Cell Death in Culture: Mechanisms, Detection, and Strategies for Bioprocess Optimization
This article provides a comprehensive resource for researchers, scientists, and drug development professionals working with mammalian cell cultures.
Cell Death in Culture: Mechanisms, Detection, and Strategies for Bioprocess Optimization
Abstract
This article provides a comprehensive resource for researchers, scientists, and drug development professionals working with mammalian cell cultures. It explores the fundamental molecular mechanisms of regulated cell death—including apoptosis, autophagy, and necroptosis—and their critical impact on biopharmaceutical production and research outcomes. The scope extends from foundational knowledge to advanced methodological applications, detailing current and emerging biomarkers and detection techniques such as flow cytometry and ELISA. The content further offers practical troubleshooting and optimization strategies to inhibit cell death in bioreactors, such as genetic engineering with anti-apoptotic genes and media supplementation. Finally, it addresses the validation and comparative analysis of cell death modalities, synthesizing key takeaways and future directions for improving yield in bioprocessing and therapeutic development.
Understanding Cell Death: Fundamental Mechanisms and Morphological Hallmarks
Foundational Concepts: What is Regulated Cell Death?
What is the fundamental difference between Accidental Cell Death (ACD) and Regulated Cell Death (RCD)?
ACD is an uncontrollable, instantaneous process caused by extreme physical, chemical, or mechanical insults, such as ischemia or freeze-thaw cycles, leading to uncontrolled cell destruction [1]. In contrast, RCD is a finely tuned process activated by specific signal transduction pathways and is controllable by genetic or pharmacological intervention [2] [1]. This controllability makes RCD a key target for therapeutic development.
How does Programmed Cell Death (PCD) relate to RCD?
PCD is a subtype of RCD that occurs during embryonic development and tissue homeostasis, a physiological form of death not directly linked to external disturbances [1]. RCD is a broader term that also includes pathways activated in response to stress or perturbations of the cellular environment, such as during infection or toxin exposure [2] [1].
What are the key morphological features distinguishing different RCD pathways?
The table below summarizes the core characteristics of the most well-studied RCD pathways.
| RCD Pathway | Morphological Hallmarks | Core Mediators/Executioners | Immunological Profile |
|---|---|---|---|
| Apoptosis [2] [3] | Cell shrinkage, chromatin condensation, nuclear fragmentation, membrane blebbing, formation of apoptotic bodies [4]. | Caspase-3, -7 (executioners); Caspase-8, -9 (initiators); BCL-2 family proteins [2] [3]. | Immunologically silent; no inflammation [2] [4]. |
| Pyroptosis [2] [4] | Rapid plasma membrane rupture, cytoplasmic swelling, release of proinflammatory intracellular contents [4]. | Gasdermin D (GSDMD) pore formation; Caspase-1, -4, -5, -11 [2]. | Inflammatory; releases potent inflammatory mediators [2]. |
| Necroptosis [2] [4] | Cytoplasmic swelling (oncosis), organelle dilation, plasma membrane rupture [4]. | RIPK1, RIPK3, MLKL pore formation [2] [4]. | Inflammatory; releases alarmins and other proinflammatory signals [4]. |
| Ferroptosis [2] | Accompanied by iron accumulation and lipid peroxidation [2]. | Molecular executioners not fully defined; characterized by iron-dependent phospholipid peroxide accumulation [2] [5]. | Inflammatory [2]. |
What is PANoptosis?
PANoptosis is a unified, multifaceted cell death pathway that integrates components from pyroptosis, apoptosis, and necroptosis [2]. It is characterized by the simultaneous activation of biochemical markers from these three pathways in response to specific triggers, such as viral or bacterial infection [2]. The combined loss of key regulators from all three pathways is required to prevent this cell death, which is not achievable by targeting any single pathway alone [2].
Detection and Methodologies
What are the primary assays for detecting apoptosis in my cell cultures?
Apoptosis detection requires multiple assays to capture its multi-stage complexity [3]. The table below organizes key methodologies based on their detection target.
| Detection Target | Assay/Method | Key Reagents & Kits | Technical Insight |
|---|---|---|---|
| Membrane Changes (Early Apoptosis) | Annexin V / Propidium Iodide (PI) staining [3]. | Annexin V-FITC Apoptosis Detection Kit (e.g., Thermo Fisher Scientific) [6]. | Distinguishes early apoptotic (Annexin V+/PI-), late apoptotic/necrotic (Annexin V+/PI+) cells [3]. |
| DNA Fragmentation (Late Apoptosis) | TUNEL (Terminal deoxynucleotidyl transferase dUTP nick end labeling) assay [3]. | Commercial TUNEL assay kits. | Labels 3'-OH ends of fragmented DNA; detectable by flow cytometry or microscopy [3]. |
| Caspase Activation | Fluorogenic substrate cleavage or fluorescent inhibitor binding [3]. | Caspase-3, -8, -9 activity assay kits. | Measures activity of initiator and executioner caspases [3]. |
| Mitochondrial Alterations | Mitochondrial membrane potential (ΔΨm) loss [3]. | JC-1, TMRM, TMRE dyes [3]. | Shift in JC-1 fluorescence from red (aggregates) to green (monomers) indicates ΔΨm loss [3]. |
| Cytomorphological Changes | Fluorescence microscopy with DNA-binding dyes [3]. | DAPI, Hoechst stains [3]. | Visualizes chromatin condensation and nuclear fragmentation [3]. |
Could you provide a detailed protocol for flow cytometry-based apoptosis detection using Annexin V/PI?
This protocol is a cornerstone for quantifying cell death in culture.
- 1. Cell Preparation: Harvest adherent cells using a gentle, non-enzymatic dissociation buffer (e.g., EDTA-based) to preserve phosphatidylserine (PS) on the outer leaflet. Wash cells once with cold PBS.
- 2. Staining: Resuspend ~1x10^5 cells in 100 µL of 1X Annexin V Binding Buffer. Add Annexin V-fluorochrome conjugate (e.g., FITC) and incubate for 15 minutes at room temperature (25°C) in the dark [3].
- 3. Propidium Iodide Addition: Add PI to the staining mixture immediately before analysis. Note: Some protocols recommend adding PI simultaneously with Annexin V.
- 4. Flow Cytometry Analysis: Analyze cells on a flow cytometer within 1 hour. Use appropriate lasers and filters for your chosen fluorochromes.
- Data Interpretation:
- Annexin V-/PI-: Viable, healthy cells.
- Annexin V+/PI-: Early apoptotic cells.
- Annexin V+/PI+: Late apoptotic or necrotic cells.
Troubleshooting Common Experimental Issues
My primary cells are dying unexpectedly in culture. What are the common culprits?
Unexpected cell death is often linked to culture technique, incubation conditions, and media [7].
- Technique: Uneven handling, insufficient mixing of the cell inoculum, or excessive pipetting can create foam or bubbles that hinder cell attachment and growth [7]. Static electricity in low-humidity environments can also disrupt cell attachment to plastic vessels [7].
- Incubation: Repeatedly opening the incubator causes temperature fluctuations and evaporation, which severely affect growth rate and viability [7]. Ensure water reservoirs are full to maintain humidity. Vibration from loose incubator fans or external sources can cause unusual, concentric cell growth patterns [7].
- Media: Media defects are not always visible. Test by comparing your current media with a batch from a different manufacturer. Issues can arise from insufficient reagent quality, incorrect pH buffering, or inadequate filtration [7].
My apoptosis assay shows high background necrosis. How can I mitigate this?
High necrosis often indicates excessive cellular stress during the experiment.
- Optimize Handling: Use gentle cell harvesting techniques. Avoid trypsinization for extended periods; use enzyme-free cell dissociation buffers instead.
- Confirm Treatment Specificity: Ensure your death-inducing agent is not causing overwhelming, nonspecific toxicity. Perform a dose-response curve to find a concentration that reliably induces regulated death without causing accidental lysis.
- Timing is Critical: Analyze your cells at the appropriate time point after inducing death. If you wait too long, apoptotic cells will undergo secondary necrosis, confounding your results [4].
I am detecting markers for multiple RCD pathways. Is this possible?
Yes. Mounting genetic and biochemical evidence shows remarkable flexibility and crosstalk among RCD pathways [2]. This interconnectedness is the basis for the concept of PANoptosis [2]. For example, Caspase-8 is a crucial molecular switch that can promote apoptosis or, when its activity is inhibited, shift the cell toward necroptosis [4]. Detecting overlapping markers suggests a complex, integrated cell death response, which may be the intended physiological outcome in response to specific triggers like viral infection [2].
Core Signaling Pathways in Regulated Cell Death
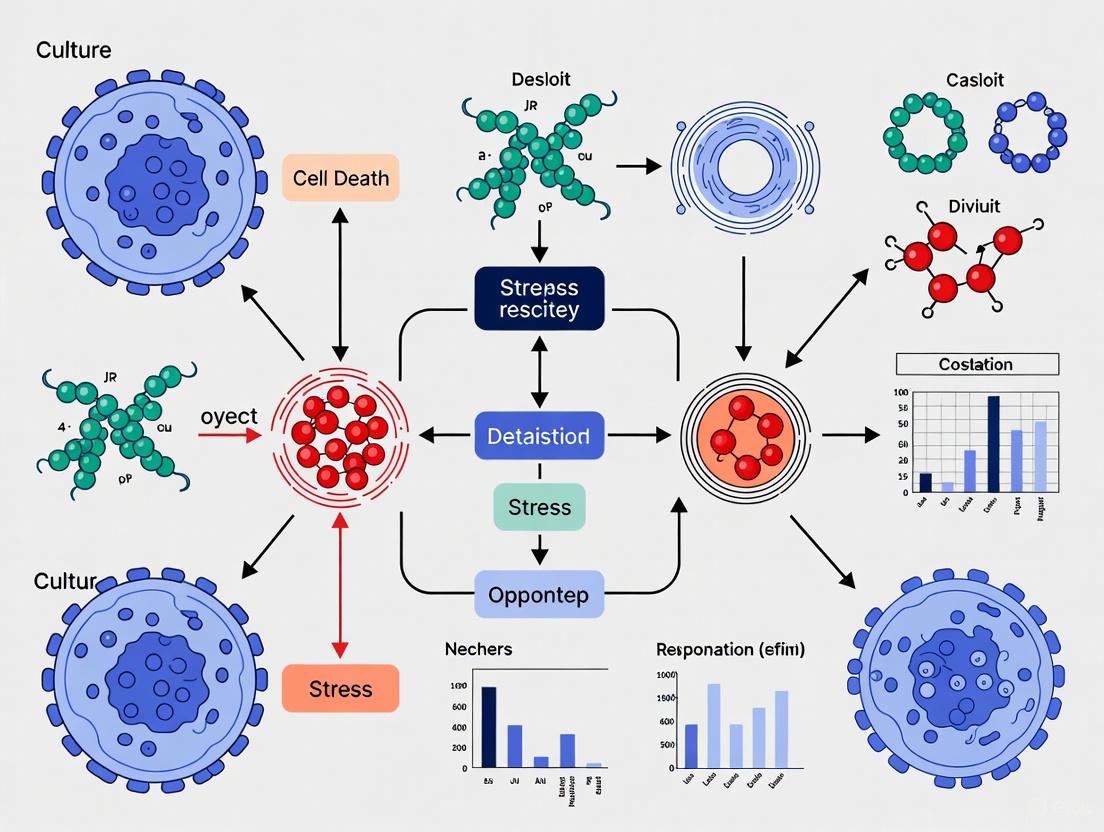
The following diagrams illustrate the core molecular machinery of key RCD pathways, highlighting potential points of crosstalk.
Apoptosis Signaling Pathways
PANoptosis: An Integrated Cell Death Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential reagents and kits for studying RCD, a market projected to grow significantly in North America [6].
| Research Tool | Primary Function | Example Application |
|---|---|---|
| Annexin V Assay Kits | Detects phosphatidylserine externalization on the outer leaflet of the cell membrane [3]. | Flow cytometric or microscopic identification of early apoptotic cells [6] [3]. |
| Caspase Activity Assays | Fluorogenic or luminescent measurement of caspase enzyme activity [3]. | Determining the specific initiator or executioner caspase involved in a death pathway [3]. |
| TUNEL Assay Kits | Labels fragmented DNA in late-stage apoptotic cells [3]. | Histological or flow cytometric detection of apoptosis in fixed cells or tissue sections [3]. |
| Anti-Cleaved Caspase-3 Antibodies | Detects the activated (cleaved) form of the key executioner caspase [3]. | Western blot or immunofluorescence confirmation of apoptotic commitment [3]. |
| Gasdermin D Antibodies | Detects full-length and cleaved (active) forms of GSDMD [2]. | Western blot confirmation of pyroptosis induction. |
| Phospho-MLKL Antibodies | Detects the phosphorylated, active form of MLKL [2] [4]. | Immunofluorescence or Western blot confirmation of necroptotic signaling. |
| Ferroptosis Inducers/Inhibitors | Compounds like Erastin (inducer) or Ferrostatin-1 (inhibitor) to modulate the pathway [2]. | Investigating the role of ferroptosis in a specific disease model or treatment context. |
Core Concepts: The Two Main Pathways to Apoptosis
What are the intrinsic and extrinsic pathways of apoptosis?
Apoptosis, or programmed cell death, is triggered through two primary signaling cascades: the intrinsic and extrinsic pathways. Both pathways are crucial for development, tissue homeostasis, and immune function, and both culminate in the activation of caspases that execute cell death [8] [9].
- Extrinsic Pathway (Death Receptor Pathway): This pathway is initiated outside the cell when extracellular death ligands bind to cell surface death receptors. This binding leads to the formation of a Death-Inducing Signaling Complex (DISC), which activates initiator caspase-8. Caspase-8 can then directly activate executioner caspases (like caspase-3) or amplify the death signal via the intrinsic pathway [8] [10].
- Intrinsic Pathway (Mitochondrial Pathway): This pathway begins from within the cell in response to severe internal stress, such as DNA damage, oxidative stress, or growth factor deprivation. These stresses trigger mitochondrial outer membrane permeabilization (MOMP), leading to the release of cytochrome c and other pro-apoptotic factors. Cytochrome c, together with Apaf-1, forms the apoptosome, which activates initiator caspase-9, subsequently activating executioner caspases [8] [9] [11].
The following table summarizes the key characteristics of these two pathways:
| Feature | Extrinsic Pathway | Intrinsic Pathway |
|---|---|---|
| Initiation | External death ligands (e.g., FasL, TNF-α) bind to death receptors [8] [11] | Internal cellular stress (e.g., DNA damage, hypoxia) [8] [9] |
| Key Initiator Caspase | Caspase-8 [8] [12] | Caspase-9 [8] [12] |
| Key Regulatory Proteins | Death Receptors (Fas, TNFR1), FADD, c-FLIP [8] | Bcl-2 family proteins (Bax, Bak, Bcl-2, Bcl-xL), p53 [8] [9] |
| Central Signaling Complex | Death-Inducing Signaling Complex (DISC) [8] [13] | Apoptosome [8] [11] |
| Mitochondrial Involvement | Can be involved via caspase-8 cleavage of Bid (crosstalk) [8] [10] | Central; defined by MOMP and cytochrome c release [8] [14] |
Troubleshooting Common Experimental Challenges
FAQ 1: My TUNEL assay is positive, but I do not detect other apoptotic markers. Is my cell death truly apoptotic?
A positive TUNEL assay alone is not conclusive evidence of apoptosis. While TUNEL detects DNA fragmentation, a hallmark of late apoptosis, this can also occur during necrotic cell death [9]. To confirm apoptosis, you should use a multi-parameter approach:
- Combine with Morphological Analysis: Apoptotic cells display characteristic morphology—cell shrinkage, chromatin condensation, and formation of small, round apoptotic bodies. Necrotic cells, in contrast, show cell and organelle swelling and membrane rupture [11].
- Measure Additional Apoptotic Markers:
- Caspase Activation: Detect cleaved, active forms of executioner caspases (e.g., caspase-3) via western blot or flow cytometry using activation-specific antibodies [9].
- Phosphatidylserine Exposure: Use Annexin V staining in combination with a viability dye (e.g., Propidium Iodide) to distinguish early apoptotic (Annexin V+/PI-) from late apoptotic/necrotic (Annexin V+/PI+) cells [9].
- Mitochondrial Membrane Potential (ΔΨm): Use dyes like TMRE to detect the loss of ΔΨm, an early event in the intrinsic pathway. Remember that this can also occur in necrosis and requires validation with other markers [9].
FAQ 2: I am not observing caspase activation in my cell death model, despite clear signs of cell demise. What could be happening?
The absence of caspase activation suggests your cells may be undergoing a form of non-apoptotic, programmed cell death. Caspase-independent death is a well-documented phenomenon [13] [12].
- Investigate Alternative Death Pathways:
- Necroptosis: This caspase-independent pathway can be activated by death receptors when caspase-8 is inhibited. Key markers include phosphorylation of RIPK1, RIPK3, and MLKL [13] [12].
- Caspase-Indicated Apoptosis: The intrinsic pathway can sometimes release factors like Apoptosis-Inducing Factor (AIF) and Endonuclease G (EndoG), which can trigger chromatin condensation and DNA fragmentation without caspase activity [8] [11].
- Experimental Validation:
- Use pharmacological inhibitors (e.g., the pan-caspase inhibitor Z-VAD-FMK) to see if cell death is suppressed. If death proceeds unabated, it is likely caspase-independent.
- Employ genetic models, such as cells deficient in key apoptotic components (e.g., Apaf-1⁻/⁻ or Bax⁻/⁻Bak⁻/⁻), where residual death often indicates alternative pathways [13].
FAQ 3: My background cell death is high in my optogenetic apoptosis induction system. How can I reduce it?
High background (light-independent) death is a common challenge in optogenetic systems like OptoBAX, where Cry2/CIB dimerization is used to activate BAX at the mitochondria [14].
- Utilize Improved Constructs: Newer generations of optogenetic switches have been engineered to reduce dark-state interactions. For example, using longer Cry2 variants (e.g., Cry2(1-531)) or incorporating point mutations (e.g., L348F) can significantly decrease background cytotoxicity while maintaining light-dependent efficacy [14].
- Optimize Expression Levels: High levels of pro-apoptotic component expression can lead to spontaneous activation. Titrate your transfection conditions to use the lowest effective concentration of your optogenetic construct.
- Verify Control Conditions: Always include cells expressing the optogenetic construct without light stimulation as a critical control to quantify and account for background death levels [14].
Essential Methodologies for Apoptosis Research
Protocol 1: Differentiating Apoptosis from Necroptosis using Genetic and Pharmacological Inhibitors
This protocol is essential for characterizing cell death pathways when caspase activity is absent [13] [12].
Materials:
- Pan-caspase inhibitor: Z-VAD-FMK
- Necroptosis inhibitor: Necrostatin-1 (Nec-1, targets RIPK1)
- Wild-type (WT) and relevant knockout cells (e.g., RIPK3 KO, Caspase-8 KO)
Method:
- Seed cells in culture plates and pre-treat for 1-2 hours with the following:
- DMSO (vehicle control)
- Z-VAD-FMK (e.g., 20 µM)
- Nec-1 (e.g., 10 µM)
- Z-VAD-FMK + Nec-1
- Apply your death-inducing stimulus.
- After an appropriate incubation period (e.g., 6-24 hours), quantify cell death using a method that distinguishes death mechanisms, such as:
- Flow Cytometry: Annexin V/PI staining to identify apoptotic (Annexin V+/PI-) and necroptotic/necrotic (Annexin V+/PI+) populations.
- Viability Assay: Measure ATP levels or metabolic activity.
- Interpretation:
- Death suppressed by Z-VAD-FMK → Apoptosis.
- Death suppressed by Nec-1 but not Z-VAD-FMK → Necroptosis.
- In genetic models, increased cell survival in RIPK3/Caspase-8 DKO versus single knockouts indicates coordinated roles for both extrinsic apoptosis and necroptosis [13].
Protocol 2: Timelapse Imaging of Early Apoptotic Events using Fluorescent Reporters
This protocol leverages live-cell imaging to establish a kinetic timeline of early apoptosis following a defined trigger, such as optogenetic BAX activation [14].
Materials:
- Cells expressing your apoptosis inducer (e.g., OptoBAX 2.0 system) [14].
- Fluorescent reporters:
- Caspase activity sensor: e.g., a FRET-based reporter or a bright-to-dark GFP mutant containing a caspase-3 cleavage site (DEVD) [15].
- Actin dynamics: LifeAct-GFP or similar.
- Membrane integrity dye: Propidium Iodide (PI).
- Mitochondrial potential dye: TMRE.
Method:
- Plate cells expressing the inducer and relevant reporters in an imaging-appropriate dish.
- Place the dish on a live-cell imaging system with environmental control (37°C, 5% CO₂).
- Acquire baseline images for all channels.
- Initiate apoptosis (e.g., deliver a pulse of blue light for OptoBAX).
- Continuously or intermittently acquire images over several hours.
- Analyze the sequence of events. A typical timeline in HEK293T cells after MOMP might be [14]:
- 0-30 min: Loss of TMRE fluorescence (ΔΨm collapse).
- ~1-2 hours: Caspase-3 reporter cleavage/activation.
- ~2 hours: Actin cytoskeleton redistribution and collapse.
- >2 hours: Plasma membrane permeabilization (PI uptake).
The Scientist's Toolkit: Key Reagents for Apoptosis Research
The following table lists essential reagents for studying apoptosis, along with their primary applications.
| Research Reagent | Function / Application |
|---|---|
| Annexin V Conjugates | Detects phosphatidylserine exposure on the outer leaflet of the plasma membrane, a marker of early apoptosis. Used in flow cytometry and microscopy [9]. |
| Caspase Activity Assays | Measure the activation of initiator and executioner caspases. Includes fluorogenic substrates, antibodies against cleaved caspases (e.g., cleaved caspase-3), and FRET-based live-cell reporters [9] [15]. |
| TUNEL Assay Kits | Labels the 3'-OH ends of fragmented DNA, identifying cells in late-stage apoptosis. Can be used for fluorescence microscopy, IHC, and flow cytometry [9]. |
| BCL-2 Family Antibodies | Detect expression and localization of pro- and anti-apoptotic BCL-2 family proteins (e.g., Bax, Bak, Bim, Bcl-2). Critical for studying the intrinsic pathway [9] [10]. |
| Mitochondrial Dyes (e.g., TMRE, JC-1) | Assess mitochondrial health and function. The loss of fluorescence indicates a collapse in mitochondrial membrane potential (ΔΨm), an early event in intrinsic apoptosis [9]. |
| Death Receptor Ligands (e.g., FasL, TRAIL) | Recombinant proteins used to specifically activate the extrinsic apoptosis pathway by engaging their cognate death receptors on the cell surface [8] [10]. |
| Pharmacological Inhibitors | Tools to dissect death pathways. Z-VAD-FMK (pan-caspase inhibitor), Necrostatin-1 (RIPK1 inhibitor for necroptosis), and BH3 mimetics (e.g., Venetoclax to inhibit Bcl-2) [9] [12]. |
| Optogenetic Systems (e.g., OptoBAX) | Allows precise, light-controlled initiation of apoptosis via specific pathways (e.g., mitochondrial membrane permeabilization), enabling high-resolution kinetic studies [14]. |
For researchers in cell culture and drug development, the classical view of cell death centered on apoptosis has significantly expanded. It is now clear that cells can undergo several other regulated cell death (RCD) pathways, including autophagy, necroptosis, and mitotic catastrophe, each with distinct morphological and biochemical characteristics [16] [17]. Understanding these pathways is crucial for interpreting experimental results, especially in cancer research where therapeutic agents often trigger multiple death mechanisms. This technical support center provides essential troubleshooting guides and FAQs to help you accurately identify, distinguish, and investigate these complex cell death processes in your experimental models.
Defining the Pathways: Morphology and Key Biomarkers
Accurately identifying a specific cell death pathway requires correlating distinct morphological features with definitive biochemical biomarkers. The table below serves as a quick-reference guide for the essential characteristics of each process.
Table 1: Key Characteristics of Non-Apoptotic Cell Death Pathways
| Cell Death Pathway | Morphological Features | Key Biomarkers | Primary Triggers |
|---|---|---|---|
| Autophagy | Extensive cytoplasmic vacuolization, formation of double-membraned autophagosomes, no chromatin condensation early stages [16] [17] | LC3-I to LC3-II conversion, degradation of p62/SQSTM1, increased autophagic flux [18] | Nutrient deprivation, energy depletion, mTOR suppression, rapamycin [19] [17] |
| Necroptosis | Cellular & organellar swelling, plasma membrane rupture, no apoptotic body formation, no chromatin condensation [16] [17] | Phosphorylation of RIP1, RIP3, and MLKL; caspase-independent; inhibited by Necrostatin-1s [18] | Death receptor ligation, caspase inhibition (e.g., zVAD-fmk), TNF-α + BV6 + zVAD [18] |
| Mitotic Catastrophe | Formation of giant cells with multi- and/or micronucleation (>4N DNA content) [18] [20] [21] | Unscheduled activation of cyclin B1-CDK1, caspase-2 activation, mitotic arrest [19] | DNA-damaging agents (doxorubicin), anti-mitotic drugs (microtubule poisons like paclitaxel, colcemid) [22] [23] [21] |
Critical FAQ: The Status of Mitotic Catastrophe
Q: Is mitotic catastrophe a standalone form of regulated cell death?
A: No. According to the Nomenclature Committee on Cell Death (NCCD), mitotic catastrophe is not classified as a separate form of RCD. Instead, it is an oncosuppressive mechanism that serves as a preliminary stage or process that precedes and primes cells for death via other pathways, such as apoptosis, necrosis, or senescence [16] [24]. It is a defensive process that senses mitotic failure and guides the cell toward an irreversible fate.
Pathway Interplay and Experimental Decision Points
A central challenge in cell death research is the extensive crosstalk between pathways. Your experimental conditions, such as genetic background or pharmacological inhibition, can determine the dominant death mechanism.
Key Crosstalk and Switching Mechanisms
- Mitotic Catastrophe as a Decision Platform: When mitotic catastrophe is induced, the cell's fate depends on its molecular profile. The balance between mitochondrial anti-apoptotic proteins (Bcl-xL, Mcl-1) can dictate whether the outcome is apoptosis or autophagy [22]. Furthermore, when apoptosis is suppressed (e.g., with the pan-caspase inhibitor zVAD-fmk), cells with mitotic catastrophe hallmarks can switch to necroptosis [18].
