Combating Cell Culture Microbial Contamination: From Foundational Knowledge to Cutting-Edge Detection Strategies
This article provides a comprehensive guide for researchers and drug development professionals on managing microbial contamination in cell culture.
Combating Cell Culture Microbial Contamination: From Foundational Knowledge to Cutting-Edge Detection Strategies
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on managing microbial contamination in cell culture. It covers the foundational knowledge of common contaminants like bacteria, mycoplasma, and viruses, explores traditional and novel detection methodologies including machine learning-aided UV spectroscopy and VOC analysis, and offers practical troubleshooting and optimization strategies for both research and GMP environments. Furthermore, it discusses validation requirements and compares the efficacy of various detection techniques, concluding with future directions for ensuring the integrity and safety of cell-based products and research.
Understanding the Invisible Enemy: A Guide to Common Cell Culture Contaminants
Within the broader scope of research on microbial contamination in cell culture, bacterial contamination represents one of the most common and immediately detectable challenges. It can surreptitiously affect data quality, compromise experimental results, and lead to costly setbacks [1] [2]. For researchers, scientists, and drug development professionals, the ability to rapidly identify bacterial contamination through visual cues like turbidity and pH shifts is a fundamental skill for maintaining culture integrity. This guide provides targeted troubleshooting support for recognizing and addressing these specific contamination indicators.
FAQ: Turbidity and pH Shifts in Cell Culture
Q1: What are the primary visual signs of bacterial contamination in my cell culture? The most immediate signs are increased turbidity (a cloudy or hazy appearance) and a sharp drop in the pH of the medium, often indicated by a color change to yellow [1] [3] [4]. This occurs because bacteria metabolize nutrients and produce acidic byproducts. Under a low-power microscope, you may observe tiny, shimmering granules moving between your cells [4].
Q2: Why does the pH of my culture medium drop suddenly? A sudden pH drop is a metabolic signature of bacterial contamination. Bacteria consume nutrients in the medium, such as glucose, and produce acidic waste products like lactic acid. Most cell culture media contain phenol red, a pH indicator that turns yellow under acidic conditions, providing a visible alert [3] [4].
Q3: I see turbidity, but my cells still look okay. Should I be concerned? Yes, you should treat this as a confirmed contamination. Bacterial growth can be incredibly rapid. Even if your cells appear unaffected initially, the bacteria will eventually outcompete them for nutrients, release toxic waste, and lead to cell death. It is recommended to discard the culture promptly to prevent spread [5] [4].
Q4: How can I distinguish bacterial contamination from other types, like yeast or fungi? While all can cause turbidity, the specifics differ. Yeast appears as individual ovoid or spherical particles that may bud off smaller particles, and pH may only increase with heavy contamination [5] [4]. Fungi present as thin, wispy filamentous mycelia or clumps of spores [5] [4]. Bacteria, in contrast, typically cause a rapid pH drop and under the microscope appear as tiny, moving rods or cocci [1] [4].
Q5: What are the most common sources of bacterial contamination? Contamination can originate from multiple sources, including lab personnel, unfiltered air, non-sterile reagents or media, humidified incubators, and unsterilized equipment like biosafety cabinets [1].
Troubleshooting Guide: Data and Detection
Characteristic Signs of Common Contaminants
The table below summarizes the key characteristics to help differentiate between major types of biological contaminants.
Table 1: Identification Guide for Common Cell Culture Contaminants
| Contaminant | Visual Culture Appearance | Microscopic Observation (100–400x) | Typical pH Change |
|---|---|---|---|
| Bacteria | Cloudy (turbid) medium; possibly a thin film on the surface [4] | Tiny, shimmering granules; rods or cocci may be observed [5] [4] | Sharp drop (acidic) [1] [5] |
| Yeast | Cloudy medium, especially in advanced stages [4] | Round or ovoid particles that bud off smaller particles [5] [4] | Stable initially, then may increase with heavy infection [5] [4] |
| Fungi/Mold | Cloudy medium; floating clumps [2] | Thin filamentous mycelia; sometimes clumps of spores [5] [4] | Changes sometimes; can be stable [5] |
| Mycoplasma | No turbidity; no obvious visual signs [3] [5] | Not detectable by routine microscopy; requires DNA staining (e.g., Hoechst) or PCR [1] [3] | No consistent change [5] |
A robust contamination control program employs a variety of detection methods, chosen based on the suspected contaminant.
Table 2: Overview of Microbial Contamination Detection Methods
| Detection Method | Primary Use | Brief Protocol Overview | Key Advantage |
|---|---|---|---|
| Visual & Microscopic Inspection | Routine monitoring for bacteria, yeast, fungi [2] | Daily observation of culture clarity and color. Examine under phase-contrast microscope for foreign particles or structures [3]. | Rapid, low-cost, first line of defense [6] |
| Microbial Culture | Detecting cultivable bacteria, yeast, and fungi [1] | Inoculate a sample of the cell culture into nutrient broth or agar and incubate for 1-3 days to observe for microbial growth [1]. | Confirms viability of contaminants |
| PCR (Polymerase Chain Reaction) | Detecting mycoplasma, viruses, and specific pathogens [1] [2] | Extract nucleic acids from the cell culture or supernatant and use target-specific primers to amplify unique microbial DNA/RNA sequences [1] [3]. | Highly sensitive and specific; detects non-cultivable organisms [1] |
| DNA Staining (e.g., Hoechst) | Detecting mycoplasma and viral plaques [1] [3] | Stain fixed cells with a fluorescent DNA-binding dye (e.g., Hoechst 33258) and examine under a fluorescence microscope for particulate or filamentous staining outside the cell nuclei [3] [5]. | Visual confirmation of mycoplasma DNA [5] |
| ELISA (Enzyme-Linked Immunosorbent Assay) | Detecting viral antigens or endotoxins [2] | Use antibodies immobilized on a plate to capture specific viral antigens or endotoxins from a sample, followed by detection with an enzyme-linked antibody and a colorimetric substrate [2]. | Can screen for specific viruses and toxins |
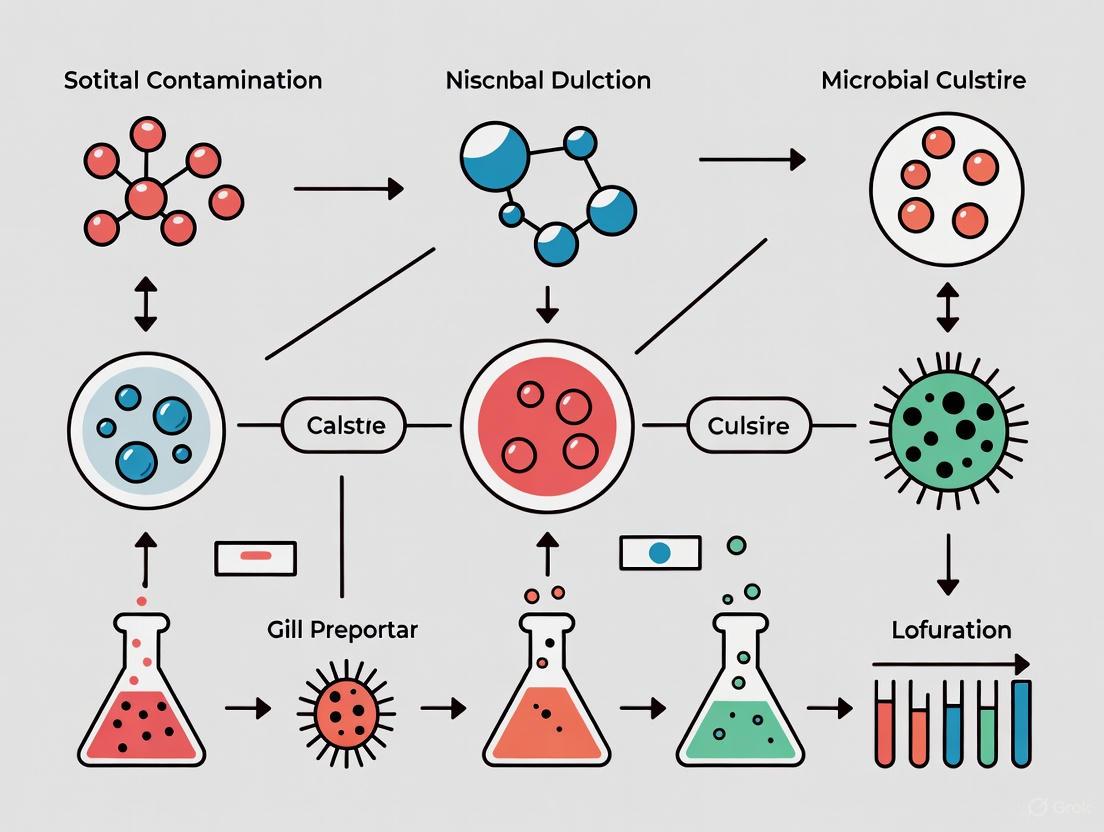
Visual Workflow: From Detection to Action
The following diagram outlines the logical decision-making process for addressing suspected bacterial contamination.
Essential Research Reagent Solutions
The table below lists key reagents and materials critical for both preventing contamination and conducting detection experiments.
Table 3: Key Reagents and Materials for Contamination Control
| Item | Function/Application | Key Considerations |
|---|---|---|
| 70% Ethanol | Surface and glove disinfection in the BSC and lab [1] [7] | Effective concentration for microbial kill; evaporates quickly without residue [7]. |
| Phenol Red Medium | Visual pH indicator for culture health [3] | Yellow color indicates acidic shift (potential bacterial growth); pink indicates alkaline shift [3] [4]. |
| Antibiotics/Antimycotics | Suppression of microbial growth (e.g., Penicillin/Streptomycin) [1] [4] | Use strategically, not routinely, to avoid masking low-level contamination and breeding resistance [2] [4]. |
| Sterile Filtration Units (0.22 µm) | Sterilization of heat-sensitive solutions [1] | Standard pore size for removing bacteria; not effective for mycoplasma (<0.1 µm required) [1] [3]. |
| Hoechst 33258 Stain | Fluorescent detection of mycoplasma DNA [1] [5] | Requires fluorescence microscopy; reveals mycoplasma as particulate or filamentous staining outside cell nuclei [3] [5]. |
| PCR Kits for Mycoplasma | Highly sensitive detection of mycoplasma DNA [1] [3] | More sensitive than staining; available as a service from many cell banks and testing companies [3] [6]. |
Proactive Prevention Strategy
Preventing contamination is far more efficient than dealing with its consequences. A multi-layered defense strategy is most effective.
The most critical element in combating all cell culture contamination, including bacterial, remains consistent and meticulous aseptic technique [1]. Those techniques—combined with the strategic use of antibiotics, proper cell repository management, and a robust contamination monitoring program—form the cornerstone of reliable and reproducible cell culture research [1].
Mycoplasma contamination represents one of the most significant yet frequently overlooked problems in cell culture laboratories worldwide. These stealthy contaminants are the smallest and simplest self-replicating prokaryotes, lacking a cell wall and possessing a minimal genome of approximately 580-1358 kb [8]. Their small size (0.3-0.8 μm in diameter) allows them to readily pass through standard 0.22 μm filters used for sterilizing cell culture media [9]. Unlike bacterial contamination that often causes turbidity in media, mycoplasma contamination typically doesn't trigger visible changes, meaning most contaminated cultures show no obvious signs of infection [10] [11]. This invisible nature, combined with their resistance to common antibiotics like penicillin and streptomycin, makes them a persistent threat to research integrity [9] [12].
The incidence of mycoplasma contamination in continuous cell cultures is alarmingly high, estimated to affect 15-35% of cell lines, with primary cell cultures exhibiting at least a 1% contamination rate [12]. More than 200 mycoplasma species have been identified, but only about 20 species of human, bovine, and porcine origin typically contaminate cell cultures [9] [12]. A mere eight species account for approximately 95% of all contamination incidents: M. arginini (bovine), M. fermentans (human), M. hominis (human), M. hyorhinis (porcine), M. orale (human), M. pirum (human), M. salivarium (human), and Acholeplasma laidlawii (bovine) [12].
Detection and Diagnosis: Identifying the Contaminant
Why Routine Detection is Challenging
Mycoplasma contamination rarely produces the dramatic visual changes associated with other microbial contaminants. However, careful observation can reveal subtle indicators that should trigger formal testing:
- Reduced cell proliferation rates due to competition for nutrients with mycoplasmas [10]
- Cell aggregation and morphological changes in previously uniform cultures [10]
- Poor transfection efficiencies in cells that previously showed high transfection rates [10]
- Interference with biochemical assays including MTT tetrazolium dye-based cytotoxicity assays [13]
Available Detection Methods
Multiple methods are available for mycoplasma detection, each with advantages and limitations. The table below summarizes the most commonly used techniques:
Table 1: Comparison of Mycoplasma Detection Methods
| Method | Principle | Time to Result | Sensitivity | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Microbiological Culture | Growth on selective agar/broth media | 4-5 weeks [12] | Moderate | Detects only cultivable mycoplasmas [8] | Long incubation period [8] |
| DNA Staining (DAPI/Hoechst) | Fluorescent dyes bind to mycoplasma DNA | 1-3 days [8] | Moderate to High | Visual confirmation possible | Requires indicator cells [8] |
| PCR-Based Methods | Amplification of mycoplasma-specific DNA sequences | Several hours [9] [14] | High (~10 CFU/mL) [14] | Rapid and sensitive | Detects DNA from non-viable organisms |
| Enzymatic Labeling | Incorporation of modified nucleotides into mycoplasma DNA | Several hours [8] | High | Does not intensely stain nuclear DNA [8] | Newer, less established method |
| RPA-CRISPR/Cas12a | Isothermal amplification with CRISPR-based detection | <1 hour [15] | Very High (0.1-10 copies/μL) [15] | Extreme sensitivity and speed | Requires specialized reagents |
Recommended PCR Protocol for Detection
For most laboratories, PCR-based methods offer the optimal balance of speed, sensitivity, and practicality. The following protocol adapted from current research provides reliable detection:
Sample Preparation:
- Transfer 200 μL of cell culture supernatant (after at least 12 hours of cell culture) to a sterile 1.5 mL tube
- Incubate at 95°C for 5 minutes to release DNA
- Samples can be stored at 2-8°C for up to one week or at -20°C for several months [9]
PCR Reaction Setup:
- Use universal primers targeting the 16S rRNA gene:
- Forward: 5'-GGGAGCAAACAGGATTAGTATCCCT-3'
- Reverse: 5'-TGCACCATCTGTCACTCTGTTAACCTC-3' [9]
- Employ a touchdown PCR protocol to increase sensitivity and specificity
- Include appropriate positive and negative controls
Thermocycling Conditions:
- Initial denaturation: 94°C for 2 minutes
- 35-40 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing: 55-65°C for 30 seconds (temperature varies by protocol)
- Extension: 72°C for 1 minute
- Final extension: 72°C for 5 minutes
Result Analysis:
- Analyze PCR products by gel electrophoresis on 1.5% agarose-TAE gel
- Visualize with appropriate DNA staining
- Expected product size varies by species but typically ranges from 500-1000 bp
Troubleshooting Guide: Frequently Asked Questions
Q: My cell culture isn't showing visible contamination, but cell growth has slowed significantly and experiments are yielding inconsistent results. Could this be mycoplasma contamination?
A: Yes, these are classic signs of mycoplasma contamination. Unlike bacterial contamination that often causes turbidity or pH changes, mycoplasma contamination manifests through more subtle effects including reduced cell proliferation rates, changes in cellular metabolism, and inconsistent experimental results [10] [11]. We recommend implementing routine PCR-based testing every 2-4 weeks or whenever introducing new cell lines.
Q: I've confirmed mycoplasma contamination in my prized cell line that would be extremely difficult to replace. Is eradication possible?
A: While complete elimination is challenging, several approaches can be attempted for irreplaceable cell lines:
- Antibiotic treatments specifically targeting mycoplasma (different from standard penicillin/streptomycin)
- Mycoplasma removal agents available commercially
- Passage through mice for certain cell types
- Limiting dilution cloning to isolate uncontaminated subpopulations
However, prevention remains vastly superior to treatment, as eradication success rates vary and may alter cell characteristics [16] [11].
Q: How does mycoplasma contamination affect specialized techniques like ATAC-seq and RNA-seq?
A: Mycoplasma contamination significantly compromises epigenetic and transcriptomic studies:
- ATAC-seq results are particularly vulnerable as the method employs Tn5 transposase to detect chromatin accessibility on a genome-wide scale, which is substantially affected by mycoplasma DNA [9]
- RNA-seq samples can be partially protected through poly(A) enrichment of RNA, but contamination still poses significant risks [9]
- Gene expression profiles become unreliable as mycoplasma infection can dysregulate hundreds of host genes [9]
Q: What are the most common sources of mycoplasma contamination in research laboratories?
A: Primary contamination sources include:
- Contaminated cell lines received from other laboratories (most common)
- Laboratory personnel through poor aseptic technique
- Contaminated reagents of animal origin, particularly serum
- Contaminated equipment shared between cell lines
- Environmental sources in laboratories with inadequate airflow control [11] [12]
Mycoplasma Interference with Cellular Metabolism and Signaling
Mycoplasma contamination exerts profound effects on cellular functions through multiple mechanisms, primarily by competing for essential nutrients and altering metabolic pathways. The diagram below illustrates key metabolic pathways disrupted by mycoplasma contamination:
Liquid chromatography mass spectrometry (LC/MS)-based metabolomics studies have demonstrated that mycoplasma contamination induces significant metabolic changes in infected cells. Research using PANC-1 human pancreatic carcinoma cells identified 23 significantly altered metabolites involved in three primary pathways [13]:
Table 2: Metabolic Pathways Affected by Mycoplasma Contamination
| Affected Pathway | Specific Alterations | Functional Consequences |
|---|---|---|
| Arginine Metabolism | Depletion of arginine, accumulation of ornithine and urea | Disruption of nitric oxide synthesis, polyamine metabolism, and protein synthesis [13] |
| Purine Metabolism | Changes in adenosine, inosine, hypoxanthine, and adenine levels | Alteration of DNA/RNA synthesis, energy transfer, and signaling pathways [13] |
| Energy Metabolism | Disruption of TCA cycle intermediates (succinate, fumarate, malate) | Compromised mitochondrial function and cellular energy production [13] |
| Choline Metabolism | Depletion of choline and phosphocholine | Impacts membrane integrity and cell signaling [13] |
These metabolic disruptions explain many observed phenotypic effects of mycoplasma contamination, including:
- Chromosomal aberrations and disruption of nucleic acid synthesis [12]
- Changes in membrane antigenicity and receptor expression [12]
- Inhibition of cell proliferation and metabolic activity [12]
- Altered response to chemotherapeutic agents in cancer cell lines [11]
- Modulation of immune cell functions including cytokine production and lymphocyte activation [8]
Prevention Protocols: Building a Contamination Defense System
Preventing mycoplasma contamination requires a systematic, multi-layered approach. The following evidence-based practices significantly reduce contamination risk:
Laboratory Practice Controls
- Strict aseptic technique: Always wear appropriate personal protective equipment (PPE) including gloves and lab coat. Change lab coats at least weekly [9]
- Biosafety cabinet maintenance: Keep culture hoods clean and well-organized, ensuring unobstructed airflow. Disinfect all items with 75% alcohol before placing in hood [9]
- Proper container management: Ensure adequate covering of plates and bottles at all times [9]
- Spill management: Clean spills immediately to prevent aerosol contamination [9]
Cell Culture Management
- Quarantine all new cell lines: Isolate untested cell lines in a designated incubator until confirmed mycoplasma-free [9] [11]
- Implement cell banking: Adhere to the seed stock principle to ensure availability of fresh, uncontaminated stocks [12]
- Regular incubator maintenance: Disinfect incubators regularly with bleach, change water in humidifying pans weekly [9]
- Avoid antibiotic overuse: Recognize that standard antibiotics don't prevent mycoplasma contamination and may mask problems [12]
Quality Control Measures
- Routine testing schedule: Test cell lines every 2-4 weeks using PCR-based methods
- Reagent qualification: Use only mycoplasma-free media, sera, and reagents from qualified suppliers [12]
- Personnel training: Ensure all laboratory staff receive proper training in aseptic technique and contamination prevention
Research Reagent Solutions: Essential Tools for Contamination Management
Table 3: Key Reagents for Mycoplasma Detection and Prevention
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| PCR Detection Kits | MycoSEQ Mycoplasma Detection Kits [14] | qPCR-based detection with TaqMan chemistry | Meets regulatory sensitivity requirements (10 CFU/mL) [14] |
| Culture Media | PPLO broth [8] | Selective cultivation of mycoplasmas | Requires supplementation with serum and specific nutrients [8] |
| DNA Staining Dyes | DAPI, Hoechst 33258 [8] [12] | Fluorescent staining of mycoplasma DNA | Often requires indicator cell lines for sufficient sensitivity [8] |
| Specialized Media Supplements | Horse serum, yeast extract, L-arginine [8] | Support mycoplasma growth in culture media | Essential for microbiological culture methods [8] |
| Antibiotic/Antimycotic Solutions | Zell Shield [9] | Prevention of bacterial and fungal contamination | Note: Most standard antibiotics are ineffective against mycoplasma [9] |
| Rapid Test Kits | MycoStrip [9] | Quick detection of mycoplasma contamination | Useful for regular screening without specialized equipment |
| Mycoplasma Removal Agents | Specific antibiotics targeting mycoplasma | Elimination of contamination from valuable cultures | Success rates vary; may alter cell characteristics |
Mycoplasma contamination remains a persistent, invisible threat that compromises cellular functions and jeopardizes research validity. The stealthy nature of these contaminants, combined with their profound effects on cellular metabolism, gene expression, and experimental outcomes, necessitates rigorous detection and prevention protocols. By implementing regular testing schedules, adhering to strict aseptic techniques, quarantining new cell lines, and maintaining proper laboratory hygiene, researchers can protect their valuable cell cultures and ensure the reliability of their scientific data. Remember: when it comes to mycoplasma contamination, vigilance is not optional—it's essential for research integrity.
Troubleshooting Guides
Guide 1: How do I identify a fungal or yeast contamination in my cell culture?
Problem: Suspected microbial contamination causing cloudy media or unusual pH shifts in cell culture.
