Demonstrating Comparability for Biological Products: A 2025 Guide to Regulatory Strategy, Analytical Methods, and Lifecycle Management
This article provides a comprehensive guide for researchers and drug development professionals on demonstrating comparability for biological products.
Demonstrating Comparability for Biological Products: A 2025 Guide to Regulatory Strategy, Analytical Methods, and Lifecycle Management
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on demonstrating comparability for biological products. Covering foundational principles from ICH Q5E to the latest 2025 regulatory updates from the FDA and EMA, it details a risk-based methodology for analytical, non-clinical, and clinical assessments. The content explores troubleshooting for expedited programs and complex changes, alongside a comparative analysis of biosimilar pathways and global regulatory convergence. By synthesizing current guidelines and expert consensus, this resource aims to equip scientists with the strategies needed to efficiently manage manufacturing changes and biosimilar development, accelerating patient access to vital therapies.
The Foundations of Comparability: From ICH Q5E Principles to the 2025 Regulatory Paradigm Shift
The development and manufacturing of biotechnological/biological products are inherently dynamic, often necessitating process changes throughout the product lifecycle. ICH Q5E provides the foundational framework for assessing the comparability of a product before and after such manufacturing changes, introducing the crucial concept of "highly similar" as the standard for successful demonstration. This whitepaper delves into the technical and regulatory nuances of this standard, explaining that it does not imply identity but rather demands a comprehensive analytical and scientific evaluation to ensure that differences have no adverse impact on the product's quality, safety, or efficacy. Framed within the broader context of demonstrating comparability for biological products research, this guide provides drug development professionals with a detailed examination of the regulatory expectations, a strategic framework for risk-based study design, and specific methodological protocols for key analytical experiments. By synthesizing the principles of ICH Q5E with contemporary industry practices, this document aims to equip scientists with the knowledge to design robust, defensible comparability exercises that facilitate continuous process improvement while ensuring patient safety and regulatory compliance.
The International Council for Harmonisation (ICH) Q5E guideline, titled "Comparability of Biotechnological/Biological Products Subject to Changes in Their Manufacturing Process," is the definitive regulatory document governing how manufacturers should evaluate changes to the manufacturing process of biological products [1] [2]. Its primary objective is to assist in the collection of relevant technical information that serves as evidence that a manufacturing process change will not adversely impact the quality, safety, and efficacy of the drug product [3]. The guideline emphasizes that the focus of the assessment should be primarily on quality aspects, and it does not prescribe a one-size-fits-all analytical, nonclinical, or clinical strategy [2].
Central to the ICH Q5E philosophy is the concept of "highly similar." This is a critical distinction from "identical," acknowledging the inherent complexity and natural variability of biological products. A biotechnological product is considered "highly similar" to its pre-change counterpart when the observed differences in quality attributes are thoroughly evaluated and scientifically justified as having no adverse impact on safety or efficacy [4]. This means that the product's safety, identification, purity, and activity should be highly similar and fully predictable based on existing knowledge [5]. The goal of the comparability exercise is therefore not to prove that the two products are exactly the same, but to ascertain that they are sufficiently comparable to ensure that the existing data on safety and efficacy remains valid for the post-change product [6] [4]. When a thorough analytical comparison can robustly demonstrate this "highly similar" state and link it to the clinical experience, additional non-clinical or clinical studies may be unnecessary [7].
The Scientific and Regulatory Foundation of "Highly Similar"
The Role of Product and Process Understanding
Demonstrating that a product is "highly similar" after a manufacturing change is fundamentally predicated on a deep and comprehensive understanding of the product and its manufacturing process. Biotechnological products are highly complex and are defined by their manufacturing process, a concept often summarized as "the product is the process" [6]. This complexity means that any process change has the potential to affect the product. A well-designed comparability exercise should therefore be capable of detecting discrete differences in selected quality attributes. Regulators expect that some differences will be revealed through modern, sensitive analytical techniques; the key scientific question is not whether any difference exists, but whether the observed differences are meaningful and could negatively impact safety or efficacy [6].
The foundation for this assessment is a well-defined list of Product Quality Attributes (PQAs), which are physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality [6]. Among these, Critical Quality Attributes (CQAs) are those PQAs that have a direct link to safety and efficacy. A robust risk-management process, as outlined in ICH Q9, is used to determine the criticality of each attribute [6] [4]. This product knowledge, accumulated throughout development, is essential for designing a focused and effective comparability study, as it allows the development team to predict which attributes are most likely to be affected by a specific process change.
The Hierarchy of Evidence and Regulatory Flexibility
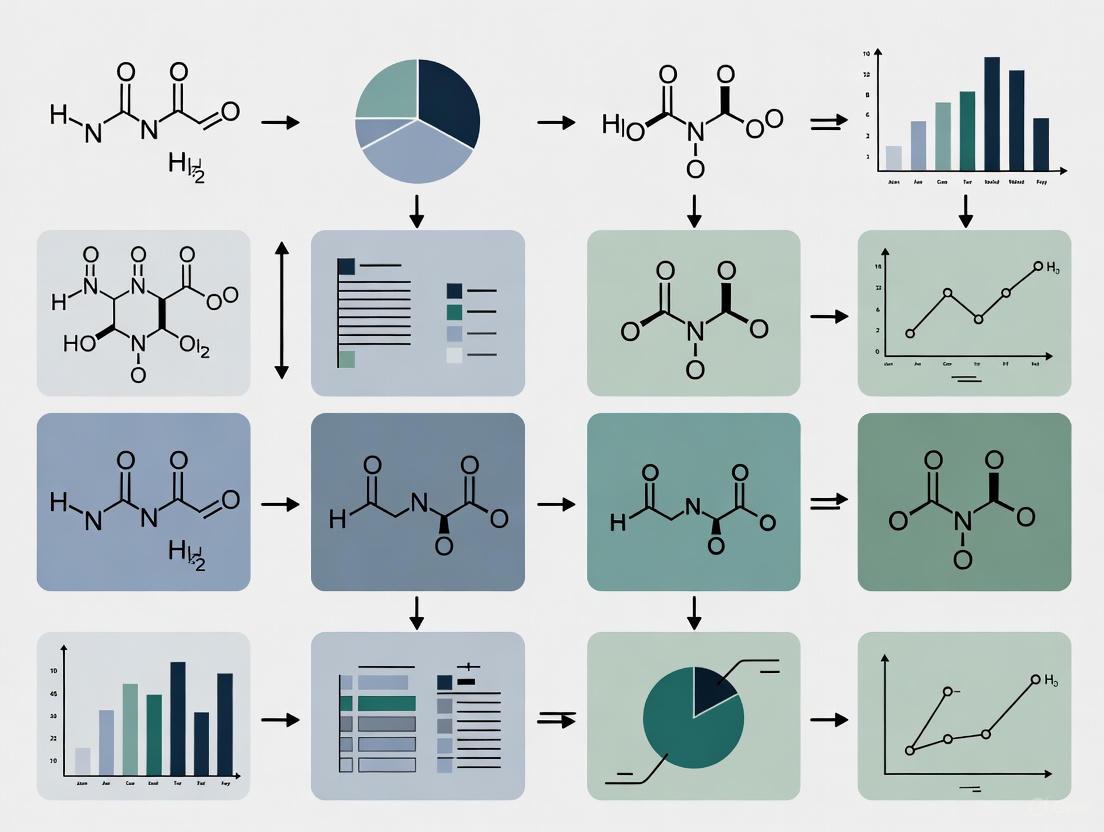
ICH Q5E establishes a hierarchical approach to demonstrating comparability, with analytical studies forming the cornerstone of the assessment [4]. The guideline envisions a stepwise progression of evidence gathering, as illustrated in the diagram below.
Diagram 1: The hierarchical, stepwise approach to demonstrating comparability, starting with analytical studies, as endorsed by ICH Q5E.
As shown, a comprehensive analytical comparability exercise is always the first and most critical step. If this analytical demonstration is successful in proving the products are "highly similar," then the comparability exercise can be considered complete without further non-clinical or clinical studies [7] [4]. However, if uncertainty remains after the analytical comparison, or if a difference with potential clinical impact is identified, the manufacturer may need to progress to non-clinical or clinical bridging studies to resolve the uncertainty and establish a link to the existing safety and efficacy data [6] [5]. The level of evidence required is also phase-appropriate; the extent of the comparability exercise should align with the stage of product development, with more comprehensive data expected for products in or near the marketing application stage compared to those in early clinical development [4].
Designing a Risk-Based Comparability Study
The Comparability Protocol: A Prospectively Written Plan
A cornerstone of a successful comparability exercise is the Comparability Protocol (CP), known in the EU as a Post-Approval Change Management Protocol (PACMP) [7]. This is a comprehensive, prospectively written plan that outlines how the effect of a proposed change will be assessed [7]. Drafting the protocol should be initiated approximately six months before the manufacture of the post-change batch(es) and must be finalized before testing begins [6]. Submitting a CP for regulatory feedback prior to execution can de-risk the entire process, as it ensures alignment with regulatory authorities on the study design, analytical methods, and acceptance criteria. A key advantage is that meeting all predefined criteria in an approved protocol can allow for faster implementation of the change post-approval [7] [4].
A well-structured Comparability Protocol typically includes the following elements [6]:
- A detailed description and rationale for the process change(s).
- A risk-based impact assessment identifying potentially affected Product Quality Attributes (PQAs).
- A detailed analytical testing plan, including specified methods and sample types.
- Predefined acceptance criteria for the comparability study.
- A plan for stability studies, if required.
- A description of all available supportive historical data.
Risk Assessment and Impact Analysis
A critical early step in designing the study is to conduct a systematic risk assessment to identify which product quality attributes are most likely to be impacted by the specific manufacturing change. This involves a cross-functional team with representatives from analytical, process development, non-clinical, and regulatory affairs [6]. The team uses a structured template to link each process change to potentially affected PQAs, providing a scientific rationale for the potential impact.
Table 1: Risk Assessment Template for Linking Process Changes to Quality Attributes
| Process Change | Potentially Affected PQA | Rationale for Potential Impact | Recommended Analytical Method |
|---|---|---|---|
| Upstream Scale-Up | Glycosylation Profile | Alterations in cell culture conditions (shear stress, nutrient gradients) can affect glycosylation. | Oligosaccharide profiling (HPLC/UPLC) |
| Purification Resin Change | Charge Variants | Differences in ligand chemistry and separation mechanism may selectively remove certain charge species. | cIEF or CEX-HPLC |
| Cell Line Change | Primary Structure | A new clone may have different sequence variants or post-translational modification tendencies. | Peptide Mapping (LC-MS) |
| Drug Product Formulation Change | Higher-Order Structure & Aggregation | Changes in excipients or pH can destabilize the protein structure. | SEC-HPLC, DSC, CD Spectroscopy |
This risk assessment directly informs the scope and depth of the analytical testing plan, ensuring that resources are focused on monitoring the attributes that matter most for the specific change, thereby making the study both efficient and scientifically defensible [6] [4].
Batch Selection and Study Design
The number of batches selected for a comparability study depends on the product's development stage and the magnitude of the change. For major changes to marketed products, ≥3 batches of commercial-scale post-change material are generally recommended [5]. These are compared against historical data from multiple pre-change batches. An optimized study design leverages routine lot release and stability testing data generated for the post-change batches and compares them statistically to the historical data of all pre-change batches, rather than retesting a limited number of pre-change batches side-by-side [7]. This approach compares the post-change product against the manufacturer's entire experience with the pre-change process, providing a more robust assessment.
The following workflow outlines the key stages of a comparability exercise, from initial preparation to final reporting.
Diagram 2: The key stages of a comparability exercise, from foundational preparation through to final reporting.
Quantitative Standards and Analytical Methodologies
Defining Acceptance Criteria
A fundamental principle of ICH Q5E is the establishment of prospective acceptance criteria [6]. These criteria, defined before testing the post-change batches, are the objective standards against which comparability will be judged. It is important to note that these acceptance criteria are not necessarily the same as the routine quality standards for batch release. They should be set based on historical data from the pre-change process, taking into account the variability of the analytical methods and the observed range of the quality attributes [7] [5]. The criteria can be quantitative (e.g., a statistical range for a potency assay) or qualitative (e.g., comparable peak shapes in a chromatogram) [5].
Table 2: Examples of Acceptance Criteria for Common Analytical Tests
| Test Type | Specific Analysis | Example Acceptance Standards |
|---|---|---|
| Routine Release | SEC-HPLC for Aggregates | Meets release criteria; percentage of main peak (monomer) within a statistical range (e.g., ETTI) based on historical data; comparable elution profiles. |
| Peptide Map | Meets release criteria; comparable peak shapes based on retention time and relative intensity; no new or lost peaks. | |
| Cell-Based Potency Assay | Meets release criteria; relative potency within a predefined statistical acceptance range based on historical data. | |
| Extended Characterization | Intact Mass (LC-MS) | Molecular weight within the instrument's accuracy range; same species detected. |
| Circular Dichroism (CD) | No significant qualitative differences in the spectra; quantitative analysis shows comparable conformational ratios. | |
| Stability | Real-time Stability | Degradation rates for key attributes (e.g., potency, purity) are equivalent to or slower than the historical average of pre-change batches. |
The Scientist's Toolkit: Key Analytical Techniques for Demonstrating "Highly Similar"
A multi-tiered analytical strategy is employed, leveraging methods from routine release, extended characterization, and stability testing. The following table details key reagent solutions and analytical methodologies essential for a comprehensive comparability study.
Table 3: Research Reagent Solutions and Key Analytical Methods for Comparability
| Analytical Category | Technique / Reagent | Primary Function in Comparability |
|---|---|---|
| Primary Structure | Peptide Mapping (LC-MS) with Trypsin | Confirms amino acid sequence and identifies post-translational modifications (e.g., oxidations, deamidations) by comparing peptide fingerprints. |
| Intact and Reduced Mass Spectrometry | Verifies correct molecular weight and detects mass variants. | |
| Higher-Order Structure | Circular Dichroism (CD) Spectroscopy | Probes secondary (far-UV) and tertiary (near-UV) structure to ensure conformational integrity. |
| Differential Scanning Calorimetry (DSC) | Measures thermal stability and unfolding profiles, indicating overall structural robustness. | |
| Charge Variants | capillary Isoelectric Focusing (cIEF) / Cation-Exchange Chromatography (CEX-HPLC) | Separates and quantifies charge variants (e.g., acidic and basic species) which can impact activity and stability. |
| Purity & Impurities | Size-Exclusion Chromatography (SEC-HPLC) | Quantifies soluble aggregates and fragments. |
| CE-SDS (reduced and non-reduced) | Provides high-resolution separation and quantification of size variants, including fragments and non-glycosylated heavy chain. | |
| Glycosylation | Oligosaccharide Profiling (HPLC/UPLC) | Characterizes the glycan distribution, a CQA for many biologics that can affect efficacy (e.g., ADCC) and safety. |
| Functionality | Cell-Based Bioassays | Measures the biological potency of the product by assessing its mechanism-of-action (MoA)-relevant activity. |
| Surface Plasmon Resonance (SPR) | Quantifies binding affinity (KD) to relevant targets and receptors. | |
| Process-Related Impurities | ELISA Kits (HCP, Protein A) | Quantifies residual host cell proteins and leached Protein A from chromatography resins. |
The strategy should prioritize quantitative methods and employ orthogonal methods (multiple methods that measure the same attribute through different physical principles) for quality attributes that are closely linked to function, such as higher-order structure and glycosylation [6]. The methods must be fit-for-purpose, meaning they have been shown to be capable of reliably detecting differences that might be expected from the specific manufacturing change [7].
Experimental Protocols for Key Analytical Methods
Protocol for Peptide Mapping with LC-MS for Primary Structure Analysis
Objective: To confirm the amino acid sequence and identify post-translational modifications (PTMs) in the post-change product compared to the pre-change reference.
Methodology:
- Denaturation, Reduction, and Alkylation: Dilute the protein sample to a target concentration (e.g., 1 mg/mL) in a denaturing buffer (e.g., 6 M Guanidine HCl). Reduce disulfide bonds using dithiothreitol (DTT) or tris(2-carboxyethyl)phosphine (TCEP). Alkylate the free thiols with iodoacetamide or iodoacetic acid to prevent reformation.
- Digestion: Desalt the protein using a buffer exchange cartridge or dialysis into a digestion-compatible buffer (e.g., 50 mM Tris-HCl, pH 8.0). Add a proteolytic enzyme, typically trypsin, at an enzyme-to-substrate ratio of 1:20 to 1:50 (w/w). Incubate at 37°C for 4-18 hours.
- LC-MS Analysis: Separate the resulting peptides using reversed-phase U/HPLC on a C18 column with a water-acetonitrile gradient (0.1% Formic Acid as modifier). Couple the HPLC system to a high-resolution mass spectrometer (e.g., Q-TOF, Orbitrap).
- Data Processing and Comparison: Use software to deconvolute the MS data and identify peptides based on their measured mass and MS/MS fragmentation patterns. Compare the resulting peptide maps of the pre- and post-change samples. Key comparability endpoints include:
- Retention Time and Peak Area: The chromatographic profile should be highly similar.
- Sequence Coverage: Should be ≥95% and identical between samples.
- PTM Identification and Quantification: The type and level of PTMs (e.g., oxidation of Met, deamidation of Asn/Gln) should be within the historical range or predefined acceptance criteria.
Protocol for Monitoring Higher-Order Structure by Circular Dichroism (CD) Spectroscopy
Objective: To assess the secondary and tertiary structure of the protein and ensure no significant conformational changes have occurred due to the process change.
Methodology:
- Sample Preparation: Dialyze or dilute the protein into a CD-compatible buffer (e.g., phosphate buffer). Avoid buffers with high absorbance in the far-UV region (e.g., citrate, Tris). Determine the exact protein concentration using a UV spectrophotometer (A280 measurement).
- Far-UV CD (Secondary Structure): Load the sample into a quartz cuvette with a short path length (e.g., 0.1 cm). Record the spectrum from 180-260 nm. Perform multiple scans and average them to improve the signal-to-noise ratio. Subtract the buffer blank spectrum.
- Near-UV CD (Tertiary Structure): Use a higher protein concentration and a cuvette with a longer path length (e.g., 1 cm). Record the spectrum from 250-350 nm.
- Data Analysis and Comparability Assessment: Visually overlay the spectra of the pre- and post-change samples. For a more quantitative assessment, use algorithms to deconvolute the far-UV spectrum and estimate the percentages of α-helix, β-sheet, and random coil. The conclusion of "highly similar" is supported by:
- No significant shifts in the peak positions (wavelength) for both far- and near-UV spectra.
- Comparable mean residue ellipticity values at key peaks and troughs.
- A comparable calculated secondary structure composition.
Protocol for Stability Study Comparison
Objective: To demonstrate that the degradation pathways and kinetics of the post-change product are comparable to the pre-change product.
Methodology:
- Study Design: Place a minimum of three post-change batches and, if available for side-by-side testing, three pre-change batches on stability under recommended storage conditions (e.g., 5°C ± 3°C) and accelerated conditions (e.g., 25°C/60%RH). For supportive data, forced degradation studies (e.g., exposure to elevated temperature, light, oxidants) can be performed.
- Testing Time Points: Test at initial (T=0), 3, 6, 9, 12, 18, 24, and 36 months for real-time studies. Accelerated studies may have more frequent time points (e.g., 1, 2, 3, 6 months).
- Test Attributes: Monitor CQAs that are known to be stability-indicating, such as:
- Purity: SEC-HPLC (aggregates), CE-SDS (fragmentation), CEX/cIEF (charge variants).
- Potency: Cell-based bioassay.
- Activity: Binding affinity assays.
- Data Evaluation: Plot the degradation trends for each attribute over time. Statistically compare the degradation rates (slopes) of the post-change batches to the historical data from pre-change batches. The products are considered comparable in stability if:
- The degradation pathways are the same (no new degradation products appear).
- The degradation rates for key attributes are statistically equivalent to or slower than those of the pre-change product.
The "highly similar" standard articulated in ICH Q5E represents a pragmatic and scientifically rigorous framework for managing the inevitable evolution of biological manufacturing processes. It acknowledges the complexity of these products while demanding a level of evidence sufficient to ensure that process changes do not adversely affect patient safety or product efficacy. Successfully navigating this standard requires more than just routine testing; it demands a deep, proactive product and process understanding, a risk-based strategy for study design, and the skillful application of a broad panel of sophisticated analytical techniques. By embracing the principles outlined in this whitepaper—developing a comprehensive comparability protocol, conducting a systematic risk assessment, setting scientifically justified acceptance criteria, and employing fit-for-purpose analytical methods—drug development professionals can build robust, defensible comparability packages. This approach not only fulfills regulatory expectations but also fosters a culture of continuous improvement, ultimately enabling the delivery of high-quality, innovative biological therapies to patients in an efficient and reliable manner.
The 1996 FDA Guidance, "Demonstration of Comparability of Human Biological Products, Including Therapeutic Biotechnology-derived Products," established the foundational principle that biological products could be scientifically evaluated after manufacturing changes without necessarily repeating clinical efficacy studies [8]. This document represented a significant shift in regulatory philosophy, acknowledging that as characterization methods improved, biological products could be increasingly defined by their specific attributes rather than solely by their manufacturing process. The guidance provided a structured framework for demonstrating that pre-change and post-change products remained comparable in safety, identity, purity, and potency through rigorous analytical, functional, and sometimes preclinical testing [8]. This evolution from a purely process-based definition to an attribute-based understanding of biological products has enabled manufacturers to implement important improvements in product quality, yield, and manufacturing efficiency while maintaining regulatory compliance.
Over the past three decades, this conceptual framework has evolved substantially through international harmonization and adaptation to novel therapeutic modalities. The comparability concept has expanded from addressing relatively straightforward manufacturing changes to encompassing complex scenarios including the demonstration of biosimilarity and the evaluation of innovative platform technologies for personalized therapies. This article examines the trajectory of regulatory thinking from the seminal 1996 guidance through the recent updates and novel pathways announced in 2025, providing researchers and drug development professionals with both historical context and practical methodologies for navigating the current regulatory landscape for biological products.
The 1996 Guidance: A Foundational Framework
Core Principles and Regulatory Context
Issued in April 1996, the FDA's guidance on comparability represented a pivotal moment in the regulation of biological products. Historically, these products were regarded as complex mixtures that were difficult to characterize as individual entities, leading to a regulatory framework where the manufacturing process itself defined the product [8]. This perspective was reflected in the establishment license application (ELA) requirement for biologics, which acknowledged that changes in manufacturing could fundamentally alter the product itself. The 1996 guidance acknowledged that scientific advancements in production methods, process controls, and characterization techniques had evolved sufficiently to allow for a more nuanced approach [8]. It explicitly stated that manufacturers could implement manufacturing changes without additional clinical studies if they could demonstrate "product comparability" between the pre-change and post-change product through rigorous analytical and functional testing.
The guidance established that FDA would determine comparability based on whether manufacturing changes affected the safety, identity, purity, or potency of the biological product [8]. This represented a significant regulatory flexibility initiative, allowing manufacturers to bring improved products to market more efficiently while maintaining appropriate safeguards for product quality. The document emphasized that this approach applied to both products regulated by the Center for Biologics Evaluation and Research (CBER) and therapeutic biotechnology-derived products regulated by the Center for Drug Evaluation and Research (CDER) [8]. Importantly, the guidance clarified that it represented the FDA's current thinking on demonstration of product comparability but did not set forth binding requirements, allowing for alternative approaches with prior FDA discussion.
Structured Approach to Comparability Testing
The 1996 guidance outlined a comprehensive, scientifically-grounded approach to comparability assessment that emphasized knowledge of the manufacturing process as integral to designing an appropriate testing program [8]. The recommended testing strategy typically progressed from analytical characterization to biological assays, and when necessary, to preclinical and clinical evaluation, though the approach was not strictly hierarchical. The guidance recognized that different tests often provided complementary information, and that understanding the extent of manufacturing changes and their stage of implementation was crucial for designing an appropriate assessment program [8].
Manufacturers were advised to provide extensive side-by-side analyses of the pre-change and post-change products, using well-characterized reference standards when available [8]. The testing strategy incorporated both routine release assays and additional tests specifically designed to evaluate the impact of the particular manufacturing change. The guidance specifically highlighted several categories of critical assessment methods:
- Analytical Testing: Comprehensive chemical and physical characterization to identify similarities and differences between products [8]
- Bioassays: In vitro or in vivo assessments of biological activity that reflect the product's mechanism of action [8]
- Preclinical Animal Studies: Evaluations of pharmacokinetics, pharmacodynamics, and potential toxicity in relevant animal models [8]
- Clinical Studies: Assessments of human pharmacokinetics, pharmacodynamics, safety, and efficacy when needed [8]
The guidance emphasized that the most important consideration was whether any observed differences would translate into significant changes in clinical safety or efficacy, with the overall goal of determining whether additional clinical studies were necessary [8].
The Evolution to ICH Q5E: International Harmonization
Refinement of Scientific Principles
The International Council for Harmonisation (ICH) Q5E guideline, issued in June 2005, represented the next major evolution in comparability thinking by providing an internationally harmonized framework for assessing comparability of biotechnological/biological products after manufacturing changes [2]. Building upon the foundation established in the 1996 FDA guidance, Q5E more explicitly articulated the scientific principles underlying comparability assessment and provided greater detail on the technical considerations for demonstrating that manufacturing changes do not adversely affect product quality, safety, and efficacy. The guideline emphasized that the overall goal of comparability exercise is to ensure the quality, safety, and efficacy of drug product produced by a changed manufacturing process, through collection and assessment of relevant data [2].
A significant advancement in Q5E was its more detailed discussion of the risk-based approach to comparability assessment, considering factors such as the extent of the manufacturing change, the stage of product development, and the relationship between quality attributes and safety and efficacy. The guideline also provided more specific guidance on the types of analytical studies needed, including assessments of product quality attributes such as physicochemical properties, biological activity, immunochemical properties, purity, and impurities [2]. While the 1996 FDA guidance had established the basic framework for comparability assessment, Q5E refined these concepts through international scientific consensus and reflected the accumulated experience with implementing comparability assessments across a range of biotechnology products.
Continued Relevance in Modern Context
Despite being issued nearly two decades ago, the ICH Q5E guideline remains the primary international standard for comparability assessment of biotechnology products, demonstrating the enduring relevance of its scientific principles [2]. The guideline's flexible, risk-based approach has proven adaptable to increasingly complex products and manufacturing technologies. Q5E established the important principle that comparability does not necessarily mean that the pre-change and post-change products are identical, but rather that they are highly similar and that any observed differences have no adverse impact on quality, safety, or efficacy [2].
The guideline also acknowledged that the amount and type of data needed to demonstrate comparability depends on the stage of product development, the scope of the manufacturing change, and the understanding of the product and its relationship to clinical outcomes. This nuanced approach has allowed the Q5E framework to remain applicable even as product complexity has increased, including for advanced therapy medicinal products such as cell and gene therapies. The enduring implementation of Q5E principles in regulatory practice worldwide demonstrates the success of this harmonized approach to maintaining product quality while enabling manufacturing innovation and improvement.
The 2025 Landscape: Novel Pathways and Updated Frameworks
The "Plausible Mechanism" Pathway for Personalized Therapies
A landmark development in 2025 has been the proposal of a novel regulatory approach termed the "plausible mechanism" (PM) pathway by FDA Commissioner Martin Makary and CBER Director Vinay Prasad [9]. This pathway aims to address unique challenges in the development of bespoke, personalized therapies, particularly in cases where traditional randomized trials are not feasible or practical. The PM pathway is structured as a phased operational model that begins with treating consecutive patients with personalized therapies, with the potential to progress toward marketing authorization after demonstrating success across several patients [9].
The FDA has outlined five key characteristics defining eligibility for the PM pathway:
- Identification of specific abnormality: A known and clear molecular or cellular abnormality with a direct causal link to the disease [9]
- Targeting underlying alteration: Interventions that directly target the proximate biological alteration rather than acting broadly on affected systems [9]
- Use of natural history data: Well-characterized natural history data for the disease in untreated populations [9]
- Evidence of target engagement: Confirmatory evidence showing successful targeting or editing of the intended biological target [9]
- Demonstration of clinical improvement: Evidence of durable improvements in clinical outcomes consistent with disease biology [9]
This pathway represents a significant regulatory innovation specifically designed for personalized therapies, particularly in the rare disease space where traditional development pathways face substantial practical and ethical challenges [9].
2025 Guidance Agenda and Policy Updates
The FDA's Center for Biologics Evaluation and Research (CBER) has released an ambitious 2025 guidance agenda that includes multiple documents addressing contemporary challenges in biological product development [10]. The agenda reflects continued regulatory evolution across several key product areas, with particular emphasis on cell and gene therapies and advanced blood products. Notable planned guidances include:
Table: Selected 2025 CBER Guidance Agenda Items
| Product Category | Guidance Title | Focus Area | Status |
|---|---|---|---|
| Therapeutic Products | Potency Assurance for Cellular and Gene Therapy Products | Quality assessment for advanced therapies | New in 2025 |
| Therapeutic Products | Post Approval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products | Post-market evidence generation | New in 2025 |
| Blood and Blood Components | Recommendations for Evaluation of Devices Using Non-DEHP Materials | Safety of alternative materials | New in 2025 |
| Other | Recommendations for Validation and Implementation of Alternative Microbial Methods | Modernized testing approaches | New in 2025 |
Additionally, the FDA has been active in 2025 with safety communications and regulatory actions reflecting the ongoing lifecycle management of biological products [11] [12]. These include investigations into adverse events associated with specific products, new boxed warnings, and labeling changes based on emerging post-market safety data [12]. These actions demonstrate the continued emphasis on post-market surveillance and the application of a lifecycle approach to biological product regulation, consistent with the principles established in the original 1996 comparability guidance but adapted to contemporary products and risks.
Comparative Analysis: Evolution of Key Concepts
Changing Standards for Evidence
The evolution from the 1996 comparability guidance to the 2025 regulatory landscape reveals significant shifts in the types of evidence accepted for regulatory decision-making. The 1996 guidance established a primarily quality-focused approach to comparability, with progression to clinical studies only when analytical and preclinical data were insufficient to demonstrate comparability [8]. The 2005 ICH Q5E guideline reinforced this approach while providing greater international harmonization and detail on quality attribute assessment [2]. In contrast, the 2025 "plausible mechanism" pathway introduces greater flexibility in the evidence requirements for initial authorization, particularly for personalized therapies targeting rare diseases with high unmet need [9].
This evolution reflects a more nuanced understanding of the relationship between evidence types and regulatory decision-making contexts. While the fundamental principle of using the least burdensome approach to generate necessary evidence remains constant, the specific applications have expanded to address new product categories and development challenges. The table below illustrates key comparative aspects:
Table: Evolution of Key Regulatory Concepts from 1996 to 2025
| Aspect | 1996 Guidance | ICH Q5E (2005) | 2025 Updates |
|---|---|---|---|
| Primary Focus | Manufacturing changes for established biologicals | Manufacturing changes for biotechnological products | Personalized therapies, rare diseases |
| Evidence Hierarchy | Analytical → Biological → Preclinical → Clinical | Quality → Nonclinical → Clinical (when needed) | Natural history → Target engagement → Clinical improvement |
| Clinical Data Requirements | Possibly waived with sufficient analytical data | Based on risk and product knowledge | May leverage real-world evidence and expanded access data |
| Post-Marketing Evidence | Not explicitly addressed | Mentioned for unresolved questions | Explicit requirement for ongoing data collection |
| Applicable Products | Human biologicals, therapeutic biotechnology products | Biotechnological/biological products | Cell and gene therapies, personalized interventions |
Adaptation to Novel Product Categories
The regulatory framework has demonstrated remarkable adaptability to new technologies over the past three decades. The 1996 guidance primarily addressed traditional biological products and therapeutic biotechnology-derived products [8], while the 2025 regulatory agenda explicitly encompasses cell and gene therapies, personalized treatments, and novel vaccine technologies [9] [10]. This expansion has required evolving approaches to fundamental concepts such as product characterization, potency assessment, and comparability demonstration.
