Overcoming Limited Batch Comparability: A Phase-Appropriate Roadmap for Biologics and Advanced Therapies
This article provides a comprehensive guide for researchers and drug development professionals facing the critical challenge of demonstrating product comparability with limited batch numbers.
Overcoming Limited Batch Comparability: A Phase-Appropriate Roadmap for Biologics and Advanced Therapies
Abstract
This article provides a comprehensive guide for researchers and drug development professionals facing the critical challenge of demonstrating product comparability with limited batch numbers. As manufacturing processes for biologics, cell, and gene therapies evolve, changes are inevitable, yet the small batch sizes and inherent variability of these complex products make traditional comparability approaches impractical. This piece explores the foundational principles of a phase-appropriate and risk-based strategy, details methodological frameworks for study design and execution, offers troubleshooting and optimization tactics for real-world constraints, and outlines validation techniques to meet regulatory standards. By synthesizing current regulatory thinking and scientific best practices, this resource aims to equip scientists with the tools to build robust, defensible comparability packages that facilitate continued product development and ensure patient safety.
Understanding the Comparability Imperative: Why Limited Batches Pose a Unique Challenge
For researchers in drug development, demonstrating comparability is a critical regulatory requirement after making a manufacturing change. It is the evidence that ensures the biological product before and after the change is highly similar, with no adverse impact on the product's safety, purity, or potency [1]. The goal is not to prove the two products are identical, but that any differences observed do not affect clinical performance, thereby allowing manufacturers to implement improvements without needing to repeat extensive clinical trials [2] [1].
This guide provides targeted support for the unique challenge of conducting comparability studies with a limited number of batch numbers, where statistical power is low and variability can be a significant concern [2].
Frequently Asked Questions (FAQs) on Comparability
Q1: What is the regulatory basis for demonstrating comparability? The FDA's guidance document, "Demonstration of Comparability of Human Biological Products, Including Therapeutic Biotechnology-derived Products," outlines the framework. It states that for manufacturing changes made prior to product approval, a sponsor can use data from nonclinical and clinical studies on the pre-change product to demonstrate that the post-change product is comparable, potentially avoiding the need for new clinical efficacy studies [1].
Q2: Our team only has 3 batches of the pre-change product. Is this sufficient for a comparability study? While low batch numbers present statistical challenges, they are a common reality in development. Sufficiency depends on the extent and robustness of your analytical data. The focus should be on employing orthogonal analytical methods and leveraging advanced statistical models tailored for small datasets to compensate for the limited numbers and ensure data robustness [2].
Q3: During a TR-FRET assay for potency, we see no assay window. What is the most common cause? The most common reason for a complete lack of assay window is an incorrect instrument setup. We recommend referring to instrument setup guides for your specific microplate reader. Verify that the correct emission filters are being used, as this is critical for TR-FRET assays [3].
Q4: What does a high Z'-factor tell us about our bioassay? The Z'-factor is a key metric for assessing the quality and robustness of an assay. An assay with a Z'-factor greater than 0.5 is considered to have an excellent separation band and is suitable for use in screening. It accounts for both the assay window (the difference between the maximum and minimum signals) and the data variation (standard deviation) [3].
Q5: Why might we see different EC50 values between our lab and a partner's lab using the same compound? A primary reason for differences in EC50 (or IC50) values between labs is often related to differences in the stock solutions prepared by each lab. Ensure consistency in the preparation, handling, and storage of all stock solutions [3].
Troubleshooting Common Experimental Issues
| Issue | Possible Cause | Recommended Solution |
|---|---|---|
| No Assay Window | Incorrect microplate reader setup or emission filters [3]. | Validate instrument setup using recommended guides and confirm filter specifications. |
| High Data Variability | Low batch numbers amplify normal process variability [2]. | Apply orthogonal analytical methods and advanced statistical models for small datasets [2]. |
| Inconsistent Potency Results | Inconsistent stock solution preparation or cell-based assay conditions [3]. | Standardize protocols for stock solutions and validate cell passage numbers and health. |
| Poor Z'-Factor | High signal noise or insufficient assay window [3]. | Optimize reagent concentrations and incubation times. Review protocol for consistency. |
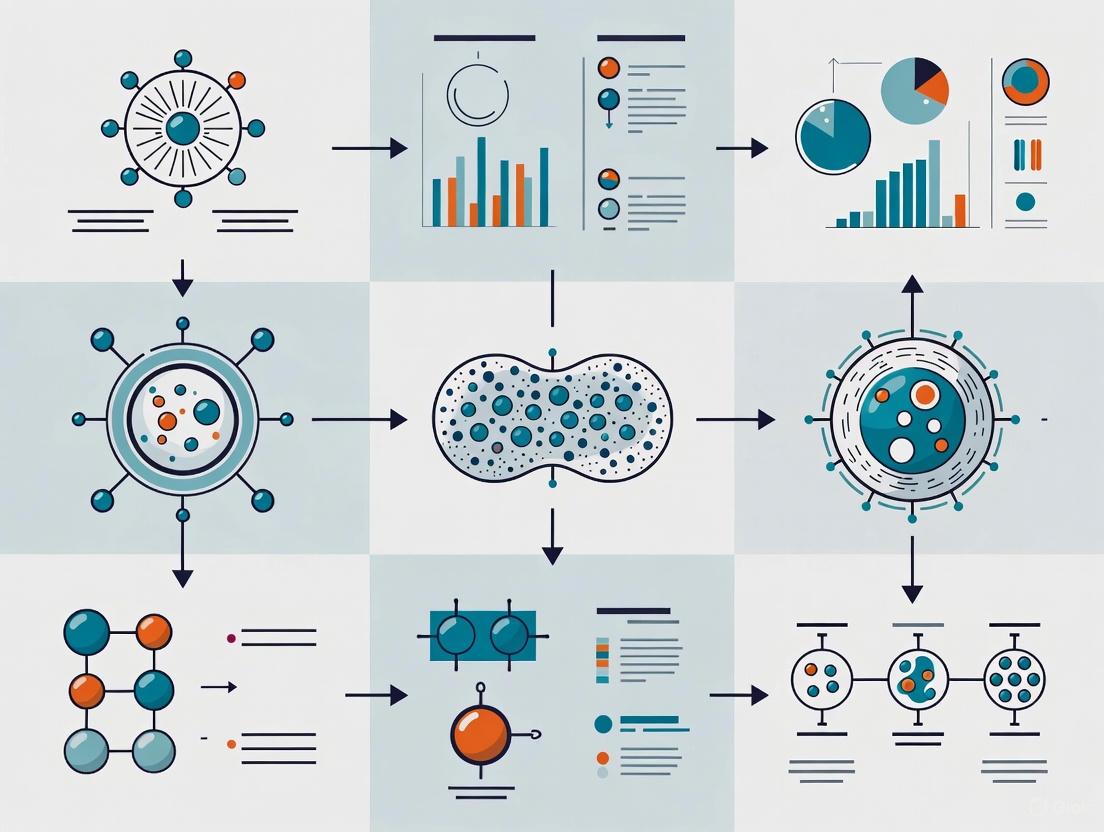
The Comparability Study Workflow
The following diagram outlines a strategic workflow for establishing comparability, emphasizing analytical rigor, especially when batch numbers are limited.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions in conducting robust comparability studies.
| Research Reagent / Material | Function in Comparability Studies |
|---|---|
| Fully Characterized Reference Standards | Serve as a benchmark for side-by-side analysis of pre-change and post-change products; critical for ensuring the consistency of analytical measurements [1]. |
| Orthogonal Analytical Methods | Techniques based on different physical or chemical principles (e.g., SEC, CE-SDS, MS) used together to comprehensively profile product attributes and confirm results [2]. |
| TR-FRET Assay Kits | Used for potency and binding assays; time-resolved fluorescence reduces background noise, providing a robust assay window for comparing biological activity [3]. |
| Validated Cell Lines | Essential for bioassays (e.g., proliferation, reporter gene assays) that measure the biological activity of the product, a key aspect of demonstrating functional comparability. |
| Stable Isotope Labels | Used in advanced mass spectrometry for detailed characterization of post-translational modifications (e.g., glycosylation) that may be critical for function. |
Technical Support & Troubleshooting Hub
This section addresses frequently asked questions and provides guided troubleshooting for researchers navigating the complexities of product development with limited batch numbers.
Frequently Asked Questions (FAQs)
FAQ 1: How can we demonstrate product comparability after a necessary manufacturing process change, especially with high inherent variability in our starting materials?
Demonstrating comparability—proving product equivalence after a process change—is particularly difficult for complex products like cell therapies where "the product is the process" and full characterization is often impossible [4]. To address this:
- Implement a Robust Comparability Protocol: Before any change, establish a detailed, written plan that outlines the tests, studies, analytical procedures, and acceptance criteria to demonstrate that the change does not adversely affect the product's quality, safety, or efficacy [4].
- Focus on Critical Quality Attributes (CQAs): Base your assessment on the physical, chemical, biological, or microbiological properties that are critical to ensuring the desired product quality. Use historical and process development data to set meaningful acceptance criteria [4].
- Leverage Advanced Analytical Tools: Invest in orthogonal analytical methods and potent, mechanism-relevant potency assays that are capable of detecting meaningful quality changes, as these are most critical for assessing comparability [5] [4].
FAQ 2: Our small-batch production for a Phase I clinical trial is plagued by high costs and material loss. What strategies can we employ to improve efficiency?
Small-batch manufacturing for early-stage trials is inherently less cost-efficient and faces challenges like limited material availability and high risk of waste [6].
- Adopt Low-Loss Filling Technologies: Partner with CDMOs that offer filling lines specifically designed for small batches. For example, some innovative fillers can process batches of less than 1L with total product loss under 30 mL, preserving valuable product [7].
- Utilize Single-Use and Modular Systems: Implement single-use technologies and modular manufacturing units to enhance flexibility, reduce cross-contamination risk, and minimize downtime and validation efforts between batches [6].
- Engage a Flexible CDMO: Outsourcing to a specialized Contract Development and Manufacturing Organization (CDMO) can provide access to expert small-batch capabilities, advanced technologies, and shared resources, helping to control costs and mitigate risk [6].
FAQ 3: What is the best approach to manage the complexity that arises from offering a wide variety of product configurations?
Increasing product variety leads to significant complexity in manufacturing and supply chains. Simply counting the number of product variants is an insufficient measure of this complexity [8].
- Quantify Variety-Induced Complexity: Apply metrics from information theory, such as entropy-based measures, to better understand the structural complexity arising from the relations between the portfolio of optional components and the final product variants [8].
- Analyze with a Design Structure Matrix (DSM): Transform your product platform structure into a DSM to map the mutual relationships between functional requirements (product variants) and design parameters (components). This helps identify and manage the core sources of complexity [8].
Troubleshooting Guides
Problem: Inconsistent Product Quality and Potency Between Small Batches
- Potential Cause 1: High variability in starting materials (e.g., donor cells). The variability of starting materials is one of the largest obstacles to consistent manufacturing, impacting both the quality and potency of the final product [5].
- Solution: Implement stronger donor selection and cell source characterization criteria. For critical materials, perform full genomic characterization to provide important safeguards [5].
- Potential Cause 2: Immature or inadequate analytical procedures. The field's analytical technologies are still maturing, making it challenging to reliably assess product consistency [5].
- Solution: Invest early in developing and qualifying analytical tools. Leverage Process Analytical Technology (PAT) for real-time monitoring and control of critical manufacturing steps to ensure consistency [5].
- Potential Cause 3: Manual processes prone to human error. Small-batch production often involves manual operations due to the need for flexibility, which increases the risk of inconsistencies [6].
- Solution: Where possible, introduce automation or mechanization. Automating a manual process enhances repeatability and reduces risk, while mechanization can achieve performance beyond human capability [4].
Problem: Navigating Divergent Global Regulatory Requirements for a Novel Complex Product
- Potential Cause: Lack of global regulatory harmonization. There is an absence of global consensus on definitions, approval pathways, and technical standards for complex products like cell and gene therapies, creating complexity for developers [5].
- Solution:
- Engage Early with Regulators: Seek early and transparent communication with regulatory authorities to anticipate expectations and align development approaches [5].
- Advocate for Regulatory Pilots: Support the creation of "regulatory sandboxes"—controlled environments where regulators and developers can experiment with new assessment methods for manufacturing changes under close supervision [5].
- Utilize Cross-Referencing Tools: Develop a crosswalk (comparison) of expedited pathways across different agencies to identify opportunities for convergence and streamline regulatory planning [5].
- Solution:
The table below consolidates key quantitative challenges and metrics related to managing complex products with small batch sizes.
Table 1: Key Quantitative Data on Complex Product and Small-Batch Challenges
| Category | Metric / Challenge | Data / Context | Source |
|---|---|---|---|
| Product Complexity | Metric for variety-induced complexity | The number of product variants alone is an insufficient measure. Entropy-based metrics and Design Structure Matrix (DSM) analysis are more reliable. | [8] |
| Small-Batch Manufacturing | Acceptable product loss in fill-finish | For batches <1L, specialized low-loss fillers can achieve total product loss (line, filter, transfer) of <30 mL. Batches with a bulk volume as low as 100 mL are feasible. | [7] |
| Drug Development Pipeline | Number of gene therapy drugs in development (2025) | Over 2,000 drugs in development, with only 14 on the market. Highlights the volume of products in early, small-batch phases. | [7] |
| Therapeutic Area Cost Impact | Price reduction of complex generics vs. branded drugs | Complex generics can provide a 40-50% reduction in price compared to their branded counterparts. | [9] |
| Manufacturing Cost Impact | Cost increase due to product variety (automotive industry) | Increased product variety can lead to a total cost increase of up to 20%. | [8] |
Experimental Protocol: Demonstrating Process Comparability After a Manufacturing Change
This protocol provides a detailed methodology for conducting a comparability study following a defined change in the manufacturing process of a complex biological product (e.g., a cell-based therapy).
1. Objective: To generate sufficient evidence to demonstrate that the product manufactured after a process change is highly similar to the pre-change product in terms of quality, safety, and efficacy, with no adverse impact.
2. Pre-Study Requirements:
- Define the Change: Clearly document the nature, scope, and rationale for the manufacturing process change.
- Establish a Comparability Protocol: As per FDA guidance, prepare a pre-approved, detailed plan outlining the tests, studies, analytical procedures, and, most importantly, the pre-defined acceptance criteria [4].
- Risk Assessment: Conduct a risk-based assessment to identify which Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs) are most likely to be impacted by the change [4].
3. Methodology:
- Study Design:
- Arm 1: Product manufactured using the established, pre-change process (Reference).
- Arm 2: Product manufactured using the new, post-change process (Test).
- A minimum of 3 batches per arm is recommended to account for process variability, though this may be adapted for small-batch scenarios.
- Sample Analysis:
- Test both Reference and Test batches against a panel of quality control assays.
- Key Assays to Include:
- Identity/Purity: Flow cytometry, HPLC, etc., as relevant.
- Potency: A biologically relevant assay that reflects the product's mechanism of action. This is considered the most critical assay for comparability [4].
- CQAs: All attributes deemed critical for product quality, safety, and function.
- Data Analysis:
- Compare the Test data against the pre-defined acceptance criteria and the historical data range of the Reference product.
- Use appropriate statistical methods (e.g., equivalence testing) to determine if observed differences are within the justified, acceptable range of variability.
- Any significant differences must be investigated and justified in terms of potential impact on safety and efficacy.
4. Outcome:
- Successful Comparability: If all data meet the pre-defined acceptance criteria, the products are deemed comparable, and the new process can be implemented.
- Failed Comparability: If acceptance criteria are not met, further investigation, process optimization, and potentially additional non-clinical or clinical studies may be required before the change can be approved [4].
Process Visualization: Comparability Assessment Workflow
The following diagram illustrates the logical workflow and decision points in a comparability assessment following a manufacturing change.
The Scientist's Toolkit: Essential Research Reagents & Materials
This table lists key reagents and materials critical for the development and characterization of complex biological products, especially in a small-batch context.
Table 2: Key Research Reagent Solutions for Complex Product Development
| Item | Function / Explanation |
|---|---|
| Good Manufacturing Practice (GMP) Cell Banks | High-quality, well-characterized starting cell banks are foundational. Starting with research-grade plasmids and establishing GMP banks early lays a foundation for faster transitions and cost-effective scaling, improving product consistency [5]. |
| Research-Grade Plasmids | Used in early development and engineering runs to build the data needed to support process changes and scale-up without consuming costly GMP-grade materials [5]. |
| Process Analytical Technology (PAT) Tools | A suite of tools for real-time monitoring and control of critical process parameters during manufacturing. Enables better control over consistency and quality of complex products with inherent variability [5]. |
| Advanced Analytical Assays (e.g., for Potency) | Complex bioassays that measure the biological activity of the product and reflect its mechanism of action. These are the most critical assays for assessing comparability and detecting impactful variations [4]. |
| Single-Use Bioreactors / Manufacturing Components | Disposable equipment used in small-batch manufacturing to enhance flexibility, reduce cleaning validation, and lower the risk of cross-contamination between batches [6]. |
| Modular Manufacturing Platforms | Flexible, scalable production systems that allow for efficient small-batch production and can be adapted quickly to process changes or different product specifications [6]. |
Foundational Concepts: Understanding Comparability and Batch Effects
What is the fundamental principle of ICH Q5E, and why is it critical for biological products?
ICH Q5E provides the framework for assessing comparability of biological products before and after manufacturing process changes. Its fundamental principle is to establish that pre- and post-change products have highly similar quality attributes, and that the manufacturing change does not adversely impact the product's quality, safety, or efficacy [10]. This is particularly critical for biotechnological/biological products due to their inherent complexity and sensitivity to manufacturing process variations.
How do "batch effects" relate to manufacturing process changes in regulatory science?
Batch effects are technical variations introduced due to changes in experimental or manufacturing conditions over time, different equipment, or different processing locations [11]. In the context of manufacturing process changes, these effects represent unwanted technical variations that can confound the assessment of true product quality. If uncorrected, they can lead to misleading conclusions about product comparability, potentially hindering biomedical discovery if over-corrected or creating misleading outcomes if uncorrected [11].
What profound risks do batch effects pose in regulatory decision-making?
Batch effects can act as a paramount factor contributing to irreproducibility, potentially resulting in:
- Retracted articles and invalidated research findings
- Economic losses
- Incorrect classification outcomes affecting patient treatment decisions
- Misleading conclusions about product quality and performance [11]
In one documented case, batch effects from a change in RNA-extraction solution resulted in incorrect classification for 162 patients, 28 of whom received incorrect or unnecessary chemotherapy regimens [11].
