Mastering Aseptic Technique: Essential Protocols for Contamination-Free Cell Culture
This article provides a comprehensive guide to aseptic technique for researchers, scientists, and drug development professionals.
Mastering Aseptic Technique: Essential Protocols for Contamination-Free Cell Culture
Abstract
This article provides a comprehensive guide to aseptic technique for researchers, scientists, and drug development professionals. It covers foundational principles, step-by-step methodological protocols for both 2D and advanced 3D cultures, troubleshooting for common contamination issues, and validation strategies to ensure data integrity and reproducibility. By synthesizing current best practices and novel insights, this resource aims to equip laboratory personnel with the knowledge to maintain sterile work environments, safeguard valuable cell lines, and enhance the reliability of preclinical research and biomanufacturing.
The Principles of Asepsis: Building a Foundation for Sterile Science
In cell culture and bioprocessing, the integrity of research and the safety of therapeutic products are paramount. The critical foundation for ensuring this integrity lies in the rigorous application of contamination control strategies, primarily through aseptic and sterile techniques. While the terms "aseptic" and "sterile" are often used interchangeably in casual conversation, they represent distinct, complementary concepts in the scientific and medical fields. Aseptic technique refers to the set of procedures and practices designed to prevent the introduction of contaminating microorganisms into a sterile environment or culture [1]. In contrast, sterile technique describes a state that is completely free from all living microorganisms, including bacteria, fungi, viruses, and spores [2]. Understanding this distinction is not merely an issue of semantics; it is a fundamental requirement for any researcher, scientist, or drug development professional aiming to produce reliable, reproducible, and uncontaminated results. A single lapse can compromise months of work, invalidate experimental data, or render a cell therapy product unsafe for patient use [2]. This application note delineates the critical differences between these techniques, provides structured protocols for their implementation, and integrates quantitative data on contamination control, all framed within the context of advanced cell culture research.
Defining the Concepts: Aseptic vs. Sterile
The core distinction lies in the objective: sterilization is a state of absolute absence of microorganisms, while asepsis is a dynamic process of protection to maintain that state.
Sterile Technique: Achieving an Absolute State
Sterilization is an absolute state; an item or environment is either sterile or it is not [2]. This state is achieved through processes that destroy or eliminate all forms of microbial life. Common methods include steam sterilization (autoclaving), dry heat, chemical sterilants, and radiation. In a cell culture context, the term "sterile" is most correctly applied to the instruments, environments, and materials that have undergone these processes [1]. For example, an autoclaved set of surgical instruments, a filter-sterilized media solution, or a pre-sterilized disposable pipette are all considered sterile. The efficacy of sterilization is often verified using biological and chemical indicators that confirm the elimination of highly resistant bacterial endospores [3].
Aseptic Technique: Maintaining a Protected State
Aseptic technique, on the other hand, is a collection of procedural practices performed under controlled conditions to prevent contamination from microorganisms [2]. It does not create a sterile state but is used to maintain it. Think of it as a barrier system: the initial environment and tools are rendered sterile, and aseptic technique is the skill set used to handle these components without introducing contaminants from the surrounding air, surfaces, or the operator [4]. This includes actions such as working in a biosafety cabinet, flaming the necks of culture vessels, using sterile pipettes, and wearing appropriate personal protective equipment (PPE). The focus is on minimizing the risk of exposure and cross-contamination during experimental procedures [5].
Table 1: Conceptual Comparison of Aseptic and Sterile Techniques
| Feature | Sterile Technique | Aseptic Technique |
|---|---|---|
| Core Objective | To achieve a state completely free of all living microorganisms [2]. | To prevent the introduction of contaminants into a sterile field or culture [1]. |
| Nature | An absolute, binary state (sterile or not sterile). | A process, a set of practices and procedures. |
| Primary Application | Environments (operating rooms), instruments (scalpels, forceps), and reagents (media, solutions) [3] [1]. | Techniques and procedures (cell culture handling, sample manipulation, surgical procedures) [1] [4]. |
| Common Methods | Autoclaving, dry heat, chemical sterilization, radiation, filtration. | Use of laminar flow hoods, PPE, sterile handling practices, disinfection with 70% ethanol. |
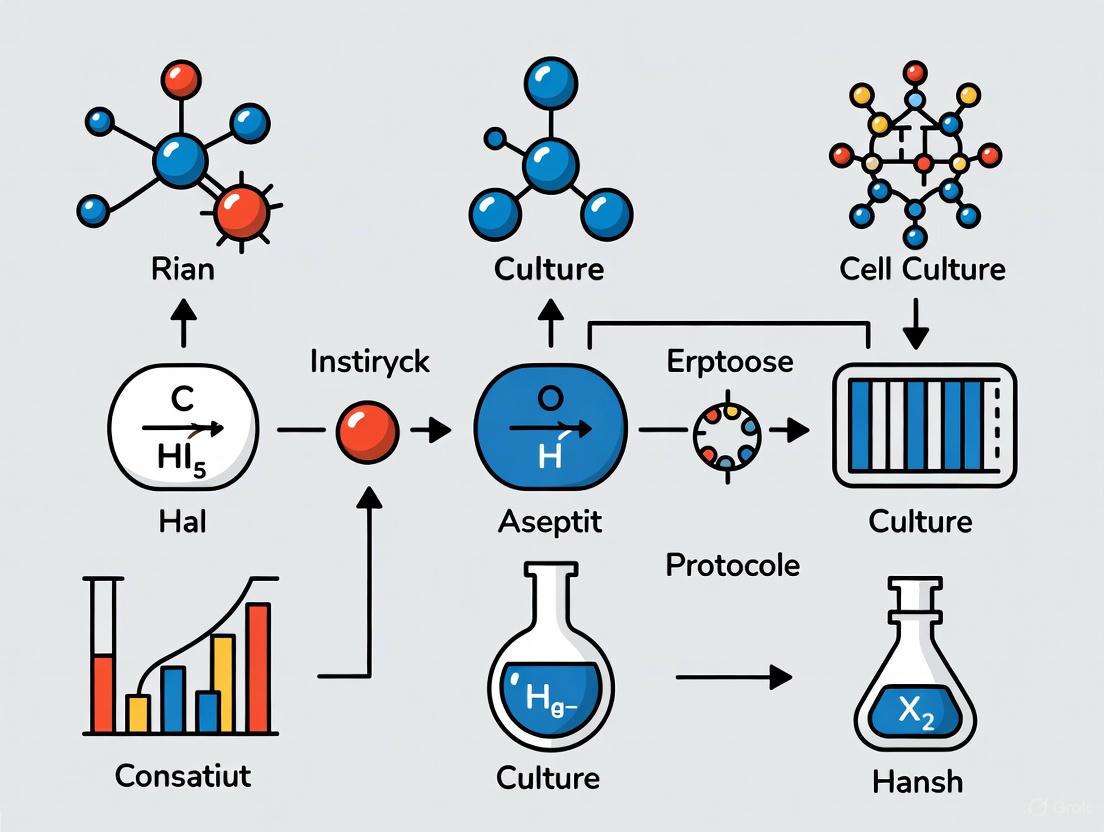
Diagram 1: The sequential relationship between sterile and aseptic techniques in establishing and maintaining a contamination-free workflow.
Quantitative Data and Contamination Analysis
Empirical data underscores the critical importance of precise contamination control. Traditional methods of monitoring microbial load, such as semi-quantitative culture analysis, can be unreliable, leading to undetected contamination that jeopardizes cell cultures and bioprocesses.
A 2021 study compared semi-quantitative culture analysis to the quantitative gold standard (colony-forming units per gram of tissue, CFU/g) using 428 tissue biopsies from 350 chronic wounds. The results, summarized in Table 2, reveal a high degree of variability and overlap in the bacterial loads corresponding to each semi-quantitative category [6]. For instance, "light growth," often considered an insignificant finding, corresponded to a mean bacterial load of 2.5 × 10⁵ CFU/g, a level clinically significant enough to impede wound healing [6]. This imprecision highlights a major vulnerability in relying on such methods for sensitive cell culture work and reinforces the need for impeccable technique to prevent contamination from reaching detectable—and damaging—levels.
Table 2: Correlation Between Semi-Quantitative and Quantitative Culture Results
| Semi-Quantitative Category | Mean Quantitative Value (CFU/g) | Quantitative Range (CFU/g) |
|---|---|---|
| Occasional Growth | 4.9 × 10⁴ | 3.1 × 10² – 7.3 × 10⁶ |
| Light Growth | 2.5 × 10⁵ | 3.0 × 10³ – 1.4 × 10⁷ |
| Moderate Growth | 5.4 × 10⁶ | 1.0 × 10⁴ – 1.0 × 10⁸ |
| Heavy Growth | 1.3 × 10⁸ | 1.0 × 10⁴ – 1.0 × 10¹⁰ |
Data adapted from a comparative study of 428 wound biopsies [6].
Essential Protocols for Aseptic Technique in Cell Culture
The following protocols provide a detailed methodology for establishing and maintaining aseptic conditions during routine cell culture work. Adherence to these steps is critical for preventing the introduction of bacterial, fungal, and mycoplasma contaminants.
Protocol: Standard Aseptic Cell Culture Handling
Objective: To subculture adherent mammalian cells without introducing contamination. Principle: This protocol utilizes a biosafety cabinet (BSC) to create a sterile work area and outlines the steps for sterile handling of cells and reagents to maintain culture purity [2] [4].
Materials & Reagents: Table 3: Research Reagent Solutions for Aseptic Cell Culture
| Reagent/Item | Function | Sterilization Method |
|---|---|---|
| Complete Culture Medium | Provides nutrients for cell growth and proliferation. | Typically filter-sterilized (0.2 µm pore size). |
| Phosphate-Buffered Saline (PBS) | Used for washing cells to remove residual serum and media without causing osmotic shock. | Autoclaving or filter sterilization. |
| Trypsin-EDTA Detaching Agent | Enzyme solution used to detach adherent cells from the culture vessel surface for subculturing. | Filter sterilization. |
| 70% Ethanol Solution | Broad-spectrum disinfectant used to decontaminate work surfaces, gloves, and reagent exteriors. | Prepared with sterile water. |
| Dimethylsulfoxide (DMSO) | Cryoprotective agent used for the freezing and long-term storage of cells. | Pre-sterilized or filter sterilized. |
Methodology:
- Preparation: Tie back long hair, remove jewelry, and wash hands thoroughly. Disinfect hands and put on a clean lab coat, safety goggles, and sterile gloves [2] [4].
- Biosafety Cabinet (BSC) Preparation: Turn on the BSC and allow it to run for at least 15 minutes to purge the work surface. Wipe down all interior surfaces (sides, back, and work area) thoroughly with 70% ethanol using a lint-free wipe [2].
- Material Gathering and Organization: Wipe the outside of all media bottles, pipette boxes, and other containers with 70% ethanol before introducing them into the BSC. Arrange materials in a logical, uncluttered manner within the cabinet, ensuring nothing blocks the front or rear grilles to maintain proper laminar airflow [2] [4].
- Cell Handling: a. Washing: Aspirate the old culture medium from the culture vessel. Gently add a sufficient volume of pre-warmed, sterile PBS to the cell monolayer to cover it. Swirl gently and aspirate the PBS to remove any residual serum that would inhibit trypsin. b. Detachment: Add an appropriate volume of pre-warmed trypsin-EDTA to cover the cell layer. Place the vessel in a 37°C incubator for a few minutes until cells detach (verify under a microscope). c. Neutralization: Add a volume of complete medium containing serum (which inhibits trypsin) that is at least double the volume of trypsin used. Pipette the solution gently across the cell layer to disaggregate the cells into a single-cell suspension.
- Subculturing or Analysis: Transfer the cell suspension to a sterile centrifuge tube for centrifugation or directly to new culture vessels containing fresh, pre-warmed medium for subculturing.
- Cleanup: Cap all bottles and vessels immediately. Remove all materials from the BSC and discard waste appropriately. Wipe down the interior surfaces of the BSC again with 70% ethanol [4].
Diagram 2: Aseptic cell culture workflow, detailing the sequential steps from preparation to cleanup.
Advanced Application: Automated Aseptic Sampling in Bioprocessing
Objective: To aseptically extract small-volume samples from microbioreactors for at-line metabolite monitoring without compromising sterility. Principle: Manual sampling is a primary source of contamination and operator variability in bioprocesses, especially in cell therapy manufacturing where small volumes are critical. The Automated Cell Culture Sampling System (Auto-CeSS) was developed to address this challenge [7].
Experimental Protocol Integration (Based on Auto-CeSS):
- System Integration: The Auto-CeSS is aseptically integrated with the bioreactor (e.g., a 2 mL perfusion microbioreactor) using sterile tubing and micro-connectors, establishing multiple aseptic points (APs) in the fluid path [7].
- Sampling Cycle: A microfluidic-peristaltic pump, regulated by pinch valves, accurately draws a predetermined sample volume (as low as 30 µL) from the bioreactor through a sample line.
- Wash and Purge Cycle: To prevent cross-contamination between samples, the system executes a wash cycle using phosphate-buffered saline (PBS) from a dedicated wash line, purging the sampling pathway.
- Sample Collection: The extracted sample is directed to a multi-port rotary valve, which diverts it to a designated collection outlet (e.g., a multi-well plate) for subsequent off-line analysis, such as metabolite profiling (glucose, lactate, glutamine) [7].
Key Quantitative Findings: Integration of the Auto-CeSS with a 2 mL microbioreactor for T cell culture demonstrated the system's capability for consistent, periodic sampling (minimum 15-minute interval) of 200 µL supernatant daily. Metabolic profiles (glucose, lactate, glutamine, glutamate) of automatically extracted samples showed insignificant differences compared to manually extracted samples, validating the system's accuracy and its potential to eliminate contamination risks associated with manual handling [7].
Troubleshooting and Quality Control
Despite best efforts, contamination occurs. Rapid identification and response are crucial.
Table 4: Common Contamination Sources and Corrective Actions
| Contamination Type | Visual Indicators | Common Sources | Corrective Actions |
|---|---|---|---|
| Bacterial | Cloudy, turbid culture medium; sudden pH shift (yellow); fine granules under phase-contrast microscopy [2]. | Non-sterile reagents, contaminated water baths, poor aseptic technique. | Discard culture and affected reagents. Review sterile technique, autoclave water bath reservoirs, use aliquots. |
| Fungal/Yeast | Fungal: floating, fuzzy, filamentous mycelia. Yeast: small, refractile spherical particles in suspension [2]. | Spores in laboratory air, contaminated incubators, operator skin. | Discard culture. Decontaminate incubators and BSC. Enhance environmental controls. |
| Mycoplasma | No visible turbidity; subtle effects on cell growth and morphology; requires specialized detection kits [2]. | Fetal bovine serum, cross-contamination from other cell lines. | Quarantine and discard culture. Test all new cell lines and reagents upon receipt. |
The distinction between aseptic and sterile technique is a cornerstone of robust and reliable scientific practice in cell culture and bioprocessing. Sterile techniques are used to create a germ-free state for instruments, media, and environments, while aseptic techniques are the continuous procedural practices that protect and maintain this sterility. As the field advances towards greater automation, as demonstrated by systems like the Auto-CeSS for small-volume sampling, the fundamental principles of asepsis remain unchanged. Mastering these techniques is non-negotiable; it is the definitive factor that protects invaluable research, ensures the integrity of data, and guarantees the safety and efficacy of cell-based therapies. Diligent application of the protocols and guidelines outlined here provides a solid foundation for a contamination-free laboratory environment.
Aseptic technique is a foundational pillar of successful cell culture, encompassing a set of procedures performed under controlled conditions to prevent contamination by microorganisms [2]. In the high-stakes environments of biomedical research and pharmaceutical development, mastering these techniques is not merely a best practice but a critical necessity. The integrity of experimental data, the conservation of valuable resources, and the very reproducibility of scientific findings depend directly on the consistent application of aseptic principles.
This application note details the profound consequences of technical failures in aseptic technique and provides validated protocols to safeguard cell-based research. We frame this discussion within the context of a broader thesis on cell culture protocols, addressing the critical needs of researchers, scientists, and drug development professionals who rely on uncontaminated, reproducible biological data for decision-making in both R&D and Good Manufacturing Practice (GMP) environments.
The High Cost of Contamination
Contamination in cell culture manifests in multiple forms, each with the potential to derail research and development projects. The table below summarizes the primary contamination types, their observable signs, and their direct impacts on research and development.
Table 1: Types of Cell Culture Contamination and Their Impacts
| Contamination Type | Common Signs | Impact on Research & Development |
|---|---|---|
| Bacterial | Cloudy culture media; rapid pH shift; tiny, shimmering particles under microscopy [8] [2]. | Compromised cell viability; altered metabolism; invalidated experimental endpoints [8]. |
| Fungal/Yeast | Fuzzy, off-white, or black growth (mold); refractile spheres (yeast); turbidity [8] [2]. | Overgrowth of culture; consumption of nutrients; secretion of interfering metabolites [8]. |
| Mycoplasma | No visible turbidity; subtle effects on cell growth, gene expression, and metabolism [8] [9]. | Insidious alteration of cellular function; misleading experimental results; difficult to detect without specialized testing [8] [9]. |
| Viral | Often no immediate visible changes; can alter cellular metabolism [8]. | Safety concerns for derived products; altered cell behavior; difficult to detect and eradicate [8]. |
| Cross-Contamination | Overgrowth by a fast-growing cell line; misidentification [8] [9]. | Invalidated studies due to use of misidentified cell lines; an estimated 30,000 studies have reported research with misidentified cell lines [9]. |
The repercussions of contamination extend far beyond the loss of a single cell culture. In research settings, contamination is a primary contributor to the broader reproducibility crisis in the life sciences. A 2015 analysis reported that over 50% of preclinical research is irreproducible, at an estimated cost of $28 billion annually [9]. Contaminants like mycoplasma can subtly alter gene expression and cellular metabolism, leading to publication of false conclusions and a waste of scientific resources [8] [9].
In GMP manufacturing and drug development, the stakes are even higher. Contamination can lead to the loss of an entire production batch, resulting in massive financial losses, regulatory scrutiny, and serious patient safety risks [8]. The presence of microbial or viral contaminants in a biologics product intended for patient administration represents a critical failure in quality control.
The following diagram illustrates the cascading negative consequences that result from a failure in aseptic technique.
Core Principles and Essential Tools
Aseptic vs. Sterile: A Critical Distinction
A key conceptual foundation is understanding the difference between "sterile" and "aseptic" [2]:
- Sterile describes an absolute state—the complete absence of all living microorganisms. It is achieved through processes like autoclaving, filtration, or chemical treatment. Equipment and reagents are sterilized before use.
- Aseptic Technique is the set of practices used to maintain sterility by preventing contaminants from entering a sterile environment, sample, or culture. It is a continuous process of protection.
The Scientist's Toolkit: Essential Research Reagent Solutions
Aseptic technique relies on both proper practice and the correct materials. The following table details key reagents and equipment essential for maintaining a contamination-free workflow.
Table 2: Essential Materials for Aseptic Cell Culture
| Item | Function & Importance |
|---|---|
| Biosafety Cabinet (BSC) | Creates a HEPA-filtered, sterile work environment; the primary physical barrier against airborne contaminants [2]. |
| 70% Ethanol | Gold-standard for surface disinfection; disrupts microbial cell membranes through protein denaturation [2] [10]. |
| Sterile, Single-Use Pipettes | Pre-sterilized, disposable pipettes prevent cross-contamination between samples and reagent stocks [8] [2]. |
| Validated Serum & Media | Culture media and supplements from reputable sources that have been tested for sterility and the absence of contaminants like viruses and mycoplasma [8] [9]. |
| Personal Protective Equipment (PPE) | Sterile gloves, lab coats, and safety glasses protect the culture from the user and the user from the culture [2] [11]. |
| Mycoplasma Testing Kits | PCR-based or fluorescence-based detection kits are essential for routine screening of this invisible contaminant [8] [9]. |
Validated Protocols for Aseptic Technique
The following step-by-step protocol synthesizes best practices for handling cell cultures under aseptic conditions.
Protocol: Standard Aseptic Cell Culture Handling
Objective: To maintain sterile conditions during routine cell culture passage to prevent microbial contamination and cross-contamination.
Materials:
- Biosafety Cabinet (BSC)
- 70% ethanol in spray bottle and sterile lint-free wipes
- Pre-sterilized pipette tips and culture vessels
- Sterile cell culture media and reagents
- Water bath (for thawing frozen stocks)
- Personal Protective Equipment (sterile gloves, lab coat, safety glasses)
Method:
Preparation:
Biosafety Cabinet Setup:
- Turn on the BSC and allow it to run for at least 15 minutes to purge the work surface with HEPA-filtered air [2].
- Thoroughly disinfect all interior surfaces of the BSC—including the work surface, side walls, and back panel—with 70% ethanol and sterile wipes [2].
- Arrange all materials logically within the cabinet, ensuring no objects block the front or rear grilles to maintain proper laminar airflow [2].
Aseptic Manipulation:
- Work deliberately and minimize rapid movements to avoid disrupting the laminar airflow barrier [2].
- Flame the necks of glass media bottles and flasks using a Bunsen burner or alcohol lamp to create an upward convection current that prevents airborne particles from falling in [2].
- When uncapping vessels, hold caps face-down on the sterile work surface to prevent contamination of the inner surface [2].
- Keep sterile containers open for the minimum time necessary. Do not pass hands or non-sterile objects over the open tops of sterile vessels [2].
- Use sterile pipettes only once. Never use a pipette that has been exposed to the ambient lab environment to handle sterile media or cells [8].
Post-Procedure Cleanup:
- Immediately cap all bottles and flasks.
- Remove all materials from the BSC and dispose of used consumables in appropriate biohazard waste containers.
- Wipe down the entire interior surface of the BSC again with 70% ethanol to ensure it is clean for the next user [2].
The workflow for a typical cell culture experiment, from setup to analysis, is summarized below.
Quality Control and Data Reproducibility
Ensuring Cell Line Authenticity
Aseptic technique also involves protecting the genetic identity of cell lines. Cross-contamination and misidentification are rampant problems, with one study citing over 30,000 publications based on misidentified lines [9]. Quality control is essential:
- Cell Line Authentication: Use Short Tandem Repeat (STR) profiling for human cell lines to confirm identity against reference databases like Cellosaurus [9].
- Routine Mycoplasma Testing: Implement mandatory, regular screening using PCR, ELISA, or fluorescence-based methods, as mycoplasma contamination affects most cell functions without causing media turbidity [8] [9].
The Role of Standard Operating Procedures (SOPs)
Robust reproducibility is achieved through standardization. Developing and adhering to detailed SOPs for all cell culture processes is critical [9]. These SOPs should cover:
- Standardized media formulations and reagent preparation.
- Defined seeding densities and passage protocols.
- Clear documentation and record-keeping for every culture, including passage number and any deviations from the protocol [9].
Aseptic technique is a non-negotiable, foundational discipline in cell culture, serving as the primary defense against the multi-faceted threat of contamination. Its rigorous application is directly linked to the integrity of experimental data, the efficient use of time and financial resources, and the overall reproducibility and credibility of scientific research. By embracing the principles, utilizing the essential tools, and adhering to the validated protocols outlined in this document, researchers and drug development professionals can significantly mitigate risk, enhance the quality of their outputs, and contribute to a more robust and reliable scientific enterprise.
Within the context of cell culture aseptic technique protocols, biological contamination represents a persistent and formidable adversary that can compromise experimental integrity, jeopardize product safety, and invalidate research findings. The nutrient-rich environment optimized for mammalian cell growth simultaneously supports the proliferation of opportunistic biological invaders, including bacteria, fungi, mycoplasma, and viruses. Unlike in vivo systems where immune defenses provide protection, in vitro cultures remain entirely vulnerable to these contaminants, necessitating rigorous defensive strategies [12]. This application note delineates the primary sources and characteristics of common biological contaminants, provides structured protocols for their detection and prevention, and establishes a framework for maintaining contamination-free cell culture systems within research and drug development environments.
Understanding the morphological characteristics, common sources, and visible indicators of each contaminant type forms the foundation of effective contamination control. Different contaminants present unique challenges in detection and eradication, requiring tailored approaches for management.
