Decoding Cell Therapy Mechanisms of Action: From Biological Principles to Clinical Application and Regulatory Strategy
This article provides a comprehensive analysis of cell therapy mechanisms of action (MoA) for researchers, scientists, and drug development professionals.
Decoding Cell Therapy Mechanisms of Action: From Biological Principles to Clinical Application and Regulatory Strategy
Abstract
This article provides a comprehensive analysis of cell therapy mechanisms of action (MoA) for researchers, scientists, and drug development professionals. It explores the foundational biology of diverse cell modalities, including CAR-T, TCR-T, TIL, and emerging NK cell therapies, detailing their distinct functional principles. The content delves into methodological frameworks for MoA-aligned analytical development and potency testing, addressing common challenges in clinical translation and manufacturing. It further examines troubleshooting strategies for optimization and the critical role of MoA validation in regulatory success, incorporating insights from recent FDA approvals and global regulatory landscapes. This resource synthesizes current scientific understanding with practical development considerations to advance effective and compliant cell therapy programs.
The Cellular Arsenal: Deconstructing Fundamental Mechanisms of Action in Modern Therapies
Defining Mechanism of Action (MoA) in the Context of Complex Cell Therapy Products
For researchers and drug development professionals in the cell therapy space, defining a product's Mechanism of Action (MoA) represents both a scientific necessity and a regulatory requirement. Unlike small molecule drugs with well-defined target engagement, cell therapies exhibit complex, often multifaceted biological activities that present unique characterization challenges. The MoA specifically refers to "the specific process, often pharmacologic, through which a product produces its intended effect" [1]. Understanding MoA is particularly crucial for Complex Cell Therapy Products such as CAR-Ts, TCR-Ts, and tumor-infiltrating lymphocytes (TILs), where the biological activity cannot be fully described by a single parameter.
Regulatory agencies consider potency—the attribute that enables a product to achieve its intended MoA—a Critical Quality Attribute (CQA) that must be measured for each lot to ensure the therapy will have its intended clinical effect [2]. This review examines current approaches to MoA determination for cell therapies, compares methodologies across different product types, and provides practical experimental frameworks to advance product characterization.
The MoA-Potency-Efficacy Framework in Cell Therapies
Conceptual Distinctions and Relationships
A fundamental challenge in cell therapy development lies in properly distinguishing between three interconnected concepts: MoA, potency, and efficacy. According to regulatory guidelines and metrological principles [1]:
- Mechanism of Action (MoA): The specific biological process through which a product produces its intended therapeutic effect
- Potency: The attribute of a product that enables it to achieve its intended MoA (a laboratory-measured CQA)
- Efficacy: The ability of the product to have the desired effect in patients (a clinical outcome)
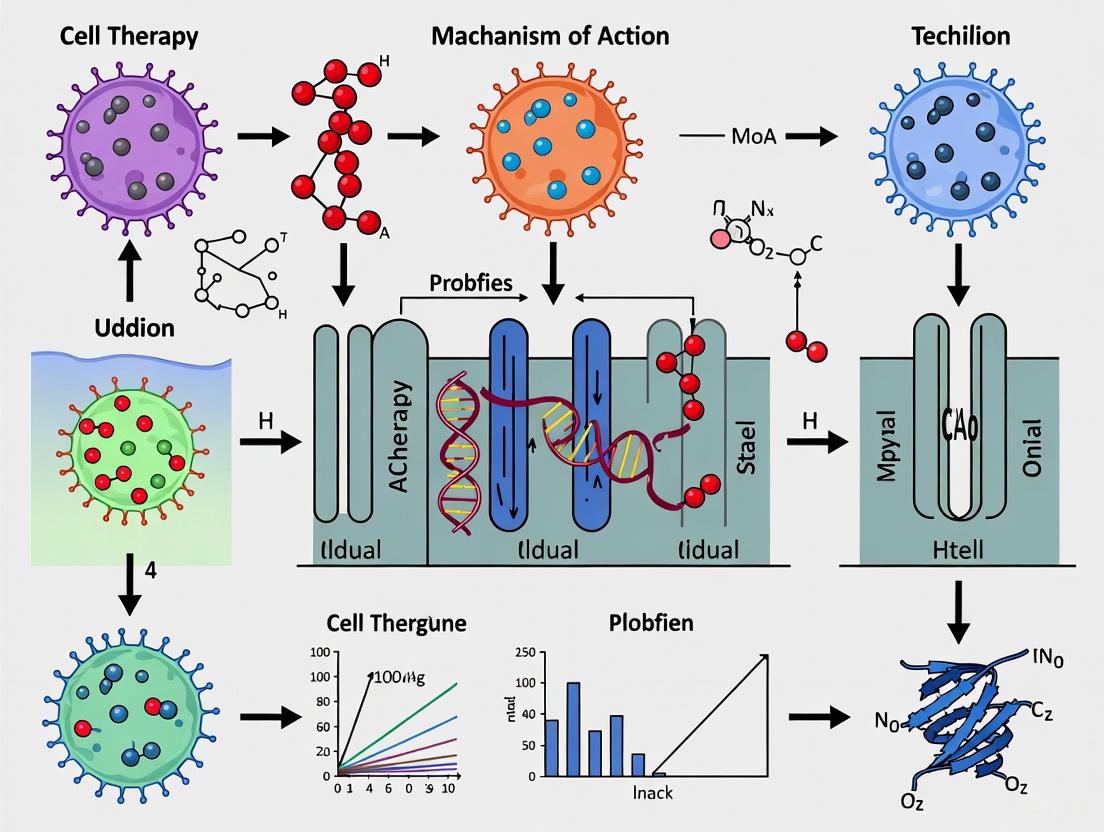
These relationships can be visualized through the following potency and efficacy process charts adapted from regulatory science frameworks [1]:
Regulatory Significance of MoA Determination
For the 27 FDA-approved cell therapy products (as of February 2024), the relationship between MoA and potency assays shows considerable variability [1]. Regulatory documentation reveals that:
- For Provenge, Gintuit, MACI and Amtagvi, the MoA is explicitly stated as not known
- For Kymriah, regulators noted difficulty correlating potency test results with efficacy
- For Rethymic and Lantidra, documentation uses tentative language ("proposed," "believed") when discussing MoA
This uncertainty underscores the challenge in definitively establishing MoA for complex cell products. Despite this, regulators require potency tests based on the proposed or theoretical MoA, recognizing that complete understanding may evolve as clinical experience accumulates.
Comparative MoA Analysis Across Cell Therapy Modalities
Established vs. Emerging Cell Therapy Modalities
The global cell therapy landscape encompasses both established and emerging modalities with varying levels of MoA understanding. According to BCG's 2025 analysis of new drug modalities [3]:
Table 1: Growth Trends and MoA Understanding Across Cell Therapy Modalities
| Modality | Growth Trend | Level of MoA Understanding | Primary Therapeutic Applications | Key Challenges in MoA Definition |
|---|---|---|---|---|
| CAR-T Therapies | Robust growth | Moderate | Hematologic malignancies, expanding to autoimmune diseases | Cytokine release dynamics, long-term persistence mechanisms |
| TCR-T Therapies | Emerging (first approval in 2024) | Low-Moderate | Solid tumors (e.g., synovial sarcoma) | MHC-restricted recognition, tumor microenvironment interactions |
| TIL Therapies | Emerging (first approval in 2024) | Low | Solid tumors | Polyclonal specificity, migration and infiltration mechanisms |
| Stem Cell Therapies | Mixed results | Low | GVHD, regenerative applications | Differentiation cascades, paracrine signaling mechanisms |
| CAR-NK Therapies | Declining interest | Low | Hematologic malignancies | Multiple killing mechanisms, limited persistence |
MoA-Based Classification of Approved Cell Therapies
Analysis of regulatory documentation for approved cell therapies reveals distinct patterns in MoA characterization [1]:
Table 2: MoA Characterization Patterns in FDA-Approved Cell Therapies
| MoA Characterization Pattern | Representative Products | Regulatory Language | Implications for Potency Assay Development |
|---|---|---|---|
| Explicitly Unknown MoA | Provenge, Gintuit, MACI, Amtagvi | "Mechanism of action is not known" | Focus on descriptive potency assays measuring outputs rather than mechanistic understanding |
| Proposed/ Theoretical MoA | Rethymic, Lantidra | "MOA is believed to involve...", "Proposed mechanism..." | Mechanism-informed potency assays with acknowledgment of uncertainty |
| Partially Characterized MoA | Kymriah, Yescarta | Description of specific pathways with noted limitations | Multi-parametric potency assays addressing known mechanisms |
| Correlation Challenges | Multiple CAR-T products | "Difficult to correlate potency test with efficacy" | Development of biomarker matrices rather than single potency measures |
Experimental Approaches for MoA Determination
Integrated Workflow for MoA Establishment
Establishing MoA for cell therapies requires an iterative approach spanning nonclinical and clinical development stages. The following workflow outlines key experimental components:
Methodological Details for Key MoA Experiments
Cytokine Secretion Profiling (CAR-T Example)
Objective: Quantify effector function through cytokine release upon target engagement [1] [2].
Protocol:
- Co-culture Establishment: Plate target cells (tumor cell lines or artificial antigen-presenting cells) at optimized density
- Effector Cell Addition: Add CAR-T cells at predetermined effector:target ratios (typically 1:1 to 10:1)
- Incubation: Culture for 16-24 hours under standard conditions (37°C, 5% CO₂)
- Supernatant Collection: Remove culture supernatant without disturbing cells
- Multiplex Cytokine Analysis: Quantify IFN-γ, IL-2, TNF-α, Granzyme B using Luminex or ELISA
- Data Normalization: Express results as cytokine release per cell or per co-culture unit
Key Controls:
- Effector cells alone (background secretion)
- Target cells alone (baseline cytokine production)
- Positive control (PMA/ionomycin stimulation)
- Negative control (non-specific target cells)
Target Cell Killing Assays
Objective: Measure direct cytotoxic capacity through real-time and endpoint measurements [2].
Protocol Options:
- Real-time Cytotoxicity: Incubate effector and target cells in ratio-dependent manner with continuous monitoring of cell viability using impedance-based systems (xCELLigence)
- Flow Cytometry-Based Killing: Use dye-labeled target cells (CFSE, CellTrace) with viability dyes (propidium iodide, 7-AAD) to quantify specific killing
- Luciferase-Reporter Assays: Employ engineered target cells expressing luciferase; measure luminescence decrease as indicator of killing
Critical Parameters:
- Effector:Target ratio optimization
- Timing of measurement (early vs. late timepoints)
- Assay linearity and dynamic range
Research Reagent Solutions for MoA Studies
Essential Tools for Cell Therapy MoA Characterization
Table 3: Key Research Reagents for MoA Investigation
| Reagent Category | Specific Examples | Research Application | Considerations for Assay Qualification |
|---|---|---|---|
| Reference Target Cells | Custom cell mimics (e.g., TruCytes), Engineered cell lines | Provide consistent antigen presentation for potency assays | Documented lineage, genetic stability, antigen expression consistency |
| Cytokine Detection Kits | Multiplex Luminex panels, ELISA kits, ELISpot kits | Quantify effector function and immune modulation | Standard curve performance, sensitivity, dynamic range, cross-reactivity |
| Viability/Cytotoxicity Assays | Real-time impedance systems, flow cytometry with viability dyes, lactate dehydrogenase (LDH) release | Measure direct target cell killing | Linearity with cell number, compatibility with cell types, interference from media components |
| Cell Tracking Reagents | CFSE, CellTrace dyes, luciferase/GFP reporters | Monitor cell proliferation, persistence, and trafficking | Dye transfer concerns, effects on cell function, signal stability |
| Magnetic Selection Kits | CD3/CD28 beads, cell separation kits | Standardize cell populations for consistent starting material | Purity, recovery, and functional effects on selected cells |
Case Studies: MoA Challenges and Solutions
Kymriah (Tisagenlecleucel): Correlation Challenges
The first FDA-approved CAR-T therapy exemplifies the challenge of correlating potency measurements with clinical outcomes. Kymriah's potency is defined as the ability of CAR T-cells to secrete interferon-γ (IFN-γ) following exposure to CD19-expressing target cells [1]. However, FDA documentation states: "In the clinical trials, IFN-γ production varied greatly from lot-to-lot, making it difficult to correlate IFN-γ production in vitro with tisagenlecleucel safety or efficacy" [1].
Analysis of clinical data revealed:
- Correlation with remission but significant overlap between responders and non-responders
- Multi-parametric assessment needed beyond single cytokine measurement
- Patient-specific factors influence potency-efficacy relationship
Emerging Solutions: Multi-Assay Potency Matrices
For products with complex or incompletely understood MoAs, the field is moving toward multi-parametric potency matrices rather than single-parameter tests. The case of Iovance's TIL therapy (lifileucel) demonstrates this approach [2]:
- Initial setback: FDA requested additional potency data beyond single-assay approach
- Solution implemented: Multi-assay matrix including functional co-culture assays
- Outcome: After multi-year delay, comprehensive potency strategy supported approval
This case underscores that regulators increasingly expect mechanism-relevant potency assays that collectively reflect the complex biological activity of cell therapies, even when complete MoA understanding remains elusive.
Defining Mechanism of Action for complex cell therapy products remains challenging yet essential for product characterization and regulatory approval. The evolving landscape suggests several strategic imperatives for researchers and developers:
- Embrace Mechanistic Complexity: Recognize that cell therapies may function through multiple parallel mechanisms rather than single pathways
- Invest Early in Potency Assay Development: Begin MoA-informed potency assessment during preclinical development to avoid delays later [2]
- Implement Multi-Parametric Approaches: Develop potency matrices that collectively reflect biological activity when single-parameter tests are insufficient
- Leverage Advanced Analytical Tools: Utilize omics technologies, single-cell analysis, and computational modeling to deconvolute complex mechanisms
As the field advances from hematologic malignancies to solid tumors and autoimmune diseases, understanding MoA will grow in importance for designing safer, more effective cell therapies. The frameworks, methodologies, and comparative analyses presented here provide a foundation for advancing MoA research in this rapidly evolving field.
The field of cancer immunotherapy has been revolutionized by strategies that redirect the patient's own T cells to recognize and eliminate tumor cells. Among the most advanced of these are Chimeric Antigen Receptor T (CAR-T) cells and T-cell Engagers (TCEs). Although both modalities share the ultimate goal of achieving potent, targeted tumor cell killing, they represent fundamentally different technological approaches. CAR-T therapy involves the ex vivo genetic engineering of a patient's T cells to express synthetic receptors that target tumor-associated antigens (TAAs), effectively creating a "living drug" [4] [5]. In contrast, TCEs are typically bispecific antibody-derived molecules that act as a physical bridge between a T cell (via CD3) and a tumor cell (via a TAA), redirecting existing T cell cytotoxicity without requiring genetic modification [6] [7] [8]. This guide provides a detailed, objective comparison of their mechanisms of action, supported by experimental data and methodologies relevant to cell therapy research and development.
Mechanism of Action: A Comparative Analysis
CAR-T Cell Mechanism: Genetically Engineered Living Drugs
CAR-T cells are generated by genetically modifying patient-derived T cells to express a chimeric antigen receptor. The canonical CAR is a synthetic receptor comprising an extracellular antigen-recognition domain (often a single-chain variable fragment, or scFv, derived from a monoclonal antibody), a hinge region, a transmembrane domain, and an intracellular signaling domain [4] [5]. Upon binding to a surface antigen on a tumor cell, the CAR initiates T cell activation independently of the native T cell receptor (TCR) and major histocompatibility complex (MHC) presentation, a key differentiator from physiological T cell activation [9].
The signaling cascade leads to:
- Cytolytic Granule Release: Perforin and granzymes are released at the immune synapse, inducing apoptosis in the target tumor cell [4] [8].
- Cytokine Production: Inflammatory cytokines such as IFN-γ, TNF-α, and IL-2 are secreted, amplifying the immune response [5].
- T cell Proliferation and Clonal Expansion: The activated CAR-T cell undergoes rapid division, increasing the number of effector cells [4].
A critical limitation of first-generation CARs was suboptimal persistence. This was addressed in subsequent generations by incorporating costimulatory domains (e.g., CD28 or 4-1BB) alongside the CD3ζ activation domain, which enhance T cell survival, proliferation, and sustained antitumor activity [4] [5].
Figure 1: CAR-T Cell Activation Pathway. Antigen binding initiates a synergistic signaling cascade leading to full T-cell activation.
T-cell Engager Mechanism: Bispecific Bridging Molecules
TCEs are engineered proteins, most often bispecific antibodies, designed to simultaneously bind to the CD3ε subunit of the TCR complex on T cells and a TAA on cancer cells [6] [7]. This forced proximity creates an immunological synapse that triggers T cell activation and cytotoxic killing of the bound tumor cell, entirely independently of the T cell's intrinsic TCR specificity [8].
Key functional characteristics of TCEs are dictated by their structural design:
- Format: They range from small, fragment-based constructs like Bispecific T-cell Engagers (BiTEs) to full-length IgG-like antibodies that may include an Fc region [6] [7].
- Fc Domain Impact: The presence of an Fc region can confer a longer half-life but may also limit tissue penetration and contribute to adverse events via Fc receptor interactions [6] [8].
- Avidity Engineering: Newer formats like "2+1" TCEs (two tumor-binding domains, one CD3-binding domain) leverage avidity to improve selectivity for tumor cells with high antigen density, potentially reducing on-target, off-tumor toxicity [7].
A significant advantage of TCEs is their ability to recruit any available T cell, irrespective of its native specificity, making them an "off-the-shelf" therapeutic that does not require complex personalization [5].
Figure 2: T-cell Engager Bispecific Bridging. The TCE physically links a T cell and a tumor cell, inducing targeted cytotoxicity.
Direct Comparison of Functional Performance
Understanding the functional differences between these two modalities is critical for research and clinical development. The table below synthesizes key characteristics based on the literature.
Table 1: Functional and Operational Comparison of CAR-T Cells and T-cell Engagers
| Feature | CAR-T Cells | T-cell Engagers (TCEs) |
|---|---|---|
| Technology Type | Living, genetically engineered cells | Bispecific antibody molecules |
| Mechanism | Endogenous expression of synthetic antigen receptor | Extracellular bridge between CD3 and TAA |
| MHC Restriction | No [4] | No [8] |
| Antigen Recognition | Surface antigens only [4] | Primarily surface antigens; TCR-based formats can target peptide-MHC [6] |
| Requirement for Costimulation | Incorporated into CAR design (2nd gen+) [5] | Generally not required [8] |
| Pharmacokinetics | Single infusion, potential for long-term persistence | Short half-life (fragment-based); longer with Fc/HSA binding [6] [7] |
| Manufacturing | Complex, patient-specific, ex vivo process; time-intensive [5] | Off-the-shelf, industrial biologics production; simpler scale-up [5] |
A critical functional difference lies in their response to varying levels of antigen exposure. A 2022 study directly comparing CD20-targeting CAR-T cells and engineered TCR (eTCR) T cells (a modality with similarities to TCEs in being TCR-dependent) revealed divergent performance under high antigenic pressure [10].
Table 2: Performance as a Function of Antigen Exposure (Based on Ref [10])
| Performance Metric | CAR-T Cells | eTCR T Cells (TCR-Dependent) |
|---|---|---|
| Short-Term Potency | Higher cytotoxicity and cytokine production | Lower cytotoxicity and cytokine production |
| Expansion under High Antigen | Significantly impaired | Robust |
| Phenotype under High Antigen | Elevated exhaustion markers (e.g., coinhibitory molecules), effector differentiation | Lower exhaustion markers, maintenance of early differentiation phenotype |
| Long-Term Tumor Clearance | Compromised by exhaustion | Comparable, sustained clearance |
This data suggests that while CAR-T cells can initiate a more potent immediate response, their activation signaling—which differs from physiological TCR signaling—may predispose them to exhaustion in environments with high tumor burden [10] [9]. In contrast, TCR-dependent mechanisms appear to support better long-term expansion and persistence under the same conditions.
Experimental Protocols for Mechanistic Studies
For scientists dissecting the MoA of these therapies, the following core experimental methodologies are foundational.
In Vitro Cytotoxicity Assay
This assay quantitatively measures the ability of CAR-T cells or TCEs to kill specific target cells.
Protocol Outline:
- Effector and Target Cell Preparation: Prepare CAR-T cells or unmodified T cells (for TCE testing) as effector cells. Harvest tumor cells expressing the target antigen as target cells.
- Target Cell Labeling: Label target cells with a fluorescent dye such as calcein-AM or a membrane-labeling dye (e.g., PKH67). Alternatively, use tumor cells engineered to express a luciferase or GFP reporter.
- Co-culture Setup: Plate target cells in a multi-well plate and add effector cells at varying Effector:Target (E:T) ratios. For TCE testing, add the bispecific molecule at a range of concentrations to wells containing T cells and target cells. Include controls for spontaneous and maximum target cell lysis.
- Incubation: Incubate for a predetermined period (e.g., 4-24 hours) at 37°C, 5% CO₂.
- Lysis Measurement:
- For calcein-AM: Measure fluorescence in the supernatant (released from lysed cells).
- For luciferase: Lyse all cells and measure luminescence; specific lysis is inversely proportional to signal.
- For flow cytometry: Use a viability dye or count residual target cells via specific markers.
- Data Analysis: Calculate percent-specific lysis:
% Lysis = (Experimental - Spontaneous) / (Maximum - Spontaneous) * 100[5].
Cytokine Release Analysis
This protocol assesses T cell activation by quantifying secreted cytokines, which is also a key safety biomarker for Cytokine Release Syndrome (CRS).
Protocol Outline:
- Stimulation: Co-culture effector cells (CAR-T or unmodified T cells) with antigen-positive target cells in the presence or absence of TCEs, as appropriate.
- Supernatant Collection: Collect cell culture supernatant at various time points post-stimulation (e.g., 6, 24, 48 hours).
- Cytokine Quantification:
- ELISA: The traditional method for quantifying specific cytokines (e.g., IFN-γ, IL-2, TNF-α, IL-6) using paired antibodies. Provides absolute concentration.
- Multiplex Bead Array (e.g., Luminex): Allows simultaneous quantification of dozens of cytokines from a small sample volume. This is efficient for profiling.
- Intracellular Cytokine Staining (ICS) with Flow Cytometry: Can identify which specific T cell subsets are producing cytokines by using protein transport inhibitors to accumulate cytokines intracellularly, followed by staining and flow analysis [5] [11].
Immune Synapse Characterization
Advanced microscopy techniques are used to visualize and quantify the structure of the immune synapse formed during CAR- or TCE-mediated engagement.
Protocol Outline:
- Synapse Formation: Allow effector and target cells to interact in the presence of the engaging molecule on a coated surface (e.g., poly-L-lysine) for a short period (minutes).
- Fixation and Staining: Fix cells with paraformaldehyde, permeabilize if needed, and stain with fluorescently labeled antibodies.
- Key Staining Targets: CAR or TCR (if applicable), CD3, the target antigen, actin cytoskeleton (phalloidin), and key signaling molecules (e.g., phosphorylated proteins).
- High-Resolution Imaging: Acquire images using Confocal Microscopy or Total Internal Reflection Fluorescence (TIRF) Microscopy. TIRF is particularly useful for visualizing events at the cell membrane contact zone.
- Image Analysis: Analyze images for synaptic characteristics:
- Synapse Architecture: Assess the organization of key molecules into canonical structures like the central supramolecular activation cluster (cSMAC). CAR synapses are often noted to be more disorganized than TCR synapses [9].
- Molecular Polarization: Quantify the recruitment of cytotoxic granules and signaling proteins to the contact site.
- Synapse Stability: Measure the duration of the cell-cell contact [9].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for CAR-T and TCE Mechanism of Action Research
| Reagent / Tool | Primary Function in Research | Key Applications |
|---|---|---|
| Anti-CD3 Antibodies | T cell activation and validation | Positive control for TCE assays; component of T cell culture [5] |
| Recombinant TCE Molecules | Bispecific engagement | In vitro and in vivo proof-of-concept studies; potency assays [7] |
| Lentiviral Vectors | Stable gene delivery | Standard tool for engineering CAR expression in T cells [4] [5] |
| Cell Trace Proliferation Dyes | Tracking cell division | Monitoring CAR-T or engaged T cell proliferation (e.g., CFSE, CellTrace Violet) [11] |
| Multiplex Cytokine Assays | Profiling immune secretion | Assessing T cell activation potency and safety (CRS potential) [11] |
| pMHC Multimers | Identifying antigen-specific T cells | Validating TCR-based therapeutics and monitoring responses [12] |
CAR-T cells and T-cell Engagers are two powerful pillars of redirected T cell immunotherapy with distinct and complementary profiles. CAR-T cells offer the potential for a single-administration, living therapy capable of long-term persistence and surveillance, making them highly effective in certain hematologic malignancies. However, their complex, personalized manufacturing and propensity for exhaustion in high-burden environments remain significant challenges. TCEs, as off-the-shelf biologics, offer immediate logistical and economic advantages and can effectively recruit diverse T cell populations without prior activation. Their main challenges include managing toxicities like CRS and optimizing pharmacokinetics. The choice between these modalities, or their potential sequential or combined use, will depend on the specific clinical context, tumor type, and antigen landscape. Future research will focus on engineering next-generation products that enhance efficacy, safety, and applicability to solid tumors.
The challenge of treating solid tumors has catalyzed the development of advanced cellular immunotherapies, with Tumor-Infiltrating Lymphocyte (TIL) and T-cell receptor-engineered T-cell (TCR-T) therapies emerging as two prominent strategies. While both approaches harness the cytotoxic potential of T lymphocytes to eliminate cancer cells, they fundamentally differ in their recognition mechanisms—TILs utilize naturally selected native receptors, whereas TCR-T cells employ genetically engineered receptors for enhanced specificity [13] [14]. This distinction profoundly impacts their antigen recognition breadth, manufacturing complexity, and clinical application. Understanding these differences is crucial for researchers and drug development professionals optimizing cell therapy mechanisms of action. This guide provides a detailed comparison of these platforms, focusing on their recognition mechanisms, experimental data, and methodological protocols to inform therapeutic development decisions.
Mechanisms of Action: Native Polyclonality vs. Engineered Precision
TIL Therapy: Native Recognition of Tumor Neoantigens
TIL therapy leverages the body's natural immune response by isolating T cells that have already infiltrated a patient's tumor [15] [16]. These cells are expanded ex vivo and reinfused to enhance anti-tumor immunity. The therapeutic efficacy of TILs stems from their native T cell receptors (TCRs), which naturally recognize tumor-specific neoantigens—abnormal proteins resulting from somatic mutations in tumor cells [15].
- Polyclonal Recognition: TIL products contain multiple T-cell clones with diverse TCRs capable of recognizing a broad array of tumor antigens simultaneously, effectively addressing tumor heterogeneity [15] [14].
- Neoantigen Targeting: The native TCRs in TILs predominantly target mutation-derived neoepitopes, which are uniquely expressed on tumor cells, minimizing off-tumor toxicity [15] [17].
- Mechanism of Action: TILs recognize intracellular and surface antigens processed and presented as peptides by major histocompatibility complex (MHC) molecules on tumor cells [13]. This recognition initiates cytotoxic killing through perforin/granzyme release and cytokine secretion [18].
TCR-T Therapy: Engineered Recognition for Enhanced Specificity
TCR-T therapy involves genetically modifying a patient's peripheral blood T cells to express synthetic TCRs specifically selected for their high affinity against predefined tumor antigens [13] [19]. Unlike TILs, TCR-T cells are monoclonal or oligoclonal, targeting a limited set of carefully selected antigens.
- Precision Engineering: TCR-T cells are engineered to recognize specific intracellular antigens, such as viral oncoproteins or cancer-testis antigens, presented by MHC molecules [13] [19].
- MHC-Dependent Recognition: Like TILs, TCR-T cells require MHC presentation for antigen recognition, enabling targeting of intracellular proteins not accessible to other modalities like CAR-T [20].
- Enhanced Specificity Protocols: Advanced screening platforms identify high-affinity TCRs against defined neoantigens, with genetic screening approaches demonstrating superior sensitivity compared to conventional flow cytometry-based methods [17].
The following diagram illustrates the fundamental differences in the recognition pathways for TIL and TCR-T therapies:
Comparative Clinical Performance and Experimental Data
Clinical data demonstrate distinct response patterns for TIL and TCR-T therapies across different solid tumor indications. The following table summarizes key efficacy metrics from recent studies and trials.
Table 1: Clinical Response Comparison for TIL and TCR-T Therapies
| Therapy | Cancer Indications | Response Rates | Response Durability | Key Limitations |
|---|---|---|---|---|
| TIL Therapy [15] [16] [21] | Melanoma | 31.5%-41% ORR (Objective Response Rate) | 43.5% maintained remission >12 months; Decade-long remissions reported | Limited to immunogenic tumors; Labor-intensive manufacturing |
| Cervical Cancer | 30-35% ORR | Durable responses observed | Requires high TMB (Tumor Mutational Burden) | |
| NSCLC (Non-Small Cell Lung Cancer) | 20-30% ORR | Ongoing responses >2 years | Heterogeneous response across patients | |
| TCR-T Therapy [21] [19] | HPV-associated Cancers (Phase 2 trial) | 60% ORR (6/10 patients; 2 CR, 4 PR) | Ongoing CR (Complete Response) at 12-14 months | HLA restriction limited to specific alleles |
| Solid Tumors (Preclinical) | Target-dependent variability | Requires persistent antigen exposure | Off-target toxicity concerns |
Analysis of Clinical Performance Patterns
TIL therapy demonstrates broader applicability across multiple solid tumor types, with particularly robust response rates in immunologically "hot" tumors like melanoma and cervical cancer [15] [16]. The polyclonal nature of TILs enables targeting of multiple neoantigens simultaneously, potentially overcoming tumor heterogeneity [14]. Notably, decade-long complete remissions have been reported in metastatic cervical cancer patients, suggesting the potential for curative outcomes in selected cases [21].
TCR-T therapy shows remarkable precision in defined patient populations, as evidenced by the 60% objective response rate in HPV-associated cancers [21] [19]. The complete responses observed in this trial, ongoing at 12 and 14 months, demonstrate the potential of engineered receptors to mediate durable anti-tumor activity. However, this approach requires careful patient selection based on HLA haplotypes and specific antigen expression [13].
Experimental Protocols and Methodological Approaches
TIL Therapy Manufacturing and Expansion Protocols
TIL therapy relies on complex manufacturing processes to expand tumor-derived T cells while maintaining their anti-tumor reactivity.
Standard TIL Protocol [15] [16]:
- Tumor Resection: Surgical removal of tumor tissue (1-2 cm³)
- TIL Extraction: Mechanical and enzymatic digestion to dissociate tissue and isolate lymphocytes
- Rapid Expansion: Culture with IL-2 (6000 IU/mL) for 2-3 weeks
- REP (Rapid Expansion Protocol): Stimulation with anti-CD3 antibody and irradiated feeder cells
- Lymphodepletion: Patient preconditioning with cyclophosphamide (60 mg/kg/d × 2d) and fludarabine (25 mg/m²/d × 5d)
- TIL Infusion: Administration of expanded cells (10¹⁰ to 10¹¹ cells)
- IL-2 Support: Post-infusion IL-2 administration (720,000 IU/kg every 8-12 hours)
Young TIL Protocol [15]: This modified approach reduces manufacturing time to approximately 20 days by omitting the initial tumor reactivity screening. Young TILs exhibit superior characteristics including longer telomeres and increased CD27/CD28 expression, correlating with improved persistence post-infusion.
