagents: Anti-CD3/CD28 antibodies or other T-cell activation beads.
- Genetic Modification Vector: Lentiviral or retroviral vector encoding the CAR construct.
- Culture Vessels: G-Rex cell culture devices or static culture bags/flasks.
3.2.3 Step-by-Step Procedure
- T-cell Selection and Activation: Isolate T-cells from the leukapheresis product using Ficoll gradient or magnetic bead-based selection. Activate T-cells using anti-CD3/CD28 antibodies for 24 hours [12] [6].
- Genetic Modification: Transduce activated T-cells with the CAR-encoding viral vector. This step is often performed 24-48 hours post-activation.
- Abbreviated Expansion: Transfer transduced cells to the final expansion platform (e.g., G-Rex, culture bags). Culture for a shortened duration of 3 to 5 days [12].
- Maintain cultures at 37°C, 5% CO2.
- Supplement media with IL-2 or other cytokines as required.
- Harvest and Formulation: Harvest cells on day 3-5. Perform final cell count and viability checks. Formulate the final product for fresh infusion or cryopreservation.
3.2.4 Quality Control Assessment
- Phenotype: Flow cytometric analysis should reveal a product enriched in stem cell memory (TSCM) and central memory (TCM) phenotypes, which are associated with improved in vivo persistence and efficacy [12].
- Potency: Conduct a potency assay, such as an antigen-specific cytotoxic T-lymphocyte (CTL) assay, to confirm functionality.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials critical for successful CAR-T cell expansion, as featured in the cited research.
Table 3: Research Reagent Solutions for CAR-T Cell Expansion
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| Xeno-Free/Serum-Free Medium | Provides defined, animal-component-free nutrients for cell growth, reducing variability and safety concerns [50]. | 4Cell Nutri-T GMP medium [50]. |
| Stirred-Tank Bioreactor System with Perfusion | Scalable platform for high-density cell culture with precise control over environmental parameters and feeding strategies [50] [51]. | Ambr 250 High-Throughput Perfusion system [50] [51]. |
| ATF (Alternative Tangential Flow) System | Cell retention device for perfusion processes, enabling continuous medium exchange while retaining cells in the bioreactor [50]. | Integrated component of perfusion bioreactor systems [50]. |
| G-Rex Cell Culture Platform | Static culture vessel with a gas-permeable membrane for simplified, high-yield expansion without active oxygenation [52]. | Enables high cell densities (e.g., 2–3 × 10^9 cells in a 100 cm² device) with minimal intervention [52]. |
| T-cell Activation Reagents | Stimulates T-cells to enter the cell cycle, a prerequisite for efficient genetic modification and subsequent expansion [6]. | Anti-CD3 and anti-CD28 antibodies, often used conjugated to magnetic beads [6]. |
| Cytokines | Supports T-cell survival, proliferation, and can influence differentiation during expansion [12]. | Interleukin-2 (IL-2) is commonly used [12]. |
Product Formulation, Cryopreservation, and Release Testing Criteria
The production of autologous chimeric antigen receptor (CAR) T-cell therapies is a multi-step process that bridges immunology, gene therapy, and advanced cell manufacturing. A patient's T-cells are genetically engineered to express CARs that enable specific recognition and elimination of cancer cells [54] [55]. The formulation, cryopreservation, and release testing of these cellular products represent critical determinants of both clinical safety and efficacy. Within the broader context of autologous CAR T-cell production research, optimizing these downstream processes is essential for ensuring consistent product quality, maintaining cell viability and function, and ultimately enabling successful clinical outcomes for patients with hematological malignancies and, increasingly, autoimmune disorders [56] [57]. This document outlines detailed application notes and protocols for these crucial manufacturing stages.
Product Formulation and Cryopreservation
Product formulation and cryopreservation are vital for preserving CAR T-cell viability and function from the end of manufacturing until patient infusion. The formulation must protect cells from the stresses of freezing and thawing, while cryopreservation enables necessary quality control testing, logistical coordination, and long-term storage.
Key Components of Cryopreservation Formulations
Cryopreservation media are specifically formulated to mitigate ice crystal formation, which can physically damage cell membranes and lead to apoptosis. The core components function as follows:
- Cryoprotectants: Dimethyl sulfoxide (DMSO) is the most widely used cryoprotectant. It functions by disrupting hydrogen bonding between water molecules, thereby lowering the freezing point and reducing intracellular ice crystal formation. DMSO also interacts with lipid bilayers to stabilize cell membranes during freezing [58].
- Supplements: Formulations are typically supplemented with human AB serum or albumin, which provides proteins that further stabilize cell membranes and provide essential nutrients during the critical post-thaw recovery phase [59].
- Base Medium: A balanced salt solution, such as AIM-V, serves as the foundation, providing an isotonic environment with essential ions and buffers [59].
Optimized Cryopreservation and Thawing Protocol
The following protocol is adapted from industry and academic best practices for CAR T-cell products [58] [59].
Materials:
- Cryopreservation medium (e.g., containing 10% DMSO, human AB serum, and base medium)
- Controlled-rate freezer
- Liquid nitrogen storage tank
- 37°C water bath
- Pre-warmed wash medium (e.g., AIM-V with 5-10% human AB serum)
Procedure:
- Formulation: After final expansion and harvesting, concentrate CAR T-cells and resuspend them in pre-chilled (2-8°C) cryopreservation medium. A target cell concentration and final DMSO concentration of 10% are standard.
- Controlled-Rate Freezing: Transfer the formulated product to cryogenic vials or infusion bags. Use a controlled-rate freezer with a validated freezing curve. A typical protocol involves cooling at -1°C per minute to -40°C, followed by a rapid drop to -80°C to -120°C before transfer to long-term liquid nitrogen storage.
- Thawing: When ready for infusion, rapidly thaw the cryopreserved vial or bag in a 37°C water bath until only a small ice crystal remains.
- Dilution and Washing: Immediately after thawing, dilute the cell product drop-wise with pre-warmed wash medium to reduce DMSO toxicity. Perform a gentle wash via counterflow centrifugation to remove cryoprotectant and cellular debris.
- Final Formulation: Resuspend the washed cell pellet in an appropriate infusion solution, such as 0.9% sodium chloride with human albumin.
The diagram below illustrates the logical workflow and key decision points in the cryopreservation and thawing process.
Impact of Cryopreservation on CAR T-Cell Products
Research indicates that while fresh CAR T-cell infusion products may exhibit higher in vitro anti-tumor reactivity, cryopreserved products remain highly potent and viable for clinical use. A head-to-head analysis within the same patients showed that cryopreserved CAR T-cells still possessed high anti-tumor specificity and led to complete clinical remissions [59]. Phenotypic differences have been observed, with fresh products expressing more of the exhaustion marker TIM-3, though the clinical significance of this finding is not fully established [59].
Release Testing Criteria
Before a CAR T-cell product can be released for patient infusion, it must pass a stringent panel of quality control tests. These release criteria are designed to ensure product safety, identity, purity, potency, and viability.
Consensus Release Specifications
The following table summarizes the key release tests and their typical acceptance criteria based on consensus recommendations from organizations like the UNITC consortium and FDA guidance [60] [57].
Table 1: Essential Release Tests and Acceptance Criteria for Autologous CAR T-Cell Products
| Test Category | Specific Test | Typical Acceptance Criteria | Rationale & Notes |
|---|---|---|---|
| Viability | Viability (e.g., Trypan blue) | ≥ 70% - 80% [60] | Critical for ensuring a sufficient dose of functional cells. A limit of ≥70% is supported by clinical outcome data [60]. |
| Safety | Sterility (Bacterial/Fungal) | No growth [57] | Ensures the product is free from microbial contamination. Interim results from process testing may allow for earlier release [57]. |
| Mycoplasma | Not detected [57] | ||
| Endotoxin | < 5 EU/kg/hr [57] | ||
| Replication-Competent Virus (RCV) | Not detected [57] | Critical safety test for genetically modified products. | |
| Identity | CAR Transgene Expression (e.g., flow cytometry) | Confirmation of CAR identity [57] | Verifies the product is the intended CAR T-cell therapy. |
| Potency | In vitro cytotoxicity or cytokine release | Meets preset specifications [57] | Demonstrates biological function. A validated potency assay is a major regulatory challenge. |
| Dosage | Total Viable Cell Count & Transduced Cell Count | Dose within protocol-specified range [57] | Ensures the patient receives a therapeutically effective cell number. |
| Purity | VCN (Vector Copy Number) | Within specified limit [57] | Ensures consistent genetic modification and assesses theoretical genotoxicity risk. |
The Release Testing Workflow and Timeline
Minimizing the "vein-to-vein" time is crucial for patient outcomes, and release testing is often a rate-limiting step. To address this, a paradigm of initial and final certification has been proposed, particularly for fresh products [57]. This workflow and its associated timelines are visualized below.
Clinical Evidence for Viability Criteria
The standard 80% viability release specification has been critically examined through clinical outcomes research. A landmark retrospective study of 123 pediatric patients with Acute Lymphoblastic Leukemia (ALL) and 25 adults with Diffuse Large B-Cell Lymphoma (DLBCL) treated with tisagenlecleucel (CTL019) found no statistically significant association between product viability (below vs. above 80%) and complete response rate, in vivo CAR T-cell expansion, progression-free survival, or overall survival [60]. Based on this clinical data, the authors suggested that a viability release criterion of at least 70% could be justified, advocating for criteria driven by demonstrated effect on clinical outcomes rather than arbitrary benchmarks [60].
Detailed Experimental Protocols
Protocol for Viability and Cell Count Assessment
This is a fundamental release test performed on the final drug product before cryopreservation or infusion.
Materials:
- Hemocytometer or automated cell counter (e.g., NC-200)
- Trypan blue solution (0.4%) or dual-fluorescence viability dyes
- Phosphate Buffered Saline (PBS)
- Microcentrifuge tubes
Procedure:
- Sample Preparation: If the product is cryopreserved, thaw and wash cells as per the protocol in Section 2.2. For a fresh product, obtain a representative sample. Dilute the cell suspension as needed in PBS to achieve a concentration suitable for counting.
- Staining: Mix 10 µL of the cell suspension with 10 µL of Trypan blue solution. Incubate for 1-2 minutes at room temperature. (For automated counters, follow manufacturer-specific staining protocols).
- Counting and Calculation:
- Load the mixture onto a hemocytometer.
- Count the total number of cells and the number of blue-stained (non-viable) cells in a predefined volume.
- Viability (%) = (Number of viable cells / Total number of cells) × 100.
- Total Viable Cell Count = (Viable cell concentration) × (Total product volume).
Protocol for In Vitro Potency Assay (Cytokine Release)
Potency assays measure the biological activity of CAR T-cells. A cytokine release assay is a commonly used method.
Materials:
- Target cells expressing the cognate antigen (e.g., CD19+ Nalm-6 cells)
- Control cells not expressing the antigen
- Culture medium (e.g., RPMI-1640 with 10% FBS)
- 96-well U-bottom plate
- Human IFN-γ ELISA kit
Procedure:
- Co-culture Setup: Harvest and wash the CAR T-cell final product. Seed effector (CAR T) cells and target cells in the 96-well plate at a standardized effector-to-target (E:T) ratio (e.g., 1:1). Include controls: CAR T-cells alone, target cells alone, and CAR T-cells with control target cells.
- Incubation: Incubate the plate for 18-24 hours at 37°C and 5% CO₂.
- Cytokine Measurement: Centrifuge the plate and collect the supernatant. Quantify the concentration of IFN-γ (or other relevant cytokines like IL-2) in the supernatant using a commercial ELISA kit, following the manufacturer's instructions.
- Data Analysis: The potency is demonstrated by a significant, antigen-specific release of cytokine in the test well compared to all control wells.
The Scientist's Toolkit: Key Reagents and Solutions
Table 2: Essential Research Reagents for CAR T-Cell Production and Testing
| Reagent / Solution | Function | Example Product / Component |
|---|---|---|
| T-Cell Activation Beads | Isolates and activates T-cells from PBMCs via CD3/CD28 engagement, initiating proliferation. | Gibco CTS Detachable Dynabeads CD3/CD28 [61] |
| Cell Culture Media | Provides nutrients and environment for ex vivo T-cell expansion. | AIM-V Medium, supplemented with IL-2 and human AB serum [59] |
| Gene Delivery Vector | Mediates stable integration of the CAR transgene into the T-cell genome. | Retroviral or lentiviral vector supernatant [59] |
| Transduction Enhancer | Increases transduction efficiency by co-localizing viral vectors and target cells. | RetroNectin [59] |
| Cryopreservation Medium | Protects cells from freeze-thaw damage, ensuring high post-thaw viability. | Formulation with DMSO and protein supplements [58] |
| Cell Processing System | Automates closed-system steps like bead removal and cell concentration, reducing variability. | Gibco CTS DynaClect System; CTS Rotea System [61] |
Overcoming Hurdles: Strategies to Enhance Product Quality, Potency, and Scalability
T-cell exhaustion presents a significant barrier to effective and durable autologous chimeric antigen receptor (CAR) T-cell therapies. This dysfunctional state, induced by persistent antigen exposure in the tumor microenvironment (TME), is characterized by progressive loss of effector functions, altered metabolism, and sustained expression of multiple inhibitory receptors (IRs) [62]. In CAR T-cell production, exhaustion compromises critical therapeutic metrics including in vivo expansion, persistence, and tumoricidal activity [63]. The phenotypic and functional integrity of the final CAR T-cell product is intrinsically linked to manufacturing processes, making the understanding and mitigation of exhaustion a central focus in bioprocess development [6]. This application note details the defining markers of T-cell exhaustion and provides validated protocols to quantify this state and engineer products with enhanced durability for research and drug development.
Phenotypic and Molecular Markers of T-Cell Exhaustion
Exhausted T cells (T_EXH) possess a distinct identity separate from functional effector and memory subsets. Recognition of these markers is essential for quality control during CAR T-cell manufacturing.
Core Inhibitory Receptors
The most recognized feature of T_EXH is the co-expression of multiple IRs. The expression density and combination of these receptors often correlate with the severity of the dysfunctional state [62].
- Programmed Cell Death 1 (PD-1): A cornerstone IR that dampens T-cell receptor (TCR) signaling upon binding to its ligands PD-L1/PD-L2. PD-1 is transiently expressed on activated T cells but becomes sustained in exhaustion. Its intracellular domain contains an immunoreceptor tyrosine-based switch motif (ITSM) that recruits phosphatases SHP1/SHP2 to negatively regulate PI3K/AKT and RAS signaling pathways [62].
- Cytotoxic T-Lymphocyte-Associated Protein 4 (CTLA-4): Predominantly regulates early T-cell activation by competing with CD28 for CD80/CD86 ligands with higher affinity. CTLA-4 signaling can also mediate trans-endocytosis of these ligands from antigen-presenting cells, further limiting T-cell activation [62].
- T cell Immunoreceptor with Ig and ITIM domains (TIGIT): An IR that shares ligands (CD155/CD112) with the costimulatory receptor CD226. TIGIT engagement inhibits T and NK cell antitumor responses by outcompeting CD226 and directly disrupting its homodimerization. TIGIT's cytoplasmic tail contains an immunoglobulin tail tyrosine (ITT)-like phosphorylation motif and an ITIM [62].
