Autologous vs. Allogeneic Cell Therapy: A Comprehensive Efficacy Analysis for Drug Development
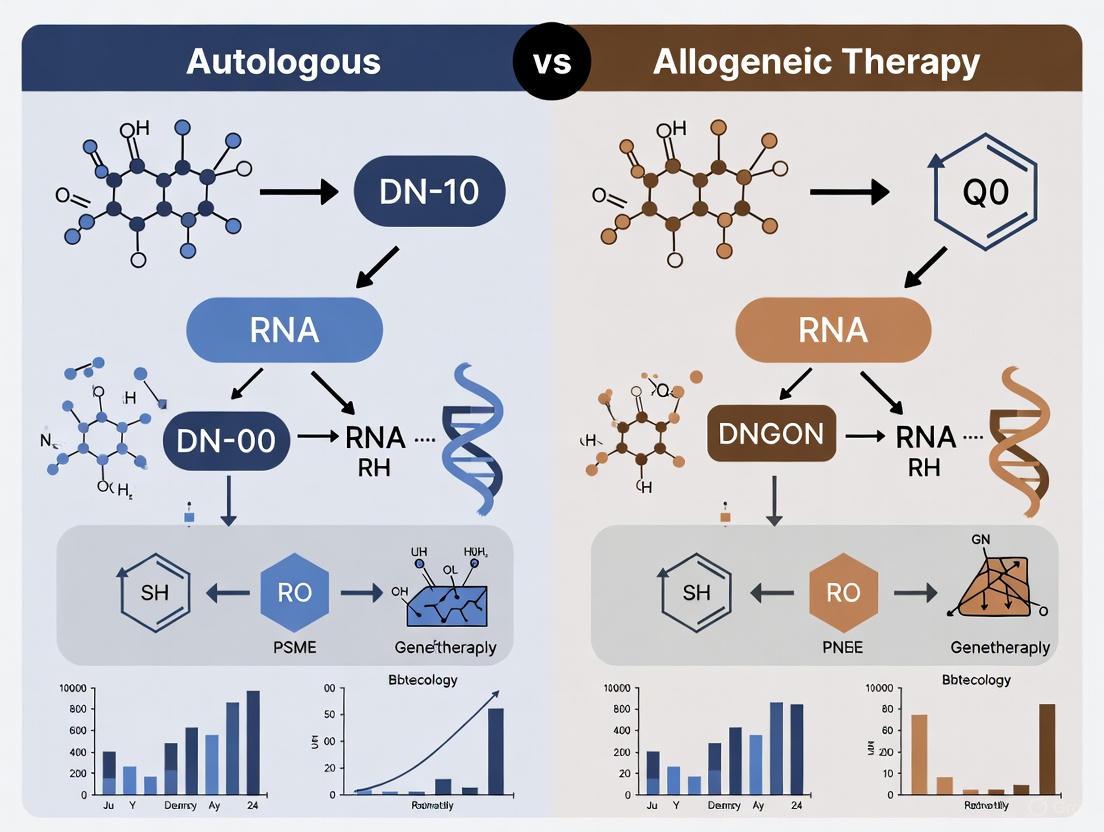
This article provides a comparative analysis of autologous and allogeneic cell therapy efficacy for researchers and drug development professionals.
Autologous vs. Allogeneic Cell Therapy: A Comprehensive Efficacy Analysis for Drug Development
Abstract
This article provides a comparative analysis of autologous and allogeneic cell therapy efficacy for researchers and drug development professionals. It explores the foundational principles, including immunological compatibility and cell sourcing, and examines clinical applications across hematologic malignancies, solid tumors, and autoimmune diseases. The content addresses key manufacturing and safety challenges, such as graft-versus-host disease and product variability, and presents validation strategies through clinical trial data and meta-analyses. Finally, it discusses future directions, including genetic engineering and scalable manufacturing, to guide therapeutic development and clinical implementation.
Defining the Battle: Core Concepts and Biological Mechanisms of Cell Therapies
The development of modern cell therapies is fundamentally guided by the origin of the therapeutic cells, creating a primary division between autologous (self-derived) and allogeneic (donor-derived) approaches. This distinction influences every aspect of therapeutic development, from manufacturing and logistics to clinical efficacy and safety profiles. Autologous cell therapy involves the extraction, manipulation, and reinfusion of a patient's own cells, ensuring perfect immune compatibility but requiring complex, personalized manufacturing [1] [2]. In contrast, allogeneic cell therapy utilizes cells from a healthy donor, enabling "off-the-shelf" availability and mass production but introducing potential immune rejection risks [3] [1]. Within the broader context of therapy efficacy research, understanding these foundational differences is critical for selecting the appropriate therapeutic strategy for specific disease indications and patient populations.
The choice between autologous and allogeneic sources extends beyond mere cell origin; it represents a strategic decision that impacts scalability, cost, treatment timelines, and ultimately, patient access. As the field advances, research continues to address the inherent challenges of both approaches, particularly through genetic engineering and process optimization, to enhance the therapeutic potential of cell-based treatments across a widening spectrum of medical conditions [3] [4].
Fundamental Definitions and Key Characteristics
Autologous Cell Therapy
Autologous cell therapy is a highly personalized treatment modality where cells are harvested from the patient, processed or manipulated ex vivo, and then reinfused back into the same individual [1] [2]. This approach creates a closed, patient-specific system that fundamentally avoids immune rejection, as the treated immune system recognizes the therapeutic cells as "self." A prominent clinical example is Chimeric Antigen Receptor T-cell (CAR-T) therapy for hematological malignancies, where a patient's own T-cells are genetically engineered to target specific cancer cells before being reinfused [2]. Other applications include autologous hematopoietic stem cell transplantation and the use of a patient's somatic cells for reprogramming into induced pluripotent stem cells (iPSCs) for regenerative purposes, such as in Parkinson's disease research [4].
Allogeneic Cell Therapy
Allogeneic cell therapy involves the use of cells derived from a donor who is genetically distinct from the recipient [1]. These cells can come from a matched (HLA-compatible) donor or be developed as universal "off-the-shelf" products from donor cell banks or induced pluripotent stem cell (iPSC) lines [3] [2]. A key advantage is immediate availability, eliminating the weeks-long manufacturing delay associated with autologous therapies, which is a critical factor for acute conditions [2]. Examples include allogeneic hematopoietic stem cell transplants (HSCT) for leukemia and the emerging use of allogeneic CAR-NK cells from cord blood or iPSCs for treating cancer and autoimmune diseases like systemic lupus erythematosus [3] [5]. The primary challenge remains the risk of immune complications, such as graft-versus-host disease (GVHD), where donor immune cells attack the patient's tissues, or host-mediated rejection of the therapeutic cells [1] [4].
Table 1: Core Characteristics of Autologous vs. Allogeneic Cell Therapies
| Characteristic | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [1] | Healthy donor (related/unrelated) [1] |
| Immune Compatibility | High (No rejection risk) [2] | Variable (Risk of GVHD/rejection) [1] |
| Manufacturing Model | Personalized, patient-specific batch [1] | Standardized, "off-the-shelf" batch [3] [1] |
| Typical Production Time | Several weeks [4] | Pre-manufactured, available on demand [2] |
| Scalability | Challenging (Scale-out) [1] | Favorable (Scale-up) [1] |
| Cost Structure | High (Service-based model) [4] | Potentially lower (Mass production) [4] |
Clinical Efficacy and Safety Data
Recent clinical trials provide compelling data on the efficacy and safety profiles of both autologous and allogeneic cell therapies across different disease areas, enabling a more nuanced comparison.
Efficacy Outcomes from Recent Trials
In the oncology domain, a phase 2 trial investigating a novel "sandwich" strategy for Philadelphia chromosome-negative B-cell acute lymphoblastic leukemia (B-ALL) demonstrated the potent efficacy of an autologous approach. The therapy combined sequential CD22/CD19 CAR-T cell therapy with autologous hematopoietic stem cell transplantation (auto-HSCT). With a median follow-up of 28 months, the regimen achieved a remarkable 2-year overall survival rate of 97% and a 2-year leukemia-free survival rate of 72%. Deep molecular remissions were induced, with 80% of patients maintaining continuous measurable residual disease (MRD)-negative status [6].
In the autoimmune field, a 2025 case series from China evaluated an allogeneic CD19 CAR Natural Killer (NK)-cell therapy in patients with relapsed or refractory systemic lupus erythematosus (SLE). The results indicated promising efficacy, with 67% (6 out of 9) of patients with more than 12 months of follow-up attaining DORIS remission and lupus low disease activity state. This suggests that allogeneic CAR-NK therapy can be a potent option for treating autoimmune diseases, potentially addressing the limitations of autologous CAR-T cells [5].
Safety and Tolerability Profiles
The safety profiles of the two approaches also show distinct characteristics. The autologous CAR-T plus auto-HSCT "sandwich" therapy in B-ALL was reported to be well-tolerated. Notably, no instances of severe (grade ≥3) cytokine release syndrome (CRS) or immune effector cell-associated neurotoxicity syndrome (ICANS) were observed. Mild CRS occurred in a subset of patients, and while all patients experienced expected grade 3-4 hematotoxicity, no severe organ toxicity was reported. The study highlighted a non-relapse mortality rate of 0%, which compared favorably to an external allogeneic HSCT control group that had a 15% rate [6].
For the allogeneic CD19 CAR-NK therapy in SLE, the safety profile was also favorable. Cytokine release syndrome was reported in only one (6%) of the 18 patients, and it was low-grade (grade 1). The study reported no observed neurotoxicity, other severe adverse events related to the therapy, or dose-limiting toxicities. This indicates that allogeneic CAR-NK therapy might mitigate some of the significant safety concerns, particularly severe CRS and neurotoxicity, which are known risks associated with autologous CAR-T therapy [5].
Table 2: Comparative Clinical Trial Outcomes in Specific Indications
| Parameter | Autologous Approach (B-ALL) [6] | Allogeneic Approach (SLE) [5] |
|---|---|---|
| Therapy Description | CD22/CD19 CAR-T + Auto-HSCT "Sandwich" | Allogeneic CD19 CAR NK-Cell Therapy |
| Study Design | Phase 2 Trial (n=37) | Case Series (n=18) |
| Key Efficacy Result | 97% 2-year Overall Survival | 67% DORIS Remission (at >12 months) |
| Key Safety Finding | 0% Severe (≥Grade 3) CRS/ICANS | 6% Incidence of Low-Grade (Grade 1) CRS |
| Mortality | 0% Non-Relapse Mortality | Not Reported |
| Notable Risk | Relapse (20%, all CD19+) | No dose-limiting toxicities observed |
Manufacturing and Logistics Comparison
The operational backbone of cell therapies reveals a stark contrast between autologous and allogeneic paradigms, impacting everything from production to patient delivery.
Manufacturing Workflows
The manufacturing journey for autologous therapies is circular and patient-specific. It begins with apheresis at a clinical center to collect the patient's cells, which are then shipped to a manufacturing facility. Here, cells undergo complex, small-scale processes including activation, genetic modification (e.g., viral transduction), expansion, and formulation into a final drug product. This product is cryopreserved and shipped back to the treating hospital for infusion, with the entire "vein-to-vein" time being a critical variable [1] [4]. Each batch is unique to a single patient, requiring rigorous chain-of-identity tracking and adaptable processes to accommodate variability in starting material from sick patients [1].
In contrast, allogeneic manufacturing follows a more linear, scalable path. Cells are sourced from healthy donors, cord blood, or master iPSC banks. The processes—activation, engineering, and expansion—occur at a much larger scale, often in bioreactors, to produce thousands of doses from a single batch. The final "off-the-shelf" products are cryopreserved and stored in inventories, ready for immediate distribution to treating physicians, eliminating the lengthy manufacturing wait [1] [2]. This allows for standardized processes, rigorous quality control on a batch-by-batch basis, and comprehensive pre-release testing [1].
Supply Chain and Scalability
The logistical implications of these two models are profound. The autologous supply chain is a complex, circular network that necessitates robust cold chain logistics, precise scheduling to minimize cell handling times, and an unwavering focus on chain-of-identity to prevent patient-product mix-ups. Scalability is achieved through "scale-out" – establishing multiple, parallel, small-scale production lines, which is capital and resource-intensive [1]. The high degree of personalization, coupled with low utilization of manufacturing capacity per patient, results in a high cost structure, making it a "service-based" model [4].
The allogeneic supply chain is more linear and resembles that of traditional biopharmaceuticals. It allows for bulk processing, long-term storage, and distribution from a central inventory. Scalability is achieved through "scale-up" – using larger bioreactors to produce greater quantities per batch, which leads to economies of scale and a potentially lower cost per dose [1] [4]. This model is financially appealing to the biopharmaceutical industry as it enables broader patient access and more sustainable commercial production [4].
Table 3: Manufacturing and Logistics Comparison
| Aspect | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Supply Chain Model | Circular, patient-specific [1] | Linear, centralized inventory [1] |
| Scalability Strategy | Scale-out (multiple parallel lines) [1] | Scale-up (larger batch sizes) [1] |
| Production Focus | Customization for individual patients [1] | Standardization for patient populations [1] |
| Key Logistical Challenge | Minimizing vein-to-vein time [1] | Managing donor cell variability & quality [1] |
| Cost Drivers | Custom manufacturing, complex logistics [4] | Donor screening, cell banking, immunosuppression [2] [4] |
| Batch Consistency | High variability (patient-derived) [4] | High consistency (donor-screened) [4] |
Experimental Protocols and Research Reagents
Translating cell sources into viable therapies requires specialized experimental workflows and reagents. The following section outlines a core protocol for evaluating allogeneic cell therapies and the essential tools for this research.
Detailed Methodology: Assessing Allogeneic CAR-NK Cell Efficacy & Safety
The following protocol is adapted from a 2025 clinical case series investigating allogeneic CD19 CAR-NK cells in systemic lupus erythematosus [5], providing a template for preclinical assessment of allogeneic therapies.
1. Cell Sourcing and Engineering:
- Cell Source: Isolate NK cells from healthy donor peripheral blood mononuclear cells (PBMCs) or obtain from a cord blood bank or an induced pluripotent stem cell (iPSC) line [3] [5].
- Genetic Modification: Engineer cells using lentiviral or retroviral transduction to express a CD19-targeting Chimeric Antigen Receptor (CAR). The CAR construct typically includes an extracellular anti-CD19 scFv, a transmembrane domain (e.g., CD28 or CD8), and intracellular signaling domains (e.g., CD3ζ plus 4-1BB or CD28) [3].
- Expansion: Cultivate and expand the transduced CAR-NK cells ex vivo in a GMP-compliant facility using media supplemented with cytokines (e.g., IL-2, IL-15) to achieve the target cell dose [5].
2. Preclinical In Vivo Model:
- Animal Model: Utilize immunodeficient mice (e.g., NSG or NOG strains) engrafted with human CD19+ target cells (e.g., B-cell lymphoma lines for oncology or human PBMCs for autoimmune modeling).
- Treatment Groups: Randomize animals into groups receiving: a) allogeneic CAR-NK cells, b) unmodified allogeneic NK cells (control), and c) vehicle only (control).
- Dosing: Administer cells via intravenous injection at a predefined dose (e.g., (0.75 \times 10^9) cells per dose in the clinical study [5]). Multiple doses may be administered.
3. Endpoint Analysis:
- Efficacy: Monitor tumor burden via bioluminescent imaging (oncology) or measure biomarkers of autoimmune activity (e.g., anti-dsDNA antibodies in SLE models) over time. Assess survival and disease remission rates.
- Safety/Toxicity: Monitor animals daily for signs of Cytokine Release Syndrome (CRS; e.g., weight loss, lethargy, hypothermia) and neurotoxicity. Score CRS severity using established grading systems. Upon study termination, analyze blood serum for cytokine levels (e.g., IFN-γ, IL-6) and major organs for histopathological signs of damage or Graft-versus-Host Disease (GVHD) [5].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Cell Therapy Research
| Research Reagent / Solution | Function in Experimental Protocol |
|---|---|
| Lentiviral / Retroviral Vectors | Delivery system for stable genomic integration of CAR transgenes into effector cells (T-cells, NK cells) [2]. |
| Cytokines (e.g., IL-2, IL-15) | Critical components of cell culture media to promote activation, survival, and ex vivo expansion of immune cells [5]. |
| Lymphodepleting Chemotherapy (e.g., Fludarabine, Cyclophosphamide) | Pre-conditioning agents used in vivo to suppress the host immune system, creating a favorable environment for the engraftment and persistence of administered cells [5]. |
| Flow Cytometry Antibodies | Panel of fluorescently-labeled antibodies for characterizing cell phenotypes (e.g., CD3, CD56 for NK cells), confirming CAR expression, and assessing target cell depletion (e.g., CD19+ B-cells) [5] [6]. |
| Cryopreservation Medium | Formulation containing DMSO and serum/proteins to enable long-term storage of cell therapy products in liquid nitrogen without loss of viability or function [1]. |
The comparative analysis of autologous and allogeneic cell sources reveals a landscape of complementary strengths and challenges. The choice between these two foundational paradigms is not a matter of declaring a universal winner but of strategically matching the approach to the clinical and commercial context. Autologous therapies offer the key advantage of immune compatibility, making them powerful for personalized, long-term interventions, as evidenced by high remission rates in B-ALL, albeit with complex logistics and high costs [6] [4]. Allogeneic therapies, conversely, offer the transformative potential of "off-the-shelf" immediacy and superior scalability, with emerging data showing promising efficacy and manageable safety profiles in diseases like SLE, though they must navigate the hurdles of immune rejection [3] [5].
Future directions in efficacy research will likely focus on convergence and optimization. For autologous therapies, efforts are centered on streamlining manufacturing, automating processes, and reducing vein-to-vein time to improve accessibility [1] [4]. For allogeneic therapies, the research frontier involves advanced genetic engineering—using technologies like CRISPR to create "hypoimmune" universal donor cells that evade host immune detection, thereby mitigating the risks of rejection and GVHD without the need for extensive immunosuppression [3] [2]. As both fields evolve, the ongoing synthesis of clinical data and manufacturing innovation will continue to refine these paradigms, ultimately expanding the arsenal of curative treatments available to patients.
The advent of cell-based immunotherapies represents a paradigm shift in cancer treatment, particularly for hematological malignancies. These therapies are broadly categorized into autologous approaches (using the patient's own cells) and allogeneic approaches (using donor-derived cells) [4]. While autologous CAR-T therapies have demonstrated remarkable efficacy, their widespread application is constrained by manufacturing limitations, including lengthy production times, high costs, and significant patient-to-patient variability in product quality [7] [8]. Allogeneic, or "off-the-shelf," cell therapies from healthy donors offer a promising alternative with potential for immediate administration, scalable production, and more consistent product quality [7] [8] [9].
However, the clinical application of allogeneic cell therapies introduces complex immunological challenges, primarily Graft-versus-Host Disease (GvHD) and Host-versus-Graft Reaction (HVGR). GvHD occurs when immunocompetent T cells from the donor graft recognize and attack recipient tissues, while HVGR involves the recipient's immune system rejecting the donor cells [8] [10]. This article provides a comprehensive comparison of these immunological barriers, detailing their underlying mechanisms, experimental approaches for investigation, and current strategies for mitigation within the context of autologous versus allogeneic therapy efficacy.
Immunopathological Mechanisms: A Comparative Analysis
Graft-versus-Host Disease (GvHD) in Allogeneic Transplants
GvHD is a systemic disorder that progresses through a well-defined series of immunological phases, beginning with tissue damage and culminating in targeted organ destruction [7] [10]. The process initiates when conditioning regimens (chemotherapy or radiation) damage host tissues, releasing inflammatory cytokines and activating host Antigen-Presenting Cells (APCs) [11] [10]. Donor T cells are then activated upon encountering alloantigens presented by host APCs, leading to their proliferation and differentiation into inflammatory T-helper cells (Th1, Th17) and cytotoxic T lymphocytes (CTLs) [11]. Finally, these activated effector cells migrate to target organs—primarily the skin, gastrointestinal tract, and liver—causing apoptosis and tissue damage through direct cytotoxicity (perforin/granzyme, Fas/FasL) and cytokine-mediated inflammation [7] [10].
The diagram below illustrates the three-phase pathogenesis of GvHD:
Table 1: Clinical Manifestations and Target Organs in GvHD
| Target Organ | Clinical Manifestations | Histopathological Findings |
|---|---|---|
| Skin | Maculopapular rash (palms, soles, shoulders), pruritus, pain, bullous lesions in severe cases | Vacuolization of epidermis, dyskeratotic bodies, subepidermal cleft formation, dermal-epidermal separation [10] |
| Gastrointestinal Tract | Diarrhea (secretory, may be bloody), abdominal pain, nausea, vomiting, mucositis | Apoptosis of epithelial cells, dilated crypts, crypt destruction, villus atrophy, neutrophilic infiltration [10] |
| Liver | Elevated bilirubin and alkaline phosphatase, hepatomegaly, pale stool/dark urine | Dysmorphic small bile ducts, portal inflammation [10] |
GvHD is clinically categorized as acute (aGvHD) or chronic (cGvHD), distinguished by timing and pathological features. aGvHD typically occurs within 100 days post-transplant and presents as an inflammatory syndrome affecting the skin, GI tract, and liver [11] [10]. It develops in 30-50% of patients receiving transplants from matched related donors [11]. cGvHD, the leading cause of late morbidity, often manifests after 100 days and affects 30-70% of transplant recipients. It presents with heterogeneous, pleomorphic symptoms resembling autoimmune disorders, characterized by tissue inflammation and fibrosis that can lead to permanent organ dysfunction [11].
Host-versus-Graft Reaction (HVGR)
In contrast to GvHD, HVGR occurs when the recipient's immune system recognizes the donor cells as foreign and mounts an immune response to eliminate them [8]. This reaction is primarily mediated by host T cells that remain following lymphodepleting conditioning regimens, as well as host NK cells and antibodies that recognize donor HLA molecules [8]. The consequence of HVGR is rapid clearance of the allogeneic cell therapy, significantly limiting its persistence and therapeutic efficacy in vivo. This presents a major barrier to achieving the long-term durable responses observed with autologous therapies [8].
The Paradox of Autologous GvHD
While GvHD is typically associated with allogeneic transplantation, a clinically and histologically similar syndrome can rarely occur following autologous stem cell transplantation (auto-HCT), with an incidence of approximately 5-20% [12] [13]. The pathophysiology of autologous GvHD (auto-GvHD) is distinct and believed to involve disrupted thymic-dependent immune reconstitution and a failure to reestablish peripheral self-tolerance, leading to an "auto-aggression" syndrome [12]. This condition most commonly affects the skin and is frequently associated with multiple myeloma and specific induction therapies like bortezomib, which may induce apoptosis and break self-tolerance [13]. Auto-GvHD is often self-limited or responsive to corticosteroids, though severe, steroid-refractory cases have been reported [12] [13].