For particularly challenging product categories such as cell-based therapies where full analytical characterization may be limited, the regulatory approach has evolved to incorporate additional elements such as functional potency assays, process validation, and in some cases, clinical data as part of the comparability assessment [10]. The 2025 guidance agenda includes specific documents addressing "Potency Assurance for Cellular and Gene Therapy Products" and "Post Approval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products," reflecting the continued evolution of regulatory thinking for these advanced modalities [10].
Practical Implementation: Methodologies and Protocols
Experimental Design for Comparability Studies
Designing appropriate comparability studies requires careful consideration of the manufacturing change, product understanding, and relationship of quality attributes to clinical performance. The foundational approach from the 1996 guidance remains relevant: manufacturers should conduct side-by-side analyses of multiple pre-change and post-change lots using orthogonal analytical methods [8]. The experimental design should adequately power studies to detect clinically relevant differences, with statistical approaches appropriate for the analytical methodology being used.
For analytical comparability, a tiered approach is often employed where quality attributes are categorized based on their potential impact on safety and efficacy. Critical quality attributes that potentially impact clinical performance warrant more rigorous assessment with predefined acceptance criteria [8] [2]. The 1996 guidance emphasized that tests should include those routinely used for product release plus additional methods specifically designed to evaluate the impact of the specific manufacturing change, particularly focusing on manufacturing steps most likely affected by the change [8].
Advanced Methodologies for Novel Products
For complex biological products including cell and gene therapies, demonstrating comparability often requires specialized methodologies beyond conventional analytical approaches. The 2025 guidance agenda indicates continued attention to "Potency Assurance for Cellular and Gene Therapy Products," recognizing the unique challenges these products present [10]. Methodologies may include:
- Multi-parameter flow cytometry for cell surface marker characterization
- Next-generation sequencing approaches to evaluate genetic stability or vector integration sites
- Functional potency assays that measure biologically relevant responses
- Molecular characterization techniques to assess critical quality attributes
For products following the "plausible mechanism" pathway, methodologies to demonstrate target engagement become particularly important, potentially including biopsy assessments, molecular imaging, or biomarker evaluations [9]. The evidence of successful target editing or engagement may come from animal models, non-animal models, or clinical biopsies, with FDA potentially accepting evidence from a subset of patients or even the first-in-class subject dosed in certain cases [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing comparability assessments for biological products requires specialized reagents and materials that enable comprehensive characterization. The following table details key research solutions and their applications in comparability studies:
Table: Essential Research Reagent Solutions for Comparability Assessment
| Reagent/Material | Function in Comparability Assessment | Application Examples |
|---|---|---|
| Reference Standards | Serve as benchmarks for side-by-side comparison of pre- and post-change products [8] | Quality attribute testing, bioassay normalization, method qualification |
| Characterized Cell Lines | Enable performance of relevant bioassays that reflect mechanism of action [8] | Potency assays, receptor binding studies, functional activity assessments |
| Quality-Characterized Antibodies | Facilitate specific detection and quantification of product and process-related impurities [8] | Immunoassays, Western blotting, impurity detection, host cell protein assays |
| Validated Assay Kits | Provide standardized approaches for critical quality attribute assessment | Glycan analysis, residual DNA quantification, endotoxin testing |
| Process-Related Impurity Standards | Allow detection and quantification of manufacturing process residuals | Host cell protein standards, chromatography resin leachables, antibiotic residues |
Regulatory Workflows: From Traditional Comparability to Novel Pathways
The following diagram illustrates the evolution of regulatory decision-making from the traditional comparability assessment to the novel plausible mechanism pathway:
The evolution of regulatory thinking from the 1996 comparability guidance to the 2025 updates demonstrates a consistent trajectory toward more nuanced, science-based approaches that balance innovation with appropriate regulatory oversight. The fundamental principle established in 1996—that manufacturing changes could be assessed through rigorous scientific evaluation without necessarily requiring additional clinical studies—has proven remarkably durable and adaptable [8]. This framework has expanded through international harmonization in ICH Q5E [2] and continues to evolve to address novel product categories and development challenges.
The 2025 regulatory landscape introduces important innovations, particularly the "plausible mechanism" pathway for personalized therapies [9] and updated guidance addressing contemporary challenges in cell and gene therapy development [10]. These developments reflect both continuity with established principles and adaptation to new scientific opportunities. For researchers and drug development professionals, understanding this evolutionary trajectory provides valuable context for navigating current regulatory expectations and anticipating future directions. The consistent theme across this nearly 30-year evolution is the commitment to scientific rigor coupled with appropriate regulatory flexibility, enabling continued innovation in biological products while maintaining standards for quality, safety, and efficacy.
The development and manufacturing of complex biological drugs operate on a fundamental principle distinct from traditional pharmaceuticals: the manufacturing process defines the product's inherent characteristics. For biologic drugs, which are large, complex molecules produced by living cells, the production process is inextricably linked to the final product's quality, efficacy, and safety. This whitepaper explores the scientific and regulatory foundations of this principle, detailing how process control, advanced analytics, and rigorous comparability exercises ensure that biologic products, including biosimilars, consistently meet their critical quality profiles.
Biological drugs, or biologics, represent a revolutionary class of therapeutics derived from living organisms. Unlike small-molecule drugs—which are simple, chemically synthesized compounds with well-defined structures—biologics are large, complex molecules, such as monoclonal antibodies, fusion proteins, and antibody-drug conjugates [13] [14]. A single monoclonal antibody can consist of over 25,000 atoms, making it orders of magnitude more complex than a drug like aspirin, which comprises only 21 atoms [14].
This structural complexity leads to an intrinsic challenge: inherent variability. Because biologics are produced by living cells in a multistep manufacturing process, they are impossible to replicate identically, even between batches of the same originator product [13] [14]. The living cell expression system imprints distinct post-translational modifications (PTMs), such as glycosylation, phosphorylation, and deamidation, which can generate millions of molecular variants of a single biologic [13]. These PTMs are not merely structural details; they can directly impact the biologic's clinical properties, including its potency, stability, pharmacokinetics, and immunogenicity [13]. Consequently, the biological activity of a therapeutic protein is defined not only by its amino acid sequence but also by the cell-based manufacturing process used to produce it [13].
The Scientific Foundation: How Process Defines Product
Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs)
The "process defines the product" paradigm is operationalized through the framework of Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs).
- CQAs are physical, chemical, biological, or microbiological properties that must be controlled within an appropriate limit, range, or distribution to ensure the desired product quality. They are the characteristics that have a direct impact on the product's efficacy or safety [13]. For a monoclonal antibody, dozens of CQAs may exist.
- CPPs are process parameters whose variability impacts CQAs and therefore must be monitored or controlled to ensure the process produces the desired product quality [15] [16].
The relationship is direct: controlling CPPs within predefined ranges ensures that CQAs remain within their specified limits. Table 1 summarizes key CQAs for a monoclonal antibody and their potential clinical impact.
Table 1: Critical Quality Attributes (CQAs) of a Monoclonal Antibody and Their Clinical Impact
| Attribute Category | Specific CQA | Potential Impact on Efficacy/Safety |
|---|---|---|
| Structure | High-order structure, Disulfide bonds, Aggregates | Impacts potency; higher aggregates can lead to immunogenicity [13] |
| Charge Heterogeneity | Acidic/Basic forms, Deamidation, Oxidation | Can negatively impact potency [13] |
| Glycosylation Profile | Fucosylation, Mannosylation, Sialylation, Galactosylation | Alters effector functions (e.g., ADCC), pharmacokinetics (half-life), and can elicit immunogenic response [13] |
| Biological Activity | Binding to Fcγ receptors, FcRn affinity, ADCC, CDC | Directly impacts mechanism of action and pharmacokinetics [13] |
| Process Impurities | Host cell proteins, Protein A leachate, Host cell DNA | Can be toxic or elicit immunogenic response [13] |
The manufacturing process for biologics is a primary source of variability, influencing CQAs in two key areas:
- Upstream Process (Cell Culture): The conditions in the bioreactor—such as temperature, pH, nutrient levels, and dissolved gases—can significantly impact cell health and the PTMs of the expressed protein [13] [16]. For instance, subtle changes can induce protein aggregation or alter glycosylation patterns, which in turn affect safety and efficacy [13].
- Downstream Process (Purification and Formulation): Unit operations like Ultrafiltration/Diafiltration (UF/DF) are critical for concentrating the protein and exchanging it into the final formulation buffer. Inadequate control here can lead to inconsistencies in protein concentration or excipient levels, impacting the final drug substance [17].
The following diagram illustrates how the manufacturing process flow determines the final product quality through its impact on CQAs.
Diagram 1: The process-to-product relationship, showing how manufacturing steps influence CPPs, which in turn control CQAs to define final product quality.
Analytical and Experimental Methodologies for Process Control
Demonstrating control over the process requires a suite of advanced analytical technologies. The following experimental protocols and tools are essential for characterizing CQAs and monitoring CPPs.
Protocol 1: In-line Monitoring of Downstream UF/DF Using PAT
Objective: To monitor in real-time the concentration of the therapeutic protein and key excipients (e.g., trehalose) during the critical Ultrafiltration/Diafiltration (UF/DF) step [17].
Methodology:
- Technology: Implement a mid-infrared (MIR) spectroscopy-based Process Analytical Technology (PAT) tool (e.g., Monipa, Irubis GmbH) in-line on the UF/DF system.
- Principle: MIR spectroscopy detects the interaction of molecular bonds with light in the mid-infrared range (400–4000 cm⁻¹). Proteins absorb at 1600–1700 cm⁻¹ (amide I) and 1450–1580 cm⁻¹ (amide II), while excipients like trehalose absorb at 950–1100 cm⁻¹ [17].
- Procedure:
- The PAT probe is installed directly in the process stream.
- During the UF/DF process, the system continuously collects MIR spectra.
- The ultrafiltration (UF1) phase concentrates the protein, tracked via the amide I/II peaks.
- The diafiltration (DF) phase exchanges the buffer; the removal of original buffers and introduction of new excipients (e.g., trehalose) is tracked via their specific spectral fingerprints.
- A final ultrafiltration (UF2) phase concentrates the protein to its target drug substance concentration, which is verified in real-time.
- Validation: The real-time concentration data is validated against a reference method (e.g., SoloVPE), typically achieving an error margin of <5% for protein and <+1% for excipients like trehalose [17].
Protocol 2: Advanced Cell Health Monitoring in Upstream Processing
Objective: To move beyond basic viability measurements and detect early-stage apoptosis and cell aggregation to optimize bioreactor conditions [16].
Methodology:
- Technology: Use a dynamic imaging analyzer (e.g., Canty Dynamic Imaging System, DIA) coupled with an automated sampler (e.g., SegFlow).
- Principle: The DIA is a flow-through microscope that captures images of cells directly from the bioreactor. It uses a Support Vector Machines (SVM) algorithm trained on known cell images to classify cells based on 42 morphological features into categories: viable, necrotic, aggregated, and apoptotic [16].
- Procedure:
- An automated sampler draws a sample from the bioreactor and performs real-time dilution.
- The sample flows through the DIA, which captures high-resolution images of thousands of cells.
- The SVM model analyzes each cell's morphology to determine its health status.
- This allows for the detection of early apoptosis before the cell membrane is compromised—a stage invisible to traditional trypan blue exclusion methods [16].
- Advantage: Early detection of stress enables timely intervention (e.g., nutrient feeding, temperature shift) to prevent cell death and maintain productivity [16].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the above protocols requires specific tools and reagents. The following table details key solutions used in the featured experiments.
Table 2: Key Research Reagent Solutions and Essential Materials
| Item | Function/Explanation |
|---|---|
| PAT Probe (MIR Spectroscopy) | Enables real-time, in-line monitoring of product and excipient concentrations during downstream processing by detecting molecule-specific infrared absorption [17]. |
| Dynamic Imaging Analyzer (DIA) | Provides high-resolution, flow-through imaging of cells for advanced morphological analysis, enabling early detection of apoptosis and cell aggregation [16]. |
| Automated Bioreactor Sampler | Automatically draws and dilutes samples from the bioreactor, ensuring consistent delivery to analytical instruments like the DIA while preserving fragile cell aggregates [16]. |
| Capacitance Probe | An in-line PAT tool that measures viable cell density and viable cell volume in the bioreactor by polarizing the culture and measuring charge retained by cells with intact membranes [16]. |
| Formulation Buffer Components | Excipients (e.g., histidine, trehalose) that stabilize the final drug substance. Their consistent concentration, achieved through controlled UF/DF, is a key CQA [17]. |
| SVM Algorithm Training Set | A pre-classified set of cell images (viable, necrotic, apoptotic) used to train the supervised learning model that powers the DIA's cell classification capabilities [16]. |
The Regulatory and Comparability Framework
The "process defines the product" principle is the cornerstone of the global regulatory framework for biologics, particularly for comparability assessments and biosimilar development.
Demonstrating Comparability After a Process Change
When a manufacturer changes the process for an approved biologic, it must demonstrate that the pre-change and post-change products are comparable. The foundation of this assessment is analytical comparability [18]. The goal is to show that the products are so similar in their CQAs that their clinical properties will be indistinguishable; clinical studies are seldom required [18]. This relies on:
- Orthogonal Analytical Methods: Using multiple, sensitive techniques (e.g., mass spectrometry plus chromatography) to cross-verify CQAs [18].
- Risk-based Weighting: Attributing more importance to CQAs with a direct known impact on clinical outcomes (e.g., primary structure must be identical, while minor glycoform variation may be acceptable) [18].
The Biosimilarity Exercise
A biosimilar is a biologic developed to be highly similar to an already licensed reference product. Its development is a focused, reverse-engineered comparability exercise [13] [14]. The following diagram outlines the step-wise approach to establishing biosimilarity, which places primary emphasis on analytical and functional comparisons.
Diagram 2: The step-wise biosimilar development pathway, demonstrating that analytical similarity is the foundation for approval.
The biosimilar developer must match the originator's "fingerprint" of CQAs as closely as possible using analytical tools that are more sensitive than clinical trials in detecting meaningful differences [13] [18]. Clinical studies for biosimilars are not designed to re-establish efficacy and safety from scratch, but to confirm sufficient likeness predicted by the analytical data [18] [14].
For complex biologics, the manufacturing process is not merely a production sequence—it is an intrinsic determinant of the product's identity. The principle that "the process defines the product" is driven by the inherent variability of molecules produced in living systems and the profound impact that process parameters have on Critical Quality Attributes. Maintaining consistent product quality requires a deep process understanding achieved through advanced Process Analytical Technologies, robust control strategies, and a rigorous risk-based approach to comparability. As the biologics and biosimilars market continues to evolve, adherence to this core principle, supported by convergent global regulatory standards, remains paramount for ensuring that patients receive medicines that are consistently safe, pure, and potent.
For researchers and drug development professionals working with biological products, the demonstration of comparability represents a fundamental scientific and regulatory requirement. The concept of comparability provides a structured framework for evaluating whether two versions of a biologic—whether the same product before and after a manufacturing change, or a biosimilar and its reference product—are sufficiently similar to ensure equivalent safety and efficacy profiles [18]. While both scenarios utilize the same foundational scientific principles of analytical and functional comparison, they differ significantly in their underlying context, knowledge base, and regulatory expectations [19].
This technical guide examines the critical distinctions between these two applications of comparability assessment, providing a detailed framework for designing appropriate studies within the context of biological products research. Understanding these distinctions is essential for efficiently allocating resources, designing scientifically valid studies, and meeting regulatory expectations for both innovator and biosimilar development programs.
Fundamental Conceptual Distinctions
Knowledge Base and Starting Points
The most fundamental distinction between these scenarios lies in the available knowledge about the manufacturing process and product understanding.
Manufacturing Process Changes: Occur within a single, controlled knowledge environment where the manufacturer possesses complete understanding of and historical data on the original manufacturing process, cell line, and product characteristics [19]. The manufacturer has established extensive knowledge of critical quality attributes (CQAs) and their acceptable ranges based on clinical experience with the original product.
Biosimilar Development: Begins with a significant knowledge gap regarding the reference product's proprietary manufacturing process [19] [20]. The biosimilar developer must reverse-engineer the reference product's critical attributes without access to the originator's manufacturing details, cell line, or process parameters, relying instead on extensive analytical characterization of the final product.
Regulatory Philosophies and Standards
The regulatory approaches for these two scenarios, while sharing scientific principles, differ in their fundamental questions and evidence requirements:
Manufacturing Process Changes: The central regulatory question is whether the change has adversely impacted the already approved product's safety, purity, and potency [8]. The burden of proof is demonstrating that differences, if any, have no adverse impact on the product's established clinical profile.
Biosimilar Development: The central question is whether the biosimilar candidate is highly similar to the reference product despite minor differences in clinically inactive components, with no clinically meaningful differences in safety, purity, and potency [19] [20]. The burden of proof is demonstrating similarity to a reference product with established efficacy and safety.
Table 1: Fundamental Conceptual Differences Between Scenarios
| Parameter | Manufacturing Process Change | Biosimilar Development |
|---|---|---|
| Knowledge Base | Complete process knowledge | Limited to public domain and analytical data |
| Cell Line | Same parental cell line | Different cell line |
| Starting Point | Well-characterized original product | Reference product characterization |
| Regulatory Standard | No adverse impact | High similarity |
| Evidence Threshold | Often analytical data sufficient | Totality of evidence across multiple study types |
Regulatory Frameworks and Guidelines
The comparability exercise for both scenarios operates within well-established regulatory frameworks that have evolved significantly since the 1990s [18].
Manufacturing Process Changes
For manufacturing changes, the ICH Q5E guideline provides the primary international framework for assessing comparability [2] [1]. This guideline outlines a risk-based approach where the scope of the manufacturing change dictates the extent of analytical studies required [19]. The FDA's 1996 guidance "Demonstration of Comparability of Human Biological Products" established the initial foundation, allowing manufacturers to implement changes without additional clinical studies when comparability could be demonstrated through analytical and functional testing [8].
The FDA's current approach for CMC changes to approved biological applications is detailed in the 2021 guidance "Chemistry, Manufacturing, and Controls Changes to an Approved Application: Certain Biological Products" [21]. This guidance employs a tiered-reporting system based on the potential impact of the change, ranging from prior-approval supplements to changes-being-effected supplements to annual reportable changes.
Biosimilar Development
The biosimilar pathway was established more recently, with the EU approving the first biosimilar (Omnitrope) in 2006 and the US following with the Biologics Price Competition and Innovation Act of 2009 [18]. The FDA's comprehensive guidance "Development of Therapeutic Protein Biosimilars: Comparative Analytical Assessment and Other Quality-Related Considerations" outlines a stepwise approach to biosimilar development [20] [22].
This approach begins with extensive analytical characterization, moves through non-clinical assessments, and culminates in targeted clinical studies [20]. The "totality of the evidence" from these cumulative studies supports a demonstration of biosimilarity, with the analytical data forming the foundation of this assessment [22].
Methodological Approaches: Analytical and Statistical Assessment
Analytical Characterization Strategies
Both scenarios require extensive analytical characterization, but the breadth and depth differ significantly:
Manufacturing Process Changes: Analytical comparison focuses specifically on attributes potentially affected by the particular process change, utilizing historically qualified methods and established acceptance criteria based on prior knowledge and experience with the product [8].
Biosimilar Development: Requires comprehensive side-by-side analysis using orthogonal analytical techniques to compare structural, physicochemical, and functional attributes [20] [18]. This includes detailed assessment of primary, secondary, tertiary, and quaternary structure; post-translational modifications (particularly glycosylation); biological activity; impurities; and immunochemical properties [22].
Statistical Approaches for Comparability
A risk-based, tiered statistical approach is recommended for comparability assessments, particularly for biosimilars [23]. This framework classifies quality attributes based on their potential impact on safety and efficacy:
Table 2: Tiered Statistical Approaches for Comparability Assessment
| Tier | Application | Statistical Method | Acceptance Criteria |
|---|---|---|---|
| Tier 1 | Critical Quality Attributes (CQAs) | Equivalence testing (TOST) or K-sigma comparison | Pre-defined equivalence margins (e.g., ±1.5σ) based on risk assessment |
| Tier 2 | Less critical quality attributes, in-process controls | Range testing | High percentage (85-95%) of biosimilar measurements within reference distribution limits |
| Tier 3 | Monitored parameters, qualitative assessments | Graphical comparison | Visual assessment for similar patterns and trends |
For Tier 1 CQAs, the equivalence test using two one-sided t-tests (TOST) is often employed to demonstrate that the mean difference between products falls within a pre-specified equivalence margin [23]. The K-sigma approach provides an alternative method where the absolute difference in means divided by the reference standard deviation must not exceed an acceptance limit (typically 1.5) [23].
The following diagram illustrates the comprehensive comparability assessment workflow for both scenarios:
Experimental Design and Study Requirements
Study Scope and Clinical Data Requirements
The evidence requirements for both scenarios reflect their different knowledge bases and regulatory standards:
Manufacturing Process Changes: For many changes, especially those with limited scope, analytical studies alone may be sufficient to demonstrate comparability [19] [8]. Comparative clinical studies are typically required only for major changes that could potentially impact clinical performance, such as cell line changes [19].
Biosimilar Development: Requires a stepwise approach incorporating comparative analytical, non-clinical, and clinical studies [20]. Clinical comparisons typically begin with pharmacokinetic (PK) and pharmacodynamic (PD) studies, progressing to comparative clinical efficacy and safety trials in patients when necessary [20].
Risk Assessment and Weight of Evidence
A critical distinction lies in how evidence is weighted and interpreted:
Manufacturing Process Changes: The assessment employs prior knowledge of the product's characterization and clinical experience to focus on specific attributes potentially affected by the change [8]. The manufacturer can leverage historical data to establish meaningful acceptance criteria.
Biosimilar Development: Uses a risk-based system for weighting analytical data according to its relevance to clinical properties [18]. For the most critical attributes (e.g., primary protein structure), identicality is typically required, while wider variances may be acceptable for lower-weighted attributes [18].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful comparability assessment requires carefully selected reagents and methodologies. The following table outlines essential materials and their applications in comparability studies:
Table 3: Essential Research Reagents and Materials for Comparability Assessment
| Reagent/Material | Primary Function | Application in Comparability Studies |
|---|---|---|
| Reference Standards | Benchmark for analytical comparisons | Quality control for both scenarios; primary comparator for biosimilars |
| Characterized Cell Banks | Production of biologic material | Same cell line for process changes; new but similar cell line for biosimilars |
| Chromatography Systems | Separation and analysis of product variants | Purity analysis, impurity profiling, charge variant assessment |
| Mass Spectrometry Platforms | Structural characterization | Sequence confirmation, post-translational modification analysis |
| Biological Assay Reagents | Functional activity assessment | Cell-based assays, binding assays, enzyme activity measurements |
| Immunogenicity Assay Components | Detection of immune responses | Assessment of potential differences in immunogenic profiles |
For researchers and drug development professionals, understanding the critical distinctions between comparability assessment for manufacturing changes versus biosimilar development is essential for designing efficient, scientifically sound, and regulatory-compliant development programs. While both scenarios utilize the same advanced analytical technologies and statistical approaches, they differ fundamentally in their knowledge base, regulatory standards, and evidence requirements.
Manufacturing process changes benefit from complete process knowledge and historical data, often allowing demonstration of comparability through focused analytical studies. In contrast, biosimilar development must address significant knowledge gaps through comprehensive structural and functional characterization, employing a totality-of-the-evidence approach to demonstrate high similarity to the reference product.
As analytical technologies continue to advance, the sensitivity and reliability of comparability assessments will further improve, potentially reducing regulatory requirements for clinical data in both scenarios. However, the fundamental distinction between demonstrating "no adverse impact" for process changes and "high similarity" for biosimilars will continue to shape study design and regulatory expectations for biological products.
The totality of evidence approach represents a foundational paradigm in the development and evaluation of biological products, serving as a scientific bridge that connects analytical characterization with clinical performance. This systematic framework requires sponsors to develop a comprehensive body of evidence that convincingly demonstrates product comparability following manufacturing changes or establishes biosimilarity to a reference product. Unlike small-molecule drugs, biological products exhibit inherent complexity due to their large size, heterogeneous molecular structures, and sensitivity to manufacturing processes. Even minor alterations in production can potentially impact critical quality attributes (CQAs) that influence safety, purity, and potency [24]. The totality approach acknowledges this complexity by integrating data from multiple evidence streams—analytical studies, functional assays, pharmacokinetic/pharmacodynamic (PK/PD) evaluations, and comparative clinical studies—to form a conclusive scientific narrative about product similarity [24].
Regulatory agencies worldwide, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), recognize that biological products cannot be fully characterized by analytical methods alone. The totality of evidence approach provides a structured methodology for addressing residual uncertainty about product performance when a stepwise evaluation reveals no meaningful differences between the proposed product and its reference. This framework has evolved significantly over the past decade, with regulators gaining substantial experience in evaluating integrated data packages for biosimilar development and manufacturing changes [25] [26]. The approach continues to adapt to scientific advancements, particularly as analytical technologies become increasingly sensitive at detecting structural and functional characteristics [25].
Regulatory Framework and Evolution
Foundational Principles and Guidelines
The regulatory foundation for the totality of evidence approach stems from key guidance documents that outline scientific considerations for demonstrating biosimilarity and comparability. The ICH Q5E guideline establishes principles for assessing comparability of biotechnological/biological products after manufacturing changes, focusing on the collection of technical information that provides evidence that process changes do not adversely impact quality, safety, or efficacy [1]. This guideline emphasizes that comparability does not necessarily mean identical quality attributes but rather that the existing knowledge base adequately justifies the conclusion that no adverse impact occurs.
Similarly, FDA's "Scientific Considerations in Demonstrating Biosimilarity to a Reference Product" guidance, initially finalized in 2015 and updated in 2025, outlines a stepwise approach to biosimilar development that culminates in a totality-of-evidence assessment [25] [26]. The 2015 guidance recommended comparative efficacy studies (CES) if residual uncertainty remained after analytical, toxicity, PK, and immunogenicity assessments. However, the 2025 draft guidance represents a significant evolution in regulatory thinking, suggesting that for many therapeutic protein products (TPPs), CES may not be necessary when modern analytical technologies can provide sufficient characterization [25].
Recent Regulatory Developments
Recent regulatory updates reflect the FDA's growing confidence in advanced analytical methods as reliable tools for establishing biosimilarity and comparability. The October 2025 draft guidance marks a substantial shift by proposing that comparative efficacy studies may be unnecessary for certain well-characterized biological products when sufficient analytical and pharmacokinetic data exist [26]. This streamlined approach applies specifically to therapeutic protein products that meet three key conditions:
- The biosimilar and reference product are manufactured from clonal cell lines, are highly purified, and can be well-characterized analytically
- The relationship between quality attributes and clinical efficacy is well understood and can be evaluated by validated assays
- An appropriately designed human pharmacokinetic similarity study and immunogenicity assessment can address residual uncertainty [25] [26]
This evolution signals the FDA's recognition that comparative analytical assessments are often more sensitive than comparative efficacy studies for detecting clinically meaningful differences between products [25] [26]. The guidance reflects over a decade of regulatory experience evaluating biosimilar applications and acknowledges that analytical technologies can now structurally characterize highly purified therapeutic proteins and model in vivo functional effects with a high degree of specificity and sensitivity [25].
Table 1: Evolution of FDA's Approach to Evidence Requirements for Biosimilars
| Aspect | 2015 Guidance Approach | 2025 Draft Guidance Updates |
|---|---|---|
| Analytical Data | Foundation, but often insufficient alone | May be sufficient with robust modern analytical techniques |
| Comparative Efficacy Studies | Generally expected unless scientifically unnecessary | May be unnecessary for well-characterized TPPs |
| Primary Evidence Source | Clinical studies | Comparative analytical assessment (CAA) |
| Residual Uncertainty | Addressed through clinical studies | Addressed through PK studies and immunogenicity assessment |
| Regulatory Mindset | Prove why CES isn't needed | Default to no CES when conditions met |
Core Components of the Totality of Evidence
Analytical Characterization
Comparative analytical assessment forms the cornerstone of the totality of evidence approach, providing the most sensitive tool for detecting structural and functional differences between biological products. The FDA's guidance "Development of Therapeutic Protein Biosimilars: Comparative Analytical Assessment and Other Quality-Related Considerations" emphasizes that analytical studies should comprehensively evaluate critical quality attributes (CQAs) that may impact safety, purity, and potency [22]. These attributes include primary structure (amino acid sequence), higher-order structure (folding), post-translational modifications (glycosylation patterns), biological activity, purity, and impurities [24].
The analytical comparability exercise must demonstrate that the proposed biosimilar or changed product is highly similar to the reference product notwithstanding minor differences in clinically inactive components [24]. Manufacturers must employ state-of-the-art analytical technologies—including mass spectrometry, chromatography, capillary electrophoresis, nuclear magnetic resonance, and various spectroscopic methods—to characterize both products extensively. The depth of analytical characterization required depends on product complexity, the understanding of structure-function relationships, and the capability of analytical methods to detect clinically relevant differences [22].
Functional and Nonclinical Studies
Functional assays provide critical evidence about biological activity and mechanism of action, serving as a bridge between analytical characterization and clinical performance. These in vitro studies evaluate the binding and functional properties of the product, including receptor binding affinity, signal transduction, effector functions, and other mechanism-relevant activities [24]. The assay validation is crucial, with sponsors expected to demonstrate that the methods are sufficiently sensitive to detect potential differences in functional activities that might impact clinical performance [22].
In some cases, animal studies may be necessary to address specific questions about toxicity, pharmacokinetics, or pharmacodynamics that cannot be adequately evaluated through in vitro methods alone [24]. However, the 2025 draft guidance indicates that for many well-characterized TPPs, the need for animal studies may be reduced when analytical and functional data provide sufficient evidence of similarity [25]. The determination of necessary nonclinical studies should be based on residual uncertainty after comprehensive analytical and functional assessment.
Clinical Studies
While the recent FDA draft guidance reduces the emphasis on comparative efficacy studies for certain products, clinical evaluation remains an essential component of the totality of evidence in many circumstances [25] [26]. The clinical development program typically includes:
- Pharmacokinetic studies comparing exposure metrics (AUC, Cmax) between the proposed and reference products
- Pharmacodynamic studies comparing biomarker responses when relevant PD markers exist
- Immunogenicity assessment evaluating potential differences in immune response
- Comparative efficacy and safety studies when residual uncertainty remains after other assessments [24]
The design of clinical studies should focus on sensitive populations and endpoints capable of detecting potential differences between products. For biosimilars, the clinical study goal is not to re-establish benefit-risk profile but to confirm similarity to the reference product [24]. When analytical and functional data are highly conclusive, clinical studies may be streamlined to focus primarily on pharmacokinetics and immunogenicity [25].
Table 2: Key Evidence Components in a Totality of Evidence Approach
| Evidence Category | Key Elements | Purpose | When Required |
|---|---|---|---|
| Analytical Characterization | Structural analysis, physicochemical properties, biological activity, purity, impurities | Foundation for similarity demonstration; most sensitive for detecting differences | Always required |
| Functional Assays | Binding assays, cell-based bioassays, mechanism-of-action specific assays | Bridge analytical and clinical findings; assess biological activity | Always required |
| Pharmacokinetic/Pharmacodynamic Studies | AUC, Cmax, clearance; biomarker responses where applicable | Compare in vivo exposure and response | Usually required for biosimilars; may be sufficient for some TPPs |
| Immunogenicity Assessment | Anti-drug antibody incidence, neutralizing antibodies, clinical impact | Evaluate potential differences in immune response | Always required for proteins with immunogenicity concerns |
| Comparative Clinical Studies | Efficacy, safety, immunogenicity in sensitive patient population | Resolve residual uncertainty about clinical performance | When uncertainty remains after other assessments |
Implementation Framework: Stepwise Approach to Evidence Generation
The Stepwise Development Process
Implementing a successful totality of evidence strategy requires a systematic, stepwise approach that begins with extensive analytical characterization and progressively moves to clinical evaluation only when necessary to resolve residual uncertainty [24]. This hierarchical methodology ensures resources are allocated efficiently while building the most compelling scientific case for product comparability or biosimilarity.