Table 1: Characteristics and Identification of Common Biological Contaminants
| Contaminant | Common Species/Examples | Primary Sources | Visual/Microscopic Indicators | Culture Medium Effects |
|---|---|---|---|---|
| Bacteria | Escherichia coli, Staphylococcus epidermidis, Bacillus species [12] | Lab personnel, contaminated water baths, non-sterile reagents [12] [13] | Tiny, motile granules between cells; "quicksand" appearance [14] [15] | Rapid turbidity; yellow color shift (acidic pH) [14] [16] |
| Fungi (Yeast) | Candida species [12] | Airborne spores, humidified incubators, cellulose products [17] | Spherical or ovoid particles that reproduce by budding [14] [12] | Turbidity in advanced stages; possible alkaline pH shift [14] [16] |
| Fungi (Mold) | Aspergillus, Penicillium species [12] | Unfiltered air, improper cleaning, contaminated storage areas [17] | Filamentous, thread-like hyphae; fuzzy patches [14] [12] | Floating mycelial clumps; stable pH initially [14] [18] |
| Mycoplasma | M. fermentans, M. orale, M. arginini, M. hyorhinis [12] [19] | Lab personnel (oral cavity), contaminated serum/trypsin, infected cell lines [12] [19] | Not visible by standard microscopy; tiny black dots at high magnification [15] | No turbidity; subtle changes in cell growth/metabolism [18] [19] |
| Viruses | Retroviruses, Herpesviruses, Adenoviruses [12] | Original tissues, serum supplements, cross-contamination [18] [17] | Not visible by light microscopy; may cause cytopathic effects [18] [12] | No consistent change; latent infections common [18] [12] |
Special Considerations for Mycoplasma and Viral Contaminants
Mycoplasma contamination presents unique detection challenges due to its small size (0.15-0.3 µm) and absence of a cell wall, making it resistant to common antibiotics like penicillin and allowing it to pass through standard 0.22µm filters [18] [19]. With an estimated 15-35% of continuous cell lines infected worldwide, mycoplasma can significantly alter cellular metabolism, gene expression, and viability without causing turbidity in the medium [12] [19]. Viral contamination is equally problematic, as these obligate intracellular parasites can establish persistent, silent infections without visible manifestation, potentially compromising both experimental data and laboratory personnel safety, particularly when working with human or primate cells [18] [12].
Detection Methodologies and Experimental Protocols
Implementing routine, systematic detection protocols is critical for identifying contamination before it spreads through multiple cultures. The following section provides standardized methodologies for detecting various contaminant types.
Routine Microscopic and Visual Analysis
Daily microscopic examination represents the first line of defense against contamination. For bacterial and fungal contaminants, the following protocol should be implemented:
- Daily Observation: Examine cultures under phase-contrast microscopy at 100-400x magnification prior to experimentation or feeding [14] [18].
- pH Monitoring: Document medium color daily using phenol red indicator (yellow = acidic; pink = alkaline; orange = optimal pH ~7.4) [18] [16].
- Turbidity Assessment: Observe medium clarity against a white background; cloudiness suggests microbial proliferation [14] [16].
- Morphological Documentation: Record any changes in cell morphology, adherence, or growth patterns compared to established baselines [14].
Mycoplasma Detection Protocol
Given the prevalence and stealthy nature of mycoplasma, specialized detection methods are required. The DNA fluorescence staining method using Hoechst 33258 provides reliable results:
Sample Preparation:
Staining Procedure:
Analysis and Interpretation:
Table 2: Advanced Detection Methods for Biological Contaminants
| Contaminant | Detection Method | Protocol Summary | Key Reagents/Equipment |
|---|---|---|---|
| Bacteria & Fungi | Gram Staining [16] | 1. Heat-fix air-dried smear2. Crystal violet (1 min)3. Iodine mordant (1 min)4. Alcohol decolorization (5-10s)5. Counterstain with safranin (30-60s) | Crystal violet, Gram's iodine, ethanol, safranin, microscope |
| Mycoplasma | PCR Detection [13] [16] | 1. Extract DNA from culture supernatant2. Amplify with mycoplasma-specific primers3. Analyze amplicons by gel electrophoresis | Mycoplasma-specific primers, PCR reagents, thermal cycler, gel electrophoresis system |
| Viruses | PCR/RT-PCR [14] [16] | 1. Extract nucleic acids from cells/supernatant2. Amplify with viral-specific primers3. Detect amplification products in real-time or by gel analysis | Viral-specific primers, PCR reagents, thermal cycler |
| All Microbes | Microbial Culture [16] [17] | 1. Inoculate culture supernatant into nutrient broth/agar2. Incubate at 37°C and 20-25°C3. Monitor turbidity/colony formation for 7-14 days | Soybean-casein digest broth, blood agar, Sabouraud dextrose agar |
Contamination Identification and Response Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Maintaining contamination-free cultures requires access to specific reagents and equipment for prevention, detection, and eradication. The following toolkit represents essential components for an effective contamination control strategy.
Table 3: Essential Research Reagent Solutions for Contamination Control
| Category | Specific Reagents/Items | Function/Application |
|---|---|---|
| Disinfectants | 70% Ethanol, 10% sodium hypochlorite (bleach), benzalkonium chloride [18] [15] | Surface decontamination of biosafety cabinets, incubators, and work areas |
| Detection Reagents | Hoechst 33258, DAPI, mycoplasma-specific PCR kits, Gram stain kits [18] [16] [15] | Identification and confirmation of contaminating organisms |
| Antimicrobial Agents | Penicillin-Streptomycin solution, Amphotericin B, Tetracycline, Plasmocin [16] [15] | Treatment of contaminated cultures (use as last resort) |
| Sterile Supplies | 0.1µm and 0.22µm filters, sterile pipettes, single-use culture vessels [17] [19] | Maintenance of aseptic environment and sterile reagent preparation |
| Quality Control Tools | Mycoplasma detection kits, endotoxin testing kits, authentication services [14] [15] | Regular screening and validation of cell lines and reagents |
Vigilance against biological contamination requires a multifaceted approach combining rigorous aseptic technique, routine screening protocols, and prompt intervention when contamination is detected. Researchers must recognize that prevention consistently proves more effective than remediation in contamination control. The continuous implementation of these protocols, coupled with systematic documentation and staff training, forms the cornerstone of reliable cell culture practice. By understanding the unique characteristics and sources of common contaminants, research and drug development professionals can implement effective defensive strategies that preserve the integrity of their cell-based systems and ensure the generation of reliable, reproducible scientific data.
Within cell culture aseptic technique protocols, the creation of a reliable barrier between sterile cultures and the non-sterile environment is foundational to research integrity. Successful cell culture is heavily dependent on keeping cells free from contamination by microorganisms such as bacteria, fungi, and viruses [4]. Nonsterile supplies, media, reagents, and airborne particles are all potential sources of biological contamination that can compromise experimental results, lead to wasted resources, and in a biomanufacturing context, pose patient safety risks [8]. This document delineates the critical roles, selection criteria, and standardized application protocols for three cornerstone components of contamination control: biosafety cabinets, personal protective equipment (PPE), and 70% ethanol. Adherence to these detailed protocols is essential for ensuring the reproducibility and validity of research, particularly in advanced drug development workflows.
Essential Equipment and Reagents
Biosafety Cabinets (BSCs): Primary Engineering Controls
Biosafety Cabinets are primary containment devices that provide a sterile work area through the combined use of laminar airflow and High-Efficiency Particulate Air (HEPA) filters. These filters are capable of trapping particles as small as 0.3 μm with an efficiency of at least 99.97% [20]. Their fundamental purpose is to protect the user and the environment from exposure to biohazards, while most classes (Class II and III) also protect sensitive research materials from external contamination [20].
BSC Classification and Selection
The class of BSC selected must align with the biosafety level of the work and the need for product protection. Table 1 summarizes the principal characteristics of different BSC classes.
Table 1: Classification and Characteristics of Biological Safety Cabinets
| BSC Class/Type | Personnel Protection | Product Protection | Environmental Protection | Typical Applications |
|---|---|---|---|---|
| Class I | Yes | No | Yes | Enclosing equipment (e.g., centrifuges) or procedures that generate aerosols; not for sterile work. |
| Class II (All Types) | Yes | Yes | Yes | The most frequently used cabinets in research and clinical labs for handling low- to moderate-risk agents [20]. |
| Class III | Yes | Yes | Yes | A totally enclosed, gas-tight cabinet for the highest level of protection; used with BSL-3/4 agents. |
Standard Operating Protocol for BSC Use
The following protocol is essential for maintaining the integrity of the cabinet's sterile field.
Prior to Use:
- Preparation: Wash hands thoroughly with soap and water. Put on appropriate PPE (at a minimum, gloves and a buttoned-down lab coat or disposable gown) [20] [4].
- Decontamination: Wipe down all surfaces of the BSC (work surface, side walls, and viewscreen) with 70% ethanol [4].
- Purging: Turn on the blower and let the cabinet purge for at least 10 minutes to establish proper airflow and remove contaminants [20].
- Loading: Load all necessary materials and reagents into the cabinet, ensuring they are wiped with 70% ethanol first. Do not block the front or rear air grills [20] [4].
During Use:
- Minimize Disruption: Avoid rapid movements in and out of the cabinet, as this disrupts the protective airflow barrier [20].
- Work Flow: Always work from a clean to dirty area within the cabinet. Keep all items away from the front grill [20].
- Avoid Contaminants: Never use a Bunsen burner inside a BSC, as heat disrupts airflow and can damage the fragile HEPA filters [20] [4].
After Use:
- Decontaminate and Remove: Decontaminate all materials before removal. Wipe down the interior of the BSC with 70% ethanol [20] [4].
- Purging: Allow the cabinet to run for several minutes to purge any airborne contaminants before turning off the blower and light [20].
- UV Light (if applicable): If equipped, UV lights may be used for additional surface sterilization when the room is unoccupied. Never operate UV light when personnel are present due to risks of skin burns and eye damage [20].
Personal Protective Equipment (PPE): A Critical Personnel Barrier
PPE forms an immediate protective barrier between the researcher and the hazardous agent, serving a dual purpose: protecting the user from biological materials and protecting the cell cultures from microorganisms shed by the user (e.g., from skin and clothing) [4].
Key PPE Components and Protocol
- Lab Coat/Gown: A dedicated, clean lab coat or disposable gown must be worn to prevent the introduction of contaminants from personal clothing [4] [21].
- Gloves: Non-sterile or sterile gloves must be worn at all times. Gloved hands should be frequently wiped with 70% ethanol during work. Gloves are single-use and should be disposed of after work or if they become contaminated [4].
- Additional Protection: Safety glasses, masks, and hair coverings are recommended to further minimize contamination risks from the user [22].
70% Ethanol: The Universal Decontaminant
70% ethanol is the disinfectant of choice in cell culture laboratories due to its effectiveness against a broad range of bacteria and fungi, and its rapid evaporation without leaving residues [21]. Its efficacy is concentration-dependent; a 70% solution is more effective than 100% ethanol because the presence of water slows evaporation and allows for sufficient contact time to penetrate microbial cell walls.
Application Protocol
70% ethanol is used to disinfect all surfaces and items that enter the BSC or come into contact with cultures.
- Work Surfaces: Wipe the BSC work surface and other equipment (incubators, microscopes) before and after use, and especially after any spillage [4].
- Reagent Containers: Wipe the outside of all media bottles, flasks, and pipette boxes with 70% ethanol before placing them in the BSC [4].
- Gloved Hands: Routinely wipe gloved hands during procedures to maintain sterility [4].
Integrated Workflow for Aseptic Technique
The following diagram illustrates the logical sequence and interdependency of the core aseptic technique components to maintain a sterile field.
Experimental Validation and Data
Efficacy of Alcohol Swabbing: A Pilot Study
A 2025 randomized controlled trial investigated the necessity of swabbing single-use injectate vials with 70% isopropyl alcohol, a common aseptic practice. The study hypothesized that this step may not affect the risk of bacterial colonization under clean conditions [23].
Experimental Protocol:
- Design: Double-blind, randomized controlled trial.
- Samples: 40 new single-use vials (20 with aluminum caps, 20 with plastic caps).
- Intervention: Vials were randomly assigned to a "swab" group (firmly swabbed once with 70% isopropyl alcohol and air-dried) or a "no-swab" group.
- Sampling & Culture: A blinded researcher sampled each vial's rubber stopper with a sterile saline-moistened cotton swab. Swabs were plated on blood agar and incubated for 5 days at 35°C in a CO₂ environment. A blinded microbiologist assessed bacterial growth [23].
Results and Analysis:
- Quantitative Data: No bacterial growth was observed in any of the 40 samples after 5 days of incubation. Statistical testing (two-sided Fisher's exact test) confirmed no significant difference between groups (P=1.00) [23].
- Conclusion: The findings suggest that for the specific vial types assessed in a clean clinical environment, routine alcohol swabbing did not provide a measurable sterility benefit. The authors note that further research with larger sample sizes is warranted to confirm these findings [23].
Table 2: Culture Results from Alcohol Swabbing Efficacy Study
| Group | Bacterial Growth (CFU > 0) | No Bacterial Growth (CFU = 0) | Total |
|---|---|---|---|
| Swab (70% Alcohol) | 0 | 20 | 20 |
| No-Swab | 0 | 20 | 20 |
| Total | 0 | 40 | 40 |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Aseptic Cell Culture
| Item | Function / Purpose | Application Notes |
|---|---|---|
| 70% Ethanol / Isopropanol | Broad-spectrum disinfectant for surfaces, gloves, and equipment. | Effective against bacteria and fungi; fast-evaporating. The preferred concentration for microbial penetration [23] [21]. |
| HEPA Filters | Provides sterile airflow in BSCs and cleanrooms. | Traps 99.97% of particles ≥0.3 μm, including bacteria and spores. Fragile; must be handled with care and certified annually [20]. |
| Sterile Disposable Pipettes | For precise, aseptic transfer of liquid media and reagents. | Single-use to prevent cross-contamination. Used with a pipettor; tips should not touch non-sterile surfaces [4]. |
| Personal Protective Equipment (PPE) | Creates a barrier to protect cultures from user and user from hazards. | Includes gloves, lab coats, and safety glasses. Worn to minimize shedding of skin and dirt into cultures [4] [22]. |
| Autoclave | Sterilizes equipment, liquids, and waste using steam and pressure. | Standard cycle: 121°C and 15 psi for 15 minutes. Over-autoclaving can degrade heat-sensitive components [21]. |
The integrated use of biosafety cabinets, appropriate personal protective equipment, and 70% ethanol forms an indispensable defense system against contamination in cell culture. While engineering controls like BSCs establish the primary sterile field, the consistent and correct application of PPE and disinfectants by trained personnel is what makes the technique truly aseptic. The protocols and data presented here provide a foundational framework that can be adapted and scaled, from basic research to current Good Manufacturing Practice (cGMP) environments, ultimately safeguarding both scientific investment and patient safety in drug development.
In the context of cell culture aseptic technique protocols, human-derived contamination represents a critical and persistent risk to research integrity. Personnel are a primary source of biological contaminants, including bacteria, fungi, and viruses, which can be introduced through shed skin, hair, respiratory droplets, and improper handling [4] [2]. This application note details evidence-based protocols and methodologies designed to minimize human-derived contamination, thereby safeguarding cell cultures and ensuring the reliability of experimental outcomes in drug development and basic research.
Contamination events carry significant consequences, including invalidated results, wasted resources, and compromised patient safety in translational applications [24]. The following table summarizes common human-derived contaminants and their typical impacts on cell cultures.
Table 1: Common Human-Derived Contaminants and Their Characteristics
| Contaminant Type | Common Sources | Visible Signs in Culture | Impact on Experimental Data |
|---|---|---|---|
| Bacterial | Skin, breath, improper aseptic technique | Cloudy (turbid) media; possible pH change [2] | Altered cell growth; cytokine release; complete culture loss [4] |
| Fungal/Yeast | Skin, hair, laboratory environment | Fuzzy or powdery colonies (mold); spherical particles (yeast) [2] | Nutrient depletion; culture overgrowth; toxic byproducts [25] |
| Mycoplasma | Oral flora, contaminated reagents | No visible turbidity; subtle morphological changes [2] | Altered metabolism, growth rates, and gene expression [4] |
| Viral | Primary human cell lines, laboratory personnel | Often latent; may require PCR for detection [26] | Changes in cell viability, proliferation, and transcriptome [26] |
Experimental Protocols for Mitigating Human-Derived Contamination
Protocol 1: Personal Hygiene and Preparation for Laboratory Entry
Principle: To establish a physical and procedural barrier between the researcher and the sterile cell culture environment [2].
Materials:
- Dedicated laboratory shoes or shoe covers [27]
- Clean, non-shedding lab coat (buttoned/zipped) [2]
- Nitrile or latex gloves
- Hair net or bouffant cap
- Safety glasses or face shield
- Hand soap and 70% ethanol for disinfection [4]
Methodology:
- Remove External Clothing Items: Store personal items like jackets, bags, and hats in a designated area outside the cell culture laboratory [4].
- Hand Washing: Thoroughly wash hands and forearms with soap and water for at least 20 seconds, drying with disposable paper towels [4].
- Don Personal Protective Equipment (PPE): In sequence, put on:
- Final Disinfection: Upon entering the culture room or before approaching the biosafety cabinet (BSC), disinfect gloved hands with 70% ethanol [4].
Protocol 2: Aseptic Workflow within a Biosafety Cabinet (BSC)
Principle: To maintain sterility of the work area and prevent contamination during open-container manipulations [2].
Materials:
- Laminar Flow Biosafety Cabinet (BSC)
- 70% ethanol and lint-free wipes
- Pre-sterilized pipettes, tips, and culture vessels
- Bunsen burner or alcohol lamp (if used by the institution) [2]
- Waste container for used tips and disposable items
Methodology:
- BSC Preparation: Turn on the BSC and allow it to run for at least 15 minutes to purge particulate matter from the work surface [2]. Wipe all interior surfaces—including the work area, side walls, and back—with 70% ethanol [4] [2].
- Material Organization: Arrange all necessary sterile reagents, media, and equipment in an uncluttered manner within the cabinet. Ensure items are placed at least six inches from the front grille to maintain laminar airflow [2].
- Aseptic Handling:
- Work deliberately and slowly to minimize turbulence [4].
- Flame the necks of bottles and flasks using a Bunsen burner or alcohol lamp before opening and after closing to create a sterile convection current [2].
- When removing caps, never place the sterile inner surface face-up. Place it face-down on the disinfected work surface [4].
- Avoid speaking, singing, or whistling over open containers to prevent droplet contamination [4].
- Never use a sterile pipette more than once to avoid cross-contamination [4].
- Cleanup: Discard all waste materials. Upon completion of work, wipe down the BSC interior surfaces again with 70% ethanol [2].
Protocol 3: Monitoring and Verification of Contamination
Principle: To routinely screen for overt and covert contaminants to validate the health and sterility of cell cultures [2].
Materials:
- Inverted phase-contrast microscope
- Mycoplasma detection kit (e.g., PCR-based, Hoechst staining)
- Sterile culture media for negative controls
Methodology:
- Daily Visual Inspection: Observe culture media for cloudiness (turbidity) or unusual color changes, which can indicate bacterial growth [2].
- Microscopic Examination: Daily, examine cells under an inverted microscope for signs of contamination. Look for:
- Routine Mycoplasma Testing: Perform mycoplasma testing quarterly or for each new cell line introduced into the laboratory, using a validated method such as PCR [2].
- Control Cultures: Maintain negative control cultures (media only) to monitor the sterility of reagents and the environment.
Workflow Visualization
The following diagram illustrates the logical workflow for personnel entering and working within a cell culture facility, integrating the protocols outlined above.
Personal Hygiene and Aseptic Workflow for Cell Culture
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for executing the protocols and maintaining a contamination-free cell culture environment.
Table 2: Essential Materials and Reagents for Contamination Control
| Item | Function/Application | Key Considerations |
|---|---|---|
| 70% Ethanol | Primary disinfectant for gloves, BSC surfaces, and exterior of reagent bottles [4] [2]. | More effective than higher concentrations due to better penetration [2]. |
| Sterile Disposable Gloves | Creates a barrier between personnel and cultures; prevents transfer of skin flora [4]. | Change frequently, especially after touching non-sterile surfaces [2]. |
| Laminar Flow BSC | Provides a HEPA-filtered, sterile work environment for culture manipulations [27] [2]. | Must be certified annually; run for 15+ min before use to stabilize airflow [2]. |
| HEPA Filter | Traps 99.9% of airborne particulates and microbes, creating the sterile air for the BSC [27]. | Integrity must be regularly tested; lifespan depends on usage [27]. |
| Sterile Pipettes and Tips | For sterile liquid transfer without introducing contaminants [4]. | Use single-use only to prevent cross-contamination between cultures and reagents [4]. |
| Mycoplasma Detection Kit | For routine screening of this common, invisible contaminant [2]. | PCR-based methods are highly sensitive and recommended for definitive results [2]. |
| Automated Liquid Handler | Reduces human error and direct contact with samples, minimizing contamination risk [27]. | Enclosed hood with HEPA filtration provides an additional sterile barrier [27]. |
From Theory to Practice: A Step-by-Step Aseptic Protocol for the Lab
Within the framework of aseptic technique protocols for cell culture, the initial setup of the biosafety cabinet (BSC) and sterile field constitutes the most critical step for ensuring research integrity. Successful cell culture depends heavily on keeping cells free from contamination by microorganisms such as bacteria, fungi, and viruses [4]. Nonsterile supplies, airborne particles, unclean equipment, and dirty work surfaces are all potential sources of biological contamination that can compromise experimental results and lead to costly losses of valuable cell lines and reagents [4]. This protocol outlines detailed methodologies for establishing a proper sterile field and preparing the biosafety cabinet, providing the foundation for all subsequent aseptic procedures in mammalian cell culture.
Materials and Reagents
Research Reagent Solutions
The following reagents are essential for proper disinfection and maintenance of the sterile field:
Table 1: Essential Reagents for Sterile Field Preparation
| Reagent | Concentration | Primary Function | Application Notes |
|---|---|---|---|
| Ethanol | 70% | Surface disinfection; effective against most bacteria and fungi [28] | Primary disinfectant for wiping down BSC surfaces and gloves; allows sufficient contact time for evaporation [4] [2] |
| Sodium Hypochlorite | 1% | Powerful disinfectant for contamination incidents [28] | Used for periodic deep cleaning or after known contamination events [28] |
| Virkon-S | 1% | Broad-spectrum disinfectant for persistent contaminants [28] | Applied in triple-cleaning strategy for stubborn contamination sources [28] |
| Sterile Distilled Water | N/A | Removing disinfectant residues | Used after bleach application to prevent corrosion of stainless steel surfaces [29] |
Methodology
Pre-Preparation Procedures
Proper preparation begins before entering the cell culture laboratory:
- Personal Hygiene: Wash hands thoroughly with germicidal soap before entering the laboratory [29].
- Personal Protective Equipment (PPE): Don appropriate PPE including a long-sleeved lab coat, gloves, and safety goggles [4] [2]. Gloves should be changed frequently, especially after touching non-sterile surfaces [2].
- Material Gathering: Collect all necessary materials before beginning work to minimize movement during the procedure. Extra supplies should be placed outside the BSC [29].
Biosafety Cabinet Setup Protocol
The BSC (Class II) is designed to prevent escape of pathogens into the workers' environment and bar contaminants from the research work zone through HEPA-filtered air [29].
Table 2: Sequential BSC Preparation Protocol
| Step | Procedure | Purpose | Timing/Duration |
|---|---|---|---|
| 1. Cabinet Activation | Turn on BSC and allow to run for at least 15 minutes [2] (or 5 minutes [30]) before beginning work. | Allows cabinet airflow to stabilize and purges airborne contamination from work area [29] [2]. | 15-30 minutes pre-work |
| 2. Surface Disinfection | Thoroughly wipe all interior surfaces (work surface, side walls, back panel) with 70% ethanol [4] [2]. | Eliminates microbial contaminants from surfaces; 70% concentration provides optimal bactericidal activity [28]. | Before material placement |
| 3. Material Placement | Arrange all necessary materials strategically within the hood, ensuring workflow from "clean to dirty" [29]. | Organized workflow prevents crossing contaminated items over clean ones [29]. | After surface disinfection |
| 4. Item Disinfection | Wipe outside of all bottles, flasks, and containers with 70% ethanol before introducing to BSC [4]. | Prevents introduction of contaminants from container exteriors. | Before opening containers |
| 5. Pre-Work Purging | Once materials are placed, wait 2-5 minutes before beginning work [29]. | Allows sufficient time for cabinet air flow to purge airborne contaminants introduced during setup [29]. | 2-5 minutes |
Establishing and Maintaining the Sterile Field
The following practices are essential for maintaining sterility during work procedures:
- Spatial Awareness: Keep all equipment and materials at least 4-6 inches inside the cabinet window and away from the front grille [29] [2]. Never block the rear exhaust grill [29].
- Traffic Control: Minimize room activity that can create disruptive air currents [29]. The ideal location for a BSC is at a quiet end of the laboratory, removed from doorways and air conditioning/heating vents [29].
- Movement Minimization: Limit rapid movements of hands and arms into and out of the BSC, as such movement causes turbulent air currents that disrupt the air barrier [29].