Experimental Models and Assessment Methodologies
In Vitro Assays for Evaluating Alloreactivity
Table 2: Key In Vitro Assays for GvHD and Alloreactivity Assessment
| Assay/Model | Experimental Setup | Key Readouts | Application in Therapy Development |
|---|---|---|---|
| Mixed Lymphocyte Reaction (MLR) | Co-culture of effector lymphocytes with gamma-irradiated stimulator PBMCs from a different donor [7] | T cell activation (flow cytometry), IFN-γ secretion (ELISA), proliferation, differentiation markers [7] | Measures the potential of donor cells to mount alloreactive response against host antigens; used to validate efficacy of TCR knockout [7] |
| Organoid & 3D Tissue Models | Intestinal or colonic organoids derived from pluripotent stem cells or tissue-resident stem cells exposed to donor immune cells [7] | Epithelial damage, apoptosis, cytokine profiles, gene expression changes [7] | Provides a more physiologically relevant platform to study tissue-specific GvHD pathogenesis and test protective interventions [7] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for GvHD and Alloreactivity Research
| Research Reagent / Tool | Primary Function in Experimental Protocols |
|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of effector and stimulator cells for MLR assays; used to establish alloreactive potential [7] |
| ELISA Kits (e.g., IFN-γ) | Quantification of pro-inflammatory cytokine release in MLR co-cultures as a measure of T cell activation [7] |
| Flow Cytometry Antibodies | Analysis of T cell activation markers (CD69, CD25), differentiation subsets, and intracellular cytokines [7] |
| CRISPR/Cas9 Systems (e.g., for TRAC) | Genetic disruption of TCRαβ to eliminate alloreactivity while preserving CAR-mediated antitumor function [7] [8] |
| Intestinal Organoid Culture Systems | Modeling human GI tract GvHD in a physiologically relevant ex vivo system for pathogenesis studies [7] |
The experimental workflow for evaluating alloreactivity integrates these tools and models, as shown below:
Mitigation Strategies and Clinical Translation
Engineered Solutions for Allogeneic Cell Therapies
The primary strategy for mitigating GvHD in allogeneic cell products involves genetic disruption of the T-cell receptor (TCR). Since the TCRαβ complex is the primary mediator of alloreactivity, its elimination prevents donor T cells from recognizing host antigens while preserving CAR-mediated antitumor activity [7] [8]. The most efficient approach involves knocking out the T cell receptor Alpha Constant (TRAC) gene using genome-editing technologies like CRISPR/Cas9 or TALENs [7] [8]. This is often combined with magnetic bead depletion to remove any residual TCRαβ+ cells, further reducing alloreactive potential [8]. Alternative approaches include using virus-specific T cells or inherently alloreactive cell types like CAR-NK cells or double-negative T cells (DNTs; CD3+ CD4- CD8-), which have demonstrated potent graft-versus-leukemia effects with minimal GvHD in clinical studies [8].
To address HVGR, strategies include matching donor and recipient HLA profiles and additional genetic engineering of donor cells to reduce their immunogenicity, such as knocking out HLA class I and II molecules [8]. However, these modifications must be balanced against potential impacts on cell persistence and function, as complete TCR ablation has been associated with diminished T cell survival and functional exhaustion upon repeated antigen stimulation [8].
Pharmacological and Cellular Approaches
Pharmacological prophylaxis remains a cornerstone for GvHD prevention, particularly in allogeneic hematopoietic stem cell transplantation. The standard backbone includes calcineurin inhibitors (cyclosporine, tacrolimus) combined with methotrexate [11]. Newer agents like the selective T cell co-stimulation modulator Abatacept have also been approved for aGvHD prophylaxis [11]. For established GvHD, high-dose corticosteroids are first-line treatment, though 40% of patients develop steroid-refractory disease with a poor prognosis [11]. Novel therapeutic options for steroid-refractory GvHD include ruxolitinib (JAK1/2 inhibitor), ibrutinib (BTK inhibitor), and belumosudil (ROCK2 inhibitor) [11].
Advanced cellular therapies are also emerging as promising interventions. Decidua stromal cells (DSCs) have shown improved effectiveness over mesenchymal stromal cells in severe aGvHD, with one study reporting a one-year survival rate of 76% in albumin-supplemented DSC-treated patients compared to 20% in the control group [11].
Clinical Trial Outcomes: Autologous vs. Allogeneic
Table 4: Comparative Clinical Outcomes of Autologous and Allogeneic CAR-T Therapies
| Therapy Characteristic | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| Manufacturing Time | Several weeks, leading to treatment delays [7] [4] | Immediate availability ("off-the-shelf"); median 2 days from enrollment to treatment [9] |
| GvHD Risk | Minimal to none (self-tolerance maintained) [4] | Significant risk without mitigation; effectively prevented with TCR knockout [7] [9] |
| Persistence | Potential for long-term persistence (months to years) [7] [4] | May be limited by host immune rejection (HVGR) [8] |
| Clinical Efficacy (LBCL) | High ORR and CR rates in R/R disease [7] | Comparable ORR (67%) and CR (58%) with selected regimen; durable responses observed (median DOR 23.1 months in CR patients) [9] |
| Key Limitations | Product variability, manufacturing failures, T cell exhaustion [7] [8] | Requires genetic engineering, risk of HVGR, potential functional exhaustion with complete TCR ablation [7] [8] |
Recent clinical trials of allogeneic CAR-T products demonstrate promising efficacy and safety. The ALPHA/ALPHA2 trials of cemacabtagene ansegedleucel (cema-cel), an allogeneic anti-CD19 CAR-T product, reported no GvHD across 87 treated patients, confirming the efficacy of TCR knockout strategies [9]. The overall response and complete response rates of 67% and 58%, respectively, with a median duration of response of 23.1 months in complete responders, demonstrate that allogeneic CAR-T cells can induce durable remissions comparable to approved autologous products [9].
The immunological divide between autologous and allogeneic cell therapies is fundamentally defined by the reciprocal threats of GvHD and HVGR. Allogeneic therapies offer substantial practical advantages in scalability and immediate availability but require sophisticated engineering to overcome immunological barriers. Autologous therapies provide a more physiologically compatible option but face limitations in manufacturing and reliability.
Current evidence suggests that genetic engineering approaches, particularly TCR knockout, effectively mitigate GvHD risk in allogeneic products, enabling efficacy comparable to autologous therapies. The emerging clinical data, demonstrating durable responses without GvHD in allogeneic CAR-T trials, signals a promising future for "off-the-shelf" cell therapies. Further research addressing HVGR and enhancing the persistence of allogeneic cells will be crucial to fully realizing the potential of universally accessible cell-based immunotherapies.
The choice of cell source is a foundational decision in biomedical research and therapy development, with significant implications for experimental outcomes and therapeutic efficacy. This guide provides a comparative analysis of three critical cell sources: Peripheral Blood Mononuclear Cells (PBMCs), Umbilical Cord Blood (UCB), and Induced Pluripotent Stem Cells (iPSCs). Framed within the broader context of autologous (patient-specific) versus allogeneic (donor-derived) therapy models, this comparison synthesizes collection methodologies, expansion capabilities, and key performance data to inform selection for research and drug development applications.
The distinction between autologous and allogeneic therapies is a central thesis in modern cell therapy research. Autologous therapies use a patient's own cells, minimizing risks of immune rejection but often involving complex, personalized manufacturing processes [4] [1]. Allogeneic therapies use cells from a healthy donor, enabling "off-the-shelf" availability but requiring careful donor-recipient matching and often immunosuppression to prevent graft-versus-host disease (GvHD) [4] [14].
Within this framework, PBMCs are typically used in an autologous context, UCB is an allogeneic source, and iPSCs can be leveraged for both autologous and allogeneic applications [4] [15]. The following sections provide a detailed, data-driven comparison to guide their use.
The table below summarizes the core characteristics, advantages, and challenges of each cell source, providing a high-level overview for researchers.
| Feature | PBMCs (Peripheral Blood Mononuclear Cells) | Umbilical Cord Blood (UCB) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|---|
| Source & Collection | Collected from peripheral blood via apheresis; minimally invasive [16]. | Collected from umbilical vein post-delivery; non-invasive for donor [17]. | Reprogrammed from somatic cells (e.g., skin fibroblasts, urinary epithelial cells) [18] [15]. |
| Primary Cell Types | Lymphocytes (T-cells, B-cells, NK cells), Monocytes [16]. | Hematopoietic Stem Cells (HSCs), Mesenchymal Stem Cells (MSCs), Endothelial Progenitors [17]. | Pluripotent cells capable of differentiation into any somatic cell type [15]. |
| Proliferation & Expansion Potential | Limited ex vivo expansion; short half-life [4] [16]. | High proliferative capacity; UCB HSCs expand significantly better than PB HSCs [16] [17]. | Virtually unlimited self-renewal capacity [18] [15]. |
| Key Advantages | Readily available from adults; ideal for immunology studies [16]. | Immunologically immature (less stringent HLA matching); high angiogenic potential [17]. | Unlimited source; enables autologous therapies; models human diseases in vitro [18] [15]. |
| Major Challenges | Cellular senescence in culture; donor health/age affects quality [4]. | Limited cell volume per unit; finite resource requiring banking [17]. | Risk of genomic instability during reprogramming; complex differentiation protocols [18] [15]. |
Quantitative Performance Data in Applied Research
The selection of a cell source directly impacts experimental outcomes. The following table consolidates quantitative data from key studies comparing these sources in specific applications, such as hematopoietic differentiation and stem cell therapy.
| Performance Metric | PBMCs | Umbilical Cord Blood | iPSCs | Experimental Context & Citations |
|---|---|---|---|---|
| HSC Proliferation | Baseline (Reference) | Significantly higher (P < 0.0001) | Not Applicable | Expansion of isolated hematopoietic stem cells in vitro [16]. |
| Megakaryocyte Differentiation (CD42b+/CD41+) | 44% ± 9% | 76% ± 11% (P < 0.0001) | Not Applicable | Differentiation efficiency from HSCs to megakaryocytes [16]. |
| Platelet Production Yield | 7.4 PLP*/input cell | 4.2 PLP*/input cell (P = 0.02) | Not Applicable | Yield of platelet-like particles (PLP) under shear flow conditions [16]. |
| Therapeutic Persistence | Limited (Autologous) | Limited (Allogeneic) | High (Maintained characteristics at passage 15) | Long-term culture stability; iPSC-derived MSCs maintained markers vs. UCB-MSCs which started to lose them [18]. |
| Wound Healing/Migration | Variable | Lower | Superior | Migration assay of iPSC-derived MSCs (iMSCs) vs. UCB-MSCs [18]. |
| Immunogenicity Risk | Low (Autologous) | Moderate (Allogeneic, but immune-privileged) | Low (if autologous) to Moderate (if allogeneic) | Risk of graft-versus-host disease (GvHD) or immune rejection [4]. |
Detailed Methodologies and Experimental Protocols
iPSC Generation and Differentiation into MSCs
This protocol, adapted from a 2021 study, details the non-viral generation of iPSCs from urinary epithelial cells and their subsequent differentiation into mesenchymal stem/stromal cells (iMSCs) [18].
- Cell Source and Culture: Urinary epithelial (UE) cells are isolated from 150-200 mL of human urine via centrifugation. The cell pellet is cultured in DMEM complete medium with 15% FBS [18].
- Non-Viral Reprogramming: At ~80% confluence, UE cells are transfected with mRNA encoding the reprogramming factors (OCT4, NANOG, SOX2, KLF4, MYC, LIN28) along with a cocktail of microRNAs using a lipofection agent. This process is repeated for 10 days [18].
- iPSC Colony Selection: From day 9, granulated iPSC colonies appear. Colonies are selected based on TRA1-60 live staining, manually picked, and expanded on Matrigel-coated plates in NutriStem (NS) medium [18].
- Differentiation into iMSCs: Established iPSCs are directed to differentiate into iMSCs using specific culture conditions. The resulting iMSCs are characterized by:
- Trilineage Differentiation: Capacity to form osteocytes, chondrocytes, and adipocytes is confirmed.
- Surface Marker Expression: High expression of CD73, CD90, and CD105 is verified via qRT-PCR and Western blot [18].
Haematopoietic Stem Cell Isolation and Megakaryocyte Culture
This protocol, used for comparing UCB and PB-derived HSCs, focuses on in vitro platelet production [16].
- HSC Isolation:
- UCB: CD34+ cells are isolated using immunomagnetic cell sorting. Red blood cells are first lysed, and mononuclear cells are separated via density-gradient centrifugation with ficoll before the magnetic selection [16].
- PB (Buffy Coats): Buffy coats from donated blood are pooled. A similar immunomagnetic sorting is used, but with adjusted bead-to-cell ratios and additional washing steps due to the lower frequency of HSCs in peripheral blood [16].
- Cell Culture and Differentiation:
- Isolated CD34+ cells are cultured in HP01 medium supplemented with thrombopoietin (TPO), stem cell factor (SCF), and interleukin-3 (IL-3) for 6 days for expansion.
- On day 7, cells are switched to a differentiation medium containing TPO and SCF to direct them towards megakaryocytes.
- On day 12, megakaryocytes are harvested and separated from small particles via a BSA gradient centrifugation [16].
- In Vitro Platelet Production:
- Differentiated megakaryocytes are perfused through custom-built microfluidic flow chambers coated with von Willebrand factor (VWF) under controlled shear stress to mimic physiological platelet release [16].
Visualizing Workflows and Relationships
iPSC Generation and Differentiation Workflow
The diagram below illustrates the key steps involved in creating and differentiating iPSCs, as described in the experimental protocol.
Autologous vs. Allogeneic Cell Therapy Pathways
This diagram outlines the fundamental logistical differences between autologous and allogeneic therapy development, highlighting where PBMCs, UCB, and iPSCs are utilized.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their functions for working with these cell sources, based on the cited methodologies [18] [16].
| Reagent / Material | Function / Application | Cell Source Context |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolation of mononuclear cells (PBMCs, UCB-MNCs) from whole blood or cord blood. | PBMCs, UCB [16] |
| Immunomagnetic CD34+ Beads | Positive selection and isolation of haematopoietic stem cells (HSCs) from heterogeneous cell populations. | UCB, PB (from Buffy Coats) [16] |
| Reprogramming Factor mRNAs | Non-viral induction of pluripotency in somatic cells (e.g., OCT4, SOX2, KLF4, MYC). | iPSCs [18] |
| Lipofectamine Transfection Agent | Delivery of mRNA reprogramming factors into somatic cells. | iPSCs [18] |
| Thrombopoietin (TPO) & Stem Cell Factor (SCF) | Critical cytokines for the expansion and differentiation of HSCs into megakaryocytes. | UCB, PBMCs (for Platelet Production) [16] |
| Matrigel / iMatrix | Basement membrane matrix for coating culture vessels to support pluripotent stem cell attachment and growth. | iPSCs [18] |
| NutriStem (NS) Medium | Xeno-free, defined culture medium optimized for the maintenance of pluripotent stem cells. | iPSCs [18] |
| Flow Cytometry Antibodies (CD34, CD42b, CD41, CD73, CD90, CD105) | Characterization of cell surface markers to identify, quantify, and purify specific cell populations. | All (for HSCs, Megakaryocytes, MSCs) [18] [16] |
The field of advanced therapeutics is increasingly defined by a fundamental distinction between two cellular sourcing strategies: autologous and allogeneic cell therapies. Autologous cell therapy involves the extraction, manipulation, and reinfusion of a patient's own cells, creating a perfectly matched biological product [1] [4]. This approach forms the foundation of current CAR-T (Chimeric Antigen Receptor T-cell) treatments for hematological malignancies, where a patient's T-cells are genetically engineered to target cancer cells [1] [2]. In contrast, allogeneic cell therapy utilizes cells from a healthy donor,
which can be manufactured in large batches, cryopreserved, and made readily available as an "off-the-shelf" treatment for multiple patients [1] [19] [20]. This paradigm encompasses a range of platforms, including donor-derived CAR-T cells, CAR-NK (Natural Killer) cells from cord blood or induced pluripotent stem cells (iPSCs), and mesenchymal stem cell (MSC) therapies [3] [20].
The choice between these models represents a critical strategic decision in therapy development, balancing the personalized immunological safety of autologous products against the scalable, accessible nature of allogeneic therapies. This comparison guide examines the inherent advantages of each approach within the broader context of efficacy research, providing researchers and drug development professionals with a detailed, data-driven analysis to inform platform selection and development pathways.
Comparative Advantage Analysis: Core Characteristics
The following analysis synthesizes key performance indicators and characteristics of autologous versus allogeneic cell therapies, drawing from current clinical trends and manufacturing data.
Table 1: Core Characteristics and Performance Indicators of Autologous vs. Allogeneic Cell Therapies
| Characteristic | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [1] [4] | Healthy donor (related or unrelated) [1] [20] |
| Immunological Compatibility | Inherently compatible; minimal rejection risk [1] [2] | Requires HLA matching/engineering; risk of GvHD and immune-mediated clearance [1] [4] [21] |
| Typical Manufacturing Time | Several weeks [2] [21] | Batch-produced in advance; "off-the-shelf" [19] [20] |
| Scalability | Limited; scale-out for individual patients [1] | High; scale-up for mass production [1] [19] |
| Cost Structure | High-cost, service-based model [1] [4] | Potential for lower cost per dose due to economies of scale [1] [19] |
| Product Consistency | Variable; depends on patient's cell health and prior treatments [19] [4] [21] | High; standardized batches from healthy donors [19] [21] |
| Clinical Trial Dominance (China 2014-2024) | T cells: 51.4% of 206 trials [22] | Emerging area within the T-cell and stem cell trial landscape [3] [22] |
Table 2: Analysis of Key Therapeutic Applications and Targets (Based on Clinical Trial Data from China, 2014-2024)
| Therapy/Disease Area | Prominent Cell Types | Common Targets | Trial Phase Distribution (n=206) |
|---|---|---|---|
| Lymphoma (Top Indication) | T cells (e.g., CAR-T) [22] | CD19 (54.9% of targeted trials) [22] | Phase I: 64.1% (132 trials) [22] |
| Leukemia | T cells, Hematopoietic Stem Cells [22] [20] | CD19, BCMA (9.9%) [22] | Phase II: 32.5% (67 trials) [22] |
| Inflammatory/Autoimmune Diseases | Stem Cells (e.g., MSCs) [22] [20] | N/A (Immunomodulatory) | Phase III: 3.4% (7 trials) [22] |
The Autologous Advantage: Personalized Immunological Safety
Mechanism of Immunological Compatibility
The principal advantage of autologous cell therapy lies in its inherent immunological safety profile. Because the therapeutic cells are derived from the patient's own body, they express the patient's unique human leukocyte antigen (HLA) profile [2]. This self-recognition prevents the host immune system from identifying the infused cells as foreign, thereby eliminating the risk of immune rejection and the life-threatening complications of Graft-versus-Host Disease (GvHD) [1] [4] [2]. In GvHD, immune cells from the donor (the graft) mount an attack on the patient's (the host) tissues, which can manifest as acute or chronic inflammatory conditions affecting the skin, liver, and gastrointestinal tract [4]. The autologous framework naturally circumvents this risk, creating a biologically closed system.
Consequently, patients receiving autologous therapies typically do not require concurrent immunosuppressive regimens [4] [2]. This is a significant clinical advantage, as immunosuppressive drugs carry their own risks, including increased susceptibility to infections, kidney and liver toxicity, metabolic disturbances, and hypertension [4]. The absence of this pharmacological burden allows the engineered cells to proliferate and persist in the patient's body for months or even years, potentially eliciting durable long-term therapeutic responses, which is a hallmark of successful CAR-T therapies in hematological malignancies [4].
Experimental Workflow and Protocol for Autologous CAR-T Generation
The production of autologous cell therapies is a complex, patient-specific workflow that demands rigorous chain-of-identity management and precision. The following diagram and protocol detail the standard methodology for generating autologous CAR-T cells, a cornerstone of the approach.
Detailed Experimental Protocol: Autologous CAR-T Cell Manufacturing
Leukapheresis and Shipment: Peripheral blood mononuclear cells (PBMCs) are collected from the cancer patient via leukapheresis. The apheresis material is shipped cryopreserved or fresh under strict temperature-controlled conditions (typically 4-10°C) to a centralized Good Manufacturing Practice (GMP) facility [1].
T-cell Activation: Upon receipt, T-cells are isolated from the PBMCs using density gradient centrifugation or magnetic bead-based separation (e.g., CD3/CD28 bead selection). The isolated T-cells are then activated ex vivo using antibodies against CD3 and CD28, often conjugated to the magnetic beads, in the presence of specific cytokines like IL-2 [21].
Genetic Modification via Viral Transduction: The activated T-cells are genetically engineered to express the chimeric antigen receptor (CAR). This is most commonly achieved through lentiviral or retroviral vector transduction [22]. The viral vector, containing the CAR transgene, is introduced to the activated T-cells in the presence of enhancers like polybrene or protamine sulfate to increase transduction efficiency. The CAR construct is typically designed to target a specific tumor antigen (e.g., CD19, BCMA) and contains intracellular signaling domains (e.g., CD3ζ, 4-1BB, CD28) for T-cell activation [22] [21].
Ex Vivo Expansion: The transduced T-cells are cultured in a bioreactor system for a period of 7-10 days to expand their numbers to a clinically relevant dose (often in the range of 10^8 to 10^9 cells). This is performed in xeno-free, serum-free cell culture media formulated to support T-cell growth and maintain a favorable phenotype (e.g., less differentiated, memory-like T-cells which are associated with better persistence in vivo) [21]. The use of closed-system bioreactors minimizes contamination risk and supports reproducibility [19] [21].
Formulation, Cryopreservation, and Release Testing: The expanded CAR-T cell product is washed, formulated in a final infusion bag with cryoprotectant (e.g., DMSO), and cryopreserved in the vapor phase of liquid nitrogen. A sample is taken for rigorous Quality Control (QC) release testing, which includes assessments of sterility (bacterial/fungal culture, mycoplasma), viability, cell count and identity, CAR expression (e.g., by flow cytometry), vector copy number, and potency (e.g., in vitro tumor cell killing assay) [1].
Patient Infusion and Monitoring: The cryopreserved product is shipped back to the treatment center, thawed, and infused into the patient after a brief course of lymphodepleting chemotherapy (e.g., fludarabine/cyclophosphamide). Patients are closely monitored for both efficacy and acute toxicities, primarily Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) [2].
The Allogeneic Advantage: Off-the-Shelf Scalability
Mechanisms for Scalable and Accessible Therapeutics
The allogeneic model transforms cell therapy from a bespoke service into a standardized, distributable drug product. Its scalability advantage is multi-faceted, rooted in manufacturing, logistics, and economic principles. By sourcing cells from a single, healthy donor, manufacturers can create a master cell bank (MCB) that serves as a renewable, consistent starting material for thousands of therapeutic doses [19] [20]. This enables mass production in large-scale bioreactors, moving away from the single-patient lots that characterize autologous production [1] [19]. This scale-up strategy, akin to the production of monoclonal antibodies, leverages economies of scale to significantly reduce the cost per dose, making the therapy more financially sustainable for healthcare systems [1] [19].