Troubleshooting Guides: Addressing Common Scenarios
Troubleshooting Scenario: Limited Batch Numbers in Comparability Studies
Table 1: Troubleshooting Limited Batch Scenarios
| Challenge | Root Cause | Recommended Mitigation Strategy |
|---|---|---|
| Insufficient statistical power | Small sample size (limited batches) | Leverage historical data and controls; employ Bayesian methods |
| Inability to distinguish batch from biological effects | Confounded study design | Implement randomized sample processing; balance experimental groups across batches |
| High technical variability masking true product differences | Minor treatment effect size compared to batch effects | Enhance analytical method precision; implement robust normalization procedures |
| Difficulty determining if detected changes are process-related | Inability to distinguish time/exposure effects from batch artifacts | Incorporate additional control points; use staggered study designs |
Diagnostic Framework: Is a Batch Effect Significant Enough to Require Correction?
When facing potential batch effects in limited batch scenarios, apply this diagnostic workflow:
Experimental Protocol: Batch Effect Assessment in Limited Batch Environments
Objective: Systematically identify and quantify batch effects when batch numbers are limited Materials: Multi-batch dataset, historical controls, appropriate analytical tools
Visual Assessment Phase
- Generate PCA scatterplots coloring samples by batch
- Create hierarchical clustering dendrograms
- Visualize using t-SNE/UMAP projections
Quantitative Assessment Phase
- Apply k-nearest neighbor batch effect test (kBET) to measure local batch mixing
- Calculate average silhouette widths for batch separation
- Perform differential expression analysis between batches
Statistical Decision Phase
- Determine if batch variance exceeds biological variance of interest
- Assess whether batch is confounded with outcome variables
- Evaluate statistical power for batch effect correction
Correction Implementation Phase
- Select appropriate batch effect correction algorithm (BECA)
- Apply chosen correction method
- Validate correction effectiveness using above metrics
Table 2: Batch Effect Correction Algorithms (BECAs) for Different Data Types
| Data Type | Recommended BECAs | Strengths | Limitations |
|---|---|---|---|
| Bulk genomics | ComBat, limma | Established methods, handles small sample sizes | May over-correct with limited batches |
| Single-cell RNA-seq | BERMUDA, scVI, Harmony | Designed for complex single-cell data | Requires substantial cell numbers per batch |
| Proteomics | Combat, SVA adaptations | Handles missing data common in proteomics | Less developed for new proteomics platforms |
| Multi-omics | MDUFA, cross-omics integration | Integrates multiple data types simultaneously | Complex implementation, emerging field |
FAQ: Addressing Common Technical Challenges
How should we approach comparability assessment when we have only 2-3 batches post-manufacturing change?
With limited batches, employ a weight-of-evidence approach combining:
- Extensive characterization using orthogonal analytical methods
- Leveraging historical data and controls as additional reference points
- Implementing advanced statistical methods like Bayesian approaches that can incorporate prior knowledge
- Focusing on critical quality attributes with known clinical relevance
Batch effects in Cell and Gene Therapy (CGT) products commonly arise from:
- Reagent variability: Different lots of fetal bovine serum (FBS), enzymes, growth factors
- Process parameters: Variations in cell culture duration, transduction efficiency, purification methods
- Analytical timing: Differences in sample processing time prior to analysis
- Operator techniques: Different technical staff performing procedures
- Equipment variations: Different instruments or maintenance states
How does the new FDA guidance for CGT products in small populations address limited batch challenges?
The FDA's 2025 draft guidance on "Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations" provides recommendations for:
- Alternative clinical trial designs suitable for small populations
- Innovative endpoint selection strategies
- Generating meaningful clinical evidence despite limited patient numbers
- Leveraging biomarkers and surrogate endpoints
- Using adaptive designs that maximize information from limited data [12]
When should we consider a study redesign rather than statistical batch correction?
Consider study redesign when:
- Batch effects are completely confounded with biological variables of interest
- The number of batches is insufficient for reliable statistical correction
- Batch effects are so substantial they overwhelm biological signals
- Critical control samples are missing across batches
- The cost of incorrect conclusions outweighs the cost of study repetition
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Research Reagent Solutions for Batch Effect Mitigation
| Reagent/ Material | Function | Batch Effect Considerations |
|---|---|---|
| Reference standards | Analytical calibration | Use same lot across all batches; characterize extensively |
| Cell culture media | Support cell growth | Pre-qualify multiple lots; use large lot sizes |
| Fetal bovine serum (FBS) | Cell growth supplement | Pre-test and reserve large batches; document performance |
| Enzymes (e.g., trypsin) | Cell processing | Quality check multiple lots; establish performance criteria |
| Critical reagents | Specific assays | Characterize and reserve sufficient quantities |
| Control samples | Process monitoring | Include in every batch; use well-characterized materials |
| Calibration materials | Instrument performance | Use consistent materials across all experiments |
Advanced Methodologies: Deep Learning Approaches for Batch Effect Correction
Emerging Deep Learning Solutions for Complex Batch Effects
With the advent of more complex data types in CGT development, deep learning approaches are emerging as powerful tools for batch effect correction:
Autoencoder-based Methods: These artificial neural networks learn complex nonlinear projections of high-dimensional data into lower-dimensional embedded spaces representing biological signals while removing technical variations [13].
Transfer Learning Approaches: Methods like BERMUDA use deep transfer learning for single-cell RNA sequencing batch correction, enabling discovery of high-resolution cellular subtypes that might be obscured by batch effects [13].
Integrated Solutions: Newer algorithms simultaneously perform batch effect correction, denoising, and clustering in single-cell transcriptomics, providing comprehensive solutions for complex CGT data [13].
Implementation Workflow for Advanced Batch Effect Correction
Regulatory Strategy: Integrating ICH Q5E with Modern CGT Development
Implementing a Risk-Based Comparability Assessment
For CGT products with limited batch numbers, adopt a risk-based approach that:
- Identifies Critical Quality Attributes (CQAs): Focus on attributes with potential impact on safety and efficacy
- Leverages Orthogonal Methods: Use multiple analytical techniques to compensate for limited batches
- Incorporates Historical Data: Where appropriate, use data from similar products or processes
- Implements Continuous Monitoring: Collect data post-implementation to confirm comparability assessment
Documentation Strategies for Limited Batch Scenarios
When batch numbers are limited, comprehensive documentation becomes critical:
- Detailed rationale for sample size and statistical approaches
- Complete characterization of all materials and reagents
- Thorough investigation of any outliers or unexpected results
- Clear explanation of risk mitigation strategies
- Plan for post-implementation data collection and assessment
By applying these structured troubleshooting approaches, leveraging appropriate technical solutions, and implementing robust regulatory strategies, researchers can successfully navigate comparability assessment challenges even when faced with limited batch scenarios in CGT development.
Troubleshooting Guide: CPP Deviations and CQA Impact
Q: What should I do if my CPPs are in control, but my CQAs are still out of specification?
This indicates that your current control strategy may be incomplete. The measurable CQAs you are monitoring might not be fully predictive of the product's true quality and biological activity [14].
- Investigate Unmeasured CQAs: The product's critical quality may be defined by attributes you are not currently measuring. Re-evaluate the product's Mechanism of Action (MOA) to identify potential CQAs that your assays are not capturing [15] [14].
- Challange Your Potency Assay: A poorly correlated or insensitive potency assay is a common culprit. The FDA has issued complete response letters specifically due to a lack of scientific rationale linking potency measurements to biological activity [14]. Develop a matrix of candidate potency assays that reflect the intended MOA[s [15].
- Review Your Process Parameters: A CPP you have not identified as critical may be affecting an unmeasured CQA. Deepen your process understanding through risk assessment and additional design of experiments (DoE) studies [16] [17].
Q: How can I demonstrate comparability with a very limited number of batches?
Limited batch numbers are a common challenge in cell and gene therapy. A successful strategy involves leveraging strong scientific rationale and proactive planning [15].
- Adopt a Prospective Approach: Where possible, plan manufacturing changes and generate "split-stream" data by running the old and new processes side-by-side, even with a small number of batches. This is often more robust than retrospective comparison [15].
- Focus on a Science-Driven Narrative: Use existing knowledge of your product's CQAs, MOA, and process to build a strong comparability narrative. Regulators expect a data-driven, scientifically justified proposal [15].
- Utilize All Available Data: Incorporate data from all stages of development. Even data from research or non-clinical batches can help establish a baseline for variability and support your narrative [15].
- Employ Statistical Science: Choose statistical methods wisely. For small sample sizes, equivalence testing with pre-defined acceptance criteria based on biological relevance is often more appropriate than tests relying solely on statistical power [15].
Frequently Asked Questions (FAQs)
Q: What is the fundamental relationship between a CPP and a CQA? A critical process parameter (CPP) is a variable process input (e.g., temperature, pH) that has a direct impact on a critical quality attribute (CQA) [16] [18] [17]. A CQA is a physical, chemical, biological, or microbiological property (e.g., potency, purity) that must be controlled to ensure product quality [14] [17]. Controlling CPPs within predefined limits is how you ensure CQAs meet their specifications [17].
Q: Are CQAs fixed throughout the product lifecycle? No. CQAs are not always fully known at the start of development and are typically refined as product and process knowledge increases [14]. As you gain a better understanding of the product's Mechanism of Action (MOA) through clinical trials, you can refine your CQAs, particularly your potency assays, to ensure they are truly predictive of clinical efficacy [15] [14].
Q: What is the role of Quality Assurance (QA) in managing CPPs and CQAs? Quality Assurance (QA) has an oversight role to ensure that CPPs and CQAs are properly identified, justified, and controlled [17]. QA reviews and approves the risk assessments, process validation protocols, and control strategies related to CPPs and CQAs. They also ensure deviations are investigated and that corrective actions are effective [17].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions in developing and controlling a bioprocess, particularly for complex modalities like cell and gene therapies.
| Reagent / Material | Function in Experimentation |
|---|---|
| Bioprocess Sensors (pH, DO, pCO₂) [16] | In-line or on-line monitoring of Critical Process Parameters (CPPs) in real-time within bioreactors to ensure process control [16]. |
| Potency Assay Reagents [15] [14] | Used to develop and run bioassays that measure the biological activity of the product, which is a crucial CQA linked to the mechanism of action [15] [14]. |
| Cell Culture Media & Supplements [14] | Provides the nutrients and environment for cell growth and production. Their quality and composition are vital raw materials that can impact both CPPs and CQAs [14]. |
| Surface Marker Antibodies [14] | Used in flow cytometry to monitor cell identity and purity, which are common CQAs for cell therapy products like MSCs [14]. |
| Differentiation Induction Kits (e.g., trilineage) [14] | Used to assess the differentiation potential of stem cells, a standard functional CQA for certain cell therapies [14]. |
Experimental Protocol: Designing a Comparability Study
Objective: To demonstrate that a product manufactured after a process change (e.g., scale-up, raw material change) is highly similar to the product from the prior process, with no adverse impact on safety or efficacy [15].
Methodology:
Define Scope & Risk Assessment:
- Clearly describe the manufacturing change.
- Perform a risk assessment to identify which CQAs and CPPs have a high likelihood of being impacted by the change [15].
Develop a Study Protocol:
Execute Analytical Testing:
- Test pre-change and post-change batches for a comprehensive panel of CQAs. ICH Q5E recommends testing for identity, purity, potency, and safety [15].
- A side-by-side (split-stream) analysis is preferred over a retrospective comparison [15].
- Key Focus on Potency: Employ a potency assay that is relevant to the product's known or postulated MOA. The assay should be able to detect differences in biological activity [15] [14].
Data Analysis & Statistical Evaluation:
- Use statistical methods appropriate for the data set and sample size. The goal is to show "comparability" and not just "no significant difference," which can be a function of low statistical power [15].
- Determine if any observed differences are statistically significant and, more importantly, biologically relevant [15].
Prepare the Comparability Report:
- Document all data and the scientific rationale concluding that the products are comparable. The report should tell a clear story for regulator review [15].
CQA and CPP Relationships Across the Product Lifecycle
The table below summarizes how the focus on CQAs and CPPs evolves from early development to commercial manufacturing.
| Product Lifecycle Stage | CQA Focus | CPP Focus |
|---|---|---|
| Early Development (Pre-clinical, Phase 1) | • Identification of potential CQAs based on limited MOA knowledge and literature [14].• Use of general, often non-specific, potency assays [14]. | • Identification of key process parameters through initial experimentation (DoE) [16].• Establishing initial, wide control ranges. |
| Late-Stage Development (Phase 2, Phase 3) | • Refinement of CQAs, especially potency, based on clinical data [15] [14].• Linking CQAs to clinical efficacy. | • Narrowing of CPP operating ranges based on increased process understanding [16].• Process validation to demonstrate consistent control of CPPs. |
| Commercial Manufacturing | • Ongoing monitoring of validated CQAs to ensure consistent product quality [18]. | • Strict control of CPPs within validated ranges to ensure the process remains in a state of control [17]. |
Process Control and Quality Relationship
Comparability Study Workflow
Frequently Asked Questions: Troubleshooting Batch Variability
Q1: Our bioequivalence (BE) study failed because the Reference product batches were not equivalent. What went wrong? This is a documented phenomenon. A randomized clinical trial demonstrated that different batches of the same commercially available product (Advair Diskus 100/50) can fail the standard pharmacokinetic (PK) BE test when compared to each other. In one study, all pairwise comparisons between three different batches failed the statistical test for bioequivalence, showing that batch-to-batch variability can be a substantial component of total variability [19] [20].
Q2: Why is this a critical problem for generic drug development? The current regulatory framework for BE studies typically assumes that a single batch can adequately represent an entire product. When substantial batch-to-batch variability exists, the result of a standard BE study becomes highly dependent on the specific batches chosen for the Test (T) and Reference (R) products. This means a study might show bioequivalence with one set of batches but fail with another, making the result unreliable and not generalizable [19] [21].
Q3: What is the core statistical issue? In standard single-batch BE studies, the uncertainty in the T/R ratio estimate does not account for the additional variability introduced by sampling different batches. The 90% confidence interval constructed in the analysis only reflects within-subject residual error and ignores the variance between batches. When batch-to-batch variability is high, this leads to an artificially narrow confidence interval that overstates the certainty of the result [19] [21].
Q4: Are there study designs that can mitigate this problem? Yes, researchers have proposed multiple-batch approaches. Instead of using a single batch for each product, several batches are incorporated into the study design. The statistical analysis can then be adapted to account for batch variability, for instance by treating the "batch" effect as a random factor in the statistical model, which provides a more generalizable conclusion about the products themselves [21].
Q5: For which types of drugs is this most problematic? Batch-to-batch variability poses significant challenges for the development of generic orally inhaled drug products (OIDPs), such as dry powder inhalers (DPIs). The complex interplay between formulation, device, and manufacturing processes for these locally acting drugs can lead to PK variability between batches, complicating BE assessments [20] [21].
Technical Troubleshooting Guide: Methodologies for Limited Batch Research
When your research is confounded by limited batch comparability, the following experimental protocols and methodologies can provide more robust conclusions.
1. Protocol: Multiple-Batch Pharmacokinetic Bioequivalence Study
This design incorporates multiple batches directly into the clinical study to improve the reliability of the BE assessment without necessarily increasing the number of human subjects [21].
- Objective: To determine bioequivalence between Test (T) and Reference (R) products while accounting for batch-to-batch variability.
- Study Design: A two-period, randomized crossover design arranged in cohorts.
- Subjects are divided into
ccohorts. - Each cohort receives a single, unique batch of T and a single, unique batch of R in random order (TR or RT).
- Different cohorts receive different batches of T and R.
- The total number of batches assessed per product is equal to the number of cohorts (
c) [21].
- Subjects are divided into
- Key Parameters:
c: Number of cohorts (and batches per product)m: Number of subjects per sequence per cohort- Total subjects,
N=2 * m * c
- Statistical Analysis Models: The performance and interpretation depend on how batch effects are handled in the analysis of variance (ANOVA) [21]:
| Approach | Description | Statistical Question | Handles Batch Sampling Uncertainty? |
|---|---|---|---|
| Random Batch Effect | Batch included as a random factor in the ANOVA. | Are the T and R products bioequivalent? | Yes |
| Fixed Batch Effect | Batch included as a fixed factor in the ANOVA. | Are the selected T batches bioequivalent to the selected R batches? | No |
| Superbatch | Data from multiple batches are pooled; batch identity is ignored in ANOVA. | Are the selected T batches bioequivalent to the selected R batches? | No |
| Targeted Batch | An in vitro test is used to select a median batch of each product for a standard BE study. | Are the selected T batches bioequivalent to the selected R batches? | No |
The following workflow illustrates the decision process for selecting and implementing these methodologies:
2. Quantitative Data on Batch-to-Batch Variability
The following table summarizes key PK data from a clinical study that investigated three different batches of Advair Diskus 100/50, with one batch (Batch 1) replicated. The data illustrate the magnitude of variability that can exist between batches of a marketed product [19].
Table 1: Pharmacokinetic Data Demonstrating Batch-to-Batch Variability for Advair Diskus 100/50 (FP) [19]
| PK Parameter | Batch 1 - Replicate A | Batch 1 - Replicate B | Batch 2 | Batch 3 |
|---|---|---|---|---|
| Cmax (pg/mL) | 44.7 | 45.4 | 69.2 | 58.9 |
| AUC(0-t) (h·pg/mL) | 178 | 177 | 230 | 220 |
- Key Finding: The replicated batch (A vs. B) showed consistent results, confirming the study's precision. However, Batches 2 and 3 showed notably higher systemic exposure (Cmax and AUC) compared to Batch 1, with differences large enough to cause bio-inequivalence in a standard BE test [19]. The between-batch variance was estimated to be ~40–70% of the total residual error [19].
The Scientist's Toolkit: Key Research Reagent Solutions
When designing studies to address batch variability, the following statistical and methodological "reagents" are essential.
Table 2: Essential Materials and Methods for Batch Variability Research
| Item | Function/Description | Key Consideration |
|---|---|---|
| Replicate Crossover Design | A study design where the same formulation (often the Reference) is administered to subjects more than once. | Allows for direct estimation of within-subject, within-batch variability and provides more data points without increasing subject numbers [22] [23]. |
| Statistical Assurance Concept | A sample size calculation method that integrates the power of a trial over a distribution of potential T/R-ratios (θ), rather than a single assumed value. | Provides a more realistic "probability of success" by formally accounting for uncertainty about the true T/R-ratio before the trial [24]. |
| Batch Effect Adjustment Methods | Statistical techniques (e.g., using the batchtma R package) to adjust for non-biological variation introduced by different batches or processing groups. |
Critical for retaining "true" biological differences between batches while removing technical artifacts. The choice of method (e.g., simple means, quantile regression) depends on the data structure and goals [25]. |
| In Vitro Bio-Predictive Tests | Physicochemical tests (e.g., aerodynamic particle size distribution) used to screen batches and select representative ones for clinical studies. | A well-established in vitro-in vivo correlation (IVIVC) is required for this approach to be valid and predictive of clinical performance [20] [21]. |
Building Your Comparability Protocol: A Phase-Appropriate and Risk-Based Blueprint
Crafting a Prospective Study Protocol with Predefined Acceptance Criteria
Technical Support Center
Troubleshooting Guides and FAQs
FAQ 1: Why is a prospective comparability study design recommended over a retrospective one?