- Autophagy's Dual Role: Autophagy can serve as a pro-survival mechanism, degrading damaged components and promoting recovery. However, it can also contribute to cell death. Inhibiting autophagy in cells undergoing mitotic catastrophe (e.g., with Bafilomycin A1 or ATG13 knockout) can upregulate RIP1 phosphorylation and promote a shift to necroptosis [18].
- The Apoptosis-Necroptosis Switch: The Ripoptosome complex (containing caspase-8, RIP1, and FADD) acts as a key switch. Active caspase-8 promotes apoptosis, but when its activity is inhibited, the balance shifts towards RIP1/RIP3/MLKL-mediated necroptosis [18].
The diagram below illustrates how mitotic catastrophe acts as a central hub, directing cell fate toward apoptosis, autophagy, or necroptosis based on specific experimental and cellular contexts.
Figure 1: Cell Fate Decisions Following Mitotic Catastrophe. Mitotic catastrophe serves as a pre-stage, with final death mode determined by specific inhibitors and protein expressions.
Troubleshooting Guides: Resolving Experimental Ambiguities
Guide 1: Differentiating Apoptosis from Necroptosis
Problem: Cell death is occurring, but classic apoptosis markers are negative, and the morphology appears necrotic.
Investigation Flow:
- Check Caspase Activity: If cleaved caspase-3/8 and PARP are not detected, apoptosis is unlikely.
- Test Inhibitors: Pre-treat cells with Necrostatin-1s (RIP1 inhibitor). If cell death is significantly suppressed, it indicates RIP1-dependent necroptosis.
- Confirm with Phospho-MLKL: Use immunofluorescence or Western blot to detect phosphorylated MLKL, the executioner of necroptosis [18].
- Control Experiment: Use a known necroptosis inducer (e.g., TNF-α + BV6 + zVAD-fmk) as a positive control for phospho-MLKL staining [18].
Guide 2: Determining the Role of Autophagy in Cell Death
Problem: It is unclear whether autophagy is contributing to cell death or acting as a pro-survival mechanism in your model.
Investigation Flow:
- Monitor Autophagic Flux: Do not rely on a single time point. Measure:
- LC3-II accumulation (Western blot) in the presence and absence of lysosomal inhibitors (Bafilomycin A1 or Chloroquine). An increase in LC3-II with inhibition indicates functional flux.
- p62/SQSTM1 degradation: A decrease in p62 levels suggests active autophagic degradation [18].
- Functional Inhibition: Use multiple approaches to inhibit autophagy:
- Assess Cell Viability: If inhibiting autophagy increases cell death, autophagy is likely pro-survival. If inhibiting autophagy decreases cell death, it is likely contributing to the death mechanism itself [18] [20].
The Scientist's Toolkit: Essential Reagents for Cell Death Research
The following table lists key reagents used to study and modulate these cell death pathways, as cited in the literature.
Table 2: Research Reagent Solutions for Cell Death Studies
| Reagent / Tool | Function / Target | Example Application in Research |
|---|---|---|
| zVAD-fmk | Pan-caspase inhibitor | Used to inhibit apoptosis and unmask alternative death pathways like necroptosis following mitotic catastrophe [18]. |
| Necrostatin-1s | RIP1 kinase inhibitor | Specific inhibitor to confirm RIP1-dependent necroptosis; prevents phosphorylation of RIP1 and MLKL [18]. |
| Bafilomycin A1 | V-ATPase inhibitor (blocks autophagy flux) | Inhibits autophagosome-lysosome fusion; used to measure autophagic flux and study autophagy's functional role [18] [20]. |
| 3-Methyladenine (3-MA) | Class III PI3K inhibitor (blocks autophagy initiation) | Inhibits early-stage autophagosome formation [20]. |
| Doxorubicin | DNA-damaging agent | Used at sub-lethal doses (e.g., 600 nM) to induce mitotic catastrophe in various carcinoma cell lines [22] [18]. |
| Colcemid | Microtubule polymerization inhibitor | Anti-mitotic agent used to arrest cells in metaphase and induce mitotic catastrophe [22]. |
| Podophyllotoxin (PPT) | Microtubule-targeting agent | Induces mitotic catastrophe and subsequent apoptosis in cancer cell models [21]. |
| Antibody: Phospho-MLKL | Detects active necroptosis executor | Key biomarker for confirming necroptosis via immunofluorescence or Western blot [18]. |
| Antibody: LC3B | Detects lipidated LC3 (LC3-II) | Standard marker for visualizing autophagosome formation and monitoring autophagy [18]. |
Advanced Considerations: Immunological Consequences
Beyond identifying the death mechanism, understanding its immunological impact is critical for cancer research. The mode of cell death can significantly influence anti-tumor immune responses.
- Mitotic Catastrophe and Immunogenicity: Cells undergoing mitotic catastrophe are characterized by multi/micronucleation. These micronuclei can activate the cGAS-STING pathway, a key sensor of cytosolic DNA that drives type I interferon production and enhances anti-tumor immunity [20]. This links chemotherapy-induced mitotic catastrophe to potentially improved responses to immunotherapy.
- Autophagy as an Immune Rheostat: Autophagy can degrade components of the anticancer immune response. For example, it can selectively degrade MHC-I molecules, thereby reducing antigen presentation and promoting immune evasion. Inhibiting autophagy in this context can enhance immune recognition of tumor cells [20].
The diagram below summarizes how a chemotherapeutic agent inducing mitotic catastrophe can lead to opposing outcomes on cancer immunity, regulated by autophagy.
Figure 2: Autophagy determines the immune outcome of mitotic catastrophe. While mitotic catastrophe can stimulate immunity via cGAS-STING, concomitant autophagy can dampen this response, suggesting a therapeutic benefit for autophagy inhibition in combination therapy.
FAQs: Cell Death Phenotypes in Research
Q1: What are the key morphological features that distinguish different types of regulated cell death?
A1: Different types of regulated cell death (RCD) exhibit distinct morphological characteristics under microscopy. The table below summarizes the hallmarks of major cell death types based on current classifications [25].
Table 1: Morphological Hallmarks of Major Cell Death Types
| Cell Death Type | Key Morphological Features |
|---|---|
| Apoptosis | Cell shrinkage, membrane blebbing, chromatin condensation (pyknosis), nuclear fragmentation (karyorrhexis), formation of apoptotic bodies. |
| Autophagic Cell Death | Appearance of double-membrane autophagic vacuoles in the cytoplasm, degradation of cytoplasmic contents without immediate nuclear collapse. |
| Necroptosis | Cellular and organelle swelling (oncosis), plasma membrane rupture, release of intracellular contents, minimal chromatin condensation. |
| Pyroptosis | Cell swelling, formation of large pores in the plasma membrane, pro-inflammatory release of cytokines. |
| Ferroptosis | Shrunken mitochondria with increased membrane density, loss of mitochondrial cristae, but an absence of classic apoptotic or necrotic nuclear changes. |
Q2: Why might my Cell Painting assay fail to detect specific cell death phenotypes reliably?
A2: This is a common challenge. The timing of phenotype assessment is critical. A 2025 study indicates that shorter incubation periods (e.g., 6 hours for some cell lines) can better capture primary cellular alterations caused by a treatment, providing a more immediate and specific depiction of its action. Longer incubation times (e.g., 48 hours) can lead to an overwhelming of the assay by downstream secondary changes and disintegrated cells, masking the primary phenotype [26]. Furthermore, ensure your staining panel is optimized. For instance, an assay using dyes for actin, mitochondria, Golgi, ER, and nucleus provides compartment-specific information that is crucial for distinguishing death modalities [27].
Q3: How can I determine if a resistant phenotype in my cancer cell line is driven by genetic mutations or non-genetic plasticity?
A3 This requires a multi-faceted approach. The "genes-first" pathway is characterized by the acquisition of specific resistance mutations (e.g., BTK C481S mutations in CLL patients on ibrutinib). To investigate this, use DNA sequencing. In contrast, the "phenotypes-first" pathway involves non-heritable, dynamic transcriptional states and epigenetic reprogramming that allow cells to survive treatment without underlying genetic mutations. To probe this, employ single-cell RNA sequencing to reveal a continuum of transcriptional states, or use functional assays that test for drug sensitivity reversibility upon drug withdrawal [28].
Q4: My single-cell morphology data is inconsistent across experimental batches. How can I improve generalizability?
A4: Generalizability is a significant hurdle in single-cell phenotype prediction. Focus on robust, reproducible feature sets. One analysis found that nuclear AreaShape features (e.g., area, eccentricity, perimeter) were more resilient to dataset-specific biases than intensity-based features when models were applied to new data. Implement a rigorous leave-one-image-out (LOIO) cross-validation strategy to truly stress-test your model's performance on unseen data, as standard train-test splits can give a false sense of accuracy [29].
Troubleshooting Guides
Issue: Weak or Non-Specific Signal in Optical Pooled Screening
Problem: You are conducting a genome-wide morphological screen (e.g., using PERISCOPE or a similar platform) but are getting weak phenotypic signals or cannot confidently assign phenotypes to genetic perturbations [27].
Table 2: Troubleshooting Optical Pooled Screening
| Observed Problem | Potential Cause | Solution |
|---|---|---|
| High background noise in phenotypic images | Non-specific antibody binding or fluorescent dye precipitation. | - Titrate all antibodies and dyes.- Include blocking steps with serum from the secondary antibody host.- Filter sterile fluorescent dyes. |
| Poor correlation between optical and NGS barcode counts | Inefficient in situ sequencing (ISS) or barcode cross-talk. | - Optimize the TCEP destaining step to fully liberate fluorophores before ISS [27].- Validate that the Levenshtein distance between sgRNA barcodes is sufficient for error detection [27]. |
| Inability to detect compartment-specific phenotypes (e.g., mitochondrial defects) | Suboptimal staining or image analysis. | - Use a validated antibody for the compartment (e.g., anti-TOMM20 for mitochondria) [27].- Ensure your image analysis pipeline (e.g., in CellProfiler) is specifically tuned to extract features from the correct subcellular compartments. |
Issue: Differentiating Apoptosis from Other Death Mechanisms
Problem: Your viability assay indicates cell death, but you are unsure if it is apoptosis or another mechanism like ferroptosis or necroptosis.
Solution: Implement a multi-parameter assessment.
- Morphology: Use high-content imaging (as in Table 1) to look for classic features like membrane blebbing (apoptosis) vs. cell swelling (necroptosis) [25].
- Biochemical Probes: Use specific small-molecule inhibitors and activators.
- To rule in/out apoptosis: Use a pan-caspase inhibitor like Z-VAD-FMK. If death is inhibited, it is likely apoptosis.
- To rule in/out necroptosis: Use Necrostatin-1 (Nec-1), an inhibitor of RIPK1 [30].
- To rule in/out ferroptosis: Use Ferrostatin-1 or Liproxstatin-1, which inhibit lipid peroxidation. Conversely, compounds like erastin or RSL3 can be used as specific inducers to see if they replicate the phenotype [30].
- Pathway Analysis: Validate findings by checking for key biochemical events, such as the cleavage of caspase-3 (apoptosis) or the accumulation of lipid peroxides (ferroptosis) [25] [30].
Experimental Protocols
Detailed Protocol: Cell Painting for Cell Death Morphology Profiling
This protocol is adapted from the PERISCOPE pipeline for generating high-dimensional morphological profiles [27].
Principle: Simultaneously label multiple organelles to create a comprehensive morphological fingerprint of the cell, which can be used to classify different death phenotypes.
Reagents:
- Fixative: 4% Formaldehyde in PBS.
- Permeabilization Solution: 0.1% Triton X-100 in PBS.
- Blocking Solution: 1-3% BSA in PBS.
- Staining Panel (destainable, via disulfide linkers recommended):
- Actin: Phalloidin conjugated to a fluorophore (e.g., Alexa Fluor 488).
- Mitochondria: Anti-TOMM20 antibody, followed by a fluorescent secondary.
- Golgi and Plasma Membrane: Wheat Germ Agglutinin (WGA) conjugated to a fluorophore.
- Endoplasmic Reticulum: Concanavalin A (ConA) conjugated to a fluorophore.
- Nucleus: 4',6-Diamidino-2-Phenylindole (DAPI).
- Destaining Solution: Tris(2-carboxyethyl)phosphine (TCEP).
Procedure:
- Cell Culture and Perturbation: Seed cells in an appropriate multi-well plate (e.g., 96-well). Treat with compounds or perform genetic perturbations to induce cell death.
- Fixation: Aspirate media and add 4% formaldehyde for 15-20 minutes at room temperature.
- Permeabilization and Blocking: Wash with PBS, then permeabilize and block with blocking solution containing 0.1% Triton X-100 for 30-60 minutes.
- Staining: Incubate with the pre-mixed staining panel in blocking solution for 1-2 hours at room temperature or overnight at 4°C. Protect from light.
- Imaging: Acquire high-content images using a fluorescent microscope with the appropriate filter sets for each dye.
- Destaining (if performing subsequent ISS): Treat cells with TCEP to cleave the disulfide-linked fluorophores and remove the phenotypic stain [27].
- Image Analysis: Use open-source software like CellProfiler to segment cells and identify subcellular compartments. Then, use Pycytominer to process and normalize the extracted single-cell features for downstream analysis [27] [29].
Protocol: Chemical Biology Screening for Non-Apoptotic Cell Death
This protocol outlines the use of specific chemical tools to discover and characterize non-apoptotic cell death pathways like ferroptosis [30].
Principle: Use selective small-molecule inducers and inhibitors to trigger and probe a specific cell death pathway in an agnostic phenotypic screen.
Reagents:
- Inducers:
- Erastin: Inhibits system xc-, depleting glutathione.
- RSL3, ML162, ML210: Direct inhibitors of GPX4.
- Inhibitors:
- Ferrostatin-1, Liproxstatin-1: Potent inhibitors of ferroptosis that scavenge lipid radicals.
- Deferoxamine (DFO): An iron chelator.
Procedure:
- Phenotypic Screening: Seed cells in 384-well plates. Treat with a library of small molecules alongside known inducers (e.g., Erastin) and controls.
- Viability Readout: After 24-72 hours, measure cell viability using a metabolism-based assay (e.g., ATP content). Crucially, do not use an assay specific only for apoptosis.
- Hit Validation: Re-test hits for dose-dependent lethality.
- Mechanism Elucidation:
- Specificity Test: Co-treat hit compounds with Ferrostatin-1 or Liproxstatin-1. If cell death is rescued, the compound likely induces ferroptosis.
- Biochemical Confirmation: Measure downstream events like glutathione depletion, lipid peroxidation (e.g., with BODIPY 581/591 C11 probe), or GPX4 activity.
- Target Identification: Use techniques like chemoproteomics or chemical genetic analysis to identify the molecular target of the hit compound [30].
Signaling Pathway & Experimental Workflow Diagrams
Core Apoptotic Signaling Pathways
Diagram 1: Core Apoptotic Signaling Pathways.
PERISCOPE Screening Workflow
Diagram 2: Genome-Wide Morphology Screening Workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Cell Death Morphology Research
| Reagent / Tool | Function / Target | Key Application in Cell Death Research |
|---|---|---|
| CRISPR-Cas9 Libraries (e.g., CROP-seq vector) | Targeted gene knockout at scale. | Enables genome-wide screening for genes whose knockout alters cell morphology or induces specific death phenotypes [27]. |
| Cell Painting Panel (Phalloidin, TOMM20, WGA, ConA, DAPI) | Multiplexed staining of actin, mitochondria, Golgi/ membrane, ER, and nucleus. | Generates high-dimensional morphological profiles to classify and distinguish different cell death mechanisms [27] [26]. |
| Chemical Biology Probes (e.g., Erastin, RSL3, Nec-1, Fer-1) | Specific inducers and inhibitors of non-apoptotic death pathways (e.g., ferroptosis, necroptosis). | Used as tool compounds to trigger or inhibit specific death pathways for phenotypic characterization and target validation [30]. |
| CellProfiler | Open-source software for image analysis and feature extraction. | Segments cells and quantifies thousands of morphological features from microscopy images for objective phenotype classification [27] [29]. |
| Pycytominer | Data processing package for morphological profiles. | Normalizes, aggregates, and annotates single-cell data from CellProfiler, preparing it for downstream machine learning analysis [27] [29]. |
Scientific Foundations of Cell Death in Culture
In cell culture research, cell death is not merely an endpoint but a critical, dynamic process that must be carefully monitored and managed. Understanding the different forms of cell death is essential for interpreting experimental results and maintaining the integrity of your research models.
Forms of Cell Death in Experimental Systems
Cell death in culture can be broadly categorized into several distinct forms, each with unique morphological and biochemical characteristics:
Apoptosis: A highly regulated, programmed cell death process characterized by cell shrinkage, chromatin condensation, and formation of apoptotic bodies. It is typically non-inflammatory and crucial for eliminating damaged or unnecessary cells. Key executors are caspases, which are activated through either the extrinsic (death receptor) or intrinsic (mitochondrial) pathways [31] [32].
Necroptosis: A form of programmed necrosis that is inflammatory in nature. It depends on receptor-interacting protein kinases (RIPK1 and RIPK3) and culminates in plasma membrane rupture [33] [34].
Pyroptosis: An inflammatory lytic cell death mediated by gasdermin proteins, which form pores in the plasma membrane. It often occurs in response to pathogenic infections and involves inflammasome activation [33] [34].
Ferroptosis: An iron-dependent form of cell death driven by excessive lipid peroxidation of cell membranes. It is characterized by mitochondrial shrinkage and is regulated by cellular redox balance and iron metabolism [33] [34] [35].
The table below summarizes the key characteristics of these cell death pathways:
| Cell Death Type | Key Regulators/Mediators | Morphological Features | Inflammatory Response | Primary Triggers in Culture |
|---|---|---|---|---|
| Apoptosis | Caspases, BCL-2 family, Cytochrome c [31] | Cell shrinkage, chromatin condensation, apoptotic bodies [31] | No | Serum withdrawal, UV irradiation, DNA damage [31] |
| Necroptosis | RIPK1, RIPK3, MLKL [33] | Cellular swelling, plasma membrane rupture | Yes | TNFα signaling, caspase inhibition [33] |
| Pyroptosis | Gasdermins, Inflammasomes, Caspase-1/4/5 [34] | Pore formation, cell lysis, IL-1β release | Yes | Pathogen-associated molecular patterns (PAMPs) [34] |
| Ferroptosis | Lipid peroxides, Iron, GPX4, FSP1 [33] [35] | Mitochondrial shrinkage, loss of cristae | Variable | Glutathione depletion, GPX4 inhibition, FSP1 inhibition [35] |
The Homeostatic Imperative in Culture Systems
In a healthy organism, approximately one million cells die every second to maintain tissue homeostasis [33]. This delicate balance is replicated in vitro, where the equilibrium between cell proliferation, adaptation, and death determines the health of your culture. Disruption of this balance—through excessive or insufficient cell death—leads to experimental artifacts and unreliable data [33] [31].
Excessive cell death in culture can manifest in inflammatory and degenerative phenotypes, mirroring pathologies such as neurodegenerative diseases. Conversely, insufficient cell death, often resulting from the silencing of pro-death genes or activation of survival pathways, creates models of cancer where cells evade normal turnover mechanisms [33].
Technical Support & Troubleshooting Center
Frequently Asked Questions (FAQs)
Q1: My cultured cells are dying rapidly after passaging. What could be the cause? Rapid cell death post-passaging often results from enzymatic over-digestion during detachment. Over-exposure to trypsin/EDTA degrades cell surface proteins and activates cell death pathways [36] [37]. Solution: Optimize dissociation time and consider milder enzyme mixtures like Accutase for sensitive cells [38]. Always neutralize enzymatic activity promptly with serum-containing medium.
Q2: How can I determine if cell death in my experiment is apoptotic versus necrotic? Use multiparameter assessment combining morphology and specific markers:
- Apoptosis: Look for cell shrinkage, membrane blebbing, and caspase activation (detectable with fluorogenic substrates). Annexin V staining (for phosphatidylserine exposure) combined with a viability dye is a standard assay [31].
- Necrosis/Necroptosis: Characterized by cellular swelling and plasma membrane rupture. Measure release of lactate dehydrogenase (LDH) into the culture medium. Specific necroptosis can be inhibited by necrostatin-1 (RIPK1 inhibitor) [31].
Q3: My cancer cell lines are not responding to pro-apoptotic stimuli. How can I overcome this? Many cancer cells develop resistance to apoptosis by upregulating anti-apoptotic proteins like BCL-2 [31]. Strategy: Consider inducing alternative death pathways. Research shows that triggering ferroptosis using FSP1 inhibitors can effectively eliminate apoptosis-resistant melanoma and lung cancer cells in vivo [35]. This approach exploits the specific metabolic dependencies of cancer cells.
Q4: What are the consequences of using high-passage cell lines? High-passage cell lines undergo phenotypic and genotypic changes (genetic drift), which can alter their response to stimuli. For example, transfection efficiency may increase or decrease, and sensitivity to cell death inducers can shift dramatically [36]. Best Practice: Authenticate cell lines regularly and use low-passage stocks for critical experiments. Maintain detailed records of population doubling levels (PDLs) rather than just passage numbers [36].
Q5: How does serum starvation induce cell death and is it a good model? Serum withdrawal primarily activates the intrinsic (mitochondrial) apoptosis pathway due to deprivation of survival signals. While a common model for stress-induced apoptosis, be aware that the response is cell-type specific and may not fully replicate in vivo death contexts [31].
Advanced Troubleshooting Guide
| Problem | Potential Causes | Recommended Solutions | Cell Death Pathway Involved |
|---|---|---|---|
| Unexpected cell clustering and death in suspension | Release of DNA from dead cells increases medium viscosity; Cell stress [37] | Add low concentrations of DNase I to the medium; Optimize seeding density and agitation | Apoptosis, Secondary Necrosis |
| Poor attachment and anoikis | Inappropriate surface coating; Lack of essential survival signals [38] | Pre-coat with ECM proteins (e.g., collagen, fibronectin); Use conditioned medium or Rho-kinase (ROCK) inhibitor for sensitive cells | Anoikis (a form of apoptosis) |
| Failure to induce ferroptosis despite using known inducers | Redundant antioxidant systems (e.g., FSP1, GSH); Inadequate iron availability [35] | Combine GPX4 inhibition with FSP1 inhibitors; Ensure medium contains transferrin or other iron sources | Ferroptosis |
| Inconsistent death responses in 3D vs 2D culture | Poor penetrance of inducers; Differential microenvironments [38] | Optimize inducer concentration and exposure time; Validate death markers specific to 3D context (e.g., core vs. periphery) | Varies (often Apoptosis) |
| Cell line contamination with mycoplasma | Alters metabolism and sensitizes cells to death; masks genuine experimental effects [38] [37] | Implement routine mycoplasma testing using PCR-based kits; quarantine new cell lines; use antibiotics specifically effective against mycoplasma | Variable (often increases baseline apoptosis) |
Essential Experimental Protocols
Protocol: Assessing Apoptosis via Annexin V/Propidium Iodide Staining
Principle: This flow cytometry-based assay distinguishes live cells (Annexin V-/PI-), early apoptotic cells (Annexin V+/PI-), late apoptotic cells (Annexin V+/PI+), and necrotic cells (Annexin V-/PI+).
Procedure:
- Harvest cells: Gently collect adherent cells using non-enzymatic dissociation buffer to prevent degradation of phosphatidylserine [38].
- Wash: Pellet cells (300 x g for 5 min) and resuspend in cold phosphate-buffered saline (PBS).
- Stain: Resuspend 1x10^5 cells in 100 μL of binding buffer containing Annexin V-fluorochrome conjugate (as per manufacturer's recommendation) and incubate for 15 minutes in the dark at room temperature.
- Add PI: Add propidium iodide (final concentration 1 μg/mL) to the cell suspension immediately before analysis.
- Analyze: Acquire data on a flow cytometer within 1 hour. Use unstained and single-color controls for compensation [31].
Protocol: Inducing and Validating Ferroptosis
Principle: Ferroptosis is triggered by glutathione depletion or direct GPX4 inhibition, leading to accumulation of lipid peroxides.
Procedure:
- Induction:
- Validation:
- Viability Assay: Measure cell viability using a resazurin-based assay.
- Lipid Peroxidation: Detect using C11-BODIPY 581/591 fluorescent probe (5 μM, 30 min incubation) by flow cytometry or fluorescence microscopy.
- Inhibition Test: Confirm ferroptosis specificity by co-treating with 100 nM Ferrostatin-1 (lipophilic antioxidant) or 1 μM Liproxstatin-1 [35].
Signaling Pathway Diagrams
Diagram Title: TNF Signaling to Apoptosis or Necroptosis
Diagram Title: Core Ferroptosis Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Trypsin/EDTA [39] [36] | Proteolytic enzyme mixture for dissociating adherent cells. | Routine passaging of adherent cell lines. |
| Milder Dissociation Agents (Accutase, Accumax) [38] | Enzyme blends less damaging to surface proteins than trypsin. | Passaging sensitive cells; when surface protein integrity is crucial for downstream assays. |
| Annexin V Conjugates [31] | Binds to phosphatidylserine exposed on the outer leaflet of the plasma membrane. | Flow cytometric detection of early apoptosis. |
| Caspase Inhibitors (e.g., Z-VAD-FMK) [31] | Broad-spectrum, cell-permeable irreversible caspase inhibitor. | To confirm caspase-dependent apoptosis or to shift death to necroptosis. |
| Ferroptosis Inhibitors (Ferrostatin-1, Liproxstatin-1) [35] | Potent, specific inhibitors of ferroptosis that reduce lipid peroxidation. | To confirm ferroptotic cell death in experimental settings. |
| FSP1 Inhibitors [35] | Small molecules targeting the ferroptosis suppressor protein 1. | To induce ferroptosis in cancer models, especially those resistant to apoptosis. |
| Gasdermin Inhibitors | Compounds that inhibit gasdermin pore formation. | To specifically inhibit pyroptosis in models of infection or inflammation. |
| ROCK Inhibitor (Y-27632) | Inhibits Rho-associated coiled-coil kinase. | Reduces anoikis in primary cells and stem cells after passaging. |
Detecting Cell Death: A Guide to Biomarkers and Analytical Techniques
FAQs: Biomarkers for Cell Death Detection and Troubleshooting
1. What are the key differences between biomarkers for apoptosis, necrosis, and autophagy?
Biomarkers detect distinct morphological and biochemical events in each cell death pathway. The table below summarizes the primary biomarkers used to differentiate these processes.
