PCR vs. Culture for Mycoplasma Testing: A Strategic Guide for Biopharmaceutical Quality Control
This article provides a comprehensive analysis for researchers and drug development professionals on selecting between PCR and culture-based methods for mycoplasma testing.
PCR vs. Culture for Mycoplasma Testing: A Strategic Guide for Biopharmaceutical Quality Control
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on selecting between PCR and culture-based methods for mycoplasma testing. It covers the foundational principles of mycoplasma contamination and its risks, delves into the methodological workflows of PCR and culture techniques, and offers troubleshooting strategies for optimization. A detailed validation framework is presented to guide method selection and compliance with global pharmacopeia standards, empowering scientists to implement robust, efficient testing protocols that ensure product safety and accelerate biopharmaceutical development.
Mycoplasma Contamination: Understanding the Invisible Threat to Cell Cultures and Biologics
Mycoplasma species represent a significant and unique challenge in biomedical research and biopharmaceutical production. As the smallest known free-living organisms, their size and absence of a rigid cell wall make them a pervasive threat to cell cultures, with contamination rates estimated between 15% and 35% for continuous cultures [1] [2]. This contamination can lead to costly batch failures, product recalls, and poses potential risks to patient safety [1]. Furthermore, in clinical settings, Mycoplasma pneumoniae is a common cause of pediatric community-acquired pneumonia, and the global rise of macrolide-resistant strains is complicating treatment strategies [3] [4] [5]. This guide objectively compares the performance of PCR-based and culture-based methods for detecting these elusive contaminants, providing critical data to help researchers, scientists, and drug development professionals safeguard their work.
Unpacking the Threat: Mycoplasma's Distinctive Biology
The unique risk profile of Mycoplasma is a direct consequence of its fundamental biology, which differentiates it from typical bacterial contaminants.
Size and Filterability: Mycoplasmas are remarkably small, with diameters ranging from 0.1 to 0.3 µm [2]. This diminutive size, coupled with their metabolic activity, allows them to passively penetrate the 0.2 µm filters commonly used to sterilize cell culture media and biopharmaceutical products, providing a direct route for contamination [2].
Lack of a Cell Wall: Unlike most bacteria, Mycoplasmas lack a rigid cell wall. This makes them naturally resistant to a broad class of common antibiotics, including beta-lactams (e.g., penicillin), which target cell wall synthesis [2] [5]. This trait necessitates the use of different classes of antibiotics for treatment, such as macrolides, which target protein synthesis [5].
Stealth and Impact: Their small size and plastic morphology make them difficult to detect by conventional optical microscopy. They do not cause the visible turbidity in culture media typical of other bacterial contaminants. However, they can profoundly alter the function and metabolism of infected cell cultures, compromising research data and the safety of biologically derived products [1] [2].
Comparative Methodologies: PCR vs. Culture for Mycoplasma Testing
The two primary methods for Mycoplasma detection are culture-based techniques, the historical gold standard, and PCR-based molecular tests. The experimental protocols and key differentiators are outlined below.
Experimental Protocols in Practice
Protocol 1: Culture-Based Method The culture-based method relies on cultivating the organism in specialized media. A typical protocol, as used in clinical isolate studies, involves the following steps [3]:
- Sample Inoculation: Clinical specimens (e.g., throat swabs) are immediately inoculated into a nutrient-rich PPLO broth, supplemented with horse serum, yeast extract, and antibiotics to inhibit competing flora.
- Incubation and Monitoring: Cultures are incubated at 37°C with 5% CO₂ for 2–3 weeks. Due to slow growth and lack of turbidity, cultures are monitored for a color change (red to yellow) of a phenol red pH indicator, signifying acid production from glucose metabolism.
- Subculture and Identification: Positive broths are subcultured onto solid PPLO agar and incubated for an additional 1–2 weeks. Colonies are examined microscopically for the characteristic "fried-egg" appearance.
- Antimicrobial Susceptibility Testing (AST): Using a multiple dilution method, isolates are tested against a panel of antibiotics (e.g., macrolides, tetracyclines, quinolones) to determine the Minimum Inhibitory Concentration (MIC) and assess resistance profiles [3].
Protocol 2: PCR-Based Method (PCR-MALDI-TOF MS) Advanced molecular techniques combine PCR with mass spectrometry for high-throughput genotyping. A detailed protocol is described as follows [3]:
- Nucleic Acid Extraction: DNA is extracted from purified isolates, quantified (e.g., to 12–83 ng/μL using Qubit 3.0), and diluted in nucleic acid-free water as a negative control.
- Multiplex PCR Amplification: A 5 µL reaction volume is prepared containing DNA template, PCR buffer, and a primer mixture. Amplification conditions include initial denaturation at 95°C for 15 min, followed by 30 cycles of denaturation (95°C for 15 s), annealing (59°C for 30 s), and extension (72°C for 30 s).
- Post-PCR Treatment: PCR products are treated with Shrimp Alkaline Phosphatase (SAP) to remove free dNTPs.
- Mass Probe Extension (MPE): An MPE mixture containing primers, enzymes, and termination nucleotides (E-ddNTPs) is added to the SAP-treated products. Thermocycling is performed to conduct a single base pair extension.
- Salt Purification and Analysis: The products are purified with resin and ultrapure water. The supernatant is mixed with a chemical matrix (3-HPA) and crystallized for analysis.
- SNP Identification: The purified samples are tested using a MALDI-TOF MS system (e.g., QuanTOF I). The resulting mass spectra are analyzed to identify single-nucleotide polymorphisms (SNPs) associated with antibiotic resistance, such as mutations in the 23S rRNA gene [3].
Side-by-Side Performance Comparison
The following table summarizes the critical differences in performance between the two methods, drawing from direct experimental data and market analyses.
Table 1: Direct Comparison of Mycoplasma Testing Methods
| Feature | PCR-Based Method | Culture-Based Method |
|---|---|---|
| Principle | Detection of microbial DNA via amplification | Microbial growth in specialized media |
| Turnaround Time | ~4.8 hours to result [6]; same-day possible [7] | 24-48 hours for AST; 2-3 weeks for full culture [3] |
| Sensitivity | High; detects DNA from non-viable and viable cells | Lower; dependent on viable, cultivable organisms |
| Key Advantage | Speed, high-throughput, identifies resistance mutations | Phenotypic resistance profile, historical gold standard |
| Key Limitation | Genotype-phenotype discordance possible [3] | Lengthy process, cannot detect non-viable organisms |
| Cost (USD) | ~$300 - $1,200 per kit [8] | ~$100 per kit [8] |
Critical Experimental Data and Emerging Resistance Profiles
Empirical data from recent studies highlights the practical implications of method choice and underscores the growing challenge of antibiotic resistance.
Diagnostic and Clinical Outcomes Data
Recent comparative studies across different clinical fields demonstrate a consistent trend of PCR-based methods outperforming traditional culture.
Table 2: Performance Data of PCR vs. Culture from Clinical Studies
| Study Focus | PCR Sensitivity | PCR Specificity | Key Finding |
|---|---|---|---|
| Wound Infections | 98.3% (vs. culture) [7] | 73.5% (vs. culture) [7] | PCR detected 110 significant pathogens missed by culture [7]. |
| Complicated UTI | N/A | N/A | PCR-guided treatment provided significantly better clinical outcomes (88.1% vs 78.1% success) [9]. |
| Bloodstream Infections | N/A | N/A | dPCR detected 63 pathogenic strains across 42 positive samples, compared to 6 strains via blood culture [6]. |
The Antibiotic Resistance Crisis in Mycoplasma pneumoniae
The utility of culture-based AST is evident in tracking the alarming rise of macrolide-resistant M. pneumoniae (MRMP), a major clinical concern, particularly in pediatrics.
Resistance Mechanisms: Resistance is primarily linked to point mutations in the 23S rRNA gene, most commonly at positions A2063G, A2064G, and A2617C [3] [4]. These mutations reduce macrolide binding affinity, rendering first-line therapies like azithromycin ineffective [3].
Global Prevalence: Resistance rates vary significantly by region. A 2023-2024 Russian study found the A2063G mutation in ~40% of clinical samples [4]. In contrast, a 2023 study in Xi'an, China, reported that 100% of cultured isolates harbored A2063G, A2064T, and A2617C mutations, with a phenotypic resistance rate of 38.6% for macrolides [3]. Japanese data from November 2024 indicates that 20-30% of infections are antibiotic-resistant [8].
Genotype-Phenotype Discordance: The Xi'an study revealed a critical finding: while resistance mutations were universally present genotypically, phenotypic resistance was observed in only 38.6% of isolates [3]. This discordance underscores the importance of integrating both molecular and culture-based susceptibility testing to guide effective clinical management and avoid unnecessary use of second-line antibiotics [3].
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the right reagents and kits is fundamental for effective Mycoplasma testing. The following table details key solutions used in the featured experiments and the broader field.