- Additional Markers: Exhausted populations are also frequently enriched for Tim-3, LAG-3, CD160, 2B4, CD39, and CD352 [64] [62] [65].
Transcriptional and Functional Hallmarks
Beyond surface markers, T_EXH are defined by a unique transcriptional and functional profile.
- Transcriptional Regulation: Exhausted T cells exhibit a transcriptional program marked by low TCF1 and high expression of Eomes, TOX, and Blimp1 [64] [62]. A subset with an intermediate level of PD-1 and high T-bet retains some proliferative capacity and cytokine secretion, while a more terminally exhausted subset with high PD-1 and Eomes exhibits severe dysfunction [62].
- Functional Impairment: A hierarchical loss of function is characteristic, beginning with reduced IL-2 and TNFα production, followed by impaired IFNγ secretion, and ultimately a complete loss of cytotoxic degranulation and proliferative capacity [62].
- Metabolic Alterations: T_EXH display a metabolically quiescent profile with impaired mitochondrial biogenesis and fatty acid oxidation, shifting away from the metabolic flexibility of memory T cells [6].
Table 1: Key Phenotypic Markers of T-Cell Exhaustion
| Marker Category | Specific Marker | Expression/Function in T_EXH | Detection Method |
|---|---|---|---|
| Inhibitory Receptors | PD-1 (CD279) | Sustained high expression; transduces inhibitory signals via SHP1/SHP2 [62]. | Flow Cytometry |
| CTLA-4 (CD152) | Competes with CD28; mediates trans-endocytosis of CD80/CD86 [62]. | Flow Cytometry | |
| TIGIT | Binds CD155/CD112; inhibits CD226 costimulation [62]. | Flow Cytometry | |
| Tim-3, LAG-3 | Often co-expressed with PD-1; marks severely exhausted subsets [62] [65]. | Flow Cytometry | |
| Transcription Factors | TOX | High expression drives exhaustion program [64]. | qPCR, Western Blot |
| Eomes | High expression associated with terminal exhaustion [62]. | qPCR, Western Blot | |
| TCF1 (TCF7) | Low expression; loss of memory/stem-like potential [64] [62]. | qPCR, Western Blot | |
| Functional Markers | CD39 (ENTPD1) | Ectoenzyme associated with chronic activation and immunosuppression [64]. | Flow Cytometry |
| CD45RA/RO | Skewed distribution; terminal effectors often re-express CD45RA [63]. | Flow Cytometry |
Diagram 1: The T-Cell Exhaustion Pathway. Chronic stimulation in the TME initiates a transcriptional program leading to phenotypic and functional changes that ultimately impair CAR-T cell persistence and therapeutic efficacy.
Strategies to Improve T-Cell Persistence in Manufacturing
Overcoming exhaustion requires integrated strategies throughout the CAR T-cell manufacturing workflow, from starting material selection to final product formulation.
Starting Material and Culture Optimization
The initial T-cell population and its ex vivo manipulation profoundly impact the product's differentiation state and persistence potential.
- T-Cell Subset Selection: Products enriched for less differentiated subsets like naive (TN), stem cell memory (TSCM), and central memory (TCM) T cells are associated with superior in vivo expansion and longevity compared to those derived from effector memory (TEM) or terminally differentiated T cells [63] [6]. These subsets are characterized by surface expression of CD62L, CCR7, and CD28 [63].
- Defined CD4:CD8 Ratios: Adopting a defined ratio of CD4+ and CD8+ T cells, rather than using an unselected mix, can produce more consistent and potent products. Some clinical-grade processes manufacture CD4+ and CD8+ cells separately before admixing, ensuring a precise ratio that promotes synergistic antitumor activity [6].
- Cytokine Manipulation: Replacing or supplementing the pro-differentiation cytokine IL-2 with cytokines that support memory formation, such as IL-7, IL-15, and IL-21, during ex vivo expansion can help maintain a less differentiated, more persistent phenotype [63].
- Rapid Manufacturing Protocols: Shortening the ex vivo culture duration from several weeks to as little as 1-3 days minimizes time-induced differentiation and exhaustion. These "reduce-duration" or "no-expansion" protocols have been shown to significantly improve the memory phenotype and in vivo function of the final CAR T-cell product [12].
Pharmacologic and Genetic Interventions
Direct targeting of exhaustion pathways can reinvigorate T-cell function.
- Combined Checkpoint Blockade: In vitro blockade of multiple IRs during manufacturing or post-infusion can reverse exhaustion. For example, combined inhibition of PD-1 and IL-6 was shown to substantially enhance the effector function of CD8+ T cells from NSCLC patients and inhibit tumor growth in mouse models [64]. Similarly, combinatorial blockade of PD-1 and Tim-3 restored viral suppression in CD8+ T cells from HIV patients [65].
- Genetic Engineering: Knocking out genes for inhibitory receptors like PD-1 using CRISPR/Cas9 or engineering T cells to express dominant-negative receptors can produce CAR T-cells resistant to exhaustion signals in the TME [66].
Table 2: Strategies to Enhance CAR-T Cell Persistence
| Strategy Category | Specific Approach | Mechanism of Action | Application in Manufacturing |
|---|---|---|---|
| Starting Material | Selection of TN/TSCM subsets | Harnesses inherent longevity and proliferative capacity of less differentiated cells [63]. | Magnetic/fluorescence-activated cell sorting prior to activation. |
| Defined CD4:CD8 Ratio | Ensures optimal CD4+ help for CD8+ persistence and function [6]. | Separate isolation and culture, followed by final product admixing. | |
| Culture Optimization | Cytokine Cocktails (IL-7/IL-15) | Promotes memory-like phenotype over terminal effector differentiation [63]. | Use in culture media during ex vivo expansion. |
| Shortened Culture (≤3-9 days) | Limits time-induced differentiation and exhaustion [12]. | "Rapid" or "next-day" manufacturing platforms. | |
| Pharmacologic | Combined Checkpoint Blockade (e.g., αPD-1 + αIL-6) | Reverses established exhaustion pathways and restores function [64]. | Add to culture media or as adjunct therapy post-infusion. |
| Genetic | Knockout of IRs (e.g., PD-1) | Generates exhaustion-resistant CAR-T cells [66]. | CRISPR/TALEN engineering during manufacturing. |
Experimental Protocols
Protocol 1: Flow Cytometric Analysis of T-Cell Exhaustion Phenotype
This protocol details a method to characterize the exhaustion phenotype in human T-cell or CAR T-cell cultures, adapted from foundational research [64] [65].
1. Sample Preparation:
- Prepare single-cell suspensions from in vitro cultures, leukapheresis samples, or tumor tissues. For tissues, mechanically dissociate and filter through a 70-µm cell strainer.
- Wash cells with cold FACS buffer (PBS + 2% FBS). Count cells and aliquot 1 × 10^6 cells per staining tube.
2. Surface Staining:
- Re-suspend cell pellet in 100 µL of FACS buffer.
- Add the pre-titrated antibody cocktail for surface markers. A typical panel for exhaustion may include: anti-CD3, CD8, CD45RA, CCR7, PD-1, Tim-3, TIGIT, LAG-3.
- Vortex gently and incubate for 30 minutes at room temperature (RT) in the dark.
- Wash cells twice with 2 mL of FACS buffer. Centrifuge at 500 × g for 5 minutes.
3. Viability Staining (Optional):
- Re-suspend cell pellet in 100 µL of FACS buffer containing a viability dye (e.g., Zombie Aqua). Incubate for 15-20 minutes at RT in the dark. Wash twice.
4. Intracellular Staining (for transcription factors):
- For intracellular targets (e.g., Eomes, TOX), fix and permeabilize cells using the Foxp3 / Transcription Factor Staining Buffer Set per manufacturer's instructions.
- After permeabilization, incubate cells with fluorochrome-conjugated antibodies against the target transcription factors for 30-60 minutes at RT in the dark.
- Wash twice with permeabilization buffer, then once with FACS buffer.
5. Data Acquisition and Analysis:
- Re-suspend cells in FACS buffer and acquire data on a flow cytometer.
- Analyze data using FlowJo or similar software. Gate on live, single CD3+CD8+ (or CAR+) cells. Exhaustion is assessed by the co-expression of multiple IRs (e.g., PD-1+Tim-3+TIGIT+).
Protocol 2: Functional Assessment via Cytokine Secretion Assay
This protocol measures the functional capacity of T cells, which is hierarchically lost in exhaustion [64] [62].
1. Cell Stimulation:
- Re-suspend prepared cells at 1 × 10^6 cells/mL in complete RPMI-1640 medium.
- Seed cells in a 12-well plate and stimulate with PMA (phorbol 12-myristate 13-acetate) / Ionomycin at a concentration of 2 µL/mL. Include a protein transport inhibitor (e.g., Brefeldin A) in the culture.
- Incubate for 6 hours at 37°C in 5% CO_2.
2. Cell Staining:
- Harvest cells and perform surface staining as described in Protocol 1.
- Fix and permeabilize cells using the Foxp3 / Transcription Factor Staining Buffer Set or a dedicated intracellular staining kit.
- Stain intracellular cytokines with antibodies against IFNγ, TNFα, and IL-2 for 30-60 minutes at RT in the dark.
- Wash and acquire data on a flow cytometer.
3. Data Interpretation:
- Functionally competent T cells will produce high levels of all three cytokines.
- Exhausted T cells will show a hierarchical loss, typically with preserved IFNγ but significantly reduced or absent TNFα and IL-2.
Protocol 3: In Vitro Checkpoint Blockade Reinvigoration Assay
This protocol tests the potential of checkpoint blockade to restore T-cell function [64].
1. Experimental Setup:
- Isolate T cells from a model system (e.g., tumor-infiltrating lymphocytes, chronically stimulated co-culture) or use expanded CAR-T cells.
- Seed cells in the presence of target cells (e.g., tumor cells expressing the target antigen).
- Add blocking antibodies against inhibitory pathways. For example:
- Experimental Group 1: Anti-PD-1 antibody (e.g., 10 µg/mL)
- Experimental Group 2: Anti-IL-6 antibody (e.g., 10 µg/mL)
- Experimental Group 3: Combined anti-PD-1 + anti-IL-6
- Control Group: Isotype control antibody.
2. Co-culture and Readout:
- Co-culture for 24-96 hours.
- Assess functional reinvigoration using one or more of the following readouts:
- Cytokine Release: Measure IFNγ in supernatant by ELISA or CBA.
- Cytotoxicity: Measure specific lysis of target cells using a real-time impedance-based analyzer (e.g., xCelligence) or standard chromium-release assay.
- Proliferation: Use CFSE dilution or Ki-67 staining to assess T-cell expansion.
Diagram 2: Integrated Experimental Workflow for Addressing T-Cell Exhaustion. A quality-controlled manufacturing process incorporating exhaustion phenotyping, functional assessment, and targeted reinvigoration strategies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for T-Cell Exhaustion Research
| Reagent Category | Specific Example | Function/Application | Key Considerations |
|---|---|---|---|
| Flow Cytometry Antibodies | Anti-human PD-1, Tim-3, LAG-3, TIGIT | Phenotypic characterization of exhausted T-cell subsets [64] [65]. | Titrate for optimal signal-to-noise; check fluorochrome compatibility. |
| Anti-human CD3, CD8, CD45RA, CCR7 | Defining T-cell differentiation stages (TN, TCM, T_EM) [63]. | Essential for gating and subset analysis. | |
| Anti-human IFNγ, TNFα, IL-2 | Intracellular staining for functional assessment [64]. | Requires cell stimulation and permeabilization. | |
| Cell Activation/Stimulation | PMA / Ionomycin | Strong polyclonal stimulators for functional cytokine assays [64]. | Can induce atypical signaling; use at recommended concentrations. |
| Cell Activation Beads (anti-CD3/CD28) | Mimic antigen-specific activation during manufacturing [6]. | Bead-to-cell ratio is critical for optimal activation. | |
| Cell Culture Cytokines | Recombinant IL-2 | Promotes T-cell expansion; can drive effector differentiation [63]. | |
| Recombinant IL-7 / IL-15 | Supports survival and maintenance of memory-like phenotypes [63]. | Preferred for generating persistent products. | |
| Checkpoint Blockers | Anti-PD-1, Anti-CTLA-4 blocking antibodies | In vitro reinvigoration of exhausted T cells [64] [62]. | Use validated functional-grade antibodies. |
| Cell Isolation Kits | CD4+ / CD8+ T Cell Isolation Kits | Magnetic separation for defined starting populations [6]. | Impacts purity and final product composition. |
Autologous chimeric antigen receptor (CAR) T-cell therapy faces a critical challenge: the quality of a patient’s starting T cells significantly impacts manufacturing success and clinical outcomes. T-cell fitness—influenced by disease history, prior therapies, and patient-specific factors—directly affects CAR-T product phenotype, persistence, and efficacy [6]. This Application Note synthesizes current evidence and protocols to quantify T-cell fitness, mitigate variability, and standardize manufacturing for robust CAR-T production.
Quantitative Impact of Patient Factors on CAR-T Product Quality
Patient-specific variables correlate with critical quality attributes (CQAs) of CAR-T products, such as expansion capacity, persistence, and safety. The table below summarizes key relationships derived from clinical and manufacturing data [6] [67]:
Table 1: Patient Factors and Their Impact on CAR-T Product Variability
| Patient Factor | Impact on T-Cell Fitness | Effect on CAR-T Product CQAs | Supporting Data |
|---|---|---|---|
| Prior Lymphotoxic Therapies (e.g., chemotherapies) | Reduced T-cell yield from apheresis; increased exhausted (TEXH) and senescent subsets | Lower expansion potential (<50% in heavily pretreated patients); shorter persistence (in vivo half-life < 30 days) | Correlation with CD4+:CD8+ ratio shifts and memory cell depletion [6] |
| Disease Type & Burden | High tumor burden in hematologic malignancies depletes naive T cells (TN) and stem-cell memory T cells (TSCM) | Impaired cytotoxic activity; increased risk of cytokine release syndrome (CRS)/ICANS | 30–50% reduction in TSCM pools in late-stage patients [6] |
| Age & Comorbidities | Age-related immunosenescence; reduced telomere length and proliferative capacity | Slower ex vivo expansion; lower peak CAR-T levels post-infusion (Cmax < 10,000 copies/μg DNA) [67] | 40% longer doubling time in patients >65 years [6] |
| Prior Exposure to BCMA-/CD19-Targeted Agents | Antigen-specific T-cell exhaustion; downregulation of targetable epitopes | Reduced CAR-T persistence (t1/2 < 15 days); antigen-negative relapse [67] | Flow cytometry shows >60% PD-1+/TIM-3+ T cells in pre-manufacturing apheresis [6] |
Experimental Protocols for Assessing T-Cell Fitness
Standardized pre-manufacturing screening is essential to predict CAR-T product quality. The following protocols enable quantitative assessment of T-cell fitness:
Pre-Manufacturing T-Cell Phenotyping by Flow Cytometry
Objective: Quantify memory, naive, and exhausted T-cell subsets in apheresis material. Reagents:
- Antibody Panel: Anti-CD3/CD4/CD8/CD45RA/CCR7/PD-1/TIM-3/LAG-3.