- Container Management: When removing caps, place them with the opening facing down on the sterile work surface [4]. Minimize the time that containers remain open [4].
- Flaming Practices: While some protocols recommend flaming bottle necks with a Bunsen burner [2], others explicitly advise against using a Bunsen burner in a BSC as the flame can cause turbulence in the airstream and the heat may damage the HEPA filter [29]. If a procedure requires a flame, use a burner with a pilot light and place it to the rear of the work space [29].
The workflow for the complete pre-work preparation process is systematically outlined in the following diagram:
Quality Control and Troubleshooting
BSC Certification and Maintenance
Regular certification and maintenance of the BSC are imperative for proper function:
- Certification Schedule: BSCs must be tested and certified at the time of installation, after moving, after servicing internal plenums, after replacing filters, and at least annually thereafter [29].
- Filter Monitoring: Many BSCs have gauges to indicate pressure differential across the supply filters. If filters must be replaced, the BSC must be decontaminated first [29].
- Operational Considerations: Unless the BSC is hard-ducted to an outside exhaust system, do not use noxious, toxic, or corrosive chemicals which create a hazardous atmosphere since the BSC recirculates filtered air into the laboratory space but does not remove gas or vapor state contaminants [29].
Contamination Source Identification
When contamination occurs, systematic identification of sources is necessary:
- Incubator Inspection: Incubators are frequently identified as contamination sources, particularly their internal air, shelves, and water trays [28].
- Microscope Examination: Microscope stages and objectives can harbor contaminants and are often overlooked [28].
- Environmental Monitoring: Regular monitoring of laboratory surfaces using sterile swabs and blood agar plates can identify contamination sources before they affect cultures [28].
Ultraviolet Light Considerations
Ultraviolet (UV) lamps are sometimes used in BSCs but require careful consideration:
- Limited Efficacy: UV light is useful for extra precaution in keeping the work area decontaminated between uses but should never be relied on alone to disinfect a contaminated work area [29].
- Safety Hazards: UV lamps must be turned off when the room is occupied to protect occupants' skin and eyes from UV exposure, which can cause burns to the corneas and skin cancer [29].
- Maintenance Requirements: UV lamps must be cleaned weekly with 70% ethanol to maintain effectiveness and tested periodically to ensure sufficient energy output [29].
Proper pre-work preparation of the sterile field and biosafety cabinet establishes the foundational conditions necessary for successful cell culture experimentation. By meticulously following these protocols for BSC setup, material preparation, and sterile field maintenance, researchers can significantly reduce the risk of biological contamination, thereby protecting valuable cell cultures, ensuring experimental reproducibility, and maintaining the integrity of scientific research. Regular quality control measures, including BSC certification and systematic monitoring for contamination sources, provide additional safeguards for maintaining optimal aseptic conditions in the cell culture laboratory.
Aseptic technique is a fundamental set of procedures designed to create a barrier between microorganisms in the environment and the sterile cell culture, thereby reducing the probability of contamination [4]. In the context of routine culture, consistent application of aseptic technique is critical for maintaining cell line integrity, ensuring experimental reproducibility, and protecting valuable laboratory resources. Contamination events can compromise research outcomes, lead to erroneous conclusions, and result in significant time and financial losses [11]. This guide provides a comprehensive, practical checklist and detailed protocols to help researchers establish and maintain impeccable aseptic practices for successful cell culture work.
Fundamental Principles of Aseptic Technique
The core objective of aseptic technique is to prevent the introduction of contaminants (bacteria, fungi, viruses, and chemical impurities) into cell cultures and reagents. This is achieved through two complementary approaches: creating a sterile operating environment and preventing the introduction of foreign microorganisms during handling and cultivation [31]. A key distinction exists between sterile technique, which aims to eliminate every potential microorganism, and aseptic technique, which focuses on maintaining a previously sterilized environment by not introducing contamination [4] [32]. For routine culture, this involves a mindset of constant vigilance, where every action is performed with the intention of preserving sterility.
The Comprehensive Aseptic Technique Checklist
The following checklist provides a structured framework for ensuring aseptic conditions before, during, and after routine culture procedures. Use it to standardize practices across your laboratory.
Table 1: Comprehensive Aseptic Technique Checklist for Routine Culture
| Category | Task | Completed (✓/✗) |
|---|---|---|
| Pre-Work Preparation | Confirm all necessary materials are available and sterilized. | |
| Perform appropriate hand hygiene (washing with soap and water). | ||
| Don appropriate Personal Protective Equipment (PPE) (lab coat, gloves). | ||
| Tie back long hair. | ||
| Work Area & BSC Setup | Ensure the Biosafety Cabinet (BSC) is in an area free from drafts and through traffic. | |
| Wipe the BSC work surface and all items with 70% ethanol before introduction. | ||
| UV sterilize the BSC for a minimum of 30 minutes pre-use (if applicable). | ||
| Run the BSC blower for at least 5 minutes before starting work. | ||
| Organize the work surface to be uncluttered, containing only essential items. | ||
| Reagents & Media | Sterilize all reagents, media, and solutions prepared in-lab via autoclaving or filtration. | |
| Wipe the outside of all bottles, flasks, and plates with 70% ethanol before placing in BSC. | ||
| Inspect reagents for cloudiness, floating particles, or unusual color; discard if contaminated. | ||
| Keep all containers capped when not in use. Store plates in sterile re-sealable bags. | ||
| Sterile Handling | Work slowly, deliberately, and mindfully. Avoid rapid movements that disrupt airflow. | |
| Flame-sterilize inoculating loops to red-hot before and after use; allow to cool. | ||
| Flame the necks of bottles and test tubes by passing them through a Bunsen burner flame. | ||
| Use only sterile glass or disposable plastic pipettes. Use each pipette only once. | ||
| Place caps or covers face-down on the work surface if they must be removed. | ||
| Avoid touching sterile pipette tips to non-sterile surfaces (e.g., bottle threads). | ||
| Minimize talking, singing, or whistling during procedures. | ||
| Post-Work Cleanup | Mop up any spillage immediately and wipe the area with 70% ethanol. | |
| Remove all items from the BSC and wipe the surface again with 70% ethanol. | ||
| UV sterilize the BSC for 5 minutes post-use (if applicable). | ||
| Properly dispose of all contaminated waste. |
Experimental Protocols for Key Aseptic Procedures
Protocol: Sterile Transfer Using an Inoculating Loop
This protocol is essential for transferring microorganisms between solid and liquid media while maintaining purity [33].
- Sterilize the Loop: Hold the handle of the wire loop close to the top. Sterilize the loop by heating it to red-hot in the roaring blue cone of a Bunsen burner flame. Heat the entire length of the wire gradually to prevent splattering [33].
- Cool the Loop: Allow the sterilized loop to cool for a few seconds in the sterile air near the flame. Do not wave it around or place it on a non-sterile surface [31].
- Sample the Culture: For a broth culture, briefly flame the neck of the tube. Insert the cooled loop and remove a loopful of culture. For a plate, lift the lid slightly, cool the loop by touching an empty area of agar, then touch a single colony.
- Inoculate: Transfer the sample to the new, sterile medium (e.g., streak onto an agar plate, inoculate a broth tube, or use a zigzag pattern on an agar slant) [31].
- Re-sterilize: Immediately after the transfer, re-sterilize the loop in the flame to destroy any remaining microorganisms before placing it down.
Protocol: Aseptic Pipetting and Liquid Handling
This protocol ensures sterile transfer of liquid cultures, media, and reagents [4] [33].
- Select Pipette: Use a sterile graduated or Pasteur pipette. Remove it from its wrapper by the end containing the cotton wool plug, touching as little of the shaft as possible.
- Attach Teat: Fit a sterile teat. It can be helpful to dip the teat first in sterile liquid to lubricate it.
- Aspirate Liquid: Hold the pipette like a pen. Squeeze the teat before placing the tip into the liquid to avoid introducing air bubbles. Gently release pressure to draw up the required volume, ensuring liquid does not wet the cotton plug [33].
- Transfer Liquid: Move the pipette to the receiving vessel. Flame the neck of the vessel if it is a bottle or tube. Dispense the liquid gently.
- Discard: Immediately after use, place the contaminated pipette into a nearby pot of disinfectant. Remove the teat only once the pipette is within the discard pot.
Protocol: Flaming the Neck of Bottles and Test Tubes
This procedure creates an upward convection current that prevents airborne contaminants from entering vessel openings [33].
- Loosen Cap: Loosen the cap of the bottle or tube so it can be removed easily with one hand.
- Remove Cap: Hold the vessel in your non-dominant hand. Remove the cap or cotton wool plug with the little finger of your dominant hand (curled towards the palm). Do not place the cap on the bench.
- Flame the Neck: Pass the neck of the vessel forwards and back through the hottest part of the Bunsen burner flame (above the inner blue cone). Do not hold it in place.
- Perform Procedure: While the neck is still warm, quickly perform the required procedure (e.g., pouring, pipetting).
- Recap: Flame the neck once more and replace the cap using the little finger. Turn the bottle, not the cap, to secure it.
Workflow and Logical Relationships
The following diagram illustrates the logical sequence of actions required to establish and maintain an aseptic environment for routine culture, from preparation to final cleanup.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful aseptic culture relies on the consistent use of specific, high-quality reagents and materials. The table below details the core components of this toolkit.
Table 2: Essential Materials and Reagents for Aseptic Culture
| Item | Function & Application | Key Considerations |
|---|---|---|
| 70% Ethanol | Primary disinfectant for wiping down work surfaces, gloves, and the outside of containers introduced into the BSC [4] [33]. | More effective than higher concentrations due to slower evaporation, allowing more contact time with microbes. |
| Sterile Cell Culture Media | Provides essential nutrients, growth factors, and hormones to support cell growth and proliferation. | Must be pre-sterilized (typically by filtration). Check for cloudiness or color change before use, indicating potential contamination [4]. |
| Sterile Pipettes (Plastic/Glass) | For precise, sterile transfer of liquid cultures, media, and reagents. | Disposable plastic pipettes are single-use. Sterile glass pipettes must be re-sterilized by autoclaving after each use [4]. |
| Personal Protective Equipment (PPE) | Forms a barrier between the researcher and biological materials, protecting both the culture and the personnel [4] [34]. | Includes lab coat, gloves, and safety glasses. Gloves should be changed frequently and if contaminated. |
| Inoculating Loops/Needles | Essential tools for transferring and streaking microbial cultures. | Must be sterilized by heating to red-hot in a Bunsen burner flame before and after every use to prevent cross-contamination [33]. |
| Bunsen Burner | Creates an updraft and provides a sterile zone for procedures like flaming loops and vessel necks [33]. | The flame should have a roaring blue cone. Work is performed in the sterile hot air surrounding the flame. |
| Disinfectant (e.g., 1% Virkon) | Used for decontaminating surfaces and for discarding contaminated liquids and equipment [33]. | A safer alternative to ethanol for student use; surface must remain wet for at least 10 minutes for effective disinfection. |
Mastering aseptic technique is not a one-time event but a continuous commitment to quality and precision in the cell culture laboratory. By systematically implementing the checklist, protocols, and principles outlined in this guide, researchers can build a robust defense against contamination. This diligence directly translates to more reliable data, reproducible experiments, and the efficient use of time and resources, thereby accelerating the pace of scientific discovery and drug development.
In cell culture, the integrity of experimental results is entirely dependent on the quality of the liquid handling techniques employed. Proper manipulation of liquids, media, and reagents through precise pipetting, careful pouring, and disciplined container management forms the first and most critical line of defense against contamination. These fundamental skills are essential for maintaining the sterility of the workspace, ensuring the viability of cell lines, and guaranteeing the reproducibility of scientific data [4]. This guide details the core principles and protocols for handling materials in a cell culture setting, framed within the broader context of aseptic technique essential for successful research and drug development.
Fundamental Principles of Aseptic Liquid Handling
The core objective of aseptic technique is to prevent microorganisms from the environment from contaminating sterile cultures, media, and reagents [4]. This is achieved by creating and maintaining barriers between sterile and non-sterile surfaces.
- Aseptic vs. Sterile Technique: It is crucial to distinguish between these two concepts. Sterilization is a process that destroys all microbial life, creating a state of absolute freedom from microorganisms (e.g., autoclaving). Aseptic technique, conversely, is the set of practices used to maintain sterility by preventing contaminants from contacting sterile materials during handling [2].
- The Sterile Field: The primary barrier is the biosafety cabinet (BSC) or laminar flow hood, which provides a HEPA-filtered, sterile airflow [2]. All manipulations with open containers should occur within this space. A properly maintained and disinfected workspace is fundamental; the working surface must be uncluttered and thoroughly wiped with 70% ethanol before and after work [4] [35].
- Personal Protective Equipment (PPE): Lab personnel must wear appropriate PPE—including a clean lab coat, gloves, and sometimes safety glasses—to minimize the introduction of contaminants from the body and clothing [4] [2]. Gloved hands should be wiped with 70% ethanol before working in the BSC.
Pipetting Techniques and Protocols
Pipetting is the most common method for transferring liquids in the cell culture lab. Accuracy and sterility are paramount.
Air Displacement Pipette Principles
Most laboratory pipettes are air displacement pipettes. They operate by moving a piston to create a vacuum that draws liquid into a disposable tip. A critical air cushion separates the piston from the liquid, preventing contamination of the pipette interior [36] [37]. The accuracy of this system can be affected by temperature, liquid density, and vapor pressure [38].
Forward and Reverse Pipetting
The choice between forward and reverse pipetting is determined by the physical properties of the liquid being handled. The table below provides a comparative overview.
Table 1: Comparison of Forward and Reverse Pipetting Techniques
| Feature | Forward Pipetting (Standard Mode) | Reverse Pipetting |
|---|---|---|
| Primary Use | Aqueous solutions (buffers, diluted acids, culture media) [36] [39] | Viscous, foaming, or volatile liquids (glycerol, detergents, proteins, organic solvents) [36] [37] |
| Technique | 1. Press plunger to first stop.2. Aspirate liquid.3. Dispense by pressing to first stop, then press to second stop (blow-out) to expel residual liquid [36] [37]. | 1. Press plunger to second stop.2. Aspirate liquid (excess is drawn in).3. Dispense by pressing only to the first stop, leaving excess in the tip, which is then discarded [36] [38]. |
| Mechanism | Delivers the exact volume set on the pipette [37]. | Aspirates excess to compensate for liquid retained on the tip wall, ensuring accurate delivery of the set volume despite retention [36]. |
Aseptic Pipetting Protocol
The following workflow outlines the key steps for sterile pipetting within a biosafety cabinet. Adhering to this protocol minimizes the risk of contaminating your samples, reagents, and cultures.
Essential Pipetting Tips for Accuracy
- Pre-wetting: For volatile compounds or to improve accuracy, aspirate and expel the liquid 2-3 times before taking the sample for delivery. This saturates the air cushion within the tip, reducing evaporation [36] [39].
- Consistent Immersion: Immerse the tip just 2-3 mm below the liquid's surface for small volumes. Too little immersion can lead to air aspiration, while too much can cause liquid to cling to the tip's exterior [39].
- Smooth Operation: Use consistent plunger pressure and speed during aspiration and dispensing. Rapid movements can cause splashing, inaccuracies, and aerosol formation [39].
- Temperature Equilibrium: Allow pipettes, tips, and liquids to equilibrate to room temperature before use. Temperature differences cause expansion or contraction of the air cushion, leading to significant volume errors [36] [39] [38].
- Minimal Handling: Handle pipettes loosely and set them down in a stand when not in use. Body heat transferred to the pipette can affect the temperature of the air inside and lead to volume variations [39].
Pouring, Transfer, and Container Management
While pipetting is preferred for precision, pouring is sometimes necessary for larger volumes. Both activities require stringent container management.
Aseptic Pouring Protocol
Pouring is a higher-risk activity for contamination and should be performed with extreme care.
- Flaming: Before opening, briefly pass the neck of a glass bottle or flask through a Bunsen burner flame (if outside a BSC) or use an alcohol lamp. This creates an upward convection current that prevents airborne particles from falling into the container [2]. The cap should be held in the hand, facing down, and never placed on the bench [4].
- Controlled Pouring: Work slowly and deliberately. Pour against the inner neck of the receiving vessel to create a single stream and minimize splashing. Avoid pouring between vessels if sterile pipettes are available, as pouring creates more turbulence and aerosol exposure than pipetting [4].
Container Management Workflow
Proper handling of culture vessels, media bottles, and reagent containers is a continuous process throughout any laboratory procedure.
The Scientist's Toolkit: Essential Materials and Reagents
Table 2: Key Research Reagent Solutions and Materials for Aseptic Handling
| Item | Function & Application |
|---|---|
| 70% Ethanol | The primary disinfectant for decontaminating work surfaces, the exterior of containers, gloved hands, and equipment. Its effectiveness is concentration-dependent [4] [2]. |
| Air Displacement Pipettes | The workhorse for accurate measurement and transfer of small liquid volumes (1 µL to 10 mL), used with sterile disposable tips for most aqueous solutions [36] [37]. |
| Sterile, Filtered Pipette Tips | Create an airtight seal with the pipette cone. Filter tips are especially important for preventing aerosol contamination of the pipette shaft when working with biological samples [36] [38]. |
| Biosafety Cabinet (BSC) | Provides a HEPA-filtered sterile work environment, protecting both the cell culture from environmental contaminants and the user from potential biohazards [4] [2]. |
| Personal Protective Equipment (PPE) | Includes lab coats, gloves, and safety glasses. Forms a barrier to prevent contamination of cultures from the user and protects the user from hazardous materials [11] [4]. |
| Sterile Culture Media | Nutrient-rich solutions (e.g., DMEM, RPMI) formulated to support specific cell growth needs. Must be sterile and often supplemented with serum, antibiotics, and other factors [40]. |
| Sterile Reagents & Solutions | Includes trypsin for cell detachment, phosphate-buffered saline (PBS) for washing, and other specialized reagents. All must be sterilized and handled aseptically [4] [40]. |
Quality Control and Troubleshooting
- Pipette Calibration: Regular calibration is non-negotiable for data integrity. Pipettes should be calibrated every 3-12 months, depending on usage frequency and application criticality, following ISO 8655 standards [37] [38]. This typically involves gravimetric measurement (weighing water) to check dispensed volume accuracy [37].
- Contamination Monitoring: Routinely check cultures and reagents for signs of contamination. Bacterial contamination often manifests as sudden turbidity in the medium; fungal contamination appears as floating mycelial spheres or filaments; and mycoplasma contamination may cause subtle changes in cell growth and morphology without media clouding [2]. Any contaminated material should be immediately quarantined and decontaminated.
By integrating these detailed protocols for pipetting, pouring, and container management into daily practice, researchers and drug development professionals can establish a robust foundation of aseptic technique, thereby safeguarding their valuable cell cultures and ensuring the generation of reliable and reproducible scientific data.
Within the broader context of aseptic technique protocol research, the fundamental division between adherent and suspension cell cultures necessitates distinct methodological approaches. The core principle of successful cell culture lies in mimicking the in vivo environment, which for anchorage-dependent cells means providing a solid substrate, and for non-adherent cells, ensuring a homogenous liquid environment [41] [42]. This document provides detailed application notes and protocols, framed within a thesis on aseptic techniques, to guide researchers and drug development professionals in adapting their methods for these specific cell types. The adherence to correct protocols is not merely a procedural requirement but a critical factor in maintaining cell health, functionality, and the integrity of experimental data, especially as the field advances toward more complex systems like cell and gene therapies and large-scale biomanufacturing [43] [41].
Fundamental Differences and Selection Criteria
Comparative Analysis of Culture Platforms
The choice between adherent and suspension culture systems is foundational to experimental design and process scaling. Each platform offers distinct advantages and poses specific challenges, which are summarized in the table below.
Table 1: Key Differences Between Adherent and Suspension Culture Platforms
| Parameter | Adherent Culture | Suspension Culture |
|---|---|---|
| Growth Mechanism | Requires attachment to a solid substrate [41] [42]. | Grows free-floating in the culture medium [41] [44]. |
| Scalability | Limited by available surface area; scaled out by adding more units [43] [42]. | Highly scalable in volume using bioreactors [41] [45]. |
| Process Handling | More labor-intensive; requires enzymatic (e.g., trypsin) or mechanical detachment for subculturing [42] [44]. | Less laborious; subcultured via simple dilution [42] [44]. |
| Cell Types | Mesenchymal stem cells (MSCs), iPSCs, HEK293, fibroblasts, epithelial cells [41] [42]. | Hematopoietic cells, immune cells (e.g., Jurkat), CHO cells, adapted HEK293 [41] [42]. |
| Shear Stress | Generally low in static culture [42]. | Higher, due to agitation requirements; may need media additives for protection [42] [45]. |
| Physiological Relevance | Better recapitulates tissue architecture and cell-matrix interactions [42] [45]. | Less suitable for tissue modeling; ideal for cells native to blood or lymph [44] [45]. |
Decision Framework for Culture Method Selection
The following workflow outlines a systematic approach for researchers to select the appropriate culture method based on their cell type and experimental objectives.
Diagram 1: Culture Method Selection Workflow
Essential Materials and Reagent Solutions
Successful culture maintenance relies on a suite of specialized reagents and equipment. The following table catalogs the essential tools for both adherent and suspension culture workflows.
Table 2: Research Reagent Solutions for Cell Culture
| Item | Function | Application Notes |
|---|---|---|
| Culture Vessels (T-flasks, Dishes) | Provides a treated surface for cell attachment and growth. | Used for small-scale adherent culture; surface may be coated with collagen or poly-lysine to enhance attachment [41] [42]. |
| Stirred-Tank Bioreactor | Scalable vessel with agitation for homogeneous suspension culture. | Ideal for large-scale suspension culture of CHO or adapted HEK293 cells; requires optimization to minimize shear stress [41] [42]. |
| Serum-Free Media | Defined formulation without animal serum supports consistent growth. | Crucial for suspension adaptation and biomanufacturing; reduces risk of contamination and variability [43] [42]. |
| Trypsin/EDTA | Enzymatic solution for detaching adherent cells from surfaces. | Critical for passaging adherent cells; must be quenched with serum-containing media post-detachment [42] [44]. |
| Microcarriers | Small beads providing a surface for adherent cells in suspension bioreactors. | Enables scalable culture of anchorage-dependent cells (e.g., MSCs, Vero) in a suspension-like system [42]. |
| Laminar Flow Hood (BSC) | Provides a sterile work environment via HEPA-filtered air. | Non-negotiable for all open aseptic procedures to prevent microbial contamination [4] [2]. |
Detailed Experimental Protocols
Core Protocol 1: Subculturing of Adherent Cells
Adherent cells grow as a monolayer and require periodic passaging to maintain logarithmic growth. This protocol details the process for cells grown in flasks.
Key Materials:
- Pre-warmed culture medium and trypsin-EDTA solution [42] [46].
- Phosphate-buffered saline (PBS) without calcium and magnesium.
- Culture vessel (e.g., T-flask) with adherent cells at 70-80% confluence.
- Centrifuge tubes and a calibrated hemocytometer or automated cell counter.
Methodology:
- Aspiration and Wash: Visually inspect the culture. Aseptically aspirate and discard the spent culture medium. Gently rinse the cell monolayer with PBS to remove residual serum and dead cells, which can inhibit trypsin activity [46].
- Cell Detachment: Add a sufficient volume of pre-warmed trypsin-EDTA solution to cover the monolayer (e.g., 2-3 mL for a T-75 flask). Incubate the flask at 37°C for 2-5 minutes. Observe cells under a microscope until they round up and detach. Gently tap the flask to facilitate complete detachment [42] [46].
- Enzyme Neutralization: Add a volume of complete culture medium (containing serum) that is at least double the volume of trypsin used. Pipette the medium across the surface to collect all cells and neutralize the trypsin.
- Cell Collection and Counting: Transfer the cell suspension to a centrifuge tube. Centrifuge at 200 x g for 5 minutes. Aspirate the supernatant and resuspend the cell pellet in fresh, pre-warmed complete medium. Perform a cell count and viability assessment using Trypan Blue exclusion [46].
- Re-seeding (Split): Seed an appropriate number of viable cells into new culture vessels containing fresh, pre-warmed medium. The split ratio is cell line-dependent and should be determined empirically to achieve 70-80% confluence within the desired timeframe.
Core Protocol 2: Maintenance of Suspension Cells
Suspension cells are maintained by dilution, as they do not require enzymatic detachment. This protocol is typical for cells grown in shaker flasks or small-scale bioreactors.
Key Materials:
- Suspension cell line (e.g., CHO, Jurkat, adapted HEK293) in logarithmic growth phase.
- Pre-warmed, appropriate serum-free suspension medium.