Table 3: Key Research Reagent Solutions for Mycoplasma Testing
| Product / Solution | Function / Application | Specific Example (if cited) |
|---|---|---|
| PPLO Broth & Agar | Nutrient-rich culture media for cultivating fastidious Mycoplasma species. | Used in clinical isolate culture protocols [3]. |
| PCR & Multiplex Kits | Amplify specific Mycoplasma DNA sequences for highly sensitive detection. | Mycoplasma pneumoniae/Chlamydophila pneumoniae-FRT kit [4]. |
| Antimicrobial Susceptibility Test Plates | Pre-configured panels to determine Minimum Inhibitory Concentration (MIC). | M. pneumoniae culture and susceptibility test kit (Autobio Diagnostics) [3]. |
| Nucleic Acid Extraction Kits | Purify DNA from samples for downstream molecular analysis. | MagMAX Viral/Pathogen Nucleic Acid Isolation Kit [4]. |
| MALDI-TOF MS System | High-throughput platform for rapid microbial identification and genotyping. | QuanTOF I system (Intelligene Biosystems) [3]. |
| Lateral Flow Test Kits | Rapid, convenient immunochromatographic tests for preliminary screening. | SwiftDx Mycoplasma Detection Kit [1]. |
| Pruvonertinib | Pruvonertinib, CAS:2064269-82-3, MF:C27H32N8O2, MW:500.6 g/mol | Chemical Reagent |
| AD 0261 | AD 0261, MF:C27H31F2N3O, MW:451.6 g/mol | Chemical Reagent |
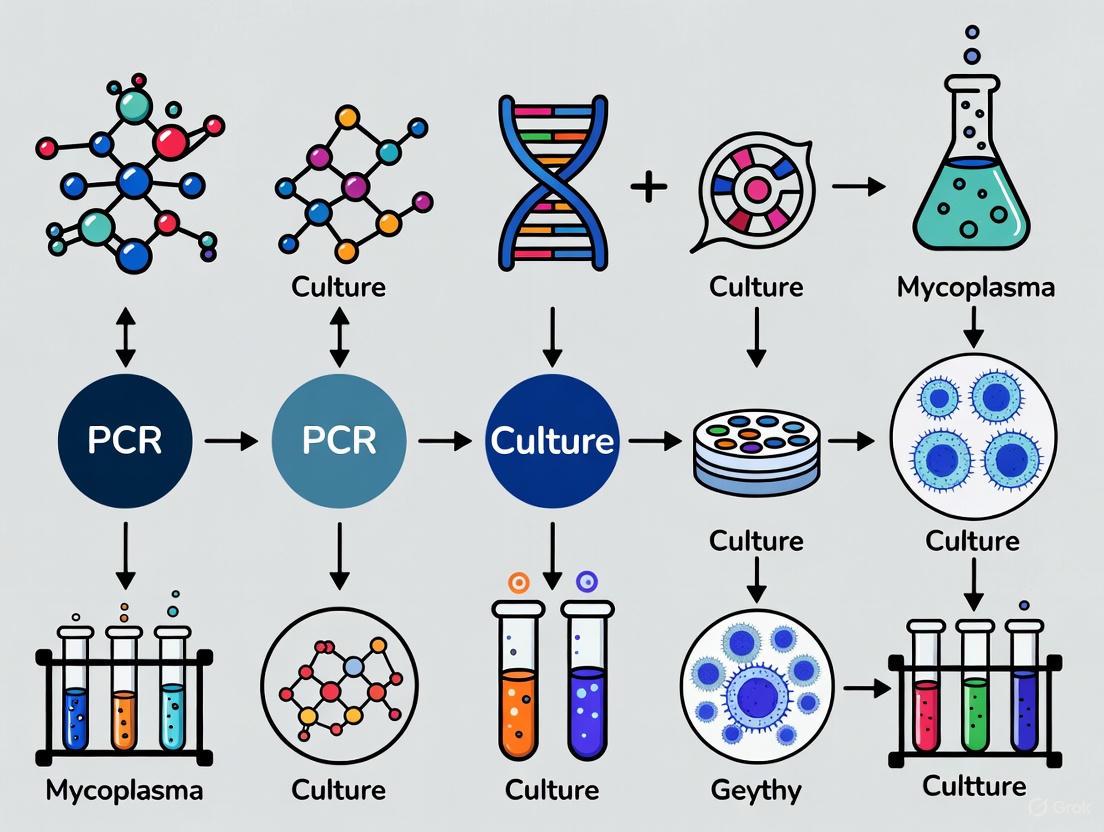
Visualizing the Testing Workflows
The diagrams below illustrate the logical flow and key decision points for the two primary testing methodologies.
Culture-Based Testing Workflow
PCR-Based Testing Workflow
The unique biological characteristics of Mycoplasma—its minimal size, filterability, and intrinsic resistance to common antibiotics—demand vigilant and effective testing strategies. The data clearly demonstrates that PCR-based and culture-based methods are not mutually exclusive but are, in fact, complementary. PCR offers unparalleled speed, sensitivity, and the ability to screen for resistance genotypes, making it ideal for rapid quality control and initial diagnosis. Culture remains indispensable for obtaining phenotypic antibiotic susceptibility profiles and investigating cases where genotypic predictions do not match phenotypic expression [3]. For researchers and drug developers, a layered approach is optimal: employing rapid, high-throughput PCR for routine screening and follow-up with culture-based AST when resistance is suspected or confirmation is required. This integrated strategy, leveraging the strengths of both technologies, is the most robust defense against the unique and persistent threat posed by Mycoplasma contamination and infection.
Mycoplasma contamination represents one of the most significant yet frequently overlooked threats in cell culture laboratories worldwide. With the potential to alter cellular metabolism, compromise research validity, and jeopardize biopharmaceutical product safety, these minute contaminants demand sophisticated detection strategies. The scientific community increasingly recognizes that traditional culture-based methods, long considered the gold standard, may no longer suffice for modern applications requiring rapid results and extreme sensitivity. This comprehensive analysis examines the profound impacts of mycoplasma contamination and objectively compares the performance of polymerase chain reaction (PCR) versus culture methodologies within the framework of mycoplasma testing research, providing researchers, scientists, and drug development professionals with evidence-based guidance for safeguarding their work.
The Hidden Threat: How Mycoplasma Contamination Compromises Cellular Systems
Understanding the Contaminant
Mycoplasmas are the smallest self-replicating organisms known to science, measuring just 0.2-0.3 microns in diameter [10]. Their minute size and lack of a cell wall make them resistant to common antibiotics like penicillin and streptomycin and allow them to pass through standard sterilization filters of 0.45-0.22 µm porosity [11] [12]. These bacteria can grow to extremely high concentrations (10â·-10⸠organisms/mL) in cell cultures while remaining invisible under conventional light microscopy [10]. Of the more than 200 known Mollicutes species, approximately 20 have been isolated from infected cell cultures, with eight species—M. arginini, M. fermentans, M. orale, M. hyorhinis, M. hominis, M. salivarium, M. pirum, and Acholeplasma laidlawii—responsible for over 95% of contamination incidents [11].
Metabolic Consequences of Contamination
Mycoplasmas possess limited biosynthetic capabilities and consequently depend entirely on their host cells for essential nutrients. This parasitic relationship leads to significant metabolic alterations in contaminated cells:
Nutrient Depletion: Mycoplasmas compete with host cells for fundamental nutrients including amino acids, fatty acids, sugars, nucleic acid precursors, and choline [12]. This competition can deplete culture media of components essential for host cell viability and function.
Arginine and Purine Metabolism Disruption: Liquid chromatography mass spectrometry (LC/MS)-based metabolomics studies reveal that mycoplasma contamination induces significant perturbations in arginine and purine metabolic pathways [13]. Research using human pancreatic carcinoma cells (PANC-1) demonstrated that 23 identified metabolites showed significant alterations following mycoplasma infection.
Energy System Alteration: The metabolic changes extend to cellular energy supply systems, potentially explaining the observed effects on various cell functions when mycoplasma is present [13]. Since cell metabolism is involved in virtually every aspect of cellular function, these disruptions can have far-reaching consequences for research outcomes.
Impacts on Research Validity and Product Safety
The effects of mycoplasma contamination extend beyond metabolic changes to fundamentally compromise scientific research and product quality:
Cellular Function Modifications: Contaminated cells can exhibit up to 15-fold increased resistance to chemotherapeutic agents like doxorubicin, vincristine, and etoposide in tetrazolium-based MTT assays [13]. Mycoplasma contamination has also been shown to stimulate prostaglandin E2 production and interfere with amyloid-beta peptide degradation.
Genetic and Molecular Changes: Mycoplasmas can disrupt nucleic acid synthesis, cause chromosomal aberrations, alter cell membrane antigenicity, and change cellular responses to transfection and viral infection [10]. These changes potentially invalidate experimental results across multiple research domains.
Biopharmaceutical Risks: In manufacturing environments, mycoplasma presence can decrease bioreactor yields, interfere with in vitro tests, and potentially cause patient disease [14]. For cell-based therapies and advanced therapy medicinal products (ATMPs), these contaminants present significant patient safety concerns.
Methodological Comparison: PCR Versus Culture-Based Detection
Detection Sensitivity and Specificity
Robust comparative studies demonstrate significant performance differences between detection methodologies:
Table 1: Comparative Performance of Mycoplasma Detection Methods
| Detection Method | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive Predictive Value (%) | Negative Predictive Value (%) |
|---|---|---|---|---|---|
| Real-time PCR | 100 | 100 | 100 | 100 | 100 |
| Conventional PCR | 94.44 | 100 | 96.77 | 100 | 92.85 |
| Enzymatic MycoAlert | 53.33 | Not specified | Not specified | Not specified | Not specified |
| DNA DAPI Staining | 46.66 | Not specified | Not specified | Not specified | Not specified |
| Microbial Culture | 33.33 | Not specified | Not specified | Not specified | Not specified |
Data adapted from a comparative study evaluating 30 cell lines using five different detection techniques [11].
The superior performance of PCR-based methods, particularly real-time PCR, is further evidenced by dilution experiments demonstrating correct detection of infecting mycoplasmas at levels as low as 1/10â´, significantly surpassing the sensitivity of alternative assays [15].