- Viability Stain: 7-AAD or propidium iodide.
- CAR Detection Reagent: FMC63-based anti-idiotype antibody for CD19-CAR constructs [67].
Procedure:
- Isolate PBMCs from apheresis via Ficoll gradient centrifugation.
- Stain 1 × 106 cells with antibody cocktail (30 min, 4°C).
- Acquire data on a flow cytometer (e.g., BD Symphony) and analyze using FCS Express or FlowJo.
- Calculate ratios:
- TSCM = CD45RA+CCR7+CD95+
- Exhaustion Index = (PD-1+ + TIM-3+) / CD3+
Quality Thresholds: TSCM >15% correlates with superior persistence; Exhaustion Index <0.3 predicts optimal expansion [6].
qPCR/ddPCR for CAR Transgene Copy Number
Objective: Monitor CAR-T expansion and persistence in vivo post-infusion. Reagents:
- Primers/Probes: CAR-specific sequences (e.g., FMC63 scFv for CD19-CAR).
- Standard Curve: Serial dilutions of plasmid encoding CAR transgene.
- Template DNA: Isolated from patient whole blood (days 7, 14, 28 post-infusion) [67].
Procedure:
- Extract DNA from 200 μL blood using QIAamp DNA Blood Mini Kit.
- Run qPCR/ddPCR with CAR-specific assays (40 cycles).
- Calculate transgene copies/μg DNA using the standard curve.
- Report Cmax (peak expansion), Tmax (time to peak), and AUC0–28 days (area under the curve) [67].
Table 2: Key Pharmacokinetic Parameters for CAR-T Monitoring
| Parameter | Optimal Range | Clinical Significance |
|---|---|---|
| Cmax | >50,000 copies/μg DNA | Correlates with tumor response [67] |
| Tmax | 7–14 days | Delayed peaks indicate poor expansion |
| AUC0–28 days | >1 × 106 copy-days/μg DNA | Predicts long-term persistence |
| t1/2 | >30 days | Associated with durable remission |
Mitigation Strategies for High-Risk Patients
For patients with compromised T-cell fitness, process adaptations can rescue product quality:
T-Cell Selection and Enrichment:
- Use CD4/CD8 magnetic bead separation to control CD4:CD8 ratios (e.g., liso-cel process) [6].
- Deplete CD25+ Treg cells to enhance antitumor activity.
Cytokine Supplementation:
- Add IL-7/IL-15 during ex vivo expansion to promote TSCM phenotype [6].
Process Modifications:
Visualizing the Manufacturing Workflow and Critical Control Points
The diagram below maps the CAR-T manufacturing process, highlighting steps where patient-specific variability impacts product quality and where interventions can be applied:
The Scientist’s Toolkit: Essential Reagents and Technologies
Table 3: Key Research Reagent Solutions for CAR-T Development
| Reagent/Technology | Function | Example Application |
|---|---|---|
| Anti-idiotype Antibodies (e.g., FMC63) | Detect CAR expression by flow cytometry | Monitoring CAR-T persistence in patient blood [67] |
| Lentiviral/Viral Vectors | Deliver CAR transgene | Engineering CD19- or BCMA-targeting CAR-T cells [6] |
| Magnetic Cell Separation Beads | Isulate CD4+/CD8+ subsets | Control T-cell composition in starting material [6] |
| Cytokine Cocktails (IL-2, IL-7, IL-15) | Enhance T-cell expansion and memory phenotype | Improving TSCM generation during manufacturing [6] |
| qPCR/ddPCR Assays | Quantify CAR transgene copies | Pharmacokinetic analysis of CAR-T products [67] |
Managing patient-derived variability in autologous CAR-T manufacturing requires integrated strategies: rigorous pre-manufacturing screening, process adaptations for high-risk patients, and standardized monitoring of critical quality attributes. Implementing these protocols enhances product consistency and clinical success, advancing the broader thesis of robust, scalable CAR-T production.
The efficacy of autologous chimeric antigen receptor T-cell (CAR-T) therapy is profoundly influenced by the composition and differentiation state of the T-cell subsets infused back into the patient. A growing body of evidence indicates that less differentiated T-cell populations—specifically naive T cells (TN) and stem cell memory T cells (TSCM)—possess superior engraftment potential, proliferative capacity, and persistence in vivo compared to their more differentiated effector counterparts [70] [71]. Furthermore, the CD4+/CD8+ ratio within the final CAR-T product is emerging as a critical determinant of synergistic anti-tumor activity and long-term functional persistence [70] [72]. Within the context of autologous CAR-T production, where starting material is inherently variable due to patient-specific factors like prior treatments and age, actively steering the manufacturing process to enrich for these favorable subsets is a key strategy to overcome variability and enhance clinical outcomes. This Application Note provides a detailed framework for the identification, monitoring, and optimization of these critical T-cell subsets throughout the CAR-T manufacturing workflow.
Quantitative Profiling of Key T-cell Subsets
A prerequisite for optimization is the accurate phenotypic identification and quantification of T-cell subsets. The table below summarizes the defining surface markers and functional characteristics of the primary subsets of interest in CAR-T manufacturing [70] [73].
Table 1: Phenotypic and Functional Characteristics of T-cell Subsets Relevant to CAR-T Therapy
| T-cell Subset | Key Phenotypic Markers (Human) | Proliferative Capacity | Persistence In Vivo | Differentiation Potential |
|---|---|---|---|---|
| Naive (TN) | CD45RA+, CD45RO-, CCR7+, CD62L+, CD95lo | High | High (upon activation) | Can generate all memory and effector subsets |
| Stem Cell Memory (TSCM) | CD45RA+, CD45RO-, CCR7+, CD62L+, CD95+ | Very High | Very High | Self-renewing; can reconstitute entire T-cell repertoire |
| Central Memory (TCM) | CD45RO+, CCR7+, CD62L+ | High | High | Generates TEM and TEFF |
| Effector Memory (TEM) | CD45RO+, CCR7-, CD62L- | Intermediate | Intermediate | Generates TEFF |
| Effector (TEFF) | CD45RA+ (often), CCR7-, CD62L- | Low | Low | Terminally differentiated, direct cytotoxicity |
The distribution of these subsets is not static and is significantly impacted by donor age. Understanding these shifts is crucial when working with autologous samples from a diverse patient population.
Table 2: Age-Related Changes in T-cell Subsets in Peripheral Blood (Adapted from [73])
| Parameter | Change with Age | Notes |
|---|---|---|
| CD8+ Naive T-cells | Sharp decrease in both percentage and absolute number | Linked to thymic involution and antigen exposure over time. |
| CD4+ Naive T-cells | Sharp decrease in both percentage and absolute number | More stable than CD8+ TN, but still significantly decreased. |
| TSCM (CD8+) | Absolute number decreases | The rate of decrease is slower than for naive T cells. |
| TSCM (CD4+) | Frequency and absolute number relatively stable | Suggests a key role in maintaining CD4+ T-cell homeostasis with ageing. |
| TSCM/TN Ratio | Increases with age | Highlights the increasing relative importance of TSCM as the naive pool contracts. |
Protocol: Advanced Flow Cytometry for T-cell Subset Immune Monitoring
Objective: To longitudinally monitor T-cell subsets, including CAR-T cells, and their activation status in peripheral blood during CAR-T therapy using a standardized, high-resolution flow cytometry assay [74].
Materials & Reagents:
- Samples: EDTA- or heparin-anticoagulated whole blood from patients and healthy controls.
- Staining Panels: Pre-formulated dry antibody panels in DURA Innovations tubes (or equivalent) for standardization. The core panel should include antibodies against:
- Lineage/Subset: CD3, CD4, CD8, CD45RA, CCR7 (CD197), CD62L, CD95
- CAR Detection: Recombinant protein for the CAR target antigen (e.g., CD19-Fc for anti-CD19 CAR) or anti-idiotype antibody.
- Activation/Exhaustion: CD25, CD137 (4-1BB), PD-1, TIM-3
- Viability Dye: 7-AAD or similar.
- Counting Beads: For absolute count determination (e.g., DURAClone IM-count tube).
Methodology:
- Sample Preparation: Add 100 µL of EDTA whole blood to the pre-formulated tube. Mix gently and incubate for 15 minutes in the dark at room temperature (RT).
- Red Blood Cell Lysis: Add 2 mL of a lysing solution (e.g., VersaLyse). Mix and incubate for 10 minutes at RT in the dark.
- Wash and Resuspend: Centrifuge at 200 x g for 5 minutes. Discard supernatant, wash cells with 3 mL PBS, centrifuge again, and resuspend in 0.5 mL of PBS with 0.1% formaldehyde.
- Data Acquisition: Acquire data on a flow cytometer equipped with at least 3 lasers (405nm, 488nm, 638nm) and 13 fluorescence detectors. Perform daily instrument calibration and quality control.
- Data Analysis: Use the gating strategy below to identify T-cell subsets and analyze CAR-T cell phenotype and activation status.
Diagram 1: Flow cytometry gating strategy for T-cell subsets.
Protocol: Optimizing Manufacturing to Preserve Favorable Subsets
Objective: To minimize T-cell differentiation and exhaustion during ex vivo manufacturing by controlling the stimulation dose and shortening process time, thereby preserving TN and TSCM phenotypes [75] [76].
Materials & Reagents:
- T-cell Activators: Artificial antigen-presenting cell scaffolds (APC-ms) for precise stimulation dosing [76] or traditional Dynabeads CD3/CD28.
- Culture Media: Serum-free T-cell medium.
- Cytokines: Recombinant human IL-2.
- Bioreactor: Closed, automated system (e.g., Gibco CTS Rotea System, CTS DynaCellect System) for robust, gentle processing [61].
Methodology:
- T-cell Isolation & Phenotyping: Isolate CD3+ T-cells from leukapheresis product. Take an aliquot for baseline phenotyping via flow cytometry (Protocol 1) to determine the initial CD4/CD8 ratio and subset distribution.
- Personalized Stimulation Dose Determination:
- The optimal stimulation dose (e.g., density of anti-CD3/anti-CD28 on APC-ms) is not one-size-fits-all and should be calibrated based on the initial T-cell phenotype [76].
- Model Input: Pre-culture levels of naive and memory subsets serve as predictors for the required stimulation.
- Model Output: A precise stimulation dose (e.g., 0.1 mol% biotin for APC-ms) predicted to yield a product with less exhaustion markers (PD-1lo TIM-3lo) and a more favorable memory phenotype.
- Activation and Transduction: Activate T-cells using the predetermined dose for 24-48 hours. Transduce with lentiviral or retroviral CAR vector.
- Shortened Ex Vivo Culture: Expand cells for a shortened duration (e.g., 3-7 days total, versus traditional 14-21 days) [61] [75]. Monitor cell count and phenotype.
- Product Formulation: Harvest cells, perform bead removal if necessary, and formulate the final product. Determine the final CD4/CD8 ratio and T-cell subset composition before cryopreservation.
Diagram 2: Personalized CAR-T manufacturing workflow.
The Scientist's Toolkit: Essential Reagents and Instruments
Table 3: Key Research Reagent Solutions for T-cell Subset Analysis and Manufacturing
| Product Category | Example Product | Key Function in Workflow |
|---|---|---|
| Standardized Flow Cytometry Panels | DURA Innovations dry antibody tubes [74] | Standardized, pre-formulated panels for reproducible immunophenotyping of T-cell subsets and activation markers. |
| Precise T-cell Activators | Artificial APC scaffolds (APC-ms) [76] | Presents T-cell activating ligands (anti-CD3/anti-CD28) at highly defined, tunable densities to prevent overstimulation. |
| Traditional T-cell Activators | CTS Detachable Dynabeads CD3/CD28 [61] | Magnetic beads for efficient T-cell activation and expansion; used at fixed bead-to-cell ratios. |
| Automated Cell Processing System | CTS Rotea Counterflow Centrifugation System [61] | Enables gentle, low-shear cell washing and concentration, preserving cell viability and function. |
| Automated Magnetic Separation System | CTS DynaCellect Magnetic Separation System [61] | Automated system for cell isolation and, critically, efficient magnetic bead removal post-activation. |
| Process Automation Software | CTS Cellmation Software for DeltaV System [61] | Digital integration and control of modular cell therapy instruments to minimize process variability. |
Concluding Remarks
The intentional optimization of T-cell subsets represents a paradigm shift in autologous CAR-T production, moving from a focus solely on cell number to a more nuanced emphasis on cell quality. By implementing the detailed protocols for monitoring (Protocol 1) and manufacturing (Protocol 2), and by leveraging the essential tools outlined, researchers and developers can systematically create more potent and persistent CAR-T products. The strategic enrichment of TSCM and naive subsets, coupled with a controlled CD4+/CD8+ ratio, directly addresses critical limitations of current therapies, such as T-cell exhaustion and poor long-term persistence. Integrating these subset-focused strategies is therefore paramount for advancing the next generation of autologous CAR-T therapies, particularly for extending their success into solid tumors and achieving more consistent patient responses.
Within the framework of autologous CAR T-cell production research, managing the immunogenic potential of therapeutic constructs is paramount for ensuring patient safety and treatment efficacy. The antigen-recognition domain, most traditionally derived from murine single-chain variable fragments (scFvs), can elicit undesirable immune responses against the CAR T cells themselves, potentially limiting their persistence and antitumor activity [77] [78]. This application note details two principal strategies for mitigating this risk: the humanization of scFvs and the utilization of camelid-derived nanobodies. We provide a structured comparison, detailed experimental protocols for their development, and contextualize their application within the current regulatory and manufacturing landscape of CAR T-cell therapies.
Structural and Functional Comparison
The choice of antigen-binding domain fundamentally influences the characteristics of the resulting CAR T-cell product. Conventional scFvs and nanobodies represent distinct architectural paradigms with implications for immunogenicity, stability, and functionality [79] [78].
Conventional monoclonal antibodies (mAbs) are large (~150 kDa) molecules comprising two heavy and two light chains. The antigen-binding site is formed by the variable domains of the heavy and light chains (VH and VL), which associate via a hydrophobic interface [78] [80]. A single-chain variable fragment (scFv) is an engineered fusion of the VH and VL domains connected by a short, flexible peptide linker, reducing the size to approximately 25-30 kDa [81]. However, the inherent hydrophobicity of the VH-VL interface can lead to instability and aggregation, complicating production and potentially increasing immunogenicity [78]. Furthermore, scFvs of murine origin require humanization to minimize the risk of a human anti-mouse antibody (HAMA) response [81] [82].
In contrast, nanobodies (VHH) are the smallest known antigen-binding fragments (~15 kDa), derived from the heavy-chain-only antibodies found in camelids [79] [83]. As single-domain entities, they lack a hydrophobic VH-VL interface, which confers superior solubility and stability, and reduces aggregation propensity [78] [80]. Their small size promotes enhanced tissue penetration and allows access to cryptic epitopes that may be inaccessible to bulkier scFvs [79] [83]. Additionally, their high sequence homology with human VH domains and the ease of humanization contribute to their low immunogenicity profile [83] [77].