Table 1: Key Biomarkers for Major Cell Death Pathways
| Cell Death Pathway | Key Biomarkers | Detection Methods | Key Characteristics |
|---|---|---|---|
| Apoptosis | Activated caspases (e.g., Caspase-3), caspase-cleaved substrates (e.g., CK18), phosphatidylserine externalization, DNA fragmentation [40] [41] | TUNEL assay, Annexin V staining, ELISA (M30), IHC for cleaved caspases [40] | Caspase-dependent, regulated process, no inflammatory response [40] |
| Necrosis/Necroptosis | Release of intracellular contents (e.g., HMGB1), plasma membrane rupture, RIP1/RIP3 kinase activation [41] | Trypan blue uptake, LDH release assay [42] | Accidental or regulated, inflammatory, loss of membrane integrity [42] |
| Autophagy | LC3-I to LC3-II conversion, autophagosome formation, p62 degradation [41] | Western blot (LC3-II/p62), fluorescence microscopy (GFP-LC3) [41] | Formation of double-membrane vesicles, role in cell survival and death [41] |
2. My cell culture is showing high mortality. How can I determine if apoptosis is the primary cause and which biomarker should I use?
First, perform careful microscopic examination for classic morphological features of apoptosis, such as cell shrinkage, membrane blebbing, and the presence of cell "ghosts" or debris [42]. For confirmation, follow these steps:
- Initial, Accessible Assay: Use a trypan blue exclusion assay to quickly assess the percentage of cells with compromised plasma membranes, a late feature of apoptosis [42].
- Specific Apoptosis Detection: To specifically confirm apoptosis, use an Annexin V staining assay, which detects the externalization of phosphatidylserine on the outer leaflet of the plasma membrane, an early apoptotic event. This is often used in conjunction with propidium iodide (PI) to distinguish early apoptotic (Annexin V+/PI-) from late apoptotic or necrotic cells (Annexin V+/PI+) [40].
- For High-Specificity and Quantification: Implement an ELISA-based assay such as the M30 Apoptosense ELISA, which detects a caspase-cleaved neo-epitope of cytokeratin 18 (CK18). This provides a highly specific, quantitative measure of epithelial cell apoptosis in plasma or culture supernatant and can be correlated with tumor burden or treatment response [43].
3. The M30 and M65 ELISAs both measure cytokeratin-18. What is the difference, and when should I use each?
The M30 and M65 assays detect different forms of Cytokeratin-18 (CK18) and provide complementary information on the type and extent of cell death.
- M65 Assay: Measures both intact and caspase-cleaved CK18. It is a biomarker of overall epithelial cell death, capturing death through both caspase-dependent (apoptosis) and caspase-independent pathways [43].
- M30 Assay: Detects only a specific neo-epitope on CK18 exposed after caspase cleavage at amino acids 387-396. It is considered a specific biomarker for epithelial apoptosis [43].
You should use these assays in tandem to gain a deeper understanding of your cell death mechanism. A high M30 value indicates significant apoptosis, while a high M65 value with a low M30 value suggests cell death is occurring primarily through non-apoptotic pathways (e.g., necrosis) [43].
4. What are the most promising emerging biomarkers in cell death research?
The field is rapidly moving beyond traditional markers towards highly sensitive, non-invasive biomarkers that can provide real-time insights.
- Circulating Tumor DNA (ctDNA): Fragments of DNA released by tumor cells into the bloodstream. It shows great promise for early cancer detection and monitoring treatment response through liquid biopsies [44].
- Non-Coding RNAs (ncRNAs): This class includes:
- MicroRNAs (miRNAs): Small RNAs that regulate gene expression post-transcriptionally. Aberrant miRNA expression is linked to tumor progression and treatment response [45].
- Long Non-Coding RNAs (lncRNAs) and Circular RNAs (circRNAs): These can act as "molecular sponges" for miRNAs or interact with proteins to modulate key signaling pathways like apoptosis [40] [45].
- Exosomes: Small extracellular vesicles that carry proteins, lipids, and nucleic acids (including ncRNAs). They are emerging as crucial mediators of intercellular communication in the tumor microenvironment and are a rich source of biomarkers [44].
5. How can machine learning (ML) aid in biomarker discovery for complex diseases like cancer and atherosclerosis?
Machine learning is transformative for analyzing high-dimensional data from omics technologies (e.g., metabolomics, transcriptomics). Key applications include:
- Handling Complex Data: ML algorithms can identify subtle patterns in large, complex datasets where traditional statistics fail, integrating clinical and molecular data for a holistic view [46].
- Feature Selection: ML methods like LASSO regression, Random Forest, and Support Vector Machines (SVM) can identify the most predictive features from thousands of candidates, refining biomarker panels for accuracy and clinical utility [46] [47].
- Improved Diagnostic Models: Studies have demonstrated that ML models can integrate clinical risk factors (e.g., smoking, BMI) with metabolite profiles to predict diseases like large-artery atherosclerosis with high accuracy (AUC > 0.90) [46].
Experimental Protocols
Protocol 1: Detecting Epithelial Cell Death via M30 and M65 ELISAs
This protocol is adapted from research evaluating circulating CK18 as a biomarker of drug-induced apoptosis [43].
1. Sample Collection and Preparation:
- Collect blood samples in heparin-coated tubes.
- Centrifuge samples at 3000 rpm for 10 minutes at 4°C to isolate plasma.
- Aliquot plasma and store immediately at -70°C until analysis.
2. M30 and M65 ELISA Procedure:
- Add 25 µL of each standard, control, or plasma sample to the pre-coated 96-well plate.
- Add 75 µL of horseradish peroxidase (HRP)-conjugated detection antibody to each well.
- Add 4 µL of a heterophilic antibody blocking reagent (e.g., HBR) to prevent false-positive signals.
- Incubate the plate at room temperature for 2 hours (M65 assay) or 4 hours (M30 assay).
- Wash the plate to remove unbound conjugate.
- Add 200 µL of TMB substrate and incubate for 20 minutes in the dark.
- Stop the reaction by adding 50 µL of 1.0 M sulphuric acid.
- Read the absorbance at 540 nm. Calculate the concentration of antigen (U/L) based on the standard curve. Values below 20 U/L are typically considered at the limit of detection.
Protocol 2: Profiling Non-Coding RNA Expression via RNA Sequencing
This outline describes a standard workflow for investigating ncRNAs as biomarkers [45].
1. RNA Extraction and Quality Control:
- Extract total RNA from cells, tissue, or biofluids (e.g., plasma) using a method that preserves small RNAs.
- Assess RNA integrity and concentration using an instrument like a Bioanalyzer.
2. Library Preparation and Sequencing:
- For miRNA sequencing, use a protocol that includes size selection to enrich for small RNAs.
- For lncRNA and circRNA analysis, use ribosomal RNA depletion to remove abundant ribosomal RNAs.
- Prepare sequencing libraries and perform high-throughput sequencing on a platform such as Illumina.
3. Bioinformatic Analysis:
- Align sequencing reads to the reference genome.
- Use specialized tools to quantify expression levels of known miRNAs, lncRNAs, and circRNAs, and to discover novel transcripts.
- Perform differential expression analysis to identify ncRNAs associated with your experimental condition (e.g., treated vs. control).
- Conduct pathway analysis to predict the biological functions and pathways regulated by the differentially expressed ncRNAs.
Key Signaling Pathways
The Intrinsic Apoptosis Pathway and Regulatory Networks
This diagram illustrates the core intrinsic apoptosis pathway and its regulation by Bcl-2 family proteins and non-coding RNAs, a key mechanism often investigated in cell death research.
Experimental Workflow for Biomarker Discovery and Validation
This diagram outlines a modern, integrated workflow for discovering and validating novel cell death biomarkers, incorporating machine learning and multi-modal data.
Research Reagent Solutions
Table 2: Essential Reagents and Kits for Cell Death Biomarker Research
| Reagent/Kits | Primary Function | Example Application |
|---|---|---|
| M30 Apoptosense ELISA | Quantifies caspase-cleaved CK18 (Asp396) | Specific detection of epithelial apoptosis in plasma/supernatant [43] |
| M65 ELISA | Quantifies total CK18 (intact and cleaved) | Measuring overall epithelial cell death [43] |
| Annexin V Staining Kits | Detects phosphatidylserine externalization | Flow cytometry or microscopy to identify early apoptotic cells [40] |
| Absolute IDQ p180 Kit | Targeted metabolomics profiling | Quantifying 194 metabolites from 5 classes for biomarker discovery [46] |
| LC3 Antibody | Detects LC3-I to LC3-II conversion | Western blot or immunofluorescence to monitor autophagy [41] |
| TUNEL Assay Kits | Labels DNA strand breaks | Detecting late-stage apoptosis in fixed cells or tissues [40] |
| Heterophilic Antibody Blocking Reagent (HBR) | Blocks interfering antibodies | Improving specificity in immunoassays like M30/M65 ELISA [43] |
Within the critical field of cell death research, accurately distinguishing between different mechanisms of death, such as apoptosis and necrosis, is paramount. Flow cytometry serves as a powerful tool for this purpose, allowing researchers to quantitatively analyze key biochemical events including DNA fragmentation and loss of membrane integrity. However, the accuracy of this data is highly dependent on optimized protocols and careful troubleshooting. This technical support center addresses common experimental challenges and provides detailed methodologies to ensure the reliability of your flow cytometry data in cell death studies.
Troubleshooting Guides
Common Experimental Issues and Solutions
| Problem | Possible Causes | Recommendations |
|---|---|---|
| Weak or No Signal for DNA Stain | - Incorrect flow rate [48]- Insufficient staining [48]- Inadequate fixation/permeabilization [48] | - Use the lowest flow rate setting [48]- Ensure sufficient incubation time with DNA dye (e.g., PI/RNase for ≥10 min) [48]- Confirm fixation/permeabilization protocol is appropriate for DNA staining (e.g., ice-cold methanol) [48] |
| High Background in Membrane Integrity Staining | - Presence of dead cells [48] [49]- Non-specific antibody binding [48] [49]- Insufficient washing [48] | - Use a viability dye to gate out dead cells during live cell surface staining [48]- Block cells with BSA or Fc receptor blocking reagents prior to staining [48] [49]- Increase the number of washes after antibody incubation steps [48] [49] |
| Poor Resolution of Cell Cycle Phases | - High flow rate [48]- Insufficient cell number or dye concentration [50]- Presence of cellular aggregates [50] | - Run samples at the lowest flow rate setting [48]- Optimize cell number and dye concentration; ensure incubation time and temperature are correct [50]- Use doublet discrimination gates in analysis to exclude aggregates [50] |
| Abnormal Scatter Profile | - Clogged flow cell [48]- Cell sample is lysed or contains debris [49]- Bacterial contamination [50] | - Unclog the instrument per manufacturer's instructions (e.g., run 10% bleach followed by dH₂O) [48]- Ensure gentle sample preparation; avoid high-speed centrifugation/vortexing; filter cells to remove debris [49]- Check sample for contamination [50] |
| Excessive Fluorescence Signal | - Antibody concentration too high [49]- Insufficient blocking [49]- Fluorophore too bright for antigen density [49] | - Titrate the antibody to find the optimal concentration [49]- Increase concentration of blocking agent and/or blocking incubation time [49]- Pair a dim fluorochrome (e.g., FITC) with a high-density target [48] |
Frequently Asked Questions (FAQs)
General Experimental Setup
Q1: What are the essential controls for a flow cytometry experiment analyzing cell death? For reliable data, include the following controls:
- Unstained cells: To assess cellular autofluorescence [48].
- Untreated/Unstimulated cells: To establish a baseline signal.
- Single-stained controls: Critical for compensation when using multiple fluorochromes [50].
- Viability dye control: To properly gate out dead cells and reduce background [48].
- FMO (Fluorescence Minus One) controls: For accurate gating when setting up multicolor panels, as they help distinguish positive from negative populations better than unstained cells alone [50].
Q2: My antibody works in other applications (e.g., immunofluorescence) but not in flow cytometry. What could be wrong? An antibody's performance is application-specific. First, check the manufacturer's data sheet to confirm it is validated for flow cytometry [48]. If it is only approved for immunofluorescence, you may need to perform a titration series to determine the optimal concentration for flow [48]. The experimental conditions, including fixation and permeabilization, can significantly impact antibody binding and require optimization.
Sample Preparation and Staining
Q3: How should I prepare adherent cells for Annexin V staining to avoid artifactual results? Treating adherent cells with trypsin or other detachment reagents can damage the cell membrane and cause false-positive Annexin V staining. After detachment, allow your cells to recover for 30-45 minutes in culture medium in the incubator, gently swirling periodically to prevent re-attachment. After this recovery period, you can proceed with Annexin V labeling and analysis [50].
Q4: Why is it critical to differentiate between assays for "viability," "cell death," and "apoptosis"? These terms represent distinct biological claims and require different experimental evidence [51].
- Viability is a broad term for the number of living cells, often measured by metabolic activity (e.g., MTT, resazurin assays) or total protein content.
- Cell Death specifically requires evidence of dying cells, measured by assays for death-related alterations like loss of membrane integrity (e.g., PI uptake, LDH release).
- Apoptosis is a specific, programmed form of cell death that requires evidence of its characteristic features, such as phosphatidylserine externalization (Annexin V), caspase activation, or DNA fragmentation (TUNEL assay).
Using a single assay, like a tetrazolium reduction test, to support multiple distinct claims is a common misinterpretation that can lead to incorrect conclusions [51].
Instrumentation and Analysis
Q5: I am detecting a very high event rate. What should I check? A high event rate can be caused by several factors [50]:
- An air bubble in the flow cell.
- A sample threshold set too low.
- The photomultiplier tube (PMT) voltage for the threshold parameter being set too high.
- A sample that is too concentrated.
- Bacterial contamination in the sample. Systematically check these parameters, starting with sample concentration and instrument threshold settings.
Experimental Protocols
Protocol 1: Analyzing DNA Fragmentation for Apoptosis
Principle: This protocol detects the internucleosomal cleavage of DNA, a hallmark of apoptosis, by using terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay. The enzyme TdT incorporates fluorescently-labeled dUTP at the free 3'-OH ends of fragmented DNA, which can be quantified by flow cytometry.
Reagents:
- Phosphate-Buffered Saline (PBS)
- Fixative (e.g., 4% methanol-free formaldehyde [48])
- Permeabilization Buffer (e.g., 0.1% Triton X-100 in citrate buffer or ice-cold 70% ethanol [48])
- TUNEL Assay Kit (containing TdT enzyme and fluorescent-dUTP)
- Propidium Iodide/RNase Staining Buffer (optional for cell cycle correlation)
Procedure:
- Prepare Single-Cell Suspension: Harvest and wash cells in PBS. Adjust concentration to 1-5 x 10^6 cells/mL.
- Fix Cells: Fix cells in 4% formaldehyde for 15-30 minutes at room temperature. Critical: Use methanol-free formaldehyde to prevent loss of intracellular proteins and preserve TUNEL reactivity [48].
- Permeabilize Cells: Pellet cells and permeabilize with ice-cold 70% ethanol or 0.1% Triton X-100 for 15-30 minutes on ice. Note: For ethanol permeabilization, chill cells on ice first and add ethanol drop-wise while vortexing to prevent hypotonic shock [48].
- Wash: Wash cells twice with PBS to remove residual fixative and permeabilization buffer.
- Label DNA Strand Breaks: Resuspend the cell pellet in the TUNEL reaction mixture according to the manufacturer's instructions. Incubate for 60 minutes at 37°C in the dark.
- Wash and Analyze: Wash cells twice with PBS and resuspend in PBS for flow cytometry analysis. If performing dual staining, resuspend in PI/RNase solution and incubate for at least 10 minutes before analysis [48].
- Flow Cytometry: Acquire data using a low flow rate to improve resolution and reduce coefficient of variation (CV) [48].
Protocol 2: Assessing Plasma Membrane Integrity
Principle: This protocol distinguishes between intact and compromised plasma membranes, a key differentiator between early apoptotic (intact membrane) and necrotic (compromised membrane) cells. It utilizes Annexin V, which binds to phosphatidylserine (PS) exposed on the outer leaflet of the membrane in apoptotic cells, and a viability dye like Propidium Iodide (PI) that is excluded by live cells but enters dead cells.
Reagents:
- Annexin V Binding Buffer
- Fluorescently-conjugated Annexin V
- Viability Stain (e.g., Propidium Iodide (PI) or 7-AAD)
- PBS
Procedure:
- Harvest Cells Gently: For adherent cells, use gentle enzymatic (e.g., non-trypsin) or mechanical dissociation to avoid artifactual membrane damage. Allow cells to recover post-detachment for 30-45 minutes [50].
- Wash: Wash cells once with cold PBS.
- Resuspend in Binding Buffer: Resuspend cell pellet (approximately 10^5 - 10^6 cells) in Annexin V Binding Buffer.
- Stain: Add fluorescently-conjugated Annexin V and viability dye (PI/7-AAD) to the cell suspension. Incubate for 15-20 minutes at room temperature in the dark.
- Analyze: Without washing, analyze the cells by flow cytometry within 1 hour. Note: Since Annexin V binding is calcium-dependent, the binding buffer must contain Ca²⁺.
Data Interpretation:
- Annexin V-/ PI-: Viable, healthy cells.
- Annexin V+/ PI-: Early apoptotic cells (PS externalized, membrane intact).
- Annexin V+/ PI+: Late apoptotic or necrotic cells (membrane integrity lost).
The Scientist's Toolkit: Research Reagent Solutions
| Reagent Category | Specific Examples | Function in Cell Death Analysis |
|---|---|---|
| DNA Stains | Propidium Iodide (PI) [48], DAPI [48], DRAQ5 [48] | DNA intercalating dyes used for cell cycle analysis and, when combined with RNase, to distinguish apoptotic sub-G1 peaks. PI is also used as a viability dye to assess membrane integrity. |
| Viability Dyes | 7-AAD [48], Fixable Viability Dyes (e.g., eFluor) [48], LIVE/DEAD Fixable Stains [50] | Used to identify and gate out dead cells from analysis, which is crucial as dead cells can bind antibodies non-specifically and increase background [48]. |
| Apoptosis Markers | Annexin V conjugates [50], Caspase Activity Assays, TUNEL Assay Kits | Annexin V binds to externalized phosphatidylserine, an early marker of apoptosis. Caspase assays detect enzyme activity, and TUNEL kits label fragmented DNA. |
| Fixation & Permeabilization Reagents | Formaldehyde (4%, methanol-free) [48], Methanol (90%, ice-cold) [48], Triton X-100 [48], Saponin [48] | Fixation stabilizes cells and prevents degradation. Permeabilization allows intracellular access for antibodies or DNA dyes. The choice depends on the target antigen and application. |
| Blocking Agents | Bovine Serum Albumin (BSA) [48], Normal Serum [48], Fc Receptor Blocking Reagents [48] [49] | Reduce non-specific antibody binding by blocking reactive sites on cells and Fc receptors, thereby lowering background signal. |
Core Principles and Application to Cell Death Research
The Enzyme-Linked Immunosorbent Assay (ELISA) is a powerful plate-based technique widely used for detecting and quantifying peptides, proteins, antibodies, and hormones within complex biological samples. [52] [53] Its principle relies on immobilizing a target antigen to a solid surface, complexing it with a specific antibody linked to an enzyme, and then measuring the conjugated enzyme's activity via incubation with a substrate to produce a quantifiable product. [52] [53] In the context of cell death research, such as apoptosis, ELISA provides a reliable method to quantify specific circulating biomarkers like activated caspases or other released intracellular proteins. For instance, apoptosis can be monitored by detecting mono- and oligonucleosomes released into the cell culture media using a specialized Cell Death Detection ELISA. [54]
ELISA Formats and Their Utility in Biomarker Detection
Several ELISA formats can be employed based on the research goal, each with distinct advantages for detecting cell death biomarkers:
- Sandwich ELISA: This method is highly specific and ideal for quantifying biomarkers like cytokines or activated caspases in complex samples such as cell culture supernatants or patient serum. It uses two antibodies specific to different epitopes on the target antigen, enhancing specificity and sensitivity without requiring sample purification. [52]
- Competitive ELISA: Often used to measure small molecules or antibodies, this format is based on the competition between a sample antigen and an enzyme-labeled antigen for a limited number of antibody-binding sites. [52] [53]
- Direct ELISA: A simpler, faster format where the antigen is directly immobilized and detected by an enzyme-labeled primary antibody. [52]
- Indirect ELISA: Similar to direct ELISA but uses an unlabeled primary antibody followed by an enzyme-labeled secondary antibody, offering signal amplification. [52]
Troubleshooting Guide: Common ELISA Challenges and Solutions
Researchers often encounter specific issues during ELISA experiments. The following tables outline common problems, their potential causes, and recommended solutions.
Table 1: Troubleshooting Signal and Background Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Weak or No Signal [55] [56] | Reagents not at room temperature | Allow all reagents to sit for 15-20 minutes before starting the assay. [55] |
| Incorrect reagent storage or expired reagents | Double-check storage conditions (typically 2-8°C) and confirm all reagents are within their expiration dates. [55] | |
| Insufficient or improper antibody binding | Ensure you are using an ELISA plate (not a tissue culture plate) and confirm correct antibody concentrations and incubation times. [55] [56] | |
| Plate read at incorrect wavelength | Verify the recommended wavelength for the substrate being used (commonly 450 nm) and set the plate reader accurately. [55] | |
| Wells scratched during pipetting or washing | Use caution when dispensing and aspirating; calibrate automated washers so tips don't touch the well bottom. [55] | |
| High Background [55] [56] | Insufficient washing | Follow appropriate washing procedures, including soak steps. Invert the plate on absorbent tissue and tap forcefully to remove residual fluid. [55] |
| Substrate exposed to light | Store substrate in the dark and limit exposure to light during the assay. [55] | |
| Contaminated buffers | Prepare fresh buffers. [56] | |
| Plate sealers reused | Use a fresh plate sealer for each incubation step to prevent cross-contamination. [55] | |
| Too Much Signal [55] [56] | Insufficient washing | Ensure thorough washing to remove unbound enzyme conjugate. [55] [56] |
| Incubation times longer than recommended | Adhere strictly to the protocol's specified incubation times. [55] | |
| Too much detection reagent | Check the dilution of enzyme-conjugated antibodies (e.g., streptavidin-HRP) and titrate if necessary. [56] |
Table 2: Troubleshooting Data Quality and Reproducibility
| Problem | Possible Cause | Solution |
|---|---|---|
| Poor Replicate Data (Poor Duplicates) [55] [56] | Insufficient or uneven washing | Ensure consistent and thorough washing across all wells. If using an automatic washer, check that all ports are clean and unobstructed. [56] |
| Inconsistent pipetting | Check pipetting technique and calibrate pipettes regularly. [55] | |
| Plate sealers not used or reused | Always use a fresh plate sealer during incubations to prevent well-to-well contamination and evaporation. [55] [56] | |
| Poor Standard Curve [55] [56] | Incorrect serial dilution preparation | Double-check pipetting technique and calculations when preparing standard dilutions. [55] [56] |
| Capture antibody did not bind properly to the plate | Use high-affinity antibodies and ensure correct coating buffer and incubation conditions. [55] | |
| Inconsistent Results Assay-to-Assay [55] [56] | Variations in incubation temperature or time | Adhere to recommended incubation temperatures and be aware of environmental fluctuations. Use a calibrated incubator. [55] |
| Improper calculation of standard curve dilutions | Check calculations and use internal controls to normalize data between assays. [55] [56] | |
| Lot-to-lot reagent variability | Re-qualify critical reagents with each new lot to ensure consistent performance. [57] | |
| Edge Effects [55] [56] | Uneven temperature across the plate | Avoid stacking plates during incubation. Ensure the plate is sealed completely and incubated in the center of the incubator. [55] |
| Evaporation | Seal the plate completely with a plate sealer during all incubations. [55] |
Experimental Protocol: Measuring Apoptosis via Nucleosome Detection
This protocol is adapted from a cited study detecting cell death in culture. [54]
Materials and Equipment
- Cell Culture: Appropriate cell line, complete RPMI 1640 media, 24-well cell culture plates.
- Cell Death Detection ELISA Kit: e.g., Cat# 11544675001 from Roche.
- Equipment: Microplate reader capable of 405 nm absorbance, multichannel and single-channel pipettes, microplate washer, incubator, centrifuge. [54] [58]
Workflow Diagram: Cell Death ELISA
Step-by-Step Procedure
- Cell Plating: Plate cells at a density of 25,000 cells per well in a 24-well plate using complete RPMI 1640 media without selection agents. [54]
- Treatment: Apply the experimental treatment to the cells 24 hours after plating. Include appropriate controls (e.g., untreated, positive apoptosis control). [54]
- Incubation: Incubate cells for the desired treatment duration to induce apoptosis.
- Sample Collection: Collect the cell culture media from each well. Centrifuge to remove any floating cells or debris. The supernatant contains the mono- and oligonucleosomes released from apoptotic cells. [54]
- ELISA Procedure: Detect the nucleosomes in the media using the Cell Death Detection ELISA kit, strictly following the manufacturer's instructions. [54] This typically involves:
- Incubating samples in antibody-coated wells.
- Washing to remove unbound material.
- Adding a detection antibody.
- Adding substrate solution to develop color.