A prospective study is designed before implementing a manufacturing change. Participants are identified and observed over time to see how outcomes develop, establishing a temporal relationship between exposures and outcomes [26]. In comparability research, a prospective design is recommended because it de-risks delays in clinical development. It typically involves split-stream and side-by-side analyses of material from the old and new processes. While it may require more resources, it does not typically require formal statistical powering, unlike retrospective studies [15].
FAQ 2: What are the most critical elements to define in a prospective comparability protocol?
Your protocol should clearly define the following elements before initiating the study:
- Analytical Methods: A matrix of candidate potency assays that reflect the product's mechanism of action (MOA) is critical [15].
- Critical Quality Attributes (CQAs): Identity, strength, purity, and potency should be assessed [15].
- Predefined Acceptance Criteria: Establish quality ranges or equivalence ranges for each attribute, ensuring they are tied to biological meaning and not just statistical significance [15].
- Statistical Approach: The choice of statistical methods (e.g., quality range vs. equivalence testing) must consider data normality, paired/unpaired analysis, and statistical power [15].
FAQ 3: Our study yielded a statistically significant difference. Does this mean the processes are not comparable?
Not necessarily. A key principle is that statistically significant differences may not be biologically meaningful. The clinical impact of the difference must be evaluated. Your acceptance criteria should be based on a risk assessment that determines the likelihood of an impact on product safety and effectiveness. The finding necessitates a thorough, science-driven investigation to determine the true impact of the change [15].
FAQ 4: What is the primary cause of irreproducibility in comparability studies, and how can it be avoided?
Batch effects are a paramount factor contributing to irreproducibility. These are technical variations introduced due to changes in experimental conditions, reagents, or equipment over time [27]. To avoid them:
- Plan Proactively: Save sufficient product retains throughout development to support future analytical testing [15].
- Control Reagents: Be aware that reagent variability (e.g., different batches of fetal bovine serum) can invalidate results [27].
- Use Correction Methods: In omics data, employ batch effect correction algorithms (BECAs), especially when sample size is sufficient (e.g., including principal components in linear models) [28].
Common Experiment Discrepancies and Resolutions
| Issue | Possible Cause | Resolution |
|---|---|---|
| Inability to establish comparability | Flawed study design; confounded batch effects; insufficient statistical power [27]. | Perform a proactive risk assessment; ensure sufficient sample size and use a prospective design; correct for known batch effects [15] [27]. |
| Statistically significant but biologically irrelevant difference | Acceptance criteria based solely on statistical power without linkage to biological relevance [15]. | Base acceptance criteria for each attribute on biological meaning and a science-driven risk assessment [15]. |
| Inability to reproduce key results | Changes in reagent batches or other uncontrolled technical variations (batch effects) [27]. | Implement careful experimental design to minimize batch effects; use retains from previous product batches for side-by-side testing [15] [27]. |
| High variability in potency assay | Potency assay not sufficiently robust or not reflective of the MOA [15]. | Invest early in developing a matrix of candidate potency assays; select the most robust one for the final specification [15]. |
Detailed Experimental Protocol for a Prospective Comparability Study
Objective: To demonstrate the comparability of a cellular or gene therapy product before and after a specific manufacturing process change.
Methodology: This is a prospective, side-by-side analysis of multiple batches produced from the old (original) and new (changed) manufacturing processes.
Workflow:
- Risk Assessment: Identify potential impacts of the manufacturing change on product CQAs, safety, and efficacy [15].
- Protocol Finalization: Define the specific CQAs, analytical methods, statistical approach, and predefined acceptance criteria [15].
- Batch Manufacturing: Generate a sufficient number of batches (N) using both the old and new processes.
- Side-by-Side Testing: Analyze all batches using the battery of methods defined in the protocol. Testing should include, but is not limited to, the assays listed in the table below.
- Data Analysis: Compare the data from the new process batches against the predefined acceptance criteria, which are often derived from the historical data of the old process [15].
- Conclusion: Determine if the data demonstrate comparability or if further investigation or process optimization is required.
Key Experiments and Analytical Methods
The table below summarizes the essential quality attributes and examples of methods used to assess them in a comparability study [15].
| Critical Quality Attribute (CQA) | Example Analytical Methods | Function in Comparability Assessment |
|---|---|---|
| Identity | Flow cytometry, PCR, Immunoassay | Confirms the presence of the correct therapeutic entity (e.g., cell surface markers, transgene). |
| Potency | Cell-based bioassay, Cytokine secretion assay, Enzymatic activity assay | Measures the biological activity linked to the product's Mechanism of Action (MOA); considered a critical component. |
| Purity/Impurities | Viability assays, Endotoxin testing, Residual host cell protein/DNA analysis | Determines the proportion of active product and identifies/quantifies process-related impurities. |
| Strength (Titer & Viability) | Cell counting, Vector genome titer, Infectivity assays | Quantifies the amount of active product per unit (e.g., viable cells per vial, vector genomes per mL). |
Visual Workflow: Prospective Comparability Study
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in Comparability Research |
|---|---|
| Reference Standard | A well-characterized batch of the product used as a biological benchmark for all comparative assays to ensure consistency and accuracy [15]. |
| Characterized Cell Banks | Master and Working Cell Banks with defined characteristics ensure a consistent and reproducible source of cells, minimizing upstream variability [15]. |
| Critical Reagents | Key antibodies, enzymes, growth factors, and culture media. Their quality and consistency are vital; batch-to-batch variations can introduce significant batch effects [27]. |
| Validated Assay Kits/Components | Analytical test kits (e.g., for potency, impurities) that have been validated for robustness, accuracy, and precision to reliably detect differences between products [15]. |
Troubleshooting Guides & FAQs
FAQ: Managing Limited Batch Numbers
Q1: With only 2-3 early-stage batches available, which analytical techniques provide the most meaningful comparability data? A1: For limited batches (n=2-3), prioritize Orthogonal Multi-Attribute Monitoring:
- Intact Mass Analysis (MS): Confirms primary structure
- Peptide Mapping (LC-MS/MS): Identifies post-translational modifications
- Size Exclusion Chromatography (SEC-HPLC): Quantifies aggregates and fragments
- Ion Exchange Chromatography (IEX-HPLC): Assesses charge variants These techniques provide a multi-dimensional comparability assessment with high information yield per batch.
Q2: How do we determine if observed analytical differences are significant when we have low statistical power? A2: Implement a Tiered System for data evaluation:
- Tier 1 (Quality Ranges): For critical quality attributes (CQAs) with known clinical impact
- Tier 2 (Acceptance Criteria): For attributes with potential impact
- Tier 3 (Descriptive): For characterization attributes
Table: Tiered Approach for Limited Batch Comparison
| Tier | Attribute Type | Statistical Approach | Acceptance Criteria |
|---|---|---|---|
| 1 | CQAs with clinical impact | ±3σ of historical data | Tight, based on safety margins |
| 2 | Potential impact | ±3σ or % difference | Moderate, process capability |
| 3 | Characterization | Visual comparison | Qualitative assessment |
FAQ: Method Transitions
Q3: When transitioning from research-grade to GMP-compliant methods, how do we maintain comparability with limited data? A3: Execute a Method Bridging Study:
- Analyze the same 2-3 batches with both old and new methods
- Establish correlation coefficients for key attributes
- Define equivalence margins based on method precision
- Document any systematic biases for future reference
Table: Method Bridging Acceptance Criteria
| Parameter | Minimum Requirement | Target Criteria |
|---|---|---|
| Correlation (r) | >0.90 | >0.95 |
| Slope of regression | 0.80-1.25 | 0.90-1.10 |
| % Difference in means | <15% | <10% |
Experimental Protocols
Protocol 1: Accelerated Stability for Comparability
Purpose: Assess comparability of stability profiles with limited batches.
Materials:
- Test articles: 2-3 batches each of reference and test material
- Storage conditions: 5°C, 25°C/60% RH, 40°C/75% RH
- Timepoints: 0, 1, 3, 6 months
Methodology:
- Prepare aliquots for each timepoint/condition combination
- Store samples in controlled stability chambers
- At each timepoint, analyze using the orthogonal methods from FAQ A1
- Calculate degradation rates and compare between batches using pairwise statistics
Analysis:
- Plot degradation profiles for each CQA
- Calculate similarity of slopes using equivalence testing
- Establish 90% confidence intervals for differences
Protocol 2: Forced Degradation Study
Purpose: Compare degradation pathways with limited batches.
Stress Conditions:
- Thermal: 40°C for 1 month
- Oxidative: 0.01% H₂O₂, 25°C, 24h
- pH: pH 3 and pH 9, 25°C, 1 week
- Mechanical: Vortexing and freeze-thaw cycles
Analysis:
- Monitor formation of degradation products
- Compare degradation profiles using principal component analysis (PCA)
- Assess qualitative and quantitative differences in degradation pathways
Visualizations
Early-Phase Comparability Workflow
Late-Phase Comprehensive Strategy
Comparability Decision Framework
The Scientist's Toolkit
Table: Essential Research Reagents for Comparability Studies
| Reagent/Material | Function | Phase-Appropriate Application |
|---|---|---|
| Reference Standard | Benchmark for comparison | All phases - qualification level varies |
| Orthogonal LC Columns | Separation mechanism diversity | Early: 2-3 methods; Late: 4-5 methods |
| MS Calibration Standards | Mass accuracy verification | Critical for peptide mapping and intact mass |
| Forced Degradation Reagents | Stress testing agents | Early: limited stresses; Late: comprehensive |
| Stability Indicating Assay Kits | Rapid stability assessment | Early: screening; Late: validated methods |
| Process-Related Impurity Standards | Specific impurity detection | Late-phase comprehensive assessment |
| Biological Activity Assay Reagents | Functional assessment | Early: binding assays; Late: potency assays |
Troubleshooting Guides and FAQs
Q: How do we prioritize risks when we only have data from a very limited number of batches for our comparability study?
A: A structured risk assessment is crucial. Begin with a qualitative analysis to quickly identify which process changes pose the highest risk to product quality, safety, and efficacy. For these high-priority risks, you can then apply a semi-quantitative approach to standardize scoring and justify your focus, even with limited data [29]. The initial risk assessment should directly determine the scope and depth of your comparability study [30].
Q: What is the practical difference between qualitative and quantitative risk assessment methods in this context?
A: The choice significantly impacts the defensibility of your decisions with limited batches:
- Qualitative Risk Analysis is scenario-based and uses scales like "High/Medium/Low" for probability and impact. It is quick to implement and ideal for initial, broad screening of risks when data is sparse [31].
- Quantitative Risk Analysis uses objective numerical values and measurable data. It is more rigorous but requires high-quality data, which may not be available with a small number of batches. It is best reserved for high-priority risks where you need to justify investments in controls [31]. A semi-quantitative approach can offer a middle ground [29].
Q: For a major process change like a cell line change, what is the recommended number of batches, and how can we defend using fewer?
A: For a major change, ≥3 batches of commercial-scale post-change product are generally recommended. To justify a smaller number, you must provide a scientifically sound rationale based on a risk assessment. This can include leveraging prior knowledge of process robustness, using a bracketing or matrix approach, or presenting data from a well-justified small-scale model [30].
Q: How do we set meaningful acceptance criteria for comparability studies with limited historical data?
A: Establish prospective acceptance criteria based on all available historical data for the pre-change product. These criteria do not have to be your final quality standards but must be justified. For quantitative methods, the criteria must be a defined range. For qualitative methods, like chromatographic peak shapes, the criteria should be based on a direct comparison to pre-change profiles, demonstrating highly similar patterns and the absence of new variants [30].
Quantitative Risk Analysis Data
Table 1: Key Quantitative Risk Analysis Formulas and Values [31]
| Term | Description | Formula | Application in Comparability |
|---|---|---|---|
| Single Loss Expectancy (SLE) | Monetary loss expected from a single risk incident. | SLE = Asset Value × Exposure Factor |
Estimates financial impact of a single batch failure due to a process change. |
| Annual Rate of Occurrence (ARO) | Number of times a risk is expected to occur per year. | ARO is estimated from historical data or vendor statistics. | For a new process, this may be based on reliability data for new equipment or systems. |
| Annual Loss Expectancy (ALE) | Expected monetary loss per year due to a risk. | ALE = SLE × ARO |
Used for cost-benefit analysis of implementing a new control or mitigation strategy. |
Table 2: Comparability Study Batch Requirements Based on Risk [30]
| Type of Process Change | Comparability Risk Level | Recommended Number of Post-Change Batches |
|---|---|---|
| Production site transfer | Low | ≥1 batch (Release testing, accelerated stability) |
| Site transfer with minor process changes | Low-Medium | ≥3 batches (Transfer all assays, add functional tests) |
| Changes in culture or purification methods | Medium | 3 batches (May require additional non-clinical PK/PD studies) |
| Cell line changes | Medium-High | ≥3 batches (May require GLP toxicology and human bridging studies) |
Experimental Protocols for Key Analyses
Protocol: Primary Structure Analysis via Peptide Mapping
- Objective: To confirm that the amino acid sequence and post-translational modifications are highly similar before and after the process change.
- Methodology:
- Sample Preparation: Digest the protein from both pre-change and post-change batches with a specific enzyme (e.g., trypsin).
- Analysis: Separate the resulting peptides using Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) coupled with Mass Spectrometry (LC-MS).
- Acceptance Criteria: The peptide maps should confirm the primary structure. The profiles must have comparable peak shapes based on retention time and relative intensity. There should be no new or lost peaks in the post-change batch [30].
Protocol: Purity and Impurity Analysis via Size-Exclusion Chromatography (SEC-HPLC)
- Objective: To quantify and compare the levels of aggregates, monomers, and fragments.
- Methodology:
- Sample Preparation: Prepare formulations of the pre-change and post-change products under non-denaturing conditions.
- Analysis: Inject samples onto an SEC-HPLC column to separate species by molecular size.
- Acceptance Criteria: The percentage of the main peak (monomer) should be within statistically derived acceptance criteria. The aggregate, monomer, and fragment peaks should have the same retention times. The profile should show no new species [30].
Risk Assessment and Comparability Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Biologics Comparability Studies
| Research Reagent | Function in Comparability Studies |
|---|---|
| Trypsin (Sequencing Grade) | Enzyme used in peptide mapping to digest the protein for primary structure confirmation by LC-MS [30]. |
| Reference Standard | A well-characterized sample of the pre-change product used as a benchmark for all head-to-head analytical comparisons [30]. |
| Cell-Based Assay Reagents | Includes cells, cytokines, and substrates used in potency assays (e.g., ADCC) to demonstrate functional comparability [30]. |
| SEC-HPLC Molecular Weight Standards | Used to calibrate the Size-Exclusion Chromatography system for accurate analysis of aggregates and fragments [30]. |
| Ion-Exchange Chromatography Buffers | Critical for characterizing charge variants of the protein, which can impact stability and biological activity [30]. |
FAQs on Extended Characterization for Comparability
1. Why is extended characterization critical for comparability studies with limited batches?
Extended characterization provides a deeper, more granular understanding of a molecule's quality attributes than routine release testing [32]. When batch numbers are limited, this orthogonal approach is essential to maximize the information gained from each batch. It helps demonstrate that despite process changes, the molecule's critical quality attributes (CQAs) affecting safety and efficacy remain highly similar, strengthening the scientific evidence for comparability [32] [33].
2. What are the key differences between release testing and extended characterization?
The table below summarizes the core differences:
| Feature | Release Testing | Extended Characterization |
|---|---|---|
| Purpose | Verify a batch meets pre-defined specifications for lot release [34] | Gain deep molecular understanding for comparability assessments [32] |
| Scope | Focuses on strength, identity, purity, quality (SISPQ) [34] | Orthogonal, in-depth analysis of structure, function, and stability [32] |
| Methods | Validated, routine methods [34] | Platform and molecule-specific methods, including forced degradation studies [34] [32] |
| Frequency | Performed on every batch [34] | Performed at specific development milestones or for comparability [32] |
3. How can we design a phase-appropriate comparability study with few batches?
The strategy should be risk-based and phase-appropriate. In early development, comparability can often be established using single pre- and post-change batches analyzed with platform methods [32]. As development advances toward commercial filing, the standard is a more rigorous, multi-batch comparison (e.g., 3 pre-change vs. 3 post-change) [32]. The key is to focus the testing on CQAs most likely to be impacted by the specific process change [33].
4. What are common CQAs revealed by extended characterization?
Recombinant monoclonal antibodies are complex and heterogeneous. The table below lists key CQAs often investigated during extended characterization [33]:
| Critical Quality Attribute (CQA) | Potential Impact on Product |
|---|---|
| N-terminal Modifications (e.g., pyroglutamate) | Generally low risk; forms charge variants [33] |
| C-terminal Modifications (e.g., lysine truncation) | Generally low risk; forms charge variants [33] |
| Fc-glycosylation (e.g., afucosylation, high mannose) | Can impact effector functions (ADCC) and half-life [33] |
| Charge Variants (e.g., deamidation, isomerization) | Can decrease potency if located in Complementarity-Determining Regions (CDRs) [33] |
| Oxidation (e.g., of Methionine, Tryptophan) | Can decrease potency and stability; may impact half-life [33] |
| Aggregation | High risk for immunogenicity; loss of efficacy [33] |
5. How do forced degradation studies strengthen a comparability package?
Forced degradation studies "pressure-test" the molecule under stressed conditions (e.g., heat, light, acidic pH) to intentionally degrade it [32]. Comparing the degradation profiles of pre- and post-change batches is a powerful way to show that the molecular integrity and degradation pathways are highly similar, revealing differences not always visible in real-time stability studies [32].
Troubleshooting Guides
Issue 1: Inconclusive Comparability Results with Limited Batches
Problem Description After a process change, analytical data from limited batches (e.g., 1 pre-change vs. 1 post-change) shows minor but statistically significant differences in some quality attributes. It is unclear if these differences impact safety or efficacy, potentially blocking regulatory progression.
Impact Drug development timeline is delayed, and additional non-clinical or clinical studies may be required, increasing costs significantly [33].
Context This often occurs during late-stage development when process changes are scaled up. The risk is higher when the historical data for the attribute is limited and the acceptance criteria are not well-established.
Solution Architecture
Quick Fix (Immediate Action)
- Risk Assessment: Immediately convene a cross-functional team to perform a risk assessment based on the structure-function relationship of the attribute in question [33].
- Method Suitability: Verify the analytical method's performance using a qualified reference standard to ensure data reliability [34].