Table 1: Quantitative Comparison of scFv and Nanobody Properties
| Property | Humanized scFv | Nanobody (VHH) |
|---|---|---|
| Molecular Size | ~25-30 kDa [79] [81] | ~15 kDa [79] [83] |
| Structural Domains | VH and VL connected by a linker [81] | Single VHH domain [79] |
| Solubility & Stability | Moderate; prone to aggregation due to hydrophobic VH-VL interface [78] | High; hydrophilic interface, resistant to aggregation [79] [80] |
| Immunogenicity Risk | Moderate; requires careful humanization to minimize HAMA response [81] [82] | Low; high homology to human VH, easily humanized [83] [77] |
| Epitope Recognition | Conventional, surface-exposed epitopes [78] | Can access unique, cryptic epitopes and cavities [79] [78] |
| Production in E. coli | Feasible, but can be challenging due to aggregation [82] | Highly efficient and cost-effective [79] [83] |
| Tumor Penetration | Good [81] | Excellent due to small size [79] [83] |
| Typical Affinity | Nanomolar range [81] | Nanomolar to picomolar range [79] |
| CAR-T Application | Well-established in approved therapies (e.g., Kymriah, Yescarta) [84] | Emerging, with multiple candidates in pre-clinical and clinical trials [79] [77] |
Experimental Protocols
Protocol 1: Humanization of a Murine scFv for CAR-T Applications
This protocol outlines a standardized method for humanizing a murine scFv via CDR grafting, incorporating structural modeling to preserve antigen-binding affinity [81].
Procedure:
- Sequence Murine Variable Regions: Isolve total RNA from the hybridoma cell line producing the murine monoclonal antibody of interest. Amplify and sequence the genes encoding the variable heavy (VH) and variable light (VL) chains using reverse transcription-PCR (RT-PCR) with degenerate primers [81].
- Identify CDR and Framework Regions: Analyze the VH and VL sequences using tools like the IgBlast Kabit program to delineate the complementarity-determining regions (CDRs) and framework regions (FRs) according to the Kabat definition [81].
- Select Human Acceptor Frameworks: Use IMGT/V-QUEST or the Kabat database to identify human germline V-gene sequences with the highest amino acid identity in the FRs to the murine sequences [81].
- Design Humanized scFv:
- Graft the murine CDRs onto the selected human FRs.
- Retain key murine FR residues that are critical for maintaining the structure of the antigen-binding paratope, such as those in the "Vernier zone" which underpins CDR loop conformations [81].
- In Silico Modeling and Validation:
- Construct 3-D structural models of both the original murine scFv and the designed humanized scFv using computer-assisted molecular modeling (e.g., based on PDB templates) [81].
- Calculate the root-mean-square deviation (RMSD) between the two models to evaluate the preservation of the original CDR conformation. A low RMSD value indicates successful grafting with minimal structural perturbation [81].
- Gene Synthesis and Cloning: Synthesize the humanized scFv gene de novo, with codon optimization for expression in the desired host (e.g., E. coli). Clone the gene into an appropriate expression vector, such as pET-22b(+), in either VH-linker-VL or VL-linker-VH orientation with a C-terminal tag (e.g., His-tag) for purification [81] [82].
- Expression and Purification: Transform the expression construct into E. coli BL21(DE3) cells. Induce protein expression and purify the soluble scFv from the periplasmic or cytoplasmic fraction using immobilized metal affinity chromatography (IMAC) [81].
- Binding Affinity Validation: Validate the binding specificity and affinity of the purified humanized scFv for its target antigen using techniques like ELISA or surface plasmon resonance (SPR), and compare its performance to the original murine antibody [81].
Protocol 2: Generation and Validation of a Nanobody-Based CAR
This protocol describes the process of isolating antigen-specific nanobodies and incorporating them into a CAR construct for T-cell engineering [79] [77].
Procedure:
- Nanobody Library Generation and Selection:
- Immunize a camelid (e.g., alpaca or llama) with the target antigen of interest.
- Isolve peripheral blood lymphocytes to extract mRNA and construct a VHH phage display library.
- Pan the library against the immobilized antigen to isolate antigen-specific VHH clones. Alternatively, use synthetic nanobody libraries [79] [83].
- Sequence Analysis and Humanization: Sequence the selected VHH clones. Due to their high natural homology to human VH, humanization is typically straightforward, often requiring only a few point mutations in the framework regions to further reduce immunogenicity [83] [77].
- CAR Vector Construction:
- Design a CAR cassette comprising, from 5' to 3': a signal peptide, the nanobody sequence, a hinge region (e.g., CD8α), a transmembrane domain, and intracellular T-cell signaling domains (e.g., CD3ζ plus a costimulatory domain such as 4-1BB or CD28) [77].
- Clone this nanobody-CAR cassette into a lentiviral or retroviral vector backbone under the control of a strong promoter (e.g., EF-1α or CMV) [26].
- Virus Production and T-Cell Transduction:
- Produce recombinant lentiviral vectors by transfecting HEK-293T cells with the CAR transfer plasmid and packaging plasmids using standard protocols. Harvest and concentrate the viral supernatant [26].
- Activate human primary T-cells isolated from donor PBMCs using anti-CD3/CD28 antibodies.
- Transduce the activated T-cells with the lentiviral vector by spinfection in the presence of a polycation such as protamine sulfate.
- CAR-T Cell Expansion and Phenotyping:
- Expand the transduced T-cells in culture medium supplemented with IL-2 for 7-14 days.
- Assess the transduction efficiency by flow cytometry using a detection method for the CAR, such as a tag-specific antibody or a recombinant antigen protein [26].
- Functional Validation:
- Cytotoxicity: Co-culture CAR T-cells with target antigen-positive and negative tumor cell lines. Measure specific lysis using a real-time cell analyzer or a lactate dehydrogenase (LDH) release assay [77].
- Cytokine Release: Quantify the secretion of effector cytokines like IFN-γ and IL-2 in the co-culture supernatant via ELISA, confirming antigen-specific T-cell activation [77].
The following workflow diagram illustrates the parallel paths for developing humanized scFv-CARs and nanobody-CARs.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for scFv and Nanobody-Based CAR-T Development
| Reagent / Solution | Function | Example & Notes |
|---|---|---|
| pET-22b(+) Vector | Prokaryotic expression vector for scFv/nanobody production. | Commonly used for high-yield expression in E. coli with a C-terminal His-tag for purification [81] [82]. |
| CliniMACS Prodigy | Automated, closed-system cell processor for CAR-T manufacturing. | Enables decentralized, point-of-care production of CAR-T cells under GMP-like conditions, standardizing the process [26] [35]. |
| Lentiviral Vector System | Gene delivery vehicle for stable genomic integration of the CAR. | Preferred for high transduction efficiency in primary T-cells. Third-generation systems enhance safety [26]. |
| Anti-CD3/CD28 Antibodies | T-cell activation and expansion. | Magnetic beads or soluble antibodies are used to activate T-cells prior to transduction, critical for robust expansion [26]. |
| Recombinant Human IL-2 | T-cell growth factor. | Added to culture media to support the survival and proliferation of transduced CAR T-cells during ex vivo expansion [26]. |
| Ubiquitin Fusion Tag | Solubility enhancer for recombinant protein expression. | Fusion to scFvs or nanobodies can improve solubility, yield, and protect against proteolytic degradation during production in E. coli [82]. |
Application in Autologous CAR T-Cell Production
Integrating low-immunogenicity binding domains into the autologous CAR T-cell production workflow is critical for enhancing product quality and patient outcomes. The entire process, from leukapheresis to infusion, is complex and regulated.
The critical quality attributes (CQAs) of the final CAR T-cell product are directly influenced by the choice of binding domain. Nanobodies, due to their stability and solubility, can contribute to more consistent CAR surface expression and reduce tonic signaling, a phenomenon associated with scFv aggregation that can lead to premature T-cell exhaustion [77] [78]. Furthermore, the lower immunogenicity profile of both well-humanized scFvs and nanodies is a key consideration for regulatory approval, as it impacts the risk-benefit assessment of the therapy [84]. The move towards decentralized, point-of-care manufacturing models for autologous CAR-T products places a premium on robust and reproducible processes, where the advantageous biophysical properties of nanodies can be particularly beneficial [26] [35].
Concluding Remarks
The strategic reduction of immunogenicity is a cornerstone in the advancement of durable and safe autologous CAR T-cell therapies. While humanized scFvs represent a validated and clinically proven technology, the intrinsic properties of nanodies—including their small size, high stability, and low immunogenicity—offer a compelling alternative for next-generation CAR designs. The experimental protocols and analytical tools outlined herein provide a foundation for researchers to evaluate and implement these critical technologies, ultimately contributing to the development of more effective and accessible cell-based immunotherapies.
The commercialization of autologous Chimeric Antigen Receptor (CAR) T-cell therapies faces significant hurdles, primarily due to high costs and complex logistics inherent in centralized manufacturing models. This application note details how the adoption of automated, closed systems and a shift towards point-of-care (POC) manufacturing can address these challenges. We provide a quantitative analysis of cost structures and present a detailed protocol for a shortened, automated CAR-T cell manufacturing workflow. Supported by data on equipment and reagent solutions, this document serves as a guide for researchers and therapy developers aiming to enhance the accessibility and economic viability of these life-saving treatments.
Autologous CAR-T cell therapy represents a paradigm shift in cancer treatment. However, its personalized nature—manufacturing a unique batch for each patient—makes it susceptible to high costs and logistical inefficiencies. The traditional, centralized model relies on time-consuming, labor-intensive processes and complex cold-chain logistics for transporting patient apheresis material and the final product, leading to prolonged vein-to-vein times [40] [85]. This model strains healthcare systems and limits patient access [18]. Decentralized manufacturing, particularly at the point of care, emerges as a promising alternative by locating production closer to the patient, thereby reducing transport times and costs [40]. The successful implementation of this model is critically dependent on automation and closed-system technologies to ensure robustness, consistency, and compliance with Good Manufacturing Practice (GMP) in a distributed network [86] [87].
Quantitative Analysis of Cost and Logistical Challenges
A clear understanding of the cost components and operational inefficiencies is essential for evaluating the impact of new manufacturing paradigms. The following tables summarize key quantitative data.
Table 1: Cost Analysis of Decentralized CAR-T Cell Production Data based on a study of an academic non-profit setting in Germany, calculated for a clean room with one automated manufacturing machine [88].
| Cost Component | Annual Fixed Cost (€) | Cost per Production (€) |
|---|---|---|
| Personnel & Technician Salaries | Incorporated in fixed costs | Incorporated in variable costs |
| Equipment & Clean Room | 438,098 | - |
| Production Materials | - | 34,798 |
| Total (at maximum capacity) | - | ≈ 60,000 |
| Total (with 3 machines, at capacity) | - | ≈ 45,000 |
| Total (with 3 machines & cheaper lentivirus alternative) | - | ≈ 33,000 |
Table 2: Key Logistical and Manufacturing Challenges Data synthesized from a cross-sectional survey of 40 academic institutions engaged in CAR-T cell production [18].
| Challenge | Percentage of Institutions Reporting |
|---|---|
| Cost Constraints | 70% (28/40) |
| Regulatory Complexities | 70% (28/40) |
| Facility/Infrastructure Requirements | 57% (17/40)* |
| Variability in Final Product Quality | 73% (29/40) |
Note: The percentage for facility requirements is based on a subset of 30 respondents [18].
Experimental Protocol: Automated 24-Hour CAR-T Cell Manufacturing Workflow
The protocol below demonstrates how automation and integrated closed systems can drastically shorten production time and reduce manual intervention, addressing the challenges outlined above. This protocol is adapted from a next-generation process that reduces typical 7-14 day timelines to 24 hours [40].
Objective
To manufacture autologous CAR-T cells within a 24-hour timeframe using a fully automated, closed, lentivirus-based system, yielding a product with a less differentiated, naive T-stem cell memory (TSCM) phenotype.
Materials and Equipment
- Starting Material: Quarter Leukopak or apheresis product.
- Instrumentation:
- Gibco CTS DynaCellect Magnetic Separation System
- Gibco CTS Rotea Counterflow Centrifugation System
- Thermo Scientific CryoMed Controlled-Rate Freezer
- Gibco CTS Cellmation Software for digital integration
- Reagents and Consumables:
- Gibco CTS Detachable Dynabeads CD3/CD28
- Gibco CTS Detachable Dynabeads Release Buffer
- Lentiviral vector (e.g., produced with LV-MAX system) with CD19 CAR construct
- Gibco Cell Therapy Systems (CTS) media and supplements
Methodology
Step 1: One-Step Isolation and Activation
- Load the leukopak onto the CTS DynaCellect System.
- Use CTS Detachable Dynabeads CD3/CD28 for simultaneous isolation and activation of T cells. This one-step process yields a highly pure T-cell population and begins the activation cascade necessary for transduction.
- The process is controlled via Cellmation Software, ensuring a closed and automated workflow from the start.
Step 2: Lentiviral Transduction
- Following isolation, directly transduce the cells with the lentiviral vector at a low multiplicity of infection (MOI of 2).
- The closed system minimizes contamination risk during this critical genetic modification step.
Step 3: Active Release Debeading
- Following transduction, initiate the automated debeading process on the CTS DynaCellect System.
- Use the CTS Detachable Dynabeads Release Buffer to actively detach the magnetic beads from the T cells. This step provides greater control over the process, preventing T-cell exhaustion and death associated with overactivation from beads that release passively.
Step 4: Wash and Concentration
- Transfer the cell suspension to the CTS Rotea Counterflow Centrifugation System.
- Perform washing and concentration steps in a low-shear environment to ensure minimal cell damage and achieve high cell recovery and viability.
Step 5: Final Formulation and Cryopreservation
- The final product is divided for immediate cryopreservation or analytical testing.
- For cryopreservation, use the CryoMed Controlled-Rate Freezer to ensure a consistent freeze profile, which is critical for maintaining cell viability and function.
Expected Results and Quality Control
- Manufacturing Time: The entire process from cell isolation to cryopreservation is completed within 24 hours.
- Phenotype: Flow cytometry analysis (e.g., for CD45RA+/CCR7+ markers) will show a significantly higher proportion of naive TSCM phenotype cells compared to cells from a traditional 7-day expansion process. This phenotype is associated with improved in vivo persistence and anti-tumor activity [40].
- Quality Control: The integrated digital platform (Cellmation Software) maintains electronic batch records, ensuring data integrity and facilitating regulatory compliance.
Visualization of Workflows and Systems
The following diagrams illustrate the core concepts of the automated protocol and the system architecture enabling decentralized manufacturing.