- Signal Measurement: Measure the absorbance of each well at 405 nm using a microplate reader. [54]
- Cell Growth Assay: Perform a parallel cell growth assay (e.g., MTT, cell counting) on the treated cells in the wells to determine viable cell count. [54]
- Data Normalization: Normalize the apoptosis absorbance values from the ELISA to the cell count from the growth assay. This controls for variations in cell number and provides a more accurate measure of the rate of apoptosis. [54] All conditions should be performed in technical triplicate, and the experiment should be repeated at least twice for statistical power. [54]
Research Reagent Solutions for Cell Death Biomarker ELISA
Table 3: Essential Materials and Their Functions
| Reagent / Equipment | Function in ELISA |
|---|---|
| ELISA Microplate [52] [58] | Solid phase that passively binds and immobilizes antibodies or proteins. Specialized high-binding plates (e.g., Nunc MaxiSorp) are used for optimal coating. [52] [58] |
| Capture & Detection Antibodies [52] [57] | Key reagents for specific antigen recognition. Matched antibody pairs are essential for Sandwich ELISA to ensure high specificity and sensitivity. [52] [57] |
| Enzyme-Conjugated Secondary Antibody [52] [53] | For indirect or sandwich detection, this antibody binds the primary antibody and carries the enzyme (e.g., HRP) for signal generation. [52] [53] |
| Enzyme Substrate (e.g., TMB) [52] [53] | Reacts with the enzyme (e.g., HRP) to produce a measurable colored product. The reaction is stopped with an acid, changing the color for measurement. [52] [53] |
| Plate Reader (Spectrophotometer) [53] [58] | Measures the intensity of the color developed in each well, typically at 450 nm for TMB, to quantify the target analyte. [53] [58] |
| Blocking Buffer (e.g., BSA) [57] | Covers any unsaturated binding sites on the plate well after coating to prevent non-specific binding of antibodies, thereby reducing background noise. [57] |
| Wash Buffer [55] [53] | Used to remove unbound reagents and decrease background between each assay step, critical for a clean signal. [55] [53] |
| Coating Buffer (e.g., PBS) [55] | The buffer used to dilute the capture antibody for immobilization on the plate surface. [55] |
Frequently Asked Questions (FAQs)
Q1: What are the key validation parameters I need to establish for a robust in-house ELISA for caspase activity? A robust ELISA validation should characterize several core parameters: [57]
- Precision and Reproducibility: Assess both intra-assay (same plate) and inter-assay (different days, different operators) precision. A coefficient of variation (CV) of less than 10% is typically acceptable. [57]
- Accuracy and Recovery: Determined through spike-and-recovery experiments, where a known amount of the analyte is added to a sample and the measured value is compared to the expected value. [57]
- Sensitivity (LLOD): The lowest concentration of the analyte that can be reliably distinguished from the background. [57]
- Specificity and Cross-reactivity: Confirm that the assay detects only the target caspase and does not cross-react with other related proteins or matrix components. [57]
- Linearity and Range: The range of analyte concentrations where the assay provides accurate and precise results, demonstrated by a linear standard curve. [57]
- Robustness: The assay's capacity to remain unaffected by small, deliberate variations in method parameters, such as incubation time or temperature. [57]
Q2: My samples are reading above the upper limit of my standard curve. What should I do? This indicates that your samples contain cytokine (or other biomarker) levels above the dynamic range of the assay. [56] The solution is to dilute your samples and re-run the assay. It is recommended to test several dilutions (e.g., 1:2, 1:5, 1:10) to ensure that the measured concentration falls within the linear range of the standard curve. [56]
Q3: How can I minimize variability between replicate wells? Poor duplicates are often caused by insufficient washing, inconsistent pipetting, or contamination. [55] [56] [59] Ensure thorough and consistent washing across all wells. Check pipette calibration and use good pipetting technique. Always use fresh plate sealers to prevent evaporation and well-to-well contamination, and avoid scratching the bottom of the wells with pipette or washer tips. [55] [56]
Q4: What are the most common sources of error in manual ELISA, and how can they be mitigated? Common errors include inaccurate pipetting, inconsistent incubation times, improper reagent mixing, and manual data transcription errors. [59] These can be mitigated by rigorous technique, using calibrated equipment, adhering strictly to timed protocols, and implementing automation where possible for liquid handling, washing, and data capture to improve reproducibility and reduce human error. [59]
Core Principles of Cell Death Detection
The study of programmed cell death is a cornerstone of cell biology, oncology, and drug development research. Accurate detection of apoptosis is crucial for understanding cellular responses to treatment, disease mechanisms, and developmental processes. Two fundamental biochemical hallmarks of apoptosis are DNA fragmentation and the externalization of phosphatidylserine from the inner to the outer leaflet of the plasma membrane. This guide details the core methodologies for detecting these events, with a focus on practical troubleshooting and protocol optimization for researchers.
DNA fragmentation is a late-stage apoptotic event where activated endonucleases, such as CAD (Caspase-Activated DNase), cleave nuclear DNA at internucleosomal linker sites, generating fragments of approximately 180-200 base pairs [60]. This cleavage produces a characteristic "ladder" pattern when separated by agarose gel electrophoresis [60]. The TUNEL assay is the gold-standard method for detecting this DNA fragmentation in situ.
The principle of the TUNEL assay relies on the enzyme Terminal Deoxynucleotidyl Transferase (TdT), which catalyzes the addition of labeled dUTP (e.g., fluorescein-dUTP, BrdUTP, or EdUTP) to the 3'-hydroxyl termini of fragmented DNA [61] [62] [63]. These labels are then detected via fluorescence microscopy, flow cytometry, or colorimetric methods, allowing for the visualization and quantification of apoptotic cells within a sample [62] [63].
Concurrently, the loss of membrane asymmetry and the externalization of phosphatidylserine (PS) is an early apoptotic event. This is most commonly detected using Annexin V, a calcium-dependent phospholipid-binding protein with high affinity for PS [60]. When conjugated to a fluorochrome, Annexin V provides a sensitive means for identifying cells in the early stages of apoptosis, typically used in conjunction with a viability dye like propidium iodide (PI) to distinguish early apoptosis from necrosis.
The following diagram illustrates the relationship between these key apoptotic events and the methodologies used to detect them.
DNA Fragmentation Analysis: Protocols & Troubleshooting
DNA Gel Electrophoresis Protocol
The DNA fragmentation protocol is a semi-quantitative gel-based method to detect the characteristic apoptotic DNA ladder [60].
Stage 1: Harvest and Lyse Cells
- Pellet approximately 1-5 x 10^6 cells.
- Resuspend the cell pellet in 0.5 mL of detergent lysis buffer (e.g., 10 mM Tris pH 7.4, 5 mM EDTA, 0.2% Triton X-100).
- Vortex the mixture and incubate on ice for 30 minutes.
- Centrifuge at 27,000 x g for 30 minutes to separate fragmented DNA (in supernatant) from intact chromatin (pellet) [60].
Stage 2: Precipitate and Purify DNA
- Divide the supernatant into two 250 µL aliquots. Add 50 µL of ice-cold 5 M NaCl to each and vortex.
- Add 600 µL of ethanol and 150 µL of 3 M sodium-acetate (pH 5.2) to precipitate the DNA. Mix by pipetting.
- Incubate at -80°C for 1 hour.
- Centrifuge at 20,000 x g for 20 minutes and carefully discard the supernatant.
- Pool the DNA pellets and re-dissolve them in 400 µL of extraction buffer (10 mM Tris, 5 mM EDTA).
- Add 2 µL of DNase-free RNase (10 mg/mL) and incubate at 37°C for 5 hours.
- Add 25 µL of proteinase K (20 mg/mL) and 40 µL of buffer (100 mM Tris pH 8.0, 100 mM EDTA, 250 mM NaCl). Incubate overnight at 65°C.
- Extract DNA with phenol/chloroform/isoamyl alcohol (25:24:1) and re-precipitate with ethanol [60].
Stage 3: Agarose Gel Electrophoresis
- Air-dry the DNA pellet and resuspend in 20 µL Tris-acetate EDTA (TAE) buffer with 2 µL sample buffer (0.25% bromophenol blue, 30% glycerol).
- Separate the DNA on a 2% agarose gel containing 1 µg/mL ethidium bromide.
- Visualize the DNA ladder pattern under UV transillumination [60].
TUNEL Assay Protocol
The TUNEL assay allows for in situ detection of apoptotic cells. The protocol below highlights a key modification that preserves protein antigenicity for co-staining.
Key Modification for Multiplexing: Traditional TUNEL uses Proteinase K for antigen retrieval, which degrades protein epitopes and hinders subsequent immunofluorescence. Replacing this step with pressure cooker-induced antigen retrieval in TE buffer (pH=9) for 20 minutes preserves and even enhances protein antigenicity, enabling seamless integration with multiplexed immunofluorescence methods like MILAN or CycIF [64] [65].
Core TUNEL Workflow:
- Deparaffinization and Rehydration: For FFPE tissues, immerse slides in xylene (2x 10 min), then a gradient of ethanol (100%, 95%, 70%, 50%) for 5 min each, and finally rehydrate in PBS for 10 minutes [61] [64].
- Antigen Retrieval: Use a pressure cooker with TE buffer (pH=9) for 20 minutes at pressure. Cool slides to 50°C before proceeding [64].
- Permeabilization: Wash slides in permeabilization buffer (e.g., PBS with 0.1% Triton X-100) for 10-15 minutes at room temperature [64].
- TdT Reaction:
- Prepare the TUNEL reaction mastermix on ice. For one slide: 5 µL TdT reaction buffer, 5 µL CoCl₂, 0.5 µL BrdUTP or EdUTP (10 mM), 0.5 µL Terminal Transferase (TdT) enzyme, and 39 µL nuclease-free water [64].
- Apply 50 µL of mastermix to each tissue section, cover with a coverslip to prevent drying, and incubate in a dark, humidified chamber at 37°C for 60-90 minutes [61] [64].
- Detection and Visualization:
- For direct detection: If using fluorescein-dUTP, wash slides and proceed to counterstaining (e.g., with DAPI) and mounting [63].
- For indirect detection: If using BrdUTP or EdUTP, detect the incorporated nucleotide with an appropriate fluorescently-labeled anti-BrdU/anti-EdU antibody or via a click chemistry reaction, respectively [64] [62].
- Microscopy and Analysis: Image slides using a fluorescence microscope. The apoptotic rate is calculated as the percentage of TUNEL-positive cells among the total cell population (e.g., DAPI-positive nuclei) [63].
Troubleshooting DNA Fragmentation Assays
Researchers often encounter specific technical challenges when performing these assays. The table below summarizes common issues, their causes, and solutions.
Table 1: Troubleshooting Guide for DNA Fragmentation Assays
| Problem | Possible Cause | Solution |
|---|---|---|
| Weak or absent DNA ladder on gel [60] | Insufficient cell lysis or poor DNA recovery. | Ensure proper buffer preparation and incubation times; avoid disturbing the loose DNA pellet during ethanol precipitation [60]. |
| Weak or no TUNEL signal [61] [63] [66] | Inactive TdT enzyme, insufficient permeabilization, fluorescence quenching, or over-fixation. | Include a positive control (DNase I-treated sample); validate reagents; optimize Proteinase K concentration (10–20 µg/mL) or permeabilization time; avoid light exposure; use 4% paraformaldehyde for fixation (not alcohols) and control fixation time [61] [63] [66]. |
| High background/ Non-specific staining in TUNEL [61] [63] [66] | Excessive TdT enzyme/dUTP, prolonged reaction time, incomplete washing, tissue autolysis, or random DNA fragmentation from necrosis. | Lower concentrations of TdT and labeled dUTP; shorten reaction time (typically 60 min at 37°C); increase number of PBS washes (e.g., 5 times); minimize tissue processing time; combine with H&E staining to confirm apoptotic morphology [61] [63] [66]. |
| Strong fluorescence background [61] [66] | Inadequate washing, prolonged exposure during imaging, or high autofluorescence. | Increase PBS washes after TUNEL reaction; adjust exposure time using the negative control as a reference; for autofluorescence, use quenching agents or select fluorophores outside the autofluorescence spectrum [61] [66]. |
| Loss of protein antigenicity for co-staining [64] [65] | Use of Proteinase K in TUNEL protocol. | Replace Proteinase K with pressure cooker-induced antigen retrieval in TE buffer (pH=9). This preserves protein epitopes for multiplexed immunofluorescence [64] [65]. |
The Scientist's Toolkit: Research Reagent Solutions
Successful experimentation relies on high-quality reagents. The following table details essential materials for DNA fragmentation detection assays.
Table 2: Key Reagents for DNA Fragmentation Detection
| Reagent | Function | Application Notes |
|---|---|---|
| Terminal Deoxynucleotidyl Transferase (TdT) | Key enzyme that catalyzes the template-independent addition of labeled nucleotides to the 3'-OH ends of fragmented DNA [61] [62]. | Sensitive to inactivation; prepare reaction mix on ice and avoid prolonged storage. The core component of the TUNEL assay [61]. |
| Labeled dUTP (e.g., Fluorescein-dUTP, BrdUTP, EdUTP) | Substrate incorporated into DNA breaks; serves as the detection moiety [61] [62] [63]. | Fluorescein-dUTP allows direct detection; BrdUTP requires an antibody for detection; EdUTP enables highly specific detection via click chemistry, offering flexibility and reduced background [62] [63]. |
| Proteinase K | Proteolytic enzyme that permeabilizes the cell and nuclear membranes by digesting proteins, allowing reagent entry [61]. | Concentration and time must be optimized (e.g., 20 µg/mL for 10-30 min). Over-digestion damages cell morphology and causes false positives. Can be replaced with pressure cooking to preserve antigenicity [61] [64]. |
| Click-iT Chemistry Reagents | A copper-catalyzed azide-alkyne cycloaddition reaction used to detect EdUTP. Offers high specificity and low background [62]. | The "Plus" kits feature optimized copper concentrations to preserve the signal of fluorescent proteins (e.g., GFP) and compatibility with phalloidin staining [62]. |
| DNase I (Recombinant) | Used to intentionally fragment DNA in a positive control sample to validate the TUNEL assay procedure and reagents [61] [64]. | A mandatory control to confirm that a lack of signal is due to biological reasons and not technical failure [61]. |
| Equilibration Buffer (with divalent cations) | Provides optimal reaction conditions for the TdT enzyme. Contains Mg²⁺ (reduces background) and/or Mn²⁺ (enhances staining efficiency) [61]. | A key component of commercial kits that enhances the signal-to-noise ratio of the assay [61]. |
The workflow below compares the pathways of two common TUNEL detection methods, highlighting their key reagents.
FAQs: Resolving Common Experimental Challenges
Q1: Can TUNEL staining be combined with immunofluorescence (IF)? What is the recommended order? Yes, TUNEL can be combined with IF. It is generally recommended to perform the TUNEL assay first, followed by immunofluorescence staining [63]. A critical factor for success is preserving protein antigenicity. Replacing the traditional Proteinase K digestion step with pressure cooker-induced antigen retrieval allows for robust TUNEL signaling while maintaining full protein antigenicity for subsequent antibody-based detection [64] [65].
Q2: My positive control works, but my experimental samples show no TUNEL signal. What should I check? A functional positive control confirms your reagents and protocol are working. The issue likely lies with the samples themselves. Verify the conditions used to induce apoptosis are appropriate and have been correctly applied. Also, confirm that your fixation process is suitable; over-fixation (e.g., >24 hours in formalin) can cause excessive cross-linking, masking DNA breaks and reducing labeling efficiency [63] [66].
Q3: How can I distinguish true apoptotic staining from false positives in my TUNEL assay? False positives can arise from necrosis, tissue autolysis, or over-digestion with Proteinase K [61] [63]. To distinguish apoptosis:
- Morphology is key: Always correlate TUNEL staining with nuclear morphology using a counterstain like DAPI. Look for condensed and fragmented nuclei characteristic of apoptosis.
- Use multiple methods: Combine TUNEL with another apoptotic marker, such as Annexin V for early apoptosis or active caspase staining.
- Optimize protocols: Avoid excessive TdT enzyme concentration or prolonged reaction times, and ensure thorough washing after the assay [61] [63] [66].
Q4: What are the main advantages of the Click-iT TUNEL assay over traditional methods? The Click-iT TUNEL assay, which incorporates an alkyne-modified dUTP (EdUTP) and uses a copper-catalyzed "click" reaction for detection, offers several advantages:
- Higher Specificity: The azide-alkyne reaction partners are virtually absent in biological systems, leading to very low non-specific background staining.
- Greater Sensitivity: This method has been shown to detect a higher percentage of apoptotic cells under identical conditions compared to BrdUTP or fluorescein-dUTP methods [62].
- Flexibility: The same incorporated EdUTP can be detected with a variety of azide-labeled dyes or biotin, allowing for easy multiplexing and adaptation to different detection platforms [62].
Q5: How long can I store stained samples after a TUNEL assay? Fluorescence in stained cell samples is relatively transient, typically lasting for 1–2 days if stored at 4°C in the dark. For long-term preservation, tissue sections stained with chromogenic substrates (e.g., DAB) can be mounted with neutral balsam and stored for extended periods. For fluorescent samples, it is best to image them as soon as possible after completing the protocol [63].
Multiplexed and High-Throughput Approaches for Comprehensive Cell Death Profiling
Within the context of cell culture research, understanding and accurately profiling cell death is paramount. The shift towards multiplexed and high-throughput methodologies allows researchers to investigate complex cell death mechanisms with greater efficiency, scale, and reproducibility. However, these advanced approaches introduce specific technical challenges that can compromise data integrity. This technical support center addresses common issues encountered during experiments, providing targeted troubleshooting guides and detailed protocols to ensure the reliability of your cell death profiling data.
Troubleshooting Guides & FAQs
Fundamental Cell Culture Health
Q: My cell cultures are showing abnormal growth patterns and uneven attachment. What could be the cause? A: Abnormal growth and attachment often stem from technique, incubation, or media issues [7].
- Handling Technique: Insufficient mixing of the cell inoculum can create foam or bubbles, hindering attachment. Static electricity on plastic vessels, especially in low-humidity environments, can also disrupt cell attachment [7].
- Incubation Conditions: Repeated opening of the incubator causes temperature variations. Evaporation can alter growth rates and patterns; ensure water reservoirs are full. Vibration from equipment or foot traffic can cause unusual concentric rings of cell growth [7].
- Culture Media: Media defects are not always visible. Test by comparing your current media with a formulation from another manufacturer. If the problem persists, the issue is likely with your technique or incubation [7].
Q: After passaging my adherent cells for a death assay, my flow cytometry results are inconclusive. Why? A: The cell dissociation method is likely degrading cell surface epitopes. Common agents like trypsin time-dependently cleave cell surface proteins, preventing subsequent antibody binding for detection [38]. Solution: Use milder enzyme mixtures such as Accutase or Accumax, or non-enzymatic cell dissociation buffers containing EDTA to preserve epitopes for flow cytometry analysis [38].
Q: How do I know if my cell line is misidentified or cross-contaminated? A: Cell misidentification is a widespread problem that can invalidate your data. The International Cell Line Authentication Committee (ICLAC) lists over 576 misidentified cell lines [38]. Solution: Regularly authenticate cell lines using methods like STR profiling to ensure you are working with the correct cells [38].
High-Throughput & Multiplexed Experimentation
Q: My high-throughput fluid shear stress (FSS) device does not generate enough shear stress. How can I modify it? A: You can significantly increase the fluid shear stress in a multiplex pipetting device by modifying the tips. Researchers have successfully adapted a VIAFLO96 multichannel pipettor by fitting it with 22-gauge needles. This modification increased the maximum FSS 94-fold, from ~8.79 dyn cm⁻² with an unmodified "long" tip to 290 dyn cm⁻² [67].
Q: What is a key advantage of using a semi-automated system like the VIAFLO96 for mechanotransduction studies? A: It overcomes the throughput limitations of traditional methods like cone-and-plate viscometers or syringe pumps, which are often single-channel and labor-intensive. The VIAFLO96 allows for semi-automated shearing, staining, and processing of cells in a 96-well format, enabling the simultaneous testing of an array of conditions (e.g., different shear durations, multiple cell lines, various drug concentrations) for cell death profiling [67].
Flow Cytometry Detection & Data Quality
Q: My flow cytometry data shows events piling up on the axis edges. What does this indicate? A: This indicates incorrect voltage (gain) settings on the cytometer. If the FSC (Forward Scatter), SSC (Side Scatter), or fluorophore detector voltages are set too low, events will be forced to the bottom or left axes. Conversely, if set too high, a significant population of events may saturate the detector and pile up on the top or right edges. Once data is acquired, these settings cannot be altered; the samples must be re-run with adjusted voltages [68].
Q: How can I identify a compensation error in my multicolor panel? A: After applying compensation, check the negative population on a bivariate plot (dot plot). A healthy, well-compensated plot will show negative events distributed symmetrically around the axis. A "teardrop" shape or asymmetric spreading of the negative population below zero is a classic indicator of a compensation error [68].
Q: I see a pattern of super-bright, anomalous events in my flow data. What are they? A: This is likely caused by antibody aggregates. These can be removed during analysis by gating. To prevent them in future experiments, centrifuge your antibody stocks at 10,000 RPM for 3 minutes before using them to stain cells [68].
Data Analysis and Interpretation
Q: My positive and negative cell populations are too close together after data acquisition. Can I fix this in analysis? A: While you cannot create true positive/negative separation after acquisition, you can use the Transform function in analysis software like FlowJo to change the axis scaling (e.g., to logarithmic or biexponential). This can help visualize and better distinguish dim populations that are compressed near the axis [69].
Q: What does an uneven signal in the "Time" parameter of my flow data mean? A: Gaps or drastic drops in the signal over time suggest problems with the cytometer's fluidics, such as a partial clog. You may be able to salvage the data by manually gating on the portion of the acquisition where the signal was stable. If clogging is a recurring issue, pre-filter your samples before running them [68].
Summarized Quantitative Data
The table below summarizes key quantitative findings from a referenced high-throughput study on fluid shear stress and its synergistic effect on cell death [67].
Table 1: High-Throughput Fluid Shear Stress (FSS) Parameters and Cell Death Enhancement
| Parameter | Value / Range | Experimental Context |
|---|---|---|
| FSS Intensity (max) | 290 dyn cm⁻² | Achieved with VIAFLO96 using custom 22G needles [67]. |
| FSS Intensity (unmodified tip) | 8.79 dyn cm⁻² | Using "long" INTEGRA pipette tip on VIAFLO96 [67]. |
| FSS Fold-Increase | 94-fold | Increase from unmodified tip to needle-modified setup [67]. |
| Shearing Cycles | 500 - 10,000 mixes | Range used for prostate cancer (PCa) cell studies [67]. |
| Experimental Runtime | 20 - 400 minutes | Corresponding to the shearing cycle range [67]. |
| Synergistic Agent | TRAIL Therapeutic | FSS-induced Piezo1 activation enhanced TRAIL-mediated apoptosis [67]. |
Experimental Protocols
Detailed Protocol: High-Throughput Cell Death Profiling Under Fluid Shear Stress
This protocol outlines a method for studying the synergistic effects of physiological fluid shear stress and therapeutic agents on cell death, adapted for a high-throughput workflow [67].
Key Materials:
- Equipment: VIAFLO96 multichannel electronic pipettor (or equivalent), custom-fitted with 22-gauge luer-fit needles.
- Software: VIALINK software for programming the pipettor.
- Cells: Cell line of interest (e.g., prostate cancer PC3 or LNCaP cells).
- Reagents: Cell culture media, apoptosis-inducing ligand (e.g., TRAIL), staining dyes (e.g., for viability and mitochondrial membrane potential), fixation/permeabilization buffers, flow cytometry antibodies.
Workflow Steps:
- Cell Preparation: Seed cells into a 96-well plate at a uniform density and allow them to adhere and grow to the desired confluency.
- Treatment: Add the therapeutic agent of interest (e.g., TRAIL) to the wells.
- Shearing Program Setup: Using the VIALINK software, design a program to expose cells to FSS. The program should consist of repeated mixing cycles (aspirate and dispense). The number of cycles and the flow rate will determine the total FSS exposure dose [67].
- Apply Fluid Shear Stress: Attach the needle-modified pipette head to the VIAFLO96. Execute the shearing program on the 96-well plate.
- Semi-Automated Staining: Develop a multiplex program on the VIAFLO96 to sequentially add live-cell stains, fixation, permeabilization, and intracellular antibody staining buffers to the wells without manual transfer.
- Flow Cytometry Preparation: Use the device to transfer the processed cells to flow cytometry tubes or a suitable plate for analysis.
- Data Acquisition & Analysis: Run samples on a flow cytometer. Analyze data for markers of cell death (e.g., Annexin V, caspase activity), mitochondrial depolarization, and cell surface markers.
Diagram 1: High-throughput cell death profiling workflow.
Signaling Pathway: Synergistic Cell Death Induction
The following diagram illustrates the signaling pathway by which fluid shear stress can synergize with receptor-mediated apoptosis, a key concept in high-throughput cell death profiling [67].
Diagram 2: FSS and TRAIL synergistic cell death pathway.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Multiplexed Cell Death Profiling
| Item / Reagent | Function in Experiment |
|---|---|
| VIAFLO96 System | A multichannel, semi-automated pipettor that forms the core of the high-throughput workflow, allowing for programmable fluid handling and FSS application [67]. |
| 22-Gauge Needles | Custom modification to pipette tips to dramatically increase the maximum fluid shear stress achievable in the system [67]. |
| TRAIL (TNF-α-related apoptosis-inducing ligand) | A therapeutic agent that binds to death receptors DR4/DR5 to induce extrinsic apoptosis; used to study synergistic cell death with mechanical stimulation [67]. |
| Piezo1 Agonist/Antagonist | Pharmacological tools to activate or inhibit the Piezo1 mechanosensitive ion channel, used to validate its role in the cell death pathway [67]. |
| Accutase/Accumax | Milder enzyme-based cell dissociation reagents that help preserve cell surface epitopes for more accurate flow cytometry analysis post-detachment [38]. |
| Flow Cytometry Panel Design Tool (e.g., from Thermo Fisher) | Online tools to assist in selecting compatible fluorophore-antibody conjugates for designing multicolor flow panels [70]. |
| ROCK Inhibitor (Y-27632) | Improves the survival of sensitive cells, such as stem cells or primary cells, after passaging or cryopreservation, reducing stress-induced death in experiments [71]. |
Controlling Cell Fate: Strategies to Inhibit Death and Enhance Culture Viability
This technical support guide addresses the critical triggers of cell death in bioreactor cultures: nutrient depletion, metabolic by-product accumulation, and osmotic stress. Understanding these triggers is fundamental to maintaining cell viability, optimizing productivity, and ensuring the reliability of bioprocesses for drug development. The following FAQs, troubleshooting guides, and experimental protocols provide a structured approach to identifying and mitigating these common issues.
Frequently Asked Questions (FAQs)
1. What are the primary signs that my culture is experiencing nutrient depletion? A sudden slowdown or cessation in growth rate, a drop in the oxygen uptake rate (OUR), or a rapid decline in viability are key indicators. For specific nutrients like glucose or sulfate, direct measurement of their concentration in the spent medium will show depletion. Metabolic flux analysis can also reveal redistributed fluxes, favoring energy formation over growth [72] [73].