The "off-the-shelf" nature of these products is perhaps their most transformative characteristic. Unlike autologous therapies, which involve a weeks-long "vein-to-vein" time, allogeneic products are cryopreserved and stored until needed, allowing for immediate treatment upon diagnosis [19] [4]. This is particularly critical for patients with aggressive diseases who cannot endure the wait associated with personalized manufacturing. Furthermore, this model decouples production from the patient, enabling centralized manufacturing hubs to supply a global network of treatment centers, thereby dramatically improving geographic accessibility and helping to overcome "CGT deserts" where advanced therapies are unavailable [19] [23].
Genetic Engineering Workflow for Universal Allogeneic Cells
A key technological enabler for allogeneic therapies is advanced gene editing, which is used to overcome the inherent immunological hurdles of using donor cells. The following diagram and protocol describe the creation of "universal" allogeneic CAR-T cells, a leading platform in the field.
Detailed Experimental Protocol: Generating Universal Allogeneic CAR-T Cells
Donor Screening and T-cell Collection: A healthy donor undergoes rigorous screening for pathogens and communicable diseases. T-cells are collected via leukapheresis. These cells, being treatment-naive and robust, often demonstrate superior expansion and engineering potential compared to cells from pre-treated patients [19] [21].
Gene Editing to Ablate Endogenous T-cell Receptor (TCR): A critical step to prevent GvHD is the knockout of the endogenous αβ T-cell receptor (TCR). This is achieved using gene-editing tools such as CRISPR-Cas9 or TALEN [19] [21]. Ribonucleoprotein (RNP) complexes of Cas9 protein and guide RNAs (gRNAs) targeting the constant regions of the TCRα or TCRβ chain are delivered into the donor T-cells via electroporation. This disruption prevents the donor T-cells from recognizing and attacking the recipient's healthy tissues.
Gene Editing to Evade Host Immune Rejection: To mitigate the risk of the recipient's immune system rejecting the donor cells, HLA class I molecules are often knocked out using similar gene-editing techniques [20]. This makes the donor cells "invisible" to the host's CD8+ T-cells. Some strategies also target HLA class II to avoid CD4+ T-cell mediated rejection. An emerging alternative is the engineering of "hypoimmune" cells from induced pluripotent stem cells (iPSCs), which are genetically modified to modulate immune recognition pathways [24] [2].
Introduction of the Chimeric Antigen Receptor (CAR): The gene-edited T-cells are then engineered to express the CAR, typically via lentiviral vector transduction [3]. This step is analogous to the autologous process but is performed on a much larger scale, using bioreactors capable of producing a single batch for hundreds of patients [19].
Purification and Expansion: Following gene editing and CAR transduction, a purification step (e.g., using magnetic bead-based selection for the CAR+ population) is often employed to remove any remaining unedited or non-transduced cells, ensuring a pure and safe final product [21]. The purified CAR-T cells undergo large-scale expansion in bioreactors to generate a master cell bank, which is then used to create working cell banks for clinical production.
Quality Control, Cryopreservation, and Distribution: The final universal CAR-T cell product undergoes comprehensive QC testing, including checks for editing efficiency (e.g., via next-generation sequencing to confirm TCR knockout), CAR expression, sterility, and potency. The product is then cryopreserved in individual patient doses, creating an inventory of "off-the-shelf" therapies that can be distributed globally and administered on demand [19] [20].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and manufacturing of both autologous and allogeneic cell therapies rely on a sophisticated suite of reagents, instruments, and platforms. The table below details key solutions essential for researchers in this field.
Table 3: Essential Research Reagent Solutions for Cell Therapy Development
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Serum-Free Cell Culture Media | Formulated for ex vivo T-cell/NK cell expansion [21]. | Xeno-free composition critical for regulatory compliance; formulations impact T-cell phenotype and yield [21]. |
| CRISPR-Cas9 or TALEN Systems | Gene-editing tools for TCR and HLA knockout in allogeneic therapies [19] [21]. | High editing efficiency and specificity; delivery via electroporation (RNP complexes preferred) [21]. |
| Lentiviral/Viral Vectors | Delivery of CAR transgene into target cells [22]. | High titer and transduction efficiency; safety testing for replication-competent viruses [22]. |
| Magnetic Bead Separation Kits | Isolation of specific immune cells (e.g., CD3+ T-cells); purification of CAR+ populations [21]. | Closed-system automation compatibility; high purity and cell viability post-selection [1] [21]. |
| Closed-System Bioreactors | Automated, scalable expansion of cells [19] [21]. | Minimizes contamination risk; enables process control and monitoring; essential for scale-up [19] [21]. |
| iPSC Lines | Source for deriving "off-the-shelf" NK cells, T-cells, and other therapeutic cell types [3] [24]. | Clonal origin ensures consistency; requires robust differentiation protocols [24]. |
The dichotomy between autologous and allogeneic cell therapies presents the field with two powerful, yet fundamentally different, paths forward. The autologous approach leverages the body's own biological machinery to create a perfectly matched therapy, prioritizing personalized immunological safety and demonstrating remarkable efficacy, particularly in oncology, without the need for immunosuppression [1] [2]. Conversely, the allogeneic model embraces industrialization, utilizing advanced gene editing and manufacturing technologies to create standardized, off-the-shelf products that promise greater scalability, accessibility, and potential cost-effectiveness [3] [19].
The future of cell therapy will not be dominated by one approach over the other, but rather will see the coexistence and refinement of both paradigms. Autologous therapies will likely remain the gold standard for certain indications where cell quality from pre-treated patients is less concerning or where long-term persistence is paramount. Allogeneic therapies are poised to expand the reach of cell therapy to larger patient populations and into new disease areas, including autoimmune disorders and solid tumors, provided the challenges of immune rejection and long-term engraftment are fully overcome [3] [23]. For researchers and drug developers, the strategic choice between these platforms will continue to depend on a balanced consideration of the target disease, patient population, manufacturing capabilities, and the ultimate goal of delivering transformative treatments to those in need.
From Bench to Bedside: Clinical Platforms and Therapeutic Applications
The field of cellular immunotherapy has been fundamentally shaped by the distinction between autologous (patient-derived) and allogeneic (donor-derived) approaches. Autologous therapies, such as most approved CAR-T cells, leverage the patient's own cells, minimizing risks of immune rejection and graft-versus-host disease (GvHD) [2] [4]. However, they face challenges related to manufacturing complexity, high costs, and variable cell quality due to a patient's disease state or prior treatments, which can lead to significant treatment delays [2] [4]. In contrast, allogeneic therapies, derived from healthy donors, offer the potential for "off-the-shelf" availability, shorter manufacturing times, lower costs, and more consistent product quality [3] [25] [26]. Their primary challenges include the risk of host immune rejection and GvHD, which are being addressed through genetic engineering strategies like TCR knockout [4] [26]. This framework of autologous versus allogeneic sourcing is a critical lens for evaluating the performance, applications, and future development of CAR-T, CAR-NK, TCR-T, and Mesenchymal Stem Cell (MSC) therapy platforms.
Comparative Performance Analysis of Clinical Platforms
Table 1: Comparative Overview of Leading Cellular Immunotherapy Platforms
| Therapy Platform | Key Mechanism of Action | Primary Clinical Applications | Autologous vs. Allogeneic Feasibility | Key Advantages | Major Challenges & Limitations |
|---|---|---|---|---|---|
| CAR-T | Engineered T cells target surface antigens independently of MHC [27] [28]. | Hematological malignancies (B-cell lymphomas, leukemias) [25] [28]. | Primarily Autologous; Allogeneic in development [2] [26]. | High efficacy in B-cell malignancies; potential for long-term persistence [25] [4]. | CRS/ICANS toxicity; antigen escape; limited efficacy in solid tumors [27] [28]. |
| CAR-NK | Engineered NK cells target antigens, leveraging innate cytotoxicity [28] [5]. | Hematological malignancies, emerging data in autoimmunity (e.g., SLE) [5] [26]. | Primarily Allogeneic ("off-the-shelf") [5] [26]. | Favorable safety profile (low CRS/ICANS, no GvHD); "off-the-shelf" availability [25] [5]. | Shorter in vivo persistence; complex large-scale manufacturing [28] [26]. |
| TCR-T | Engineered T cells target intracellular antigens via MHC presentation [27]. | Solid tumors, viral-associated cancers (limited data in results). | Primarily Autologous. | Can target a broader range of antigens, including intracellular targets. | MHC-restricted; requires high-affinity TCR identification; risk of on-target/off-tumor toxicity. |
| CAR-MSC | Combines CAR targeting with MSC's immunomodulatory & tropic functions [27]. | Cancer (e.g., GBM, sarcoma), GvHD, inflammatory disorders [27]. | Primarily Allogeneic [27] [29]. | Dual targeting/immunomodulation; low immunogenicity; tissue homing [27] [30]. | Heterogeneous cell sources; limited persistence; scalability and manufacturing hurdles [27] [29]. |
Table 2: Summary of Key Efficacy and Safety Outcomes from Clinical Studies
| Therapy Platform | Disease Context | Best Overall Response Rate (ORR) | Best Complete Response Rate (CRR) | Key Safety Profile |
|---|---|---|---|---|
| Allogeneic CAR-T & CAR-NK [25] [26] | Relapsed/Refractory Large B-Cell Lymphoma (LBCL) | 52.5% (95% CI, 41.0-63.9) [25] [26] | 32.8% (95% CI, 24.2-42.0) [25] [26] | Very low severe CRS (0.04%) & ICANS (0.64%); only one GvHD case in 334 patients [25] [26]. |
| Allogeneic CD19 CAR-NK [5] | Systemic Lupus Erythematosus (SLE) | 6 of 9 (67%) patients achieved remission at >12 months [5]. | Not Applicable | Only 1 of 18 patients had grade 1 CRS; no neurotoxicity or severe adverse events [5]. |
| CAR-T (CD123-targeted) [28] | Relapsed/Refractory Acute Myeloid Leukemia (AML) | Complete Remission (CR) rates of 50-66% [28]. | Not Specified | Manageable Cytokine Release Syndrome (CRS) [28]. |
Detailed Experimental Protocols and Methodologies
Protocol 1: Manufacturing of Allogeneic "Off-the-Shelf" CAR-NK Cells
This protocol outlines the production of allogeneic CAR-NK cells from cord blood, a common source for clinical applications [26].
- Cell Sourcing and Isolation: Obtain umbilical cord blood units from healthy donors under informed consent. Isolate mononuclear cells using density gradient centrifugation (e.g., Ficoll-Paque). NK cells are then positively selected using magnetic-activated cell sorting (MACS) with anti-CD56 beads [26].
- Genetic Modification (CAR Transduction): Activate isolated NK cells with IL-2 and IL-15. Transduce the cells with a replication-incompetent lentiviral vector encoding the CAR construct (e.g., anti-CD19 scFv, CD8 hinge/transmembrane, and 4-1BB/CD3ζ signaling domains). A critical enhancement is the inclusion of a gene for autocrine IL-15 in the vector to support cell survival and persistence in vivo [26].
- In Vitro Expansion: Culture the transduced cells in a GMP-compliant bioreactor system using a medium supplemented with cytokines. Monitor cell density, viability, and CAR expression percentage over 2-3 weeks.
- Quality Control and Formulation: Perform rigorous quality control assays, including flow cytometry for CAR expression and CD56+ purity, sterility testing (mycoplasma, endotoxin), and potency assays (e.g., cytotoxicity against target cell lines). The final product is cryopreserved in infusion bags, creating an "off-the-shelf" inventory [26].
Protocol 2: Clinical Workflow for Allogeneic CAR Therapy in Lymphoma
This protocol describes the patient journey in a clinical trial for allogeneic CAR-T or CAR-NK therapy for relapsed/refractory Large B-Cell Lymphoma [25] [26].
- Patient Lymphodepletion: The patient receives a lymphodepleting conditioning regimen, typically consisting of fludarabine (25 mg/m² per day) and cyclophosphamide (300 mg/m² per day), administered daily for three days (e.g., from days -5 to -3 relative to infusion) [5] [26]. This step is crucial to create a favorable environment for the engraftment and expansion of the donor cells.
- Product Thaw and Infusion: On the designated treatment day (Day 0), a cryopreserved vial of the allogeneic CAR-T or CAR-NK cell product is thawed at the patient's bedside. The cells are administered via intravenous infusion without further manipulation [26].
- Toxicity Monitoring and Management: Patients are closely monitored for adverse events, primarily Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), using standardized grading systems (ASTCT criteria). Supportive care, including the IL-6 receptor antagonist tocilizumab for CRS, is administered as needed [25].
- Efficacy Assessment: Response to treatment is evaluated according to the Lugano classification. Tumor burden is assessed via PET-CT scans at predefined intervals (e.g., at 1, 3, and 6 months post-infusion) to determine objective response rates (ORR) and complete response rates (CRR) [25] [26].
Molecular Mechanisms and Signaling Pathways
CAR-T Cell Activation and Intracellular Signaling
Diagram 1: CAR-T cell activation signaling pathway. This diagram illustrates the intracellular signaling cascade following CAR engagement with its target antigen, leading to T-cell activation, proliferation, and execution of cytotoxic functions [28].
Mesenchymal Stem Cell (MSC) Mediated Immunomodulation
Diagram 2: MSC immunomodulation and CAR-MSC targeting. This diagram shows how MSCs modulate the immune environment via paracrine factors and how engineering them with CARs (creating CAR-MSCs) directs this activity to specific disease sites like tumors [27] [29] [30].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents and Materials for Cell Therapy Research
| Research Tool Category | Specific Examples | Critical Function in R&D |
|---|---|---|
| Cell Isolation & Selection | Anti-CD3/CD28 beads (T cells), Anti-CD56 beads (NK cells), Ficoll-Paque [26]. | Isolation and activation of specific immune cell subsets from donor apheresis or tissue samples. |
| Genetic Engineering | Lentiviral / Retroviral vectors, CRISPR-Cas9 systems, mRNA for transient expression [27] [28] [26]. | Stable or transient introduction of CAR constructs or genetic modifications (e.g., TCR knockout). |
| Cell Culture & Expansion | GMP-grade IL-2, IL-15, serum-free media, large-scale bioreactors [26]. | Ex vivo expansion of engineered cells to clinical doses while maintaining phenotype and function. |
| Characterization & QC | Flow cytometry antibodies (CD3, CD56, CD105, CD73, CD90), cytotoxicity assays (Incucyte, LDH) [29] [30]. | Confirmation of cell identity, purity, CAR expression, and pre-infusion potency. |
| In Vivo Modeling | NSG (NOD-scid-gamma) mice, patient-derived xenograft (PDX) models [27]. | Preclinical evaluation of therapy efficacy, persistence, and safety in an in vivo system. |
Chimeric Antigen Receptor T-cell (CAR-T) therapy represents a paradigm shift in the treatment of relapsed or refractory B-cell malignancies. By genetically engineering a patient's or donor's T cells to express a synthetic receptor targeting CD19—a surface antigen consistently expressed on B-cell lymphomas and leukemias—this modality redirects the immune system to eradicate malignant cells. The therapeutic landscape is divided into two primary manufacturing approaches: autologous CAR-Ts, which use a patient's own T cells, and allogeneic CAR-Ts, which use T cells from healthy donors to create "off-the-shelf" products. Autologous CD19-targeting CAR-Ts like axicabtagene ciloleucel and tisagenlecleucel have demonstrated remarkable efficacy, establishing a new standard of care. However, challenges including manufacturing delays, product variability, and access limitations have spurred the development of allogeneic alternatives. This guide provides a systematic, data-driven comparison of the efficacy, safety, and underlying experimental data for these platforms, contextualized within the broader thesis of autologous versus allogeneic therapy research.
Efficacy and Safety: A Comparative Data Analysis
Direct comparisons of autologous and allogeneic CD19 CAR-T therapies reveal distinct efficacy and safety profiles, influenced by product design and patient factors. The data below summarize key clinical outcomes.
Table 1: Comparative Efficacy of CD19-Targeted CAR-T Therapies
| CAR-T Product / Type | Malignancy | Complete Response (CR) Rate | Overall Survival (OS) | Reference |
|---|---|---|---|---|
| Autologous hCART19 | R/R B-ALL | 93.1% (CR/CRi, n=54/58) | Median OS: 21.5 months | [31] |
| Autologous CD19 CART | R/R DLBCL | Used as study comparator | Inferior median OS vs. dual-target | [32] |
| Dual-Target CD19/20 CART (Prizlon-cel) | R/R DLBCL | Significantly higher CR rate at 3 months | Median OS: 31.8 months longer than CD19 CART | [32] |
| Dual-Target CD19/22 CART | R/R B-ALL & NHL | High CR rates in B-ALL | Improved outcomes in high-risk patients | [33] |
Table 2: Comparative Safety Profile of CD19-Targeted CAR-T Therapies
| Adverse Event | Autologous CD19 CART | Dual-Target CD19/20 CART | Allogeneic CAR-T Considerations | Reference |
|---|---|---|---|---|
| Cytokine Release Syndrome (CRS) | Baseline incidence | Significantly higher incidence | Risk varies with gene-editing strategy | [32] |
| Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) | Reported | Not significantly different | -- | [32] |
| Hematological Toxicity | Reported | Higher incidence | -- | [32] |
| Graft-versus-Host Disease (GvHD) | Not applicable | Not applicable | A key risk requiring TCR ablation | [34] [8] |
| Infections | -- | Higher incidence | -- | [32] |
Key Insights from Clinical Data
- Superiority of Dual-Targeting Strategies: A single-center retrospective analysis of 70 patients with R/R DLBCL demonstrated that dual-target CD19/20 CAR-T (C-CAR039) achieved significantly superior 3-month complete response rates and extended median overall survival by 31.8 months compared to single-target CD19 CAR-T therapy [32].
- Impact of Humanization: A clinical trial with 58 R/R B-ALL patients showed that humanized CD19-targeted CAR-T (hCART19) achieved a 93.1% complete remission rate and was associated with longer event-free survival and B-cell aplasia (up to 616 days) compared to murine-based CAR-Ts, indicating enhanced persistence [31].
- The Allogeneic Challenge: The primary risks for allogeneic "off-the-shelf" products are Graft-versus-Host Disease (GvHD) and host-versus-graft rejection. Mitigation relies on gene-editing technologies (e.g., CRISPR/Cas9, TALEN) to disrupt the T-cell receptor (TCR) complex (e.g., TRAC locus) and sometimes HLA class I molecules [34] [35] [8].
Experimental Protocols: Methodologies for Evaluating CAR-Ts
Clinical Trial Design for Efficacy and Safety
The protocols for evaluating CAR-T therapies in human trials are standardized to ensure rigorous assessment of efficacy and safety.
- Lymphodepletion: Patients uniformly receive a lymphodepleting chemotherapy regimen, typically fludarabine (25 mg/m²/day) and cyclophosphamide (300 mg/m²/day) for three days prior to CAR-T infusion [32] [31].
- Cell Infusion: CAR-T cells are administered intravenously at a dose ranging from 1-5 × 10⁶ cells per kilogram of patient weight [32].
- Response Assessment: Treatment response is evaluated using the Lugano classification (2014) for lymphomas, which relies on PET-CT and CT scans to categorize outcomes as Complete Response (CR), Partial Response (PR), Stable Disease (SD), or Progressive Disease (PD). Response is typically assessed at one and three months post-infusion [32] [36].
- Safety Monitoring: The occurrence and severity of adverse events like CRS and ICANS are graded according to the American Society for Transplantation and Cellular Therapy (ASTCT) consensus guidelines [32] [37].
- Endpoint Definitions: Key endpoints include Overall Survival (OS), Progression-Free Survival (PFS), and Duration of Response (DOR), calculated from the time of CAR-T cell infusion [32].
In Vitro and In Vivo Preclinical Assessment
Preclinical models are crucial for establishing the potency and anti-tumor activity of novel CAR-T constructs.
- Cytotoxicity Assays: Target cancer cells (e.g., AML cell lines like MOLM-13) are co-cultured with CAR-T cells at various effector-to-target (E:T) ratios. After 24-48 hours, cytotoxicity is calculated based on the percentage of live tumor cells remaining compared to control cultures without effector cells [38].
- In Vivo Xenograft Models: Immunodeficient NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) mice are injected intravenously with patient-derived xenograft (PDX) cells or luciferase-expressing cancer cell lines to establish tumors. CAR-T cells are then administered intravenously, and tumor burden is tracked over time using bioluminescence imaging (Xenogen IVIS system) and analysis software (Living Image) [38].
Signaling Pathways and Engineering Logic
The core architecture of a second-generation CAR, which forms the basis of most approved therapies, integrates multiple signaling domains to achieve robust T-cell activation. The following diagram illustrates the structure and activation logic of a CD19-targeting CAR.
Diagram 1: CD19 CAR-T Activation Logic
The CAR construct is a synthetic protein with three main domains. The extracellular domain contains a single-chain variable fragment (scFv) derived from an anti-CD19 antibody, which is responsible for antigen recognition. This is fused to a transmembrane domain that anchors the receptor to the T-cell membrane. The intracellular signaling domain is typically a second-generation design, combining a primary costimulatory domain (such as CD28 or 4-1BB) with the CD3ζ chain, which contains Immunoreceptor Tyrosine-Based Activation Motifs (ITAMs). Upon binding to CD19, the CAR initiates coordinated signaling through both CD3ζ and the costimulatory domain, leading to full T-cell activation, proliferation, and cytotoxic killing of the target B-cell [39] [33].
Manufacturing Workflows: Autologous vs. Allogeneic
The fundamental difference between autologous and allogeneic CAR-T therapies lies in their manufacturing pipelines and the requisite genetic engineering steps, as illustrated below.
Diagram 2: CAR-T Manufacturing Workflow Comparison
The autologous pathway (yellow nodes) begins with leukapheresis of the patient's own T cells. These cells are then activated, transduced with a viral vector (e.g., lentivirus) encoding the CAR, and expanded ex vivo before being infused back into the patient. This process is patient-specific, minimizes the risk of immunogenic rejection, but is time-consuming and can be hampered by the poor quality of patient-derived T cells [34] [35].
The allogeneic pathway (green nodes) starts with T cells collected from a healthy donor. A critical, additional step (red node) is the use of gene-editing technologies (e.g., CRISPR/Cas9) to knock out the T-cell receptor (TCR) alpha constant (TRAC) locus. This prevents the donor T cells from recognizing the patient's tissues as foreign, thereby mitigating the risk of GvHD. These edited cells are then transduced, expanded, and cryopreserved to create an "off-the-shelf" product that is readily available for multiple patients [34] [35] [8].