Standard Resolution (Root Cause Investigation)
- Expand Characterization: Perform extended characterization on the available batches, focusing on the specific attribute and its variants. Use orthogonal methods (e.g., LC-MS for charge variants) to gain a deeper understanding [32].
- Forced Degradation: Subject both batches to forced degradation studies. Similar degradation patterns and rates can provide strong evidence that the molecule's stability and intrinsic properties are comparable, even if initial values differ [32].
- Leverage Platform Knowledge: Use prior knowledge about the molecule class (e.g., common mAb modifications) to justify whether the observed difference is likely to have a clinical impact [34] [33].
Long-Term Strategy (Process Improvement)
- Enhanced Control Strategy: If the difference is confirmed and considered a low risk, justify it to regulators and implement it as part of the updated control strategy for the post-change process.
- Build Historical Data: As more post-change batches are manufactured, incorporate their data to build a new historical data set and refine acceptance criteria.
Issue 2: Failing System Suitability with Platform Methods
Problem Description A platform analytical method, used for years across multiple products, is failing system suitability when testing a new molecule, halting characterization work.
Impact Unable to generate reliable data for comparability assessment. Investigation and method re-development or re-validation can take weeks and cost $50,000-$100,000 [34].
Context Platform methods are designed for molecules with structural similarities but can fail due to unique characteristics of a new molecule or a specific process-related variant.
Solution Architecture
Quick Fix (Restart Testing)
- Use Qualified Reference Standards: Employ a well-characterized, system-suitability standard, such as those from USP, to confirm the instrument and method performance are functioning as intended [34].
- Re-prepare Samples: Re-prepare mobile phases and sample solutions to rule out preparation errors.
Standard Resolution (Identify Cause)
- Troubleshoot the Method: Isolate the cause of failure. Check for column degradation, instrument performance, and buffer pH. Minor adjustments to the method (e.g., gradient, pH) may be sufficient.
- Analyze the Molecule: Investigate if a unique attribute of the molecule (e.g., a specific charge variant or aggregation profile) is interfering with the method. This may require data from other characterization techniques.
Long-Term Strategy (Ensure Robustness)
- Method Optimization or Adaptation: If the platform method is not suitable, optimize it for the new molecule. Using a compendial method (e.g., from USP-NF) as a starting point can save time and cost compared to full in-house development [34].
- Document the Justification: Thoroughly document the investigation and any method modifications, providing a scientific rationale for the changes to ensure regulatory compliance.
Experimental Protocols & Workflows
Protocol 1: Forced Degradation Study for Comparability
Objective: To compare the degradation profiles of pre- and post-change monoclonal antibody batches under stressed conditions to demonstrate similarity in stability behavior [32].
Materials:
- Research Reagent Solutions:
- mAb Samples: Pre-change and post-change drug substance.
- Buffers: Various pH buffers (e.g., pH 3, 5, 9).
- Oxidizing Agent: 0.1% hydrogen peroxide (H₂O₂).
- Control Buffer: Histidine or phosphate buffer at formulation pH.
Methodology:
- Sample Preparation:
- Dialyze all mAb samples into a common, appropriate control buffer.
- Concentrate to the desired protein concentration (e.g., 1-10 mg/mL).
- Stress Conditions:
- Thermal Stress: Incubate samples at 40°C for 1-4 weeks.
- Agitation Stress: Agitate samples on an orbital shaker for 24-72 hours.
- Light Stress: Expose samples to UV and visible light per ICH Q1B guidelines.
- Oxidative Stress: Incubate samples with 0.1% H₂O₂ for 2-4 hours at 25°C.
- Acidic/Basic Stress: Adjust samples to low (e.g., pH 3) or high (e.g., pH 9) conditions and incubate for a short duration (e.g., 1 hour).
- Analysis:
- Stop the stress reactions (e.g., by neutralizing pH, adding catalase to quench H₂O₂).
- Analyze all stressed samples and unstressed controls side-by-side using a panel of methods:
- SEC-HPLC: For aggregates and fragments.
- CE-SDS / SDS-PAGE: For fragments and size variants.
- IEC-HPLC / cIEF: For charge variants.
- Peptide Map with LC-MS: For specific PTM identification (e.g., oxidation, deamidation).
Protocol 2: Extended Characterization for mAb Comparability
Objective: To perform an in-depth, orthogonal analysis of the primary, secondary, and higher-order structure of mAbs to establish analytical comparability [32] [33].
Materials:
- Research Reagent Solutions:
- mAb Samples: Pre-change and post-change drug substance.
- Digestion Enzymes: Trypsin, Lys-C.
- Reducing & Alkylating Agents: Dithiothreitol (DTT), Iodoacetamide.
- LC-MS Grade Solvents: Water, acetonitrile, formic acid.
Methodology:
- Primary Structure Analysis:
- Intact Mass Analysis: Use LC-ESI-TOF MS under reduced and non-reduced conditions to confirm molecular weight and detect major mass variants.
- Peptide Mapping: Denature, reduce, alkylate, and digest the mAb with trypsin. Analyze the peptides using RP-UPLC coupled with MS. Identify and quantify post-translational modifications (PTMs) like deamidation, isomerization, and oxidation.
- Higher-Order Structure (HOS) Analysis:
- Circular Dichroism (CD): Perform far-UV and near-UV CD to assess secondary and tertiary structure.
- Differential Scanning Calorimetry (DSC): Measure thermal stability and determine melting temperatures (Tm) of different domains.
- Purity and Impurity Analysis:
- Size Variants: Use SEC-MALS to quantify aggregates and fragments and determine absolute molecular weight.
- Charge Variants: Use cation-exchange chromatography (CEX-HPLC) or capillary isoelectric focusing (cIEF) to profile acidic and basic species.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials used in extended characterization studies for mAbs.
| Research Reagent | Function in Characterization |
|---|---|
| USP Reference Standards | Well-characterized standards for system suitability and method qualification; ensure accuracy and regulatory compliance [34]. |
| Cell Culture Supplements | Chemically defined raw materials used during production; their quality can directly impact product CQAs like glycosylation [33]. |
| Chromatography Resins | Used in purification (e.g., Protein A). Changes in resin lots can impact impurity clearance and must be evaluated for comparability [33]. |
| Enzymes (Trypsin, Lys-C) | Proteases used for peptide mapping to analyze amino acid sequence and identify post-translational modifications [32] [33]. |
| Stable Cell Line | The foundational source of the recombinant mAb; critical for ensuring consistent product quality and a primary focus of comparability studies [33]. |
Leveraging Split-Manufacturing and Historical Data When Concurrent Batches Are Limited
Troubleshooting Guide: Common Experimental Issues & Solutions
| Problem Area | Specific Symptom | Potential Root Cause | Recommended Solution | Key Considerations & References |
|---|---|---|---|---|
| Experimental Design & Power | Insufficient power to detect meaningful differences; high variability masks effects. | Limited batch numbers, high inherent batch-to-batch variability, suboptimal allocation of resources in split-plot design [35]. | Use I-optimal designs to minimize prediction variance; leverage historical data to inform model priors and reduce required new batches [35]. | In split-plot designs, ensure at least one more whole plot than the number of hard-to-change factor levels to accurately estimate variance [36]. |
| Failed Comparability | Analytical results show significant differences between pre- and post-change batches. | The manufacturing change genuinely impacted a Critical Quality Attribute (CQA); analytical methods are not sufficiently sensitive or specific [37] [30]. | Conduct a risk assessment to focus on CQAs; use head-to-head testing with cryopreserved samples; employ extended characterization assays [30]. | Comparability does not require identical attributes, but highly similar ones with no adverse impact on safety/efficacy [37]. |
| Data Integration & Analysis | Inability to integrate or analyze diverse data sources (historical, process, analytical). | Data silos, inconsistent formats, lack of a unified data management platform [38]. | Implement data integration approaches (e.g., ELT/ETL) to create a single source of truth; use statistical models that account for split-plot error structure [38] [36]. | For split-plot ANOVA, use different error terms for whole-plot and subplot effects to avoid biased results [36]. |
| Handling Missing Data | Failed experimental runs (e.g., no product formed). | Process robustness issues; specific combinations of covariates and mixture variables are non-viable [35]. | Document all failures; use experimental designs that are robust to a certain percentage of missing data; analyze failure patterns to understand root causes [35]. | In the potato crisps case study, 47 of 256 runs failed, and analyzing the conditions for failure provided valuable insight [35]. |
| Regulatory Scrutiny | Regulatory questions on the adequacy of the limited-batch comparability study. | The justification for the number of batches and the statistical approach was not sufficiently detailed [37] [30]. | Base batch number justification on risk and phase of development; use all available data (including process development); pre-define acceptance criteria based on historical data [37] [30]. | For a major change, ≥3 post-change batches are typical. For minor changes, ≥1 batch may suffice with sound justification [30]. |
Frequently Asked Questions (FAQs)
Q1: With only 1-2 new batches, how can we possibly demonstrate comparability? A: The key is to leverage the breadth of historical data rather than the quantity of new batches. Use a risk-based approach to identify the most critical quality attributes. Then, compare the data from your 1-2 new batches against the historical data distribution (e.g., using control charts) for those attributes. The new batches should fall within the normal range of variation seen in the historical process. This approach is supported by regulatory guidelines like ICH Q5E, which emphasize the use of existing knowledge and data [37] [30].
Q2: What is the most critical mistake to avoid in a split-plot design for limited batches? A: The most critical mistake is using a standard statistical analysis that does not account for the split-plot structure. In a split-plot design, factors applied to "whole plots" (e.g., a manufacturing campaign) have a different and often larger error term than factors applied to "subplots" (e.g., samples within a campaign). Using an incorrect model inflates the risk of falsely declaring a significant effect for a hard-to-change factor. You must use a split-plot ANOVA with distinct error terms for whole-plot and subplot effects [36].
Q3: Our process change is major, but we only have resources for 3 new batches. How do we justify this to regulators? A: Justification rests on a multi-faceted strategy. First, conduct a comprehensive risk assessment to define the study scope. Second, supplement the 3 GMP batches with data from non-GMP process characterization studies. Third, employ an advanced analytical toolbox, including extended characterization and forced degradation studies, to deeply interrogate product quality. Finally, if concerns remain, a nonclinical or clinical bridging study might be necessary. Document this entire risk-based strategy clearly [37] [30].
Q4: Can active learning help when batches are expensive and limited? A: Yes. Active learning is a machine learning strategy where the algorithm selects the most informative data points to be labeled next, optimizing model performance with minimal experiments. In drug discovery, novel batch active learning methods like COVDROP and COVLAP have been shown to significantly reduce the number of experiments needed to build high-performance models for properties like ADMET and affinity. This approach prioritizes both uncertainty and diversity in batch selection, maximizing information gain from each batch [39].
Q5: How do we set acceptance criteria for comparability with limited new data? A: Acceptance criteria should be prospectively defined and based on historical data. Use data from multiple pre-change batches to establish a normal variability range for each quality attribute. The acceptance criteria for comparability (e.g., "the new batch mean shall be within ±3SD of the historical mean") are not necessarily the same as routine quality standards but must be scientifically justified. For qualitative tests, acceptance is typically based on visual comparison and the absence of new peaks or bands [30].
Experimental Workflows & Logical Diagrams
Split-Plot Batch Experiment Workflow
Strategy for Limited Batch Comparability
The Scientist's Toolkit: Essential Research Reagents & Solutions
| Tool / Reagent Category | Function / Purpose | Example Application in Comparability |
|---|---|---|
| I-optimal Experimental Design | A criterion for generating experimental designs that minimizes the average prediction variance across the design space, ideal for process optimization and model building [35]. | Used in the potato crisps case study to efficiently optimize the recipe mixture despite constraints and limited batches [35]. |
| Extended Characterization Assays | Advanced analytical methods (beyond routine release tests) to deeply probe molecular structure and function (e.g., LC-MS peptide mapping, circular dichroism) [30]. | Critical for head-to-head comparison to detect subtle differences in product attributes when batch numbers are low [30]. |
| Active Learning Algorithms (e.g., COVDROP) | Machine learning methods that select the most informative samples for testing to maximize model performance with minimal experimental cycles [39]. | Applied in drug discovery to reduce the number of experiments needed for ADMET and affinity model optimization [39]. |
| Split-Plot ANOVA Model | A statistical model that correctly accounts for different sources of variation (whole-plot and subplot error) in a split-plot experimental design [36]. | Essential for obtaining valid p-values and confidence intervals when analyzing data from experiments with hard-to-change and easy-to-change factors [36]. |
| Forced Degradation Studies | Studies that intentionally stress a product (e.g., with heat, light, pH) to understand its degradation pathways and profile [30]. | Used in comparability to demonstrate that pre- and post-change products follow the same degradation pathways, supporting similarity [30]. |
Solving Real-World Comparability Problems: Tactics for Constrained Environments
Core Concepts of Analytical Variability
- Sources of Variation: Measured concentrations of analytes are subject to several key sources of variation. Analytical imprecision is the random error inherent to any testing method. Within-subject biological variation is the natural fluctuation around a homeostatic set-point for an individual. Between-subject biological variation is the difference in baseline values between different individuals. Pre-analytical variation (from sample handling) and analytical bias (systematic error) are also important but can be minimized through proper procedures [40].
- Quantifying Variation: Variation is typically described using the Standard Deviation (SD) or the Coefficient of Variation (CV), which is the SD expressed as a percentage of the mean. When multiple independent sources of variation contribute to a measurement, the total observed variation (CV-T) is the square root of the sum of their squared variances [40]. For a single measurement on one person, the total variation is calculated as:
CV_T = √(CV_A² + CV_I²), whereCV_Ais the analytical imprecision andCV_Iis the within-subject biological variation [40]. - Goals for Analytical Imprecision: The acceptability of an assay's imprecision is judged against the magnitude of within-subject biological variation. A
CV_A / CV_Iratio of ≤ 0.5 is considered desirable, meaning the analytical method is precise enough that it adds only minimally to the natural biological variation you are trying to detect [40].
Experimental Protocols & Methodologies
A Practical Protocol for Estimating Method Variability from Routine Testing This novel methodology allows for the estimation of analytical method variability directly from data generated during the execution of a routine test method, supporting continuous performance verification as advocated by ICH Q14 [41].
- Objective: To directly evaluate the variability of an analytical method in a cost-effective manner without requiring extensive additional experiments.
- Applicability: Demonstrated for a small molecule liquid chromatographic assay method using a single-point external reference calibration. The approach can be broadened to a wide range of analytical methods [41].
- Procedure:
- Data Collection: Utilize results generated during the standard execution of the analytical method. The methodology aims to reduce the amount of additional data that needs to be collected specifically for variability assessment [41].
- Variance Estimation: Apply the novel methodology to these routine results to estimate the component of variability introduced by the analytical method itself [41].
- Implementation: This approach can be integrated into the method's lifecycle from development through routine use, aiding in the identification of variability sources and the selection of effective replication strategies [41].
Designing a Replication Strategy to Reduce the Impact of Variability Research studies often use replicates to improve data precision, but this must be balanced against resource constraints.
- Decision Framework: The decision to average multiple results (technical replicates) or to repeat tests on different samples (biological replicates) depends on the relative magnitudes of analytical (
CV_A) and within-subject biological (CV_I) variation [40]. - Effectiveness of Averaging: The table below shows how the ratio of total observed variation (
CV_T) to the true variation (CV_true) improves as more measurements are averaged. Averaging is most effective when analytical imprecision is high relative to biological variation (CV_A/CV_true≥ 1.0) [40].
| CVA/CVtrue | CVT/CVtrue (1 Measurement) | CVT/CVtrue (2 Measurements) | CVT/CVtrue (3 Measurements) |
|---|---|---|---|
| 0.2 | 1.02 | 1.01 | 1.01 |
| 0.5 | 1.12 | 1.06 | 1.04 |
| 1.0 | 1.41 | 1.22 | 1.15 |
| 2.0 | 2.24 | 1.73 | 1.53 |
Source: Adapted from Biomark Med. 2012 Oct;6(5) [40].
- Resource-Aware Replication: In research, blindly assaying all samples in duplicate can halve the scope of a project. The decision to use replicates should be intentional, based on which source of variability (analytical or biological) you are trying to reduce, and whether the study is focused on classifying groups or tracking changes in individuals over time [40].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Why is it critical to test pre- and post-change samples in the same assay run? Running all comparative samples within the same batch minimizes the impact of analytical bias and between-batch variability on your results. This ensures that any observed differences are more likely due to the actual change being studied (e.g., a formulation change) rather than external factors like reagent lot differences or daily calibration shifts in the laboratory [40] [19].
Our method has high precision (low CVA), but we still see significant variation in results from the same subject. What could be the cause? High subject-level variation despite good method precision strongly indicates significant within-subject biological variation. This biological "noise" can mask true trends. In such cases, increasing the number of biological replicates (samples collected from the subject at different times) is more effective than running more technical replicates from the same sample [40].
How can we design a robust study when limited to a small number of batches for comparability research? When batch numbers are limited, it is crucial to characterize the batch-to-batch variability of your key materials first. For your main experiment, use a replicated study design where at least one batch is tested multiple times. This allows you to statistically separate the residual error from the between-batch variance, providing a more reliable and generalizable conclusion about comparability [19].
Troubleshooting High Analytical Variability
| Symptom | Possible Cause | Investigation & Action |
|---|---|---|
| High variation between replicate measurements of the same sample. | High analytical imprecision, unstable reagents, equipment malfunction, or inconsistent pipetting. | 1. Review quality control (QC) data for the assay.2. Check instrument calibration and maintenance logs.3. Re-train staff on standardized pipetting techniques.4. Implement a replication strategy to average out noise, if appropriate [40]. |
| Consistent differences between results obtained from different batches of the same reagent or material. | Substantial batch-to-batch variability in a critical raw material (e.g., plasmids, viral vectors) [42]. | 1. Statistically compare results from multiple batches in a controlled study [19].2. Qualify new vendors or insist on more stringent quality specifications from suppliers.3. Adjust the manufacturing process to accommodate or reduce this variability [42]. |
| Good assay precision but poor ability to detect a change in an individual over time. | High within-subject biological variation relative to the change you are trying to detect [40]. | 1. Consult literature for known biological variation (CV_I) of your analyte.2. Calculate the Reference Change Value (RCV) to determine the minimum significant change.3. Increase the number of longitudinal samples per subject to better establish a personal baseline [40]. |
The Scientist's Toolkit
Essential Research Reagent Solutions
| Item | Function in Mitigating Variability |
|---|---|
| Standardized Lysis Buffer (e.g., RIPA) | Ensures consistent protein extraction and denaturation from samples, reducing pre-analytical variation. A standardized, detergent-free protocol like SPEED can be adapted for various biological matrices [43]. |
| Single-Point External Reference Standards | Used for instrument calibration in chromatographic assays. A consistent source and preparation of standards are vital for minimizing analytical bias and ensuring day-to-day comparability [41]. |
| Characterized Biological Matrices | Using well-defined and consistent matrices (e.g., plasma, tissue homogenates) for preparing standards and controls helps account for matrix effects, a common source of analytical bias and imprecision. |
| Critical Raw Materials (e.g., Vectors, Lipids) | These are core components in advanced therapies. Sourcing from suppliers with tight quality controls and low batch-to-batch variability is essential for producing reproducible results in cell therapy manufacturing [42]. |
Workflow and Decision Pathways
The following diagram illustrates the logical workflow for planning an experiment to robustly compare pre- and post-change samples, taking into account the various sources of variability.