Solution: A combination of macroscopic observation, microscopic analysis, and advanced detection techniques can confirm and identify the contaminant.
Step-by-Step Identification Protocol:
Macroscopic Observation: Visually inspect the culture medium.
- Turbidity: Look for an increase in turbidity (cloudiness) in the medium. This is a common sign of microbial growth [17] [4].
- pH Changes: Note any changes in the color of the medium if it contains phenol red as a pH indicator. Bacterial contamination often causes a rapid yellow shift (acidification), while yeast contamination may show little to no color change in the initial stages, with the pH usually increasing only in advanced stages [17] [4].
Microscopic Analysis:
- Use an inverted phase-contrast microscope for examination [17].
- Magnification: Observe at 100x to 400x magnification [17].
- Visual Identification:
- Yeasts: Appear as single, ovoid, or spherical particles. You may observe them budding off smaller particles. They can exist as single cells or in chains [17] [4].
- Molds: Appear as thin, filamentous structures (hyphae). These may appear as wispy filaments or denser clumps of spores (mycelia) under the microscope [4].
Advanced and Rapid Detection Methods: For faster, more sensitive, or automated detection, consider these emerging technologies:
- UV Absorbance Spectroscopy with Machine Learning: A novel, label-free method that uses ultraviolet light absorbance patterns of cell culture fluids and machine learning to provide a definitive contamination assessment within 30 minutes [18].
- Electronic Nose (e-nose): A sensor-based device that can detect and identify fungal contamination by analyzing the profile of volatile organic compounds (MVOCs) released by microbes in the headspace of a sample [19].
- Microfluidic Systems: Integrated systems capable of enriching and detecting specific airborne fungal spores (e.g., Aspergillus niger) through immunofluorescence analysis within 2-3 hours [20].
Interpretation of Results: The table below summarizes the key characteristics to differentiate common contaminants.
Table 1: Identifying Common Biological Contaminants in Cell Culture
| Contaminant Type | Macroscopic Signs | Microscopic Morphology | Typical pH Change |
|---|---|---|---|
| Yeast [17] [4] | Cloudy (turbid) medium | Ovoid or spherical particles, often budding | Stable initially, increases later |
| Mold [4] | Cloudy medium, sometimes with floating films | Thin, wispy filaments (hyphae) | Stable initially, increases later |
| Bacteria [4] | Cloudy medium, thin surface film | Tiny, moving granules (rods, cocci) | Rapid decrease (acidification) |
Guide 2: What are the best practices to prevent airborne fungal and yeast contamination?
Problem: Recurring contamination incidents are compromising experimental results and cell line integrity.
Solution: Implement a rigorous aseptic technique protocol and maintain a clean laboratory environment.
Prevention and Contamination Control Protocol:
Personal Protective Equipment (PPE) and Aseptic Zone:
Proper Use of Cell Culture Hood:
- Wipe down all surfaces of the hood with 70% ethanol or IMS before and after every use [21].
- Do not block the front and rear grilles to ensure proper airflow [21].
- Work with all materials and containers within a clean, uncluttered workspace inside the hood, not near the edges [21].
- Use UV light to sterilize the hood when not in use [21].
Laboratory and Equipment Hygiene:
- Incubators: Clean and disinfect incubators regularly according to the manufacturer's protocol. Change the water in humidifying trays frequently and add a microbiostatic agent [21].
- Water Baths: Change the water in water baths used for warming media regularly and treat it to prevent microbial growth [21].
- Reagents and Labware: Use only sterile, certified reagents and materials. Aliquot reagents to avoid contaminating entire stocks. Sterilize labware via autoclaving where appropriate [21].
Antibiotic and Antimycotic Use:
- Note: Antibiotics and antimycotics should not be used routinely as a substitute for good aseptic technique. Their continuous use can lead to resistant strains and mask cryptic contaminants like mycoplasma [4].
- If used, they should be for short-term applications only, and antibiotic-free cultures should be maintained in parallel as a control [4].
Diagram: Contamination Prevention and Response Workflow
Frequently Asked Questions (FAQs)
Q1: My cell culture looks cloudy, but I see no bacteria or yeast under the microscope. What could it be? A1: Cloudy culture in the absence of visible bacteria or yeast can indicate contamination with mycoplasma [4]. These are very small bacteria that lack a cell wall and are extremely difficult to detect with standard microscopy. You should test your culture using specialized methods such as PCR, immunostaining, or commercial mycoplasma detection kits.
Q2: I've identified a contamination. Can I save my irreplaceable cell line with antibiotics? A2: It is possible to attempt decontamination, but success is not guaranteed and carries risks. The process involves [4]:
- Isolating the contaminated culture.
- Determining the toxicity level of a high-concentration antibiotic/antimycotic to your specific cell line.
- Treating the culture for 2-3 passages at a concentration just below the toxic level.
- Culturing the cells in antibiotic-free medium for several passages to verify the contamination has been eliminated. However, the use of antibiotics can induce cellular stress and alter cell physiology, potentially compromising future experimental results. Cryopreserving a clean stock is always preferable to decontamination.
Q3: What are the common sources of fungal and yeast contamination in a lab? A3: These contaminants are ubiquitous in the environment. Common sources include [19] [21]:
- Air: Unfiltered air handling systems or drafts can introduce spores.
- Personnel: Skin, hair, and clothing.
- Surfaces: Non-sterile workbenches, incubators, and water baths.
- Reagents: Non-sterile media, sera, or other supplements.
Q4: Are there any rapid, modern methods for detecting contamination beyond the microscope? A4: Yes, the field is advancing rapidly. Two promising methods are:
- Machine Learning with UV Spectroscopy: This method analyzes the UV light "fingerprint" of the cell culture fluid and can provide a yes/no contamination result in under 30 minutes, enabling early detection during manufacturing [18].
- Electronic Nose (e-nose): This device uses an array of gas sensors to detect volatile organic compounds (MVOCs) produced by microbes, allowing for early identification of fungal genus without lengthy culture steps [19].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Reagents for Contamination Management
| Item | Function / Application | Technical Notes |
|---|---|---|
| Phase-Contrast Microscope [17] | Visualization of live cells and contaminants (yeast, molds) without staining. | Essential for routine monitoring. Magnification of 100x-400x is sufficient for initial detection. |
| 70% Ethanol / IMS [21] | Surface and equipment decontamination within the cell culture hood and laboratory. | The water content in 70% solution increases efficacy against bacteria and viruses. |
| Antibiotic/Antimycotic Solutions [4] | Suppression of microbial growth in cell cultures. | Use as a last resort, not routinely. Determine optimal (non-toxic) concentration empirically for your cell line. |
| UV Absorbance Spectrometer [18] | Core component of a rapid, machine learning-based detection system for contamination. | Enables label-free, non-invasive, and real-time analysis of culture sterility. |
| Electronic Nose (MOS Gas Sensor Array) [19] | Early detection and identification of fungal contamination by analyzing MVOC profiles. | Useful for environmental monitoring of labs and incubators, as well as sample analysis. |
| Microfluidic Immunoassay System [20] | Rapid, high-throughput detection and enrichment of specific airborne pathogenic spores. | Provides targeted analysis; whole process can be completed in 2-3 hours. |
Viral contamination represents a unique and formidable challenge in cell culture. Unlike bacterial or fungal contamination, which often present visible signs, viral contaminants are silent, intracellular threats that can compromise research integrity and product safety without obvious warning [22] [23]. This guide provides troubleshooting and FAQs to help researchers navigate these hidden risks.
Troubleshooting Guides
FAQ: Detection and Identification
Q: How can I detect a viral contaminant that isn't causing visible cell death? Many viruses, particularly retroviruses, establish chronic infections without cytopathic effects [11]. Detection requires specific methods beyond routine microscopy:
- PCR assays: Effective for known viruses like Epstein-Barr virus (EBV) [24]
- Broad-spectrum methods: In vitro virus assays using multiple detector cell lines can identify contaminants through cytopathic effects, hemadsorption, or immunofluorescence [25]
- Next-generation sequencing (NGS): Powerful for detecting unknown adventitious agents without prior selection of nucleic acids [25]
Q: What are the most common sources of viral contamination in cell culture? Contamination typically originates from three primary sources [22]:
- Original tissues/tumor material: Primary cultures may harbor latent viruses from the donor organism [26]
- Biological reagents: Animal-derived components like fetal bovine serum and trypsin are frequent contamination vectors [25] [26]
- Cross-contamination: Between cell lines or through laboratory personnel [27]
Q: Which viruses should I be most concerned about in my cell cultures? Risk profiles vary by cell type, but prevalent contaminants include:
- Minute Virus of Mice (MVM): Particularly problematic in CHO cell cultures, resistant to inactivation [25]
- Epstein-Barr Virus (EBV): Ubiquitous in human populations, potentially latent in human-derived cell lines [24]
- Retroviruses: Can silently integrate as proviruses into host genomes [22]
- Ovine Herpesvirus 2 (OvHV-2): Broad species tropism, concerning for laboratories using diverse animal models [24]
FAQ: Prevention and Risk Mitigation
Q: What is the most effective strategy for preventing viral contamination? A comprehensive, multi-layered approach is essential [25]:
- Rigorous sourcing: Obtain cell lines from reputable banks that provide viral testing certification
- Raw material control: Use gamma-irradiated serum and animal-free reagents when possible
- Process design: Implement multiple orthogonal viral clearance steps in downstream processing
Q: Can I use antibiotics to prevent viral contamination? No. Antibiotics are ineffective against viruses, though they may control bacterial and mycoplasma contaminants [23] [28].
Experimental Protocols & Data Presentation
Viral Detection Workflow
The following diagram outlines a comprehensive strategy for detecting viral contaminants in cell cultures:
Essential Detection Methods
Table: Viral Detection Method Comparison
| Method | Principle | Applications | Sensitivity | Limitations |
|---|---|---|---|---|
| PCR/RT-PCR | Amplification of viral nucleic acid sequences | Detection of specific known viruses (e.g., EBV, MVM) | High for targeted viruses | Only detects pre-defined targets; misses novel viruses |
| In Vitro Virus Assay | Inoculation onto multiple detector cell lines; observation for CPE, hemadsorption | Broad detection of viruses capable of growing in tissue culture | Variable; depends on virus and cell line permissivity | Not all viruses produce CPE; limited detector cell range |
| Next-Generation Sequencing | Unbiased sequencing of all nucleic acids in sample | Detection of unknown adventitious agents; no prior selection | High with sufficient depth | Requires specialized resources and bioinformatics expertise |
| Electron Microscopy | Direct visualization of virus particles in samples | Detection of intracellular viruses; no amplification needed | ~10^6 particles/mL | Lower sensitivity; requires specialized equipment |
| In Vivo Assay | Injection into suckling mice, embryonated eggs | Detection of viruses that don't grow well in tissue culture | Variable | Ethical concerns; decreasing regulatory acceptance |
Viral Risk Mitigation Strategy
The following diagram illustrates the three complementary approaches to viral risk mitigation in bioprocessing:
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Reagents for Viral Contamination Management
| Reagent/Supply | Function | Application Notes |
|---|---|---|
| Gamma-Irradiated Fetal Bovine Serum | Cell culture supplement | Viral inactivation through irradiation; superior to heat-inactivated only [27] |
| PCR/RT-PCR Kits | Viral nucleic acid detection | Target specific contaminants (e.g., EBV, MVM); validate sensitivity for your application [25] |
| Next-Generation Sequencing Kits | Unbiased detection of adventitious agents | Comprehensive contaminant screening; requires bioinformatics support [25] |
| Viral Filtration Systems | Physical removal of viral particles | Nanofilters (≤20 nm) for parvovirus removal; validate for specific process [25] |
| Mycoplasma Testing Kits | Detection of common co-contaminants | PCR-based or Hoechst stain methods; mycoplasma increases vulnerability to viral infection [23] |
| Animal-Free Recombinant Trypsin | Cell passage and subculturing | Eliminates risk of animal-derived viral contaminants present in porcine trypsin [27] |
| Certified Cell Culture Media | Nutrient supply without contaminants | Low-endotoxin, certified composition reduces variable introduction [23] |
Troubleshooting Guides
How do I identify and address chemical contamination in my cell cultures?
Problem: Unexplained changes in cell health or erratic experimental results, potentially caused by non-biological contaminants.
Solution: Chemical contamination arises from non-living substances that interfere with cell processes. Common sources include impurities in water, media, sera, disinfectant residues, and plasticizers leaching from equipment [4] [29] [30].
Detection and Diagnosis:
- Observe Cell Behavior: Look for signs of acute toxicity, such as slow growth, vacuole appearance, sloughing, decrease in confluency, and cell rounding [4].
- Identify the Source: Systematically review and replace reagents like media, water, and serum one at a time to isolate the contaminated component [29].
- Test for Endotoxins: Use a Limulus Amebocyte Lysate (LAL) assay to detect endotoxins, which can significantly affect cell metabolism. Always source media and sera from suppliers that provide endotoxin testing certification [29].
Corrective Action:
- Discard Contaminated Reagents: Immediately dispose of any suspected reagents [29].
- Use High-Quality Water: Always use laboratory-grade water for preparing buffers and media [29].
- Thoroughly Rinse Labware: Ensure all reusable glassware and equipment are thoroughly rinsed and air-dried to remove detergent or disinfectant residues, as autoclaving does not eliminate these chemicals [29].
My cell lines are not behaving as expected; could they be cross-contaminated?
Problem: Inconsistent experimental data or unexpected morphological changes in a cell culture, potentially due to misidentification or overgrowth by another cell line.
Solution: Cross-contamination is a serious, often undetected problem. One study found over 15% of cell culture studies use misidentified or cross-contaminated cell lines [31].
Detection and Diagnosis:
- Routine Authentication: Implement mandatory cell line authentication using methods like Short Tandem Repeat (STR) profiling, karyotype analysis, or isoenzyme analysis [4] [32].
- Monitor Morphology: Regularly check cells for unexpected changes in morphology or growth rate compared to established baselines [32].
Corrective and Preventive Action:
- Work with One Cell Line: Only handle one cell line at a time in the biosafety cabinet to prevent accidental mix-ups [5] [32].
- Use Dedicated Reagents: Assign separate bottles of media, reagents, and pipettes for each cell line [5].
- Label Meticulously: Clearly label all flasks and plates with the cell line name, passage number, and date [32].
- Source Authentically: Obtain cell lines only from reputable cell banks that provide authentication data [5] [4].
How can I detect and eradicate a mycoplasma contamination?
Problem: Mycoplasma contamination is common, affecting an estimated 5-30% of cell cultures, and is typically invisible to the naked eye without altering culture conditions [5] [29].
Solution: Due to their small size and lack of a cell wall, mycoplasma are resistant to common antibiotics and require specific detection and eradication methods [5] [29].
Detection Protocols:
- PCR-Based Testing: This is a highly sensitive and common method for detecting mycoplasma-specific DNA sequences [5] [32].
- Fluorescent Staining: Use DNA-binding dyes like Hoechst 33258 to stain a fixed cell monolayer. Under fluorescence microscopy, mycoplasma appear as tiny, bright particles on the cell surface or in intercellular spaces (see diagram below) [5] [29].
- Commercial Kits: Many companies offer specialized mycoplasma detection kits based on PCR, ELISA, or enzymatic reactions [32] [1].
Eradication Protocol (Use with Caution):
- Consider Discarding: The best practice for a contaminated culture is to autoclave it and discard it. Only attempt eradication if the cell line is irreplaceable [5] [30].
- Quarantine: Move the contaminated culture to an isolated hood, preferably in a separate room [5].
- Antibiotic Treatment: Treat with commercially available antibiotics effective against mycoplasma, such as quinolone derivatives (e.g., Mycoplasma Removal Agent), ciprofloxacin, or a combination of tiamulin and minocycline (BM-Cyclin). Always follow the supplier's instructions for concentration and duration [5].
- Post-Treatment Validation: After treatment, culture the cells in antibiotic-free medium for 4-6 passages and re-test for mycoplasma to confirm eradication [4].
Frequently Asked Questions (FAQs)
The most overlooked sources are often procedural. These include using the same media bottle or pipettor for different cell lines, working with multiple cell lines simultaneously in the hood, and inadequate cleaning between handling different lines [5] [31] [32]. Aerosol generation during pipetting is another subtle risk, which can be mitigated by using filter tips [31].
Are antibiotics a reliable long-term solution for preventing biological contamination?
No, routine use of antibiotics is strongly discouraged. Their continuous use can promote the development of antibiotic-resistant strains, hide low-level contaminations (like mycoplasma), and can be toxic to cells or interfere with cellular processes under investigation [4] [29] [32]. Antibiotics should only be used as a last resort for short-term applications [4].
How can I prevent chemical contamination from my water source?
Always use laboratory-grade water for preparing all media and buffers [29]. Ensure water purification systems are well-maintained. For critical applications, consider using sterile, endotoxin-tested water from commercial suppliers to rule out water as a source of ions, endotoxins, or organic impurities [29].
My culture is contaminated with mold. What should I do?
Discard the contaminated culture immediately by autoclaving. Decontaminate the incubator and biosafety cabinet thoroughly, including shelves, door gaskets, and water trays, as fungal spores are airborne and persistent [32] [1]. Review your aseptic technique and ensure HEPA filters in your hood and incubator are functioning correctly [32].
Quantitative Data on Contamination
The tables below summarize the characteristics and detection methods for common contaminants to aid in identification and reporting.
Table 1: Characteristics of Common Microbial Contaminants
| Contaminant Type | Visual/Microscopic Signs | Effect on Medium pH | Growth Rate |
|---|---|---|---|
| Bacteria [5] [4] [32] | Turbidity; tiny, moving granules between cells. | Sharp drop (acidic, yellow). | Very rapid. |
| Yeasts [5] [4] | Turbidity; ovoid or spherical particles that bud. | Little change initially, increases with heavy infection. | Rapid. |
| Molds/Fungi [5] [4] | Thin, filamentous mycelia; fuzzy structures. | Changes sometimes; usually increases with heavy infection. | Moderate to rapid. |
| Mycoplasma [5] [29] [32] | No turbidity; not visible under standard microscope. | No direct change. | Slow, often unnoticed. |
Table 2: Recommended Detection Methods for Contaminants
| Contaminant Type | Primary Detection Methods | Recommended Testing Frequency |
|---|---|---|
| Bacteria, Fungi, Yeast [4] [29] | Visual inspection, microscopy, microbial culture. | Daily (microscopy), routine culture. |
| Mycoplasma [5] [29] [32] | PCR, fluorescent DNA staining (Hoechst), ELISA. | Every 1-2 months; for all new cell lines. |
| Viral [4] [29] [32] | PCR/RT-PCR, immunoassays (ELISA), electron microscopy. | Prior to use for bioproduction; as required for safety. |
| Cross-Contamination [4] [32] [1] | STR profiling, karyotype analysis, isoenzyme analysis. | Upon acquisition and every 6-12 months thereafter. |
Experimental Protocols
Protocol 1: Routine Screening for Mycoplasma via PCR
Principle: This method amplifies mycoplasma-specific DNA sequences, offering high sensitivity and specificity [32].
- Sample Collection: Collect 0.5 - 1 mL of cell culture supernatant from a test culture that has been without antibiotics for at least 3-5 days.
- DNA Extraction: Extract total DNA from the sample using a commercial DNA extraction kit, following the manufacturer's instructions.
- PCR Setup: Prepare a PCR master mix containing primers specific for conserved mycoplasma genes (e.g., 16S rRNA). Include both positive (known mycoplasma DNA) and negative (nuclease-free water) controls.
- Amplification: Run the PCR using the recommended cycling conditions for your primer set.
- Analysis: Analyze the PCR products by gel electrophoresis. A positive result is indicated by a band of the expected size in the test sample and positive control, absent in the negative control.
Protocol 2: Cell Line Authentication by STR Profiling
Principle: STR profiling analyzes highly polymorphic short tandem repeat loci in the genome to create a unique DNA fingerprint for a cell line [32].
- DNA Sample Preparation: Isolate high-quality genomic DNA from the cell line in question.
- Multiplex PCR: Amplify a standard set of STR loci (e.g., the 8-core loci used by ATCC) using fluorescently labeled primers.
- Capillary Electrophoresis: Separate the amplified fragments by size using capillary electrophoresis.
- Data Analysis: Software analyzes the fragment sizes to generate an allelic profile for each locus.
- Comparison: Compare this profile to reference profiles in a database (e.g., ATCC, DSMZ). A match confirms authenticity, while a mismatch indicates cross-contamination or misidentification.
The Scientist's Toolkit: Essential Reagent Solutions
Table 3: Key Reagents and Materials for Contamination Control
| Item | Function & Importance | Considerations |
|---|---|---|
| Mycoplasma-Tested FBS [32] [1] | Provides essential growth factors for cells. | Source from suppliers that provide certification for being tested and free of mycoplasma and viruses. |
| Endotoxin-Tested Media [29] | The nutrient base for cell growth. | High levels of endotoxins can adversely affect cell metabolism and experimental outcomes. |
| Sterile, Filtered Pipette Tips [31] | Prevents aerosol contamination from entering pipettors, reducing cross-contamination risk. | Use filter tips as a standard practice for all cell culture work. |
| 70% Ethanol / IMS [21] [1] | Standard disinfectant for decontaminating gloves, work surfaces, and equipment outside the biosafety cabinet. | Effective concentration for killing bacteria; must be used liberally throughout the procedure. |
| Mycoplasma Detection Kit [5] [32] | Allows for routine in-house screening for mycoplasma contamination. | Kits are available based on PCR, fluorescence, or enzymatic methods. |
| STR Profiling Kit/Service [32] | The gold-standard method for authenticating cell lines and ruling out cross-contamination. | Can be performed as a service by core facilities or commercial cell banks. |
Modern Arsenal for Contamination Detection: From Traditional Tests to Rapid Tech
Troubleshooting Guides
Guide 1: Troubleshooting Sterility Test Failures and Inconclusive Results
Problem: A sterility test conducted according to USP <71> has shown microbial growth (a positive result), or the results are questionable, potentially jeopardizing a product batch.
Solution: Follow this structured investigation flow to determine the root cause—whether it's a true product contamination or a false positive from laboratory error.
Investigation Workflow:
Actionable Steps:
- Confirm and Identify Growth: Sub-culture the organism from the positive test media to isolate it for identification [33].