Methodology:
- Cell Density Assessment: Aseptically take a small sample (e.g., 1 mL) from the suspension culture. Determine the cell concentration and viability using a hemocytometer or automated cell counter.
- Culture Dilution: Calculate the volume of cell suspension required to initiate a new culture at the recommended seeding density (e.g., 2-5 x 10^5 cells/mL) in a fresh vessel containing pre-warmed medium. There is no need for centrifugation in routine passaging.
- Agitation and Incubation: Cap the vessel and place it on an orbital shaker platform or inside a stirred bioreactor. Maintain constant, gentle agitation to keep the cells in suspension and ensure adequate gas exchange. Incubate at 37°C with 5% CO₂.
- Monitoring: Monitor cell growth daily by counting cells and assessing viability. Passage the cells when they reach the maximum density recommended for the specific cell line, typically in the late logarithmic growth phase, to prevent nutrient depletion and loss of viability.
Aseptic Technique and Contamination Control
Maintaining aseptic conditions is paramount, regardless of the culture platform. Contamination can compromise months of work and render data useless [2].
Critical Aseptic Practices:
- Personal Protective Equipment (PPE): Always wear a lab coat, gloves, and safety glasses. Gloves should be disinfected with 70% ethanol before working in the biosafety cabinet (BSC) [4] [2].
- Biosafety Cabinet Management: Turn on the BSC 15 minutes prior to use. Disinfect all interior surfaces with 70% ethanol before and after use. Arrange all necessary materials inside the cabinet in an orderly fashion before starting work, minimizing movement once begun [2].
- Sterile Handling: Flame the necks of bottles and flasks before opening and after closing to create a sterile convection current [2]. Work deliberately and quickly to minimize the exposure of sterile surfaces and media to the environment. Never use a pipette more than once without sterilization to avoid cross-contamination [4].
Advanced Applications and Industrial Context
The choice between adherent and suspension systems has significant implications in industrial biotechnology and therapy development. The following workflow illustrates the industrial decision-making process for viral vector manufacturing, a key area in gene therapy.
Diagram 2: Industrial Process Selection
As illustrated, adherent platforms have proven commercially viable for therapies like Luxturna (using roller bottles) and Zolgensma (using the iCELLis fixed-bed bioreactor), particularly where doses are low or patient populations are small [43]. The industry principle of "not letting perfection be the enemy of progress" has allowed these therapies to reach the market using optimized adherent processes [43]. However, for products requiring massive volumes, such as many vaccines or systemic gene therapies, the scalability of suspension culture in stirred-tank bioreactors makes it the dominant and more cost-effective choice [43] [42]. A notable example is the transition of Glybera's manufacturing from an adherent process for early studies to a suspension process to meet higher vector quantity demands [43].
Troubleshooting and Optimization Strategies
Even with rigorous protocols, challenges can arise. The table below outlines common issues and potential solutions for both culture types.
Table 3: Troubleshooting Common Cell Culture Challenges
| Problem | Potential Causes | Corrective Actions |
|---|---|---|
| Slow Growth (Adherent) | Over-confluence, poor attachment, suboptimal media, contamination. | Passage at lower density; ensure surface is properly coated; check media formulation and pH; test for mycoplasma [42] [46]. |
| Poor Cell Detachment | Inactive trypsin, insufficient incubation time, overgrown cells. | Use fresh, pre-warmed trypsin; increase incubation time slightly; passage cells before they become over-confluent [42]. |
| Low Viability (Suspension) | Agitation-induced shear stress, nutrient depletion, toxic metabolite buildup. | Optimize agitation speed; add surfactants (e.g., Pluronic F-68); increase feeding frequency or use perfusion systems [42]. |
| Cell Clumping (Suspension) | Lack of agitation, presence of cell debris, excessive divalent cations. | Ensure consistent agitation; subculture before stationary phase; use EDTA in media to reduce cell-cell adhesion [42]. |
| Contamination (All) | Break in aseptic technique, non-sterile reagents, compromised equipment. | Quarantine contaminated cultures; review and practice aseptic techniques; filter-sterilize reagents; perform routine equipment maintenance [4] [2]. |
The adaptation of aseptic technique protocols for specific cell types is a critical competency in biomedical research and development. A deep understanding of the inherent requirements of adherent versus suspension cultures—from basic passaging and scale-up principles to advanced bioprocess design—is fundamental to ensuring data reproducibility and progressing therapeutic innovations. As the field evolves, hybrid technologies like microcarriers and organ-on-a-chip models continue to blur the lines between these traditional categories. However, the foundational principles outlined in this document—rigorous aseptic practice, informed platform selection, and tailored protocol execution—remain the bedrock of successful cell culture.
The transition from conventional two-dimensional (2D) cell culture to three-dimensional (3D) models, including spheroids, organoids, and complex co-culture systems, represents a paradigm shift in biomedical research. These advanced models more accurately simulate the natural in vivo environment, including tissue architecture, cell-cell interactions, and metabolic gradients, thereby providing more physiologically relevant data for drug discovery and developmental biology [47]. However, this increased biological complexity introduces significant technical challenges in maintaining aseptic conditions throughout experimental workflows. The extended culture periods required for 3D model development and the manipulation-intensive nature of co-culture establishment create multiple critical control points for potential microbial contamination. This application note details specialized aseptic protocols designed to address the unique vulnerabilities of 3D spheroid and co-culture systems, providing a critical framework for ensuring data integrity and reproducibility within a thesis focused on cell culture aseptic technique protocols.
Unique Aseptic Challenges in 3D and Co-culture Systems
Working with 3D cultures exposes researchers to contamination risks that are less prevalent or non-existent in standard 2D cultures. The table below summarizes the primary challenges and their implications for experimental outcomes.
Table 1: Key Aseptic Challenges in 3D and Co-culture Systems
| Challenge | Description | Impact on Experiment |
|---|---|---|
| Extended Culture Duration | 3D spheroids and organoids often require culture periods of weeks, unlike the days typical for 2D cultures [48]. | Prolonged exposure increases probability of environmental contamination, compromising long-term studies. |
| Frequent Media Changes | 3D structures require nutrient-rich media, necessitating frequent feeding, which increases manipulation frequency [49]. | Each manipulation is a potential contamination event; standard pipetting can aspirate and damage spheroids. |
| Complex Matrix Materials | Use of basement membrane extracts (e.g., Matrigel) and other hydrogel scaffolds [50] [48]. | These materials can act as growth media for contaminants if not handled aseptically. |
| Multiple Cell Source Handling | Co-culture systems involve isolating and combining different cell types (e.g., epithelial and immune cells) [50] [51]. | Combining cells from multiple sources increases the risk of introducing contaminants from one cell population to another. |
| Limited Antibiotic Use | Researchers often avoid antibiotics to preserve natural microbiome interactions or avoid cellular stress responses [28]. | Eliminates a safety net, placing greater emphasis on perfect aseptic technique. |
The diagram below illustrates the primary contamination pathways and their relationships in a 3D cell culture workflow, highlighting critical control points.
Essential Aseptic Technique Foundations
Personal Protective Equipment and Laboratory Hygiene
Strict personal hygiene forms the first defensive barrier against contamination. Researchers must wear appropriate personal protective equipment (PPE), including laboratory coats, gloves, and, if necessary, safety glasses or face shields. Wearing PPE not only protects the researcher from biological hazards but also significantly reduces the probability of contamination from shed skin as well as dirt and dust from clothing [4]. Before initiating work, researchers should wash their hands thoroughly and ensure that all personal items are stored away from the aseptic work area.
Sterile Work Area Management
The biosafety cabinet (BSC), or laminar flow hood, is the cornerstone of the sterile work area and must be utilized correctly.
- Setup and Operation: The BSC should be located in an area with no through traffic and free from drafts from doors, windows, and other equipment. It must be turned on and allowed to run for at least 15 minutes before use to purge particulate matter from the work area. The work surface should be uncluttered and contain only items required for the specific procedure [4].
- Surface Decontamination: Before and after all work, and especially after any spillage, the entire interior work surface must be thoroughly wiped with 70% ethanol [4] [28]. All items placed into the BSC, including reagent bottles, pipette tip boxes, and culture vessels, should also be wiped with 70% ethanol.
- Proper Workflow: It is crucial to work slowly and deliberately, mindful of aseptic technique. All bottles, flasks, and other containers should be capped when not in immediate use to minimize exposure to the environment. Sterile glass or disposable plastic pipettes should be used with a pipettor for all liquid handling, and each pipette should be used only once to avoid cross-contamination [4].
Specialized Protocols for 3D Spheroid and Co-culture Systems
Protocol 1: Aseptic Generation of 3D Spheroids
This protocol is adapted for using ultra-low attachment (ULA) plates, a common scaffold-free method.
Table 2: Reagent Solutions for 3D Spheroid Culture
| Reagent/Material | Function | Aseptic Handling Consideration |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Hydrophilic polymer coating inhibits cell adhesion, forcing cell-cell aggregation into spheroids [47]. | Remove from sterile packaging just before use. Limit exposure to air by replacing lid when not seeding. |
| Basement Membrane Extract (BME) | Provides a scaffold for organoid growth or invasion assays; mimics the extracellular matrix [50] [48]. | Thaw on ice overnight in 4°C fridge; pre-chill tips and tubes to prevent premature polymerization. |
| Cell Dissociation Reagent (e.g., Accutase) | A milder enzyme mixture than trypsin for creating single-cell suspensions while preserving cell surface proteins [52]. | Wipe outside of bottle with 70% ethanol before placing in BSC. Aliquot to avoid contaminating stock. |
| Specialized Growth Media | Rich media often containing growth factors (e.g., EGF, FGF-2) and supplements (e.g., B-27, N-acetylcysteine) [50]. | Filter-sterilize all in-house prepared media. Wipe bottle exteriors with ethanol before use. |
Step-by-Step Procedure:
- Cell Preparation: Harvest cells using a mild dissociation reagent like Accutase to create a single-cell suspension. Count cells and assess viability using Trypan Blue exclusion; do not proceed if viability is below 90% [48].
- Seeding in ULA Plates: Resuspend the cell pellet in the appropriate culture medium at the desired density (e.g., 2,000-5,000 cells per well for a 96-well format). Using a sterile pipette, carefully dispense the cell suspension into each well of the ULA plate.
- Spheroid Formation: Place the ULA plate in a 37°C, 5% CO₂ incubator for 48-72 hours to promote spheroid formation. Minimize movement and disturbance of the plate during this critical aggregation period.
- Aseptic Media Changes: This is a high-risk step. Use specialized 3D-tips (pipette tips with an integrated 40-μm mesh barrier) to remove spent media. The mesh acts as a barrier, preventing the aspiration of spheroids while allowing liquid to pass [49]. Gently add fresh, pre-warmed media to the wells. This method is superior to the 50/50 media exchange or centrifugation, which can lead to significant spheroid loss or damage.
The workflow for this protocol, including critical aseptic control points, is visualized below.
Protocol 2: Establishing Immune Cell-Organoid Co-cultures
This advanced protocol for establishing autologous co-cultures, as used in intestinal research, involves significant manipulation [50].
Step-by-Step Procedure:
Primary Cell Isolation:
- Tissue Processing: Process intestinal tissue samples in a BSC using sterile instruments. Thoroughly wash tissue segments in cold PBS containing antibiotics (e.g., Primocin) and antifungals if permitted by the experimental design.
- Epithelial Isolation: Isolate crypts or epithelial cells using chelating agents like EDTA and density centrifugation.
- Immune Cell Isolation: Process the lamina propria tissue by enzymatic digestion (e.g., with Collagenase/DNase I blends) to liberate immune cells, which can then be purified using density gradient centrifugation (e.g., Percoll).
Organoid Culture from Epithelium:
- Embed the isolated epithelial crypts/cells in a droplet of BME. Allow the BME to polymerize in an incubator for 15-30 minutes.
- Overlay with a specialized organoid growth medium containing essential factors like Wnt, R-Spondin-1, and Noggin [50]. Culture for 5-7 days, with media changes every 2-3 days using 3D-tips, until mature organoids form.
Aseptic Co-culture Assembly:
- Harvest the desired immune cell population (e.g., lamina propria lymphocytes, macrophages) and resuspend them in fresh organoid growth medium.
- Using 3D-tips, carefully remove the existing media from the organoid culture wells.
- Gently add the immune cell suspension directly over the BME dome containing the organoids.
- Return the co-culture to the incubator and monitor regularly. Refresh the co-culture medium every 2-3 days, taking care not to disturb the interacting cells.
Environmental Monitoring and Validation
Routine monitoring of the cell culture environment is essential for identifying and eradicating contamination sources before they compromise valuable 3D cultures.
- Active Air and Surface Sampling: Use sterile cotton swabs to sample critical areas—incubator shelves, water trays, BSC work surfaces, microscope stages—and streak onto blood agar plates. Incubate the plates for 48 hours to check for microbial growth [28]. This is particularly important for incubators, which have been identified as a major contamination source.
- Rigorous Decontamination Schedules: Beyond daily 70% ethanol cleaning, implement a weekly or bi-weekly deep-cleaning regimen for all equipment using a triple-cleaning strategy: 70% ethanol, followed by 1% sodium hypochlorite, and then a commercial disinfectant like 1% Virkon-S [28]. Incubators should undergo a specialized disinfection cycle, potentially using a mobile UV lamp or a manufacturer-provided disinfection kit that heats a chemical solution to 90°C for several hours.
Maintaining stringent asepsis in 3D spheroid and co-culture systems is a demanding but achievable standard. It requires an integrated approach that combines foundational aseptic practices with specialized techniques and tools designed for the unique vulnerabilities of these complex models. The protocols detailed herein, from the use of 3D-tips for media changes to rigorous environmental monitoring, provide a robust framework for researchers. Adherence to these guidelines is paramount for ensuring the reliability, reproducibility, and ultimate success of advanced in vitro studies in drug development and basic research, forming a critical methodological component for any thesis in the field of cell culture sciences.
Crisis Control: Identifying, Troubleshooting, and Preventing Contamination
Maintaining aseptic technique is fundamental to successful cell culture, yet biological contamination remains a common and serious challenge in research and drug development [14]. Early and accurate identification of contamination is critical to protect the integrity of experiments, ensure reproducible results, and conserve valuable resources. The most accessible and immediate methods for detecting contamination rely on visual cues and simple biochemical indicators observable during routine culture maintenance. This application note details the core visual signs of contamination—cloudy media, pH shifts, and unusual cellular morphology—providing researchers with structured protocols for monitoring, identifying, and responding to potential contaminants.
Key Visual and Biochemical Indicators of Contamination
Contamination manifests through distinct changes in the culture medium and the cells themselves. The table below summarizes the primary indicators for the most common contaminant types.
Table 1: Primary Indicators of Common Cell Culture Contaminants
| Contaminant Type | Visual Media Changes | pH Shift | Microscopic Appearance |
|---|---|---|---|
| Bacteria | Cloudy or turbid; thin film on surface may be present [14] [53] | Sudden, sharp drop (becomes acidic) [14] [54] | Tiny, shimmering granules between cells; rod (bacillus) or spherical (coccus) shapes may be resolved at high power [14] |
| Yeast | Turbid, especially in advanced stages [14] | Stable initially, then increases (becomes basic) with heavy contamination [14] | Individual ovoid or spherical particles that may bud off smaller particles [14] |
| Mold | Turbid; fuzzy, filamentous clumps may be visible to the naked eye [14] | Stable initially, then rapidly increases (becomes basic) [14] | Thin, wispy filaments (hyphae) forming a mycelial network [14] |
| Mycoplasma | No change; media remains clear [14] | No change | No visible signs; requires specialized detection methods (e.g., PCR, immunostaining) [14] |
The Role of pH as a Contamination Indicator
The pH of culture media is a critical process parameter, typically maintained between 7.0 and 7.4 for most mammalian cells [54]. Metabolic byproducts from contaminants can cause rapid pH shifts. Bacterial contamination often leads to acidification, turning phenol red indicator yellow, while fungal contamination can cause alkalinization, turning it pink [54]. It is important to note that pH changes can also result from normal cellular metabolism or improper CO₂ levels; therefore, pH should be considered alongside other signs like turbidity [54].
Experimental Protocols for Contamination Monitoring
Implementing systematic monitoring protocols is essential for early contamination detection.
Protocol 1: Daily Visual and Microscopic Inspection
Purpose: To identify early signs of contamination through routine observation. Materials: Inverted phase-contrast microscope, laboratory disinfectant (e.g., 70% ethanol), personal protective equipment (PPE). Procedure:
- Macroscopic Observation: With the naked eye, inspect the culture vessel for cloudiness or turbidity in the medium, which is a primary indicator of microbial growth [14] [53]. Note any unexpected color change in the phenol red indicator.
- Microscopic Examination:
- Place the culture vessel on the stage of an inverted microscope.
- First, observe at low magnification (e.g., 40x) to scan the entire field for signs of unusual movement (e.g., tiny, shimmering granules indicative of bacteria) or floating particles [14].
- Switch to higher magnification (e.g., 200x or 400x) to resolve the morphology of any suspected contaminants. Look for bacterial rods or cocci, budding yeast, or filamentous molds [14] [55].
- Documentation: Record all observations, including media clarity, pH (via color), and any unusual cellular or microbial structures.
Protocol 2: Monitoring Contamination Through Metabolic Changes
Purpose: To correlate pH shifts with potential contamination. Materials: Cell culture with pH indicator (e.g., phenol red), pH meter or test strips (optional for verification). Procedure:
- During media changes or daily inspection, note the color of the culture medium.
- Match the medium's color to the phenol red scale:
- A sudden, unexplained shift in pH, particularly when accompanied by other signs like turbidity, strongly suggests contamination and warrants further investigation [14] [53].
The following workflow diagram outlines the decision-making process for identifying and responding to suspected contamination.
Aseptic Technique and Contamination Prevention
Prevention is the most effective strategy for managing cell culture contamination. Adherence to strict aseptic technique is non-negotiable [4]. Key practices include:
- Personal Hygiene: Thoroughly wash hands and wear appropriate PPE, including a lab coat and gloves [4].
- Work Area Management: Perform all culture work in a certified laminar flow hood that is regularly disinfected with 70% ethanol. Keep the work surface uncluttered and avoid rapid movements that can disrupt the sterile airflow field [4].
- Sterile Handling: Flame the necks of bottles, use sterile disposable pipettes only once, and never leave culture vessels open to the environment. All reagents and media that come into contact with cells must be sterile [4].
- Quality Control: Regularly check cultures for contamination and obtain cell lines from reputable banks to avoid cross-contamination [14].
The Researcher's Toolkit: Essential Reagents for Contamination Control
Table 2: Key Reagents and Materials for Maintaining Aseptic Culture
| Item | Function/Application |
|---|---|
| 70% Ethanol | Broad-spectrum surface disinfectant for the laminar flow hood, instruments, and gloves [4]. |
| Phenol Red | pH indicator in culture media; color change provides an early warning of microbial metabolism [54]. |
| Antibiotics/Antimycotics | Used selectively to control or eliminate bacterial (e.g., penicillin/streptomycin) and fungal (e.g., amphotericin B) contaminants. Not recommended for long-term, continuous use [14]. |
| Sterile Disposable Pipettes | Pre-sterilized, single-use items to prevent cross-contamination between cultures and reagent bottles [4]. |
| Trypsin/EDTA | Enzyme solution used for passaging adherent cells; must be sterile-filtered to avoid introducing contaminants during subculturing. |
Vigilant monitoring for the visual cues of contamination—cloudy media, pH shifts, and unusual morphology—forms the first and most critical line of defense in cell culture management. By integrating the structured protocols and preventive measures outlined in this application note into daily practice, researchers and drug development professionals can significantly mitigate the risks associated with contamination, thereby safeguarding the validity of their experimental data and the efficiency of their research operations.
Contamination represents one of the most frequent and serious challenges in cell culture laboratories, compromising experimental data, jeopardizing product safety in biopharmaceutical development, and wasting valuable resources [14] [52]. This guide provides a structured approach to identifying and tracing the most common biological contaminants—bacteria, fungi, and mycoplasma—within the broader context of aseptic technique research. For researchers and drug development professionals, prompt and accurate contamination investigation is essential for maintaining culture integrity and ensuring the reproducibility of results [8]. The following sections detail the characteristic profiles of each contaminant and provide systematic protocols for source identification and eradication.
Bacterial Contamination
Identification and Characteristics
Bacterial contamination is prevalent due to the ubiquity and rapid growth of microorganisms [14]. Recognition begins with macroscopic and microscopic observation.
- Visual/Macroscopic Signs: The most common indicator is a sudden change in medium turbidity. The culture medium appears cloudy, sometimes with a thin film on the surface [14] [13]. A rapid drop in pH, often indicated by a yellow color shift in phenol red-containing media, is also frequently observed [13] [56].
- Microscopic Signs: Under low-power microscopy, bacteria appear as tiny, shimmering granules between cultured cells. Higher magnification can resolve individual shapes (e.g., spheres, rods) [14].
- Other Signs: Cultures may develop a sour or unpleasant odor [13].
Table 1: Characteristics of Bacterial Contamination
| Characteristic | Description |
|---|---|
| Medium Appearance | Cloudy, turbid [14] [56] |
| pH Shift | Rapid drop to acidic (yellow with phenol red) [13] [56] |
| Microscopic View | Tiny (1-5 µm), motile granules; shapes vary (cocci, bacilli) [14] [13] |
| Common Sources | Improper aseptic technique, contaminated reagents, unclean surfaces [13] |
Tracing the Source
A systematic approach is required to trace the origin of bacterial contamination.
Figure 1: Workflow for tracing the source of bacterial contamination.
The investigative protocol involves:
- Culture Isolation: Immediately move the contaminated culture to an isolated quarantine area to prevent cross-contamination [8].
- Process Review:
- Aseptic Technique: Audit handling procedures. Common failures include inadequate glove disinfection, working outside a certified biosafety cabinet, or incorrect use of pipettes [13] [57].
- Reagent Testing: Test all recently used reagents, including media, serum, and supplements, by incubating small aliquots separately under culture conditions and monitoring for turbidity [13].
- Environmental Monitoring:
- Gram Staining Protocol: To further characterize the contaminant [56]:
- Prepare a smear of the culture medium on a microscope slide and heat-fix.
- Flood the smear with crystal violet solution for 60 seconds, then rinse gently with water.
- Apply Gram's iodine solution for 60 seconds, then rinse.
- Decolorize with ethyl alcohol or acetone for ~5-15 seconds, then rinse immediately.
- Counterstain with safranin solution for 60 seconds, then rinse and blot dry.
- Observe under oil immersion. Gram-positive bacteria appear purple, while Gram-negative bacteria appear pink/red. This result can help narrow down potential environmental sources.
Fungal Contamination
Identification and Characteristics
Fungal contaminants, including molds and yeasts, are ubiquitous airborne threats [58].
- Yeast Contamination: Appears as individual ovoid or spherical particles that may bud off smaller particles. In advanced stages, the medium becomes turbid with little initial pH change, though the pH may later increase [14].
- Mold Contamination: Presents as multicellular, thin, wispy filaments (hyphae) under microscopy, potentially forming denser clumps of spores. Like yeast, the pH is stable initially but increases with heavy contamination [14] [58].
Table 2: Characteristics of Fungal Contamination
| Characteristic | Yeast | Mold |
|---|---|---|
| Medium Appearance | Turbid in advanced stages [14] | Turbid; visible fuzzy patches (white, green, black) [58] [13] |
| pH Shift | Stable initially, then increases (pink with phenol red) [14] [56] | Stable initially, then increases [14] [58] |
| Microscopic View | Ovoid/spherical budding particles (~10 µm) [14] [13] | Filamentous mycelia (hyphae) [14] [58] |
| Common Sources | Airborne spores, contaminated incubator water trays, seasonal air changes [58] [13] | Airborne spores, humid environments, contaminated air-handling systems [58] [13] |
Tracing the Source
Fungal spores are resilient and can be introduced via multiple pathways.
Figure 2: Workflow for tracing the source of fungal contamination.
The investigative protocol involves:
- Airborne Source Investigation:
- Seasonal Factors: Be aware that contamination rates often increase in spring and fall when building heating/air-conditioning systems are switched, disturbing spores [58].
- Lab Environment: Check for recent construction, open windows, or high traffic near the culture area. Verify the biosafety cabinet's HEPA filters and integrity [13].
- Incubator and Humidity Source Check:
- Reagent and Supply Check: Inspect water baths for microbial growth and test media and supplements as described for bacterial contamination.
Mycoplasma Contamination
Identification and Characteristics
Mycoplasma is a particularly insidious contaminant because it is not visible under standard microscopy and does not cause medium turbidity [59] [13]. Its effects are often subtle and can persist undetected for long periods.