TCR-T Discovery and Engineering Platforms
Advanced screening technologies enable identification of high-affinity TCRs for therapeutic engineering.
High-Throughput TCR Discovery Platform [17]:
- Tumor Sequencing: Whole exome and RNA sequencing of tumor biopsies to identify mutations
- Neoantigen Prediction: In silico prediction of HLA-binding neoantigen peptides
- Library Construction: Synthesis of tandem minigene (TMG) libraries encoding 12 neoantigens flanked by LAMP1 sequences for enhanced MHC class II presentation
- Combinatorial TCR Library: Assembly of all possible TCRα and TCRβ chain combinations from TIL sequencing data
- Functional Screening: Pooled TCR library transduction into Jurkat reporter T cells followed by co-culture with autologous antigen-presenting cells (APCs)
- Activation-Based Sorting: Isolation of CD69-high T cells via FACS (Fluorescence-Activated Cell Sorting)
- TCR Identification: Next-generation sequencing of enriched TCR sequences
Optimized Antigen Presentation System [17]: The platform utilizes immortalized autologous B cells as APCs, engineered to express BCL-6/BCL-xL for expansion and CD40L for enhanced antigen presentation. This system supports both HLA class I and II restricted antigen presentation, enabling comprehensive TCR screening.
The following workflow diagram illustrates the key methodological differences between TIL and TCR-T development:
Research Reagent Solutions and Essential Materials
Successful implementation of TIL and TCR-T research requires specialized reagents and platforms. The following table details essential research tools for investigating these cellular therapies.
Table 2: Essential Research Reagents for TIL and TCR-T Investigations
| Research Tool | Application | Function | Example Implementation |
|---|---|---|---|
| IL-2 (Interleukin-2) [15] [16] | TIL Expansion | T cell growth and activation | Culture at 6000 IU/mL for 2-3 weeks |
| Anti-CD3 Antibody [15] | TIL REP (Rapid Expansion Protocol) | TCR stimulation for rapid proliferation | Used with irradiated feeder cells |
| Lymphodepletion Agents [15] [21] | Patient Preconditioning | Create immune space for infused cells | Cyclophosphamide + fludarabine regimen |
| Tandem Minigene (TMG) Libraries [17] | TCR Discovery | Express neoantigen panels for screening | TMG12 design with LAMP1 sequences |
| Immortalized B Cells [17] | Antigen Presentation | Autologous APCs for TCR screening | Engineered with BCL-6/BCL-xL and CD40L |
| Jurkat Reporter Cells [17] | TCR Functional Screening | Monitor TCR activation via CD69 expression | CD8+ TCR KO Jurkat with NFAT-GFP |
| Oxford Nanopore Sequencing [17] | TCR Identification | Characterize paired TCRαβ chains from libraries | PCR/ONT sequencing with optimized filtering |
| G-Rex Flasks [15] | Large-Scale TIL Expansion | Gas-permeable culture vessels | Enable 2310-fold cell expansion |
| Microbubble Technology [20] | T Cell Separation | Gentle, buoyancy-based cell isolation | Akadeum's BACS for T cell enrichment |
TIL and TCR-T therapies represent complementary approaches in the solid tumor immunotherapy landscape, each with distinct advantages for specific research and clinical contexts. TIL therapy offers a polyclonal, native recognition system capable of targeting multiple tumor antigens simultaneously, making it particularly suitable for immunologically "hot" tumors with high mutational burden [15] [16]. The decade-long complete remissions observed in metastatic cervical cancer patients highlight its potential for achieving durable responses [21]. Conversely, TCR-T therapy provides a precision medicine approach with defined antigen specificity, demonstrating remarkable efficacy in virally-associated cancers and situations where target antigens are well-characterized [21] [19].
The choice between these platforms depends on multiple factors including tumor immunogenicity, antigen availability, manufacturing capabilities, and desired specificity. For research applications focused on discovering novel tumor antigens or targeting heterogeneous malignancies, TIL-based approaches provide a comprehensive discovery platform. For targeted intervention against defined oncogenic drivers, TCR-T platforms offer precise engineering solutions. As both fields advance, convergence of these technologies—such as applying TCR engineering principles to enhance TIL specificity—may yield next-generation therapies with optimized recognition capabilities for solid tumor treatment.
Natural Killer (NK) cells are large granular lymphocytes of the innate immune system that play a critical role in rapidly recognizing and eliminating abnormal, virally infected, and tumor cells without prior sensitization [22]. Their unique biological properties position them as compelling candidates for cell therapy, particularly due to mechanisms of action (MoA) that diverge significantly from T-cell-based approaches. Unlike T-cell activation, which is governed by antigen-specific T-cell receptors requiring major histocompatibility complex (MHC) presentation, NK cell stimulation is regulated by a complex balance of activating and inhibitory receptors that operate independently of antigen processing or presentation [22]. This innate recognition capability, coupled with their capacity to modulate immunity through cytokine secretion, underscores their pivotal role in orchestrating immune responses within tumor microenvironments (TME) [22]. The therapeutic application of NK cells represents a paradigm shift in cell therapy MoA research, leveraging innate immunity's speed and flexibility while overcoming limitations of adaptive immunity approaches.
Biological Mechanisms: Innate Recognition and Cytotoxic Pathways
Fundamental NK Cell Biology
NK cells exert their primary cytotoxic functions through several distinct biological mechanisms that operate in concert. Their defining feature is the ability to detect and eliminate target cells through integrated signaling from multiple surface receptors [23]. The "missing-self" hypothesis, proposed in 1986, explains one fundamental NK cell MoA: the recognition and elimination of cells that have lost MHC class I expression, a common occurrence in cancerous or virally infected cells attempting to evade T-cell immunity [23]. This capability provides a complementary mechanism to T-cell responses, targeting pathological cells that might otherwise escape adaptive immune surveillance.
NK cells perform target cell killing primarily through the release of cytotoxic granules containing perforin and granzymes [22] [23]. Perforin forms pores (~16 nm inner diameter) in the target cell membrane, facilitating the delivery of proteolytic granzymes that activate caspase-mediated apoptosis [23]. Additionally, NK cells express death receptors such as FasL and TRAIL, which can induce programmed cell death through extrinsic apoptosis pathways [23]. A third key mechanism is antibody-dependent cellular cytotoxicity (ADCC), mediated through CD16 (FcγRIII) receptors that recognize antibody-coated target cells [23]. This versatile arsenal enables NK cells to rapidly eliminate diverse threats through multiple parallel pathways.
Receptor Signaling and Activation Dynamics
NK cell activity is governed by a sophisticated integration of signals from activating and inhibitory receptors. Major activating receptors include NKG2D (binds to MICA, MICB, ULBP), natural cytotoxicity receptors (NKp30, NKp44, NKp46), and DNAM-1 [23]. Inhibitory receptors, primarily killer-cell immunoglobulin-like receptors (KIRs) and NKG2A, recognize MHC class I molecules on healthy cells, providing a crucial "off" signal that prevents autoimmunity [23]. The transition from inhibition to activation occurs when activating signals overwhelm inhibitory inputs, typically when target cells display stress-induced ligands while downregulating MHC class I.
Table 1: Key NK Cell Receptors and Their Functions in Tumor Immunity
| Receptor | Type | Ligand(s) | Signaling Pathway | Functional Role |
|---|---|---|---|---|
| NKG2D | Activating | MICA, MICB, ULBP, Rae-1 | DAP10 | Recognizes stress-induced ligands on tumor cells |
| NKp30 | Activating | B7-H6, BAT3 | CD3ζ, FcεRIγ | Natural cytotoxicity against transformed cells |
| NKp46 | Activating | Complement factors, viral hemagglutinins | CD3ζ, FcεRIγ | Primary natural cytotoxicity receptor |
| KIRs | Inhibitory | MHC class I | ITIM domains | Prevents killing of healthy self-cells |
| NKG2A | Inhibitory | HLA-E | ITIM domains | Inhibits cytotoxicity against MHC-expressing cells |
| CD16 | Activating | IgG Fc region | CD3ζ, FcεRIγ | Mediates antibody-dependent cellular cytotoxicity |
The diagram below illustrates the core signaling pathways governing NK cell activation and cytotoxicity:
Comparative Advantages: NK Cells vs. T Cells in Therapeutic Applications
Mechanism of Action Differences
The fundamental MoA differences between NK cells and T cells create distinct therapeutic profiles with complementary strengths. While T cells require antigen presentation via MHC and generate memory responses, NK cells operate through germline-encoded receptors that provide immediate reactivity without prior exposure [22]. This innate recognition capability enables NK cells to target a broader spectrum of abnormal cells, including those that have downregulated MHC to evade T-cell surveillance—a common immune escape mechanism in cancer [22]. Additionally, NK cells exhibit a lower risk of inducing cytokine release syndrome (CRS) and neurotoxicity, severe side effects often associated with CAR-T therapies [22] [24].
Clinical evidence demonstrates that CAR-NK cell therapy causes fewer immune-related adverse events than CAR-T cell approaches. A Phase I/II trial of cord blood-derived CD19-targeted CAR-NK therapy reported no cases of cytokine release syndrome, neurotoxicity, or graft-versus-host disease, despite achieving a 48.6% response rate and one-year overall survival of 68% in patients with CD19-positive B-cell malignancies [24]. This improved safety profile is attributed to differences in cytokine secretion patterns and activation kinetics between NK and T cells [22].
"Off-the-Shelf" Potential and Manufacturing Considerations
A transformative advantage of NK cell therapies is their capacity for allogeneic "off-the-shelf" applications without triggering significant graft-versus-host disease (GvHD) [25] [24]. While most CAR-T cell therapies are autologous, requiring weeks for custom manufacturing for each patient, NK cells can be sourced from healthy donors, cord blood banks, or stem cell lines and manufactured in advance for immediate use [24]. This approach addresses critical limitations of current cell therapies, including manufacturing bottlenecks, high costs, and treatment delays that exclude patients with rapidly progressive diseases [25].
Table 2: Comparative Analysis of CAR-NK vs. CAR-T Cell Therapies
| Parameter | CAR-NK Cells | CAR-T Cells |
|---|---|---|
| Source | Allogeneic (healthy donors, iPSCs, cord blood) | Primarily autologous (patient's own cells) |
| Manufacturing Time | Pre-manufactured, immediate availability | 3-5 weeks custom manufacturing |
| MHC Restriction | No MHC restriction, target recognition is MHC-independent | MHC-dependent antigen presentation required |
| Toxicity Profile | Low incidence of CRS, neurotoxicity, and GvHD | Significant risk of CRS, neurotoxicity, and GvHD |
| Killing Mechanisms | CAR-dependent + natural cytotoxicity receptors | Primarily CAR-dependent |
| Persistence | Shorter persistence in vivo | Long-term persistence possible |
| Target Spectrum | Broad, can target heterogeneous tumors | Narrow, requires uniform antigen expression |
| Cost | Lower potential cost (off-the-shelf) | Higher cost (patient-specific manufacturing) |
Engineering advances are further enhancing the "off-the-shelf" potential of NK cell therapies. Recent research from MIT and Harvard Medical School has demonstrated that NK cells can be modified to evade host immune rejection by downregulating HLA class I proteins using siRNA, while simultaneously incorporating protective proteins like PD-L1 or single-chain HLA-E [26]. In murine models with humanized immune systems, these engineered CAR-NK cells persisted for at least three weeks and nearly eliminated lymphoma, while unmodified NK cells were rejected within two weeks [26].
Clinical Trial Landscape and Experimental Evidence
Hematological Malignancies: Efficacy and Safety Data
Clinical trials investigating NK cell therapies, particularly against hematological malignancies, are demonstrating compelling efficacy with favorable safety profiles. An interim analysis from the phase I SENTI-202-101 clinical trial presented at AACR 2025 reported complete remissions in patients with relapsed or refractory acute myeloid leukemia (AML) treated with SENTI-202, a logic-gated CAR-NK cell therapy [25]. Among seven evaluable patients, four achieved complete remission with no evidence of measurable residual disease, and all responses were ongoing with maximum follow-up exceeding eight months [25]. Notably, no dose-limiting toxicities were observed, and the maximum tolerated dose was not reached, supporting the favorable safety profile of NK cell approaches [25].
The innovative design of SENTI-202 incorporates logic-gating technology to enhance specificity. The CAR-NK cells recognize two different AML targets (CD33 and FLT3) to address tumor heterogeneity, while containing an inhibitory receptor that prevents killing of healthy cells co-expressing EMCN, a protein found on normal hematopoietic stem cells [25]. This sophisticated targeting strategy demonstrates how engineered NK cells can overcome fundamental challenges in cancer therapy that have limited more conventional approaches.
Solid Tumors: Challenges and Emerging Strategies
While NK cell therapies show promise in hematological malignancies, their application against solid tumors presents unique challenges. A comprehensive analysis of the global clinical landscape for NK cell therapies in solid tumors identified 141 relevant trials registered on ClinicalTrials.gov as of December 2024 [27]. The geographical distribution shows China leading with 62 trials (44.0%), followed by the United States with 45 trials (31.9%), while no relevant trials were conducted in Africa or South America, highlighting significant global disparities in cell therapy research [27].
Most clinical investigations for solid tumors remain in early development phases, with Phase I trials constituting the largest proportion (39.7%), followed by Phase I/II trials (30.5%) [27]. No Phase III or IV clinical trials have been initiated, indicating the field is still establishing foundational safety and efficacy data [27]. Lung cancer is the most frequently targeted solid tumor (14.2% of trials), with a substantial portion of trials (29.1%) focusing on solid tumors generally rather than specific cancer types [27].
Table 3: Global Clinical Trial Landscape for NK Cell Therapies in Solid Tumors
| Parameter | Distribution | Number | Percentage |
|---|---|---|---|
| Geographical Distribution | China | 62 | 44.0% |
| United States | 45 | 31.9% | |
| Spain | 4 | 2.8% | |
| Other countries | 30 | 21.3% | |
| Trial Phase | Phase I | 56 | 39.7% |
| Phase I/II | 43 | 30.5% | |
| Phase II | 28 | 19.9% | |
| Not specified | 14 | 9.9% | |
| Tumor Types | Lung cancer | 20 | 14.2% |
| Breast cancer | 12 | 8.5% | |
| Colorectal cancer | 10 | 7.1% | |
| Ovarian cancer | 9 | 6.4% | |
| Glioblastoma | 8 | 5.7% | |
| Various/unspecified | 41 | 29.1% |
Major barriers to NK cell efficacy in solid tumors include the immunosuppressive tumor microenvironment (TME), physical barriers formed by dense extracellular matrix, and tumor heterogeneity [27]. The TME contains various cell populations, including cancer-associated fibroblasts (CAFs) and tumor-associated macrophages (TAMs), that secrete factors suppressing NK cell function [22]. Strategies to overcome these limitations include engineering CAR-NK cells to target solid tumor antigens, armoring with cytokines to enhance persistence, and combining with checkpoint inhibitors to reverse NK cell exhaustion [24] [27].
Engineering Innovations and Experimental Approaches
Advanced Engineering Strategies
The engineering landscape for NK cells is rapidly evolving beyond first-generation CAR constructs to incorporate sophisticated control systems and enhanced functionality. Logic-gating approaches, such as those employed in the SENTI-202 therapy, represent a significant advancement in precision targeting [25]. These systems require recognition of multiple antigens before initiating cytotoxic responses, reducing off-target effects against healthy tissues that express only single targets. The incorporation of inhibitory receptors that recognize "self" markers provides an additional layer of selectivity, potentially expanding the therapeutic window for targeting antigens expressed at varying levels on both malignant and healthy cells.
Other innovative engineering strategies include cytokine armoring to enhance persistence and functionality. At MD Anderson Cancer Center, researchers are developing IL-21 engineered NK cells for glioblastoma treatment, with preclinical models demonstrating superior safety, metabolic fitness, and anti-tumor activity compared to IL-15 engineered counterparts [24]. Alternative approaches include engineering NK cells with T-cell receptors (TCRs) to recognize intracellular targets, significantly expanding the repertoire of targetable antigens [24]. Additionally, induced pluripotent stem cell (iPSC)-derived NK cells offer advantages in homogeneity, genetic engineering flexibility, and scalable manufacturing [27].
Experimental Protocols for NK Cell Engineering
A representative experimental protocol for generating engineered CAR-NK cells involves several critical stages. The following methodology synthesizes approaches from recent high-impact studies:
NK Cell Isolation and Activation:
- Source NK cells from peripheral blood, cord blood, or iPSCs using density gradient centrifugation
- Isolate pure NK cell populations using magnetic-activated cell sorting (MACS) with CD56 or CD3 depletion/CD56 positive selection
- Activate cells with IL-2 (100-200 IU/mL) + IL-15 (10-20 ng/mL) for 24-48 hours to enhance transduction efficiency
Genetic Modification:
- Employ lentiviral or retroviral transduction with CAR constructs, typically achieving 30-60% transduction efficiency
- Alternative approach: Use electroporation for mRNA-based transient CAR expression (higher safety profile)
- Advanced engineering: Incorporate siRNA to downregulate HLA class I proteins, preventing host immune rejection [26]
CAR Construct Design:
- Second-generation CARs typically include: extracellular scFv targeting domain, hinge region, transmembrane domain, and intracellular signaling domains (CD3ζ plus co-stimulatory domains such as 4-1BB or CD28)
- Incorporate suicide genes (iCasp9) or elimination tags for safety control
- Logic-gate constructs: Include multiple antigen recognition domains with AND/NOT logic capabilities [25]
Expansion and Quality Control:
- Expand engineered NK cells using feeder cells (e.g., K562-based artificial antigen-presenting cells) or cytokine-only methods
- Culture for 14-21 days to achieve clinical-scale cell numbers (1-5×10^9 cells)
- Validate CAR expression by flow cytometry, cytotoxic function against target cells, and cytokine production profile
The following diagram illustrates the workflow for generating engineered "off-the-shelf" CAR-NK cells:
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents for NK Cell Therapy Development
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Isolation Kits | CD56 MicroBeads, CD3 Depletion Kits | NK cell purification from PBMCs | Positive/negative selection for pure NK populations |
| Cytokines | IL-2, IL-15, IL-21, IL-12, IL-18 | NK cell activation and expansion | Enhance cytotoxicity, persistence, and metabolic fitness |
| Activation Reagents | K562-based aAPCs, Fc-coated beads | Large-scale NK cell expansion | Provide co-stimulatory signals for proliferation |
| CAR Constructs | Lentiviral/retroviral vectors, mRNA | Genetic modification of NK cells | Introduce tumor-targeting specificity |
| Flow Cytometry Antibodies | Anti-CD56, CD16, NKG2D, NKp46 | Phenotypic characterization | Identify NK subsets and activation status |
| Functional Assays | Degranulation (CD107a), Cytotoxicity | Functional validation | Measure target cell killing capacity |
| Cell Lines | NK-92, NKL, K562, 721.221 | In vitro studies | Provide standardized models for experimentation |
NK cell therapies represent a transformative approach in the cell therapy landscape, distinguished by their unique innate immune mechanisms and compelling "off-the-shelf" potential. Their capacity for rapid, MHC-unrestricted target recognition, coupled with favorable safety profiles and reduced manufacturing constraints, positions them as powerful complements to established T-cell therapies. Current clinical evidence demonstrates particular promise in hematological malignancies, with ongoing engineering innovations addressing the challenges of solid tumors and therapeutic precision.
The future trajectory of NK cell therapy development will likely focus on enhancing persistence and functionality within suppressive tumor microenvironments, refining logic-gated control systems for improved safety profiles, and establishing scalable manufacturing platforms for widespread clinical accessibility. As the field advances toward later-stage clinical trials and potential regulatory approvals, NK cell therapies are poised to expand the armamentarium of cell-based immunotherapies, ultimately increasing treatment options for patients with diverse malignancies. Continued investigation into the fundamental biology of NK cells will undoubtedly reveal new opportunities for engineering refinement and therapeutic application across a broadening spectrum of diseases.
The therapeutic application of stem cells, particularly Mesenchymal Stem Cells (MSCs), is a cornerstone of modern regenerative medicine. For researchers and drug development professionals, a critical understanding of the two primary proposed mechanisms of action (MoA)—direct differentiation and paracrine signaling—is essential for designing effective therapies. Initially, the field was dominated by the paradigm of direct differentiation, where stem cells were thought to engraft and replace damaged tissues. However, emerging clinical and preclinical evidence now strongly suggests that the primary MoA is the secretion of bioactive molecules, a phenomenon known as paracrine signaling [28] [29]. This guide provides a comparative analysis of these mechanisms, supported by experimental data and methodologies, to inform strategic decisions in cell therapy research.
Direct Differentiation: The Engraftment and Replacement Hypothesis
The direct differentiation mechanism posits that administered stem cells migrate to the site of injury, engraft into the host tissue, and subsequently differentiate into specific functional cell types to replace those that are damaged or lost.
Supporting Experimental Evidence and Protocols
Evidence for this mechanism often comes from in vitro differentiation assays and in vivo lineage tracing.
In Vitro Trilineage Differentiation: This is a foundational protocol per the International Society for Cell & Gene Therapy (ISCT) criteria for defining MSCs [29]. The methodology involves culturing MSCs under specific conditions to induce differentiation.
- Osteogenic Differentiation: Culture MSCs in medium supplemented with dexamethasone, ascorbic acid, and β-glycerophosphate for 2-3 weeks. Differentiated osteoblasts are confirmed by staining for mineral deposits with Alizarin Red S [29].
- Chondrogenic Differentiation: Pellet cultures of MSCs are maintained in a medium containing TGF-β3 and dexamethasone for 3-4 weeks. Chondrogenesis is verified by staining for proteoglycans with Alizarin Blue or immunohistochemistry for collagen type II [29].
- Adipogenic Differentiation: Culture MSCs with dexamethasone, indomethacin, and insulin. Differentiated adipocytes are identified by the presence of lipid vacuoles stained with Oil Red O [29].
In Vivo Lineage Tracing: Advanced genetic fate-mapping in animal models is used to track the persistence and differentiation of transplanted donor cells. However, these studies frequently show low engraftment efficiency, with most donor cells being cleared within days to weeks [28].
Quantitative Data on Direct Differentiation
The following table summarizes key quantitative findings related to the direct differentiation mechanism:
Table 1: Experimental Data Supporting Direct Differentiation
| Evidence Type | Experimental Model | Key Finding | Reference/Context |
|---|---|---|---|
| In Vitro Differentiation | Human MSCs | Capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages (ISCT criteria). | [29] |
| In Vivo Engraftment | Murine Models | Low engraftment efficiency; donor cells are often transient. | [28] |
| Functional Improvement | Clinical Trials (e.g., Stroke) | Improvement in NIHSS, BI, and mRS scores observed over 6-12 months. | [30] |
Paracrine Signaling: The Bioactive Secretome as the Primary Driver
The paracrine signaling mechanism suggests that the therapeutic benefits of stem cells are mediated predominantly through their secretome—a complex mixture of growth factors, cytokines, and extracellular vesicles (EVs). These factors modulate the local microenvironment, reduce inflammation, promote angiogenesis, and activate endogenous repair pathways.
Molecular Mechanisms and Key Signaling Pathways
The paracrine effects are coordinated through several key signaling pathways that can be pharmacologically modulated to enhance therapeutic efficacy [31].
Figure 1: Key paracrine signaling pathways activated by the MSC secretome and their primary therapeutic effects.
Supporting Experimental Evidence and Protocols
- Secretome Analysis: The critical step is profiling the MSC-conditioned medium.
- Protocol: Serum-starve confluent MSCs and collect conditioned medium after 24-48 hours. Analyze the composition using proteomics (e.g., mass spectrometry for growth factors like VEGF, HGF), cytokine arrays, and techniques for characterizing extracellular vesicles (e.g., nanoparticle tracking analysis, electron microscopy) [32] [29].
- Functional In Vitro Assays:
- Angiogenesis Assay: Treat human umbilical vein endothelial cells (HUVECs) with MSC-conditioned medium. The formation of tube-like structures on a Matrigel substrate is quantified, demonstrating the pro-angiogenic effect of the secretome [32].
- Immune Modulation Assay: Isolate peripheral blood mononuclear cells (PBMCs) and stimulate them with a mitogen like concanavalin A. Co-culture with MSCs or their conditioned medium, and measure T-cell proliferation via 3H-thymidine incorporation or CFSE staining, confirming immunomodulatory capacity [29].
- In Vivo Validation with Cell-Free Therapies: The therapeutic efficacy of the secretome alone can be tested.
- Protocol: In a rodent myocardial infarction model, administer MSC-derived exosomes or concentrated conditioned medium versus a control. Evaluate outcomes through histology (reduction in infarct size), echocardiography (improvement in left ventricular ejection fraction), and immunohistochemistry (increased capillary density) [32] [28].
Quantitative Data on Paracrine Signaling
The table below consolidates quantitative evidence highlighting the significance of the paracrine mechanism.
Table 2: Experimental Data Supporting Paracrine Signaling
| Evidence Type | Experimental Model | Key Finding | Reference/Context |
|---|---|---|---|
| Cell Survival Post-Transplant | Coronary MSC Delivery | MSC survival rate < 5-10% within 72 hours, yet functional improvement is observed. | [32] [28] |
| Exosome/Secretome Efficacy | Rodent Myocardial Infarction | MSC-derived exosomes improve cardiac function, reduce fibrosis, and enhance vessel density. | [32] [28] |
| Clinical Safety & Efficacy | Stroke Clinical Trials | Significant functional recovery (NIHSS, BI) without correlation to long-term engraftment. | [30] |
| Specific Molecule Action | In Vitro/In Vivo Models | MSC exosomes carry miRNAs (e.g., miR-21, miR-146a) that regulate apoptosis and fibrosis. | [32] [29] |
Direct Comparison: Paracrine Signaling vs. Direct Differentiation
A head-to-head comparison of these mechanisms reveals distinct characteristics, with the paracrine effect offering several translational advantages.
Table 3: Comprehensive Comparison of Primary Therapeutic Mechanisms
| Feature | Direct Differentiation | Paracrine Signaling |
|---|---|---|
| Primary MoA | Cell replacement and structural integration. | Modification of the host microenvironment via secreted factors. |
| Therapeutic Speed | Slow (requires engraftment and maturation). | Relatively fast (immediate bioactivity of molecules). |
| Engraftment Requirement | Absolutely critical; a major technical hurdle. | Not required; effects are elicited transiently. |
| Key Evidence | In vitro trilineage differentiation; early histology. | Functional recovery despite low cell survival; efficacy of conditioned medium/exosomes. |
| Major Challenges | Extremely low efficiency; poor cell survival; risk of ectopic tissue formation. | Standardizing the secretome; manufacturing reproducible cell-free products. |
| Clinical Translation | Challenging due to engraftment barriers. | Highly promising; facilitates "off-the-shelf" and cell-free products. |
The following diagram synthesizes the experimental workflow for elucidating the dominant mechanism of action in a therapeutic context.
Figure 2: Experimental workflow for determining the primary mechanism of action (MoA).
The Scientist's Toolkit: Essential Research Reagents
Advancing research in this field requires a suite of reliable reagents and tools. The following table details key solutions for studying stem cell mechanisms.
Table 4: Essential Research Reagents for Investigating Stem Cell MoA
| Research Reagent / Solution | Function and Application | Experimental Example |
|---|---|---|
| Trilineage Differentiation Kits | Defined media supplements for in vitro induction of osteogenic, chondrogenic, and adipogenic lineages. | Validating multipotency of MSC batches per ISCT criteria [29]. |
| Cell Tracking Dyes (e.g., CFSE, PKH26) | Fluorescent labels for tracking the migration, persistence, and fate of administered cells in vivo. | Quantifying MSC engraftment and distribution in animal disease models [28]. |
| Exosome Isolation Kits | Polymer-based precipitation or size-exclusion chromatography for purifying extracellular vesicles from conditioned medium. | Isposing MSC-derived exosomes for functional cell-free therapy studies [32] [29]. |
| Cytokine & Growth Factor Arrays | Multiplexed immunoassays for simultaneous quantification of dozens of secreted proteins in conditioned medium. | Profiling the MSC secretome under different priming conditions (e.g., hypoxia) [29]. |
| CRISPR-Cas9 Systems | Gene-editing tool for knocking out (KO) specific genes in MSCs to study their functional role in the secretome. | Creating TGF-β1 KO MSCs to test the pathway's necessity for immunomodulation [31]. |
| SMAD & β-catenin Inhibitors | Small molecule inhibitors (e.g., SB431542 for TGF-β, IWR-1 for Wnt) to block specific signaling pathways. | Pharmacologically dissecting the contribution of pathways to MSC therapeutic effects [31]. |
The accumulated evidence from both preclinical models and clinical trials strongly positions paracrine signaling as the dominant mechanism of action for most MSC-based therapies. The observed functional recoveries in conditions like stroke and myocardial infarction, despite minimal long-term engraftment, are difficult to attribute to direct differentiation [30] [32] [28]. This paradigm shift has significant implications for drug development, redirecting focus towards optimizing the secretome, developing potent cell-free therapeutics, and utilizing pharmacological strategies to enhance endogenous stem cell function [31]. Future research will concentrate on standardizing secretome-based products, engineering MSCs to overexpress beneficial factors, and leveraging pharmacological modulators to precisely control stem cell fate and function, thereby ushering in a new era of safe and effective regenerative medicines.
For researchers and drug development professionals in the cell and gene therapy space, demonstrating a product's mechanism of action (MoA) and quantitatively measuring its biological activity through potency assays represents one of the most significant development challenges. Regulatory agencies worldwide recognize potency as a Critical Quality Attribute (CQA) that must be measured for each product lot to ensure the therapy will achieve its intended clinical effect [2] [33]. The fundamental relationship between these concepts can be visualized as a continuous chain: a therapy's MoA defines its functional attributes (potency), which must be measurable through biological assays, and successful execution of this mechanism in patients manifests as clinical efficacy [1].
The development path requires connecting laboratory measurements to clinical outcomes. As noted in analyses of FDA-approved cell therapy products (CTPs), "potency is laboratory whereas efficacy is clinical; and the two are tied together by the MOA" [1]. This perspective examines this critical link, exploring how MoA understanding directly shapes potency assay development, the challenges in correlating these assays with clinical outcomes, and emerging solutions for researchers developing advanced therapies.
MoA as the Foundation for Potency Assessment
Defining the Framework
Clear conceptual distinctions between mechanism of action, potency, and efficacy are essential for effective assay development and regulatory communication. According to recent frameworks published in the Journal of Translational Medicine, these key terms can be defined as follows [1]:
- Mechanism of Action (MoA): The specific process, often pharmacologic, through which a product produces its intended effect
- Potency: The attribute of a product that enables it to achieve its intended mechanism of action
- Potency Test: A test that measures the attribute of a product that enables it to achieve its intended mechanism of action
- Efficacy: The ability of the product to have the desired effect in patients
- Efficacy Endpoint: Attributes related to how a patient feels, functions, or survives
This framework highlights that potency and efficacy, while related, exist in different domains - with potency being a product attribute measurable in the laboratory, and efficacy being the clinical manifestation of that attribute in patients.
Current Landscape of Approved Therapies
Analysis of the 27 FDA-approved cell therapy products (as of February 2024) reveals significant challenges in connecting MoA, potency, and clinical efficacy. For many products, including Provenge, Gintuit, MACI, and Amtagvi, regulatory documentation indicates that the MoA is not fully known [1]. For other therapies like Kymriah, the first approved CAR-T cell therapy, regulators have noted difficulty correlating potency test results with efficacy, despite the product demonstrating clinical benefit [1].