The first and most critical step involves comprehensive analytical and functional comparison using state-of-the-art technologies. Sponsors must invest in extensive side-by-side testing of the proposed product and reference product, evaluating a wide range of quality attributes through orthogonal analytical methods [22]. The objective is to demonstrate that the products are highly similar notwithstanding minor differences in clinically inactive components and that these differences fall within the acceptable range of natural heterogeneity observed in the reference product [24].
If analytical and functional studies reveal no clinically meaningful differences, sponsors proceed to clinical pharmacokinetic and pharmacodynamic studies designed to confirm similar exposure and response profiles [25]. These studies should be conducted in sensitive populations using validated methods capable of detecting potential differences. Only when uncertainty persists after these evaluations should sponsors consider comparative efficacy trials, which are increasingly viewed as a measure of last resort for well-characterized products under the updated regulatory framework [25] [26].
Statistical Considerations and Acceptance Criteria
A robust totality of evidence approach requires predefined acceptance criteria and statistical methods capable of demonstrating similarity with high confidence. For analytical comparisons, sponsors should establish equivalence margins based on the natural variability of the reference product and the sensitivity of analytical methods to detect clinically meaningful differences [22]. Statistical approaches may include equivalence testing, quality range methods, or tolerance intervals, depending on the type of data and regulatory expectations.
For clinical pharmacokinetic studies, the standard approach involves demonstrating that the 90% confidence intervals for the geometric mean ratios of AUC and Cmax fall within the predefined equivalence margins of 80-125% [24]. Sample size calculations should provide sufficient power to demonstrate equivalence, typically requiring 80-200 subjects depending on expected variability. Similar statistical rigor should be applied to pharmacodynamic, efficacy, and safety endpoints when comparative clinical studies are necessary.
Experimental Protocols and Methodologies
Comprehensive Analytical Characterization Protocol
Objective: To perform exhaustive structural and functional characterization of both the proposed product and reference product using orthogonal analytical methods to demonstrate high similarity.
Methodology:
Primary Structure Analysis:
- Intact Mass Analysis: Using LC-MS with electrospray ionization to determine molecular weight within 50 Da of reference product
- Peptide Mapping: Tryptic digestion followed by LC-MS/MS with sequence coverage >95%
- Amino Acid Analysis: Hydrolysis and derivatization to confirm composition
- N- and C-terminal Sequencing: Edman degradation and carboxypeptidase digestion
Higher-Order Structure Assessment:
- Circular Dichroism: Far-UV (190-250 nm) and near-UV (250-350 nm) scanning
- Fluorescence Spectroscopy: Intrinsic tryptophan fluorescence with excitation at 295 nm
- FTIR Spectroscopy: Amide I region (1600-1700 cm⁻¹) for secondary structure
- X-ray Crystallography/NMR: For products where precise structure determination is critical
Post-Translational Modifications:
- Glycan Analysis: HILIC-UPLC with fluorescence detection for N-linked and O-linked glycans
- Glycosylation Site Mapping: LC-MS/MS following tryptic digestion
- Oxidation/Deamidation: Peptide mapping with targeted MS for modified peptides
- Other PTMs: Phosphorylation, sulfation, acetylation as product-specific
Purity and Impurity Profile:
- Size Variants: SEC-HPLC with light scattering detection for aggregates and fragments
- Charge Variants: CEX-HPLC and capillary isoelectric focusing
- Product-Related Impurities: Host cell proteins, DNA, residuals from purification
Acceptance Criteria: All quality attributes must fall within the reference product variability range established through testing of multiple reference product lots. No structurally or functionally significant differences outside qualified limits.
Functional Characterization Protocol
Objective: To compare the biological activities and mechanism of action of the proposed product and reference product through in vitro bioassays.
Methodology:
Binding Assays:
- Surface Plasmon Resonance: Kinetic analysis of target binding (ka, kd, KD)
- ELISA/Electrochemiluminescence: Affinity measurements and epitope mapping
- Cell-Based Binding: Flow cytometry with relevant cell lines
Bioactivity Assays:
- Cell Proliferation/Apoptosis: For growth factors and cytokines
- Signal Transduction: Phosphorylation assays, reporter gene assays
- Effector Functions: ADCC, CDC, Fc receptor binding for antibodies
- Enzyme Activity: Kinetic parameters (Km, Vmax) for enzymatic products
Potency Determination:
- Parallel Line Assay: Relative potency calculation with 95% confidence intervals
- Full dose-response curves: IC50/EC50 comparison with similarity margin ±1.5-fold
Acceptance Criteria: Relative potency must fall within 80-125% of reference product with 95% confidence intervals. Binding kinetics should show no statistically significant differences in mechanism-relevant parameters.
Clinical Pharmacokinetic Study Protocol
Objective: To demonstrate similar pharmacokinetic profiles between the proposed biosimilar and reference product in a sensitive population.
Methodology:
Study Design:
- Population: Healthy volunteers or patients with the condition (n=80-200)
- Design: Randomized, parallel-group or crossover design
- Dosing: Single dose or multiple doses based on product characteristics
- Duration: Sufficient to characterize elimination phase (typically 5 half-lives)
Blood Sampling:
- Intensive Sampling: Pre-dose and at 12-18 timepoints post-dose
- Trough Concentrations: For multiple-dose studies
- Sample Handling: Standardized processing and storage conditions
Bioanalytical Methods:
- Validated ELISA or ECL: Specific for the product with LLOQ sufficient for PK characterization
- Anti-drug antibody detection: Bridge format or similar with appropriate sensitivity
- Neutralizing antibody assay: Cell-based if indicated
PK Parameters:
- Primary: AUC0-inf, AUC0-t, Cmax
- Secondary: Tmax, t1/2, CL, Vd
Statistical Analysis: ANOVA on log-transformed parameters with 90% CIs for geometric mean ratios (test/reference) falling within 80-125% equivalence margin.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the totality of evidence approach requires access to high-quality reference materials and specialized reagents. The following table details essential components of the biosimilar or comparability assessment toolkit.
Table 3: Essential Research Reagents and Materials for Comparability Assessment
| Reagent/Material | Specifications | Critical Function | Quality Controls |
|---|---|---|---|
| Reference Product | Multiple lots (≥10) covering manufacturing variability | Gold standard for comparison | Full characterization; proper storage conditions |
| Cell-Based Bioassay Systems | Relevant cell lines with validated responsiveness | Measures biological activity | Passage number control; mycoplasma testing |
| Target Antigens/Receptors | Recombinant proteins with confirmed activity | Binding studies and affinity measurements | Purity >95%; functional validation |
| Anti-Product Antibodies | Monoclonal and polyclonal, various epitopes | Immunoassays and characterization | Specificity confirmation; titer determination |
| Chromatography Standards | System suitability standards for each method | Method performance verification | USP/EP standards where available |
| Mass Spectrometry Standards | Intact protein and peptide standards | Instrument calibration and quantification | Sequence-verified; purity confirmed |
| Clinical Assay Reagents | Validated kit components or individual reagents | PK and immunogenicity assessments | Lot-to-lot consistency; stability data |
Regulatory Submission Strategy
Assembling the Evidence Dossier
The regulatory submission for a biosimilar or manufacturing change should present a coherent narrative that integrates all evidence streams into a compelling demonstration of similarity. The dossier should begin with comprehensive analytical data, progress through functional characterization, and culminate with clinical data when required [25] [22]. Each section should explicitly reference how the evidence addresses specific regulatory criteria and reduces residual uncertainty about product performance.
Sponsors should emphasize the sensitivity of analytical methods to detect clinically meaningful differences, particularly highlighting technological advancements that enable more precise characterization than was possible when the reference product was initially approved [25] [26]. For products seeking waiver of comparative efficacy studies, the submission must convincingly demonstrate that the relationship between quality attributes and clinical efficacy is well understood and that analytical and pharmacokinetic data adequately predict clinical performance [25].
Engagement with Regulatory Agencies
Early and frequent communication with regulatory agencies is critical for successful implementation of the totality of evidence approach. The FDA's 2025 draft guidance specifically encourages sponsors to engage with the agency "early in product development" to confirm alignment on evidence requirements [25] [26]. These discussions should focus on:
- Proposed analytical similarity acceptance criteria and statistical approaches
- Justification for any proposed waivers of comparative efficacy studies
- Design of necessary clinical studies, including population, endpoints, and equivalence margins
- Strategies for addressing residual uncertainty through focused data collection
Sponsors should prepare comprehensive briefing documents that present the scientific rationale for their approach, including data from preliminary studies and literature reviews supporting the connection between quality attributes and clinical outcomes.
The totality of evidence approach continues to evolve as regulatory science advances and analytical technologies improve. The recent FDA draft guidance signals a significant shift toward greater reliance on comparative analytical assessment for well-characterized therapeutic protein products, reflecting both increased regulatory comfort with advanced characterization methods and a desire to reduce unnecessary clinical testing burdens [25] [26]. This evolution promises to accelerate the development of biosimilars and facilitate manufacturing improvements for innovator products, ultimately enhancing patient access to biological therapies.
However, the core principles of the approach remain unchanged: sponsors must still develop a comprehensive, scientifically rigorous data package that addresses all potential sources of uncertainty about product quality, safety, and efficacy. The stepwise evaluation process continues to prioritize analytical characterization as the most sensitive tool for detecting product differences, with clinical studies reserved for addressing residual uncertainty that cannot be resolved through other means [24]. As the regulatory landscape continues to evolve, sponsors should maintain focus on robust scientific principles while adapting to new opportunities for efficient evidence generation.
Executing a Successful Comparability Study: A Step-by-Step Methodological Guide
For researchers and drug development professionals, demonstrating that a biological product remains highly similar after a manufacturing change is a critical regulatory requirement. A risk-based approach to comparability is a systematic process that uses existing product and process knowledge to focus assessment efforts on the changes most likely to impact product quality, safety, and efficacy [27] [28]. The core principle is that not all manufacturing changes carry equal risk; the scope and depth of the comparability study should be proportionate to the level of risk and the product's stage of development [28] [29].
This approach is foundational for navigating Chemistry, Manufacturing, and Controls (CMC) post-approval changes throughout the product lifecycle. Regulatory guidelines like ICH Q5E form the basis for ensuring that "any differences in quality attributes have no adverse impact upon safety or efficacy of the drug product" [29]. By leveraging a risk-based framework, manufacturers can design scientifically rigorous yet efficient comparability protocols (CP) that satisfy regulatory expectations while optimizing resources.
Foundational Principles of Risk Assessment
Key Definitions and Regulatory Context
A robust risk-based comparability assessment is built upon clearly defined concepts. The following table summarizes the core principles and their regulatory foundations.
Table 1: Core Principles of a Risk-Based Comparability Approach
| Principle | Description | Regulatory Reference |
|---|---|---|
| Highly Similar | The pre- and post-change products do not need to be identical but must be highly similar with no adverse impact on safety or efficacy [29]. | ICH Q5E |
| Risk-Based Evaluation | The assessment focuses on the potential impact of a change on Critical Quality Attributes (CQAs) based on prior knowledge [27] [28]. | FDA Guidance on Comparability Protocols |
| Phase-Appropriateness | The depth of comparability testing is aligned with the product's development stage (e.g., Phase I vs. Commercial) [28] [29]. | ICH Guidelines |
| Comparability Protocol (CP) | A detailed, pre-approved plan for assessing the effect of a proposed CMC change on the product [30] [31]. | FDA Guidance (2022) |
The Risk Assessment Workflow
The risk assessment process for defining the comparability study scope involves a logical sequence of steps, from identifying the change to finalizing the testing strategy. The following diagram visualizes this workflow:
This process ensures that the final comparability study scope is targeted and justified. The risk level dictates the testing burden. For a high-risk change, such as a switch in cell line, extensive molecular and functional analyses are warranted [31]. Conversely, a low-risk change may only require a limited set of analytical tests to confirm comparability.
Implementing the Risk-Based Framework
A Phase-Appropriate Testing Strategy
The rigour of a comparability study is not static; it must evolve with the product's lifecycle. The following table outlines a phase-appropriate testing strategy, balancing scientific thoroughness with development efficiency.
Table 2: Phase-Appropriate Comparability Testing Strategy
| Development Phase | Recommended Testing Scope | Lot Selection Strategy | Risk Consideration |
|---|---|---|---|
| Preclinical / Phase I | Platform characterization; limited forced degradation screening (e.g., thermal stress) [28]. | Single pre- and post-change batches [29]. | Focus on critical attributes; platform knowledge used to mitigate limited product-specific data. |
| Phase II / Early Phase III | More extensive characterization; confirmation of forced degradation pathways (oxidative, shear stress) [28]. | Multiple pre- and post-change batches. | Increased understanding of CQAs allows for more targeted assessment of process change impact. |
| Phase III to Commercial / Post-Approval | Extended characterization (structural, biophysical, biological potency); real-time stability; full forced degradation studies [28] [29]. | The gold standard: 3 pre-change vs. 3 post-change batches [29]. | Comprehensive data required to justify high-stakes commercial decision; lowest uncertainty acceptable. |
Designing the Analytical and Functional Experimentation Protocol
The experimental core of a comparability study is a head-to-head analysis of pre- and post-change materials using a suite of orthogonal methods. The workflow below outlines the key experimental stages from sample preparation to data interpretation.
Detailed Methodologies for Key Experiments
1. Primary Structure Analysis
- Objective: To confirm the amino acid sequence and identify post-translational modifications (PTMs) like glycosylation, oxidation, and deamidation [28] [29].
- Protocol: Use peptide mapping with Liquid Chromatography-Mass Spectrometry (LC-MS). The protein is digested with an enzyme like trypsin, and the resulting peptides are separated by reversed-phase HPLC and analyzed by high-resolution mass spectrometry. Compare the peptide maps and MS spectra of pre- and post-change samples to verify sequence integrity and quantify PTM levels [29].
- Critical Reagents: Trypsin (protease for digestion), reference standard (for system suitability), and appropriate mobile phases (e.g., water/acetonitrile with trifluoroacetic acid).
2. Higher-Order Structure and Purity Analysis
- Objective: To assess the three-dimensional structure, aggregation, and fragmentation profiles.
- Protocol:
- Circular Dichroism (CD): Measures secondary and tertiary structure by analyzing differential absorption of left- and right-handed circularly polarized light.
- Size Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS): Quantifies soluble aggregates and fragments under native conditions. MALS provides an absolute molecular weight, confirming oligomeric state [29].
- Critical Reagents: High-purity buffers for sample formulation (e.g., phosphate-buffered saline) and SEC column calibration standards.
3. Functional Activity and Potency Assessment
- Objective: To demonstrate the biological mechanism of action is retained. This is a crucial surrogate for clinical efficacy [31].
- Protocol: Employ cell-based bioassays that measure the biological response (e.g., inhibition of cell proliferation, cytokine release). For monoclonal antibodies, this includes binding assays (e.g., Surface Plasmon Resonance for binding kinetics to the target antigen) and Fc effector function assays (e.g., ADCC, CDC) if relevant to the mechanism of action [32].
- Critical Reagents: Relevant cell lines, target antigens, effector cells (for ADCC), and a validated reference standard are essential for these complex assays.
4. Forced Degradation Studies
- Objective: To "pressure-test" the molecule and uncover differences in degradation pathways that are not apparent under standard stability conditions [29].
- Protocol: Expose pre- and post-change samples to various stress conditions and analyze degradation products. Key stresses include:
- The degradation profiles are compared using techniques like SEC (for aggregation), CE-SDS (for fragmentation), and IEX-HPLC (for charge variants).
The Scientist's Toolkit: Essential Research Reagent Solutions
The success of a comparability study hinges on the quality and consistency of its critical reagents.
Table 3: Key Research Reagent Solutions for Comparability Studies
| Reagent / Material | Function in Comparability Protocol | Criticality Notes |
|---|---|---|
| Cell Banks (MCB/WCB) | Source for producing the biologic drug substance. A change in cell line is a major risk factor [31] [32]. | Storage sites must be stated in regulatory dossiers; characterization is vital [32]. |
| Reference Standard | A well-characterized batch used as a benchmark for all analytical and functional comparisons [29]. | The cornerstone of the entire study; its quality and stability dictate the reliability of all results. |
| Critical Assay Components | Cell lines, antigens, enzymes, and antibodies used in potency and impurity testing (e.g., HCP assays) [32]. | For HCP assays, the detecting antibody must be validated for coverage of HCPs representative of the specific process [32]. |
| Chromatography Resins | Used in downstream purification. Their re-use qualification must be validated [32]. | A validation protocol for post-approval full-scale validation of resin re-use is typically required [32]. |
| Culture Media & Raw Materials | Components used in the upstream manufacturing process. Changes can introduce impurities [32]. | Qualitative composition must be known for risk assessment of residual impurities [32]. |
A risk-based approach to designing a comparability protocol is not merely a regulatory checkbox but a strategic scientific exercise. It demands a deep understanding of the product's Critical Quality Attributes and their link to clinical performance. By systematically assessing risk, implementing a phase-appropriate scope, and executing a robust analytical and functional experimental plan, developers can effectively demonstrate comparability. This ensures that necessary manufacturing improvements can be implemented without compromising the quality, safety, or efficacy of biological products, ultimately benefiting both developers and patients.
In the development and quality control of biological products, such as biosimilars, gene therapies, and cell therapies, an orthogonal approach is a foundational scientific strategy mandated by global regulatory agencies. This approach involves the integrated use of multiple independent analytical methods to assess a single Critical Quality Attribute (CQA) [33]. The primary goal is to provide a comprehensive characterization of a product's properties and composition while eliminating the risk of false results that might arise from the limitations of any single method [33] [34]. For complex biological products, whose safety and efficacy are intimately tied to their structural and functional integrity, this methodology is not merely best practice but a regulatory expectation to ensure product quality, batch-to-batch consistency, and patient safety [33] [35].
The terms "orthogonal" and "complementary" are often used in guidance documents, and clear definitions are crucial for designing robust characterization strategies. Orthogonal measurements use different physical or chemical principles to measure the same property of the same sample, aiming to minimize method-specific biases and interferences to determine the true value of a product attribute [34]. In contrast, complementary measurements are a broader set of methods that, while they may assess different attributes, corroborate each other to support the same overall decision about product quality [34]. This whitepaper delineates the practical application of orthogonal methods, providing a detailed toolkit for researchers and scientists focused on demonstrating comparability for biological products.
The Rationale for an Orthogonal Approach
The biological products of today, including engineered antibodies, viral vectors, and cell-based therapies, are structurally complex and heterogeneous. Relying on a single analytical method for characterization is fraught with risk, as every technique has inherent limitations and potential interferences.
- Risk Mitigation: A key rationale for orthogonality is to mitigate the risk of measurement bias and uncertainty in decision-making. For instance, in glycan analysis, peptide mapping can detect glycopeptides but may cause artificial fragmentation of glycan structures during mass spectrometry ionization, leading to an inaccurate profile. This method must be orthogonal to analysis of fluorescently labeled released glycans, which provides a more reliable relative quantitation without such fragmentation issues [36].
- Regulatory Expectation: Major regulatory bodies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), explicitly recommend orthogonal testing strategies. This is emphasized for the characterization of biosimilars, gene therapy products, and vaccines containing nanomaterials [33] [34] [35]. The FDA guidance on biosimilars underscores that even with advanced analytical techniques, a single method cannot detect all relevant differences, necessitating a comprehensive assessment with multiple methods [35].
- Comprehensive Understanding: Using independent methods provides a more holistic view of the product. For example, characterizing a protein's higher-order structure (HOS) requires a combination of techniques like circular dichroism (CD), Fourier-transform infrared (FTIR) spectroscopy, and nuclear magnetic resonance (NMR), where each probes different aspects of secondary and tertiary structure [36].
The following workflow illustrates the strategic process of implementing an orthogonal approach for a quality attribute, from selection to data integration:
Orthogonal Methods for Key Product Attributes
The application of orthogonal methods spans all critical quality attributes of a biological product. The specific techniques employed are tailored to the nature of the product, whether it is a viral vector, a therapeutic antibody, or a cell therapy.
Identity and Purity Characterization
For cell therapy products, identity is confirmed through an orthogonal set of genotypic, phenotypic, and morphological analyses. This may include flow cytometry for surface markers, short tandem repeat (STR) profiling for genetic fingerprinting, and karyological analysis for genetic stability [33]. For viral vector-based therapies, such as recombinant adeno-associated virus (rAAV), identity and purity require characterization of structural integrity, transgene expression, and the ratio of full to empty capsids [33]. The presence of empty capsids is a critical related impurity that can reduce product efficacy and trigger immune responses.
Table 1: Orthogonal Methods for Characterizing rAAV Full/Empty Capsid Ratio
| Method | Principle | Application in Development | Suitability for GMP Release |
|---|---|---|---|
| Analytical Ultracentrifugation (AUC) | Separates particles based on sedimentation velocity under centrifugal force. | High-resolution characterization during product development. | Less suitable due to low throughput and complexity [33]. |
| Size Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS) | Separates particles by size and uses light scattering to determine molecular weight. | Optimal for quality control and stability studies. | Optimal for GMP release testing, though cannot resolve partially filled capsids [33]. |
| Transmission Electron Microscopy (TEM) | Provides direct visual quantification of particles. | Used for product characterization and validation. | Used as a complementary qualitative technique [33]. |
| Dynamic Light Scattering (DLS) | Measures hydrodynamic size distribution of particles in solution. | Rapid assessment of sample heterogeneity and aggregation [33]. | Used for general particle size and aggregation assessment. |
Higher-Order Structure and Stability Assessment
For therapeutic proteins and antibodies, higher-order structure (HOS) is a critical quality attribute directly linked to biological function and efficacy. A suite of biophysical techniques is employed orthogonally to probe different aspects of protein conformation and stability.
- Thermal Stability: nano-Differential Scanning Fluorimetry (nanoDSF) measures the unfolding of a protein as it is heated by tracking intrinsic fluorescence, providing a melting temperature (Tm) [37].
- Size and Aggregation: Size Exclusion Chromatography (SEC) separates protein monomers from aggregates and fragments based on hydrodynamic volume. Dynamic Light Scattering (DLS) measures the hydrodynamic radius and polydispersity in solution, providing a rapid assessment of aggregation propensity and sample homogeneity [37].
- Secondary and Tertiary Structure: Circular Dichroism (CD) spectroscopy detects changes in the protein's secondary structure (alpha-helix, beta-sheet) by measuring differential absorption of left- and right-handed circularly polarized light [36] [37].
The utility of these orthogonal methods is evident in characterizing engineered antibody fragments. Studies show that while full-length IgGs exhibit high thermal and structural stability, smaller fragments like single-chain variable fragments (scFvs) and bispecific tandem scFvs display increased aggregation propensity and reduced conformational stability. These differences are captured orthogonally by higher polydispersity in DLS, early elution peaks in SEC, and altered thermal unfolding profiles in nanoDSF [37].
Post-Translational Modification Analysis
Post-translational modifications (PTMs), such as glycosylation and C-terminal lysine processing, can significantly impact the safety, efficacy, and stability of therapeutic proteins. Orthogonal methods are essential for accurate characterization.
Glycan Analysis: As highlighted in the biosimilar testing example, peptide mapping via LC-MS can identify glycopeptides but is prone to in-source fragmentation, artificially generating truncated glycan species [36]. An orthogonal method involving the release, fluorescent tagging, and subsequent analysis of glycans provides a more accurate profile without these artifacts, thereby verifying and extending the conclusions from the peptide map [36].
C-Terminal Lysine Analysis: The presence or absence of C-terminal lysine on the heavy chain of monoclonal antibodies can be detected in a peptide map. An orthogonal technique, imaged capillary isoelectric focusing (icIEF), separates charge variants. The basic lysine residue causes species with the modification to migrate to a more basic isoelectric point (pI). The identity of these peaks is confirmed by treating the sample with carboxypeptidase B, which removes C-terminal lysine and eliminates the corresponding peaks in the icIEF profile [36].
Experimental Protocols for Key Orthogonal Techniques
Protocol: Orthogonal Particle Size and Distribution Analysis
This protocol combines DLS and SEC-MALS for orthogonal analysis of protein complexes or nanoparticles like viral vectors [33] [37].
Method 1: Dynamic Light Scattering (DLS)
- Instrument Setup: Use a instrument such as an Anton Paar Litesizer 100. Allow the laser to warm up for at least 15 minutes.
- Sample Preparation: Dialyze or dilute the protein sample (e.g., purified antibody fragment or viral vector) into a suitable buffer (e.g., PBS). Filter the buffer and sample through a 0.1 µm or 0.22 µm filter to remove dust.
- Measurement: Load the sample into a clean, disposable microcuvette. Set the measurement temperature (typically 20-25°C). Perform a minimum of 10-12 measurements per sample.
- Data Analysis: Analyze the correlation function to determine the hydrodynamic radius (Rh) and the polydispersity index (PdI). A PdI below 0.2 is generally considered monodisperse.
Method 2: Size Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS)
- Chromatography System: Use an HPLC system (e.g., ÄKTA system from Cytiva) equipped with a suitable SEC column (e.g., Superdex Increase 10/300).
- Detectors: Connect the column in series to a MALS detector (e.g., a Wyatt miniDAWN TREOS) and a refractive index (RI) detector.
- Run Conditions: Equilibrate the column with the mobile phase (e.g., PBS). Maintain a constant flow rate (e.g., 0.5-0.75 mL/min). Load 50-100 µL of sample at a concentration of 1-2 mg/mL.
- Data Analysis: Use the MALS and RI data with the known dn/dc (refractive index increment) of the protein to calculate the absolute molecular weight of the species in solution independently of elution volume, allowing differentiation of monomers, aggregates, and fragments.
Protocol: Orthogonal Higher-Order Structure Analysis
This protocol outlines the use of nanoDSF and CD for orthogonal assessment of protein structure and stability [37].
Method 1: nano-Differential Scanning Fluorimetry (nanoDSF)
- Instrument: Use a Prometheus Panta NT48 instrument (NanoTemper) or equivalent.
- Sample Preparation: Dialyze the protein sample (e.g., a full-length IgG or an scFv) into a non-fluorescent buffer (e.g., PBS). Adjust the protein concentration to an A280 of ~0.1-0.5.
- Measurement: Load the sample into standard grade capillaries. Program a temperature ramp from 20°C to 95°C with a ramp rate of 1°C/min. The instrument will monitor the fluorescence ratio at 350 nm/330 nm.
- Data Analysis: Identify the inflection point (Tm) of the unfolding transition from the resulting sigmoidal curve. Multiple transitions may indicate domain-specific unfolding.
Method 2: Circular Dichroism (CD) Spectroscopy
- Instrument: Use a spectropolarimeter (e.g., JASCO J-1500).
- Sample Preparation: Dialyze the protein into a volatile buffer or use ultrafiltration to exchange into a CD-compatible buffer (e.g., 5 mM sodium phosphate). Adjust protein concentration to 0.1-0.2 mg/mL for far-UV CD.
- Far-UV Measurement (Secondary Structure): Use a quartz cuvette with a path length of 0.1 cm. Set the wavelength range from 190-260 nm. Perform scans at 20°C and subtract the buffer baseline.
- Data Analysis: Analyze the resulting spectrum (characterized by minima at 208 nm and 222 nm for alpha-helices) to determine the relative secondary structure content.
The Scientist's Toolkit: Essential Research Reagent Solutions
A robust orthogonal characterization strategy relies on high-quality reagents and materials. The following table details essential solutions used in the experiments and methods cited.
Table 2: Key Research Reagent Solutions for Orthogonal Characterization
| Reagent / Material | Function and Application | Example from Literature |
|---|---|---|
| Protein-G Sepharose | Affinity chromatography resin for purification of antibodies and Fc-fusion proteins from cell culture supernatants. | Used for purification of recombinant full-length IgG and fusion antibodies from Expi293 cell culture [37]. |
| Carboxypeptidase B | Proteolytic enzyme that specifically removes C-terminal lysine and arginine residues. Used for orthogonal verification of C-terminal lysine on mAbs. | Treatment of mAb samples prior to icIEF analysis to confirm the identity of basic peaks corresponding to C-terminal lysine variants [36]. |
| Site-Specific Peptide Tags (e.g., MiniVIPER) | Small peptide tags for orthogonal labeling of multiple cellular proteins for imaging; form high-affinity heterodimers with probe peptides. | Used for specific, multi-color fluorescence microscopy of cellular proteins like TOMM20, actin, and histone 2B without cross-reactivity [38]. |
| Host Cell Proteins (HCP) Assay Kits | Immunoassays to detect and quantify process-related impurities derived from the expression system. Must be validated with the product's specific cell substrate. | Critical for assessing purity and safety; requires orthogonal methods to ensure accuracy and sensitivity [35]. |
| Fluorescently Labeled Glycan Standards | Released and tagged N-glycans used as standards for orthogonal characterization of protein glycosylation profiles. | Provides verification and extension of glycan data obtained from peptide mapping experiments [36]. |
Implementing Orthogonal Strategies in Product Development
Integrating orthogonal methods from the early stages of product development is critical for success. A systematic workflow should be established, starting with a risk assessment to identify CQAs that have the potential to impact activity, pharmacokinetics/pharmacodynamics (PK/PD), safety, efficacy, or immunogenicity [35]. Attributes deemed high risk for any one of these categories should be classified as high priority for orthogonal assessment [35].
The relationship between analytical techniques used to characterize a complex biological product, such as an engineered antibody, is multifaceted. The following diagram maps these methods as either orthogonal or complementary based on the attributes they measure:
For biosimilar development, the FDA emphasizes a "comparative analytical assessment" [35]. If differences between the proposed biosimilar and the reference product are observed, sponsors must provide a scientific justification and risk assessment explaining why these differences do not preclude a demonstration of high similarity. In some cases, resolving these differences may require manufacturing process changes, followed by re-analysis using the same orthogonal methods to demonstrate that the differences have been resolved [35].
In conclusion, a well-designed orthogonal analytical toolbox is indispensable for navigating the complex landscape of biological product development. By employing independent methods to cross-verify critical quality attributes, scientists can build a robust and defensible data package that ensures product quality, facilitates regulatory approval, and ultimately guarantees the safety and efficacy of life-changing medicines for patients.
Extended characterization and forced degradation studies are critical, systematic approaches used in the development of biopharmaceuticals to understand the intrinsic stability of drug substances and products. By employing conditions more severe than accelerated stability protocols, these studies rapidly identify potential degradation pathways and products, providing essential insights for formulation development, manufacturing process control, and establishing stability-indicating analytical methods. When framed within the context of demonstrating comparability for biological products, a well-executed forced degradation study becomes a powerful tool. It can reveal subtle differences in degradation profiles between pre- and post-change products, supporting a justification that a manufacturing change has not adversely impacted the product's safety, identity, purity, or potency [39] [8] [40].
Biological products, including recombinant monoclonal antibodies (mAbs), are complex macromolecules susceptible to a variety of degradation pathways throughout their lifecycle—from manufacturing and storage to shipping and administration. Unlike small molecules, biologics are defined not only by their chemical structure but also by their higher-order structure, which is critical for biological function. Degradation can negatively affect product quality, safety, and efficacy, making its detection and understanding paramount [39].