Automated CAR-T Process Workflow
Point-of-Care System Architecture
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Automated CAR-T Cell Manufacturing
| Item | Function in the Workflow |
|---|---|
| CTS Detachable Dynabeads CD3/CD28 | Enables one-step isolation and activation of T cells. Its active-release property allows for precise control over activation time, reducing the risk of T-cell exhaustion [40]. |
| CTS DynaCellect Magnetic Separation System | A closed, automated system for cell isolation and, critically, the active removal of magnetic beads post-transduction [40] [86]. |
| CTS Rotea Counterflow Centrifugation System | A closed cell processing system for gentle washing and concentration of cells, offering high recovery and viability in low volumes [40] [86]. |
| LV-MAX Lentiviral Production System | A system for producing high-quality lentiviral vectors, which are essential for efficient and stable genetic modification of T cells [40]. |
| CTS Cellmation Software | Provides digital integration and automation of the entire workflow, reducing manual touchpoints and improving data integrity for regulatory compliance [40] [86]. |
The integration of automation, closed systems, and decentralized manufacturing models presents a viable path to overcoming the primary cost and logistical barriers to widespread autologous CAR-T therapy adoption. The experimental protocol for a 24-hour manufacturing process demonstrates that it is feasible to significantly shorten vein-to-vein time while simultaneously improving the therapeutic potential of the final product by preserving favorable T-cell phenotypes.
The future of point-of-care manufacturing will be further shaped by Artificial Intelligence (AI) and Industry 4.0 principles. AI-driven platforms can interpret real-time process data to provide insights for optimization and predictive control, enhancing consistency and success rates [85]. Furthermore, a phased approach to automation—transitioning from manual to semi-automated and finally to highly automated systems—allows organizations to strategically manage investment and build operational expertise [89]. As the industry moves towards producing therapies for solid tumors and earlier lines of treatment, these advanced, efficient, and scalable manufacturing strategies will be indispensable for making curative treatments accessible to all eligible patients.
Benchmarking and Future Directions: Analytical Methods and the Allogeneic Paradigm
The commercialization and expanding clinical indications for Chimeric Antigen Receptor (CAR) T-cell therapies necessitate a robust and standardized framework for analytical quality control. Autologous CAR T-cell production presents unique challenges, as each drug product is manufactured from an individual patient's cells. This application note details standardized methodologies and protocols for the critical stages of the CAR T-cell workflow—from initial apheresis material characterization to final drug product release and post-infusion immunomonitoring. The establishment of these standardized assays is vital for ensuring product safety, identity, purity, potency, and efficacy, ultimately enhancing patient access to these transformative therapies across Europe and beyond [90].
Current Landscape and the Need for Harmonization
A recent European survey conducted by the T2Evolve Consortium under the Innovative Medicines Initiative (IMI) provides a critical snapshot of current practices and highlights significant variability in the field. The survey, which gathered responses from 53 stakeholders across 13 European countries, revealed a pressing need for harmonization, particularly in the areas of functional potency assays and post-infusion patient monitoring [90].
Table 1: Key Findings from the European Survey on CAR T-Cell Analytical Methods
| Process Stage | Current Common Practices | Identified Gaps & Variability | Harmonization Needs |
|---|---|---|---|
| Apheresis Material | Viability and cell count assays [90] | Variable depth of immunophenotypic characterization | Standardized panels for T-cell subset analysis |
| Drug Product | Safety tests (e.g., sterility, endotoxin) per Pharmacopeia [90] | Minority assess T-cell activation/exhaustion profiles [90] | Standardized functional potency assays |
| Post-Infusion Immunomonitoring | Short-term patient follow-up [90] | Significant variability across clinical centers [90] | Identification of predictive biomarkers for response, relapse, and toxicity [90] |
This variability underscores the necessity for the standardized protocols outlined in the following sections, which are designed to ensure consistency, improve comparability of clinical data, and support regulatory submissions.
Experimental Protocols & Workflows
Apheresis Material Characterization
The initial quality of the apheresis material is a critical determinant of the success of the entire manufacturing process. The following protocol provides a standardized approach for its characterization.
Protocol 1: Immunophenotypic Characterization of Apheresis Material
- Objective: To determine the viability, total nucleated cell count, and composition of T-cell subsets in the leukapheresis starting material.
- Sample: Fresh or thawed leukapheresis sample.
- Reagents: PBS, viability dye (e.g., 7-AAD), antibody panel against CD3, CD4, CD8, CD45RA, CD62L, CD19 (for B-cell depletion assessment).
- Equipment: Flow cytometer, hematology analyzer, cell counter.
- Methodology:
- Sample Preparation: Dilute the apheresis sample appropriately in PBS. Perform total nucleated cell count and viability analysis using an automated cell counter with trypan blue exclusion or an equivalent method.
- Staining: Aliquot a defined number of cells (e.g., 1x10^6) into flow cytometry tubes. Stain with a pre-optimized cocktail of fluorescently labeled antibodies and a viability dye. Incubate for 20-30 minutes in the dark at 4°C.
- Washing and Fixation: Wash cells twice with PBS to remove unbound antibody. Resuspend in fixation buffer if required.
- Acquisition and Analysis: Acquire data on a flow cytometer. Analyze the data to determine the percentages and absolute counts of CD3+ T-cells, CD4+ helper T-cells, CD8+ cytotoxic T-cells, and naive (CD45RA+CD62L+) and memory subsets.
The following workflow diagram outlines the key steps from apheresis to drug product release.
Drug Product Quality Control
The drug product must undergo rigorous testing to ensure it meets predefined specifications for identity, purity, potency, and safety before patient infusion.
Protocol 2: Drug Product Potency and Safety Assays
- Objective: To assess the critical quality attributes of the final CAR T-cell product, including identity, potency, purity, and safety.
- Sample: Final formulated, washed CAR T-cell drug product.
- Reagents:
- For Identity/Potency: Target cells expressing the cognate antigen, control cells (antigen-negative), cytokine release assay reagents (e.g., ELISA for IFN-γ), flow cytometry antibodies against the CAR construct (e.g., anti-idiotype or protein L) and T-cell markers.
- For Safety: Sterility culture media, Endotoxin-Single Test Kit (chromogenic method) [91].
- Equipment: Flow cytometer, CO2 incubator, ELISA plate reader, LAL-testing compatible spectrophotometer or incubating microplate reader.
- Methodology:
- Identity and Purity (CAR Expression): Determine the percentage of CAR-positive T-cells by flow cytometry using a specific detection method. Purity is reported as %CAR+ of live CD3+ cells.
- Potency (Cytokine Release and Cytotoxicity):
- Cytokine Release: Co-culture CAR T-cells with antigen-positive and antigen-negative target cells at a defined effector-to-target ratio for 24 hours. Measure the concentration of IFN-γ (and other relevant cytokines) in the supernatant using an ELISA.
- Cytotoxicity: Co-culture CAR T-cells with fluorescently labeled target cells. After a defined period, measure target cell lysis using a real-time cell analyzer or by flow cytometry.
- Safety Testing:
- Sterility: Inoculate samples into aerobic and anaerobic culture media according to Ph. Eur. 2.6.1/USP <71> and monitor for growth.
- Endotoxin Testing: Use a chromogenic Limulus Amebocyte Lysate (LAL) assay. The method uses a synthetic chromogenic substrate that is cleaved by clotting enzymes activated in the presence of endotoxin, releasing a yellow chromophore (para-nitroaniline, pNA) measurable at 405 nm [91]. The kinetic variant of this assay is preferred for its wider dynamic range and automation potential [92].
Table 2: Drug Product Release Criteria and Assays
| Quality Attribute | Recommended Assay | Typical Release Specification |
|---|---|---|
| Viability | Flow cytometry with viability dye / Cell counter | ≥ 80% |
| Identity & Purity | Flow cytometry for CD3, CAR | ≥ XX% CAR+ of CD3+ cells |
| Potency | In vitro cytokine release (IFN-γ) upon antigen stimulation | Significant increase vs. non-stimulated control |
| Safety (Sterility) | Microbial culture (BacT/ALERT) | No growth after 14 days |
| Safety (Endotoxin) | Kinetic Chromogenic LAL Assay [92] [91] | ≤ 5.0 EU/kg/hr |
| Vector Copy Number | qPCR/ddPCR | Defined per product |
Post-Infusion Immunomonitoring
Monitoring patients after CAR T-cell infusion is crucial for understanding pharmacokinetics, pharmacodynamics, and correlating clinical outcomes with product attributes.
Protocol 3: Monitoring CAR T-Cell Kinetics and Phenotype In Vivo
- Objective: To quantify and characterize persisting CAR T-cells in patient peripheral blood and assess their functional status.
- Sample: Patient peripheral blood collected at predefined timepoints (e.g., Day 7, 14, 28, Month 3, 6, etc.).
- Reagents: Antibodies for flow cytometry (CD3, CD4, CD8, CAR, activation markers like CD69, exhaustion markers like PD-1, LAG-3, TIM-3), DNA extraction kit, qPCR reagents for vector copy number detection.
- Equipment: Flow cytometer, qPCR system, centrifuge.
- Methodology:
- PBMC Isolation: Isolate Peripheral Blood Mononuclear Cells (PBMCs) from whole blood via density gradient centrifugation.
- CAR T-cell Quantification:
- Flow Cytometry: Directly stain PBMCs to identify the frequency of CAR-positive T-cells among total lymphocytes or CD3+ T-cells.
- qPCR: Extract genomic DNA from PBMCs and quantify the vector copy number per microgram of DNA, providing a sensitive measure of CAR T-cell persistence.
- Phenotypic Characterization: Use extended flow cytometry panels on the PBMCs to assess the differentiation (naive, central memory, effector memory), activation, and exhaustion status of the persisting CAR T-cells.
The relationship between key analytes and the biological processes they measure is summarized in the following diagram.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CAR T-Cell Analytical Assays
| Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| Chromogenic LAL Reagent | Endotoxin detection in drug product via a synthetic substrate that releases a measurable chromophore (pNA) upon cleavage [91]. | The kinetic chromogenic method offers a wider dynamic range and is less operator-dependent than endpoint assays [92]. |
| Anti-Idiotype Antibodies | Specific detection of the CAR construct on the T-cell surface by flow cytometry for identity and purity assessment. | Critical for accurately quantifying CAR expression without interference from endogenous T-cell receptors. |
| Cytokine-Specific ELISA Kits | Quantification of cytokine release (e.g., IFN-γ, IL-2) in co-culture supernatants as a measure of CAR T-cell potency. | Ensure the assay has the required sensitivity and dynamic range to detect differences in antigen-specific response. |
| Viability Dyes (e.g., 7-AAD) | Discrimination of live/dead cells during flow cytometric analysis to ensure accurate immunophenotyping. | Use of a viability dye is essential for excluding false-positive signals from dead cells. |
| qPCR/ddPCR Assays for VCN | Quantitative measurement of the number of CAR vector copies integrated into the genome of patient PBMCs for persistence monitoring. | Provides a highly sensitive and quantitative readout of CAR T-cell levels in vivo. |
The standardized analytical methods and detailed protocols presented herein for apheresis material, drug product, and post-infusion monitoring provide a critical framework for advancing autologous CAR T-cell therapy. Widespread adoption of such harmonized approaches will enhance product quality, improve the reliability of cross-study comparisons, facilitate regulatory review, and accelerate the safe and effective delivery of these innovative treatments to a broader patient population. The ongoing work of consortia like T2Evolve is essential to drive this standardization forward, addressing current gaps, particularly in potency assay harmonization and predictive biomarker identification [90].
Within the framework of autologous CAR T-cell production research, the functional characterization of the final product is a critical determinant of both clinical efficacy and safety. Potency assays are essential quantitative measures of the biological activity of these "living drugs," directly linked to their mechanism of action (MoA) [93] [57]. A comprehensive potency profile must evaluate key functional attributes: the direct cytotoxicity against target cells, the concomitant cytokine secretion that orchestrates immune activity, and the exhaustion profiles that can predict long-term persistence and efficacy [93] [94]. As manufacturing strategies evolve, including rapid production protocols and novel CAR designs, the development of robust, predictive functional potency assays becomes increasingly important to fully capture product complexity and ensure patient outcomes [93] [6] [57].
Core Functional Potency Assays
The mechanism of action of CAR T-cells is multifaceted, necessitating a matrix of assays that collectively reflect their therapeutic potential. The following core functions are routinely assessed.
Cytotoxicity Assays
Cytotoxicity, the direct lytic ability of CAR T-cells to eliminate antigen-expressing target cells, is a fundamental component of potency. Multiple in vitro methods are available, each with distinct advantages and applications [95].
Table 1: Comparison of Common Cytotoxicity Assays
| Assay Format | Principal Measure | Endpoint/Kinetic | Throughput | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Chromium Release | Release of radioactive ⁵¹Cr | Endpoint | Low | Considered a "gold standard" | Use of radioactive materials; short assay duration |
| Bioluminescence | Luciferase activity in living cells | Endpoint | High | High sensitivity; suitable for long-term assays | Requires genetic modification of target cells |
| Impedance | Electrical impedance reflecting cell adherence | Real-time, Kinetic | High | Real-time, label-free measurement | Measures indirect parameter (detachment) |
| Flow Cytometry | Cell membrane integrity via live/dead staining | Endpoint | High | Multiplexing capability (phenotype + death); measures differential killing | Requires target cell labeling [95] |
A validated flow cytometry-based killing assay protocol is detailed below [96].
Detailed Protocol: Flow Cytometric Cytotoxicity Assay
- Objective: To quantify the specific lytic activity of anti-CD19 CAR T-cells against CD19-positive target cells.
- Materials:
- Effector Cells: Anti-CD19 CAR T-cell product and non-transduced (NT) T-cells as a control.
- Target Cells: CD19+ cell line (e.g., REH) and a CD19- cell line (e.g., MOLM-13) for specificity control.
- Staining Reagents: Anti-CD3 antibody, anti-CD19 antibody, and 7-Amino-Actinomycin D (7-AAD) viability dye.
- Equipment: Flow cytometer, cell culture incubator, 24-well plates.
- Method Workflow:
- Preparation: Thaw and wash effector and target cells. Confirm CD19 expression on target cells and CAR expression on effector cells by flow cytometry.
- Co-culture: Seed effector and target cells in a 24-well plate at a defined ratio (e.g., 1:1) based on validated parameters. Include controls for spontaneous target cell death (target cells alone) and background killing (NT T-cells + target cells).
- Incubation: Co-culture cells for 24 hours at 37°C and 5% CO₂.
- Staining and Acquisition: Harvest cells, stain with anti-CD3, anti-CD19, and 7-AAD, and acquire data on a flow cytometer.
- Analysis: Gate on CD3-/CD19+ target cells. The frequency of dead target cells is determined by 7-AAD positivity.
- Calculation:
Specific Lysis (%) = [(% 7-AAD+ in CAR T sample) - (% 7-AAD+ in NT T-cell control)][96] - Validation Parameters: This method has been validated for specificity, linearity, accuracy, robustness (23-25h co-culture), and precision (inter-analyst ICC > 0.4) [96].
Diagram 1: Cytotoxicity Assay Workflow.
Cytokine Secretion Assays
Upon antigen recognition and activation, CAR T-cells secrete a cascade of cytokines, such as IFN-γ, TNF-α, and IL-2, which are critical for orchestrating a robust anti-tumor response. Measuring cytokine release is a widely adopted surrogate potency assay [93] [97].
Detailed Protocol: CD69 Activation Marker Assay as a Surrogate for Potency
- Objective: To provide a quantitative, flow cytometry-based potency test by measuring CD69 upregulation on CAR T-cells upon antigen engagement [97].
- Principle: CD69 is an early T-cell activation marker. Its expression on CAR-positive cells, measured as Mean Fluorescence Intensity (MFI), is a specific indicator of CAR functionality and correlates with cytotoxicity [97].