Table 1: MoA and Potency Assessment in Approved Cell Therapies
| Product Name | Therapy Type | Indication | Reported MoA Understanding | Potency Test Correlation |
|---|---|---|---|---|
| Kymriah | CAR-T Cell | Leukemia | Targeted cell destruction | Difficult to correlate IFN-γ production with efficacy |
| Provenge | Autologous Cellular | Prostate Cancer | Not known | Based on CD54 upregulation |
| MACI | Tissue-Engineered | Cartilage Defects | Not known | Cell viability and morphology |
| Gintuit | Allogeneic Cellular | Mucosal Tissue | Not known | Cell viability and identity |
| Amtagvi | Autologous T Cell | Melanoma | Not known | T cell activation and phenotype |
| Rethymic | Allogeneic Cellular | Congenital Athymia | Proposed | T cell population composition |
| Lantidra | Allogeneic Islet Cell | Type 1 Diabetes | Believed | Insulin secretion and mitochondrial function |
MoA-Based Potency Assay Development: Methodologies and Case Studies
CAR T-Cell Therapy: Multi-Functional Assessment
For CAR T-cell therapies, the MoA involves a multi-step process beginning with antigen recognition, followed by T-cell activation, proliferation, cytokine release, and ultimately target cell destruction [11]. This complex mechanism necessitates a matrix of potency assays that capture these different functional dimensions:
- Immediate Effector Function: Measured through cytotoxicity assays, cytokine release (IFN-γ, TNF-α, IL-2), and degranulation markers (e.g., LAMP1 expression)
- Expansion Capacity: Assessed through cell proliferation and viability measurements
- Persistence Potential: Evaluated through phenotypic characterization, in vivo tracking, and CAR transgene expression monitoring [11]
The potency of FDA-approved CAR T-cell products is primarily assessed by measuring IFN-γ release in response to target cells, alongside other factors including cell viability and CAR expression levels [11]. However, recent advances in multi-omics approaches are revealing additional product characteristics that correlate with clinical function, suggesting future potency assays may need greater sophistication.
Table 2: CAR T-Cell Potency Assay Matrix Based on MoA Components
| MoA Component | Assay Type | Measured Parameters | Technology Platforms |
|---|---|---|---|
| Antigen Recognition | Binding Assay | CAR surface expression, binding affinity | Flow cytometry, SPR |
| T-cell Activation | Functional Assay | Activation markers, early signaling | CD69/CD137 detection, phospho-flow |
| Effector Function | Co-culture Assay | Cytotoxicity, cytokine secretion | Incucyte, ELISA, Luminex |
| Expansion Capacity | Proliferation Assay | Cell division, population doubling | CFSE dilution, cell counting |
| Persistence Potential | Phenotypic Assay | Memory markers, exhaustion markers | scRNA-seq, flow cytometry |
CD34+ Cell Therapy: Pro-angiogenic Secretion
For ProtheraCytes (expanded autologous CD34+ cells) used in myocardial regeneration, the MoA involves revascularizing damaged myocardial tissue through secretion of pro-angiogenic factors, particularly vascular endothelial growth factor (VEGF) [34]. This understanding directly informed the development of a potency assay based on VEGF quantification during CD34+ cell expansion.
Experimental Protocol: VEGF Potency Assay Validation
- Cell Culture: CD34+ cells from AMI patients expanded for 9 days in StemFeed medium
- Sample Collection: Supernatants collected after expansion period
- Analysis Platform: Automated ELLA immunoassay system with VEGF cartridge
- Validation Parameters: Specificity, linearity (20-2800 pg/mL), precision (CV ≤10% repeatability, ≤20% intermediate precision), accuracy (85-105% recovery) [34]
The validated assay demonstrated significant VEGF secretion (596.2 ± 242.3 pg/mL in AMI patients, comparable to healthy donors) while negative controls (culture medium alone) showed minimal VEGF (2.8 ± 0.2 pg/mL) [34]. This MoA-based approach provided a quantitative, reproducible potency measure that regulatory agencies deemed acceptable for clinical batch release.
Gene Therapy: Functional Transgene Assessment
For gene therapies like voretigene neparvovec (Luxturna), an AAV2 vector expressing RPE65 for retinal disease, the MoA involves successful transduction of target cells and functional transgene expression producing biologically active protein [35]. This informed development of a cell-based relative potency assay measuring both transduction efficiency and enzymatic activity.
Experimental Protocol: Luxturna Potency Assay
- Cell Line: HEK293 cells
- Transduction: AAV2-hRPE65v2 vector
- Functional Readout: RPE65 enzymatic conversion of all-trans-retinol to 11-cis-retinol
- Quantification Method: Liquid chromatography with tandem mass spectrometry (LC-MS/MS)
- Validation Range: 50%-150% of reference standard potency [35]
This approach successfully supported regulatory approval by demonstrating lot-to-lot consistency and biological activity aligned with the therapy's MoA, representing the first validated in vitro cell-based relative potency assay for an AAV vector [35].
Advanced Technologies and Methodologies
Multi-Omics Approaches in Potency Assessment
Advanced profiling technologies are expanding our understanding of CAR T-cell products at multiple molecular levels, revealing new potential potency correlates:
- Genomic Profiles: Vector copy number (VCN), integration sites, TCR repertoire diversity
- Epigenomic Profiles: DNA methylation patterns, chromatin accessibility associated with persistence
- Transcriptomic Profiles: Gene expression signatures, T-cell differentiation states
- Proteomic Profiles: Protein expression, activation markers, cytokine secretion
- Metabolomic Profiles: Metabolic fitness, energy pathways [11]
These approaches are particularly valuable for identifying correlates of clinical response. For example, DNA methylation analysis of 114 CD19 CAR T-cell products identified 18 distinct epigenetic loci associated with complete response, event-free survival, and overall survival [11].
Essential Research Reagents and Tools
Table 3: Research Reagent Solutions for MoA-Based Potency Assays
| Reagent/Tool | Function in Potency Assessment | Application Examples |
|---|---|---|
| Automated Immunoassay Systems (e.g., ELLA) | Quantitative protein detection | VEGF measurement in CD34+ cell supernatants [34] |
| Custom Cell Mimics (e.g., TruCytes) | Standardized target cells for functional assays | CAR T-cell activation and cytokine response [2] |
| Single-Cell RNA Sequencing | Transcriptional profiling at single-cell resolution | T-cell differentiation states, exhaustion signatures [11] |
| Droplet Digital PCR (ddPCR) | Absolute quantification of vector copy number | CAR transgene quantification for lot-release [11] |
| LC-MS/MS Systems | Quantitative analysis of enzymatic products | RPE65 enzymatic activity in gene therapy [35] |
| Flow Cytometry Panels | Multiparameter cell surface and intracellular staining | Immunophenotyping, activation markers, memory subsets |
Visualizing the MoA-Potency-Efficacy Relationship
The following diagram illustrates the conceptual framework and experimental workflow connecting MoA understanding to potency assay development and clinical efficacy assessment:
MoA to Efficacy Assessment Pathway - This diagram maps the logical relationships from mechanism of action understanding through potency measurement to clinical efficacy evaluation.
The experimental workflow for developing and validating MoA-based potency assays follows a systematic process:
Potency Assay Development Workflow - This chart outlines the staged process from initial MoA research through to validated assay implementation for product lot release.
Challenges and Future Directions
Correlation with Clinical Outcomes
A fundamental challenge in potency assay development remains demonstrating correlation between in vitro potency measurements and clinical efficacy. Analysis of the Kymriah clinical program revealed that while IFNγ production (the potency measure) showed some correlation with remission, there was significant overlap between responders and non-responders [1]. FDA documentation noted that "IFN-γ production varied greatly from lot-to-lot, making it difficult to correlate IFN-γ production in vitro with tisagenlecleucel safety or efficacy" [1].
This challenge is compounded when MoA is incompletely understood. As noted in analyses of approved products, "for many of the 27 US FDA-approved CTPs, the relationships between the potency tests and proposed MOAs are unclear" [1]. This reality necessitates a pragmatic approach where products may receive regulatory approval based on demonstrated clinical efficacy and acceptable risk-benefit profile, even when the potency test doesn't fully correlate with efficacy endpoint test results [1].
Emerging Solutions and Strategies
Several strategies are emerging to address these challenges:
- Early Potency Planning: Initiating potency assay development during preclinical stages helps guide process decisions and prevent late-stage delays [2] [36]
- Assay Matrices: For complex therapies with multifaceted MoAs, a matrix of complementary potency assays may better capture biological activity than any single assay [11]
- Advanced Analytics: Multi-omics approaches can identify novel potency correlates that better predict clinical performance [11]
- Standardized Reagents: Custom cell mimics and other standardized tools enable more reproducible potency assessment [2]
The field continues to evolve toward more predictive potency models that better reflect the complex biology of advanced therapies while meeting regulatory requirements for quantifiable, reproducible measurements of biological activity.
The critical link between MoA understanding, potency assay development, and clinical efficacy remains both a scientific and regulatory imperative for cell and gene therapy developers. While significant challenges persist in correlating in vitro potency measurements with clinical outcomes, the continued refinement of MoA-based assays, coupled with advanced analytical technologies, is steadily strengthening this connection. By anchoring potency assessment in rigorous MoA understanding and employing a strategic approach to assay development throughout the product lifecycle, researchers can better ensure their therapies will deliver consistent clinical benefits to patients while navigating the complex regulatory pathway to approval.
From Blueprint to Bench: Analytical Methods and Potency Assurance for MoA Demonstration
In cell therapy development, a product's potency—its specific biological activity—is a critical quality attribute (CQA) that regulatory agencies require be measured for every product lot to ensure intended clinical effects [2]. Traditionally, potency assessment has relied on single-parameter assays, such as measuring IFN-γ release in response to target cells for CAR-T therapies [37]. However, as cell therapies evolve in complexity, these conventional approaches fail to capture the multifaceted biological mechanisms underlying therapeutic efficacy.
The mechanism of action (MoA) of cell therapies involves a coordinated sequence of events: target recognition, cell activation, proliferation, cytotoxic activity, and long-term persistence [37]. A robust potency strategy must therefore transition from single-parameter measurements to a comprehensive matrix of assays that collectively reflect this functional complexity. This guide compares conventional and emerging approaches to potency testing, providing researchers with the experimental frameworks needed to develop MoA-aligned potency matrices that ensure product consistency, guide process optimization, and satisfy evolving regulatory expectations.
Comparative Analysis of Potency Assay Strategies
The table below objectively compares the performance characteristics of different potency assay approaches, highlighting how multi-parameter strategies address the limitations of conventional methods.
Table 1: Performance Comparison of Potency Assay Strategies
| Assay Characteristic | Traditional Single-Parameter | Functional Multi-Parameter | Multi-Omics Profiling |
|---|---|---|---|
| MoA Coverage | Limited to one functional dimension (e.g., cytokine release) | Captures multiple functional dimensions (cytotoxicity, activation) | Provides comprehensive molecular profiling beyond function |
| Correlation with Clinical Outcomes | Moderate; may miss critical contributors | Stronger; captures integrated functional capacity | Potentially predictive; identifies novel biomarkers |
| Regulatory Acceptance | Well-established for some products | Increasingly expected for complex therapies | Emerging; used for characterization and lot-to-lot comparison |
| Technical Variability | Typically low | Moderate, requires careful optimization | Higher, especially in single-cell methods |
| Implementation Timeline | Weeks | Several months | 6+ months for establishment |
| Cost Considerations | Lower | Moderate | Higher |
| Key Limitations | May not predict full therapeutic effect | May not fully explain mechanistic basis of potency | Complex data interpretation; standardization challenges |
Experimental Protocols for Multi-Parameter Potency Assessment
Protocol 1: Functional Co-culture Assay for Cytotoxic Potency
This protocol measures direct cytotoxic activity, a fundamental MoA for many cell therapies.
Materials and Reagents:
- Target cells (appropriate antigen-positive cell line or primary cells)
- Effector cells (CAR-T or other cell therapy product)
- Culture medium (RPMI-1640 + 10% FBS)
- 96-well U-bottom plates
- Flow cytometer with apoptosis detection capabilities
- Recombinant human IL-2 (optional)
Procedure:
- Target Cell Preparation: Harvest and count target cells. Label with CFSE (5 μM, 15 min, 37°C) if distinguishing by flow cytometry.
- Effector Cell Preparation: Thaw and rest effector cells overnight in complete medium with IL-2 (50 U/mL).
- Co-culture Setup: Plate target cells at 5,000 cells/well in 96-well plates. Add effector cells at effector-to-target (E:T) ratios of 1:1, 5:1, and 10:1. Include target-only and effector-only controls.
- Incubation: Incubate for 24-48 hours at 37°C, 5% CO₂.
- Analysis: Harvest cells and stain with Annexin V/PI or alternative viability dyes. Analyze by flow cytometry. Calculate specific lysis as: (\% dead targets in co-culture - \% spontaneous dead targets in control) / (100 - \% spontaneous dead targets in control) × 100.
Data Interpretation: The assay provides quantitative cytotoxicity measurements across multiple E:T ratios, generating a potency curve rather than a single endpoint.
Protocol 2: Multi-Omics Readiness Assessment
This advanced protocol evaluates cellular characteristics predictive of in vivo performance.
Materials and Reagents:
- Cell therapy product (fresh or properly preserved)
- RNA/DNA extraction kits
- Single-cell RNA sequencing platform (10X Genomics or equivalent)
- Seahorse XF Analyzer and assay kits
- Flow cytometer with >15-parameter capability
- Cytometry by Time-of-Flight (CyTOF) equipment (optional)
Procedure:
- Transcriptomic Profiling:
- Extract total RNA from product aliquots.
- Perform bulk RNA-seq or single-cell RNA-seq per manufacturer protocols.
- Analyze data for memory, exhaustion, and activation signatures.
Metabolic Profiling:
- Seed 2×10⁵ cells/well in Seahorse XFp cell culture miniplates.
- Perform mitochondrial stress test per manufacturer protocol.
- Calculate basal respiration, maximal respiration, and spare respiratory capacity.
High-Dimensional Phenotyping:
- Stain cells with antibody panel targeting differentiation (CD45RO, CD62L), inhibition (PD-1, TIM-3, LAG-3), and activation (CD69, CD25) markers.
- Acquire data on flow cytometer or CyTOF.
- Analyze using dimensionality reduction algorithms (t-SNE, UMAP).
Data Interpretation: Integrated analysis reveals correlations between transcriptional states, metabolic fitness, and surface phenotypes that collectively predict in vivo expansion and persistence.
Visualizing the Multi-Dimensional Potency Matrix
The following diagram illustrates the conceptual framework for building a comprehensive MoA-aligned potency matrix, integrating various analytical dimensions to fully characterize cell therapy products.
Diagram 1: MoA-Aligned Potency Matrix Framework
Essential Research Reagent Solutions
The table below details key reagents and their applications in developing robust potency assays, providing researchers with a practical resource for experimental planning.
Table 2: Essential Research Reagents for Potency Assay Development
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Reference Materials | Custom cell mimics (e.g., TruCytes) | Potency assay standardization | Provide consistent antigen-positive targets for functional assays; enable earlier assay development [2] |
| Cell Culture Supplements | Recombinant human cytokines (IL-2, IL-7, IL-15) | Cell expansion and maintenance | Support viability and preserve functional properties during assay execution |
| Detection Antibodies | Fluorochrome-conjugated antibodies for flow cytometry/CyTOF | High-dimensional phenotyping | Enable simultaneous measurement of multiple surface and intracellular markers |
| Functional Assay Kits | Cytotoxicity detection (Annexin V, LDH), metabolic assays (Seahorse) | Functional potency assessment | Quantify target cell killing and cellular metabolic fitness |
| Genomic Analysis Kits | TCR sequencing, viral integration site analysis (INSPIIRED) | Genomic profiling | Assess TCR diversity and monitor vector integration safety [37] |
| Transcriptomic Tools | Single-cell RNA-seq kits, bulk RNA-seq reagents | Transcriptional profiling | Characterize differentiation states and identify predictive signatures |
Implementation Strategy and Regulatory Considerations
Successful implementation of a potency matrix requires careful planning and staging throughout the product development lifecycle. During preclinical stages, focus should be on comprehensive product characterization using research-grade assays to identify key parameters that correlate with biological activity. By Phase 1-2 clinical trials, these methods should transition toward assays amenable to qualification, using standardized reagents and controls. For late-stage development and commercialization, the potency assay matrix must be fully validated according to regulatory guidelines, demonstrating accuracy, precision, linearity, range, and robustness [2].
Regulatory agencies emphasize that potency assays should be quantitative and reflect the biological MoA [2]. The multi-parameter approach detailed here addresses this expectation by capturing the complexity of cell therapy products rather than relying on oversimplified surrogate measurements. When making process changes, this comprehensive matrix provides compelling evidence of comparability by demonstrating consistent product characteristics across multiple orthogonal dimensions.
As cell therapies grow increasingly sophisticated, so too must our approaches to potency assessment. The multi-parameter matrix framework presented here moves beyond traditional single-parameter assays to provide a comprehensive characterization approach aligned with complex mechanisms of action. By integrating functional, genomic, transcriptomic, and metabolic dimensions, researchers can develop robust potency models that not only satisfy regulatory requirements but also provide meaningful insights into product quality and consistency. This comprehensive approach ultimately accelerates development by enabling data-driven decisions, facilitating process improvements, and ensuring that patients receive cell therapies with predictable and potent biological activity.
Understanding the Mechanism of Action (MoA) of cell therapies, such as Chimeric Antigen Receptor (CAR) T-cell therapies, is critical for their development and regulatory approval. These complex biological products require robust analytical methods to demonstrate their potency, safety, and identity. A comprehensive MoA investigation hinges on three key analytical technology pillars: flow cytometry for cell phenotyping and transgene expression, cytokine release assays for assessing T-cell activation and functionality, and cell-based killing assays for quantifying cytotoxic potency. These methods provide orthogonal data that, when combined, offer a deep understanding of how a cell therapy product engages with its target, becomes activated, and executes its intended therapeutic function. This guide objectively compares the performance and applications of these technologies, providing researchers and drug development professionals with the experimental data and protocols needed to inform their analytical strategies.
Technology Comparison and Performance Data
The following tables provide a structured comparison of the three key analytical technologies, summarizing their primary applications, performance characteristics, and relative advantages.
Table 1: Overview and Applications of Key Analytical Technologies
| Technology | Primary Application in MoA | Measurable Parameters | Throughput | Key Advantage |
|---|---|---|---|---|
| Flow Cytometry | Cell phenotyping, Transgene expression (e.g., CAR+), Intracellular cytokine staining [38] | % CAR+ cells, Immune cell subsets, Surface receptor expression (e.g., PD-1, TIGIT) [39] | Medium | Multiplexing of surface and intracellular markers at single-cell resolution. |
| Cytokine Release Assay | Functional potency, T-cell activation [38] | Concentration of IFN-γ, TNF, ILs via ELISA/ELLA/MSD [38] | High | Quantifies a critical downstream functional response to activation. |
| Cell-Based Killing Assay | Functional potency, Cytotoxic activity [40] [38] | % Specific lysis of target cells (via luminescence, impedance, flow cytometry) [40] | Low to Medium | Directly measures the fundamental cytotoxic function of the product. |
Table 2: Performance Comparison of Cytokine Release Assay Platforms
| Assay Platform | Technology Principle | Sensitivity (IFN-γ) | Multiplexing Capability | Key Experimental Findings |
|---|---|---|---|---|
| Flow Cytometry ICS | Intracellular Cytokine Staining [41] | Higher (detected 134/141 vs 120/141 positive samples in a comparative study) [41] | High (can be combined with phenotyping) | Greater sensitivity for detecting SARS-CoV-2-S-reactive T cells compared to QuantiFERON [41]. |
| QuantiFERON | ELISA-based cytokine detection from plasma [41] | Lower | Low (single analyte per tube) | Significantly discordant results vs. FC-ICS, with most discrepancies being FC-ICS+/QF- [41]. |
| One-Step Multiplex FCM Assay | Bead-based immunoassay with lyophilized reagents [42] [43] | Similar to conventional FCM | High (12-plex demonstrated) | Reduces operation and reaction time; enables machine learning analysis of patient stratification [42] [43]. |
| ELLA (Automated Immunoassay) | Microfluidic cartridge-based immunoassay [40] | Not explicitly stated | Medium | Automates and standardizes the cytokine detection process, reducing labor [40]. |
Table 3: Performance Comparison of Cell-Based Killing Assay Platforms
| Assay Platform | Technology Principle | Label / Readout | Throughput | Key Experimental Findings |
|---|---|---|---|---|
| 51Cr Release Assay | Radioactive isotope release [40] | 51Cr in supernatant | Low | Historical gold standard; involves radioactive materials and waste [40]. |
| Flow Cytometry Killing Assay | Differential staining of effector and target cells [40] | Fluorescent cell labels / viability dyes | Medium | Allows endpoint analysis of different cell populations and can identify specific mechanisms of death [40]. |
| Impedance-Based (e.g., xCELLigence) | Real-time cell impedance monitoring [40] | Label-free (electrical impedance) | Medium | Provides real-time, label-free monitoring of cell killing in co-culture [40]. |
| Luminescence-Based | Release of luminescent markers (e.g., LDH) | Luminescence signal | High | Amenable to higher-throughput formats; measures membrane integrity. |
| Incucyte Live-Cell Analysis | Time-lapse imaging with fluorescent labels [40] | Fluorescence (e.g., caspase activation) | Medium | Offers real-time monitoring of cell death; requires fluorescent labelling of cells [40]. |
Experimental Protocols for Key Assays
One-Step Multiplex Cytokine Assay via Flow Cytometry
This protocol, adapted from a 2025 study, simplifies the conventional multi-step cytokine detection process into a single incubation step, reducing hands-on time and facilitating rapid profiling [42] [43].
Detailed Methodology:
- Reagent Preparation: Capture antibodies are conjugated to fluorescently encoded microspheres using an EDC and sulfo-NHS coupling method. Detection antibodies are labeled with Phycoerythrin (PE) via SMCC and DTT crosslinking [42]. These reagents are lyophilized together in a buffer containing PBS, BSA, and stabilizers like trehalose or mannitol to form stable reagent beads that do not require cold storage [42] [43].
- Assay Procedure:
- Add 100 µL of standard or clinical serum sample to a well of a 96-well plate containing the lyophilized reagent bead [42] [43].
- Incubate the plate with shaking at room temperature for 1.5 hours.
- Wash the beads to remove unbound components.
- Add reading buffer and analyze the plate immediately on a flow cytometer (e.g., Beckman Coulter DxFlex) [42].
- Data Analysis: The flow cytometer identifies the cytokine-specific bead based on its fluorescent encoding and quantifies the amount of bound cytokine via the PE signal. Data can be analyzed using machine learning models (e.g., logistic regression, random forest) for patient stratification or predicting disease severity [42].
Intracellular Cytokine Staining (ICS) Assay for T-cell Functionality
This protocol measures the frequency of antigen-reactive T cells capable of producing cytokines like IFN-γ upon stimulation [41].
Detailed Methodology:
- Stimulation:
- Collect heparinized whole blood.
- Aliquot 0.5 mL of blood and stimulate with a peptide mix (e.g., overlapping peptides spanning the SARS-CoV-2 Spike protein at 1 μg/mL per peptide) in the presence of costimulatory antibodies (anti-CD28 and anti-CD49d, 1 μg/mL each) [41].
- Include a mock-stimulated control (PBS/DMSO with costimulatory antibodies).
- Incubate for 6 hours at 37°C. Add Brefeldin A (10 μg/mL) for the last 4 hours of incubation to inhibit protein transport and allow cytokine accumulation intracellularly.
- Staining and Fixation:
- Lyse red blood cells using a commercial lysing solution (e.g., BD FACS lysing solution).
- Permeabilize cells (e.g., using BD permeabilizing solution).
- Stain cells with a combination of fluorescently labeled monoclonal antibodies: typically, anti-CD3, anti-CD4 or anti-CD8, and anti-IFN-γ [41].
- Include positive (e.g., phytohemagglutinin) and isotype controls.
- Analysis: Analyze the cells on a flow cytometer. Gate on CD3+CD4+ or CD3+CD8+ T cells and analyze for IFN-γ production. The result is expressed as the percentage of cytokine-producing T cells after background (mock control) subtraction [41].
Flow Cytometry-Based Cytotoxicity Assay
This protocol uses differential fluorescent labeling to distinguish effector from target cells and quantify target cell killing.
Detailed Methodology:
- Cell Labeling:
- Co-culture:
- Seed labeled target cells in a culture plate.
- Add effector cells at a specific Effector:Target (E:T) ratio (e.g., 1:2) [45].
- Include control wells with target cells alone (to determine spontaneous death) and target cells with a lytic agent (to determine maximum death).
- Centrifuge the plate briefly to initiate cell contact and incubate at 37°C for a defined period (e.g., 4-24 hours).
- Staining and Analysis:
- After incubation, stain the cells with a viability dye (e.g., Propidium Iodide or 7-AAD).
- Analyze by flow cytometry.
- Gate on the target cell population based on their fluorescent label and determine the percentage of dead target cells by quantifying the proportion of viability dye-positive cells.
- Calculation:
- Calculate % Specific Lysis using the formula:
( % Death in Test - % Spontaneous Death ) / ( % Maximum Death - % Spontaneous Death ) * 100
- Calculate % Specific Lysis using the formula:
Signaling Pathways and Experimental Workflows
The following diagrams, generated using DOT language, illustrate the core signaling pathways in T-cell activation and the standard workflows for the key assays discussed.
T-cell Activation and Cytokine Signaling Pathway
T-cell Activation and Cytokine Signaling Pathway
One-Step Multiplex Cytokine Assay Workflow
One-Step Multiplex Cytokine Assay Workflow
Flow Cytometry Killing Assay Workflow
Flow Cytometry Killing Assay Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of these analytical methods relies on a suite of critical reagents and instruments. The table below details essential materials and their functions in the context of cell therapy MoA research.
Table 4: Key Research Reagent Solutions for Cell Therapy MoA Assays
| Reagent / Material | Function / Application | Specific Examples / Targets |
|---|---|---|
| Fluorescently Labeled Antibodies | Cell phenotyping, intracellular staining, detection. | Anti-CD3, CD4, CD8, CD45, CAR detection antibody, IFN-γ [42] [41]. |
| Capture Microspheres / Beads | Multiplexed analyte detection. | Carboxylated fluorescently encoded microspheres for cytokine capture [42] [43]. |
| Cell Viability & Tracking Dyes | Distinguish live/dead cells, track cell divisions. | Propidium Iodide, 7-AAD, CellTrace Violet, Vibrant-DiD [44]. |
| Stimulation Cocktails | Activate T-cells to induce cytokine production. | Peptide pools (e.g., SARS-CoV-2 S protein peptides), PMA/Ionomycin, Costimulatory antibodies (anti-CD28/CD49d) [41]. |
| Protein Transport Inhibitors | Retain cytokines intracellularly for ICS. | Brefeldin A, Monensin [41]. |
| Lyophilization Stabilizers | Preserve reagent activity without cold chain. | Trehalose, Mannitol, BSA in PBS buffer [42] [43]. |
| Target Cell Lines | Serve as antigen-presenting targets in killing/activation assays. | Cell lines expressing the target antigen (e.g., PSCA for prostate cancer models) [45] [38]. |
| Flow Cytometer | Multi-parameter cell analysis and sorting. | Beckman Coulter DxFlex, BD LSRFortessa, spectral analyzers [42] [41]. |
| ELISA/ELLA/MSD Platforms | Quantify soluble cytokine concentrations. | QuantiFERON kits, ELLA (ProteinSimple), MSD platforms [40] [41]. |
For cell therapy developers, navigating the path to a successful Investigational New Drug (IND) application requires a sophisticated understanding of how to balance analytical robustness with development speed. The complex biological nature of cell therapies, combined with often expedited regulatory pathways like Accelerated Approval or Regenerative Medicine Advanced Therapy (RMAT) designation, creates unique challenges for Chemistry, Manufacturing, and Controls (CMC) teams [46]. These accelerated pathways typically compress development timelines, forcing teams to perform critical validation and manufacturing activities in parallel with significantly less time to develop the full suite of analytical methods needed for a traditional Biologics License Application (BLA) [46].
At the heart of this challenge lies the fundamental tension between method precision and accuracy—two distinct but interrelated measurement concepts that must be prioritized appropriately throughout development. Precision, the ability to obtain consistent results repeatedly when conducting an assay on the same substrate, provides the foundation for dose escalation studies in Phase I clinical trials [46]. Accuracy, which refers to how closely a method's result matches an accepted reference value, often becomes a greater focus as products move toward later-stage development and commercialization [46]. Understanding how to strategically balance these attributes in a phase-appropriate manner is critical for IND success and ultimately for delivering life-saving therapies to patients in need.
Comparative Analysis of Phase-Appropriate Analytical Strategies
Strategic Prioritization Across Development Phases
A phase-appropriate approach to analytical development continues to be widely accepted and adopted to support the clinical development of cell and gene therapies [47]. This strategy recognizes that analytical methods should evolve throughout the product lifecycle, with increasing rigor and validation as programs advance from preclinical studies to commercial marketing applications. The life cycle of analytical methods closely aligns with the product life cycle, beginning with method development activities to establish methods that address potential critical quality attributes (pCQAs) before initiating first-in-human studies [47].
Table 1: Analytical Method Requirements Across Development Phases
| Development Phase | Primary Analytical Focus | Precision Requirements | Accuracy Requirements | Key Validation Elements |
|---|---|---|---|---|
| Preclinical/Phase I | Safety, identity, dose-finding | High precision essential for dose escalation [46] | Demonstrated for safety-related methods [47] | Specificity, precision, linearity [48] |
| Phase II | Refining CQAs, understanding MOA | Intermediate precision across analysts/instruments [49] | Accuracy established for potency and characterization methods | Add accuracy, range, robustness [48] |
| Phase III/BLA | Commercial consistency, stability | Full validation including intermediate precision [47] | Comprehensive accuracy demonstration across method range | Full ICH Q2(R2) validation including robustness [49] |
For early-phase development, the emphasis typically shifts toward precision, particularly for methods such as cell count and viability, as this foundation supports critical early development decisions and initial clinical safety [46]. Under the pressure of expedited timelines and tight budgets, teams may be tempted to defer implementation of system-suitability controls and method qualification, only to discover at the IND or Phase 2 stage that the data aren't reliable [46]. The result of such shortcuts is often costly method redevelopment, comparability studies, and IND revisions—creating significant delays in getting therapies to patients.
MoA-Aligned Potency Method Development
One of the most challenging aspects of developing advanced cell therapy products is defining the mechanism of action (MOA), potency, and efficacy of the product [1]. US regulations require that cell therapies have a potency test for licensure, and these tests should ideally be based on the product's MOA [1]. The fundamental relationship between these concepts can be visualized through potency and efficacy process charts that distinguish six key elements: MOA, potency, potency test, efficacy, efficacy endpoint, and efficacy endpoint test [1].
For cell therapies, a single method often cannot effectively measure a product's complex MOA. Therefore, a MOA-aligned potency and characterization matrix—which connects product quality to biology, accounts for variability, supports comparability, and correlates with outcomes—guides development decisions and builds regulatory confidence for IND submissions [46]. This approach is often factored into the potency assurance strategy and typically involves multiple assay formats that collectively reflect the biological activity of the therapeutic product.