Table 3: Key Research Reagent Solutions for CAR-T Development
| Reagent / Tool | Function in CAR-T Research | Example Use Case |
|---|---|---|
| Lentiviral Vectors | Delivery of CAR transgene into T-cell genome | Stable expression of CD19-targeting CAR in primary T cells [31] |
| Anti-CD3/CD28 Magnetic Beads | Ex vivo T-cell activation and expansion | Stimulating T cells prior to transduction [31] |
| Cytokine ELISA Kits | Quantification of cytokine levels (e.g., IL-6, IFN-γ) | Monitoring CRS potential in CAR-T co-culture supernatants [31] |
| Flow Cytometry Antibodies | Analysis of CAR expression and immune phenotyping | Detecting CD19 CAR transduction efficiency via tag detection [38] |
| CRISPR/Cas9 Systems | Gene editing for allogeneic CAR-T development | Knocking out TRAC to prevent GvHD [34] [8] |
| NSG (NOD-Scid-Gamma) Mice | In vivo assessment of CAR-T efficacy and persistence | Patient-derived xenograft (PDX) models of AML [38] |
The field of adoptive cell therapy is undergoing a significant transformation, moving from patient-specific autologous treatments towards universally available allogeneic "off-the-shelf" products. While autologous Chimeric Antigen Receptor (CAR)-T cell therapies have demonstrated remarkable success in hematological malignancies, their application in solid tumors and autoimmune diseases faces substantial biological and logistical barriers [40]. Allogeneic approaches, utilizing cells from healthy donors, are emerging as promising alternatives that overcome challenges such as high costs, labor-intensive manufacturing, and lengthy production times [3]. This evolution is particularly critical for solid tumors, which constitute approximately 90% of all human cancers and present unique therapeutic challenges including heterogeneous antigen expression, immunosuppressive microenvironments, and physical barriers to T-cell infiltration [40]. Simultaneously, researchers are exploring engineered cellular therapies for autoimmune conditions, representing a frontier expansion for this technology beyond oncology.
The fundamental distinction between autologous and allogeneic approaches lies in their source material and manufacturing implications. Autologous therapies use the patient's own cells, minimizing immunogenic risks but creating complex logistical challenges and production delays [4]. Allogeneic therapies leverage healthy donor cells, enabling standardized, large-scale manufacturing and immediate product availability [41] [42]. This review systematically compares the performance of these competing platforms in solid tumors and autoimmune diseases, analyzing clinical outcomes, experimental methodologies, and technological innovations that are shaping the future of cellular therapeutics.
Comparative Clinical Trial Outcomes: Solid Tumors
Current Clinical Landscape
Clinical development of allogeneic CAR-T therapies for solid tumors remains in earlier stages compared to hematological malignancies, though promising early-phase trials are establishing proof-of-concept. NKG2D CAR-T cells targeting stress ligands (MICA/B, ULBP1–6) represent one of the most advanced allogeneic platforms, recognizing antigens expressed on over 80% of diverse solid tumors including pancreatic and ovarian cancers [41]. Preliminary clinical data demonstrate encouraging signals of biological activity despite the formidable barriers presented by the solid tumor microenvironment.
The table below summarizes key clinical findings from allogeneic CAR-T trials in solid tumors:
Table 1: Clinical Outcomes of Allogeneic CAR-T Cell Therapy in Solid Tumors
| CAR Target | Tumor Types | Clinical Efficacy | Safety Profile | Notable Findings |
|---|---|---|---|---|
| NKG2D [41] | Pancreatic, ovarian, and other solid malignancies | Early evidence of antitumor activity in phase I trials | Manageable toxicity profile; Risks of off-target effects from gene editing | Recognizes stress ligands on >80% of solid tumors; CRISPR-edited to prevent GvHD |
| B7-H3 [40] | Various solid tumors | Preclinical evidence of efficacy | Under evaluation in early clinical trials | An immunomodulatory molecule overexpressed on many solid tumors |
| Mesothelin [40] | Mesothelioma, pancreatic, ovarian | Early clinical development | On-target, off-tumor toxicity concerns | Often combined with safety switches |
Autologous vs. Allogeneic Comparison in Solid Tumors
Direct comparisons between autologous and allogeneic CAR-T approaches in solid tumors are limited by the early stage of clinical development. However, distinct patterns are emerging regarding their respective advantages and limitations:
Table 2: Autologous vs. Allogeneic CAR-T Approaches for Solid Tumors
| Parameter | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| Manufacturing Time | 3+ weeks [42] | Immediate availability from cryopreserved stocks [41] |
| Starting Cell Quality | Often compromised by prior therapies [42] | Optimal from healthy donors [4] |
| T-cell Fitness | Variable; may exhibit exhaustion [42] | Consistent; robust proliferative capacity [41] |
| GvHD Risk | Minimal (self-derived) [4] | Requires TCR disruption via gene editing [41] |
| Host Rejection | Limited (autologous) | Significant concern; requires HLA modification [8] |
| Scalability | Limited (patient-specific) [4] | High (off-the-shelf) [3] |
| Solid Tumor Challenges | Applicable to both platforms: antigen heterogeneity, immunosuppressive TME, trafficking barriers [40] |
Emerging Applications in Autoimmune Diseases
Preclinical and Clinical Developments
The application of allogeneic CAR-engineered cell therapies is expanding beyond oncology into autoimmune diseases, representing a frontier area of therapeutic development. Early-phase clinical trials are investigating allogeneic CAR-T and CAR-NK cell approaches for conditions where immune dysregulation drives pathology [3]. These innovative approaches aim to selectively target and eliminate pathogenic immune cells or restore immune tolerance, offering potential advantages over broad immunosuppression.
Research in this area leverages the same technological platforms being developed for cancer therapy, including allogeneic off-the-shelf CAR-T cells derived from healthy donor peripheral blood mononuclear cells and CAR-NK cell therapies from cord blood or induced pluripotent stem cells [3]. The genetic engineering strategies employed include TCR disruption to prevent GvHD and enhancement of persistence through cytokine signaling pathways, mirroring approaches used in oncology applications.
Experimental Protocols and Methodologies
Allogeneic CAR-T Cell Manufacturing Workflow
The production of allogeneic CAR-T cells follows a standardized protocol with critical modifications to mitigate alloreactivity risks:
Diagram 1: Allogeneic CAR-T Manufacturing Workflow
Step 1: Donor Selection and Cell Sourcing - Healthy donors undergo leukapheresis to collect peripheral blood mononuclear cells (PBMCs). Alternative sources include umbilical cord blood or induced pluripotent stem cells (iPSCs), each offering distinct advantages in alloreactivity and scalability [42].
Step 2: T-cell Isolation and Activation - T-cells are isolated from PBMCs using antibody-coated magnetic beads (e.g., anti-CD3/CD28 Dynabeads) which simultaneously activate the cells and initiate proliferation [40].
Step 3: Genetic Modification - This critical step introduces three key genetic changes:
- TCR Disruption: Using CRISPR/Cas9 or other gene-editing tools to knockout T-cell receptor alpha constant (TRAC) or beta chain (TRBC) genes to prevent GvHD [41] [8].
- HLA Modification: Disruption of β2-microglobulin (B2M) to reduce host-versus-graft rejection [41].
- CAR Integration: Introduction of CAR construct via viral vectors (lentivirus/retrovirus) or non-viral methods (transposons, mRNA) [40].
Step 4: Ex Vivo Expansion - Genetically modified T-cells are expanded in bioreactors with cytokine support (IL-2, IL-15) to achieve therapeutic doses [40].
Step 5: Quality Control and Cryopreservation - Rigorous testing ensures product safety, including absence of TCR expression, CAR expression validation, and sterility. The final product is cryopreserved for off-the-shelf use [8].
Genetic Engineering Strategies for Allogeneic Platforms
Advanced gene editing technologies are central to overcoming the immunological barriers of allogeneic cell therapy:
Diagram 2: Genetic Engineering Strategies
GvHD Prevention: Disruption of the T-cell receptor (TCR) through knockout of TRAC or TRBC genes prevents donor T-cells from recognizing host tissues as foreign, effectively eliminating the risk of GvHD [41] [8]. Residual TCR-positive cells are typically depleted using magnetic bead selection to ensure product purity.
Host Rejection Mitigation: Knockout of β2-microglobulin (B2M) reduces surface expression of HLA class I molecules, minimizing recognition by host T-cells and consequent rejection [41]. Emerging approaches include overexpression of non-classical HLA molecules (HLA-E, HLA-G) that inhibit NK cell-mediated clearance while avoiding allorecognition [26].
Functional Enhancement: Additional engineering strategies include:
- Cytokine Support: Incorporation of membrane-bound IL-15 or inducible cytokine expression to enhance persistence [26].
- Checkpoint Disruption: Knockout of PD-1 or other inhibitory receptors to resist tumor microenvironment suppression [40].
- Safety Switches: Inclusion of suicide genes (e.g., caspase-9) for controlled elimination of CAR-T cells if toxicity occurs [40].
The Scientist's Toolkit: Essential Research Reagents
Successful development of allogeneic CAR therapies requires specialized reagents and platforms throughout the research and development pipeline:
Table 3: Essential Research Reagents for Allogeneic CAR Therapy Development
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Gene Editing Tools | CRISPR/Cas9 systems, TALENs, ZFNs [41] [8] | TCR disruption (TRAC/TRBC KO), HLA modification (B2M KO) |
| Vector Systems | Lentiviral vectors, retroviral vectors, transposon systems [40] | Stable CAR integration into host T-cell genome |
| Cell Separation | Anti-CD3/CD28 magnetic beads [40] | T-cell activation and expansion |
| Cytokines | IL-2, IL-7, IL-15, IL-21 [40] | T-cell proliferation, persistence, and functionality |
| Cell Culture | Serum-free media, activation supplements [42] | Ex vivo T-cell expansion and maintenance |
| Analytical Tools | Flow cytometry antibodies, cytotoxicity assays [8] | Assessment of CAR expression, purity, and function |
The evolving landscape of allogeneic cell therapy demonstrates significant promise for addressing the formidable challenges of solid tumors and autoimmune diseases. While autologous approaches established the therapeutic potential of CAR-engineered cells, allogeneic platforms offer distinct advantages in scalability, consistency, and immediate availability that may ultimately broaden patient access [3] [4]. Current clinical evidence, though early-stage, indicates that allogeneic CAR-T and CAR-NK cells can achieve encouraging responses with remarkably low rates of severe CRS, ICANS, and GvHD in heavily pretreated patients [25] [26].
Critical barriers remain, particularly in solid tumors, where the immunosuppressive microenvironment, antigen heterogeneity, and limited persistence continue to challenge both autologous and allogeneic approaches [40]. Future research directions include optimizing gene editing to enhance persistence while maintaining safety, developing strategies to overcome host immune rejection without compromising antitumor activity, and identifying optimal antigen targets with sufficient specificity for solid tumors and autoimmune applications. As genetic engineering technologies advance and clinical experience matures, allogeneic cell therapies are positioned to potentially transform treatment paradigms across both oncology and autoimmunity.
The field of adoptive T cell therapy has been revolutionized by the clinical success of autologous chimeric antigen receptor (CAR)-T cells in treating hematological malignancies [43]. However, the autologous approach faces significant challenges including high costs, lengthy manufacturing times, and variable product quality due to patient-specific T cell fitness [43] [8]. These limitations have spurred intensive research into allogeneic "off-the-shelf" alternatives derived from healthy donors [3]. A critical barrier to allogeneic therapies is host immune rejection, primarily mediated through T cell receptor (TCR) recognition of mismatched human leukocyte antigen (HLA) molecules on donor cells [8] [44]. This review comprehensively compares the genetic engineering strategies—particularly TCR knockout and HLA ablation—being deployed to overcome these hurdles, framing them within the broader thesis of autologous versus allogeneic therapy efficacy. We evaluate the experimental protocols, efficiency, and safety profiles of different genome editing platforms, including CRISPR, TALENs, and meganucleases, to provide researchers with a practical guide for technology selection.
Strategic Imperatives: Comparing Key Genetic Modifications
The development of universal allogeneic T cell products hinges on two primary genetic engineering objectives: preventing graft-versus-host disease (GvHD) and avoiding host immune rejection. The strategic approaches to address these challenges, along with emerging safety measures, are summarized in the table below.
Table 1: Key Genetic Engineering Strategies for Allogeneic T Cell Therapies
| Strategy | Molecular Target | Intended Function | Impact on Allogeneic Therapy Efficacy |
|---|---|---|---|
| TCR Knockout | TRAC (TCR Alpha Constant) and/or TRBC (TCR Beta Constant) loci [8] |
Eliminates surface expression of the αβTCR, preventing recognition of host alloantigens and thereby mitigating GvHD [8]. | Enables use of donor T cells without causing GvHD; however, complete TCR ablation may impair long-term T cell persistence and function [8]. |
| HLA Ablation | B2M (Beta-2 Microglobulin) and CIITA (Class II Transactivator) [44] |
Disrupts surface expression of HLA Class I (B2M KO) and Class II (CIITA KO) molecules, rendering cells invisible to host T cells [44]. |
Prevents Host-versus-Graft Reaction (HVGR) mediated by host T cells; B2M KO alone can trigger "missing-self" killing by host NK cells [44]. |
| HLA Engineering | B2M locus with HLA-E transgene [44] |
Replaces polymorphic HLA Class I with a single, non-polymorphic HLA-E molecule which engages the inhibitory receptor NKG2A on NK cells [44]. | Creates "hypo-immunogenic" T cells that evade both T cell and NK cell-mediated rejection, significantly improving in vivo persistence [44]. |
| Safety Switches | Introduction of suicide genes (e.g., inducible caspase systems) | Provides a mechanism for controlled elimination of engineered cells in case of adverse events like cytokine release syndrome or on-target/off-tumor toxicity [43]. | A critical safety layer for both autologous and allogeneic therapies, potentially increasing the therapeutic window and clinical safety profile [43]. |
Technology Landscape: A Comparative Analysis of Genome Editing Tools
Multiple genome-editing platforms can be employed to implement the strategies outlined above. The choice of technology involves trade-offs between specificity, efficiency, ease of design, and practical feasibility.
Table 2: Comparison of Major Genome Editing Platforms
| Platform | Mechanism of Action | Target Site Constraints | Reported Efficiency | Key Safety Considerations |
|---|---|---|---|---|
| CRISPR-Cas9 | Cas9 nuclease complexed with a single-guide RNA (sgRNA) recognizes a 20-nt target site adjacent to a 5'-NGG-3' PAM [45]. | Requires a protospacer adjacent motif (PAM), which can limit targetable sites [45]. | High indel formation rates (>70% reported) [45]. | Can tolerate sgRNA mismatches, leading to off-target activity; improved specificity with high-fidelity Cas9, paired nickases, or RNA-guided FokI nucleases (RFNs) [46] [45]. |
| TALENs | A pair of custom Transcription Activator-Like Effector proteins fused to FokI nuclease; FokI dimerization required for DSB creation [45]. | Minimal constraints; target site must allow for two TALEN binding sites spaced 14-20 bp apart [45]. | Highly variable; one study reported 33% indel formation [45]. | High specificity due to long (≈36 bp) combined target sequence; minimal evidence of off-target activity [45]. Sensitive to cytosine methylation [45]. |
| Meganucleases | Single protein enzyme with a long natural recognition sequence (12-40 bp) [46]. | Requires a specific central 4-base pair recognition motif within the target sequence [46]. | Variable (e.g., 2.2% to 6% reported in different studies) [46]. | Very high inherent specificity due to long recognition site and an "indirect readout" mechanism; retargeting requires extensive protein engineering [46]. |
| Base Editing | Fusion of a catalytically impaired Cas9 to a deaminase enzyme, enabling direct chemical conversion of one base pair to another without inducing a DSB [8]. | Dependent on the PAM requirement of the Cas9 variant used; requires a protospacer and a specific "activity window" within the sgRNA hybridisation region [8]. | Varies by system and target; can achieve high rates of precise base conversion. | Avoids DSB-related genotoxicity (chromosomal translocations, large deletions); potential for off-target RNA and DNA editing, and bystander editing within the activity window [8]. |
The following diagram illustrates the fundamental mechanism of the two most widely used editing platforms, CRISPR-Cas9 and TALENs, in creating a double-strand break (DSB) in DNA.
Experimental Protocols: Detailed Workflows for Key Modifications
Protocol 1: TCR Knockout in Primary Human T Cells via CRISPR-Cas9 RNP Electroporation
This protocol, adapted from a live-cell imaging study on TCR T cell behavior, details the knockout of TCR-related genes using ribonucleoprotein (RNP) complexes, a method favored for its reduced off-target effects and high efficiency in hard-to-transfect primary T cells [47].
- T Cell Isolation and Activation: Obtain leukopaks from healthy donors. Isolate primary human T cells using an immunomagnetic negative selection kit. Seed T cells at a density of 1 million cells per mL in X-Vivo-15 medium supplemented with serum, beta-mercaptoethanol, N-acetyl-L-cysteine, and 100 IU/mL of IL-2. Activate cells with Dynabeads Human T-Activator CD3/CD28 at a 1:1 bead-to-cell ratio [47].
- RNP Complex Formation: Design sgRNAs targeting the constant region of the TCR α chain (
TRAC) or β chain (TRBC). For example, theTRACsequence is a common target. Synthesize crRNA and tracrRNA, then complex them 1:1 by volume and incubate for 30 minutes at 37°C to form sgRNAs. Mix the sgRNAs with purified Cas9 protein (e.g., 40 µM stock) at a 1:1 volume ratio and incubate for 15 minutes at 37°C to form RNP complexes [47]. - Electroporation: At 48 hours post-activation, count the T cells and resuspend them in a specialized electroporation buffer (e.g., P3 buffer from Lonza) at a concentration of 1 × 10^6 cells per 20 µl. Mix the cell suspension with 3 µl of the prepared RNP complexes and transfer it to a 96-well electroporation plate. Perform electroporation using a predefined protocol (e.g., the EH115 protocol on a Lonza 4D-Nucleofector system) [47].
- Recovery and Culture: Immediately after electroporation, recover cells by adding 80 µl of pre-warmed T cell medium and incubating at 37°C for 15 minutes. Then, transfer the cells to appropriate culture vessels containing complete X-Vivo-15 medium with IL-2 (100 IU/mL) [47].
- Validation: Confirm knockout efficiency 48-72 hours post-editing. This is typically done by flow cytometry to assess loss of TCR surface expression (e.g., using anti-TCRαβ antibodies) and by next-generation sequencing (NGS) of the target locus to quantify indel formation [8].
Protocol 2: Multiplex HLA Engineering for Hypo-Immunogenic T Cells
This advanced protocol, based on work demonstrating the in vivo efficacy of allogeneic regulatory T cells, combines multiple edits to create T cells that evade both T and NK cell recognition [44].
- Disruption of HLA Class I (
B2MKnockout): Use CRISPR-Cas9 RNP electroporation (as in Protocol 1) to target theB2Mgene. This disrupts the stability and surface expression of all HLA Class I molecules. Validate successful knockout by flow cytometry staining for HLA-ABC [44]. - Knock-in of HLA-E Transgene: Co-deliver a donor DNA template containing an
HLA-E-B2Mfusion gene along with theB2M-targeting RNP. The template is designed for homology-directed repair (HDR) into theB2Mlocus. This fusion gene replaces the polymorphic HLA Class I with the non-polymorphic HLA-E, which engages the inhibitory receptor NKG2A on NK cells to prevent "missing-self" killing [44]. - Disruption of HLA Class II (
CIITAKnockout): To eliminate HLA Class II expression, target theCIITAgene, the master regulator of HLA Class II. This can be performed in a second editing step using CRISPR-Cas9 or, for greater specificity, an adenine base editor (ABE) to introduce a knockout mutation without creating a double-strand break [44]. - Functional Validation: Confirm the phenotype of the fully engineered cells.
- Flow Cytometry: Verify the absence of HLA-ABC and HLA-DR/DP/DQ, and confirm surface expression of HLA-E.
- In Vitro Suppression Assay: Demonstrate that the engineered T cells retain their suppressive function, comparable to unedited autologous Tregs [44].
- Cytotoxicity Assay: Co-culture the engineered T cells with allogeneic NK cells to validate their resistance to NK-mediated lysis [44].
The successful implementation of the above protocols relies on a suite of specialized reagents and tools.
Table 3: Essential Research Reagents for T Cell Genome Engineering
| Reagent / Solution | Function | Example Product / Component |
|---|---|---|
| T Cell Isolation Kit | Negative selection to purify untouched human T cells from PBMCs or leukopaks. | EasySep Human T Cell Isolation Kit [47] |
| T Cell Activation Beads | Provides stimulatory signals (anti-CD3/CD28) to activate T cells, a prerequisite for efficient gene editing. | Dynabeads Human T-Activator CD3/CD28 [47] |
| Cell Culture Medium | A serum-free, specialized medium optimized for the expansion of human T cells. | X-Vivo-15 [47] |
| Recombinant Human IL-2 | A critical cytokine that promotes T cell survival and proliferation during ex vivo culture. | Various GMP-grade suppliers |
| Cas9 Nuclease | The core enzyme of the CRISPR system that creates the double-strand break in DNA. | QB3 Macrolab or commercial suppliers [47] |
| sgRNA / crRNA:tracrRNA | The guide RNA component that confers target specificity to the Cas9 nuclease. | Synthesized commercially (e.g., IDT) [47] |
| Electroporation System | A device that uses electrical pulses to create transient pores in cell membranes, enabling RNP delivery. | 4D-Nucleofector System (Lonza) with P3 Primary Cell Kit [47] |
| Flow Cytometry Antibodies | For validating edits (e.g., anti-TCRαβ, anti-HLA-ABC) and assessing cell phenotype (anti-CD4, CD25, FOXP3). | Various commercial suppliers [47] [44] |
The strategic knockout of TCR and ablation of HLA molecules represent foundational pillars in the development of effective allogeneic T cell therapies. The choice of genome editing technology—whether CRISPR for its versatility and high efficiency, TALENs for their high specificity, or base editors for their safety profile—is contextual and depends on the specific application, target site, and risk-benefit analysis [46] [45]. As the field progresses, the combination of these disruptive genetic engineering strategies with advanced safety switches and manufacturing innovations is poised to bridge the efficacy gap between autologous and allogeneic products. This will ultimately enable the widespread availability of potent, safe, and "off-the-shelf" cellular therapies for a broad spectrum of human diseases.
Navigating Challenges: Safety, Scalability, and Persistence Hurdles
The therapeutic landscape for hematological malignancies, autoimmune diseases, and organ failure has been revolutionized by cell therapies and transplantation. However, their efficacy is fundamentally constrained by two major immunological barriers: graft-versus-host disease (GVHD) and host immune rejection. These complications represent a pivotal dichotomy in treatment outcomes: GVHD primarily threatens recipients of allogeneic (donor-derived) cell products, where donor immune cells attack host tissues, while host rejection endangers both allogeneic cellular therapies and solid organ transplants through recipient immune destruction of the graft [48] [2]. The strategic mitigation of these risks forms the cornerstone of successful transplantation biology, influencing choices between autologous and allogeneic approaches and dictating the requirement for concomitant immunosuppressive regimens.