- Compare with Environmental Isolates: Compare the identified microorganism against the environmental monitoring (EM) and personnel monitoring (PM) data from the day of testing. If a match is found, the test is considered invalid due to laboratory error and must be repeated [33].
- Review Aseptic Technique: If no EM match is found, conduct a thorough review of aseptic techniques. This includes checking records for media sterilization, equipment assembly, and technician gowning certification [33].
- Check Method Suitability: Verify that a valid Method Suitability Test (also known as Bacteriostasis and Fungistasis test) was conducted for the product. This test confirms that the product itself does not inhibit microbial growth, ensuring the test's validity [33] [34].
- Final Determination:
Guide 2: Addressing Undetected Contamination in Cell Cultures
Problem: Despite passing routine sterility checks, cell cultures exhibit unexplained issues like reduced growth rates, altered metabolism, or strange morphology, suggesting the presence of contaminants not detected by standard USP <71> methods.
Solution: USP <71> is designed for sterile products and may not detect all contaminants in a dynamic cell culture system. Implement a broader detection strategy targeting specific, hard-to-detect organisms.
Diagnosis and Resolution Workflow:
Actionable Steps:
- Expand Detection Methods:
- For Mycoplasma: Routinely use DNA staining (e.g., Hoechst stain) or PCR-based methods, as these contaminants are invisible to standard light microscopy and can pass through 0.22 µm filters [23] [6].
- For Viruses: Implement PCR, electron microscopy, or in vivo testing, as these are not detected by culture-based sterility tests [27] [23].
- Review Aseptic Technique: Reinforce strict aseptic practices. This includes working with one cell line at a time, proper use of biological safety cabinets, and routine cleaning with 70% alcohol and 10% bleach [27] [23].
- Source Control: Use gamma-irradiated serum and source cell lines from reputable banks that provide viral and mycoplasma testing certifications [27] [23].
- Containment and Elimination:
- Immediately quarantine any suspect cultures.
- Antibiotics or antimycotics can be attempted for bacterial or fungal contamination but use them cautiously as they can mask low-level contamination and lead to resistant strains [23].
- For valuable cultures contaminated with mycoplasma, specialized elimination kits or services may be an option [23]. Often, discarding the culture is the safest course of action to protect other cells in the laboratory.
Frequently Asked Questions (FAQs)
How does USP <71> ensure its sterility testing methods are reliable?
USP <71> mandates two critical validation tests to ensure reliability [33] [34]:
- Growth Promotion Test (GPT): This test verifies that the culture media (FTM and TSB) can support the growth of a small number of representative microorganisms. It confirms that a "no growth" result is due to the product's sterility, not faulty media.
- Method Suitability Test (Bacteriostasis and Fungistasis): This test confirms that the product itself does not contain antimicrobial properties that would inhibit microbial growth during the test. The product is inoculated with a low level of specific microorganisms, and the method must be able to recover them. If inhibition occurs, the method is modified, for example, by adding neutralizers or increasing rinse volumes, to ensure accurate detection.
What are the primary limitations of USP <71> and other culture-based methods?
While considered the gold standard, these methods have inherent limitations:
- Lengthy Incubation Time: The mandatory 14-day incubation period can create significant delays in product release [33] [34].
- Inability to Detect All Contaminants: The method may not support the growth of viable but non-culturable (VBNC) organisms, certain fastidious bacteria, or viruses [35].
- Low Throughput and Manual Labor: The process is labor-intensive and not easily scalable for high-throughput needs [36].
- Potential for Human Error: As a manual process, it is susceptible to false positives due to accidental contamination during testing [33].
When are automated blood culture systems a suitable alternative to the compendial USP <71> method?
Automated systems like BacT/Alert can be suitable alternatives but require careful validation. A 2019 study found that the BacT/Alert system incubated at 32.5°C, when paired with a supplemental Sabouraud Dextrose Agar (SDA) plate, performed equivalently to the manual USP <71> method after extended incubation [36]. In contrast, the Bactec FX system was found to be suboptimal, particularly for detecting environmental molds, highlighting that not all automated systems are equally effective for product sterility testing [36].
What is the difference between a Sterility Test (USP <71>) and a Bioburden Test?
These are two distinct types of microbial control tests:
- Sterility Test (USP <71>): A qualitative, pass/fail test designed to demonstrate the absence of viable microorganisms in a stated portion of a sterile product batch. It is a release test for products labeled "sterile" [33] [37].
- Bioburden Test: A quantitative test used for non-sterile products or for in-process monitoring of sterile products. It estimates the total number of viable microorganisms present in or on a product before terminal sterilization. This is not a direct measure of sterility but a quality control metric [37].
Table 1. Performance Comparison of Sterility Testing Methods Against Compendial USP <71> [36]
| Testing Method | Sensitivity at <144 hrs (vs. USP <71>) | Sensitivity with Extended Incubation & Visual Inspection | Key Limitations |
|---|---|---|---|
| Compendial USP <71> | 84.7% (Baseline) | 95.7% (Baseline) | Lengthy process (14 days), labor-intensive |
| BacT/Alert at 32.5°C | 78.8% (Not Significant) | 89.0% (Not Significant) | Requires supplemental SDA plate for optimal fungal detection |
| Bactec FX | 64.4% (Significantly Lower) | 71.2% (Significantly Lower) | Suboptimal for detecting environmental molds |
Table 2. Recovery Rates of Sampling Methods for Duodenoscope Surveillance [38]
| Organism | Modified ESGE Protocol (MEP) | Interim CDC Protocol |
|---|---|---|
| P. aeruginosa | 80.3% ± 23.5 | 46.2% ± 12.6 |
| E. coli | 46.0% ± 13.0 | 25.6% ± 7.8 |
| K. pneumoniae | 66.0% ± 9.7 | 32.1% ± 3.2 |
| E. faecium | 67.2% ± 15.6 | 60.2% ± 4.2 |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3. Essential Materials for Sterility Testing and Contamination Control
| Item | Function | Example & Notes |
|---|---|---|
| Culture Media | Supports growth of potential contaminants. | Fluid Thioglycollate Medium (FTM): For anaerobes and aerobes. Soybean-Casein Digest Medium (TSB): For aerobes and fungi [33]. |
| Membrane Filter | Traps microorganisms from filterable products. | 0.45 µm pore size filter, used in Membrane Filtration method [33]. |
| Neutralizing Agents | Counteracts antimicrobial properties in a product. | Added to rinse fluids or media during Method Suitability to ensure microbial recovery [33] [34]. |
| RODAC Plates | For environmental and personnel monitoring. | Agar plates used to sample surfaces and gloves to monitor aseptic processing areas [33]. |
| DNA Stains & PCR Kits | Detects non-culturable contaminants. | Hoechst Stain: For mycoplasma visualization [23]. PCR Kits: For specific, rapid detection of mycoplasma and viruses [23] [6]. |
| Disinfectants | Maintains sterile working environment. | Rotation of 70% alcohol, 10% bleach, and sporicidal agents is recommended [33] [27]. |
Within cell culture research and the development of advanced therapies, microbial contamination poses a significant risk to experimental integrity and patient safety. Rapid Microbiological Methods (RMMs) are advanced technologies designed to detect, identify, and quantify microorganisms faster and more accurately than traditional, labor-intensive culture-based methods [39]. This technical support center focuses on two automated microbial detection systems—BACTEC and BACT/ALERT 3D—within the broader context of a thesis on cell culture microbial contamination. These systems are critical for researchers and drug development professionals working with sensitive biological materials, including cell therapy products (CTPs), where timely contamination detection can be life-saving for critically ill patients awaiting treatment [18] [40].
Traditional sterility testing methods, based on microbiological culture, are labor-intensive and can require up to 14 days to detect contamination [18]. This delay is unacceptable for many advanced therapies with short shelf lives. RMMs address this need for speed, automation, and improved accuracy, directly supporting the contamination control strategies required in modern pharmaceutical manufacturing and biotechnological research [39] [41].
The BACT/ALERT 3D instrument is a state-of-the-art, automated microbial detection system. Its modular design, easy touch-screen operation, and flexible data management options make it suitable for laboratories of all sizes [42] [43].
Key Features, Benefits, and Technical Specifications
The system is primarily used for detecting microorganisms in blood and sterile body fluids [42]. It utilizes patented colorimetric sensor technology that changes color in response to carbon dioxide produced by microbial growth, allowing for early detection and immediate intervention [43].
Table 1: Key Features and Benefits of BACT/ALERT 3D
| Feature | Benefit for Research and Diagnostics |
|---|---|
| Modular, Scalable Design | Adapts to laboratory space and volume needs; the same footprint as smaller platforms with 2-3 times the bottle capacity [43]. |
| Easy-to-Use Touchscreen | Facilitates cross-training, reduces errors, and minimizes labor needs [42] [43]. |
| Plastic, Shatter-Resistant Bottles | Reduces biohazard exposure risk and offers cost-effective shipping and disposal [42] [43]. |
| Flexible Data Management | Options range from basic (Select) to advanced LIS connectivity (Signature), supporting compliance with data integrity regulations [42] [41]. |
| Rapid Response Time | Low false-positive rate and rapid time-to-detection enable researchers to do more in less time with greater accuracy [42]. |
Table 2: Technical Specifications for BACT/ALERT 3D Configurations
| Parameter | BACT/ALERT 3D 120 Combo | BACT/ALERT 3D 240 Incubator Module |
|---|---|---|
| Dimensions (HxWxL) | 30.8 x 19.5 x 24.5 inches (77 x 48.8 x 61.2 cm) [43] | 36 x 19.5 x 24.3 inches (90 x 48.8 x 60.8 cm) [43] |
| Capacity | 120 cells (60 cells/drawer) [43] | 240 cells (60 cells/drawer) [43] |
| Weight (Loaded) | 216.5 lbs (98.3 kg) [43] | 233 lbs (105.8 kg) [43] |
| Power Consumption | 115 VAC, 640 Watts (typical) [43] | 115 VAC, 640 Watts (typical) [43] |
BACT/ALERT 3D Experimental Workflow
The following diagram illustrates the standard operational workflow for using the BACT/ALERT 3D system in a laboratory setting.
The Scientist's Toolkit: Key Research Reagent Solutions
The performance of automated systems is highly dependent on the culture media used. The table below details key media bottles for the BACT/ALERT 3D system, which are designed to ensure the recovery of a wide variety of microorganisms, including bacteria, fungi, and mycobacteria [42] [43].
Table 3: BACT/ALERT Culture Media Portfolio for Research
| Product Name | Media Type & Function | Specimen Type | Specimen Volume |
|---|---|---|---|
| BACT/ALERT FA Plus [42] | Aerobic. FAN Plus media with Adsorbent Polymeric Beads (APB) to neutralize antimicrobials. | Blood or Sterile Body Fluids (SBF) | Up to 10 mL |
| BACT/ALERT FN Plus [42] | Anaerobic. FAN Plus media with APB for fastidious and anaerobic organisms. | Blood or SBF | Up to 10 mL |
| BACT/ALERT SA [42] | Standard Aerobic. For recovery and detection of aerobic microorganisms (bacteria and fungi). | Blood or SBF | Up to 10 mL |
| BACT/ALERT SN [42] | Standard Anaerobic. For recovery and detection of anaerobic and facultative anaerobic bacteria. | Blood or SBF | Up to 10 mL |
| BACT/ALERT MP [42] | Mycobacteria. For recovery and detection of mycobacteria. | Digested or decontaminated specimens | 0.5 mL |
Troubleshooting Guide: Common Issues and Solutions
This section addresses specific issues users might encounter during experiments with microbial detection systems.
Issue 1: Delayed or No Detection of Known Positives
- Potential Cause: Incorrect sample volume used, leading to a dilution effect that extends the time to detection (TTD).
- Solution: Verify that the recommended sample volume is used for the specific bottle type (e.g., up to 10 mL for FA/FN Plus bottles). Ensure samples are injected directly into the broth and not onto the sensor at the bottom [42].
Issue 2: High Rate of False-Positive Signals
- Potential Cause: Contamination during sample inoculation or bottle handling. Non-microbial gas production from certain sample types.
- Solution: Aseptically validate the sample collection and loading technique. Review the lot-specific quality control documentation for the media. For unique sample types, method suitability testing is recommended to establish a baseline TTD [42].
Issue 3: Instrument Does Not Recognize Loaded Bottles
- Potential Cause: Damaged or obsolete barcode labels on bottles. Malfunctioning barcode reader within the instrument drawer.
- Solution: Inspect bottle labels for integrity. Clean the barcode scanner window with a soft, lint-free cloth. If the problem persists, contact technical service for module diagnostics [43].
Issue 4: Communication Error with Laboratory Information System (LIS)
- Potential Cause: Incorrect data mapping or interface configuration between the BACT/ALERT 3D data management system (e.g., Signature) and the LIS.
- Solution: Verify the connectivity settings in the instrument software. Confirm that the data string format matches the LIS requirements. Consult with both the instrument and LIS support teams [42] [41].
Frequently Asked Questions (FAQs)
Q1: How does the detection technology in BACT/ALERT 3D work? The system uses a colorimetric sensor embedded in the bottom of each culture bottle. As microorganisms grow, they produce CO₂, which changes the color of the sensor. The instrument's optical system continuously monitors each bottle for this color change, signaling a positive result [42] [43].
Q2: What are the main advantages of using plastic culture bottles? Plastic bottles are shatter-resistant, which reduces the risk of biohazard exposure from broken glass. They are also lightweight, reducing shipping costs and making disposal easier and potentially more cost-efficient [42] [43].
Q3: Can the BACT/ALERT 3D system be used for sterility testing of cell therapy products (CTPs)? While the system is optimized for blood and sterile body fluids, its principle of automated, continuous monitoring aligns with the need for rapid sterility testing in CTP manufacturing. However, for final product release, the method must be validated according to regulatory standards for sterility testing [39]. Novel RMMs, such as UV spectroscopy with machine learning, are also emerging specifically for CTPs, offering results in under 30 minutes [18] [40].
Q4: What is the regulatory stance on using RMMs like BACT/ALERT 3D? Regulatory agencies (FDA, EMA) recognize RMMs as alternatives to conventional methods. The revised EU GMP Annex 1 explicitly encourages the use of modern technologies to improve contamination control [41]. However, implementing any RMM requires a validation process to demonstrate its equivalence or superiority to the pharmacopoeial method it is intended to replace [39] [41].
Q5: Our lab is considering implementing an RMM. What are the key challenges? The main challenges include the initial cost of investment, the need for technical expertise to operate and maintain the system, and the rigorous validation required for regulatory alignment. A successful implementation requires careful technology selection, feasibility studies, and change management [39] [41].
This technical support center provides essential guidance for implementing a novel method for detecting microbial contamination in cell cultures. This machine learning-aided UV absorbance spectroscopy technique represents a significant advancement over traditional sterility testing, reducing detection time from days to minutes while maintaining high sensitivity and specificity [18] [44]. The method is particularly valuable for cell therapy product (CTP) manufacturing, where timely administration of treatments can be life-saving for critically ill patients [40].
The following FAQs, troubleshooting guides, and experimental protocols will assist researchers, scientists, and drug development professionals in successfully implementing this technology within their laboratories.
Frequently Asked Questions (FAQs)
Q1: How does machine learning-aided UV spectroscopy detect microbial contamination? This method combines ultraviolet light absorbance measurements with machine learning algorithms to identify contamination. Microorganisms in cell culture media alter the fluid's biochemical composition, which changes its UV absorbance spectrum. These spectral patterns serve as "fingerprints" that a trained one-class support vector machine (SVM) model recognizes as anomalous compared to sterile samples [44] [45]. The system provides a definitive yes/no contamination assessment within 30 minutes without requiring cell extraction or staining [40].
Q2: What are the key advantages over traditional sterility testing methods? Traditional sterility tests like USP <71> require 14 days for results, while rapid microbiological methods (RMMs) still need approximately 7 days [18]. This new approach offers:
- Speed: Results in <30 minutes [40]
- Sensitivity: Detection as low as 10 colony-forming units (CFUs) [44]
- Non-invasiveness: No cell extraction required [18]
- Label-free operation: No staining or tagging needed [44]
- Automation potential: Enables continuous culture monitoring [40]
Q3: What instrumentation is required to implement this method? The essential equipment includes:
- UV-Vis spectrophotometer (standard commercial unit)
- Sample holder/cuvette with 10mm path length
- Computer system for machine learning analysis
- Optional: Automated sampling system for bioreactor integration [46] [45]
Q4: What microbial contaminants can this method detect? Research has successfully detected 7 microbial organisms spiked into mesenchymal stromal cell supernatants, though specific organisms beyond E. coli K-12 (ATCC 25404) aren't detailed in the available literature. Future research aims to broaden detection to a wider range of contaminants representative of cGMP environments [44] [40].
Q5: How does this method perform compared to USP <71> and BACT/ALERT 3D? The method detects E. coli contamination at 10 CFUs in approximately 21 hours, comparable to USP <71> (~24 hours) but longer than BACT/ALERT 3D (16 hours). However, it provides continuous monitoring capability and much faster analysis once samples are collected [44].
Experimental Protocols
Protocol 1: Standard Contamination Detection Assay
Purpose: To detect microbial contamination in cell therapy products during manufacturing [44].
Materials:
- Cell culture supernatant samples (≤1 mL)
- UV-transparent cuvettes (10mm path length)
- Phosphate Buffer Solution (PBS)
- UV-Vis spectrophotometer
- Trained one-class SVM model
Procedure:
- Collect cell culture supernatant samples (1 mL volume) under aseptic conditions
- Transfer samples to UV-transparent cuvettes
- Measure absorbance spectra using UV-Vis spectrophotometer across appropriate wavelength range
- Input spectral data into trained one-class SVM model
- Record contamination prediction (yes/no output)
- For confirmed contamination, implement corrective actions and consider secondary confirmation with RMMs
Technical Notes:
- Sample preparation should be minimal with no additional reagents required
- Measurements should be performed in triplicate for statistical reliability
- The model should be trained on sterile samples from the specific cell type being monitored
Protocol 2: Model Training and Validation
Purpose: To develop and validate a machine learning model for contamination detection [44] [45].
Materials:
- Sterile cell culture media samples from multiple donors
- Selected microbial strains for spiking
- UV-Vis spectrophotometer
- Machine learning environment (Python with scikit-learn recommended)
Procedure:
- Collect sterile cell culture media samples from various culture conditions
- Split samples into two groups: sterile control and experimental (spiked with microorganisms)
- Obtain UV absorbance spectra for all samples
- Use spectra from sterile samples exclusively to train a one-class SVM model
- Validate model performance using mixture of sterile and contaminated samples
- Calculate true positive and true negative rates to assess model accuracy
Technical Notes:
- Include samples from multiple donors to improve model robustness
- Test model across different cell types beyond those used in initial training
- Optimal performance achieved when excluding samples with anomalously high nicotinic acid content [44]
Performance Data Tables
Table 1: Comparison of Microbial Detection Methods
| Method | Detection Time | Sensitivity | Sample Volume | Labor Intensity |
|---|---|---|---|---|
| Traditional USP <71> | 14 days | ~10 CFUs | 1 mL | High [18] |
| Rapid Microbiological Methods (RMMs) | 7 days | ~10 CFUs | 1 mL | Moderate [18] |
| BACT/ALERT 3D | 16 hours | ~10 CFUs | 1 mL | Low [44] |
| ML-aided UV Spectroscopy | <30 minutes analysis | 10 CFUs | <1 mL | Low (automation compatible) [44] [40] |
Table 2: Detection Performance Across Donors
| Parameter | Value | Notes |
|---|---|---|
| Mean True Positive Rate | 92.7% | All microorganisms tested [44] |
| Mean True Negative Rate | 77.7% | Across multiple donors [44] |
| Improved True Negative Rate | 92% | After excluding donor with high nicotinic acid [44] |
| Time to Detection (10 CFUs E. coli) | 21 hours | Comparable to USP <71> [44] |
Method Workflow and Data Analysis
The following diagrams illustrate the experimental workflow and data analysis process for machine learning-aided UV absorbance spectroscopy.
Experimental workflow for contamination detection.
Data analysis pathway for contamination assessment.
Research Reagent Solutions
Table 3: Essential Materials for Implementation
| Item | Function | Specifications |
|---|---|---|
| UV-Vis Spectrophotometer | Measures light absorption | Standard commercial unit, 220-700 nm range [46] |
| Cuvettes | Sample holder | Quartz or UV-transparent, 10mm path length [46] |
| Mesenchymal Stromal Cell Cultures | Demonstration model | Commercial donors, various sources [44] |
| Phosphate Buffer Solution (PBS) | Control preparation | Standard formulation [44] |
| Microbial Strains | Method validation | 7 organisms including E. coli K-12 (ATCC 25404) [44] |
| Software | Machine learning analysis | Python with scikit-learn, custom algorithms [44] |
Troubleshooting Guides
Problem 1: Poor Model Performance with High False Positive Rates
- Potential Cause: Spectral interference from compounds like nicotinic acid in certain donor samples [44]
- Solution: Pre-screen donors for anomalous metabolite levels or exclude problematic samples from training set
- Prevention: Include diverse donor samples in training to improve model robustness
Problem 2: Inconsistent Absorbance Measurements
- Potential Cause: Air bubbles or particulate matter in samples [46]
- Solution: Centrifuge samples before analysis or use filtration to remove debris
- Prevention: Ensure proper sample preparation techniques and cuvette handling
Problem 3: Limited Detection Range for Microbial Species
- Potential Cause: Model trained on insufficient variety of contaminants [40]
- Solution: Expand training set to include more microbial species common to cGMP environments
- Prevention: Continuously update model with new contamination data as available
Problem 4: Difficulty Integrating with Bioreactor Systems
- Potential Cause: Manual sampling introduces variability and contamination risk [45]
- Solution: Implement automated sampling systems for closed-loop operations
- Prevention: Design integrated sampling ports specifically for spectroscopic analysis
Future Directions
Ongoing research aims to expand this technology's capabilities by:
- Broadening detection to encompass more microbial contaminants representative of cGMP environments [40]
- Testing model robustness across diverse cell types beyond mesenchymal stromal cells [18]
- Developing complete automated monitoring systems integrated with bioreactors [45]
- Exploring applications beyond cell therapy, such as food and beverage quality control [40]
For additional technical support, researchers are encouraged to consult the primary literature and consider collaborative opportunities with developing institutions to further refine this promising technology.