Extended characterization provides a deep profile of the molecule's attributes under normal conditions, while forced degradation studies proactively challenge these attributes under controlled, aggressive stress conditions. The data generated are fundamental for Critical Quality Attributes (CQA) assessment, manufacturability evaluation, and, crucially, for comparability studies [39]. As per regulatory guidance from the FDA and EMA, demonstrating comparability after a manufacturing change requires a comprehensive analytical comparison, and forced degradation serves as a stress test that can uncover differences not readily apparent under standard testing conditions [8].
Purpose and Application in Comparability Assessments
Forced degradation studies support the entire lifecycle of a biologic therapeutic. Their purposes are multifaceted and align directly with the needs of a successful comparability assessment [39] [8].
Table 1: Purposes of Forced Degradation Studies in Biologics Development [39] [40]
| Purpose | Rationale and Role in Comparability |
|---|---|
| Manufacturability Evaluation | Evaluates the propensity of multiple candidates or different batches to degrade under relevant process conditions. For comparability, it assesses the intrinsic stability of the product before and after a change. |
| Formulation Development | Identifies optimal buffers, excipients, pH, and storage conditions to provide long-term stability, ensuring that a formulation change does not compromise stability. |
| Stability-Indicating Method Development | Using degraded samples to test and validate analytical methods ensures they can monitor degradation products that may arise during shelf-life. This is critical for detecting potential new impurities post-change. |
| Degradation Pathway Elucidation | Characterizes degradation products to define major pathways (e.g., aggregation, deamidation). A shift in pathways after a manufacturing change can indicate a lack of comparability. |
| CQA Assessment and Variant Isolation | Generates specific modifications (e.g., oxidized or clipped species) at higher abundance, facilitating their identification and qualification. This helps determine if a new variant impacts safety/efficacy. |
| Comparability Evaluation | Differences that are undetectable by release assays can become apparent under stress. Similar degradation profiles and kinetics between pre- and post-change product provide high assurance of comparability. |
Within a comparability protocol, forced degradation acts as an accelerated and more sensitive assessment of product stability. It helps to answer the critical question: Could the manufacturing change have introduced a subtle alteration that affects the product's degradation behavior, and by extension, its stability profile and performance? [39] [8]. Successful demonstration of comparable degradation behavior under stress can often reduce the need for additional clinical studies to reaffirm safety and efficacy [8].
Major Degradation Pathways and Forcing Conditions
Understanding the specific degradation pathways a biologic may undergo is key to designing effective forced degradation studies. The commonly used conditions are chosen based on the likelihood of exposure during processing, packaging, shipping, and handling [39]. Each condition tends to accelerate specific degradation routes.
Table 2: Common Forced Degradation Conditions and Associated Degradation Pathways for mAbs [39] [40]
| Stress Condition | Major Degradation Pathways | Key Influencing Factors |
|---|---|---|
| High Temperature | Aggregation (soluble/insoluble), fragmentation (especially hinge region), deamidation (Asn/Gln), oxidation (Met), isomerization (Asp), formation of acidic variants. | pH, buffer species, ionic strength, protein concentration. |
| Freeze-Thaw | Formation of aggregates (primarily non-covalent dimers and multimers), precipitation. | Cooling/warming rates, pH, excipients (e.g., surfactants, sugars), protein concentration, container. |
| Agitation | Insoluble and soluble aggregation (covalent via disulfide scrambling or non-covalent), surface-induced denaturation. | Interface (air-liquid, solid-liquid), headspace, pH, presence of surfactants (e.g., polysorbate). |
| Low pH / High pH | Low pH: Fragmentation, aggregation, deamidation. High pH: Deamidation, disulfide scrambling (thioether formation), fragmentation, β-elimination. | Specific pH value, buffer, duration of exposure, temperature. |
| Oxidation | Oxidation of Methionine, Tryptophan, Histidine, and Cysteine residues; potential aggregation and loss of activity. | Oxidant type (e.g., H₂O₂, AAPH), concentration, temperature, presence of catalytic metals. |
| Photolysis | Side-chain oxidation (Trp, Tyr, His), backbone cleavage, disulfide bond disruption. | Light intensity and wavelength, clarity of solution container, photosensitizers. |
The following workflow diagram outlines a systematic approach to designing and executing a forced degradation study, from condition selection to data application.
Experimental Design and Methodologies
A successful forced degradation study requires a strategic balance between generating sufficient degradation and avoiding over-stressing, which can create irrelevant secondary degradation products.
Strategic Approach and Condition Selection
A general strategy begins with defining the goal, typically to achieve approximately 5-20% degradation for the drug substance to generate meaningful levels of products for identification and method development [40]. Studies are often initiated with a drug concentration of 1 mg/mL [40]. A minimal set of stress factors should include acid and base hydrolysis, thermal degradation, photolysis, and oxidation [40]. While a one-factor-at-a-time (OFAT) approach is common, Design of Experiments (DoE) is increasingly recognized for its ability to create more variance in the data set by combining stress factors, which helps reduce correlation structures between co-occurring modifications and enables more robust statistical analysis for establishing structure-function relationships [41].
Table 3: Example Experimental Conditions for Forced Degradation Studies [39] [40]
| Degradation Type | Common Experimental Conditions | Typical Duration & Sampling |
|---|---|---|
| Hydrolysis | 0.1 M HCl or 0.1 M NaOH; various pH buffers (e.g., pH 2, 4, 6, 8). | 40°C or 60°C; sample at 1, 3, 5 days. |
| Oxidation | 0.1% - 3% H₂O₂; radical initiators (e.g., AAPH, AIBN). | 25°C or 40°C; sample at 1, 3, 5 days (shorter for H₂O₂, e.g., 24h). |
| Thermal | Solid-state or solution state at elevated temperatures (e.g., 40°C, 60°C, 80°C) with/without controlled humidity. | Sample at 1, 3, 5 days and up to 2 weeks. |
| Photolytic | Exposure to UV (320-400 nm) and visible light per ICH Q1B guidelines (e.g., 1x and 3x ICH exposure). | Sample at 1, 3, 5 days. |
| Physical Stress | Multiple freeze-thaw cycles (e.g., -20°C to 25°C); agitation (shaking, stirring). | 1-10 cycles; 1-72 hours of agitation. |
Analytical Techniques for Monitoring Degradation
A suite of orthogonal analytical techniques is required to detect and characterize the diverse range of degradation products.
- Size-Based Methods: Size-Exclusion Chromatography (SEC) is the primary workhorse for quantifying soluble aggregates and fragments. Capillary Electrophoresis-SDS (CE-SDS) under reduced and non-reduced conditions provides detailed information on fragmentation and incomplete disulfide bonding, distinguishing covalent from non-covalent aggregates [39].
- Charge-Based Methods: Ion-Exchange Chromatography (IEC) or imaged capillary isoelectric focusing (icIEF) are used to monitor charge variants resulting from deamidation, isomerization, sialylation, or C-terminal lysine processing. An increase in acidic variants is a common observation under thermal stress [39].
- Mass Spectrometry (MS): Liquid Chromatography-Mass Spectrometry (LC-MS) is indispensable for precise identification of modification sites (e.g., deamidation, oxidation) and elucidating the structure of degradation products [39].
- Biological Assays: Cell-based bioassays or binding assays (ELISA, SPR) are critical for determining if the observed physicochemical modifications translate to a loss of biological potency, a key consideration in comparability [42].
The Scientist's Toolkit: Key Reagents and Materials
The following table details essential materials and reagents used in forced degradation studies.
Table 4: Research Reagent Solutions for Forced Degradation Studies
| Reagent / Material | Function in Forced Degradation Studies |
|---|---|
| Hydrochloric Acid (HCl) / Sodium Hydroxide (NaOH) | Used to prepare acidic and basic solutions for hydrolytic stress studies at various concentrations (e.g., 0.1 M) and pH values. |
| Hydrogen Peroxide (H₂O₂) | A common chemical oxidant used to simulate oxidative stress, typically at concentrations ranging from 0.01% to 3%. |
| Azobisisobutyronitrile (AIBN) / AAPH | Radical initiators used to induce metal-free oxidative degradation via peroxyl radicals, simulating certain types of oxidative pathways. |
| Phosphate and Other Buffer Salts | Used to maintain specific pH conditions during stress studies, as pH is a critical factor influencing the rate and pathway of degradation. |
| Polysorbate 80 / 20 | Surfactants added to formulations to mitigate agitation-induced aggregation at the air-liquid interface during shaking stress studies. |
| Light Cabinets (ICH Q1B Compliant) | Equipment that provides controlled exposure to ultraviolet (UV) and visible light for photostability testing. |
| Stability Chambers / Ovens | Provide precise temperature and humidity control (e.g., 40°C/75% RH, 60°C) for thermal and humidity stress studies. |
Data Interpretation and Advanced Statistical Approaches
Interpreting forced degradation data for comparability requires more than a qualitative comparison of chromatograms. Advanced statistical tools are employed to derive objective conclusions.
Establishing Structure-Function Relationships
A primary goal is to link specific chemical modifications (structure) to changes in biological activity (function). Traditional OFAT studies often lead to multiple simultaneous modifications, making it difficult to pinpoint the causative agent for a loss of potency. The DoE approach, by creating a wider variation in modification patterns, allows for the use of multivariate statistical methods like Partial Least Squares (PLS) regression to model and identify which modifications are most predictive of changes in potency or other functional assays [41]. The following diagram visualizes this analytical process.
Stability Trend Analysis
For comparability, the degradation kinetics (rates of formation of aggregates or fragments) between pre- and post-change products should be comparable. Statistical tools like regression analysis and analysis of covariance (ANCOVA) are used to model degradation trends and ensure that the slopes of degradation profiles are statistically equivalent across different batches, providing a quantitative basis for claiming comparability [42].
Forced degradation studies are a regulatory expectation, though specific protocols are not prescribed. The FDA and EMA emphasize the need for these studies to understand degradation pathways and validate stability-indicating methods [39] [8]. In the context of comparability, as outlined in the FDA's 1996 guidance, a manufacturer may demonstrate that a product made after a manufacturing change is comparable to the pre-change product through extensive analytical, functional, and sometimes animal testing, potentially obviating the need for new clinical efficacy studies [8].
The data from forced degradation studies are presented in regulatory submissions to justify the proposed shelf life, support the validation of analytical procedures, and, most importantly, to build a compelling case for product comparability. A successful comparability assessment, underpinned by robust forced degradation data, provides regulatory agencies with the confidence that the manufacturing change has not adversely affected the quality, safety, or efficacy of the biological product [39] [8].
In conclusion, extended characterization and forced degradation studies are not merely a regulatory checkbox but a fundamental scientific exercise. They provide a deep understanding of a biologic's stability profile and serve as a sensitive, powerful tool for ensuring patient safety and product efficacy through successful comparability demonstrations across the product lifecycle.
For biopharmaceutical manufacturers, the journey from drug discovery to commercial product is rarely linear. Throughout a product's lifecycle, changes in manufacturing processes, scales, or sites are often necessary due to supply chain demands, process optimization, and scaling requirements [29]. According to the ICH Q5E guideline, the fundamental goal of a comparability study is to establish that the pre-change and post-change biological products are highly similar and that the manufacturing process changes have no adverse impact on the product's quality, safety, or efficacy [1]. Demonstrating comparability is not about proving the products are identical, but rather providing scientific evidence that any differences in quality attributes do not adversely affect safety or efficacy [29]. This whitepaper explores the central role of High-Resolution Accurate Mass Spectrometry (HRAM) and orthogonal biophysical techniques in providing the definitive analytical evidence required for successful comparability assessments.
High-Resolution Accurate Mass Spectrometry (HRAMS) is an analytical technique that determines a sample's molecular weight and chemical composition with exceptional precision. It operates by ionizing a sample using techniques such as electrospray ionization (ESI), separating these ions in a mass analyzer based on their mass-to-charge ratio (m/z), and then detecting them. The "high-resolution" aspect refers to the mass analyzer's ability to separate ions with very similar m/z ratios, providing extremely precise measurements of an ion's mass [43]. This capability is fundamental for the detailed characterization required in comparability studies.
HRAM Mass Spectrometry: Fundamental Principles and Technical Advantages
HRAM Mass Spectrometry represents a significant advancement over traditional low-resolution MS. The key differentiator is its high resolving power, which allows it to distinguish between ions of very similar mass, effectively separating isobaric compounds that would co-elute and be misidentified by other techniques [43]. The "accurate mass" capability provides measurements precise enough to determine elemental compositions, a critical function for identifying unknown impurities or confirming the structure of biomolecules.
The primary technical advantages of HRAM MS include:
- Unparalleled Specificity and Sensitivity: HRAM MS can detect and accurately identify trace-level compounds within complex biological matrices, with some applications achieving detection limits in the high-attomole range [44].
- Comprehensive Data Acquisition: Unlike targeted methods, HRAM MS can perform full scanning while maintaining quantitative precision, enabling the simultaneous identification of anticipated and unanticipated analytes [45].
- Orthogonal Confirmation: The high-resolution and accurate mass data provide a second dimension of confirmation beyond retention time, increasing confidence in identifications for regulatory submissions [46].
Table 1: Key HRAM Mass Analyzers and Their Characteristics in Biopharmaceutical Analysis
| Mass Analyzer Type | Resolving Power | Key Strengths | Common Applications in Biologics |
|---|---|---|---|
| Orbitrap | Up to 500,000+ | Ultra-high resolution, high mass accuracy, multiplexed capability | Host Cell Protein (HCP) identification, post-translational modification (PTM) analysis [47] [46] |
| Time-of-Flight (TOF) | 40,000-80,000 | Fast acquisition speed, high sensitivity | Impurity profiling, metabolite identification, sequence variant analysis [29] |
| Quadrupole-Orbitrap | 140,000-500,000 | High resolution with precursor isolation, targeted quantification | Targeted quantitation of leachables, structure elucidation of degradants [45] |
Core Applications in Biologics Comparability Studies
Host Cell Protein (HCP) Identification and Monitoring
Host Cell Proteins are process-related impurities that can compromise drug safety and efficacy through immunogenic responses or enzymatic degradation of the active pharmaceutical ingredient [47] [46]. While ELISA has traditionally been used for HCP quantification, it lacks the specificity to identify individual HCPs and may suffer from antibody coverage limitations [47]. LC-HRAM MS/MS has emerged as a powerful orthogonal technique that provides sequence-specific identification and monitoring of individual HCPs throughout the downstream purification process [47] [46].
A robust UHPLC-HRAM MS/MS method for HCP analysis typically involves:
- Native Digestion: Utilizing trypsin digestion under nondenaturing conditions where the therapeutic protein remains largely intact while HCPs are digested, effectively reducing the dynamic range for MS detection [47].
- High-Separation Chromatography: Using long UHPLC C18 columns (e.g., 2.1 mm × 250 mm) to increase loading capacity and separation efficiency [47].
- Data-Dependent HRAM MS/MS Acquisition: Each full MS scan is followed by multiple MS/MS scans of the most intense precursor ions. High-resolution MS/MS scans (e.g., 30,000 resolution) with long maximum ion injection times (e.g., 150 ms) enhance sensitivity for low-abundance HCP peptides [47].
- Advanced Data Processing: Using multiple database search algorithms (e.g., Sequest HT and CHIMERYS) increases HCP identification coverage. Acceptance criteria typically include a 1% false discovery rate at the protein level and at least two unique peptides per protein [47].
In a case study assessing HCP clearance for an in-house trastuzumab product, an analytical flow UHPLC-HRAM MS/MS method successfully demonstrated the efficiency of a new polishing purification resin. The method identified 380 HCPs in the Protein A pool, which were reduced to just 78 HCPs after polish purification, with most remaining HCPs showing significantly decreased abundances [47].
Analysis of Extractables and Leachables from Single-Use Systems
Single-use technologies are increasingly used in biopharmaceutical manufacturing, but their plastic components can be a source of chemical contamination through extractable and leachable compounds (E&Ls) [48]. Characterizing these compounds is a critical step in establishing product quality and demonstrating comparability after process changes.
An optimized HRAM MS method for identifying polymer additives involves:
- Accelerated Solvent Extraction (ASE): A powerful extraction technique optimized using design of experiments. Key variables include solvent type (ethyl acetate or cyclohexane), temperature (90-100 °C), pressure (1500 psi), and extraction time (30 minutes in 2 cycles) [48].
- Ultra-High Performance Liquid Chromatography (UHPLC): For separating complex mixtures of extracted compounds.
- Orbitrap-Based High-Resolution Accurate Mass Spectrometry: Enables confident identification of additives and their degradation products. In one study, this approach identified more than 100 additives and degradation products from multilayer polymer systems used in single-use bags [48].
Characterization of Reactive Carbonyl Compounds
Reactive carbonyl compounds are another class of impurities that can form through various pathways and potentially impact product quality and safety. These electrophilic compounds can covalently bind to nucleophilic sites in proteins, inducing modifications that may affect therapeutic protein stability or function [44].
A specialized HRAM MS method for characterizing these compounds involves:
- Derivatization with 2,4-Dinitrophenylhydrazine: This step increases the molecular weight of small, polar aldehydes, improving their chromatographic retention and ionization efficiency during LC-MS analysis [44].
- Neutral Loss Triggering MS3 Fragmentation: A unique data-dependent acquisition strategy that triggers further fragmentation based on the diagnostic neutral loss of a hydroxyl radical, which is characteristic of DNPH-derivatized carbonyls in positive ionization mode [44].
- Isotope Labeling for Relative Quantitation: Using deuterated d3-DNPH enables relative quantitation to assess changes in carbonyl compound levels before and after process changes [44].
Essential Research Reagent Solutions
A successful comparability study requires carefully selected reagents and materials to ensure reliable and reproducible results.
Table 2: Key Research Reagents and Materials for HRAM MS-based Comparability Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Trypsin (Sequencing Grade) | Protein digestion for peptide mapping | Native digestion protocol for HCP analysis; sample preparation for sequence variant analysis [47] |
| d3-DNPH (Deuterated) | Isotopic derivatization agent | Relative quantitation of reactive carbonyl compounds; tracking process-related impurities [44] |
| DNPH (2,4-Dinitrophenylhydrazine) | Carbonyl compound derivatization | Analysis of reactive carbonyl impurities in biologics formulations [44] |
| POROS Chromatography Resins | Downstream purification | HCP clearance studies; polishing step evaluation (e.g., Caprylate Mixed-Mode resin) [47] |
| Strata-X SPE Cartridges | Solid-phase extraction | Sample clean-up and concentration for impurity analysis; partial purification of hydrazone products [44] |
| NISTmAb Reference Material (RM 8671) | Method development and standardization | System suitability testing; HCP method performance evaluation [47] |
Experimental Workflows for Comparability Assessment
Comprehensive HCP Clearance Workflow
The following diagram illustrates the integrated workflow for assessing host cell protein clearance during downstream process changes, a critical component of comparability studies.
Workflow Title: HCP Clearance Assessment for Comparability
This workflow demonstrates how native digestion coupled with HRAM MS effectively addresses the significant dynamic range challenge in HCP analysis. By maintaining the therapeutic antibody in a mostly intact state while digesting HCPs, the method enhances the detection of low-abundance HCPs that would otherwise be masked by the dominant product [47]. The use of a long UHPLC column increases loading capacity and separation efficiency, while the HRAM MS system provides the sensitivity and specificity needed to identify and quantify individual HCPs at low ppm levels.
Extractables and Leachables Profiling Workflow
The assessment of extractables and leachables is particularly important when implementing changes in manufacturing equipment or container closure systems.
Workflow Title: E&L Profiling for Process Changes
This extractables and leachables workflow highlights the comprehensive characterization needed when changing manufacturing components. The accelerated solvent extraction, optimized through design of experiments, efficiently extracts additives from complex multilayer polymer systems [48]. The non-targeted analysis capability of HRAM MS is crucial for identifying both anticipated and unanticipated compounds, providing a complete impurity profile that supports the safety assessment of the post-change product.
Regulatory Integration and Future Perspectives
Regulatory agencies are increasingly recognizing mass spectrometry as a reliable tool for quality control in drug manufacturing [46]. The FDA's guidance on therapeutic protein biosimilars emphasizes the importance of comparative analytical studies in demonstrating biosimilarity, a specialized form of comparability assessment [22]. When submitting comparability data, it is essential to pre-define both quantitative and qualitative acceptance criteria for extended characterization methods in the study protocol to avoid subjective interpretation of complex results [29].
The future of HRAM MS in comparability studies is closely tied to several technological advancements:
- Artificial Intelligence and Advanced Data Processing: AI supports more reliable analysis by improving spectral data interpretation and reducing false results [46]. Using multiple search algorithms (e.g., Sequest HT and CHIMERYS) has been shown to increase HCP identification coverage [47].
- Increased Sensitivity and Throughput: Instrument manufacturers continue to develop mass spectrometers with higher sensitivity, faster scan rates, and improved robustness, making HRAM MS more accessible for routine analysis in controlled environments [43] [46].
- Standardized Workflows for Regulatory Submission: As regulatory agencies gain more experience with HRAM MS data, standardized approaches for method validation and data presentation are emerging, facilitating smoother regulatory reviews [22] [46].
HRAM Mass Spectrometry, particularly when integrated with orthogonal biophysical techniques, provides an indispensable toolkit for demonstrating comparability of biological products after manufacturing changes. Its unparalleled resolution, mass accuracy, and sensitivity enable scientists to detect and characterize subtle differences in product quality attributes that older technologies would miss. As the biopharmaceutical industry continues to evolve with increasingly complex modalities and accelerated development timelines, the central role of HRAM MS in ensuring product quality, safety, and efficacy while facilitating necessary manufacturing innovations will only become more pronounced.
The development and manufacturing of biological products are inherently dynamic processes. Changes to the manufacturing process are inevitable throughout a product's lifecycle, driven by the need for process efficiency improvements, increases in production scale, raw material adjustments, evolving regulatory requirements, or manufacturing site transfers [29] [28]. Unlike small molecule drugs, biologics are large, complex molecules produced using living systems, making them highly susceptible to alterations in their quality attributes based on manufacturing conditions [28]. Even seemingly minor changes can significantly impact the product's safety, identity, purity, and potency [8].
The concept of comparability has emerged as a fundamental regulatory and scientific principle to manage these manufacturing changes. Comparability assessments demonstrate that a biological product remains highly similar before and after a manufacturing change, ensuring that no adverse impacts on safety or efficacy have occurred [29]. According to the ICH Q5E guideline, demonstrating comparability does not require the pre- and post-change materials to be identical, but they must be highly similar, with sufficient knowledge to ensure that any differences in quality attributes have no adverse impact upon safety or efficacy of the drug product [29]. These assessments represent a risk-based approach that evolves throughout the product lifecycle, from early development through commercial stages, with the level of evidence required being phase-appropriate [49] [28].
Regulatory Framework and Foundational Principles
The regulatory foundation for comparability assessments was established through initiatives by major regulatory agencies globally. The U.S. Food and Drug Administration (FDA) pioneered the approach in the late 1980s and early 1990s, formalizing it in the 1996 "Demonstration of Comparability of Human Biological Products" guidance [8] [18]. This was followed by the International Council for Harmonisation (ICH) Q5E guideline, which has become the globally accepted standard for evaluating manufacturing process changes for biologics produced by recombinant technology [18]. The European Medicines Agency (EMA) also developed complementary guidelines, creating a comprehensive regulatory framework that enables both the management of manufacturing changes and the development of biosimilars [18].
The fundamental principle underlying comparability assessments is that function follows form – the clinical properties of a biologic are determined by its structural characteristics [18]. The assessment aims to demonstrate that pre- and post-change products are sufficiently alike that their clinical properties will be indistinguishable. This approach has been validated through decades of successful implementation, with most biologics undergoing multiple comparability assessments throughout their lifecycles [18]. The robustness of this system rests on four key advancements: clear and convergent regulatory guidelines, risk-based weighting of analytical data, progressive improvements in analytical methods, and advanced understanding of post-translational modifications [18].
Table 1: Key Regulatory Guidelines for Comparability Assessments
| Guideline | Issuing Authority | Scope and Application |
|---|---|---|
| ICH Q5E | International Council for Harmonisation | Comparability of Biotechnological/Biological Products Subject to Changes in Their Manufacturing Process |
| Comparability Protocols for Post-approval Changes | U.S. FDA | Chemistry, Manufacturing, and Controls Information in an NDA, ANDA, or BLA |
| Guideline on Comparability of Biotechnology-Derived Medicinal Products | European Medicines Agency | Comparability after a change in the manufacturing process |
| Biological Assay Validation <1033> | United States Pharmacopeia | Validation of biological assays used in comparability assessments |
Phase-Appropriate Approach to Comparability
Early Development (Preclinical to Phase I)
During early development, the primary objective is to establish baseline product characteristics and identify critical quality attributes (CQAs) with limited historical data and product knowledge [49]. At this stage, manufacturers typically work with platform characterization methods and may screen forced degradation conditions to understand the molecule's basic behavior [29] [28]. The approach is necessarily more flexible, with fewer batches available for comparison – often single batches of pre- and post-change material may be sufficient to establish biophysical characteristics using platform methods [29].
The testing strategy at this stage focuses on qualitative or retrospective approaches to identify differences between compared materials rather than rigorous statistical comparisons [49]. It is often sufficient to outline the testing strategy and product quality expectations without pre-defined comparability assessment criteria. The emphasis is on learning and molecular understanding rather than comprehensive validation [29]. Forced degradation studies at this stage help analysts gain preliminary understanding of the molecule, inform analytical test method limits, and prepare for more formal forced degradation studies later in development [29].
Mid-Stage Development (Phase II to Early Phase III)
As development progresses into mid-stages, the comparability approach becomes more structured and rigorous. The product and process knowledge has increased, and critical quality attributes are better defined [49]. During this phase, manufacturers typically implement more extensive characterization, including confirmation of forced degradation conditions that cover a full scale of potential degradation pathways such as oxidative stress, thermal stress, sheer stress, and photostability [28].
The number of batches used for comparability assessment increases, with head-to-head testing of multiple pre- and post-change batches becoming more common [29]. Analytical methods become more molecule-specific rather than relying solely on platform methods. The understanding of post-translational modifications (PTMs) deepens, and their impact on product quality and functionality becomes a greater focus [18]. At this stage, predefined acceptance criteria become more important, and the analytical comparability exercise is expected to detect discrete differences in selected quality attributes [6].
Late-Stage to Commercial (Phase III to Post-Approval)
At late development and commercial stages, comparability assessments reach their highest level of rigor and comprehensiveness. The "gold standard" format of three pre-change versus three post-change batches is typically employed to demonstrate robust comparability [29]. The assessment includes extended characterization using orthogonal analytical techniques, real-time stability studies, and comprehensive forced degradation studies [28].
The analytical methods used at this stage provide a finer level of detail that is orthogonal to release methods, especially for critical quality attributes [29]. The expectation for commercial products is that manufacturers have demonstrated sufficient control over the process so that delivery of high-quality product is ensured despite manufacturing changes [29]. Any observed differences between processes must be thoroughly explained based on deep molecular characterization and understanding [29].
Table 2: Evolution of Comparability Strategies Across Development Phases
| Development Phase | Batch Requirements | Analytical Approach | Stability Assessment | Acceptance Criteria |
|---|---|---|---|---|
| Early Development (Preclinical-Phase I) | Single batches often sufficient | Platform methods; screening forced degradation conditions | Limited accelerated stability | Qualitative or retrospective; may lack pre-defined criteria |
| Mid-Stage (Phase II-early III) | Multiple batches; head-to-head testing becoming common | Molecule-specific methods emerging; confirmation of forced degradation conditions | More extensive accelerated stability | Pre-defined criteria becoming important |
| Late-Stage to Commercial (Phase III-Post-approval) | Gold standard: 3 pre- vs 3 post-change batches | Extended characterization with orthogonal methods; comprehensive forced degradation | Real-time and accelerated stability | Rigorous, statistically-based criteria |
Experimental Design and Methodologies
Risk Assessment as Foundation
A risk-based approach forms the cornerstone of effective comparability study design [49] [28]. The risk assessment process begins with a thorough understanding of the proposed manufacturing change and its potential impact on product quality attributes. This involves systematic evaluation of which attributes might be affected based on the type of change implemented [6]. For instance, a change in the expression system might potentially affect glycosylation patterns, while modifications to purification processes might impact purity profiles or higher-order structure [6].
The risk assessment outcome directly drives the extent of analytical testing and the selection of analytical techniques [49]. Risk-based thinking allows for a more flexible, less rigid approach to regulation, maintaining focus on variables that truly impact quality while de-emphasizing those that do not [18]. This approach leverages existing product and process knowledge, including product-specific data, cross-product knowledge, clinical data, internal findings, analytical and biophysical results, and published literature [28].
Analytical Methodologies and Techniques
The analytical toolkit for comparability studies has evolved significantly, with progressive improvements in methods allowing for ever more sensitive and precise characterization [18]. A comprehensive comparability study typically employs a panel of orthogonal analytical techniques, where data from different methods confirm and amplify each other [18]. These methods can be categorized based on the product attributes they assess.
For primary structure analysis, techniques include peptide mapping with LC-MS/MS, amino acid analysis, and terminal sequencing using MALDI-MS and high-resolution mass spectrometry [50]. These methods confirm the amino acid sequence and identify any sequence variants or modifications. Higher-order structure analysis employs orthogonal techniques such as circular dichroism (CD), nuclear magnetic resonance (NMR), Fourier-transform infrared spectroscopy (FTIR), intrinsic fluorescence studies, and ultraviolet-visible spectroscopy [50].
Post-translational modification analysis is particularly critical for biologics, as PTMs like glycosylation significantly impact pharmacokinetics and biological functions [18]. Glycosylation studies typically include determination of neutral and amino monosaccharides, sialic acids, assessment of glycoform distribution, and glycan structure elucidation using technologies such as MALDI-TOF mass spectrometry, HPAEC-PAD, HILIC-FLD, or CE-LIF [50]. For purity and impurity profiles, techniques include size exclusion chromatography (SEC), capillary electrophoresis (CE-SDS), ion exchange chromatography (IEC), and assays for host cell proteins (HCP), DNA, and Protein A residuals [5].
Biological activity assessment forms a critical component, utilizing cell-based assays, binding affinity studies, and potentially Fc functionality tests for antibodies [5]. The selection of methods should be both targeted to measure differences in potentially affected product quality attributes and broad enough to allow detection of possible but unexpected consequences [49].
Stability Assessment in Comparability
Stability studies form an integral part of comparability assessments, providing critical information about the degradation pathways and shelf-life predictions for the post-change product [28]. The stability assessment typically includes real-time stability studies under recommended storage conditions, accelerated stability studies under stressed conditions, and forced degradation studies that deliberately stress the product to understand its degradation mechanisms [29] [28].
Forced degradation studies subject the product to various stress conditions including thermal stress, oxidative stress, pH variations, light exposure, and mechanical stress [29]. These studies serve to compare the degradation kinetics and degradation pathways between pre- and post-change products [5]. The results demonstrate quality alignment between the two processes through analysis of trendline slopes, bands, and peak patterns [29]. When the degradation profiles are highly similar, it provides strong evidence that the manufacturing change has not altered the fundamental stability characteristics of the product [29].
Table 3: Research Reagent Solutions for Comparability Assessments
| Reagent/Category | Function in Comparability Assessment | Key Applications |
|---|---|---|
| Reference Standards | Qualified pre-change material for head-to-head comparison | All analytical testing; benchmark for quality attributes |
| Cell-Based Assay Reagents | Assessment of biological activity and potency | Functional comparability of mechanism of action |
| Chromatography Columns | Separation and analysis of product variants and impurities | SEC, IEC, HIC, RP-HPLC for purity and heterogeneity |
| Mass Spectrometry Reagents | Detailed structural characterization | Peptide mapping, PTM analysis, sequence confirmation |
| Enzymes for Digestion | Controlled fragmentation for structural analysis | Peptide mapping (trypsin, pepsin, etc.) |
| Glycan Analysis Reagents | Characterization of glycosylation patterns | Release and analysis of N-linked and O-linked glycans |
| Electrophoresis Standards | Migration reference for size and charge variants | CE-SDS, iCIEF, cIEF methodologies |
Implementation and Best Practices
Protocol Development and Acceptance Criteria
A well-constructed comparability protocol is essential for successful comparability assessment. This protocol should be drafted well in advance – approximately six months before manufacture of new batches – and must describe all process changes, assess their effects on the product, define all planned analyses along with their acceptance criteria, describe stability studies, and include all available supportive data [6]. The protocol development should follow a systematic approach that takes into consideration requirements of ICH Q5E, Q8, and Q9 guidances [6].