Table 2: MOA-Aligned Potency Assay Comparison
| Assay Format | Key Strengths | Key Limitations | Phase-Appropriate Application | Example Cell Therapy Applications |
|---|---|---|---|---|
| Cytokine Release | Functional, quantitative, can correlate with clinical response [1] | May not fully capture complex biology | Late-phase optimization | CAR-T therapies (e.g., IFN-γ secretion [1]) |
| Cell Killing/Viability | Direct measurement of proposed MOA | May not reflect secondary mechanisms | Early-phase development | CAR-T, NK cell therapies |
| Gene Expression | Can capture complex phenotypic changes | Requires deep biological understanding | Early characterization | Macrophage therapies, stem cell therapies |
| Multi-parameter Flow Cytometry | High-content, single-cell resolution | Complex data analysis, qualification challenges | Phase I/II characterization | Immune cell therapies |
| Biomarker Secretion | Functional, quantifiable, scalable | May represent surrogate marker only | Phase-appropriate from early development | Engineered macrophage therapies (e.g., IL-10, MMP9 [50]) |
The experience with Kymriah (tisagenlecleucel), the first CAR-T therapy approved by the FDA, illustrates the challenges in correlating potency measurements with clinical outcomes. While the potency was defined as the ability of CAR-T cells to secrete interferon-γ following exposure to target cells expressing CD19, the FDA noted that "IFN-γ production varied greatly from lot-to-lot, making it difficult to correlate IFN-γ production in vitro with tisagenlecleucel safety or efficacy" [1]. This highlights the very real challenge of ensuring that potency assays not only measure biological activity but also reflect clinical performance.
Experimental Protocols for Robust Analytical Development
Phase-Appropriate Method Validation Protocols
The validation of analytical procedures follows a phase-appropriate approach that gradually increases in rigor throughout clinical development. While validation is usually not required for original IND submissions for Phase 1 studies, it should be demonstrated that test methods are appropriately controlled and scientifically sound [47]. The International Council for Harmonisation (ICH) Q2(R2) guideline provides the framework for analytical method validation, recognizing that "the scientific principles described in this guideline can be applied in a phase-appropriate manner during clinical development" [47].
Early-Phase Validation Protocol (Phase I/II): For early-phase cell therapy programs, method qualification typically focuses on the parameters most critical for initial safety and dosing decisions. A phase-appropriate validation for a Phase I material should include assessment of accuracy, precision, linearity, specificity, and detection/quantitation limits [48]. The experimental approach involves:
- Accuracy Assessment: Spike recovery studies using known quantities of analyte in relevant matrix, with target recovery typically 80-120% for biological assays [49]
- Precision Evaluation: Minimum of six replicate measurements of a single sample to determine repeatability, expressed as relative standard deviation (RSD) [49]
- Linearity Testing: Series of minimum five concentrations across the anticipated range, with correlation coefficient (R²) typically ≥0.98 [49]
- Specificity Demonstration: Testing against potentially interfering matrix components to ensure selective measurement of the analyte [49]
Late-Phase Validation Protocol (Phase III/BLA): As products advance toward commercialization, method validation expands to include additional parameters that ensure robustness and reliability in a commercial setting. The experimental protocol expands to include:
- Intermediate Precision: Testing variations across different analysts, instruments, and days to assess method consistency [49]
- Robustness Testing: Deliberate variations in method parameters (e.g., temperature, pH, incubation times) to establish operating ranges [49]
- Range Establishment: Demonstration that method provides acceptable accuracy, precision, and linearity throughout the entire claimed range [49]
- Solution Stability: Evaluation of analyte stability under various storage conditions and timepoints [48]
MoA-Aligned Potency Assay Development Protocol
Developing meaningful potency assays for cell therapies requires a systematic approach that connects analytical measurements to biological function. Resolution Therapeutics' development of a "mode of action-based testing suite" for their regenerative macrophage therapy RTX001 provides an excellent example of this approach [50]. Their experimental protocol included:
Anti-inflammatory MoA Assessment:
- Phagocytosis Assay: Quantitative measurement of the ability of engineered macrophages to engulf fluorescently-labeled particles or cellular debris [50]
- Monocyte Recruitment Assay: Evaluation of chemotactic factor secretion and subsequent monocyte migration using transwell systems [50]
- Macrophage Polarization Assay: Assessment of the ability to shift naïve macrophages toward a regenerative phenotype through cytokine secretion profiling [50]
Anti-fibrotic MoA Assessment:
- Collagen Degradation Assay: Direct measurement of matrix metalloproteinase (MMP9) activity against natural collagen substrates [50]
- Myofibroblast Deactivation: Co-culture systems evaluating the suppression of alpha-smooth muscle actin expression in activated fibroblasts [50]
This comprehensive testing suite enabled the identification of IL-10+MMP9 as the optimal payload combination for RTX001 and provided robust data to support regulatory submissions [50]. The systematic approach directly measured multiple aspects of the proposed mechanism of action, creating a compelling correlation between product characteristics and biological function.
Visualization of Key Method Development Concepts
Phase-Appropriate Analytical Development Workflow
The following diagram illustrates the interconnected relationship between product development phases and analytical method life cycle activities, highlighting key decision points and regulatory interactions:
MOA-Aligned Potency Testing Strategy
This diagram outlines the logical relationship between mechanism of action, potency, and efficacy, illustrating how analytical measurements connect to biological function and clinical outcomes:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Cell Therapy Analytical Development
| Reagent/Category | Function in Analytical Development | Phase-Appropriate Considerations |
|---|---|---|
| Reference Standards | Qualification/validation of methods, system suitability controls | Early: well-characterized research materials; Late: GMP-grade, fully qualified standards [46] |
| Cell-Based Assay Reagents | Potency and functional assessment (cytokines, target cells, detection antibodies) | Early: research-grade with demonstrated functionality; Late: GMP-grade, qualified critical reagents [1] |
| Flow Cytometry Panels | Identity, purity, characterization, and potency assessment | Early: research-use-only panels; Late: validated antibody panels with demonstrated specificity and reproducibility [47] |
| Molecular Biology Reagents | Vector copy number, transduction efficiency, genetic modification assessment | Early: standard laboratory reagents; Late: qualified kits with defined performance characteristics [47] |
| Cell Culture Media | Maintenance of reference cells, assay performance qualification | Consistent sourcing throughout development; avoid frequent changes to maintain assay comparability [46] |
Successful IND submissions for cell therapies require a carefully balanced approach to analytical development that emphasizes precision in early phases while systematically building toward comprehensive accuracy and validation. The strategic prioritization of method precision for early-phase decision making, combined with ongoing development of MOA-aligned potency assays, creates a foundation for regulatory success while maintaining development efficiency. As noted by Roger Herr, PhD, Director of Analytical Development at Kincell Bio, "Given compressed timelines and budget constraints, many innovators think about analytical investments in a phase-appropriate manner. While we never advise overengineering, phase-appropriate should not mean short-cuts, as insufficient analytical method development will require future assay redesign and method comparability studies" [46].
The most successful analytical programs recognize that phase-appropriate development is not about cutting corners, but rather about making strategic investments in the most critical methods early in development while maintaining flexibility for method refinement as product and process knowledge increases. By implementing MOA-aligned analytical strategies, focusing on precision for early-phase decision making, and following structured validation approaches that evolve with the product lifecycle, developers can create robust analytical programs that support IND success and ultimately bring transformative cell therapies to patients in need.
In the field of cell therapy, potency assays serve as critical quality control measures that quantitatively measure the biological activity of a therapeutic product and its ability to elicit a specific therapeutic effect. For Chimeric Antigen Receptor T-cell (CAR-T) therapies targeting CD19 in B-cell malignancies, interferon-γ (IFN-γ) secretion has emerged as a cornerstone potency measurement that correlates with clinical efficacy [11]. The measurement of IFN-γ provides researchers with a quantifiable metric that reflects the functional activation of CAR-T cells upon engagement with their target antigen, serving as a key indicator in the mechanism of action (MoA) for these living drugs [11].
This case study examines the central role of IFN-γ secretion as a potency measure for CD19-targeted CAR-T therapies, providing a comprehensive comparison of its implementation across different therapeutic contexts and presenting detailed experimental protocols for researchers in the field. Within the broader thesis of cell therapy MoA research, understanding and quantifying IFN-γ secretion enables scientists to bridge the gap between product characterization and clinical performance, supporting the development of more potent and predictable CAR-T products [11].
The Biological Basis: IFN-γ in CAR-T Cell Mechanism of Action
IFN-γ Secretion as a Marker of T-cell Activation
Upon recognition of CD19-positive target cells, CAR-T cells undergo activation through signaling cascades initiated by the CD3ζ domain and co-stimulatory molecules (e.g., CD28 or 4-1BB) in second-generation CARs [51] [52]. This activation triggers a robust transcriptional reprogramming that includes the production and secretion of IFN-γ, a pleiotropic cytokine with potent immunomodulatory effects [11]. The secretion of IFN-γ serves as an integrated measure of successful CAR signaling, reflecting the critical steps of target recognition, activation cascade initiation, and effector function elicitation [11].
The diagram below illustrates the signaling pathway from CD19 recognition to IFN-γ secretion in CAR-T cells:
Correlation Between IFN-γ and Clinical Outcomes
Research has consistently demonstrated that IFN-γ secretion levels in vitro correlate with clinical response in patients receiving CD19-targeted CAR-T therapies [11]. This correlation establishes IFN-γ as a predictive potency marker that can help forecast therapeutic efficacy during product development and quality control. The table below summarizes key evidence supporting this relationship:
Table 1: Evidence Supporting IFN-γ as a Predictive Potency Marker
| Evidence Type | Correlation Finding | Reference/Context |
|---|---|---|
| Clinical Validation | IFN-γ release correlates with expansion and persistence of functional CAR-T cells in patients | [11] |
| Product Characterization | High IFN-γ secreting capacity associated with favorable T-cell differentiation states | [11] |
| Manufacturing Quality | IFN-γ secretion used in lot-release testing for FDA-approved CAR-T products | [11] |
| MoA Research | Integrated measure of successful target recognition and activation cascade | [11] |
Comparative Analysis: IFN-γ Secretion Across CD19-Targeted CAR-T Products
Standardized IFN-γ Potency Assays in Approved Products
For the six FDA-approved CD19-targeted CAR-T cell products, potency assessment primarily relies on measuring IFN-γ release in response to target cells, alongside other product-specific attributes [11]. While all approved products utilize second-generation CAR constructs, they differ in their costimulatory domains—with some employing CD28-based signaling (axicabtagene ciloleucel, brexucabtagene autoleucel) and others using 4-1BB-based signaling (tisagenlecleucel, lisocabtagene maraleucel) [52]. These design differences influence the kinetic profiles and magnitude of IFN-γ secretion, necessitating product-specific potency criteria.
The experimental workflow for standardized IFN-γ potency testing typically follows this path:
Quantitative Comparison of IFN-γ Secretion in CD19 CAR-T Therapies
The table below summarizes quantitative data on IFN-γ secretion and corresponding efficacy measures for different CD19-targeted CAR-T approaches:
Table 2: Comparative IFN-γ Secretion and Efficacy Profiles of CD19-Targeted CAR-T Therapies
| CAR-T Product/Type | Costimulatory Domain | IFN-γ Secretion Profile | Corresponding Efficacy Measures | Reference |
|---|---|---|---|---|
| Axicabtagene ciloleucel | CD28 | Robust early secretion, rapid kinetics | ORR: 83%, CR: 58% (ZUMA-1) | [52] [53] |
| Tisagenlecleucel | 4-1BB | Sustained secretion, prolonged kinetics | ORR: 81%, CR: 60% (ELIANA) | [52] [53] |
| CD19/20 Bi-CAR | 4-1BB | Enhanced magnitude vs single-target | 3-month CR superior to CD19 CAR alone | [54] |
| CD19 CAR (research grade) | CD28/4-1BB | Varies with T-cell differentiation states | Correlates with memory T-cell subsets | [11] |
Impact of CAR-T Product Attributes on IFN-γ Secretion
Research has identified several critical quality attributes (CQAs) that significantly influence IFN-γ secretion capacity in CD19-targeted CAR-T products. These include:
- T-cell differentiation state: Products enriched with stem cell memory (Tscm) and central memory (Tcm) T-cells demonstrate enhanced IFN-γ secretion capacity and persistence compared to those dominated by effector memory (Tem) and terminally differentiated subsets [11].
- CAR integration characteristics: Specific viral vector integration sites (e.g., TET2, CBL genes) can enhance CAR-T cell potency and IFN-γ secretion through effects on expansion and persistence [11].
- TCR repertoire diversity: Products with higher TCR clonotypic diversity generally exhibit more robust IFN-γ responses, while restricted clonality associates with exhaustion signatures and diminished function [11].
Experimental Protocols: Measuring IFN-γ Secretion for Potency Assessment
Standardized ELISA-Based Potency Assay
The enzyme-linked immunosorbent assay (ELISA) provides a quantitative measurement of IFN-γ secretion in CAR-T cell potency assessment [11].
Protocol Summary:
- Co-culture Establishment: Plate CD19-expressing target cells (e.g., NALM-6 or Raji cells) at a predetermined density in multi-well plates
- Effector Cell Addition: Add CAR-T cells at specific effector-to-target (E:T) ratios (typically 1:1 to 10:1)
- Incubation: Culture cells for 18-24 hours under standard conditions (37°C, 5% CO₂)
- Supernatant Collection: Harvest culture supernatants by centrifugation
- IFN-γ Quantification: Process supernatants using validated IFN-γ ELISA kits per manufacturer instructions
- Data Analysis: Calculate potency relative to a reference standard
Key Technical Considerations:
- Include appropriate controls (CAR-T cells alone, target cells alone, untransduced T cells with targets)
- Establish acceptance criteria based on clinical correlation data
- Validate assay precision, accuracy, and linearity for potency determination
ELISpot Assay for Functional Frequency Assessment
The enzyme-linked immunospot (ELISpot) assay measures the frequency of IFN-γ-secreting cells within CAR-T products, providing complementary information to bulk secretion measurements [11].
Protocol Summary:
- Plate Preparation: Coat PVDF membrane plates with anti-IFN-γ capture antibody
- Cell Plating: Seed CAR-T cells and CD19+ target cells at appropriate densities
- Incubation: Culture for 24-48 hours to allow spot development
- Detection: Process plates with detection antibodies and enzyme conjugates per kit protocols
- Spot Quantification: Analyze using automated ELISpot readers
- Frequency Calculation: Express results as spot-forming units (SFU) per input cell number
Advanced Methodologies: Integrating IFN-γ Assessment with Multi-Omics Approaches
Single-Cell Resolution Analysis
Advanced single-cell technologies now enable correlation of IFN-γ secretion with detailed cellular phenotypes. Paired single-cell RNA sequencing and TCR repertoire analysis allows researchers to identify specific T-cell clonotypes with superior IFN-γ secretion capacity and persistence potential [11]. Studies applying this approach have demonstrated that products associated with poor clinical responses exhibit reduced TCR clonotypic diversity and show exhaustion signatures despite potentially maintaining IFN-γ secretion capacity [11].
Epigenomic Correlates of IFN-γ Secretion
DNA methylation profiling of CD19 CAR-T products has identified distinct epigenetic loci associated with complete response, event-free survival, and overall survival post-infusion [11]. These epigenetic signatures correlate with functional capacity including IFN-γ secretion, providing earlier predictive markers of product potency than secretion measurements alone.
Table 3: Research Reagent Solutions for IFN-γ Potency Assays
| Reagent/Resource | Function in Potency Assessment | Implementation Example |
|---|---|---|
| CD19-Expressing Target Cells | Provide antigen-specific stimulation | NALM-6 (B-ALL), Raji (Burkitt lymphoma) cell lines |
| IFN-γ ELISA Kits | Quantify secreted IFN-γ in supernatants | Commercial kits with GMP-grade components for lot release |
| ELISpot Kits | Determine frequency of IFN-γ-secreting cells | Validated kits with automated readout systems |
| Flow Cytometry Panels | Characterize T-cell differentiation states | Antibodies against CD45RA, CCR7, CD62L for memory subsets |
| qPCR/ddPCR Assays | Measure vector copy number and persistence | Droplet digital PCR for precise transgene quantification |
IFN-γ secretion has established itself as an indispensable potency measure for CD19-targeted CAR-T therapies, providing a quantifiable functional output that integrates multiple aspects of product quality and biological activity. As the field advances toward more complex CAR designs—including dual-targeted constructs [54], armored CARs [51] [55], and gene-edited products [56]—IFN-γ potency assessment will continue to evolve, potentially incorporating kinetic measures, multiplexed cytokine profiling, and integration with multi-omics data. For researchers focused on cell therapy MoA, understanding the strengths and limitations of IFN-γ as a potency marker provides a foundation for developing increasingly predictive assays that bridge product characterization with clinical performance, ultimately supporting the development of more effective and reliable CAR-T therapies.
Allogeneic cell therapies represent a paradigm shift in regenerative medicine and oncology, offering the potential for "off-the-shelf" treatments that overcome the logistical and manufacturing limitations of patient-specific (autologous) therapies. However, their development is constrained by two interconnected scientific challenges: ensuring consistent donor qualification and maintaining a reliable mechanism of action (MoA). Donor-to-donor biological variability introduces significant heterogeneity into the starting material, which can directly impact critical quality attributes (CQAs) of the final product and, consequently, its therapeutic MoA [57] [58]. This guide objectively compares the performance of allogeneic products against these critical parameters, providing researchers with a framework for navigating the complex landscape of cell therapy development. The ensuing analysis synthesizes current regulatory perspectives, experimental data, and methodological protocols essential for establishing a robust and consistent product profile.
Comparative Analysis: Donor Variability and Its Impact on MoA
The fundamental distinction between allogeneic and autologous therapies lies in the source of cellular material, which dictates their respective performance profiles concerning scalability, consistency, and risk [58] [59]. The following comparative analysis outlines how these differences directly influence the challenges of donor qualification and MoA consistency.
Table 1: Performance Comparison of Allogeneic vs. Autologous Cell Therapies
| Parameter | Allogeneic Therapy | Autologous Therapy |
|---|---|---|
| Cell Source | Healthy donor(s) [59] | Patient's own cells [59] |
| Scalability & Cost | High scalability via mass production; potential for lower cost per dose [58] | Limited scalability; individualized batches lead to higher costs [58] |
| Donor Qualification Challenge | High: Requires rigorous, standardized screening of donors for genetics, infectious diseases, and cell quality [57] [60] | Not Applicable: No donor screening needed [61] |
| MoA Consistency Challenge | Variable: Subject to donor-to-donor variability impacting product characteristics and potency [57] | High: MoA is patient-specific, but the product is consistent for that individual [58] |
| Key Safety Concern | Graft-versus-host disease (GvHD) and immune rejection [59] [61] | Risk of re-infusing contaminated or malignant cells [61] |
| Therapeutic Advantage | Potential for graft-versus-tumor (GvT) effect in oncology [61] | No risk of immune rejection [58] [59] |
The "allogeneic problem" is multi-faceted. Logistically, global supply chains for starting material are fragile, and regulatory requirements for donor testing—such as the FDA-approved kits required in the U.S. or Japan's mandatory Parvovirus testing—vary significantly between regions, complicating international development [57]. Biologically, genetic diversity among donors is a primary source of variability. This includes differences in Human Leukocyte Antigen (HLA) profiles, which influence immunogenicity, and genetic polymorphisms that can affect cell expansion potential, differentiation capacity, and ultimately, the product's functional MoA [57]. For allogeneic therapies, this variability directly threatens MoA consistency because the biological effect of the therapy, whether it be through immunomodulation, direct tumor killing, or tissue repair, must be reproducible across batches derived from different donors [57].
Quantitative Data: Success Rates and Variability Metrics
Recent clinical data and manufacturing studies provide quantitative evidence of the challenges and progress in allogeneic therapy. While success rates are promising, the underlying variability necessitates rigorous control strategies.
Table 2: Quantitative Data on Allogeneic Therapy Outcomes and Variability
| Metric | Reported Value / Finding | Context & Implication |
|---|---|---|
| Stem Cell Therapy Overall Success Rate | Up to 78% (varies by indication) [62] | Demonstrates the overall potential of cell therapies, but is indication-specific. |
| Hematopoietic Stem Cell Transplant Survival | 79% at 3-year follow-up [62] | A benchmark for allogeneic transplant success in hematologic malignancies. |
| Treatment-Related Mortality (Allogeneic) | Significantly higher than autologous [61] | Driven by GvHD, regimen-related toxicity, and infection. |
| Donor Screening Panels (U.S.) | Comprehensive testing for HIV, HBV, HCV, HTLV, syphilis, CMV, WNV [60] | Highlights the extensive infectious disease screening required for donor qualification. |
| Impact of Donor Age on Outcome | Younger donors consistently lead to better patient outcomes [62] | A key quantitative factor in donor selection, affecting regenerative potential. |
The data underscores that successful outcomes are achievable but are highly dependent on careful patient and donor selection. The higher treatment-related mortality associated with allogeneic transplants, as noted in Table 2, is a direct consequence of the biological challenges, including GvHD and opportunistic infections due to immunosuppression [61]. Furthermore, the success of the therapy is closely tied to the donor's health and age, with stem cells from younger donors demonstrating greater regenerative potential and leading to superior clinical outcomes [62]. This quantitative evidence reinforces the necessity of a science-driven donor qualification strategy.
Experimental Protocols for Donor and MoA Assessment
To address these challenges, researchers employ a suite of standardized experimental protocols designed to qualify starting material and characterize the product's MoA.
Protocol 1: Comprehensive Donor Cell Characterization
This protocol aims to ensure the quality and safety of the cellular starting material.
- Methodology:
- Source Material Collection: Collect donor cells via leukapheresis (for immune cells like T/NK cells) or bone marrow aspiration (for MSCs) [60].
- Infectious Disease Testing: Perform serological and molecular testing per 21 CFR 1271 for relevant agents, including HIV, HBV, HCV, HTLV, syphilis, CMV, and WNV, using FDA-licensed or equivalent kits [57] [60].
- Genetic & HLA Screening: Conduct high-resolution HLA typing to assess compatibility and potential immunogenicity. Consider genetic screening for specific markers (e.g., APOE expression for certain neurological therapies) [57].
- Cell Phenotyping & Viability: Use multiparameter flow cytometry to characterize cell surface markers (e.g., CD45, CD11b for microglial-like cells) and assess viability via dye exclusion assays [57].
- Data Analysis: Establish acceptance criteria for donor eligibility, including minimum cell counts, viability thresholds, and negative results for infectious disease panels. Data should be recorded in a standardized format for traceability.
Protocol 2: Potency Assay Linking to Mechanism of Action
This is a critical experiment for demonstrating batch-to-batch consistency in the product's biological function.
- Methodology:
- Define MoA: Clearly delineate the proposed biological mechanism (e.g., target cell cytotoxicity, immunomodulation via cytokine secretion, engraftment and differentiation) [57] [63].
- Develop Functional Assay:
- For Cytotoxic Therapies (e.g., CAR-NK/CAR-T): Use a co-culture assay with fluorescently labeled target cells. Measure specific lysis via flow cytometry or a platform like xCelligence [63].
- For Immunomodulatory Therapies (e.g., MSCs): Use a mixed lymphocyte reaction (MLR) or an assay measuring inhibition of T-cell proliferation. Quantify relevant cytokine levels (e.g., IFN-γ, IL-10) via ELISA or multiplex assays [64].
- Characterize Critical Quality Attributes (CQAs): Correlate functional potency with physical attributes, such as transgene expression (for CAR products) or specific marker profiles, using flow cytometry [63].
- Data Analysis: The potency assay should be quantitative and have a defined range. Results from multiple donors should be compared to establish the expected range of biological activity and demonstrate consistency. FDA guidance emphasizes the need for adequate potency assurance by Phase 2/3 IND stages [63].
The following diagram illustrates the logical workflow and key decision points in establishing a robust donor qualification and MoA consistency strategy.
The Scientist's Toolkit: Essential Research Reagents & Materials
A successful allogeneic program relies on a suite of specialized reagents and platforms to control for variability and characterize the product.
Table 3: Essential Research Reagents for Allogeneic Development
| Research Reagent / Platform | Function in Experimental Protocol |
|---|---|
| Multiparameter Flow Cytometry | Cell phenotyping, quantification of transgene expression (e.g., CAR), assessment of activation markers, and measurement of target cell cytotoxicity [63]. |
| HLA Typing Kits | High-resolution genetic screening to determine donor-recipient compatibility and assess the diversity of a donor pool [57]. |
| qPCR/dPCR Assays | Quantification of vector copy number (for genetically modified therapies), residual vector, and on-target editing efficiency [63]. |
| GMP-grade Cell Culture Media & Supplements | Critical raw materials for cell expansion; variability can significantly impact cell growth, phenotype, and function, requiring strict qualification [57] [63]. |
| Cytokine Detection Kits (ELISA/MSD) | Quantification of secreted factors to characterize immunomodulatory MoA (e.g., for MSC therapies) or cytokine release syndrome potential [64]. |
| Genome Editing Tools (e.g., CRISPR/Cas9) | Used to engineer universal allogeneic products (e.g., knock-out of TCR to prevent GvHD) [65] [63]. Requires controls for on/off-target analysis. |
| Functional Assay Platforms (e.g., xCelligence) | Real-time, label-free monitoring of cell-mediated cytotoxicity, a key potency assay for allogeneic CAR-T and CAR-NK products [63]. |
Navigating the challenges of donor qualification and MoA consistency is a multidisciplinary endeavor central to the advancement of allogeneic cell therapies. A strategic approach that integrates rigorous, globally-compliant donor screening with the early development of MoA-relevant potency assays is paramount. By leveraging the experimental protocols and tools outlined in this guide, researchers can systematically address the inherent variability of donor-derived starting materials. This scientific rigor is the foundation for developing robust, consistent, and effective "off-the-shelf" therapies that can fulfill their transformative potential for patients. The future of the field will be shaped by advances in machine learning for donor prediction, platform process technologies, and adaptive regulatory strategies that together will enhance control over these critical parameters [57] [65].
Navigating Development Hurdles: Optimizing MoA for Clinical Translation and Manufacturing
The therapeutic effect of cell therapies, particularly Chimeric Antigen Receptor (CAR) T-cell therapies, is driven by a specific Mechanism of Action (MOA): the engineered recognition and elimination of target cells expressing a specific antigen [1]. However, the clinical application of this mechanism is fraught with two major, and often opposing, challenges that can limit both the safety and long-term efficacy of these treatments. On-target, off-tumor toxicity occurs when the CAR T cells attack healthy tissues that express the target antigen, causing serious adverse events [66] [67]. Conversely, antigen escape describes the process where tumor cells evade therapy by downregulating or losing the target antigen, leading to disease relapse [68] [69]. This guide provides a comparative analysis of these challenges, supported by experimental data and methodologies relevant to drug development professionals.
On-Target, Off-Tumor Toxicity
Clinical Problem and Underlying Biology
On-target, off-tumor toxicity (OTOT) is a potentially dose-limiting challenge in the development of CAR T-cell therapies for solid tumors and some hematological malignancies. Its root cause is the shared expression of a target antigen on both malignant and certain healthy tissues. When CAR T cells are infused, they execute their mechanism of action indiscriminately against all antigen-positive cells, resulting in damage to normal organs [66] [67]. Severe OTOT has been observed in clinical trials targeting various antigens, such as claudin 18.2 (CLDN18.2) in gastric cancer, where it caused gastric mucosal damage, hemorrhage, and denudation [70].
Key Experimental Models and Data
Preclinical models are crucial for evaluating OTOT risk. The following table summarizes quantitative data from a study investigating CLDN18.2-directed CAR T cells, which illustrates the consistency of this toxicity across different experimental variables [70].
Table 1: Experimental Data on CLDN18.2 CAR T Cell-Induced On-Target, Off-Tumor Toxicity [70]
| CAR Construct | Tumor Model | Incidence of Weight Loss >20% | Tumor Regression | Key Histopathological Finding |
|---|---|---|---|---|
| Zolbe-CD28z | GSU (gastric cancer) | 100% | Yes | Extensive CD3+ T cell infiltration, loss of gastric glandular epithelium |
| hu8e5-CD28z | GSU (gastric cancer) | 100% | Yes | Extensive CD3+ T cell infiltration, loss of gastric glandular epithelium |
| hu8e5-CD28z (Donor 2) | GSU (gastric cancer) | 0% | Yes | No significant T cell infiltration or gastric damage |
This study demonstrated that OTOT was independent of the CAR binder (scFv), co-stimulatory domain (CD28), or tumor model. The toxicity was directly linked to robust in vivo CAR T cell expansion, as the only donor that did not cause toxicity (Donor 2) also showed no measurable CAR T cell expansion in the peripheral blood [70].
Detailed Experimental Protocol for OTOT Assessment
Objective: To evaluate the potential for on-target, off-tumor toxicity of a CLDN18.2-directed CAR T-cell therapy in an in vivo mouse model [70].
- Animal Model: Use immunodeficient NSG mice. This model is valid because murine and human CLDN18.2 share 100% identity in the first extracellular loop, the epitope recognized by the CAR binders.
- Tumor Engraftment: Inject human gastric cancer cells (e.g., GSU line) subcutaneously.
- Treatment Administration: Once tumors are established, randomly assign mice to groups and administer a single intravenous injection of either:
- Experimental Group: CLDN18.2 CAR T cells (e.g., 3 million cells/mouse).
- Control Group: Untransduced T cells (UTD).
- Toxicity and Efficacy Monitoring:
- Tumor Volume: Measure 2-3 times per week via calipers.
- Body Weight: Record 2-3 times per week as a surrogate for systemic toxicity.
- Blood Collection: Perform serial retro-orbital or submandibular bleeds to quantify circulating CAR T cell levels by flow cytometry.
- Endpoint Analysis (Day 22):
- Necropsy: Collect stomach, lung, and tumor tissues.
- Histopathology: Process tissues for formalin-fixed, paraffin-embedding and sectioning.
- Immunohistochemistry (IHC): Stain stomach sections for:
- Human CD3: To quantify T-cell infiltration into gastric mucosa.
- CLDN18.2: To assess the integrity and loss of antigen-expressing gastric epithelium.
- Data Correlation: Correlate the degree of gastric damage with the levels of circulating CAR T cells and anti-tumor efficacy.
Antigen Escape
Clinical Problem and Underlying Biology
Antigen escape is a leading cause of relapse following initially successful CAR T-cell therapy. It occurs when tumor cells, under the selective pressure of a highly specific immunotherapy, evolve mechanisms to reduce or eliminate the expression of the target antigen. This allows them to evade immune recognition despite the continued presence of functional CAR T cells [68]. This phenomenon has been documented for numerous targets, including CD19 in B-cell acute lymphoblastic leukemia (B-ALL) and BCMA in multiple myeloma [71] [68] [69]. The mechanisms are diverse and include selection of pre-existing antigen-negative clones, acquired mutations, alternative splicing, and impaired antigen presentation [68] [69].
Key Experimental Models and Data
Genomic analyses of relapsed patients provide direct evidence of antigen escape. The table below summarizes data from studies on CD38 and BCMA, highlighting how tumors genetically alter the antigen to evade therapy.
Table 2: Experimental Data on Genomic Antigen Escape in Multiple Myeloma [71] [68]
| Target Antigen | Therapy | Prevalence of Biallelic Loss in Relapse | Genomic Alterations Identified | Functional Consequence |
|---|---|---|---|---|
| CD38 | Anti-CD38 mAbs (Daratumumab) | 6% in R/R MM (0% in untreated) | Deletions, copy-neutral LOH, missense mutations | Disruption of CD38 structure, abrogation of antibody binding |
| BCMA | BCMA CAR T cells (Idecabtagene vicleucel) | Rare (case reports) | Homozygous gene deletion | Complete, irreversible loss of BCMA surface expression |
One study performed whole-genome sequencing (WGS) on 50 patients who relapsed after anti-CD38 antibody therapy. They found that 6% of patients had biallelic disruption of the CD38 gene, a event not observed in 701 newly diagnosed patients, directly linking these genomic events to therapeutic selective pressure [71].