- Visual/Macroscopic Signs: No visible change in the medium; no turbidity or consistent pH shift [60] [13].
- Cellular Effects: Unexplained changes in cell growth rate, morphology, or metabolism; reduced transfection efficiency; and altered gene expression [59] [13].
- Detection Methods: Requires specialized tests, including PCR, fluorescence staining (e.g., Hoechst 33258), ELISA, or microbial culture on selective media [59] [60] [56].
Table 3: Mycoplasma Detection Methods
| Method | Principle | Duration | Sensitivity & Notes |
|---|---|---|---|
| PCR | Amplifies mycoplasma-specific DNA sequences (e.g., 16S rRNA) [59] [56] | Several hours [59] | High sensitivity; can detect non-viable mycoplasma; risk of false positives from contamination [59] |
| Fluorescence Staining (Hoechst) | DNA-binding dye stains mycoplasma DNA on indicator cells [60] [56] | 1-2 days [59] | Detects viable mycoplasma; reveals filamentous DNA on cell surface; requires fluorescence microscope [59] |
| Microbial Culture | Grows mycoplasma on specialized agar (e.g., Frey, Friis media) [59] [60] | 2-4 weeks [59] | Considered the "gold standard"; slow but highly specific; cannot detect all species (e.g., M. hyorhinis) [59] |
| Enzyme Assays (ELISA) | Detects mycoplasma-specific enzymes or antigens [59] | ~30 minutes [59] | Lower sensitivity; less commonly used [59] |
Tracing the Source
Mycoplasma contamination typically originates from introduced materials or personnel.
Figure 3: Workflow for tracing the source of mycoplasma contamination.
The investigative protocol involves:
- Confirm and Quarantine: Use a reliable method (e.g., PCR) to confirm mycoplasma presence. Immediately quarantine all positive cultures and any cultures handled in parallel [8] [13].
- Material and Reagent Audit:
- Cell Lines: Focus on recently introduced cell lines. Mycoplasma is most commonly spread from one contaminated culture to another via aerosol droplets during pipetting [60] [13]. Test all frozen master and working cell banks.
- Biological Reagents: Audit the source of fetal bovine serum (FBS) and other supplements, as these can be a source of introduction. Use only certified, mycoplasma-free reagents [13].
- Personnel and Technique Audit:
- Some mycoplasma species are part of human skin flora and can be introduced through poor aseptic technique [60]. Review and reinforce training on proper gowning and handling procedures.
- Protocol for Hoechst Staining:
- Seed indicator cells (e.g., Vero cells) in a culture dish with a coverslip and incubate until 50-60% confluent.
- Inoculate the test sample onto the indicator cells and culture for 3-5 days.
- Fix the cells with a fresh Carnoy's fixative (methanol:glacial acetic acid, 3:1) for 10 minutes.
- Stain with Hoechst 33258 dye (e.g., 0.05-0.1 µg/mL in PBS) for 30 minutes in the dark.
- Rinse with water and mount the coverslip on a slide.
- Examine under a fluorescence microscope. Mycoplasma contamination appears as bright, punctate or filamentous fluorescence on the cell surface or in intercellular spaces, while clean cells show fluorescence only in the nucleus [59] [56].
The Scientist's Toolkit: Key Reagent Solutions
The following reagents and tools are essential for effective contamination prevention, detection, and management.
Table 4: Essential Reagents for Contamination Control
| Reagent/Tool | Function | Example Applications |
|---|---|---|
| Antibiotics & Antimycotics | Suppress or eliminate microbial growth. Use sparingly for short-term rescue, not routine prevention [14] [13]. | Amphotericin B (antifungal) [58], Plasmocin (anti-mycoplasma) [13]. |
| PCR Kits | Detect microbial DNA with high sensitivity. Essential for mycoplasma and viral screening [59] [56]. | Routine mycoplasma screening of cell stocks and cultures [13]. |
| Hoechst 33258/33342 | Fluorescent DNA-binding dyes used to stain and visualize mycoplasma DNA adherent to infected cells [60] [56]. | Staining protocol for mycoplasma detection as described in Section 4.2. |
| Selective Culture Media | Support the growth of specific microbes for isolation and identification. | Frey's and Friis media for mycoplasma culture per pharmacopoeia guidelines [60]. |
| Gram Stain Kit | Differentiates bacteria into Gram-positive and Gram-negative based on cell wall properties [56]. | Preliminary characterization of bacterial contaminants. |
| Certified Sera & Reagents | Reduce risk of introducing contaminants from external sources. | Use of mycoplasma-free, virus-screened FBS [13] [57]. |
A proactive and systematic approach is the cornerstone of effective contamination control. Key prevention strategies include:
- Strict Aseptic Technique: This is the single most important factor. Always work within a properly maintained and certified biosafety cabinet using disciplined practices [14] [57].
- Routine Quality Control: Implement a schedule for regular mycoplasma testing (e.g., every 1-2 months) and cell line authentication [59] [13].
- Judicious Antibiotic Use: Avoid the continuous use of antibiotics in routine culture, as this can mask low-level contamination and promote resistant strains [14] [13].
- Environmental Control: Maintain clean and monitored workspaces and equipment. Perform regular decontamination of incubators, water baths, and biosafety cabinets [8] [13].
- Quarantine Protocol: Always quarantine and test all new cell lines and biological reagents before integrating them into your main laboratory workflow [13] [57].
By integrating the troubleshooting methodologies and preventive protocols outlined in this guide, researchers and drug development professionals can significantly mitigate the risks associated with cell culture contamination, thereby safeguarding the integrity of their scientific and production outcomes.
Decontamination and Disposal Protocols for Contaminated Cultures
Biological contamination is a pervasive and critical challenge in cell culture laboratories, capable of compromising experimental integrity and leading to significant losses of time and resources. Contaminants encompass a wide range of biological entities, including bacteria, fungi, yeasts, viruses, and mycoplasma [61]. The morphology of the specific cells under study and the potential contaminants they've been exposed to must be understood to enable accurate identification [61]. Some biological contaminants, particularly mycoplasma, present a severe challenge due to their small size and resistance to most routine antibiotics, often requiring specialized detection methods beyond simple visual inspection [62] [61].
The consequences of contamination extend beyond lost experiments. Contaminated cultures can produce irreproducible data, potentially invalidating research findings and contaminating the scientific literature [63]. Furthermore, certain contaminants, especially viruses in human or primate cells, can pose serious health hazards to laboratory personnel [61]. Thus, establishing and adhering to robust decontamination and disposal protocols is not merely a matter of experimental convenience but a fundamental requirement for research validity and laboratory safety. This document outlines standardized procedures within the broader context of a thesis on aseptic technique, providing researchers with clear protocols for managing contamination events.
Identification and Classification of Contaminants
The first step in addressing contamination is accurate identification, which dictates the subsequent decontamination and disposal strategy. Different contaminants exhibit distinct visual and morphological characteristics.
Table 1: Identification of Common Biological Contaminants in Cell Culture
| Contaminant Type | Visual/Macroscopic Signs | Microscopic Appearance | Other Indicators |
|---|---|---|---|
| Bacteria | Culture medium appears turbid (cloudy); sometimes with a thin surface film [61]. | Tiny, moving granules between cells; individual shapes (rods, spheres) resolvable under high power [61]. | Sudden, rapid drop in the pH of the culture medium (yellowing) [61]. |
| Yeast | Culture medium becomes turbid, particularly in advanced stages [61]. | Individual ovoid or spherical particles; may be observed budding off smaller particles [61]. | Little initial pH change; pH usually increases when contamination becomes heavy [61]. |
| Mold | Turbid culture; may appear as floating, filamentous clumps [61]. | Thin, wisp-like filaments (hyphae); denser clumps of spores [61]. | Stable pH in initial stages, rapidly increasing with heavy growth [61]. |
| Mycoplasma | No obvious visual change to the culture medium; cultures may show altered growth patterns or viability over time [62] [61]. | Not detectable by routine microscopy [62]. | Requires specialized tests: PCR, ELISA, immunostaining, or electron microscopy [62] [61]. |
Beyond biological contaminants, cross-contamination by other cell lines represents a significant, though less visible, problem. Extensive cross-contamination with fast-growing cell lines like HeLa is a well-established issue with serious consequences for data integrity [61]. Cell line authentication through methods such as DNA fingerprinting, karyotype analysis, and isotype analysis is essential to confirm the absence of cross-contamination [61].
Decontamination Protocols
When a contamination event occurs, the immediate priority is to prevent its spread. The affected culture should be isolated from other cell lines immediately [61]. All subsequent work must be performed within a biosafety cabinet following strict aseptic technique. Following the initial response, a decision must be made on whether to attempt decontamination of an irreplaceable culture or to proceed directly to disposal.
Decision Workflow for Contamination Events
The following diagram outlines the critical decision-making process upon suspecting contamination.
Chemical Decontamination of Cultures
For irreplaceable cultures, a targeted decontamination procedure using antibiotics or antimycotics can be attempted. It is critical to note that these chemicals can be toxic to the cells, so a dose-response test is mandatory [61].
Table 2: Guide to Reagents for Decontamination
| Research Reagent Solution | Function / Target | Key Considerations |
|---|---|---|
| Antibiotics (e.g., Penicillin-Streptomycin) | Inhibit bacterial growth by targeting cell wall synthesis or protein production [61]. | High concentrations can be toxic to cells; can lead to antibiotic-resistant strains; may mask low-level mycoplasma infections [61]. |
| Antimycotics (e.g., Amphotericin B) | Inhibit fungal and yeast growth by disrupting cell membrane integrity [61]. | Similar toxicity concerns as antibiotics; optimal concentration must be determined empirically [61]. |
| 70% Ethanol (EtOH) | Denatures proteins and dissolves lipids in contaminating organisms; used for surface and item decontamination [4] [62]. | Concentration is critical; 70% is most effective for penetration. Water is required for the protein denaturation process [62]. |
| EPA-registered Hospital Disinfectant | General surface decontamination; some are tuberculocidal and effective against a broad spectrum of pathogens [64]. | Follow manufacturer's instructions for dilution, contact time, and safe use. Contact time is often at least 1 minute [64]. |
| Sodium Hypochlorite (Bleach) Solution | Strong oxidizing agent used for decontaminating spills of blood or other potentially infectious materials [64]. | For surface decontamination of small spills (<10 mL), use a 1:100 dilution (525-615 ppm available chlorine) [64]. |
Experimental Protocol for Decontamination with Antibiotics/Antimycotics:
- Determine Toxicity: Dissociate, count, and dilute the contaminated cells in antibiotic-free medium. Dispense the cell suspension into a multi-well plate. Add the chosen antibiotic or antimycotic to the wells across a range of concentrations. Observe the cells daily for signs of toxicity (e.g., sloughing, vacuole appearance, decrease in confluency, rounding) for several days to establish the toxic threshold [61].
- Treat Cultures: Culture the cells for two to three passages using the antibiotic at a concentration one- to two-fold lower than the determined toxic concentration [61].
- Monitor Efficacy: Culture the cells for one passage in antibiotic-free media. Then, repeat the treatment (step 2) to target any residual, dormant contaminants [61].
- Verify Eradication: Finally, culture the cells in antibiotic-free medium for 4 to 6 passages. Monitor closely via microscopy and other relevant tests (e.g., PCR for mycoplasma) to confirm the contamination has been eliminated [61].
Physical Decontamination Methods
Physical methods are the cornerstone of sterilizing equipment, liquids, and surfaces.
- Moist Heat (Autoclaving): An autoclave uses steam under pressure (typically 121-132°C for at least 20 minutes) to achieve sterilization, which is the complete destruction of all life forms, including bacterial spores [65]. This method is required for all media and surgical instruments that enter sterile tissue [64] and is the primary method for decontaminating liquid waste and labware prior to disposal.
- Surface Disinfection: The work surface of a biosafety cabinet and other equipment must be decontaminated before and after work, especially after any spillage. 70% ethanol is routinely used for this purpose [4] [62]. For more robust decontamination, especially following spills of potentially infectious materials, an EPA-registered tuberculocidal disinfectant or a diluted sodium hypochlorite solution is recommended [64].
- Ultraviolet (UV) Light: UV light can be used to sterilize the air and exposed work surfaces within a biosafety cabinet between uses. It is a secondary environmental control that helps reduce airborne contaminants [4].
Disposal Protocols
Proper disposal is the final, critical step in managing contaminated materials. All materials that have come into contact with microorganisms are considered infectious waste and must be decontaminated prior to disposal [35] [65].
- Liquid Waste: Contaminated culture media and liquid solutions should be inactivated by adding a chemical disinfectant (e.g., bleach at a final concentration of at least 1% sodium hypochlorite) and allowing sufficient contact time (e.g., 30 minutes). The inactivated liquid can then be disposed of via the sink, followed by flushing with copious amounts of water. Alternatively, liquids can be collected in a sealed container and sterilized by autoclaving before disposal [64] [65].
- Solid Waste: Contaminated solid materials, such as plastic pipettes, tips, culture vessels, and gloves, must be placed in a dedicated, autoclavable biohazard bag. The bag must be securely closed and then subjected to steam sterilization by autoclaving. Once decontaminated, the solid waste can be disposed of as regular non-hazardous waste, in compliance with local regulations [4] [35].
- Sharp Objects: Contaminated sharps (e.g., needles, scalpels, broken glass) must be placed in a puncture-resistant, leak-proof sharps container [4]. The entire closed container is typically treated by incineration or autoclaving before final disposal, following institutional and federal regulations [4] [64].
Note: Always consult and adhere to your institution's specific Environmental Health and Safety (EHS) policies and local regulations, as they may have additional requirements or approved variations to these general protocols [4] [35].
In cell culture research, the integrity of experimental data is profoundly influenced by the quality of reagents and the reliability of laboratory equipment. Aseptic technique extends beyond the immediate handling of cell lines; it encompasses the entire workflow, from how reagents are prepared and stored to how essential equipment is maintained. Contamination or variable reagent performance introduced during aliquoting can compromise months of research, leading to unreliable results and wasted resources [66]. Similarly, improper equipment maintenance creates unforeseen variables that threaten experimental reproducibility. This application note provides detailed protocols and best practices for the aliquoting of common reagents and the preventive maintenance of key equipment, framing these tasks as critical, non-negotiable components of a robust aseptic technique protocol within a cell culture laboratory.
The Critical Role of Aliquoting in Aseptic Technique
Aliquoting—the process of dividing a bulk reagent into smaller, single-use volumes—is a fundamental practice for preserving reagent quality and ensuring experimental consistency. The core benefits are:
- Minimizing Contamination Risk: Repeatedly opening a primary reagent stock bottle introduces multiple opportunities for microbial contamination (bacteria, fungi, viruses) each time [66]. Using single-use aliquots confines this risk to a single event.
- Preserving Reagent Integrity: Many reagents, particularly complex biologicals like fetal bovine serum (FBS), contain heat-labile proteins and growth factors that are degraded by repeated freeze-thaw cycles [66]. Aliquoting prevents this degradation.
- Ensuring Consistency: Proper aliquoting, coupled with gentle mixing of the primary stock before division, helps ensure that each experiment is conducted with a reagent of identical composition, thereby enhancing data reproducibility [66].
- Improving Inventory Management: Smaller, labeled aliquots facilitate a first-in-first-out (FIFO) system, preventing the use of expired reagents and simplifying stock management [66].
Risks of Improper Aliquoting
Failure to adhere to proper aliquoting techniques introduces several hidden risks:
- Introduction of Microbial Contaminants: This is the most direct risk, potentially leading to the loss of cell cultures and invalidated experimental data [66].
- Degradation of Growth Factors: Repeated freezing and thawing can diminish the activity of essential components in serum and other complex media, leading to altered cell growth and behavior [66].
- Uneven Distribution of Components: Without thorough mixing before aliquoting, gravitational settling can cause nutrient gradients within a bottle, leading to inconsistent performance across aliquots from the same stock [66].
Detailed Protocol: Aseptic Aliquoting of Reagents
This protocol uses FBS as a model reagent but is adaptable to other sensitive liquid reagents such as antibiotics, growth factors, and enzymes.
Pre-Procedure Preparation: The Scientist's Toolkit
Table 1: Essential Materials for Aseptic Aliquoting
| Item | Function |
|---|---|
| Personal Protective Equipment (PPE) | Lab coat, gloves, and safety goggles are mandatory to protect the user and prevent shedding of skin and hair into the workspace [4] [66]. |
| Laminar Flow Hood (Biosafety Cabinet) | Provides a sterile work environment with HEPA-filtered air, protecting the reagent from airborne contaminants [2] [67]. |
| 70% Ethanol Spray/Wipes | The primary disinfectant for all surfaces, equipment, and gloved hands within the work area [4] [2]. |
| Sterile Aliquot Tubes (e.g., 50 ml Conical Tubes) | Pre-sterilized, sealable containers for storing individual aliquots. The size should be chosen based on typical usage to avoid freeze-thaw cycles [66]. |
| Sterile Pipettes and Pipettor | For the accurate and sterile transfer of liquid from the stock bottle to the aliquot tubes [4]. |
| Permanent, Ethanol-Resistant Marker | For clear labeling of aliquots with critical information. Smudge-proof labels are recommended [66]. |
| Cryoprotective Agent (e.g., DMSO) | For protecting cells during freezing, though not typically needed for FBS itself [68]. |
| Cooled Storage Container (-20°C or -80°C Freezer) | For long-term storage of aliquots at a consistent temperature [66]. |
Step-by-Step Workflow
1. Workspace and Material Preparation
- Turn on the laminar flow hood and allow it to run for at least 15-30 minutes to purge contaminants from the work surface [2] [66].
- Thoroughly wipe down all interior surfaces of the hood—the work surface, side walls, and back panel—with 70% ethanol [2] [11].
- Gather all necessary materials listed in Table 1 and place them strategically within the hood. Wipe the outside of all containers, including the stock FBS bottle and boxes of sterile tubes, with 70% ethanol before introducing them [4] [66].
- Wear appropriate PPE and wipe gloved hands with 70% ethanol [4].
2. Reagent Preparation and Mixing
- If the stock FBS is frozen, thaw it completely under controlled conditions (e.g., in a refrigerator or cool water bath). Do not thaw at room temperature or at 37°C, as this can accelerate degradation.
- Once fully thawed, gently but thoroughly mix the bottle by inverting it several times. This is a critical step to ensure a homogeneous suspension and even distribution of precipitates and growth factors across all aliquots [66]. Avoid vortexing or vigorous shaking, which can cause foaming and denature proteins.
3. Aseptic Transfer
- Working within the laminar flow hood, use a sterile pipette to transfer the desired volume from the stock bottle into each pre-labeled sterile tube.
- Maintain sterility: Work deliberately but not hastily. Keep the stock bottle open for the minimum time necessary. Avoid touching the sterile pipette tip to any non-sterile surface, including the threads of the stock bottle [4]. If using a glass pipette, flame the neck of the stock bottle before and after pipetting to create a sterile convection current [2].
- Cap each aliquot tube immediately after filling.
4. Labeling and Storage
- Label every tube clearly with a permanent marker. Essential information includes: Reagent identity (e.g., "FBS"), Batch/Lot number, Date of aliquoting, Initials of the researcher [66].
- Promptly transfer the aliquots to the appropriate storage freezer (-20°C for short-term, -80°C for long-term). Ensure the freezer maintains a stable temperature with minimal fluctuation [66].
- Implement a first-in-first-out (FIFO) inventory system by placing new aliquots behind older ones [66].
The following workflow diagram summarizes the key stages of this protocol:
Equipment Maintenance for Optimal Performance
Regular and systematic maintenance of core cell culture equipment is essential for sustaining a contamination-free environment and ensuring stable cell growth conditions.
Table 2: Equipment Maintenance Schedule and Protocol
| Equipment | Maintenance Task | Frequency | Protocol & Purpose |
|---|---|---|---|
| Laminar Flow Hood / Biosafety Cabinet (BSC) | Surface Decontamination | Before and after every use [4] [2]. | Wipe all interior surfaces with 70% ethanol. Removes contaminants introduced during work. |
| HEPA Filter Integrity Testing | Certified annually by a professional [2]. | Ensures the filter is intact and providing a sterile airflow to the work surface. | |
| UV Light Decontamination | Used between sessions (e.g., overnight) in some labs [4] [69]. | Sterilizes exposed surfaces and air. Note: UV light is not a substitute for chemical disinfection and should not be used while the cabinet is occupied [4]. | |
| Incubator | Routine Cleaning & Decontamination | Weekly to monthly, according to manufacturer's protocol [4] [69]. | Remove shelves and accessories; clean all surfaces with a mild detergent followed by 70% ethanol or a laboratory disinfectant. Prevents fungal and bacterial growth in a warm, humid environment. |
| Water Tray Refilling & Cleaning | For humidity-controlled incubators: use sterile, distilled water only. Clean and refill weekly to prevent microbial blooms [4] [68]. | Maintains humidity and prevents contamination from the water source. | |
| Microscopes & Centrifuges | Surface Decontamination | After every use [4] [68]. | Wipe eyepieces, stage, and outer surfaces with 70% ethanol. Prevents cross-contamination when moving between the hood and equipment. |
| Autoclave | Performance Verification | Regularly, using biological indicators (e.g., spore tests) [69]. | Confirms that the autoclave reaches the required temperature and pressure (e.g., 121°C, 15 psi) for a sufficient time to achieve sterility [69]. |
| Water Bath | Cleaning and Treatment | Weekly; use only with clean, distilled water [68]. | Empty, clean, and refill the bath. Consider adding a laboratory biocide to the water to inhibit microbial growth. |
Optimizing your cell culture workflow requires a holistic view of aseptic technique that integrates meticulous reagent management with disciplined equipment care. The protocols outlined herein for aliquoting and maintenance are not peripheral tasks but are foundational to research integrity. By systematically minimizing contamination risks and ensuring reagent and equipment consistency, researchers can safeguard their valuable cell cultures, enhance the reproducibility of their experiments, and generate more reliable and impactful scientific data.
The evolution of cell culture aseptic technique protocols represents a critical frontier in biomedical research and pharmaceutical development. Within the context of advanced Good Manufacturing Practice (GMP) manufacturing and high-throughput laboratories, traditional aseptic methods are being transformed by technological innovation and systematic quality management. Current Good Manufacturing Practices (cGMP) emphasize the "current" nature of these standards, requiring manufacturers to employ up-to-date technologies and systems to prevent contamination, mix-ups, and errors [70] [71]. This progression is particularly vital for Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies, which cannot undergo terminal sterilization and are highly sensitive to cryopreservation and transportation variables [72].
The transition from centralized to decentralized point-of-care (POC) manufacturing models addresses several limitations inherent in traditional production frameworks. By enabling on-site manufacturing within or near clinical settings, POC approaches minimize transportation risks, reduce time-to-treatment, and allow administration of fresh, non-cryopreserved products [72]. However, hospitals and clinics present inherent contamination risks due to their high microbial burden, necessitating rigorous aseptic processing and comprehensive quality control [72]. This application note explores advanced strategies and protocols that bridge the gap between foundational aseptic techniques and the demanding requirements of modern GMP manufacturing and high-throughput research environments.
Advanced GMP Manufacturing Strategies
Isolator-Based Systems for Point-of-Care Manufacturing
Isolator-based systems have emerged as transformative technologies for decentralized manufacturing of cell-based therapies and extracellular vesicles (EVs). These systems provide modular, sterile, automation-compatible environments that support both autologous and selected allogeneic product manufacturing at clinical sites [72]. Unlike biological safety cabinets (BSCs) or restricted access barrier systems (RABS), isolators are completely closed systems that maintain asepsis independent of the surrounding environment, featuring integral glove ports, rapid transfer ports, and integrated decontamination units such as vaporized hydrogen peroxide (VHP) cycles [72].
The fundamental advantage of isolator technology lies in its ability to enable entire workflows—from tissue acquisition and cell processing to final formulation and reinfusion—within a controlled, closed environment at or near the patient's bedside [72]. This integrated approach significantly reduces supply chain complexity while enhancing sterility assurance and preserving the biological integrity of sensitive ATMPs. Configurations include positive pressure isolators for handling sterile products to protect them from external contamination and negative pressure isolators for handling hazardous substances to protect operators [72].