Establishing scientifically-justified acceptance criteria is one of the most challenging aspects of comparability protocol development. These criteria should be established prospectively and based on historical data of process and product quality [5]. For quantitative methods, acceptance criteria typically define acceptable ranges based on statistical analysis of historical data, while for qualitative methods, criteria may focus on comparable patterns or peak identities [5]. The set acceptance criteria cannot be lower than the quality standard unless scientifically justified [5]. During early-stage development, it can be challenging to set meaningful comparability assessment criteria, and it may be sufficient to outline testing strategy and product quality expectations without pre-defined criteria [49].
Material Selection and Study Design
The selection of appropriate materials for comparability studies is critical for generating meaningful data. The pre- and post-change batches should be manufactured as close together as possible to avoid natural age-related differences, which could convolute the results [29]. It is recommended to use the latest available batches that have passed release criteria to avoid even the appearance of "cherry-picking" [29].
The number of batches included in the study depends on the product development stage, type of changes, and the understanding of the process and product [5]. For major changes, ≥3 batches of commercial-scale samples are generally selected after the change; for medium changes, that number is 3; while minor changes can be studied with fewer batches, generally ≥1 batch [5]. The selection strategy should be defined in the comparability protocol or study plan before testing begins [29].
The testing strategy should leverage both historical data from release, stability, and in-process tests for comparison, as well as head-to-head experiments using cryopreserved samples when new purity or potency tests are developed that weren't available when the pre-change material was analyzed [49]. Extended characterization methods typically require head-to-head comparative analysis since there is not enough historical data for statistical comparison [5].
Phase-appropriate comparability strategies represent a scientific, risk-based framework for managing manufacturing changes throughout the biologic product lifecycle. From early development through commercial stages, the approach evolves in rigor and comprehensiveness, balanced against the level of product and process knowledge and the associated patient risk. The foundation remains analytical comparability, with increasing emphasis on orthogonal methods, extended characterization, and stability assessment as the product advances.
The successful implementation of these strategies requires careful planning, robust protocol development, appropriate material selection, and scientifically-justified acceptance criteria. By adopting a phase-appropriate approach, manufacturers can effectively manage process changes while maintaining product quality and regulatory compliance. As analytical technologies continue to advance and regulatory expectations evolve, the comparability paradigm will continue to mature, enabling more efficient lifecycle management of biological products while ensuring consistent delivery of safe and effective medicines to patients.
Navigating Complexities: Risk Mitigation and Strategy Optimization for Challenging Scenarios
For researchers and developers of biological products, expedited development programs such as Fast Track (FT), Breakthrough Therapy (BT), Regenerative Medicine Advanced Therapy (RMAT), and Accelerated Approval (AA) present a critical opportunity to address unmet medical needs for serious conditions. These pathways, particularly Accelerated Approval, can reduce development time by more than two years compared to traditional routes, which sometimes span 15+ years [51]. However, this compressed timeline introduces significant challenges for Chemistry, Manufacturing, and Controls (CMC) activities, where regulatory safety and quality requirements are not relaxed despite the accelerated pace [51]. For biological products, demonstrating comparability throughout development becomes especially critical as manufacturing processes evolve rapidly toward commercial scale. Recent 2025 draft guidances from FDA's Center for Biologics Evaluation and Research emphasize these challenges specifically for cell and gene therapies, highlighting expanded flexibilities and updated examples for navigating expedited programs [52].
CMC Challenges in Compressed Timelines
Primary Constraints and Risks
Expedited programs compress development activities that traditionally occur sequentially into parallel processes, creating specific pressure points for CMC teams.
Table 1: Key CMC Challenges in Expedited Development Programs
| Challenge Area | Specific Risks | Impact on Development |
|---|---|---|
| Manufacturing Process | Expedited scale-up, formulation changes for commercial supply [51] | Potential supply chain disruptions, inadequate process characterization |
| Manufacturing Sites | Technology transfer under pressure, facility changes [51] | Comparability demonstration complexities, validation delays |
| Stability Data | Limited registration stability data at submission [51] | Reduced product understanding, potential shelf-life limitations |
| Method Development | Limited dataset for commercial method validation [51] | Risk of method inadequacy, specification justification challenges |
| Process Changes | Limited adaptability once "to-be-marketed" formulation is locked [51] | Difficulty incorporating improvements, comparability burden |
The Accelerated Approval pathway, which can be based on a surrogate endpoint reasonably likely to predict clinical benefit, introduces particular CMC challenges as sponsors must quickly transition from clinical to commercial manufacturing [53]. The compressed timeline from New Drug Application (NDA) or Biologics Licensing Application (BLA) submission to approval places tremendous pressure on teams to select manufacturers and finalize product manufacturing plans [51].
Regulatory Expectations for CMC Readiness
Recent FDA draft guidance emphasizes that appropriate product quality controls, grounded in defined critical quality attributes and critical process parameters, must be in place early in development [52]. The agency "strongly encourages sponsors to discuss CMC readiness, including any perceived manufacturing challenges" through the increased interactions that expedited programs provide [52]. This is particularly crucial for biological products where demonstrating comparability between the product used to generate preliminary clinical evidence and the product planned for clinical development is essential [52].
Strategic Approaches for CMC Success
Proactive Planning and Risk Assessment
Successful navigation of expedited CMC challenges begins with proactive planning well before regulatory designation is granted. Sponsors should:
- Initiate manufacturing discussions early throughout development, as these should be "a priority from the beginning" [51]
- Create comprehensive risk assessments that identify potential manufacturing and supply chain vulnerabilities [51]
- Select manufacturers who align with development goals and timeline, ensuring compliance history and inspection readiness [51]
- Consider commercial launch requirements prior to scaling up product development and plan for technology transfer to final commercial facilities [51]
Engaging with FDA review divisions during development about the possibility of accelerated approval, including the use of planned endpoints, helps ease the burden of uncertainty after designation is granted [51].
Demonstrating Comparability Despite Limited Data
For biological products, demonstrating comparability between early clinical batches and commercial material is paramount. Strategies include:
- Tie planned commercial batches back to early development batches, particularly the toxicology batch, to show impurities remain within qualified safety limits [51]
- Document all changes comprehensively throughout development, capturing as much context as possible [51]
- Employ orthogonal analytical methods to characterize critical quality attributes when limited stability data exists
- Implement platform approaches where possible to leverage prior knowledge across similar products
Table 2: Stability Data Strategy for Expedited Programs
| Strategy Element | Implementation Approach | Risk Mitigation |
|---|---|---|
| Submission Timing | Provide updated stability data within 30 days of initial submission [51] | Maintain ongoing dialogue with health authorities |
| Data Package | Submit less than 12 months of data at time of submission if agreed with FDA [51] | Early engagement on stability protocol design |
| Post-approval Commitment | Plan for ongoing stability monitoring | Ensure continuous data generation |
Experimental Protocols for Comparability Assessment
Comprehensive Analytical Similarity Assessment
Establishing comparability for biological products requires a rigorous, multi-attribute analytical approach. The following protocol outlines key experiments:
Protocol 1: Extended Characterization Panel
- Purpose: Demonstrate similarity in critical quality attributes between pre- and post-change material
- Methods:
- Intact Mass Analysis: LC-MS under non-denaturing and denaturing conditions
- Higher Order Structure: Circular Dichroism (CD), Fourier-Transform Infrared Spectroscopy (FTIR)
- Biological Assays: Binding affinity (SPR/BLI), cell-based potency assays
- Purity and Impurities: CE-SDS, SEC-HPLC, product-related impurity profiling
- Acceptance Criteria: Statistically similar profiles within pre-defined equivalence margins
Protocol 2: Forced Degradation Studies
- Purpose: Demonstrate similar degradation pathways under stress conditions
- Methods:
- Thermal Stress: 2-8°C, 25°C, 40°C for predefined intervals
- Oxidative Stress: Incubation with 0.01-0.1% hydrogen peroxide
- Light Exposure: According to ICH Q1B guidelines
- Mechanical Stress: Agitation, freeze-thaw cycles
- Analysis: Compare degradation rates and profiles using primary stability-indicating methods
Process Characterization Design
Protocol 3: Scalability and Robustness Assessment
- Purpose: Ensure manufacturing process consistency across scales
- Methods:
- Parameter Ranging Studies: Deliberately vary critical process parameters beyond normal operating ranges
- Scale-Down Model Qualification: Demonstrate that small-scale models accurately predict manufacturing performance
- Residence Time Distribution Studies: For column chromatography and filtration operations
- Cell Culture Metabolic Analysis: Compare growth, viability, and metabolite profiles across scales
- Data Analysis: Multivariate analysis to identify significant scale-dependent factors
Figure 1: Comparability Study Workflow for Expedited Programs
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biological Comparability Studies
| Reagent/Material | Function | Application in Comparability |
|---|---|---|
| Reference Standards | Benchmark for quality attributes | Primary comparator for analytical similarity assessment |
| Cell-Based Potency Assays | Measure biological activity | Critical for demonstrating functional equivalence |
| Characterized Cell Banks | Consistent substrate for production | Ensure manufacturing consistency across scales |
| Platform Chromatography Resins | Purification with established performance | Reduce method development time, leverage prior knowledge |
| Critical Reagent Qualification Kits | Standardize assay performance | Ensure analytical method robustness throughout development |
Navigating Regulatory Interactions
The increased engagement with regulatory authorities that expedited programs provide represents a significant opportunity for sponsors. FDA encourages early discussions about CMC challenges, particularly for complex biological products [52]. Key interaction points include:
- Pre-BTD/RMAT meetings: Discuss preliminary CMC strategy and potential challenges
- Type C meetings: Address specific technical questions as they arise during development
- Pre-NDA/BLA meetings: Align on submission content and format, including stability data packages
- Post-approval commitment discussions: Plan for ongoing studies and manufacturing improvements
Recent draft guidances indicate FDA's willingness to consider innovative approaches to CMC development, provided sponsors maintain rigorous quality standards and comprehensive documentation [52].
Successfully navigating CMC constraints in expedited development programs requires strategic foresight, proactive planning, and robust scientific approaches to demonstrate comparability. By implementing the methodologies and strategies outlined in this guide, researchers and drug development professionals can accelerate breakthrough biological products to patients in need while maintaining the rigorous quality standards required for therapeutic products. The key lies in leveraging increased regulatory interactions, implementing risk-based approaches, and maintaining comprehensive documentation throughout the development lifecycle.
This technical guide provides a structured framework for addressing minor quality attribute differences during comparability assessments for biological products. For researchers and drug development professionals, justifying that a process change does not adversely impact product quality, safety, or efficacy requires robust analytical strategies and evidence-based decision-making. This whitepaper outlines systematic approaches for evaluating minor differences within the context of Critical Quality Attributes (CQAs), leveraging risk assessment methodologies, and implementing appropriate statistical and scientific justification protocols. By integrating comparability exercises and quality by design principles, this guide supports the demonstration that minor variations fall within an acceptable range of analytical similarity, ensuring regulatory compliance while advancing biological product development.
Demonstrating comparability after manufacturing process changes is a fundamental requirement in biological product development. According to regulatory guidelines, comparability assessments evaluate the potential impact of manufacturing changes on the quality, safety, and efficacy of biotechnological/biological products [1]. These assessments rely on comprehensive analytical characterization to determine whether pre-change and post-change products are sufficiently similar to preclude the need for additional clinical studies.
Critical Quality Attributes (CQAs) are defined as physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality [54]. For biologics, CQAs typically include molecular attributes such as glycosylation patterns, charge variants, biological activity, and higher-order structure, which potentially influence purity, potency, stability, immunogenicity, or pharmacokinetic profiles. Identifying these attributes early in product development enables better decision-making throughout the translation process and provides greater confidence that observed effects are reproducible in clinical phases [55].
When minor differences in quality attributes are detected during comparability exercises, a systematic, scientifically-justified approach to their interpretation is essential. This guide outlines the methodologies and experimental strategies for evaluating and justifying that such differences remain within acceptable boundaries and do not adversely impact product performance.
Regulatory Framework for Comparability Assessment
Foundational Principles
The ICH Q5E guideline establishes the fundamental principle for assessing comparability of biotechnological/biological products subject to changes in their manufacturing process [1]. This guideline provides a framework for collecting relevant technical information that serves as evidence that manufacturing process changes will not adversely impact the quality, safety, and efficacy of the drug product. The core objective is to demonstrate that the pre-change and post-change products are highly similar notwithstanding observed minor differences.
For biosimilar development, the FDA guidance recommends a stepwise approach beginning with extensive comparative analytical characterization between the proposed biosimilar and the reference product [22]. This analytical assessment serves as the foundation for a comprehensive comparison, and when successful, may reduce the necessary clinical data requirements. The guidance emphasizes that the goal of analytical studies is to demonstrate that the proposed biosimilar is highly similar to the reference product notwithstanding minor differences in clinically inactive components [22].
The Role of Critical Quality Attributes
Within the regulatory framework, CQAs provide the primary metrics for assessing comparability. As highlighted by the National Academies workshop on regenerative medicine, developing and validating assays for CQAs as early as possible in the pre-clinical product development process leads to better decision-making at each step along the translation pathway and generates greater confidence that an observed effect is reproducible in the clinical phase [55].
The risk-based approach to CQA identification and assessment, as outlined in ICH Q9, forms the basis for prioritizing quality attributes according to their potential impact on safety and efficacy [54]. This approach enables manufacturers to focus resources on attributes with the greatest potential clinical impact while establishing scientifically justified acceptance criteria for minor variations in less critical attributes.
Risk-Based Approach to Quality Attributes
CQA Identification and Classification
A systematic risk assessment process is essential for identifying and classifying quality attributes according to their criticality. The initial step involves defining potential CQAs (pCQAs) based on the Quality Target Product Profile (QTPP) and mechanism of action understanding [54]. For example, if Fc effector function is integral to the mechanism of action, specific Fc glycosylation variants would be considered pCQAs.
Quality attributes are typically categorized into three groups for analysis:
- Product-specific attributes: Structural and physio-chemical characteristics of the molecule (e.g., molecular size, amino acid sequence, glycosylation patterns, aggregation) [54].
- Process-related impurities: Characteristics influenced by process-associated factors that impact safety (e.g., host cell proteins, DNA, cell culture media components) [54].
- Obligatory CQAs: Attributes that certainly affect safety and efficacy (e.g., pH, concentration, osmolality, endotoxin levels) [54].
Table 1: Categorization of Quality Attributes for Risk Assessment
| Attribute Category | Examples | Risk Assessment Approach |
|---|---|---|
| Product-Specific Attributes | Molecular size, charge variants, glycosylation, aggregation | Structure-activity relationship studies, impact on biological activity and mechanism of action |
| Process-Related Impurities | Host cell proteins, DNA, media components | Safety and toxicology studies, clearance validation |
| Obligatory CQAs | Endotoxin levels, sterility, pH, osmolality | Verification against regulatory standards, typically not risk-assessed |
Risk Ranking and Filtering
A risk ranking and filtering approach is employed to assess the criticality of pCQAs with respect to their impact on bioactivity, pharmacokinetics, pharmacodynamics, immunogenicity, and safety [54]. This evaluation typically utilizes a scoring system based on two factors: impact and uncertainty.
While approaches vary among organizations, a common method uses a scale with up to 5 levels where impact and uncertainty factors are scored independently, with greater weight given to the impact factor [54]. The two values are multiplied to obtain a risk score for each product quality attribute, resulting in a listing of quality attributes along a criticality continuum.
Table 2: Example Risk Scoring Matrix for Quality Attributes
| Impact Score | Uncertainty Score | Risk Priority | Recommended Action |
|---|---|---|---|
| High (4-5) | Low (1-2) | High | Extensive characterization, tight acceptance criteria |
| Medium (3) | Medium (3) | Medium | Moderate characterization, justified ranges |
| Low (1-2) | High (4-5) | Medium to Low | Limited studies, science-based justification |
| Low (1-2) | Low (1-2) | Low | Standard monitoring, general acceptance criteria |
This risk assessment is performed iteratively throughout process development, with studies designed to enhance product knowledge and reduce uncertainty. The scoring system objective is to ensure consistency of the assessment approach throughout the product lifecycle [54].
Experimental Strategies for Comparative Analysis
Analytical Method Selection and Validation
The foundation of meaningful comparability assessment lies in employing validated analytical methods capable of detecting relevant differences in product quality attributes. As emphasized in regenerative medicine manufacturing, developing assays that generate comparable data allows for a better understanding of important product characteristics and facilitates learning from collective experiences [55].
Method validation should characterize an assay's precision, reproducibility, accuracy, robustness, sensitivity, specificity, dynamic range, response function, and limit of detection [55]. This comprehensive characterization builds confidence that measurements yield reliable data to support sound decision-making. When unexpected results occur, understanding these method parameters helps determine whether the observation stems from actual product changes or assay variability.
For comparability assessment, particular attention should be paid to analytical sensitivity to ensure methods can detect differences that may impact clinical performance. As noted in the NCBI workshop proceedings, "academic researchers will often not have a problem getting reproducible results from an assay in their laboratories, but when results of that assay are compared across laboratories, the results can vary considerably" [55]. Addressing this through inter-laboratory studies and standardized protocols is essential for reliable comparability assessment.
Study Design Considerations
Comparative analytical studies should be designed to comprehensively evaluate the similarity between pre-change and post-change products. The FDA guidance on biosimilar development recommends using an appropriate number of lots of the reference product to understand the range of quality attributes and their variability [22]. Similarly, for comparability assessments, multiple batches representing the historical manufacturing consistency and post-change material should be included.
The statistical approach should account for the natural variability of the manufacturing process and analytical methods. Appropriate statistical power should be considered to detect clinically meaningful differences while accounting for multiple comparisons where applicable. Experimental designs that incorporate orthogonal analytical methods provide more robust assessments of quality attribute similarity.
When designing comparability studies, consider the following elements:
- Sample size: Sufficient lots to understand process variability
- Reference standards: Well-characterized materials for assay calibration
- Orthogonal methods: Multiple techniques measuring the same attribute
- Forced degradation studies: To understand degradation pathways and profile similarities
- Accelerated stability studies: To compare degradation rates under stress conditions
Data Interpretation and Statistical Approaches
Establishing Acceptance Criteria
Acceptance criteria for quality attribute comparability should be established based on process capability, analytical method variability, and clinical relevance. According to regulatory guidance, acceptance criteria using known reference and patient samples should be established before clinical trials to help streamline the manufacturing process [55].
For quantitative attributes, acceptance ranges can be established using statistical tolerance intervals based on historical data from the reference manufacturing process. The approach should consider:
- Process capability (e.g., ±3σ from historical mean)
- Analytical method variability (e.g., accounting for method precision)
- Clinical relevance (e.g., differences known to impact safety or efficacy)
When clinical relevance is uncertain, a worse-case approach using tighter acceptance criteria based on process and analytical capability is recommended.
Table 3: Statistical Approaches for Setting Acceptance Criteria
| Data Type | Recommended Approach | Considerations |
|---|---|---|
| Continuous Data | Equivalence testing with pre-defined margin | Margin based on process capability and clinical relevance |
| Categorical Data | Chi-square or Fisher's exact test | Assessment of distribution patterns |
| Multivariate Data | Principal component analysis, Mahalanobis distance | Holistic assessment of profile similarity |
| Stability Data | Comparison of slope and intercept | Time-dependent degradation behavior |
Addressing Minor Differences
When minor quality attribute differences are detected, a systematic approach to their justification should include:
Assessment of magnitude: Evaluating whether the difference falls within the normal variability of the manufacturing process and analytical method.
Clinical relevance assessment: Determining whether the difference is likely to impact safety or efficacy based on available structure-activity relationship data and clinical experience.
Historical data analysis: Reviewing previous knowledge to determine if similar differences have been observed without clinical impact.
Orthogonal method correlation: Confirming findings with complementary analytical techniques.
As noted in the context of regenerative medicine, "if manufacturers are unable to demonstrate that a product has the same characteristics as it did in the past, they may be asked to perform additional experiments or even perform another clinical trial" [55]. Therefore, a robust scientific justification for any observed differences is paramount.
The following diagram illustrates the decision process for addressing minor quality attribute differences:
Case Studies and Practical Applications
Monoclonal Antibody Case Example
A common scenario involves glycosylation pattern changes in monoclonal antibodies following manufacturing process changes. While glycosylation is often a CQA due to its potential impact on effector function, minor differences in specific glycan species may not necessarily impact clinical performance.
In such cases, a systematic approach would include:
Risk assessment: Evaluating the specific glycan species affected and their known impact on mechanism of action.
Functional testing: Conducting binding assays (e.g., FcγR binding) and effector function assays (e.g., ADCC, CDC) to determine if the observed glycosylation differences translate to functional changes.
Historical comparison: Comparing the observed glycan profiles to historical data from clinical trial material with established safety and efficacy.
Justification: If no functional impact is detected and the differences fall within the range of qualified impurities, a scientific justification can be established referencing published data on structure-function relationships for similar molecules.
Biosimilar Comparability Exercise
For biosimilar development, the comparative analytical assessment aims to demonstrate that the proposed biosimilar is highly similar to the reference product notwithstanding minor differences in quality attributes [22]. The FDA guidance recommends using a totality-of-the-evidence approach, where the collective data from analytical studies, animal studies, and clinical studies demonstrate biosimilarity.
When minor differences are observed, additional analytical characterization may be necessary to justify that these differences are not clinically meaningful. This may include:
- Extended structural characterization using orthogonal methods
- In vitro functional assays covering multiple mechanisms of action
- Forced degradation studies to compare stability profiles
- Analysis of available clinical data for the reference product
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful comparability assessment requires carefully selected reagents and reference materials. The following table details key research solutions for evaluating quality attribute differences:
Table 4: Essential Research Reagent Solutions for Comparability Assessment
| Reagent/Material | Function in Comparability Assessment | Key Considerations |
|---|---|---|
| Reference Standards | Calibrate analytical methods and provide benchmark for comparison | Well-characterized, traceable to recognized standards, appropriate stability |
| Characterized Biosimilar Aliquots | Reference materials for analytical comparison | Sourced from approved drugs, original formulation maintained [54] |
| Critical Reagents | Enable specific analytical measurements (e.g., antibodies, enzymes) | Qualified for intended use, demonstrated specificity and reproducibility |
| Forced Degradation Materials | Stress samples for comparative stability assessment | Well-controlled conditions, representative degradation pathways |
| Cell-Based Assay Reagents | Evaluate biological activity and potency | Relevant mechanism of action, qualified response range |
| CRM for Flow Cytometry | Calibrate flow cytometry measurements | Traceable to reference materials (e.g., NIST standards) [55] |
Justifying minor quality attribute differences in biological products requires a systematic, science-based approach grounded in comprehensive product and process understanding. By implementing rigorous risk assessment practices, robust analytical methods, and statistically sound acceptance criteria, manufacturers can develop compelling scientific justifications for minor differences that fall within qualified ranges.
The totality of evidence approach, which integrates analytical characterization, functional assessment, and prior knowledge, provides a framework for demonstrating that minor quality attribute differences do not adversely impact product safety or efficacy. This approach facilitates successful comparability demonstrations while maintaining product quality and regulatory compliance throughout the product lifecycle.
As the field advances, continued development of advanced analytical methods and increased understanding of structure-function relationships will further enhance the ability to interpret and justify minor quality attribute differences with greater precision and confidence.
For researchers and scientists in drug development, demonstrating the comparability of biological products, such as biosimilars, is a critical and complex challenge. It requires a comprehensive understanding of how a drug behaves in the body and how its manufacturing process ensures consistent quality. Within this framework, Population Pharmacokinetic (PopPK) and Pharmacodynamic (PD) modeling have become cornerstone methodologies for assessing comparability by quantifying and predicting drug exposure and response across diverse patient populations [56] [57].
Simultaneously, Artificial Intelligence (AI) and Machine Learning (ML) are emerging as transformative tools that augment these traditional modeling approaches. AI/ML can identify complex, non-linear patterns in high-dimensional clinical and manufacturing data that may be difficult to capture with conventional methods [58] [59]. The integration of PopPK modeling and AI/ML creates a powerful synergy for optimizing manufacturing control strategies, enhancing process understanding, and providing robust evidence for the comparability of biological products. This technical guide explores these innovative approaches, providing detailed methodologies and data frameworks for their application in biopharmaceutical development.
Traditional Foundation: Population PK/PD Modeling
Population PK/PD modeling is a well-established statistical technique that quantifies the typical values, inter-individual variability, and residual unexplained variability of PK and PD parameters in a target population. It is particularly vital for assessing biosimilarity, as it allows for a holistic comparison of the drug behavior between a proposed biosimilar and its reference product.
Core Components and Workflow
A typical population PK/PD analysis uses non-linear mixed-effects (NLME) models to describe drug concentration-time and response-time profiles. The model development process involves several key stages, from structural model identification to model validation and simulation. The following workflow outlines the core steps in a sequential PopPK/PD modeling approach, as used in the development of biosimilars like denosumab [57].
Experimental Protocol: PopPK/PD Model for Biosimilarity Assessment
Objective: To develop a combined PopPK/PD model using data from a biosimilar and its reference product to support a demonstration of biosimilarity.
Methodology:
Data Collection: Pool individual patient data from Phase I and Phase III clinical studies. This includes:
- PK Data: Serial serum drug concentration measurements following subcutaneous or intravenous administration.
- PD Data: Relevant biomarker measurements over time (e.g., lumbar spine bone mineral density (BMD) for osteoporosis treatments).
- Covariates: Patient demographics (e.g., body weight, age, race, sex), laboratory values, and disease status [57].
Structural Model Development:
- PK Model: Begin with a base structural model. For monoclonal antibodies like denosumab, a two-compartment model with first-order absorption and target-mediated drug disposition (TMDD) is often appropriate to characterize non-linear clearance [56] [57].
- PD Model: An indirect response model is frequently used to link drug concentration to the pharmacological effect. For denosumab, a maximal inhibitory (Imax) function on the formation rate of the PD marker (e.g., bone resorption) effectively captures the increase in BMD [57].
Covariate Model Building: Systematically evaluate the influence of patient covariates on model parameters. For denosumab, body weight is a known covariate on clearance (CL) and central volume of distribution (V2). The effect is typically incorporated using a power model, e.g., CLi = CLpop × (WTi / WTmedian)^θCL, where CLi is the clearance for individual i, CLpop is the population clearance, and θCL is the estimated exponent [57].
Model Validation: Validate the final model using techniques such as visual predictive checks (VPC) and bootstrap analysis to ensure its robustness and predictive performance.
Simulation for Comparability: Using the final model, perform simulations to compare the predicted PK and PD profiles of the biosimilar and the reference product. The treatment group (biosimilar vs. reference) should not be a statistically significant covariate on any key PK/PD parameters, and simulated exposures and responses should be highly similar [57].
Table 1: Key PK/PD Parameter Estimates from a Denosumab Biosimilarity Study
| Parameter | Symbol | Population Estimate | Explanation |
|---|---|---|---|
| Clearance | CL | 0.564 L/day | Represents the volume of plasma cleared of the drug per unit time. |
| Central Volume | V2 | 12.3 L | Volume of distribution of the central compartment. |
| Absorption Rate | ka | 0.602 1/day | First-order absorption rate constant after SC administration. |
| Bioavailability | F | 0.719 | Fraction of the administered dose that reaches the systemic circulation. |
| Imax | Imax | 0.915 | Maximal inhibitory effect on the PD response driver. |
| IC50 | IC50 | 20.4 µg/L | Drug concentration that produces 50% of the maximal inhibitory effect. |
The AI/ML Revolution in Pharmacometrics and Manufacturing
AI and ML are introducing a paradigm shift in how we approach pharmacokinetic modeling and process control in pharmaceutical manufacturing. These technologies excel at handling large, complex datasets without relying on pre-defined mathematical assumptions.
AI/ML for Predictive Concentration Modeling
Objective: To compare the predictive performance of AI models against traditional PopPK models for forecasting drug concentrations.
Experimental Protocol:
Data Source: Extract therapeutic drug monitoring (TDM) records and linked electronic medical records (EMRs) for specific drugs over a defined period (e.g., 2010-2021). The dataset should include drug dosing history, concentration measurements, and patient-specific variables (demographics, lab results, comorbidities) [58].
Data Preprocessing: Handle missing data using imputation techniques like Multivariate Imputation by Chained Equations (MICE). Scale continuous variables and remove covariates with high multicollinearity using the Variance Inflation Factor (VIF) [58].
Model Training & Validation: Randomly split the dataset into training, validation, and test sets (e.g., 60:20:20). Train and tune a suite of AI models, including:
- Ensemble Methods: Random Forest (RF), Adaboost (ADA), eXtreme Gradient Boosting (XGB), Light Gradient Boosting (LGB).
- Deep Learning: Artificial Neural Networks (ANN), Convolutional Neural Networks (CNN).
- Regularized Regression: Lasso (LR) and Ridge Regression (RR) [58].
Performance Comparison: Compare the performance of the best AI model against published PopPK models for the same drug using the Root Mean Squared Error (RMSE) on the test dataset. A lower RMSE indicates superior predictive accuracy.
Table 2: Performance Comparison of AI vs. PopPK Models for Antiepileptic Drugs (AEDs)
| Drug | Best-Performing AI Model | AI Model RMSE (µg/mL) | PopPK Model RMSE (µg/mL) |
|---|---|---|---|
| Carbamazepine (CBZ) | Adaboost | 2.71 | 3.09 |
| Phenobarbital (PHB) | eXtreme Gradient Boosting | 27.45 | 26.04 |
| Phenytoin (PHE) | Ensemble Models | 4.15 | 16.12 |
| Valproic Acid (VPA) | Random Forest | 13.68 | 25.02 |
Source: Adapted from [58]
The data demonstrate that AI models, particularly ensemble methods, can meet or exceed the predictive performance of traditional PopPK models, especially for drugs with high pharmacokinetic variability like phenytoin and valproic acid [58].
AI for Automated PopPK Model Development
Automation is addressing the labor-intensive nature of traditional PopPK model development. The following workflow illustrates an automated, out-of-the-box approach using a tool like pyDarwin to efficiently search a vast space of potential model structures.
Methodology:
- Model Search Space: A generic search space of over 12,000 unique PopPK model structures for extravascular drugs is defined, encompassing various compartment models, absorption mechanisms, and error models [60].
- Optimization Algorithm: A Bayesian optimization with a random forest surrogate is used to explore the model space efficiently, evaluating fewer than 2.6% of possible models on average [60].
- Penalty Function: A key component of the automation is a penalty function that discourages over-parameterization and biologically implausible parameter values. This function combines the Akaike Information Criterion (AIC) with terms that penalize high relative standard errors, abnormally high/low inter-subject variability, or high shrinkage values, mimicking an expert modeler's decision-making process [60].
- Outcome: This approach has been shown to reliably identify model structures comparable to expert-developed models in less than 48 hours on average, significantly accelerating PopPK analysis [60].
Integration with Manufacturing Control Strategies
The insights generated from PopPK and AI models are directly applicable to developing enhanced control strategies for pharmaceutical manufacturing, as outlined in ICH Q10. A control strategy is a planned set of controls derived from product and process understanding that ensures process performance and product quality [61].