2. How does osmotic stress directly lead to cell death? Osmotic stress creates an imbalance between intracellular and external osmotic pressure. This can cause cytoplasmic wall separation and water loss (plasmolysis), disrupting essential metabolic functions. Cells expend significant energy on osmoregulation, increasing maintenance coefficients and diverting resources from growth and productivity, ultimately leading to inactivation or cell death [72] [74].
3. Can metabolic by-products be beneficial? While typically detrimental at high concentrations, some strategies leverage by-products. For instance, in some cell cultures, lactate produced during the growth phase may be consumed during the production phase. However, this requires careful process control to prevent the accumulation from reaching toxic levels [75].
4. My process works at a small scale but fails upon scale-up. Why? Scale-up introduces gradients (e.g., in substrate, pH, dissolved oxygen) due to longer mixing times. Cells circulate through zones of varying nutrient and by-product concentrations, experiencing cyclical stress. Furthermore, key parameters like the power input per unit volume (P/V) and gas-flow rates change nonlinearly with scale, altering the cellular environment [76].
Troubleshooting Guides
Guide 1: Diagnosing Nutrient Depletion and By-product Accumulation
| Symptom | Possible Cause | Investigation Method | Corrective Action |
|---|---|---|---|
| Sudden growth arrest | Depletion of carbon source (e.g., glucose) | Measure residual glucose concentration in spent medium [75]. | Implement a fed-batch or perfusion feeding strategy to maintain low, non-depleting levels [75] [77]. |
| Decline in Oxygen Uptake Rate (OUR) | Depletion of a key nutrient (e.g., cysteine, sulfate) [73]. | Analyze spent medium for amino acids or sulfur sources; perform proteomics for oxidative stress responses [73]. | Supplement with a balanced nutrient feed based on consumption rates [75]. |
| Low product yield despite high cell density | Nutrient depletion or imbalance affecting synthetic pathways. | Use spent medium analysis and Design of Experiments (DoE) to identify depleted micronutrients [75]. | Supplement with a rich nutrient concentrate or tailor feed to include critical components like specific amino acids or lipids [75]. |
| Lactate/Ammonia accumulation | "Overflow metabolism" from excess substrate or imbalance in metabolic pathways. | Monitor metabolite levels offline or use in-line sensors; track the lactate/glucose yield [75]. | Shift to a low-glucose set point; use a feeding strategy based on OUR to control nutrient levels [75]. |
Guide 2: Diagnosing and Mitigating Osmotic Stress
| Symptom | Possible Cause | Investigation Method | Corrective Action |
|---|---|---|---|
| Reduced cell productivity & inactivation | High osmolality from product accumulation or medium design. | Measure medium osmolality; quantify maintenance coefficients (e.g., for substrate, ATP) [72]. | Use osmotic stress priming (OSP)—a stepwise increase in salinity during process startup to enhance microbial acclimation [74]. |
| Poor granulation & biomass washout | High-salinity environment in anaerobic wastewater treatment. | Monitor microbial community structure via DNA sequencing (e.g., loss of non-salt-tolerant bacteria) [74]. | Acclimatize sludge with gradually increasing salinity; consider OSP for more robust, diversified osmoregulation [74]. |
| Cessation of growth despite nutrient availability | Osmotic shock from sudden introduction to high-salt conditions. | Check for cytoplasmic wall separation; analyze for upregulation of compatible solute synthesis genes (e.g., for trehalose, ectoine) [74]. | Pre-adapt cells to moderate salinity or supplement the medium with compatible solutes like betaines [74]. |
Key Experimental Protocols
Protocol 1: Quantifying the Impact of Osmotic Stress
Objective: To quantify the metabolic changes in a microorganism (e.g., Corynebacterium glutamicum) under a saline gradient, focusing on maintenance energy and flux redistribution [72].
Materials:
- Bioreactor: 2-liter Braun Biostat B with 1.5-liter working volume.
- Microorganism: C. glutamicum ATCC 21253.
- Medium: Defined, threonine-growth-limiting medium.
- Saline Feed: Medium supplemented with 1.2 M NaCl.
Methodology:
- Cultivation: Grow the culture in batch mode until it approaches the growth limitation threshold.
- Continuous Culture: Initiate continuous feeding at a fixed dilution rate (e.g., D = 0.09, 0.13, 0.17, or 0.21 h⁻¹).
- Saline Gradient: Once a steady state is reached, impose a linear osmolality gradient from 280 mosmol kg⁻¹ to 1,800 mosmol kg⁻¹ over 36 hours using the saline feed pump, while keeping the dilution rate constant.
- Sampling & Analysis: Periodically sample to determine:
- Macroparameters: Osmolality, dry cell weight, substrate (glucose), and product (lysine) concentrations.
- Metabolic Fluxes: Calculate using stoichiometric models and measured uptake/production rates.
- Maintenance Coefficients: Determine using equation:
q_substrate = μ/Y°_substrate + m_substrate, wherem_substrateis the maintenance coefficient [72].
Protocol 2: Investigating Nutrient Depletion-Triggered OMV Release
Objective: To investigate the mechanism of outer membrane vesicle (OMV) release in Neisseria meningitidis triggered by sulfur source depletion [73].
Materials:
- Bioreactor: Benchtop bioreactor with dissolved oxygen control.
- Bacterial Strain: Neisseria meningitidis.
- Media: Chemically defined medium with either cysteine or sulfate as the sole sulfur source.
Methodology:
- Cultivation: Grow N. meningitidis in a bioreactor with dissolved oxygen controlled at 30% air saturation.
- Depletion: Allow the culture to consume the sole sulfur source (cysteine or sulfate), which will trigger the onset of the stationary phase and OMV release.
- Sampling: Take samples at different time points: during exponential growth (nutrient replete), at the point of depletion, and in the stationary phase.
- Analysis:
- OMV Quantification: Measure OMV concentration in the culture supernatant.
- Proteomics: Analyze the cellular proteome via LC-MS/MS to identify upregulated pathways (e.g., antioxidant activity, phospholipid biosynthesis).
- Biochemical Composition: Analyze the phospholipid content of the harvested OMVs.
| Dilution Rate (h⁻¹) | Osmolality (mosmol kg⁻¹) | Specific Glucose Consumption | ATP Maintenance Coefficient | Phenotypic Observation |
|---|---|---|---|---|
| 0.21 | 280 ➔ 1800 | Increased linearly | Increased 5-fold | Flux redistribution toward energy formation over growth. |
| 0.09 | 280 ➔ 1800 | Increased at a higher rate | Increased 5-fold | Cell metabolism accelerated. |
| Cell Type | Metabolic Characteristic | Relative Flow Rate Need | Key Nutrient Concern |
|---|---|---|---|
| Smooth Muscle Cells (SMCs) | Present in various tissues; responsive to stress. | Moderate | Oxygen and glucose [78]. |
| Chondrocytes | Less metabolic demand; anatomically less proliferative. | Lower | Oxygen and glucose [78]. |
| Hepatocytes | Highly metabolically active; nutrient-sensitive. | Very High | Oxygen consumption is critical [78]. |
Signaling Pathways and Experimental Workflows
Cellular Stress Pathway
Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application |
|---|---|
| Chemically Defined Medium | Provides a consistent, serum-free base for cell culture, allowing precise control over all nutrient components [72] [73]. |
| Stoichiometrically Balanced Nutrient Supplement | A feed solution designed to replace consumed nutrients in the correct ratios, preventing depletion and metabolite accumulation [75]. |
| Acid/Base for pH Control | Used to maintain optimal pH, the consumption rate of which can also serve as a cue for nutrient feeding [75]. |
| Sparger | A bioreactor component that introduces air or oxygen into the culture medium, critical for controlling dissolved oxygen levels [77] [76]. |
| Cell Retention Device (CRD) | A module (e.g., using Tangential Flow Filtration) used in perfusion bioreactors to retain cells while removing spent medium and metabolites [77]. |
| Compatible Solutes (e.g., Ectoine, Betaines) | Molecules accumulated by cells to balance internal and external osmotic pressure without disrupting metabolic function, used to mitigate osmotic stress [74]. |
The B-cell lymphoma 2 (Bcl-2) protein family constitutes critical regulators of apoptosis, with Bcl-2 and Bcl-xL serving as prominent anti-apoptotic members that maintain cellular survival. These proteins function primarily at the mitochondrial outer membrane to prevent the release of cytochrome c, thereby blocking activation of the caspase cascade that executes programmed cell death [79] [80]. The overexpression of these proteins represents a strategic genetic engineering approach to suppress unwanted apoptosis in cell culture systems, particularly in primary cells difficult to maintain long-term, protein production bioreactors, and disease modeling where cell survival enhances experimental outcomes. This technical support center provides comprehensive guidance for researchers implementing these strategies within the broader context of cell death research.
Key Biological Functions and Differences
Mechanism of Action
Bcl-2 and Bcl-xL belong to the multi-domain anti-apoptotic group within the BCL2 protein family, characterized by the presence of four BCL2 homology (BH) domains [79]. Their canonical function involves forming heterodimers with pro-apoptotic proteins like BAX and BAK, preventing mitochondrial outer membrane permeabilization (MOMP) and subsequent cytochrome c release [79] [80]. Both proteins integrate into the outer mitochondrial membrane via a C-terminal transmembrane domain and also localize to the endoplasmic reticulum, where they regulate calcium signaling [79].
Functional Distinctions Between Bcl-2 and Bcl-xL
Despite structural similarities and shared anti-apoptotic functions, Bcl-2 and Bcl-xL exhibit significant qualitative and quantitative differences:
- Potency Variation: Bcl-xL demonstrates approximately ten times greater anti-apoptotic activity than Bcl-2 against specific stimuli like doxorubicin [81].
- Pathway Specificity: Bcl-2 localized to the endoplasmic reticulum inhibits apoptosis induced by ceramide and thapsigargin but not by doxorubicin or TNFα, while Bcl-xL at the same location is active against all four agents [81].
- Dual Cell Cycle Function: Both proteins coordinately regulate apoptosis and cell cycle progression, enhancing G0 arrest and delaying S phase entry [82].
Table 1: Comparative Analysis of Bcl-2 and Bcl-xL Properties
| Property | Bcl-2 | Bcl-xL |
|---|---|---|
| Primary Function | Inhibition of mitochondrial cytochrome c release | Inhibition of mitochondrial cytochrome c release |
| Relative Potency | Baseline | ~10x more potent against doxorubicin [81] |
| ER-localized Activity | Limited pathway inhibition (ceramide, thapsigargin) [81] | Broad pathway inhibition [81] |
| Cell Cycle Effect | Enhances G0 arrest, delays G1-S transition [82] | Enhances G0 arrest, delays G1-S transition [82] |
| Domain Structure | BH4, BH3, BH1, BH2, Transmembrane | BH4, BH3, BH1, BH2, Transmembrane |
| Therapeutic Targeting | Venetoclax (specific inhibitor) [79] | Navitoclax (inhibitor, causes thrombocytopenia) [79] |
Research Reagent Solutions
Table 2: Essential Research Reagents for Bcl-2/Bcl-xL Studies
| Reagent Type | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| cDNA Clones | BCL2 (NM_000633) Human Untagged Clone [83] | Bcl-2 overexpression studies | In pCMV6-XL4 vector, 720 bp ORF, transfection-ready |
| Antibodies | Bcl-xL Antibody #2762 [84] | Western Blot (1:1000), IP (1:50) | Rabbit monoclonal, detects endogenous Bcl-xL (30 kDa) |
| Antibodies | Anti-Bcl-XL antibody [2H12] (ab270253) [85] | WB (1-2 µg/mL), IHC-P | Mouse monoclonal, immunogen within aa 1-50 of human BCL2L1 |
| Chemical Inhibitors | ABT-263 (Navitoclax) [86] | Bcl-2/Bcl-xL inhibition controls | Dual Bcl-2/Bcl-xL inhibitor, used in PROTAC development |
| Chemical Inhibitors | ABT-199 (Venetoclax) [79] | Selective Bcl-2 inhibition | Bcl-2-specific BH3-mimetic, FDA-approved for leukemia |
| PROTAC Degraders | DT2216 [86] | Selective Bcl-xL degradation | VHL-recruiting PROTAC, degrades Bcl-xL but not Bcl-2 |
Experimental Protocols
Protocol: Evaluating Apoptosis Protection via Overexpression
Purpose: To validate the functional consequences of Bcl-2 or Bcl-xL overexpression by measuring resistance to induced apoptosis.
Reagents:
- Expression plasmid for Bcl-2 (e.g., Origene SC125546) or Bcl-xL
- Transfection reagent
- Appropriate cell line (e.g., MCF-7, HEK293, or primary cells)
- Apoptosis inducer (e.g., 1-5 µM Doxorubicin, 70 µM Ceramide, 400 nM Thapsigargin, or TNFα with cycloheximide) [81]
- Annexin V staining kit
- Caspase-3/7 activity assay
- Western blot reagents and antibodies for Bcl-2/Bcl-xL, cleaved caspase-3, and PARP
Procedure:
- Cell Seeding and Transfection: Seed cells in 6-well or 12-well plates and transfect with Bcl-2, Bcl-xL, or empty vector control plasmids using standard protocols.
- Selection and Validation: If using stable expression, apply appropriate selection antibiotics for 1-2 weeks. Validate overexpression via Western blotting 48-72 hours post-transfection using antibodies specific for Bcl-2 or Bcl-xL [84] [85].
- Apoptosis Induction: 24 hours post-transfection (or after stable pool selection), treat cells with the chosen apoptosis-inducing agent for 16-24 hours.
- Functional Assessment:
- Annexin V/PI Staining: Harvest cells, stain with Annexin V and propidium iodide, and analyze by flow cytometry to quantify early and late apoptotic populations.
- Caspase Activity: Measure caspase-3/7 activity using a commercial luminescent or fluorescent assay.
- Western Blot Analysis: Probe for apoptosis markers like cleaved caspase-3 and cleaved PARP.
- Data Analysis: Compare the percentage of apoptotic cells and levels of apoptosis markers between Bcl-2/Bcl-xL overexpressing cells and vector controls.
Protocol: Testing Specific Pathway Protection
Purpose: To determine whether Bcl-2 or Bcl-xL overexpression protects against cell death induced by specific organelle-specific stressors.
Reagents:
- Established cell lines overexpressing Bcl-2 or Bcl-xL (or targeted mutants)
- ER stress inducers: Thapsigargin (SERCA inhibitor, 400 nM), Ceramide (70 µM) [81]
- DNA damage inducers: Doxorubicin (1-5 µM), Etoposide (50-100 µM)
- Mitochondrial stressors: e.g., Staurosporine
- MTT or Cell Titer-Glo viability assay
Procedure:
- Cell Preparation: Seed isogenic cell lines expressing vector control, wild-type Bcl-2, wild-type Bcl-xL, or organelle-targeted mutants at equal densities.
- Treatment: 24 hours after seeding, treat cells with the panel of apoptosis inducers at optimized concentrations.
- Viability Assessment: After 24-48 hours of treatment, measure cell viability using MTT or ATP-based assays.
- Data Interpretation: Compare viability across cell lines and treatments. Bcl-xL typically provides broader protection across all stimuli, while Bcl-2's protection may be more restricted, particularly for ER-targeted mutants [81].
Signaling Pathway Visualization
Diagram 1: Bcl-2/Bcl-xL Apoptosis Inhibition Pathway
Troubleshooting Guide
FAQ 1: My Bcl-2/Bcl-xL overexpressing cells are still undergoing apoptosis at high rates. What could be wrong?
- Verify Protein Expression: Confirm successful overexpression via Western blot. Use validated antibodies like Bcl-xL Antibody #2762 [84] or Anti-Bcl-XL antibody [2H12] [85]. Ensure expression levels are sufficiently high to counteract the apoptotic stimulus.
- Check Apoptosis Pathway Specificity: Remember that Bcl-2 localized to the ER does not inhibit apoptosis induced by all stimuli (e.g., doxorubicin, TNFα) [81]. Ensure your apoptotic stimulus is appropriate. Consider using Bcl-xL for broader protection.
- Confirm Transfection Efficiency: If using transient transfection, assess efficiency via a fluorescent marker. The protective effect will only occur in successfully transfected cells. Consider using stable cell lines for homogeneous expression.
- Test Inhibitor Specificity: If using chemical inducers, verify their mechanism of action. Some stimuli may activate strong extrinsic apoptosis pathways that can bypass mitochondrial regulation.
FAQ 2: How can I determine whether to use Bcl-2 or Bcl-xL for my specific cell type or application?
- Prioritize Bcl-xL for Potency: If maximal anti-apoptotic effect is needed, Bcl-xL is approximately ten times more potent than Bcl-2 against common insults like doxorubicin [81].
- Consider Tissue-Specific Expression: Consult literature for your specific cell type. Some cells endogenously express one protein more highly, and adding the other may provide more significant effects.
- Evaluate Desired Outcome: If studying cell cycle effects, note that both proteins enhance G0 arrest [82]. For ER-stress specific protection, Bcl-xL may be more effective [81].
- Test Both Empirically: For critical applications, create parallel models expressing each protein and compare their performance in your specific apoptosis assays.
FAQ 3: What are the best controls for confirming that apoptosis suppression is specifically due to Bcl-2/Bcl-xL overexpression?
- Pharmacologic Inhibition: Use specific BH3-mimetics like venetoclax (BCL-2 specific) or navitoclax (BCL-2/BCL-xL dual) to reverse the protective effect [79] [86]. Reversal of protection confirms specificity.
- Genetic Controls: Include empty vector controls and/or cells expressing a non-functional mutant (e.g., lacking the transmembrane domain). The Y28F mutant of Bcl-2, previously thought to separate functions, still inhibits apoptosis and delays cell cycle [82].
- Knockdown Rescues: In systems with endogenous expression, use siRNA knockdown to demonstrate increased sensitivity to apoptosis, which can then be rescued by your overexpression construct.
FAQ 4: I notice my overexpressing cells are growing slower. Is this expected?
- Yes, This is Documented: Bcl-2 and Bcl-xL not only inhibit apoptosis but also delay cell cycle progression, particularly the transition from G0 to S phase [82]. This is mediated through regulation of p27 and p130 [82].
- Confirm with Cell Cycle Analysis: Perform flow cytometry with PI staining to confirm the specific cell cycle stage that is prolonged.
- Consider Experimental Implications: This dual function is important to remember in proliferation assays, as reduced cell numbers may reflect both reduced death and reduced division rates.
Advanced Applications
Combination with Other Modalities
The combination of Bcl-2/Bcl-xL overexpression with other genetic engineering strategies can yield synergistic effects. For instance, research in glioblastoma demonstrated that combining miR-34a (which downregulates Bcl-2) with a suicide gene therapy produced enhanced apoptosis and significant tumor growth suppression [87]. Similar combinatorial approaches can be designed where survival signaling is precisely tuned alongside other therapeutic transgenes.
Novel Targeting Technologies
Beyond simple overexpression, novel technologies like Proteolysis Targeting Chimeras (PROTACs) offer sophisticated tools for precision control. PROTACs such as DT2216 can selectively degrade Bcl-xL but not BCL-2, despite the warhead binding both, due to differential lysine accessibility for ubiquitination [86]. These tools can be used as experimental controls or to model the effects of acute protein loss after establishing overexpression.
Media Optimization and Feeding Strategies to Counteract Environmental Stress
Foundational Concepts: Environmental Stress and Cell Death
Environmental stresses in cell culture, such as osmotic pressure, oxidative stress, and suboptimal feeding strategies, can disrupt cellular homeostasis and trigger programmed cell death, ultimately compromising experimental results and bioproduction yields [88] [89]. Media optimization and advanced feeding strategies are therefore critical to maintain cell viability and function.
Key Stressors and Cellular Consequences:
- Oxidative Stress: Caused by an imbalance between reactive oxygen species (ROS) and cellular antioxidants, leading to macromolecular damage [89].
- Osmotic Stress: Results from fluctuations in solute concentration, challenging cells to maintain volume and internal equilibrium [89].
- Nutrient Stress: Occurs from nutrient depletion or byproduct accumulation in suboptimal feeding regimes, triggering energy failure and death pathways [90].
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: My cell cultures are experiencing high rates of cell death. Could environmental stress be a cause, and how can I adjust the media to counter this?
High cell death is a common symptom of environmental stress. A systematic approach to media optimization is recommended.
Initial Diagnosis:
- Check Metabolites: Measure glucose, glutamine, and lactate levels to assess nutrient exhaustion and waste product accumulation.
- Confirm Osmolality: Ensure the osmolality of your media is within the physiological range for your cell type.
- Review Protocol: Document any recent changes to media formulation, feeding schedule, or passaging techniques.
Media Optimization Workflow: The following diagram outlines a generalized iterative process for optimizing culture media to improve cell viability.
Actionable Solutions:
- Switch to Serum-Free Media (SFM): SFM offers a more consistent composition, reduces risk of contamination, and simplifies downstream processing. It can be formulated with specific additives for your cell line [91] [38].
- Add Protective Osmolytes: Supplement media with compatible solutes like glycerol or amino acids (e.g., glycine, proline) to help cells counteract osmotic stress [89].
- Incorporate Antioxidants: Add compounds such as glutathione or N-acetylcysteine to the media to mitigate oxidative damage [89].
FAQ 2: What is the most effective feeding strategy for high-density cell cultures to prevent nutrient stress and cell death?
For high-density cultures, such as those in bioreactors, perfusion feeding strategies often outperform traditional batch feeding.
- Problem: In repeated batch feeding, the culture environment is heterogeneous, with nutrient depletion and metabolic byproduct accumulation occurring between media changes. This "feast-or-famine" cycle induces stress [90].
- Solution: Perfusion Feeding: This strategy involves the continuous addition of fresh media and simultaneous removal of spent media, while cells are retained in the bioreactor.
Protocol: Implementing a Perfusion Process in a Stirred-Tank Bioreactor [90]:
- Bioreactor Setup: Use a single-use, stirred-tank bioreactor equipped with a cell retention device (e.g., a porous filter with 20-40 µm pores).
- Inoculation: Inoculate the bioreactor with a single-cell suspension at a target density (e.g., 5.0 x 10⁵ cells/mL) in media supplemented with a Rho-kinase (ROCK) inhibitor to enhance single-cell survival.
- Process Parameters: Maintain constant temperature (37°C), dissolved oxygen, and pH. Set the agitation speed to 60-70 rpm to keep aggregates in suspension without causing shear stress.
- Initiate Perfusion: After 48 hours, begin continuous media perfusion. A common starting flow rate is 4.2 mL/hour for a 125 mL culture, equating to approximately one volume exchange per day.
- Monitoring: Sample daily to monitor cell density, viability, aggregate size, and key metabolites (glucose, lactate). Adjust the perfusion rate based on cell growth and nutrient consumption.
Expected Outcome: Perfusion leads to a more homogeneous environment, supports higher cell densities (e.g., 2.85 x 10⁶ cells/mL), and can increase final cell yields by over 47% compared to repeated batch culture by reducing environmental stress [90].
FAQ 3: Which algorithmic approach should I use for media optimization, given my limited experimental budget?
The choice of algorithm depends on the number of media components and the experimental budget. The table below compares common approaches.
Table 1: Comparison of Media Optimization Algorithms
| Algorithm Type | Key Principle | Best For | Experimental Iterations Required |
|---|---|---|---|
| One-Factor-at-a-Time (OFAT) [92] | Varying one component while holding others constant. | Simple, quick checks of single components. | Very Low |
| Design of Experiments (DOE) [92] | Statistically designed experiments to screen multiple factors and their interactions. | Efficiently identifying a few critical components from a larger set. | Low to Medium |
| Stochastic Metaheuristics (e.g., Differential Evolution) [92] | Using randomness and population-based search to explore complex solution spaces. | Optimizing complex media with many interacting components. | Medium to High |
For limited budgets, begin with a DOE to identify the most influential media components. Subsequently, a Direct Search algorithm (e.g., Nelder-Mead simplex) can be effective for fine-tuning the concentrations of 5-10 key components, as it typically requires fewer than 10 iterative experimental rounds to find a near-optimal formulation [92].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Stress Mitigation and Media Optimization
| Reagent / Material | Function in Counteracting Environmental Stress |
|---|---|
| Serum-Free Media (SFM) [91] [38] | Provides a defined, consistent environment; eliminates variability and contaminants from animal serum, reducing unspecified stress. |
| Rho-Kinase (ROCK) Inhibitor [90] | Enhances survival of single cells (e.g., in bioreactor inoculation) and dissociated primary cells by suppressing apoptosis. |
| Compatible Osmolytes (e.g., Glycerol) [89] | Accumulates intracellularly to balance external osmotic pressure without disrupting cellular function. |
| Antioxidants (e.g., Glutathione) [89] | Scavenges reactive oxygen species (ROS), protecting cellular components from oxidative damage. |
| Stirred-Tank Bioreactor System [90] | Enables precise control of culture parameters (pH, O₂) and implementation of advanced feeding strategies like perfusion. |
| Cell Retention Device [90] | A filter or settler that allows for continuous media exchange (perfusion) while keeping high-density cells in the culture vessel. |
Visualizing the Cellular Stress Response
Understanding the intracellular signaling pathways activated by environmental stress is key to developing effective countermeasures. The diagram below illustrates a generalized stress response pathway in a eukaryotic cell, integrating mechanisms from yeasts like Debaryomyces hansenii and higher eukaryotes [88] [89].
In the context of cell death research, the processes of cryopreservation, thawing, and seeding are not merely logistical steps but are critical experimental variables that can directly influence cellular stress responses, viability, and the very cell death pathways under investigation. Inconsistent post-thaw recovery can introduce significant confounding variables, skewing data on apoptosis, necrosis, or other mechanisms of cell death. This technical guide provides detailed protocols and troubleshooting advice to ensure maximum cell recovery and reproducibility, thereby enhancing the reliability of your experimental outcomes in cell culture research.
Core Principles and Quantitative Data
Understanding the Balance of Cryoinjury
The fundamental challenge in cryopreservation is balancing two primary mechanisms of cryoinjury. On one hand, slow cooling can lead to excessive cell dehydration and solute damage (the "solute effect" or "solution effects"). On the other hand, rapid cooling promotes lethal intracellular ice formation (IIF), which mechanically disrupts organelles and the plasma membrane [93] [94]. An optimal cooling rate minimizes the sum of these two injuries [93]. The following diagram illustrates the thermodynamic path and competing injury mechanisms during a standard slow-freezing process.