Experimental Planning Workflow
The diagram below outlines a specific replication strategy based on the primary source of variability in your experiment, guiding you on whether to prioritize technical or biological replicates.
Frequently Asked Questions (FAQs)
Q1: Our comparability study has a very limited number of batches. How can we be confident in our conclusions? A1: With limited batches, a data-centric approach is key. Focus on building a comprehensive Control Strategy that leverages multivariate analysis. Instead of relying only on traditional univariate tests, use multivariate tools like Principal Component Analysis (PCA) to understand the total variability in your data. This helps in identifying if the limited observed variation is consistent with the normal operating ranges of your established process, providing a more robust basis for concluding comparability [44].
Q2: What are the key CMC considerations for a comparability study under an accelerated development pathway? A2: Regulatory agencies recognize the challenges of accelerated development. The core focus should be on demonstrating a thorough understanding of your product and process. Key considerations include [44]:
- Justified Control Strategy: Your control strategy should be risk-based and scientifically justified, potentially leveraging prior knowledge and data from development.
- Innovative Approaches: Consider the use of innovative approaches to process validation, such as leveraging continuous process verification principles.
- Stability Data: Explore the use of alternative approaches for setting shelf-life if real-time stability data is limited at the time of submission, with robust plans for post-approval commitment.
Q3: During DoE data analysis, my residual plots show a pattern, not random scatter. What does this mean and how can I fix it? A3: Patterned residuals indicate that your model is missing something—it may not be capturing the true relationship between factors and the response. This is a common issue when the underlying process is more complex than the model you've fitted [45]. To troubleshoot:
- Check for Missing Terms: Your model might be missing a key interaction effect or a quadratic term. Revisit your interaction effect analysis to see if adding these terms improves the model.
- Transform the Response: If the variance of your data isn't constant, applying a transformation (e.g., log, square root) can often stabilize it and improve model fit.
- Validate Model Assumptions: Conduct a formal residual analysis, including normality and independence tests, to systematically diagnose the issue [45].
Q4: How can I effectively identify and interpret interaction effects in my DoE? A4: Interaction effects occur when the effect of one factor depends on the level of another factor [45].
- Identification: In your ANOVA, a statistically significant interaction term (with a low p-value) indicates its presence.
- Interpretation: The best way to interpret an interaction is through an interaction plot. This graph shows the response for different levels of one factor, across the levels of another. If the lines on the plot are not parallel, it confirms an interaction.
- Troubleshooting: If interactions are making your model complex, focus on the interactions that are both statistically and practically significant. Use domain knowledge to decide which interactions are meaningful for your process.
Troubleshooting Guides
Guide 1: Troubleshooting Model Fit in DoE Analysis
A poor model fit can undermine the entire DoE. Follow this logical workflow to diagnose and resolve the issue.
Diagnosis and Actions:
- If you have patterned residuals: Your model is misspecified.
- Action: Add higher-order terms to your model, such as interaction effects (e.g., Factor A * Factor B) or quadratic terms (e.g., Factor A²), to capture the non-linear relationship [45].
- If your Adjusted R² is much lower than R²: Your model may be overfitted with too many non-significant terms.
- Action: Use stepwise regression or your ANOVA p-values to remove the least significant predictors from the model. This simplifies the model without greatly reducing its explanatory power.
- If residuals are not normally distributed: The assumptions for statistical tests (like ANOVA) are violated.
- Action: Apply a transformation to your response variable (e.g., log, Box-Cox). Also, investigate potential outliers that could be skewing the results and ensure they are not due to data entry errors [45].
Guide 2: Troubleshooting Control Strategy for Limited Batch Comparability
Establishing a control strategy with limited data requires a focus on process understanding over mere data volume.
Diagnosis and Actions:
- Leverage Prior Knowledge: The control strategy should be built on a foundation of prior knowledge and risk assessment. Clearly define your Critical Quality Attributes (CQAs) based on this understanding [44].
- Use Multivariate Analysis: Apply Principal Component Analysis (PCA) to your limited batch data. This creates a multivariate "process signature" that is more sensitive than looking at individual attributes.
- Action if batches are within limits: If all batches (pre- and post-change) fall within the established multivariate control limits, it provides strong evidence of comparability. Your control strategy can be justified based on this holistic assessment.
- Action if a batch is outside limits: If a batch is an outlier in the multivariate space, you must investigate the root cause. This may involve refining your process understanding and potentially updating your control strategy before concluding comparability [44].
Protocol 1: Standard DoE Analysis Workflow for Process Understanding
This protocol provides a detailed methodology for analyzing DoE results to build robust process understanding, which is critical for justifying comparability with limited data [45].
Data Preprocessing:
- Data Cleaning: Remove invalid or duplicate data entries.
- Missing Value Handling: Use interpolation methods or delete records with missing values, depending on the extent and nature of the missingness.
- Outlier Detection: Use statistical methods (e.g., Grubbs' test) or visualization tools (e.g., box plots) to identify and handle anomalous data points that could skew results.
Descriptive Statistical Analysis:
- Calculate the mean and standard deviation for each experimental run or condition.
- Create preliminary visualizations (e.g., main effects plots, interaction plots) to identify obvious trends and patterns.
Variance Analysis (ANOVA):
- Construct an ANOVA table to decompose the total variability into contributions from each factor, their interactions, and error.
- Calculate the F-value and p-value for each model term to determine statistical significance. A typical significance level (alpha) of 0.05 is used.
- Output: A list of significant main effects and interaction terms that influence the response variable.
Model Fitting and Validation:
- Fit a regression model (linear or quadratic) using the significant factors identified in the ANOVA.
- Evaluate the model's fit using metrics like R-squared (R²) and Adjusted R².
- Perform a residual analysis by plotting residuals vs. predicted values and a normal probability plot of the residuals to validate model assumptions.
Interpretation and Optimization:
- Use contour plots or response surface plots to visualize the relationship between factors and the response.
- Identify the factor level settings that optimize the response (e.g., maximize yield, minimize impurity).
Quantitative Data from DoE Analysis
Table 1: Key Model Fit Statistics and Their Interpretation
| Statistic | Definition | Target Value / Interpretation | Troubleshooting Tip |
|---|---|---|---|
| R-Squared (R²) | Proportion of variance in the response explained by the model. | Closer to 1.00 is better (e.g., >0.80). | A low R² indicates the model is missing key factors. |
| Adjusted R² | R² adjusted for the number of terms in the model. | Prefer over R² for model comparison; should not be much lower than R². | A large gap from R² suggests overfitting; remove non-significant terms. |
| P-value (ANOVA) | Probability that the observed effect is due to random chance. | < 0.05 indicates a statistically significant effect. | A high p-value for a factor means it has no detectable effect. |
| F-value | Ratio of model variance to error variance. | A larger value indicates a more significant model. | Used in conjunction with the p-value to assess significance. |
Table 2: Common DoE Challenges and Mitigation Strategies in Comparability Studies
| Challenge | Impact on Comparability | Data-Centric Mitigation Strategy | Regulatory Consideration |
|---|---|---|---|
| Limited Batch Numbers | Reduced statistical power and confidence in conclusions. | Use of multivariate analysis (e.g., PCA) and leveraging prior knowledge to strengthen the control strategy [44]. | Agencies may accept justified approaches using approved post-approval change management protocols (PACMP) for data collection [44]. |
| High Measurement Noise | Obscures true process signals and differences. | Increase measurement replicates; use nested DoE designs to separate source of variation; employ signal processing techniques. | A well-understood and controlled analytical method is a prerequisite. |
| Unexpected Interactions | Complicates the understanding of the process change's impact. | Include interaction terms in the initial DoE model; use sequential experimentation to deconvolute complex effects [45]. | Interaction effects should be documented and understood as part of process validation. |
The Scientist's Toolkit: Research Reagent & Solution Essentials
Table 3: Essential Research Reagent Solutions for DoE-driven Bioprocessing
| Item / Solution | Function in Experimentation | Key Consideration for Comparability | |
|---|---|---|---|
| Cell Culture Media | Provides nutrients for cell growth and protein production. | Even slight formulation changes can impact Critical Quality Attributes (CQAs). A DoE is crucial for comparing media from different sources or formulations. | |
| Chromatography Resins | Used for purification to separate the target molecule from impurities. | Resin lot-to-lot variability is a key risk. DoE can be used to define the operating space that is robust to this variability. | |
| Reference Standards | Calibrate assays and serve as a benchmark for product quality attributes. | Essential for ensuring data consistency across pre- and post-change batches in a comparability study. | |
| Critical Process Parameters (CPPs) | (e.g., pH, Temperature, Dissolved Oxygen) | These are not reagents, but are "materials" in the experimental design. Their ranges are systematically varied in a DoE to understand their effect on CQAs [45]. | A change in a CPP is often the subject of the comparability study itself. The DoE defines the acceptable range for the new setpoint. |
Addressing the Cumulative Impact of Multiple Small Changes
Frequently Asked Questions
Q: With a limited number of batches, how can we justify that a series of minor process changes have not had a cumulative adverse effect? A: A risk-based approach is essential. For each individual change, a comparability study should demonstrate the change has no adverse impact. When changes are sequential, use data from extended characterization and stability studies across multiple batches to build a cumulative data package that shows quality attributes remain highly similar and predictable [30].
Q: What is the minimum number of batches needed for a comparability study following a minor change? A: For a minor change, a comparability study can typically be performed with ≥1 batch of the changed product. For medium changes, 3 batches are generally recommended, and for major changes, ≥3 commercial-scale batches are advised [30].
Q: How should acceptance criteria for comparability studies be set, especially when batch numbers are low? A: Acceptance criteria should be established prospectively based on historical data of the process and product quality. The criteria should be justified with sufficient scientific reasoning and cannot be lower than the established quality standards unless proven reasonable. They can be quantitative (e.g., meeting a specified range) or qualitative (e.g., comparable peak shapes) [30].
Experimental Protocols for Comparability Studies
1. Protocol for Quality Attribute Comparison
- Objective: To demonstrate that the product's critical quality attributes (CQAs) remain highly similar after process changes.
- Methodology: Compare the changed product's CQAs against historical batch data. For attributes with insufficient historical data, perform head-to-head analysis using cryopreserved samples from before the change [30].
- Key Analyses:
- Purity: SEC-HPLC, CE-SDS (reduced and non-reduced), IEC-HPLC.
- Identity: Peptide mapping, iCIEF.
- Potency: Cell-based bioassays, binding affinity assays.
- Extended Characterization: Primary structure analysis (LC-MS), higher-order structure analysis (circular dichroism), and post-translational modification analysis [30].
2. Protocol for Stability Comparison
- Objective: To ensure the degradation profile and pathway of the product are comparable pre- and post-change.
- Methodology: Conduct real-time, accelerated, and forced degradation studies on batches from the changed process. Compare the results with historical stability data [30].
- Key Metrics:
- Degradation rate should be equivalent or slower.
- Degradation pathways must be the same.
- Degradation kinetics under forced conditions should be comparable [30].
Data Presentation
Table 1: Acceptable Standards for Key Analytical Assays in Comparability Studies [30]
| Test Type | Specific Analysis | Acceptable Standards |
|---|---|---|
| Routine Release | Peptide Map | Comparable peak shapes; no new or lost peaks. |
| SDS-PAGE/CE-SDS | Main band/peak within statistical acceptance criteria; no new species. | |
| SEC-HPLC | Percentage of main peak within statistical acceptance criteria. | |
| Charge Variants (CEX, cIEF) | Percentage of major peaks within acceptance criteria; no new peaks. | |
| Biological Activity | Potency within acceptance criteria based on statistical analysis. | |
| Extended Characterization | Peptide Mapping (LC-MS) | Confirmation of primary structure; post-translational modifications within an acceptable range. |
| Circular Dichroism | No significant difference in spectra and calculated conformational ratios. | |
| Free Sulfhydryl | Free cysteine content within acceptable range based on statistical analysis. |
Table 2: Key Research Reagent Solutions [30]
| Reagent / Material | Function in Comparability Studies |
|---|---|
| Cell-Based Assay Kits | Determine the biological activity (potency) of the product in a head-to-head manner. |
| Characterized Reference Standards | Serve as a benchmark for comparing product quality attributes (e.g., identity, purity) before and after a change. |
| ELISA Kits (e.g., HCP, Protein A) | Quantify process-related impurities to ensure the changed process maintains or improves impurity clearance. |
| Stable Cell Lines | Provide a consistent and reproducible system for conducting potency assays throughout the comparability study. |
Workflow Visualization
Risk Assessment and Study Design
For researchers, scientists, and drug development professionals, scaling a process introduces significant challenges in maintaining product comparability. This is particularly critical when working with limited batch numbers, where process changes can introduce variability that confounds results and threatens regulatory compliance. Choosing between scaling up (vertical scaling) and scaling out (horizontal scaling) is a strategic decision that directly impacts your analytical comparability burden.
Frequently Asked Questions (FAQs)
1. What is the fundamental difference between scale-up and scale-out in a research context?
- Scale-Up (Vertical Scaling) refers to adding more power (e.g., CPU, memory, storage) to an existing single server or system. In a lab context, this is analogous to moving from a small benchtop bioreactor to a single, larger-capacity bioreactor [46] [47].
- Scale-Out (Horizontal Scaling) refers to adding more instances of servers or nodes to a distributed system. In research, this is like running multiple, identical benchtop bioreactors in parallel to increase total output [46] [48].
2. How does my choice of scaling method affect analytical comparability studies?
Your scaling strategy directly influences the sources of variability in your process. Scale-up can introduce new physicochemical conditions when moving to a larger vessel, potentially altering critical quality attributes (CQAs). Scale-out, while using identical smaller units, introduces inter-batch variability across multiple units. With limited batch numbers, this inter-batch variability can be difficult to statistically distinguish from product-related changes, increasing the comparability burden [2] [49].
3. We have very few production batches. Which scaling method is less likely to complicate our statistical analysis?
With low batch numbers, scale-out often presents a lower initial comparability burden. The process parameters and equipment geometry remain consistent with your original small-scale studies, minimizing scale-dependent variables. However, it requires a robust strategy to manage and minimize inter-batch variation across all parallel units [2].
4. What are the key infrastructure considerations when planning for scale-out?
A successful scale-out architecture requires:
- Symmetrical Nodes: All units (e.g., servers, bioreactors) should have identical configurations to ensure consistent performance and output [50].
- Load Balancer: A system to distribute workloads evenly across all nodes, preventing any single unit from becoming a bottleneck [50].
- Data Replication: A strategy to ensure data is synchronized across the system for fault tolerance and high availability [50].
Troubleshooting Guides
Issue: Significant Batch Differences Detected After Scale-Out
Symptoms: Analysis of results from multiple parallel units shows statistically significant differences in key intermediate or product CQAs [49].
Solution:
- Assess Between-Batch Differences: Use statistical methods to evaluate the differences.
- Develop Conversion Models: If batch differences are consistent and predictable, use Generalized Linear Models (GLMs) to convert values between batches, creating a harmonized dataset for analysis. This is preferable to simply including batch as a covariate, especially when biomarkers serve as predictors [49].
- Review Process Rigor: Ensure standard operating procedures (SOPs) for unit operation, sampling, and analytics are meticulously followed to reduce introduced variability.
Issue: Performance Bottlenecks and Inconsistent Results After Scale-Up
Symptoms: The scaled-up process (e.g., in a single, larger vessel) suffers from performance limits, longer processing times, or yields a product with different profiles than the small-scale model [47].
Solution:
- Identify the Bottleneck: Monitor system resources (in IT) or process parameters (in bioprocessing). Determine if the issue is related to compute power, memory, storage I/O, or, in a bioreactor, factors like oxygen transfer or mixing time [47].
- Evaluate Hardware/Equipment Limits: Scale-up has inherent physical limits. Check if the current server hardware or bioreactor system has been maxed out. Further vertical scaling may not be possible [47] [48].
- Consider a Hybrid Approach: It may be necessary to scale out by adding nodes or parallel units, rather than attempting to scale up further. This is often the long-term solution for overcoming the ceiling of a single system [47] [50].
Comparative Data Tables
Table 1: Scale-Up vs. Scale-Out at a Glance
| Aspect | Scale-Up (Vertical) | Scale-Out (Horizontal) |
|---|---|---|
| Basic Approach | Add resources to a single node [47] | Add more nodes to a distributed system [47] |
| Complexity | Simple and straightforward [47] [48] | Higher; requires robust orchestration [47] [48] |
| Comparability Focus | Managing changes within a single, evolving system | Managing consistency across multiple, identical systems |
| Hardware Limits | Hits a ceiling based on maximum server capacity [46] [47] | Practically boundless, limited by network [47] |
| Cost Profile | Higher upfront cost for premium hardware; lower operational complexity [48] | Lower incremental cost with commodity hardware; higher soft costs for management [48] |
Table 2: Scaling Strategy Decision Matrix
| Factor | Favors Scale-Up | Favors Scale-Out |
|---|---|---|
| Architecture | Monolithic, traditional applications [47] [50] | Microservices, distributed applications [47] |
| Workload Type | Memory-intensive, real-time analytics, traditional RDBMS [47] [50] | Stateless applications, web servers, high concurrency, distributed processing [47] |
| Batch Numbers | Lower risk if the single system is well-characterized | Preferred for maintaining process identicalness across units [2] |
| Growth Forecast | Predictable, moderate growth [48] | Unpredictable, rapid, or large-scale growth [48] |
| Future-Proofing | Limited | High [48] |
Workflow and Relationship Visualizations
Scaling Strategy Decision Flow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Scaling and Comparability Studies
| Item | Function in Scaling/Comparability Context |
|---|---|
| Orthogonal Analytical Methods | Provides multiple lines of evidence to confirm CQAs are maintained post-scaling, increasing confidence in comparability [2]. |
| Standardized Reference Materials | Serves as a benchmark across different batches and scales to minimize measurement variability [49]. |
| Stable Cell Line Banks | Ensures consistency of the biological production system across multiple batches or scales. |
| Defined Culture Media | Reduces a major source of variability by using consistent, high-quality raw materials. |
| Generalized Linear Models (GLMs) | A statistical tool to adjust for between-batch differences and harmonize data, making comparisons valid [49]. |
Frequently Asked Questions (FAQs)
Q1: Why is establishing a statistical confidence level critical for comparability studies with limited batches? Establishing a statistical confidence level (e.g., 95% or 97%) is crucial because it quantifies the reliability of your study results. With a limited number of batches, there is inherent uncertainty and a higher risk of drawing an incorrect conclusion. A pre-defined confidence level, based on a risk assessment, ensures that the comparison between pre-change and post-change product is statistically rigorous and defensible to regulators, despite the small sample size [51] [52].