Process Analytical Technology (PAT) and Real-Time Release
AI-driven models support the implementation of Process Analytical Technology (PAT), a framework for designing, analyzing, and controlling manufacturing through real-time measurement of Critical Process Parameters (CPP) to ensure Critical Quality Attributes (CQA) [62] [15]. For example:
- Fermentation Control: AI algorithms can analyze real-time off-gas data (O2, CO2) from bioreactors to monitor the physiological state of cell culture, pinpoint contaminants, and determine the optimal harvest time for maximum yield [62].
- Solvent Drying Process: PAT tools like mass spectrometers can monitor solvent levels in the headspace above a product during drying. AI can use this quantitative data to precisely control the drying endpoint, moving beyond traditional Loss on Drying (LOD) tests that occur only at the process end [62].
The integration of AI/ML with PAT enables real-time release testing (RTRT), where quality can be ensured based on process data rather than end-product testing alone, significantly reducing cycle times [15] [61].
The Control Strategy as a Dynamic Hub
In a modern quality system, the control strategy functions as a dynamic "Controls Hub" for feedback and feedforward loops. PopPK and AI models contribute vital product and process understanding to this hub [61].
- Feedback: Commercial manufacturing experience and post-market PK/PD data can be analyzed with AI to refine the control strategy continually.
- Feedforward: Knowledge from development, including PopPK models that identify critical patient covariates, can inform the design space and in-process controls for manufacturing, ensuring the product consistently delivers the intended clinical performance [61].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key computational and analytical tools essential for implementing the approaches discussed in this guide.
Table 3: Essential Tools for Advanced PK Modeling and AI Integration
| Tool Category | Example | Function in Research |
|---|---|---|
| NLME Modeling Software | NONMEM, Monolix | Industry-standard software for developing population PK/PD models using non-linear mixed-effects modeling. Essential for traditional model development and simulation. |
| Automated PopPK Platform | pyDarwin | A library utilizing optimization algorithms (e.g., Bayesian optimization) to automatically search and identify optimal PopPK model structures from a pre-defined space, reducing manual effort. |
| Process Mass Spectrometer | Thermo Scientific Prima PRO | Provides fast, precise, multi-component gas analysis (e.g., O2, CO2) for PAT applications in fermentation and cell culture processes, providing real-time data for AI/ML process control. |
| Machine Learning Libraries | scikit-learn, XGBoost, TensorFlow | Open-source libraries providing implementations of a wide range of AI/ML algorithms (e.g., Random Forest, Gradient Boosting, Neural Networks) for building predictive models from clinical and manufacturing data. |
| In-line Process Analyzer | MarqMetrix All-In-One Process Analyzer | Leverages Raman spectroscopy and data science tools for real-time, non-destructive metabolite monitoring (e.g., glucose) in bioprocesses, enabling dynamic feeding strategies. |
The convergence of traditional PopPK modeling and cutting-edge AI/ML represents a significant leap forward in pharmaceutical development and control. PopPK modeling remains the gold standard for robust, mechanism-based comparability assessment for biological products. Meanwhile, AI/ML offers powerful complementary capabilities: enhancing predictive accuracy, automating labor-intensive tasks, and enabling real-time control of manufacturing processes. By integrating these innovative approaches into a dynamic, knowledge-driven control strategy, drug development professionals can achieve a deeper level of process understanding, ensure consistent product quality, and confidently demonstrate the comparability of complex biological products, ultimately accelerating patient access to critical medicines.
For developers of biological products, manufacturing changes are inevitable throughout a product's lifecycle, driven by needs for process improvements, scale-up, raw material changes, or supply chain adjustments [29]. The comparability protocol serves as a scientifically rigorous plan to demonstrate that a product made after a manufacturing change is highly similar to the pre-change product and that the change has no adverse impact on safety or efficacy profiles [8] [6]. According to regulatory guidelines like ICH Q5E, demonstrating comparability does not require the pre- and post-change materials to be identical, but they must be highly similar with sufficient evidence that any differences in quality attributes do not adversely affect safety or efficacy [29]. This technical guide examines core principles and common pitfalls in lot selection and study design, providing a framework for developing robust comparability protocols that meet regulatory expectations.
Foundations of Comparability Protocols
Regulatory Framework and Key Principles
The concept of comparability was pioneered by the FDA in the late 1980s and formalized in its 1996 guidance document, with principles later synthesized into the ICH Q5E guideline now implemented by major regulators globally [8] [63]. A comparability exercise should provide analytical evidence that a product has highly similar quality attributes before and after manufacturing process changes [6]. The foundation of this assessment rests on the principle that function follows form – sufficiently similar structural characteristics predict similar clinical properties [63].
The Comparability Exercise Workflow
A well-executed comparability protocol follows a systematic workflow from planning through documentation. The diagram below illustrates the key stages in developing and executing a robust comparability protocol.
Strategic Lot Selection for Comparability Studies
Fundamental Principles of Lot Selection
Lot selection forms the foundation of a scientifically sound comparability study. Representative batches should be manufactured as close together as possible to avoid natural age-related differences that could convolute results [29]. The pre- and post-change batches must be manufactured consistently according to their respective processes and should have passed all release criteria [29]. A documented selection strategy should be defined in the comparability protocol before testing begins to prevent even the appearance of "cherry-picking" favorable batches [29].
Phase-Appropriate Lot Selection Strategies
The number of lots and rigor of testing should align with the product's development stage. The table below outlines recommended practices for different clinical development phases.
Table 1: Phase-Appropriate Approaches to Lot Selection and Testing
| Development Phase | Recommended Lot Selection Strategy | Statistical Considerations | Level of Evidence |
|---|---|---|---|
| Early Phase (Phase 1-2) | Single pre-change and post-change batches acceptable; Use platform methods for biophysical characterization [29] | Limited statistical power; Qualitative assessment focused on major attributes [29] | Establish initial product profile; Identify critical quality attributes [29] |
| Late Phase (Phase 3) | Multiple batches (typically 3 pre-change vs 3 post-change); Include process performance qualification (PPQ) lots [29] | Statistical analysis of historical release data; Trend analysis [29] | Comprehensive characterization; Formal statistical comparison for key attributes [29] |
| Post-Approval | Commercial-scale batches; Consider manufacturing history and variability; Include stability cohorts [6] | Robust statistical analysis with predefined acceptance criteria; Consider process capability [6] | Confirm commercial process control; Support process improvements [6] |
Common Pitfalls in Lot Selection
- Insufficient representation of process variability: Selecting batches that do not represent the full range of normal process variation can lead to false comparability conclusions [29].
- Age-disparate batches: Comparing batches of significantly different ages may introduce degradation-related differences unrelated to the manufacturing change [29].
- Inadequate documentation of selection rationale: Failure to document the selection criteria and rationale in the protocol can raise regulatory questions about potential bias [29] [6].
- Overlooking intermediate process steps: For complex changes, failure to analyze appropriate intermediate materials can miss important differences [6].
Designing Robust Comparability Studies
Risk-Based Approach to Study Design
A risk-based approach to comparability assessments is widely recommended by regulators and industry experts [64] [63]. This involves estimating the product risk level based on factors such as the type of molecule, extent of manufacturing changes, potential impact on pharmacokinetics and pharmacodynamics, and stage of clinical development [64]. The risk assessment should be documented and used to determine the scope and depth of the comparability exercise.
Analytical Methods and Testing Strategies
Analytical testing forms the foundation of all comparability exercises [8] [63]. The testing strategy should include orthogonal methods that provide complementary data, with methods specifically selected for their ability to detect potential impacts of the specific manufacturing change [63] [6].
Table 2: Analytical Testing Strategy for Monoclonal Antibody Comparability
| Quality Attribute Category | Recommended Analytical Methods | Criticality Assessment |
|---|---|---|
| Primary Structure | LC-MS, peptide mapping, sequence variant analysis, ESI-TOF MS [29] | High (requires identity or high similarity) [63] |
| Higher Order Structure | Circular dichroism, NMR, X-ray crystallography, SEC-MALS [29] | High (directly related to biological function) [63] |
| Charge Variants | cIEF, capillary zone electrophoresis, ion-exchange chromatography [29] [6] | Medium-High (may impact potency or pharmacokinetics) [6] |
| Glycosylation Patterns | LC-MS, HILIC-UPLC, MALDI-TOF MS [29] [63] | High for Fc-mediated functions (ADCC, CDC) [63] |
| Biological Activity | Cell-based assays, binding assays (SPR, ELISA), enzyme activity assays [8] [6] | High (direct measure of function) [6] |
| Impurities & Product-Related Variants | HP-SEC, CE-SDS, reversed-phase LC, host cell protein assays [29] | Medium (potential impact on immunogenicity) [6] |
Forced Degradation Studies
Forced degradation studies serve as a "stress test" to compare the degradation pathways of pre- and post-change materials under various stress conditions. These studies can reveal differences not apparent in real-time stability studies and provide confidence in product similarity [29].
Table 3: Forced Degradation Stress Conditions and Their Applications
| Stress Condition | Typical Parameters | What It Reveals | Protocol Considerations |
|---|---|---|---|
| Thermal Stress | 5°C to 50°C for 1-3 months [29] | Aggregation, fragmentation, oxidation | Include multiple timepoints; monitor appearance, potency, fragments [29] |
| Photo-Stability | Per ICH Q1B conditions [29] | Photo-oxidation, color changes | May be justified for omission with protective container closure [29] |
| Oxidative Stress | 0.01-0.1% hydrogen peroxide [29] | Methionine oxidation, other modifications | Use concentration and time course to achieve moderate degradation [29] |
| Acidic/Basic Stress | pH 3-10 for various durations [29] | Deamidation, fragmentation, aggregation | Screen pH conditions to identify optimal degradation profile [29] |
| Mechanical Stress | Shaking, agitation, freeze-thaw [29] | Subvisible particle formation, aggregation | Particularly relevant for drug product processing and shipping [29] |
Stability Study Design
Stability studies in comparability protocols should demonstrate that the degradation profiles of pre- and post-change materials are comparable. The studies should be conducted under accelerated and real-time conditions using statistically appropriate number of lots and timepoints [29]. Analysis should focus not only on whether both materials meet specifications, but whether the pattern and rate of change for critical quality attributes are similar over time [29].
Common Pitfalls and Risk Mitigation Strategies
Protocol Development Pitfalls
- Inadequate predefined acceptance criteria: Failure to establish scientifically justified acceptance criteria before testing post-change batches is a critical regulatory deficiency [6]. The acceptance criteria should be based on process capability and historical data, not just specification limits [6].
- Poorly justified analytical methods selection: Choosing methods based on convenience rather than their ability to detect potential changes impacts the validity of the entire study [6]. The protocol should justify why selected methods are appropriate for detecting potential impacts of the specific change [6].
- Insufficient impact assessment: Failure to conduct a thorough assessment of which quality attributes might be affected by the specific manufacturing change can lead to inadequate testing coverage [6].
Study Execution and Analysis Pitfalls
- Over-interpreting similar results: Assuming that comparable analytical results automatically translate to comparable clinical performance without considering the relevance of attributes to safety and efficacy [6].
- Under-interpreting minor differences: Dismissing small but consistent differences without adequate scientific justification [29] [6].
- Inadequate statistical analysis: Using inappropriate statistical methods or failing to account for normal process variability in data analysis [29].
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for Comparability Studies
| Reagent/Material | Function in Comparability Studies | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Serves as benchmark for quality attributes; used in side-by-side analyses [6] | Well-characterized, representative of pre-change material, sufficient quantity [6] |
| Critical Reagents | Antibodies, enzymes, cell lines used in bioassays and binding assays [6] | Specificity, sensitivity, lot-to-lot consistency, appropriate qualification [6] |
| Characterized Reference Material | Used for system suitability tests and method controls [29] | Defined modifications (e.g., glycoforms, oxidized species) to demonstrate method capability [29] |
| Process-Related Impurities | Host cell proteins, DNA, culture media components for impurity method development [6] | Purity, identity, relevance to manufacturing process [6] |
Risk Assessment and Decision-Making Framework
A structured risk assessment framework is essential for making scientifically sound decisions throughout the comparability exercise. The following workflow illustrates a risk-based approach to determining the need for additional studies beyond analytical comparability.
Documentation and Regulatory Considerations
Comparability Protocol and Report Structure
A comprehensive comparability protocol should include: detailed description of the manufacturing change, risk assessment of potential impact on product quality attributes, list of quality attributes to be assessed, analytical methods and justification for their selection, predefined acceptance criteria with scientific rationale, statistical analysis plan, stability study design, and lot selection strategy [6]. The subsequent comparability report should present raw data and results, comparative analysis, evaluation against predefined criteria, discussion of any differences observed, and final conclusion regarding comparability [6].
Navigating Regulatory Expectations
Regulators expect that manufacturers will demonstrate control in each version of the process, ensuring delivery of high-quality product throughout the product lifecycle [29]. Molecular properties should be well characterized and understood so that observed differences between processes can be explained scientifically [29]. For expedited development programs, close collaboration with regulators is crucial to align on opportunities for accelerated approval while maintaining appropriate quality standards [64].
Robust comparability protocols are essential tools for managing the lifecycle of biological products while ensuring consistent quality, safety, and efficacy. Strategic lot selection and comprehensive study design form the foundation of scientifically sound comparability exercises. By applying a risk-based approach, implementing phase-appropriate strategies, avoiding common pitfalls, and maintaining thorough documentation, developers can successfully navigate manufacturing changes without compromising product quality or patient safety. A well-executed comparability protocol ultimately provides regulators with confidence in the manufacturer's process understanding and control, paving the way for new drug approvals and future manufacturing improvements [29].
For developers of biological products, proactive regulatory engagement is a critical strategic imperative. This guide details a science-driven framework for securing early alignment with health authorities on novel, science-based justifications, particularly within the context of demonstrating product comparability. A structured approach, grounded in robust analytical data and clear communication, can de-risk development, accelerate timelines, and facilitate the approval of safe and effective biological products [22].
The development of biological products, including biosimilars and innovator biologics undergoing manufacturing changes, hinges on the ability to demonstrate high similarity or comparability to a reference product. Regulatory pathways for these products are inherently science-based, requiring sponsors to justify their approaches through extensive analytical and functional data [22]. A reactive strategy—submitting a complete data package without prior discussion—carries significant risk of regulatory setbacks. Proactive engagement transforms the regulatory process from a hurdle into a collaborative dialogue, ensuring that the design of development studies and the nature of the evidence gathered are aligned with regulatory expectations from the outset. This is especially crucial when justifying novel analytical approaches or leveraging advanced statistical models where precedent may be limited.
The Regulatory Framework for Comparability
At its core, demonstrating comparability is about establishing that two products are highly similar and that any differences in quality attributes have no adverse impact on safety or efficacy. The U.S. Food and Drug Administration (FDA) emphasizes a "totality-of-the-evidence" approach, where the comparative analytical assessment forms the foundation [22].
Key Regulatory Guidance and Principles
The FDA's guidance, "Development of Therapeutic Protein Biosimilars: Comparative Analytical Assessment and Other Quality-Related Considerations," outlines the central role of analytical studies in building the scientific case for biosimilarity, a concept that extends to general comparability exercises [22]. The overarching principle is that the analytical data should be sufficiently comprehensive and sensitive to detect meaningful differences. The guidance recommends a stepwise approach, beginning with extensive structural and functional characterization, and underscores that the goal of the analytical assessment is to "resolve residual uncertainty" about the product's similarity.
Table: Core Principles of a Science-Based Comparability Justification
| Principle | Regulatory Rationale | Sponsor Action |
|---|---|---|
| Totality of Evidence | Decisions are based on the collective weight of all data, not a single study [22]. | Integrate data from multiple orthogonal assays to build a cohesive product story. |
| Analytical Foundation | Analytical studies are the most sensitive for detecting product differences and form the foundation of the development program [22]. | Invest in state-of-the-art analytical technologies and method validation. |
| Risk-Based Approach | The level of evidence required is proportional to the potential impact on safety and efficacy. | Prioritize resources on characterizing critical quality attributes (CQAs). |
| Stepwise Development | The program should be designed to refine the scope of subsequent clinical studies based on analytical and functional data [22]. | Use analytical outcomes to justify the reduction or extent of clinical testing. |
A Strategic Framework for Proactive Engagement
Securing regulatory alignment is a process that requires meticulous planning and execution. The following workflow outlines the critical path from internal assessment to successful agency agreement.
Phase 1: Internal Assessment and Planning
Before initiating contact, sponsors must conduct a rigorous internal gap analysis. This involves:
- Defining the Novel Justification: Precisely articulate the novel scientific approach or justification. Is it a new potency assay, a unique statistical model for quality attribute comparison, or a non-standard approach to establishing acceptance criteria?
- Anticipating Regulatory Concerns: Conduct a critical review from the regulator's perspective. What questions would you have? What are the potential weaknesses in the proposed approach?
- Building a Robust Scientific Rationale: Assemble all supporting data, including literature references, pilot study results, and data from similar molecules, to build a compelling case for the proposed methodology.
Phase 2: Crafting the Pre-Meeting Package
The pre-meeting package is the cornerstone of effective engagement. It must be a self-contained, clear, and concise document that enables agency reviewers to understand the proposal and provide meaningful feedback [65]. Its structure should be logical and easy to follow, simplifying complex information [66].
Key Components of an Effective Package:
- Briefing Document (BPD): A comprehensive yet concise summary of the program, the novel justification, and specific questions for the agency.
- CQA Risk Assessment: A detailed justification for the classification of product attributes (e.g., Critical, Key, Non-Critical) based on their potential impact on safety and efficacy.
- Proposed Experimental Plan: Detailed methodologies for the key experiments intended to support the justification (see Section 4.2).
- Preliminary Data: All relevant data that supports the feasibility and scientific soundness of the proposed approach.
- Specific Questions for the Agency: A focused list of questions, often requesting agreement on a specific aspect of the proposed plan (e.g., "Does the agency agree that the proposed...?").
Phase 3: The Regulatory Meeting and Follow-Up
During the meeting, the goal is clarification and alignment, not simply presentation. Designate a subject matter expert to lead the discussion on the novel justification. Actively listen to agency feedback and be prepared to discuss alternatives. Crucially, formalize the outcomes in the meeting minutes and, if necessary, in a follow-up communication to the agency to confirm mutual understanding.
Data Generation and Presentation for Alignment
The credibility of a novel justification rests on the quality, relevance, and clarity of the supporting data.
The Scientist's Toolkit: Essential Research Reagents & Materials
A successful comparability study relies on well-characterized reagents and materials. The following table details key items essential for generating high-quality, reproducible data.
Table: Key Research Reagent Solutions for Comparability Studies
| Reagent / Material | Function & Importance in Comparability |
|---|---|
| Reference Standard | Serves as the benchmark for all comparative analyses. Must be well-characterized, representative of the reference product, and stored under controlled conditions to ensure stability. |
| Test Article | The product under evaluation (biosimilar or post-change innovator product). Must be manufactured at a representative scale and purity. |
| Critical Assay Reagents | Includes cell lines, antibodies, enzymes, and substrates used in functional (bioassays) and immunochemical assays. Consistent reagent performance is vital for assay validity and must be monitored with appropriate controls. |
| Characterized Reference Panel | A panel of molecules with known, deliberately introduced variations (e.g., glycoforms, oxidized species). Used to demonstrate the ability (orthogonality) of analytical methods to detect specific product differences. |
Experimental Protocols: Core Methodologies
Below are detailed methodologies for key experiments cited in a comparability assessment.
Protocol 1: Primary Structure Analysis by Mass Spectrometry
- Objective: To confirm amino acid sequence and detect sequence variants.
- Methodology: Intact mass analysis and peptide mapping. The protein is digested with a specific protease (e.g., trypsin), and the resulting peptides are separated by reversed-phase liquid chromatography and analyzed by high-resolution mass spectrometry.
- Data Analysis: Experimental peptide masses are matched against a theoretical digest. Post-translational modifications (PTMs) are identified by mass shifts. Coverage should typically exceed 98% to ensure confidence.
Protocol 2: Functional Characterization by Cell-Based Bioassay
- Objective: To demonstrate similar biological activity relative to the reference product.
- Methodology: A cell line responsive to the biological product is cultured with serial dilutions of both the test and reference articles. A relevant functional endpoint (e.g., cell proliferation, apoptosis, reporter gene activation) is measured.
- Data Analysis: Dose-response curves are generated. Relative potency is calculated by parallel-line analysis, and the 95% confidence interval for the relative potency should fall within pre-defined equivalence margins (e.g., 80%-125%).
Summarizing Quantitative Data for Comparison
Presenting data in clearly structured tables is essential for easy comparison and interpretation by regulators [65]. Effective tables draw attention to the data, not the table itself, and allow the reader to form an opinion quickly [65].
Table: Example Summary of Comparative Functional Bioassay Data
| Assay Parameter | Reference Product (n=12) | Test Product (n=12) | Acceptance Criteria | Conclusion |
|---|---|---|---|---|
| Relative Potency (%) | 100 (98 - 103) | 101 (96 - 106) | 80 - 125 | Meets |
| IC50 (pM) | 10.2 ± 1.5 | 9.8 ± 1.7 | N/A | Similar |
| Hill Slope | 1.05 ± 0.10 | 1.02 ± 0.12 | N/A | Similar |
| Assay Validity (Positive Control RP%) | 95 - 105 | 95 - 105 | 70 - 130 | Meets |
Data presented as Mean (95% CI) or Mean ± SD. RP: Relative Potency.
Best practices for data tables include using footnotes for abbreviations, ordering rows logically, and avoiding unnecessary clutter to ensure the table is self-explanatory [65]. Visualizations like parallel boxplots can be highly effective for comparing the distribution of a quantitative variable, such as potency, across different product batches, showing medians, quartiles, and potential outliers [67].
Visualizing Complex Relationships and Workflows
Diagrams are powerful tools for conveying complex experimental strategies and logical pathways, making it easier for regulators to understand your proposal [66]. The following diagram illustrates the overarching "Totality of Evidence" strategy for a biosimilar development program, which is driven by the analytical comparability exercise.
When creating such diagrams, it is critical to ensure accessibility by maintaining sufficient color contrast between all foreground elements (like text and arrows) and their backgrounds [68] [69]. This ensures the information is accessible to all reviewers, including those with low vision or color blindness [69]. The color palette used here adheres to this principle and the user's specification.
In the rigorous development of biological products, proactive regulatory engagement is not merely a tactical step but a core strategic component. By adopting a structured, science-driven, and collaborative approach—centered on robust data, clear communication, and well-justified novel approaches—sponsors can significantly de-risk their development programs. Securing early alignment on the scientific principles and methodologies for demonstrating comparability paves the way for more efficient development and a successful regulatory outcome, ultimately facilitating patient access to critical medicines.
Beyond the Basics: Biosimilars, Global Frameworks, and the Future of Comparability
The development of follow-on products for branded pharmaceuticals represents a critical pathway for reducing healthcare costs and improving patient access. For small-molecule drugs, this pathway is well-established through generic approvals, while for complex biological products, the biosimilar pathway was formally created in 2010. Understanding the distinction between these regulatory frameworks is essential for drug development professionals, particularly as regulatory requirements continue to evolve based on scientific advances and accumulated agency experience.
This technical guide provides a comparative analysis of generic and biosimilar development requirements, with specific attention to significant recent regulatory changes that are transforming the biosimilar landscape. The content is framed within the broader context of demonstrating comparability for biological products, emphasizing the scientific rationale behind evolving regulatory standards and their implications for development strategies.
Fundamental Distinctions: Generics vs. Biosimilars
Scientific and Regulatory Definitions
Generic drugs are chemically synthesized, small-molecule products that are identical (bioequivalent) to their reference branded drug in dosage form, safety, strength, route of administration, quality, performance characteristics, and intended use [70]. The approval pathway for generics was established under the Drug Price Competition and Patent Term Restoration Act of 1984 (Hatch-Waxman Act), which created an abbreviated approval process requiring proof of bioequivalence rather than full clinical trials.
Biosimilars are biological products that are highly similar to an already FDA-approved biological reference product, with no clinically meaningful differences in terms of safety, purity, and potency [70]. The approval pathway for biosimilars was established by Congress in 2010 through the Biologics Price Competition and Innovation Act (BPCIA) as part of the Affordable Care Act [71] [70]. Biological products differ fundamentally from conventional drugs as they are generally large, complex molecules produced through biotechnology in living systems, making them impossible to exactly replicate [70].
Key Comparative Characteristics
Table 1: Fundamental Characteristics of Generics vs. Biosimilars
| Characteristic | Generic Drugs | Biosimilars |
|---|---|---|
| Molecular Size | Low molecular weight [70] | High molecular weight [70] |
| Structural Complexity | Simple, well-defined structure [70] | Complex, potential for structural variation [70] |
| Manufacturing Process | Chemical synthesis [70] | Specialized biological process using living systems [70] |
| Analytical Characterization | Easy to fully characterize [70] | Difficult to fully characterize [70] |
| Stability Profile | Generally relatively stable [70] | Sensitive to storage and handling conditions [70] |
| Immunogenicity Potential | Lower potential [70] | Higher potential [70] |
Approval Standards and Requirements
Generic Drug Approval Requirements:
- Submission of an Abbreviated New Drug Application (ANDA) [70]
- Demonstration of bioequivalence to the reference product [70]
- No requirement for preclinical (animal) or clinical (human) data to establish safety and effectiveness in most cases [70]
- Same active ingredient, strength, dosage form, and route of administration as reference product [70]
Traditional Biosimilar Approval Requirements:
- Submission of a 351(k) Biologics License Application under the Public Health Service Act [70]
- Analytical studies demonstrating the biological product is highly similar to the reference product [70]
- Animal studies assessing toxicity [70]
- Clinical study or studies assessing immunogenicity, pharmacokinetics (PK), and/or pharmacodynamics (PD) [70]
- For certain products, comparative efficacy and safety studies [70]
Historical Development Challenges
Table 2: Traditional Development Requirements Comparison
| Development Aspect | Generic Drugs | Traditional Biosimilars |
|---|---|---|
| Approval Pathway | ANDA [70] | 351(k) BLA [70] |
| Analytical Studies | Bioequivalence testing [70] | Extensive structural/functional analyses [70] |
| Animal Studies | Generally not required [70] | Toxicity assessment required [70] |
| Clinical Studies | Generally not required [70] | PK/PD, immunogenicity, and potentially efficacy studies required [70] |
| Development Timeline | Relatively short (typically 3-5 years) | Lengthy (could extend 5-9 years) |
| Development Cost | Relatively low ($1-5 million) | High (historically $100-300 million) |
The Evolving Biosimilar Regulatory Landscape
Recent FDA Policy Changes
In October 2025, the FDA announced significant reforms to streamline biosimilar development through a new draft guidance titled "Scientific Considerations in Demonstrating Biosimilarity to a Reference Product: Updated Recommendations for Assessing the Need for Comparative Efficacy Studies" [71] [72]. These changes represent a fundamental shift in the agency's scientific approach based on a decade of experience evaluating biosimilars since the first U.S. approval in 2015.
The key regulatory updates include:
Reduced Clinical Study Requirements: The FDA now proposes that for many biosimilars, comparative efficacy studies (CES) are unnecessary and can be replaced with more sensitive analytical assessments [71] [73]. These studies historically required 1-3 years and cost approximately $24 million on average [71].
Streamlined Interchangeability Designation: The FDA now generally does not recommend switching studies for biosimilars licensed as interchangeable, moving to designate all biosimilars as interchangeable based on existing evidence [71] [74] [75].
Emphasis on Analytical Assessment: The updated guidance recognizes that comparative analytical assessment (CAA) is generally more sensitive than clinical studies for detecting product differences [72] [73].
Scientific Rationale for Regulatory Evolution
The policy changes reflect evolving scientific understanding that for many biological products, especially therapeutic proteins:
- Analytical methodologies have advanced significantly, enabling more sensitive detection of product differences [74] [73]
- The relationship between quality attributes and clinical efficacy is better understood for many reference products [73]
- Comparative clinical efficacy studies generally have low sensitivity compared to analytical assessments for detecting product differences [71] [72]
- Manufacturing processes for many therapeutic proteins have become more standardized and well-characterized [74]
Updated Regulatory Requirements: A Comparative Analysis
Current Approval Standards
Table 3: Updated Regulatory Requirements (Post-2025 Guidance)
| Requirement | Generic Drugs | Updated Biosimilar Pathway |
|---|---|---|
| Approval Pathway | ANDA [70] | 351(k) BLA [70] |
| Analytical Assessment | Bioequivalence testing [70] | Extensive comparative analytical assessment (primary basis) [71] [73] |
| Clinical Efficacy Studies | Not required [70] | Generally not required for most therapeutic proteins [71] [73] |
| Pharmacokinetic Studies | Bioequivalence study [70] | Required (when feasible and clinically relevant) [73] |
| Immunogenicity Assessment | Not typically required | Required [73] |
| Interchangeability Designation | Automatic therapeutic equivalence rating [74] | All biosimilars expected to be designated as interchangeable [74] [75] |
Experimental Protocols for Biosimilar Development
Updated Biosimilar Development Workflow
Diagram 1: Updated Biosimilar Development
Key Methodological Considerations
Comparative Analytical Assessment (CAA) Protocol:
- Purpose: To provide sensitive and comprehensive evaluation of structural and functional similarity between proposed biosimilar and reference product [73]
- Methodology: State-of-the-art orthogonal analytical methods including mass spectrometry, chromatography, capillary electrophoresis, nuclear magnetic resonance, circular dichroism, and biological assays [73]
- Key Metrics: Primary and higher-order structure, post-translational modifications, biological activity, impurities, and stability [73]
Pharmacokinetic Similarity Study Protocol:
- Study Design: Randomized, parallel-group or crossover design comparing the proposed biosimilar with the reference product [73]
- Population: Healthy volunteers or patients, depending on product characteristics [73]
- Key Endpoints: AUC0-t, AUC0-∞, Cmax [73]
- Statistical Analysis: 90% confidence intervals for geometric mean ratios of PK parameters must fall within pre-specified equivalence margins (typically 80-125%) [73]
Immunogenicity Assessment Protocol:
- Purpose: To compare anti-drug antibody (ADA) responses between proposed biosimilar and reference product [73]
- Methodology: Validated immunoassays for detecting binding and neutralizing antibodies [73]
- Timing: Typically conducted alongside PK study and/or in dedicated immunogenicity studies [73]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Biosimilar Development
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Reference Product | Gold standard for comparative assessments | Must be sourced from appropriate market (US for US submission); multiple lots recommended [70] |
| Cell Lines | Production of proposed biosimilar | Clonal cell lines with appropriate expression systems; comprehensive characterization required [73] |
| Analytical Standards | Method qualification and validation | Well-characterized reference materials; should demonstrate assay precision, accuracy, and robustness [73] |
| Characterization Assays | Structural and functional analysis | Orthogonal methods including MS, HPLC, CE-SDS, icIEF, CD, NMR, SPR [73] |
| Binding Reagents | Immunoassay development | Antibodies for ELISA, neutralizing antibody assays; requires demonstration of specificity and sensitivity [73] |
Impact and Future Directions
Expected Outcomes of Regulatory Streamlining
The updated regulatory approach is projected to significantly impact biosimilar development:
- Reduced Development Timelines: Potentially cutting development time by half for some biosimilars [76]
- Cost Reduction: Estimated savings of up to $100 million per biosimilar development program [76]
- Increased Biosimilar Competition: Addressing the current situation where only about 10% of biologic drugs expected to lose patent protection in the next decade have a biosimilar in development [71] [77]
- Improved Patient Access: Potentially expanding treatment options for conditions such as cancer, autoimmune diseases, and rare disorders [71]
Remaining Challenges and Considerations
Despite regulatory advances, several challenges persist:
- Patent Litigation Hurdles: Unlike the generic pathway which includes a 30-month stay for patent resolution, the biosimilar pathway divorces FDA approval from patent litigation, potentially delaying market entry even after approval [74]
- State Substitution Laws: Variability in state-level regulations regarding pharmacist substitution of biosimilars, even with interchangeable designation [74]
- Market Competition Dynamics: Biosimilar price reductions typically require multiple market entrants, unlike the generic model where significant competition drives down prices [74]
- Product Complexity Considerations: The streamlined approach primarily benefits well-characterized therapeutic proteins like monoclonal antibodies, while more complex biologics (cell and gene therapies) will likely still require comparative efficacy studies [74]
Regulatory Convergence and Global Implications
The FDA's updated guidance reflects a trend toward international regulatory convergence, particularly with the European Medicines Agency (EMA) which published similar draft guidance in April 2025 aimed at streamlining biosimilar development [75]. This alignment may facilitate more efficient global development strategies for biosimilar sponsors.