- Materials:
- Effector Cells: CAR-transduced Jurkat cells or primary CAR T-cells.
- Target Cells: Antigen-positive and antigen-negative (e.g., KO) cell lines.
- Staining Reagents: Anti-CD69 antibody, antibody against the CAR (e.g., anti-c-Myc-FITC), viability dye.
- Equipment: Flow cytometer.
- Method Workflow:
- Co-culture: Incubate CAR T-cells with antigen-positive and antigen-negative target cells for a defined period (e.g., 6-24 hours).
- Staining: Harvest cells and stain for surface CD69 and CAR expression.
- Acquisition and Analysis: Acquire data on a flow cytometer. Gate on viable, CAR-positive cells and quantify CD69 MFI.
- Quantification: The assay uses an intra-assay standard curve calibration to convert CD69 MFI into quantitative units of potency, demonstrating high precision, specificity, robustness, and linearity [97].
Exhaustion and Persistence Profiling
Long-term therapeutic success depends on the persistence of functional CAR T-cells. A terminally differentiated or exhausted phenotype is associated with poor clinical outcomes. Profiling exhaustion is therefore integral to a comprehensive potency assessment [93] [6] [94].
Detailed Protocol: Exhaustion Marker Profiling
- Objective: To characterize the differentiation and exhaustion state of a CAR T-cell product.
- Materials:
- Cells: CAR T-cell product at the end of manufacturing.
- Staining Reagents: Antibody panel for T-cell phenotyping and exhaustion markers: anti-CD45RA, anti-CCR7, anti-PD-1, anti-LAG-3, anti-TIM-3, anti-TOX.
- Equipment: Flow cytometer, preferably with high-parameter capability.
- Method Workflow:
- Sample Preparation: Aliquot a sample of the final CAR T-cell product.
- Staining: Stain cells with a predefined antibody cocktail targeting surface markers and, if required, intracellular markers (e.g., TOX) following fixation and permeabilization.
- Acquisition and Analysis: Acquire data on a flow cytometer. Analyze the data to determine the frequencies of naïve (TN, CD45RA+ CCR7+), stem cell memory (TSCM), and exhausted (PD-1+ LAG-3+ TIM-3+) subpopulations within the CAR-positive compartment [93] [94].
- Advanced Models: For a more functional assessment of exhaustion, in vitro models of chronic antigen exposure can be employed. These models replicate the conditions leading to T-cell exhaustion and can be combined with secondary functional assays like re-stimulation cytokine secretion or cytotoxicity assays [94].
Diagram 2: T-cell Activation vs. Exhaustion Pathway.
The Scientist's Toolkit: Essential Research Reagents
The following table summarizes key reagents and their functions in conducting the described functional potency assays.
Table 2: Key Research Reagent Solutions for CAR T-cell Potency Assays
| Reagent / Solution | Function / Application | Specific Examples |
|---|---|---|
| Flow Cytometry Antibodies | Phenotyping, activation, and exhaustion marker detection. | Anti-CD3, CD4, CD8, CAR idiotype, CD69 (activation), PD-1, LAG-3, TIM-3 (exhaustion) [97] [96]. |
| Viability Dyes | Discrimination of live/dead cells in cytotoxicity assays. | 7-Amino-Actinomycin D (7-AAD) [96]. |
| Cell Line Pairs | Target cells for specificity and potency testing. | CD19+ line (REH) & CD19- line (MOLM-13) for anti-CD19 CAR-T [96]. |
| Cytokine Detection Kits | Quantification of cytokine secretion (IFN-γ, TNF-α, IL-2). | ELISA or multiplex bead-based immunoassays [93]. |
| Cell Culture Media | Ex vivo expansion and maintenance of T-cells and target lines. | TexMACS medium supplemented with IL-7 and IL-15 [96]. |
Advanced Assay Considerations and the Path Forward
The field of CAR T-cell therapy is moving beyond conventional potency assays. The integration of multi-omics approaches (genomics, epigenomics, transcriptomics, proteomics, metabolomics) is providing unprecedented insights into the molecular determinants of product potency and persistence [93]. For instance, DNA methylation profiles in CD19 CAR T-cell products have been linked to clinical response and survival [93].
Furthermore, there is a push to develop more physiologically relevant assays. This includes the use of 3D tumor spheroid models to better mimic the tumor microenvironment and assess CAR T-cell infiltration and function, as demonstrated in cholangiocarcinoma research [98]. Another innovation involves manufacturing CAR T-cells under conditions that mimic the tumor microenvironment (e.g., hypoxia) to generate products with enhanced stem-like phenotypes and superior serial killing activity, which can then be evaluated using advanced functional potency platforms [99].
As the industry moves towards fresh, locally manufactured CAR T-cell products with shortened vein-to-vein times, the development of rapid, robust, and clinically predictive potency assays that can keep pace with manufacturing will be paramount to ensuring product quality and patient benefit [57].
Chimeric Antigen Receptor T-cell (CAR-T) therapy represents a paradigm shift in cancer treatment, leveraging the power of a patient's own immune system to fight malignancies. This innovative form of immunotherapy involves genetically engineering T-cells to express synthetic receptors that target specific tumor antigens [100]. The remarkable success of CAR-T therapy in treating hematological malignancies has led to the approval of multiple commercial products, with the global CAR-T market expected to grow from USD 5,206.15 million in 2025 to approximately USD 23,247.29 million by 2034, reflecting a compound annual growth rate of 18.10% [101].
Currently, two primary manufacturing approaches dominate the CAR-T landscape: autologous and allogeneic. Autologous CAR-T therapy utilizes the patient's own T-cells, which are collected, genetically modified, expanded ex vivo, and reinfused into the same patient [26]. In contrast, allogeneic CAR-T therapy employs T-cells from healthy donors to create "off-the-shelf" products that can be administered to multiple patients [102] [103]. This analysis provides a comprehensive comparison of these approaches across efficacy, safety, and accessibility parameters to inform research and drug development strategies.
Comparative Clinical Performance
Efficacy and Clinical Response
Autologous CAR-Ts have demonstrated exceptional efficacy in treating hematologic malignancies, with response rates ranging from 70% to over 90% in relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL) [104]. The humanized CD19-targeted CAR-T (hCART19) clinical trial showed a 93.1% complete remission rate in B-ALL patients, with 53 out of 58 patients achieving minimal residual disease negativity [104]. With a median follow-up of 13.5 months, the estimated 1-year overall survival was 73.6%, demonstrating durable responses in heavily pretreated patients [104].
Allogeneic CAR-Ts show promising efficacy but face challenges with persistence due to host versus graft (HvG) reactions [102] [105]. While early clinical trials demonstrate the feasibility of this approach, persistence and long-term efficacy data remain areas of active investigation. The use of allogeneic CAR-Ts presents opportunities for multi-antigen targeting and combination CAR approaches that may enhance efficacy against heterogeneous tumors [102].
Table 1: Clinical Efficacy and Response Comparison
| Parameter | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| Complete Remission Rate (B-ALL) | 70-93.1% [104] | Under investigation |
| 1-Year Overall Survival (B-ALL) | 73.6% [104] | Limited long-term data |
| Manufacturing Failure Rate | 2-10% [103] [105] | Varies by donor and editing technology |
| Persistence | Long-term (BCA >616 days) [104] | Limited by host immune rejection |
| T-cell Fitness | Variable (patient-dependent) [26] | Consistent (healthy donor source) [103] |
Safety Profile and Adverse Events
Both autologous and allogeneic CAR-T therapies share class-effect toxicities, including cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) [102] [103]. In the hCART19 trial, severe CRS (grade ≥3) developed in 36% of patients and severe neurotoxicity in 5% of patients, with all toxicities being reversible [104].
Allogeneic CAR-T introduces unique safety concerns, primarily graft-versus-host disease (GVHD), where donor T-cells attack recipient tissues [102] [103]. Strategies to mitigate GVHD include gene editing technologies (CRISPR/Cas9, TALEN, ZFN) to disrupt the T-cell receptor (TCR) and selection of alternative cell sources with reduced alloreactivity [102] [103] [105].
Table 2: Safety and Adverse Event Profile
| Safety Parameter | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| CRS (Severe, Grade ≥3) | 36% of patients [104] | Similar profile expected |
| Neurotoxicity (Severe) | 5% of patients [104] | Similar profile expected |
| GVHD Risk | Not applicable | Significant concern requiring mitigation [102] |
| Host vs. Graft Reaction | Not applicable | Primary limitation affecting persistence [105] |
| Mitigation Strategies | Toxicity management protocols | TCR disruption, HLA matching, cell source selection [102] [105] |
Manufacturing and Accessibility
Production Workflows and Challenges
The fundamental distinction between autologous and allogeneic CAR-T therapies lies in their manufacturing workflows, which directly impact production time, cost, and scalability.
Autologous manufacturing faces significant logistical challenges, with vein-to-vein times typically ranging from 2 to 4 weeks [26]. This delay can be problematic for patients with aggressive diseases who may deteriorate during the waiting period [26]. The centralized production model strains finite manufacturing resources even in developed countries, making patient access infeasible for most of the developing world [26].
Allogeneic manufacturing offers the advantage of decoupling cell collection from treatment administration, enabling immediate product availability [103] [105]. This off-the-shelf approach allows a single manufacturing run to produce doses for multiple patients, significantly improving scalability [103].
Cost and Market Considerations
The current costs of commercially manufactured autologous CAR-T products total nearly $500,000 USD, in addition to other clinical costs, presenting a major burden on healthcare systems [26]. This high cost is prohibitive for most populations in the developing world [26].
Allogeneic CAR-T therapies have the potential to reduce costs through scaled production and economies of scale [103] [105]. A single manufacturing run can produce doses for multiple patients, distributing the fixed manufacturing costs across more treatments [103].
Table 3: Manufacturing and Accessibility Comparison
| Parameter | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| Vein-to-Vein Time | 2-4 weeks [26] | Immediate (off-the-shelf) [103] |
| Production Model | Single-patient batches [26] | Multi-patient batches [103] |
| Product Cost | ~$500,000 [26] | Potential for significant reduction [103] |
| Scalability | Limited by patient-specific manufacturing | High (banked cells) [103] |
| Manufacturing Failure Impact | Treatment deprivation for specific patient [105] | Loss of batch affecting multiple patients |
Research Protocols and Methodologies
Autologous CAR-T Manufacturing Protocol
Objective: To manufacture clinical-grade autologous CAR-T cells targeting CD19 for treatment of B-cell malignancies.
Materials:
- Leukapheresis product from patient
- CD3/CD28 activation beads
- Lentiviral vector encoding CAR construct
- X-VIVO 15 serum-free medium
- Recombinant human IL-2
- Cell culture reagents and supplements
Procedure:
- Cell Collection & Transportation: Collect PBMCs via leukapheresis. Transport in stringent cold chain system (2-8°C for fresh products or below -150°C for cryopreserved products) [26].
- T-cell Enrichment & Activation: Isolate T-cells from PBMCs. Activate using CD3/CD28 antibodies overnight [26] [104].
- Genetic Modification: Transduce activated T-cells with lentiviral vector at multiplicity of infection 1:10 ratio [104].
- Ex Vivo Expansion: Culture transduced cells in X-VIVO 15 serum-free medium with 300 IU/mL interleukin-2 for 5-8 days [104].
- Harvesting & Formulation: Harvest expanded CAR-T cells, wash, and formulate in appropriate infusion medium.
- Quality Control Testing: Perform release testing including sterility, viability, transduction efficiency, and potency assays. Release typically takes 2-3 weeks [26].
Expected Outcomes: Mean lentiviral CAR gene transfer efficiency of approximately 48.9% (range 8.2%-89.7%) with CD4:CD8 ratio of approximately 5.91 [104].
Allogeneic CAR-T Manufacturing with TCR Disruption
Objective: To manufacture allogeneic CAR-T cells from healthy donor PBMCs with disrupted TCR to prevent GVHD.
Materials:
- Leukapheresis product from healthy donor
- CRISPR/Cas9 system with TCR-targeting guide RNA
- Lentiviral or retroviral vector encoding CAR construct
- T-cell culture media and supplements
- Electroporation system
Procedure:
- Donor Selection & Cell Collection: Select HLA-matched healthy donor. Collect PBMCs via leukapheresis [105].
- TCR Disruption: Isolate T-cells. Disrupt TCR α constant (TRAC) locus using CRISPR/Cas9 gene editing via electroporation [102] [103].
- CAR Transduction: Transduce TCR-disrupted T-cells with viral vector encoding CAR construct [105].
- Selection & Expansion: Expand successfully edited and transduced cells under appropriate culture conditions.
- Banking & Cryopreservation: Create master and working cell banks. Cryopreserve multiple doses for future use [105].
- Quality Control: Test for TCR expression, CAR expression, sterility, viability, and editing efficiency.
Expected Outcomes: TCR-negative CAR-T cells with minimal risk of GVHD, suitable for multiple patients.
Technology Platforms and Engineering Strategies
Engineering Approaches for Allogeneic CAR-Ts
The development of effective allogeneic CAR-T products requires sophisticated engineering strategies to overcome immunological barriers.
Gene editing technologies are crucial for developing allogeneic CAR-T products. CRISPR/Cas9 has emerged as a powerful tool for disrupting endogenous TCR genes to prevent GVHD [102] [103]. Additional edits may include ablation of HLA class I molecules to reduce host rejection, though this must be balanced against potential NK cell-mediated clearance [102].
Alternative cell sources such as umbilical cord blood (UCB) and induced pluripotent stem cells (iPSCs) offer advantages for allogeneic CAR-T production. UCB-derived T-cells have reduced NF-κB activation and pro-inflammatory cytokine production, resulting in lower GVHD incidence and severity [103] [105]. iPSCs provide a renewable cell source with potential for homogeneous genetic modification [103] [105].
Automated Manufacturing Systems
Both autologous and allogeneic CAR-T production benefit from automated closed-system technologies such as the CliniMACS Prodigy and Lonza Cocoon platforms [26]. These systems integrate multiple manufacturing steps into a single-use disposable kit, reducing hands-on time and improving consistency [26]. Automated systems enable decentralized manufacturing at point-of-care facilities, potentially increasing patient access while maintaining quality standards [26].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for CAR-T Development
| Reagent/Category | Function | Examples/Applications |
|---|---|---|
| Cell Separation | T-cell isolation from apheresis product | CD3/CD28 magnetic beads for activation [26] [104] |
| Gene Delivery Vectors | CAR gene insertion into T-cells | Lentiviral, retroviral vectors; Non-viral transposon systems [26] |
| Gene Editing Tools | TCR disruption for allogeneic CAR-Ts | CRISPR/Cas9, TALEN, ZFN systems [102] [103] |
| Cell Culture Media | T-cell expansion and maintenance | X-VIVO 15 serum-free medium [104] |
| Cytokines | T-cell growth and survival | Recombinant human IL-2 (300 IU/mL) [104] |
| Quality Control Assays | Product characterization and release | Flow cytometry (transduction efficiency), sterility testing, potency assays [26] |
The choice between autologous and allogeneic CAR-T approaches involves balancing multiple factors including efficacy, safety, manufacturing complexity, and accessibility. Autologous CAR-T therapy has demonstrated remarkable success in hematologic malignancies but faces challenges related to manufacturing time, cost, and scalability. Allogeneic CAR-T therapy offers the potential for off-the-shelf availability and reduced costs but must overcome immunological barriers including GVHD and host-mediated rejection.