Turnaround Time and Operational Considerations
The operational characteristics of detection methods present substantial practical implications for research and quality control environments:
Table 2: Operational Characteristics of Mycoplasma Detection Methods
| Parameter | Microbial Culture | Conventional PCR | Real-time PCR | New Automated NAT Systems |
|---|---|---|---|---|
| Total Turnaround Time | 4-28 days [14] | 1-2 days | Several hours | ~1 hour [14] |
| Hands-on Time | Moderate to high | Significant | Moderate | Minimal [14] |
| Operator Skill Requirements | High | High | High | Minimal training needed [14] |
| Suitability for Short Shelf-life Products | Limited | Moderate | Good | Excellent [14] |
The lengthy turnaround time associated with culture methods (up to 28 days) creates significant bottlenecks in biopharmaceutical manufacturing, particularly for products with short shelf lives [14]. In contrast, modern nucleic acid amplification techniques (NAT), including fully automated systems like the BIOFIRE Mycoplasma Test, can deliver results in approximately one hour with minimal hands-on time [14].
Regulatory Recognition and Method Validation
Global regulatory frameworks have evolved to recognize the value of NAT methods:
The revised European Pharmacopoeia chapter 2.6.7 "Mycoplasmas" (version 12.2) establishes NAT as equivalent to culture-based methods, harmonizing requirements with the Japanese Pharmacopoeia (JP 18 G3) and United States Pharmacopoeia (USP <63> and USP <77> draft) [16].
Defined sensitivity requirements for NAT methods specify a limit of detection of ≤10 CFU/mL or <100 genomic copies/mL, with genomic copies enhancing comparability between NAT and culture results [16].
Method validation must be performed in the user's own product matrix, even when using validated commercial kits, to ensure absence of inhibitory substances and confirm assay sensitivity under real conditions [16].
Experimental Approaches and Methodologies
Protocol 1: Real-Time PCR Detection Methodology
The superior performance of real-time PCR for mycoplasma detection is demonstrated through specific experimental protocols:
Sample Preparation: Cell lines are cultured in antibiotics-free medium for at least 4-7 days without medium exchange to allow mycoplasma proliferation [11]. Both cells and supernatant must be tested as mycoplasmas can adhere to or reside within cells [16].
DNA Extraction: Nucleic acids are extracted from both positive and negative control cell lines. Five mycoplasma-contaminated cell lines are typically designated as positive controls and five mycoplasma-free cell lines as negative controls [11].
Amplification and Detection: Real-time PCR is conducted using commercial diagnostic kits with genus-specific primers targeting the 16S ribosomal RNA gene [11]. The PCR Mycoplasma Test Kit I/RT from PromoKine has been used in comparative studies.
Quality Control: The system must include an internal control to rule out inhibition and an external positive control with defined genomic copies or CFU content close to the limit of detection, plus a negative control [16].
Protocol 2: Metabolic Impact Assessment via LC/MS-Based Metabolomics
The metabolic consequences of mycoplasma contamination can be quantified using sophisticated analytical approaches:
Sample Collection: Cells are grown to approximately 90% confluence, quenched with liquid nitrogen, and harvested by scraping. Metabolites are extracted using chilled methanol followed by centrifugation at 14,000×g for 15 minutes at 4°C [13].
Chromatographic Separation: Hydrophilic interaction liquid chromatography (HILIC) is performed using an Atlantis Silica HILIC column with a binary mobile phase system and linear gradient over 30 minutes [13].
Mass Spectrometric Analysis: A Q Exactive benchtop Orbitrap mass spectrometer equipped with heated ESI source operates in both positive and negative modes at 70,000 FWHM resolution for full scan mode (80-900 m/z) followed by data-dependent MS/MS at 17,500 FWHM resolution [13].
Data Processing: Multivariate principal component analysis (PCA) and univariate analysis are performed using specialized bioinformatics software. Metabolites of interest are filtered based on significant fold changes (fold change >2 or <-2) and statistical significance (p<0.05) [13].
Essential Research Reagents and Solutions
Implementing robust mycoplasma detection requires specific quality-controlled reagents and reference materials:
Table 3: Essential Research Reagents for Mycoplasma Detection
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Quantitative DNA Reference Materials | Analytical sensitivity evaluation | ATCC provides titered reference strains with low GC/CFU ratio under ISO 17034 accreditation [17] |
| Venor Mycoplasma qPCR Assay | Regulatory-compliant detection | Fully aligned with EP 2.6.7, detects >130 mollicute species via reverse transcriptase qPCR [16] |
| 100GC Mycoplasma Standards | Quantitative reference | Traceable 100 genomic copies/vial for sensitivity verification in product-specific matrices [16] |
| Universal Mycoplasma Detection Kit | Multiple species detection | ATCC kit detects over 60 species of Mycoplasma, Acholeplasma, Spiroplasma, and Ureaplasma [17] |
| MycoAlert Assay Kit | Enzymatic detection | Detects ATP generation as indicator of mycoplasma activity; shows 53.33% sensitivity in comparative studies [11] |
| BIOFIRE Mycoplasma Test | Automated NAT system | Closed "lab in a pouch" system with minimal hands-on time, results in ~1 hour [14] |
The high stakes of mycoplasma contamination demand rigorous detection strategies that balance sensitivity, specificity, speed, and regulatory compliance. The evidence clearly demonstrates that PCR-based methods, particularly real-time PCR, outperform traditional culture-based approaches in detecting these insidious contaminants. As the field advances, fully automated NAT systems promise to further reduce detection times while maintaining the sensitivity required for protecting research integrity and biopharmaceutical products. Researchers and manufacturers must prioritize routine mycoplasma testing using the most appropriate detection methodology for their specific application, ensuring the validity of scientific discoveries and the safety of biological products.
The United States Pharmacopeia (USP), European Pharmacopoeia (EP), and Japanese Pharmacopoeia (JP) establish the legally binding quality standards for biological products in their respective regions. These pharmacopeias provide comprehensive frameworks for testing biologics to ensure their identity, purity, potency, and safety before patient release. Harmonization efforts by the Pharmacopoeial Discussion Group (PDG), formed in 1990, have created greater alignment between these standards, though critical differences remain that global manufacturers must navigate [18]. For biologics, which include vaccines, cell and gene therapies, and therapeutic proteins, adherence to these compendial requirements is not merely advisory but a regulatory imperative for market authorization and lot release.
This guide focuses specifically on the application of USP, EP, and JP standards to biologics, with a detailed examination of mycoplasma testing—a critical safety requirement where the choice between traditional culture methods and modern PCR-based assays presents significant practical and regulatory considerations.
Comparative Analysis of USP, EP, and JP Frameworks
The three pharmacopeias share the common goal of ensuring drug quality and patient safety but reflect their regions' distinct regulatory histories and medical traditions. The table below summarizes their core characteristics.
Table 1: Fundamental Comparison of the Major Pharmacopoeias
| Feature | USP (United States) | EP (European) | JP (Japanese) |
|---|---|---|---|
| Governing Body | United States Pharmacopeial Convention [19] | European Directorate for the Quality of Medicines (EDQM) [19] | Ministry of Health, Labour and Welfare (MHLW) [19] |
| Legal Status | Enforceable by the FDA [19] | Legally binding in member states [19] | Forms the legal basis for all pharmaceuticals in Japan [19] |
| Update Cycle | Ongoing revisions [19] | New edition every 3 years [19] | New edition every 5 years, with supplements [19] |
| Unique Focus | Broad scope, including drugs, supplements, and food ingredients [19] | Strong emphasis on packaging standards and herbal products [19] | Integration of modern pharmaceuticals with traditional Kampo medicines [19] |
| Testing Specialties | Leader in biotech and biologics testing methods [19] | Extensive protocols for herbal products [19] | Advanced techniques like quantitative NMR [19] |
The JP uniquely balances modern pharmaceutical science with traditional Kampo medicine, while the EP places significant emphasis on packaging standards [19]. The USP's scope is notably broad, extending into dietary supplements and food ingredients, and its standards are recognized in over 140 countries, giving it a wide international influence [19]. A key difference for manufacturers is the update cycle: the EP's formal three-year cycle and the JP's five-year cycle offer more predictable revision schedules compared to the USP's ongoing revision process, which can present a dynamic compliance landscape [19].
Harmonization and Key Differences in Testing Requirements
The Drive for Harmonization
The Pharmacopoeial Discussion Group (PDG) works to harmonize excipient monographs and general chapters to ease the global trade of medicines [18]. This collaboration is crucial for reducing redundant testing for companies operating internationally. The International Council for Harmonisation (ICH) further supports this through its Q4B Expert Working Group, which evaluates and recommends specific pharmacopoeial texts for use across the ICH regions [18]. For example, the ICH has declared that the sterility test chapters of the USP (<61>, <71>), EP (2.6.1, 2.6.12), and JP (4.05, 4.06) can be used interchangeably, subject to certain conditions [18].
Specific Testing Mandates for Biologics
Biologics require a multi-faceted testing strategy to guard against various impurities and contaminants. The following diagram illustrates the comprehensive testing workflow integrated throughout the bioproduction process.
Key testing categories include:
- Sterility Testing: Governed by USP <61>, <62>, and <71>; EP 2.6.1, 2.6.12, and 2.6.13; and JP 4.05 and 4.06. These tests detect the presence of viable microorganisms and are required for final product release. The ICH Q4B has deemed these chapters interchangeable [18].
- Endotoxin Testing: Primarily using the Limulus Amebocyte Lysate (LAL) assay, this test is covered under USP <85>, EP 2.6.14, and JP 4.01. These chapters are also considered interchangeable, as their reference standards are calibrated against the WHO international standard [18].