Table 1: Key Components of Isolator-Based POC Manufacturing Systems
| Component | Function | GMP Consideration |
|---|---|---|
| Positive Pressure Enclosure | Maintains sterile environment by preventing ingress of contaminants | Requires continuous pressure monitoring and alarm systems |
| Rapid Transfer Ports (RTPs) | Enable sterile transfer of materials without breaching isolation | Validation of transfer cycles and integrity testing |
| Integrated Decontamination | Vaporized Hydrogen Peroxide (VHP) or sporicidal cycles | Validation of biological indicators and residue testing |
| Glove Port Systems | Allow operator manipulation while maintaining barrier | Regular integrity testing and scheduled replacement |
| HEPA Filtration Modules | Provide ISO Class 5 environments within non-classified rooms | Periodic testing and certification per ISO 14644 standards |
Comprehensive cGMP Framework Implementation
Successful implementation of advanced manufacturing strategies requires adherence to the core principles of cGMP, which serve as the regulatory foundation for pharmaceutical quality. The FDA defines cGMP as systems that "assure proper design, monitoring, and control of manufacturing processes and facilities" [70]. These regulations provide for flexible implementation, allowing manufacturers to utilize modern technologies and innovative approaches to achieve higher quality through continual improvement [70] [71].
The cGMP framework encompasses several interconnected systems, often conceptualized as the "5 P's": People, Processes, Procedures, Premises, and Products [73]. Quality Management Systems must oversee all manufacturing operations, establishing strong quality management, obtaining appropriate quality raw materials, establishing robust operating procedures, detecting and investigating product quality deviations, and maintaining reliable testing laboratories [70] [74]. This systematic approach ensures that quality is built into the design and manufacturing process at every step, rather than relying solely on end-product testing [70].
High-Throughput Laboratory Applications
Contamination Control in Scale-Up Environments
High-throughput laboratories face amplified contamination risks due to increased manipulation frequency, shared equipment usage, and complex experimental workflows. The most prevalent contamination challenges include microbial contamination (bacteria, fungi, yeast), viral contamination, mycoplasma contamination, cross-contamination between cell lines, and chemical contamination [8]. Each presents distinct detection challenges and requires specialized prevention strategies.
In GMP manufacturing environments, contamination control extends beyond traditional aseptic technique to encompass comprehensive environmental monitoring, validated sterilization processes, and rigorous personnel training. Closed and single-use systems (SUS) have emerged as particularly valuable for reducing contamination risks from reusable culture vessels and eliminating complex cleaning validation requirements [8]. These systems, when integrated with automated monitoring technologies, provide robust contamination prevention while supporting scalable production needs.
Automated Processing and Digital Integration
The integration of automation and digital technologies represents a paradigm shift in high-throughput cell culture operations. Software solutions play a multifaceted role in enabling cGMP compliance through electronic batch records, digital work instructions, equipment monitoring, and automated data collection [71]. These systems enhance data integrity and traceability in accordance with FDA 21 CFR Part 11 requirements while reducing human error associated with manual documentation [71].
The Pharma 4.0 era has seen the industry embrace digital solutions that enable significant advances across the production process, resulting in substantial improvements to overall product quality and production efficiency [71]. Interactive digital training guides workers through processes more effectively than paper-based instructions, while media-rich standard operating procedures (SOPs) provide clearer operational guidance and troubleshooting support [71]. These technologies are particularly valuable in high-throughput environments where procedural consistency and documentation accuracy are paramount.
Detailed Experimental Protocols
Protocol: Comprehensive Aseptic Technique for GMP Compliance
This protocol establishes standardized procedures for maintaining aseptic conditions during cell culture operations in GMP and high-throughput environments, integrating traditional techniques with advanced technological safeguards.
Materials and Equipment:
- Class II Biological Safety Cabinet (recently certified)
- Pre-sterilized disposable pipettes and culture vessels
- 70% ethanol or isopropanol in spray bottles and wipes
- Personal protective equipment (sterile gloves, lab coat, hair cover)
- Automated cell culture system (if available)
- Environmental monitoring equipment (particle counters, active air samplers)
Procedure:
- Personal Hygiene and Garbing
- Remove jewelry and wash hands thoroughly with bactericidal soap
- Don appropriate PPE following documented gowning procedures
- Inspect gloves for integrity before entering manufacturing area
Workspace Preparation
- Activate biosafety cabinet and allow to run for minimum 15 minutes
- Wipe all surfaces with sporicidal agent followed by 70% ethanol
- Arrange materials to maximize workflow efficiency without clustering
- Implement UV irradiation if available (as supplementary measure only)
Material Introduction and Handling
- Wipe all container surfaces with 70% ethanol before introducing to workspace
- Minimize exposure of sterile materials to non-sterile environments
- Avoid simultaneous handling of non-sterile and sterile items
- Use single-use, pre-sterilized materials whenever possible
Aseptic Manipulation
- Work deliberately and methodically, avoiding rapid movements
- Maintain unobstructed airflow between HEPA filter and work surface
- Never leave containers open when not in active use
- Discard any equipment suspected of contamination immediately
Post-Procedure Activities
- Remove all materials from workspace and disinfect surfaces
- Document all activities and any deviations in batch records
- Perform environmental monitoring as required by quality system
Quality Control Considerations:
- Regular personnel training and competency assessment
- Media fills to validate aseptic processing capabilities
- Environmental monitoring with established alert and action limits
- Investigation of all deviations with corrective and preventive actions
Protocol: Mycoplasma Detection and Prevention in High-Throughput Settings
Mycoplasma contamination represents a particular challenge in high-throughput environments due to its cryptic nature and potential to compromise experimental results and production batches. This protocol outlines comprehensive detection and prevention strategies.
Materials and Equipment:
- Mycoplasma detection kit (PCR-based preferred for sensitivity)
- DNA extraction reagents and equipment
- Positive control DNA
- PCR thermal cycler and electrophoresis equipment
- Indicator cell lines (e.g., Vero cells)
- DAPI or Hoechst staining solutions
- Fluorescence microscope
Detection Procedure (Monthly Testing):
- Sample Collection
- Collect supernatant from test cultures 3-5 days post-passage
- Include positive and negative controls with each test run
- Process samples within 24 hours or store at -80°C
DNA Extraction and PCR Amplification
- Extract DNA according to manufacturer's instructions
- Set up PCR reactions with mycoplasma-specific primers
- Include appropriate controls (positive, negative, extraction blank)
- Perform amplification following validated thermal cycling parameters
Result Analysis and Documentation
- Analyze PCR products by gel electrophoresis
- Document results in cell culture maintenance records
- Investigate any positive results immediately
- Quarantine contaminated cultures until resolution
Prevention Strategies:
- Implement routine testing every 2-4 weeks for actively growing cultures
- Test all incoming cell lines before incorporation into workflow
- Use antibiotics specifically effective against mycoplasma cautiously
- Maintain segregated areas for quarantine and processing of new cell lines
- Employ single-use materials when possible to prevent cross-contamination
Quality Control and Validation Methodologies
Comprehensive QC Testing Framework
Robust quality control systems are fundamental to GMP compliance, requiring testing of raw materials, in-process samples, and finished products. The cGMP regulations mandate that manufacturers establish reliable testing laboratories with properly validated analytical methods [70] [74]. For cell-based products, this extends beyond conventional chemical testing to include identity testing, potency assays, purity assessments, and sterility testing.
The Quality by Design (QbD) approach encouraged by regulatory agencies emphasizes building quality into the manufacturing process rather than relying solely on finished product testing [73]. This involves defining a Quality Target Product Profile (QTPP) and using risk assessment to identify Critical Quality Attributes (CQAs) that must be monitored during production and at release [73]. Analytical methods must be developed and validated using a multivariate Design of Experiment (DoE) approach to adequately assess these CQAs.
Table 2: Essential Quality Control Tests for Cell-Based Therapies
| Test Category | Specific Assays | Acceptance Criteria | Frequency |
|---|---|---|---|
| Identity | STR profiling, Flow cytometry for specific markers | Match to donor or master cell bank | Each manufacturing run |
| Viability | Trypan blue exclusion, Flow cytometry with viability dyes | >70% (process-dependent) | Each processing step |
| Potency | Functional assays (e.g., cytokine secretion, cytotoxicity) | Meets predefined specification | Each product lot |
| Sterility | BacT/ALERT, Membrane filtration | No growth in 14 days | Each product lot |
| Mycoplasma | PCR, Culture method | Negative | Each product lot and master cell bank |
| Endotoxin | LAL test | <5 EU/kg/hr (product-dependent) | Each product lot |
Data Integrity and Documentation Practices
Comprehensive documentation represents a cornerstone of cGMP compliance, providing evidence that proper procedures were followed and quality standards were met [74]. Good Documentation Practices (GDP) require that all records are created, maintained, and archived to ensure accuracy, completeness, and compliance with regulatory standards [74] [75]. This includes standard operating procedures (SOPs), batch manufacturing records, laboratory records, equipment logs, and deviation reports.
In high-throughput environments, electronic systems have become indispensable for managing the volume and complexity of required documentation. These systems must comply with 21 CFR Part 11 requirements for electronic records and signatures, ensuring data integrity through features such as audit trails, access controls, and system validation [71] [73]. The ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) provide a framework for assessing data integrity across both paper-based and electronic systems [71].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Critical Reagents and Materials for Advanced Cell Culture Applications
| Reagent/Material | Function | GMP-Grade Considerations |
|---|---|---|
| Defined Culture Media | Provides nutrients and growth factors for cell proliferation | Formulation consistency, raw material traceability, endotoxin testing |
| Cell Dissociation Reagents | Detaches adherent cells while maintaining viability | Reduced enzyme activity variability, absence of animal components |
| Serum Alternatives | Replaces fetal bovine serum with defined components | Lot-to-lot consistency, comprehensive viral safety testing |
| Cryopreservation Media | Preserves cells at ultra-low temperatures | Defined composition, validated cooling rate protocols |
| Quality Control Kits | Detects contamination and verifies product quality | Validated sensitivity and specificity, included controls |
| Single-Use Bioprocess Containers | Closed-system cell culture and fluid handling | Extractables and leachables testing, sterilization validation |
The integration of advanced aseptic techniques with robust GMP manufacturing principles and high-throughput technologies represents the future of cell-based product development. Isolator-based systems, comprehensive quality control frameworks, and sophisticated contamination control strategies provide the foundation for manufacturing next-generation therapies with the required safety, efficacy, and consistency. As the field continues to evolve, maintaining "current" in cGMP will necessitate ongoing adoption of innovative technologies, refinement of analytical methods, and commitment to quality culture at all organizational levels. The protocols and strategies outlined in this application note provide a roadmap for researchers and manufacturing professionals seeking to excel in this demanding regulatory and technical environment.
Ensuring Excellence: Validation, Monitoring, and Comparative Analysis of Aseptic Practices
Maintaining sterility is a cornerstone of successful cell culture, impacting everything from basic research reproducibility to the safety and efficacy of clinically administered cell therapy products (CTPs) [76] [8]. Validation of sterility is not a single test but a comprehensive system encompassing controlled environments and rigorous testing protocols. This involves two critical and interdependent practices: environmental monitoring to control the external conditions and routine contamination screening to test the cultures themselves. For researchers and drug development professionals, mastering these protocols is essential for ensuring data integrity, complying with Good Manufacturing Practices (cGMP) for advanced therapies, and ultimately safeguarding patient safety [76] [77]. This document provides detailed application notes and experimental protocols for establishing a robust sterility assurance program within the broader context of cell culture aseptic technique research.
Environmental Monitoring Systems
Environmental monitoring provides objective evidence that the cell culture environment is controlled and is a fundamental requirement under cGMP quality systems [76] [77]. Its goal is to proactively detect microbial and particulate contamination before it compromises the product.
Monitoring Cleanroom and Air Quality
A classified cleanroom with HEPA-filtered laminar airflow is the first line of defense [77]. Monitoring involves regular checks of airborne and surface microorganisms, as well as non-viable particle counts, against standards like ISO 14644 [77].
Table 1: Key Parameters for Environmental Monitoring
| Parameter | Method | Frequency | Acceptance Criteria Example |
|---|---|---|---|
| Airborne Viable Particles (Microbes) | Active Air Sampling (Impaction) | Each operating session [78] | According to ISO 14644 & EU GMP Annex 1 Grade A/B/C/D classifications [77] |
| Surface Viable Particles | Contact Plates (e.g., Rodac plates) | Each operating session [78] | According to ISO 14644 & EU GMP Annex 1 Grade A/B/C/D classifications [77] |
| Non-Viable Particles | Laser Particle Counter | Routinely [77] | According to ISO 14644-1 classification [77] |
| Personnel Monitoring | Gloved Fingertip Testing | Each session [76] | No growth [76] |
Equipment and Facility Qualification
Equipment used in cGMP manufacturing, including incubators, refrigerators, and biosafety cabinets, must undergo a formal validation process known as Installation, Operational, and Performance Qualification (IOPQ) [76].
- Installation Qualification (IQ): Verifies the equipment is received and installed correctly according to manufacturer specifications [76].
- Operational Qualification (OQ): Tests the equipment's functionality to ensure it operates as intended under defined conditions (e.g., temperature uniformity in an incubator) [76].
- Performance Qualification (PQ): Demonstrates the equipment consistently performs according to pre-defined acceptance criteria under real-world conditions [76].
The workflow below outlines the core process for establishing and maintaining a validated sterile environment through monitoring and qualification.
Protocols for Routine Contamination Screening
Routine screening provides a direct assessment of the cell culture's sterility status. While traditional methods are culture-based and can take up to 14 days, rapid microbiological methods (RMMs) are increasingly being adopted to accelerate release times, which is critical for short-lived cell therapies [77].
Traditional Sterility Testing Methods
Protocol 1: Membrane Filtration Sterility Test [78] [79]
- Principle: The test product is filtered through a membrane with a pore size of 0.45 µm or less, which retains microorganisms. The membrane is then incubated in culture media to promote the growth of any captured organisms.
- Applications: Final product release testing for injectable drugs, cell therapy products, and other sterile fluids [79].
- Materials:
- Sterile membrane filtration apparatus
- 0.45 µm pore size membrane filters
- Vacuum source
- Fluid A (peptone solution with preservative inactivators)
- Culture Media: Tryptone Soya Broth (TSB) and Fluid Thioglycollate Medium (FTM)
- Procedure:
- Preparation: Aseptically assemble the filtration apparatus. Transfer an appropriate volume of the product (as per USP guidelines) to the funnel.
- Filtration: Apply a vacuum to draw the fluid through the membrane filter.
- Rinsing: Rinse the membrane with sterile Fluid A to remove any residual product that might inhibit microbial growth.
- Incubation: Aseptically transfer the membrane to a vessel containing TSB. For anaerobic culture, transfer to FTM.
- Incubation Conditions: Incubate TSB at 20-25°C for at least 7 days and FTM at 30-35°C for at least 7 days [78].
- Observation & Interpretation: Examine the media for turbidity indicating microbial growth daily. A clear appearance indicates a passing test. Any growth requires investigation.
Protocol 2: Automated Culture Systems (e.g., BacT/ALERT, BACTEC)
- Principle: These systems automatically detect microbial growth by monitoring CO2 production or other metabolic by-products using colorimetric or fluorometric sensors. They are widely used for sterility testing of hematopoietic stem cells [76].
- Procedure: The sample is inoculated into a specialized culture vial and loaded into the automated instrument, which continuously monitors for signs of growth, often reducing detection time compared to manual methods.
Rapid and Novel Screening Methods
Protocol 3: Machine Learning-Aided UV Absorbance Spectroscopy [80]
- Principle: This novel, label-free method detects microbial contamination by measuring the unique ultraviolet light absorption "fingerprints" of cell culture fluids. A machine learning model is trained to recognize patterns associated with contamination.
- Applications: Preliminary, real-time contamination screening early in the cell therapy manufacturing process [80].
- Materials:
- UV spectrophotometer
- Trained machine learning model/software
- Sterile cuvettes
- Procedure:
- Sampling: At designated intervals, a small aliquot of cell culture fluid is taken aseptically.
- Measurement: The aliquot is transferred to a cuvette, and its UV absorbance spectrum is measured.
- Analysis: The spectral data is analyzed by the pre-trained machine learning model.
- Result: The model provides a rapid "yes/no" contamination assessment within 30 minutes [80].
- Advantages: Non-invasive, requires no cell extraction or staining, and provides results much faster than growth-based methods [80].
Protocol 4: Next-Generation Sequencing (NGS) for Microbial Identification
- Principle: NGS can detect and characterize a wide range of microbial contaminants, including bacteria, fungi, and viruses, by sequencing all genetic material in a sample without the need for culture [77].
- Applications: Root-cause investigation of contamination events and comprehensive screening for difficult-to-culture organisms [77].
The following workflow compares the pathways of traditional, automated, and rapid screening methodologies.
Aseptic Process Simulation (Media Fill)
Media fill is the definitive validation study for an aseptic process, simulating manufacturing using microbial growth media instead of the actual product [78].
- Principle: All aseptic manipulations are performed with culture media, which is then incubated to detect any contamination introduced during the process.
- Protocol Highlights [78]:
- Media: Use Tryptone Soya Broth (TSB), which supports a wide range of aerobes and facultative anaerobes.
- "Worst-Case" Simulation: The study should challenge the process with slowest line speed, maximum number of personnel, longest hold times, and include all routine and justified non-routine interventions.
- Incubation: Incubate filled units at 20-25°C for 7 days, followed by 30-35°C for 7 days.
- Acceptance Criteria: For fills of less than 5,000 units, regulatory expectation is zero contaminated units. For larger fills, one contaminated unit triggers an investigation, and two require revalidation [78].
Table 2: Contamination Types and Detection Methods
| Contaminant Type | Common Signs | Primary Detection Methods |
|---|---|---|
| Bacteria | Cloudy, turbid culture medium; rapid pH change (yellow) [8] [2] | Traditional sterility test, automated culture systems, UV spectroscopy [80] [79] |
| Fungi (Mold/Yeast) | Fuzzy, off-white/black growth; turbidity; clumping [8] [2] | Traditional sterility test, automated culture systems |
| Mycoplasma | No visible turbidity; subtle effects on cell growth/metabolism [8] [2] | PCR, fluorescence-based assays, NGS [77] [8] |
| Viral | Often no visible signs; can alter cellular metabolism [8] | PCR, NGS, specific antigen/antibody tests [8] |
| Cross-Contamination | Altered growth patterns or morphology [8] | Cell line authentication (e.g., STR profiling) |
Validation and Qualification of Sterility Procedures
Validation provides documented evidence that a process consistently produces a result meeting its predetermined specifications [76].
Equipment IOPQ
As noted in Section 2.2, the IOPQ process for equipment is a foundational element of the cGMP quality system and is expected from the earliest phases of clinical development [76].
Method Validation
Any sterility testing method, especially RMMs, must be validated against the compendial method to demonstrate equivalent or superior performance. Parameters include accuracy, precision, specificity, and limit of detection.
Aseptic Process Validation (Media Fill)
The media fill, detailed in Section 3.3, is the primary method for validating the aseptic manufacturing process itself [78].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Sterility Validation
| Item | Function/Application |
|---|---|
| Tryptone Soya Broth (TSB) | General-purpose liquid microbial growth medium used for sterility tests, media fills, and growth promotion tests [78]. |
| Fluid Thioglycollate Medium (FTM) | Liquid medium for cultivating anaerobic and aerobic microorganisms; used in sterility testing to support growth of obligate anaerobes [78]. |
| Contact Plates (e.g., Rodac plates) | Contain solid culture media (like TSA) for monitoring microbial contamination on flat surfaces (floors, benches, equipment) [78]. |
| 70% Ethanol | The primary disinfectant for decontaminating gloves, work surfaces within the biosafety cabinet, and the exterior of vessels [4] [2]. |
| HEPA Filter | Provides a continuous flow of sterile, particle-free air within a biosafety cabinet or cleanroom, creating the aseptic work zone [77] [2]. |
| Sterile Single-Use Pipettes | For aseptic transfer of liquids; single-use prevents cross-contamination between samples and reagents [4] [81]. |
| Membrane Filtration Units | Apparatus used for the membrane filtration sterility test, consisting of a funnel and base designed to hold a sterile membrane filter [79]. |
| Rapid Microbiological Method (RMM) Kits | Kits for technologies like PCR, ATP bioluminescence, or flow cytometry that enable faster detection of microbial contaminants [77]. |
The Role of Cell Line Authentication in Preventing Cross-Contamination
Cell line authentication (CLA) serves as a critical quality control procedure in biomedical research, directly supporting the principles of aseptic technique by ensuring cellular purity and identity. Cross-contamination, the accidental introduction of foreign cells into a culture, poses a persistent threat to research integrity, leading to misidentified cell lines that compromise data reliability and reproducibility [82] [83]. Within the broader framework of cell culture aseptic technique protocols, authentication acts as a final verification step, detecting contamination that strict handling procedures aim to prevent. This Application Note details the implementation of CLA through Short Tandem Repeat (STR) profiling, providing researchers and drug development professionals with validated protocols to safeguard their work against the costly consequences of cross-contamination.
The Impact and Prevalence of Cell Line Cross-Contamination
Cross-contamination presents a widespread challenge in life sciences. Estimates suggest that 18 to 36% of popular cell lines are misidentified, often due to contamination by fast-growing lines such as HeLa cells [84] [85]. The consequences are severe: erroneous experimental results, wasted resources, and diminished confidence in the scientific literature. Instances of cross-contamination have led to study retractions after publication, as occurred with a 2005 paper on stem cell transformation where the observed phenomenon was later attributed to contamination by HT1080 cancer cells [86].
Table 1: Quantitative Impact of Cell Line Misidentification
| Metric | Statistic | Source/Reference |
|---|---|---|
| Prevalence of misidentified cell lines | 18-36% of popular lines | [84] |
| Researchers who authenticate cell lines | ~33% | ATCC SDO ASN-0002 [86] |
| Manuscript rejections due to cell line issues | ~4% | International Journal of Cancer [84] |
Standardized Authentication Method: Short Tandem Repeat (STR) Profiling
STR profiling is the internationally recognized gold standard method for authenticating human cell lines [82] [83] [87]. This technique analyzes short, repetitive DNA sequences (typically 2-7 base pairs long) that are highly variable between individuals. The number of repeats at specific chromosomal loci (locations) creates a unique DNA fingerprint for each cell line, allowing for unambiguous identification [87].
The process, standardized in the ANSI/ATCC ASN-0002-2022 guideline, involves amplifying these STR loci via polymerase chain reaction (PCR) and separating the fragments by size using capillary electrophoresis to generate an electropherogram, or peak plot [83] [87]. The resulting STR profile is a dataset of allele sizes across multiple loci, which serves as the basis for comparison with reference profiles.
Diagram 1: STR Profiling Workflow for Cell Line Authentication.
Interpretation Guidelines and Match Criteria
A submitted cell line is considered authenticated when its STR profile shows a high degree of similarity to a known reference profile. For human cell lines, a match of 80% or above is generally considered authenticated, while results below this threshold indicate potential misidentification or contamination [86]. The interpretation accounts for genetic instability, a common feature in cancer cell lines that may cause minor, progressive changes in their STR profiles over high passage numbers [86].
Integrated Experimental Protocol for Cell Line Authentication
STR Profiling Protocol
This protocol is adapted from commercial STR kit procedures and follows the ANSI/ATCC ASN-0002 standard [84] [83] [87].
I. Sample Preparation and DNA Extraction
- Harvest Cells: Grow cells to 70-80% confluence. Wash with PBS, trypsinize, and collect a cell pellet via centrifugation.
- Extract Genomic DNA: Use a commercial gDNA extraction kit. Resuspend the final DNA pellet in TE buffer or nuclease-free water.
- Quantify DNA: Measure DNA concentration using a spectrophotometer (e.g., Nanodrop). Ensure the A260/A280 ratio is between 1.7 and 2.0. A minimum of 0.5-1.0 ng/µL of DNA is typically required.
II. Multiplex PCR Amplification
- Prepare Reaction Mix: Use a validated commercial STR kit (e.g., Thermo Fisher's GlobalFiler or Identifiler kits). The kit contains a master mix, primers, and PCR reaction buffer.
- Set Up PCR: Combine 1-2 µL of template DNA with the PCR master mix according to the kit's instructions.
- Amplify: Run the PCR in a thermal cycler using the cycling conditions specified by the kit manufacturer. A typical program includes an initial denaturation (95°C for 1 min), followed by 28-30 cycles of denaturation (94°C for 3 sec), annealing (59°C for 1 min), and extension (72°C for 1.5 min), with a final extension (60°C for 25 min) [83].
III. Fragment Analysis and Data Collection
- Prepare Samples for Electrophoresis: Mix 1 µL of the PCR product with 8.7 µL of Hi-Di formamide and 0.3 µL of an internal size standard (e.g., GS600 LIZ) in a sample plate.
- Perform Capillary Electrophoresis: Run the samples on a genetic analyzer (e.g., Applied Biosystems 3500 or SeqStudio Flex Series). The instrument separates the DNA fragments by size and detects the fluorescently labeled PCR products.
- Generate Electropherogram: The software produces a peak plot where each peak represents a specific STR allele, with its size (in base pairs) and height (signal intensity) recorded.