The pathogenesis of these conditions, while distinct, shares common immunological pathways. GVHD occurs when immunocompetent T lymphocytes from the graft recognize alloantigens in the immunocompromised recipient, initiating a cascade that damages skin, liver, gastrointestinal tract, and other organs [48]. Conversely, host immune rejection involves a multifaceted attack by the recipient's immune system—including T cells, natural killer (NK) cells, and alloantibodies—on the transplanted graft, perceiving it as foreign [49]. The context of autologous versus allogeneic therapy efficacy research is critical; while autologous therapies (using the patient's own cells) circumvent GVHD and minimize rejection risks, they face challenges of manufacturing complexity, time delays, and variable cell quality [2] [4]. Allogeneic "off-the-shelf" therapies offer immediate availability and standardized quality but necessitate sophisticated strategies to overcome immunological incompatibility [2]. This guide provides a comparative analysis of current and emerging strategies to navigate this complex immunologic terrain, offering researchers a framework for selecting and optimizing protective regimens.
Understanding the Immunological Landscape
Risk Profiles: Autologous vs. Allogeneic Therapies
The choice between autologous and allogeneic cell sources dictates the spectrum and magnitude of immunological risks. Table 1 summarizes the core differences.
Table 1: Core Immunological Differences Between Autologous and Allogeneic Therapies
| Feature | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Cell Source | Patient's own cells [2] | Healthy donor (matched or mismatched) [2] |
| Major Risk | Disease contamination, limited cell quality/quantity [2] [4] | Graft-versus-Host Disease (GVHD) and Host Graft Rejection [2] |
| Rejection Mechanism | Minimal to none (lacks foreign antigens) [2] | Host T cells and antibodies target donor HLA/minor antigens [49] |
| GVHD Risk | None (no alloreactive T cells) [2] | High (donor T cells attack host tissues) [48] |
| Immunosuppression Needed | Typically not required [2] | Almost always required, often long-term [2] |
| Therapeutic "Graft-vs-Tumor" | No | Yes, a potential benefit in hematologic cancers [48] |
Molecular and Cellular Actors in Rejection
The immunobiology of rejection is orchestrated by a complex interplay of molecules and cells. Key players include:
- Human Leukocyte Antigens (HLAs): These highly polymorphic cell surface proteins are the primary triggers of allorecognition. Mismatches in HLA class I (HLA-A, -B, -C) and class II (HLA-DR, -DQ, -DP) between donor and recipient are strongly correlated with both GVHD and graft rejection [49]. Direct recognition of donor HLA by host T cells (or vice-versa) initiates a potent effector response.
- T Lymphocytes: CD8+ cytotoxic T cells directly lyse graft cells, while CD4+ helper T cells orchestrate broader immune responses, including B-cell activation for antibody production [48] [49].
- B Cells and Alloantibodies: B cells produce donor-specific antibodies (DSA) that mediate antibody-dependent cellular cytotoxicity (ADCC) and activate the complement system, leading to graft damage [49].
- Natural Killer (NK) Cells: NK cells can directly kill graft cells that lack "self" HLA class I molecules, a phenomenon known as "missing-self" recognition [49].
The following diagram illustrates the core pathways of T-cell activation, a central event in both GVHD and cellular rejection, and the primary targets of mainstream prophylactic drugs.
Diagram 1: T-Cell Activation Pathway and Pharmacologic Inhibition. This diagram outlines the primary signaling cascade in T-cell activation following alloantigen recognition. Mainstream prophylactic drugs (dashed outlines) target key steps: Calcineurin Inhibitors (CNIs) block NFAT activation and subsequent IL-2 production; Antimetabolites like Mycophenolate Mofetil (MMF) and Methotrexate (MTX) inhibit the proliferation of activated T cells [48].
Standard Prophylactic Strategies & Clinical Evidence
Prophylaxis against GVHD and rejection remains heavily reliant on pharmacologic immunosuppression, particularly in allogeneic settings. Table 2 compares the mechanisms, applications, and clinical evidence for widely used agents.
Table 2: Comparison of Standard Pharmacologic Prophylaxis Strategies
| Strategy (Class) | Mechanism of Action | Therapeutic Context | Key Clinical Evidence & Outcomes |
|---|---|---|---|
| Calcineurin Inhibitors (CNIs):Cyclosporine, Tacrolimus | Inhibits calcineurin, blocking NFAT-mediated IL-2 transcription and T-cell activation [48]. | Foundation of most allogeneic HSCT and solid organ transplant regimens [48]. | Tacrolimus+MTX superior to Cyclosporine+MTX for reducing aGVHD; no significant OS difference [48]. CNI-based regimens reduce GVHD incidence but still fail in 40-60% of recipients [48]. |
| Methotrexate (MTX) | Cytotoxic anti-metabolite; attenuates T-cell activation at low doses [48]. | Combined with CNIs in myeloablative allogeneic HSCT [48]. | Cyclosporine+MTX combination superior to either agent alone in reducing GVHD and improving survival [48]. "Mini-dose" (5 mg/m²) reduces GI toxicity [48]. |
| Mycophenolate Mofetil (MMF) | Prodrug of mycophenolic acid; inhibits inosine monophosphate dehydrogenase in T and B cells [48]. | Combined with CNIs in non-myeloablative and cord blood transplants [48]. | Phase I/II trials show faster neutrophil engraftment and less mucositis vs. MMF alone, but no significant improvement in grade 2-4 aGVHD incidence [48]. |
| Anti-Thymocyte Globulin (ATG) | Polyclonal antibodies causing in vivo T-cell depletion via complement-mediated lysis and apoptosis [48]. | Used in mismatched or unrelated donor HCT to prevent GVHD and graft rejection [48]. | Rabbit ATG (15 mg/kg) reduced grade 3-4 aGVHD vs. no ATG, but increased lethal infections [48]. ATG-F reduced aGVHD (33% vs 51%) and cGVHD (30.9% vs 58.8%) vs. standard prophylaxis, with no significant survival benefit [48]. |
Emerging and Novel Strategies
Despite standard prophylaxis, GVHD and rejection rates remain high, driving research into more targeted and sophisticated approaches.
Advanced Cellular Engineering
- T-Cell Depletion (TCD): The most effective strategy for preventing GVHD involves physically removing T cells from the donor graft. However, this is offset by increased risks of graft failure, disease relapse, and delayed immune reconstitution [48]. Modern approaches favor selective TCD or in vivo depletion using agents like ATG to balance risks [48].
- Shield CAR-T Cell Technology: A groundbreaking approach designed to protect allogeneic cell therapies from host antibody-mediated rejection. Researchers engineered CAR-T cells to express the bacterial immunoevasin IdeS (IgG-degrading enzyme of S. pyogenes), which is a cysteine protease that cleaves human IgG [50] [51]. IdeS can be either membrane-tethered (IdeS-tm) or secreted (IdeS-sec). These "Shield" cells cleave host IgG (including anti-CAR antibodies) bound to their surface, shedding the Fc portion and averting Fc-dependent effector functions like phagocytosis and complement activation [50]. The remaining F(ab')2 fragments coat the cell, forming an "inert shield" that blocks further IgG binding, thus protecting the cell from clearance and allowing sustained anti-tumor activity [50] [51].
Diagram 2: Mechanism of Shield CAR-T Cell Protection. Shield CAR-T cells are engineered to express the IdeS enzyme, which cleaves bound host IgG antibodies. The release of the Fc fragment neutralizes effector functions, while the surface-retained F(ab')2 fragments create a protective barrier against further humoral attack [50] [51].
Targeted Biologics and Molecular Regulators
Emerging strategies focus on specific pathways in the immune response cascade, offering the potential for greater efficacy with reduced broad-spectrum immunosuppression.
- Chemo-Cytokine Antagonists: Agents like Maraviroc (CCR5 antagonist) block T-cell migration to tissues, while inhibitors of TNF-α, IL-2, and IL-6 receptors aim to dampen the inflammatory cytokine storm that drives GVHD pathology [48].
- Novel Molecular Regulators: Drugs such as atorvastatin and bortezomib, as well as epigenetic modulators, are under investigation. They target multiple cell types simultaneously, including T cells, B cells, and antigen-presenting cells, to disrupt the initiation and propagation of the alloreactive response [48].
- Mesenchymal Stem Cells (MSCs): Allogeneic MSCs have been approved for steroid-refractory acute GVHD. They exert potent immunomodulatory effects by suppressing T-cell proliferation, modulating dendritic cell function, and promoting a regulatory immune environment, with minimal risk of rejection due to their immune-privileged status [2].
Comparative Analysis: Efficacy and Research Data
Quantitative Outcomes of Prophylactic Regimens
Table 3 synthesizes clinical efficacy data for key strategies, providing a direct comparison of their performance in mitigating GVHD.
Table 3: Comparative Efficacy of Select Strategies for GVHD Prevention
| Prophylaxis Strategy | Clinical Context | Reported Efficacy (Acute GVHD) | Key Trade-offs & Limitations |
|---|---|---|---|
| CNI + Methotrexate | Myeloablative HSCT [48] | Remains the standard; baseline for comparison. 40-60% incidence despite prophylaxis [48]. | Nephrotoxicity (CNI), mucositis (MTX) [48]. |
| CNI + Mycophenolate Mofetil | Non-myeloablative HSCT [48] | Not established as superior in myeloablative setting; widely used based on engraftment data [48]. | Faster engraftment, less mucositis than MTX, but no proven superiority in GVHD prevention [48]. |
| + Anti-Thymocyte Globulin (ATG) | Unrelated Donor HSCT [48] | Grade 2-4: 33% (with ATG-F) vs. 51% (standard prophylaxis) [48]. | Delayed neutrophil/platelet engraftment; increased infection risk at high doses [48]. |
| T-Cell Depletion (TCD) | Mismatched/Unrelated Donor [48] | Most effective method for GVHD prevention [48]. | Increased graft failure, relapse, and delayed immune reconstitution [48]. |
| Shield CAR-T (Preclinical) | Allogeneic CAR-T in presence of antibody [50] | Efficient cleavage of cytotoxic IgG (e.g., ATG); retained anti-tumor cytolysis in vitro and in vivo [50]. | Preclinical stage; potential immunogenicity of bacterial IdeS enzyme in humans requires evaluation [50]. |
Detailed Experimental Protocol: Evaluating Shield CAR-T Cell Efficacy
To facilitate replication and further development, a key experiment from the search results is detailed below [50].
- Aim: To validate the function of Shield CAR-T cells in cleaving surface-bound IgG and protecting against antibody-mediated cytotoxicity.
- Materials:
- CAR T-cells: Parental 19BBζ CAR T-cells, IdeS-tm 19BBζ, and IdeS-sec 19BBζ.
- Antibodies: Rabbit-derived Anti-Thymocyte Globulin (ATG).
- Assay Kits: Flow cytometry antibodies for detecting human IgG Fc and F(ab')2 fragments.
- Instrumentation: Flow cytometer, western blot apparatus.
- Methodology:
- Incubation with ATG: The three types of CAR T-cells are incubated with ATG, which contains antibodies that bind to cell surface antigens like CD3, CD4, CD8, and MHC molecules.
- Detection of IgG Cleavage:
- Flow Cytometry: Cells are stained with fluorescent antibodies specific for the Fc portion of IgG. Shield CAR-T cells (both IdeS-tm and IdeS-sec) show loss of Fc signal compared to parental CAR T-cells, demonstrating cleavage.
- Western Blot: Supernatants from the cell cultures are analyzed. Released Fc fragments (~25 kDa) are detected in supernatants from Shield CAR-T cells but not parental cells.
- Confirmation of F(ab')2 Shield: Cells are stained with antibodies recognizing F(ab')2 fragments after ATG incubation. All three cell types show equivalent high levels of F(ab')2 surface coating, confirming the inert shield remains on the Shield CAR-T cells.
- Cytotoxicity Assay: The anti-tumor cytotoxic activity of Shield CAR-T cells is confirmed against target cells (e.g., Raji lymphoma cells) at various effector-to-target (E:T) ratios to ensure IdeS expression does not impair core therapeutic function.
- Outcome Measures:
- Primary: Loss of Fc surface detection via flow cytometry.
- Secondary: Presence of Fc fragments in supernatant via western blot; retained F(ab')2 coating; unimpaired cytolytic activity.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating GvHD and Rejection
| Reagent / Tool | Primary Function in Research | Example Application |
|---|---|---|
| Anti-Thymocyte Globulin (ATG) | In vivo T-cell depletion; creates lymphopenic host or studies immunoablation [48]. | Modeling GVHD prophylaxis in humanized mouse models; conditioning regimen simulation [48]. |
| IdeS Enzyme | Recombinant IgG-cleaving cysteine protease; tools for studying humoral rejection [50] [51]. | Engineering Shield cells; decomplementing serum in vitro to isolate Fc-mediated effects [50]. |
| Cyclosporine A / Tacrolimus | Calcineurin inhibition; standard pharmacologic control for T-cell suppression experiments [48] [52]. | Establishing baseline immunosuppression in vitro (T-cell activation assays) and in vivo [48]. |
| Recombinant Cytokines (IL-2, TNF-α) | Immune cell activation and polarization; creating pro-inflammatory environments [48]. | Stimulating T-cells in vitro; amplifying GVHD or rejection responses in animal models [48]. |
| Anti-HLA / DSA Sera | Source of pre-formed alloantibodies; modeling antibody-mediated rejection (AMR) [49]. | Testing efficacy of Shield technologies; investigating complement activation and endothelial injury [50] [49]. |
The strategic mitigation of GVHD and host rejection is a dynamic and multifaceted challenge that dictates the feasibility and success of advanced cell therapies and transplantation. The current arsenal, dominated by calcineurin inhibitors and antimetabolites, successfully manages acute rejection but fails to prevent chronic complications in a significant proportion of patients and carries substantial toxicity [48] [53].
The future lies in precision immunomodulation. Strategies like Shield CAR-T cells represent a paradigm shift from broadly suppressing the host or the graft to actively arming therapeutic cells with self-defense mechanisms [50] [51]. Similarly, the exploration of novel biologics and cellular products like MSCs aims to re-establish immune tolerance rather than merely applying brute-force immunosuppression [48] [2]. The ongoing refinement of "gentler" conditioning regimens that promote hybrid immune system formation, as seen in recent studies curing Type 1 diabetes in mice, further underscores this trend [54].
For researchers, the path forward involves leveraging these emerging technologies while critically evaluating their trade-offs. The choice between autologous and allogeneic platforms, and the selection of a concomitant prophylactic strategy, must be guided by the specific clinical indication, the urgency of treatment, and the depth of HLA mismatch. As the field evolves, the integration of advanced engineering, predictive analytics, and deep immunologic profiling will be crucial to unlock the full potential of safe and effective transplantation medicine.
The development of advanced cell therapies, encompassing both autologous (patient-specific) and allogeneic (donor-derived, "off-the-shelf") products, presents two distinct manufacturing and logistics challenges. The core of this comparison lies in the fundamental trade-off between the inherent variability of large-scale batch production and the managed complexities of personalized production pipelines. Autologous therapies, such as personalized CAR-T cell treatments, require a dedicated manufacturing batch for each individual patient, introducing immense logistical challenges but potentially reducing immunological complications [4] [2]. In contrast, allogeneic therapies aim to produce a single, large batch from a donor's cells to treat numerous patients, offering scalability but facing hurdles related to batch-to-batch consistency and immune rejection [55] [3]. This guide objectively compares these paradigms, focusing on their impact on manufacturing and logistics within the context of therapy efficacy research for scientific and drug development professionals.
Core Concept Comparison: Allogeneic vs. Autologous Manufacturing
Defining the Manufacturing Workflows
Allogeneic Cell Therapy manufacturing begins with sourcing cells from a healthy donor or a pre-established cell bank [55]. These cells then undergo processing, genetic modification (e.g., using CRISPR to reduce immunogenicity or introduce a Chimeric Antigen Receptor), and expansion in large-scale bioreactors to produce one batch intended for multiple patients [56] [3]. This process is designed for standardization, where a single batch must demonstrate consistent quality and therapeutic effectiveness across a diverse patient population [55]. The final products are cryopreserved and stored as "off-the-shelf" inventories, ready for on-demand administration [55].
Autologous Cell Therapy manufacturing follows a patient-specific model. The process initiates with the apheresis of a patient's own cells at a clinical center [4] [57]. This cellular material is then shipped under stringent, temperature-controlled conditions to a manufacturing facility. There, the cells undergo similar steps of genetic modification and expansion, but each batch is exclusively for the original patient [4] [2]. The finished therapy is shipped back to the treating clinic and administered to the patient. This creates a complex, time-sensitive, and logistically demanding cycle for a single dose [57].
Quantitative Comparison of Manufacturing and Product Attributes
The following table summarizes key quantitative and qualitative differences between the two manufacturing approaches, highlighting the core trade-offs between scalability and personalization.
Table 1: Comparative Analysis of Allogeneic and Autologous Cell Therapy Manufacturing
| Attribute | Allogeneic (Batch) Therapy | Autologous (Personalized) Therapy |
|---|---|---|
| Production Scale | One batch for hundreds to thousands of patients [55] | One batch for a single patient [57] |
| Key Variability Challenge | Donor-to-donor variability affecting batch consistency and therapeutic potency [55] | Patient-to-patient variability in starting cell quality due to disease state, age, and prior treatments [4] [2] |
| Production Cost Drivers | Scaling efficiency, quality control for large batches, cryopreservation [55] | High-touch labor, complex logistics, multiple shipments per batch [58] [57] |
| Target Cost per Dose | More scalable model, aiming for lower cost per dose at volume [4] | High cost; estimates from ~$170,000-$220,000 per batch, with innovation targeting $40,000-$70,000 [58] |
| Logistics & Supply Chain | Centralized production; "off-the-shelf" availability simplifies distribution [55] | Highly complex, with tight timelines (often 40-50 hours door-to-door) and cryogenic shipping for patient cells and final product [57] |
| Regulatory Batch Definition | Based on a defined quantity of product or a fixed production time interval [59] | A specific amount of a drug intended to have uniform character, made per a single production order [59] |
| Key Efficacy Challenge | Immunogenicity: Host immune rejection (GvHD) can eliminate therapy before effect [4] [56] | Product Heterogeneity: Variable cell quality and potency can impact safety and efficacy [4] |
Experimental Protocols for Manufacturing and Efficacy Analysis
To objectively compare these paradigms, researchers employ specific experimental protocols to analyze critical quality attributes and logistical performance.
Protocol 1: Assessing Allogeneic Batch Consistency and Immunogenicity
This methodology is designed to quantify the batch-to-batch variability of allogeneic products and their potential to elicit immune responses.
1. Objective: To characterize the consistency of multiple production batches of an allogeneic CAR-T or CAR-NK cell product and evaluate their susceptibility to immune-mediated rejection in vitro. 2. Materials: * Starting Material: Peripheral Blood Mononuclear Cells (PBMCs) from multiple healthy donors. * Cell Culture: G-Rex bioreactors or similar large-scale culture systems, serum-free media. * Genetic Engineering: CRISPR/Cas9 system for TCR/ HLA knockout, viral or non-viral vectors for CAR insertion. * Analytical Tools: Flow Cytometer, PCR machine, LC-MS. 3. Procedure: * Step 1: Donor Screening & Cell Sourcing. Procure PBMCs from 5-10 qualified healthy donors following informed consent [55]. * Step 2: Parallel Batch Manufacturing. For each donor, initiate a separate manufacturing batch. Expand cells in controlled bioreactors, perform simultaneous genetic modification (e.g., TCR knockout and CAR integration), and harvest after a set expansion period [55] [3]. * Step 3: In-Process Analytics & Potency Assay. For each batch, measure Critical Quality Attributes (CQAs): * Viability and Expansion: Use trypan blue exclusion and cell counting daily. * Phenotype: Analyze CAR expression and memory cell markers via flow cytometry. * Potency: Conduct a co-culture assay with target tumor cells; measure cytokine secretion (e.g., IFN-γ via ELISA) and specific cytolytic activity [55]. * Step 4: Immunogenicity Co-culture. Isolate T-cells and NK cells from a panel of different PBMC samples to represent a diverse patient population. Co-culture these immune effector cells with the allogeneic CAR-T batches. Measure residual allogeneic cell survival and activation of host immune cells after 24-48 hours [56]. 4. Data Analysis: Calculate the coefficient of variation for CQAs (e.g., expansion fold, CAR expression, potency) across the different donor batches. A higher percentage indicates greater batch-to-batch variability. For immunogenicity, determine the percentage of allogeneic cells eliminated in the co-culture to predict in vivo rejection risk.
Protocol 2: Analyzing Autologous Product Heterogeneity and Logistics
This protocol evaluates the impact of patient-specific factors and logistical timelines on the quality of final autologous products.
1. Objective: To correlate patient clinical status and logistical transit times with the critical quality attributes of their corresponding autologous cell therapy products. 2. Materials: * Patient Samples: Apheresis material from patients with varying disease stages and prior treatment histories. * Logistics: Temperature-controlled smart shippers with real-time GPS and temperature monitoring (e.g., Marken Smart Box) [57]. * Cell Processing: Automated closed-system processing units (e.g., CliniMACS Prodigy) [58]. * Analytical Tools: Flow cytometer, automated cell counter, metabolic flux analyzer. 3. Procedure: * Step 1: Patient Stratification & Apheresis. Enroll 10-15 patients, recording their age, number of prior chemotherapy lines, and disease burden. Perform apheresis to collect source T-cells [4] [2]. * Step 2: Simulated Logistics & Manufacturing. For each apheresis unit: * Log the initial cell count, viability, and T-cell composition. * Ship units to a central manufacturing facility using smart shippers; record transit time, temperature excursions, and shock events [57]. * Upon receipt, re-measure viability and cell count. * Process each unit individually through the same automated manufacturing protocol for CAR-T generation [58]. * Step 3: Final Product Analysis. For each final product, assess: * Product Characteristics: Total cell yield, final viability, CAR transduction efficiency. * Functional Quality: In vitro tumor killing efficiency and T-cell exhaustion markers (e.g., PD-1, LAG-3) via flow cytometry. 4. Data Analysis: Perform multivariate regression analysis to determine the correlation between patient factors (e.g., prior chemotherapy) and logistical stresses (e.g., transit time) with the key output variables of final product yield and potency. A strong negative correlation would highlight the critical impact of these variables on product heterogeneity.
Visualizing Workflows and Logical Relationships
The following diagrams, generated with Graphviz, illustrate the core workflows and decision points for each manufacturing paradigm.
Allogeneic vs. Autologous Manufacturing Workflow
Key Decision Points for Therapy Selection
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development in this field require specialized tools to address the unique challenges of each manufacturing model. The following table details key reagents and their functions in critical experiments.