- Subvisible Particulate Testing: For injectables like biologics, USP <788> (which is harmonized with EP 2.9.19 and JP 6.07) sets limits on particulate matter. Therapeutic protein injections have a tailored chapter, USP <787> [20].
- Mycoplasma Testing: This is a critical and complex release requirement for products derived from cell cultures, detailed in the following section.
Mycoplasma Testing: A Critical Release Requirement
The Contamination Risk
Mycoplasmas are the smallest free-living organisms and are a major concern in biopharmaceutical manufacturing. They are notorious contaminants of cell cultures, with estimates suggesting they affect 15–35% of all continuous cell cultures globally [2]. Unlike many bacteria, mycoplasmas lack a rigid cell wall, making them resistant to many antibiotics and allowing them to pass through standard sterilizing filters. Critically, contamination often causes no visible changes to the cell culture, such as turbidity or pH shifts, meaning specialized testing is the only reliable detection method [18] [21].
Compendial Testing Methods: Culture vs. PCR
The pharmacopeias specify two primary methodological approaches for mycoplasma testing, each with distinct advantages and limitations.
Table 2: Comparison of Mycoplasma Testing Methods per USP, EP, and JP
| Aspect | Culture-Based Method | PCR-Based Method |
|---|---|---|
| Principle | Growth in broth/agar media and indicator cell lines [21] | Nucleic acid amplification of Mycoplasma DNA [18] |
| Turnaround Time | 28 days [22] [21] | As little as a few hours [18] |
| Sensitivity | High for cultivable species | High and broad for species with known sequences |
| Key Regulatory Chapters | USP <63>, EP 2.6.7, JP 9 [21] | EP 2.6.7 (includes NAT), general guidance in USP <1223> [18] |
| Primary Use | Lot release testing (where required) | In-process testing, raw material release, rapid lot release |
The culture method is the historical gold standard for final product release. It involves inoculating the sample into both broth and agar media and incubating for 28 days, with regular subculturing to enrich for any present mycoplasmas. The method is validated for its ability to detect a panel of representative species, such as M. pneumoniae, M. orale, and A. laidlawii [18] [21]. While highly sensitive, the 28-day duration often makes it the rate-limiting step for product release [22].
PCR-based methods, or Nucleic Acid Amplification Techniques (NAATs), offer a rapid alternative. These tests can provide results in hours, enabling faster decision-making during manufacturing [18]. While traditionally used for in-process testing, their acceptance for final lot release is growing, supported by technological advances and their inclusion in pharmacopeial chapters like EP 2.6.7.
Experimental Comparison: Culture vs. PCR for Mycoplasma Detection
Experimental Protocol for Method Comparison
A standard protocol to validate a PCR method against the compendial culture method involves the following steps:
- Sample Preparation: Spike a representative biologic product (e.g., a monoclonal antibody solution) with low levels (10-100 CFU/mL) of compendial mycoplasma strains (e.g., M. pneumoniae and A. laidlawii) [18] [21]. Include unspiked samples as negative controls.
- Culture Method Arm:
- Inoculate the sample into both liquid broth and agar media as specified in USP <63>, EP 2.6.7, and JP 9.
- Incubate at 36±1°C under both aerobic and microaerophilic conditions.
- Subculture from the broth to fresh media on days 3, 7, 14, and 21 post-inoculation.
- Observe agar plates for characteristic "fried-egg" colonies and check broth for turbidity over a 28-day period [21].
- PCR-Based Arm:
- Extract nucleic acids from an aliquot of the same spiked and unspiked samples.
- Perform PCR using primers targeting a conserved region of the mycoplasma 16S rRNA gene.
- Include appropriate positive controls (mycoplasma genomic DNA) and negative controls (no-template).
- Run the assay and analyze results, which can be completed within one working day.
- Data Analysis: Compare the detection sensitivity, specificity, and rate of contamination detection between the two methods.
Data and Outcomes
This experimental approach consistently reveals the trade-offs between the two methods. A recent clinical study in another diagnostic context demonstrated that PCR panels reduced the turnaround time from ~48 hours to ~12 hours—a four-fold improvement—while also increasing the diagnostic yield by over 19 percentage points [23]. While this data is from a clinical setting, it underscores the profound efficiency gains of PCR.
In the context of biologics testing, the data can be summarized as follows:
Table 3: Experimental Data from Comparative Method Testing
| Performance Metric | Culture-Based Method | PCR-Based Method |
|---|---|---|
| Turnaround Time | 28 days [22] [21] | 1-2 days [18] |
| Ability to Detect Non-Cultivable Species | Limited to cultivable strains | High (with appropriate primer design) |
| Risk of Viable but Non-Culturable (VBNC) Miss | High (cannot detect VBNC organisms) | Low (detects DNA regardless of cultivability) |
| Susceptibility to Sample Inhibition | Low | Moderate (requires careful validation to rule out inhibitors) |
| Quantification | Semi-quantitative (CFU) | Quantitative (with qPCR standard curve) |
The experimental outcomes clearly show that PCR offers superior speed and broader detection capability, while the culture method remains a robust, growth-based standard. The regulatory trend is moving toward greater acceptance of rapid methods, particularly for products with short shelf-lives like cell and gene therapies, where a 28-day wait is impractical [18].
The Scientist's Toolkit: Essential Reagents and Materials
Successfully implementing compendial testing requires the use of qualified reagents and reference materials.
Table 4: Essential Research Reagent Solutions for Compliance Testing
| Reagent / Material | Function | Application in Testing |
|---|---|---|
| Mycoplasma Positive Control Strains (e.g., M. pneumoniae, M. orale) [18] | Acts as a positive control to demonstrate the test can support growth or detect target DNA. | Used in both culture and PCR methods for assay validation and as a run control. |
| Control Standard Endotoxins (CSE) [18] | A standardized endotoxin preparation traceable to an international standard. | Used to generate standard curves and positive controls in LAL tests for endotoxin detection. |
| Validated PCR Kits & Reagents | Provides optimized primers, probes, and master mixes for specific detection of mycoplasma DNA. | Used in NAAT for mycoplasma testing; must be validated for sensitivity and specificity. |
| Qualified Culture Media (Broth & Agar) | Supports the growth of a wide range of mycoplasma species. | Used in the compendial 28-day culture method for mycoplasma detection. |
| International Reference Standards | The highest-order standard for a given analyte (e.g., endotoxin, a specific protein). | Used to qualify in-house secondary standards and ensure global assay comparability. |
| GLX351322 | GLX351322, MF:C21H25N3O5S, MW:431.5 g/mol | Chemical Reagent |
| MEK-IN-4 | MEK-IN-4, MF:C21H18N4OS, MW:374.5 g/mol | Chemical Reagent |
Navigating the regulatory imperatives of USP, EP, and JP is fundamental to the successful development and commercialization of biological products. While harmonization efforts have created significant alignment, understanding the nuanced differences in testing requirements, particularly for critical areas like mycoplasma detection, is essential. The data and comparisons presented demonstrate a clear industry trend: the future of biologics release testing lies in the strategic integration of rapid, sensitive methods like PCR with the established robustness of traditional culture-based assays. This hybrid approach balances the need for speed and efficiency with the unwavering commitment to patient safety mandated by global regulatory authorities.
In the biopharmaceutical industry, ensuring the sterility of cell banks and production processes is not merely a quality control step but a fundamental prerequisite for patient safety and product efficacy. Mycoplasma contamination constitutes one of the most prevalent and serious threats, affecting an estimated 15-35% of continuous cell cultures globally, with some selected populations reporting rates as high as 65-80% [24] [25] [26]. These bacteria, devoid of a cell wall, can profoundly alter cell physiology and metabolism, leading to erroneous research data, compromised product quality, and significant economic losses [27] [25]. The following comparison guide provides an objective analysis of the primary methods used to detect mycoplasma, framing this critical quality control issue within the broader thesis of PCR versus traditional culture methods.
Understanding the scope and origin of contamination is the first step in its control. The rates of mycoplasma infection are persistently high within biopharmaceutical manufacturing, posing both safety and economic risks [24] [26].
The introduction of mycoplasma into a production process can be traced to several key sources:
- Laboratory Personnel: Operations staff are a major source of human-origin mycoplasma species. Improper techniques, such as mouth pipetting, can introduce organisms from the oropharyngeal tract [11] [25].
- Contaminated Biologicals: While less common today due to improved vendor qualification, raw materials of animal origin, particularly fetal bovine serum (FBS) and trypsin, historically were significant sources of bovine and swine mycoplasma species [25] [26].
- Cross-Contamination in the Lab: A single infected cell culture can rapidly spread mycoplasma to other cultures in the same laboratory. Live mycoplasma can be recovered from laminar flow hood surfaces days after working with a contaminated culture, leading to the infection of clean cultures subcultured in the same hood [25].
Distribution of Mycoplasma Species
While over 190 species of mycoplasma exist, only a handful account for the vast majority of cell culture contaminations. The table below summarizes the most common species and their origins.
Table 1: Common Mycoplasma Species in Cell Culture Contamination
| Mycoplasma Species | Primary Source | Approximate Frequency of Contamination |
|---|---|---|
| M. orale | Human | 20 - 40% [11] [26] |
| M. hyorhinis | Porcine | 10 - 40% [11] |
| M. arginini | Bovine | 20 - 30% [11] |
| M. fermentans | Human | 10 - 20% [11] [26] |
| M. hominis | Human | 10 - 20% [11] [26] |
| Acholeplasma laidlawii | Bovine | 5 - 20% [11] [26] |
Method Comparison: PCR vs. Culture for Mycoplasma Detection
The choice of detection method is critical for accurate and timely quality control. The following experimental data and protocols provide a direct comparison between the rapid, molecular-based PCR methods and the traditional, gold-standard culture approach.