Troubleshooting Guides
Common Instrumental and Data Analysis Issues
Q1: My GC-IMS analysis shows poor separation of volatile compounds, resulting in overlapping peaks. What could be the cause and how can I resolve this?
A: Poor peak separation can often be attributed to issues with the chromatographic column or incorrect method parameters. First, ensure the GC column (e.g., MXT-5 or similar wide-bore column) is properly conditioned and not degraded [47]. Verify the carrier gas flow rate; nitrogen is typically used, and an unstable or incorrect flow can compromise separation [47]. Method parameters such as the column temperature and the ramp rate should be optimized for your specific analytes. Increasing the GC runtime can sometimes improve resolution, as a longer column (e.g., 15m) provides more theoretical plates for separation [47].
Q2: The signal intensity from my GC-IMS is weak or inconsistent when analyzing microbial cultures. What steps should I take?
A: Weak signals often stem from sampling procedure inefficiencies. Focus on the headspace sampling method. The sampling bottle should be sealed and incubated (e.g., at 60°C for 10 minutes) to allow sufficient accumulation of volatile metabolites in the headspace [47]. Ensure the injection volume (typically 1 mL of headspace gas) is correctly set [47]. For microbial cultures, using a direct method—where bacteria are cultured directly in the sampling bottle—significantly improves the accumulation and detection of mVOCs compared to transferring an aliquot of culture (indirect method) [47]. Also, confirm that the Ion Mobility Spectrometer's drift gas is pure and flowing correctly, as impurities can quench the signal.
Q3: How can I differentiate between specific microbial species in a mixed culture using GC-IMS data?
A: Identifying species in a mixed culture relies on pattern recognition and multivariate data analysis rather than a single unique marker. GC-IMS generates a unique volatile metabolite "fingerprint" for pure and mixed cultures [48] [47]. Follow this data analysis workflow:
- Acquire Reference Spectra: First, run pure cultures of the expected microorganisms (e.g., E. coli, S. aureus, P. aeruginosa) to establish a library of known patterns [47].
- Conduct Pattern-Based Analysis: Use software like LAV (G.A.S.) to mark significant peaks and compare the overall 2D spectrum of your mixed sample against the reference library [47].
- Apply Statistical Models: Employ Principal Component Analysis (PCA) or Partial Least Squares Discriminant Analysis (PLS-DA) to the GC-IMS data. These models can differentiate between microorganisms and even separate pure from mixed cultures with high accuracy based on the combined VOC profile [48].
Sample Preparation and Contamination
Q4: I am detecting unexpected volatile compounds in my chromatograms. What are potential sources of this contamination?
A: Unexpected peaks typically indicate contamination from the sample preparation process or the culture medium itself.
- Culture Medium: The growth medium (e.g., Thioglycolate medium) contains its own VOCs. Always run a blank sample of the sterile medium under identical conditions and subtract its background signal from your experimental data [47].
- Reagents and Labware: Impurities in solvents or VOCs leaching from plastic tubes and septa can contaminate the headspace. Use high-purity reagents and inert glassware whenever possible.
- Cross-Contamination: Ensure proper cleaning of sampling bottles and the automatic sampler needle between runs to prevent carryover [47].
Q5: What is the best way to prepare and introduce my cell culture sample into the GC-IMS to maximize detection of microbial VOCs (mVOCs)?
A: The sample introduction method is critical for sensitive detection of mVOCs.
- Recommended: Direct Method. Inoculate the culture medium directly in the headspace sampling vial and incubate it to allow the mVOCs to accumulate. This method concentrates the volatile metabolites and leads to a stronger, more representative signal [47].
- Alternative: Indirect Method. Transfer 1 mL of a pre-grown culture to the sampling vial. This method is less effective as mVOCs can be lost during transfer [47].
- Protocol: Regardless of the method, incubate the sealed sampling vial at a defined temperature (e.g., 60°C) with shaking for a set time (e.g., 10 min) to promote the transfer of VOCs from the liquid medium to the headspace before the automated sampler injects the 1 mL gas sample [47].
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of using GC-IMS for monitoring microbial contamination in cell cultures? GC-IMS offers exceptional sensitivity with detection limits in the low parts-per-billion volume (ppbv) range, allowing for early detection of microbial metabolism [48]. It provides rapid analysis, with results potentially available in minutes after headspace sampling, which is faster than traditional culture-based methods that can take over 18 hours [47]. The technique is robust and can differentiate between microorganisms based on their unique volatile metabolite patterns, even in mixed cultures [48] [47].
Q2: Can GC-IMS identify the specific species of contaminating microorganisms? GC-IMS excels at differentiation rather than definitive identification. It can distinguish between different pure cultures and mixed cultures based on their unique VOC fingerprints using statistical models like PCA and PLS-DA [48] [47]. While it may detect specific known compounds (e.g., ethanol, 2-heptanone), identification is primarily based on the overall pattern of peaks (retention time and drift time) compared to a reference library [47]. For absolute species identification, techniques like MALDI-TOF MS or genetic sequencing are still required.
Q3: How does GC-IMS compare to other analytical techniques like GC-MS for VOC analysis? GC-IMS is highly complementary to GC-MS. Its key strengths are its high sensitivity and the ability to operate at atmospheric pressure, making it simpler and more robust for routine, high-throughput analysis [48]. While GC-MS is unparalleled in identifying unknown compounds through extensive spectral libraries, GC-IMS is ideal for rapid fingerprinting and pattern recognition in complex samples like microbial headspace [48] [47].
Q4: What are the critical steps in the experimental workflow to ensure reproducible GC-IMS results? Reproducibility depends on strict adherence to protocol in these areas:
- Consistent Sample Preparation: Use the same culture medium, incubation time, and temperature for biological replicates. The direct sampling method is preferred for better reproducibility [47].
- Stable Instrument Parameters: Maintain consistent GC oven temperature programs, carrier and drift gas flow rates, and injection volumes [47].
- Routine Blank Subtraction: Always include and subtract the medium blank to account for background VOCs [47].
Experimental Protocols and Data Presentation
Standard Protocol for Identifying Microbes in Mixed Culture
This protocol is adapted from research for identifying common bacteria such as E. coli, S. aureus, and P. aeruginosa in mixed culture [47].
1. Culture Preparation:
- Inoculate pure cultures of target microorganisms (e.g., E. coli, S. aureus, P. aeruginosa) in a suitable medium like Thioglycolate (TH) broth.
- For mixed cultures, combine the microorganisms in the desired ratios.
- Using the direct method, inoculate 1.5 mL of sterile medium in a 20 mL GC-IMS sampling vial and incubate at 37°C for 12-15 hours without agitation [47].
2. GC-IMS Instrument Setup:
- GC Column: Use a wide-bore column (e.g., MXT-5, 15 m × 0.53 mm × 1 μm) [47].
- Carrier and Drift Gas: High-purity nitrogen (N₂) [47].
- Sample Incubation: Place the sealed sampling vial in the autosampler incubator. Shake and heat at 60°C for 10 min [47].
- Injection: The automated sampler should inject 1 mL of the headspace gas [47].
3. Data Acquisition and Analysis:
- Acquire the GC-IMS spectrum, which plots drift time (y-axis) against retention time (x-axis).
- Use analysis software (e.g., LAV from G.A.S.) to mark significant VOC peaks in the 2D spectrum [47].
- Perform statistical analysis, such as Principal Component Analysis (PCA), to differentiate between the VOC profiles of pure and mixed cultures [47].
Quantitative Data from Microbial VOC Studies
Table 1: Characteristic Microbial Volatile Organic Compounds (mVOCs) from Selected Bacteria [47]. Dt = Drift Time, Rt = Retention Time.
| Detected Substance | E. coli | S. aureus | P. aeruginosa | Remarks |
|---|---|---|---|---|
| Ethanol | Detected | Not Detected | Not Detected | Specific to E. coli under these conditions |
| 2-Heptanone | Not Detected | Detected | Not Detected | Specific to S. aureus under these conditions |
| Phenylacetaldehyde | Not Detected | Detected | Not Detected | Specific to S. aureus under these conditions |
| Isoamyl acetate | Not Detected | Detected | Not Detected | Specific to S. aureus under these conditions |
| Unidentified VOC (Index) | Detected (e.g., #2) | Detected (e.g., #5) | Detected (e.g., #8) | Pattern is often more important than single compounds |
Table 2: Performance of GC-IMS with Multivariate Analysis for Microbial Differentiation [48].
| Analysis Type | Model Used | Prediction Accuracy / Outcome |
|---|---|---|
| Differentiation between microorganisms | PLS-DA | Accuracy of 0.92 [48] |
| Separating mixed from pure cultures | PLS-DA | Accuracy between 0.87 and 1.00 [48] |
| Modeling microbial growth curves | GC-IMS data vs. Optical Density | Root Mean Squared Error (RMSE) of 10-20% of max value [48] |
Workflow and Signaling Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for GC-IMS-based Microbial Contamination Studies.
| Item / Reagent | Function / Application | Example / Specification |
|---|---|---|
| GC-IMS Instrument | Core analytical unit for separating and detecting volatile compounds. | Systems from manufacturers like G.A.S., equipped with automatic sampler [47]. |
| GC Column | Primary separation of volatile compounds in the gas phase. | MXT-5-type, 15 m length, 0.53 mm diameter, 1 μm film thickness [47]. |
| Nitrogen Generator | Provides high-purity carrier and drift gas for GC and IMS. | Required for stable operation and high sensitivity [47]. |
| Sampling Vials | Sealed containers for culturing microbes and accumulating mVOCs. | 20 mL glass vials, compatible with the autosampler [47]. |
| Culture Medium | Supports microbial growth and production of volatile metabolites. | Thioglycolate (TH) medium, Brain Heart Infusion (BHI) broth; medium-dependent VOC profiles [47]. |
| Reference Strains | Provide known VOC fingerprints for building identification models. | ATCC strains (e.g., E. coli ATCC25922, S. aureus ATCC25923) [47]. |
| Data Analysis Software | Processes 2D GC-IMS data, performs peak marking, and statistical analysis. | LAV (G.A.S.), GC-IMS Library Search; used for PCA and PLS-DA [48] [47]. |
PCR and Other Molecular Tools for Mycoplasma and Viral Screening
Cell culture is a fundamental tool in biomedical research and drug development, but its reliability is consistently challenged by microbial contamination. Among these, mycoplasma and viral contaminants pose a significant threat due to their elusive nature and potential to alter experimental outcomes. This technical support center provides a comprehensive guide on utilizing modern molecular tools, including PCR and other advanced techniques, for the effective detection and troubleshooting of these contaminants, framed within the context of cell culture microbial contamination research.
Mycoplasma Detection
FAQ: Why is mycoplasma contamination particularly problematic in cell culture?
Mycoplasma are bacteria that lack a cell wall, making them resistant to common antibiotics like penicillin and allowing them to pass through standard 0.2-micron filters used for media sterilization [49]. They do not typically kill host cells or cause turbidity in media, meaning contamination can go unnoticed for long periods [50] [29]. However, they can profoundly affect cell physiology by altering metabolism, gene expression, growth rates, and inducing chromosomal instability, thereby compromising the integrity of experimental data [50] [29]. It is estimated that between 5% and 35% of all cell lines are contaminated with mycoplasma [50] [29].
FAQ: What are the primary molecular methods for detecting mycoplasma?
The table below summarizes the key molecular techniques used for mycoplasma detection.
| Method | Principle | Key Features |
|---|---|---|
| PCR/qPCR [50] [51] [49] | Amplifies mycoplasma-specific DNA sequences (e.g., 16S rRNA) using targeted primers. | High sensitivity and specificity; rapid (hours); can be designed to cover a broad range of species; cost-effective. |
| DNA Staining (e.g., Hoechst/DAPI) [49] [29] | Fluorescent dyes bind to DNA in the sample, revealing extranuclear mycoplasma DNA under a microscope. | Relatively fast; requires expertise for interpretation; can produce false negatives with low-level contamination. |
| Enzyme-based Bioluminescence Assays [49] | Detects specific mycoplasma enzymes not found in eukaryotic cells, generating a luminescent signal. | Kit-based; sensitive; does not require microscopic analysis. |
| Culture on Agar/Broth [49] | Grows mycoplasmas on specific nutrient media. | Considered a historical "gold standard"; can take 1-2 weeks; may not detect all non-cultivable strains [50]. |
Detailed Protocol: A Universal PCR Method for Mycoplasma Screening
A robust PCR protocol has been developed to establish a universal standard for routine testing [50].
- 1. Primer Design: The strategy uses ultra-conserved primers targeting the 16S rRNA gene. Bioinformatic analysis shows this primer pair covers 92% of all species across the six orders of the class Mollicutes (phylum Mycoplasmatota), including 198 out of 216 mycoplasma species [50].
- 2. Sample Preparation: Use cell culture supernatant or a cell lysate. To increase detection sensitivity and include an internal control, the protocol utilizes eukaryotic DNA from cell extracts.
- 3. PCR Setup: A four-primer PCR is performed. This includes:
- The mycoplasma-specific primers.
- Primers targeting a highly conserved eukaryotic DNA sequence (e.g., generating a 105 bp product) to confirm the presence of amplifiable DNA and a successful PCR reaction [50].
- 4. Analysis: Amplification of a 166-191 bp product indicates mycoplasma contamination. The internal eukaryotic control band (105 bp) must be present in all samples for the test to be valid.
Performance Data:
- Limit of Detection (LOD): The assay can detect as little as 6.3 pg of Mycoplasma orale genomic DNA, which is equivalent to approximately 8.21 x 10³ genomic copies [50].
- Coverage: The primers are designed to cover common cell culture contaminants such as Acholeplasma laidlawii, Mycoplasmopsis fermentans, and Mesomycoplasma hyorhinis with high efficiency (89-100% for most genera) [50].
The following workflow illustrates the key steps and decision points in this universal PCR method:
Research Reagent Solutions for Mycoplasma PCR
| Reagent / Material | Function | Example / Specification |
|---|---|---|
| Ultra-Conserved Primers [50] | Amplify mycoplasma 16S rRNA genes with broad coverage. | Primer pair covering 92% of Mollicutes species. |
| Eukaryotic Control Primers [50] | Internal control for DNA quality and PCR efficiency. | Primers for a conserved eukaryotic gene (e.g., producing a 105 bp amplicon). |
| DNA Polymerase | Enzymatically amplifies target DNA sequences. | Heat-stable polymerase for standard or qPCR. |
| Cell Lysis Buffer | Releases DNA from sampled cells for analysis. | Buffer containing non-ionic detergents and proteinase K. |
| Agarose Gel | Separates and visualizes PCR amplicons by size. | Standard 2-3% agarose in TAE or TBE buffer. |
Viral Detection
FAQ: How does viral contamination differ from mycoplasma contamination?
Unlike mycoplasma, viruses are obligate intracellular pathogens that require host cell machinery to replicate [52]. Viral contamination is often non-cytopathic, meaning it may not cause visible changes in the cell culture, allowing it to remain undetected indefinitely [24] [29]. The primary concerns are the alteration of host cell biology, which can skew research data, and the potential biosafety risk to laboratory personnel, especially when working with human-derived materials [29]. Prevalent viral contaminants include Epstein-Barr virus (EBV) and Ovine Herpesvirus 2 (OvHV-2) [24].
FAQ: What molecular tools are available for detecting viral contaminants?
A range of molecular techniques is employed for viral screening, from traditional methods to next-generation diagnostics.
| Method | Principle | Application in Viral Screening |
|---|---|---|
| PCR/qRT-PCR [24] [53] | Amplifies viral DNA or RNA sequences. | Gold standard for specific virus detection (e.g., EBV, OvHV-2); highly sensitive and specific. |
| CRISPR-Based Assays [54] | Uses Cas proteins (e.g., Cas12, Cas13) with guide RNA for target recognition, triggering collateral cleavage of a reporter molecule. | Rapid, portable, and ultrasensitive detection; suitable for point-of-care use (e.g., SHERLOCK, DETECTR). |
| Immunoassays (ELISA) [53] | Detects viral antigens or host antibodies against viruses using enzyme-linked antibodies. | Useful for serosurveillance; detects immune response or viral proteins. |
| Next-Generation Sequencing (NGS) | Sequences all nucleic acids in a sample, enabling unbiased detection of known and unknown viruses. | Most comprehensive method; used for thorough panel testing and discovering novel contaminants. |
Detailed Protocol: CRISPR-Based Detection of Viral RNA
CRISPR/Cas systems have emerged as powerful tools for rapid and specific viral diagnostics [54]. The following protocol focuses on using the Cas13 protein for RNA virus detection.
- 1. Principle: The Cas13 protein, guided by a specific crRNA, binds to a target viral RNA sequence. Upon binding, its "collateral" or trans-cleavage activity is activated, indiscriminately degrading nearby single-stranded RNA (ssRNA) reporter molecules, which generates a detectable signal [54].
- 2. Sample Preparation: Extract total RNA from the cell culture sample. For increased sensitivity, couple the CRISPR assay with an isothermal pre-amplification step, such as Recombinase Polymerase Amplification (RPA) or Loop-Mediated Isothermal Amplification (LAMP), to amplify the viral RNA target [54].
- 3. CRISPR Reaction Setup: Combine the following in a reaction tube:
- Cas13 protein (e.g., from Leptotrichia wadei LwCas13a).
- crRNA designed to be complementary to the target viral RNA sequence.
- ssRNA reporter molecule (e.g., labeled with a fluorophore and quencher).
- The extracted and/or pre-amplified RNA sample.
- 4. Incubation and Detection: Incubate the reaction at 37°C (for LwCas13a) for 30-60 minutes. The signal can be measured in real-time on a plate reader or visualized at the endpoint with a lateral flow strip. Cleavage of the reporter molecule results in a fluorescent signal or a visible line on the strip.
The logical flow of how different CRISPR systems are selected based on the type of viral genetic material is outlined below:
Research Reagent Solutions for Viral Screening
| Reagent / Material | Function | Example / Specification |
|---|---|---|
| Cas Proteins [54] | Target and cleave specific viral nucleic acid sequences. | Cas9 (DNA), Cas12 (DNA), Cas13 (RNA). |
| Guide RNA (gRNA/crRNA) [54] | Directs the Cas protein to the complementary viral target sequence. | Synthetic RNA designed for the virus of interest (e.g., SARS-CoV-2, EBV). |
| Reporter Molecules [54] | Produce a signal upon collateral cleavage. | Fluorescent or colorimetric ssRNA (for Cas13) or ssDNA (for Cas12) probes. |
| Isothermal Amplification Mix [54] | Pre-amplifies viral nucleic acids to enhance detection sensitivity without complex thermocycling. | RPA or LAMP enzyme mixes and primers. |
Emerging Technologies and Future Directions
The field of contamination screening is evolving rapidly. A novel method developed by MIT and SMART CAMP researchers combines UV absorbance spectroscopy with machine learning [18] [40]. This technique measures the unique UV light "fingerprint" of cell culture fluids and uses a trained algorithm to recognize patterns associated with microbial contamination. It offers a label-free, non-invasive, and rapid (under 30 minutes) "yes/no" assessment, making it highly suitable for automated, real-time monitoring during the manufacturing of sensitive products like cell therapies [18] [40].
Effective management of mycoplasma and viral contamination is non-negotiable for ensuring the validity of cell culture-based research and the safety of biologics. While PCR remains a cornerstone for its sensitivity and specificity, emerging technologies like CRISPR-based assays and machine learning-powered spectroscopy promise even faster and more integrated solutions. Implementing a rigorous, routine screening program that utilizes these molecular tools is essential for any research or production facility dedicated to data integrity and product quality.
Building a Fortified Defense: Proactive Prevention and Decontamination Protocols
Core Principles and Troubleshooting
Fundamental Principles of Aseptic Technique in a BSC
Aseptic technique is a method that involves target-specific practices and procedures under suitably controlled conditions to reduce contamination from microbes. In the context of cell culture, it is a compulsory laboratory skill to ensure research reproducibility and the integrity of your cellular models [55]. Proper aseptic technique prevents culture contamination from microbes in the environment, such as those from the operator, lab benchtop, unsterilized equipment, and dust [55].
The Aseptic Non-Touch Technique (ANTT) framework provides a structured approach, built on four key principles [56]:
- Always wash hands effectively.
- Never contaminate key parts (any sterile part of equipment, like syringe tips or needle hubs).
- Touch non-key parts with confidence.
- Take appropriate infective precautions.
Troubleshooting Common Aseptic Technique Failures
Even with careful practice, issues can arise. The table below outlines common problems, their likely causes, and corrective actions.
Table 1: Troubleshooting Guide for Common Aseptic Technique Issues
| Problem | Potential Causes | Corrective Actions & Prevention |
|---|---|---|
| Rapid microbial contamination in cultures | - Unsterile reagents or media [57]- Compromised sterile equipment (e.g., cracked filters, damaged packaging) [57]- Improper hand hygiene or personal protective equipment (PPE) [55] [56] | - Visually inspect all items before use; use only properly autoclaved or pre-sterilized reagents [57].- Verify integrity of filters and packaging; do not use if damaged.- Perform effective handwashing and wear appropriate PPE (lab coat, gloves) [55] [58]. |
| Persistent mold or fungal growth | - Contaminated water bath [57]- Dirty incubator or storage area [57]- Inadequate disinfection of BSC interior or work surfaces [58] | - Use only sealed, sanitized vessels in water baths. Clean water baths regularly.- Establish a strict schedule for cleaning incubators and storage areas.- Decontaminate all readily accessible interior BSC surfaces with an appropriate disinfectant before and after work [58]. |
| Unexplained changes in cell morphology or physiology | - Mycoplasma contamination [59] | - Implement routine Mycoplasma testing for all cell lines upon receipt, during regular culture, and before critical experiments like high-throughput screening [59].- Immediately destroy contaminated stocks and source new ones from a reputable supplier. |
| Compromised BSC containment | - Disruption of the protective air barrier [58]- Blocked front grill or rear vents [58]- Rapid arm movements into/out of the cabinet [58] | - Allow the BSC to purge for at least 5 minutes before beginning work [58].- Work at least 4 inches inside the front grill. Do not block vents with arms or materials.- Minimize rapid movements and limit the number of times arms are moved in and out. |
Essential Experimental Protocols
Protocol 1: Routine Mycoplasma Testing
Background: Mycoplasma contamination is a major pitfall in tissue culture, with initial testing at some institutes revealing contamination rates exceeding 10% [59]. Because Mycoplasma can profoundly alter cellular biology and lead to irreproducible data without visible signs of infection, systematic testing is critical [59].