Table 2: Key Research Reagent Solutions for Cell Therapy Development
| Research Reagent / Tool | Primary Function | Relevance to Manufacturing Paradigm |
|---|---|---|
| CRISPR/Cas9 Systems | Gene editing for knocking out endogenous T-cell receptors (TCR) and HLA molecules to reduce allogeneic immunogenicity [56] [3]. | Allogeneic: Critical for creating "universal" donor cells that evade host immune detection. |
| Immunosuppressants (e.g., Cyclosporin A) | Suppress host immune system in in vitro co-culture assays to model patient pre-conditioning and measure its effect on allogeneic cell survival [4]. | Allogeneic: Used in research to test strategies for mitigating GvHD and rejection. |
| Anti-CD3/CD28 Antibody Beads | Artificial antigen presenting structures used to activate and expand T-cells during the manufacturing process for both autologous and allogeneic therapies [2]. | Both: A fundamental reagent for T-cell activation and expansion in research and GMP manufacturing. |
| Lentiviral / Retroviral Vectors | Vehicles for the stable integration of chimeric antigen receptor (CAR) genes into the genome of T-cells or NK-cells [2] [3]. | Both: The most common method for engineering CAR cells in both paradigms. |
| Cryopreservation Media (DMSO-based) | Protect cells from ice crystal formation and osmotic shock during freezing for long-term storage of allogeneic batches or patient apheresis material [55]. | Both: Essential for creating allogeneic cell banks and for storing autologous starting/final products during transport. |
| Smart Shipping Systems | Thermal boxes with integrated GPS and sensors for real-time monitoring of location, temperature, and shock during transit of cell therapy products [57]. | Autologous: Critical for ensuring the integrity of patient-specific cells throughout the complex logistics chain. |
| Automated Cell Processing Systems | Closed, integrated systems that automate cell separation, activation, transduction, and expansion, reducing manual handling and variability [58]. | Both (leans Autologous): Increases process consistency; particularly valuable for scaling up the number of parallel autologous batches. |
| Cytokine Detection Kits (e.g., ELISA for IFN-γ) | Quantify cytokine secretion in co-culture assays as a measure of T-cell activation and potency against target tumor cells [55]. | Both: A standard analytical method for assessing the functional quality of any cell therapy batch. |
The choice between allogeneic and autologous manufacturing is not a simple binary but a strategic decision based on balancing scalability against complexity. Allogeneic therapies offer a promising path to treat a broader patient population more affordably but must overcome the scientific hurdle of immune rejection and the manufacturing challenge of ensuring consistent quality across large, donor-derived batches [56] [55]. Autologous therapies provide a personalized treatment with a de-risked immunological profile but are burdened by a costly, logistically intricate, and highly variable production process [4] [57]. For researchers and drug developers, the future lies in innovating within these paradigms—through advanced gene editing to improve allogeneic products and through automation and logistics optimization to streamline autologous manufacturing—to fully realize the potential of cell therapies for patients.
The efficacy of T-cell-based therapies, whether autologous or allogeneic, is critically limited by two interconnected biological phenomena: T-cell exhaustion and poor in vivo persistence. T-cell exhaustion is a dysfunctional state arising from persistent antigen exposure during chronic viral infections or cancer, characterized by progressive loss of effector functions, sustained expression of inhibitory receptors, and distinct transcriptional and epigenetic rewiring [60] [61]. This state fundamentally undermines the long-term effectiveness of cellular therapies. Poor in vivo persistence refers to the inability of therapeutic T cells to survive, expand, and maintain functional activity in the patient over time, leading to diminished therapeutic responses and disease relapse [62] [63].
Within the context of autologous versus allogeneic therapies, the mechanisms and severities of these limitations differ. Autologous CAR-T cells, derived from the patient's own T cells, face exhaustion primarily due to tonic signaling and an immunosuppressive tumor microenvironment [62]. In contrast, allogeneic CAR-T cells, derived from healthy donors, must additionally contend with host-versus-graft rejection and graft-versus-host disease (GvHD), which further curtail their persistence [41]. Understanding these distinct challenges is paramount for developing next-generation therapies with enhanced durability and efficacy.
Molecular Mechanisms of T-cell Exhaustion
Transcriptional and Epigenetic Reprogramming
T-cell exhaustion is not a passive state of energy but an active differentiation process driven by a distinct transcriptional and epigenetic program. Key transcription factors involved in this process include:
- NFAT: Under conditions of chronic stimulation, a shift in the balance of NFAT and its partner AP-1 leads to the formation of NFAT homodimers. These homodimers bind to promoters of genes encoding inhibitory receptors like PD-1, LAG-3, and TIM-3, driving the exhaustion phenotype [60].
- TOX: This master regulator is required for the formation of exhausted CD8+ T cells. It promotes chromatin remodelling and the expression of exhaustion-associated genes, including multiple inhibitory receptors and transcription factors such as EOMES [60] [64].
- TCF-1 (encoded by TCF7): This transcription factor is crucial for maintaining a population of stem-like or "precursor exhausted" T cells. These TCF-1+ cells possess self-renewal capacity and can give rise to terminally exhausted effector cells, playing a vital role in sustaining the T-cell response during chronic antigen exposure [60] [64].
Epigenetically, exhausted T cells undergo progressive reinforcement of their fate through modifications such as DNA methylation. The de novo DNA methyltransferase DNMT3A mediates the acquisition of repressive DNA methylation programs that limit developmental plasticity and the capacity to respond to immunotherapies like immune checkpoint blockade [64].
Signaling Pathways in T-cell Exhaustion
The following diagram illustrates the key signaling pathways that drive T-cell exhaustion, integrating signals from chronic antigen exposure and the tumor microenvironment.
Comparative Analysis of Autologous and Allogeneic Therapeutic Platforms
The functional limitations of T-cell exhaustion and poor persistence manifest differently across autologous and allogeneic therapeutic platforms. The table below provides a comparative summary of the performance, strengths, and weaknesses of each approach.
Table 1: Performance Comparison of Autologous vs. Allogeneic T-cell Therapies
| Parameter | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Source of T-cells | Patient-derived [41] | Healthy donor-derived [41] |
| Key Exhaustion Triggers | Tonic CAR signaling, immunosuppressive TME, prolonged ex vivo culture [62] | Immune rejection (HvG), GvHD potential, TME [41] |
| Manufacturing & Scalability | Personalized, logistically complex, limited scalability, treatment delays [41] | "Off-the-shelf," scalable, standardized, immediate availability [41] |
| Persistence Data | Durable persistence in responders (e.g., CD19 CAR-T) [63] | Limited persistence due to host immune rejection [41] [65] |
| Clinical Efficacy (e.g., Multiple Myeloma) | Superior OS and PFS as second-line therapy after first auto-SCT relapse [65] | Inferior OS and PFS compared to second auto-SCT; higher non-relapse mortality [65] |
| Major Safety Concerns | Cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS) [63] | Graft-versus-host disease (GvHD), host-versus-graft (HvG) rejection, infection risk [41] [65] |
Experimental Models and Methodologies for Studying Exhaustion and Persistence
In Vivo and Ex Vivo Models
Researchers employ a variety of models to dissect the mechanisms of T-cell exhaustion and test interventions.
- Chronic LCMV Infection Model: This is a foundational murine model for studying T-cell exhaustion in chronic viral infection. It allows for the tracking of virus-specific T cells as they progress from functional effectors to an exhausted state [60] [64].
- Heterotopic Ossicle Model: This adaptable in vivo model involves engineering bone marrow niches in subcutaneous sites of mice. It enables the functional study of how specific microenvironmental factors, such as anabolic parathyroid hormone (PTH) treatment, influence hematopoietic stem and progenitor cell (HSPC) maintenance and activity, providing insights into niche-specific regulation of cell persistence [66].
- In Vivo HSPC Gene Therapy Model: A novel approach demonstrating that systemic lentiviral vector administration to newborn mice can achieve in vivo gene delivery to trafficking HSPCs. This model successfully targeted long-term, multipotent HSCs, as confirmed by serial transplantation and clonal tracking, offering a potential pathway to overcome the limitations of ex vivo manipulation [67].
- Ex Vivo T-cell Exhaustion Models: These involve generating exhausted T-cells in vitro through methods like repetitive antigen stimulation or specific cytokine exposure (e.g., IL-2). These models facilitate high-throughput screening of exhaustion-reversing agents and detailed study of T-cell intrinsic pathways [60].
Key Methodologies and Workflows
The experimental workflow for evaluating novel strategies to overcome T-cell limitations often involves a multi-step process, as outlined below.
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential reagents and materials used in experimental research aimed at overcoming T-cell exhaustion and improving persistence.
Table 2: Essential Research Reagents for T-cell Exhaustion and Persistence Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| CRISPR/Cas9 Systems | Genome editing to knock out exhaustion-associated genes (e.g., PDCD1) or alloreactivity genes (e.g., TRAC, B2M) [41] [61] | TRAC knockout to prevent GvHD; B2M knockout to reduce host rejection [41] |
| Lentiviral Vectors | Stable delivery of CAR constructs or genetic payloads into T cells or HSPCs [67] | GFP-expressing LVs for tracking; CD47-high LVs for phagocytosis shielding [67] |
| Cytokines | Directing T-cell differentiation during ex vivo culture toward less exhausted, memory-like phenotypes [62] | IL-15, IL-7, IL-21 (promote stemness); avoidance of IL-2 to limit exhaustion [62] |
| Immune Checkpoint Inhibitors | Reinvigorating exhausted T cells by blocking inhibitory pathways in vitro and in vivo [61] [64] | Anti-PD-1, anti-PD-L1, anti-LAG-3 antibodies |
| Mobilizing Agents | Enhancing in vivo gene transfer or cell trafficking by increasing circulating stem/progenitor cells [67] | G-CSF, plerixafor |
| Pharmacologic Regulators | Providing external control over CAR signaling and activation to mitigate exhaustion [62] | Dasatinib (reversible CAR signaling inhibitor), Shield-1 (regulates destabilizing domain systems) |
Strategies to Overcome Functional Limitations
CAR Design and Engineering Innovations
Optimizing the structure of the chimeric antigen receptor itself is a primary strategy for reducing exhaustion.
- Mitigating Tonic Signaling: CAR designs that minimize ligand-independent, tonic signaling are critical. This can be achieved by optimizing scFv sequences, selecting costimulatory domains like 4-1BB over CD28, and mutating specific residues in signaling domains (e.g., asparagine to phenylalanine in CD28) [62].
- Regulating CAR Expression: Instead of using strong constitutive promoters, inducible promoters (e.g., AP1-NFκB) or systems that yield lower baseline CAR expression can prevent tonic signaling and exhaustion. Synthetic Notch (synNotch) receptors provide an additional layer of control, activating CAR expression only upon encounter with a specific tumor antigen [62].
- Multispecific Targeting: Engineering CAR-T cells to target multiple tumor antigens (e.g., bispecific CARs) can help overcome antigen escape and reduce the selective pressure that drives exhaustion [41].
Manufacturing and Culture Optimization
The conditions under which therapeutic T cells are expanded ex vivo profoundly impact their eventual in vivo function.
- Cytokine Modulation: Using cytokines such as IL-7, IL-15, and IL-21 during culture promotes the development of central memory (Tcm) and stem cell memory (Tscm) T cells, which are associated with enhanced persistence and anti-tumor efficacy, compared to cultures using IL-2 [62] [64].
- Shortened Culture Time: Reducing the duration of ex vivo expansion generates "younger" T cells with lower expression of exhaustion markers and superior long-term function upon infusion [62].
Combating the Host Environment
For allogeneic therapies, overcoming host immunity is essential for persistence.
- Genetic Disruption of Alloreactivity: CRISPR/Cas9-mediated knockout of the T-cell receptor alpha constant (TRAC) gene eliminates the endogenous TCR, preventing GvHD. Concurrent knockout of β2-microglobulin (B2M) reduces surface MHC class I expression, mitigating host-versus-graft rejection [41].
- Targeting Novel Antigens: The development of allogeneic CAR-T cells targeting receptors like NKG2D, which recognizes stress ligands expressed on over 80% of solid tumors, broadens the applicability of off-the-shelf therapies beyond hematological malignancies [41].
The challenges of T-cell exhaustion and poor in vivo persistence represent significant hurdles for both autologous and allogeneic cellular therapies. Autologous products, while achieving remarkable successes in hematologic malignancies, are plagued by exhaustion and manufacturing hurdles. Allogeneic "off-the-shelf" products offer a solution to scalability but face additional barriers of host rejection and limited persistence. The future of the field lies in sophisticated engineering approaches that integrate optimized CAR designs, epigenetic reprogramming, and strategic modulation of the host environment. By leveraging the comparative insights from both platforms, next-generation therapies can be designed to resist exhaustion and achieve durable persistence, ultimately expanding the curative potential of T-cell immunotherapy to a wider range of cancers and patients.
The field of advanced cell therapies is bifurcating into two principal paradigms: autologous (patient-derived) and allogeneic (donor-derived) approaches. Each presents a unique profile of advantages and challenges concerning efficacy, safety, and manufacturability [2] [4]. Autologous therapies, such as personalized CAR-T cells, boast minimal risk of immune rejection but face hurdles related to lengthy, costly manufacturing and variable product quality due to a patient's disease state or prior treatments [3] [4]. In contrast, allogeneic, or "off-the-shelf," therapies offer immediate availability and scalable production from a single donor source but grapple with risks of host immune rejection (graft-versus-host disease, GvHD) and recipient-mediated elimination of the therapeutic cells [3] [4]. This guide objectively compares three frontier optimization techniques—cytokine armoring, desensitization strategies, and process automation—that are being leveraged to overcome these distinct challenges, directly supporting the broader research thesis on enhancing the efficacy and applicability of both therapeutic modalities.
Armoring with Cytokines: Enhancing Cell Potency and Persistence
A primary technique for augmenting the efficacy of cell therapies, particularly against the hostile solid tumor microenvironment (TME) or for improving persistence, is "armoring" through cytokine engineering. This involves genetically modifying therapeutic cells to express stimulating cytokines, aiming to reprogram the local immune milieu and boost the cells' inherent functions [68].
Experimental Data on Cytokine-Armored CAR-T Cells
The table below summarizes key clinical and preclinical findings for selected cytokine-armoring strategies, illustrating their application in both autologous and allogeneic contexts.
Table 1: Experimental Data on Selected Cytokine-Armored CAR-T Cell Therapies
| Armoring Cytokine | Therapy Context (Target Antigen) | Key Experimental Findings | Reported Efficacy Outcomes | Clinical Trial Identifier (if applicable) |
|---|---|---|---|---|
| IL-18 [68] [69] | Autologous anti-CD19 CAR-T for Lymphoma (after prior CAR-T failure) [69] | - Phase I trial (n=21); lymphodepleting chemo followed by huCART19-IL18 infusion.- Secreted IL-18 designed to recruit immune cells and boost T-cell function [69]. | - At 3 months: 81% overall response rate (ORR), 52% complete remission (CR) rate.- Several patients in remission >2 years [69]. | NCT (Not specified in source) |
| IL-15 [68] | Allogeneic/autologous CAR-T for Solid Tumors (e.g., GPC3) [68] | - Preclinical/early clinical: Enhanced proliferation, anti-tumor efficacy, and persistence.- Promoted central memory phenotype and remodeled TME in murine models [68]. | - In a syngeneic melanoma model: Enhanced intrinsic T-cell function and NK cell activation; reduced immunosuppressive M2 macrophages [68]. | NCT02905188; NCT02932956; NCT04377932 [68] |
| IL-12 [68] | Autologous CAR-T for Solid Tumors (e.g., MUC16ecto) [68] | - Functions as a "TRUCK" (T-cells Redirected for Universal Cytokine Killing) to secrete pro-inflammatory cytokines and modulate the TME [68]. | - Early-phase trials for ovarian cancer and other solid tumors show potential for enhancing anti-tumor activity [68]. | NCT02498912 [68] |
Detailed Experimental Protocol: IL-18 Armored CAR-T Cells (huCART19-IL18)
The following methodology details the process used in the recent phase I trial of huCART19-IL18 for lymphoma [69].
- Cell Sourcing & Isolation: Collect peripheral blood mononuclear cells (PBMCs) from the patient (autologous) via leukapheresis.
- Genetic Modification & Armoring:
- Isolate T-cells from PBMCs and activate them ex vivo.
- Genetically engineer the T-cells using a viral vector (e.g., lentivirus) to co-express two key components:
- A chimeric antigen receptor (CAR) targeting CD19.
- A transgene for the pro-inflammatory cytokine Interleukin-18 (IL-18).
- Expand the genetically modified CAR-T cells in culture.
- Accelerated Manufacturing: Utilize a truncated, 3-day manufacturing process (compared to the standard 9-14 days) to enable rapid treatment for patients with progressive disease [69].
- Lymphodepletion & Infusion: Patients receive a course of lymphodepleting chemotherapy (e.g., fludarabine/cyclophosphamide) prior to a single infusion of the huCART19-IL18 product at a specified dose level.
- Assessment & Monitoring:
- Efficacy: Tumor response is assessed at 3 months post-infusion using standard radiological criteria (e.g., Lugano classification) with ORR and CR as primary endpoints [69].
- Safety: Patients are closely monitored for adverse events, including Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), graded using established toxicity scales [69].
- Mechanism: Blood samples are analyzed for CAR-T cell expansion/persistence and the pharmacodynamic impact of IL-18 secretion on the immune system [69].
Signaling Pathway of IL-18 Armored CAR-T Cell
The following diagram illustrates the mechanism by which an IL-18-armored CAR-T cell enhances anti-tumor immunity upon engaging a target tumor cell.
Combating Allosensitization: Enabling Allogeneic Transplants
Allosensitization—the development of antibodies against donor human leukocyte antigens (HLAs)—is a major barrier in transplantation and allogeneic cell therapy, limiting access and increasing rejection risk [70]. Novel desensitization strategies aim to deplete these antibodies and their source cells.
Experimental Data on Novel Desensitization Agents
The table below compares emerging desensitization agents, primarily in the context of organ transplantation, with direct relevance to enabling allogeneic cell therapies.
Table 2: Experimental Data on Novel Desensitization Strategies
| Therapeutic Agent / Strategy | Mechanism of Action | Key Experimental Findings | Reported Efficacy Outcomes | Clinical Context |
|---|---|---|---|---|
| Anti-CD38 (e.g., Daratumumab, Isatuximab) [70] | Monoclonal antibody targeting CD38 on plasma cells and plasmablasts, depleting them via ADCC/CDC [70]. | - Non-human primate study: Reduced memory B & plasma cells, lowered DSA, prolonged renal graft survival (transient).- Phase I/II in kidney transplant (n=23): Transient anti-HLA antibody reduction; <40% durable response [70]. | - Creates a "window" of reduced cPRA for transplantation. Phase I/II heart transplant studies ongoing [70]. | Pre-transplant desensitization for highly sensitized patients [70]. |
| Costimulation Blockade (e.g., Belatacept) [70] | CTLA-4-Ig fusion protein blocks CD28/CD80/86 costimulation, critical for T-cell help to B-cells, disrupting germinal centers [70]. | - Preclinical: Reverses established DSA responses, prevents new B-cell activation.- Clinical (case series, n=4, cPRA>99%): Combined with proteasome inhibitor, enabled transplant across C1q-binding DSA [70]. | - Reduces anti-HLA antibodies when combined with other therapies (e.g., proteasome inhibitors) [70]. | Pre-transplant desensitization, often in combination regimens [70]. |
| Interleukin-6 (IL-6) Inhibition (e.g., Clazakizumab) [70] | Monoclonal antibody blocking IL-6, a key cytokine for plasma cell survival and T-follicular helper cell function [70]. | - Clinical: Used post-transplant for desensitization. When added to regimens for non-responsive candidates, reduces DSA mean fluorescence intensity (MFI) and prevents rebound [70]. | - Increases relative frequencies of regulatory T and B cells post-transplant. Limited data on pre-transplant monotherapy [70]. | Primarily post-transplant AMR treatment; pre-transplant use under investigation [70]. |
Detailed Experimental Protocol: Desensitization with Anti-CD38 Therapy
This protocol outlines the use of anti-CD38 therapy for desensitizing highly sensitized transplant candidates, based on recent clinical studies [70].
- Patient Selection & Baseline Assessment: Identify patients with high levels of allosensitization (e.g., calculated Panel Reactive Antibody (cPRA) >99%) and detectable Donor-Specific Antibodies (DSA). Quantify DSA levels and specificity via solid-phase immunoassays (e.g., Luminex).
- Therapeutic Regimen:
- Administer an anti-CD38 monoclonal antibody (e.g., Daratumumab) intravenously according to a defined schedule (e.g., weekly for several weeks).
- This is often an add-on therapy for patients non-responsive to standard desensitization (IVIg, PLEX, rituximab) [70].
- Monitoring & Endpoint Assessment:
- Primary Efficacy: Monitor changes in DSA strength (Mean Fluorescence Intensity, MFI) and cPRA values weekly during treatment and for several weeks post-treatment.
- Cell Depletion: Use flow cytometry to track the reduction of CD38+ plasma cells and HLA-specific IgG memory B cells in peripheral blood [70].
- Clinical Outcome: Record the proportion of patients achieving a predefined reduction in cPRA (e.g., to a level that permits identification of a suitable donor) and the success of subsequent transplantation.
- Safety Monitoring: Closely monitor for infusion-related reactions and infections due to the targeted depletion of immune cells.
Signaling Pathway of Novel Desensitization Strategies
The diagram below maps the cellular targets of key novel desensitization agents within the alloantibody production pathway.
Automation and AI: Streamlining Therapy Development and Delivery
Automation and artificial intelligence (AI) are being deployed to optimize the complex, time-sensitive manufacturing and clinical processes for both autologous and allogeneic therapies, addressing critical bottlenecks in scalability, consistency, and cost [71] [4].
Experimental Data on AI and Automation Applications
The application of these technologies spans from clinical documentation to complex manufacturing logistics.
Table 3: Experimental Data on Automation and AI in Therapeutic Processes
| Technology / Application | Stated Function | Key Experimental / Study Findings | Reported Outcome Metrics | Therapy Context |
|---|---|---|---|---|
| AI Scribe for Documentation [71] | Automatically transcribes therapy sessions and generates clinical notes using ambient AI. | - Study with 22 physicians: 89% reported reduced workload; 91% improved work-life integration; 68% observed enhanced patient engagement [71]. | - Significant reduction in time spent on clinical documentation. | Psychotherapy; applicable to clinical trial and patient management documentation. |
| AI Copilot for Clinical Workflows [71] | Assists with treatment planning and automates administrative tasks (scheduling, reminders, payments) by leveraging context from EHR. | - Use-case example: AI synthesizes client history from EHR to critique and suggest improvements to a drafted treatment plan. Automates scheduling/follow-ups [71]. | - Optimization of administrative processes, leading to more time for direct client care. | Clinical practice management; potential for patient scheduling and follow-up in clinical trials. |
| Automated & Scalable Manufacturing [4] | Uses bioreactor-based expansion and automation to scale cell production, reducing manual processes and costs. | - Allogeneic model: Enables mass production of "off-the-shelf" doses from a single donor, improving consistency and reducing cost per dose [4]. | - Transition from a high-cost, "service-based" autologous model to a scalable, financially sustainable industrial model [4]. | Manufacturing of allogeneic cell therapies; scaling up autologous production. |
Detailed Experimental Protocol: Assessing an AI Scribe in Therapeutic Practice
This methodology evaluates the impact of an AI scribe tool on therapist workload and patient engagement, based on a cited study [71].