Experimental Protocol for Method Comparison
A definitive study conducted by the National Cell Bank of Iran offers a robust experimental framework for comparing detection techniques [11].
- Sample Preparation: Thirty cell lines suspected of mycoplasma contamination were selected. Prior to testing, each cell line was cultured in an antibiotics-free medium for at least 4-5 days without exchanging the medium to allow for potential mycoplasma proliferation [11].
- Control Groups: Five mycoplasma-contaminated cell lines were used as positive controls, and five mycoplasma-free cell lines served as negative controls to validate the results of each method [11].
- Compared Methods: Each cell line was evaluated in parallel using five different techniques:
- Microbial Culture: The direct culture method, considered the regulatory gold standard.
- Indirect DNA Staining (DAPI): A fluorescent dye that binds to DNA, revealing filamentous staining in the cytoplasm of infected cells.
- Enzymatic Assay (MycoAlert): A biochemical assay that detects mycoplasma-specific enzyme activity.
- Conventional PCR: A gel-based PCR method using genus-specific primers targeting the 16S rRNA gene.
- Real-time PCR (qPCR): A fluorescence-based PCR method that allows for real-time monitoring of amplification, also targeting the 16S rRNA gene [11].
Performance Data and Results
The study yielded clear, quantitative results on the efficacy of each method, as summarized below.
Table 2: Comparative Performance of Mycoplasma Detection Methods [11]
| Detection Method | Contamination Detection Rate | Sensitivity | Specificity | Accuracy |
|---|---|---|---|---|
| Microbial Culture | 33.33% | Not specified (Reference) | Not specified (Reference) | Not specified (Reference) |
| DNA Staining (DAPI) | 46.66% | Data not available in source | Data not available in source | Data not available in source |
| Enzymatic Assay | 53.33% | Data not available in source | Data not available in source | Data not available in source |
| Conventional PCR | 56.66% | 94.44% | 100% | 96.77% |
| Real-time PCR (qPCR) | 60.00% | 100% | 100% | 100% |
The analysis concluded that the real-time PCR assay was superior to all other methods, offering the highest sensitivity, specificity, and accuracy [11]. This superior performance is attributed to PCR's ability to correctly detect the infecting mycoplasmas at extremely low levels, with some nested PCR protocols capable of detecting as few as 1 CFU per 10^4 cells [15].
The Scientist's Toolkit: Essential Research Reagent Solutions
The effective implementation of either PCR or culture methods relies on a suite of specific reagents and tools. The following table details key solutions used in the featured experiments and the field at large.
Table 3: Key Research Reagent Solutions for Mycoplasma Detection
| Reagent / Kit | Function / Application | Example Use in Experiment |
|---|---|---|
| MycoAlert Assay Kit | Enzymatic detection of mycoplasma contamination; measures ATP levels in sample. | Used as one of the five comparative methods in the National Cell Bank of Iran study [11]. |
| PromoKine qPCR Kit | Real-time PCR-based detection of mycoplasma DNA. | Used with proven 100% sensitivity and specificity for mycoplasma detection in cell cultures [11]. |
| Hoechst 33258 / DAPI Stain | Fluorescent DNA dyes for indirect staining of mycoplasma in cell cultures. | Used in DAPI staining method to visualize mycoplasma DNA in the cytoplasm of infected cells [27] [25]. |
| PowerSoil Pro DNA Kit | Automated extraction of high-quality microbial DNA from complex samples. | Used in a cosmetics QC study to extract bacterial and fungal DNA from enriched samples prior to rt-PCR [28]. |
| 16S rRNA Primers | PCR primers targeting conserved regions of the bacterial 16S rRNA gene for universal mycoplasma detection. | Designed for conventional PCR in the featured study; product size of 425 bp [11]. This target is highly conserved and allows for broad species detection [15]. |
| Fetal Bovine Serum (FBS) | Critical growth supplement for cell culture media; a potential source of bovine mycoplasma. | All cell culture media in the featured study were supplemented with 10-20% FBS [11]. Requires sourcing from certified, mycoplasma-free suppliers. |
| HJC0123 | HJC0123, MF:C24H16N2O3S, MW:412.5 g/mol | Chemical Reagent |
| RBC10 | RBC10, MF:C24H25ClN2O2, MW:408.9 g/mol | Chemical Reagent |
Workflow and Decision Pathways
The choice between quality control methods involves a trade-off between speed and regulatory acceptance. The following diagram illustrates the key steps and decision points in the two primary testing pathways.
Regulatory bodies worldwide, including the FDA and EMA, mandate testing for mycoplasma in cell banks, viral seeds, and bulk harvest materials [29] [26]. While traditional culture methods are often cited as the regulatory gold standard in pharmacopoeias (e.g., USP <63>, Ph. Eur. 2.6.7), their 28-day incubation period is a significant bottleneck [27] [26].
In conclusion, the data clearly demonstrates that real-time PCR is superior to culture-based methods in terms of speed, sensitivity, and accuracy for detecting mycoplasma contamination. While culture methods retain their place in regulatory compliance, the biopharmaceutical industry's drive for efficiency and safety is leading to the increased adoption and regulatory acceptance of robust, validated PCR assays. This is particularly critical for advanced therapies and time-sensitive products, where a 28-day wait for results is impractical. A comprehensive quality control strategy will leverage the strengths of both methods—using qPCR for rapid in-process control and culture as a definitive, long-term release test—to effectively mitigate the pervasive risk of mycoplasma contamination.
A Deep Dive into Testing Workflows: From Traditional Cultures to Modern Molecular Assays
For decades, microbial culture has served as the undisputed gold standard for detecting and identifying pathogens across clinical, pharmaceutical, and research settings. This method relies on allowing microorganisms to proliferate in specialized nutrient media, enabling both detection and subsequent analysis. Culture methods are particularly crucial for mycoplasma detection in cell cultures, where these minute, cell wall-deficient bacteria can persist as covert contaminants, potentially compromising years of research or biopharmaceutical production. The phrase "28-day process" references the standard incubation period mandated by major pharmacopoeias for mycoplasma testing, a timeline that underscores the method's thoroughness but also its most significant limitation—time. This guide objectively compares the performance of this traditional benchmark against modern molecular alternatives, providing researchers and drug development professionals with the experimental data necessary to inform their diagnostic strategies.
Core Principles of the Culture Method
The culture method's validity stems from its fundamental principle: supporting the replication of viable organisms. Unlike molecular methods that detect genetic material, culture demonstrates the presence of living, metabolically active pathogens. For mycoplasma, this involves using both broth and agar media formulated to provide the specific nutrients and environmental conditions these fastidious organisms require. Broth media, such as Friis broth, allow for the enrichment of even low levels of mycoplasma, while semi-solid agar media facilitate the formation of characteristic "fried-egg" colonies that are visible under microscopy. The extended incubation period—up to 28 days—is necessary because of the slow growth rate of many mycoplasma species; some contaminants may not be detectable until the final days of the protocol. This process is considered the definitive test for viability, as it confirms the presence of organisms capable of sustained propagation.
Experimental Protocol: The 28-Day Mycoplasma Culture Test
The following workflow details the standard operational procedure for mycoplasma testing using the culture method, as employed in diagnostic laboratories and quality control testing.
Diagram Title: 28-Day Mycoplasma Culture Workflow
Detailed Methodology
- Sample Inoculation: The test sample (e.g., cell culture supernatant, biological product) is inoculated into a liquid broth medium, typically in a ratio of 1:10 to 1:20 (sample:broth). Common broth media include Friis modification or Hayflick modification, which are enriched with serum, yeast extract, and other essential growth factors [30].
- Broth Enrichment Phase: The inoculated broth is incubated at 35-37°C for a minimum of 14 days, often extended to 21 days. This extended enrichment period is critical for amplifying low-level contaminants that would otherwise go undetected. Subcultures from the broth are performed onto agar plates at multiple time points (e.g., day 3-7 and day 14-21) to capture any growing mycoplasma.
- Agar Plating and Incubation: The subcultured agar plates are incubated under anaerobic or microaerophilic conditions at 35-37°C for an additional 7-14 days. The anaerobic environment is crucial for the growth of many mycoplasma species.
- Colony Observation and Identification: Following incubation, agar plates are examined microscopically at 100-200x magnification for the presence of characteristic mycoplasma colonies. These appear as granular, "fried-egg" colonies due to their central growth into the agar and superficial peripheral zone. The entire process, from inoculation to final reading, constitutes the 28-day duration that defines this gold standard method.
Performance Comparison: Culture vs. PCR
The following tables summarize key performance metrics and characteristics of the culture method compared to PCR-based diagnostics, drawing on data from multiple studies across different pathogen types.