Detailed Experimental Protocol for Investigating Antigen Escape
Objective: To identify genomic mechanisms of antigen escape in multiple myeloma patients relapsing after anti-CD38 monoclonal antibody therapy [71].
- Patient Cohorts:
- Test Cohort: 50 patients with relapsed/refractory multiple myeloma (RRMM) who relapsed after CD38-directed therapy.
- Control Cohorts:
- 701 patients with newly diagnosed MM (NDMM) from the CoMMpass database.
- 72 patients with RRMM who were naïve to anti-CD38 therapy.
- Genomic Sequencing:
- Perform Whole-Genome Sequencing (WGS) at 60-100x coverage on tumor-normal pairs (when available) from all cohorts.
- Perform RNA Sequencing (RNA-seq) on available samples to correlate genomic findings with expression.
- Bioinformatic Analysis:
- Variant Calling: Identify single nucleotide variants (SNVs), insertions/deletions (indels), and structural variants (SVs) affecting the CD38 gene locus.
- Copy Number Analysis: Assess for monoallelic and biallelic deletions or copy-neutral loss of heterozygosity (LOH) at the CD38 locus.
- Clonality Analysis: Determine if the CD38 alterations are clonal or subclonal.
- Functional Validation:
- 3D Protein Modeling: Model identified missense mutations on the CD38 protein structure to predict their impact on antibody (e.g., daratumumab, isatuximab) binding.
- Flow Cytometry: For patients with missense mutations, use engineered cell lines to confirm reduced or altered antibody binding.
- Cytotoxicity Assays: Co-culture patient-derived or engineered tumor cells with anti-CD38 CAR T cells or antibodies to demonstrate reduced killing.
Comparative Analysis of Mitigation Strategies
The research community has developed sophisticated engineering strategies to overcome these dual challenges. The table below compares the primary approaches, which often aim to increase the specificity or breadth of tumor recognition.
Table 3: Strategies to Overcome MoA-Related Clinical Challenges
| Challenge | Strategy | Mechanism | Example & Experimental Support |
|---|---|---|---|
| On-Target, Off-Tumor | Logic-Gated CARs (e.g., AND-gate) | CAR T cell fully activates only upon recognizing TWO tumor-associated antigens, sparing healthy cells expressing only one [70]. | A LINK CAR AND-gate system mitigated gastric toxicity in a mouse model of CLDN18.2 CAR T therapy while preserving anti-tumor efficacy [70]. |
| On-Target, Off-Tumor | Affinity Tuning | Modifying the scFv binding affinity to require high antigen density for activation, as often found on tumor cells. | Preclinical models show that lower-affinity CARs can discriminate between tumors with high antigen density and healthy tissues with low-level expression [67]. |
| Antigen Escape | Multi-Targeting CARs | Engineering T cells to target multiple antigens simultaneously (e.g., tandem CARs, co-infusion). | Targeting both CD19 and CD22 in B-ALL reduces the probability of relapse due to single-antigen loss [68]. |
| Antigen Escape | Pharmacologic Antigen Upregulation | Using drugs to increase the surface density of the target antigen on tumor cells. | γ-Secretase inhibitors increase BCMA density on myeloma cells and improved the efficacy of anti-BCMA CAR T cells in a phase I trial [68]. |
The Scientist's Toolkit: Key Research Reagents and Models
This table details essential materials and models used in the featured experiments for studying these MoA-related challenges.
Table 4: Essential Research Tools for Investigating MoA Challenges
| Reagent / Model | Function / Rationale | Example Use Case |
|---|---|---|
| NSG Mouse Model | Immunodeficient mouse strain that permits engraftment of human tumors and T cells; used for in vivo efficacy and toxicity modeling. | Modeling CLDN18.2 CAR T cell OTOT due to shared epitope between human and mouse CLDN18.2 [70]. |
| CLDN18.2-Expressing Gastric Cancer Cell Lines (GSU, NUGC-4) | In vitro and in vivo tumor models to assess the anti-tumor potency of CLDN18.2-targeted therapies. | Used for initial in vitro cytotoxicity assays and as subcutaneous tumor models in NSG mice [70]. |
| Lentiviral CAR Vectors | Gene delivery system for stable integration of CAR constructs into human T cells. | Used to generate CAR T cells with different scFvs (Zolbe, hu8e5) and co-stimulatory domains for comparative studies [70]. |
| Commercial Anti-CLDN18.2 Antibody (e.g., EPR19202) | reagent for immunohistochemistry (IHC) to confirm tissue-specific protein expression of the target. | Used to validate CLDN18.2 expression patterns in human and murine tissue microarrays [70]. |
| Whole-Genome Sequencing (WGS) | Comprehensive genomic analysis to identify mutations, deletions, and structural variants in antigen genes. | Identified biallelic CD38 disruptions in relapsed multiple myeloma patients [71]. |
| γ-Secretase Inhibitors | Small molecule inhibitors that block BCMA shedding, increasing its surface density on myeloma cells. | Used in combination with BCMA CAR T cells to enhance efficacy by preventing antigen escape via low antigen density [68]. |
In the field of cell therapy, the clarity of a product's mechanism of action (MOA) is the cornerstone of clinical and commercial success. Insufficient development of analytical methods during early research phases creates a ripple effect, leading to severe financial and developmental consequences later in the product lifecycle. This guide examines the tangible costs of these pitfalls and compares the outcomes of robust versus inadequate early analytical development, providing a framework for researchers and drug development professionals to navigate this complex landscape.
The Foundational Link: MOA, Potency, and Efficacy
For cell therapy products (CTPs), the chain of evidence connecting the mechanism of action to clinical efficacy is established through analytical methods. A precise understanding of the MOA—the specific pharmacological process by which the product produces its effect—is necessary to define potency, the product attribute that enables it to achieve that MOA [1]. Potency is measured with a potency test, a critical quality control assay required for regulatory licensure [1].
The relationship between these concepts is logical but fragile: a poorly understood MOA leads to an ill-defined potency attribute, which in turn results in a suboptimal potency test. If the potency test does not adequately reflect the product's biological function, it cannot ensure manufacturing consistency or predict clinical performance. As documented for several approved CTPs, the MOA is often not fully known, making it difficult to correlate potency test results with efficacy endpoints [1]. This foundational weakness undermines the entire development process.
Quantifying the Cost of Poor Development
Underdeveloped analytical methods create significant and measurable financial drains across the development lifecycle. The table below summarizes the primary cost drivers and their impacts.
Table 1: Financial Impacts of Insufficient Early-Phase Analytical Development
| Cost Driver | Impact Phase | Financial Consequence |
|---|---|---|
| Inconsistent Manufacturing [72] | Process Development & Scale-Up | High batch failure rates; inability to demonstrate process comparability for scale-up or site changes. |
| Extended Development Timelines [73] | Clinical to Commercial | Increased R&D spending; delayed market entry and reduced period of patent exclusivity. |
| High Cost of Goods (COG) [74] [75] | Commercial Manufacturing | Labor-intensive, small-batch processes with expensive raw materials exceed product reimbursable value. |
| Regulatory Delays & Uncertainty [72] [1] | Marketing Application | Incomplete potency data can lead to refusal to file or require additional, costly studies. |
| Limited Patient Access [72] | Post-Approval | High product costs and lack of payer reimbursement restrict market adoption and patient reach. |
The downstream effects are substantial. The cell and gene therapy sector has seen an 83% drop in investment from 2021 to 2024, with manufacturing bottlenecks and high costs cited as key deterrents for investors [73]. Furthermore, manufacturing complexities contribute to high Cost of Goods (COG), with media alone estimated to account for over 20% of COG for many therapies [74]. These economic realities make early investment in robust analytics not just a technical necessity, but a strategic financial imperative.
Comparative Analysis: Robust vs. Inadequate Method Development
The choice to invest in comprehensive analytical development during early phases has a dramatic impact on a program's trajectory. The following comparison outlines the outcomes for two divergent paths.
Table 2: Outcomes of Robust vs. Inadequate Early Analytical Development
| Aspect | Robust Early-Phase Development | Insufficient Early-Phase Development |
|---|---|---|
| MOA Understanding | Deeply investigated; MOA drives Critical Quality Attribute (CQA) identification [76]. | MOA is uncertain or poorly defined, leading to misplaced focus [1]. |
| Potency Assay | Based on relevant biological function; predictive of product performance [1]. | Based on convenience or incomplete science; difficult to correlate with clinical outcome [1]. |
| Manufacturing | Consistent, scalable processes with real-time monitoring (e.g., Process Analytical Technology) [72]. | Variable product quality; struggles with scale-up and tech transfer; high failure rates [72]. |
| Regulatory Strategy | Clear, aligned with evolving guidance; facilitates global harmonization [72]. | Complex, unpredictable; requires frequent amendments and additional data submissions [72]. |
| Overall Cost & Viability | Lower long-term COG; sustainable business model with better investment profile [74]. | High COG and recurring failure costs; risk of being commercially non-viable [73] [74]. |
A Framework for Early-Phase Analytical Success
To avoid these pitfalls, developers should adopt a proactive, structured approach from the outset.
Establish a Target Product Profile (TPP) as a Living Document
Initiate a TPP early, treating it as a dynamic roadmap that aligns manufacturing process requirements with product specifications [76]. The TPP should define minimal, target, and ideal specifications for critical elements like dose, volume, and shelf-life, providing a framework for all subsequent development activities [76].
Implement a "Quality by Design" (QbD) Framework
Employ QbD principles and Design of Experiment (DoE) approaches to optimize process parameters systematically [76]. This strategy helps identify the functional relationship between process inputs and product CQAs, building robustness into the process from the start.
Invest in Advanced Analytical Technologies
Leverage tools like Process Analytical Technology (PAT) for real-time monitoring and control of manufacturing steps [72]. As the field matures, AI-driven modeling and automation are becoming key to improving scalability and regulatory confidence [72].
Plan for Comparability
Anticipate process changes and plan for comparability studies early. An emerging ICH Comparability Annex for Advanced Therapy Medicinal Products (ATMPs) could offer new pathways, but developers must generate high-quality data to support any process changes [72].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for developing robust analytical methods for cell therapies.
Table 3: Key Research Reagent Solutions for Cell Therapy Analytics
| Reagent/Material | Primary Function | Application in Analytical Development |
|---|---|---|
| Defined Culture Media [76] [77] | Supports cell growth and function under standardized conditions. | Used in potency bioassays and during manufacturing to ensure consistency and reduce variability. |
| Cytokines (e.g., IL-2, IL-7, IL-15) [77] | Directs cell expansion, differentiation, and alters phenotype. | Critical for functional assays to maintain or modulate cell function ex vivo. |
| Cell Isolation Reagents (MACS/FACS) [77] | Isulates specific cell populations (e.g., T cells) from a heterogeneous mixture. | Ensures purity and consistency of the starting material for both manufacturing and analytical testing. |
| CRISPR/Cas9 Systems [77] | Provides precise genetic modification. | Used in MOA research to validate targets and engineer reporter cell lines for potency assays. |
| Flow Cytometry Antibodies [1] [77] | Labels specific cell surface and intracellular markers. | Enables phenotypic analysis, a key component of cell characterization and identity testing. |
| Cryoprotectants (e.g., DMSO) [77] | Protects cells from damage during freezing and thawing. | Essential for maintaining cell viability and function in stability studies and between testing intervals. |
Visualizing the Analytical Development Workflow
The following diagram illustrates the integrated workflow for developing robust analytical methods, highlighting the critical feedback loops between process steps and the Target Product Profile.
Overcoming the high costs of insufficient analytical development requires a paradigm shift from reactive testing to proactive, science-based development. The path forward demands concerted action across industry, academia, and regulators [72]. This includes embracing risk-based approaches, advancing global regulatory harmonization, and fostering transparency to accelerate collective progress. For researchers and developers, the mandate is clear: invest deeply in understanding the product's MOA and translate that knowledge into robust, controllable processes from the very beginning. The future affordability, accessibility, and success of transformative cell therapies depend on it.
Strategies for Multi-Antigen Targeting to Enhance Efficacy and Prevent Resistance
Chimeric Antigen Receptor (CAR)-T cell therapy has revolutionized cancer treatment, particularly for hematological malignancies. Despite remarkable initial response rates, the long-term efficacy of these therapies is often compromised by the development of therapeutic resistance. A predominant mechanism of this resistance is antigen escape, wherein tumor cells evade immune surveillance by downregulating or losing the target antigen recognized by CAR-T cells [78] [79] [80]. This challenge has catalyzed the development of sophisticated multi-antigen targeting strategies designed to broaden the recognition spectrum of engineered T cells and prevent relapse. This guide objectively compares the performance of these emerging multi-targeting approaches, providing a foundational resource for ongoing cell therapy Mechanism of Action (MoA) research.
Understanding the Challenge: Antigen Escape as a Primary Resistance Mechanism
The success of single-antigen targeted CAR-T cells, particularly those against CD19 in B-cell malignancies, is well-documented. However, multi-center clinical trials reveal that approximately 30-50% of responding patients with B-cell acute lymphoblastic leukemia (B-ALL) eventually relapse [79] [81]. A significant proportion of these relapses—up to 70% in some studies—are characterized by the loss or downregulation of the target antigen, a phenomenon known as antigen escape [82] [80].
Mechanisms of Antigen Escape:
- Genetic Mutations: Acquired mutations or alternative splicing of the gene encoding the target antigen (e.g., CD19) can lead to the expression of truncated isoforms that lack the epitope recognized by the CAR [83] [82].
- Lineage Switch: In rare cases, malignant cells can undergo a phenotypic switch to a different lineage that inherently does not express the target antigen, such as B-ALL transforming to acute myeloid leukemia (AML) [82].
- Trogocytosis: CAR-T cells can extract target antigens from tumor cells and display them on their own surface. This not only reduces the antigen density on the tumor cell, potentially below the activation threshold for CAR-T cells, but can also lead to CAR-T cell fratricide [81].
- Epitope Masking: A single leukemic cell captured during the CAR-T manufacturing process was reported to express the CAR protein on its surface, which bound to and masked its own CD19 antigen, preventing recognition by therapeutic CAR-T cells [82].
The consistent observation of these escape mechanisms across hematological malignancies and solid tumors underscores the critical limitation of monospecific targeting and provides the rationale for multi-antigen approaches.
Comparative Analysis of Multi-Antigen Targeting Platforms
To counter antigen escape, several engineering strategies have been developed. The table below provides a structured comparison of the four principal platforms for multi-antigen targeting.
Table 1: Comparison of Multi-Antigen Targeting CAR-T Cell Platforms
| Platform | Core Design Principle | Key Advantages | Key Limitations | Representative Experimental Outcomes |
|---|---|---|---|---|
| Pooled CAR-T Cells [83] [81] | Co-administration of two separate T-cell products, each expressing a distinct CAR. | Simpler manufacturing of individual vectors; Flexible dosing ratios. | Lower cytokine secretion and cytolysis compared to integrated designs [84]; Risk of immunodominance where one product expands more than the other. | In mixed tumor models, pooled anti-HER2/IL13Rα2 CAR-Ts showed improved tumor control over single-target cells but were less effective than TanCARs [81]. |
| Dual CAR-T Cells [83] [84] | A single T cell transduced with two separate CAR constructs, each targeting a different antigen. | "OR" gate logic; Reduces risk of antigen escape; Dual signaling can enhance persistence. | Potential for tonic signaling from two constructs; Complex manufacturing (bicistronic vector required for purity). | Dual CD19/CD123 CAR-T cells demonstrated efficacy against CD19-negative relapsed B-ALL in preclinical models, preventing antigen escape [83]. |
| Tandem CAR-T Cells (TanCAR) [85] [84] | A single CAR protein with two antigen-binding scFvs linked in tandem, sharing one signaling domain. | Single-vector system; Can bind one or both antigens simultaneously; Superior cytotoxicity in some models [85]. | ScFv arrangement and linker length critically impact function and must be optimized empirically [85]. | TanCAR targeting Mesothelin/MUC16 outperformed monospecific CAR-Ts in heterogeneous ovarian/pancreatic tumor models in vivo, overcoming escape [85]. |
| Logic-Gated CAR-T Cells [83] [81] | Engineering T cells with circuits that require specific antigen combinations (e.g., "AND", "NOT"). | Enhances specificity and safety; Reduces on-target, off-tumor toxicity by requiring multiple antigens for full activation. | Lower potency compared to "OR"-gated cells; Highly complex design and manufacturing. | "AND"-gated CAR-T cells for PSCA/PSMA showed specific lysis only of dual-positive prostate cancer cells, sparing single-positive healthy cells [81]. |
The choice of platform involves a direct trade-off between the simplicity and proven efficacy of "OR"-gated strategies (Pooled, Dual, Tandem CARs) for preventing escape, and the enhanced safety profile of "AND"-gated strategies for reducing on-target, off-tumor toxicity. The optimal choice is heavily influenced by the specific antigen expression profile in the target malignancy.
Experimental Deep Dive: Tandem CAR-T Cells Targeting Mesothelin and MUC16
Detailed Experimental Protocol
A seminal 2025 study developed a tandem CAR (TanCAR1) targeting mesothelin (meso) and MUC16ecto for ovarian and pancreatic cancers [85]. The methodology provides a template for evaluating multi-targeting approaches.
- CAR Construct Design: A series of tandem CARs were created using anti-meso (SS1) and anti-MUC16ecto (4H11) single-chain variable fragments (scFvs). Designs varied in the order of scFvs (SS1-4H11 vs. 4H11-SS1) and the length of the (G4S) linker separating them (1x vs. 3x repeats) [85].
- In Vitro Functional Assays: Transduced T cells were co-cultured with tumor cell lines expressing one or both antigens. Key metrics included:
- Cytokine Production: Measurement of IFN-γ and IL-2 by ELISA to assess T-cell activation.
- Cytolytic Activity: Using real-time cell cytotoxicity assays or chromium-51 release assays to quantify tumor cell killing.
- Proliferation: CFSE dilution assays to measure T-cell expansion upon antigen exposure.
- Advanced Biophysical Analysis: Acoustic Force Microscopy was employed to characterize binding mechanics. This technique revealed that the optimal TanCAR1 bound to one antigen at a time rather than simultaneously engaging both, a crucial insight for understanding its MoA [85].
- Complex Tumor Modeling: Efficacy was evaluated in vitro using mixed tumor models (2D and 3D) containing a heterogeneous population of antigen-positive and negative cells, and in vivo in mouse models with established mixed tumors [85].
Key Data and MoA Insights
The experimental data revealed several critical performance differentiators.
Table 2: Experimental Data for Mesothelin/MUC16 Tandem CAR Constructs
| Construct Name | ScFv Arrangement (distal-proximal) | Linker Length | CAR Expression Level | Activation by Single Antigen | Superior Killing in Mixed Tumors |
|---|---|---|---|---|---|
| TanCAR1 | SS1 - 4H11 | 1x G4S | High | Yes (Meso and MUC16) | Yes [85] |
| Other Configurations | e.g., 4H11 - SS1 | 3x G4S | Variable / Low | Reduced or unbalanced | No |
The TanCAR1 configuration demonstrated antigen-driven killing, effectively eliminating tumor cells based on antigen density and clearing heterogeneous tumors that resisted monospecific CAR-T cells. This was achieved without requiring simultaneous binding to both antigens, a finding that may simplify the design criteria for future TanCARs [85].
The workflow and key findings from this study are summarized in the diagram below.
The Scientist's Toolkit: Essential Reagents and Technologies
Advancing multi-antigen CAR-T therapies requires a specific set of research tools and reagents. The following table details key solutions for their development and evaluation.
Table 3: Essential Research Reagent Solutions for Multi-Targeting CAR-T Development
| Reagent / Technology | Core Function | Application in Multi-Targeting Research |
|---|---|---|
| Phage Display Libraries [80] | Generation of human or murine scFvs for antigen binding. | Source of high-affinity, specific scFv domains for novel tumor antigen targets for Dual or Tandem CARs. |
| Bicistronic/Lentiviral Vectors [84] | Gene delivery vehicle for stable genomic integration. | Essential for co-expressing two independent CARs in Dual CAR-T cells or for delivering single-gene TanCAR constructs. |
| Acoustic Force Microscopy [85] | Single-molecule biophysical analysis of binding forces and kinetics. | Critical for elucidating MoA, e.g., confirming whether a TanCAR binds antigens simultaneously or sequentially. |
| Mixed Tumor Model Systems [85] | In vitro (2D/3D co-culture) and in vivo (mouse) models with heterogeneous antigen expression. | Gold-standard for pre-clinical evaluation of a therapy' s ability to prevent antigen escape. |
| Flow Cytometry Panels | Multiplexed cell surface and intracellular protein analysis. | To validate CAR expression, quantify antigen density on target cells, and profile T-cell differentiation and exhaustion markers (e.g., PD-1, TIM-3). |
The strategic shift from monospecific to multi-antigen targeting represents a pivotal evolution in CAR-T cell therapy MoA research. While first-generation products demonstrated profound proof-of-concept, their vulnerability to antigen escape has been a critical limitation. The platforms detailed herein—Pooled, Dual, Tandem, and Logic-Gated CAR-T cells—each offer distinct paths to overcome this resistance.
Current experimental data, particularly from solid tumor targets like mesothelin and MUC16, strongly suggests that Tandem CARs can provide superior control of heterogeneous tumors compared to monospecific approaches [85]. For hematological malignancies, Dual CARs targeting CD19 and CD123 show promise in preventing relapse after CD19-negative escape [83]. The future of the field lies in the continued refinement of these platforms, the careful selection of optimal antigen combinations, and the development of more sophisticated, tunable systems that can maximize efficacy while maintaining a stringent safety profile. As MoA research progresses, the integration of these multi-targeting strategies is poised to significantly expand the therapeutic window of CAR-T cell therapy for a broader range of cancers.
In the development of cell therapies, the biological mechanism of action (MoA) is intrinsically linked to the manufacturing process. Unlike traditional pharmaceuticals, the product's identity, purity, and biological function are defined by the complex processes used to create it. Consequently, any change in manufacturing—whether to scale up, improve yield, or reduce costs—carries the inherent risk of altering the therapy's critical quality attributes (CQAs) and, ultimately, its clinical safety and efficacy profile [86]. A well-designed comparability protocol is therefore not merely a regulatory requirement but a fundamental scientific exercise to ensure that process changes do not adversely impact the therapeutic MoA.
The field is accelerating rapidly, with the first-ever New Drug Application (NDA) submission for a CAR-T therapy in solid tumors marking a watershed moment in 2025 [87]. As the industry moves beyond boutique production towards industrial-scale manufacturing to meet patient demand, robust strategies for managing process evolution are paramount. This guide compares approaches for executing process changes while safeguarding the therapeutic MoA, providing researchers and developers with a structured framework for comparability assessments.
Comparative Analysis of Key Manufacturing Changes and MoA Impact
Implementing manufacturing changes requires a risk-based assessment of how specific modifications might impact the product's MoA. The table below summarizes common scaling changes, their potential risks to MoA, and recommended mitigation strategies.
Table 1: Impact of Common Manufacturing Changes on Cell Therapy MoA
| Manufacturing Change Category | Illustrative Process Modification | Potential Impact on Critical Quality Attributes (CQAs) & MoA | Recommended Mitigation & Comparability Focus |
|---|---|---|---|
| Cell Culture System | Transition from adherent to suspension culture; Serum-dependent to serum-free media [86] | Altered cell metabolism, differentiation, and activation state; Changes in secretome and surface marker expression impacting potency and homing. | • Side-by-side analytical comparison (release, characterization, stability).• Head-to-head potency assays reflecting MoA.• Non-clinical studies (e.g., animal model dose-response) if analytical gaps exist [86]. |
| Scale-Up/Scale-Out | Increased bioreactor scale; Multi-site production; Adoption of automated, closed systems [88] | Shifts in nutrient/waste gradients affecting cell fitness and phenotype; Process parameter drift impacting product consistency. | • Process characterization studies to define parameter ranges.• Concurrent validation across scales/sites.• Extended process performance qualification (PPQ) to demonstrate robustness. |
| Vector Manufacturing & Transduction | Switch in viral vector system (e.g., LVV producer cell line); Changes in transduction enhancers [86] | Altered vector copy number, transduction efficiency, and genomic integration profile; Risk of insertional mutagenesis; Changes in CAR/TCR expression and persistence. | • Comprehensive vector analytics (titer, identity, purity, potency).• Detailed characterization of transduced cell product (VCN, integration sites).• In-depth functional potency assays. |
| Raw Material Sourcing | Change in critical reagents (e.g., cytokines, activation beads, media components) | Variability in T-cell activation, expansion, and differentiation; Shifts in final product composition (e.g., memory subsets). | • Supplier qualification and rigorous incoming material testing.• Structured risk assessment for material criticality.• Small-scale engineering runs to assess impact before full implementation. |
Experimental Protocols for Demonstrating Comparability
A multifaceted experimental strategy is essential to prove that pre- and post-change products are highly similar and that no adverse impact on MoA or safety has occurred.
Comprehensive Analytical Comparability Workflow
This foundational protocol relies on a battery of in vitro tests to directly compare product attributes.
Table 2: Key Analytical Methods for MoA-Focused Comparability
| Assay Category | Specific Method Examples | Measured Attribute & Relevance to MoA | Research Reagent Solutions |
|---|---|---|---|
| Identity & Purity | Flow cytometry for surface markers (e.g., CD3, CD4, CD8, CD62L, CD45RO); VCN analysis by ddPCR/qPCR | Confirms product composition and genetic modification; Memory subset distribution predicts in vivo persistence [86]. | • Fluorochrome-conjugated antibodies: Cell type identification and phenotyping.• ddPCR/qPCR reagents: Precise, absolute quantification of vector copy number. |
| Potency & Function | Cytokine release assay (IFN-γ, IL-2); Cytotoxicity assay (real-time, impedance-based); Degranulation (CD107a); Serial killing assay | Quantifies target cell killing and T-cell activation/effector functions; Directly correlates with clinical MoA [86]. | • Recombinant target cells: Engineered to express target antigen for functional challenge.• ELISA/MSD kits: Multiplexed quantification of secreted cytokines.• Vital dyes/probes (e.g., CFSE, propidium iodide): Track cell division and death. |
| Characterization & Stability | Telomere length analysis; Metabolomic/proteomic profiling; Assessment of senescence markers; Extended culture stability | Interrogates cellular fitness, metabolic state, and replicative lifespan; Predicts long-term in vivo efficacy. | • Senescence-associated beta-galactosidase kit: Detects aged, non-functional cells.• Metabolomics kits: Profile energy metabolism pathways critical for T-cell function. |
The following workflow outlines the sequential, risk-based decision process for a comprehensive comparability assessment:
In Vivo Biofunctionality and Efficacy Assessment
When analytical studies are insufficient to resolve residual uncertainty regarding MoA, in vivo studies provide a critical line of evidence.
Objective: To compare the in vivo efficacy, persistence, and biodistribution of pre-change and post-change products using a biologically relevant animal model.
Methodology:
- Animal Model: Utilize an immunodeficient mouse model (e.g., NSG) engrafted with human tumor cells expressing the target antigen.
- Study Arms: Include three groups (n=10-12): Pre-change product, Post-change product, and Vehicle control.
- Dosing: Administer a single, equivalent dose of each product intravenously.
- Endpoint Monitoring:
- Tumor Biweekly: Measure tumor volume via calipers to generate growth curves.
- Persistence: Collect peripheral blood periodically for flow cytometric analysis of human T-cell levels.
- Biodistribution: At terminal endpoint, harvest and analyze tumors, spleen, and bone marrow for T-cell infiltration.
- Data Analysis: Compare tumor growth kinetics (e.g., time to progression), overall survival, and T-cell expansion/persistence between the two product groups. Statistical equivalence supports comparability.
Visualizing the MoA and Its Manufacturing Dependencies
Understanding the complete therapeutic mechanism is the first step in protecting it. The diagram below maps a generic CAR-T cell MoA and highlights points where manufacturing process variations can introduce critical deviations.
Successfully navigating process changes requires a proactive, scientifically rigorous strategy centered on the therapy's MoA. As emphasized in regulatory guidance, comparability does not demand identity but rather evidence that any differences have no adverse impact on safety or efficacy [86]. This is best achieved by:
- Early Investment in MoA Understanding: Begin product and process characterization early in development. Invest in developing robust, mechanism-relevant potency assays.
- Risk-Based Protocol Design: The extent of the comparability study should be commensurate with the magnitude of the change, the stage of development, and the level of existing product and process knowledge.
- Holistic Data Integration: Rely on a totality-of-evidence approach, combining analytical, biofunctional, and, when necessary, nonclinical or clinical data.
- Adoption of Advanced Technologies: Leverage novel analytical tools, digital twins for process modeling, and automation to generate high-quality, reproducible data that can de-risk scale-up and tech transfer [89] [88].
By embedding these principles into the product lifecycle, developers can build a robust scientific case for comparability, enabling scalable manufacturing of cell therapies without compromising the biological mechanism that defines their therapeutic promise.
Addressing the 'Potent but Not Efficacious' Paradox in Clinical Trial Design
The "potent but not efficacious" paradox describes a critical challenge in advanced therapy development: a cellular product can demonstrate potent activity in controlled laboratory assays (potency) yet fail to produce the desired therapeutic effect in human patients (efficacy). This disconnect represents a significant hurdle in cell therapy development, often leading to late-stage clinical trial failures despite promising preclinical data. Understanding this paradox requires precise differentiation between fundamental concepts in product characterization. Potency refers to the specific biological activity of a product that enables its intended mechanism of action (MOA), typically measured through in vitro assays. In contrast, efficacy represents the product's ability to elicit the desired clinical effect in patients, measured through clinical endpoints [1] [90].
The regulatory and scientific framework for cell therapies distinguishes these concepts clearly. For the 27 US FDA-approved cell therapy products (CTPs) as of February 2024, the relationship between potency tests and proposed MOAs often remains unclear. For instance, regulatory documentation for several approved products, including Provenge, Gintuit, MACI, and Amtagvi, explicitly states that their MOA is not fully known, while for others like Kymriah, the FDA has noted the difficulty in correlating potency test results with clinical efficacy [1]. This framework highlights the complex interplay between product characterization and clinical performance that forms the core of the potency-efficacy paradox.
Mechanistic Foundations: Disconnect Between MOA and Clinical Outcome
The potency-efficacy paradox frequently originates from fundamental mismatches between a product's demonstrated laboratory activity and the biological requirements for clinical success. Several interrelated factors contribute to this disconnect, spanning from product characterization to patient-specific variables.
Inadequate Mechanism of Action Understanding
Many CTPs receive regulatory approval without complete understanding of their MOA. For example, Kymriah (tisagenlecleucel), the first FDA-approved CAR-T cell therapy, utilizes interferon-γ (IFN-γ) secretion upon CD19 engagement as its potency measure. However, clinical data reveal significant overlap in IFN-γ production between responders and non-responders, indicating this potency readout does not reliably predict clinical outcome [1]. This suggests that the measured potency (IFN-γ secretion) may not fully capture the complex biological processes required for tumor elimination in patients.