Quantitative Comparison of Freezing Methods
The choice of freezing method and the specific cooling profile are critical process parameters. Research on sensitive cells like spermatogonial stem cells (SSCs) demonstrates that the cooling rate, especially through critical temperature zones, directly impacts post-thaw viability and function [94]. The table below summarizes a comparative study of cooling profiles.
Table 1: Comparison of Cooling Profiles for Cryopreserving Sheep Spermatogonial Stem Cells (SSCs) [94]
| Cooling Profile Description | Approximate Cooling Rate (0°C to -10°C) | Post-Thaw Viability | Proliferation Rate | Stemness Marker Activity |
|---|---|---|---|---|
| Profile 1: Isopropanol "Mr. Frosty" | 1°C/min | 68.8% | Good (similar to pre-freeze) | Well maintained |
| Profile 2: Programmable Freezer | 0.3°C/min (after seeding) | 58.5% | Reduced | Reduced |
| Profile 3: Uncontrolled Rapid Freezing | >50°C/min (direct placement in -80°C) | 45.2% | Significantly Reduced | Significantly Reduced |
Industry Practices and Scaling Challenges
A recent industry survey by the ISCT Cold Chain Management & Logistics Working Group provides insight into real-world practices and challenges. It was found that 87% of respondents use controlled-rate freezing (CRF) for cell-based products, while 13% rely on passive freezing, predominantly in early clinical stages [95]. A significant challenge identified was a lack of consensus on qualifying controlled-rate freezers, with nearly 30% of users relying solely on vendor qualification, which may not represent the final use case [95]. Furthermore, scaling cryopreservation was noted as a major hurdle for the cell and gene therapy industry [95].
Detailed Experimental Protocols
Standardized Cryopreservation Protocol for Maximal Recovery
This protocol is adapted for general mammalian cells, including adherent and suspension cultures [96] [97].
- Pre-freeze Preparation: Use cells in the logarithmic growth phase and confirm the absence of microbial contamination. Cells should be at a high concentration of at least 90% viability [96] [97].
- Harvesting:
- Centrifugation and Counting: Centrifuge the cell suspension at 100–400 × g for 5–10 minutes. Aspirate the supernatant and resuspend the pellet in a small volume of growth medium. Determine the total cell count and viability using an automated cell counter or hemocytometer with Trypan Blue exclusion [98] [96].
- Freezing Medium Preparation: Prepare a cold freezing medium. A common formulation is 90% complete growth medium (e.g., RPMI or DMEM with serum) and 10% DMSO. Alternatively, use a commercial, serum-free freezing medium like Gibco Synth-a-Freeze or Gibco Recovery Cell Culture Freezing Medium [96] [99].
- Resuspension and Aliquoting: Resuspend the cell pellet in the freezing medium to achieve a high cell concentration (e.g., 1 x 10^6 to 1 x 10^7 cells/mL). Gently mix to ensure a homogeneous suspension. Aseptically aliquot the cell suspension into sterile cryovials (e.g., 1 mL/vial) [96].
- Controlled-Rate Freezing:
- Optimal: Use a programmable controlled-rate freezer. A standard profile often starts at 4°C, then cools at -1°C/min to at least -40°C, before rapidly cooling to -90°C or lower [97] [99] [94].
- Alternative: Use an isopropanol freezing chamber (e.g., "Mr. Frosty"). Place the filled cryovials in the chamber at room temperature and store it overnight at -80°C. This apparatus achieves an approximate cooling rate of -1°C/min [96] [94].
- Long-Term Storage: Transfer the frozen cryovials to a liquid nitrogen storage tank, ideally in the vapor phase (typically -150°C to -160°C) to minimize the risk of explosion, or to a -150°C ultra-low freezer. Storing at temperatures above the glass transition point (e.g., -80°C) is not recommended for long-term preservation of most cell types [96] [97].
Optimized Thawing and Seeding Protocol
The thawing process is critical to minimize osmotic stress and the toxic effects of DMSO.
- Rapid Thawing: Remove the cryovial from storage and immediately thaw it by gentle agitation in a 37°C water bath. Thawing should be rapid (approximately 1-2 minutes). Remove the vial when a small ice crystal remains inside [97] [99].
- Dilution and CPA Removal: Decontaminate the vial with 70% ethanol. Gently transfer the cell suspension to a sterile 15 mL centrifuge tube. Slowly dilute the suspension (e.g., drop-wise with gentle agitation) with 10 mL of pre-warmed complete growth medium to reduce osmotic shock. For sensitive cells like iPSCs, adding a Rho kinase (ROCK) inhibitor (e.g., Y-27632) to the medium can improve post-thaw survival [100] [97].
- Centrifugation: Centrifuge the cell suspension at approximately 200 × g for 5–10 minutes. Carefully aspirate the supernatant, which contains the diluted cryoprotectant.
- Reseeding: Gently resuspend the cell pellet in fresh, pre-warmed complete growth medium. Count the cells and assess viability using Trypan Blue exclusion. Seed the cells at the recommended density into an appropriately coated culture vessel (e.g., Matrigel for iPSCs). Ensure uniform seeding for reproducible growth and experimental outcomes [97] [101].
- Post-Thaw Monitoring: Place the culture vessel in a 37°C, 5% CO2 incubator. Monitor the cells daily for attachment, morphology, and confluency. A medium change 24 hours post-thaw can help remove cell debris and residual DMSO.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Cryopreservation and Recovery Workflows
| Reagent / Material | Function / Purpose | Example Products / Formulations |
|---|---|---|
| Cryoprotective Agent (CPA) | Penetrates cells, lowers freezing point, reduces ice crystal formation [102] [97]. | Dimethyl sulfoxide (DMSO), Glycerol, Commercial serum-free media (e.g., Gibco Synth-a-Freeze) [96]. |
| Controlled-Rate Freezing Device | Ensures reproducible, optimal cooling rate to minimize cryoinjury [95] [94]. | Programmable freezer (CRF), Passive cooling chamber (e.g., Nalgene "Mr. Frosty") [96] [94]. |
| Basal Freezing Medium | Provides nutrients and a protein source to support cells during freeze-thaw stress. | Serum-containing medium (e.g., with FBS), Serum-free chemically defined media [96] [99]. |
| Rho Kinase (ROCK) Inhibitor | Improves survival and attachment of single pluripotent stem cells post-thaw by inhibiting apoptosis [100] [97]. | Y-27632 [100]. |
| Cell Dissociation Reagent | Gently detaches adherent cells for harvesting prior to freezing. | Trypsin-EDTA, TrypLE Express [96]. |
| Viability Stain | Accurately quantifies live and dead cell populations before freezing and after thawing. | Trypan Blue, Propidium Iodide (PI) [98] [99]. |
Troubleshooting FAQs
Q1: My post-thaw cell viability is consistently low, but the cells were healthy before freezing. What are the most likely causes?
- A: The problem likely lies in the freezing or thawing kinetics. Key factors to check are:
- Cooling Rate: Ensure you are using the optimal cooling rate for your specific cell type. A rate of -1°C/min is standard for many mammalian cells, but some require optimization [97] [94]. Verify that your isopropanol chamber is properly equilibrated to room temperature before use, or that your programmable freezer profile is correct.
- Thawing Rate: Thawing must be rapid to avoid devitrification and ice recrystallization. Use a 37°C water bath with gentle agitation until only a small ice crystal remains [97] [93].
- Dilution Shock: The sudden dilution of cryoprotectant after thawing causes osmotic shock. Always dilute the thawed cell suspension slowly (drop-wise) into a larger volume of warm medium [97].
Q2: After thawing and seeding, my adherent cells do not attach properly or show delayed proliferation. How can I improve recovery?
- A: Poor attachment indicates sublethal damage to cell adhesion mechanisms or apoptosis.
- Cell Condition: Freeze only healthy, log-phase cells at a high viability (>90%) [96].
- Post-Thaw Environment: For sensitive cells like iPSCs, include a ROCK inhibitor in the recovery medium for the first 24 hours to enhance attachment and survival [100] [97].
- Seeding Density: Seed cells at a sufficiently high density to promote cell-cell contact and paracrine signaling, which supports survival [97] [101].
- Coating: Ensure your culture vessels are properly coated with extracellular matrix proteins (e.g., Matrigel, collagen) to facilitate attachment [97].
Q3: I observe high variability in recovery between different cell lines or even different passages of the same line. Is this normal and how can I manage it?
- A: Some variability is inherent due to biological differences, but it can be managed.
- Clone-to-Clone Variability: Different cell lines (e.g., iPSCs vs. MSCs) and even different clones have distinct membrane permeabilities and cryotolerance. Optimize the protocol (CPA concentration, cooling rate) for each critical cell line [97].
- Passage Number: Use cells at as low a passage number as possible. High-passage cells may have accumulated genetic and phenotypic drifts that affect their resilience [96].
- Freeze Format: Consider whether your cells recover better when frozen as single cells or as small aggregates. Freezing as aggregates can sometimes improve recovery for colony-forming cells like iPSCs by maintaining cell-cell contacts [97].
Q4: What are the best practices for the long-term storage of cryopreserved cells to ensure stability?
- A: Consistent storage temperature is key to preventing recrystallization and metabolic stress.
- Storage Temperature: Store cells below -135°C, which is the common glass transition temperature for water and cryoprotectant solutions. The vapor phase of liquid nitrogen (approx. -150°C to -160°C) or a -150°C ultra-low freezer is recommended [102] [97].
- Avoid Temperature Fluctuations: Do not store cells at -80°C for long-term preservation, as molecular motion and damaging reactions are not completely arrested. Minimize the time cells spend out of storage during inventory checks [97].
Cell Detachment and Dissociation Issues
Problem: "My cells are not detaching properly during passaging, or they are damaged after dissociation. What went wrong?"
This is a common issue often related to the use of trypsin, a serine protease that cleaves peptide bonds to dissociate adherent cells [103] [104]. Incorrect usage can lead to poor cell performance or death.
Solutions and Protocols:
- Optimize Digestion Time: Digestion time should be adjusted based on cell type, typically between 1-5 minutes. Over-digestion can damage cells, making them rounded and creating debris, while under-digestion will leave cells attached. Monitor cells under a microscope; detached cells appear round and refractive [103].
- Use Appropriate Trypsin Formulations: For sensitive cells like primary cells or stem cells, use trypsin-EDTA. EDTA chelates calcium and magnesium ions, weakening cell-to-cell adhesion and enhancing trypsin's effect. Consider recombinant alternatives like TrypLE for gentler dissociation [103].
- Ensure Proper Neutralization: Immediately after dissociation, inactivate trypsin by adding a 2x volume of complete growth medium containing serum [103] [104]. For serum-free cultures, use a soybean trypsin inhibitor at an equimolar concentration [104].
- Check Reagent Quality and Temperature: Use pre-warmed trypsin (37°C for optimal activity) and ensure it has been stored correctly and is not expired [103] [104].
Contamination Identification and Eradication
Problem: "I suspect my culture is contaminated. How can I identify the type and get rid of it?"
Contamination is a primary cause of cell death and unreliable data. swift identification and action are crucial. The table below summarizes common contaminants and solutions.
Table 1: Identifying and Addressing Common Cell Culture Contaminants
| Contaminant | Key Characteristics | Recommended Solutions |
|---|---|---|
| Bacteria [105] | Culture medium turns yellow and appears turbid. Under the microscope, fine sand-like particles are visible. | Use antibiotics in the medium for prevention. Ensure complete sterilization of all equipment and solutions. |
| Molds/Fungi [105] | Medium remains clear. Branched, filamentous, thread-like structures are visible under the microscope. | Isolate contaminated cultures immediately. Disinfect the incubator with copper sulfate, peracetic acid, or other disinfectants [105]. |
| Mycoplasma [105] [106] | No obvious change; culture may gradually die. Confirmed via fluorescent staining (green dots on cell periphery) or PCR. | Difficult to cure. Prevention is key: test new cell lines. Treatments include high-dose antibiotics (e.g., 50 µg/ml Kanamycin) or heat treatment at 41°C [105]. |
| Black Worm [105] | Small, moving black dots under the microscope, with little effect on cell growth. | Increase cell seeding density and change medium daily. It may clear with healthy cell growth. |
Experimental Protocol for Mycoplasma Detection (Fluorescent Staining): [105]
- Culture cells on a sterile cover slip.
- Fix cells and stain with a DNA-binding fluorescent dye (e.g., Hoechst stain).
- Observe under a fluorescence microscope.
- Positive result: Mycoplasma DNA appears as bright green speckles scattered around the cell periphery or on the cell surface.
Poor Cell Growth and Viability
Problem: "My cells are not growing well and viability is low, but there's no obvious contamination."
This vague symptom can stem from multiple factors, including the culture environment and cell state.
Solutions:
- Check the CO₂ Incubator: For mammalian cells, CO₂ concentration is typically maintained at 5% to keep the medium's pH at 7.2-7.4 [107]. Use an infrared sensor for high-precision control (±0.1%) and calibrate the incubator regularly (every 6-12 months) [107].
- Assess Cell State and Passage: Use cells in their logarithmic growth phase. Avoid using old, senescent, or over-confluent cells. Check for cell density before passaging [103].
- Verify Culture Reagents: Use fresh, high-quality medium and serum. Test new batches if necessary.
The Scientist's Toolkit: Essential Reagents and Equipment
Table 2: Key Research Reagent Solutions for Cell Culture
| Item | Function | Key Considerations |
|---|---|---|
| Trypsin-EDTA [103] [104] | Dissociates adherent cells for passaging. | Concentration typically 0.05%-0.25%. Pre-warm to 37°C. Neutralize with serum-containing media. |
| Recombinant Trypsin (e.g., TrypLE) [103] | Gentler alternative to animal-sourced trypsin. | Ideal for sensitive cells (stem cells, primary cells) and proteinomics studies to avoid serum. |
| Phenol Red [104] | pH indicator in culture media. | Pink at pH 7-7.4 (optimal). Turns orange/yellow if acidic (contamination/metabolism) and purple if basic. |
| Antibiotics & Antimycotics | Prevents bacterial and fungal growth. | Use for short-term experiments. Avoid long-term use to mask contamination and promote antibiotic resistance. |
| CO₂ Incubator [108] [107] | Provides a stable environment (temp, humidity, CO₂) for cell growth. | Look for precise CO₂ control (±0.1%), temperature uniformity, and contamination control features (e.g., copper surfaces, HEPA filters, UV sterilization). |
| Centrifuge [108] | Pellets cells after passaging for resuspension and counting. | Use low speed (100-300 x g) for 5-10 minutes to avoid damaging cells [104]. |
| Biological Safety Cabinet [108] | Provides an aseptic work area protecting both the user and the cell culture. | Follow best practices for cleaning and airflow. Do not block grilles. |
Experimental Protocol: Standard Cell Passaging with Trypsin
This is a detailed methodology for a key cell culture experiment [104].
Workflow Diagram: Cell Passaging Protocol
Detailed Steps:
- Preparation: Pre-warm trypsin-EDTA, phosphate-buffered saline (PBS) without Ca²⁺/Mg²⁺, and complete growth medium in a 37°C water bath. Work in a biosafety cabinet using aseptic technique [104] [106].
- Rinsing: Remove and discard the culture medium from the flask. Gently rinse the cell layer with PBS to remove residual serum and divalent cations, which can inhibit trypsin activity [104].
- Digestion: Add a sufficient volume of pre-warmed trypsin to cover the cell layer (e.g., 0.5 mL per 10 cm²). Gently swirl the flask and incubate at 37°C for 1-5 minutes [104].
- Monitoring: Observe the cells under a microscope. Detached cells will appear round and refractile. If fewer than 90% of cells are detached, tap the flask gently and incubate for another minute. Avoid exposure to trypsin for more than 10 minutes [104].
- Neutralization: Once cells are detached, immediately add 2 volumes of pre-warmed complete growth medium to inactivate the trypsin. Gently pipette the medium over the cell layer surface to ensure >95% cell recovery [104].
- Harvesting: Transfer the cell suspension to a centrifuge tube. Centrifuge at 100-300 x g for 5-10 minutes. Discard the supernatant [104].
- Reseeding: Resuspend the cell pellet in fresh, pre-warmed complete medium. Count cells using a hemocytometer or automated cell counter with Trypan Blue exclusion. Dilute the cell suspension to the desired seeding density and transfer to a new culture flask. Place the flask in a 37°C, 5% CO₂ incubator [104].
Ensuring a Sterile Working Environment
Problem: "I follow protocols, but I keep getting random contaminations. What are the best practices for sterile technique?"
Solutions and Protocols:
- Biosafety Cabinet (BSC) Practices: [106]
- Decontaminate: Before use, wipe down all surfaces, gloves, and items entering the BSC with 70% ethanol.
- Minimize Disruption: Do not block the front or rear grilles. Limit the number of items in the BSC to maintain proper laminar airflow.
- Avoid Pouring: Never pour from one bottle to another; always use sterile pipettes.
- Incubator Hygiene: [105]
- Clean the CO₂ incubator regularly (e.g., every 2 months). Use a solution of copper sulfate or other disinfectants to wipe the interior and water pan to prevent fungal growth.
- In case of contamination, clean the incubator thoroughly with a disinfectant like peracetic acid.
Validating and Differentiating Cell Death: Guidelines for Accurate Interpretation
This technical support center provides guidance for researchers on selecting and validating assays for cell death research, with a focus on overcoming common challenges to ensure data reliability.
Frequently Asked Questions (FAQs)
Q1: My assay results are inconsistent between replicates. What are the most common causes? Poor reproducibility often stems from technical, procedural, or equipment issues. Key areas to investigate include:
- Pipetting Technique: Inaccurate pipetting is a major source of error. Ensure pipettes are properly calibrated, tips are firmly seated, and tips are changed between samples to avoid cross-contamination [109].
- Washing Steps: Overly aggressive or inconsistent plate washing can dissociate bound reactants, leading to high variability. Automated washers should use gentle settings, and manual methods should ensure uniform washing time for all wells [110].
- Reagent Contamination: Trace contamination from concentrated upstream samples (e.g., cell culture media) can severely impact sensitive assays. Perform assays in a dedicated, clean area away from high-concentration sample handling [110].
- Instrumentation: A failing microplate reader, indicated by high well-to-well variability in blank wells, can cause inconsistent results, particularly at low signal levels [110].
Q2: How can I validate that my cell death assay is accurately measuring what it claims to? Assay validation involves testing several key performance characteristics [111]:
- Accuracy: Demonstrate that your method recovers a known quantity of analyte spiked into a sample. For example, spike a known amount of a purified cell death marker (e.g., caspase-3) into a buffer or control matrix.
- Specificity: Prove that the assay signal is generated only by the target analyte. In a cell death assay, this means showing that the measurement is not interfered with by other components in the sample, such as unrelated proteins or drugs.
- Precision: Evaluate the agreement between repeated measurements. This includes repeatability (same day, same analyst) and intermediate precision (different days, different analysts) [111].
Q3: Why do I get different results when using different platforms to measure the same cell death marker? Different technologies have inherent strengths and limitations that impact their performance. A comparison of biomarker profiling platforms revealed significant differences in reproducibility, accuracy, and sensitivity [112]. For instance:
- Reproducibility: Coefficients of variation (CV) for technical replicates can vary widely between platforms, from as low as 6.9% to over 22% [112].
- Bias: Some platforms may over- or under-represent certain targets due to sequence-specific detection biases. One study showed that the percentage of targets with signals within 2-fold of the expected value ranged from 31% to 76% across different platforms [112]. These differences can directly impact your ability to detect true biological changes.
Key Validation Parameters and Data Interpretation
When qualifying an assay for your research, evaluate these core parameters. The table below summarizes targets and typical acceptance criteria for a well-validated method.
Table 1: Key Analytical Performance Characteristics for Assay Validation [111]
| Parameter | Definition | Typical Validation Target |
|---|---|---|
| Accuracy | Closeness of agreement between the true value and the value found. | Recovery of 90–110% for spiked analytes. |
| Precision | Closeness of agreement between a series of measurements. | % Relative Standard Deviation (RSD) < 15-20% for replicates. |
| Specificity | Ability to measure the analyte accurately in the presence of interfering components. | No interference from expected sample components; resolution of co-eluting peaks in chromatography. |
| Linearity | The ability of the method to obtain results directly proportional to analyte concentration. | Coefficient of determination (r²) > 0.99 across the method range. |
| Range | The interval between the upper and lower concentrations that can be determined with suitable precision, accuracy, and linearity. | Defined by the intended use of the method (e.g., 50-150% of expected concentration). |
| Limit of Detection (LOD) | The lowest amount of analyte that can be detected. | Signal-to-noise ratio ≥ 3:1. |
| Limit of Quantitation (LOQ) | The lowest amount of analyte that can be quantified with acceptable precision and accuracy. | Signal-to-noise ratio ≥ 10:1. |
Quantitative data from platform comparisons can guide selection. The following table compiles performance data from a study comparing microRNA profiling platforms, illustrating how core parameters can vary significantly between technologies.
Table 2: Performance Comparison of Biomarker Profiling Platforms (Adapted from Godoy et al.) [112]
| Platform | Median CV (Equimolar Pool) | % of miRNAs within 2-Fold of Expected Signal | Ability to Detect Biological Differences (Placenta miRNAs) |
|---|---|---|---|
| Small RNA-seq | 8.2% | 31% | Yes |
| EdgeSeq | 6.9% | 76% | Yes |
| nCounter | Not Assessed | 47% | No |
| FirePlex | 22.4% | Not Specified | No |
Experimental Protocols for Key Cell Death Assays
Protocol: Validating an ATP Release Assay for Monitoring Cell Death Dynamics
Background: The release of adenosine triphosphate (ATP) from dying cells acts as a critical Danger-Associated Molecular Pattern (DAMP). The timing and magnitude of ATP release differ between cell death modalities, providing functional insights [113]. This protocol measures extracellular ATP as a marker of cell death.
Materials:
- Extracellular ATP Assay Kit (Luminescence-based) [113]
- Cell culture model system (e.g., HeLa, Jurkat cells)
- Cell death inducers (e.g., Staurosporine for apoptosis, Erastin for ferroptosis) [113]
- Multiwell plate reader capable of measuring luminescence
- Sterile cell culture plates
Method:
- Cell Seeding and Treatment:
- Seed cells at an appropriate density in a multiwell plate and allow them to adhere overnight.
- Treat cells with your chosen death inducer(s). Include a vehicle control (e.g., DMSO).
- For apoptosis inhibition studies, pre-treat cells with a pan-caspase inhibitor like Z-VAD before adding Staurosporine [113].
Sample Collection:
- At designated time points post-induction, collect the cell culture supernatant.
- Centrifuge the supernatant briefly (e.g., 300 x g for 5 minutes) to pellet any floating cells or debris.
ATP Measurement:
- Transfer a clear aliquot of the supernatant to a new plate suitable for luminescence reading.
- Following the manufacturer's instructions for your ATP assay kit, add the luminescence reaction mix.
- Measure luminescence immediately on a plate reader.
Data Normalization and Analysis:
- Normalize luminescence readings to a standard curve generated with known concentrations of ATP.
- Express results as extracellular ATP concentration (nM or μM) and plot over time or against treatment dose.
- Correlate ATP release with other death markers, such as a drop in cell viability measured by a Cell Counting Kit-8 [113].
Troubleshooting:
- No Signal: Verify reagent activity and cell death induction using a viability assay.
- High Background: Ensure supernatant is free of cells, as lysis during transfer will release intracellular ATP. Check for bacterial contamination in media, which can be a source of ATP.
- Poor Precision: Check pipetting accuracy and ensure reagents are mixed thoroughly without generating bubbles.
Visualizing Cell Death Pathways and Assay Selection
This diagram illustrates the relationship between different cell death modalities and the release of ATP, a key measurable DAMP.
The Scientist's Toolkit: Essential Reagents for Cell Death Analysis
This table lists key reagents and their applications for studying cell death, based on techniques highlighted in recent research.
Table 3: Key Research Reagent Solutions for Cell Death Analysis [113]
| Reagent / Kit Name | Primary Function | Application Example in Cell Death |
|---|---|---|
| Extracellular ATP Assay Kit (Luminescence) | Measures ATP released from cells into the surrounding medium. | Differentiating ATP release profiles between apoptosis (suppressed) and pyroptosis/necroptosis (enhanced) [113]. |
| Annexin V Apoptosis Plate Assay Kit | Detects phosphatidylserine externalization on the cell surface. | Identifying early-stage apoptotic cells [113]. |
| Cytotoxicity LDH Assay Kit | Measures lactate dehydrogenase (LDH) enzyme released upon plasma membrane damage. | Quantifying necrotic cell death or final stages of lytic cell death [113]. |
| Cell Counting Kit-8 (CCK-8) | Utilizes a tetrazolium salt to quantify cellular metabolic activity. | Serving as a proxy for cell viability and proliferation in conjunction with death assays [113]. |
| FerroOrange | A probe that fluoresces upon binding to intracellular Fe²⁺. | Detecting increased labile iron, a key event in the ferroptosis pathway [113]. |
| Autophagic Flux Assay Kit | Measures the activity of the autophagic process in cells. | Investigating the role of non-canonical autophagy in sequestering ATP during apoptosis [113]. |
Within the context of cell death research, accurately discriminating between the specific modalities of programmed cell death is paramount for experimental validity and biological interpretation. The confusion between apoptosis, necroptosis, and autophagic cell death can lead to misinterpretation of experimental results, flawed mechanistic studies, and incorrect conclusions regarding drug mechanisms and therapeutic efficacy. This technical guide provides a systematic framework for distinguishing these three distinct forms of cell death, offering troubleshooting advice and methodological protocols to address common challenges faced by researchers in cell culture systems. Establishing precise diagnostic criteria is essential for advancing our understanding of cell death pathways and their implications in disease pathogenesis and treatment.
Core Concepts: Defining the Cell Death Types
Key Definitions and Characteristics
- Apoptosis: A genetically encoded, caspase-mediated cell suicide program characterized by cell shrinkage, nuclear condensation, and formation of apoptotic bodies that are efficiently cleared by phagocytes, typically without inducing inflammation [114] [115] [116].