The evolution of biosimilar regulations represents a significant step toward realizing the original intent of the BPCIA to create a robust pathway for follow-on biologics that balances innovation with competition, ultimately advancing patient access to critical biologic therapies.
The year 2025 marks a pivotal transformation in the global regulatory landscape for biosimilar medicines. Both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have independently proposed significant updates to their regulatory frameworks that could substantially reduce the requirement for comparative clinical efficacy studies (CES) in biosimilar development. This shift represents a maturation of regulatory science, built upon over two decades of experience with biosimilars and enabled by advanced analytical technologies that can characterize biological products with unprecedented precision. For researchers and drug development professionals, these changes necessitate a fundamental rethinking of development strategies centered on heightened analytical characterization and a more targeted approach to clinical testing.
The driving force behind this evolution is a growing recognition that CES, which typically add 1-3 years and an average of $24 million to development costs, often provide limited additional value for assessing biosimilarity compared to modern analytical methods [71] [78]. This regulatory streamlining aims to address the stark disparity between biosimilar and generic drug competition; while there are over 30,000 approved generics, only 76 biosimilars have been approved in the U.S., representing a small fraction of approved biologics [71]. By reducing unnecessary development barriers, regulators hope to spur greater market competition that can expand patient access to essential biologic therapies.
Scientific and Regulatory Rationale for the Shift
Foundations in Advanced Analytical Science
The regulatory evolution toward waiving CES is fundamentally grounded in scientific and technological advances in analytical characterization. Regulatory authorities have determined that comparative analytical assessment (CAA) is generally more sensitive than clinical studies for detecting product differences [26] [79]. Modern analytical technologies can now structurally characterize highly purified therapeutic proteins and model in vivo functional effects with a high degree of specificity and sensitivity [26].
This scientific premise is supported by the extensive regulatory experience gained since the first biosimilar approvals. The FDA notes it has accumulated "significant experience in evaluating data from comparative analytical and clinical studies" over the past decade [78], while the EMA references "over two decades of experience in evaluating biosimilar medicines" [80]. This substantial evidence base has demonstrated that when structural and functional similarity is established through rigorous analytical characterization, clinical efficacy studies rarely detect differences not already identified through more sensitive analytical methods [80] [26].
The Problem of "Residual Uncertainty"
The traditional role of CES in biosimilar development has been to address residual uncertainty about clinical performance after analytical and pharmacokinetic assessments [79]. However, regulators have concluded that for many product categories, particularly well-characterized therapeutic protein products, this uncertainty can now be more effectively resolved through:
- Comprehensive analytical characterization using orthogonal methods
- Comparative human pharmacokinetic (PK) studies
- Robust immunogenicity assessments [26] [79]
The 2025 guidances reflect a significant reversal of the previous regulatory approach. Under the 2015 FDA guidance, CES was expected unless sponsors could scientifically justify why one was unnecessary [26]. The updated approach makes the streamlined pathway (without CES) the expected default for appropriate products, with CES required only when specific scientific justifications exist [26] [79].
FDA's Updated Regulatory Framework
Conditions for the Streamlined Approach
The FDA's draft guidance, "Scientific Considerations in Demonstrating Biosimilarity to a Reference Product: Updated Recommendations for Assessing the Need for Comparative Efficacy Studies," outlines specific conditions under which a streamlined approach without CES may be appropriate [81] [26]. Sponsors should consider this approach when:
- Clonal Cell Line Manufacturing: The reference product and proposed biosimilar are manufactured from clonal cell lines, are highly purified, and can be well-characterized analytically [26] [79]
- Understood Quality Attributes: The relationship between quality attributes and clinical efficacy is generally well understood for the reference product and can be evaluated by assays included in the CAA [26]
- Feasible PK Studies: A human pharmacokinetic (PK) similarity study is feasible and clinically relevant to address residual uncertainty [26] [79]
The FDA emphasizes that even when CES is waived, sponsors must still demonstrate that the proposed biosimilar and reference product do not differ in immune response potential [26]. Applications lacking robust immunogenicity data may still require additional clinical investigation under the new approach.
Exception Cases Requiring Clinical Efficacy Studies
The FDA guidance identifies specific circumstances where CES may still be necessary to demonstrate biosimilarity:
- Locally Acting Products: For intravitreally administered products or other locally acting therapeutics where comparative PK data are "not feasible or clinically relevant" [26]
- Limited Structural Understanding: Biologics with limited understanding of structure-function relationships or where analytical assays cannot fully evaluate functional effects [26]
- Alternative Clinical Endpoints: Cases where "a comparative clinical study with a clinically relevant endpoint other than an efficacy endpoint" provides unique safety or performance information [26]
The FDA recommends that sponsors engage in early dialogue with the agency "prior to initiating clinical studies" to determine whether their specific product and development program qualify for the streamlined approach [26] [79].
EMA's Parallel Evolution
Draft Reflection Paper on Streamlined Development
The EMA's draft reflection paper, published for consultation until 30 September 2025, proposes a similar regulatory evolution toward reducing clinical data requirements [80] [82]. The European approach suggests that demonstrated structural and functional comparability, together with comparative pharmacokinetic data, may be sufficient to demonstrate biosimilarity to the reference medicine [80].
This streamlined approach would potentially reduce the amount of clinical data required for the development and approval of biosimilar medicines while maintaining strict EU safety standards [80]. The EMA anticipates that this regulatory optimization will improve patient access to biosimilars in the EU and ensure that Europe remains an attractive market for biosimilar development [80].
Scientific Basis for the EMA's Approach
The EMA's proposal builds on both extensive regulatory experience and advances in analytical methods, mirroring the scientific foundation of the FDA's updated approach. The agency notes that for some biosimilars, CES "may not add significant value, especially where the mechanism of action is well understood and analytical similarity is robust" [82]. The reflection paper emphasizes that waiving certain clinical data requirements would simplify the development and evaluation process "while maintaining the highest standards of safety and efficacy" [80].
Table: Comparison of FDA and EMA 2025 Biosimilar Regulatory Initiatives
| Aspect | FDA Approach | EMA Approach |
|---|---|---|
| Document Type | Draft Guidance | Draft Reflection Paper |
| Comment Deadline | October 2025 | 30 September 2025 |
| Core Principle | CES may not be needed for well-characterized TPPs | Structural/functional + PK data may be sufficient |
| Key Conditions | Clonal cell lines, understood quality attributes, feasible PK studies | Well-understood conditions, robust analytical similarity |
| Expected Impact | Reduce 1-3 years and $24M average cost per biosimilar | Improve access and ensure EU market attractiveness |
Experimental Protocols for the Streamlined Approach
Comprehensive Analytical Characterization
The foundation of the streamlined regulatory approach is a rigorous comparative analytical assessment that demonstrates the proposed biosimilar is "highly similar" to the reference product. This requires an extensive panel of orthogonal analytical methods as detailed in Table 2 below.
Table 2: Essential Analytical Methods for Comprehensive Characterization
| Method Category | Specific Techniques | Critical Quality Attributes Assessed |
|---|---|---|
| Structural Analysis | LC-MS, ESI-TOF MS, SVA | Amino acid sequence, post-translational modifications, sequence variants |
| Higher-Order Structure | Circular dichroism, NMR, HDX-MS | Secondary/tertiary structure, conformation dynamics |
| Charge Variants | icIEF, CZE, cation exchange chromatography | Charge heterogeneity, deamidation, glycosylation |
| Size Variants | SEC-MALS, CE-SDS, SV-AUC | Aggregation, fragmentation, molecular size distribution |
| Biological Activity | Cell-based assays, binding assays (SPR, ELISA) | Potency, mechanism of action, Fc functionality |
| Purity/Impurities | Host cell protein assays, DNA/residuals | Product-related substances, process-related impurities |
For forced degradation studies, which evaluate degradation pathways under stress conditions, the following protocol is recommended:
- Stress Conditions: Include oxidative (e.g., hydrogen peroxide), thermal (e.g., 25-40°C), pH (e.g., 3-10), and mechanical stress (e.g., agitation) [29]
- Sample Preparation: Test at least three pre-change and three post-change batches in head-to-head comparisons [29]
- Analysis Timeline: Conduct testing at predetermined intervals (e.g., 0, 1, 2, 4 weeks) to establish degradation kinetics [29]
- Data Interpretation: Compare trendline slopes, bands, and peak patterns to demonstrate comparable degradation profiles between biosimilar and reference [29]
Pharmacokinetic and Immunogenicity Assessment
When CES is waived, the human PK similarity study and immunogenicity assessment carry increased importance in addressing residual uncertainty about clinical performance.
PK Study Design Considerations:
- Population: Healthy volunteers or patients depending on product safety profile
- Design: Single-dose crossover or multiple-dose parallel design based on product half-life
- Endpoints: Primary AUC(0-inf) and Cmax with standard bioequivalence criteria (90% CI of 80-125%)
- Sampling: Intensive sampling strategy to fully characterize exposure profile
Immunogenicity Assessment Protocol:
- Assay Format: Tiered approach (screening, confirmation, titration, neutralization)
- Sampling Schedule: Multiple timepoints to capture both initial and treatment-emergent responses
- Comparative Design: Head-to-head assessment with reference product
- Clinical Correlation: Evaluation of potential impact on PK, safety, and efficacy
The following workflow diagram illustrates the integrated experimental approach for the streamlined development pathway:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the streamlined regulatory approach requires access to high-quality research reagents and specialized materials. The following table details essential components of the biosimilar characterization toolkit:
Table 3: Essential Research Reagents for Biosimilar Characterization
| Reagent/Material | Function/Purpose | Critical Specifications |
|---|---|---|
| Reference Product | Primary comparator for all analytical and functional studies | Sourced from appropriate market, multiple lots, proper handling |
| Cell Line Systems | Expression of biosimilar and reference product (if applicable) | Documented lineage, comprehensive characterization |
| Analytical Standards | Calibration and qualification of analytical instruments | Well-characterized, appropriate purity and stability |
| Mass Spec Standards | Instrument calibration and quantitative analysis | High purity, traceable to reference materials |
| Chromatography Columns | Separation of product variants for characterization | Appropriate chemistry (SEC, IEX, HIC, RP), lot consistency |
| Bioassay Reagents | Cell lines, cytokines, detection antibodies for potency assays | Documented provenance, consistent performance |
| Binding Assay Reagents | Antigens, ligands, anti-idiotypic antibodies for binding studies | High affinity, minimal lot-to-lot variability |
| Reference Standards | System suitability testing and assay controls | Qualified, stability-supported, representative of product |
Strategic Implementation and Global Implications
Development Program Optimization
For drug development professionals, the 2025 regulatory shifts necessitate strategic reevaluation of ongoing and planned biosimilar programs. Sponsors should:
- Conduct Gap Analysis: Evaluate existing development programs against the streamlined criteria to identify opportunities to eliminate or modify planned CES [26] [79]
- Reallocate Resources: Shift investment from clinical efficacy testing to enhanced analytical characterization capabilities [26]
- Engage Regulators Early: Initiate discussions with FDA and EMA "early in product development" to confirm alignment on data requirements [26] [79]
The following decision algorithm provides a framework for determining the appropriate development path:
Global Harmonization and Future Directions
The parallel initiatives from FDA and EMA represent significant progress toward global regulatory harmonization for biosimilars. This alignment may reduce development complexity for sponsors pursuing approvals in multiple markets and create opportunities for more efficient global development programs [26].
Looking forward, several developments will shape the continued evolution of biosimilar regulation:
- Expansion to Complex Products: Potential extension of streamlined approaches to more complex biologics beyond therapeutic proteins [79]
- Interchangeability Reforms: FDA's indicated plans to eliminate "bureaucratic switching studies" and potentially make all biosimilars interchangeable [79]
- Advanced Analytics Integration: Incorporation of novel analytical platforms with enhanced sensitivity for detecting product differences
The 2025 regulatory proposals from the FDA and EMA represent a watershed moment in biosimilar development, signaling a transition from clinical confirmation to analytical demonstration of biosimilarity for well-characterized products. This paradigm shift acknowledges that modern analytical methods, when properly applied, provide more sensitive assessment of product similarity than traditional clinical efficacy endpoints.
For the drug development community, these changes offer the potential to reduce development timelines by 1-3 years and cut approximately $24 million in costs per product while maintaining the rigorous standards for safety and efficacy [71] [78]. Realizing these benefits requires strategic reallocation of resources toward enhanced analytical characterization capabilities and early, proactive engagement with regulatory agencies.
As these draft guidelines undergo consultation and finalization throughout 2025, researchers and developers have an unprecedented opportunity to shape the future of biosimilar development while accelerating patient access to essential biologic medicines across therapeutic areas.
The development of biosimilar medicines is undergoing a fundamental transformation globally. Regulatory agencies are moving toward a more streamlined, science-driven approach that emphasizes robust analytical comparability while reducing the reliance on large, confirmatory clinical efficacy trials [83]. This paradigm shift recognizes that decades of regulatory experience, coupled with advances in analytical technologies, have created a environment where biosimilarity can be established through comprehensive structural and functional characterization, supported by targeted clinical studies [18]. The European Medicines Agency (EMA) and U.S. Food and Drug Administration (FDA) have both recently published updated guidelines that reflect this evolution, marking a significant departure from previous requirements [80] [71].
The contemporary framework for demonstrating biosimilarity is built on the "totality of evidence" approach, where comparative analytical data forms the foundation, and clinical studies are designed to resolve any residual uncertainty [18] [83]. Within this framework, pharmacokinetic (PK) and pharmacodynamic (PD) studies, along with a thorough assessment of immunogenicity, have emerged as the core clinical components. These studies are highly sensitive in detecting potential differences between a biosimilar and its reference product [83]. This technical guide details the design, methodology, and analysis of these critical studies within the context of demonstrating comparability for biological products.
The Scientific and Regulatory Foundation
The Principles of Comparability
The assessment of biosimilarity is fundamentally a comparability exercise [18]. The underlying principle is that function follows form; a detailed demonstration of structural and functional similarity provides a solid scientific basis for inferring similar clinical efficacy and safety [18] [84]. This principle is already well-established for managing manufacturing changes for originator biologics, where analytical data is almost always sufficient to demonstrate comparability [18]. The same rigorous scientific standard is now being applied to the development of biosimilars.
The Global Regulatory Shift
Major regulatory agencies are aligning their requirements to facilitate this more efficient development pathway. The following table summarizes the recent key updates:
Table 1: Recent Regulatory Updates on Biosimilar Clinical Requirements
| Agency | Update | Key Change | Reported Impact |
|---|---|---|---|
| FDA | New Draft Guidance (Oct 2025) [71] [78] | Clarifies that comparative clinical efficacy studies are generally not needed if analytical similarity is robust. | Can reduce development time by 1-3 years and save an average of $24 million per product [71] [85]. |
| EMA | Draft Reflection Paper (2025) [80] [83] | States that structural, functional, and PK similarity are the main requirements; clinical efficacy studies are only for residual uncertainty. | Aims to improve patient access to biosimilars in the EU by streamlining development [80]. |
| Both | Alignment on Core Principles [83] | PK/PD studies and immunogenicity assessment are now the central clinical requirements for most biosimilars. | Creates a more harmonized global framework, reducing unnecessary clinical trials [83]. |
This shift is underpinned by regulatory experience showing that comparative clinical efficacy studies rarely, if ever, reveal clinically meaningful differences for products that have already demonstrated robust analytical similarity [83]. The FDA notes that these large studies have low sensitivity compared to modern analytical assessments [71].
Core Clinical Study Components: PK, PD, and Immunogenicity
Pharmacokinetic (PK) Study Design
The primary goal of the PK study is to demonstrate that exposure to the biosimilar is equivalent to the reference product.
Table 2: Key Design Elements for a PK Similarity Study
| Design Element | Recommended Approach | Rationale |
|---|---|---|
| Study Population | Healthy volunteers (where safe and ethical) OR relevant patient population. | Healthy volunteers show less variability, increasing study sensitivity. Patients are used when the drug has significant toxicity [83]. |
| Study Design | Randomized, single-dose, crossover design is preferred. Parallel design may be used for products with a long half-life. | The crossover design minimizes inter-subject variability, increasing the power to detect true differences [83]. |
| Dosage and Route | The same dosage and route of administration as the reference product. | Ensures a valid comparison of exposure parameters. |
| Primary Endpoints | AUC~0-inf~ (Area Under the Curve to infinity) and C~max~ (maximum concentration). | AUC~0-inf~ reflects total exposure; C~max~ reflects peak exposure. Both are critical for assessing similarity [84]. |
| Sample Collection | Intensive sampling over a period sufficient to characterize the entire concentration-time profile. | Typically requires at least 3-5 half-lives of sampling to accurately calculate AUC~0-inf~. |
| Bioanalytical Method | Validated, sensitive ligand-binding assays (e.g., ELISA). | The assay must be accurate and precise enough to measure drug concentrations reliably for PK parameter calculation. |
The following diagram illustrates the standard workflow for a PK similarity study:
Pharmacodynamic (PD) and Efficacy Biomarkers
PD studies are incorporated when a clinically relevant, measurable, and validated biomarker of drug activity is available.
- Purpose: To provide pharmacological evidence of similar activity on the target pathway or process [83].
- Endpoint Selection: PD markers should be biologically relevant to the mechanism of action and should change dynamically in response to drug administration. Examples include:
- Receptor Occupancy
- Changes in Serum Cytokine Levels
- Absolute Neutrophil Count (for G-CSFs)
- Blood Glucose Levels (for insulins)
- Study Design: PD endpoints are typically measured alongside PK parameters in the same study. The timing of sample collection must be aligned with the known pharmacodynamics of the drug.
Immunogenicity Assessment
Immunogenicity assessment is critical as an immune response can alter PK, reduce efficacy, or cause safety concerns [84] [83]. The assessment follows a tiered approach conducted throughout the clinical program.
Table 3: Tiered Approach to Immunogenicity Assessment
| Tier | Assay Type | Function | Key Reagents |
|---|---|---|---|
| Tier 1: Screening | Binding Antibody Assay (e.g., Bridging ELISA, ECL) | Detects all anti-drug antibodies (ADAs) in samples. | Biosimilar & Reference Product (for assay calibration), Positive Control Antibodies. |
| Tier 2: Confirmation | Competitive Inhibition Assay | Confirms that the detected signal is specific to the drug. | Biosimilar & Reference Product (as competitors). |
| Tier 3: Characterization | Cell-Based or Non-Cell-Based Neutralizing Antibody (NAb) Assay | Determines if the confirmed ADAs can neutralize the biological activity of the drug. | Relevant Cell Line (for cell-based), Drug Target (e.g., soluble receptor). |
The following diagram illustrates the immunogenicity assessment workflow and its integration with PK data:
The Analytical Foundation and Statistical Analysis
The Primacy of Analytical Comparability
The updated regulatory guidelines are predicated on a foundation of exhaustive analytical comparability [71] [83]. This involves a side-by-side comparison of the biosimilar and reference product using a suite of orthogonal analytical techniques to assess:
- Primary Structure: Amino acid sequence, disulfide bonds.
- Higher-Order Structure: Secondary, tertiary, and quaternary structure.
- Post-Translational Modifications: Glycosylation, oxidation, deamidation.
- Biological Activity: In vitro functional assays (e.g., binding, potency).
The quality attributes are evaluated using a risk-based approach, where they are ranked based on their potential impact on safety and efficacy, known as Critical Quality Attributes (CQAs) [23].
Statistical Approaches for Demonstrating Comparability
A risk-based, tiered statistical approach is recommended for evaluating comparability data [23].
Table 4: Statistical Approaches for Biosimilar Comparability
| Tier | Application | Statistical Method | Acceptance Criteria |
|---|---|---|---|
| Tier 1 | Critical Quality Attributes (CQAs) with known clinical impact. | Equivalence Testing (TOST) | The 90% confidence interval for the mean difference must fall entirely within a pre-defined equivalence margin (e.g., ± 1.5 SD). |
| Tier 2 | Lower priority quality attributes or in-process controls. | Descriptive Range Test | A high percentage (e.g., 90%) of biosimilar measurements fall within the reference product's distribution range (e.g., 99% tolerance interval). |
| Tier 3 | Qualitative assessments where quantitative analysis is not feasible. | Graphical Comparison | Visual, side-by-side comparison (e.g., chromatograms, spectra) to demonstrate similar patterns. |
For the pivotal PK similarity study, the primary analysis typically uses Tier 1 equivalence testing. The standard bioequivalence range of 80.00%-125.00% for the geometric mean ratio (Test/Reference) of AUC and C~max~ is commonly applied [23].
Experimental Protocols and Reagent Solutions
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and materials required for the core analyses in biosimilar development.
Table 5: Key Research Reagent Solutions for Biosimilar Characterization and Clinical Studies
| Reagent / Material | Function and Role in Development | Technical Notes |
|---|---|---|
| Clonal Cell Line | The production engine for the biosimilar. A well-characterized cell line ensures consistent and reproducible product quality [83]. | Developed to express the biosimilar with a primary structure identical to the reference product. |
| Reference Product | The benchmark for all comparability exercises. Sourced from key markets (US, EU) over multiple lots to understand natural variability [18] [83]. | Multiple lots (typically 3-6) are analyzed to establish the reference product's quality attribute ranges. |
| Biosimilar Candidate | The product under development. Must be manufactured at commercial scale using a consistent process for all pivotal comparability studies [83]. | |
| Characterized Reference Standard | A well-defined sample of the biosimilar or reference product used to calibrate analytical assays and ensure data consistency [23]. | Critical for ensuring the accuracy and precision of bioanalytical (PK) and immunogenicity assays. |
| Positive Control Antibodies | Essential for developing, validating, and monitoring the performance of immunogenicity assays (e.g., monoclonal antibodies known to bind or neutralize the drug) [83]. | Used in both screening and neutralizing antibody assays. |
| Critical Reagents for Functional Assays | These include the drug's target (e.g., soluble receptor, ligand), and relevant cell lines to demonstrate equivalent biological activity [83]. | The assays must be qualified/validated to show they can detect differences in biological function. |
Integrated Protocol for a Pivotal PK/PD and Immunogenicity Study
This protocol outlines a single-dose, crossover study in a relevant population.
Protocol Finalization and Regulatory Alignment:
- Finalize the study protocol, including statistical analysis plan.
- Engage with health authorities (FDA, EMA) via scientific advice meetings to align on the design.
Subject Enrollment and Randomization:
- Enroll subjects meeting predefined inclusion/exclusion criteria.
- Randomize subjects 1:1 to either Sequence A (Biosimilar in Period 1, Reference in Period 2) or Sequence B (Reference in Period 1, Biosimilar in Period 2).
Study Product Administration:
- Administer a single dose of the assigned product via the commercial route (e.g., subcutaneous injection). The dose should be the most sensitive for detecting PK differences.
PK and PD Sample Collection:
- Collect blood samples for PK analysis at predefined time points pre-dose and post-dose (e.g., 0.5, 2, 4, 8, 12, 24, 48, 72, 96, 120 hours) to fully characterize the concentration-time profile.
- If applicable, collect samples for PD biomarker analysis at aligned timepoints.
Immunogenicity Sample Collection:
- Collect samples for ADA screening at pre-dose (to establish baseline) and at strategic timepoints post-dose (e.g., at the end of each period and during follow-up) to capture the immune response.
Washout Period:
- Implement a washout period of sufficient length (e.g., 5-7 half-lives) to ensure the first drug is eliminated from the body before the second period begins.
Crossover and Repeat:
- Subjects cross over to receive the alternate product, and all sampling procedures are repeated.
Bioanalytical Phase:
- Analyze PK samples using a validated quantitative method (e.g., ELISA).
- Analyze immunogenicity samples using the validated, tiered approach.
Data Analysis and Reporting:
- Calculate PK parameters (AUC~0-inf~, C~max~) using non-compartmental analysis.
- Perform equivalence testing on log-transformed PK parameters.
- Correlate immunogenicity findings with PK data and adverse events.
The landscape for biosimilar development has entered a new era of scientific precision and regulatory efficiency. The paradigm has decisively shifted from a default requirement for large, comparative clinical trials to a focused approach where state-of-the-art analytical comparability, coupled with targeted PK/PD and immunogenicity studies, forms the core of the biosimilarity exercise [80] [71] [83]. This evolution is supported by over two decades of regulatory experience and significant advancements in analytical technology, which together provide greater sensitivity for detecting clinically relevant differences than traditional efficacy trials [18].
For researchers and drug development professionals, this shift presents both an opportunity and a challenge. The opportunity lies in significantly reduced development timelines and costs, potentially accelerating patient access to critical medicines [85]. The challenge is the heightened demand for excellence in analytical science, robust study design, and rigorous statistical analysis. Success in this new environment requires a deep understanding of the "totality of evidence" approach, where every piece of data, from the molecular structure to the human PK profile, is intricately linked to build a compelling case for biosimilarity. The future of biosimilar development is one where science, not just clinical size, dictates the pathway to approval.
For researchers and scientists developing biological products, navigating divergent international regulatory landscapes presents a significant challenge to global market access. Global regulatory convergence describes the process by which regulatory authorities worldwide align their technical requirements for pharmaceutical development and marketing, while regulatory reliance refers to the practice where one regulatory authority considers and builds upon the assessments performed by another authority or trusted institution [86] [87]. For drug development professionals working with biologics, these mechanisms are not merely administrative concepts but fundamental frameworks that enable more efficient global development strategies, particularly when demonstrating product comparability after manufacturing changes.
The imperative for harmonization is clear: divergent regulatory requirements lead to duplicative testing, increased costs, and delayed patient access to innovative therapies [88] [87]. The U.S. Food and Drug Administration (FDA) acknowledges that harmonization of regulatory requirements "has many benefits such as ensuring favorable marketing conditions to support early access to medicinal products, promoting competition and efficiency, and reducing unnecessary duplication of clinical testing" [87]. This is especially critical for biological products, where manufacturing process changes require rigorous comparability studies to demonstrate that modifications do not adversely impact the product's quality, safety, or efficacy [29].
Key Initiatives and Organizations Driving Harmonization
Major International Harmonization Organizations
Multiple international organizations have established frameworks that directly impact the regulatory requirements for biological products. These organizations develop the scientific guidelines and standards that form the basis for demonstrating comparability and product quality.
Table 1: Key International Organizations Driving Regulatory Harmonization
| Organization | Primary Focus | Recent Developments (2025) | Relevance to Biologics Development |
|---|---|---|---|
| International Council for Harmonisation (ICH) | Harmonizing technical requirements for pharmaceuticals | Adoption of E6(R3) Good Clinical Practice guideline; Ongoing work on Q14 analytical procedure development [88] [89] | Provides foundational guidelines (ICH Q5E, Q12) for comparability studies and lifecycle management |
| International Pharmaceutical Regulators Programme (IPRP) | Regulatory convergence and information exchange | Consolidated platform for multilateral engagement on pharmaceutical regulation [87] | Forum for aligning regulatory approaches to complex biological products |
| Pharmaceutical Inspection Co-operation Scheme (PIC/S) | Harmonizing Good Manufacturing Practice (GMP) standards | 52 participating authorities worldwide; Development of common GMP standards [87] | Critical for manufacturing process changes and cross-border supply of biologics |
| International Coalition of Medicines Regulatory Authorities (ICMRA) | Strategic coordination on regulatory challenges | Initiatives on pharmacovigilance, supply chain integrity, and regulatory communication [87] | Addresses global challenges specific to biological products |
Regional Harmonization Efforts
Regional initiatives have emerged as practical implementations of harmonization principles, creating more standardized regulatory environments within geographic areas.
African Medicines Regulatory Harmonization (AMRH): A landmark achievement in early 2025 established full regional regulatory harmonization in Africa, with the North Africa Medicines Regulatory Harmonization (NA-MRH) Initiative focusing on critical functions including marketing authorization, GMP, quality management systems, pharmacovigilance, and information management systems [88]. The upcoming African Medicines Agency (AMA) has the potential to "allow for increased use of reliance-based procedures and harmonized regulatory requirements across Africa," significantly streamlining access to biological products on the continent [86].
Asia-Pacific Economic Cooperation (APEC): Through its Regulatory Harmonization Steering Committee (RHSC), APEC focuses on developing tools and delivering training on drug regulatory best practices, with priority areas including "Biotechnological Products" and "Cellular Therapies" – both highly relevant to biological products developers [87].
Regulatory Reliance as a Practical Mechanism for Convergence
Principles and Implementation of Regulatory Reliance
Regulatory reliance provides a practical mechanism for implementing convergence principles in everyday regulatory decision-making. According to the International Federation of Pharmaceutical Manufacturers & Associations (IFPMA), regulatory reliance is "the basis of processes by which a regulatory authority in one jurisdiction considers evaluations performed by another while remaining responsible and accountable for the decisions it takes" [86].
The World Health Organization (WHO) actively promotes regulatory reliance as a mechanism for National Regulatory Authorities (NRAs) to "better manage resource capacity and focus on core national activities" [86]. This approach is particularly valuable for biologics development, where the extensive characterization data required for comparability assessments can be resource-intensive for both manufacturers and regulators to duplicate across multiple jurisdictions.
Stakeholder Benefits from Reliance Mechanisms
The implementation of regulatory reliance creates significant advantages across the healthcare ecosystem:
- Patients and Healthcare Providers: Benefit from "more timely access to safe, effective, and quality medical products" [86], including innovative biological therapies.
- National Regulatory Authorities (NRAs): Can "use resources more efficiently by avoiding duplicating work and providing opportunities to strengthen the regulatory system while maintaining sovereignty over decision-making" [86].
- Industry and Developers: Experience "streamlined management of regulatory submissions and global supply systems and predictable, timely approvals" [86], enabling more efficient global development strategies for biological products.
Demonstrating Comparability for Biological Products in a Converged Framework
The Role of Comparability Studies in Regulatory Convergence
For biological products, the comparability study serves as a fundamental scientific exercise that enables regulatory convergence. As defined by ICH Q5E, demonstrating "comparability" does not require the pre- and post-change materials to be identical, but they must be "highly similar" such that "the existing knowledge is sufficiently predictive to ensure that any differences in quality attributes have no adverse impact upon safety or efficacy of the drug product" [29] [90].
The scientific principles underlying comparability assessment for biologics provide a natural foundation for regulatory convergence. As noted in a 2025 study on biosimilar regulatory convergence, "The scientific foundation for biosimilar development is based on comparability studies, as defined by the ICH Q5E guideline" [90]. This common scientific basis enables regulators across different jurisdictions to rely on each other's assessments when supported by robust, well-characterized data.
Experimental Protocols for Comparability Studies
A comprehensive comparability study for biological products requires multiple orthogonal analytical methods to thoroughly characterize both pre- and post-change material. The experimental approach must be phase-appropriate and scientifically justified.