Future development in the field will likely focus on optimizing gene editing strategies for allogeneic products, improving manufacturing technologies for both approaches, and expanding applications beyond hematologic malignancies to solid tumors and autoimmune diseases [56] [101]. The integration of artificial intelligence and automation in manufacturing holds promise for enhancing consistency and reducing costs, potentially making CAR-T therapy more accessible to broader patient populations [101].
Chimeric Antigen Receptor (CAR) T-cell therapy has emerged as a revolutionary treatment for hematologic malignancies. However, its rapid expansion and development of new indications have revealed significant challenges in manufacturing and analytical methodologies. The autologous nature of these therapies, where products are manufactured for each individual patient, introduces inherent variability that can impact product quality, clinical efficacy, and patient safety. Within the European Union, initiatives like the T2EVOLVE consortium have emerged to address these critical gaps. Established under the Innovative Medicines Initiative (IMI), T2EVOLVE represents a public-private partnership comprising 27 European partners from nine countries, including universities, research organizations, pharmaceutical companies, and regulatory authorities [106] [107]. Its mission is to accelerate the development of engineered T-cell therapies by bridging the gap between research and clinical application, with a core objective of harmonizing analytical methods across the therapy's lifecycle [108]. This application note details the current landscape of CAR T-cell production heterogeneity, summarizes key findings from European surveys, and provides standardized protocols to advance harmonization in this promising field.
European Landscape and the Urgency for Harmonization
A recent extensive survey conducted by the T2EVOLVE consortium between February and June 2022 provides a quantitative snapshot of the current state of CAR T-cell analytical methods across Europe. The survey, comprising 36 questions and completed by 53 respondents from 13 European countries, highlighted significant variability in practices from apheresis to post-infusion immunomonitoring [108]. This lack of standardization impedes the comparability of clinical data and poses a barrier to broader patient access.
Table 1: Key Findings from the T2EVOLVE European Survey on CAR T-Cell Analytical Methods
| Survey Aspect | Key Finding | Implication for Harmonization |
|---|---|---|
| Geographic Distribution | Majority of responses from Italy (30%), France (17%), and Germany (17%); lower representation from UK and Spain [108]. | Highlights disparities in CAR T-cell expertise and access across Europe, underscoring the need for inclusive harmonization efforts. |
| Drug Product Characterization | Only a minority of respondents conducted comprehensive phenotypical characterization of T-cell subsets or assessed T-cell activation/exhaustion profiles [108]. | Identifies a critical gap in understanding critical quality attributes (CQAs) that impact product efficacy and persistence. |
| Post-Infusion Monitoring | Significant variability in CAR T-cell monitoring during short-term patient follow-up across different clinical centers [108]. | Hinders the ability to correlate product attributes with clinical outcomes, such as response, relapse, and toxicity. |
| Primary Identified Need | Urgent necessity to standardize CAR T-cell functional potency assays and identify predictive biomarkers [108]. | Pinpoints a foundational area where consensus is required to enable reliable product comparison and potency assessment. |
The data confirms that the field has matured to a point where the lack of harmonization is a key bottleneck. The findings from this survey have provided a prioritized list of areas requiring standardization, guiding subsequent initiatives from T2EVOLVE and other consortia [108].
Consortium-Led Initiatives: Driving Standardization Forward
In response to the identified gaps, consortium-led efforts are actively developing frameworks to harmonize practices. Two key examples are T2EVOLVE and the UNITC consortium, each contributing to different aspects of the production and control paradigm.
The T2EVOLVE consortium is leveraging the existing EU regulatory framework to propose more efficient development pathways. A key recommendation is the "parent-child" approach for Investigational New Drug (IND) applications. This strategy allows for the study of multiple versions of a CAR or TCR-engineered T-cell product within a single early-phase clinical trial framework. By treating a well-characterized product as the "parent," subsequent "child" products with minor modifications (e.g., altered co-stimulatory domains or new scFvs) can be tested without requiring completely new, duplicative regulatory submissions. This facilitates an iterative, adaptive learning process, accelerating innovation while maintaining regulatory oversight [109].
Parallelly, the UNITC consortium's Bioproduction Working Group has focused on harmonizing Quality Control (QC) tests for the academic production of autologous CAR-T cells. Their position paper provides specific recommendations for critical release tests, which are vital for ensuring consistent product quality and safety, especially under the hospital exemption pathway for Advanced Therapy Medicinal Products (ATMPs) [110]. The academic production model offers advantages such as faster, more cost-effective production and the use of fresh cells, but requires robust, standardized QC processes to be scalable and successful [110].
Table 2: Overview of Key Consortium-Led Harmonization Efforts
| Consortium | Primary Focus | Key Outputs & Recommendations |
|---|---|---|
| T2EVOLVE [108] [109] [107] | Accelerating clinical development and predictive tool development. | - European survey identifying variability and gaps.- "Parent-child" IND approach for multiple product versions.- Delivery of predictive markers for efficacy/toxicity. |
| UNITC Bioproduction WG [110] | Harmonizing QC for academic (point-of-care) CAR-T production. | - Standardized protocols for critical quality control tests (e.g., mycoplasma, endotoxin, VCN).- Recommendations for potency assay standardization. |
These initiatives demonstrate a multi-faceted approach to harmonization, addressing both the regulatory workflow for faster development and the technical requirements for consistent product quality.
Experimental Protocols for Harmonized Quality Control
To translate strategic harmonization goals into practical application, the following section details standardized protocols for key quality control assays, as recommended by the UNITC consortium [110]. Implementing these methods will enhance comparability across different manufacturing sites.
Protocol for Mycoplasma Detection
Principle: Mycoplasma contamination is a critical safety concern for cell-based products. While the pharmacopeial method requires 28 days, nucleic acid amplification techniques (NAT) offer a rapid and validated alternative suitable for products with short shelf-lives [110]. Procedure:
- Sample Preparation: Collect at least 2 mL of cell culture supernatant or a cell suspension from the final CAR T-cell product.
- DNA Extraction: Use a commercial DNA extraction kit that has been validated for the specific sample matrix. The extraction method must be compatible with the subsequent amplification kit.
- Amplification & Detection: Use a commercially available, validated NAT kit (e.g., based on PCR). The kit must be validated to detect a panel of mycoplasma strains (e.g., M. orale, M. arginini, M. hyorhinis, A. laidlawii) with a sensitivity of at least 10 CFU/mL.
- Controls: Include a negative control (nuclease-free water) and a positive control (a kit-supplied mycoplasma DNA) in each run.
- Interpretation: A valid test requires the positive control to show amplification and the negative control to show no amplification. The test sample is negative for mycoplasma if no amplification signal is detected.
Protocol for Endotoxin Testing
Principle: Endotoxins, derived from gram-negative bacteria, can cause pyrogenic reactions in patients. The Limulus Amebocyte Lysate (LAL) or recombinant Factor C (rFC) assays are employed for quantification [110]. Procedure:
- Sample Preparation: Dilute the CAR T-cell product sample appropriately to overcome matrix interference, which is common in cell-based products. Validation is required to determine the optimal dilution factor.
- Assay Setup: Use a kinetic chromogenic LAL or rFC assay according to the manufacturer's instructions. The rFC assay is an animal-free alternative with comparable performance.
- Standard Curve: Prepare a series of endotoxin standards (e.g., from 0.005 to 50 EU/mL) to generate a standard curve.
- Spike Recovery (for validation): To demonstrate the assay is suitable for the product matrix, perform a spike recovery test by adding a known amount of endotoxin to the sample. Recovery should typically be within 50-200%.
- Interpretation: The endotoxin level in the product must be below the specified limit, as defined by regulatory guidelines (e.g., 5 EU/kg/hr).
Protocol for Vector Copy Number (VCN) Quantification
Principle: VCN assesses the average number of CAR transgene copies integrated into the genome of the final product, which is critical for evaluating genetic stability and potential genotoxicity [110]. Procedure:
- Genomic DNA (gDNA) Extraction: Isolate high-quality gDNA from the CAR T-cell product using a commercial kit. Determine the DNA concentration and purity (A260/A280 ratio ~1.8).
- Standard Preparation: Prepare a standard curve using a plasmid of known concentration containing the CAR transgene sequence. Serially dilute the plasmid to create a standard curve covering the expected dynamic range (e.g., 10 to 10^6 copies).
- Quantitative PCR (qPCR) or Digital Droplet PCR (ddPCR):
- qPCR: Perform reactions in triplicate using primers and a probe specific to the CAR transgene and a reference gene (e.g., RNase P). Calculate the VCN using the formula:
VCN = (CAR gene copy number) / (reference gene copy number / 2). - ddPCR: This method partitions the sample into thousands of droplets, providing absolute quantification without a standard curve and is often more robust against PCR inhibitors.
- qPCR: Perform reactions in triplicate using primers and a probe specific to the CAR transgene and a reference gene (e.g., RNase P). Calculate the VCN using the formula:
- Acceptance Criteria: The validated assay should have a limit of detection and quantification defined. The VCN for the batch must be within the pre-defined specification established during product development.
Protocol for Potency Assay via IFN-γ ELISA
Principle: Potency is a critical quality attribute reflecting the biological function of the product. A standardized method involves antigen-specific stimulation followed by quantification of IFN-γ release [110]. Procedure:
- CAR T-Cell Stimulation:
- Positive Control: Co-culture a defined number of CAR T-cells (e.g., 1x10^5) with target cells expressing the cognate antigen (e.g., CD19+ cells) at an effector-to-target ratio (e.g., 1:1).
- Negative Control 1: Co-culture CAR T-cells with target cells not expressing the antigen.
- Negative Control 2: Culture CAR T-cells alone.
- Incubate for 18-24 hours at 37°C, 5% CO2.
- Supernatant Collection: Centrifuge the co-culture plates and carefully collect the supernatant.
- IFN-γ ELISA: Use a commercial IFN-γ ELISA kit. Add supernatant to the antibody-coated plate, followed by the detection antibody, enzyme conjugate, and substrate according to the kit protocol.
- Quantification: Measure the absorbance and determine the IFN-γ concentration in the samples by interpolating from the standard curve.
- Interpretation: The potency is demonstrated by a significant, antigen-specific release of IFN-γ in the positive control well compared to the negative controls.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and their functions essential for conducting the harmonized QC assays described above.
Table 3: Research Reagent Solutions for Core Quality Control Assays
| Reagent / Kit | Function / Application | Key Characteristics |
|---|---|---|
| Validated NAT Mycoplasma Kit [110] | Rapid, sensitive detection of mycoplasma contamination. | Validated per Ph. Eur. 2.6.7; detects recommended strains; high specificity to prevent false positives. |
| LAL or rFC Endotoxin Assay Kit [110] | Quantification of bacterial endotoxins for patient safety. | Kinetic chromogenic method; validated to avoid matrix interference; rFC is an animal-free alternative. |
| gDNA Extraction Kit | Isolation of high-quality genomic DNA for VCN analysis. | High yield and purity; removes PCR inhibitors; compatible with downstream qPCR/ddPCR. |
| qPCR/ddPCR Reagents | Quantification of vector copy number (VCN) and reference genes. | qPCR: Requires specific primers/probes, standard curve. ddPCR: Provides absolute quantification, high resilience to inhibitors. |
| IFN-γ ELISA Kit [110] | Measurement of IFN-γ secretion as a surrogate for CAR T-cell potency. | High specificity and sensitivity; pre-coated plates for ease of use; includes standards for accurate quantification. |
| Antigen-Positive Target Cell Line | Used in potency assays for antigen-specific stimulation of CAR T-cells. | Stably expresses the target antigen (e.g., CD19) at a consistent level; ensures reproducible stimulation. |
Visualizing the Harmonization Framework
The following diagram illustrates the interconnected ecosystem and workflow driving CAR T-cell therapy harmonization, as championed by consortia like T2EVOLVE and UNITC.
Diagram 1: The CAR T-Cell Harmonization Framework. This diagram outlines the structured approach from problem identification to ultimate outcome, driven by consortium initiatives producing both strategic and technical outputs.
The push for harmonization in autologous CAR T-cell production, led by European surveys and global consortia, is a critical endeavor to ensure the therapy's full potential is realized. The quantitative data from the T2EVOLVE survey provides an unambiguous baseline, revealing significant variability in analytical methods that hinders progress [108]. The concerted efforts of consortia to establish standardized QC protocols [110] and more efficient regulatory frameworks [109] are foundational steps toward overcoming these challenges. The future of CAR T-cell therapy will be shaped by continued collaboration, the adoption of these harmonized practices, and the integration of next-generation technologies like AI-driven automation and point-of-care manufacturing [111] [112]. By adhering to a common framework for product characterization and quality control, researchers and drug development professionals can enhance product comparability, improve clinical outcomes, and ultimately accelerate the delivery of these transformative therapies to a broader patient population.
Conclusion
Autologous CAR T-cell production represents a remarkable fusion of scientific innovation and bespoke medicine, demonstrating curative potential for patients with refractory cancers. The process, from foundational CAR biology to a complex multi-step manufacturing workflow, continues to be refined through strategies that optimize T-cell subsets, mitigate exhaustion, and reduce immunogenicity. However, challenges in scalability, cost, and product variability persist, highlighting an urgent need for standardized analytical methods and quality controls. Looking forward, the field is poised for transformation through increased automation, point-of-care manufacturing models, and sophisticated genetic engineering. While allogeneic 'off-the-shelf' products emerge as a promising alternative, autologous therapies will likely remain crucial, especially as their production becomes more efficient and accessible, ultimately expanding this powerful modality to a broader range of patients and diseases.