- Tool Setup & Configuration:
- Implement an AI scribe tool (e.g., integrated into practice management software).
- Pre-set transcription parameters: note template, output language, participant naming convention (first name/therapist), writing perspective (clinical format), and verbosity (detailed) [71].
- Informed Consent: Prior to use, practitioners must obtain signed informed consent from patients, detailing the purpose of recording and transcription, data usage, and privacy safeguards [71].
- Intervention & Data Collection:
- Experimental Group: Therapists conduct sessions as usual with the AI scribe active, automatically transcribing the session and generating notes.
- Control Group: Therapists continue with traditional, manual note-taking.
- Outcome Assessment:
- Primary Endpoints:
- Workload: Measure time spent on documentation pre- and post-intervention using self-reported logs or system data.
- User Experience: Administer validated workload and work-life integration scales (e.g., the study reported 89% reduced workload, 91% improved integration) [71].
- Secondary Endpoint:
- Patient Engagement: Therapist-reported observations on changes in patient engagement during sessions (e.g., 68% of physicians observed enhancement) [71].
- Primary Endpoints:
- Data Analysis: Use statistical tests (e.g., t-tests) to compare the mean differences in time savings and survey scores between the experimental and control groups.
Workflow of an AI Copilot in Therapy Practice Management
The diagram below visualizes how an AI copilot integrates into and optimizes key clinical and administrative workflows.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table catalogs key reagents and technologies fundamental to implementing the optimization techniques discussed in this guide.
Table 4: Key Research Reagent Solutions for Featured Techniques
| Item / Technology | Primary Function in Research | Specific Application Example |
|---|---|---|
| Cytokine Gene Constructs (IL-18, IL-15, IL-12) [68] | Genetic payload to "armor" effector cells, enhancing their potency and persistence in the TME. | Co-expressed with a CAR in T-cells via a viral vector to create huCART19-IL18 [68] [69]. |
| Anti-CD38 Monoclonal Antibodies (e.g., Daratumumab) [70] | Research tool to deplete CD38+ plasma cells and plasmablasts in vitro and in vivo to study their role in allosensitization. | Used in pre-clinical NHP models and clinical trials to assess efficacy in reducing DSA for transplant desensitization [70]. |
| Costimulation Blockers (e.g., CTLA-4-Ig/Belatacept) [70] | To inhibit the CD28/CD80/86 costimulation pathway in vitro and in vivo, disrupting T-cell help for B-cell activation. | Studied in combination with proteasome inhibitors to prevent DSA rebound after plasma cell depletion [70]. |
| HIPAA-Compliant AI Scribe/Copilot Platform [71] | To automate and analyze clinical or laboratory documentation, transcriptions, and workflow management in a secure environment. | Used in clinical studies to transcribe therapy sessions and generate notes, reducing administrative burden on clinicians [71]. |
| CRISPR/Cas9 Gene Editing Systems [2] | To create precise genetic modifications in donor-derived cells, potentially knocking out genes to reduce immunogenicity (e.g., TCR) for allogeneic therapies. | Engineering "hypoimmune" iPSCs to evade immune detection, creating universal "off-the-shelf" cell products [2]. |
Evidence-Based Assessment: Clinical Outcomes and Comparative Efficacy
The choice between autologous (using a patient's own cells) and allogeneic (using donor-derived cells) stem cell transplantation represents a critical crossroads in the treatment of hematologic malignancies and other disorders [4]. Each approach presents a distinct risk-benefit profile, shaped by fundamental biological differences. Autologous stem cell transplantation (auto-SCT) leverages a patient's own harvested cells, thereby eliminating the risk of immune rejection and graft-versus-host disease (GvHD) and typically requiring no long-term immunosuppression [4] [2]. However, its therapeutic potential can be limited by the inability to elicit a graft-versus-tumor effect and the risk of reinfusing malignant cells [4].
In contrast, allogeneic stem cell transplantation (allo-SCT) introduces a new immune system from a healthy donor, which can mount a powerful graft-versus-leukemia (GvL) or graft-versus-myeloma (GvMM) effect, providing a potent mechanism for long-term disease control [72]. This benefit, however, comes at the cost of significant risks, including a higher incidence of treatment-related mortality, GvHD, and the need for prolonged immunosuppressive therapy [65] [73]. The clinical decision is further influenced by logistical considerations; autologous therapies are patient-specific, often involving complex, time-sensitive manufacturing, while allogeneic therapies offer the potential for "off-the-shelf" availability from pre-prepared cell banks [4] [2]. This guide objectively analyzes recent clinical trial data to compare the efficacy of these two cornerstone approaches across major disease indications.
Comparative Efficacy Data Across Hematologic Malignancies
Clinical outcomes for auto-SCT and allo-SCT vary significantly depending on the disease type, patient status, and treatment history. The following tables summarize key response and survival metrics from recent meta-analyses and clinical studies.
Table 1: Survival and Response Outcomes of Allogeneic Transplantation in Multiple Myeloma (Meta-Analysis of 61 Studies, 2013-2023) [72]
| Outcome Measure | Pooled Estimate | NDMM/Frontline Setting | RRMM/Salvage Setting |
|---|---|---|---|
| Complete Response (CR) Rate | 45% | 54% | 31% |
| 5-Year Overall Survival (OS) | 45% | 69% | 24% |
| 5-Year Progression-Free Survival (PFS) | 25% | 40% | 10% |
| 5-Year Non-Relapse Mortality (NRM) | 20% | 11% | 15% |
Table 2: Comparison of Auto-SCT vs. Allo-SCT in Relapsed/Refractory B-cell Non-Hodgkin Lymphoma (Meta-Analysis of 18 Retrospective Studies) [74]
| Outcome Measure | Autologous SCT | Allogeneic SCT | P-value |
|---|---|---|---|
| Overall Survival (OS) | Favored (OR: 1.69) | Lower | < 0.001 |
| Progression-Free Survival (PFS) | No significant difference | No significant difference | 0.891 |
| Transplant-Related Mortality (TRM) | Lower (OR: 0.23) | Higher | < 0.001 |
| Relapse/Progression Rate | Higher (OR: 2.37) | Lower | < 0.001 |
Table 3: Key Prognostic Factors for Survival after Allo-SCT in Acute Lymphoblastic Leukemia (Single-Center Analysis of 180 Patients) [73]
| Prognostic Factor | Impact on Survival | Statistical Significance |
|---|---|---|
| Remission Status at Transplant | Better survival with CR1/CR2 vs. no remission | Significant |
| Conditioning with Total Body Irradiation (TBI) | Improved survival with TBI-based conditioning | Significant |
| Patient Age (<55 vs. ≥55 years) | No significant difference observed | Not Significant |
| Immunophenotype (e.g., T-ALL, Ph+ B-ALL) | No significant difference observed | Not Significant |
Detailed Methodologies of Key Clinical Studies
The data presented in the previous section are derived from studies with rigorous methodologies. Understanding their experimental design is crucial for interpreting the results accurately.
Comprehensive Literature Review and Meta-Analysis in Multiple Myeloma
A 2024 meta-analysis sought to verify the efficacy and survival outcomes of allo-SCT in multiple myeloma patients by synthesizing a decade of evidence [72].
- Search Strategy and Data Extraction: The investigators conducted a systematic search of four major databases (PubMed, Embase, Cochrane Library, and Web of Science) for studies published between April 2013 and April 2023. The search term used was "(Allogenic) AND (myeloma)". After duplicate removal and screening, 61 studies meeting the inclusion criteria were selected for final analysis. Data extracted from each study included patient demographics, best recorded response rates (CR, VGPR, PR), and key survival metrics (Overall Survival, Progression-Free Survival, and Non-Relapse Mortality) at multiple time points (1, 2, 3, 5, and 10 years) [72].
- Statistical Analysis: The analysis employed a random-effects model to calculate pooled estimates for all outcomes, presented with 95% confidence intervals. Heterogeneity was assessed using the I² statistic. The stability of the pooled results was confirmed through sensitivity analysis, and potential publication bias was evaluated using funnel plots complemented by Begg's and Egger's tests [72].
Individual Patient Data Analysis in Relapsed Myeloma
A 2025 study directly compared allo-SCT with a second auto-SCT in patients with multiple myeloma relapsing after first-line auto-SCT [65].
- Data Sources: This analysis utilized individual patient data from two large international databases: the Japan Society for Hematopoietic Stem Cell Transplantation and the Center for International Blood & Marrow Transplant Research (CIBMTR). This provided data on 815 patients. To incorporate evidence from smaller studies, the researchers digitized Kaplan-Meier survival curves from three additional publications using the Shiny app [65].
- Outcomes and Synthesis: The primary endpoints were Overall Survival (OS) and Progression-Free Survival (PFS). Meta-analyses were performed using R software (version 4.3.3), and survival curves were compared using log-rank tests in SPSS. This methodology allowed for a powerful, pooled analysis comparing the two intervention strategies directly [65].
Meta-Analysis in B-cell Non-Hodgkin Lymphoma (B-NHL)
A 2020 meta-analysis compared the efficacy of auto-SCT versus allo-SCT in patients with relapsed or refractory B-NHL [74].
- Study Selection and Quality Assessment: Researchers searched Medline, CENTRAL, and EMBASE databases through December 2019. The analysis included 18 retrospective studies encompassing 8,058 patients. The quality of the included studies was critically appraised using the ROBINS-I tool (Risk Of Bias In Non-randomized Studies-of Interventions) by two independent reviewers [74].
- Outcome Measures and Statistical Methods: The primary endpoints were OS and PFS. Secondary outcomes included transplant-related mortality (TRM), event-free survival, and relapse/progression. Effect sizes were calculated as odds ratios (OR) with 95% confidence intervals. A random-effects model was applied when significant heterogeneity (I² >50%) was detected. Subgroup analyses were also performed for different grades and subtypes of B-NHL [74].
Visualizing Core Concepts and Decision Pathways
The following diagrams illustrate the fundamental biological principles and key clinical decision-making considerations when comparing autologous and allogeneic therapies.
The Scientist's Toolkit: Essential Reagents and Materials
The conduct of stem cell transplantation and related research relies on a suite of specialized reagents and materials. The following table details key solutions and their critical functions in both clinical and experimental settings.
Table 4: Key Research Reagent Solutions in Stem Cell Therapy
| Research Reagent / Material | Primary Function | Application Context |
|---|---|---|
| HLA Typing Kits | Identification of human leukocyte antigens to match donor and recipient, critical for minimizing GvHD and rejection in allo-SCT. | Donor selection for allogeneic transplantation [73]. |
| Mobilizing Agents (e.g., G-CSF) | Stimulate the release of hematopoietic stem cells from bone marrow into peripheral blood for collection via apheresis. | Stem cell harvest for both autologous and allogeneic donation [65] [74]. |
| Cryopreservation Media | Protect cells from ice-crystal damage during freezing and long-term storage in liquid nitrogen. | Preservation of harvested stem cell products pre-transplant [4]. |
| Conditioning Regimen Agents | Myeloablative or reduced-intensity chemotherapy/radiotherapy to eliminate residual disease and suppress host immunity. | Patient preparation pre-transplant to enable engraftment [73] [72]. |
| Immunosuppressants (e.g., Cyclosporine, MTX) | Suppress the donor's immune system to prevent graft rejection and moderate GvHD after allo-SCT. | Standard GvHD prophylaxis and management post-allo-SCT [65] [73]. |
| Cell Selection & Expansion Media | Select for specific cell populations (e.g., CD34+ cells) and support their ex vivo expansion. | Manufacturing of cellular products, particularly in autologous CAR-T therapies [2]. |
| CRISPR/Cas9 Systems | Enable precise gene editing for developing next-generation allogeneic "off-the-shelf" cell therapies with reduced immunogenicity. | Research and development of hypoimmune iPSC-derived cell products [75] [2]. |
The objective analysis of clinical trial data reveals a nuanced efficacy landscape for autologous and allogeneic stem cell transplantation. Auto-SCT is often associated with superior overall survival in certain settings, such as relapsed B-NHL and multiple myeloma, primarily due to its more favorable safety profile and lower treatment-related mortality [65] [74]. Conversely, allo-SCT provides a potent graft-versus-tumor effect that translates into lower relapse rates and can offer a curative potential for high-risk leukemias and a plateau in long-term survival curves for some myeloma patients [73] [72]. The choice is not one of superiority but of contextual optimization, heavily influenced by disease type, risk profile, remission status, and patient fitness [65] [74] [73].
Future prospects in the field are focused on overcoming the current limitations of both modalities. For allogeneic therapies, research is directed at mitigating GvHD and NRM through improved conditioning regimens, better GvHD prophylaxis, and the development of "off-the-shelf" universal cell products using gene-editing technologies like CRISPR to create hypoimmune induced pluripotent stem cells (iPSCs) [75] [2]. For autologous therapies, the goals are to reduce manufacturing time, control costs, and enhance the efficacy of products like CAR-T cells [4] [2]. The ongoing integration of advanced cellular engineering, immune modulation, and precision medicine is poised to further refine the risk-benefit calculus, ultimately expanding the therapeutic options available to patients.
The therapeutic application of mesenchymal stem cells (MSCs) has emerged as a promising regenerative strategy for heart failure (HF), a chronic progressive condition affecting over 55 million people globally and representing a significant cause of morbidity and mortality worldwide [76] [77]. Within MSC-based therapeutics, a fundamental distinction exists between autologous MSCs (AutoMSCs), derived from the patient's own tissues, and allogeneic MSCs (AlloMSCs), sourced from healthy donors. This comparison guide provides an objective analysis of their relative efficacy, synthesizing evidence from recent meta-analyses of randomized controlled trials (RCTs) to inform researchers, scientists, and drug development professionals. The central thesis framing this content posits that while AlloMSCs offer practical "off-the-shelf" advantages, the functional potency and immunological compatibility of AutoMSCs may yield differential clinical outcomes in HF patients, necessitating a nuanced understanding of their comparative performance profiles.
Comparative Efficacy Data Analysis
Functional and Structural Outcomes
Quantitative synthesis from recent meta-analyses reveals distinct patterns in how autologous and allogeneic MSCs influence cardiac function and structure. The data, derived from imaging modalities such as cardiac MRI and echocardiography, provide objective measures of therapeutic effect.
Table 1: Comparison of Functional and Structural Cardiac Outcomes
| Outcome Measure | Autologous MSCs | Allogeneic MSCs | Notes |
|---|---|---|---|
| LVEF Improvement | 2.17% (95% CI: -0.48% to 5.67%) [78] | 0.86% (95% CI: -1.21% to 2.94%) [78] | Not statistically significant between sources |
| LVEDV Reduction | Not statistically significant [78] | -2.08 mL (95% CI: -3.52 to -0.64 mL) [78] | Indicates positive reverse remodeling |
| LVESV Reduction | -9.14 mL (MD, p<0.001) [79] | Data not specifically reported | Combined analysis shows significant benefit |
| 6-MWD Improvement | 31.71 m (95% CI: -8.91 to 71.25 m) [78] | 31.88 m (95% CI: 5.03 to 58.74 m) [78] | Significant improvement only with AlloMSCs |
LVEF: Left Ventricular Ejection Fraction; LVEDV: Left Ventricular End-Diastolic Volume; LVESV: Left Ventricular End-Systolic Volume; 6-MWD: 6-Minute Walk Distance
The efficacy profile varies by cell source. Allogeneic MSCs demonstrate a statistically significant advantage in promoting reverse cardiac remodeling, as evidenced by reduced LVEDV [78]. In functional capacity, AlloMSCs also show a more consistent improvement in the 6-minute walk test, though both sources produce similar magnitude effects [78]. For LVEF improvement, autologous MSCs show a numerically greater, though not statistically significant, increase compared to allogeneic sources [78].
Clinical Event Outcomes
Analysis of hard clinical endpoints provides crucial insight into the real-world therapeutic impact of MSC source on patient outcomes.
Table 2: Clinical Event Outcomes Following MSC Therapy
| Outcome Measure | Autologous MSCs | Allogeneic MSCs | Combined MSCs |
|---|---|---|---|
| All-Cause Mortality | RR = 0.78 (95% CI: 0.62-0.99, p=0.04) [79] | Similar safety profile [78] | Significant reduction vs. controls |
| HF Rehospitalization | RR = 0.67 (95% CI: 0.49-0.90, p=0.008) [79] | Not statistically significant [79] | RR = 0.85 (95% CI: 0.71-1.01, p=0.06) [79] |
| Major Adverse Cardiac Events (MACE) | No increased risk [76] | No increased risk [78] [76] | Not associated with increased risk |
Autologous MSCs demonstrate a significant advantage in reducing heart failure rehospitalization rates, with a 33% relative risk reduction compared to controls [79]. Both MSC sources show a favorable mortality benefit when analyzed collectively, with no increased risk of Major Adverse Cardiac Events (MACE) compared to control groups, confirming an acceptable safety profile for both approaches [78] [79] [76].
Quality of Life and Long-Term Outcomes
Beyond physiological measures, MSC therapy demonstrates benefits in patient-reported outcomes. A 2025 meta-analysis found that MSC transplantation significantly improved quality of life (QoL) for HFrEF patients (Hedges' g = -0.518, p = 0.01), though it did not significantly improve other efficacy outcomes like LVEF [76]. The analysis did not distinguish between autologous and allogeneic sources for this particular outcome. For long-term functional improvement, the timing of assessment appears crucial. One meta-analysis reported that LVEF benefits from MSC therapy were significant at follow-up intervals of less than 6 months, 6 months, and 12 months, but not beyond 12 months, regardless of the cell source [80].
Methodological Approaches in Meta-Analyses
Search Strategy and Study Selection
Recent systematic reviews and meta-analyses have employed rigorous methodology following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [78] [79] [76]. The typical search strategy involves:
- Database Utilization: Comprehensive searches across major electronic databases including PubMed, EMBASE, Cochrane Library, Web of Science, clinicaltrials.gov, and regional databases [80] [79].
- Search Terms: Combination of Medical Subject Headings (MeSH) and text words including "heart failure," "congestive heart failure," "mesenchymal stem cells," "mesenchymal stromal cells," and "randomized controlled trial" [78] [79].
- Time Frame: Most recent analyses cover publications up to early 2024, with some focusing specifically on trials from 2018 onward to capture the most contemporary evidence [76].
- Screening Process: Independent review by at least two investigators with consultation from a third reviewer to resolve discrepancies [79].
Inclusion and Exclusion Criteria
Standardized criteria ensure the inclusion of comparable, high-quality evidence:
- Study Design: Restriction to phase I/II/III randomized controlled trials (RCTs) [78] [79].
- Population: Patients with heart failure with reduced ejection fraction (HFrEF), typically with LVEF <40%, both ischemic and non-ischemic etiology [79] [76].
- Intervention: MSC therapy as a sole treatment modality, regardless of route of administration [78].
- Comparator: Control groups receiving placebo or standard care only [79].
- Outcomes: Required reporting of predefined endpoints including LVEF, mortality, hospitalization, or functional capacity measures [78] [79].
Data Extraction and Quality Assessment
Standardized data extraction encompasses:
- Study Characteristics: Author, publication year, sample size, demographic information, follow-up duration [80] [79].
- Intervention Details: MSC source (autologous/allogeneic), tissue origin, cell dosage, route of administration, delivery timing [78] [79].
- Outcome Data: Baseline and follow-up values for continuous outcomes (LVEF, volumes); event counts for clinical outcomes [78].
- Quality Assessment: Evaluation using Cochrane Risk of Bias tool or Jadad scale, with studies scoring ≥3 considered high quality [78] [79].
Statistical Analysis
Analytical approaches include:
- Effect Measures: Weighted mean difference (WMD) for continuous variables; risk ratio (RR) for dichotomous outcomes [78] [79].
- Heterogeneity Assessment: I² statistic and chi-square tests to determine appropriate use of fixed or random effects models [80] [79].
- Subgroup Analysis: Preplanned analyses by cell source (autologous vs. allogeneic), delivery route, cell dosage, and HF etiology [78] [79].
- Sensitivity Analysis: Investigation of the influence of individual studies and specific cell types (e.g., exclusion of adipose-derived cells) [78].
Systematic Review Methodology for MSC Efficacy Analysis
Mechanisms of Action and Technical Considerations
Therapeutic Mechanisms of MSCs in Heart Failure
MSCs exert their beneficial effects in heart failure through multiple interconnected mechanisms rather than direct cardiomyocyte differentiation:
- Paracrine Signaling: MSCs secrete a multitude of bioactive factors including growth factors, cytokines, and chemokines that promote tissue repair, reduce apoptosis, and modulate immune responses [78] [76].
- Mitochondrial Transfer: MSCs can directly transfer healthy mitochondria to damaged cardiomyocytes via tunneling nanotubes, restoring cellular energy production and viability [76].
- Angiogenesis Induction: MSC-secreted factors stimulate the formation of new blood vessels, improving perfusion to the compromised myocardium [76].
- Anti-fibrotic Effects: MSCs reduce pathological collagen deposition and interstitial fibrosis, thereby improving myocardial compliance and function [78].
- Immunomodulation: Both autologous and allogeneic MSCs modulate the local and systemic immune environment, reducing detrimental inflammation [79].
Immunological Considerations by Cell Source
The immunological properties of MSCs significantly influence their therapeutic application:
- Autologous MSCs: Benefit from complete histocompatibility, eliminating rejection concerns. However, they may exhibit reduced potency in elderly patients or those with multiple comorbidities due to age-related cellular senescence [81].
- Allogeneic MSCs: Considered immune-privileged due to low MHC class II expression, enabling use without matching. However, they may undergo an immunogenic shift after differentiation and transplantation, potentially triggering immune memory responses that could limit long-term efficacy [78] [81].