- Necroptosis: A regulated form of necrotic cell death that occurs independently of caspases, mediated by receptor-interacting protein kinases RIPK1 and RIPK3, and mixed lineage kinase domain-like protein (MLKL), resulting in plasma membrane rupture and release of pro-inflammatory cellular contents [114] [115].
- Autophagic Cell Death: A programmed cell death process characterized by massive cytoplasmic vacuolization through autophagosome formation, which may occur independently of apoptosis or in conjunction with other death pathways [117] [116].
Comparative Analysis of Key Features
The table below summarizes the fundamental distinguishing characteristics of the three cell death modalities.
Table 1: Fundamental Characteristics of Apoptosis, Necroptosis, and Autophagic Cell Death
| Feature | Apoptosis | Necroptosis | Autophagic Cell Death |
|---|---|---|---|
| Morphological Hallmarks | Cell shrinkage, chromatin condensation, apoptotic bodies [118] [116] | Cell swelling, plasma membrane rupture, moderate chromatin condensation [119] [115] | Massive cytoplasmic vacuolization, autophagosome formation [117] [116] |
| Molecular Mediators | Caspases, Bcl-2 family, Apaf-1 [114] [118] | RIPK1, RIPK3, MLKL [114] [115] | ATG proteins, Beclin-1, LC3 [117] [120] |
| Membrane Integrity | Maintained until late stages (blebbing) [115] [116] | Lost (rupture) [119] [115] | Generally maintained until late stages [116] |
| Inflammatory Response | Immunologically silent or anti-inflammatory [114] [115] | Strongly pro-inflammatory [115] | Generally low immunogenicity [116] |
| "Point of No Return" | Mitochondrial outer membrane permeabilization (MOMP) [114] | MLKL oligomerization and membrane translocation [115] | Not precisely defined; context-dependent [117] |
The Researcher's Toolkit: Essential Reagents and Assays
Key Research Reagent Solutions
Table 2: Essential Reagents for Studying Cell Death Pathways
| Reagent/Category | Example Specific Agents | Primary Function/Application |
|---|---|---|
| Caspase Inhibitors | Z-VAD-FMK (pan-caspase inhibitor) [119] | Inhibits apoptosis; confirms caspase-dependence [119] |
| Necroptosis Inhibitors | Necrostatin-1 (RIPK1 inhibitor) [115] | Specifically inhibits necroptosis pathway [115] |
| Autophagy Inhibitors | 3-Methyladenine (PI3K inhibitor), Chloroquine (lysosomotropic agent) [119] | Blocks early (3-MA) or late (CQ) stages of autophagy [119] |
| BH3 Mimetics | ABT-199 (Venetoclax) [120] | Promotes intrinsic apoptosis by inhibiting Bcl-2 [120] |
| SMAC Mimetics | LCL161, BV6 [120] | Promotes apoptosis by antagonizing IAP proteins [120] |
| MLKL Inhibitors | Necrosulfonamide [115] | Blocks membrane pore formation during necroptosis [115] |
| LC3-Related Reagents | GFP-LC3 translocation assay [116] | Detects and monitors autophagosome formation [116] |
Troubleshooting Guide: Frequently Asked Questions
Identification and Discrimination Challenges
Q1: My treatment induces significant cell death with mixed morphological features. How can I determine the primary death modality?
- Problem: Overlapping morphological features between death pathways complicate identification.
- Solution Approach: Implement a multi-parameter assessment strategy combining functional, morphological, and biochemical analyses.
- Begin with Membrane Integrity: Use Annexin V/PI staining to detect phosphatidylserine exposure (early apoptosis) and membrane permeability (necrosis/necroptosis) [116].
- Apply Specific Pharmacological Inhibitors: Treat parallel samples with Z-VAD-FMK (apoptosis inhibitor), Necrostatin-1 (necroptosis inhibitor), and 3-Methyladenine (autophagy inhibitor). The inhibitor that most effectively rescues viability indicates the primary death pathway [119] [115].
- Assess Key Molecular Markers: Analyze cleavage of caspase-3 and PARP (apoptosis), phosphorylation of MLKL (necroptosis), and LC3-I to LC3-II conversion (autophagy) via Western blotting [119] [116].
- Preventive Consideration: Establish time-course and dose-response studies, as the dominant death pathway can shift with varying treatment intensity or duration [114].
Q2: I observe extensive cytoplasmic vacuolization, but my autophagy inhibitor does not rescue cell death. What does this indicate?
- Problem: Not all cytoplasmic vacuolization signifies autophagic cell death.
- Solution Approach:
- Confirm Autophagy Specificity: Validate autophagic vacuoles using specific markers like GFP-LC3 puncta formation or detection of LC3-II by immunoblotting [117] [116].
- Consider Alternative Death Pathways: Vacuolization can occur in other processes like paraptosis or methuosis [119] [25]. If death is not inhibited by autophagy suppression, investigate these alternatives.
- Evaluate Cross-Talk: Autophagy often interacts with other death pathways. The observed death may be autophagy-mediated but executed via apoptosis or necroptosis. Inhibit these parallel pathways to clarify interactions [117] [121].
- Preventive Consideration: Use multiple, specific autophagy assays (e.g., flux assays with bafilomycin A1) rather than relying solely on morphology or single inhibitors [117].
Q3: How can I definitively confirm that observed cell death is necroptosis rather than accidental necrosis?
- Problem: Necroptosis and necrosis share morphological endpoints (membrane rupture), but only necroptosis is regulated.
- Solution Approach:
- Genetic/Pharmacological Inhibition: Demonstrate that death is suppressed by genetic knockdown of RIPK1, RIPK3, or MLKL, or by specific pharmacological inhibitors like Necrostatin-1 [115].
- Caspase-Independence: Confirm that death occurs even when caspases are broadly inhibited by Z-VAD-FMK, a hallmark of necroptosis [114] [115].
- Detect Key Activation Events: Use phospho-specific antibodies to detect phosphorylated RIPK3 and phosphorylated MLKL, the definitive molecular signature of necroptotic signaling [115].
- Preventive Consideration: Always include a positive control for necroptosis (e.g., TNF-α + Z-VAD + SMAC mimetic) when establishing models [115].
Standard Operating Procedures: Key Experimental Workflows
A Multi-Parameter Flow Cytometry Protocol for Discriminating Cell Death
This protocol enables simultaneous assessment of multiple death parameters in a single sample [116].
Cell Staining:
- Harvest and wash cells in cold PBS.
- Resuspend cells in Annexin V binding buffer.
- Add Annexin V-FITC (for phosphatidylserine exposure) and Propidium Iodide (PI, for membrane integrity).
- Incubate for 15 minutes in the dark at room temperature.
- For caspase activity, include a cell-permeable FLICA reagent (Fluorochrome-Labeled Inhibitor of Caspases) during the culture period prior to harvesting.
Data Acquisition and Analysis:
- Analyze samples using flow cytometry within 1 hour.
- Identify populations:
- Viable cells: Annexin V⁻/PI⁻
- Early Apoptotic: Annexin V⁺/PI⁻
- Late Apoptotic/Necrotic: Annexin V⁺/PI⁺
- Caspase Activity: FLICA⁺ cells indicate apoptotic engagement.
Immunoblotting-Based Molecular Pathway Assessment
This protocol confirms activation of specific death pathways through key molecular markers.
Sample Preparation:
- Lyse cells in RIPA buffer containing protease and phosphatase inhibitors.
- Determine protein concentration and prepare equal amounts for SDS-PAGE.
Target Detection:
Microscopic Morphological Assessment Protocol
The gold standard for initial death classification based on cellular and nuclear morphology [116].
Staining:
- Culture cells on glass coverslips.
- Fix with 4% paraformaldehyde and permeabilize with 0.1% Triton X-100.
- Stain nuclei with Hoechst 33342 and actin cytoskeleton with phalloidin.
Analysis:
- Apoptosis: Look for cell shrinkage, nuclear condensation and fragmentation, and membrane blebbing [118] [116].
- Necroptosis: Identify cell swelling, plasma membrane rupture, and moderate chromatin condensation [119] [115].
- Autophagic Cell Death: Observe extensive cytoplasmic vacuolization in the absence of dominant chromatin condensation [116].
Visualizing the Pathways: Key Signaling Mechanisms
Apoptosis Signaling Pathway
Diagram 1: Apoptosis involves extrinsic and intrinsic pathways converging on caspase activation.
Necroptosis Signaling Pathway
Diagram 2: Necroptosis is triggered by caspase inhibition leading to MLKL-mediated membrane disruption.
Autophagic Cell Death Pathway
Diagram 3: Autophagy involves vesicle formation and degradation, which can promote survival or death.
Accurately distinguishing between apoptosis, necroptosis, and autophagic cell death requires a multifaceted approach that integrates morphological observation, pharmacological inhibition, and molecular marker analysis. No single assay is sufficient for definitive classification. By implementing the standardized protocols, troubleshooting guidelines, and multi-parameter assessment strategies outlined in this technical guide, researchers can significantly enhance the accuracy of their cell death classification, leading to more reliable data interpretation and more robust mechanistic insights in their research on cell death pathways.
Within cell death research, accurately predicting a cell's response to a therapeutic agent is paramount. For years, single biomarkers have been used as indicators of treatment efficacy. However, the complexity of biological systems, especially the multifaceted signaling pathways governing cell death, means that a single molecule often fails to capture the full picture. This technical support document outlines how multi-analyte biomarker panels significantly enhance predictive power for therapeutic response compared to single markers, providing troubleshooting guides and FAQs for researchers navigating this complex field.
The Quantitative Case for Biomarker Panels
The superior performance of biomarker panels is demonstrated by quantitative improvements in key diagnostic metrics such as Area Under the Curve (AUC), sensitivity, and specificity. The table below summarizes data from peer-reviewed studies comparing panel performance to single markers.
Table 1: Performance Comparison of Single Biomarkers vs. Multi-Biomarker Panels
| Disease/Condition | Single Marker (Example) | Single Marker Performance (AUC) | Biomarker Panel | Panel Performance (AUC & Other Metrics) | Source |
|---|---|---|---|---|---|
| Ovarian Cancer Detection | CA-125 (MUCIN-16) | Lower than panel | 11-protein panel (incl. MUCIN-16, WFDC2) | AUC = 0.94, Sensitivity 85%, Specificity 93% [122] | |
| Gastric Cancer Detection | Various single markers | Outperformed by panel | 19-protein signature | AUC = 0.99, Sensitivity 93%, Specificity 100% [122] | |
| Multiple Sclerosis (MS) Activity | Neurofilament Light (NfL) | AUC = 0.69 | 4-protein panel (sNfL, uPA, hK8, DSG3) | AUC = 0.87 for distinguishing relapse from remission [122] | |
| Lupus Nephritis Renal Flare Prediction | Individual urinary proteins (e.g., L-PGDS) | Lower than panel | Panel of L-PGDS, ICAM-1, VCAM-1, plus conventional markers | Excellent ability to identify flare; panel factors associated with flares in regression analysis [123] | |
| Cardiovascular Event Risk | High-sensitivity Troponin T (hs-TnT) | Informative, but improved by panel | 21-protein panel (CVD-21, incl. MMP-12, U-PAR, FGF-23) | Provided superior prognostic value for major adverse cardiovascular events [122] |
Core Signaling Pathways in Cell Death and Biomarker Correlation
Understanding the interconnected pathways of cell death is key to designing effective biomarker panels. The diagram below maps the relationship between common cell death stimuli, the organelles involved, and the biomarkers they release.
Diagram: Cell Death Pathways & Biomarker Correlation. This diagram illustrates how different stimuli trigger organelle-specific stress, leading to measurable biomarker events and potentially influencing tumor heterogeneity. The pathways are derived from studies on nanoparticle-induced cell death and apoptosis in HCC [124] [125].
Experimental Protocol: Developing a Biomarker Panel for Cell Death
This protocol provides a step-by-step methodology for discovering and validating a protein biomarker panel, using advanced multiplex proteomics.
Methodology: Multiplex Proteomics for Panel Discovery [122]
Sample Collection & Preparation:
- Collect bio-samples relevant to your cell death model (e.g., cell culture supernatant, lysates, or patient plasma/serum).
- Process samples uniformly: centrifuge to remove debris, aliquot, and store at -80°C. Avoid freeze-thaw cycles.
- Troubleshooting: Note and record the number of freeze-thaw cycles for each sample, as this can impact protein integrity.
Multiplex Protein Measurement:
- Utilize a high-throughput platform such as the Olink Explore platform (using Proximity Extension Assay - PEA technology) or Luminex xMAP bead-based immunoassays.
- These platforms allow for the simultaneous quantification of hundreds to thousands of proteins from a minimal sample volume (e.g., 1 µL of plasma).
- Follow the manufacturer's protocol for sample loading, incubation, and data acquisition.
- Troubleshooting: Include randomized control samples across plates to monitor and correct for technical batch effects.
Data Pre-processing & Normalization:
- Normalize protein expression data across all samples using quantile normalization to correct for technical variation [126].
- Scale data as required by the downstream analysis.
Feature Selection & Model Building:
- Goal: Identify the smallest set of proteins that best predicts the outcome (e.g., therapy response vs. resistance).
- Use machine learning algorithms for feature selection, such as:
- Elastic Net Regression: Performs automatic variable selection and handles correlated predictors well.
- Random Forest (with Boruta): Identifies all-relevant variables, distinguishing them from noisy predictors [122].
- Inputs: Normalized protein expression data.
- Output: A shortlist of candidate biomarkers for the panel.
Model Training & Validation:
- Using the shortlisted proteins, build a predictive model (e.g., a logistic regression model) that combines the markers into a single "risk score."
- Critical Step: Validate the model on an independent, unseen cohort of samples. This confirms that the panel is not over-fitted to the discovery dataset.
- Calculate performance metrics on the validation set: AUC, sensitivity, specificity.
Clinical/Biological Translation:
- The final model is translated into a simplified test. The values of the panel's proteins are input into the model to generate a clear "disease risk" or "therapy response" score for each sample [122].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents used in the experiments cited and their functions in cell death and biomarker research.
Table 2: Research Reagent Solutions for Cell Death & Biomarker Studies
| Reagent / Technology | Function / Application | Experimental Context |
|---|---|---|
| Olink PEA Platform | High-sensitivity multiplex immunoassay for simultaneous measurement of hundreds of proteins from minimal sample volume [122]. | Discovery and validation of protein biomarker signatures in oncology, neurology, and cardiovascular disease [122]. |
| Luminex xMAP Technology | Bead-based multiplex immunoassay for measuring multiple analytes in a single sample [122]. | Development of multi-analyte diagnostic panels [122]. |
| LysoTracker | Fluorescent dye that accumulates in acidic compartments (lysosomes). A breakdown in fluorescence indicates Lysosomal Membrane Permeabilization (LMP) [125]. | Live-cell imaging to track initiation of lysosomal-mediated cell death, e.g., after nanoparticle exposure [125]. |
| TMRM (Tetramethylrhodamine methyl ester) | Cell-permeant dye that accumulates in active mitochondria. Fluorescence loss marks Mitochondrial Outer Membrane Permeabilization (MOMP) [125]. | Single-cell analysis of mitochondrial involvement in apoptotic pathways [125]. |
| CellROX | Fluorescent probe for detecting reactive oxygen species (ROS) and oxidative burst [125]. | Measuring oxidative stress as a downstream event of MOMP or other cell death triggers [125]. |
| CellEvent Caspase-3/7 | Fluorogenic substrate that becomes activated upon cleavage by caspase-3/7, key executioner enzymes in apoptosis [125]. | Detecting the commitment phase of apoptotic cell death in live cells [125]. |
| pSIVA-IANBD | A fluorescent protein that binds to phosphatidylserine (PhS) only when it is externalized to the outer leaflet of the plasma membrane, an early marker of apoptosis [125]. | Real-time monitoring of apoptosis in live-cell imaging assays [125]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My biomarker panel performs well in my discovery cohort but fails in validation. What are the most likely causes?
- A: This is often due to overfitting or pre-analytical biases.
- Overfitting: The model may be too complex, learning noise from the discovery set rather than true biological signal. Solution: Use stricter feature selection algorithms (like Elastic Net) and ensure your discovery cohort is large enough. Always pre-define your analysis plan before seeing the data [127].
- Batch Effects: Technical variation between the sample processing in the discovery and validation phases can obscure the true signal. Solution: Implement randomization and blinding during sample processing and data generation. Process validation cohort samples in a manner identical to the discovery cohort [127].
- Population Differences: The validation cohort may differ clinically or demographically from the discovery cohort. Solution: Ensure the patient population and specimen types directly reflect the intended use of the biomarker from the very beginning [127].
Q2: When should I use a panel instead of a single, well-established biomarker?
- A: Consider a panel in these scenarios:
- When a single marker lacks sufficient sensitivity or specificity for your application, as seen with CA-125 in ovarian cancer [122].
- When the biological process is complex and involves multiple pathways, such as monitoring multiple facets of cell death (lysosomal, mitochondrial) or predicting response to complex therapies like immunotherapy [128] [126].
- When you need to capture the earliest signs of a disease or response, as different proteins in a panel may change at different times, increasing the chance of early detection [122].
Q3: How do I determine the optimal number of biomarkers to include in a panel?
- A: More is not always better. The goal is a parsimonious model.
- Use machine learning-based feature selection methods (e.g., Elastic Net, Random Forest) to identify the most informative predictors [122].
- Evaluate model performance (e.g., AUC) with sequentially added markers. The optimal number is often at the point where adding more biomarkers provides only a marginal improvement in performance, balancing accuracy with clinical practicality and cost [127] [122].
Q4: In live-cell imaging of cell death, my event times are highly heterogeneous. How should I analyze this data?
- A: Heterogeneity is an inherent feature of cell death. Move beyond ensemble averages.
- Use high-throughput, single-cell imaging and analysis platforms (like LISCA) to extract event times (e.g., tLMP, tMOMP) for each cell individually [125].
- Analyze data using two-dimensional event-time scatter plots to identify correlations and temporal sequences between different marker events (e.g., LMP always precedes MOMP). Cluster analysis can reveal subpopulations of cells following distinct death pathways [125].
Correlating In Vitro Findings with Clinical and Pathological Relevance
A critical challenge in modern biomedical research is the frequent failure of promising therapeutic candidates in human clinical trials after showing efficacy in conventional laboratory models. This translational gap is particularly pronounced in the study of cell death, where in vitro findings often do not correlate with clinical outcomes. [129] For example, several neuroprotective drugs have failed in human clinical trials despite promising pre-clinical data, suggesting that conventional cell cultures and animal models cannot precisely replicate human pathophysiology. [129] This technical support center provides troubleshooting guidance to help researchers strengthen the physiological relevance of their in vitro cell death models and improve the clinical predictability of their experimental findings.
Fundamental Concepts: Defining Cell Death Accurately
A common source of error in cell culture research is the inconsistent use and interpretation of fundamental terminology. Misinterpreting assay results can lead to false conclusions about cellular responses.
Table 1: Defining Key Cell Death and Culture Concepts
| Term | Precise Definition | Common Misinterpretations |
|---|---|---|
| Viability | The number of living cells; a broad term without specification of the factor affecting the number. [130] | Interchangeably used with proliferation or cell death. |
| Proliferation Rate | How fast a group of cells divide over time. [130] | Often conflated with viability. A decrease in viable cell number is automatically interpreted as reduced proliferation. |
| Cell Death | The process of cells dying; requires evidence of death-related alterations. [130] | Often claimed based only on a decrease in viability, which could also be caused by reduced proliferation. |
| Apoptosis | A specific form of programmed cell death with established molecular and morphological features. [131] | Frequently claimed based only on metabolic activity assays (e.g., MTT), which do not measure apoptotic markers. |
| Cytotoxicity | Being toxic to cells, typically implying cell killing. [130] | Often used to indicate any decrease in viability, not necessarily death. |
| Autophagy | A catabolic process that can promote survival or induce cell death under prolonged stress, characterized by lysosomal degradation. [131] [41] | Sometimes misinterpreted as invariably leading to cell death, though it often functions as a pro-survival mechanism. [131] |
Troubleshooting FAQ:
Q: My MTT assay shows a significant decrease in absorbance after treatment. Can I conclude that my treatment induces cell death or apoptosis?
A: Not necessarily. A decrease in MTT signal, which measures metabolic activity, indicates a reduction in viability. This reduction could be due to either cell death or a decrease in proliferation rate. To justifiably claim "cell death," you must provide additional evidence using methods that directly measure death-related events, such as loss of membrane integrity (e.g., LDH release assay, propidium iodide staining). To claim "apoptosis" specifically, you need evidence of apoptotic markers, such as caspase activation, phosphatidylserine externalization (Annexin V staining), or DNA fragmentation. [130]
Troubleshooting Guide: Common Pitfalls and Solutions
Table 2: Troubleshooting Common Issues in Cell Death Research
| Problem Scenario | Potential Cause | Recommended Solution |
|---|---|---|
| Poor correlation between in vitro and in vivo drug efficacy. | Use of oversimplified 2D monocultures that lack the physiological complexity of human tissue (e.g., missing cell-cell interactions, tumor microenvironment). [129] | Transition to more physiologically relevant 3D culture models (e.g., spheroids, organoids) that better mimic the in vivo architecture and cell interactions. [129] |
| High and variable cell death in bioreactors or long-term cultures. | Accumulation of environmental stresses such as nutrient depletion, metabolic by-product accumulation (e.g., lactate), and osmolarity shifts. [131] [41] | - Process Optimization: Supplement culture media with critical nutrients. [131] [41]- Genetic Engineering: Overexpress anti-apoptotic genes (e.g., Bcl-2, Bcl-xL) in production cell lines to delay the onset of apoptosis. [131] [41] |
| Irreproducible cell death results between experiments. | 1. Cell line misidentification or cross-contamination.2. Mycoplasma contamination.3. Genetic drift in long-passaged cells. [38] | 1. Authenticate cell lines regularly using STR profiling. [38]2. Implement routine mycoplasma testing. [38]3. Use low-passage cells and create a well-managed cell stock inventory. [38] |
| Inability to model complex disease pathology like neurodegeneration. | Reliance on immortalized cell lines or animal cells that do not capture the human genetic background of the disease. [129] | Utilize human induced Pluripotent Stem Cell (iPSC)-derived neurons and glia. These cells can be generated from patients, providing a model that carries the same genetic variants associated with the human disease. [129] |
Essential Methodologies and Protocols
Distinguishing Different Modes of Cell Death
To accurately characterize cell death, a multi-parametric approach is essential. Relying on a single assay often leads to misinterpretation.
Workflow for Characterizing Cell Death Mechanisms:
Recommended Protocols:
Annexin V/Propidium Iodide (PI) Staining for Apoptosis/Necrosis:
- Harvest cells and wash with cold PBS.
- Resuspend cells in Annexin V binding buffer.
- Add Annexin V-FITC and PI, incubate for 15 minutes in the dark.
- Analyze by flow cytometry within 1 hour.
- Interpretation: Annexin V+/PI- → Early Apoptosis; Annexin V+/PI+ → Late Apoptosis/Necrosis. [41]
LC3 Puncta Formation Assay for Autophagy:
- Culture cells on glass coverslips and apply treatments.
- Transfer cells to a low-serum or nutrient-free medium to induce autophagy if necessary.
- Fix cells and immunostain with an anti-LC3 antibody.
- Visualize using fluorescence microscopy. The formation of distinct LC3-positive puncta indicates autophagosome accumulation. [131]
Molecular Pathway Analysis
Understanding the signaling pathways involved is crucial for mechanistic insight. The diagram below summarizes the key regulators of apoptosis and autophagy, which are frequently interconnected.
Key Signaling Pathways in Cell Death and Survival:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cell Death Research
| Reagent / Assay | Primary Function | Key Considerations |
|---|---|---|
| Tetrazolium Salts (MTT, MTS) | Measures cellular metabolic activity as a viability indicator. [130] | Does not directly measure cell death or proliferation. Results can be influenced by metabolic shifts unrelated to viability. [130] |
| Annexin V / Propidium Iodide (PI) | Distinguishes between early apoptosis (Annexin V+/PI-), late apoptosis/necrosis (Annexin V+/PI+), and live cells. [41] | Requires immediate analysis by flow cytometry. Necrotic cells will also be Annexin V+ due to membrane rupture. |
| Caspase-3/7 Activity Assays | Detects the activation of executioner caspases, providing specific evidence for apoptosis. [131] | A specific marker for apoptosis, but does not rule out concurrent other death modes. |
| LC3 Antibodies | Detects the conversion of LC3-I to lipidated LC3-II, a key marker of autophagosome formation. [131] | Should be combined with lysosomal inhibitors (e.g., chloroquine) to measure "autophagic flux," not just LC-II levels. |
| Lactate Dehydrogenase (LDH) Assay | Measures the release of cytosolic LDH upon loss of membrane integrity, indicating necrotic cell death or late-stage apoptosis. [130] | Provides a quantitative measure of cytotoxicity in the culture supernatant. |
| Hydroxypropyl Methylcellulose (HPMC) | A polymer used to create sustained-release drug formulations for in vitro testing, helping to model prolonged drug exposure. [132] | Allows for more physiologically relevant drug exposure kinetics compared to a single bolus. |
| Human Induced Pluripotent Stem Cells (iPSCs) | Provides a genetically defined, human-derived source of neurons, glia, and other cells for disease modeling. [129] | Essential for studying human-specific disease mechanisms and for patient-stratified drug testing. |
Advanced Model Systems: From 2D to Physiologically Complex Platforms
To enhance clinical relevance, consider moving beyond simple 2D cultures. The following advanced systems can provide critical insights:
- 3D Organoids: These self-organizing, 3D structures derived from stem cells can model human brain regions and other tissues. They preserve critical cell-cell interactions and can capture aspects of human disease pathology that are absent in animal models or cell lines. [129]
- Co-culture Systems: Culturing multiple cell types together (e.g., neurons with glial cells) is vital as it mimics the interactive microenvironment of tissues. For instance, inflammation driven by glial cells can modify or accelerate the progression of neurodegenerative diseases like Parkinson's. [129]
- Incorporating Blood-Brain Barrier (BBB) Models: For neuroscience research, integrating brain organoids with BBB mimics is crucial. The BBB actively regulates drug delivery to the CNS, and its impairment plays a key role in the pathogenesis of several diseases. [129]
Glioblastoma (GBM) organoids have emerged as transformative preclinical models that better recapitulate the complexity of human brain tumors compared to traditional 2D cultures or animal models. These 3D structures preserve tumor heterogeneity, cell-cell interactions, and key characteristics of the native tumor microenvironment [133] [134]. Within the context of cell death research, rigorous validation frameworks are essential, as inaccurate cell death quantification can lead to flawed conclusions about therapeutic efficacy and mechanisms of drug resistance. This case study establishes a technical support center to address the most pressing experimental challenges in GBM organoid research, with particular emphasis on validating cell death responses within these complex 3D systems.