Table 1: Diagnostic Performance Metrics of Culture vs. PCR
| Metric | Culture Method | PCR-Based Methods | Context of Data |
|---|---|---|---|
| Sensitivity | Gold Standard (Reference) | 58.33% - 99% [31] [32] [33] | Varies by sample type, pathogen, and protocol |
| Specificity | Gold Standard (Reference) | 77.78% - 100% [31] [34] [32] | Varies by sample type, pathogen, and protocol |
| Time to Result | 14-28 days [31] [30] | Hours to 1 day [34] [35] | Mycoplasma testing; other infections may differ |
| Viability Detection | Yes (Detects living organisms) | No (Detects genetic material) | Fundamental methodological difference |
| Strain Identification | Requires subculture & typing | Can be designed for specific strain detection | PCR panels can be tailored [34] |
Table 2: Operational Characteristics and Applications
| Characteristic | Culture Method | PCR-Based Methods |
|---|---|---|
| Key Advantage | Confirms viability; broad-spectrum detection | Speed and high sensitivity [36] [35] |
| Primary Limitation | Lengthy turnaround time [31] | Cannot determine viability; limited by primer design [34] |
| Antibiotic Susceptibility | Possible (Phenotypic testing) | Not possible (Requires detection of resistance genes) [35] |
| Throughput Capacity | Low to moderate | High, with automation potential [36] |
| Optimal Use Case | Regulatory batch release; viability confirmation | Rapid screening; detecting non-culturable organisms [36] [34] |
A systematic review and meta-analysis of molecular tests for bloodstream pathogens found that compared to traditional phenotypic culture methods, PCR tests showed 92–99% sensitivity and 99–100% specificity for identifying bacteria and associated antimicrobial resistance genes [33]. However, a direct comparison for mycoplasma tuberculosis reported a lower PCR sensitivity of 58.33% with 77.78% specificity when using a specific buffer-based DNA extraction method, highlighting how protocol variations impact performance [31]. Another large-scale study on pulmonary tuberculosis reported significantly higher PCR sensitivity (93%) and specificity (84%) [32].
Essential Research Reagent Solutions
The execution of the 28-day culture method requires specific, high-quality reagents to ensure reliable results. The following table details key materials and their functions.
Table 3: Key Reagents for Mycoplasma Culture Testing
| Research Reagent | Function in the Protocol |
|---|---|
| Enrichment Broth (e.g., Friis Medium) | Liquid medium for amplifying low levels of mycoplasma over 14-21 days. Contains serum, yeast extract, and other essential growth factors [30]. |
| Agar Plates (Semi-Solid Medium) | Solid medium for colony formation. Allows for visual identification of characteristic "fried-egg" morphology after 7-14 days of incubation. |
| Proteinase K | Enzyme used in some DNA extraction protocols for PCR to digest proteins and release microbial DNA, facilitating subsequent amplification [31]. |
| Oligonucleotide Primers | Short, specific DNA sequences designed to bind to and amplify target mycoplasma DNA regions in PCR-based methods [31] [34]. |
| Fluorochrome Dyes (e.g., Hoechst stain) | DNA-binding dyes used in indirect staining methods to visualize mycoplasma DNA adhered to infected host cells, though results can be equivocal [37]. |
The gold standard culture method, with its 28-day broth and agar cultivation process, remains an indispensable tool for confirming viable mycoplasma contamination, particularly in regulated environments like drug development and biopharmaceutical manufacturing. Its strengths of proven reliability and viability detection are counterbalanced by its protracted timeline. In contrast, PCR-based methods offer a powerful alternative with unmatched speed and high sensitivity, making them ideal for rapid screening and situations where time-to-result critically impacts decision-making [36] [34]. The evolving diagnostic landscape does not necessitate a wholesale replacement of one method by the other, but rather a strategic integration based on context. For many researchers and quality control professionals, the most robust strategy involves using PCR for rapid, sensitive screening during ongoing projects, while reserving the comprehensive 28-day culture as a definitive confirmatory test for final product release and regulatory compliance.
Within the context of mycoplasma testing research, the paradigm for pathogen detection is shifting from traditional culture-based methods to sophisticated nucleic acid amplification techniques (NAT). Quantitative PCR (qPCR) and digital PCR (dPCR) represent two powerful NATs that offer unparalleled speed, sensitivity, and specificity. This guide provides an objective comparison of qPCR and dPCR, detailing their principles, performance metrics, and experimental protocols. By summarizing key quantitative data and methodologies, we aim to equip researchers and drug development professionals with the information necessary to select the appropriate technique for their specific diagnostic and quantitative challenges.
The gold standard for mycoplasma detection has traditionally been microbial culture. However, this method is hampered by Mycoplasma's stringent growth requirements and slow replication rate, often requiring 1 to 3 weeks to obtain a result [38]. This delay is untenable in fast-paced environments like drug development and biomanufacturing, where timely contamination monitoring is critical.
Nucleic Acid Amplification Techniques (NATs), particularly qPCR and dPCR, have emerged as superior alternatives for rapid detection. These methods bypass the need for cultivation, directly targeting the pathogen's genetic material to provide results in a matter of hours [38] [39]. Their high sensitivity and specificity make them indispensable for ensuring cell culture integrity, validating bioprocesses, and managing infectious diseases. The following sections delve into how these two advanced techniques achieve rapid and reliable detection.
Fundamental Principles and Comparative Workflow
While both qPCR and dPCR amplify target DNA sequences enzymatically, their methods of quantification and data analysis differ fundamentally, leading to distinct advantages and applications.
How qPCR Works
Quantitative PCR (qPCR), also known as real-time PCR, monitors the amplification of a target DNA sequence in real time using fluorescence [40]. The process relies on the quantification cycle (Cq), which is the PCR cycle number at which the fluorescence intensity exceeds a background threshold. This Cq value is inversely proportional to the logarithm of the initial amount of target nucleic acid; a lower Cq indicates a higher starting concentration [39]. Quantification is achieved by comparing the Cq values of unknown samples to a standard curve generated from samples with known concentrations [39].
How dPCR Works
Digital PCR (dPCR) takes a different approach by partitioning a single PCR reaction into thousands of individual nanoliter-scale reactions [41]. This partitioning is achieved through microfluidic chips (cdPCR) or water-in-oil emulsion droplets (ddPCR) [41]. Following endpoint amplification, each partition is analyzed as either positive (containing the target sequence) or negative (lacking the target). The absolute concentration of the target nucleic acid, in copies per microliter, is then calculated directly using Poisson statistics, without the need for a standard curve [41] [42].
Visualizing the Workflows
The diagram below illustrates the core procedural differences between these two techniques.
Performance Comparison: qPCR vs. dPCR
The fundamental differences in how qPCR and dPCR operate translate into distinct performance characteristics, as summarized in the table below and supported by experimental data.
Table 1: Comparative Performance of qPCR and dPCR for Pathogen Detection
| Performance Characteristic | qPCR | dPCR | Supporting Experimental Data |
|---|---|---|---|
| Principle of Quantification | Relative (via Cq and standard curve) | Absolute (via Poisson statistics) | dPCR quantifies without a standard curve [41] [42]. |
| Dynamic Range | Wide (up to 7-8 orders of magnitude) [39] | Narrower than qPCR [41] | |
| Analytical Sensitivity (LoD) | ~10.8 copies/reaction for M. pneumoniae [43] | Higher sensitivity; ~2.9 copies/reaction for M. pneumoniae [43] | ddPCR identified one positive sample that was negative by qPCR [43]. |
| Precision with Inhibitors | Susceptible; Cq values and efficiency are affected [44] | Tolerant; quantification is less affected [41] [44] | In samples with contaminants, qPCR efficiency dropped to 67%, while ddPCR results remained stable [44]. |
| Precision for Low Abundance Targets | Higher variability (CV) for low target concentrations (Cq ≥ 29) [44] | Superior precision and reproducibility for low abundance targets [44] | For low-level targets, ddPCR produced more precise and statistically significant data [44]. |
| Ability to Detect Fold-Changes | Good for high-abundance targets | Superior for detecting small (<2-fold) changes in low-abundance targets [44] | ddPCR accurately quantified 2-fold dilutions in contaminated samples where qPCR failed [44]. |
A key application of these techniques is in monitoring mycoplasma contamination. A 2019 study optimized a direct qPCR protocol to detect mycoplasma in cell cultures without DNA purification, achieving results in just 65 minutes [45]. The protocol used a 52°C annealing-extension temperature and a 6 µl sample volume, demonstrating that direct qPCR could achieve higher sensitivity than qPCR with purified DNA, making it ideal for rapid contamination monitoring and treatment efficacy studies [45].
Experimental Protocols in Practice
To illustrate how these principles are applied in real-world research, below are summarized methodologies from key studies on mycoplasma detection.
Protocol 1: Direct qPCR for Mycoplasma Contamination Monitoring
This protocol [45] is designed for speed and simplicity, eliminating the DNA purification step.
- Objective: To directly detect Mycoplasma DNA in U937 suspension cell culture without DNA purification.
- Sample Preparation: Supernatant from Mycoplasma-infected U937 cell cultures was used directly as the PCR template.
- qPCR Reaction:
- Kit: PhoenixDx Mycoplasma Mix (Procomcure Biotech).
- System: Bio-Rad CFX Connect.
- Reaction Volume: 20 µL.
- Sample Volume: 6 µL of cell culture supernatant.
- Cycling Conditions:
- Annealing-Extension: 52°C for 20 seconds.
- Total Run Time: 65 minutes.
- Key Finding: The direct qPCR protocol with 6 µl of template showed nearly identical sensitivity to regular qPCR performed with DNA purified from a 60 µl sample, demonstrating its efficiency and high sensitivity for rapid monitoring [45].
Protocol 2: ddPCR for Absolute Quantification ofMycoplasma pneumoniae
This protocol [43] highlights the use of ddPCR for precise quantification in clinical specimens.
- Objective: Absolute quantification of M. pneumoniae in clinical samples to track disease severity and treatment efficacy.
- Sample Preparation: DNA was extracted from 200 µL of clinical samples (sputum, throat swabs) using the QIAamp DNA Mini Kit and eluted in 150 µL [43].
- ddPCR Reaction:
- System: TargetingOne Digital PCR System.
- Reaction Volume: 20 µL.
- Master Mix: 15 µL reaction buffer, 2.4 µL of each primer (10 µM), 0.75 µL probe (10 µM), and DNase-free water.