Q2: How does risk assessment influence the design of a comparability study? A risk assessment directly determines the stringency of your statistical criteria. Attributes are scored based on the severity of their impact on product quality, the likelihood of occurrence, and the detectability of problems [52]. A high Risk Priority Number (RPN) dictates the use of higher statistical confidence and a higher proportion of the population to cover in your analysis, ensuring that more critical attributes are evaluated with greater statistical power [52].
Q3: What is the practical difference between the Tolerance Interval (TI) and Process Performance Capability (PpK) methods? Both methods determine the number of PPQ runs needed, but they approach the problem differently. The Tolerance Interval method focuses on the range needed to cover a fixed proportion (p) of the population with a specified confidence [52]. The Process Performance Capability (PpK) method compares the spread of your process data (based on the mean and standard deviation) to the specification limits [52]. The choice of method can depend on regulatory guidance and the specific nature of the quality attribute being measured.
Q4: Our historical data is limited. How can we compensate for this in our sample size calculation? The uncertainty from small historical sample sizes can be compensated for by using confidence intervals for the mean and standard deviation in your calculations. Instead of using the sample standard deviation (s) directly, you would use the upper confidence limit for the standard deviation (SUCL). This builds in a "margin of error" that accounts for the instability of estimates from small datasets, leading to a more robust and conservative sample size calculation [52].
Troubleshooting Guides
Issue: Batch Processing Job Results in an Error
Problem: A batch processing job, such as a data analysis routine, has failed or ended with an error.
Solution: Follow this systematic triage process to identify and resolve the issue:
- Review the Batch Run Tree and Logs: The first step is always to access the batch execution details. Check the status of all threads and instances. Download and meticulously review the standard output (stdout) and standard error (stderr) log files. Search for keywords like "error," "exception," or database error codes (e.g., "ORA-") [53].
- Check for Common Parameter Errors: Verify all batch job parameters. A common issue is an incorrect batch date or a misconfigured parameter that causes the job to fail immediately [53].
- Investigate Data Quality: If the logs point to a "severe Java error" or a null pointer exception, the underlying cause is often corrupt or invalid data, such as a bad foreign key or a null value that the job cannot process [54] [53].
- Resubmit with Simplified Parameters:
Issue: High Latency Causing Outdated Information
Problem: Batch processing schedules cause delays, making the resulting information outdated for timely decision-making.
Solution:
- Implement Incremental Processing: Modify batch jobs to only process new or changed data since the last run, instead of reprocessing the entire dataset each time. This significantly reduces processing time and data latency [55].
- Evaluate a Hybrid Model: For critical data that requires fresher insights, consider a hybrid processing model. Use real-time data streaming for immediate, time-sensitive alerts and actions, while retaining batch processing for large-scale, comprehensive data consolidation and historical reporting [56] [57].
Issue: Ensuring Data Integrity Across Batch Jobs
Problem: Errors during batch processing or accidental reruns of jobs compromise data integrity, leading to duplicated or inaccurate results.
Solution:
- Design Reentrant Jobs: Create batch jobs that can be safely paused, resumed, or restarted without unintended side effects or errors. This often involves leveraging checkpointing functionality to track progress [58].
- Enable Exactly-Once Processing: Where supported, use processing frameworks that provide exactly-once semantics. This ensures each record is processed once and only once, preventing duplicate results even if a job is rerun after a failure [54].
- Implement Data Validation: Incorporate data validation and error-checking mechanisms as part of the pre-processing workflow to prevent bad data from entering downstream systems [54] [56].
Statistical Approaches for Limited Batch Comparability
When dealing with a limited number of batches, selecting the right statistical method and acceptance criteria is essential for a successful comparability study. The following methodologies provide a structured framework.
Key Statistical Methods:
| Method | Core Objective | Key Output |
|---|---|---|
| Tolerance Interval (TI) | To define a range that covers a fixed proportion (p) of a population at a stated confidence level (1–α) [52]. | A two-sided interval: ( TI = X_{avg} \pm k \times s ) [52] |
| Process Performance (PpK) | To compare the spread of process data to specification limits, assessing process capability [52]. | An index quantifying how well the process fits within specs [52]. |
Risk-Based Acceptance Criteria: The required statistical confidence and population proportion are not arbitrary; they are set through a risk assessment [52].
| Risk Priority Number (RPN) | Risk Category | Statistical Confidence (1–α) | Population Proportion (p) |
|---|---|---|---|
| > 60 | High | 0.97 - 0.99 | 0.80 - 0.90 |
| 30 - 60 | Medium | 0.95 | 0.90 |
| < 30 | Low | 0.95 | 0.99 |
Scoring Note: RPN = Severity (S) × Occurrence (O) × Detectability (D), each scored 1-5 [52].
Experimental Protocol: Tolerance Interval Method for PPQ Runs
This protocol outlines the steps for calculating the necessary number of Process Performance Qualification (PPQ) runs using the Tolerance Interval method, compensating for limited historical data [52].
Workflow Overview:
Step-by-Step Methodology:
- Perform Risk Assessment: Score the attribute for Severity (S), Occurrence (O), and Detectability (D) on a scale (e.g., 1-5). Calculate the Risk Priority Number (RPN = S × O × D). Use the RPN to set the target statistical confidence (1–α) and the proportion of the population (p) to cover from the risk-based table above [52].
- Gather and Characterize Historical Data: Collect all available historical stability data (e.g.,
n = 12batches) from the old process. For the data, calculate the sample mean (Xavg) and sample standard deviation (s) [52]. - Compensate for Sample Size Uncertainty: To account for the uncertainty in the standard deviation (
s) from the small sample size, calculate the Upper Confidence Limit for the standard deviation (SUCL). This is done using the chi-square distribution:SUCL = s * √( (n-1) / χ²_(1-α, n-1) )[52]. - Calculate Maximum Acceptable Tolerance Estimator: Using the specification limits (SL), compute the maximum acceptable value for the tolerance estimator,
kmax, accep. For a two-sided specification, the formula is:kmax, accep = min( (USL - Xavg)/SUCL , (Xavg - LSL)/SUCL )[52]. - Iterate to Find Required PPQ Runs: The number of PPQ runs (
n) is found by iteratively solving for the smallestn(starting from 3) where the calculated tolerance factork'is less than or equal tokmax, accep. The factork'is calculated as:k' = t_(1-α, n-1) * √( (n+1)/n ) / z_((1-p)/2)(using approximations for the t, normal, and chi-square distributions) [52]. This step is typically performed using statistical software like Excel's solver function.
The Scientist's Toolkit: Research Reagent & Statistical Solutions
This table details key materials and statistical concepts essential for executing a robust comparability study.
| Item / Concept | Type | Function / Explanation |
|---|---|---|
| Historical Stability Data | Data | Existing batch data from the "old" manufacturing process. Serves as the statistical baseline for comparing the "new" process [52]. |
| Risk Assessment Matrix | Protocol | A structured tool (e.g., with S, O, D scores) to objectively quantify the risk of each quality attribute, guiding the statistical rigor of the study [52]. |
| Tolerance Interval Estimator (k) | Statistical Factor | A multiplier that defines how many standard deviations from the mean are needed to cover a proportion (p) of the population at a given confidence. It is central to the sample size calculation [52]. |
| Linear Mixed-Effects Model | Statistical Model | A model used for stability data that accounts for both fixed effects (e.g., overall degradation rate) and random effects (e.g., lot-to-lot variability in degradation) [51]. |
| Equivalence Test | Statistical Test | A hypothesis test used to demonstrate that the average degradation rates from two processes do not differ by more than a pre-defined acceptance margin (Δ) [51]. |
Demonstrating Success: Statistical Analysis, Regulatory Submission, and Case Studies
Frequently Asked Questions (FAQs)
1. When should I use an equivalence test instead of a standard t-test? You should use an equivalence test when your research goal is to demonstrate that two methods, processes, or products are similar, rather than different [59] [60]. Standard difference tests (like t-tests) are designed to detect differences; failing to reject the null hypothesis in a difference test does not allow you to claim equivalence [59]. Equivalence testing is particularly critical in comparability studies, such as when you need to show that a new manufacturing process produces a product equivalent to the original.
2. How do I justify and set an appropriate equivalence range? The equivalence range, or region of practical equivalence, should be defined based on the smallest difference that is considered practically or clinically important in your specific field [59] [60]. This is not a statistical decision, but a subject-matter one. Justification can come from prior evidence, regulatory guidelines, or expert consensus. For example, you might define two analytical methods as equivalent if their mean results are within ±10% of each other [59].
3. My data is not normally distributed. Can I still perform an equivalence test? Yes. While some underlying assumptions are similar, you have several options for handling non-normal data:
- Data Transformation: Apply a transformation (e.g., logarithmic, square root, or Box-Cox) to make the data more normal before analysis [61] [62].
- Nonparametric Methods: Use distribution-free tests, though you may need to adapt the equivalence testing logic as these tests often work with ranks rather than raw means [61] [63].
- Bootstrap Methods: Use bootstrapping to construct confidence intervals for the difference, which does not rely on the normality assumption [61].
4. What are the consequences of using a standard difference test when I want to prove similarity? Relying on a non-significant p-value from a difference test (e.g., p > 0.05) to claim similarity is logically flawed and can be highly misleading [59] [60]. This practice has a high risk of a Type II error—falsely concluding "no difference" simply because your study lacked the statistical power to detect a meaningful difference that actually exists. Equivalence testing is the statistically correct framework for such objectives.
Troubleshooting Guides
Guide 1: Selecting the Correct Statistical Test for Comparability
Problem: Researchers are unsure whether to use a test for difference or a test for equivalence in their comparability study, leading to incorrect conclusions.
Solution: Follow the decision workflow below to select the appropriate statistical approach based on your research objective.
Guide 2: Handling Non-Normal Data in Analysis
Problem: Data violates the normality assumption required for parametric equivalence tests, threatening the validity of the analysis.
Solution: Diagnose the issue and apply an appropriate corrective strategy. The workflow below outlines a standard approach.
Detailed Steps:
- Diagnose Normality: Use both statistical tests (like the Shapiro-Wilk test) and visualizations (like Q-Q plots or histograms) to assess if your data significantly deviates from a normal distribution [61] [63].
- Apply Transformation: If the data is non-normal, apply a transformation.
- Log Transformation: Effective for right-skewed data.
- Square Root Transformation: Useful for count data.
- Box-Cox Transformation: A more advanced, power transformation that finds the optimal parameter (λ) to make the data as normal as possible [62].
- Re-check Normality: After transformation, re-check the data for normality. If the assumption is now met, you can proceed with a parametric equivalence test on the transformed data.
- Use Robust Methods: If transformation fails to normalize the data, consider nonparametric alternatives or bootstrapping techniques to construct your confidence intervals [61] [63].
Experimental Protocols & Data Presentation
Table 1: Comparison of Statistical Test Objectives and Interpretation
This table summarizes the key differences between the testing approaches relevant to comparability studies.
| Test Type | Research Objective | Null Hypothesis (H₀) | Alternative Hypothesis (H₁) | Key Interpretation of a Significant Result |
|---|---|---|---|---|
| Standard Difference Test | To detect a meaningful difference between groups. | The means are equivalent (difference = 0). | The means are not equivalent (difference ≠ 0). | A "significant" effect indicates evidence of a difference. |
| Equivalence Test | To confirm that two groups are practically equivalent. | The means are meaningfully different (difference ≤ -Δ OR difference ≥ Δ). | The means are equivalent (-Δ < difference < Δ). | We can reject the presence of a meaningful difference and claim equivalence. |
| Minimum Effect Test | To confirm that an effect is larger than a trivial threshold. | The effect is trivial or negative (effect ≤ Δ). | The effect is meaningfully positive (effect > Δ). | The effect is both statistically and practically significant. |
Table 2: Strategies for Dealing with Non-Normal Data
This table provides a quick reference for handling violations of the normality assumption.
| Method | Description | Best Use Case | Considerations |
|---|---|---|---|
| Data Transformation | Applying a mathematical function (e.g., log, square root) to all data points to make the distribution more normal. | When data has a consistent skew or when the underlying theory supports a transformed scale. | Interpreting results is done on the transformed scale, which can be less intuitive [61]. |
| Nonparametric Tests | Using tests that do not assume a specific data distribution (e.g., Mann-Whitney U test, Kruskal-Wallis test). | When data is ordinal, severely skewed, or has outliers that cannot be resolved. | Often less statistically powerful than their parametric counterparts when data is normal; uses ranks of data [63]. |
| Bootstrap Methods | A resampling technique that empirically estimates the sampling distribution of a statistic (e.g., the mean difference). | When the sample size is small or the data distribution is complex and unknown. | Computationally intensive, but highly flexible and does not rely on distributional assumptions [61]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Analytical and Statistical Tools for Comparability Research
This table details key components for designing and analyzing a robust comparability study, especially under constraints like limited batch numbers.
| Tool / Material | Function / Purpose | Application in Comparability Studies |
|---|---|---|
| Equivalence Range (Δ) | A pre-specified margin of practical insignificance. | Defines the critical boundary within which differences between the test and reference material are considered negligible. Justification is paramount [59] [60]. |
| Two One-Sided Tests (TOST) | A standard statistical procedure for testing equivalence. | Formally tests whether the true difference between two means lies entirely within the -Δ to Δ equivalence range [59] [60]. |
| Box-Cox Transformation | A family of power transformations used to stabilize variance and make data more normal. | Prepares non-normal assay data (e.g., potency, impurity levels) for parametric statistical analysis, improving the validity of results [62]. |
| Shapiro-Wilk Test | A formal statistical test for normality. | Used during data diagnostics to check if the dataset violates the normality assumption of parametric tests [63]. |
| 90% Confidence Interval | An interval estimate for the population parameter. | In a TOST equivalence test with α=0.05, if the entire 90% CI for the mean difference falls within the equivalence region (-Δ, Δ), equivalence is declared [59]. |
| Statistical Software (e.g., R, JASP) | Platforms capable of running specialized analyses. | Essential for performing equivalence tests (TOST), advanced transformations (Box-Cox), and nonparametric analyses that may not be available in basic software [63]. |
Setting Biologically Meaningful Acceptance Criteria Beyond Statistical Significance
Frequently Asked Questions (FAQs)
What does it mean for acceptance criteria to be "biologically meaningful"?
A biologically meaningful result is one where the observed effect is not just statistically significant (unlikely due to chance) but is also large enough, consistent enough, and relevant enough to indicate a real impact on human health or physiology. A p-value below 0.05 only tells you an effect is detectable; it does not confirm the change is physiologically important for the target population [64]. Regulatory bodies like the European Food Safety Authority (EFSA) emphasize that a small, statistically significant change in a biomarker may have no meaningful health benefit [64].
My study has a strong assay window (Z'-factor >0.5) and a statistically significant result (p<0.05). Why was my comparability study still questioned?
A strong assay window and a low p-value confirm your tool is robust and detected a signal. However, regulators focus on the effect size and its biological relevance [64]. Your result might have been questioned for reasons such as:
- Tiny Effect Size: The change detected, while precise, is too small to confer any real-world health or functional benefit [64].
- Short Study Duration: The effect was measured over a period too short to confirm it is sustained [64].
- Lack of Dose-Response: You tested only a single dose, missing the opportunity to show that the effect strengthens with increased dose—a key proof of a real biological relationship [64].
- Endpoint Mismatch: The biomarker or measurement you used is not validated or recognized as a predictor of a meaningful health outcome [64].
How can I set robust acceptance criteria with a limited number of batches?
With limited batches, estimating the true variability of your process is challenging. Using simple "3-sigma" limits from a small sample can set criteria that are too tight and lead to failures [65]. A more robust approach uses probabilistic tolerance intervals.
- This method accounts for uncertainty from small sample sizes by using larger multipliers (e.g., 3.5-sigma instead of 3-sigma for a sample size of 62) to define a range where you can be, for example, "99% confident that 99% of the population will fall within the limits" [65].
- The table below shows how the sigma multiplier increases as the sample size decreases, ensuring your criteria are not unrealistically strict.
Table: One-Sided Sigma Multipliers (MU) for Different Sample Sizes (99% Confidence, 99.25% Coverage)
| Sample Size (N) | Sigma Multiplier (MU) |
|---|---|
| 10 | 4.90 |
| 20 | 4.00 |
| 30 | 3.70 |
| 62 | 3.46 |
| 100 | 3.27 |
| 200 | 3.09 |
Source: Adapted from [65]
What are the core elements regulators look for in a biologically relevant study?
Regulators evaluate a combination of factors beyond a single p-value. The following table outlines the core components for demonstrating biological relevance.
Table: Core Elements of Biologically Relevant Evidence
| Component | What Regulators Expect |
|---|---|
| Effect Size | A measurable change large enough to influence health, not just a minor decimal shift. |
| Dose-Response | Evidence that higher intake produces stronger or more sustained effects, supporting causality. |
| Population Relevance | Results applicable to healthy or at-risk groups, not just diseased patient cohorts, if the claim is for the general population. |
| Duration & Sustainability | Effects must persist for a duration relevant to the health claim; short-lived biomarker spikes are not convincing. |
| Consistency Across Studies | Reproduction of the effect in multiple independent trials and settings. |
| Mechanistic Plausibility | A clear biological explanation that links the ingredient or process change to the observed effect. |
Source: Summarized from [64] [66]
Troubleshooting Guides
Problem: Inability to Demonstrate Comparability Due to High Batch-to-Batch Variability
Background: Biological products are inherently variable. In a comparability study with limited batches, this natural heterogeneity can mask true differences or create false alarms if acceptance criteria are not set appropriately [51].
Investigation and Solution Strategy:
- Characterize Variability: Use all available historical data to understand the contributions of both analytical variability and true lot-to-lot variability in degradation rates or other key attributes [51].
- Apply Advanced Statistical Models: Use a linear mixed-effects model for your stability or performance data. This model separately accounts for the random variation between batches and the analytical error within batches, providing a more realistic assessment [51].
- Set Equivalence Acceptance Criteria: Define your acceptance margin (Δ) for equivalence testing based on this comprehensive understanding of total variability. The goal is to demonstrate that the difference between the pre-change and post-change average degradation rates is less than this pre-defined, justified margin [51].