Biological Barriers Limiting Clinical Translation
Cell therapies face substantial biological barriers that are not present in controlled laboratory environments. The tumor microenvironment (TME) in solid tumors presents particular challenges, including physical barriers, immunosuppressive factors, and antigenic heterogeneity that can render potent cells ineffective upon administration [91]. Additionally, limited tissue exposure and poor biodistribution may prevent sufficiently potent cells from reaching their target tissue in adequate numbers, despite demonstrating strong activity in vitro. Furthermore, product attributes beyond the measured potency, such as persistence, migratory capacity, and metabolic fitness, significantly influence clinical efficacy but may not be reflected in standard potency assays [1] [91].
Table 1: Factors Contributing to the Potency-Efficacy Disconnect
| Factor Category | Specific Challenge | Impact on Clinical Translation |
|---|---|---|
| MOA Understanding | Incomplete understanding of biological mechanisms | Potency tests measure irrelevant or partial activities |
| Biological Barriers | Hostile tumor microenvironment | Inactivates or suppresses administered cells |
| Product Characterization | Narrow potency assay focus | Fails to capture critical quality attributes needed for in vivo function |
| Patient Factors | Host immune system interactions | Unexpected clearance or modification of administered cells |
Quantitative Evidence: Clinical Data Illustrating the Paradox
Empirical evidence from clinical trials and approved products provides compelling quantitative demonstration of the potency-efficacy disconnect across multiple therapy platforms.
CAR-T Cell Therapy Clinical Evidence
The relationship between potency measurements and clinical outcomes for Kymriah presents a telling example. While the product's potency is defined by IFN-γ secretion upon CD19 engagement, clinical data reveal substantial variability in this measurement across manufacturing lots, with significant overlap between clinical responders and non-responders [1]. This indicates that while the product must demonstrate minimum potency for release, the specific level of IFN-γ secretion does not reliably predict the magnitude of clinical response.
In solid tumors, the challenges are even more pronounced. Despite numerous CAR-T constructs targeting antigens such as MSLN, GPC3, GD2, and HER2 demonstrating potent in vitro cytotoxicity and cytokine secretion, clinical efficacy remains limited [91]. For instance, early clinical trials of MSLN-targeted CAR-T cells in ovarian cancer demonstrated potent in vitro activity but yielded only modest clinical outcomes, with one patient achieving stable disease and another achieving partial response in a phase I study [91]. This disconnect highlights how biological barriers not present in vitro systems fundamentally limit clinical translation.
Statistical Evidence from Clinical Trials
A broader analysis of randomized clinical trials reveals that statistically nonsignificant results often provide substantial evidence for lack of treatment effect. Among 169 statistically nonsignificant primary outcomes from trials published in leading medical journals in 2021, 52.1% yielded a likelihood ratio exceeding 100 for the null hypothesis of no effect versus the alternate hypothesis of clinical efficacy [92]. This statistical evidence underscores the frequency with which potentially "potent" interventions fail to demonstrate clinical efficacy in rigorous trials.
Table 2: Clinical Evidence of Potency-Efficacy Disconnect Across Modalities
| Therapy Platform | Potency Measure | Clinical Efficacy Outcome | Evidence Level |
|---|---|---|---|
| Kymriah (CAR-T) | IFN-γ secretion upon CD19 engagement | Overlap in potency values between responders and non-responders | Clinical trial data [1] |
| MSLN-CAR-T for Ovarian Cancer | In vitro cytotoxicity | 1/3 patients partial response, 1/3 stable disease in phase I | Phase I clinical trial [91] |
| General RCT Outcomes | Preclinical efficacy data | 52.1% of nonsignificant trials showed strong evidence for null hypothesis | Analysis of 169 trial outcomes [92] |
Experimental Approaches: Methodologies for Paradox Resolution
Addressing the potency-efficacy paradox requires sophisticated experimental strategies that bridge the gap between laboratory measurements and clinical outcomes. The following methodologies provide robust approaches for evaluating and resolving these disconnects.
Integrated Workflow for MOA-Potency-Efficacy Relationship Evaluation
Protocol for Establishing MOA-Driven Potency Assays
Objective: Develop potency assays that better predict clinical efficacy by incorporating multiple functional attributes reflective of the complete MOA.
Materials:
- CAR-T Cell Lines: Second-generation (CD28 or 4-1BB costimulatory domains) and fifth-generation (incorporating cytokine receptor signaling) constructs [52] [91]
- Target Cells: CD19-positive tumor cell lines (e.g., NALM-6) and antigen-negative control lines
- Assessment Platforms: Flow cytometry, impedance-based real-time cell analysis, multiplex cytokine arrays, genomic editing tools (CRISPR/Cas9)
Methodology:
- Multi-Parameter Functional Assessment:
- Measure target cell killing using real-time impedance monitoring over 72 hours
- Quantify cytokine secretion (IFN-γ, IL-2, TNF-α) following antigen exposure
- Evaluate serial killing capacity through repeated tumor cell challenges
TME-Mimicking Conditions:
- Incorporate immunosuppressive cytokines (TGF-β, IL-10) in co-culture systems
- Assess function under metabolic stress (nutrient restriction, hypoxia)
- Evaluate migration capacity through endothelial barriers
Correlative Analysis:
- Compare in vitro potency measurements with in vivo efficacy in PDX models
- Establish correlation matrices between multiple potency parameters and tumor reduction
Validation: Confirm assay precision (CV <20%), accuracy (recovery 80-120%), and stability under varied conditions [1].
Research Reagent Solutions: Essential Tools for Paradox Resolution
Table 3: Key Research Reagents for Investigating Potency-Efficacy Relationships
| Reagent Category | Specific Examples | Research Application | Role in Addressing Paradox |
|---|---|---|---|
| CAR Constructs | Second-generation (CD28/4-1BB), Fifth-generation (IL-2Rβ) [52] [91] | Comparing costimulatory domain impact on persistence and efficacy | Identifies engineering approaches that enhance in vivo function |
| Target Antigen Panels | MSLN, GPC3, GD2, HER2, CEA, CLDN18.2 [91] | Solid tumor target validation | Determines antigen selection influence on therapeutic window |
| TME-Mimicking Systems | Immunosuppressive cytokine cocktails, Hypoxia chambers, 3D tumor spheroids | Simulating physiological barriers | Tests potency under clinically relevant conditions |
| Analytical Tools | Multiplex cytokine arrays, SCRB-seq, high-content imaging | Comprehensive product characterization | Identifies critical quality attributes beyond standard potency |
Strategic Implications for Clinical Trial Design
Resolving the potency-efficacy paradox requires fundamental shifts in clinical trial design and product characterization strategies. The conventional linear development pathway must evolve to incorporate parallel assessment of multiple potency parameters and their correlation with clinical biomarkers.
Biomarker-Driven Potency Assessment
Incorporating biomarker assessments throughout clinical development enables direct correlation between potency measurements and biological activity in patients. This includes:
- Pharmacodynamic biomarkers that demonstrate target engagement and modulation
- Product tracking biomarkers that quantify persistence, expansion, and tissue distribution
- TME modulation biomarkers that assess changes in the pathological environment
These biomarkers create feedback loops that refine potency assays to better predict clinical effects, addressing the critical disconnect between laboratory measurements and patient outcomes [1] [93].
Adaptive Potency Assay Development
Developing potency assays with built-in adaptability allows for incorporation of new insights regarding MOA throughout clinical development. This includes:
- Multi-attribute potency panels that capture various aspects of biological activity
- Platform assays that can be modified as understanding of the MOA evolves
- Correlative analysis that continuously evaluates relationships between potency parameters and clinical outcomes
This adaptive approach acknowledges that initial potency assays may not fully capture the complex attributes required for clinical efficacy and allows for method refinement based on emerging clinical data [1] [90].
The "potent but not efficacious" paradox represents a fundamental challenge in advanced therapy development that requires multidisciplinary approaches for resolution. By embracing more sophisticated potency assessment strategies that incorporate multiple functional attributes, environmental challenges, and continuous correlation with clinical outcomes, the field can gradually bridge the gap between laboratory measurements and patient benefits. The evolving regulatory landscape for cell therapies reflects this complexity, with approved products often advancing despite incomplete understanding of their MOA. However, enhanced approaches to potency assessment will ultimately improve clinical success rates by ensuring that products demonstrating laboratory potency also possess the necessary attributes to achieve clinical efficacy in the complex physiological environment of human patients.
For researchers and drug development professionals in cell and gene therapy (CGT), the intricate link between a product's Mechanism of Action (MoA) and its Chemistry, Manufacturing, and Controls (CMC) strategy is a critical determinant of clinical and commercial success. A deep, scientifically-grounded understanding of MoA is no longer a mere academic exercise; it is a fundamental prerequisite for designing robust, phase-appropriate CMC strategies that can navigate the entire drug development lifecycle. In an era of selective funding, capital allocation is increasingly flowing toward programs that integrate MoA-driven CMC principles from the outset, de-risking development and enhancing long-term viability. This guide examines the current funding landscape and provides a comparative analysis of how different strategic approaches to CMC, grounded in MoA understanding, impact program success.
The 2025 Funding Landscape for Cell and Gene Therapy
The biopharma funding environment in 2025 is characterized by a selective rebound, with capital discipline being the overarching theme. After a prolonged downturn, venture funding showed signs of stabilization in Q3 2025, but this recovery is highly concentrated [94].
Table 1: Q3 2025 Biopharma Funding Snapshot
| Metric | Q3 2025 Data | Quarter-over-Quarter Change | Context & Implications |
|---|---|---|---|
| Global Venture Funding | $5.8-6.0B [94] | ~22% increase [94] | Indicates a thaw, but capital is consolidating into fewer companies. |
| Number of Financing Rounds | ~86 rounds [94] | Down from ~96 in Q2 [94] | Confirms the trend of selective, larger checks for de-risked programs. |
| Notable Therapeutic Focus Areas | CNS, Metabolic Diseases (e.g., GLP-1), Autoimmunity [94] | Gaining share relative to oncology [94] | Reflects market demand and scientific progress in larger patient populations. |
| Key Investor Types | Traditional VC, Corporate Venture (Pharma), Family Offices/Sovereigns [94] | Corporate venture has been a consistent source [94] | Strategic pharma investors are scouting for platforms that align with their core franchises. |
Despite this cautious optimism, the CGT sector faces specific headwinds. A risk-averse funding environment and regulatory uncertainty have led to significant underutilization of CDMO capacity, as developers prioritize pipeline hygiene and focus on fewer clinical programs [95]. Furthermore, transitioning from clinical to commercial scale presents substantial challenges, including reimbursement hurdles, infrastructure limitations, and geographic access disparities ("CGT deserts") that can impede patient access [96].
MoA Research: Core Methodologies and Experimental Protocols
Elucidating a compound's Mechanism of Action is a multi-faceted endeavor that involves understanding the biological interaction through which a molecule produces its pharmacological effect [97]. A systems-level view is crucial, moving beyond simple target identification to comprehend the subsequent effects on signaling pathways, networks, and ultimate cellular response [97]. Different data modalities and computational methods are employed to build this understanding.
Diagram: Integrated Workflow for MoA Elucidation
Detailed Experimental Protocols for MoA Analysis
Transcriptomic Profiling for Pathway Analysis: This protocol uses gene expression data to infer pathway modulation.
- Method: Treat relevant cell lines with the therapeutic compound versus a vehicle control. After a predetermined incubation period, extract total RNA and perform RNA sequencing (RNA-Seq).
- Analysis: Identify differentially expressed genes (DEGs) using a bioinformatics pipeline (e.g., DESeq2). Submit the DEG list to pathway enrichment analysis tools like Gene Set Enrichment Analysis (GSEA) or DAVID to identify statistically overrepresented signaling pathways (e.g., PI3K/AKT, MAPK) [97]. This links molecular changes to broader biological processes.
Cell-Based Potency Assay Development: This functional assay is critical for CMC and directly reflects the product's biological MoA.
- Method: Depending on the proposed MoA, this may involve a cell line engineered with a reporter gene (e.g., luciferase) under the control of a pathway activated by the therapy. Alternatively, it may measure a direct downstream effect, such as target cell apoptosis (for a cytotoxic therapy) or secretion of a specific cytokine (for an immunomodulatory therapy) [98] [99].
- Analysis: The assay result (e.g., luminescence, percentage of apoptotic cells) is plotted against the product concentration to generate a dose-response curve. The relative potency is calculated by comparing the sample's curve to a reference standard [98]. This assay is a cornerstone of the CMC control strategy, ensuring batch-to-batch consistency based on biological function.
Computational Target Prediction via Connectivity Mapping:
- Method: Upload the gene expression signature (the list of up- and down-regulated genes) from the transcriptomic profiling experiment to a connectivity mapping platform such as the CLUE platform from the Broad Institute.
- Analysis: The algorithm compares your signature to a vast database of signatures from known compounds. A high negative connectivity score suggests your compound induces an opposite effect to a reference drug, potentially revealing a shared or related target or pathway, thus generating testable MoA hypotheses [97].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for MoA and CMC Research
| Research Reagent / Tool | Primary Function in MoA/CMC Research |
|---|---|
| Engineered Reporter Cell Lines | Enable functional, mechanism-based potency assays by producing a quantifiable signal (e.g., luminescence) upon target engagement or pathway activation [98]. |
| Validated Antibody Panels | Used for critical quality attribute (CQA) analysis, including purity/impurity profiling (e.g., residual host cell protein) and characterization of product variants (e.g., oxidation, aggregation) via techniques like ELISA and Western Blot [98]. |
| Reference Standard | A well-characterized sample of the therapeutic product used as a benchmark in assays for potency, purity, and identity, ensuring consistency and enabling comparability assessments throughout development [99]. |
| High-Fidelity DNA Vectors | Serve as the starting genetic material for many therapies. Cell-free DNA manufacturing platforms can supply high-quality, complex DNA faster than traditional plasmid-based workflows, accelerating process development [95]. |
| Multi-Omics Analysis Software | Computational tools that integrate transcriptomic, proteomic, and metabolomic data to build a systems-level model of a compound's biological effects, moving beyond single-target identification [97]. |
Comparative Analysis of CMC Strategies: MoA-Driven vs. Conventional
A CMC strategy encompasses the definition of the drug substance, establishment of manufacturing methods, and the roadmap for controlling quality and stability from early development through commercial production [98]. The depth of MoA understanding profoundly influences the effectiveness of this strategy. The following diagram and table contrast two strategic approaches.
Diagram: CMC Strategy Workflow Comparison
Table 3: Strategic Comparison of CMC Approaches
| Aspect | MoA-Driven CMC Strategy | Conventional CMC Strategy |
|---|---|---|
| Basis for CQAs | CQAs are identified through a science-driven process rooted in the product's MoA and proactive risk assessment [99]. | CQAs are often based primarily on product composition and physicochemical properties, with less initial linkage to biological function. |
| Potency Assay Design | A matrix of candidate potency assays reflecting the biological MoA is developed early. The final validated assay is a direct measure of the product's biological function [99]. | Often relies on surrogate or non-mechanistic assays (e.g., viability, titer) that may not fully capture the biological activity, posing a risk during late-stage development. |
| Approach to Manufacturing Changes | Plans proactively for process changes by investing in process understanding and analytical methods. Uses prospective comparability protocols with pre-defined acceptance criteria [99]. | Often reactive, leading to resource-intensive, retrospective comparability studies that can jeopardize clinical timelines when changes are required [99]. |
| Resilience to Funding Shifts | More resilient. A robust, science-backed CMC narrative provides a compelling de-risking story for investors, aligning with the demand for "de-risked everything" [94]. | More vulnerable. Lack of a deep product and process understanding can make programs appear riskier in a selective funding environment. |
| Regulatory Engagement | Facilitates more strategic and confident interactions with regulators, as sponsors can present a coherent, data-driven narrative linking product quality to safety and efficacy [99]. | Can lead to challenging regulatory interactions, particularly if comparability arguments are weak or potency assays are not fit-for-purpose, requiring major remediation. |
The convergence of a selective funding market and the inherent complexity of cell and gene therapies demands a paradigm shift in CMC strategy. The evidence clearly demonstrates that an MoA-driven approach is not a luxury but a necessity for long-term success. This strategy enables the development of robust, phase-appropriate control strategies, de-risks manufacturing changes through proactive comparability planning, and creates a compelling value proposition for increasingly disciplined investors. For research and drug development professionals, integrating deep MoA understanding into every facet of CMC is the most critical investment that can be made—one that builds a foundation for sustainable development, regulatory success, and ultimately, the delivery of transformative therapies to patients.
Proving Biological Action: MoA Validation, Regulatory Frameworks, and Cross-Modality Analysis
Potency assurance represents a fundamental paradigm in the development of cellular and gene therapy (CGT) products, serving as the critical bridge between a product's proposed mechanism of action (MoA) and its demonstrated biological activity. According to the U.S. Food and Drug Administration's (FDA) 2023 draft guidance, "Potency Assurance for Cellular and Gene Therapy Products," potency is defined as the "specific ability or capacity of the product, as indicated by appropriate laboratory tests or by adequately controlled clinical data obtained through the administration of the product in the manner intended, to effect a given result" [100] [101]. For researchers and drug development professionals, this guidance emphasizes a fundamental shift from viewing potency as merely a release test to implementing a comprehensive, science- and risk-based strategy that ensures every product lot possesses the intended biological activity throughout its lifecycle [100].
The FDA's updated guidance, which replaces the 2011 document, positions potency assurance within the context of overall pharmaceutical quality systems articulated in ICH Q8-Q13 guidelines [101]. This holistic approach integrates manufacturing process design, process controls, material controls, in-process testing, and potency release assays to create a multi-faceted strategy for mitigating risks to product potency [100]. For MoA research, this means that the biological assays developed must not only measure quantitative activity but must also be strategically linked to the therapeutic effect proposed in the product's mechanism of action.
Evolution of FDA Potency Expectations: From Testing to Assurance
The regulatory landscape for potency testing has evolved significantly from the 2011 guidance to the 2023 draft, reflecting the increasing complexity of CGT products and the need for more sophisticated approaches to quality assurance. The table below summarizes the key distinctions between these regulatory frameworks.
Table 1: Evolution of FDA Potency Guidance for CGT Products
| Aspect | 2011 Guidance | 2023 Draft Guidance |
|---|---|---|
| Core Focus | Potency testing as a lot release requirement [101] | Comprehensive potency assurance strategy [100] [101] |
| Strategic Approach | Focused primarily on the potency assay itself [101] | Holistic approach incorporating ICH Q8-Q13 principles [101] |
| Scope | Technical aspects of potency assay development [101] | Includes raw material control, process parameters, and in-process testing [101] |
| Assay Redundancy | Supported matrix approach with multiple assays [101] | Advises avoiding assay redundancy while maintaining matrix approach [101] |
| Animal Testing | No explicit discouragement of animal-based assays | Clear recommendation to avoid animal-based assays due to variability [101] |
This evolution reflects the FDA's recognition that assuring potency requires more than end-product testing; it necessitates building quality into the entire manufacturing process through critical process parameters (CPPs) and critical quality attributes (CQAs) [101]. The guidance emphasizes that manufacturing process controls are particularly imperative for alternative release strategies for short-shelf-life products, where potency release data may not be available when the product is administered to patients [101].
Framework for Potency Assurance Strategy
Core Components of a Comprehensive Strategy
The FDA's recommended potency assurance strategy consists of multiple interconnected elements, each contributing to the overall goal of ensuring consistent biological activity across all product lots. The diagram below illustrates the relationship between these core components and their collective contribution to potency assurance.
The potency assurance strategy requires a systematic approach to identifying and controlling factors that impact the product's biological activity. Critical raw material control is particularly important for autologous cell therapies, where the starting material variability must be thoroughly characterized [101]. Similarly, the guidance emphasizes assessment of contact materials, including container closure systems, which can potentially affect potency through interactions with the product [101].
For MoA substantiation, the strategy must demonstrate how critical quality attributes (CQAs) relate to the biological activity responsible for the therapeutic effect. This requires thorough process understanding and identification of critical process parameters (CPPs) that significantly impact these CQAs [101]. Effective manufacturing process controls thus become essential for reducing risks to product potency, particularly for products with complex mechanisms of action involving multiple biological functions.
Bioassay Development and Validation
The FDA guidance mandates that there must be at least one biological assay (bioassay) that measures the specific biological activity of the product [101]. While the bioassay does not necessarily need to fully recapitulate the complete MoA, it should clearly mitigate risk to product potency by measuring a key biological function linked to the therapeutic effect.
Table 2: Bioassay Development Requirements for MoA Substantiation
| Requirement | Description | Considerations for MoA Research |
|---|---|---|
| Risk Assessment | Identify risks to assay performance in terms of design, reagents, and parameters [101] | Focus on biological functions most critical to therapeutic efficacy |
| MoA Linkage | Assay should mitigate risk to product potency; direct MoA reflection not always required [101] | Select surrogate endpoints that correlate with clinical activity when direct measurement isn't feasible |
| ICH Q5 Principles | Follow general principles for assay attributes including specificity, accuracy, and precision [101] | Implement phase-appropriate validation with increasing rigor throughout development |
| Animal Testing | Avoid animal-based assays where possible due to variability and 3R principles [101] | Develop human cell-based systems or in vitro models that better predict human response |
| Reference Materials | Appropriate qualification of reference standards and control materials [101] | Establish well-characterized biological reference standards tied to clinical batches |
The guidance specifically advises against assay redundancy, potentially conflicting with the previously recommended matrix approach to potency testing [101]. However, the guidance maintains support for using different release assays that address various potency-related CQAs, suggesting a focused approach where one key mechanistic assay serves as the primary potency measure, supplemented by additional assays as needed [101].
For complex cell therapies with multiple mechanisms of action, such as mesenchymal stem cells (MSCs) that exert therapeutic effects through immunomodulation, trophic factor secretion, and potentially differentiation, the potency assay strategy must adequately represent the primary MoA for the intended indication [29]. MSCs demonstrate their therapeutic effects through release of bioactive molecules, including growth factors, cytokines, and extracellular vesicles, which play crucial roles in modulating the local cellular environment, promoting tissue repair, angiogenesis, and cell survival, and exerting anti-inflammatory effects [29].
Experimental Approaches for MoA-Driven Potency Assay Development
Establishing Correlation Between Bioassay and Therapeutic Effect
Substantiating the link between a potency assay and the clinical MoA requires systematic experimental approaches. The FDA guidance acknowledges that while a fully quantitative correlation to clinical efficacy is ideal, it may not always be achievable [101]. The following workflow outlines a robust methodology for establishing this critical relationship.
The experimental protocol for developing MoA-substantiated potency assays involves multiple validation stages:
MoA Identification Phase: Conduct comprehensive in vitro and in vivo studies to identify the key biological functions responsible for the therapeutic effect. For MSC-based therapies, this would include experiments to characterize their immunomodulatory properties through interactions with various immune cells (T cells, B cells, dendritic cells, and macrophages) and measurement of secreted bioactive molecules [29].
Assay Development Phase: Create robust cell-based systems that quantitatively measure the identified biological functions. Implement design of experiments (DoE) approaches to identify critical assay parameters and optimize performance characteristics. For gene therapies, this may involve developing assays that measure transduction efficiency, transgene expression, and functional activity of the expressed protein.
Correlation Establishment Phase: Utilize materials from nonclinical studies and early-phase clinical trials to establish a relationship between assay results and biological activity. Employ statistical methods such as linear regression and multivariate analysis to quantify correlations. For products with clinical efficacy data, establish the quantitative relationship between potency measurements and clinical outcomes.
Lifecycle Management Phase: Continuously monitor assay performance and correlation to therapeutic effect as manufacturing processes evolve. Implement comparability protocols for assay changes and maintain comprehensive documentation of all changes and their impact on potency measurements.
Research Reagent Solutions for Potency Assay Development
The development of robust, MoA-substantiated potency assays requires specialized reagents and materials designed to specifically measure the biological functions relevant to the therapeutic effect. The table below outlines essential research tools for this purpose.
Table 3: Essential Research Reagents for Potency Assay Development
| Reagent Category | Specific Examples | Function in Potency Assessment |
|---|---|---|
| Cell-Based Systems | Reporter cell lines, Primary human cells, Co-culture models | Measure biological response to product activity in physiologically relevant systems |
| Characterization Antibodies | Flow cytometry panels, ELISA kits, Immunocytochemistry reagents | Quantify specific cell markers, secreted factors, or transgene expression |
| Reference Materials | Qualified reference standards, Biological controls, Calibrators | Provide benchmarks for assay performance and product comparability |
| Cytokines & Growth Factors | Recombinant proteins, Pathway-specific agonists/antagonists | Modulate specific pathways to demonstrate mechanism-specific activity |
| Molecular Biology Tools | qPCR probes, RNA-seq kits, CRISPR-based screening tools | Assess genomic and transcriptomic responses to product exposure |
These research reagents enable the development of potency assays that measure specific aspects of a product's biological activity. For example, in the development of CAR-T cell therapies, potency assays may utilize target cancer cell lines with defined antigen expression to measure cytotoxic activity, combined with cytokine secretion profiling to characterize the potency of different product batches [64]. Similarly, for induced pluripotent stem cell (iPSC)-derived therapies, potency assays may focus on markers of terminal differentiation and functional characterization of the differentiated cells [102].
Regulatory Considerations for MoA Substantiation
Integration with Expedited Development Programs
The draft guidance "Expedited Programs for Regenerative Medicine Therapies for Serious Conditions" emphasizes that regenerative medicine therapies with expedited clinical development may "face unique challenges in expediting product development activities to align with faster clinical timelines" [103]. This creates particular pressure on potency assay development, as sponsors must pursue a "more rapid CMC development program to accommodate the faster pace of the clinical program" [103].
For products with RMAT (Regenerative Medicine Advanced Therapy) designation, the FDA encourages flexibility in clinical trial design while maintaining rigorous standards for product quality [103]. This includes innovative trial designs that may compare several different investigational agents to each other and a common control, or the use of natural history data as historical controls when populations are adequately matched [103]. However, the guidance specifically notes that an RMAT designation does not change the chemistry, manufacturing, and controls (CMC) information required to assure product quality [103].
Lifecycle Management and Post-Approval Considerations
The recently released draft guidance "Postapproval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products" emphasizes that "given the potential for long-lasting effects of CGT products, and the generally limited number of participants treated in clinical trials conducted to support approval of CGT products, postapproval monitoring is important for gathering data on product safety and effectiveness over time" [104]. This has implications for potency assurance, as post-approval data may reveal new insights into the relationship between potency measurements and clinical outcomes.
The FDA recommends that monitoring plans for clinical trials include both short-term and long-term safety assessments, and encourages the use of digital health technologies to collect safety information [103]. For potency assurance, this means establishing systems to correlate potency measurements with long-term clinical outcomes, potentially leading to refinements in potency assays based on real-world evidence.
When manufacturing changes occur post-approval, the FDA recommends that sponsors conduct a risk assessment to determine whether the changes impact product quality [103]. If manufacturing changes are made after receiving the RMAT designation, the post-change product may no longer qualify for the designation if comparability cannot be established with the pre-change product [103]. This underscores the importance of developing robust potency assays early in development that can adequately demonstrate comparability after manufacturing changes.
The FDA's modernized approach to potency assurance represents a significant evolution from traditional quality control testing toward an integrated strategy that connects mechanism of action to measurable product quality attributes. For researchers and drug development professionals, successful implementation requires:
- Early investment in understanding the biological basis of the product's therapeutic effect and identification of quantifiable functions related to the MoA.
- Development of a comprehensive potency assurance strategy that encompasses controls across the entire manufacturing process, not just final product testing.
- Creation of biologically relevant potency assays that specifically measure functions linked to the therapeutic mechanism, with appropriate scientific justification for the selected approach.
- Implementation of phase-appropriate assay validation that evolves throughout product development, incorporating knowledge from nonclinical and clinical studies.
- Planning for lifecycle management of potency assays, including strategies for managing manufacturing changes and incorporating post-approval learning.
By adopting this strategic approach to potency assurance, sponsors can not only meet regulatory expectations but also build a deeper understanding of their product's biology, ultimately leading to more consistent and effective therapies for patients. The FDA encourages early engagement with the Office of Therapeutic Products (OTP) staff to discuss potency assurance strategies, particularly for innovative therapies with complex mechanisms of action [103].
The development of cell therapy products (CTPs) represents a paradigm shift in treating a range of diseases, particularly cancer. As of February 2024, the U.S. Food and Drug Administration (FDA) has approved 27 cellular and gene therapy products [1]. However, a significant challenge persists across this therapeutic class: defining the precise mechanism of action (MoA) for many of these complex biological products. For regulators, clinicians, and developers, understanding how these therapies produce their clinical effects is crucial for validating potency assays, optimizing clinical applications, and guiding future development.
This guide provides an objective comparison of the current landscape of FDA-approved CTPs, with a focused analysis on the known and proposed mechanisms by which they achieve therapeutic benefit. We synthesize available public data from regulatory documents to highlight the relationship between MoA, potency, and clinical efficacy, providing researchers with a framework for interpreting real-world evidence in this rapidly evolving field.
Comprehensive Landscape of Approved Cell Therapies
The 27 FDA-approved CTPs encompass a diverse range of technological approaches, including chimeric antigen receptor (CAR) T-cells, viral vector-mediated gene therapies, and various engineered cellular products [105] [1]. The table below categorizes a representative subset of these therapies by their technological platform, primary indication, and MoA status.
Table 1: Classification and MoA Status of Select FDA-Approved Cell Therapies
| Product Name | Technology Platform | Indication | Reported MoA Status |
|---|---|---|---|
| Kymriah (tisagenlecleucel) [1] | CAR T-cell | B-cell leukemia | Proposed |
| Yescarta (axicabtagene ciloleucel) [105] | CAR T-cell | Lymphoma | Proposed |
| Provenge (sipuleucel-T) [1] | Autologous cellular immunotherapy | Prostate cancer | Not known |
| Gintuit [1] | Allogeneic cultured keratinocytes and fibroblasts | Mucogingival conditions | Not known |
| MACI [1] | Autologous cultured chondrocytes | Knee cartilage defects | Not known |
| Lantidra (donislecel) [1] | Allogeneic pancreatic islet cells | Type 1 diabetes | Proposed |
| Rethymic [1] | Allogeneic processed thymus tissue | Congenital athymia | Proposed |
| Stratagraft [1] | Allogeneic cultured keratinocytes and dermal fibroblasts | Thermal burns | Activity described |
The regulatory documentation for these products frequently reveals uncertainty in the definitive establishment of MoA. For several products, including Provenge, Gintuit, and MACI, the MoA is explicitly stated as "not known" [1]. For others, such as Kymriah, Lantidra, and Rethymic, the language used is more tentative, employing terms like "proposed" or "believed" when discussing the MoA, indicating the presence of hypotheses that are not yet fully validated [1].
Analyzing Mechanism of Action: From Concept to Clinical Correlation
Defining the Framework: MoA, Potency, and Efficacy
A critical step in analyzing CTPs is to clearly distinguish between interrelated but distinct concepts: Mechanism of Action (MoA), potency, and efficacy. The following diagram illustrates the logical relationship between these key elements as adapted from regulatory and metrological perspectives [1].
As illustrated, potency is a laboratory-measured attribute, while efficacy is a clinical outcome [1]. They are connected through the MoA. A common mistake is to assume a potency test directly measures efficacy; however, it is intended to assure the product's ability to function via its MoA. This separation explains why a product can be "potent" in a lab assay but not "efficacious" in patients, or vice versa, if the measured attribute does not fully capture the biological mechanism responsible for the clinical benefit.