- Cycling Conditions: 95°C for 10 min, followed by 40 cycles of 94°C for 30 s and 60°C for 1 min.
- Droplet Generation & Reading: The reaction mix was partitioned into droplets using a droplet generator. After PCR, droplets were read using a droplet reader, and the target concentration was calculated using Poisson statistics [43].
- Key Finding: The bacterial load in patients with severe M. pneumoniae pneumonia was significantly higher than in patients with general infection, and loads decreased significantly after macrolide treatment, demonstrating the utility of ddPCR in monitoring therapeutic efficacy [43].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of qPCR and dPCR relies on a suite of specialized reagents and instruments.
Table 2: Key Reagents and Kits for PCR-Based Detection
| Item | Function | Example Use Case |
|---|---|---|
| Probe-based qPCR Kit | Provides high-specificity detection of target DNA through sequence-specific probes. | PhoenixDx Mycoplasma Mix for specific mycoplasma contamination monitoring [45]. |
| DNA Extraction Kit | Purifies and concentrates nucleic acid from complex biological samples, removing PCR inhibitors. | QIAamp DNA Mini Kit used to extract DNA from clinical samples for ddPCR [43]. |
| dPCR System | Partitions reactions and performs absolute quantification. | TargetingOne System and QX100/200 systems for ddPCR [43] [41]. |
| Reverse Transcriptase | For RT-qPCR; synthesizes complementary DNA (cDNA) from RNA templates. | Essential for detecting RNA viruses or gene expression studies [46]. |
| Automated Nucleic Acid Extraction System | Automates the purification process, increasing throughput and reproducibility. | MagNA Pure 96 [38] and Panther Fusion [38] systems for high-throughput clinical diagnostics. |
| Dimericconiferylacetate | Dimericconiferylacetate, MF:C24H26O8, MW:442.5 g/mol | Chemical Reagent |
| RB-005 | RB-005, MF:C21H35NO, MW:317.5 g/mol | Chemical Reagent |
Both qPCR and dPCR are powerful NATs that have revolutionized rapid pathogen detection, displacing slower culture-based methods in many applications. The choice between them depends on the specific requirements of the experiment:
- Choose qPCR for high-throughput, cost-effective screening where relative quantification is sufficient, and sample inhibitors are well-controlled. Its broad dynamic range and established protocols make it a workhorse for routine diagnostics and monitoring [39].
- Choose dPCR when absolute quantification is critical, particularly for targets with low abundance, or when high precision is needed to detect small fold-changes. Its resilience to inhibitors and lack of reliance on a standard curve make it ideal for analyzing complex samples and validating biomarkers [43] [41] [44].
In the context of mycoplasma testing, direct qPCR offers an optimal balance of speed and sensitivity for routine contamination checks [45], while dPCR provides a powerful tool for clinical research requiring precise quantification to assess bacterial load and treatment response [43].
In the field of microbiological testing, particularly for mycoplasma, the choice between traditional culture methods and modern molecular techniques like Polymerase Chain Reaction (PCR) has significant implications for research and drug development workflows. This guide provides an objective, data-driven comparison of these two foundational methodologies, focusing on the critical practical metrics of turnaround time, hands-on time, and sample volume. The analysis is framed within the broader context of optimizing laboratory efficiency while maintaining diagnostic accuracy, enabling researchers and scientists to make informed decisions that align with their project requirements and resource constraints.
The following table summarizes the core workflow differences between culture and PCR methods, highlighting the distinct advantages each method offers across key operational parameters.
Table 1: Core Workflow Comparison Between Culture and PCR Methods
| Parameter | Culture Method | PCR Method |
|---|---|---|
| Total Turnaround Time | 18 hours to several weeks [9] [47] [31] | 5 hours to 2 days [9] [48] [49] |
| Typical Hands-on Time | High (multiple processing steps, subculturing) | Lower (automated nucleic acid extraction and amplification) |
| Sample Volume Requirements | Often higher (e.g., 25g for food samples) [50] | Can be very low (e.g., clinical swabs, body fluids) [31] |
| Key Workflow Limitation | Slow growth rate of fastidious organisms [34] [31] | Limited to detecting targeted pathogens in the panel [34] |
Quantitative Data Comparison
Data compiled from recent clinical and laboratory studies clearly quantify the performance differences between these two methodologies.
Table 2: Quantitative Performance Metrics from Recent Studies
| Application / Study | Metric | Culture Method | PCR Method |
|---|---|---|---|
| Complicated UTI Management [9] [49] | Mean Turnaround Time | 104.4 hours | 49.68 hours |
| Complicated UTI Management [9] [49] | Clinical Success Rate | 78.11% | 88.08% |
| Automated Urine Culture System [47] | Time to Negative Result | 18-24 hours | 5 hours |
| Bacterial Meningitis Diagnosis [51] | Detection Rate in CSF | 3% (10/38) | 10% (38/38) |
| Listeria Detection in Food [50] | Performance in High-Background Microflora | Poor (many false negatives) | Excellent sensitivity |
Detailed Experimental Protocols
To contextualize the data in the previous tables, this section outlines the standard experimental workflows for both culture and PCR methods as cited in the literature.
Conventional Culture Protocol for Mycobacteria
The following protocol, based on the study by Mshana et al., describes the gold standard culture method for detecting Mycobacterium tuberculosis, a process that can take several weeks [31].
Sample Processing:
- Decontamination & Homogenization: Clinical specimens (e.g., bronchoalveolar lavage, pleural fluid) are decontaminated and homogenized using the Petroff technique [31].
- Inoculation: The processed sample is inoculated onto solid culture media, such as Lewenstein-Jensen (LJ) slant medium [31].
- Incubation: The inoculated media is incubated at 37°C. Visible colonies of M. tuberculosis typically take 4 to 8 weeks or longer to appear due to the organism's slow growth rate [31].
- Identification: Once growth is observed, further biochemical tests and phenotypic analysis are required for definitive identification, adding additional time to the process [31].
Real-Time PCR Protocol for Bacterial Identification
This protocol, synthesized from multiple studies, describes a standard real-time PCR workflow for detecting bacterial pathogens, which can provide results within hours [48] [50] [51].
1. Nucleic Acid Extraction:
- Method: DNA templates are extracted from clinical samples or enrichment broths. This can involve boiling samples with a reagent like PrepMan Ultra, followed by centrifugation to pellet debris [50]. Automated systems like the KingFisher Flex or STARlet are also used for higher throughput and consistency [52].
- Output: Purified DNA or crude lysate for amplification.
2. PCR Amplification and Detection:
- Reaction Setup: The extracted DNA is combined with a master mix containing PCR buffer, primers, nucleotides (dNTPs), Taq DNA polymerase, and a fluorescent probe [31].
- Thermocycling: The reaction is placed in a real-time PCR thermocycler (e.g., Bio-Rad CFX96). The instrument runs through 35-45 cycles of denaturation, annealing, and extension, during which the fluorescent signal is measured in real-time [52] [31].
- Result Interpretation: The cycle threshold (Ct) value, which indicates the amplification cycle at which the fluorescent signal crosses a predefined threshold, is determined. A positive result is confirmed based on the Ct value [52]. Under optimal conditions, the entire process from sample to result can be completed in as little as 4-6 hours [48].
Workflow Visualization
The fundamental difference between the two methods lies in their core processes: culture relies on biological amplification of the organism itself, while PCR relies on molecular amplification of genetic material. The following diagram illustrates this conceptual distinction.
Conceptual Workflow: Culture vs. PCR
The practical, step-by-step workflows for each method, as derived from the experimental protocols, are shown below. The contrast in complexity and number of steps is a key determinant of overall turnaround and hands-on time.
Procedural Workflow: Step-by-Step Comparison
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful implementation of either culture or PCR workflows depends on a suite of essential reagents and instruments.
Table 3: Key Research Reagent Solutions and Their Functions
| Item | Function | Application Context |
|---|---|---|
| Selective Culture Media (e.g., Oxford Agar, LJ Medium) | Supports growth of target organisms while inhibiting background flora. | Culture-based isolation and identification [50] [31]. |
| Listeria Enrichment Broth / Fraser Broth | Selective liquid medium for enriching low numbers of target bacteria. | Broth enrichment step in standard culture methods [50]. |
| PrepMan Ultra Reagent | Prepares crude DNA templates by boiling and lysing bacterial cells. | Rapid nucleic acid extraction for PCR [50]. |
| PCR Master Mix (Buffer, dNTPs, Taq Polymerase) | Provides the essential components for DNA amplification. | Real-time and conventional PCR assays [31]. |
| Specific Primer/Probe Sets (e.g., for IS6110, 16S rRNA) | Binds to and enables amplification of unique target DNA sequences. | Specific pathogen detection in PCR [52] [31]. |
| Automated Nucleic Acid Extractors (e.g., KingFisher Flex, STARlet) | Automates the purification of nucleic acids from samples. | High-throughput, consistent PCR workflow [52]. |
| Real-time PCR Thermocyclers (e.g., QIAcuity, Bio-Rad CFX96) | Instruments that perform thermal cycling and fluorescent detection. | Quantitative real-time PCR analysis [52]. |
| 3-Methylglutaric acid-d4 | 3-Methylglutaric acid-d4, MF:C6H10O4, MW:150.17 g/mol | Chemical Reagent |
| ROS inducer 4 | ROS inducer 4, MF:C49H62BrO4P, MW:825.9 g/mol | Chemical Reagent |
Mycoplasma contamination represents a significant risk in biopharmaceutical manufacturing, potentially compromising both product safety and efficacy. These small, cell wall-less bacteria can evade standard sterility testing and are difficult to detect without specialized methods. Throughout the drug development process—from raw material qualification to final product release—controlling for mycoplasma is a critical regulatory requirement. The two primary methodological approaches for detection are traditional culture-based methods and molecular techniques based on Polymerase Chain Reaction (PCR). Culture methods, historically the gold standard, rely on growing mycoplasma in specialized media. In contrast, PCR-based methods detect specific mycoplasma genetic sequences, offering a fundamentally different approach to contamination screening. This guide provides an objective comparison of these techniques across key biomanufacturing testing scenarios, supported by experimental data, to inform method selection by researchers, scientists, and drug development professionals.