Methodology (Using a Commercial Detection Kit, e.g., MycoAlert):
- Sample Collection: Aseptically collect a sample of expended cell culture media from the culture vessel.
- Assay Principle: The assay couples the production of ATP by an endogenous Mycoplasma enzyme with a luciferase enzyme to produce a measurable chemiluminescent signal [59].
- Testing Schedule:
- Test all cell lines upon receipt before they are thawed into culture.
- Test all cell lines in regular culture at least once per month.
- Test cell lines immediately prior to critical experiments (e.g., high-throughput screening) [59].
- Response to Positive Results: Contaminated cell lines should be destroyed immediately. If possible, back-up frozen stock should be cultured and assessed. Decontaminate all work areas and equipment that may have been exposed [59].
Protocol 2: Weekly BSC Startup and Shutdown
Startup Procedure:
- Safety: Turn off any ultraviolet (UV) sterilizer. Never have the UV light on while working in the BSC, as it can cause eye and skin damage [58].
- Activation: Turn on the blower and cabinet illumination light.
- Purging: Allow the cabinet to run for at least 5 minutes to purge the system and establish the sterile airflow barrier [58].
- Surface Decontamination: Decontaminate all readily accessible interior surfaces with an appropriate disinfectant (e.g., 70% ethanol) [58].
Shutdown Procedure:
- Decontaminate and Remove: Decontaminate and remove all items from the interior work area.
- Final Surface Clean: Decontaminate interior surfaces once more with a suitable disinfectant [58].
- UV (if applicable): If a UV lamp is present and must be used, turn it on only after the cabinet is empty, the sash is closed, and the lab is unoccupied [58].
- Final Purge: Allow the cabinet to run for 5 minutes to purge contaminants from the system before turning off the blower [58].
Visual Workflow: Contamination Identification and Resolution
The following diagram outlines the logical workflow for identifying and addressing suspected contamination in cell culture, based on established laboratory protocols.
Frequently Asked Questions (FAQs)
Q1: Can I use a Bunsen burner inside my Biological Safety Cabinet for sterilization? A: No. Bunsen burners and other continuous flame devices are prohibited in biosafety cabinets [58]. The heat and turbulence from the flame disrupt the delicate laminar airflow that provides containment. Use safer alternatives like touch-plate microburners with a pilot light, small electric "furnaces," or pre-sterilized disposable loops [58].
Q2: How often should I replace the HEPA filter in my BSC or air purifier? A: Standard HEPA filters are not typically cleaned but replaced. They are not designed to be washed, as water can damage the delicate fiber mesh, compromising its 99.97% efficiency for 0.3-micron particles [60]. Some are marketed as "permanent" and can be gently vacuumed, but replacement is the standard and most reliable procedure. The exact replacement schedule depends on usage and environmental load and should be determined by regular certification and performance testing.
Q3: My cells are not contaminated, but their growth rate has suddenly changed. What should I investigate? A: Beyond microbial contamination, you should consider:
- Cell Line Authenticity: Perform Short Tandem Repeat (STR) profiling to rule out misidentification or cross-contamination with another, faster-growing cell line [59]. The HeLa cell line is a notorious example of a contaminant.
- Passage Number: High passage numbers can lead to senescence and reduced growth rates [57].
- Culture Conditions: Check the pH of your media, ensure your incubator is maintaining correct CO₂ levels and temperature, and confirm that your culture vessels are properly vented for gas exchange [57].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Aseptic Cell Culture
| Item | Function / Purpose | Key Considerations |
|---|---|---|
| 70% Ethanol | Primary disinfectant for spraying down all surfaces, equipment, and gloves before introducing them into the BSC [57]. | Effective concentration is critical; higher concentrations evaporate too quickly for optimal microbial kill. |
| Appropriate Cell Culture Media (e.g., DMEM, RPMI) | Provides essential nutrients, growth factors, and hormones for cell growth and maintenance [57]. | Must be supplemented with serum (e.g., FBS) and other additives like glutamine. Always use sterile, filtered media. |
| Mycoplasma Detection Kit | Routine monitoring for this common, invisible contaminant that can drastically alter experimental results [59]. | Kits are based on PCR or enzymatic assays (e.g., MycoAlert). Test upon receipt, monthly, and before key experiments. |
| Sterile, Individually Wrapped Pipettes | For handling media and reagents without introducing contamination. | Use each pipette only once to avoid cross-contamination. Never unwrap sterile pipettes outside the BSC [57]. |
| Personal Protective Equipment (PPE) | Protects the operator and the cell cultures. Includes lab coat, gloves, and safety glasses [55] [58]. | Gloves should be worn at all times and disinfected with 70% ethanol while working in the BSC. |
This technical support center addresses a critical dilemma in cell culture: the use of antibiotics to prevent microbial contamination versus their potential to mask underlying problems. While antibiotics can protect valuable cultures, their misuse can lead to silent contamination, altered cellular responses, and compromised data integrity. This guide provides troubleshooting advice and protocols to help researchers navigate these challenges within the broader context of microbial contamination research.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Q1: How can antibiotics mask contamination in my cell cultures?
Antibiotics can suppress bacterial or fungal growth without fully eliminating contaminants, creating a persistent, low-level infection that goes undetected. This "masking" effect occurs because:
- Incomplete Elimination: Antibiotics may only inhibit microbial reproduction rather than kill all contaminants, allowing persistent populations to survive [61].
- Undetectable Overgrowth: The suppression of visible signs (e.g., media turbidity, pH changes) prevents researchers from identifying contamination through routine microscopy [61].
- Mycoplasma Resistance: Standard antibiotics like Penicillin-Streptomycin are ineffective against Mycoplasma due to its lack of a cell wall, allowing it to persist undetected while inducing morphological changes and altering cellular metabolism [61] [62].
Troubleshooting Guide: If you suspect masked contamination:
- Culture your cells antibiotic-free for at least 2-3 passages.
- Use specialized detection methods like PCR-based tests for Mycoplasma.
- Submit samples for microbial culture to identify low-grade contaminants.
Q2: What are the proven effects of antibiotics on cell physiology and experimental outcomes?
Beyond masking contamination, antibiotics can directly influence cell biology, potentially skewing experimental data. Key effects include:
- Altered Gene Expression: Studies with HepG2 cells found over 200 genes were differentially expressed when cultured with Penicillin-Streptomycin, including genes involved in stress response and metabolism [61].
- Cytotoxic Effects: Gentamicin and Amphotericin B can impair membrane function and slow cell proliferation, particularly in sensitive cell types like stem cells [61].
- Morphological and Physiological Changes: Masked contaminants can induce changes in cell morphology, chromosome aberrations, and altered metabolic pathways [62].
Risk Mitigation Protocol:
- For sensitive assays (gene expression, epigenetics, phenotyping): Use antibiotic-free conditions.
- For long-term cultures: Maintain cultures without antibiotics to prevent gradual drift in cell characteristics.
- Validation requirement: Validate key findings in antibiotic-free conditions to confirm results are not artifactually influenced.
Q3: When is it scientifically justified to use antibiotics in cell culture?
Antibiotics are valuable tools when used intentionally rather than as a routine default. Justified scenarios include:
- Protecting Irreplaceable Cultures: Primary cells or valuable stocks during initial thawing and expansion [61] [62].
- High-Risk Situations: Working in shared incubators, training new personnel, or producing working stocks for critical experiments [61].
- Short-Term Protection: During primary cell culture establishment where contamination risk is highest [61].
Decision Framework:
- Assess the cost-benefit ratio for your specific experiment.
- Limit use to initial cell recovery phases when possible.
- Never use antibiotics as a substitute for proper aseptic technique.
Q4: What are the best practices for using antibiotics if they are necessary?
If antibiotics are required, follow these protocols to minimize risks:
Recommended Working Concentrations [61]
| Antibiotic | Common Stock Concentration | Working Concentration | Key Considerations |
|---|---|---|---|
| Penicillin-Streptomycin (Pen-Strep) | 100X (10,000 U/mL - 10 mg/mL) | 1X (100 U/mL - 100 µg/mL) | Synergistic combo; standard for Gram-positive/negative coverage |
| Gentamicin Sulfate | 50 mg/mL | 10–50 µg/mL | Broad-spectrum; monitor for cytotoxicity in sensitive lines |
| Amphotericin B | 250 µg/mL | 0.25–2.5 µg/mL | Antifungal; light-sensitive; higher doses can impact viability |
| Antibiotic-Antimycotic | 100X | 1X | Pre-mixed solution of Pen-Strep & Amphotericin B |
Usage Protocol:
- Preparation: Thaw antibiotic aliquots slowly on ice; avoid repeated freeze-thaw cycles.
- Addition: Add antibiotics to sterile media using aseptic technique after other supplements.
- Storage: Follow manufacturer recommendations; most require -20°C storage and protection from light.
- Duration: Limit continuous use to essential periods only (typically 1-2 weeks post-thaw).
Q5: How should I handle suspected Mycoplasma contamination?
Mycoplasma requires specialized approaches since standard antibiotics are ineffective [61].
Detection Protocol:
- PCR-Based Testing: Use commercial Mycoplasma detection kits for highest sensitivity.
- DNA Staining: Use Hoechst stain to visualize Mycoplasma DNA adherent to cell membranes.
- Microbiological Culture: Submit samples to specialized testing facilities.
Elimination Workflow:
Experimental Protocols for Contamination Control
Protocol 1: Antibiotic-Free Culture Transition
Purpose: Safely transition from antibiotic-dependent to antibiotic-free culture conditions to identify masked contamination.
Materials:
- Standard culture medium without antibiotics
- Phosphate buffered saline (PBS)
- Trypsin-EDTA or appropriate dissociation reagent
- Antibiotic-free fetal bovine serum (FBS)
Procedure:
- Split contaminated culture as usual, but use antibiotic-free medium.
- Passage cells every 2-3 days for at least 3 passages.
- Monitor media daily for turbidity, pH changes, or unusual precipitation.
- Examine cells daily under phase-contrast microscope for:
- Unusual granularity in cytoplasm
- Slow growth despite fresh media
- Unexpected cell death
- Changes in cell morphology
- If no contamination appears after 3 passages, cells are likely clean.
- If contamination appears, discard culture and decontaminate workspace.
Protocol 2: Mycoplasma Detection by PCR
Purpose: Detect Mycoplasma contamination with high sensitivity.
Materials:
- Commercial Mycoplasma PCR detection kit
- Sterile water (PCR-grade)
- Cell culture supernatant or washed cell pellet
- PCR tubes and thermal cycler
- Gel electrophoresis equipment
Procedure:
- Collect 100-200 µL of cell culture supernatant or cell pellet.
- Extract DNA according to kit manufacturer's instructions.
- Prepare PCR master mix with Mycoplasma-specific primers.
- Run PCR with appropriate positive and negative controls.
- Analyze products by gel electrophoresis.
- Positive samples show bands at expected sizes; compare to controls.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function | Application Notes |
|---|---|---|
| Penicillin-Streptomycin (100X) | Broad-spectrum bacterial coverage | First-line defense; synergistic combination [61] |
| Antibiotic-Antimycotic Solution (100X) | Combined bacterial & fungal protection | Contains Pen-Strep + Amphotericin B; convenient for mixed risk [61] |
| Gentamicin Sulfate | Broad-spectrum, especially Gram-negative | Stronger coverage than Strep; monitor cytotoxicity [61] |
| Amphotericin B | Antifungal agent | Targets yeast/fungal contamination; light-sensitive [61] |
| Mycoplasma Removal Reagent | Targeted Mycoplasma elimination | Use for confirmed infections; not for routine prevention [61] |
| Mycoplasma Detection Kit | PCR-based contamination screening | Essential for routine monitoring every 1-2 months [62] |
Strategic Decision Framework for Antibiotic Use
The following workflow outlines a systematic approach to determining when and how to use antibiotics in cell culture, balancing contamination control against experimental integrity.
Antibiotics remain valuable tools in cell culture when used intentionally and strategically, but they should never substitute for proper aseptic technique. By understanding the risks of masking contamination and implementing the protocols outlined in this guide, researchers can make informed decisions that protect both their cultures and the integrity of their scientific data. Regular monitoring and validation remain essential components of responsible cell culture practice.
Troubleshooting Guides
Microbial Contamination
Q: What are the common signs and sources of microbial contamination in cell cultures, and how can they be addressed?
Microbial contamination is a major challenge that can compromise cell culture integrity and research outcomes. The table below summarizes common contaminants, their identification methods, and recommended solutions [28].
| Contaminant Type | Key Characteristics | Identification Methods | Corrective Actions |
|---|---|---|---|
| Bacteria | Turbid culture media; sudden pH shift (yellow); observable under microscope [28] | Microscopy; microbiological cultures [28] | Discard culture; review and enhance aseptic technique [28]. |
| Fungi | Visible filamentous or fuzzy floating colonies [28] | Microscopy [28] | Discard culture; decontaminate incubator and work area [28]. |
| Mycoplasma | No visible change; subtle effects on cell growth/metabolism [28] | PCR-based assays; specific kits [28] | Discard affected cultures; use validated mycoplasma removal reagents; quarantine new cell lines [28]. |
| Virus | Often no visible signs; can alter cell phenotype [28] | PCR; antibody-based tests [28] | Discard culture; source cells from reputable banks [28]. |
Q: Are there novel methods for faster detection of microbial contamination?
Yes. Traditional sterility testing can take 7-14 days, which is problematic for time-sensitive applications like cell therapy [18]. A novel method uses ultraviolet (UV) absorbance spectroscopy combined with machine learning to provide a label-free, non-invasive contamination assessment in under 30 minutes [18]. This method detects patterns in how cell culture fluids absorb UV light, allowing for early detection and timely corrective actions during manufacturing [18].
Cell Bank Management
Q: What are the best practices for establishing and characterizing Master and Working Cell Banks (MCBs/WCBs) for GxP assays?
For cells used in analytical and bioanalytical test methods, a risk-based and product-phase-appropriate approach is recommended [63]. The goal is to ensure a consistent and reliable cell source.
- Documentation and Quality: While non-production cell banking activities are not required to be performed under GxP regulations, they must be documented with sound scientific principles and good documentation practices to support their future use in GxP methods [63].
- Risk-Based Characterization: The extent of initial cell line characterization should be based on risk [63].
- Low-Risk Cells (from reputable sources with documentation): Perform minimal testing, such as a mycoplasma check (e.g., by PCR) and confirmation of sterility and bioassay responsiveness [63].
- High-Risk Cells (without clear history or documentation): Consider additional testing like species identification by isoenzyme analysis, cell line authentication by Short Tandem Repeat (STR) profiling, and screening for adventitious agents [63].
- Feasibility Assessment: Before banking, conduct initial experiments to confirm the cell line performs as expected in your specific bioassay, with ideal performance including a signal-to-background ratio >5:1 and appropriate dose response [63].
Cell Health and Growth Issues
Q: My cells are not growing to confluency, and I have ruled out contamination. What could be the cause?
If contaminants are excluded, several factors related to reagents and handling can hinder cell growth [28]:
- Culture Media and Supplements: The quality, composition, and expiration of the culture media and supplements like Fetal Bovine Serum (FBS) are critical [28]. Use optimized formulations suitable for your cell type and ensure proper storage.
- Cryopreservation and Thawing: Inaccurate cell counts before freezing, improper freeze conditions, or incorrect thawing techniques can severely impact cell viability and recovery [28].
- Passaging Techniques: The use of detaching agents (e.g., trypsin) requires optimization. Over-digestion can damage cells, while an insufficient number of subculturing passages (passage number) or allowing cells to become over-confluent can also negatively affect growth [28].
Frequently Asked Questions (FAQs)
Q: How prevalent is cell line misidentification, and how can we prevent it? Recent studies suggest that misidentification or cross-contamination may affect up to a third of cell lines in use [28]. To prevent this:
- Source Responsibly: Obtain cell lines only from reputable cell banks (e.g., ECACC) [28].
- Label Meticulously: Maintain clear labeling and detailed logs of all cell culture vessels and cryovials [28].
- Authenticate Regularly: Periodically authenticate cell lines using methods like STR profiling [63].
Q: What are the critical steps for preventing contamination during routine cell culture?
- Aseptic Technique: Always use proper aseptic technique within a laminar flow hood, with sterilized equipment and reagents [64].
- Regular Monitoring: Inspect cultures daily under a microscope for any signs of contamination [28].
- Mycoplasma Testing: Routinely test cultures for mycoplasma, as it is a common, invisible contaminant [28].
- Lab Design: Maintain a dedicated, clean cell culture room with minimal traffic and appropriate biosafety level (BSL-2 or higher) practices [64].
Q: What should I do if my cells are dying in culture? First, rule out microbial contamination. If the culture is clean, investigate the following [28]:
- Cryopreservation Process: Review the viability of your frozen stock and the conditions under which it was frozen.
- Culture Conditions: Check for environmental stressors like incorrect temperature, CO₂ levels, or osmolarity [64].
- Handling Procedures: Assess passaging frequency, confluency at passaging, and potential over-digestion with dissociating enzymes like trypsin [28].
Experimental Protocols
Protocol 1: Routine Mycoplasma Detection by PCR
Objective: To detect the presence of mycoplasma DNA in cell culture samples. Background: Up to 30% of cell cultures are estimated to be contaminated with mycoplasma, which can alter cell behavior without causing turbidity in the media [28]. PCR is a fast and sensitive detection method.
Materials:
- Test Sample: Cell culture supernatant.
- Positive Control: DNA from a known mycoplasma species.
- Negative Control: Mycoplasma-free culture medium.
- PCR Master Mix: containing DNA polymerase, dNTPs, and buffer.
- Mycoplasma-Specific Primers: targeting a conserved genomic region.
- Thermal Cycler
- Gel Electrophoresis equipment
Method:
- Sample Collection: Collect 1 mL of cell culture supernatant from the test culture.
- DNA Extraction: Extract total DNA from the supernatant and controls using a commercial DNA extraction kit.
- PCR Setup: Prepare a PCR reaction mix for each sample and control as follows:
- 12.5 µL PCR Master Mix
- 1 µL Forward Primer (10 µM)
- 1 µL Reverse Primer (10 µM)
- 2 µL Template DNA
- 8.5 µL Nuclease-Free Water
- Total Volume: 25 µL
- PCR Amplification: Run in a thermal cycler using the following typical conditions:
- Initial Denaturation: 95°C for 5 minutes.
- 35 Cycles of:
- Denaturation: 95°C for 30 seconds.
- Annealing: 55°C for 30 seconds.
- Extension: 72°C for 1 minute.
- Final Extension: 72°C for 7 minutes.
- Analysis: Analyze the PCR products using agarose gel electrophoresis. A band in the test sample at the same size as the positive control indicates mycoplasma contamination.
Protocol 2: Novel UV-Spectroscopy with Machine Learning for Contamination Screening
Objective: To rapidly detect microbial contamination in cell therapy products within 30 minutes using UV absorbance and machine learning [18]. Background: This method measures the unique "fingerprint" of UV light absorption by contaminated cell culture fluids, providing an automated, label-free, and non-invasive screening tool [18].
Materials:
- Cell Therapy Product (CTP) or cell culture sample.
- UV Spectrophotometer
- Machine Learning Model: Pre-trained on UV absorbance data from sterile and contaminated cultures.
- Sterile Cuvettes
Method:
- Sample Loading: Aseptically transfer a small aliquot of the cell culture fluid into a sterile cuvette.
- UV Absorbance Measurement: Place the cuvette in the spectrophotometer and measure the absorbance across a defined UV wavelength range (e.g., 220 nm - 300 nm).
- Data Processing: The absorbance spectrum is fed into the pre-trained machine learning algorithm.
- Result Interpretation: The model analyzes the pattern and provides a definitive "yes/no" assessment of contamination.
- Action: If a "yes" (contaminated) result is obtained, initiate corrective actions and confirm with a secondary method. A "no" result allows the manufacturing process to continue, saving critical time [18].
Workflow Visualization
Traditional vs. Novel Contamination Detection
Cell Bank Establishment and Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for maintaining contamination-free cell cultures and reliable cell banks [28] [64] [63].
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Optimized Culture Media (e.g., DMEM, RPMI-1640) | Provides essential nutrients for cell growth and proliferation. | Select formulations (e.g., with or without phenol red) based on cell type and experimental needs [28]. |
| Fetal Bovine Serum (FBS) | Rich supplement containing growth factors and hormones. | Batch testing is critical for consistency; heat-inactivation may be required [28]. |
| Antibiotics (e.g., Penicillin-Streptomycin) | Helps prevent bacterial contamination. | Should not be used as a substitute for aseptic technique. Use may be discouraged for certain critical cultures [28]. |
| Dimethylsulfoxide (DMSO) | Cryoprotective agent for freezing cells. | Reduces ice crystal formation to maintain cell viability during cryopreservation [64]. |
| Trypsin/EDTA | Detaching agent for adherent cells. | An enzyme used to dissociate cells from the culture vessel surface for subculturing. Avoid over-digestion [64]. |
| PCR Kits for Mycoplasma | Sensitive detection of mycoplasma DNA. | Essential for routine, high-sensitivity screening of this common contaminant [28]. |
| Cell Authentication Kits (e.g., STR Profiling) | Confirms cell line identity and purity. | Critical for preventing and detecting cross-contamination and misidentification [63]. |
Within cell culture microbial contamination research, a fundamental dichotomy exists in control strategies between research laboratories and Good Manufacturing Practice (GMP) facilities. While both environments share the common goal of maintaining aseptic conditions, their underlying priorities—data integrity versus patient safety and regulatory compliance—dictate profoundly different approaches to contamination control [65]. This technical support center outlines these differentiated strategies, providing researchers and drug development professionals with targeted troubleshooting guides and FAQs to navigate these distinct challenges.