Strategic Authentication Schedule
Integrating CLA at key points in the research lifecycle is essential for maintaining integrity.
Diagram 2: Strategic Schedule for Cell Line Authentication.
Table 2: Cell Line Authentication Schedule and Triggers
| Authentication Timepoint | Purpose | Recommended Action |
|---|---|---|
| Upon acquiring a new cell line | Establish a baseline profile and confirm identity before use. | Quarantine the cell line; perform STR profiling and mycoplasma testing before integrating into the main culture area [83] [85]. |
| When creating new cell lines or banks | Ensure the authenticity of newly established or banked resources. | Authenticate cells before freezing master and working cell banks [84] [85]. |
| During active culture (Routine) | Monitor for cross-contamination or genetic drift over time. | Re-authenticate every 1-3 months or every 10 passages, whichever comes first [84] [86]. |
| At key experimental milestones | Confirm identity at critical points for data integrity. | Authenticate before starting a new study, after transfection/selection, and before submitting a manuscript for publication [84] [83]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Cell Line Authentication
| Item | Function | Example Products/Specifications |
|---|---|---|
| Commercial STR Kit | Provides optimized primers and reagents for multiplex PCR of STR loci. | Thermo Fisher GlobalFiler Kit (24 loci), Identifiler Plus Kit (16 loci) [84] [83]. |
| Genetic Analyzer | Performs capillary electrophoresis to separate and detect amplified STR fragments. | Applied Biosystems 3500 Series, SeqStudio Flex Series [84] [83]. |
| Analysis Software | Automates allele calling and sizing from electropherogram data. | GeneMapper Software, Microsatellite Analysis (MSA) Software [83]. |
| Reference Database | Provides known STR profiles for comparison to verify cell line identity. | ATCC STR Database, Cellosaurus [82] [86]. |
| gDNA Extraction Kit | Ishes high-quality, purified genomic DNA for PCR amplification. | QIAamp DNA Mini Kit, DNeasy Blood & Tissue Kit [84]. |
Cell line authentication through STR profiling is a non-negotiable practice for ensuring research validity and reproducibility. By integrating the detailed protocols and strategic schedule outlined in this document, researchers can effectively shield their work from the detrimental effects of cross-contamination, thereby upholding the highest standards of scientific rigor in basic research and drug development.
Within cell culture aseptic technique protocols, the integrity of research and biopharmaceutical production is fundamentally dependent on effective sterilization. Sterilization processes eliminate all forms of microbial life, including bacteria, viruses, fungi, and spores, which is distinct from aseptic technique—the practices used to maintain sterility by preventing the introduction of contaminants into a sterile field [2] [4]. The selection of an appropriate sterilization method is critical and depends on the material composition of the items to be sterilized, the nature of the cell culture work, and the need to preserve the viability and functionality of biological agents. This analysis provides a detailed comparison of autoclaving, filtration, and chemical sterilization methods, offering structured protocols and application guidance for researchers, scientists, and drug development professionals.
Principles and Comparative Analysis of Sterilization Methods
A thorough understanding of the operational principles, advantages, and limitations of each sterilization method is a prerequisite for optimal selection and application.
Autoclaving (Steam Sterilization) utilizes saturated steam under high pressure to achieve sterilization. The typical temperature range is 121–134°C, which effectively denatures microbial proteins and destroys all microorganisms, including the most resistant bacterial spores [88] [89]. The process consists of three core phases: a purge phase where air is removed and replaced with steam; an exposure (sterilization) phase where temperature and pressure are maintained for a set time; and an exhaust phase where steam is released and the chamber is restored to ambient conditions [89]. This method is renowned for its high efficacy, cost-effectiveness, and environmental friendliness, as it uses steam and leaves no chemical residues [88].
Filtration Sterilization is a physical separation method that removes microorganisms from heat-sensitive liquids and gases by passing them through a membrane with pore sizes small enough to retain microbes (typically 0.2 µm or smaller) [90]. This method is indispensable for sterilizing solutions that would be degraded by heat, such as media supplements, antibiotics, and protein solutions. Key techniques include depth filtration, which uses a porous matrix to trap particles throughout the filter structure and is often used for clarifying cell culture harvests [90] [91], and membrane filtration, which provides absolute sterilization based on pore size.
Chemical Sterilization relies on chemical agents to destroy microorganisms and is primarily employed for heat-sensitive and moisture-sensitive devices [88] [92]. Common agents include Ethylene Oxide (EtO), a penetrating gas suitable for complex instruments; Glutaraldehyde, a liquid immersion sterilant with excellent material compatibility; Hydrogen Peroxide Gas Plasma, a low-temperature process; and Peracetic Acid, which rapidly breaks down into environmentally friendly by-products [88] [93]. These methods are essential for sterilizing items like endoscopes and plasticware but often involve toxic chemicals requiring extensive aeration and specialized handling to ensure staff safety [88] [93].
Table 1: Comparative Analysis of Sterilization Methods for Cell Culture Applications
| Feature | Autoclaving (Steam Sterilization) | Filtration | Chemical Sterilization |
|---|---|---|---|
| Mechanism of Action | Steam under pressure denatures proteins [88]. | Physical removal via membrane pores [90]. | Chemical agents disrupt microbial structures [92]. |
| Typical Cycle Time | 15-45 minutes [88] [89]. | Varies with volume and viscosity; generally rapid. | 30 min - several hours (plus prolonged aeration for EtO) [88] [93]. |
| Operating Temperature | High (121°C - 134°C) [88]. | Ambient or as specified by solution. | Low (e.g., 50°-55°C for Peracetic Acid) [93]. |
| Applicable Materials | Heat- and moisture-stable items: glassware, surgical instruments, biohazard waste [88] [94]. | Heat-labile liquids and gases: serum, antibiotics, drugs, media components [90]. | Heat- and moisture-sensitive devices: endoscopes, plastics, electronics [88] [92]. |
| Key Advantages | - Highly reliable & sporicidal- Cost-effective for reusable items- Non-toxic; no chemical residues [88] [89]. | - Gentle on heat-sensitive components- Preserves solution integrity- Can be used at point-of-use [90]. | - Effective for complex, delicate instruments- Low-temperature process- High penetration (gaseous agents) [88] [92]. |
| Key Limitations / Risks | - Not for heat-sensitive/moisture-sensitive items- Can damage plastics & electronics- Requires routine maintenance [88] [89]. | - Not for solids, oils, or viscous solutions- Membrane clogging- Initial protein adsorption [90]. | - Potential chemical toxicity to staff- Long processing & aeration times- Material compatibility concerns- Requires environmental ventilation [88] [93]. |
Table 2: Summary of Common Chemical Sterilants
| Chemical Agent | Primary Advantages | Primary Disadvantages & Hazards |
|---|---|---|
| Ethylene Oxide (EtO) | High penetration capability; suitable for a wide range of materials; does not damage heat-sensitive devices [88] [92]. | Toxic, carcinogenic, and flammable; requires long aeration; pungent odor; potential for acute toxicity [88] [92]. |
| Peracetic Acid | Rapid cycle time; low-temperature liquid immersion; environmentally friendly by-products; automated systems [93]. | Material incompatibility (e.g., aluminum); point-of-use system only; can cause serious eye/skin damage [93]. |
| Glutaraldehyde | Relatively inexpensive; excellent materials compatibility; numerous use studies published [93]. | Respiratory irritation and pungent odor; relatively slow mycobactericidal activity; can fix tissues to surfaces [93]. |
| Hydrogen Peroxide | No activation required; no disposal issues or odor; does not coagulate blood or fix tissues [93]. | Material compatibility concerns (e.g., brass, zinc); can cause serious eye damage upon contact [93]. |
Experimental Protocols for Sterilization
Protocol for Autoclaving Heat-Stable Liquids and Labware
This protocol is designed for sterilizing aqueous solutions (e.g., culture media, buffers) and laboratory glassware that are stable at high temperatures.
Materials:
- Autoclave (Gravity or Class B Vacuum)
- Autoclavable containers (e.g., borosilicate glass bottles with loose caps)
- Sterilization indicator tape
- Heat-resistant gloves
- Autoclave bags (for dry goods)
Procedure:
- Preparation:
- Liquids: Fill liquids into heat-resistant, autoclavable containers (e.g., glass bottles) only to 2/3 capacity to prevent boil-over. Loosen container caps to allow steam penetration and pressure equalization.
- Labware: Wrap dry items like glass pipettes and utensils in sterilization paper or place them in open autoclave bags to allow steam contact. Do not seal bags.
- Validation: Affix chemical indicator tape to the outside of all loads. This tape changes color upon exposure to heat, providing a visual indicator that the item has been processed.
Loading:
- Place items in the autoclave chamber, ensuring adequate space between them for uniform steam circulation. Avoid overloading the chamber [88].
- Place bottles upright in a stainless-steel tray to contain any potential spills.
Cycle Selection and Execution:
- Select the appropriate cycle based on the load:
- Gravity Cycle: Suitable for simple, solid items, unwrapped goods, and biohazard waste [94] [89].
- Liquid Cycle: Uses a slower exhaust phase to prevent violent boiling of liquids.
- Vacuum (Class B) Cycle: Essential for porous loads, wrapped items, and instruments with lumens, as it ensures more effective air removal [94].
- Start the cycle, which will automatically proceed through the purge, exposure, and exhaust phases [89].
- Select the appropriate cycle based on the load:
Unloading and Storage:
- Once the cycle is complete and the chamber temperature and pressure have returned to safe levels, put on heat-resistant gloves and open the door slightly to allow residual steam to escape. Wait 10-15 minutes before removing liquids to prevent flash boiling.
- Tighten the caps on liquid containers immediately upon removal.
- Store sterilized items in a clean, dry area. Verify the color change on the indicator tape [88].
Protocol for Sterilizing Heat-Labile Solutions by Membrane Filtration
This protocol describes the aseptic filtration of solutions using a 0.22 µm membrane filter to remove all microbial cells.
Materials:
- Sterile membrane filter unit (0.22 µm pore size)
- Sterile receiver flask (e.g., vacuum flask)
- Vacuum pump or peristaltic pump
- 70% ethanol solution and lint-free wipes
- Sterile syringes (if using a syringe-driven filter)
Procedure:
- Aseptic Setup:
- Perform all steps within a certified biosafety cabinet (BSC) with the UV light off and the blower on. Wipe the interior surface of the BSC, all solution containers, and the filter unit's external packaging with 70% ethanol [2] [4].
- Assemble the pre-sterilized filter unit onto the sterile receiver flask according to the manufacturer's instructions. Ensure all connections are secure.
Filtration Process:
- For Vacuum Filtration: Connect the receiver flask to a vacuum source. Pour the solution to be filtered into the top reservoir of the filter unit. Apply vacuum pressure to draw the solution through the membrane into the sterile receiver flask.
- For Syringe Filtration: Aseptically attach a sterile syringe to a pre-sterilized syringe filter. Draw the solution into the syringe, then gently and steadily push the plunger to express the solution through the filter into a sterile container.
- Do not exceed the recommended capacity or pressure of the filter unit to prevent membrane rupture.
Post-Filtration Handling:
- Cap the receiver flask or sterile container immediately after filtration.
- Label the container with the contents, date, and operator's initials.
- If not used immediately, store the filtered solution according to its specific requirements (e.g., 4°C, -20°C).
Protocol for Cell Harvesting and Clarification using Depth Filtration
This protocol is scaled for pilot-scale harvesting of mammalian cell cultures from a bioreactor to clarify the supernatant containing the product of interest (e.g., a monoclonal antibody).
Materials:
- Pall Stax single-use depth filter capsule system or equivalent [91]
- Peristaltic pump and appropriate tubing
- Pressure sensors
- Harvested cell culture broth
- Sterile harvest vessel
Procedure:
- System Assembly and Preparation:
- In a BSC, aseptically connect the inlet of the depth filter capsule to the cell culture broth container via the peristaltic pump tubing. Connect the outlet to the sterile harvest vessel.
- For large filter areas (≥5 m²), configure the system for bottom-in-top-out (inline) operation to equalize hydrostatic pressure and ensure optimal, scalable performance [91].
System Flush:
- Before introducing the valuable harvest, flush the system with a compatible buffer (e.g., phosphate-buffered saline) to wet the membrane and remove any extractables from the filter.
Clarification Process:
- Start the peristaltic pump at a low flow rate, gradually increasing to the target rate specified for the filter.
- Monitor the pressure differential across the filter throughout the process. A sharp pressure increase may indicate filter fouling or clogging.
- Collect the clarified harvest in the sterile vessel. This filtrate, now devoid of cells and most debris, is ready for subsequent downstream purification steps, such as chromatography.
System Disposal:
- Upon completion, the single-use filter capsule and tubing are disposed of as biohazardous waste, eliminating the need for cleaning validation [91].
Workflow Visualization and The Scientist's Toolkit
Sterilization Method Selection Workflow
The following diagram outlines the logical decision-making process for selecting an appropriate sterilization method based on the properties of the item to be sterilized.
Aseptic Cell Culture Handling Workflow
This diagram illustrates the critical steps for maintaining sterility while manipulating cells in a biosafety cabinet.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Sterilization and Aseptic Technique
| Item | Function/Application | Key Considerations |
|---|---|---|
| Biosafety Cabinet (BSC) | Provides a sterile work area for aseptic procedures via HEPA-filtered laminar airflow [2] [4]. | Must be certified annually. Run for 15+ minutes to purge before use. Avoid disrupting airflow. |
| 70% Ethanol | Primary disinfectant for all work surfaces, gloves, and exterior of containers entering the BSC [2] [4]. | Effective concentration for microbial kill; allows sufficient contact time for evaporation. |
| Sterile Pipettes and Tips | For precise, aseptic transfer of liquids without cross-contamination [2] [4]. | Use single-use, pre-sterilized disposables. Never use a pipette more than once. |
| Sterile Membrane Filters (0.22 µm) | For cold sterilization of heat-labile solutions like antibiotics, enzymes, and serum [90]. | Check chemical compatibility of membrane with solution. Pre-wet filters for certain applications. |
| Autoclavable Culture Media | Nutrient-rich medium for cell growth, sterilized by autoclaving for heat-stable formulations. | Follow precise instructions for preparation and cooling to prevent precipitation or degradation. |
| Chemical Indicator Tape | Visual monitoring of autoclave processing; confirms exposure to heat [88]. | Color change does not guarantee sterility; used in conjunction with biological indicators. |
| Personal Protective Equipment (PPE) | Protects operator from biological hazards and protects cell cultures from personal contamination [2] [4]. | Includes lab coat, gloves, and safety glasses. Gloves should be changed frequently. |
- Method Selection is Critical: The choice between autoclaving, filtration, and chemical sterilization is not one of superiority but of appropriateness. Autoclaving remains the gold standard for heat-tolerant materials due to its reliability and cost-effectiveness. Filtration is the only viable option for heat-labile liquids, while chemical methods are reserved for critical, heat-sensitive devices [88] [90] [92].
- Aseptic Technique is Paramount: Even perfectly sterilized materials can become contaminated without rigorous aseptic technique. This includes disciplined work in a BSC, meticulous personal hygiene, and sterile handling practices [2] [4]. The most advanced sterilization equipment cannot compensate for poor technique.
- Scale-Up Considerations: Processes developed at a laboratory scale must be designed with scalability in mind. For instance, depth filtration for cell harvesting requires careful system design (e.g., bottom-in-top-out configuration for large areas) to ensure performance is maintained from the lab to the manufacturing scale [91].
- Emerging Technologies: Novel technologies like fluidized bed centrifugation are being developed to address limitations in traditional cell retention and sorting methods for continuous biomanufacturing, highlighting the field's ongoing evolution [95].
In summary, a robust aseptic protocol for cell culture and drug development is built upon a foundational understanding of these sterilization methods. By strategically selecting and correctly implementing the appropriate technique—and coupling it with unwavering aseptic practice—researchers can safeguard the integrity of their experiments, ensure the safety of their products, and contribute to reliable and reproducible scientific outcomes.
Within the rigorous framework of a thesis on cell culture aseptic technique protocols, selecting the appropriate culture platform is a fundamental decision that directly impacts data integrity, reproducibility, and operational efficiency. This document provides a detailed cost-benefit analysis, application notes, and standardized protocols for evaluating traditional and novel culture systems. The transition from conventional two-dimensional (2D) monolayers to more physiologically relevant three-dimensional (3D) platforms represents a significant shift in biomedical research [96] [52]. However, this transition introduces complex considerations regarding cost, technical skill, and integration into existing workflows governed by strict aseptic technique. This analysis is designed to equip researchers and drug development professionals with the data and methodologies needed to make informed, cost-effective decisions without compromising scientific rigor or sterility.
Market Context and Quantitative Comparison
The global cell culture system market is experiencing robust growth, characterized by a clear trend of migration from 2D to 3D platforms. The market, valued at approximately $10 billion in 2025, is projected to grow at a Compound Annual Growth Rate (CAGR) of 8% through 2033 [97]. Specifically, the 3D cell culture sector is expanding even more rapidly, with a projected CAGR of 15% from 2025 to 2035, having been valued at $1.04 billion in 2022 [96]. This growth is primarily fueled by the demand for more predictive in vitro models that can reduce late-stage drug failure rates, which have historically been as high as 90% in phases II and III of clinical trials [98].
Table 1: Direct Cost and Performance Comparison of 2D vs. 3D Culture Platforms
| Feature | Traditional 2D Systems | Novel 3D Systems |
|---|---|---|
| System Cost (Entry-Level) | ~$15,000 (for stackable incubators) [98] | ~$80,000 - $150,000 (for organ-on-chip systems) [98] |
| Scalability | Highly scalable with standard vessels (flasks, plates); limited only by incubator space [99] | Scalability can be challenging; often requires specialized bioreactors or printers for larger volumes [96] |
| Physiological Relevance | Low; fails to mimic complex tissue architecture and cell-cell/matrix interactions [96] [52] | High; better recapitulates tissue microenvironment, hypoxia, and drug responses [96] [98] |
| Throughput & Automation | High; well-established for high-throughput screening in standard multi-well plates [100] | Variable; scaffold-free spheroid systems enable 384-well throughput, while microfluidic systems are advancing [98] |
| Typical Applications | Basic research, routine cell maintenance, initial cytotoxicity screens [97] [99] | Cancer research (34-45% of applications), drug discovery, personalized medicine, regenerative medicine [96] [98] |
| Concordance with Clinical Outcomes | Lower; poor prediction of human in vivo responses [98] | Higher; patient-derived organoids showed 85% correlation with clinical drug responses in validation studies [98] |
The choice of platform has a direct impact on research and development economics. The use of 3D models in drug discovery has been reported to reduce R&D costs by up to 25% by providing more accurate data earlier in the process, thereby reducing costly clinical trial failures [96]. Furthermore, the deployment of advanced liver-on-chip models has been linked to a 30% reduction in candidate withdrawal due to hepatotoxicity [98]. Despite higher initial investment, the long-term benefits of novel platforms can be substantial for applications requiring high biological fidelity.
Experimental Protocol for Comparative Evaluation
The following protocol provides a standardized methodology for directly comparing the performance and cost-in-use of traditional 2D and scaffold-based 3D culture systems, with all steps performed under strict aseptic conditions.
Research Reagent Solutions and Materials
Table 2: Essential Materials for Comparative Cell Culture Experiments
| Item | Function | Specific Examples |
|---|---|---|
| Laminar Flow Hood (BSC) | Provides a sterile work area for all culture procedures to prevent biological contamination [4] [2] | Class II Biosafety Cabinet |
| Personal Protective Equipment (PPE) | Forms a barrier to minimize contamination from the user; includes gloves, lab coat, and safety glasses [4] [11] | Sterile gloves, disposable lab coat |
| 70% Ethanol | Gold-standard disinfectant for sterilizing work surfaces, equipment, and container exteriors [4] [2] | 70% Ethanol solution in spray bottle and lint-free wipes |
| Cell Culture Media & Supplements | Provides essential nutrients, growth factors, and a buffered environment for cell growth and maintenance [52] [99] | DMEM or RPMI, supplemented with FBS, L-Glutamine |
| 2D Culture Vessels | Standard plasticware providing a flat, adherent surface for 2D cell growth. | T-75 flasks, 6-well and 96-well plates [97] |
| 3D Scaffold Matrix | Provides a 3D supportive structure that mimics the extracellular matrix (ECM) for cells. | Hydrogels (e.g., collagen, synthetic PeptiGels) [96] |
| Enzymatic Detachment Agent | Detaches adherent cells from the culture surface for sub-culture or analysis in 2D systems. | Trypsin, TryPLE, or milder alternatives like Accutase [52] [99] |
| Cryoprotectant | Protects cells from ice crystal formation during freezing for long-term storage. | DMSO (5-10%) or pre-prepared commercial solutions [99] |
Methodology: Side-by-Side Analysis of 2D and 3D Culture
Objective: To evaluate the growth, viability, functionality, and total cost of culturing the same cell line (e.g., HepG2 liver cells or patient-derived cancer cells) in 2D and 3D formats over three sequential passages.
Safety and Aseptic Precaution: All procedures must be conducted inside a properly maintained and sterilized biosafety cabinet. Researchers must wear appropriate PPE. All surfaces and equipment exteriors must be wiped with 70% ethanol before being introduced into the sterile field. Work should be performed deliberately and slowly to minimize turbulence and the risk of airborne contamination [4] [2].
Part A: Cell Seeding and Culture Maintenance
- Cell Preparation: Begin with a vial of cryopreserved cells, thawed rapidly in a 37°C water bath until only a small ice crystal remains. Transfer the cell suspension to a centrifuge tube containing pre-warmed medium to dilute the cryoprotectant. Centrifuge at 200-250 x g for 5 minutes, discard the supernatant, and resuspend the cell pellet in fresh, pre-warmed complete medium [99].
- Cell Counting and Seeding:
- Count the cells using an automated cell counter or hemocytometer.
- For 2D Culture: Seed cells at a standard density (e.g., (1x10^5) cells/mL) into standard tissue culture flasks or plates.
- For 3D Culture: Resuspend the calculated number of cells in the hydrogel scaffold solution according to the manufacturer's instructions (e.g., (1-2x10^6) cells/mL). Pipette the cell-matrix mix into a multi-well plate and incubate at 37°C for 30 minutes to allow for polymerization, before carefully adding overlay culture medium [96].
- Incubation and Feeding: Culture all systems in a humidified 37°C, 5% CO₂ incubator. Monitor medium color (with phenol red) daily for acidification. Refresh the medium every 2-3 days for both systems under strict aseptic technique, minimizing the time culture vessels are open [99].
Part B: Assessment and Data Collection
- Growth and Viability Monitoring:
- Microscopy: Observe cultures daily using a phase-contrast microscope. Document morphology, cell density, and the formation of 3D spheroids or structures. Note any signs of contamination (e.g., cloudiness, fungal hyphae) [99].
- Viability Assay: At the end of each passage (e.g., Day 5), perform a quantitative viability assay like the MTT or CellTiter-Glo 3D assay on both culture types, following the manufacturer's protocol. The latter is particularly suited for 3D cultures due to its lytic nature.
- Functional Assessment (Drug Response):
- At ~80% confluence (2D) or when spheroids are well-formed (3D), treat cultures with a range of concentrations of a test compound (e.g., a chemotherapeutic like Doxorubicin). Incubate for 48-72 hours.
- Quantify the inhibitory concentration (IC₅₀) using the viability assay from Step 1. Compare the IC₅₀ values and dose-response curves between the 2D and 3D models.
- Cost Tracking:
- Maintain a detailed log for all materials used, including culture vessels, medium volume, scaffold matrix, reagents, and plasticware. Calculate the total cost per sample for each system over the duration of the experiment.
Part C: Data Analysis and Interpretation
- Analyze the viability and drug response data for statistical significance.
- Compare the calculated IC₅₀ values from the 2D and 3D systems; it is expected that the 3D model will show higher resistance (higher IC₅₀), which is often more clinically relevant, especially in oncology [98].
- Compare the total cost per data point for each system, factoring in both consumables and the researcher's time.
Diagram 1: Experimental workflow for platform comparison.
The decision to adopt a novel culture platform is not merely a technical one but a strategic investment. The following diagram outlines the key decision-making workflow, integrating technical requirements, biological relevance, and economic considerations.
Diagram 2: Decision framework for platform selection.
This analysis demonstrates that there is no single "best" platform; the optimal choice is dictated by the research question, available resources, and required throughput. Traditional 2D systems remain a powerful, cost-effective tool for high-throughput screening, basic biology, and applications where high physiological complexity is not the primary focus [97] [100]. In contrast, novel 3D platforms, despite higher initial costs and operational complexity, offer unparalleled biological fidelity that can significantly de-risk the drug development pipeline and advance personalized medicine [96] [98].