- Justify Your Margin: The acceptance margin should be based on the variability observed in historical data from the old process and should represent a difference so small that it would have no adverse impact on the product's safety or efficacy [51].
The following workflow outlines the strategic approach to designing a robust comparability study that can withstand regulatory scrutiny, even with limited batches.
Problem: Investigational Drug Shows Statistical Significance but Lacks Clinical Meaningfulness
Background: This is a common pitfall in early drug development, where a compound shows a statistically significant effect on a biomarker, but the magnitude of change is too small to translate into a patient benefit [66].
Investigation and Solution Strategy:
- Predefine a "Meaningful" Threshold: Before the trial begins, define in the protocol what magnitude of change in the primary outcome is considered biologically or clinically meaningful. This should be based on established clinical cut-offs or recognized risk-reduction benchmarks, not just what is statistically detectable [64].
- Use a Dual-Criterion Design: Design your study and analysis plan to test for both statistical significance and the minimal clinically relevant difference. A result must pass both hurdles to be considered a success [64].
- Select Validated Endpoints: Use biomarkers and endpoints that regulatory authorities have previously recognized as predictive of clinical benefit (e.g., LDL-C for cardiovascular risk, HbA1c for glucose control). Avoid unvalidated surrogate endpoints [64].
- Incorporate Mechanistic Biomarkers: Include secondary, exploratory endpoints that help explain the biological mechanism (e.g., inflammatory cytokines). This adds plausibility and credibility to the primary effect observed [64].
Experimental Protocols for Key Scenarios
Protocol: Designing a Biologically Relevant Dose-Response Study
Objective: To establish a causal relationship and determine the dose required for a biologically meaningful effect.
Methodology:
- Dose Selection: Include at least three dose levels (low, medium, high) plus a placebo/control. The highest dose should be near the maximum tolerated or practically feasible level [64].
- Population: Use a study population relevant to the intended claim (e.g., at-risk but not diseased for a health maintenance claim) [64].
- Duration: The study duration must be long enough for the effect to stabilize and be measured sustainably (e.g., weeks to months for lipid or microbiome changes) [64].
- Primary Analysis: Plot the response against the log of the dose. A statistically significant trend (p<0.05) of increasing effect with increasing dose provides strong evidence for a real biological effect [64].
- Determining Bioactivity: The lowest dose that produces a statistically significant and biologically meaningful effect compared to the control is considered the minimal bioeffective dose.
Protocol: Conducting an Accelerated Stability Comparability Study
Objective: To quickly assess whether a manufacturing process change has altered the degradation profile of a biologic product, using a limited number of pre- and post-change batches [51].
Methodology:
- Study Design: Conduct a side-by-side accelerated stability study on multiple lots from both the old (reference) and new (test) processes. Store samples under stressed conditions (e.g., elevated temperature) [51].
- Testing Time Points: Plan a minimum of three time points (e.g., 0, 1, 2, 3 months) to establish a degradation slope for each lot [51].
- Modeling: For each lot, fit a linear regression model to the stability data (e.g., % purity vs. time) to determine the degradation rate (slope). Use a linear mixed-effects model to analyze the data collectively, accounting for lot-to-lot variability [51].
- Equivalence Testing: Perform an equivalence test to compare the average degradation slopes of the old and new processes. Predefine the equivalence margin (Δ) based on historical variability [51].
- Acceptance Criterion: Comparability is demonstrated if the 90% confidence interval for the difference in mean slopes falls entirely within the pre-specified range of -Δ to +Δ [51].
The Scientist's Toolkit: Essential Reagents & Materials
Table: Key Research Reagent Solutions for Comparability and Biologics Research
| Item | Function / Explanation |
|---|---|
| LanthaScreen TR-FRET Assays | Used for studying kinase activity and protein-protein interactions. The time-resolved fluorescence resonance energy transfer (TR-FRET) technology provides a robust, ratiometric readout that minimizes well-to-well variability [67]. |
| Terbium (Tb) & Europium (Eu) Donors | Lanthanide-based fluorescent donors used in TR-FRET assays. Their long fluorescence lifetime allows for time-gated detection, reducing background interference [67]. |
| cIEF (Capillary Isoelectric Focusing) | An analytical method preferred for characterizing charge variants of proteins (e.g., antibodies). It is quantitative and provides high-resolution separation of different glycoforms or degraded species [33]. |
| Orthogonal Analytical Methods | Using multiple different methods (e.g., cIEF, ion-exchange chromatography, mass spectrometry) to measure the same quality attribute. This strengthens comparability conclusions by providing a comprehensive quality profile [33]. |
| Validated Biomarker Panels | Sets of biomarkers (e.g., for oxidative stress, inflammation) that are recognized by regulatory bodies as being predictive of a health outcome. Their use strengthens the biological relevance of a study [64]. |
| Forced Degradation Reference Standards | Materials intentionally degraded under controlled conditions (e.g., heat, light, pH). They are used as controls in stability studies to understand degradation pathways and validate analytical methods [33]. |
Frequently Asked Questions
Q1: With a limited number of batches, how can we objectively demonstrate that a process change did not adversely impact product stability? A primary method is through statistical equivalence testing of the stability slopes (degradation rates) from the pre-change and post-change processes [68]. This approach uses a pre-defined Equivalence Acceptance Criterion (EAC). The 90% confidence interval for the difference in average slopes between the two processes is calculated. If this entire interval falls within the range of –EAC to +EAC, statistical equivalence is demonstrated [68]. This method controls the consumer's risk (type 1 error) at 5%, providing strong objective evidence of comparability even with limited data [68].
Q2: Our study has low statistical power due to few batches. Are there alternative methods to evaluate stability comparability? Yes, the Quality Range Test is a valuable heuristic approach, especially for small studies [69]. It involves calculating the mean and standard deviation of the slopes from the pre-change (reference) batches. A quality range is then established, typically as the mean ± 3 standard deviations. If the slopes from all the post-change batches fall within this quality range, the two processes are considered comparable [69]. This method provides a straightforward, visual way to assess comparability.
Q3: How does between-batch variability affect comparability conclusions, and how can we account for it? Neglecting between-batch variability can significantly impact bioequivalence conclusions. High between-batch variability can inflate the total variability, making it harder to prove equivalence and increasing the risk of both false positive and false negative conclusions [70]. The Between-Batch Bioequivalence (BBE) method is designed to account for this by incorporating the batch effect directly into its statistical model, comparing the mean difference between products to the reference product's between-batch variability [70]. This can provide a more accurate assessment of comparability for variable products.
Q4: For forced degradation studies, how can we get more informative data from a limited number of samples? Instead of a traditional one-factor-at-a-time approach, use a Design of Experiments (DoE) methodology [71]. By strategically combining multiple stress factors (e.g., temperature, pH, light) in a single experiment, DoE creates a wider variation in degradation profiles. This reduces correlation between co-occurring modifications and allows for a more robust statistical analysis, leading to clearer structure-function relationship insights from a constrained set of experiments [71].
Troubleshooting Guides
Problem: Inconclusive Result in Statistical Equivalence Test Your confidence interval straddles the EAC boundary [68].
- 1. Understand the Result: An inconclusive result (Scenario B in Figure 1) means there is not enough evidence to prove or disprove equivalence. It does not mean the processes are different [68].
- 2. Investigate Root Causes:
- High Variability: Review your data for high variability within or between batches, which widens the confidence interval.
- Inadequate Sample Size: The number of batches or time points may be insufficient to shrink the confidence interval.
- 3. Implement Corrective Actions:
- Collect More Data: The primary solution is to increase the sample size. Additional data will narrow the confidence interval, leading to a conclusive result [68].
- Re-evaluate the EAC: Ensure your Equivalence Acceptance Criterion is scientifically justified and reflects practical importance.
Problem: Inability to Reproduce a Stability Indicating Method The method performance is inconsistent when transferred to a new site or analyst.
- 1. Understand the Problem: Inconsistency can stem from unaccounted for variations in analytical procedure, equipment, or environmental conditions.
- 2. Isolate the Issue:
- Gather Information: Collect logs, instrument calibration records, and raw data from both the original and problematic runs [72].
- Reproduce the Issue: Attempt to replicate the problem in a controlled environment to confirm its root cause [72].
- Remove Complexity: Simplify the method to its core steps. Systematically reintroduce components (e.g., specific sample preparation steps, mobile phase additives) to identify which one causes the failure [72].
- 3. Find a Fix:
- Compare to a Working Version: Compare all parameters (pH, temperature, flow rate, column lot) side-by-side with a setup that works reliably [72].
- Document and Standardize: Once the critical parameter is identified, document it clearly in the method protocol and train all personnel.
Problem: High Between-Batch Variability Obscures Comparability The variability among batches of the same product is so high that it masks any true difference or similarity between the pre-change and post-change products.
- 1. Understand the Problem: High between-batch variability increases the noise in your data, reducing the statistical power to detect equivalence [70].
- 2. Investigate Root Causes:
- Process Understanding: Examine the manufacturing process for steps with poor control that could lead to batch-to-batch differences.
- Raw Materials: Investigate the variability of incoming raw materials or active pharmaceutical ingredients.
- 3. Implement Corrective Actions:
- Use BBE Testing: Consider using the Between-Batch Bioequivalence method, which is designed to handle this specific situation more effectively than traditional tests [70].
- Process Improvement: Focus on tightening the control of the manufacturing process to reduce the fundamental source of variability.
The table below summarizes the pros, cons, and applications of different statistical methods for stability comparability, particularly when dealing with a limited number of batches.
| Method | Key Principle | Advantages | Disadvantages/Limitations | Suitable for Low Batch Numbers? |
|---|---|---|---|---|
| Statistical Equivalence Testing [68] | Tests if the confidence interval for the difference in slopes is within a pre-set EAC. | Strong objective evidence; controls type 1 (consumer) risk. | Can be inconclusive with high variability or low sample size; requires statistical expertise. | Yes, but power may be low. |
| Quality Range Test [69] | Checks if all post-change batch slopes fall within the distribution of pre-change batch slopes. | Simple, visual, heuristic; good for small studies. | Less statistically rigorous; may have higher false positive rate. | Yes, designed for few batches (e.g., 3). |
| Between-Batch Bioequivalence (BBE) [70] | Compares the mean difference between products to the reference's between-batch variability. | Accounts for batch variability; can be more efficient for variable products. | Less established in some regulatory guidances; requires nested statistical model. | More efficient than ABE/PBE in this context. |
Experimental Protocol: Statistical Equivalence Testing for Stability Profiles
This protocol outlines the steps to demonstrate comparability using equivalence testing, as recommended by ICH Q5E [68].
1. Objective To demonstrate that the average degradation rate (slope) of a performance attribute (e.g., potency, purity) for a new or post-change manufacturing process is statistically equivalent to that of the historical or pre-change process.
2. Pre-Study Steps
- Step 1: Establish the Equivalence Acceptance Criterion (EAC) [68]: The EAC is the largest difference in slopes considered practically unimportant. It should be justified based on:
- Scientific knowledge of the critical quality attribute.
- Clinical experience with the product.
- The observed variability among historical batch slopes [68].
- Step 2: Study Design and Sample Size [68]:
- Design: Typically, a linear regression is performed for each lot, measuring a stability-indicating attribute at multiple time points (e.g., 0, 3, 6, 9, 12 months).
- Sample Size: The number of lots (batches) from both the pre-change and post-change processes should be determined by a power analysis to control the type 2 error (manufacturer's risk). With a type 1 error of 5%, a common design uses 3-4 lots per process [68].
3. Data Analysis
- Step 3: Compute the Test [68]:
- Calculate the least squares slope for each individual lot.
- Compute the average slope for the pre-change process (( \bar{b}{Historic} )) and the post-change process (( \bar{b}{New} )).
- Calculate the two-sided 90% confidence interval for the difference in average slopes (( \bar{b}{Historic} - \bar{b}{New} )).
- Step 4: Interpret the Results [68]:
- Pass: If the entire 90% confidence interval lies within –EAC and +EAC, equivalence is demonstrated.
- Inconclusive: If the interval straddles an EAC boundary.
- Fail: If the entire interval falls outside the –EAC to +EAC range.
Experimental Workflow: Comparability Study with Limited Batches
The diagram below outlines the logical workflow for planning and executing a successful comparability study under batch constraints.
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below details key materials and their functions in stability and comparability studies.
| Item / Reagent | Function in Stability & Comparability Studies |
|---|---|
| Reference Product Batches | Serves as the pre-change benchmark for comparing the stability profile of the new process or test product [68] [70]. |
| Well-Characterized Forced Degradation Samples | Intentionally degraded samples used to validate the stability-indicating power of analytical methods and understand potential degradation pathways [71]. |
| Stressed Stability Study Materials | Materials placed under accelerated conditions (e.g., high temperature/humidity) to quickly generate degradation data for comparison [69]. |
| Design of Experiments (DoE) Software | Enables the efficient design of forced degradation studies by combining multiple stress factors, maximizing information gain from a limited number of experiments [71]. |
| Statistical Analysis Software | Essential for performing complex statistical tests like equivalence testing, quality range, and BBE analysis to objectively demonstrate comparability [68] [70]. |
When is More Needed? Justifying the Need for Non-Clinical or Clinical Bridging Studies
FAQ: Navigating Bridging Studies in Comparability Research
1. What is the primary goal of a comparability study, and when is it considered successful?
The goal of a comparability study is to determine if a change in the manufacturing process has any adverse effects on the product's quality, safety, or effectiveness [30]. It is successful if it can demonstrate that the product after the change is highly similar to the product before the change, and that existing non-clinical and clinical data remain relevant [30]. Success does not always require the quality characteristics to be identical, but it must be shown that any differences do not adversely affect safety or efficacy [30].
2. Under what conditions are bridging studies typically required?
Bridging studies are required when a comparability study of quality attributes (identity, purity, potency) reveals significant differences that are expected to impact safety or efficacy [30]. The need is determined through a science-driven risk assessment that considers the extent of the manufacturing change and the potential impact on the product [15]. The table below summarizes common scenarios.
| Scenario Requiring Bridging Studies | Type of Bridging Study Typically Needed |
|---|---|
| A new product has lower systemic exposure (Cmax/AUC) than the listed drug [73] | Additional Phase 2 and/or Phase 3 efficacy studies [73] |
| A new product has higher systemic exposure (Cmax/AUC) than the listed drug [73] | Additional nonclinical safety studies (e.g., toxicology) [73] |
| Change in the route of administration [73] | Nonclinical and/or clinical local tolerability studies [73] |
| A change in the drug's indication or target patient population [73] | Clinical safety and/or efficacy studies in the new indication/population [73] |
| A major change, such as a cell line change for a biologic [30] | GLP toxicology studies and/or human clinical bridging studies [30] |
3. For a 505(b)(2) application, is it ever possible to avoid clinical trials?
Yes, in some cases. While many 505(b)(2) applications include a Phase 1 bioavailability/bioequivalence (BA/BE) study, it is possible to avoid clinical trials through innovative nonclinical strategies [74]. This can be accomplished by leveraging specific information in the published literature or by designing targeted animal or in-vitro studies that establish the necessary scientific bridge to the existing approved product [74].
4. How does the number of batches available impact a comparability study?
The number of batches used in a comparability study should be justified based on the product's development stage and the type of manufacturing change [30]. With limited batches, sponsors can use a science- and risk-based assessment to justify a reduced number. For major changes, ≥3 batches are generally recommended; for medium changes, 3 batches; and for minor changes, ≥1 batch may suffice [30]. Using a bracketing or matrix approach can also help reduce the number of batches needed [30].
5. What are the key analytical tests used to establish product comparability?
A combination of routine release tests and extended characterization is used. The tests chosen should reflect the product's Critical Quality Attributes (CQAs), particularly those linked to its mechanism of action [15]. Potency assays are especially critical [15].
The following table outlines key analytical methods and their purposes in comparability assessments [30].
| Test Parameter | Example Detection Items | Purpose in Comparability |
|---|---|---|
| Purity & Size Variants | SEC-HPLC; CE-SDS (reduced & non-reduced) | Quantifies aggregates, fragments, and other product-related impurities to ensure purity and structural integrity. |
| Identity & Structure | Peptide Map; LC-MS | Confirms primary amino acid sequence and identifies post-translational modifications (e.g., oxidations). |
| Charge Variants | iCIEF; IEC-HPLC | Analyzes charge heterogeneity of the product, which can impact stability and activity. |
| Potency & Function | Cell-based bioassays; Binding affinity assays | Measures the biological activity of the product, which is critical for demonstrating equivalent efficacy. |
| Process-Related Impurities | HCP (ELISA); DNA (ELISA); Protein A (ELISA) | Ensures consistent and adequate removal of process-related impurities across the manufacturing change. |
Troubleshooting Guide: A Systematic Path to Bridging Study Decisions
This workflow provides a structured, risk-based approach for determining when analytical comparability is sufficient or when bridging studies are needed. It synthesizes recommendations from regulatory guidance and industry best practices [15] [30] [75].
Step 1: Conduct a Risk Assessment Before testing, evaluate the magnitude of the manufacturing change and its potential to affect the product's Critical Quality Attributes (CQAs) [15] [30]. Consider factors such as the complexity of the change (e.g., site transfer vs. cell line change) and your understanding of the product's mechanism of action. This assessment will define the scope and depth of the required analytical studies [30].
Step 2: Design the Analytical Comparability Study Execute a head-to-head comparison of pre- and post-change batches using a suite of analytical methods that cover identity, purity, potency, and safety [30]. The specific methods should be chosen based on the risk assessment. It is critical to establish prospective acceptance criteria for these tests based on historical data and biological relevance [15] [30].
Step 3: Evaluate the Results and Decide on Next Steps
- If attributes are comparable: You have successfully established analytical comparability. Proceed to compile the data for regulatory submission [30].
- If significant differences are found: You must determine if these differences are biologically meaningful and likely to impact the safety or efficacy of the product [15]. Statistically significant differences may not always be biologically relevant.
Step 4: Justify and Execute Bridging Studies If analytical differences are deemed to pose a potential risk, bridging studies are required. The type of study depends on the nature of the risk [73]:
- For potential efficacy concerns: Clinical efficacy studies (Phase 2/3) may be needed.
- For potential safety concerns: Nonclinical studies (e.g., toxicology) or clinical safety studies may be needed. Engage with regulatory agencies early to seek alignment on the proposed bridging strategy [15].