Contamination Control: Research vs. GMP at a Glance
The table below summarizes the core differences in objectives, focus, and primary risks that shape contamination control strategies in these two settings.
| Aspect | Research Laboratories | GMP Manufacturing |
|---|---|---|
| Primary Objective | Ensure data integrity and reproducibility for scientific studies [65]. | Ensure patient safety, product quality, and batch consistency [65]. |
| Regulatory Focus | Often follows internal or grant-enforced guidelines; focus on scientific standards. | Strict adherence to regulatory standards (e.g., FDA, EMA) and cGMP guidelines [65] [66]. |
| Primary Contamination Risk | Microbial contamination (bacteria, fungi, yeast), cross-contamination between cell lines, and mycoplasma [65]. | All microbial contamination, viral contamination, and particulate matter in injectable products [65]. |
| Typical Action on Contamination | Discard contaminated culture, decontaminate areas, and restart experiments [65]. | Full root cause investigation, batch quarantine/rejection, and formal deviation reporting to regulators [65]. |
Frequently Asked Questions (FAQs)
Q1: In our research lab, we occasionally use antibiotics in our culture media. Is this considered a best practice?
A: While antibiotics can be useful for specific short-term experiments, their continuous use as a prophylactic measure is not recommended. This practice can mask low-level, persistent contaminations, promote the development of antibiotic-resistant microbes, and can have unintended effects on cell physiology, ultimately compromising data integrity. Best practice relies on strict aseptic technique in a contaminant-free environment.
Q2: What is the most overlooked source of contamination in a research setting?
A: Cross-contamination with other cell lines is a frequently overlooked threat. In shared research environments, the use of non-dedicated reagents, inadequate cleaning procedures, or simple mislabeling can lead to rapid overgrowth by fast-growing cell lines like HeLa. This misidentification can invalidate years of research [65]. Regular cell line authentication is a critical prevention strategy.
Q3: Why is particulate contamination such a critical concern in GMP manufacturing when it doesn't involve growing microbes?
A: In GMP, particularly for injectable biologics, particulate matter poses a direct risk to patient safety. Regulations like USP 788 strictly limit particulates in injections. These particles can originate from bioreactor components, tubing, or the environment and, if injected, can cause vascular and immune reactions [65].
Q4: We are a research lab planning to transition a process to GMP. What is the single biggest change in mindset we should prepare for?
A: The biggest shift is from a culture of "finding out and fixing" to one of "preventing and proving." In GMP, every process, from equipment cleaning to environmental monitoring, must be rigorously validated, meticulously documented, and proven to be in a state of control before production begins. Documentation and traceability are as important as the product itself.
Troubleshooting Guides
Problem: Persistent Bacterial Contamination in Research Cultures
Question: My cell cultures repeatedly show cloudy media and a rapid drop in pH, indicating bacterial contamination. I've already checked my aseptic technique. What should I investigate next?
Investigation Guide:
- Check Your Reagents: Thaw a fresh aliquot of culture medium, filter it using a 0.2 µm filter, and culture it alone (without cells) for several days. If contamination appears, the source is your medium, serum, or supplement [65].
- Audit Your Equipment: Check the water bath and incubator for contamination. Clean and disinfect the water bath and replace the water regularly. Place a dedicated pan of water in the incubator rather than leaving plates or flasks open in a humid atmosphere.
- Test Your Cell Stock: Thaw a new vial of cells from your frozen stock. If the contamination persists, the master cell bank itself may be contaminated. You will need to authenticate your cell line and possibly replace it from a clean source [65].
- Screen for Mycoplasma: While bacteria are visible, co-contamination with mycoplasma is common. Perform a PCR or fluorescence-based assay to rule it out, as it requires different eradication strategies [65].
Problem: Positive Sterility Test Batch in GMP Manufacturing
Question: A batch of our final drug product has failed its sterility test. What are the immediate and required actions from a GMP compliance perspective?
Action Workflow:
Detailed Actions:
- Immediate Quarantine & Investigation: The entire batch must be immediately quarantined and isolated. A formal investigation is launched to determine the root cause, which must be documented [65].
- Root Cause Analysis (RCA): The RCA is a multi-faceted process. It involves reviewing environmental monitoring data (air and surface samples) from the production period, investigating personnel practices and aseptic technique, testing retained samples of all raw materials and components, and validating the sterilization cycles of all equipment used [65] [66].
- Decontamination: The entire production suite and any associated equipment must undergo a validated decontamination procedure before production can resume.
- Regulatory Reporting: The failure and the results of the investigation are a mandatory reportable event to the relevant health authority (e.g., FDA). The batch record must document the deviation and the decision to reject the batch [65].
- Corrective and Preventive Actions (CAPA): Based on the RCA, specific CAPA must be implemented, such as revising Standard Operating Procedures (SOPs), enhancing staff training, or improving environmental controls, to prevent recurrence.
Essential Experimental Protocols
Protocol 1: Routine Mycoplasma Detection via PCR (For Research Labs)
Principle: This method detects mycoplasma-specific DNA sequences with high sensitivity and speed, ideal for routine screening of cell cultures.
Materials & Reagents:
- Template DNA: Extracted from candidate cell culture supernatant.
- Mycoplasma PCR Primer Mix: Specific primers targeting conserved bacterial 16S rRNA genes.
- PCR Master Mix: Contains Taq polymerase, dNTPs, and buffer.
- Positive Control: DNA from a known mycoplasma strain.
- Negative Control: Nuclease-free water.
- Thermal Cycler & Gel Electrophoresis Equipment.
Procedure:
- Sample Collection: Culture cells without antibiotics for at least 3 days. Collect 500 µL of cell culture supernatant.
- DNA Extraction: Use a commercial DNA extraction kit to purify DNA from the supernatant.
- PCR Setup: Prepare a reaction mix per the table below. Include positive and negative controls.
- Amplification: Run in a thermal cycler: (a) 95°C for 5 min; (b) 35 cycles of: 95°C for 30s, 55°C for 30s, 72°C for 1 min; (c) 72°C for 7 min.
- Analysis: Analyze PCR products by agarose gel electrophoresis. A band in the test sample, compared to the positive control, indicates mycoplasma contamination.
Protocol 2: Single-Use System (SUS) Integrity Test (For GMP Manufacturing)
Principle: Before use, single-use bioreactor bags or fluid transfer assemblies must be inspected for leaks or defects that could compromise sterility.
Materials & Reagents:
- Single-Use System (Bioreactor bag, tubing assembly, etc.)
- Pressure Decay Test Instrument
- Compressed Air or Nitrogen Supply
Procedure:
- Pre-Use Inspection: Visually inspect the SUS for any visible punctures, tears, or defects in the film and seams.
- System Setup: Connect the SUS to the pressure decay tester according to the manufacturer's instructions. Ensure all ports are correctly sealed.
- Pressurization: Pressurize the system to the specified test pressure (provided in the component's quality control certificate, typically a low pressure like 0.5-1.0 bar).
- Soak & Monitor: Isolate the system and start the test timer. The instrument will monitor pressure for a defined duration (e.g., 5-10 minutes).
- Pass/Fail Criteria: The test is validated and passed if the pressure decay over the test period is less than the predefined threshold. Any failure requires the SUS to be quarantined and reported, and a new unit must be used.
The Scientist's Toolkit
Table: Key Reagent Solutions for Contamination Control
| Item | Function/Brief Explanation |
|---|---|
| Ficoll-Paque Density Gradient Medium | A solution for isolating mononuclear cells (e.g., lymphocytes, monocytes) from whole blood with high purity, minimizing granulocyte and red blood cell contamination [67]. |
| 0.1 - 0.2 µm Sterilizing Grade Filters | Used for the final filtration of cell culture media, buffers, and other heat-labile solutions to remove bacteria and fungi, ensuring sterility [65]. |
| Matrigel Matrix | A basement membrane extract used to support the growth and differentiation of cells in 3D culture, creating a more in vivo-like environment [68]. |
| PCR Kits for Mycoplasma Detection | Ready-to-use kits containing optimized primers and master mixes for the sensitive and specific detection of mycoplasma contamination in cell cultures via PCR [65]. |
| Closed System Bioprocess Containers | Single-use, pre-sterilized bags and tubing assemblies that form a closed fluid path, eliminating the risk of contamination from the environment during medium preparation and bioprocessing [65]. |
FAQs on Cell Culture Contamination Response
1. How do I identify a microbial contamination in my cell culture?
Regular observation of your cultures, both with the naked eye and under a microscope, is the first line of defense. The table below summarizes the common indicators for different types of contaminants [69] [70].
| Contaminant Type | Macroscopic Observations (Naked Eye) | Microscopic Observations | Other Indicators |
|---|---|---|---|
| Bacteria | Culture medium appears cloudy (turbid); a thin film may be present on the surface [69] [70]. | Tiny, shimmering granules between cells [69]. | Sudden, rapid drop in the pH of the medium (yellow in phenol red) [69] [70]. |
| Yeast | Culture medium appears turbid, especially in advanced stages [69]. | Ovoid or spherical particles that may bud off smaller particles [69]. | Little change in pH initially; pH usually increases when contamination becomes heavy [69]. |
| Mold | Fuzzy, filamentous clumps floating in the medium or on cells [69]. | Thin, wispy filaments (hyphae) or denser clumps of spores [69]. | pH is stable initially, then increases rapidly with heavy contamination [69]. |
| Mycoplasma | No change in medium turbidity or pH; culture appears normal [7] [71]. | No visible change; requires specialized detection methods [69] [71]. | Chronic poor cell health, unexplained effects on cellular processes [69] [71]. |
2. What are the immediate steps I should take upon discovering contamination?
Your immediate response should focus on containment to prevent the spread to other cultures [69].
- Isolate the Contaminated Culture: Immediately remove the contaminated flask or dish from the incubator and cell culture hood [69].
- Decontaminate Equipment: Clean the incubator and laminar flow hood with a laboratory disinfectant (e.g., 70% ethanol) and check HEPA filters [69] [7].
- Do Not Discard Valuable Cultures Immediately: If the contaminated culture is irreplaceable, you may attempt decontamination after isolation [69].
3. Can I use antibiotics to save a contaminated culture?
The use of antibiotics and antimycotics is generally discouraged as a routine practice and should only be used as a last resort for short-term applications [69].
- Risks: Continuous use can lead to the development of antibiotic-resistant strains, allows low-level cryptic contaminants (like mycoplasma) to persist, and the antibiotics themselves can be toxic to cells and interfere with your experiments [69].
- If Attempted: If you must attempt to rescue a valuable culture, you must first determine the toxic concentration of the antibiotic for your cell line and then use a concentration one- to two-fold lower for a limited number of passages [69].
4. How can I prevent future contamination events?
Prevention is the most effective strategy for managing cell culture contamination and relies on consistent aseptic technique [7].
- Personal Practice: Always wear a clean lab coat and gloves dedicated to the cell culture room. Frequently spray gloves with 70% ethanol. Do not share media bottles between users [7].
- Workspace Management: Thoroughly clean the biological safety cabinet with 70% ethanol before and after all work. Work in a clean, uncluttered area [7].
- Routine Quality Control: Obtain cell lines from reputable cell banks and periodically authenticate them to rule out cross-contamination [69] [71]. Routinely test cultures for mycoplasma [69].
Troubleshooting Guide: Decontamination of an Irreplaceable Culture
For a valuable, contaminated culture, the following protocol can be attempted. This procedure is adapted from general guidance on decontaminating cell cultures [69].
Workflow for Culture Decontamination
Objective: To eliminate microbial contamination from a precious cell line without causing irreversible damage to the cells.
Materials Required:
- Contaminated cell culture
- Appropriate growth medium (without antibiotics)
- The selected antibiotic or antimycotic
- Multi-well culture plate or several small flasks
- Enzymatic or chemical cell detachment agent (for adherent cells)
- Centrifuge tubes, serological pipettes
Methodology:
- Identify and Isolate: Confirm the type of contaminant and immediately isolate the culture [69].
- Prepare Cells: Dissociate, count, and dilute the cells in antibiotic-free medium to the concentration used for regular passaging [69].
- Dispense and Dose: Dispense the cell suspension into a multi-well plate. Add your chosen antibiotic to each well across a range of concentrations [69].
- Determine Toxicity: Observe the cells daily for signs of toxicity, such as sloughing, appearance of vacuoles, decrease in confluency, and cell rounding. The goal is to identify the concentration at which the antibiotic becomes toxic to your cells [69].
- Treat Cultures: Culture the cells for two to three passages using the antibiotic at a concentration one- to two-fold lower than the toxic concentration determined in the previous step [69].
- Antibiotic-Free Phase: Culture the cells for one passage in antibiotic-free media [69].
- Re-treat (Optional): Repeat the treatment cycle (step 5) once [69].
- Confirm Eradication: Finally, culture the cells in antibiotic-free medium for 4 to 6 passages. Monitor carefully to determine if the contamination has been permanently eliminated [69].
The Scientist's Toolkit: Essential Reagents for Contamination Control
| Item | Function / Purpose |
|---|---|
| 70% Ethanol | A standard laboratory disinfectant used for decontaminating surfaces, gloves, and equipment within the biological safety cabinet to maintain an aseptic work environment [7]. |
| Antibiotics & Antimycotics | Chemical agents used to inhibit or kill bacterial and fungal contaminants. They should be used judiciously and not as a routine culture additive [69]. |
| DMSO (Dimethyl Sulfoxide) | A cryoprotective agent used in freezing media to protect cells from ice crystal formation and osmotic shock during the cryopreservation process [70]. |
| Phenol Red | A pH indicator added to most culture media. A color change (red to yellow) indicates acidification of the medium, which can be a sign of bacterial contamination or overgrowth of cells [70]. |
| Trypsin / Detachment Agent | An enzyme used to dissociate adherent cells from the culture vessel surface for subculturing or during the decontamination protocol [70]. |
| Cryovials | Specially designed tubes for the long-term storage of frozen cell stocks in liquid nitrogen, preserving valuable, uncontaminated cell lines [70]. |
Ensuring Data Integrity: Validation, Authentication, and Technique Comparison
The Critical Role of Cell Line Authentication and STR Profiling
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What is the gold standard method for authenticating human cell lines? Short Tandem Repeat (STR) profiling is the internationally recognized gold standard for human cell line authentication [72] [73] [74]. This method analyzes specific regions of the genome containing short, repeating DNA sequences that are highly variable between individuals. The resulting STR profile serves as a unique genetic fingerprint for the cell line, allowing for unambiguous identification [72] [74].
Q2: How often should I authenticate my cell lines? It is recommended to perform STR authentication when a new cell line enters the cell bank and routinely during long-term culture [73]. For cells in continuous culture, STR profiling should be repeated every 3-6 months or after 5-10 passages to monitor for cross-contamination or genetic drift [73]. Regular testing is crucial because cross-contamination affects an estimated 16-35% of cell cultures [72] [75].
Q3: My STR results show an 85% match to the reference profile. Is my cell line authentic? Interpreting a match depends on the algorithm used. The table below summarizes the two main algorithms and their interpretation thresholds [76]:
| Algorithm | Similarity Score | Interpretation |
|---|---|---|
| Tanabe Algorithm | ≥ 90% | Related (same donor) |
| 80% - 90% | Ambiguous/Mixed | |
| < 80% | Unrelated | |
| Masters Algorithm | ≥ 80% | Related (same donor) |
| 60% - 80% | Ambiguous/Mixed | |
| < 60% | Unrelated |
An 85% match would be considered related (authentic) using the Masters algorithm but ambiguous and requiring further investigation using the stricter Tanabe algorithm [76]. At least eight STR loci are typically used to establish identity [72].
Q4: Can STR profiling detect all types of contamination? No. STR profiling is highly effective for detecting intra-species cross-contamination (e.g., one human cell line contaminating another) but has limitations [73] [74]. Its sensitivity threshold is approximately 10%, meaning low-level contamination may not be detected [73]. Furthermore, it does not identify microbial contaminants like bacteria, yeast, fungi, or mycoplasma, nor does it detect chemical contaminants or viruses [26] [77] [75]. A comprehensive quality control program should include specific tests for these contaminants.
Q5: Are there specific STR guidelines for mouse cell lines? Yes, mouse cell line authentication requires a different approach. Due to the inbred nature of laboratory mice, their genetic diversity is low, and different match criteria apply [78] [73]. A multiplex PCR assay has been validated with 18 mouse STR loci and two human markers (to screen for human cell contamination) [78] [73]. Because STR profiles from different mouse cell lines of the same strain can show over 80% similarity, results should be supplemented with data on cell background, growth characteristics, and phenotype [73].
Troubleshooting Common STR Profiling Issues
Problem: Inconsistent STR allele calls between laboratories.
- Cause: This is often due to difficulties in interpreting PCR artifacts, particularly "stutter peaks," which are small peaks caused by polymerase slippage during amplification [78].
- Solution: Implement standardized stutter filters and interpretation rules. For example, one consensus guideline is to call a peak in the -4 stutter position as a true allele if its stutter ratio is greater than 20%, and a peak in the +4 position if the ratio is above 10% [78]. Consistent use of allelic ladders and software analysis tools is also critical.
Problem: Suspected low-level cross-contamination not definitively confirmed by STR.
- Cause: STR profiling has a sensitivity limit; contamination below ~10% may not generate significant peak alterations in the profile [73].
- Solution: Continue subculturing the cells without antibiotics for 3-5 more passages and re-test [73]. If a contaminating population is present, it may expand to a detectable level. Also, ensure your analysis software is not automatically filtering out low-intensity peaks.
Problem: Cell line shows a new allele not present in the original STR profile.
- Cause: This indicates genetic alteration, which could be due to chromosomal mutation or, if multiple new alleles appear, contamination with another cell line [76] [73].
- Solution: First, re-authenticate the cell line after 3-5 passages to confirm the result [73]. Compare the new profile to databases of common cell lines to rule out cross-contamination. If it is a unique, stable genetic change, it may represent a clonal evolution or genetic drift, and a new reference profile should be established [76].
Experimental Protocols
Detailed Methodology: STR Profiling of Human Cell Lines
The following protocol details the core steps for authenticating human cell lines via STR profiling [72] [76].
1. Sample Preparation and DNA Extraction
- For Adherent Cells: Remove culture medium, rinse the cell monolayer with PBS, and dissociate the cells using trypsin-EDTA or another dissociation reagent. Wash the cell pellet and resuspend in PBS [72].
- DNA Extraction: Extract genomic DNA using a commercial kit, such as the QIAamp DNA Blood Mini Kit. Quantify the DNA concentration using a fluorometer (e.g., Qubit) [76].
2. STR Amplification by PCR
- PCR Reaction: The PCR mix contains fluorescently labeled primers that target specific STR loci. A common approach is to use a commercial multiplex kit that co-amplifies several STRs (e.g., 8, 13, or 23 markers) in a single reaction [72] [76].
- Thermal Cycling: Transfer the reaction plate to a thermal cycler and run the recommended protocol. After amplification, samples can be stored at 4°C [72].
3. Detection and Analysis
- Capillary Gel Electrophoresis: The amplified PCR products are separated by size using capillary gel electrophoresis. Internal size standards are added to the samples for precise fragment sizing [72] [76].
- Genotype Calling: Software (e.g., GeneMapper) compares the size of DNA fragments with internal standards and an allelic ladder to convert the data into specific alleles for each STR locus [72].
The workflow below summarizes the authentication process.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function / Application | Example / Note |
|---|---|---|
| STR Multiplex Kit | Simultaneously amplifies multiple STR loci in a single PCR reaction. | Kits are available for human (e.g., 23-plex), mouse (19-plex), and other species [76] [78]. |
| DNA Extraction Kit | Ishes high-quality, pure genomic DNA from cell samples. | QIAamp DNA Blood Mini Kit [76]. |
| Fluorometer | Accurately quantifies DNA concentration, which is critical for successful PCR. | Qubit fluorometer [76]. |
| Thermal Cycler | Equipment used to perform the PCR amplification under controlled temperature cycles. | Gene Amp 9700 or Veriti thermal cycler [79]. |
| Genetic Analyzer | Separates fluorescently labeled PCR fragments by size via capillary electrophoresis. | Classic 116 Genetic Analyzer or similar [76]. |
| Analysis Software | Sizes DNA fragments, calls alleles, and compares profiles to references. | GeneMapper ID-X software [72]. |
| FTA Cards | A classic method for the stable storage of DNA samples from cell spots. | Used to spot 200,000 cells in PBS for storage and later punching of disks for PCR [72]. |
Data Presentation
Quantitative Data on Contamination and STR Match Interpretation
Table 1: Common Cell Culture Contaminants and Detection Methods
| Contaminant Type | Common Examples | Key Detection Methods |
|---|---|---|
| Microbial | ||
| Bacteria | E. coli, Staphylococcus sp., Bacillus sp. | Visual inspection (turbidity, pH drop), microscopy [26] [77] [75]. |
| Mycoplasma | M. orale, M. fermentans, M. arginini | PCR, fluorescent staining, ELISA. Note: Difficult to detect by microscopy [26] [80] [75]. |
| Fungi/Yeast | Candida sp., Aspergillus sp., Penicillium sp. | Visual inspection (cloudy media, clumps), microscopy [26] [77] [75]. |
| Viruses | Hepatitis viruses, Retroviruses | PCR, ELISA, immunostaining [26] [77]. |
| Cellular (Cross-Contamination) | HeLa, other fast-growing cell lines | STR Profiling, karyotyping, isoenzyme analysis [72] [77] [75]. |
Table 2: STR Profile Match Interpretation Guidelines
This table consolidates the quantitative thresholds for interpreting STR matches, which are critical for troubleshooting authentication results [72] [76].
| Similarity Match Score | Tanabe Algorithm Interpretation | Masters Algorithm Interpretation |
|---|---|---|
| ≥ 90% (Tanabe)≥ 80% (Masters) | Related: The query and reference cell lines are likely from the same donor [76]. | Related: The query and reference cell lines are likely from the same donor [76]. |
| 80% - 90% (Tanabe)60% - 80% (Masters) | Ambiguous/Mixed: The result is inconclusive and requires further investigation [76]. | Ambiguous/Mixed: The result is inconclusive and requires further investigation [76]. |
| < 80% (Tanabe)< 60% (Masters) | Unrelated: The query and reference cell lines are from different donors [76]. | Unrelated: The query and reference cell lines are from different donors [76]. |
The following diagram illustrates the logical decision process for authenticating a cell line based on its STR profile.
Troubleshooting Guides and FAQs
Q1: My cell culture does not look cloudy, but the cells are exhibiting unexplained metabolic changes and slow growth. What could be the cause and how can I confirm it?