Table 2: Experimental Framework for Biologics Comparability Studies
| Study Component | Key Methodologies | Critical Parameters | Regulatory Reference |
|---|---|---|---|
| Extended Characterization | LC-MS, SEC-MALS, ESI-TOF MS, CE-SDS, icIEF, SVA, HPLC, Potency assays [29] | Primary structure, higher order structure, post-translational modifications, biological activity | ICH Q5E, ICH Q6B |
| Forced Degradation Studies | Thermal stress, photo stress, oxidative stress, pH variation, mechanical stress [29] | Identification of degradation pathways, comparison of degradation profiles and rates | ICH Q1A, ICH Q5C |
| Stability Assessment | Real-time and accelerated stability studies under recommended storage conditions [29] | Rate of formation of degradation products, changes in critical quality attributes | ICH Q1A, ICH Q5C |
| Statistical Analysis | Multivariate analysis, equivalence testing, quality range approach [29] | Demonstration of similarity within qualified ranges, identification of significant differences | FDA Statistical Guidance for Biologics |
The experimental workflow for designing and executing a comparability study follows a logical progression from study planning through data interpretation and regulatory submission.
Figure 1: Comparability Study Workflow for Biological Products
Essential Research Reagents and Materials
The successful execution of comparability studies requires carefully characterized materials and reagents to ensure generation of reliable, reproducible data acceptable across multiple regulatory jurisdictions.
Table 3: Essential Research Reagents for Comparability Studies
| Reagent/Material | Function in Comparability Assessment | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Serves as benchmark for quality attributes; enables longitudinal comparison | Well-characterized, stored under controlled conditions, representative of licensed material |
| Cell Banks | Ensure consistent production of biological material with consistent quality | Genetic stability, microbial contamination, viability, productivity |
| Critical Reagents | Support analytical method performance (antibodies, enzymes, substrates) | Specificity, affinity, purity, stability, qualification against reference |
| Reference Product | Provides comparator for biosimilar development or manufacturing changes | Sourced from appropriate markets, handled according to manufacturer specifications |
Emerging Trends and Future Directions
Advanced Analytical Technologies
The ongoing advancement of analytical technologies is enabling more sophisticated characterization of complex biological products, which in turn supports greater regulatory convergence. Methods such as mass spectrometry, nuclear magnetic resonance, and advanced separation techniques provide increasingly detailed understanding of critical quality attributes [29]. This enhanced analytical capability builds scientific confidence among regulators, facilitating greater reliance on each other's assessments.
A 2025 study on biosimilar regulatory convergence found "high consensus" among regulators, academics, and industry representatives on recommendations including "enhancing stakeholder education on science-based biosimilarity principles" and "promoting regulatory convergence through reliance" [90]. The study also identified strong support (mean score: 4.50/5) for "eliminating in vivo animal studies" and "accepting clinical studies conducted for global submissions" where scientifically justified [90].
Digital Transformation and AI Integration
The integration of artificial intelligence and machine learning into regulatory processes is creating new opportunities for convergence. In 2025, new "AI literacy requirements for pharmaceutical companies came into effect in the European Union," reflecting the growing importance of digital capabilities in regulatory submissions [88]. The International Medical Device Regulators Forum (IMDRF) has released guidance on "Good Machine Learning Practice for Medical Device Development," establishing principles that may extend to AI-enabled biological products [88].
The digital transformation of regulatory systems also includes moves toward structured, data-driven submissions. The FDA's eSTAR submission system for device components, now required for combination products, improves "consistency and transparency" in regulatory reviews [89]. Such digital initiatives create technical foundations for more efficient reliance mechanisms.
Real-World Evidence and Regulatory Convergence
The use of real-world evidence (RWE) represents both an opportunity and a challenge for regulatory convergence. As of February 2025, the U.S. FDA had released the most RWE guidance documents (n=13), followed by the European Medicines Agency (EMA) and China's NMPA (n=7 each) [91]. While four regulators (US FDA, EMA, Taiwan FDA, Brazil ANVISA) have defined key RWE terms including "reliability, relevance, and quality," definitional alignment remains incomplete [91].
The International Council for Harmonisation (ICH) has published draft guidelines on "M14 General Principles on Plan, Design, and Analysis of Pharmacoepidemiological Studies That Utilize Real-World Data for Safety Assessment of Medicines" [91], representing a significant step toward global convergence in this emerging area.
Global regulatory convergence through reliance mechanisms and harmonization efforts provides a strategic framework for efficiently advancing biological products through development and to patients worldwide. The established principles of comparability assessment, as defined in ICH Q5E, create a scientific foundation upon which regulatory convergence can be built. For researchers and drug development professionals, understanding these evolving frameworks is essential for designing efficient global development strategies that maximize the benefits of regulatory reliance while maintaining the rigorous scientific standards required for biological products.
As regulatory systems continue to evolve toward greater cooperation and alignment, the development of robust, scientifically justified comparability packages remains the cornerstone of successful global regulatory strategies for biological products. Through continued dialogue between industry, regulators, and other stakeholders, the vision of a truly converged global regulatory system for biological products continues to advance, promising more efficient development pathways and accelerated patient access to innovative therapies.
For developers of biological products, demonstrating product comparability after a manufacturing change has traditionally been a resource-intensive process, often requiring additional clinical studies to confirm that safety and efficacy profiles remained unchanged. This paradigm is rapidly shifting. Advanced analytical characterization technologies are now enabling a more precise understanding of product quality attributes, thereby reducing the need for extensive clinical data packages. Within the regulatory framework for biologics comparability, the ability to comprehensively characterize molecules through orthogonal methods provides a scientific basis for concluding that no adverse impact on the product has occurred, fundamentally changing the evidence requirements for manufacturing changes.
The U.S. Food and Drug Administration (FDA) recognizes that "the level of CMC information submitted should be appropriate to the phase of investigation" but emphasizes that manufacturing variability for biologics can directly impact safety and efficacy [92]. This article explores the technological advances and regulatory strategies that are enabling sponsors to leverage analytical data to reduce clinical data requirements, accelerating patient access to vital therapies while maintaining rigorous safety standards.
The Regulatory Foundation: Comparability Through Analytical Science
The Evolution of Comparability Assessments
Regulatory guidance has progressively recognized the central role of analytical characterization in comparability assessments. According to FDA guidance, "a sponsor may be able to demonstrate product comparability between a biological product made after a manufacturing change and a product made before implementation of the change through different types of analytical and functional testing, with or without preclinical animal testing" [8]. This principle establishes the foundation for reducing clinical study requirements through robust analytical data.
The ICH Q5E guideline further formalizes this approach, emphasizing that comparability assessments should primarily focus on quality attributes and that extensive nonclinical or clinical data may be unnecessary when analytical studies demonstrate high similarity between pre-change and post-change products [2]. The guideline maintains that "the goal of the comparability exercise is to ensure the quality, safety, and efficacy of drug product produced by a changed manufacturing process," with analytical characterization providing the primary evidence [2].
The Phase-Appropriate Approach
A strategic, phase-appropriate approach to characterization is critical for successful regulatory outcomes. In early development, the focus is primarily on safety, while later stages require comprehensive analysis [93]. As one expert notes, "In the early phase, the focus is on safety and proof of concept, and the investigational new drug (IND) stage requires a fast, basic characterization package using platform methods to support first-in-human trials" [93]. This progressive approach allows manufacturers to build the necessary analytical foundation early, enabling more substantial comparability claims with reduced clinical data in later stages.
Table: Evolution of Regulatory Thinking on Comparability
| Time Period | Primary Focus | Clinical Data Requirements | Analytical Capabilities |
|---|---|---|---|
| 1990s | Process definition | Often required for manufacturing changes | Limited characterization capabilities |
| 2005 (ICH Q5E) | Risk-based approach | Reduced when analytical data sufficient | Emerging orthogonal methods |
| 2025 | Enhanced characterization | Significantly reduced with advanced analytics | High-resolution mass spectrometry, advanced methods |
Advanced Technologies Driving the Analytical Revolution
Mass Spectrometry Methodologies
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has emerged as a cornerstone technology for precise biomolecular quantification, often replacing traditional immunoassays. The superior performance of LC-MS/MS has been demonstrated across multiple therapeutic areas, from immunosuppressant monitoring to endocrine hormone analysis [94] [95] [96].
A recent study comparing measurement techniques for renin-angiotensin-aldosterone system (RAAS) components found that "LC-MS/MS is a reliable assay for measurement of the RAAS components in hypertensive patients under different pathophysiological conditions" [96]. Similarly, for salivary sex hormone analysis, "machine-learning classification models revealed better results with LC-MS/MS" compared to traditional ELISA, highlighting its superior accuracy and reliability [95].
The experimental protocol for LC-MS/MS typically involves:
- Sample preparation and purification: Using solid-phase extraction or protein precipitation to isolate analytes
- Chromatographic separation: Employing specialized columns to resolve complex mixtures
- Mass spectrometric detection: Utilizing multiple reaction monitoring for precise quantification
- Data analysis: Applying internal standardization and calibration curves for accurate measurement [94] [96]
High-Dimensional Flow Cytometry
Advanced flow cytometry data analysis techniques are revolutionizing cellular characterization, with high-dimensional data reduction methods like Principal Component Analysis and t-Distributed Stochastic Neighbor Embedding providing unprecedented resolution of complex cell populations [97]. These techniques enable researchers to detect subtle changes in cellular products that might previously have required clinical evaluation.
Cluster analysis algorithms further enhance interpretation by automatically identifying distinct cell populations without prior knowledge. "Algorithms such as K-means clustering, hierarchical clustering, and more sophisticated methods like FlowSOM and Phenograph are prevalent" in modern analytical workflows [97]. When these advanced analytical approaches demonstrate consistent cellular signatures before and after process changes, the justification for reduced clinical requirements becomes substantially stronger.
Multi-Attribute Methodologies and Orthogonal Approaches
The 2025 regulatory landscape shows "stronger emphasis on comparability protocols" and "advanced analytical characterization" with sponsors expected to use orthogonal methods to fully define biologic attributes [92]. This multi-attribute approach examines numerous product characteristics simultaneously, creating a comprehensive product quality profile that provides high confidence in detecting meaningful changes.
The integration of artificial intelligence and machine learning with these analytical datasets further enhances their predictive power. As noted in flow cytometry applications, "AI-driven platforms can process large data sets quickly, learning from the data to identify patterns that may not be immediately apparent to human analysts" [97]. This capability allows for more sophisticated linking of quality attributes to clinical outcomes, further reducing uncertainty in comparability assessments.
Experimental Protocols for Advanced Characterization
LC-MS/MS for Simultaneous Multi-Analyte Quantification
A validated protocol for simultaneous quantification of multiple immunosuppressants in microvolume whole blood demonstrates the power of modern analytical methods. This approach addresses the challenge of separate analyses for different drug classes by enabling unified testing, significantly enhancing efficiency while reducing sample volume requirements [94].
Table: Key Research Reagent Solutions for Advanced Characterization
| Reagent/Equipment | Function | Application Example |
|---|---|---|
| Triple Quadrupole Mass Spectrometer | Precise quantification of target analytes | Therapeutic drug monitoring [94] |
| C18 Chromatography Columns | Separation of complex mixtures | Resolving angiotensin metabolites [96] |
| Electrospray Ionization Source | Gentle ionization of biomolecules | LC-MS/MS analysis of proteins and peptides [96] |
| Solid-Phase Extraction Plates | Sample clean-up and concentration | Preparing plasma samples for hormone analysis [96] |
| Stable Isotope-Labeled Internal Standards | Quantification reference | Correcting for matrix effects in mass spectrometry [94] |
Experimental Workflow:
- Sample Preparation: Add precipitation reagent to plasma samples, vortex, and transfer to supported liquid extraction plates
- Extraction: Elute analytes using organic solvents under gravity flow
- Concentration: Evaporate extracts under nitrogen stream and reconstitute in compatible solvent
- Chromatographic Separation: Employ reverse-phase chromatography with gradient elution
- Mass Spectrometric Detection: Monitor specific multiple reaction monitoring transitions for each analyte
- Data Analysis: Quantify against calibration curves with internal standardization [94] [96]
High-Resolution Characterization for Biologics
The characterization strategy for biotherapeutics must be appropriately phased, with BLA-stage requirements demanding "100% amino acid sequence coverage and in-depth characterization of impurities down to the 0.1% level" [93]. This comprehensive analysis employs multiple orthogonal techniques to fully understand product attributes and potential variants.
Critical steps include:
- Intact mass analysis by high-resolution mass spectrometry to confirm primary structure
- Peptide mapping with LC-MS/MS to verify sequence coverage and post-translational modifications
- Size variant analysis using SEC-MALS and CE-SDS to quantify aggregates and fragments
- Charge variant analysis via imaged capillary isoelectric focusing to characterize heterogeneity
- Higher-order structure assessment by circular dichroism, fluorescence spectroscopy, and HDX-MS
- Biological activity assays using cell-based systems to confirm functional potency [92] [93]
Advanced Characterization Workflow for Biologics
Quantitative Evidence: Analytical Performance Versus Clinical Outcomes
The superior performance of advanced analytical methods is demonstrated through multiple comparative studies. In a study of hypertensive patients, chemiluminescent immunoassay (CLIA) showed significantly higher values compared to LC-MS/MS, with "median PAC-CLIA was 46.0% higher (P < 0.01) than PAC-LC-MS/MS" [96]. More importantly, LC-MS/MS demonstrated better clinical correlation, as "median PAC-CLIA, 18-OHB-LC-MS/MS and 18-OHF-LC-MS/MS were higher (P < 0.01) in patients with renal dysfunction compared with patients with normal renal function, whereas median PAC-LC-MS/MS did not show a significant difference between the two groups" [96].
Table: Method Comparison Studies Demonstrating Analytical Superiority
| Analyte Category | Traditional Method | Advanced Method | Key Finding | Clinical Impact |
|---|---|---|---|---|
| Salivary Sex Hormones | ELISA | LC-MS/MS | Poor ELISA performance for estradiol and progesterone; LC-MS/MS superior [95] | More reliable endocrine profiling |
| RAAS Components | CLIA | LC-MS/MS | PAC-CLIA 46% higher than LC-MS/MS; better clinical correlation with LC-MS/MS [96] | Improved hypertension diagnosis |
| Immunosuppressants | Immunoassay | LC-MS/MS | Strong linearity (R² > 0.995) and correlation with clinical results [94] | Enhanced therapeutic drug monitoring |
For immunosuppressant monitoring, an LC-MS/MS method demonstrated "strong linearity (R2 > 0.995) at <2 to 35 ng/mL for three calcineurin inhibitors, 26.0 to 1866 ng/mL for CycA, and 0.1 to 50 μg/mL for MPA" [94]. This analytical performance provides the precision and accuracy necessary to detect clinically relevant changes without requiring patient studies.
Strategic Implementation: Reducing Clinical Data Through Analytical Excellence
The Comparability Protocol Framework
A strategic approach to managing manufacturing changes involves implementing comparability protocols that proactively define the analytical studies needed to demonstrate comparability. The FDA notes that "for manufacturing changes prior to product approval, the manufacturer must fully describe the change in any license application or investigational new drug application" [8]. By submitting well-designed comparability protocols in advance, manufacturers can streamline the assessment of changes and potentially avoid clinical study requirements.
The agency encourages early engagement, urging "manufacturers to consult with FDA prior to implementing changes that may result in comparability testing, in order to avoid delay in the review of applications" [8]. This collaborative approach ensures that the analytical data package will be sufficient to address regulatory concerns about product quality, safety, and efficacy.
Risk-Based Decision Making
The foundation for reducing clinical data rests on a risk-based approach that links specific quality attributes to clinical outcomes. As characterization technologies improve, manufacturers can more precisely determine which attributes are critical quality attributes (CQAs) potentially impacting safety and efficacy, and which are less likely to affect clinical performance.
Risk-Based Decision Pathway for Comparability
This scientific, risk-based framework enables manufacturers to make credible claims about comparability without clinical data when analytical studies demonstrate high similarity and provide assurance that no adverse impact on safety or efficacy is expected. As noted in regulatory guidance, "if a sponsor can demonstrate comparability, additional clinical safety and/or efficacy trials with the new product will generally not be needed" [8].
Emerging Trends and Technologies
The evolution of analytical characterization continues, with several emerging trends shaping the future of comparability assessments:
- Integration of Artificial Intelligence: AI and machine learning are increasingly being applied to analytical data streams to identify subtle patterns and predict clinical relevance [97]
- Real-Time Monitoring: Advanced process analytical technologies enable continuous quality verification during manufacturing
- Multi-Omics Integration: Combining proteomic, genomic, and metabolomic data provides comprehensive product understanding [97]
- Digital Quality Systems: Adoption of electronic batch records and AI-driven data integrity tools enhances data reliability [92]
These technologies will further strengthen the link between analytical characteristics and clinical performance, enabling even more targeted reductions in clinical data requirements.
The future of biologics development is unequivocally analytical, with advanced characterization technologies fundamentally changing the evidence requirements for demonstrating product comparability. As one industry expert aptly notes, "regulatory success is fundamentally a mix of scientific rigor and strategic stage planning" [93]. The comprehensive analytical toolkit now available—from high-resolution mass spectrometry to advanced data analysis algorithms—provides unprecedented insight into product quality attributes.
This analytical revolution creates a compelling opportunity to reduce clinical data requirements while maintaining rigorous safety standards. By implementing robust, phase-appropriate characterization strategies and engaging early with regulatory agencies, sponsors can leverage these advanced technologies to accelerate development timelines and bring important therapies to patients more efficiently. As the industry continues to embrace these approaches, the paradigm will shift further toward analytical characterization as the primary evidence for product quality and comparability, reserving clinical studies for situations where analytical approaches cannot resolve residual uncertainty.
Conclusion
The demonstration of comparability for biological products has evolved into a sophisticated, science-driven discipline where analytical characterization forms the cornerstone of regulatory confidence. The foundational principles of ICH Q5E, combined with 2025's paradigm shift at the FDA and EMA, underscore that state-of-the-art analytical methods are often more sensitive than clinical endpoints for detecting meaningful differences. For researchers and developers, this means embracing a risk-based, totality-of-evidence approach that prioritizes robust analytical data, strategic PK/PD studies, and proactive regulatory dialogue. The future points toward greater global regulatory convergence, increased reliance on prior assessments, and the continued minimization of unnecessary clinical studies. This evolution not only streamlines development and reduces costs but ultimately accelerates the delivery of high-quality, safe, and effective biological products to patients worldwide.
References
- 1. ICH Q5E Biotechnological/biological products subject to ... [https://www.ema.europa.eu/en/ich-q5e-biotechnological-biological-products-subject-changes-their-manufacturing-process-comparability-biotechnological-biological-products-scientific-guideline]
- 2. Q5E Comparability of Biotechnological/Biological Products ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q5e-comparability-biotechnologicalbiological-products-subject-changes-their-manufacturing-process]
- 3. Guidance on Q5E Comparability of Biotechnological ... [https://www.federalregister.gov/documents/2005/06/30/05-12908/international-conference-on-harmonisation-guidance-on-q5e-comparability-of]
- 4. Risk Based Comparability for Complex Molecules during ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/349362-Risk-Based-Comparability-for-Complex-Molecules-during-Expedited-Development-Leveraging-Enhanced-Technology-and-Regulatory-Mechanisms/]
- 5. Comparability study Summary of Biologics ... [https://www.bestchrom.com/comparability-study-summary-of-biologics-comparability-studies/]
- 6. Comparability Protocols for Biotechnological Products [https://www.bioprocessintl.com/monoclonal-antibodies/comparability-protocols-for-biotechnological-products]
- 7. Comparability Studies Are Inevitable Here's How To Make ... [https://www.bioprocessonline.com/doc/comparability-studies-are-inevitable-here-s-how-to-make-them-more-efficient-0001]
- 8. Demonstration of Comparability of Human Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/demonstration-comparability-human-biological-products-including-therapeutic-biotechnology-derived]
- 9. FDA Outlines “Plausible Mechanism” Approval Pathway for ... [https://www.ropesgray.com/en/insights/alerts/2025/11/fda-outlines-plausible-mechanism-approval-pathway-for-personalized-therapies-but-significant]
- 10. REGULATORY UPDATE: FDA Releases 2025 Guidance ... [https://www.aabb.org/news-resources/news/article/2025/01/03/regulatory-update--fda-releases-2025-guidance-agenda]
- 11. What's New for Biologics [https://www.fda.gov/vaccines-blood-biologics/news-events-biologics/whats-new-biologics]
- 12. 2025 Safety and Availability Communications [https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/2025-safety-and-availability-communications]
- 13. The process defines the product: what really matters in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5850795/]
- 14. Understanding Biologic and Biosimilar Drugs [https://www.fightcancer.org/policy-resources/understanding-biologic-and-biosimilar-drugs]
- 15. Process Analytical Technologies – Advances in bioprocess ... [https://www.sciencedirect.com/science/article/pii/S0731708521004908]
- 16. Process Analytical Technologies (PAT) Applications for ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/585192-Process-Analytical-Technologies-PAT-Applications-for-Upstream-Biologics/]
- 17. Drug Development Study | Real-Time Monitoring with PAT [https://www.agcbio.com/case-studies/pat-technology-real-time-process-monitoring]
- 18. Comparability of Biologics: Global Principles, Evidentiary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8295099/]
- 19. Biosimilarity Versus Manufacturing Change: Two Distinct ... [https://pubmed.ncbi.nlm.nih.gov/26381277/]
- 20. Biosimilar comparability assessment [https://www.gabionline.net/biosimilars/research/Biosimilar-comparability-assessment]
- 21. Chemistry, Manufacturing, and Controls Changes to an ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/chemistry-manufacturing-and-controls-changes-approved-application-certain-biological-products]
- 22. Development of Therapeutic Protein Biosimilars ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analytical-assessment-and-other-quality]
- 23. Statistical Approaches for Determining Comparability of ... [https://www.biopharminternational.com/view/statistical-approaches-for-determining-comparability-of-biosimilars]
- 24. Developing the Totality of Evidence for Biosimilars: Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5443883/]
- 25. FDA Seeks to Accelerate Biosimilar Development ... [https://www.wiley.law/alert-FDA-Seeks-to-Accelerate-Biosimilar-Development-by-Easing-Data-Requirements]
- 26. FDA rethinks need for comparative efficacy studies ... [https://www.hoganlovells.com/en/publications/fda-rethinks-need-for-comparative-efficacy-studies-for-certain-biosimilars]
- 27. - Risk for Analytical Based and... Approach Comparability [https://pubmed.ncbi.nlm.nih.gov/32295861/]
- 28. Leveraging Risk Assessment for Demonstrating Product ... [https://www.pharmasalmanac.com/articles/leveraging-risk-assessment-for-demonstrating-product-comparability-after-manufacturing-process-changes]
- 29. Understanding comparability studies for biologics [https://mmsholdings.com/perspectives/comparability-studies-biologics-importance/]
- 30. Comparability Protocols for Postapproval Changes to the ... [https://www.federalregister.gov/documents/2022/10/14/2022-22334/comparability-protocols-for-postapproval-changes-to-the-chemistry-manufacturing-and-controls]
- 31. Creating Effective Comparability Protocols [https://www.linkedin.com/pulse/mastering-biologics-development-quick-guide-creating-effective-narke-aepje]
- 32. Questions and answers for biological medicinal products [https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/biological-guidelines/questions-answers-biological-medicinal-products]
- 33. View of Orthogonal approach and critical quality attributes for gene... [https://rrpharmacology.ru/index.php/journal/article/view/738/629]
- 34. Orthogonal and complementary measurements of ... [https://www.sciencedirect.com/science/article/pii/S016836592200863X]
- 35. A Critical Analysis of the FDA Draft Guidance on ... [https://www.centerforbiosimilars.com/view/a-critical-analysis-of-the-fda-draft-guidance-on-development-of-therapeutic-protein-biosimilars-comparative-analytical-assessment-and-other-qualityrelated-considerations]
- 36. Biosimilar Testing: Orthogonal Techniques [https://www.bioprocessintl.com/sponsored-content/building-orthogonality-into-biosimilar-testing]
- 37. Frontiers | Enhancing therapeutic antibody profiling: orthogonal ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1667210/full]
- 38. Orthogonal Versatile Interacting Peptide Tags for Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10249344/]
- 39. Forced degradation of recombinant monoclonal antibodies [https://pmc.ncbi.nlm.nih.gov/articles/PMC5680805/]
- 40. Development of forced degradation and stability indicating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5761119/]
- 41. Advancing forced degradation studies: Design of ... [https://www.sciencedirect.com/science/article/pii/S093964112500164X]
- 42. Statistical Tools for Biologics Stability Testing [https://www.bioprocessintl.com/qa-qc/comprehensive-stability-assessment-of-biotechnological-products-degradation-mechanisms-statistical-tools-and-regulatory-compliance-part-1]
- 43. High-Resolution Accurate Mass-Spectrometry (HRAMS) [https://www.azolifesciences.com/article/High-Resolution-Accurate-Mass-Spectrometry-(HRAMS)-An-Overview.aspx]
- 44. A High Resolution/Accurate Mass (HRAM) Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5772964/]
- 45. Method comparison for the analysis of polyfluoroalkyl substances by... [https://www.sepscience.com/method-comparison-for-the-analysis-of-polyfluoroalkyl-substances-by-epa-method-537-7045]
- 46. Advanced mass spectrometry techniques for monitoring ... [https://www.sciencedirect.com/science/article/pii/S0167779925003117]
- 47. Applying UHPLC-HRAM MS/MS Method to Assess Host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11396427/]
- 48. Identification of additives in polymers from single-use bioprocessing... [https://pubmed.ncbi.nlm.nih.gov/32887108/]
- 49. Review Patient-centric Comparability Assessment of ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354924000534]
- 50. Comparability Studies for Proteins and Biologics [https://www.intertek.com/pharmaceutical/biopharmaceuticals/comparability/]
- 51. Regulatory CMC Experts Navigate Accelerated Approval ... [https://hallorancg.com/insights/2022/09/27/regulatory-cmc-experts-navigate-expedited-accelerated-approval-timelines]
- 52. Rare Disease Focus: FDA's Trio of Cell and Gene Therapy ... [https://www.ropesgray.com/en/insights/alerts/2025/11/rare-disease-focus-fdas-trio-of-cell-and-gene-therapy-draft-guidances-highlight-expedited-programs]
- 53. Flexibility and innovation in the FDA's novel regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5600139/]
- 54. Critical Quality Attributes (CQAs) of Biologic Drugs [https://evidentic.com/critical-quality-attributes-cqas-of-biologic-drugs/]
- 55. Identifying and Measuring Critical Quality Attributes - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK475684/]
- 56. Population Pharmacokinetic and Pharmacodynamic Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3483448/]
- 57. Population pharmacokinetics/pharmacodynamics analysis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1631034/full]
- 58. A Comparison of AI and Population PK Models to Predict the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547357/]
- 59. Enhancing efficiency, product quality, and safety [https://www.sciencedirect.com/science/article/pii/S2707368825000135]
- 60. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 61. Control Strategy: A Feedback-Feedforward 'Controls Hub ... [https://www.pharmtech.com/view/control-strategy-a-feedback-feedforward-controls-hub-for-risk-knowledge-and-product-lifecycle-management]
- 62. Process Analytical Technology | PAT Testing [https://www.thermofisher.com/us/en/home/industrial/pharma-biopharma/manufacturing-control-pharma-biopharma/process-analytical-technology.html]
- 63. Comparability of Biologics: Global Principles, Evidentiary ... [https://link.springer.com/article/10.1007/s40259-021-00488-5]
- 64. Comparability Considerations and Challenges for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7691403/]
- 65. Utilizing tables, figures, charts and graphs to enhance the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394528/]
- 66. How to Make Good Figures for Scientific Papers [https://www.simplifiedsciencepublishing.com/resources/how-to-make-good-figures-for-scientific-papers]
- 67. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 68. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 69. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 70. How Similar Are Biosimilars? What Do Clinicians Need to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5669137/]
- 71. FDA Moves to Accelerate Biosimilar Development and ... [https://www.fda.gov/news-events/press-announcements/fda-moves-accelerate-biosimilar-development-and-lower-drug-costs]
- 72. Scientific Considerations in Demonstrating Biosimilarity to ... [https://www.federalregister.gov/documents/2025/11/20/2025-20380/scientific-considerations-in-demonstrating-biosimilarity-to-a-reference-product-updated]
- 73. FDA Proposes To Eliminate Comparative Clinical ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-proposes-to-eliminate-biosimilar-comparative-studies]
- 74. FDA Policy Changes Could Bring Some Biosimilars to ... [https://www.skadden.com/insights/publications/2025/11/fda-policy-changes-could-bring-some-biosimilars]
- 75. FDA draft guidance on biosimilars offers “regulatory relief” [https://www.europeanpharmaceuticalreview.com/news/267537/fda-draft-guidance-on-biosimilars-offers-regulatory-relief/]
- 76. FDA to streamline approvals for generic biological drugs in ... [https://www.cnn.com/2025/10/29/health/fda-drug-costs-biosimilars]
- 77. FDA Moves to Accelerate Biosimilar Development and ... [https://www.hhs.gov/press-room/fda-accelerates-biosimilar-development-and-lowers-drug-costs.html]
- 78. New FDA Guidance Aims to Simplify the Biosimilar ... [https://www.bigmoleculewatch.com/2025/11/14/new-fda-guidance-aims-to-simplify-the-biosimilar-approval-process/]
- 79. FDA Moves to Streamline Approach to Biosimilars [https://www.lw.com/en/insights/fda-moves-to-streamline-approach-to-biosimilars]
- 80. Streamlining development and assessment of biosimilar ... [https://www.ema.europa.eu/en/news/streamlining-development-assessment-biosimilar-medicines]
- 81. Scientific Considerations in Demonstrating Biosimilarity to ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product-updated-recommendations]
- 82. Biosimilar Regulatory Changes [https://gmdpacademy.org/news/ema-advances-biosimilar-strategy-a-streamlined-pathway-with-broad-implications/]
- 83. Development: From Phase III to Analytical Comparability Biosimilar [https://kymos.com/news/biosimilar-development-change/]
- 84. Biosimilars and interchangeability: Regulatory, scientific, ... [https://www.sciencedirect.com/science/article/pii/S0928098725002234]
- 85. FDA looks to simplify biosimilar development with new draft ... [https://www.clinicaltrialsarena.com/news/fda-biosimilar-approval-draft-guidance-2025/]
- 86. Collaboration, convergence, and regulatory reliance [https://www.ifpma.org/areas-of-work/strengthening-regulatory-systems/collaboration-convergence-and-regulatory-reliance/]
- 87. International Regulatory Harmonization [https://www.fda.gov/drugs/cder-international-program/international-regulatory-harmonization]
- 88. Global Regulatory Harmonization Efforts in 2025 [https://www.freyrsolutions.com/blog/global-regulatory-harmonization-efforts-in-2025]
- 89. Combination Products in 2025: Regulatory Convergence ... [https://resource.ddregpharma.com/blogs/combination-products-in-2025-regulatory-convergence-or-compounding-complexity-2/]
- 90. Toward Regulatory Convergence and Streamlined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568798/]
- 91. A Brief Report on Proposed Areas of International ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11907323/]
- 92. FDA IND CMC Requirements for Biologics: A 2025 ... [https://scxcmc.com/fda-ind-cmc-requirements-for-biologics/]
- 93. Mastering Phase-Appropriate Characterization for ... [https://www.biopharminternational.com/view/mastering-phase-appropriate-characterization-for-biologics-approval]
- 94. Analytical Validation of an LC-MS/MS Method for ... [https://pubmed.ncbi.nlm.nih.gov/40650135/]
- 95. Comparing immunoassay and mass spectrometry ... [https://www.sciencedirect.com/science/article/pii/S0306453025001027]
- 96. Comparisons of renin-angiotensin-aldosterone levels ... [https://www.nature.com/articles/s41371-025-01071-z]
- 97. Advanced Flow Cytometry Data Analysis Techniques [https://synapse.patsnap.com/article/advanced-flow-cytometry-data-analysis-techniques]