MoA Analysis in CAR T-Cell Therapies: A Case Study
CAR T-cell therapies, such as Kymriah (tisagenlecleucel), exemplify a class where the MoA is more clearly proposed. The intended MoA is the elimination of target cells expressing a specific antigen (e.g., CD19 on B-cells) [1]. The potency of Kymriah is defined by its ability to secrete interferon-γ (IFN-γ) following exposure to CD19-positive target cells [1]. This workflow can be mapped as follows:
Table 2: MoA and Potency Analysis Framework for Kymriah
| Concept | Definition for Kymriah |
|---|---|
| Mechanism of Action (MoA) | Elimination of CD19+ target cells [1] |
| Potency Attribute | Ability to secrete IFN-γ upon target recognition [1] |
| Potency Test | In vitro co-culture assay measuring IFN-γ secretion [1] |
| Efficacy | Clinical remission in patients [1] |
| Efficacy Endpoint | Objective response rates (e.g., complete remission) [1] |
| Efficacy Endpoint Test | Clinical assessments (e.g., imaging, lab tests) [1] |
However, public data reveals the complexity of correlating this potency test with clinical outcome. While data showed a correlation between IFN-γ production and remission, there was significant overlap between responders and non-responders, and IFN-γ production varied greatly from lot-to-lot [1]. The FDA briefing document noted it was "difficult to correlate IFN-γ production in vitro with tisagenlecleucel safety or efficacy," highlighting the challenge even for a product with a relatively well-understood MoA [1].
Experimental Protocols for MoA and Potency Assessment
Protocol: CAR T-Cell Potency Assay (IFN-γ Release)
This protocol is representative of the bioassays used to measure CAR T-cell potency, based on the publicly described method for Kymriah [1].
1. Principle: This assay evaluates the functionality of CAR T-cells by measuring their antigen-specific activation through the quantification of IFN-γ secretion upon co-culture with target cells expressing the cognate antigen.
2. Key Research Reagent Solutions:
Table 3: Essential Reagents for CAR T-Cell Potency Assay
| Reagent / Solution | Function | Critical Specifications |
|---|---|---|
| CAR T-Cell Product | Test article | Final formulated product, viability >70% |
| CD19+ Target Cells | Antigen-presenting cells | Stably express target antigen (e.g., NALM-6 cell line) |
| CD19- Control Cells | Specificity control | Isogenic cell line lacking CD19 |
| Cell Culture Medium | Support cell viability | Serum-free, cytokine-free medium |
| IFN-γ ELISA Kit | Quantify cytokine | Validated for human IFN-γ, high sensitivity |
| Flow Cytometry Reagents | Cell phenotyping | Antibodies for CD3, CAR detection, viability dye |
3. Procedure:
- Step 1: Co-culture Setup. Seed target cells (CD19+) and control cells (CD19-) in a multi-well plate. Add a standardized number of CAR T-cells to achieve a pre-determined Effector:Target (E:T) ratio (e.g., 1:1). Include wells for target cells alone and CAR T-cells alone as additional controls.
- Step 2: Incubation. Incubate the co-culture for a specified period (e.g., 16-24 hours) at 37°C and 5% CO₂.
- Step 3: Supernatant Collection. Centrifuge the plate and carefully collect the cell-free supernatant.
- Step 4: IFN-γ Quantification. Analyze the supernatant using a validated ELISA kit according to the manufacturer's instructions. Include a standard curve for absolute quantification.
- Step 5: Data Analysis. Calculate the IFN-γ concentration (pg/mL) specific to antigen recognition by subtracting the value from the CD19- control co-culture from the CD19+ experimental co-culture.
Protocol: Analysis of Cell Therapy Infusion Workflow
The administration process itself can impact product quality and potentially clinical efficacy. The following protocol, derived from an analysis of three academic medical centers, outlines the key steps for handling and infusing cryopreserved cell therapies [106].
1. Principle: To ensure the consistent and timely administration of a cryopreserved cell therapy product, maintaining cell viability and function from the point of thaw to patient infusion.
2. Procedure:
- Step 1: Pre-infusion Communication. The cell therapy technologist (CTT) contacts the patient's nurse to confirm the patient's status is stable and they are ready for the infusion.
- Step 2: Product Thaw Initiation. For products thawed at the bedside or nearby, the CTT waits for explicit approval from the nurse and/or physician before beginning the thaw process to minimize the time from thaw to infusion.
- Step 3: Product Verification. Conduct three separate verification steps involving the CTT, pharmacist, nurse, and/or physician to confirm patient and product identity against electronic records and paperwork. This process averages 6 ± 3 minutes [106].
- Step 4: Thawing. Thaw the cryobag in a controlled manner using a 37°C water bath or a validated automated thawing device (e.g., Plasmatherm).
- Step 5: Infusion. Initiate infusion immediately post-thaw. The time from thaw to infusion is critical and varies by facility design: it can be less than 20 minutes when thawed near the patient room, or over 40 minutes when thawed in a distant lab [106].
The workflow analysis found that thawing location significantly impacts the timeline, underscoring the need for standardized protocols to preserve product integrity [106].
Comparative Efficacy and Cross-Trial Analysis
In the absence of direct head-to-head trials, adjusted indirect comparisons are a statistically accepted method for comparing therapies [107]. This method preserves the randomization of original trials by comparing the treatment effect of Drug A vs. a common comparator (e.g., placebo) with the effect of Drug B vs. the same common comparator.
The formula for an adjusted indirect comparison of two drugs, A and B, via a common comparator C, for a continuous outcome is [107]:
(A vs. B) = (A vs. C) - (B vs. C)
For binary outcomes, the relative risk is calculated as [107]:
(A vs. B) = (A/C) / (B/C)
This method is preferred over a "naïve direct comparison" (simply comparing results from two separate trials), which can be confounded by differences in trial populations, design, and conduct [107]. While adjusted indirect comparisons increase uncertainty, they provide a more valid basis for cross-trial inference in the evolving CTP landscape where direct comparisons are scarce.
Analysis of the 27 FDA-approved cell therapies reveals a field marked by rapid innovation but still maturing in its understanding of therapeutic MoA. A significant number of approved products lack a definitively known mechanism, and even for those with a proposed MoA, correlating in vitro potency measures with clinical efficacy remains a substantial challenge.
For researchers, this underscores several key priorities:
- Rigorous MoA Elucidation: Investing in foundational research to move from "proposed" to "confirmed" mechanisms is critical.
- Advanced Potency Assays: Developing potency tests that are more predictive of clinical outcome is necessary for ensuring consistent product quality and patient benefit.
- Standardized Administration: Implementing harmonized clinical workflows for handling and infusion can minimize process-related variability and help better isolate the true product effect.
As the pipeline continues to expand beyond oncology into autoimmune diseases, diabetes, and heart failure, these principles will be fundamental to the sustainable and effective integration of cell therapies into modern medicine [108].
Cell therapy represents a revolutionary pillar in therapeutic intervention, leveraging living cells to treat, and potentially cure, a range of diseases from cancer to genetic disorders. The fundamental mechanism of action (MoA) involves the administration of cells to replace damaged tissue, modulate immune responses, or deliver therapeutic agents directly to disease sites. These therapies can be categorized into three primary modalities based on cell source and administration strategy: autologous (using the patient's own cells), allogeneic (using cells from a healthy donor), and in vivo approaches (where genetic material is delivered directly into the patient's body to modify their own cells in situ). Understanding the distinct MoAs of these approaches is critical for researchers and drug development professionals aiming to select the optimal platform for a given therapeutic goal. This analysis provides a comparative examination of their MoAs, supported by experimental data, protocols, and key research tools, framed within the broader context of cell therapy MoA research.
Comparative Analysis of Key Characteristics
The table below summarizes the core characteristics, including the proposed MoAs, of the three therapeutic approaches.
Table 1: Key Characteristics of Cell Therapy Approaches
| Feature | Autologous Approach | Allogeneic Approach | In Vivo Approach |
|---|---|---|---|
| Cell Source | Patient's own cells (e.g., T cells, HSCs) [109] | Healthy donor (e.g., PBMCs, iPSCs, Cord Blood) [110] [111] [112] | Patient's own cells in situ |
| Key Proposed MoA | Engineered or expanded cells recognize and eliminate target cells (e.g., tumors) or repair damaged tissue upon reinfusion [109] [80] | Off-the-shelf cells recognize and eliminate target cells or repair tissue; may require gene editing to prevent immune rejection [110] [111] | Direct administration of genetic material (e.g., via viral vectors) to patient's cells to alter genetic makeup or function [113] |
| Manufacturing | Complex, patient-specific process; involves leukapheresis, external processing, and expansion [109] [111] | Single manufacturing run for multiple patients; scalable, from a master cell bank [110] [112] | No ex vivo cell culture; involves production and administration of viral vectors (e.g., AAV, LV) [113] |
| Typical Timeframe | Several weeks [111] [114] | Immediate ("off-the-shelf") [112] [114] | Direct administration |
| Immune Compatibility | High (minimizes rejection risk) [109] [114] | Lower (risks GvHD and host immune rejection) [111] [112] | High (uses patient's own cells) |
| Scalability | Low (personalized) [109] [111] | High (universal) [110] [112] | Potentially high |
| Key Challenges | High cost, manufacturing variability, T cell exhaustion in patients [109] [111] [80] | Graft-versus-host disease (GvHD), host-versus-graft (HvG) rejection, gene-editing safety [111] [112] | Immune response to vectors, controlling transduction specificity, separating empty/full capsids (AAV) [113] |
Experimental Models and Protocols for MoA Elucidation
A critical aspect of MoA research involves the use of standardized experimental models and protocols to dissect the potency and efficacy of these complex therapies. The following sections detail methodologies relevant to each approach.
Autologous CAR-T Cell Potency and Efficacy Assay
Objective: To evaluate the mechanism of action and functional potency of autologous CAR-T cells by measuring their target-cell-specific cytokine production and cytotoxic activity, and to correlate these in vitro measurements with clinical efficacy endpoints [1].
Protocol Steps:
- Cell Preparation: Generate autologous CAR-T cells from patient PBMCs via leukapheresis. Transduce T cells with a lentiviral (LV) or other vector encoding the CAR construct. Expand cells ex vivo to the desired therapeutic dose [113] [111].
- Co-culture Setup: Co-culture the manufactured CAR-T cells with target cells expressing the antigen of interest (e.g., CD19+) and control cells that do not. Use a defined effector-to-target (E:T) ratio.
- Potency Assay (IFN-γ Secretion): After a defined incubation period (e.g., 24 hours), collect the culture supernatant. Quantify the concentration of IFN-γ using an enzyme-linked immunosorbent assay (ELISA). This measures the CAR-T cells' activation upon target recognition and is a common potency test [1].
- Efficacy Endpoint Test (Clinical Correlation): Adminute the CAR-T cell product to the patient. The primary efficacy endpoint is often clinical remission. Assess this via standardized oncology response criteria (e.g., complete remission rate).
- Data Analysis: Correlate the in vitro IFN-γ potency test results with the clinical efficacy endpoint data. As demonstrated with Kymriah, a correlation may be observed, though significant lot-to-lot variability can make a definitive correlation challenging [1].
The logical relationship between these concepts in MoA research is outlined below.
Generation of Gene-Edited Allogeneic CAR-T Cells
Objective: To create universal "off-the-shelf" CAR-T cells from healthy donor PBMCs by disrupting the T-cell receptor (TCR) to prevent graft-versus-host disease (GvHD) [111].
Protocol Steps:
- Donor Cell Isolation: Isolate PBMCs from a healthy donor via leukapheresis.
- Gene Editing: Use gene-editing technology (e.g., CRISPR/Cas9) to disrupt the TCR alpha constant (TRAC) locus. This is typically done via electroporation of ribonucleoprotein (RNP) complexes.
- CAR Transduction: Transduce the gene-edited T cells with a lentiviral vector encoding the desired CAR construct.
- Cell Expansion and Characterization: Expand the resulting TCR-negative/allogeneic CAR-T cells. Validate the double-positive phenotype through flow cytometry (confirming TCR loss and CAR expression) and perform functional assays to confirm reduced alloreactivity in vitro.
- Banking: Cryopreserve the final product to create an "off-the-shelf" inventory for multiple patients [110] [111].
Manufacturing and Potency Assessment ofIn VivoGene Therapy Vectors
Objective: To produce and quality-control adeno-associated viral (AAV) vectors for direct in vivo administration, ensuring a high percentage of fully packaged, potent capsids [113].
Protocol Steps:
- Upstream Process: Culture producer cells (e.g., HEK293). Co-transfect with a cis-plasmid (carrying the therapeutic gene), a trans-acting plasmid (for replication/capsid proteins), and an adenoviral helper plasmid. Harvest the cell culture and lysate.
- Downstream Purification: Treat the lysate with nuclease to degrade unpackaged nucleic acids. Purify the full AAV capsids using chromatography and ultracentrifugation techniques. A critical quality control step is to separate empty capsids from those containing the full therapeutic genome [113].
- Potency and QC Testing: Perform QC assays, including:
- Vector Genome Titer: Quantify the concentration of packaged genomes using qPCR or ddPCR. This is a key potency attribute.
- In Vitro Potency Assay: Transduce a permissive cell line with the AAV vector and measure the expression of the therapeutic transgene (e.g., via ELISA or functional enzyme activity assay).
- Purity: Test for residual impurities from the manufacturing process, such as host cell DNA and proteins [113].
Research Reagent Solutions for MoA Studies
The table below lists essential reagents and their functions for investigating the MoAs of cell and gene therapies.
Table 2: Key Research Reagents for Cell and Gene Therapy MoA Studies
| Reagent / Solution | Function in MoA Research |
|---|---|
| Lentiviral (LV) / Viral Vectors | Delivery of CAR transgenes or therapeutic genes into target cells (for ex vivo and in vivo approaches) [113] [80]. |
| Gene Editing Tools (CRISPR/Cas9, TALEN, ZFN) | Disruption of endogenous genes (e.g., TCR, HLA) in allogeneic cells to reduce GvHD and immune rejection [111]. |
| Cell Culture Supplements (e.g., IL-2, Serum) | Support ex vivo expansion and maintenance of T cells and stem cells; critical for maintaining cell potency during manufacturing [113]. |
| CAR Signaling Domain Components (CD3ζ, CD28, 4-1BB) | Engineering intracellular domains to optimize CAR-T cell persistence, metabolic profile, and anti-tumor efficacy (e.g., CD28 for effector memory, 4-1BB for central memory) [80]. |
| AAV Capsids and Plasmids | Production of viral vectors for in vivo gene therapy; different serotypes confer varying tissue tropism [113]. |
| IFN-γ ELISA Kit | A standard bioassay to measure CAR-T cell activation and potency upon target engagement [1]. |
| Flow Cytometry Antibodies | Characterization of cell surface markers (e.g., CAR expression, TCR deletion, HLA profiling) and analysis of immune cell populations [111]. |
MoA and Efficacy Endpoint Relationships
A central challenge in advanced therapy development is linking the proposed MoA to measurable clinical outcomes. The following diagram illustrates the complete theoretical pathway from product attribute to patient benefit, which is often complex and incompletely understood.
The choice between autologous, allogeneic, and in vivo therapeutic approaches is fundamentally guided by their distinct mechanisms of action, which in turn dictate their clinical and manufacturing profiles. Autologous therapies leverage the patient's immune system with high specificity and minimal rejection risk but face scalability and cost challenges. Allogeneic "off-the-shelf" platforms offer scalability and immediate availability but require sophisticated engineering to overcome immune rejection. In vivo gene therapy represents a paradigm shift by directly modifying patient cells in situ, though it faces hurdles related to delivery and immune response. For researchers, a deep understanding of these MoAs is paramount. The experimental protocols and reagent tools outlined here provide a foundation for probing these mechanisms further. Future progress in this field will depend on continued refinement of gene-editing technologies, vector engineering, and, crucially, the development of robust in vitro potency assays that can reliably predict clinical efficacy, ultimately enabling the development of more effective and accessible cell and gene therapies.
The evaluation of a proposed Mechanism of Action (MoA) represents a fundamental component in the regulatory approval process for innovative cell therapies worldwide. Regulatory agencies including the European Medicines Agency (EMA), the U.S. Food and Drug Administration (FDA), and various Asian authorities have established distinct yet increasingly harmonized frameworks for assessing how a therapeutic product achieves its intended biological effect. For researchers and drug development professionals, understanding these nuanced regulatory landscapes is critical for designing robust preclinical and clinical development programs that adequately demonstrate product safety and efficacy.
The importance of MoA characterization has grown substantially with the emergence of complex advanced therapy medicinal products (ATMPs), particularly chimeric antigen receptor (CAR) T-cell therapies. As illustrated by recent advances in the field, including innovative approaches such as in vivo CAR-T cell generation via targeted lipid nanoparticles (tLNP), the need for comprehensive MoA data has become increasingly important for regulatory success [115]. These data not only support the primary therapeutic claims but also inform risk assessments, dosing rationale, and potential biomarker strategies across global jurisdictions.
Comparative Analysis of Regional Regulatory Frameworks
United States FDA Approach
The FDA's regulatory framework for evaluating MoA employs a risk-based classification system that categorizes medical devices (including certain software components of combination products) into Class I, II, or III based on the level of control necessary to assure safety and effectiveness [116] [117]. This classification directly influences the type of premarketing submission required – from 510(k) notifications for Class I and II devices to Premarket Approval (PMA) applications for high-risk Class III devices [117].
For novel cell therapies, the FDA has implemented several specialized programs and guidance documents that directly impact MoA assessment:
- Breakthrough Devices Program: Provides expedited development and review for devices that demonstrate potential for more effective treatment of life-threatening diseases [118]
- AI-Enabled Device Software Functions: New guidance requires clear documentation of algorithmic decision-making processes and establishes mechanisms for continuous monitoring of device performance [119]
- Quality Management System Regulation (QMSR): Transitioning to align with ISO 13485:2016 to improve consistency in manufacturing and control processes [119]
The FDA's approach to MoA evaluation emphasizes comprehensive lifecycle management, particularly for rapidly evolving technologies like AI-driven medical devices. The Agency's guidance on "Marketing Submission Recommendations for a Predetermined Change Control Plan for Artificial Intelligence-Enabled Device Software Functions" specifically addresses the need for planned modifications while maintaining demonstrated safety and effectiveness [118].
European Union EMA Framework
The European Medicines Agency operates under different regulatory frameworks for cell therapies, primarily the Advanced Therapy Medicinal Products (ATMP) Regulation and the Medical Device Regulation (MDR). Recent updates have significant implications for MoA evaluation:
- EU MDR Implementation: Completed in May 2024 after transitional periods, requiring stricter clinical evidence and technical documentation [119]
- In Vitro Diagnostic Regulation (IVDR): Full compliance deadline of May 26, 2025, significantly impacting manufacturers requiring notified body review [119]
- Product Information Requirements: Specific guidelines on content, standard headings, and terminology for all official EU languages [120]
A critical consideration for developers is the EU-U.S. Mutual Recognition Agreement (MRA), which facilitates recognition of inspection authorities between the two jurisdictions but currently excludes Advanced Therapy Medicinal Products from its scope [121]. This exclusion means that separate manufacturing inspections and compliance demonstrations are required for market authorization in both regions, extending to MoA-related manufacturing controls.
Asian Regulatory Landscape
While the search results do not provide specific details on Asian regulatory approaches to MoA evaluation, the scientific literature demonstrates significant research activity in cell therapy across Asia. Recent presentations at international conferences, such as the 2025 European Hematology Association meeting, featured prominent Asian research contributions, particularly in CD7 CAR-T cell therapy for T-cell acute lymphoblastic leukemia (T-ALL) [122]. This suggests parallel regulatory evolution to accommodate these advanced therapies, though specific MoA assessment frameworks in Asia remain outside the current search results.
Table 1: Comparison of Key Regulatory Elements in MoA Evaluation
| Regulatory Element | U.S. FDA Approach | EU EMA Approach | Asian Agencies |
|---|---|---|---|
| Classification System | Risk-based (Class I, II, III) [116] | Risk-based (Class I, IIa, IIb, III) [119] | Information missing |
| Premarket Pathway | 510(k), De Novo, PMA [117] | Conformity assessment with notified bodies [119] | Information missing |
| Lifecycle Management | Predetermined Change Control Plans for AI [118] | Limited information | Information missing |
| International Alignment | Transitioning to QMSR (aligned with ISO 13485) [119] | MDR/IVDR with capacity challenges [119] | Information missing |
MoA Evaluation in Action: CAR-T Cell Therapy Case Studies
CD7 CAR-T for T-ALL: Regulatory Considerations
Recent clinical investigations of CD7 CAR-T cell therapy for refractory/relapsed T-cell acute lymphoblastic leukemia (T-ALL) illustrate the complex interplay between MoA characterization and regulatory requirements. A multicenter I/II trial (NCT06316427) directly compared autologous, transplant donor-derived, and novel donor-derived CD7 CAR-T cells, revealing critical MoA-related safety differences [122].
The study demonstrated comparable complete remission rates across all three sources (89%, 57%, and 89% respectively) but significant variations in safety profiles. Specifically, the donor-derived CAR-T groups showed prolonged hematologic suppression and increased infection risks (43% fatal infections in the transplant donor group) [122]. These findings highlight how MoA-related considerations – including cell source and persistence – directly inform risk-benefit assessments by regulators.
From a regulatory perspective, this evidence supports the importance of comprehensive MoA characterization that extends beyond efficacy measures to include:
- Cell persistence and expansion dynamics
- On-target/off-tumor toxicity profiles
- Product-related immunogenicity
- Long-term safety implications
In Vivo CAR-T Generation: Novel MoA Considerations
The emergence of in vivo CAR-T cell generation represents a paradigm shift in cell therapy approach with distinct regulatory implications for MoA assessment. Recent research published in Science demonstrates a novel approach using CD8-targeted lipid nanoparticles (tLNP) to deliver CAR-encoding mRNA directly to T cells in vivo, bypassing traditional ex vivo manufacturing [115].
This technology introduces several unique MoA considerations for regulatory evaluation:
- Biodistribution and targeting efficiency of tLNP to specific T-cell subsets
- Kinetics and durability of CAR expression from mRNA versus viral vector integration
- Potential for "immune reset" through regeneration of naïve B cells observed in autoimmune models [115]
The regulatory pathway for such innovative approaches would likely require extensive nonclinical MoA characterization, including detailed assessments of delivery efficiency, transcript expression kinetics, and potential off-target effects. The use of novel ionizable lipid L829 to reduce liver tropism represents both a manufacturing control issue and a key component of the safety MoA [115].
Experimental Design for MoA Characterization
Core Methodologies for MoA Evaluation
Comprehensive MoA characterization for cell therapies requires a multifaceted experimental approach incorporating both established and emerging technologies. Based on current research in the field, the following methodologies provide critical MoA insights:
- Single-cell CAR T atlas construction: As employed in research identifying Type 2 immune functions in long-term leukemia remission, this approach analyzes gene expression in hundreds of thousands of CAR-T cells to identify subpopulations correlated with clinical outcomes [123]
- Metabolic profiling: Investigations into IL-4-driven CAR-T cell exhaustion have revealed the importance of glycolytic pathways in sustaining antitumor function, requiring assessment of metabolic states and mitochondrial function [123]
- Mitochondrial transfer techniques: Research demonstrating enhanced T-cell function through transfer of mitochondria from mesenchymal stem cells requires specialized co-culture systems and tracking methods [123]
- In vivo imaging and tracking: For modalities like in vivo CAR-T generation, real-time assessment of cell localization, expansion, and persistence is essential [115]
Research Reagent Solutions for MoA Studies
Table 2: Essential Research Reagents for Cell Therapy MoA Characterization
| Reagent/Category | Specific Function in MoA Studies | Application Example |
|---|---|---|
| CD8-targeted lipid nanoparticles | In vivo delivery of CAR-encoding nucleic acids | In vivo CAR-T generation without viral vectors [115] |
| Cytokine muteins (e.g., decoy-resistant IL-18) | Enhanced immune stimulation without negative regulation | Engineered E. coli expressing IL-18 mutein to boost CAR-NK responses [123] |
| Gene editing tools (CRISPR/Cas9) | Specific gene knockout to elucidate mechanism | IL-4 knockout to reverse CAR-T exhaustion [123] |
| Mitochondrial tracking dyes | Visualization of mitochondrial transfer between cells | Demonstrating MSC-to-T-cell mitochondrial transfer [123] |
| Single-cell RNA sequencing reagents | High-resolution analysis of cellular heterogeneity | Identifying Type 2 cytokine programs in durable remission [123] |
Visualization of MoA Evaluation Pathways
Regulatory Decision Pathway for Novel MoA
Diagram Title: Regulatory MoA Evaluation Pathway
CAR-T Cell MoA Characterization Workflow
Diagram Title: CAR-T Cell MoA Assessment Workflow
The evaluation of proposed Mechanisms of Action represents a dynamic and evolving aspect of global regulatory science, particularly for innovative cell therapies. The comparative analysis presented in this guide demonstrates both convergence and divergence in how major regulatory agencies approach MoA assessment. While the FDA and EMA increasingly emphasize comprehensive lifecycle management and real-world evidence generation, specific technical requirements and review processes remain distinct.
For research and development professionals, success in global regulatory strategy necessitates:
- Early engagement with relevant agencies through formal consultation procedures
- Robust preclinical MoA packages that inform clinical trial design
- Comprehensive biomarker strategies that bridge nonclinical and clinical development
- Flexible manufacturing approaches that accommodate evolving MoA understanding
As cell therapy technologies continue to advance – from in vivo CAR-T generation to enhanced persistence through mitochondrial transfer – regulatory frameworks will inevitably evolve. Development teams that proactively address MoA characterization throughout the product lifecycle will be best positioned for successful global registration and, ultimately, delivery of transformative treatments to patients worldwide.
The journey of a cell therapy from laboratory concept to clinical application hinges on a critical, yet often challenging, process: translating non-clinical findings into predictable clinical outcomes. For researchers and drug development professionals, demonstrating a consistent Mechanism of Action (MoA) across this divide is paramount. This guide objectively compares the tools at the scientist's disposal—namely, animal models and biomarkers—for building a robust evidentiary bridge. Experimental data and meta-analyses reveal significant disparities in the predictive value of different models, profoundly impacting how non-clinical data informs clinical trial design and interpretation. A recent large-scale meta-analysis of CAR-T cell therapies highlights this issue, finding that while logistic regression models could predict clinical outcomes from clinical data, they failed when using preclinical features alone, indicating that experimental factors in animal studies often do not accurately forecast human responses [124]. This underscores the necessity of a strategically selected, multi-faceted approach to non-clinical MoA evidence generation.
Animal Models: Predictive Value and Limitations
Animal models are indispensable in preclinical development, allowing for the initial evaluation of complex interactions within a living system. However, their predictive capacity for clinical efficacy and toxicity is not uniform. The choice of model introduces specific biases and limitations that must be accounted for when designing experiments and interpreting data.
Comparative Analysis of Preclinical Animal Models
The table below summarizes the key characteristics, advantages, and disadvantages of commonly used animal models in immunotherapy development, based on a comprehensive meta-analysis [124].
| Model Type | Key Characteristics | Advantages | Disadvantages / Translational Gaps |
|---|---|---|---|
| Syngeneic (Transplanted) | Mouse tumor cell lines in immunocompetent mice (e.g., C57BL/6, BALB/c) | - Cost and time-efficient- Studies with native immune system- Possible orthotopic implantation | - Limited tumor heterogeneity- Artificial TME- Lack of human antigen cross-reactivity [124] |
| Syngeneic (Spontaneous) | Induced cancer development in immunocompetent mice | - Realistic tumor development- Studies with native immune system | - Variable mutation rates and tumor onset- Time-consuming- Limited clinical comparability [124] |
| Transgenic | Controlled genetic manipulation to model human tumors | - Close modeling of human genetics- Targeted insights into specific genes | - High maintenance and cost- Time-consuming- Risk of unintended phenotypes [124] |
| Xenograft | Human tumor/immune cells in immunodeficient mice (e.g., NSG) | - Use of human biological components- Suitable for human tumor biology studies | - Graft-versus-host disease (GvHD)- Loss of host immune system- Incomplete human immunity [124] |
| Patient-Derived Xenograft (PDX) | Patient tumor cells in immunodeficient mice | - Maintains tumor heterogeneity- Increased clinical relevance | - GvHD- High cost and time-consuming- Lack of human stromal components [124] |
Quantitative Predictive Performance
The meta-analysis of CAR-T cell therapies provided quantitative data on the use and predictive power of these models. A striking finding was the extreme scarcity of immunocompetent models in the field; only 4% of the analyzed mouse studies utilized syngeneic models [124]. This heavy reliance on immunodeficient models is a significant translational bottleneck, particularly for solid tumors.
Machine learning models trained on this dataset revealed a critical performance gap: while models could predict clinical outcomes from clinical features with high accuracy (Macro F1 and AUC >0.8), they failed to predict preclinical outcomes from preclinical features (Macro F1 <0.5, AUC <0.6) [124]. This indicates that the outcomes observed in animal studies are heavily influenced by experimental conditions that do not correlate with human physiology, limiting their predictive utility.
Biomarkers: Bridging the Evidentiary Gap
Biomarkers provide a quantifiable link between non-clinical and clinical MoA evidence. They are critical for demonstrating that the biological activity observed in animals is recapitulated in patients, thereby validating the therapeutic MoA.
A Framework for Biomarker Integration
A modern approach involves integrating diverse biomarker data into a Comprehensive Oncological Biomarker Framework. This holistic strategy combines genetic, molecular, histopathological, and multi-omics data to create a "molecular fingerprint" for each patient, guiding therapy from diagnosis through treatment monitoring [125]. The following diagram illustrates the integrated flow of this framework from data acquisition to clinical application.
Biomarker Technologies and Methodologies
Advanced technologies are crucial for discovering and quantifying biomarkers that reflect MoA. The field has moved beyond single-molecule assays to highly multiplexed, sensitive platforms.
Mass Spectrometry (MS)-Based Proteomics: This technology allows for the unbiased detection and quantification of proteins in biological specimens like blood plasma or cerebrospinal fluid (CSF). It is favored for its high sensitivity, ability to detect unexpected proteins, and quantitative rigor. A key challenge in plasma proteomics is the immense dynamic range of protein concentrations. To address this, advanced sample preparation methods like magnetic bead-based enrichment (e.g., SP3, Proteograph) are used to deplete high-abundance proteins, allowing for the reproducible quantification of over 1,000-3,000 protein groups from a single plasma sample and enabling the discovery of previously undetectable, low-abundance biomarkers [126].
Affinity-Based Platforms: Technologies like Olink (using proximity extension assays) and SomaScan (using slow off-rate modified aptamers) enable highly multiplexed protein profiling with high sensitivity and specificity. These platforms are increasingly implemented in clinical trials to identify candidate biomarkers associated with treatment efficacy and toxicity [126].
Novel Biosensors: Emerging techniques include Surface-Enhanced Raman Spectroscopy (SERS), which uses metal nanoparticles for ultra-sensitive biomarker detection, and ATLAS-seq, which combines single-cell technology with aptamer-based sensors to identify antigen-reactive T cells, providing direct insight into immune MoA [125].
Case Study: Biomarker Discovery from Preclinical Model to Clinical Validation
A study from MD Anderson Cancer Center exemplifies the successful translation of a biomarker from preclinical models to human validation. Researchers used preclinical models of pancreatic cancer and melanoma to investigate the impact of TET2-mutated clonal hematopoiesis (CH) on the tumor immune microenvironment [127].
Experimental Workflow:
- Model Development: In vivo models of TET2-mutated CH were developed to accurately reflect the human condition.
- Mechanistic Insight: In these models, TET2-mutated CH was associated with an improved response to combination immunotherapy. The MoA was linked to increased antigen presentation by pro-inflammatory myeloid cells, resulting in more activated T cells.