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials and reagents critical for conducting a thorough analytical comparability assessment.
| Reagent / Material | Critical Function in Comparability Studies |
|---|---|
| Reference Standards | Serves as a benchmark for analyzing the pre-change product; essential for head-to-head comparisons in assays [30]. |
| Cell Lines for Bioassays | Used in potency assays to measure the biological activity of the product, a critical quality attribute [15]. |
| Characterized Antibodies | Used for identity testing (e.g., peptide mapping), purity analysis (e.g., CE-SDS), and detecting impurities (e.g., HCP ELISA) [30]. |
| Cryopreserved Samples | Preserved samples from pre-change batches are vital for running concurrent, head-to-head analytical tests to ensure a fair comparison [30]. |
| Stability Study Materials | Containers and conditions (e.g., temperature, light) for real-time, accelerated, and forced degradation studies to compare degradation profiles [30]. |
Frequently Asked Questions (FAQs)
Q: What is the primary goal of a comparability study? A: The goal is to provide assurance that a manufacturing change does not adversely impact the identity, purity, potency, or safety of the drug product. A successful study demonstrates that the pre-change and post-change products are highly similar and that the existing clinical data remains applicable [15].
Q: Why is early engagement with regulators on comparability strategy critical? A: Early engagement allows sponsors to align with regulators on the study design, acceptance criteria, and analytical methods before conducting the studies. This proactive approach de-risks clinical development timelines by preventing potential delays due to non-conforming strategies and builds regulatory confidence [15].
Q: What is the difference between a prospective and a retrospective comparability study? A:
- Prospective studies are designed to support a future manufacturing change. They often use split-stream or side-by-side analysis and are typically not formally statistically powered. They help de-risk development delays but require more resources [15].
- Retrospective studies are conducted after a change has been made, analyzing historical product data to support the pooling of clinical data across batches. They usually require formal statistical powering and involve less resource expenditure but carry a higher risk to development timelines [15].
Q: How should acceptance criteria for critical quality attributes (CQAs) be set? A: Acceptance criteria should be based on a thorough risk assessment and tied to biological meaning. They can be set using quality ranges or equivalence testing, but it is crucial that statistically significant differences are evaluated for their biological relevance. The criteria should be justified by process understanding and prior knowledge [15].
Q: What is the role of potency assays in comparability? A: Potency assays are a critical component of any comparability strategy. They should ideally reflect the product's known or proposed mechanism of action (MOA). A matrix of candidate potency assays should be developed early, with the final selection driven by the MOA and considerations for assay robustness [15].
Troubleshooting Guide: Navigating Common Comparability Challenges
Q: Our comparability study revealed a statistically significant but small difference in a non-critical attribute. What should we do? A:
- Assess Biological Relevance: Determine if the difference is biologically meaningful. A statistically significant difference may not be clinically relevant [15].
- Review Acceptance Criteria: Ensure your pre-defined acceptance criteria for this attribute were risk-based and phase-appropriate.
- Leverage Product Knowledge: Use our extensive product knowledge to justify that the difference does not impact safety or efficacy. A strong, science-driven narrative is key to defending this position to regulators [15].
Q: We have limited batch data for a comparability assessment. How can we strengthen our study? A:
- Utilize All Available Data: Leverage data from development batches and any retains you have saved [15].
- Focus on CQAs: Concentrate the assessment on Critical Quality Attributes (CQAs) most likely to be impacted by the manufacturing change.
- Employ Statistical Methods Wisely: Consider statistical approaches suitable for small sample sizes, clearly documenting the rationale for your chosen method [15].
- Engage Regulators Early: Proactively discuss the limited data set and your proposed approach with regulators to gain alignment [15].
Q: How do we investigate an unexpected failure in a comparability study? A:
- Understand the Problem: Confirm the failure by re-testing if sample allows. Review all analytical data for that batch and the manufacturing batch record for any deviations [72].
- Isolate the Issue:
- Remove Complexity: Investigate if the issue is isolated to a single unit operation, a specific raw material, or an analytical method [72].
- Change One Thing at a Time: Systematically investigate potential root causes individually to pinpoint the exact factor responsible [72].
- Compare to a Working Model: Compare the failing batch data against multiple successful batches to identify key discrepancies [72].
- Find a Fix:
- Based on the root cause, you may need to modify the manufacturing process, optimize an analytical method, or revise your acceptance criteria.
- Document the investigation thoroughly and update your risk assessment.
- Communicate the findings and proposed path forward transparently with regulators [15].
Data Presentation: Comparability Study Metrics
Table 1: Key Statistical Approaches for Comparability Analysis
| Statistical Method | Description | Best Use Case | Considerations |
|---|---|---|---|
| Equivalence Test | Determines if the mean difference between two groups falls within a specified equivalence margin. | Confirming that a CQA has not changed beyond a pre-defined, clinically relevant limit. | Requires a scientifically justified equivalence margin. Often used for potency assays. |
| Quality Range | Evaluates if the results for the post-change batches fall within the distribution (e.g., ±3σ) of the pre-change batches. | Assessing multiple CQAs when a historical data pool is available. | Simpler to implement but may be less sensitive than equivalence testing for critical attributes. |
| Hypothesis Testing (t-test) | Tests the null hypothesis that there is no difference between the means of two groups. | Identifying a statistically significant difference in a given attribute. | A significant p-value does not automatically imply a biologically or clinically meaningful difference [15]. |
Table 2: Essential Elements of a Proactive Comparability Plan
| Plan Element | Description | Rationale |
|---|---|---|
| Proactive Planning | Planning for potential manufacturing changes before initiating pivotal clinical trials. | Prevents delays and ensures sufficient, representative pre-change material is available for side-by-side testing [15]. |
| Risk Assessment | A science-based assessment of the impact of a manufacturing change on CQAs. | Focuses the comparability study on the attributes that matter most for product safety and efficacy [15]. |
| Analytical Method Suitability | Ensuring methods are validated and capable of detecting differences in product quality. | Forms the foundation of a credible comparability study. Inadequate methods can lead to false conclusions. |
| Retain Strategy | A policy for storing sufficient quantities of drug product and drug substance batches. | Provides crucial material for future analytical development and unforeseen comparability testing needs [15]. |
Experimental Protocol: Framework for a Comparability Study
Objective: To demonstrate the comparability of a drug product before and after a specified manufacturing process change.
Methodology:
- Protocol Development:
- Develop a prospective study protocol defining the scope, batches to be tested, analytical methods, and acceptance criteria [15].
- The acceptance criteria must be justified based on risk to patient and product quality.
Batch Selection:
- Select a sufficient number of pre-change and post-change batches to provide statistical confidence, acknowledging the challenges of limited batch numbers in CGT [15].
- Batches should be representative of the manufacturing process.
Testing Strategy:
- Execute a tiered testing approach focusing on:
- Tier 1 (Critical): High-resolution, orthogonal methods for CQAs directly linked to the MOA (e.g., potency).
- Tier 2 (Qualifying): Methods for broader characterization of identity and purity.
- The analytical panel should be comprehensive and reflect the product's complexity.
- Execute a tiered testing approach focusing on:
Data Analysis and Reporting:
- Analyze data using pre-defined statistical methods as outlined in Table 1.
- Prepare a comprehensive report that includes a scientific rationale for the change, a summary of the study, and a conclusion on comparability.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Cell and Gene Therapy Comparability Studies
| Reagent / Material | Function in Comparability Studies |
|---|---|
| Characterized Cell Bank | Provides a consistent and well-defined starting material, reducing variability in the comparability assessment. |
| Critical Quality Attribute (CQA)-Specific Assays | Analytical methods (e.g., flow cytometry, ELISA, qPCR) used to measure specific attributes critical to product function and safety. |
| Potency Assay Reagents | Essential components (e.g., specific antibodies, reporter cells, substrates) for assays that measure the biological activity of the product, which is central to comparability [15]. |
| Reference Standard | A well-characterized material used as a benchmark to qualify assays and ensure consistency of results across different testing rounds. |
Visualization: Comparability Study Workflow
Comparability Study Workflow
Visualization: Tiered Analytical Testing Strategy
Tiered Analytical Testing Strategy
Conclusion
Successfully navigating comparability with limited batches is not about proving two products are identical, but about building a scientifically rigorous and phase-appropriate narrative that demonstrates a high level of similarity with no adverse impact on safety or efficacy. The key to this lies in a proactive, risk-based strategy that begins early in development, leverages deep product and process understanding, and employs a robust analytical toolbox. As the landscape for biologics and advanced therapies continues to evolve, embracing a data-centric mindset, exploring innovative approaches like scale-out manufacturing, and engaging in early dialogue with regulators will be paramount. By adopting these principles, developers can transform comparability from a daunting regulatory hurdle into a strategic enabler that supports process improvements, accelerates development timelines, and ultimately brings transformative treatments to patients faster and more reliably.
References
- 1. Demonstration of Comparability of Human Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/demonstration-comparability-human-biological-products-including-therapeutic-biotechnology-derived]
- 2. Considerations For AVV Analytical Comparability Studies For ... [https://www.cellandgene.com/doc/considerations-for-avv-analytical-comparability-studies-for-products-with-low-batch-numbers-0001]
- 3. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 4. Comparability: manufacturing, characterization and controls ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5422032/]
- 5. The Pitfalls and Promise of Cell and Gene Therapy ... [https://globalforum.diaglobal.org/issue/november-2025/the-pitfalls-and-promise-of-cell-and-gene-therapy-development-a-time-for-concerted-action/]
- 6. Small-Batch Manufacturing for Phase 1 Clinical Trials in 2025 [https://www.sofpromed.com/small-batch-manufacturing-for-phase-1-clinical-trials]
- 7. No Batch Too Small: Choosing the Right Fill-Finish CDMO ... [https://www.sharpservices.com/expert-content/no-batch-too-small-choosing-the-right-fill-finish-cdmo-for-small-scale-batches/]
- 8. Assessment of Product Variety Complexity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9857747/]
- 9. Exploring the challenges faced by generic version of complex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482112/]
- 10. ICH Q5E Biotechnological/biological products subject to ... [https://www.ema.europa.eu/en/ich-q5e-biotechnological-biological-products-subject-changes-their-manufacturing-process-comparability-biotechnological-biological-products-scientific-guideline]
- 11. Assessing and mitigating batch effects in large-scale omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447944/]
- 12. Innovative Designs for Clinical Trials of Cellular and Gene ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/innovative-designs-clinical-trials-cellular-and-gene-therapy-products-small-populations]
- 13. Are batch effects still relevant in the age of big data? [https://www.sciencedirect.com/science/article/pii/S0167779922000361]
- 14. Critical Quality Attributes (CQAs): Know Their Importance & ... [https://www.roosterbio.com/blog/critical-quality-attributes-cqas-know-their-importance-limitations-in-product-process-development/]
- 15. The comparability tales: A phase-appropriate roadmap for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10805933/]
- 16. What are Critical Process Parameters (CPPs)? [https://www.hamiltoncompany.com/knowledge-base/article/what-are-critical-process-parameters-cpps?srsltid=AfmBOoqAfLl0RpwLVyupHhpBiwyH3xqBx2Jk2xFGvInwBrk7xDgafzgD]
- 17. How do Critical Process Parameters (CPPs) ... [https://www.linkedin.com/pulse/how-do-critical-process-parameters-cpps-quality-cqas-qa-weisbrot-gqmqe]
- 18. Critical process parameters [https://en.wikipedia.org/wiki/Critical_process_parameters]
- 19. Batch‐to‐batch pharmacokinetic variability confounds ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5102576/]
- 20. Generic dry powder inhalers bioequivalence: Batch–to- ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622003439]
- 21. Performance of Multiple-Batch Approaches to ... [https://link.springer.com/article/10.1208/s12249-021-02063-1]
- 22. Variability and impact on design of bioequivalence studies [https://pubmed.ncbi.nlm.nih.gov/20041877/]
- 23. The bioequivalence study design recommendations for ... [https://www.frontierspartnerships.org/journals/journal-of-pharmacy-pharmaceutical-sciences/articles/10.3389/jpps.2024.12398/full]
- 24. Sample size determination in bioequivalence studies using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6783617/]
- 25. Batch Effect Adjustments • batchtma - Konrad Stopsack [https://stopsack.github.io/batchtma/]
- 26. Cohort Prospective Design: Study & Examples Definition [https://www.simplypsychology.org/prospective-study.html]
- 27. Assessing and mitigating batch effects in large-scale omics ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 28. Influence of batch effect correction methods on drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6706913/]
- 29. 6 Types of Risk Assessment Methodologies + How to Choose [https://drata.com/grc-central/risk/risk-assessment-methodologies]
- 30. Comparability study Summary of Biologics ... [https://www.bestchrom.com/comparability-study-summary-of-biologics-comparability-studies/]
- 31. 2021 Volume 2 Risk Assessment and Analysis Methods [https://www.isaca.org/resources/isaca-journal/issues/2021/volume-2/risk-assessment-and-analysis-methods]
- 32. Understanding comparability studies for biologics [https://mmsholdings.com/perspectives/comparability-studies-biologics-importance/]
- 33. Analytical comparability study of recombinant monoclonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5973765/]
- 34. mAb Therapies: Reducing Costs and Accelerating Timelines [https://www.bioprocessintl.com/monoclonal-antibodies/reducing-costs-and-accelerating-timelines-with-tools-for-physicochemical-characterization-of-mab-therapies]
- 35. I-optimal design of split-plot mixture-process variable ... [https://www.sciencedirect.com/science/article/abs/pii/S0950329322000957]
- 36. Split-Plot Design Optimization: A Guide for Manufacturing [https://www.linkedin.com/advice/0/how-do-you-optimize-allocation-resources-costs]
- 37. Cell and Gene Therapy Product Comparability Strategies [https://www.bioprocessintl.com/cell-therapies/comparability-for-cell-and-gene-therapy-products-a-challenge-and-an-opportunity]
- 38. The Ultimate Guide to Data Integration in Manufacturing [https://www.netsuite.com/portal/resource/articles/erp/data-integration-manufacturing.shtml]
- 39. Deep Batch Active Learning for Drug Discovery [https://elifesciences.org/reviewed-preprints/89679]
- 40. Repeating tests: different roles in research studies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3651832/]
- 41. A practical approach to estimate analytical method ... [https://www.sciencedirect.com/science/article/pii/S0731708524003844]
- 42. How To Reduce Batch-to-Batch Variation In Cell Therapy ... [https://www.cellandgene.com/doc/how-to-reduce-batch-to-batch-variation-in-cell-therapy-manufacturing-0001]
- 43. Easy Proteomics Sample Preparation [https://pubmed.ncbi.nlm.nih.gov/41132037/]
- 44. 欧美监管机构发布突破性治疗申请的CMC和GMP联合问答文件 [https://www.phirda.com/artilce_33708.html?cId=1]
- 45. doe数据结果怎么分析 [https://www.fanruan.com/blog/article/1315883/]
- 46. Three Types of Scaling in the Cloud - Coding Out Loud [https://blog.codingoutloud.com/2010/07/27/three-types-of-scaling-in-the-cloud-scale-up-scale-out-and-now-scale-side-by-side-with-juxtaposition-scaling/]
- 47. Scale Up vs Scale Out: What is the Difference? [https://portworx.com/blog/scale-up-vs-scale-out/]
- 48. Scale-out vs. Scale-up: What's the Difference? [https://blog.purestorage.com/purely-educational/scale-out-vs-scale-up-whats-the-difference/]
- 49. Measurement batch differences and between‐ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8144935/]
- 50. Scale Out vs Scale Up: Key Differences Explained [https://synchronet.net/scale-out-vs-scale-up/]
- 51. Determination of acceptance criteria and sample sizes for ... [https://www.sciencedirect.com/science/article/abs/pii/S1045105617300891]
- 52. Process Performance Qualification Runs [https://www.bioprocessintl.com/cell-line-development/process-validation-calculating-the-necessary-number-of-process-performance-qualification-runs]
- 53. Running and Troubleshooting Batch Processing [https://docs.oracle.com/en/industries/energy-water/shared/22b/cs-live-ops-guide/CS_LIVE_OPS_22B/Cloud_Live_Operate_Troubleshooting.7.3.html]
- 54. The Top 20 Problems with Batch Processing (and How to ... [https://www.kai-waehner.de/blog/2025/04/01/the-top-20-problems-with-batch-processing-and-how-to-fix-them-with-data-streaming/]
- 55. Batch Data Processing: Challenges and Limitations in Real ... [https://www.linkedin.com/advice/1/what-challenges-limitations-batch-data-processing]
- 56. Batch Processing Demystified: Tools, Challenges, and ... [https://www.acceldata.io/blog/batch-processing-demystified-tools-challenges-and-solutions]
- 57. Stream Processing vs. Batch Processing: Benefits and ... [https://edgedelta.com/company/blog/stream-processing-vs-batch-processing]
- 58. Batch Processing: 4 Tactics To Make It Cost-Efficient and ... [https://cast.ai/blog/batch-processing-4-tactics-to-make-it-cost-efficient-and-reliable/]
- 59. A Primer on the Use of Equivalence Testing for Evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5856600/]
- 60. 9 Equivalence Testing and Interval Hypotheses - GitHub Pages [https://lakens.github.io/statistical_inferences/09-equivalencetest.html]
- 61. What to do when data is not normally distributed in statistics [https://www.statsig.com/perspectives/dealing-non-normal-data-stats]
- 62. 6.5.2. What do we do when data are non-normal [https://www.itl.nist.gov/div898/handbook/pmc/section5/pmc52.htm]
- 63. 8. Techniques for Dealing with Non-Normal, Categorical, and ... [https://openbooks.library.unt.edu/quantitative-analysis-exss/chapter/nonparametric-techniques-for-dealing-with-non-normal-data/]
- 64. Beyond P-Values: How EFSA assesses biological ... [https://www.nutritionaloutlook.com/view/beyond-p-values-how-efsa-assesses-biological-relevance-in-nutraceutical-trials]
- 65. Setting Acceptance Criteria from Statistics of the Data [https://www.biopharminternational.com/view/specification-setting-setting-acceptance-criteria-statistics-data]
- 66. Defining benefit: Clinically and biologically meaningful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11848336/]
- 67. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/hk/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 68. Demonstrating Comparability of Stability Profiles Using ... [https://www.biopharminternational.com/view/demonstrating-comparability-stability-profiles-using-statistical-equivalence-testing]
- 69. Comparability in Accelerated or Stressed Stability Studies ... [https://www.pharmtech.com/view/comparability-in-accelerated-or-stressed-stability-studies-using-a-quality-range]
- 70. Between-Batch Bioequivalence (BBE): a Statistical Test to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7651657/]
- 71. Advancing forced degradation studies: Design of ... [https://www.sciencedirect.com/science/article/pii/S093964112500164X]
- 72. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 73. 505(b)(2) Bridging Studies| Rho - RhoWorld [https://www.rhoworld.com/505b2-bridging-studies/]
- 74. 505(b)(2) FAQs Part 2: Clinical And Nonclinical Studies [https://premierconsulting.com/resources/blog/back-to-basics-505b2-faqs-part-2-clinical-and-nonclinical-studies/]
- 75. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOorcAoA--9YPzjbF8yGDZzbuxOQGsi5Z2yYoIgLISM9Ss84x4YuM]