This is a classic sign of mycoplasma contamination [29] [26]. Unlike many bacteria, mycoplasma does not cause turbidity in the media and is too small (0.15–0.3 µm) to be seen with routine microscopy [29]. To confirm:
- DNA Staining: Use a fluorescent DNA stain (e.g., DAPI or Hoechst) and look for extranuclear DNA on the cell surface under a fluorescence microscope [29].
- PCR-Based Testing: Perform a targeted PCR assay for mycoplasma DNA. This is a highly sensitive and specific method [29].
- Commercial Kits: Use specialized mycoplasma detection kits, which are considered essential for routine screening [29].
Q2: I need to screen cell therapy products quickly during manufacturing. What is the fastest available method for a sterility check?
A novel method using UV absorbance spectroscopy combined with machine learning can provide a definitive yes/no contamination assessment within 30 minutes [18]. This method is:
- Label-free and non-invasive, eliminating the need for cell extraction or staining.
- Automation-friendly, allowing for continuous monitoring during manufacturing.
- Designed as a preliminary rapid screen, with positive results triggering confirmatory testing [18].
Q3: What is the most definitive method to confirm a positive screening test for microbial contamination?
Liquid Chromatography-Mass Spectrometry (LC-MS/MS) is widely regarded as the gold standard for confirmatory testing [81]. It provides:
- Unmatched specificity and sensitivity, capable of identifying and quantifying specific contaminants at parts-per-billion (ppb) levels.
- Definitive compound identification, which is essential for regulatory compliance and legal defensibility [81]. While it is costly and requires expert personnel, it is the reference method for verifying results from rapid screens like lateral flow tests or microbial inhibition assays [81].
Q4: How can I detect viral contaminants that do not cause visible changes in the cell culture?
Viral contamination often requires specialized techniques since many viruses do not cause clear cytopathic effects [24]. Detection methods include:
- Polymerase Chain Reaction (PCR): A standard method for detecting viral DNA or RNA with high sensitivity. It can identify both active and latent viruses like Epstein-Barr virus (EBV) [24].
- Observation of Cytopathic Effects (CPE): For some viruses, you can observe morphological changes under a microscope, such as cell rounding, syncytia formation, and cell lysis [24].
- Next-Generation Sequencing (NGS): This method allows for the broad identification of unknown viral contaminants by sequencing all genetic material in a sample [82].
Comparative Analysis of Detection Methods
The table below summarizes the key characteristics of common microbial detection methods, providing a benchmark for sensitivity, speed, and cost.
| Method | Typical Time to Result | Sensitivity / Accuracy | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Rapid Strip Tests (Lateral Flow) [81] | 5 - 15 minutes | Qualitative at Maximum Residue Limit (MRL); excellent for targeted classes (e.g., β-lactams). | Fastest and cheapest; ideal for on-site, yes/no decisions. | Limited to one antibiotic or contaminant class per strip. |
| Microbial Inhibition Tests [81] | 2 - 3 hours | Broad-spectrum but may be less sensitive for some drugs. | Low-cost, wide coverage of antibacterial agents. | Too slow for immediate product release; risk of false positives. |
| ELISA (Lab Immunoassay) [81] | 1 - 2 hours | Semi-quantitative; high sensitivity below MRL for target compounds. | High throughput; good for quantitative trend monitoring. | Requires lab setup and trained personnel; class-specific. |
| UV Spectroscopy with Machine Learning [18] | ~30 minutes | Provides rapid, automated contamination assessment. | Label-free, non-invasive, and amenable to automation. | Emerging technology; model requires training with diverse contaminants. |
| PCR-Based Methods (qPCR) [82] | Several hours | Highly specific detection of low-level DNA targets; quantitative. | High specificity and sensitivity; real-time results. | Requires specialized equipment and reagents; risk of false positives from contamination. |
| LC-MS / HPLC [81] | 4 - 8 hours+ | Fully quantitative and definitive; gold standard for identification. | Unmatched specificity and legal defensibility; multi-residue panels. | Highest cost; requires sophisticated instruments and expert analysts. |
Detailed Experimental Protocols
Protocol 1: Machine Learning-Aided UV Absorbance Spectroscopy for Early Contamination Detection
This protocol outlines a novel, rapid method for detecting microbial contamination in cell therapy products [18].
1. Principle: Microbial contamination alters the biochemical composition of the cell culture fluid, changing its UV light absorption profile. A machine learning model is trained to recognize these unique "fingerprints" for a rapid yes/no assessment [18].
2. Reagents and Equipment:
- Cell culture fluid sample
- UV absorbance spectrophotometer
- Pre-trained machine learning model (algorithm)
- Data processing unit
3. Procedure:
- Step 1: Collect a small aliquot of cell culture fluid from the bioreactor or culture vessel without invasive extraction.
- Step 2: Transfer the sample to a cuvette and place it in the UV spectrophotometer.
- Step 3: Measure the UV absorbance spectrum across a defined wavelength range.
- Step 4: Input the spectral data into the trained machine learning algorithm.
- Step 5: The algorithm analyzes the pattern and returns a contamination probability, providing a "yes/no" output typically within 30 minutes [18].
4. Key Notes:
- This method is intended as a preliminary, rapid screening tool.
- Any positive result should be confirmed with a standard, validated method like LC-MS.
- The model's robustness increases when trained on a wide range of microbial contaminants and cell types [18].
Protocol 2: Digital Droplet PCR (ddPCR) for Absolute Quantification of Microbial Load
This protocol is for applications requiring high-precision quantification of specific microbial contaminants, such as in bioprocess validation [82].
1. Principle: A PCR reaction is partitioned into thousands of nanoliter-sized droplets. Each droplet acts as an individual PCR reactor, allowing for absolute quantification of the target DNA molecule without the need for a standard curve [82].
2. Reagents and Equipment:
- Sample DNA extract
- ddPCR supermix (including DNA polymerase, primers, and probes)
- Droplet generator
- Thermal cycler
- Droplet reader
3. Procedure:
- Step 1: Prepare the PCR reaction mix containing the sample DNA, supermix, and target-specific primers/Probe.
- Step 2: Generate thousands of droplets from the reaction mix using a droplet generator.
- Step 3: Transfer the droplets to a PCR plate and run a standard PCR amplification protocol.
- Step 4: After amplification, read each droplet in a droplet reader to determine if it contains the fluorescent signal (positive) or not (negative).
- Step 5: Calculate the absolute concentration of the target DNA in the original sample based on the ratio of positive to negative droplets using Poisson statistics [82].
4. Key Notes:
- ddPCR is particularly advantageous for detecting rare targets present at very low concentrations and is less susceptible to PCR inhibition compared to qPCR [82].
- The initial setup cost for ddPCR is high, and multiplexing capabilities are more limited than in qPCR [82].
Method Selection Workflow
The following diagram illustrates a logical pathway for selecting an appropriate detection method based on key decision points.
Research Reagent Solutions
The table below lists key reagents and materials essential for implementing the discussed detection methodologies.
| Item | Function/Brief Explanation |
|---|---|
| Fluorescent DNA Stains (DAPI/Hoechst) [29] | Used to stain extranuclear DNA for visualizing mycoplasma contamination under a fluorescence microscope. |
| Mycoplasma Detection Kits [29] | Commercial kits (often based on PCR or enzymatic activity) designed for specific, sensitive, and routine screening of mycoplasma. |
| Lateral Flow Strips [81] | Immunoassay-based strips for rapid, on-site detection of specific antibiotic classes or microbial antigens. |
| qPCR Master Mix [82] | Optimized reagents containing DNA polymerase, dNTPs, and buffers for quantitative real-time PCR amplification. |
| Microbial Growth Media (e.g., for Geobacillus stearothermophilus) [81] | Used in microbial inhibition assays; contains nutrients and a pH indicator to detect antibacterial activity by a color change. |
| LC-MS/MS Solvents and Columns [81] | High-purity chromatographic solvents and analytical columns essential for separating and analyzing compounds in the mass spectrometer. |
FAQs: USP <788> and Particulate Matter
What is the purpose of USP <788>? USP <788> is a critical quality standard that sets limits for subvisible particulate matter in injectable drugs (parenterals). Its primary purpose is to ensure patient safety by minimizing the risk of adverse reactions, such as inflammation, blockages in blood vessels, or other complications that can occur if particles are introduced into the bloodstream [83] [84] [85]. It applies to all parenteral formulations, from small-volume vials to large-volume infusion bags [85].
My injectable product is a therapeutic protein. Does USP <788> still apply? While USP <788> can be applied to therapeutic protein injections, there is a more specific chapter, USP <787>, which is tailored to the unique challenges of protein therapies. Protein therapies often contain fragile protein aggregates that can be difficult to analyze and are considered higher risk for patient safety. USP <787> is based on the light obscuration method but allows for a wider range of sample volumes (1-25 mL) and strongly prefers light obscuration over membrane microscopy for analysis [86].
What are the acceptance criteria for particulate matter under USP <788>? The acceptance criteria depend on the container volume and the testing method used. The limits are harmonized with the European (EP) and Japanese (JP) Pharmacopoeias, making them a global benchmark [85] [86] [87].
Table 1: USP <788> Acceptance Criteria for Particulate Matter
| Container Volume | Test Method | Particle Size ≥10 µm | Particle Size ≥25 µm |
|---|---|---|---|
| > 100 mL (LVP) | Light Obscuration | ≤ 25 per mL | ≤ 3 per mL |
| ≤ 100 mL (SVP) | Light Obscuration | ≤ 6,000 per container | ≤ 600 per container |
| > 100 mL (LVP) | Microscopic Particle Count | ≤ 12 per mL | ≤ 2 per mL |
| ≤ 100 mL (SVP) | Microscopic Particle Count | ≤ 3,000 per container | ≤ 300 per container |
When should I use the microscopic particle count test (Method II) instead of light obscuration (Method I)? Light obscuration (Method I) is the preferred and primary method [83]. However, you should use the microscopic particle count test (Method II) in the following situations [83] [86]:
- The product is too viscous to be analyzed by light obscuration.
- The product has reduced clarity or is an opaque emulsion.
- The sample contains air bubbles or emulsion droplets that could be misinterpreted as particles by the light obscuration sensor.
- To validate results if a sample fails the light obscuration test. Note: Method II cannot be used to "pass" a batch that has failed Method I [86].
How is USP <788> testing relevant to my research on cell culture and biologics? For cell culture and biologics research, controlling subvisible particles is crucial for both process development and final product quality. Particulate matter can act as a foreign substance that triggers unwanted immune responses in patients [88]. In the context of cell and gene therapies, which are comprised of living cells, the product itself consists of particles. This makes distinguishing desirable cells from undesirable particulate contamination a significant analytical challenge [89]. Adhering to USP <788> principles during research and development helps build a foundation for quality and safety, facilitating a smoother transition to commercial manufacturing and regulatory approval.
Troubleshooting Guide for USP <788> Compliance
Problem 1: High Particle Counts in Light Obscuration Test
Potential Causes and Solutions:
Cause: Air Bubbles or Emulsion Droplets. The instrument cannot distinguish these from solid particles [83].
- Solution: Degas the sample prior to analysis or use the microscopic particle count test (Method II), which allows bubbles and emulsions to pass through the filter [83].
Cause: Product Formulation. Viscous, opaque, or low-volume samples may not be suitable for light obscuration [83] [86].
- Solution: Switch to the microscopic particle count test (Method II), which offers more flexibility for complex samples [83].
Cause: Genuine Particulate Contamination. The particles may originate from raw materials, the container-closure system, or the manufacturing process itself [85] [88].
Problem 2: Different Results Between Method I and Method II
Explanation and Solution:
It is expected that the microscopic method (Method II) will yield lower counts for the same sample compared to light obscuration (Method I). This is because the membrane filtration process used in Method II can remove some "soft" particles like protein aggregates and silicone oil droplets [86]. This is also reflected in the stricter acceptance criteria for Method I [87].
- Solution: This is not necessarily an error. Ensure you are using the correct acceptance criteria for the method you are applying, as shown in Table 1.
Problem 3: Challenges with Cell and Gene Therapy Products
Specific Issues and Solutions:
Challenge: The product is living. Traditional sterilization methods would destroy the therapy, and the product cells themselves can be mistaken for particulates [89].
- Solution: Focus on contamination prevention through closed and automated manufacturing systems. For analysis, techniques like flow imaging microscopy may be used with product-specific algorithms to distinguish therapeutic cells from contaminants [89].
Challenge: Slow and manual testing methods. The standard sterility and mycoplasma tests can take weeks, which is incompatible with autologous therapies where a patient is waiting [89].
- Solution: Investigate rapid microbial methods (RMMs) and molecular techniques like PCR (Polymerase Chain Reaction) and next-generation sequencing (NGS), which can provide faster results for microbial contamination [89].
Experimental Protocol: Microscopic Particle Count Test (Method II)
This protocol is a general guide based on USP <788>. For official compliance, refer to the complete chapter in the United States Pharmacopeia.
1. Principle: The sample is filtered through a membrane filter, which captures particulate matter. The membrane is then examined under a microscope, and particles equal to or larger than 10 µm and 25 µm are counted and sized by comparison to calibrated reference circles on a graticule [83].
2. Materials and Equipment:
- Membrane filter assembly (filter holder, vacuum source)
- Graticule (calibrated for 10 µm and 25 µm circles), verified according to USP requirements [83]
- Microscope (e.g., Nikon Eclipse Ci POL) [83]
- Particulate-free water and cleaning materials
3. Procedure:
- Preparation: Clean the filtration apparatus meticulously with particulate-free water.
- Filtration: Under a laminar flow hood, pour a measured volume of the sample into the filter funnel and apply a vacuum. The volume used must be sufficient to yield a statistically valid count but must not overload the membrane.
- Rinsing: Rinse the container and filter funnel with particulate-free water to ensure all particles are transferred to the membrane.
- Drying and Mounting: Carefully remove the membrane filter and allow it to dry. Place it on a glass microscope slide, optionally using a petri dish for protection.
- Microscopic Examination: Place the slide on the microscope stage. Systematically scan the entire filtered area of the membrane. For each particle observed, compare its longest dimension to the 10 µm and 25 µm reference circles on the graticule [83].
- Counting: Count and record the number of particles that are ≥10 µm and ≥25 µm.
4. Calculation: Calculate the number of particles per container for each size class based on the sample volume filtered and the total container volume.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Equipment for USP <788> Compliance
| Item | Function | Key Considerations |
|---|---|---|
| Liquid Particle Counter (e.g., AccuSizer A7000 SIS) | Automates particle counting and sizing via Light Obscuration (Method I) [83]. | Must be validated every 6 months per USP <788> using NIST-traceable standards like Count-Cal particles [90]. |
| Microscope with USP Graticule (e.g., Nikon Eclipse Ci POL) | Essential for Manual Microscopic Particle Count (Method II) [83]. | Must be equipped with a USP-verified graticule for accurate particle sizing against 10µm and 25µm standards [83]. |
| Membrane Filters | Used to capture particles from the solution for Method II analysis [83]. | Pore size and membrane material must be suitable for the product and not introduce interference. |
| Count-Cal Validation Particles | Used for semi-annual calibration of liquid particle counters [90]. | Thermo Scientific particles with accuracy of 3000/ml ±10% are a common standard for ensuring sensor accuracy [90]. |
| Particulate-Free Water | Used for dilutions, rinsing apparatus, and as a blank [90]. | Critical for preventing background contamination that could skew results. |
| Flow Imaging Microscope (e.g., FlowCam, Halo Labs Aura+) | An orthogonal technique for root cause analysis; captures images of particles for identification [88] [86]. | Not a compendial method, but invaluable for investigating failures by determining particle type and source [86]. |
Within the critical field of cell culture and advanced therapy medicinal products (ATMPs), ensuring sterility is paramount. Microbial contamination compromises research integrity and poses a severe risk to patient safety in cell-based therapies. Traditional sterility tests, while established, are often slow, creating a critical bottleneck. This case study examines the performance of a novel method—machine learning-aided UV absorbance spectroscopy—alongside other emerging technologies, and contrasts them with traditional assays for detecting microbial contamination in cell cultures.
FAQ: Addressing Researcher Questions on Contamination Detection
Q1: What are the most common types of microbial contamination in cell cultures, and why are they problematic?
Cell culture media is nutrient-rich, making it susceptible to various biological contaminants [26]. The most common include:
- Bacteria: One of the most frequent contaminants; often causes turbidity (cloudiness) and a sudden drop in the pH of the culture medium [69]. Under a microscope, they appear as tiny, moving granules [69].
- Mycoplasma: An intracellular bacterium that is particularly problematic because it often goes unnoticed for many passages without causing turbidity. Its presence can alter cell properties, including growth, metabolism, and morphology [26].
- Fungi: This category includes yeasts and molds. Yeast contamination can also cause turbidity, with the pH usually increasing in advanced stages [69]. Mold appears as thin, filamentous mycelia under microscopy [69].
- Viruses: As obligatory intracellular parasites, viruses can be difficult to detect without specific methods like PCR or immunostaining, posing a potential health hazard to laboratory personnel [69].
Q2: My cell culture looks cloudy. What is the fastest way to confirm if it's contaminated?
Visual inspection for turbidity and microscopic examination are the fastest initial steps.
- Visual Check: A cloudy culture and an unexplained, rapid shift in pH are strong indicators of bacterial or yeast growth [69].
- Microscopy: Under a low-power microscope, bacteria appear as tiny, shimmering granules between your cells. Higher magnification can resolve their shape (e.g., rod-shaped E. coli) [69]. Yeasts appear as ovoid or spherical particles that may bud off smaller particles [69].
Q3: What are the key limitations of traditional sterility tests like the USP <71>?
The United States Pharmacopeia (USP) chapter <71> is the gold standard but has significant drawbacks for fast-paced applications like cell therapy manufacturing [44] [18]:
- Long Incubation Time: It requires an incubation period of up to 14 days to detect contamination [44] [18].
- Labor-Intensive: The process is manual and requires skilled workers for procedures like sample extraction and visual inspection for turbidity [18].
- Limited Suitability for ATMPs: The method was designed for large-batch pharmaceuticals, not for cell therapy products with short shelf-lives, where a 14-day wait can be detrimental to patient treatment [44].
Q4: How does the novel UV spectroscopy method work, and what are its main advantages?
The novel method uses UV absorbance spectroscopy combined with machine learning [44] [18].
- Principle: It measures the absorbance of ultraviolet light by the cell culture fluid. Microbial contamination alters the metabolic composition of the medium (e.g., through changes in metabolites like nicotinic acid and nicotinamide), creating a unique "fingerprint" in the UV absorbance spectrum [44].
- Machine Learning: A one-class support vector machine (SVM) model is trained on the UV absorbance spectra of known sterile samples. It then learns to recognize spectral anomalies that indicate contamination [44].
- Key Advantages:
Troubleshooting Guide: Microbial Contamination Detection
Problem: Slow detection of contamination is delaying critical cell therapy product release.
Solution: Evaluate and implement rapid microbiological methods (RMMs).
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1 | Assess Contamination Risk | Identify the stage of contamination: early (low microbial load) or advanced (turbidity). Traditional methods are unsuitable for rapid, early detection [44]. |
| 2 | Select an Appropriate Method | Compare novel and traditional methods based on your needs for speed, sensitivity, and workflow. See the performance comparison table below. |
| 3 | Validate the Chosen Method | Conduct a dose-response test if using antibiotics for decontamination to determine levels toxic to your cell line [69]. For UV spectroscopy, train the model on your specific sterile culture conditions [44]. |
| 4 | Implement and Monitor | Integrate the new method into your manufacturing process. For instance, use UV spectroscopy for continuous, at-line monitoring and reserve slower, compendial methods only for final release if required [18]. |
Performance Comparison: Traditional vs. Novel Detection Methods
The table below summarizes the quantitative performance of various microbial contamination detection methods.
| Method | Time-to-Detection (for < 10 CFUs) | Key Advantages | Key Limitations |
|---|---|---|---|
| Compendial USP <71> [44] | ~24 hours | Gold standard; required for final product release in many regions. | Long incubation (up to 14 days); labor-intensive; not ideal for cell therapies [44] [18]. |
| BACT/ALERT 3D [44] | ~16 hours | Automated continuous monitoring; shorter than USP <71>. | Requires growth enrichment; complex process [44]. |
| Machine Learning-Aided UV Spectroscopy [44] [18] | ~21 hours (10 CFUs E. coli); result in < 30 mins after sampling | Very fast output; label-free; non-invasive; low cost; simple workflow; easy to automate [44] [18]. | Lower sensitivity vs. some RMMs; model requires training on sterile samples; can be influenced by donor-specific media components [44]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) [44] | ~18 hours | High sensitivity and specificity. | Expensive equipment; requires specialized technical expertise. |
| In Vivo Confocal Microscopy (for specific pathogens) [91] | Minutes after sample preparation | High sensitivity for fungi and acanthamoeba; provides visual confirmation. | Specialized, expensive equipment; primarily used in diagnostic settings like keratitis [91]. |
| Droplet Digital PCR (ddPCR) [92] | Several hours (includes PCR run time) | Extremely high sensitivity (can be 1000x more sensitive than conventional PCR); absolute quantification without a standard curve [92]. | Targets specific DNA sequences; requires knowledge of the contaminant; does not distinguish between live and dead cells. |
Experimental Protocol: Machine Learning-Aided UV Absorbance Spectroscopy
This protocol is adapted from the method described in Scientific Reports (2025) [44] [18].
Objective: To detect microbial contamination in mesenchymal stromal cell (MSC) culture supernatants using UV absorbance spectroscopy and a one-class support vector machine (SVM) model.
Research Reagent Solutions & Essential Materials
| Item | Function in the Experiment |
|---|---|
| Cell Culture Supernatant (e.g., from MSCs) | The sample matrix to be tested for contamination. |
| Phosphate Buffered Saline (PBS) | Used as a diluent and for preparing negative control samples. |
| Tryptic Soy Broth (TSB) or similar | Microbial growth medium for preparing positive controls. |
| Reference Microbial Strains (e.g., E. coli K-12) | Used to spike samples for positive controls and model validation. |
| UV-Transparent Cuvette (e.g., Quartz) | Essential for accurate UV absorbance measurements, as plastic and glass absorb UV light [93]. |
| UV-Vis Spectrophotometer | Instrument to measure the absorbance of light by the sample across UV wavelengths. |
Methodology:
- Sample Preparation:
- Negative Controls: Prepare sterile samples by spiking MSC culture supernatant with PBS.