- Clinical Validation: Analysis of a large cohort of over 35,000 patients with non-small cell lung cancer (NSCLC) showed that patients with TET2-mutated CH had significantly improved overall survival with immunotherapy. This finding was confirmed in a separate group of 25,064 patients with colorectal cancer [127].
Conclusion: This work established TET2-mutated CH as a potential biomarker for improved immunotherapy response, demonstrating how a mechanism discovered in preclinical models can be validated as a predictive biomarker in human populations [127].
Integrated Experimental Protocols for MoA Bridging
To systematically build evidence linking non-clinical and clinical MoA, researchers can employ the following integrated protocols.
Protocol 1: Establishing a "Fit-for-Purpose" Preclinical Model Strategy
This protocol ensures that the chosen animal models are aligned with key scientific and clinical questions [128].
- Define the Question of Interest (QOI): Clearly articulate the primary MoA-related question (e.g., "Does the therapy engage the target and initiate tumor cell killing in a physiologically relevant TME?").
- Select Models Based on QOI:
- For initial proof-of-concept and immune function studies, use syngeneic models with orthotopic implantation where possible [124].
- For evaluating human-specific target engagement, use humanized or xenograft models, acknowledging their limitations regarding a fully functional immune system [124].
- Avoid reliance on a single model. Use multiple, complementary models to triangulate evidence for the MoA.
- Incorporate Longitudinal Biomarker Sampling: Design studies to collect blood and tumor tissue at multiple timepoints for biomarker analysis (e.g., cytokine levels, immune cell infiltration, tumor cell death markers).
- Correlate Biomarker Data with Efficacy Endpoints: Statistically analyze the relationship between biomarker modulation and tumor growth inhibition or survival in the animal models.
Protocol 2: Clinical Translation and Validation of Preclinical Biomarkers
This protocol outlines the steps for validating non-clinical MoA findings in human trials.
- Identify Candidate Biomarkers from Preclinical Models: Select the most promising MoA-related biomarkers from animal studies (e.g., specific proteomic signatures, immune cell populations).
- Utilize Advanced Proteomics in Clinical Samples:
- Apply MS-based or affinity-based proteomics platforms (e.g., Olink) to patient serum/plasma or CSF samples collected during clinical trials [126].
- For cellular therapies in neurodegenerative diseases, CSF is a key matrix for measuring pharmacodynamic biomarkers, as demonstrated in the NurOwn program for ALS [129].
- Correlate with Clinical Outcomes: Perform statistical analyses to link the levels of the candidate biomarkers with clinical endpoints such as overall response rate, progression-free survival, or toxicity grades.
- Validate in Independent Cohorts: Confirm the association of the biomarker with clinical outcome in a separate, larger patient cohort, as was done for the TET2-mutated CH biomarker [127].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting the experiments described in this guide.
| Research Reagent / Solution | Function and Application in MoA Research |
|---|---|
| Immunocompetent Syngeneic Models (e.g., C57BL/6, BALB/c) | Provides a intact immune system for studying complex cell therapy interactions with the tumor microenvironment [124]. |
| Humanized Mouse Models (e.g., NSG with human immune system) | Enables the study of human-specific CAR-T or other cell therapies in a more physiologically relevant, albeit still limited, in vivo context [124]. |
| Magnetic Beads for Proteomics (e.g., SP3, Seer Proteograph) | Depletes high-abundance proteins from plasma/serum to significantly deepen proteomic coverage and discover low-abundance biomarkers [126]. |
| Proximity Extension Assay Kits (e.g., Olink) | Allows for high-sensitivity, multiplexed quantification of proteins in small volume samples from clinical trials, linking MoA to clinical response [126]. |
| Cell Staining Panels for Flow Cytometry | Characterizes immune cell populations (e.g., T cell activation/exhaustion markers, myeloid subsets) in tumors and blood to demonstrate on-target MoA. |
| Digital PCR or Next-Gen Sequencing Kits | Quantifies tumor burden (e.g., via ctDNA) or identifies specific genetic biomarkers (e.g., TET2 mutations) for patient stratification and response monitoring [127] [125]. |
Bridging non-clinical and clinical MoA evidence is a multifaceted challenge that requires a critical and strategic approach. The data clearly shows that not all animal models are created equal; over-reliance on immunodeficient systems, a common practice in the field, is a major contributor to translational failure, especially in solid tumors [124]. Success depends on complementing well-chosen, fit-for-purpose animal models with a robust pipeline for biomarker discovery and validation. By employing advanced proteomics, multi-omics integration, and systematically validating findings from preclinical models in large clinical cohorts, researchers can build an irrefutable chain of evidence for their therapy's Mechanism of Action, ultimately increasing the probability of clinical success.
The cell therapy landscape in 2025 is characterized by strategic capital allocation toward therapies with novel and scalable mechanisms of action (MoAs). Allogeneic (off-the-shelf) platforms, in vivo cell engineering, and non-traditional cell types like NK cells are attracting the largest investments, reflecting investor confidence in their potential to overcome the limitations of first-generation autologous therapies. Concurrently, the application of artificial intelligence (AI) in discovery and the push for manufacturing innovation are critical enablers, underscoring a mature, platform-driven investment thesis. This guide objectively compares the performance and supporting data of the most prominent MoAs shaping the cell therapy pipeline.
Analysis of 2025 Deal Flow and Key MoA Trends
Investment trends in 2025 provide a clear window into the mechanisms of action that the industry believes hold the greatest therapeutic and commercial potential. The following analysis synthesizes global funding data to highlight dominant technological shifts.
Quantitative Snapshot of 2025 Cell Therapy Fundings
The table below summarizes key financing events from the first half of 2025, highlighting the connection between capital investment, company platform, and the underlying MoA [130].
Table 1: Key Cell Therapy Financings in 2025 (YTD)
| Company | Location | Funding Amount | Stage | Core Technology / MoA Focus |
|---|---|---|---|---|
| Wugen | Missouri, USA | $115 Million | Late-stage | Off-the-shelf CAR-T therapies |
| Neurona Therapeutics | California, USA | $102 Million | Late-stage | Regenerative cell therapy for epilepsy |
| Umoja Biopharma | Washington, USA | $100 Million | Late-stage | In vivo CAR-T pipeline |
| A2 Biotherapeutics | California, USA | $80 Million | Late-stage | Tmod platform for precision oncology |
| Gameto | New York, USA | $44 Million | Late-stage | Stem cell-based reproductive care |
| Garuda Therapeutics | Massachusetts, USA | $50 Million | Early-stage | Off-the-shelf hematopoietic stem cells |
| Somite AI | Massachusetts, USA | $47 Million | Early-stage | AI-driven foundation model for cell therapy development |
| Inovacell | Japan | $52 Million | Late-stage | Advanced clinical trial for cell therapy |
| TreeFrog Therapeutics | France | $34 Million | Late-stage | Stem cell therapy for Parkinson's disease |
| ONGeno | Poland | $3.6 Million | Early-stage | Stem cell therapy for multiple sclerosis |
Interpretation of Investment Trends by MoA
The concentration of capital reveals four dominant trends in MoA confidence:
Confidence in Allogeneic MoAs: The largest single deal of the year, Wugen's $115 million financing, along with significant rounds for Garuda Therapeutics and Allogenica, signals strong belief in the "off-the-shelf" MoA [130]. The primary advantage is the ability to overcome the logistical and scalability challenges of patient-specific (autologous) therapies, creating a more viable pharmaceutical product model.
Breakthrough of In Vivo Cell Engineering: Umoja Biopharma's $100 million Series C represents a paradigm shift in MoA [130]. Instead of engineering cells ex vivo, their platform is designed to instruct a patient's own immune cells inside the body (in vivo). This MoA could dramatically simplify treatment and reduce costs.
Expansion into Non-Oncology and Regenerative MoAs: While oncology remains dominant, large financings for neurological applications (Neurona, TreeFrog) and reproductive health (Gameto) indicate validated confidence in the MoAs for regenerative medicine [130]. These therapies often work through trophic support (secreting growth factors) or direct cell replacement to restore tissue function.
AI as an MoA Discovery and Optimization Tool: The substantial $47 million raised by Somite AI highlights a growing reliance on AI to decipher complex cell states and interactions, thereby accelerating the identification of novel MoAs and the design of more effective therapeutic cells [130] [131].
Comparative Analysis of Key Cell Therapy Mechanisms of Action
This section provides an objective, data-driven comparison of the leading MoAs, detailing their proposed mechanisms, advantages, and current experimental and clinical validation.
MoA Performance Comparison Table
Table 2: MoA Performance and Clinical Status Comparison
| Mechanism of Action | Key Companies (Pipeline) | Proposed Primary MoA | Therapeutic Area | Clinical Stage (as of 2025) | Reported Efficacy/Performance Data |
|---|---|---|---|---|---|
| Allogeneic CAR-T | Wugen, Allogenica | Off-the-shelf, universally compatible T cells targeting tumor antigens via CAR [130]. | Oncology | Phase 3 Trials | Designed to overcome manufacturing delays of autologous CAR-T; focus on demonstrating non-inferiority to autologous products. |
| In Vivo CAR-T | Umoja Biopharma | In vivo reprogramming of patient T cells using viral or non-viral vectors to express CAR [130]. | Oncology | Phase 1/2 Trials | Aims to reduce complexity and cost; early data focuses on feasibility, transduction efficiency, and initial anti-tumor activity. |
| CAR-NK Cell Therapy | MiNK Therapeutics, NK CellTech | Allogeneic Natural Killer cells engineered with CARs for tumor killing with reduced risk of CRS [130]. | Oncology | Phase 1/2 Trials | Exploits innate cytotoxic activity; data shows promising response rates with a favorable safety profile in early trials. |
| Regenerative Stem Cells | Neurona, TreeFrog | Cell replacement and/or trophic factor secretion to repair damaged neural circuits or tissues [130] [132]. | Neurology (Epilepsy, Parkinson's) | Phase 1/3 Trials | Preclinical models show functional recovery; Phase 1/2 data focuses on engraftment, safety, and biomarker evidence of activity. |
| CAR-T for Autoimmunity | Cabaletta Bio (CABA-201) | CD19-directed CAR-T for depletion of pathogenic B-cell lineages [133]. | Systemic Sclerosis, SLE | Phase 1/2 Trials | Perceived as having "curative potential"; early trial data will focus on depth and durability of B-cell depletion and disease biomarker resolution. |
Detailed Experimental Protocols for Key MoAs
For researchers developing assays around these MoAs, the following protocols are critical for quantifying product potency and activity.
Protocol: In Vitro Potency Assay for CAR-T Products (e.g., Kymriah)
This assay measures the ability of CAR-T cells to activate and execute effector functions upon target recognition [1].
- Objective: To quantify the potency of CAR-T product lots by measuring IFN-γ production upon antigen-specific stimulation.
- Workflow:
- Co-culture Setup: Seed CAR-T cells with target cells expressing the relevant tumor antigen (e.g., CD19) at a predefined effector-to-target ratio.
- Incubation: Incubate the co-culture for a specified period (e.g., 24 hours) under standard cell culture conditions (37°C, 5% CO₂).
- Supernatant Collection: Collect culture supernatant by centrifugation.
- Cytokine Quantification: Measure IFN-γ concentration in the supernatant using a validated ELISA or multiplex immunoassay.
- Key Metrics: IFN-γ concentration (pg/mL) is correlated with product potency. Note that while this is a standard release assay, its correlation with clinical efficacy can be complex, with significant lot-to-lot variability observed historically [1].
Protocol: Cell-Based Relative Potency Assay for Gene Therapies (e.g., Luxturna)
This assay, adapted for vector potency, measures the biological activity of a transgene delivered by a viral vector [35].
- Objective: To validate the biological activity of an AAV vector encoding a therapeutic protein by measuring the protein's enzymatic function.
- Workflow:
- Cell Transduction: Transduce HEK293 cells with a serial dilution of the AAV vector (e.g., AAV2-hRPE65v2).
- Lysate Preparation: After a set expression period, lyse the cells to release the transgene-encoded protein (e.g., RPE65).
- Enzymatic Reaction: Incubate the cell lysates with the protein's substrate (e.g., all-trans-retinol).
- Product Quantification: Quantify the enzymatic reaction product (e.g., 11-cis-retinol) using highly sensitive Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS).
- Key Metrics: The assay defines a potency range (e.g., 50%–150%) relative to a reference standard, ensuring lot-to-lot consistency and stability [35].
Visualizing Core Mechanisms of Action
The following diagrams illustrate the logical flow and key differences in the MoAs currently driving investment.
Mechanism of Action (MoA) and Efficacy Relationship
This chart clarifies the critical distinction between a product's potency (a measurable attribute in the lab) and its efficacy (the clinical outcome), which is a fundamental challenge in cell therapy development [1].
Comparison of Autologous vs. Allogeneic CAR-T Workflows
This diagram contrasts the fundamental manufacturing and MoA-related logistics of the established autologous model with the emerging, scalable allogeneic approach [130] [132].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and quality control of cell therapies rely on a specific set of analytical tools and reagents. The following table details key solutions for characterizing these complex products [134].
Table 3: Key Research Reagent Solutions for Cell Therapy Development
| Reagent / Material | Primary Function | Application in MoA Research |
|---|---|---|
| Flow Cytometry Antibodies | Cell surface and intracellular protein detection | Defining cell identity (e.g., CD3/CD28 for T-cells), purity, and CAR expression. Critical for characterizing the cellular product itself [134]. |
| Cytokine Detection Kits (e.g., ELISA) | Quantification of secreted proteins | Measuring functional potency (e.g., IFN-γ release upon target engagement). Used in lot-release potency assays for CAR-T products [1] [134]. |
| Cell Culture Media & Supplements | Ex vivo cell expansion and maintenance | Supporting the growth and genetic manipulation of therapeutic cells. Formulations are often proprietary and critical to maintaining cell fitness and function [130]. |
| Viral Vectors (Lentiviral/Retroviral) | Stable genetic modification of cells | Delivering CAR constructs or other therapeutic transgenes into T cells or stem cells. The vector is a critical raw material defining the therapy's MoA [130] [132]. |
| Gene Editing Reagents (e.g., CRISPR-Cas9) | Precise genomic modification | Creating allogeneic cells by knocking out endogenous T-cell receptors (TCR) to prevent GvHD, or engineering enhanced functionalities [130]. |
| LC-MS/MS Systems | Highly specific and sensitive analyte quantification | Used in potency assays for gene therapies, measuring specific enzymatic products (e.g., 11-cis-retinol in Luxturna potency assay) to confirm biological activity [35]. |
Conclusion
A deep and actionable understanding of cell therapy mechanism of action is the fundamental pillar supporting all aspects of development, from initial discovery through regulatory approval and commercial success. This synthesis of the four intents reveals that overcoming the field's central challenges—including clinical translation hurdles, manufacturing complexity, and regulatory scrutiny—requires an unwavering focus on biologically relevant MoA. Future progress will depend on developing more predictive preclinical models, creating robust and MoA-aligned potency assays that correlate with clinical outcomes, and fostering adaptive regulatory dialogues. As the industry moves toward more complex multi-targeted and off-the-shelf therapies, a rigorous, MoA-driven development strategy will be essential for delivering on the full therapeutic potential of cell therapies for patients. The integration of advanced analytics, innovative engineering approaches, and real-world evidence will further refine our understanding of these living drugs, paving the way for next-generation treatments.
References
- 1. Mechanism of action, potency and efficacy: considerations for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05179-7]
- 2. How Potency Assay Strategy Can Accelerate Cell Therapy ... [https://slingshotbio.com/how-potency-assay-strategy-can-accelerate-cell-therapy-development/]
- 3. Emerging New Drug Modalities in 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 4. Chimeric Antigen Receptor T-Cells: An Overview of Concepts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9256991/]
- 5. T Cell Engaging Immunotherapies, Highlighting Chimeric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8657024/]
- 6. Current landscape of T-cell engagers in early-phase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536262/]
- 7. T cell engagers: expanding horizons in oncology and beyond [https://www.nature.com/articles/s41416-025-03125-y]
- 8. Current landscape of T-cell engagers in early-phase ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1665838/full]
- 9. Discordant CAR-T cell signaling: implications of divergence ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06857-w]
- 10. Comparing CAR and TCR engineered T cell performance ... [https://pubmed.ncbi.nlm.nih.gov/35127255/]
- 11. New insights on potency assays from recent advances and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597888/full]
- 12. Engaging T cells for cleanup [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1551424/full]
- 13. Neoantigen identification and TCR-T therapy development for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529609/]
- 14. An Introduction to T-cell Receptor T-cell (TCR-T) Therapy [https://www.onclive.com/view/an-introduction-to-t-cell-receptor-t-cell-tcr-t-therapy]
- 15. TIL Therapy Breakthrough: New Hope For Solid Tumor ... [https://globalrph.com/2025/09/til-therapy-breakthrough-new-hope-for-solid-tumor-treatment-in-2025/]
- 16. Tumor infiltration therapy: from FDA approval to next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274268/]
- 17. Enabling next-generation engineered TCR-T therapies ... [https://www.nature.com/articles/s41467-024-55420-6]
- 18. Emerging Advances in Solid Tumor Immunotherapy [http://www.yakhak.org/journal/view.html?uid=3414&&vmd=Full]
- 19. Next-Gen TCR-T Cell Therapy Produces Strong ... [https://www.targetedonc.com/view/next-gen-tcr-t-cell-therapy-produces-strong-responses-in-hpv-associated-cancers]
- 20. CAR-T Cell Therapy vs TCR Therapy Cancer Treatments [https://www.akadeum.com/blog/car-t-cell-therapy-vs-tcr/?srsltid=AfmBOoqBFL4uIkyEP6z1RG7BWtbWPzz2E-hkFSdtRapnjKBV_IEkUUEo]
- 21. Novel T Cell Therapies Yield Decade-Long Remission in ... [https://www.cancernetwork.com/view/novel-t-cell-therapies-yield-decade-long-remission-in-epithelial-cancer]
- 22. The role of NK cells in regulating tumorimmunity [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535086/]
- 23. Comprehensive snapshots of natural killer cells functions ... [https://www.nature.com/articles/s41392-024-02005-w]
- 24. Off-the-shelf and low toxicity: How natural killer cells could ... [https://www.statnews.com/sponsor/2025/04/25/off-the-shelf-and-low-toxicity-how-natural-killer-cells-could-transform-cell-therapy/]
- 25. AACR 2025: Off-the-shelf CAR natural killer cell therapy ... [https://ecancer.org/en/news/26405-aacr-2025-off-the-shelf-car-natural-killer-cell-therapy-with-logic-gates-elicits-complete-remissions-in-relapsed-or-refractory-blood-cancers]
- 26. Engineered “natural killer” cells could help fight cancer [https://news.mit.edu/2025/engineered-natural-killer-cells-could-help-fight-cancer-1008]
- 27. Mapping the global clinical landscape of NK cell therapies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494998/]
- 28. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 29. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 30. Stem Cell–Based Therapies via Different Administration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808770/]
- 31. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 32. Stem cell therapy for myocardial infarction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512856/]
- 33. Potency Assays for Cell and Gene Therapy [https://insights.forgebiologics.com/how-potency-assays-support-gene-therapy-success]
- 34. Validation of a potency assay for CD34 + cell based therapy [https://www.nature.com/articles/s41598-025-14828-w]
- 35. Validation of a quantitative cell-based relative potency ... [https://www.sciencedirect.com/science/article/pii/S232905012500018X]
- 36. Mechanism-linked potency assays drive gene therapy ... [https://www.selectscience.net/article/mechanism-linked-potency-assays-drive-gene-therapy-success]
- 37. New insights on potency assays from recent advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12095010/]
- 38. Accelerating Innovative Cell Therapy Development ... [https://elevate.bio/elevated-insights/accelerating-innovative-cell-therapy-development-through-phase-appropriate-potency-control/]
- 39. Dual modulation of cytotoxic and checkpoint receptors ... [https://www.nature.com/articles/s43018-025-00948-9]
- 40. The potential of microfluidic cell analysis in CAR T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605917/]
- 41. Performance comparison of a flow cytometry immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8853233/]
- 42. Simplified flow cytometry-based assay for rapid multi-cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245854/]
- 43. Simplified flow cytometry-based assay for rapid multi- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1594141/full]
- 44. Effective extracellular payload release and ... [https://www.nature.com/articles/s41467-025-58266-8]
- 45. Solid tumour CAR-T cells engineered with fusion proteins ... [https://www.nature.com/articles/s41551-025-01509-2]
- 46. Designing Cell Therapy Analytical Programs for Regulatory ... [https://kincellbio.com/designing-cell-therapy-analytical-programs-for-regulatory-success/]
- 47. A Phase-Appropriate Approach For Assay Validation In ... [https://www.cellandgene.com/doc/a-phase-appropriate-approach-for-assay-validation-in-cell-gene-therapies-0001]
- 48. Designing Phase-Appropriate CMC Analytical Programs [https://www.pharmtech.com/view/designing-phase-appropriate-cmc-analytical-programs]
- 49. Introduction to Analytical Method Development and ... [https://www.labmanager.com/introduction-to-analytical-method-development-and-validation-33922]
- 50. Resolution Therapeutics Announces Regenerative ... [https://resolution-tx.com/resolution-therapeutics-announces-regenerative-macrophage-therapy-rmt-manufacturing-process-candidate-testing-suite-at-asgct-2025/]
- 51. Emerging CAR immunotherapies: broadening therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321946/]
- 52. CAR-T cell therapy for cancer: current challenges and ... [https://www.nature.com/articles/s41392-025-02269-w]
- 53. CD19 -targeted CAR T therapy treating hematologic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1490491/full]
- 54. Comparison of efficacy and adverse effects of CD19/20 ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1582944/full]
- 55. CAR-T therapy-based innovations in the enhancement of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263928/]
- 56. The next innovations in chimeric antigen receptor T cell ... [https://www.sciencedirect.com/science/article/pii/S1465324925007200]
- 57. ISCT 2025 Global Regulatory Perspectives (GRP) ... [https://www.isctglobal.org/telegrafthub/blogs/isct-head-office1/2025/09/10/isct-2025-grp-roundtable-takeaways]
- 58. Differences Between Autologous and Allogeneic Cell ... [https://www.patheon.com/us/en/insights-resources/blog/differences-between-autologous-and-allogeneic-cell-therapies.html]
- 59. Autologous vs. Allogeneic Cell Therapy [https://www.susupport.com/blogs/knowledge/autologous-vs-allogeneic-cell-therapy]
- 60. The Donor Advantage: Why U.S. Starting Materials Are ... [https://biobridgeglobal.org/uncategorized/the-us-donor-advantage-allogeneic-cell-therapy/]
- 61. Selection of Autologous or Allogeneic Transplantation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK12844/]
- 62. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 63. Navigating Regulatory Frameworks For Allogeneic CAR- ... [https://www.cellandgene.com/doc/navigating-regulatory-frameworks-for-allogeneic-car-nk-control-strategies-0001]
- 64. Cell Therapy: Revolutionizing Regenerative Medicine (2025) [https://www.dvcstem.com/post/cell-therapy]
- 65. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 66. Overcoming on-target, off-tumour toxicity of CAR T cell therapy ... [https://pubmed.ncbi.nlm.nih.gov/36418477/]
- 67. Overcoming on-target, off-tumour toxicity of CAR T cell ... [https://www.nature.com/articles/s41571-022-00704-3]
- 68. Strategies to overcome tumour relapse caused by antigen ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02334-6]
- 69. Innovative gene engineering strategies to address tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587523/]
- 70. On-target off-tumor toxicity of claudin18.2-directed CAR-T ... [https://www.nature.com/articles/s41467-025-61858-z]
- 71. Biallelic antigen escape is a mechanism of resistance to ... [https://www.sciencedirect.com/science/article/pii/S0006497125014223]
- 72. The Pitfalls and Promise of Cell and Gene Therapy ... [https://globalforum.diaglobal.org/issue/november-2025/the-pitfalls-and-promise-of-cell-and-gene-therapy-development-a-time-for-concerted-action/]
- 73. Budget blues: where are cell and gene therapies heading? [https://www.labiotech.eu/trends-news/european-cell-gene-therapy-summit-2025-funding-challenges/]
- 74. A roadmap for cost-of-goods planning to guide economic ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324917306254]
- 75. Perspectives on the cost of goods for hPSC banks ... [https://www.nature.com/articles/s41536-022-00242-7]
- 76. Process Development Considerations for Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572896/]
- 77. Process Steps in Cell Therapy Manufacturing [https://www.cellandgene.com/topic/cell-therapy-manufacturing]
- 78. underlying Mechanisms to CAR-T resistance and... cell therapy [https://pubmed.ncbi.nlm.nih.gov/40340171/]
- 79. Potential strategies against resistance to CAR T-cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7576929/]
- 80. CAR-T cell therapy: current limitations and potential ... [https://www.nature.com/articles/s41408-021-00459-7]
- 81. - Multi - antigen chimeric antigen receptor T targeted for cancer... cells [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-019-0813-7]
- 82. Frontiers | Multi CAR-T Targeted for B- Cell ... Therapies Cell [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.00146/full]
- 83. Multi-antigen-targeted chimeric antigen receptor T cells for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6884912/]
- 84. Tandem CAR-T cell therapy: recent advances and current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11907001/]
- 85. Tandem CAR-T cells targeting mesothelin and MUC16 ... [https://pubmed.ncbi.nlm.nih.gov/40930746]
- 86. Cell and Gene Therapy Product Comparability Strategies [https://www.bioprocessintl.com/cell-therapies/comparability-for-cell-and-gene-therapy-products-a-challenge-and-an-opportunity]
- 87. Cell Therapy H1 2025 Landscape Review [https://www.beacon-intelligence.com/landscape-reviews/cell-therapy-landscape-review-h1-2025/]
- 88. Cell and gene therapy: Industry predictions for 2025 [https://www.ddw-online.com/cell-and-gene-therapy-industry-predictions-for-2025-33600-202502/]
- 89. Manufacturing Scalability: Scale Manufacturing Successfully [https://www.netsuite.com/portal/resource/articles/erp/manufacturing-scalability.shtml]
- 90. Mechanism of Action, Potency and Efficacy: Considerations ... [https://www.nist.gov/publications/mechanism-action-potency-and-efficacy-considerations-cell-and-gene-therapies]
- 91. Advancements and challenges in CAR-T cell therapy for solid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374352/]
- 92. Evidence of Lack of Treatment Efficacy Derived From ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10282886/]
- 93. Why 90% of clinical drug development fails and how to ... [https://www.sciencedirect.com/science/article/pii/S2211383522000521]
- 94. Q3 2025 Biopharma Funding: The Market's Waking Up [https://www.linkedin.com/pulse/q3-2025-biopharma-funding-markets-waking-up-only-bill-gadless-sujue]
- 95. What economic or market trends are having the biggest ... [https://www.pharmasalmanac.com/articles/what-economic-or-market-trends-are-having-the-biggest-impact-on-cdmo-capacity-and-pipelines-in-2025-and-what-will-2026-bring]
- 96. 2025 Cell and Gene Therapy Report Looks at Industry ... [https://www.targetedonc.com/view/2025-cell-and-gene-therapy-report-looks-at-industry-challenges-how-to-expand-nationally]
- 97. Computational analyses of mechanism of action (MoA) [https://pmc.ncbi.nlm.nih.gov/articles/PMC8827085/]
- 98. CMC Analytical Control Strategies for Drug Development [https://www.bioagilytix.com/blog/cmc-analytical-control-strategies-for-drug-development/]
- 99. The comparability tales: A phase-appropriate roadmap for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10805933/]
- 100. Potency Assurance for Cellular and Gene Therapy Products [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/potency-assurance-cellular-and-gene-therapy-products]
- 101. Potency assurance for CGT products: an assessment of ... [https://www.parexel.com/insights/blog/potency-assurance-for-cgt-products-an-assessment-of-fdas-new-draft-guidance]
- 102. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 103. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 104. Postapproval Methods to Capture Safety and Efficacy Data [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/postapproval-methods-capture-safety-and-efficacy-data-cell-and-gene-therapy-products]
- 105. Approved Cellular and Gene Therapy Products [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/approved-cellular-and-gene-therapy-products]
- 106. Comparative analysis of cell therapy infusion workflows at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9013238/]
- 107. Overview of methods for comparing the efficacies of drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3895352/]
- 108. Cell and Gene Therapies on the Rise: New Report Reveals ... [https://www.mckesson.com/about-us/newsroom/press-releases/2025/cell-and-gene-therapies-on-the-rise/]
- 109. Autologous Cell Therapy: Types, Benefits & Challenges [https://lifesciences.danaher.com/us/en/library/autologous-cell-therapy-overview.html]
- 110. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 111. Allogeneic CART progress: platforms, current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198129/]
- 112. Allogeneic Cell Therapy - Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/allogeneic-cell-therapy.html]
- 113. Manufacturing Cell and Gene Therapies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961620/]
- 114. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 115. 读书报告|体内CAR-T细胞治疗癌症和自身免疫性疾病 [https://www.medsci.cn/article/show_article.do?id=8858906e2354]
- 116. Classify Your Medical Device [https://www.fda.gov/medical-devices/overview-device-regulation/classify-your-medical-device]
- 117. FDA Medical Device Classification: Class I, II, III Explained ... [https://www.complizen.ai/post/fda-medical-device-classification-complete-guide-to-class-i-ii-iii-devices]
- 118. Recent Final Medical Device Guidance Documents [https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/recent-final-medical-device-guidance-documents]
- 119. Top 5 Upcoming FDA and EU Regulations - MEDIcept [https://www.medicept.com/top-5-upcoming-fda-and-eu-regulations-what-to-know-for-2025/]
- 120. Product-information requirements [https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/product-information-requirements]
- 121. European Union (EU) Mutual Recognition Agreement [https://www.fda.gov/international-programs/international-arrangements/european-union-eu-mutual-recognition-agreement]
- 122. CAR-T细胞疗法攻克R/R T-ALL的创新实践与未来展望 [http://www.liangyihui.net/doc/150070]
- 123. CAR-T细胞疗法研究进展(第47期) [https://news.bioon.com/article/5e078492647b.html]
- 124. Predictive value of preclinical models for CAR-T cell therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12164627/]
- 125. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 126. Blood proteomics for quantitative biomarkers of cellular ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00837-4]
- 127. Researchers find new biomarker for improved ... [https://www.mdanderson.org/newsroom/research-newsroom/researchers-find-new-biomarker-for-improved-immunotherapy-response-in-solid-tumors.h00-159780390.html]
- 128. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 129. News - BrainStorm Cell Therapeutics [https://ir.brainstorm-cell.com/2025-05-06-BrainStorm-to-Present-Biomarker-Insights-Supporting-NurOwns-Mechanism-of-Action-and-Clinical-Impact-at-the-2025-ALS-Drug-Development-Summit]
- 130. Cell Therapy Fundings (2025 YTD): Key Deals and Trends [https://www.biopharmiq.com/post/cell-therapy-fundings-2025]
- 131. Cell Therapy Market Insights & Growth Outlook 2025–2032 [https://www.congruencemarketinsights.com/report/cell-therapy-market]
- 132. U.S. Cell Therapy Market Drives by 21.46% CAGR till 2034 [https://www.towardshealthcare.com/insights/us-cell-therapy-market-sizing]
- 133. Novel Pipeline Activity Signals Hope in Systemic Sclerosis ... [https://www.spherixglobalinsights.com/novel-pipeline-activity-signals-hope-in-systemic-sclerosis-as-rheumatologists-anticipate-first-real-therapeutic-advances-in-years/]
- 134. Analytical considerations for cellular therapy manufacturing [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/448/Analytical-considerations-for-cellular-therapy-manufacturing]