GBM Organoid Model Selection: A Technical FAQ
Frequently Asked Questions
Q: What are the main types of GBM organoid models, and how do I choose? A: The choice of model depends heavily on your research question. The main established protocols include:
- Patient-Derived Organoids (PDOs): Generated directly from patient tumor tissue, preserving the original genetic and cellular heterogeneity [133] [135]. Ideal for personalized medicine approaches and drug screening that requires maintained tumor microenvironment (TME).
- GLIoma Cerebral Organoids (GLICO): Established by co-culturing patient-derived glioma stem cells (GSCs) with human cerebral organoids ("mini-brains"). This model excels in studying tumor invasion into healthy brain tissue [133] [136].
- Induced Pluripotent Stem Cell (iPSC)-Derived Organoids: Created by introducing common GBM mutations (e.g., in TP53, PTEN, NF1) into healthy iPSCs, which are then differentiated into cerebral organoids. This model allows for the study of tumorigenesis from the earliest stages in a controlled, genetically defined background [133] [137].
Q: Our organoids show poor viability after plating. What are the critical factors for success? A: Optimizing the extracellular matrix (ECM) and culture medium is crucial:
- ECM: Matrigel is widely used but has batch-to-batch variability. Consider synthetic hydrogels like gelatin methacrylate (GelMA) for improved reproducibility [138]. The stiffness and composition of the ECM can dramatically affect organoid growth and differentiation.
- Medium Composition: Use defined, serum-free media supplemented with specific growth factors. Common additives include B27, N2, EGF, and bFGF to maintain stemness and promote growth [133] [134]. Avoid serum, as it can induce differentiation and alter genomic profiles.
Troubleshooting Cell Death Assays in 3D Cultures
A primary challenge in transitioning from 2D to 3D models is adapting functional assays. The following table outlines common pitfalls and solutions for quantifying cell death in GBM organoids.
Table 1: Troubleshooting Cell Death Detection in GBM Organoids
| Problem | Potential Cause | Solution | Key References |
|---|---|---|---|
| High background in TUNEL staining | Non-specific DNA fragmentation from mechanical sectioning or necrosis. | Combine TUNEL with a specific apoptotic marker (e.g., cleaved caspase-3) to confirm apoptosis. Always include appropriate controls (e.g., DNase-treated for positive, no enzyme for negative). | [139] [140] |
| Weak or heterogeneous caspase activity | Poor reagent penetration into the organoid core; presence of both live, dying, and dead cells. | Use optimized organoid sectioning. For whole mounts, perform extended staining with gentle agitation. Validate with a second method (e.g., Western blot for cleaved caspases from organoid lysates). | [139] [136] |
| Inconclusive flow cytometry data (Annexin V/PI) | Incomplete dissociation of organoids into single cells; cell clustering affects instrument detection. | Use gentle, validated dissociation protocols (e.g., enzymatic with Accutase). Filter cells through a strainer before analysis. Always check cell viability post-dissociation. | [139] [141] |
| Discordance between viability and cell death assays | Assays measure different things (e.g., MTT measures metabolism, not direct death). Therapeutic agents may induce cytostasis without death. | Use multiple, methodologically unrelated assays to quantify cell death. Combine a viability assay (e.g., ATP-based) with a direct death assay (e.g., membrane integrity via propidium iodide). | [139] [140] |
| Failure to detect therapy-resistant cell populations | Assays might only capture the predominant death modality, missing minor subpopulations (e.g., autophagy-dependent or ferroptotic cells). | Employ a panel of assays targeting different death pathways (e.g., LC3 for autophagy, lipid peroxidation for ferroptosis). Use single-cell RNA sequencing on treated organoids to identify rare, resistant transcriptional states. | [139] [137] |
Experimental Protocol: A Multi-Method Approach to Quantifying Apoptosis
Given the challenges above, relying on a single method is insufficient. The following workflow is recommended for robust detection of apoptosis in GBM organoids treated with a chemotherapeutic agent (e.g., Temozolomide):
- Treatment and Processing: Treat LEGO or PDO models with the agent of interest. Include a positive control (e.g., Staurosporine) and vehicle control. After treatment, process organoids for either cryosectioning or whole-mount analysis.
- Immunofluorescence (on sections):
- Stain sections with antibodies against cleaved caspase-3 (a key executioner caspase) and γH2AX (a marker for DNA damage, often a precursor to apoptosis).
- Counterstain with a nuclear marker (e.g., DAPI).
- Quantify the percentage of cleaved caspase-3 positive cells per field of view using fluorescence microscopy and image analysis software.
- TUNEL Staining (on adjacent sections):
- Perform TUNEL staining to label DNA fragmentation.
- Co-stain with a cell-type-specific marker (e.g., SOX2 for stem-like cells) to identify which subsets of cells are undergoing death.
- Western Blot Analysis (from parallel organoid lysates):
- Analyze the expression of apoptosis-related proteins, such as the shift from pro-caspase to cleaved caspase-3, and the cleavage of PARP.
- This provides a bulk biochemical confirmation that complements the spatial information from staining.
- Data Integration: Correlate data from all methods. A strong apoptotic response will show concordance: increased cleaved caspase-3 by IF and WB, increased TUNEL+ cells, and morphological changes.
The Scientist's Toolkit: Essential Reagents and Materials
Success in GBM organoid research relies on a suite of specialized reagents. The table below details key components and their functions.
Table 2: Research Reagent Solutions for GBM Organoid Culture and Validation
| Category | Reagent/Material | Function/Application | Notes & Considerations |
|---|---|---|---|
| Culture Matrix | Matrigel | Provides a basement membrane extract for 3D growth; supports complex tissue organization. | High batch-to-batch variability. Pre-test lots for optimal organoid formation. [133] [134] |
| Synthetic Hydrogels (e.g., GelMA) | Defined, reproducible ECM alternative. Allows tuning of mechanical properties. | Improves experimental reproducibility and allows for customization. [133] [138] | |
| Growth Media Supplements | B27 & N2 Supplements | Provide essential hormones, proteins, and lipids for neural cell survival and growth. | Standard components for serum-free neural and GSC media. [133] [136] |
| EGF (Epidermal Growth Factor) & bFGF (Basic Fibroblast Growth Factor) | Mitogens that promote the proliferation and maintenance of glioma stem-like cells (GSCs). | Critical for maintaining the stem cell population in patient-derived cultures. [134] [136] | |
| Cell Death Assay Reagents | Recombinant Antibodies (Cleaved Caspase-3, PARP) | Specific detection of key apoptotic proteins via immunofluorescence or Western blot. | Confirm activation of the apoptotic execution pathway. [139] [140] |
| TUNEL Assay Kits | Fluorescent labeling of DNA strand breaks, a hallmark of late-stage apoptosis. | Can also label DNA damage from other processes; requires validation with other markers. [139] [140] | |
| Annexin V / Propidium Iodide (PI) | Flow cytometry-based discrimination of early apoptotic (Annexin V+/PI-) and late apoptotic/necrotic (Annexin V+/PI+) cells. | Requires high-quality single-cell suspension from organoids. [139] [141] | |
| Advanced Tools | CRISPR/Cas9 Systems | For genetic engineering of iPSCs to generate genetically defined LEGO models (e.g., knockout of TP53, PTEN, NF1). | Enables study of specific genetic contributions to tumorigenesis and therapy response. [137] [138] |
Advanced Applications: Integrating Organoids into Drug Discovery Pipelines
GBM organoids are proving invaluable in preclinical drug discovery, particularly for identifying patient-specific responses and tackling therapy resistance.
- Personalized Drug Screening: PDOs can be used to create biobanks, which are screened against a panel of therapies (e.g., standard chemotherapies, targeted inhibitors). This can predict a patient's response, as the organoids retain the genetic and phenotypic profile of the donor tumor [142] [135]. For instance, a GlioME model accurately predicted patient response to the MET inhibitor vebreltinib [135].
- Modeling the Immunosuppressive Niche: A major breakthrough is the development of immunocompetent organoids. These are co-cultured with autologous immune cells (e.g., tumor-infiltrating lymphocytes, macrophages) to study immunotherapy responses, such as immune checkpoint inhibitors (anti-PD-1) and CAR-T cell therapies [142] [138]. This allows researchers to dissect mechanisms of immune evasion within the human TME.
- Deciphering Metabolic Resistance: Multi-omics approaches (transcriptomics, metabolomics, lipidomics) on organoid models have identified glycerol lipid reprogramming as a hallmark of GBM. This has revealed new metabolic dependencies and potential drug targets that would be difficult to identify in 2D cultures [137].
The following diagram illustrates how different GBM organoid models integrate into a comprehensive drug discovery and validation workflow.
Conclusion
The precise understanding and control of cell death in culture is paramount for advancing biopharmaceutical production and biomedical research. This synthesis of foundational mechanisms, detection methodologies, inhibition strategies, and validation frameworks provides a powerful toolkit for improving cell culture viability and product yield. The integration of genetic engineering with optimized bioprocess conditions represents a cornerstone for enhancing industrial productivity. Future directions will likely involve the increased application of multi-omics technologies to discover novel regulatory nodes and the development of sophisticated, multiplexed biomarker panels for real-time monitoring. Ultimately, mastering cell death signaling pathways opens new frontiers for refining cancer therapeutics, regenerative medicine applications, and the manufacturing of complex biological drugs, solidifying its role as a critical discipline in translational science.
References
- 1. The Mechanisms of Regulated Cell Death - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10801515/]
- 2. Regulated cell death pathways and their roles in ... [https://www.nature.com/articles/s12276-023-01069-y]
- 3. Apoptosis - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK499821/]
- 4. Programmed cell death detection methods - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9308588/]
- 5. Recent advances in cell death [https://www.nature.com/articles/s12276-023-01083-0]
- 6. North America Apoptosis Assay Market Trends 2025–2034 [https://www.gminsights.com/industry-analysis/north-america-apoptosis-assay-market]
- 7. What's Killing My Cell Cultures? Troubleshooting ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/what-is-killing-my-cell-cultures-troubleshooting-cell-growth-issues.html]
- 8. Intrinsic and Extrinsic Pathways of Apoptosis [https://www.thermofisher.com/us/en/home/life-science/antibodies/antibodies-learning-center/antibodies-resource-library/cell-signaling-pathways/cellular-apoptosis-pathway.html]
- 9. Mechanisms of Cell Death: Apoptosis | Intrinsic & Extrinsic ... [https://blog.cellsignal.com/mechanisms-of-cell-death-apoptosis]
- 10. Cell Death Pathways [https://www.cellsignal.com/pathways/by-research-area/cell-death-pathways?srsltid=AfmBOoqwhWQnoVrORrJrQ1Kkxzgy_yVRN1Y6qkhrTBc2Gjx9Z2kqFP1q]
- 11. Apoptosis: A Comprehensive Overview of Signaling Pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592877/]
- 12. Caspases as master regulators of programmed cell death [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229594/]
- 13. Extrinsic apoptosis and necroptosis in telencephalic ... [https://www.nature.com/articles/s41418-025-01594-5]
- 14. Imaging of morphological and biochemical hallmarks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6851291/]
- 15. Designing an apoptosis reporter by mutagenesis-based ... [https://www.sciencedirect.com/science/article/pii/S2090123225004795]
- 16. Molecular mechanisms of cell death - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5864239/]
- 17. Research progress on morphology and mechanism of ... [https://www.nature.com/articles/s41419-024-06712-8]
- 18. Necroptosis as a Novel Facet of Mitotic Catastrophe - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8998610/]
- 19. Current and Emerging Biomarkers of Cell Death in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4052120/]
- 20. Inhibiting autophagy enhanced mitotic catastrophe ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383524000880]
- 21. Triggering mitotic catastrophe by podophyllotoxin induces ... [https://www.sciencedirect.com/science/article/pii/S0003996925002249]
- 22. Involvement of autophagy in the outcome of mitotic ... [https://www.nature.com/articles/s41598-017-14901-z]
- 23. Cell Death Response to Anti-mitotic Drug Treatment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5557680/]
- 24. Death through a tragedy: mitotic catastrophe [https://www.nature.com/articles/cdd200847]
- 25. Comprehensive landscape of cell death mechanisms [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1611055/full]
- 26. Time resolved cell painting enables rapid assessment of ... [https://pubmed.ncbi.nlm.nih.gov/40645587/]
- 27. A genome-wide atlas of human cell morphology [https://www.nature.com/articles/s41592-024-02537-7]
- 28. Genes-first and phenotypes-first paths to treatment ... [https://www.nature.com/articles/s41419-025-08127-5]
- 29. Toward generalizable phenotype prediction from single-cell ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-024-00014-3]
- 30. Investigating Nonapoptotic Cell Death Using Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7185180/]
- 31. Histology, Cell Death - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK526045/]
- 32. Cell death [https://www.sciencedirect.com/science/article/pii/S0092867423013326]
- 33. Cell Death and Inflammation Unit: A double-edged sword ... [https://belgian-research.eu/cell-death-and-inflammation-unit-a-double-edged-sword-in-health-and-disease/]
- 34. Navigating the biology of cell death [https://www.nature.com/articles/s41556-024-01515-7]
- 35. Triggering cell death in metastatic melanoma may pave the ... [https://hsph.harvard.edu/news/triggering-cell-death-in-metastatic-melanoma-may-pave-the-way-for-new-cancer-treatments/]
- 36. Cell Culture FAQs [https://lifescience.invitro.com.au/l/cell-culture-faqs]
- 37. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOor2awir91j4weH6XUX-iVFQEtfYkDqqrzvOboz7LhNc5bwtegrv]
- 38. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 39. Cell Culture Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols.html]
- 40. Noncoding RNAs in apoptosis: identification and function - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10393110/]
- 41. Cell death in culture: Molecular mechanisms, detections ... [https://www.sciencedirect.com/science/article/abs/pii/S1226086X20303609]
- 42. Cell Death Troubleshooting in Cell Culture [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-cell-death?srsltid=AfmBOopB3EmwP54KF1G6uJcd5_s9xuu517DnyNPfdiHNiWzO1U0wmFJT]
- 43. Circulating Biomarkers of Cell Death after treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2586103/]
- 44. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 45. Non-coding RNAs: emerging biomarkers and therapeutic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1534862/full]
- 46. Machine learning approaches for biomarker discovery to ... [https://www.nature.com/articles/s41598-023-42338-0]
- 47. Integrative analysis of programmed cell death pathways ... [https://jtd.amegroups.org/article/view/105971/html]
- 48. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOoq7fAJ4-kxoOr4tnB3x-gjUROFZQjgM8pVZVq1yuCIARhn9T7oq]
- 49. Flow Cytometry Protocol & Troubleshooting - Creative Biolabs [https://www.creativebiolabs.net/flow-cytometry.htm]
- 50. Flow Cytometry Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-analysis-support-center/flow-cytometry-support/flow-cytometry-support-troubleshooting.html]
- 51. From viability to cell death: Claims with insufficient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8863264/]
- 52. ELISA Troubleshooting Guide & Principles [https://www.bosterbio.com/protocol-and-troubleshooting/elisa-principle?srsltid=AfmBOooqxVEMWCW9E0PLStqm40MtdAg_CqJyrj6OYKcPkiOcQk3t4kUL]
- 53. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 54. Cell Death ELISA [https://bio-protocol.org/exchange/minidetail?id=10834456&type=30]
- 55. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 56. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 57. ELISA Assay Validation: Best Practices, Methods, and Key ... [https://www.nebiolab.com/elisa-assay-validation-guide/]
- 58. Development of an enzyme-linked immunosorbent assay ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1542898/full]
- 59. Common errors in manual ELISA assays and how ... [https://automata.tech/case-studies/common-errors-in-manual-elisa-assays-and-how-automation-can-help/]
- 60. Apoptosis DNA fragmentation analysis protocol [https://www.abcam.com/en-us/technical-resources/protocols/apoptosis-dna-fragmentation]
- 61. Common Problems and Solutions in TUNEL Assay for ... [https://www.arcegen.com/blogs/cell-anti-contamination-assembly/common-problems-and-solutions-in-tunel-assay-for-detecting-cell-apoptosis]
- 62. TUNEL Assays | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-viability-and-regulation/apoptosis/tunel-assays.html]
- 63. How Much Do You Know About TUNEL Staining? A ... - Yeasen [https://www.yeasenbio.com/blogs/cell/how-much-do-you-know-about-tunel-staining-a-troubleshooting-guide-for-abnormal-staining-results]
- 64. TUNEL protocol that preserves protein antigenicity for co [https://www.protocols.io/view/tunel-protocol-that-preserves-protein-antigenicity-ddus26we.html]
- 65. Harmonizing TUNEL with multiplexed iterative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146639/]
- 66. TUNEL FAQ and Solutions [https://www.linkedin.com/pulse/tunel-faq-solutions-elabscience]
- 67. Multiplex, high-throughput method to study cancer and ... [https://www.nature.com/articles/s42003-024-06327-x]
- 68. How to Identify Bad Flow Cytometry Data – Bad Data Part 1 [https://voices.uchicago.edu/ucflow/2020/09/30/how-to-identify-bad-flow-cytometry-data-part-1/]
- 69. The Graph Window - FlowJo Documentation [https://docs.flowjo.com/flowjo/graphs-and-gating/gw-overview/]
- 70. Flow Cytometry Support | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-analysis-support-center/flow-cytometry-support.html]
- 71. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 72. Osmotic Stress Response: Quantification of Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC444767/]
- 73. Sulfate depletion triggers overproduction of phospholipids ... [https://www.nature.com/articles/s41598-019-41233-x]
- 74. Deciphering the fate of osmotic stress priming on ... [https://www.sciencedirect.com/science/article/abs/pii/S0960852423000822]
- 75. Nutrient Supplementation Strategies for Biopharmaceutical ... [https://www.bioprocessintl.com/biochemicals-raw-materials/nutrient-supplementation-strategies-for-biopharmaceutical-production-part-2]
- 76. Exploring Principles of Bioreactor Scale-Up [https://www.bioprocessintl.com/bioreactors/lessons-in-bioreactor-scale-up-part-1-mdash-exploring-introductory-principles]
- 77. Advanced Bioreactor Technologies in Bioprocess Operations [https://www.mabion.eu/science-hub/articles/bioprocess-operation-modes-and-advanced-bioreactor-technology/]
- 78. Modeling Nutrient Consumptions in Large Flow-Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2730170/]
- 79. The BCL2 family: from apoptosis mechanisms to new ... [https://www.nature.com/articles/s41392-025-02176-0]
- 80. Multiple Functions of BCL-2 Family Proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3552500/]
- 81. Bcl-XL is qualitatively different from and ten times more ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1560389/]
- 82. Bcl-xL/Bcl-2 coordinately regulates apoptosis, cell cycle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC213787/]
- 83. BCL2 (NM_000633) Human Untagged Clone | SC125546 [https://www.origene.com/catalog/cdna-clones/expression-plasmids/sc125546-bcl2-nm-000633-human-untagged-clone]
- 84. Bcl-xL Antibody #2762 [https://www.cellsignal.com/products/primary-antibodies/bcl-xl-antibody/2762?srsltid=AfmBOooB-MvTHrKXBg-HY5vjw7rYXXxVPW_MnwrfX6tfHI65U9vyRgKF]
- 85. Anti-Bcl-XL antibody [2H12] (ab270253) [https://www.abcam.com/en-us/products/primary-antibodies/bcl-xl-antibody-2h12-ab270253]
- 86. Development of a BCL-xL and BCL-2 dual degrader with ... [https://www.nature.com/articles/s41467-021-27210-x]
- 87. Combination of microRNA and suicide gene for targeting ... [https://pubmed.ncbi.nlm.nih.gov/39286083/]
- 88. Beat the heat: need for research studying plant cell death ... [https://pubmed.ncbi.nlm.nih.gov/40035421/]
- 89. Intracellular regulation in response to environmental ... [https://www.sciencedirect.com/science/article/abs/pii/S030881462503362X]
- 90. Impact of Feeding Strategies on the Scalable Expansion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5031176/]
- 91. Market Size to Hit USD 20.23 Billion by 2034 Cell Culture Media [https://www.precedenceresearch.com/cell-culture-media-market]
- 92. Frontiers | A review of algorithmic approaches for cell ... culture media [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1195294/full]
- 93. Advanced technologies for the preservation of mammalian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8765766/]
- 94. Comparison of different freezing rates on post-thaw viability ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224025000094]
- 95. Cryopreservation - Key Survey Findings from the ISCT ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/05/28/cryopreservation-key-survey-findings-from-the-isct]
- 96. Cell Freezing Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 97. Improving Cell Recovery: Freezing and Thawing ... [https://www.mdpi.com/2073-4409/11/5/799]
- 98. Suspension Cell Culture Protocol [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/subculturing-suspension-cells.html]
- 99. The effects of cryopreservation on PBMCs transcriptome ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1690316/full]
- 100. 3D culture and cryopreservation/thawing strategy of human ... [https://www.sciencedirect.com/science/article/abs/pii/S2214552425000951]
- 101. Cell Seeding Essentials: Strategies for Lab Success [https://opentrons.com/applications/cell-seeding?srsltid=AfmBOopQX7BJ-jgwW9KLdhy_vCTwXuA6V3E0j9TYNpm61iUFRWk3ZCix]
- 102. Strategies to enhance stability of cryopreservation ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025002496]
- 103. 胰酶在细胞培养中的选择、使用与常见错误解析 [https://www.bhkbio.com/show/30550.html]
- 104. 胰蛋白酶细胞解离方案 [https://www.sigmaaldrich.com/HK/zh/technical-documents/protocol/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-dissociation-with-trypsin?srsltid=AfmBOopTLCtOYusrC6BR1sZj388-YHOemt7Iykj7qdNm1FYTMolwopSZ]
- 105. 细胞培养常见问题_细胞污染原因_解决方法 [https://www.detaibio.com/topics/cell-culture-faq.html]
- 106. 在研究细胞培养实验室中避免真菌和细菌污染的 ... [https://www.jove.com/cn/t/64769/cell-culture-techniques-practices-to-avoid-contamination-fungi]
- 107. 精确控制二氧化碳培养箱二氧化碳浓度:优化细胞培养的关键 [https://www.jqyiqi.com/news-detail/78.html]
- 108. 细胞培养设备| Thermo Fisher Scientific - CN - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/products-and-services/promotions/life-science/essential-to-cell-culture-workflow2.html]
- 109. Getting to the root of poor ELISA data reproducibility [https://www.tecan.com/blog/getting-to-the-root-of-poor-elisa-data-reproducibility]
- 110. ELISA Assay Qualification: Precision & Reproducibility Tips [https://www.cygnustechnologies.com/evaluating-precision-and-reproducibility-in-your-elisa?srsltid=AfmBOorJZVCQl2Epp1nV-77rJcjvmn2vPmXTYPGPeldvBrRlcz55p83x]
- 111. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 112. Comparison of Reproducibility, Accuracy, Sensitivity, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7499898/]
- 113. Regulation of ATP Release in Cell Death [May 6, 2025] [https://www.dojindo.com/contents/celldeath_sn20250506.html]
- 114. Different types of cell death and their shift in shaping disease [https://www.nature.com/articles/s41420-023-01581-0]
- 115. Necroptosis, pyroptosis and apoptosis: an intricate game of ... [https://www.nature.com/articles/s41423-020-00630-3]
- 116. Cell Death: Discriminating between apoptosis, necrosis & ... [https://www.ddw-online.com/cell-death-discriminating-between-apoptosis-necrosis-autophagy-946-201412/]
- 117. Insights on the crosstalk among different cell death ... [https://www.nature.com/articles/s41420-025-02328-9]
- 118. Types of Cell Death from a Molecular Perspective - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10669395/]
- 119. Diversity and complexity of cell death: a historical review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10474147/]
- 120. Therapeutic Targeting of Apoptosis, Autophagic Cell Death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293011/]
- 121. Crosstalk between apoptosis, necrosis and autophagy [https://www.sciencedirect.com/science/article/pii/S0167488913002243]
- 122. Protein Biomarker Signatures Outperform Single [https://protavio.com/protein-biomarker-signatures-outperform-single-markers-in-early-disease-detection/]
- 123. Biomarker panels may be superior over single molecules ... [https://pubmed.ncbi.nlm.nih.gov/32211780/]
- 124. Single-cell biology uncovers apoptotic cell death and its ... [https://pubmed.ncbi.nlm.nih.gov/35034369/]
- 125. A high-throughput microscopy method for single-cell ... [https://www.nature.com/articles/s42003-019-0282-0]
- 126. Predictive biomarkers of immunotherapy response with ... [https://www.nature.com/articles/s41401-023-01079-6]
- 127. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 128. The Importance of Predictive Biomarkers and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11429372/]
- 129. In vitro Models of Neurodegenerative Diseases [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00328/full]
- 130. From viability to cell death: Claims with insufficient evidence in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0250754]
- 131. Cell death in mammalian cell culture: molecular mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2932912/]
- 132. Physiologically Relevant In Vitro-In Vivo Correlation (IVIVC ... [https://www.mdpi.com/1999-4923/11/6/251]
- 133. Development of glioblastoma organoids and their applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10246443/]
- 134. Opportunities and challenges of glioma organoids [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-021-00777-0]
- 135. A novel organoid model retaining the glioma ... [https://www.sciencedirect.com/science/article/pii/S2452199X25003081]
- 136. Organoid Models of Glioblastoma and Their Role in Drug ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2021.605255/full]
- 137. A multidimensional atlas of human glioblastoma-like ... [https://www.nature.com/articles/s41698-024-00500-5]
- 138. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 139. Guidelines for Regulated Cell Death Assays: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7970050/]
- 140. Guidelines for the use and interpretation of assays ... [https://www.nature.com/articles/cdd200944]
- 141. Guidelines for the selection of functional assays to evaluate ... [https://www.sciencedirect.com/science/article/pii/S0304419X16300750]
- 142. Glioblastoma Organoids: Pre-Clinical Applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7753120/]