Mechanisms of MSC-Mediated Cardiac Repair
Research Reagent Solutions and Technical Tools
Table 3: Essential Research Reagents and Materials for MSC Studies
| Reagent/Material | Function/Application | Specifications/Standards |
|---|---|---|
| MSC Characterization Antibodies | Verification of MSC phenotype via flow cytometry | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [76] |
| In Vitro Differentiation Kits | Assessment of multipotent differentiation capacity | Adipogenic, osteogenic, chondrogenic induction media [76] |
| Cell Delivery Catheters | Intramyocardial or intracoronary administration | Specialized catheters for transendocardial injection or intracoronary infusion [79] |
| Imaging Contrast Agents | Cardiac MRI assessment of function and remodeling | Gadolinium-based agents for scar assessment; tracking of engraftment [78] |
| Cell Culture Media | MSC expansion and maintenance | Serum-free media formulations; quality control during passage [78] |
| Cryopreservation Media | Banking for allogeneic "off-the-shelf" products | Maintain viability and potency after thawing [78] |
The research reagents outlined in Table 3 represent essential tools for conducting rigorous MSC research and clinical applications. For cell characterization, antibody panels confirming the International Society for Cellular Therapy criteria are fundamental for ensuring population purity and reproducibility across studies [76]. Differentiation kits provide critical validation of MSC multipotency, while specialized delivery catheters enable precise therapeutic targeting. Advanced imaging contrast agents facilitate comprehensive assessment of both structural and functional outcomes in preclinical and clinical studies [78].
This comparative analysis of autologous versus allogeneic MSCs for heart failure treatment reveals a complex efficacy landscape with distinct advantages for each approach. The evidence synthesized from recent meta-analyses indicates that autologous MSCs demonstrate superior performance in reducing heart failure rehospitalization and show a numerically greater, though not statistically significant, improvement in LVEF [78] [79]. Conversely, allogeneic MSCs offer significant benefits in promoting reverse cardiac remodeling and demonstrate more consistent improvement in functional capacity measures, coupled with the practical advantage of off-the-shelf availability [78].
Both MSC sources demonstrate a favorable safety profile with no increased risk of major adverse cardiac events and a potential mortality benefit compared to standard care [78] [79] [76]. The choice between autologous and allogeneic approaches therefore involves careful consideration of specific clinical priorities, logistical constraints, and patient characteristics. Future research directions should include larger, more standardized trials directly comparing both cell sources, optimization of delivery timing and methods, and development of potency assays to predict therapeutic efficacy. These advances will help refine the place of MSC therapy in the evolving landscape of heart failure treatment and potentially enable personalized approaches based on patient-specific factors and therapeutic goals.
The available literature I found focuses exclusively on choroid plexus tumors and their treatment with conventional therapies like surgery, chemotherapy, and radiation [82] [83] [84]. None of the articles discuss cellular immunotherapies or the associated adverse events you're interested in.
How to Find the Information You Need
To obtain the current and accurate data required for your guide, I suggest the following approaches:
- Search Specialized Scientific Databases: Conduct a targeted search on platforms like PubMed, Google Scholar, or Scopus. Using specific keywords such as "allogeneic CAR-T CRS incidence," "autologous vs allogeneic ICANS," or "adverse events bispecific antibodies clinical trial" will yield more relevant results.
- Consult Clinical Trial Registries: Review results on ClinicalTrials.gov for completed and ongoing studies of autologous and allogeneic therapies. The "results" sections often contain detailed safety data, including the incidence of specific adverse events.
- Reference Recent Review Articles: Look for recent meta-analyses or systematic reviews in high-impact journals (e.g., Nature Reviews Drug Discovery, Blood, The New England Journal of Medicine) that synthesize safety data across multiple clinical trials for these therapy types.
I hope these suggestions help you locate the necessary information. If you would like to explore a different aspect of choroid plexus tumors or another topic, I would be glad to assist.
The long-term success of adoptive cell therapies is fundamentally linked to the persistence and durability of the administered therapeutic cells in the recipient. Cellular persistence refers to the sustained survival and functional maintenance of engineered cells within the patient's biological environment, directly determining the durability of therapeutic response and potential for long-term disease control [85]. This correlation between cell longevity and clinical outcomes establishes persistence as a critical benchmark for evaluating both autologous (patient-derived) and allogeneic (donor-derived) therapeutic approaches [86].
The biological mechanisms governing persistence differ substantially between autologous and allogeneic platforms. Autologous cells, derived from the patient themselves, naturally avoid immune rejection but may suffer from functional exhaustion or pre-existing deficiencies due to the patient's disease state or prior treatments [4]. Conversely, allogeneic cells sourced from healthy donors typically exhibit robust potency but face host versus graft reactions and potential elimination by the recipient's immune system, necessitating sophisticated engineering strategies to overcome these barriers [86] [2]. Understanding these distinct persistence profiles is essential for selecting appropriate therapeutic modalities for specific clinical contexts and patient populations.
Comparative Persistence Profiles: Autologous vs. Allogeneic Therapies
Table 1: Key Characteristics Influencing Cellular Persistence
| Characteristic | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Immune Compatibility | High (self-origin avoids rejection) | Low (requires HLA matching/engineering) |
| Risk of GvHD | Negligible [2] | Present (requires TCR disruption) [86] |
| Host vs. Graft Response | Not applicable | Significant challenge [4] |
| Starting Cell Fitness | Variable (can be compromised) [4] | Consistently high (healthy donor) [4] |
| Persistence Timeline | Potential for long-term (months/years) [4] | Often limited (requires "stealth" engineering) [86] |
| Major Limitation | Functional exhaustion, manufacturing delays [85] [4] | Immune-mediated rejection [86] |
Clinical data reveals how these characteristics translate to tangible outcomes. For allogeneic therapies, a 2025 meta-analysis of relapsed/refractory large B-cell lymphoma reported a pooled best overall response rate of 52.5% and complete response rate of 32.8%, demonstrating encouraging efficacy despite potential persistence barriers [86]. The same analysis highlighted a remarkably low incidence of severe cytokine release syndrome (0.04%) and neurotoxicity (0.64%), suggesting that allogeneic products may have a different biological activity profile than their autologous counterparts [86].
Autologous CAR-T therapies have shown the potential for remarkable durability in responsive patients, with studies detecting CAR-positive T cells persisting up to 10 years post-infusion [86]. This long-term engraftment exemplifies the ideal persistence scenario, where patient-derived cells establish a permanent, functional population capable of sustained disease control. However, such outcomes are not universal, and a significant challenge for autologous approaches remains the variable fitness of patient-derived T cells, which can display functional exhaustion before ever reaching the manufacturing facility [85].
Measuring and Modeling Persistence: Experimental Frameworks
Methodologies for Quantifying Cellular Longevity
Tracking cellular persistence in patients and preclinical models requires sophisticated methodological approaches that combine direct detection with functional assessments:
- Flow Cytometry & PCR Tracking: Longitudinal monitoring of engineered cells in patient blood and tissue samples using flow cytometry for surface markers (e.g., CAR detection) and quantitative PCR for vector-specific sequences provides direct quantification of cell survival and expansion dynamics [86].
- Functional Potency Assays: Following in vivo persistence, cells are often isolated and re-challenged with antigen-positive targets in vitro to measure retained cytotoxic activity and cytokine production, confirming that persisting cells remain functionally competent rather than anergic [87].
- Disease-Specific Biomarkers: For non-malignant conditions, persistence is correlated with stabilization or improvement of disease-specific biomarkers. For example, in aging-related applications, successful intervention is measured by reduction in inflammatory markers like IL-6 and TNF-α, indicating functional activity of the administered cells [87].
Experimental Workflow for Persistence Studies
The following diagram illustrates a standardized experimental workflow for evaluating cellular persistence from manufacturing through long-term follow-up:
Experimental Workflow for Persistence Studies
Engineering Solutions for Enhanced Persistence
Strategies for Autologous Therapies
- Stem-like Memory T-cell Generation: Modifying culture conditions to preserve less differentiated T-cell states (T-stem cell memory, central memory) significantly enhances in vivo expansion potential and longevity compared to terminally differentiated effector T cells [85]. These precursor populations demonstrate enhanced capacity to expand and persist long-term, correlating with improved therapeutic outcomes [85].
- Epigenetic Reprogramming: Disruption of exhaustion-associated genes such as TET2 has demonstrated remarkable success in enhancing autologous CAR-T cell persistence, with one reported case showing a single CAR-T cell clone dominating the response and leading to complete remission [85].
- Cytokine Support: Incorporation of IL-7 and IL-15 signaling during manufacturing promotes the generation of memory stem T cells from naive precursors, establishing a population with superior self-renewal capacity and persistence potential [85].
Strategies for Allogeneic Therapies
- TCR Disruption: Using CRISPR/Cas9 gene editing to knockout the T-cell receptor α constant (TRAC) locus eliminates TCR-mediated graft-versus-host disease, making allogeneic T cells safer but requiring additional modifications to prevent host rejection [86].
- Immune Evasion Engineering: Strategies including β2-microglobulin (B2M) knockout to disrupt HLA class I expression, overexpression of non-classical HLA molecules (HLA-E, HLA-G), and incorporation of alloimmune-defense receptors (ADR) help engineered cells evade host immune detection and extend their functional persistence [86].
- Persistence-Enhanced NK Cells: For allogeneic CAR-NK platforms, engineering approaches include multicistronic constructs incorporating autocrine IL-15 cytokine support, which significantly enhances their persistence and antitumor activity without the need for exogenous cytokine administration [86].
Table 2: Engineering Strategies to Overcome Persistence Barriers
| Therapy Platform | Persistence Challenge | Engineering Solution | Mechanism of Action |
|---|---|---|---|
| Autologous T Cells | Functional exhaustion, differentiation | Preserve stem-like memory phenotype | Enhanced self-renewal capacity, reduced terminal differentiation [85] |
| Autologous T Cells | Epigenetic programming toward exhaustion | Disrupt exhaustion-associated genes (e.g., TET2) | Redirects differentiation toward persistent, functional memory state [85] |
| Allogeneic T Cells | Graft-versus-host disease (GvHD) | TCR knockout (e.g., TRAC disruption) | Prevents recognition of host antigens as foreign [86] |
| Allogeneic T Cells | Host immune rejection | B2M knockout + HLA engineering | Reduces host CD8+ T cell recognition while maintaining immune function [86] |
| Allogeneic NK Cells | Limited in vivo persistence | Autocrine cytokine support (e.g., IL-15) | Provides survival signals without exogenous cytokine administration [86] |
The Scientist's Toolkit: Essential Reagents and Technologies
Table 3: Key Research Reagents for Persistence Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Cell Culture Additives | IL-7, IL-15, IL-21 | Promote stem-like memory T cell differentiation and prevent exhaustion during expansion [85] |
| Gene Editing Tools | CRISPR/Cas9 systems, TALENs | Knockout of endogenous TCR (TRAC), B2M, or exhaustion-associated genes (TET2, DNMT3A) [86] [85] |
| Cell Sorting Markers | Anti-CD62L, Anti-CCR7, Anti-CD45RA | Isolation of naive and memory T cell subsets with enhanced persistence potential [85] |
| Persistence Tracking | Flow cytometry antibodies, qPCR primers | Detection of CAR expression, vector sequences, and donor-specific markers in longitudinal studies [86] |
| Cytokine Detection | IFN-γ, IL-2 ELISA/ELLA, Multiplex Luminex | Functional assessment of persisting cells upon antigen re-stimulation [87] |
Biological Pathways Governing Cell Longevity
The persistence of therapeutic cells is regulated by interconnected biological pathways that control differentiation, metabolism, and apoptosis. The following diagram illustrates key signaling networks that can be targeted to enhance cellular longevity:
Signaling Pathways Governing T Cell Persistence
This network illustrates the balance between persistence-promoting pathways (green) and exhaustion-driving pathways (red). Successful therapeutic engineering requires careful manipulation of these signaling networks to maintain cells in a state conducive to long-term survival and function.
The correlation between cellular persistence and therapeutic durability remains a fundamental consideration in advanced therapy development. While autologous approaches naturally circumvent alloreactivity risks and have demonstrated potential for long-term engraftment measured in years, their manufacturing complexities and variable starting cell quality present significant challenges [4]. Allogeneic platforms offer scalability and immediate availability but require sophisticated engineering to overcome host immune recognition and rejection [86].
Future progress will likely emerge from several promising frontiers. The application of epigenetic reprogramming to prevent or reverse exhaustion programming in both autologous and allogeneic cells represents a powerful approach to extend functional persistence [85]. Additionally, precision gene editing technologies continue to evolve, enabling more sophisticated immune evasion strategies while enhancing antitumor potency [86]. Finally, the development of novel biomarker panels that can predict persistence potential prior to treatment will enable better patient selection and product matching, ultimately improving clinical outcomes across both therapeutic platforms [87] [88]. As these technologies mature, the careful balancing of persistence, potency, and safety will continue to define the next generation of cellular therapeutics.
Conclusion
The choice between autologous and allogeneic cell therapy is not a matter of superiority but of strategic application, dictated by disease type, urgency, and patient-specific factors. Autologous therapies offer personalized safety with minimal rejection risks, while allogeneic 'off-the-shelf' products provide scalability and immediate availability. Future progress hinges on advanced genetic engineering to create hypoimmunogenic cells, refined manufacturing for consistent product quality, and combination strategies to enhance persistence and efficacy. For researchers, the focus must be on developing next-generation platforms that integrate the strengths of both approaches to broaden patient access and improve clinical outcomes across a wider range of diseases.
References
- 1. Differences Between Autologous and Allogeneic Cell ... [https://www.patheon.com/us/en/insights-resources/blog/differences-between-autologous-and-allogeneic-cell-therapies.html]
- 2. Autologous vs allogenic cell therapy: key differences and ... [https://greenelephantbiotech.com/blog/autologous-vs-allogenic-cell-therapy-key-differences-and-applications/]
- 3. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 4. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 5. Efficacy and safety of allogeneic CD19 CAR NK-cell ... [https://pubmed.ncbi.nlm.nih.gov/41240964/]
- 6. CAR T-Cell Therapy Plus Auto-HSCT Demonstrate Efficacy ... [https://www.targetedonc.com/view/car-t-cell-therapy-plus-auto-hsct-demonstrate-efficacy-safety-in-ph-b-all]
- 7. Addressing graft-versus-host disease in allogeneic cell-based immunotherapy for cancer | Experimental Hematology & Oncology | Full Text [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00654-3]
- 8. Genome-edited allogeneic CAR-T cells: the next generation of cancer immunotherapies | Journal of Hematology & Oncology | Full Text [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01745-8]
- 9. Allogene Therapeutics Announces Publication of Durable Response Data from Phase 1 ALPHA/ALPHA2 Trials of the Allogeneic CAR T Cemacabtagene Ansegedleucel/ALLO-501 in Relapsed/Refractory Large B-Cell Lymphoma in the Journal of Clinical Oncology [https://www.globenewswire.com/news-release/2025/02/13/3026325/0/en/Allogene-Therapeutics-Announces-Publication-of-Durable-Response-Data-from-Phase-1-ALPHA-ALPHA2-Trials-of-the-Allogeneic-CAR-T-Cemacabtagene-Ansegedleucel-ALLO-501-in-Relapsed-Refra.html]
- 10. Graft-Versus-Host Disease - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538235/]
- 11. Frontiers | Novel therapies for graft versus host disease with a focus on cell therapies [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1241068/full]
- 12. Myth or reality: Graft versus host disease after autologous hematopoietic cell transplantation, a multicentre experience - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0966327425001145]
- 13. Skin Graft-versus-host Disease Following Autologous Stem Cell Transplantation for Multiple Myeloma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3718921/]
- 14. Emerging trends in clinical allogeneic CAR cell therapy [https://pubmed.ncbi.nlm.nih.gov/40367950/]
- 15. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 16. A comparison of haematopoietic stem cells from umbilical cord ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6850637/]
- 17. Recent Stem Cell Advances: Cord Blood and Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4961100/]
- 18. Comparative analysis of human induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8435459/]
- 19. Allogeneic "Off-the-Shelf" Cell Therapies: [https://www.hyperec.com/blog/allogeneic-off-the-shelf-cell-therapies/]
- 20. Allogeneic Cell Therapy - Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/allogeneic-cell-therapy.html]
- 21. Supporting Scalable Cell Therapy Using Allogeneic ... [https://ispe.org/pharmaceutical-engineering/november-december-2021/supporting-scalable-cell-therapy-using-allogeneic]
- 22. Current Progress of Cell Therapy Clinical Trials in China ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547621/]
- 23. 2025 Cell and Gene Therapy Report Looks at Industry ... [https://www.targetedonc.com/view/2025-cell-and-gene-therapy-report-looks-at-industry-challenges-how-to-expand-nationally]
- 24. Evotec's Off-the-shelf iPSC-based Cell Therapy Expertise [https://www.evotec.com/solutions/next-gen-platforms/ipsc-cell-therapies]
- 25. Allogeneic CAR-engineered cellular therapy for relapsed ... [https://pubmed.ncbi.nlm.nih.gov/40698082/]
- 26. Allogeneic CAR-engineered cellular therapy for relapsed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1585556/full]
- 27. Recent advances in CAR-MSCs: the new engine of cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557984/]
- 28. CAR-T and CAR-NK cell therapies in AML: breaking barriers ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07151-5]
- 29. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 30. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 31. Safety and efficacy of autologous and allogeneic humanized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9944646/]
- 32. Comparison of efficacy and adverse effects of CD19/20 CART ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12089104/]
- 33. Dual-target CAR-T cell therapy: A new strategy to improve ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825002124]
- 34. Allogeneic CART progress: platforms, current progress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198129/]
- 35. Recent updates on allogeneic CAR-T cells in hematological ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-024-03479-y]
- 36. Efficacy and safety of CD22/CD19 dual-targeted CAR T- ... [https://lymphomahub.com/medical-information/efficacy-and-safety-of-cd22cd19-dual-targeted-car-t-cell-therapy-in-b-cell-malignancies]
- 37. Comparison of the safety profiles of CD19-targeting CAR T ... [https://www.sciencedirect.com/science/article/abs/pii/S0006497125014387]
- 38. A novel chimeric antigen receptor T-cell therapy targeting ... [https://www.nature.com/articles/s41375-025-02705-4]
- 39. Editorial: Achilles heel of CAR T-cell therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615502/]
- 40. Advancing CAR T-Cell Therapy in Solid Tumors [https://www.mdpi.com/2072-6694/17/17/2898]
- 41. Allogeneic NKG2D CAR-T Cell Therapy - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467792/]
- 42. Allogeneic CART progress: platforms, current progress and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1557157/full]
- 43. of Genetic for immunotherapy - PMC engineering T cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC8217325/]
- 44. HLA matching or CRISPR editing of HLA class I/II enables ... [https://www.nature.com/articles/s41467-025-64945-3]
- 45. GE: Which Should I Choose, TALEN or CRISPR [https://www.genecopoeia.com/resource/genome-editing-talen-or-crispr/]
- 46. Comparison of the Feasibility, Efficiency, and Safety of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8509008/]
- 47. Understanding TCR T cell knockout behavior using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456732/]
- 48. Current and emerging strategies for the prevention of graft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4151470/]
- 49. Immunocompatibility in transplantation: adapting to a ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1648534/full]
- 50. Incorporation of bacterial immunoevasins to protect cell therapies from... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8636170/]
- 51. Shield CAR T-Cells to Protect from Host Antibody-Mediated Immune ... [https://www.mskcc.org/research-advantage/support/technology/available/shield-car-t-cells-protect-host-antibody-mediated-immune-rejection]
- 52. US6245781B1 - Method for suppressing allogenic immune response... [https://patents.google.com/patent/US6245781B1/en]
- 53. Redefining the Immunobiology of Organ Transplantation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12301649/]
- 54. Type 1 diabetes cured in mice with gentle blood stem-cell and ... [https://med.stanford.edu/news/all-news/2025/11/type-1-diabetes-cure.html]
- 55. Scaling Allogeneic Cell Therapy Manufacturing [https://www.patheon.com/us/en/insights-resources/blog/scaling-allogeneic-cell-therapy-manufacturing.html]
- 56. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 57. Managing the Complexity of the Supply Chain for Cell and ... [https://www.marken.com/managing-the-complexity-of-the-supply-chain-for-cell-and-gene-therapies/]
- 58. Manufacturing innovation to drive down cell therapy costs [https://www.sciencedirect.com/science/article/abs/pii/S0167779923001270]
- 59. Continuous vs. Batch Manufacturing in Pharmaceuticals [https://www.pharmafocusamerica.com/manufacturing/continuous-batch-m00anufacturing]
- 60. The current state and future of T-cell exhaustion research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10352049/]
- 61. Energizing the immune army: T cell exhaustion explained [https://www.pennmedicine.org/news/t-cell-exhaustion-explained]
- 62. Mechanisms of CAR T cell exhaustion and current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9773844/]
- 63. CAR-T cell therapy: current limitations and potential ... [https://www.nature.com/articles/s41408-021-00459-7]
- 64. Mechanisms of T cell exhaustion guiding next generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9388609/]
- 65. Allogeneic versus autologous stem cell transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057802/]
- 66. An in vivo model to study and manipulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2852363/]
- 67. In vivo haemopoietic stem cell gene therapy enabled by ... [https://www.nature.com/articles/s41586-025-09070-3]
- 68. Current strategies for armoring chimeric antigen receptor T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460333/]
- 69. 'Armored' CAR T-Cell Therapy Shows Promise After Prior ... [https://www.aabb.org/news-resources/news/article/2025/05/14/armored--car-t-cell-therapy-shows-promise-after-prior-car-t-cell-therapy-failure]
- 70. Novel pretransplant desensitization strategies in heart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12142529/]
- 71. Saving Time as a Therapist in 2025: Automation and AI [https://www.joinheard.com/articles/saving-time-as-a-therapist-in-2025-automation-and-ai]
- 72. Efficacy and survival outcome of allogeneic stem-cell ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1341631/full]
- 73. Prognostic factors for survival after allogeneic ... [https://www.nature.com/articles/s41409-020-01101-z]
- 74. Comparison of Survival Between Autologous and Allogeneic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7784574/]
- 75. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 76. Cardiac Repair and Clinical Outcomes of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109878/]
- 77. Cardiac Repair and Clinical Outcomes of Stem Cell ... [https://www.mdpi.com/2079-9721/13/5/136]
- 78. a systematic review and meta-analysis of RCTs | Stem Cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04209-5]
- 79. Efficacy of mesenchymal stem cell transplantation on major ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05352-y]
- 80. Impact of mesenchymal stem cell therapy on cardiac function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322349/]
- 81. Challenges in allogeneic mesenchymal stem cell-mediated ... [https://pubmed.ncbi.nlm.nih.gov/22433652/]
- 82. Prognostic Factors and Nomogram for Choroid Plexus Tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC10854689/]
- 83. An overview of the European standard clinical practice ... [https://www.sciencedirect.com/science/article/pii/S2772610X25000133]
- 84. Choroid Plexus Tumors [https://braintumorcenter.ucsf.edu/condition/choroid-plexus-tumors]
- 85. Cellular networks controlling T cell persistence in adoptive cell therapy [https://www.nature.com/articles/s41577-021-00539-6?error=cookies_not_supported&code=3ddff7c8-9a73-4598-aaed-438812a90c41]
- 86. Allogeneic CAR-engineered cellular therapy for relapsed and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279871/]
- 87. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 88. 2025 Biomarkers of Aging Conference [https://www.agingconsortium.org/conference-home]