References
- 1. Scalable Manufacturing of CAR for Cancer Immunotherapy... T Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC8462122/]
- 2. - Autologous Manufacturing: CAR Standing and Future... T Cell Current [https://www.genengnews.com/insights/autologous-car-t-cell-manufacturing-current-standing-and-future-directions/]
- 3. CAR T-cell detection scoping review: an essential biomarker in ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC10230989]
- 4. What Are The Key Points Of CAR Therapy? | Cyagen APAC T Cell [https://apac.cyagen.com/community/technical-bulletin/car-t-cell-therapy-key-points.html]
- 5. Frontiers | Lymphocytes in Cellular Therapy: Functional Regulation of CAR T Cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.03180/full]
- 6. CAR-T cell manufacturing: Major process parameters and next-generation strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10791545/]
- 7. The structure of CAR - T - ProteoGenix cells [https://www.proteogenix.science/scientific-corner/car-t/car-t-structure/]
- 8. - CAR therapy: developments, challenges and expanded... T cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11754230/]
- 9. CAR-T design: Elements and their synergistic function - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2352396420303078]
- 10. Frontiers | Non- signaling but all important: how the linker, hinge , and... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1664403/full]
- 11. Hinge and Transmembrane Domains of Chimeric Antigen Receptor Regulate Receptor Expression and Signaling Threshold - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7291079/]
- 12. Accelerating and optimising CAR T-cell manufacture to deliver better patient products - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2352302624002734]
- 13. Tracing the development of CAR-T cell design: from concept to next-generation platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326545/]
- 14. - CAR Cell Therapy Market Research 2024- T : Size, Forecasts... 2025 [https://www.businesswire.com/news/home/20250106985719/en/CAR-T-Cell-Therapy-Market-Research-2024-2025-Size-Forecasts-Trials-and-Trends---Approved-CAR-T-Therapies-and-Late-stage-Clinical-Trials-that-Could-Reach-Commercialization-Soon---ResearchAndMarkets.com]
- 15. - CAR Cell Therapy Market Research 2024- T : Navigating the... 2025 [https://finance.yahoo.com/news/car-t-cell-therapy-market-090900250.html]
- 16. ASTCT’s Leadership Contributes to FDA Decision to... - PharmiWeb.com [https://www.pharmiweb.com/press-release/2025-07-01/astct-s-leadership-contributes-to-fda-decision-to-eliminate-rems-for-bcma-and-cd19-directed-autolog]
- 17. FDA Eliminates Risk Evaluation and Mitigation Strategies... | FDA [https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/fda-eliminates-risk-evaluation-and-mitigation-strategies-rems-autologous-chimeric-antigen-receptor]
- 18. Surveying local CAR T-cell manufacturing processes to facilitate standardization and expand accessibility | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06400-x]
- 19. -cell Therapy - Pipeline Insight, CAR T 2025 [https://www.researchandmarkets.com/reports/5337994/car-t-cell-therapy-pipeline-insight-2025]
- 20. Accelerating CAR T cell manufacturing with an automated next-day process - PubMed [https://pubmed.ncbi.nlm.nih.gov/39705851/]
- 21. Quick Primer | Top 5 Uses for CAR - T Proteins in Target 2025 [https://www.linkedin.com/pulse/quick-primer-top-5-uses-car-t-target-proteins-2025-mqdaf]
- 22. Preclinical Evaluation of Allogeneic CAR Cells Targeting T for... BCMA [https://pubmed.ncbi.nlm.nih.gov/31005597/]
- 23. - CAR Therapy for Multiple Myeloma Pipeline Insight, T Cell 2025 [https://www.linkedin.com/pulse/car-t-cell-therapy-multiple-myeloma-pipeline-insight-2025-gaurav-bora-xynqc]
- 24. CAR-T cell therapy for cancer: current challenges and future directions | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02269-w]
- 25. Harnessing the potential of CAR - T therapy: progress, cell ... challenges [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04292-3]
- 26. Promises and challenges of a decentralized CAR - T manufacturing... cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11235344/]
- 27. Current challenges and therapeutic advances of CAR-T cell therapy for solid tumors | Cancer Cell International | Full Text [https://cancerci.biomedcentral.com/articles/10.1186/s12935-024-03315-3]
- 28. Optimizing CAR-T cell therapy for solid tumors: current challenges and potential strategies | Journal of Hematology & Oncology | Full Text [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-024-01625-7]
- 29. Improving CAR T Cell Therapy by Optimizing Critical Quality Attributes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7518470/]
- 30. Buffy Coat vs Leukapheresis : Which Yields More PBMCs ? [https://cgt.global/buffy-coat-vs-leukapheresis-choosing-the-right-cell-source-for-your-research/]
- 31. : A powerful research tool | AllCells PBMCs [https://allcells.com/pbmcs-a-powerful-research-tool/]
- 32. The impact of leukapheresis on immune-cell number and function in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6596285/]
- 33. Leukopak PBMC Sample Processing for Preparing Quality Control Material to Support Proficiency Testing Programs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4138237/]
- 34. CAR T Cell Expansion and Activation | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/car-t-cell-therapy-role-t-cells-expansion-quality.html]
- 35. Identification of the conditions and minimum requirements necessary... [https://www.nature.com/articles/s41409-024-02504-y?error=cookies_not_supported&code=148da357-93af-4d82-a3fb-6a7b2c3dc3f4]
- 36. Frontiers | Opto-CD28-REACT: optogenetic co-stimulatory receptor... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1646135/full]
- 37. An optimized flow cytometry protocol for simultaneous detection of T cell activation induced markers and intracellular cytokines: Application to SARS-CoV-2 immune individuals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957341/]
- 38. Human Activated T Cell Markers Flow Cytometry Panel | Cell Signaling Technology [https://www.cellsignal.com/products/flow-cytometry-kits-reagents/human-activated-t-cell-markers-flow-cytometry-panel/23428]
- 39. of single copy gene‑based duplex Comparison PCR and... quantitative [https://www.spandidos-publications.com/10.3892/ijo.2022.5338]
- 40. Decentralizing Autologous Therapies with Accelerated... Cell [https://www.thermofisher.com/blog/behindthebench/decentralizing-autologous-cell-therapies-with-accelerated-manufacturing-workflows/]
- 41. Protocol for the simultaneous activation and lentiviral transduction of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11950759/]
- 42. - CAR in a Xuri T ... | SpringerLink Cell Expansion Cell Expansion [https://link.springer.com/protocol/10.1007/978-1-0716-0146-4_11]
- 43. - CAR Using Nonviral Approaches - PMC T Cell Production [https://pmc.ncbi.nlm.nih.gov/articles/PMC8019376/]
- 44. How to manufacture CAR - T - ProteoGenix cells [https://www.proteogenix.science/scientific-corner/car-t/car-t-manufacturing/]
- 45. Non-viral chimeric antigen receptor (CAR) T cells going viral - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10139995/]
- 46. Frontiers | Evaluation of Nonviral piggyBac and lentiviral Vector in Functions of CD19chimeric Antigen Receptor T Cells and Their Antitumor Activity for CD19+ Tumor Cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.802705/full]
- 47. of Human Production -Engineered CRISPR - CAR T Cells [https://www.jove.com/t/62299/production-of-human-crispr-engineered-car-t-cells]
- 48. A versatile system for rapid multiplex genome-edited CAR ... T cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC5370017/]
- 49. delivery of combinatorial Lentiviral /CRISPRi circuit into human... CAR [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02526-2]
- 50. Frontiers | Optimising and adapting perfusion feeds in serum-free... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1593895/full]
- 51. Establishing a scalable perfusion strategy for the manufacture of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079453/]
- 52. Methods and Process Optimization for Large-Scale CAR ... T Expansion [https://link.springer.com/protocol/10.1007/978-1-0716-0146-4_12]
- 53. Platforms for Clinical-Grade CAR - T | Springer Nature... Cell Expansion [https://experiments.springernature.com/articles/10.1007/978-1-0716-0146-4_10?error=cookies_not_supported&code=68e28281-f354-4271-8ffd-20c2d03f15c6]
- 54. CART Autologous Therapy Market... | Intel Market Cell Research [https://www.intelmarketresearch.com/autologous-car-t-cell-therapy-2025-2032-309-4566]
- 55. How Chimeric Antigen Receptor ( CAR )- T Therapy Works — In... Cell [https://www.linkedin.com/pulse/how-chimeric-antigen-receptor-car-t-cell-therapy-9chgf]
- 56. Frontiers | CAR - T therapies in autoimmune rheumatic diseases... cell [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1630569/full]
- 57. “Are They Ready Yet?”: release criteria for autologous CAR T cells | Bone Marrow Transplantation [https://www.nature.com/articles/s41409-024-02482-1]
- 58. in Cryopreservation and Gene Therapy | CGT Global Cell [https://cgt.global/cryopreservation-in-cell-and-gene-therapy-ensuring-high-viability-cells-for-research-manufacturing/]
- 59. Impact of cryopreservation on CAR production and clinical... T [https://pmc.ncbi.nlm.nih.gov/articles/PMC9582437/]
- 60. CAR T cell viability release testing and clinical outcomes: is there a lower limit? - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6872962/]
- 61. Enhancing Speed in CAR - T Manufacturing with Cell Therapy... Cell [https://www.thermofisher.com/blog/behindthebench/enhancing-speed-in-car-t-cell-manufacturing-with-cell-therapy-solutions/]
- 62. : from pathophysiological basics to tumor... T cell exhaustion [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-016-0160-z]
- 63. Frontiers | CAR - T Performance: How to Cell Their... Improve [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.878209/full]
- 64. Frontiers | Analysis of tumor-infiltrating exhausted highlights... T cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1486329/full]
- 65. HIV-1 controllers possess a unique CD8+ T activation cell ... phenotype [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328706]
- 66. for Strategies in Solid Tumors Improving CAR T Cell Persistence [https://pubmed.ncbi.nlm.nih.gov/39199630/]
- 67. - CAR detection scoping review: an essential biomarker in critical... T cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC10230989/]
- 68. Next-Gen CAR - T : Expanding Beyond Blood Cancers Cell Therapy [https://www.medscape.com/viewarticle/next-gen-car-t-cell-therapy-expanding-beyond-blood-cancers-2025a100077o]
- 69. 5 CAR With Autoimmune Readouts in T - BioSpace Cell Therapies 2025 [https://www.biospace.com/drug-development/5-car-t-cell-therapies-with-autoimmune-readouts-in-2025]
- 70. Different Subsets of T , Cells , Effector Functions, and... Memory [https://pmc.ncbi.nlm.nih.gov/articles/PMC4810120/]
- 71. Strategies to enhance CAR-T persistence | Biomarker Research | Full Text [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-022-00434-9]
- 72. JCI Insight - Glioblastoma-targeted CD4+ CAR T cells mediate superior antitumor activity [https://insight.jci.org/articles/view/99048]
- 73. Age related human T evolution and senescence cell subset [https://immunityageing.biomedcentral.com/articles/10.1186/s12979-019-0165-8]
- 74. Frontiers | Advanced Flow Cytometry Assays for Immune Monitoring of CAR-T Cell Applications [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.658314/full]
- 75. Accelerating and optimising - CAR manufacture to deliver better... T cell [https://pubmed.ncbi.nlm.nih.gov/39510106/]
- 76. Enhancing CAR-T cell functionality in a patient-specific manner | Nature Communications [https://www.nature.com/articles/s41467-023-36126-7]
- 77. Application of nanobody ‑based CAR‑T in tumor immunotherapy... [https://www.spandidos-publications.com/10.3892/ijmm.2025.5628?text=fulltext]
- 78. Nanobodies and Nanobody-Based Human Heavy Chain Antibodies As Antitumor Therapeutics - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5702627/]
- 79. and their derivatives: pioneering the future of cancer... Nanobodies [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02270-4]
- 80. Frontiers | Nanobodies and Nanobody -Based Human Heavy Chain... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2017.01603/full]
- 81. Design and Generation of Humanized Single-chain Fv Derived from Mouse Hybridoma for Potential Targeting Application - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4685505/]
- 82. Development and in vitro characterization of a humanized scFv against fungal infections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9621433/]
- 83. Nanobody Engineering: Toward Next Generation Immunotherapies and Immunoimaging of Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6640690/]
- 84. Navigating CAR Regulatory T : Strategy for FDA Approval Challenges [https://www.allucent.com/resources/blog/car-t-therapy-regulatory-strategy-for-fda-approval]
- 85. Frontiers | Toward Rapid, Widely Available Autologous CAR-T Cell Therapy – Artificial Intelligence and Automation Enabling the Smart Manufacturing Hospital [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.913287/full]
- 86. Guide to Cell Therapy GMP Manufacturing for Autologous CAR T [https://www.thermofisher.com/blog/behindthebench/guide-to-cell-therapy-gmp-manufacturing-for-autologous-car-t-and-beyond/]
- 87. Frontiers | Industrializing CAR - T Therapy: Impact of cell ... automation [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1612248/abstract]
- 88. Cost of decentralized CAR T-cell production in an academic nonprofit setting - PubMed [https://pubmed.ncbi.nlm.nih.gov/32535920/]
- 89. : Timing, technology... Automating autologous CAR T manufacturing [https://www.insights.bio/cell-and-gene-therapy-insights/webinars/760/automating-autologous-car-t-manufacturing-timing-technologytransfer-and-the-future-of-operational-efficiency]
- 90. European survey on CAR T-Cell analytical methods from apheresis to... [https://pubmed.ncbi.nlm.nih.gov/40342422/]
- 91. Chromogenic Substrate - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/chromogenic-substrate]
- 92. Single-step, chromogenic Limulus amebocyte lysate assay for endotoxin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC267460/]
- 93. Frontiers | New insights on potency from recent advances and... assays [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 94. T Cell Directed Cytotoxicity & T Cell Activation Assays [https://rouken.bio/capabilities/assays/immune-cell-assays/t-cell-assays]
- 95. analysis of Comparative to measure CAR T cell–mediated... assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC8064272/]
- 96. In vitro CAR-T cell killing: validation of the potency assay - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11219661/]
- 97. A Quantitative Approach to Potency Testing for Chimeric Antigen Receptor-Encoding Lentiviral Vectors and Autologous CAR-T Cell Products, Using Flow Cytometry [https://www.mdpi.com/1999-4923/17/3/303]
- 98. Enhanced cytotoxicity against cholangiocarcinoma by fifth-generation... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06453-y]
- 99. Development of cell-based functional to predict assays ... CAR T cell [https://www.labcorp.com/education-events/posters/development-cell-based-functional-assays-predict-car-t-cell-potency-and-persistence]
- 100. Global CAR-T Cell Market–Size, Forecasts, Trials, & Trends, 2025 [https://bioinformant.com/product/car-t-report/]
- 101. CAR T Cell Therapy Market Size 2025 To 2034 [https://www.precedenceresearch.com/car-t-cell-therapy-market]
- 102. Allogeneic CAR T Cells: An Alternative to Overcome Challenges of CAR T Cell Therapy in Glioblastoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7966522/]
- 103. Frontiers | Allogeneic CART progress: platforms, current progress and... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1557157/full]
- 104. and Safety of efficacy and autologous humanized... allogeneic [https://pmc.ncbi.nlm.nih.gov/articles/PMC9944646/]
- 105. Allogeneic CAR-T Therapy Technologies: Has the Promise Been Met? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814647/]
- 106. Consortium | T2Evolve [https://t2evolve.com/consortium-2/]
- 107. T2EVOLVE | IHI Innovative Health Initiative [https://www.ihi.europa.eu/projects-results/project-factsheets/t2evolve]
- 108. on CAR T-Cell analytical methods from apheresis to... European survey [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058815/]
- 109. Accelerating development of engineered T cell therapies in the EU: current regulatory framework for studying multiple product versions and T2EVOLVE recommendations - PubMed [https://pubmed.ncbi.nlm.nih.gov/38077331/]
- 110. Harmonisation of quality control tests for academic production of CAR-T cells: a position paper from the WP-bioproduction of the UNITC consortium | Bone Marrow Transplantation [https://www.nature.com/articles/s41409-025-02637-8]
- 111. Toward Rapid, Widely Available Autologous CAR-T Cell Therapy - Artificial Intelligence and Automation Enabling the Smart Manufacturing Hospital - PubMed [https://pubmed.ncbi.nlm.nih.gov/35733863/]
- 112. Cost-effective strategies for CAR-T cell therapy manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022644/]