For a comprehensive research thesis, a hybrid strategy is often most effective: utilizing 2D systems for initial, high-volume experiments and deploying 3D models for validating key findings. This approach maximizes scientific output while managing costs, ensuring that the foundational principle of aseptic technique is rigorously applied across all platforms to guarantee the integrity and reproducibility of the research.
Good Cell Culture Practice (GCCP) represents a set of guidelines that ensure the reproducibility, reliability, and ethical compliance of in vitro cell culture experiments. Within this framework, aseptic technique forms the foundational barrier protecting cell cultures from microbial contamination (bacteria, fungi, yeast, and viruses) and cross-contamination with other cell lines. The integration of rigorous aseptic procedures within the GCCP paradigm is not merely a technical requirement but a critical quality management system essential for producing valid scientific data [52] [4]. The consequences of inadequate technique are severe, ranging from compromised cell viability and altered growth patterns to the publication of irreproducible results, with an estimated 16.1% of published papers potentially using problematic cell lines [52]. Furthermore, the increasing classification of many cell lines as Genetically Modified Cell Lines (GMCLs) demands heightened safety and containment protocols, making the synergy of GCCP and aseptic technique more crucial than ever [52].
Core Principles and Contamination Risks
The core principle of aseptic technique in cell culture is to establish a barrier between the uncontrolled external environment and the sterile cell culture. This is achieved through a combination of a sterile work area, impeccable personal hygiene, sterile reagents and media, and sterile handling practices [4]. Contamination risks are omnipresent, originating from non-sterile supplies, airborne particles, unclean incubators, dirty work surfaces, and the personnel themselves [52] [4].
Biological contamination is the most direct threat, but other significant risks include:
- Cross-Contamination and Misidentification: The International Cell Line Authentication Committee (ICLAC) lists 576 misidentified or cross-contaminated cell lines, which can invalidate research findings [52].
- Chemical Contamination: From non-sterile or improperly handled reagents.
- Genetic Drift: Long-term culture can lead to genetic alterations, which, while not a direct result of aseptic failure, is a key concern addressed by GCCP quality control measures like cell authentication [52].
The table below summarizes the primary contamination types and their common sources:
Table 1: Common Cell Culture Contaminants and Sources
| Contaminant Type | Common Sources | Potential Impact on Culture |
|---|---|---|
| Bacteria & Fungi | Non-sterile surfaces, reagents, air, personnel [4] | Cloudy media, pH shift, cell death. |
| Mycoplasma | Serum, personnel, cross-contamination [52] | Chronic infection, altered metabolism, no visible turbidity. |
| Viruses | Serum, trypsin, primary cells [52] | Persistent infection, cytopathic effects. |
| Cross-Cell Contamination | Improper handling, shared reagents [52] | Misidentified cell lines, invalid research data. |
Practical Application: The Aseptic Technique Protocol
Implementing aseptic technique requires meticulous attention to detail before, during, and after cell culture procedures. The following protocol provides a detailed methodology for sterile work.
Pre-Work Preparation
- Personal Protective Equipment (PPE): Don a laboratory coat, gloves, and safety glasses or goggles. Secure long hair [4].
- Workspace Decontamination: Wipe down the entire interior surface of the biosafety cabinet (BSC) with 70% ethanol, including the walls and work surface. Place all necessary pre-wiped items (media bottles, pipettes, tip boxes) inside the BSC before starting work [4].
- Reagent Inspection: Visually inspect all media and reagents for cloudiness, unusual color, or floating particles. Discard any contaminated items immediately [4].
Sterile Workflow inside the Biosafety Cabinet
- Hand Hygiene: Regularly wipe gloved hands with 70% ethanol throughout the procedure [4].
- Container Management: Never lay cap lids face-up. Place them face-down on a sterile surface if they must be put down. Work swiftly but deliberately to minimize the exposure of open containers to the environment [4].
- Liquid Handling: Use sterile pipettes and a pipettor for all liquid manipulations. Never use the same pipette for different reagents or cell lines to prevent cross-contamination [4]. Avoid pouring from bottles or flasks.
- Bottle and Flask Care: Wipe the outside of all containers with 70% ethanol before introducing them into the BSC. Keep bottles and flasks capped when not in immediate use [4].
- Spill Management: Clean any spillage immediately with 70% ethanol [4].
Post-Work Cleanup
- Disposal: Properly dispose of all used plasticware and liquid waste according to institutional biological safety protocols.
- Surface Decontamination: Wipe down the BSC interior surfaces again with 70% ethanol.
- Equipment Maintenance: Leave the BSC running for at least 15 minutes after use to purge contaminants, or according to the manufacturer's instructions [4].
Validation and Monitoring: Media Fill Trials
Aseptic technique competency and process validation can be quantitatively assessed using Aseptic Process Simulation (APS), commonly known as a Media Fill trial. This test simulates the entire aseptic manufacturing process using a sterile microbiological growth medium (e.g., Tryptone Soya Broth) in place of the drug product [78].
Media Fill Protocol
- Preparation: Sterilize all equipment and materials as for a routine cell culture or drug filling operation.
- Simulation: Perform the standard aseptic procedure, using the growth medium to mimic all handling steps, including transfers, vial breaks, and exposure times.
- Worst-Case Challenge: The simulation should incorporate "worst-case" conditions, such as the maximum number of personnel, longest exposure times, and all routine and non-routine interventions (e.g., hopper charging, vial removal, environmental monitoring) [78].
- Incubation: All media-filled units are incubated under conditions optimal for microbial growth (e.g., 20-25°C for 7 days, then 30-35°C for 7 days) to recover slow-growing and common contaminating organisms [78].
- Inspection and Acceptance Criteria: After incubation, units are inspected for turbidity, indicating contamination. Regulatory guidelines provide clear acceptance criteria. For example, for fills of less than 5,000 units, zero contaminated units is required. For larger fills, one contaminated unit triggers an investigation, and two or more require revalidation [78].
Table 2: Industry Data on Microbiological Contamination in Cultured Products
| Parameter | Finding | Context / Implication |
|---|---|---|
| Average Batch Failure Rate | 11.2% [101] | Across cultivated meat industry (n=11); highlights practical challenge. |
| Failure Rate at R&D Scale | 19.5% [101] | Higher failure in larger, more complex facilities. |
| Most Common Vectors | Personnel, Equipment, Production Environment [101] | Targets for improved training and protocols. |
| Adjacent Industry Benchmark | ~3.2% contamination failure rate [101] | Contamination rate in commercial biopharmaceutical facilities; an aspirational target. |
Essential Materials and Reagent Solutions
The following toolkit is essential for executing and maintaining aseptic technique and GCCP compliance.
Table 3: Research Reagent Solutions and Essential Materials for Aseptic Cell Culture
| Item | Function / Application | Key Considerations |
|---|---|---|
| Biosafety Cabinet (BSC) | Provides a sterile, HEPA-filtered work environment for procedures [4]. | Must be certified annually; located in a low-traffic, draft-free area. |
| 70% Ethanol | Primary disinfectant for surfaces, gloves, and container exteriors [4]. | Effective concentration for microbial kill; used liberally throughout work. |
| Sterile Pipettes & Pipettor | For precise, aseptic transfer of liquids without pouring [4]. | Use each sterile pipette only once to prevent cross-contamination. |
| Cell Culture Media | Provides nutrients for cell growth and maintenance (e.g., DMEM, RPMI) [52]. | Check for sterility and stability; pre-warm before use. |
| Soybean Casein Digest Medium (SCM/TSB) | Microbiological growth medium for Media Fill validation studies [78]. | Supports growth of aerobic microorganisms; quality control for growth promotion is critical. |
| Personal Protective Equipment (PPE) | Forms a barrier between personnel and the biological material [4]. | Protects both the user and the culture; required at all times. |
| Non-Enzymatic Dissociation Agents (e.g., EDTA) | For detaching adherent cells while preserving surface protein epitopes [52]. | Preferable to trypsin for experiments requiring intact surface markers (e.g., flow cytometry). |
Workflow Visualization: Integrating GCCP and Aseptic Technique
The following diagram illustrates the logical workflow for integrating aseptic technique within the broader GCCP framework, from initial setup to quality control and data reporting.
Conclusion
Mastering aseptic technique is not a one-time training point but a continuous commitment to quality and precision in cell culture. A robust aseptic protocol, grounded in foundational principles and applied through meticulous methodology, is the bedrock of reliable and reproducible scientific research. By effectively troubleshooting contamination and validating sterility through rigorous monitoring, laboratories can protect invaluable cell lines, time, and resources. As cell culture evolves with more complex 3D models and co-culture systems, the principles of asepsis will remain paramount. Their diligent application directly enhances the accuracy of drug screening, the safety of biopharmaceuticals, and the overall pace of biomedical discovery, ensuring that in vitro models truly fulfill their promise as predictive tools for human health.
References
- 1. "Aseptic" vs. "Sterile": Do You Know The Difference? [https://www.dictionary.com/e/aseptic-vs-sterile/]
- 2. Mastering Aseptic Technique: The Foundation of ... [https://www.labmanager.com/mastering-aseptic-technique-the-foundation-of-successful-cell-culture-34208]
- 3. Aseptic Technique: What It Is & What To Know [https://my.clevelandclinic.org/health/treatments/aseptic-technique]
- 4. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 5. Aseptic Techniques in Cell Culture [https://gmpplastic.com/blogs/news/aseptic-techniques-in-cell-culture?srsltid=AfmBOorv3OKlVfvbhr_wnAnplbVjrwtaHJ90rVYW95QFEzC0aV5fPdTE]
- 6. Are Semi-Quantitative Clinical Cultures Inadequate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8303231/]
- 7. Automated, aseptic sampling with small-volume capacity ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1612648/full]
- 8. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 9. Ensuring Reproducibility: Critical Cell Culture Quality ... [https://www.technologynetworks.com/cell-science/articles/ensuring-reproducibility-critical-cell-culture-quality-controls-354393]
- 10. How to Reduce Sample Contamination [https://blog.omni-inc.com/blog/how-to-reduce-sample-contamination]
- 11. Mastering Aseptic Technique in Laboratories [https://cellculturecompany.com/mastering-aseptic-technique-in-laboratories/]
- 12. Types of Cell Culture Contamination and How To Prevent ... [https://www.technologynetworks.com/cell-science/articles/types-of-cell-culture-contamination-and-how-to-prevent-them-397776]
- 13. Cell Culture Contamination: 5 Common Sources and How to Prevent Them [https://www.capricorn-scientific.com/knowledge-center/cell-culture-contamination]
- 14. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 15. Troubleshooting Cell Culture Contamination: A Practical Solution Guide [https://www.yeasenbio.com/blogs/cell/troubleshooting-cell-culture-contamination-a-practical-solution-guide]
- 16. How to Detect Cell Culture Contamination [https://www.goldbio.com/blogs/articles/how-to-detect-cell-culture-contamination?srsltid=AfmBOordcQ-jKu83X3xTolGlFKGcdqR6o-8MpKYfgYAylAk9T30iHoJF]
- 17. Cell Culture Contamination: How to Prevent Fungal, Yeast, ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/how-to-control-bacterial-contamination-and-other-unwelcome-micro.html]
- 18. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination]
- 19. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 20. Biological Safety Cabinets | The University of Vermont [https://www.uvm.edu/safety/biological-safety-cabinets]
- 21. Maintaining a Clean Tissue Culture Lab Setting Using ... [https://plantcelltechnology.com/blogs/blog/how-to-maintain-a-clean-lab-setting-using-aseptic-techniques?srsltid=AfmBOopwQlxGiglMuLyeB9iyOUv24HQnmFH8pVEfKXos7Ii7jJ4XoW4W]
- 22. Aseptic technique | Research Starters [https://www.ebsco.com/research-starters/health-and-medicine/aseptic-technique]
- 23. Assessing the Efficacy of Alcohol Swabbing in Preventing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446881/]
- 24. How To Avoid Contamination in Lab [https://techsafety.com/blog/avoid-contamination-in-lab]
- 25. Mastering Cell Culture Techniques: From Basics to ... [https://cellculturecollective.com/blog/mastering-cell-culture-techniques-from-basics-to-advanced-applications/?srsltid=AfmBOorE-ZCsl5Q5SUxJeEguEBVnKPF4J2QZLa9P-K3g7shja71xDlw1]
- 26. Viral contamination in cell culture: analyzing the impact of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 27. How to Avoid Contamination in Lab Samples [https://www.aurorabiomed.com/how-to-avoid-contamination-in-lab-samples/?srsltid=AfmBOopl6oJoeLXGLaD2Jh1BtHDMEzPeVACDF2ivZsERAJUGgCF0-kOL]
- 28. An Extensive Method for Maintenance of Sterility in ... [https://www.mdpi.com/2078-1547/8/2/26]
- 29. Biological Safety Cabinets - EHSO Manual 2025-2026 [https://labman.ouhsc.edu/hbSections.aspx?ID=612]
- 30. Aseptic Technique in the Lab: Complete Step-by- ... [https://www.mantacc.com/blog/aseptic-technique?srsltid=AfmBOorjjvn9SWXko3ptvHj084I7nz47u6514OnFYhoxBYRLfySMbvBD]
- 31. Aseptic Technique in the Lab: Complete Step-by- ... [https://www.mantacc.com/blog/aseptic-technique?srsltid=AfmBOopzvDfLtjDPvseowuT4ZUtve5MSadeGLbsZbYIJV7GUmZ_xjuFh]
- 32. 4.3 Aseptic Technique – Nursing Skills – 2e [https://wtcs.pressbooks.pub/nursingskills/chapter/4-3-asceptic-technique/]
- 33. Aseptic techniques [https://practicalbiology.org/standard-techniques/aseptic-techniques]
- 34. Chapter 4 Aseptic Technique - Nursing Skills - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK593203/]
- 35. Aseptic Laboratory Techniques: Plating Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846335/]
- 36. Forward vs Reverse Pipetting: Master Lab Techniques 2025 [https://niito.kz/pipettes/pipetting-techniques-forward-reverse/]
- 37. The Ultimate Guide to Micropipettes (2025 Edition) [https://uniglobalbusiness.com/blogs/scientific-instruments/the-ultimate-guide-to-micropipettes-2025-edition?srsltid=AfmBOoqyoLydrf41zppBEszUjCUpLpijvm7UB3IIZeAcJGB09ACVfEYK]
- 38. Guide to Pipetting [https://pipette.com/blog/guide-to-pipetting?srsltid=AfmBOopJrt8WcmRj1I06Og161exaoiGlUs7aAJsdI1p1pOCX-B5FFdnp]
- 39. 12 Tips to Improve Your Pipetting Technique in 2025 [https://biosistemika.com/blog/tips-to-improve-pipetting-technique/]
- 40. Mastering Cell Culture Techniques: From Basics to ... [https://cellculturecollective.com/blog/mastering-cell-culture-techniques-from-basics-to-advanced-applications/?srsltid=AfmBOoo9ZTbfGFWJM9ZWH4vWxVvVU2dT13sCTNvd-9974XYTHhtJfl8P]
- 41. Adherent and suspension cell culture [https://greenelephantbiotech.com/blog/adherent-and-suspension-cell-culture/]
- 42. The Pros and Cons of Adherent Versus Suspension Cell ... [https://www.biopharminternational.com/view/the-pros-and-cons-of-adherent-versus-suspension-cell-culture]
- 43. Adherent versus suspension based platforms: what is the ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/2244/Adherent-versus-suspension-based-platforms-what-is-the-near-future-of-viral-vector-manufacturing]
- 44. Types of Cell Culture: Adherent vs. Suspension ... [https://bostonmedsupply.com/types-of-cell-culture-adherent-vs-suspension-cells-and-their-applications/]
- 45. Suspension Culture vs Adherent Culture: Pros and Cons ... [https://synapse.patsnap.com/article/suspension-culture-vs-adherent-culture-pros-and-cons-compared]
- 46. Mastering Cell Culture Techniques: From Basics to ... [https://cellculturecollective.com/blog/mastering-cell-culture-techniques-from-basics-to-advanced-applications/?srsltid=AfmBOoqBIj2VxEVVLwLgEmsgTfklgDFlLdfIIsZIh1-hvJCZQ0_AksxV]
- 47. Three-Dimensional (3D) in vitro cell culture protocols to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9907841/]
- 48. Cultrex® 3D Spheroid BME Invasion Assay Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/3d-cell-culture/96-well-3d-spheroid-bme-cell-invasion-assay?srsltid=AfmBOoqKj4yzWyUTXytYHRqig8NdNnyPY_dCqmW3VS7e36Ebdzqli5U-]
- 49. user-friendly mesh barrier pipette tips for 3D-spheroid culture [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-019-0210-3]
- 50. Protocol for Immune Cell Isolation, Organoid Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717717/]
- 51. Protocol for generating a co-culture of macrophages with ... [https://www.sciencedirect.com/science/article/pii/S2666166724007019]
- 52. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 53. What are the signs of contamination in cell cultures? [https://synapse.patsnap.com/article/what-are-the-signs-of-contamination-in-cell-cultures]
- 54. pH Monitoring for Suspension Cultures [https://www.scientificbio.com/ph-monitoring]
- 55. Bacterial cellular morphologies [https://en.wikipedia.org/wiki/Bacterial_cellular_morphologies]
- 56. How to Detect Cell Culture Contamination [https://www.goldbio.com/blogs/articles/how-to-detect-cell-culture-contamination?srsltid=AfmBOooBzHs-FXzWrmJDu6dokmc7BIlio362AIjYjqfI5sXXoUqou0KN]
- 57. 避免细胞培养污染的技巧贴士 - Integra Biosciences [https://www.integra-biosciences.com/china/cn/stories/tips-preventing-contamination-cell-culture]
- 58. Fungus [https://unclineberger.org/tissueculture/contaminant/funguscontam/]
- 59. 支原体污染常用检测方法 [http://cvcc.ivdc.org.cn/kyjl/201806/t20180605_49712.html]
- 60. 制药中的支原体测试 [https://www.sigmaaldrich.com/MO/zh/applications/microbiological-testing/mycoplasma-testing?srsltid=AfmBOoqn2XRzFfqyN7OzR0GhXiAtNEUHVXKf5zd0haGVzNcuucG9K6CB]
- 61. | Thermo Fisher Scientific - IN Cell Culture Contamination [https://www.thermofisher.com/in/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 62. Techniques and Practices to Avoid Cell by... Culture Contamination [https://www.jove.com/t/64769/cell-culture-techniques-practices-to-avoid-contamination-fungi]
- 63. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://www.mdpi.com/2073-4409/12/5/682]
- 64. Recommendations for Disinfection and Sterilization in ... [https://www.cdc.gov/infection-control/hcp/disinfection-sterilization/summary-recommendations.html]
- 65. 1.7: Aseptic Technique [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_Laboratory_Manual_(Hartline)/01%3A_Labs/1.07%3A_Aseptic_Technique]
- 66. Aliquoting FBS: Best Practices, Common Risks & Alternatives [https://www.capricorn-scientific.com/knowledge-center/aliquot-fbs]
- 67. Mastering Cell Culture Techniques: From Basics to ... [https://cellculturecollective.com/blog/mastering-cell-culture-techniques-from-basics-to-advanced-applications/?srsltid=AfmBOooixwKHl5ZbXcx7HCH9aqtTbJ51YQrd6DX36vY6GVOwMxYeKeaU]
- 68. Cell Culture Basics: Equipment, Fundamentals and Protocols [https://www.technologynetworks.com/cell-science/articles/cell-culture-basics-equipment-fundamentals-and-protocols-348413]
- 69. Maintaining a Clean Tissue Culture Lab Setting Using ... [https://plantcelltechnology.com/blogs/blog/how-to-maintain-a-clean-lab-setting-using-aseptic-techniques?srsltid=AfmBOorG5KxLwOumNJ8KfR6W9azR_o0_vqpH02OKTXy9m5_JWruF4--m]
- 70. Facts About the Current Good Manufacturing Practice ... [https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp]
- 71. cGMP: A Guide to Current Good Manufacturing Practices | Tulip [https://tulip.co/blog/cgmp-guide-to-current-good-manufacturing-practices/]
- 72. Isolator-based point-of-care manufacturing - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440961/]
- 73. Current Good Manufacturing Practice (cGMP): An Overview ... [https://www.chromatographyonline.com/view/current-good-manufacturing-practice-cgmp-an-overview-for-the-analytical-chemist]
- 74. Good Manufacturing Practice (GMP): Pharma Quality ... [https://intuitionlabs.ai/articles/gmp-pharmaceutical-quality-compliance]
- 75. Current Good Manufacturing Practices (cGMP) Explained [https://www.bprhub.com/blogs/what-are-current-good-manufacturing-practices]
- 76. All you need to know about equipment validation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421869/]
- 77. Evolving Cleanroom Procedures and Sterility Challenges [https://www.biopharminternational.com/view/evolving-cleanroom-procedures-sterility-challenges]
- 78. Validation of Aseptic Processes Using Media Fill [https://ispe.org/pharmaceutical-engineering/march-april-2022/validation-aseptic-processes-using-media-fill]
- 79. Sterility Testing in the Real World: 5 Uses You'll Actually ... [https://www.linkedin.com/pulse/sterility-testing-real-world-5-uses-zngye/]
- 80. Novel method detects microbial contamination in cell cultures [https://news.mit.edu/2025/novel-method-detects-microbial-contamination-smart-0425]
- 81. Cell Culture Guide - Techniques and Protocols [https://www.assaygenie.com/cell-culture-guide-techniques-and-protocols/?srsltid=AfmBOopSZEbquvPU_k5dXz3b2F7zKGMd-QSfrqrvE5xdcbuvPGym24ah]
- 82. Cell line authentication and validation is a key requirement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181071/]
- 83. Best Practices for Cell Line Authentication [https://cellculturedish.com/best-practices-for-cell-line-authentication/]
- 84. Why the Future of Biological Research Requires Cell Line ... [https://www.psomagen.com/blog/future-of-research-requires-cell-line-authentication]
- 85. Authenticating Cell Lines: Preventing Misidentification and ... [https://www.cytion.com/us/Knowledge-Hub/Blog/Authenticating-Cell-Lines-Preventing-Misidentification-and-Cross-Contamination/]
- 86. Frequently Asked Questions | Cell Line Authentication - Labcorp [https://celllineauthentication.labcorp.com/resources/frequently-asked-questions]
- 87. Authentication of Human Cell Lines Through STR Profiling [https://blog.ansi.org/ansi/authentication-human-cell-lines-str-atcc-asn-0002/]
- 88. Comparing Sterilisation Methods: Autoclaving vs. Chemical ... [https://autoclaveequipment.com/comparing-sterilisation-methods/]
- 89. Why is an Autoclave Better Than a Microwave For ... [https://plantcelltechnology.com/blogs/blog/blogwhy-is-an-autoclave-better-than-a-microwave-for-sterilization?srsltid=AfmBOopCkbIjgWhfOBznL4gjwIaAPun0HQnIWpydkjHzhru-78fXTaQo]
- 90. Cell Harvesting: Methods From Common Cell Culture Media [https://www.akadeum.com/blog/cell-harvesting/?srsltid=AfmBOopNN8hzBi7FFUsGNPRnk6ieYXdUtA9e915K8JIP0lOXoU4_Onnt]
- 91. Cell Harvesting of Biotechnological Processes By Depth ... [https://www.bioprocessintl.com/filtration/cell-harvesting-of-biotechnological-processes-by-depth-filtration]
- 92. Principle, Procedure, Merits, Demerits and Applications of ... [https://www.pharmaguideline.com/2007/02/chemical-methods-of-sterilization.html]
- 93. Table 5: Summary of advantages and disadvantages ... [https://www.cdc.gov/infection-control/hcp/disinfection-and-sterilization/advantages-disadvantages.html]
- 94. Different Types of Autoclaves and their Advantages | TOMY [https://tomy.amuzainc.com/autoclave/types-of-autoclaves-and-their-advantages/]
- 95. Viable cell sorting by fluidized bed centrifugation enables ... [https://pubmed.ncbi.nlm.nih.gov/41036387/]
- 96. 3d Cell Culture Market: Comprehensive Analysis and ... [https://www.pharmiweb.com/press-release/2025-02-12/3d-cell-culture-market-comprehensive-analysis-and-forecast-2025-2035]
- 97. Cell Culture System 2025-2033 Overview [https://www.archivemarketresearch.com/reports/cell-culture-system-545054]
- 98. 3d cell culture market size & share analysis - growth trends ... [https://www.mordorintelligence.com/industry-reports/3d-cell-culture-market]
- 99. Cell culture and maintenance protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 100. Unlocking the Future of Cell Culture System: Growth and ... [https://www.datainsightsmarket.com/reports/cell-culture-system-1728572]
- 101. Cultivated meat microbiological safety considerations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11681928/]