- Positive Controls: Spike fresh culture media (e.g., DMEM) with a high inoculum (e.g., 1000 CFUs) of a reference microbe like E. coli.
- Test Samples: Spike MSC culture supernatant with a low inoculum (e.g., 10 CFUs) of the test microorganism.
- Instrument Setup:
- Data Acquisition (Training Phase):
- Measure the UV absorbance spectra (e.g., across 200-400 nm) of multiple, known sterile (negative control) samples.
- This data forms the training set for the machine learning model.
- Machine Learning Model Training:
- Train a one-class SVM model using the absorbance spectra from the sterile samples only.
- The model learns the "fingerprint" of a sterile sample and will later identify test samples that deviate from this norm as anomalies (i.e., contaminated).
- Testing and Validation:
- Collect test samples at regular intervals (e.g., every 3 hours) post-inoculation.
- Measure their UV absorbance spectra and input the data into the trained one-class SVM model.
- The model will classify each sample as "sterile" or "contaminated." Contamination is typically detected when the model predicts all positive control samples as contaminated and all negative controls as sterile with high accuracy (e.g., 100%) [44].
The emergence of rapid methods, particularly machine learning-aided UV spectroscopy, addresses a critical need in modern biomanufacturing and cell therapy. While traditional assays like USP <71> remain the regulatory gold standard, their prolonged time-to-detection is incompatible with the timelines of personalized cell therapies.
Recommendations for Researchers:
- For Routine, High-Throughput Screening: Implement machine learning-aided UV spectroscopy as a powerful, preliminary, and continuous monitoring tool to detect contamination early in the process, enabling timely corrective actions [18].
- For Ultimate Sensitivity and Pathogen Identification: Use molecular methods like ddPCR or sequencing for final product validation or when investigating specific contaminants, as they offer unparalleled sensitivity and specificity [92].
- A Combined Approach is Optimal: The most robust strategy involves using rapid methods like UV spectroscopy for in-process control throughout manufacturing, followed by a traditional or highly sensitive molecular method for final product release, ensuring both speed and comprehensive safety assurance.
Implementing a Robust and Validated Contamination Screening Program
Frequently Asked Questions (FAQs)
1. What are the most common types of cell culture contamination? Cell culture contamination can be broadly categorized into biological contaminants, which include bacteria, fungi, viruses, and mycoplasma, as well as chemical contaminants like endotoxins. Biological contamination can lead to wasted time, resources, and affect data quality and product safety [68].
2. What are the primary sources of biological contamination in my cell cultures? Sources include non-sterile supplies/media, poor aseptic technique, contaminated air in the laboratory environment, and the operators themselves. Raw materials and in-process testing strategies should be implemented to control these sources [68].
3. How can I minimize the risk of endotoxin contamination in my cultures? Best practices to reduce endotoxin risk include using high-quality water and reagents, employing proper sterilization techniques, and following strict handling procedures. Specific guidelines are available in technical resources from leading life science suppliers [68].
4. What is the difference between sterilization and disinfection in cell culture? Sterilization eliminates all microbial life, including bacterial spores, often through methods like autoclaving, filtration, or radiation. Disinfection reduces pathogenic microorganisms to levels considered safe, but may not eliminate all spores [94].
5. When should I use antibiotics in my cell culture media? Antibiotics can be added to control bacterial and fungal contaminants, but proper aseptic technique and media handling can often make their continuous use unnecessary. They should be considered a supplement to, not a replacement for, good sterile technique [94].
Troubleshooting Guides
Bacterial Contamination
Table 1: Troubleshooting Bacterial Contamination
| Observation | Possible Cause | Corrective Action |
|---|---|---|
| Cloudy culture medium; pH shift (yellow) [68] | Non-sterile technique, contaminated reagents | Discard culture, review aseptic technique, test media and reagents for sterility [68] [94] |
| Rapid pH change in medium | High bioburden from source | Use sterile filtration (0.22 µm) on liquids, autoclave when possible [94] |
| Bacterial colonies under microscope | Airborne contamination, poor cabinet technique | Decontaminate work area, review biosafety cabinet practices, ensure proper operation [68] |
Fungal Contamination
Table 2: Troubleshooting Fungal/Yeast Contamination
| Observation | Possible Cause | Corrective Action |
|---|---|---|
| Fuzzy, filamentous structures or oval particles in medium | Spores in laboratory environment | Discard culture, decontaminate incubators and work areas, filter air supply if necessary |
| Culture viscosity changes | Widespread fungal growth | Review sterile technique, avoid simultaneous microbiological work in same area |
Mycoplasma Contamination
Table 3: Addressing Mycoplasma Contamination
| Aspect | Details |
|---|---|
| Detection Challenge | Cannot be seen microscopically; requires specialized tests [68] |
| Common Sources | Cross-contamination from infected cultures, contaminated reagents (especially serum) [68] [94] |
| Prevention | Quarantine new cell lines, use mycoplasma-free serum, regular testing [94] |
| Confirmation Tests | PCR, ELISA, fluorescent staining, microbial culture [68] |
Experimental Protocols for Contamination Control
Protocol 1: Media Preparation and Sterilization
Purpose: To prepare sterile cell culture media while maintaining nutritional components and preventing contamination introduction.
Materials:
- Media powder or liquid concentrate
- High-quality water (deionized/distilled)
- pH meter and adjustment solutions
- Sterile filtration unit (0.22 µm)
- Sterile containers
Procedure:
- Dissolution: Dissolve media powder in the appropriate volume of high-quality water per manufacturer's instructions [94].
- pH Adjustment: Adjust pH using sterile acid/base solutions while monitoring with a calibrated pH meter [94].
- Final Volume: Bring to final volume with water and mix thoroughly without creating excessive foam [94].
- Sterile Filtration: Filter sterilize through a 0.22 µm membrane filter into sterile containers [94].
- Quality Control: Perform sterility checks by incubating aliquots at appropriate temperatures [68].
- Storage: Store prepared media at 4°C, protected from light, and use within expiration period [94].
Protocol 2: Routine Sterility Testing of Cell Cultures
Purpose: To regularly screen cell cultures for microbial contamination without visible signs.
Materials:
- Test cell culture
- Sterile broth media (for bacterial/fungal growth)
- Mycoplasma testing kit (PCR-based recommended)
- Incubators set at different temperatures
Procedure:
- Sample Collection: Aseptically remove 1-2 mL of culture medium without cells [68].
- Broth Inoculation:
- Incubation:
- Mycoplasma Testing:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Contamination Control
| Reagent/Category | Function | Application Notes |
|---|---|---|
| Classical Media (DMEM, RPMI-1640) | Supports cell growth; base for experiments [94] | Choose based on cell type; supplement appropriately [94] |
| Antibiotic/Antimycotic Solutions | Inhibits bacterial/fungal growth [94] | Use selectively; continuous use may mask contamination [94] |
| Sterile Filtration Systems | Removes microorganisms from heat-sensitive solutions [94] | 0.22 µm pore size for bacteria; 0.1 µm for mycoplasma [94] |
| Animal Serum (FBS) | Provides growth factors and nutrients [94] | Source of contamination; test for sterility and mycoplasma [94] |
| Trypsin/ dissociation reagents | Passaging adherent cells [94] | Filter sterilize; quality varies by vendor [94] |
| Cryopreservation Media | Long-term storage of cell lines [68] | Proper freezing/thawing protocols affect viability and contamination risk [68] |
Contamination Screening Workflow
Proactive Contamination Prevention Strategy
Conclusion
Safeguarding cell cultures from microbial contamination is a multi-faceted challenge that requires a blend of rigorous foundational practices and the adoption of innovative technologies. The integration of advanced methods like machine learning with UV spectroscopy and VOC analysis promises a future of faster, non-invasive, and automated contamination monitoring, which is crucial for the timely delivery of cell therapies and the reproducibility of research. Moving forward, a proactive, validated, and integrated approach—combining strict aseptic technique, routine authentication, and cutting-edge detection—will be paramount in accelerating biomedical discovery and ensuring the safety and efficacy of clinical applications derived from cell culture systems.
References
- 1. : How to Prevent Fungal, Yeast... | Corning Cell Culture Contamination [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/how-to-control-bacterial-contamination-and-other-unwelcome-micro.html]
- 2. Avoiding Cell Culture in the Lab | Technology Networks Contamination [https://www.technologynetworks.com/neuroscience/infographics/detecting-and-preventing-cell-culture-contamination-405162]
- 3. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/AO/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination]
- 4. | Thermo Fisher Scientific - TR Cell Culture Contamination [https://www.thermofisher.com/tr/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 5. Find out how to eliminate common contaminants such as mycoplasma... [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/animal-cell-culture/contamination/contamination]
- 6. Microbial Preventing in Contamination : Key Detection... Cell Cultures [https://www.cytion.com/Knowledge-Hub/Blog/Preventing-Microbial-Contamination-in-Cell-Cultures-Key-Detection-Strategies/]
- 7. Techniques and Practices to Avoid Cell by... Culture Contamination [https://app.jove.com/t/64769/cell-culture-techniques-practices-to-avoid-contamination-fungi]
- 8. A New Sensitive Method for the Detection of Mycoplasmas Using... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6952905/]
- 9. Prevention, Diagnosis and Eradication of Mycoplasma ... Contamination [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668599/]
- 10. of Mycoplasma | Lonza contamination cell cultures [https://bioscience.lonza.com/lonza_bs/CH/en/mycoplasma-contamination-in-cell-culture]
- 11. Types of Cell Culture Contamination and How... | Technology Networks [https://www.technologynetworks.com/cell-science/articles/types-of-cell-culture-contamination-and-how-to-prevent-them-397776]
- 12. | ATCC Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 13. Metabolomics reveals mycoplasma interferes with the... contamination [https://link.springer.com/article/10.1007/s00216-016-9525-9]
- 14. Accelerate your Mycoplasma Testing - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/bioprocessing-accelerate-your-mycoplasma-testing/]
- 15. Rapid and sensitive Mycoplasma detection in antibody bioprocessing ... [https://pubmed.ncbi.nlm.nih.gov/40267574/]
- 16. of Mycoplasma : Incidence, sources... contamination cell cultures [https://pubmed.ncbi.nlm.nih.gov/19003295/]
- 17. How to detect a yeast in your cell culture - Eppendorf... contamination [https://www.eppendorf.com/rs-en/lab-academy/life-science/cell-biology/how-to-detect-a-yeast-contamination-in-your-cell-culture/]
- 18. Novel method detects microbial contamination in cell cultures | MIT News | Massachusetts Institute of Technology [https://news.mit.edu/2025/novel-method-detects-microbial-contamination-smart-0425]
- 19. A method for early detection and identification of fungal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6456197/]
- 20. Microfluidic System for Rapid Detection of Airborne Pathogenic... [https://pubmed.ncbi.nlm.nih.gov/30264565/]
- 21. Preventing and Avoiding Cell Culture Contamination [https://www.technologynetworks.com/cell-science/how-to-guides/preventing-and-avoiding-cell-culture-contamination-299231]
- 22. of Virus - A biotechnological view contaminations cell cultures [https://pubmed.ncbi.nlm.nih.gov/19003296/]
- 23. Culture Cell Contamination Troubleshooting [https://www.sigmaaldrich.cn/CN/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination]
- 24. Frontiers | Viral in contamination : analyzing the impact of... cell culture [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 25. Risk Mitigation Strategies: Key Considerations in the Viral ... Prevention [https://www.slideshare.net/slideshow/viral-risk-mitigation-strategies-key-considerations-in-the-prevention-and-detection-of-viral-contamination-79898083/79898083]
- 26. Microbial and viral of animal and... - MedCrave online contamination [https://medcraveonline.com/JSRT/microbial-and-viral-contamination-of-animal-and-stem-cell-cultures-common-contaminants-detection-and-elimination.html]
- 27. : How to Prevent Fungal, Yeast... | Corning Cell Culture Contamination [https://www.corning.com/emea/en/products/life-sciences/resources/stories/at-the-bench/how-to-control-bacterial-contamination-and-other-unwelcome-micro.html]
- 28. Troubleshooting Cell Culture [https://www.sigmaaldrich.com/KE/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting]
- 29. Troubleshooting Cell Culture Contamination [https://www.sigmaaldrich.com/KR/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination]
- 30. , Containment, and Correction... | Corning Cell Culture Contamination [https://www.corning.com/au/en/products/life-sciences/resources/stories/at-the-bench/cell-contamination-containment-and-correction-good-cell-culture-practices-in-3d.html]
- 31. How to prevent in contamination | INTEGRA cell culture [https://www.integra-biosciences.com/china/en/stories/tips-preventing-contamination-cell-culture]
- 32. : 5 Common Cell and How to Prevent... Culture Contamination Sources [https://www.capricorn-scientific.com/knowledge-center/cell-culture-contamination]
- 33. to Guide Sterility Testing - Certified Laboratories USP 71 [https://certified-laboratories.com/blog/step-by-step-guide-to-usp-71-sterility-testing-methods/]
- 34. Sterility Testing Services | USP Investigations 71 Microbe [https://microbe-investigations.com/usp-71-sterility-testing/]
- 35. A Comparison Study of Quantitative PCR and... | Research Square [https://www.researchsquare.com/article/rs-1497117/v1]
- 36. Comprehensive Evaluation of Compendial USP < 71 >, BacT/Alert... [https://pubmed.ncbi.nlm.nih.gov/30541938/]
- 37. The USP Testing Specifications Master Guide [https://www.surebiochem.com/guide/the-usp-testing-specifications-master-guide]
- 38. of Two Comparison for Use in Assessing Culture ... Methods Microbial [https://pmc.ncbi.nlm.nih.gov/articles/PMC4733207/]
- 39. in Quality Rapid of Sterile... | Mabion Microbiological Methods Control [https://www.mabion.eu/science-hub/articles/rapid-microbiological-methods-in-quality-control-of-sterile-drugs/]
- 40. SMART researchers develop novel UV and... - PharmiWeb.com [https://www.pharmiweb.com/press-release/2025-04-14/smart-researchers-develop-novel-uv-and-machine-learning-aided-method-to-detect-microbial-contamination-in-cell-cultures]
- 41. Micro Rapid Transform Pharma EM Methods [https://www.pharmanow.live/microbiology-insights/rapid-micro-methods-pharma-em]
- 42. / BACT | Pioneering Diagnostics ALERT ® 3 D [https://www.biomerieux.com/us/en/our-offer/clinical-products/bact-alert-3d-automated-system.html]
- 43. BACT/ALERT® 3D [https://www.biomerieux-diagnostics.com/bact-alert-3d-microbial-detection-systems-overview]
- 44. aided Machine for microbial... learning UV absorbance spectroscopy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11880552/]
- 45. Researchers Pioneer a New Way to Detect Microbial Contamination in... [https://currentsciencedaily.com/stories/628012105-researchers-pioneer-a-new-way-to-detect-microbial-contamination-in-cell-cultures]
- 46. Visible UV : Principles, Methods & Applications Spectroscopy [https://www.vedantu.com/chemistry/uv-visible-spectroscopy]
- 47. Use of GC - IMS for detection of volatile organic compounds to identify... [https://amb-express.springeropen.com/articles/10.1186/s13568-022-01367-0]
- 48. Nontargeted Volatile Metabolite Screening and Microbial ... [https://pubmed.ncbi.nlm.nih.gov/38386844/]
- 49. Contamination: Where Does It Come From and How to... Mycoplasma [https://blog.addgene.org/mycoplasma-contamination-where-does-it-come-from-and-how-to-prevent-it]
- 50. A PCR protocol to establish standards for routine mycoplasma testing... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10192841/]
- 51. DNA probes and PCR in diagnosis of mycoplasma infections [https://pubmed.ncbi.nlm.nih.gov/7700272/]
- 52. CRISPR Screening : Molecular for Studying Tools –Host... Virus [https://pmc.ncbi.nlm.nih.gov/articles/PMC8618713/]
- 53. Medical viruses : diagnostic techniques | Virology Journal | Full Text [https://virologyj.biomedcentral.com/articles/10.1186/s12985-023-02108-w]
- 54. Frontiers | Next-Generation Molecular Diagnostics Development by... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.582499/full]
- 55. The Basic Concept of Microbiology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7123386/]
- 56. 4.3 Aseptic – Nursing Skills – 2e Technique [https://wtcs.pressbooks.pub/nursingskills/chapter/4-3-asceptic-technique/]
- 57. - Step by Step Guide Cell Culture [https://www.assaygenie.com/cell-culture-guide-techniques-and-protocols/]
- 58. Biological Safety Cabinets : Usage Guidelines [https://blink.ucsd.edu/safety/research-lab/biosafety/containment/bsc/usage.html]
- 59. Keeping it clean: the cell quality culture experience at the... control [https://pmc.ncbi.nlm.nih.gov/articles/PMC8506661/]
- 60. How to Clean a HEPA and What You Should Know... - Molekule Filter [https://molekule.com/blogs/all/how-to-clean-a-hepa-filter-and-what-you-should-know-beforehand]
- 61. in Cell Culture: When and How to Use Them Antibiotics [https://www.capricorn-scientific.com/knowledge-center/antibiotics-in-cell-culture]
- 62. Why Use Antibiotics in Cell Culture? [https://www.sigmaaldrich.com/GB/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/antibiotics-in-cell-culture]
- 63. Recommendations for Cell Used in GXP Assays Banks [https://www.bioprocessintl.com/cell-therapies/recommendations-for-cell-banks-used-in-gxp-assays]
- 64. Culture Basics: Cell , Fundamentals... | Technology Networks Equipment [https://www.technologynetworks.com/cell-science/articles/cell-culture-basics-equipment-fundamentals-and-protocols-348413]
- 65. Cell culture challenges: Contamination & prevention - Green Elephant Biotech [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 66. Application of the principles of good manufacturing practices (GMP) to the design and operation of a tissue culture laboratory | Methods in Cell Science [https://link.springer.com/article/10.1007/BF02388260]
- 67. 推荐单核细胞 标 分离方法 准 [https://www.sigmaaldrich.cn/CN/zh/technical-documents/protocol/clinical-testing-and-diagnostics-manufacturing/hematology/recommended-standard-method]
- 68. 解决 细 案 | 胞 应用 | 康宁 培 养 方 细 胞 培 养 [https://www.corning.com/cn/zh/products/life-sciences/applications/cell-culture.html]
- 69. 污染 | Thermo Fisher Scientific - CN 细 胞 培 养 [https://www.thermofisher.cn/cn/zh/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 70. and maintenance Cell | Abcam culture protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 71. | SpringerLink Cell Culture Contamination [https://link.springer.com/protocol/10.1385/1-59259-406-9:309]
- 72. Human Cell by Line Authentication STR Profiling [https://www.news-medical.net/life-sciences/Human-Cell-Line-Authentication-by-STR-Profiling.aspx]
- 73. : The Gold Standard for Ensuring Cell Identity STR Authentication Cell [https://www.linkedin.com/pulse/cell-str-authentication-gold-standard-ensuring-identity-pricella-gzymc]
- 74. of Human Authentication Through Cell Lines STR Profiling [https://blog.ansi.org/ansi/authentication-human-cell-lines-str-atcc-asn-0002/]
- 75. Avoiding Cell Culture Contamination in the Lab | Technology Networks [https://www.technologynetworks.com/cell-science/infographics/detecting-and-preventing-cell-culture-contamination-405162]
- 76. Innovative use of forensic STRs for authentication of human cell ... lines [https://www.oaepublish.com/articles/jtgg.2025.08]
- 77. Culture Cell | Thermo Fisher Scientific - US Contamination [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 78. Interlaboratory study to validate a STR profiling method for... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0218412]
- 79. Authentication of African green monkey cell using human short... lines [https://bmcbiotechnol.biomedcentral.com/articles/10.1186/1472-6750-11-102]
- 80. for Methods authenticating cell lines [https://pubmed.ncbi.nlm.nih.gov/1478343/]
- 81. Rapid Strip Tests vs Lab Methods : Which Works Best in Dairy QA? [https://www.neotest.eu/blog/rapid-strip-tests-vs-lab-methods/]
- 82. A Comparison of Molecular Methods for Microbial Testing [https://www.linkedin.com/pulse/comparison-molecular-methods-microbial-testing-kraken-sense-ltd-seolc]
- 83. Deciphering USP : Particulate in Injections - Matter ... Particle [https://particletechlabs.com/ptl-press/deciphering-usp-788-particulate-matter-in-injections/]
- 84. Understanding USP Chapter < 788 >: A Critical Quality Standard for... [https://www.linkedin.com/pulse/understanding-usp-chapter-788-critical-quality-standard-injectable-qvybf]
- 85. < USP >: Ensuring 788 -Free Injectables Across Global Standards Particle [https://www.linkedin.com/pulse/usp-788-ensuring-particle-free-injectables-across-global-dommati-framc]
- 86. An Overview of USP <787>, < 788 >, and <789> Standards [https://www.fluidimaging.com/blog/usp-787-usp-788-usp-789-standards-injectables]
- 87. Understanding USP : 788 for Injectable Guidelines Safety Drug [https://cgcontainersinc.com/understanding-usp-788-guidelines-for-injectable-drug-safety/]
- 88. Decoding Cell —An In-Depth... - Halo Labs Culture Contamination [https://www.halolabs.com/blog/cell-culture-contamination/]
- 89. for Contamination and Gene Therapies Needs New... Control Cell [https://www.pharmtech.com/view/contamination-control-for-cell-and-gene-therapies-needs-new-analytics]
- 90. Regulations For Liquid Particle Counters In Cleanrooms... USP [https://www.golighthouse.com/en/blog/usp-788-regulations-for-liquid-particle-counters-in-cleanrooms-572/]
- 91. Comparison of culture , confocal microscopy and PCR in routine... [https://pubmed.ncbi.nlm.nih.gov/34741122/]
- 92. 液滴 微 流控技术在 微 研究中的应用 - PMC 生 物 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10475413/]
- 93. -Vis UV : Principle, Strengths and... | Technology Networks Spectroscopy [https://www.technologynetworks.com/analysis/articles/uv-vis-spectroscopy-principle-strengths-and-limitations-and-applications-349865]
- 94. 培养基制备_细胞培养基_培养基灭菌-默克 生 命科学 [https://www.sigmaaldrich.cn/CN/zh/applications/cell-culture-and-cell-culture-analysis/cell-culture-by-technique/cell-culture-media-preparation]