Technical Comparison: PCR versus Culture Methods
The fundamental differences between PCR and culture methods lead to distinct performance characteristics. The table below summarizes their core technical principles and inherent advantages and limitations.
Table 1: Fundamental Characteristics of PCR and Culture Methods
| Feature | PCR (Polymerase Chain Reaction) | Culture-Based Methods |
|---|---|---|
| Basic Principle | Amplifies and detects specific DNA sequences | Relies on microbial growth in specialized media |
| Detection Target | Genetic material (DNA) | Viable, reproducing organisms |
| Time to Result | Hours to a single day [53] [54] | Several days to several weeks [53] [11] [54] |
| Sensitivity | Can detect low levels of genetic material; highly sensitive [55] [54] | Requires a sufficient number of viable organisms to form colonies; may miss low-level contamination [54] |
| Key Advantage | Speed, sensitivity, and ability to automate | Confirms microbial viability and can detect a broad range of cultivable species |
| Key Limitation | Cannot distinguish between viable and non-viable organisms; may yield false positives from dead microbes [54] | Time-consuming; cannot detect non-cultivable or slow-growing species [53] [54] |
Performance Data from Comparative Studies
Independent studies have consistently highlighted the performance differences between these two methods. A large-scale study on tuberculosis detection, which shares methodological parallels with mycoplasma testing, found that in-house PCR demonstrated a sensitivity of 77.5% and a specificity of 99.7% compared to culture [56]. A more focused study on mycoplasma detection in cell cultures revealed the clear superiority of molecular methods.
Table 2: Comparison of Mycoplasma Detection Methods in Cell Cultures (30 Samples) [11]
| Detection Method | Contamination Detection Rate | Sensitivity | Specificity |
|---|---|---|---|
| Microbial Culture (Gold Standard) | 33.33% | (Baseline) | (Baseline) |
| Indirect DNA Staining (DAPI) | 46.66% | Information Missing | Information Missing |
| Enzymatic Assay (MycoAlert) | 53.33% | Information Missing | Information Missing |
| Conventional PCR | 56.66% | 94.44% | 100% |
| Real-time PCR | 60.00% | 100% | 100% |
This data demonstrates that real-time PCR is not only the most sensitive method, identifying contamination in 60% of cell lines, but it also achieved 100% sensitivity and specificity, meaning it correctly identified all positive and negative samples [11]. A separate study on genital mycoplasmas reported that a multiplex PCR assay showed a sensitivity of 87% and a specificity of 96% compared to culture [53].
Application Scenarios in the Biomanufacturing Workflow
Raw Material and In-Process Testing
During early production stages, the priority for raw material and in-process testing is often speed and sensitivity to enable rapid decision-making. PCR is exceptionally suited for this role.
- Speed of Results: PCR can provide results in hours, allowing for quicker assessment of raw materials like cell banks, viral seeds, and media components, or for monitoring bioreactors during production [53] [54]. This rapid turnaround helps prevent the use of contaminated materials and minimizes potential delays in production schedules.
- High Sensitivity: The ability of PCR to detect very low levels of microbial DNA makes it invaluable for identifying low-grade, early-stage contamination that could amplify later in the process [55] [11]. This is critical for in-process controls where catching contamination early can save a production batch.
Lot Release Testing
Lot release testing is the final quality control checkpoint before a drug product is released to the market. This phase is highly regulated, and the chosen methods must be validated to meet strict regulatory guidelines [57]. The requirements for this stage differ from earlier phases.
- Regulatory Context and "Full Verification": For final drug substance and drug product, release testing is a mandatory regulatory requirement to confirm identity, purity, and potency [57]. According to current quality systems, process validation is required where results cannot be "fully verified" by subsequent inspection and test. While statistical lot release testing is used, it is generally not considered a substitute for full process validation for commercial products [58].
- Method Selection: Both culture and PCR play important roles. Regulators often require a method that confirms the absence of viable mycoplasma, for which culture is the historical standard. However, validated PCR methods are increasingly accepted. The high specificity of PCR (often 96-100%) is essential here to prevent false positives that could unnecessarily reject a good product lot [53] [11]. The suite of tests required for lot release is comprehensive, including sterility, mycoplasma, endotoxin, and product identity/potency assays [57].
Diagram: A decision pathway for selecting between PCR and culture methods for mycoplasma testing based on the application scenario and key requirements.
Experimental Protocols and Workflows
Detailed Protocol: Multiplex PCR for Mycoplasma Detection
A developed multiplex PCR protocol for detecting Ureaplasma spp., Mycoplasma genitalium, and Mycoplasma hominis exemplifies a robust molecular method [53].
- DNA Extraction: Bacterial DNA is isolated from 100 µL of specimen using a lysis buffer followed by phenol-chloroform-isoamyl alcohol extraction. The DNA is then precipitated with isopropanol, washed with ethanol, and resuspended in RNase-DNase free water.
- PCR Reaction Setup: Hot-start PCR is performed in a 50 µL reaction volume containing:
- The equivalent of 25 µL of the prepared sample.
- 0.2 mM dNTP mixture.
- 10 mM Tris, 3 mM MgClâ‚‚.
- 25 pmol of each unlabeled forward primer and 25 pmol of biotin-labeled reverse primer.
- 1.25 U of Gold Taq polymerase.
- Thermocycling Conditions: Amplification is carried out as follows:
- 1 cycle: 10 minutes at 95°C (initial denaturation).
- 35 cycles: 15 seconds at 95°C (denaturation), 60 seconds at 60°C (annealing/extension).
- 1 cycle: 5 minutes at 72°C (final extension).
- Product Detection: PCR products are detected using an enzyme-linked oligosorbent assay (ELOSA). Biotinylated PCR products are hybridized with horseradish peroxidase-labeled probes specific to each target and detected in streptavidin-coated microtiter plates [53].
Detailed Protocol: Culture-Based Detection
The conventional culture method, while variable, follows a general workflow [53] [54].
- Inoculation: The specimen (e.g., raw material sample or in-process fluid) is inoculated onto specialized agar plates (e.g., A7 agar for genital mycoplasmas) and/or into liquid broth media.
- Incubation: The inoculated media are incubated at 37°C, often in a 5% CO₂ atmosphere, for up to 5 days or even several weeks, depending on the suspected mycoplasma species [53] [11].
- Observation & Identification: Plates are examined daily under a microscope for the appearance of characteristic "fried-egg" colonies. The A7 agar, for instance, incorporates a test for urease to differentiate Ureaplasma from other species [53]. Subcultures and additional biochemical tests may be required for definitive identification.
Diagram: A side-by-side comparison of the key steps and timeline for PCR and culture-based mycoplasma detection workflows.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for performing the mycoplasma testing methods discussed in this guide.
Table 3: Essential Reagents and Materials for Mycoplasma Testing
| Item | Function/Application | Example from Literature |
|---|---|---|
| Specialized Agar Plates | Supports the growth of fastidious mycoplasma for culture-based detection. | A7 agar for differentiation of Ureaplasma [53]. |
| Primers (Specific) | Short, single-stranded DNA sequences that bind to target mycoplasma DNA for PCR amplification. | Primers targeting urease gene (Ureaplasma), 140-kDa protein gene (M. genitalium), 16S rRNA (M. hominis) [53]. |
| Taq DNA Polymerase | Thermostable enzyme that synthesizes new DNA strands during PCR. | Gold Taq polymerase used in hot-start PCR [53]. |
| dNTP Mixture | The building blocks (nucleotides) used by the polymerase to synthesize DNA. | Included in the PCR master mix [53]. |
| Biotin-Labeled Primers | Allows for non-radioactive detection of PCR products via binding to streptavidin. | Used in reverse primers for subsequent ELOSA detection [53]. |
| Lysis Buffer | Breaks open cells and viruses to release nucleic acids for PCR. | NucliSens lysis buffer [53]. |
| Microtiter Plates (Streptavidin-Coated) | Solid phase for the capture and detection of biotinylated PCR products in an ELOSA. | Used in the final detection step of the multiplex PCR [53]. |
| BChE-IN-33 | BChE-IN-33, MF:C23H17ClN2O3, MW:404.8 g/mol | Chemical Reagent |
| Cu(II)GTSM | Cu(II)GTSM, MF:C6H10CuN6S2, MW:293.9 g/mol | Chemical Reagent |
The choice between PCR and culture methods for mycoplasma testing is not a matter of one being universally superior, but of matching the method to the specific need within the biomanufacturing workflow. PCR methods offer undeniable advantages in speed, sensitivity, and throughput, making them ideal for scenarios where rapid results are critical, such as in-process testing and raw material screening. Culture methods, while slower, provide the unique ability to detect viable organisms and remain important for certain regulatory applications, including lot release where specified. The most robust quality control strategy often involves a complementary use of both techniques. Furthermore, the integration of advanced molecular diagnostics like next-generation sequencing (NGS) and digital PCR may offer even greater sensitivity and specificity in the future, further empowering researchers and drug developers in their mission to ensure product safety.
Optimizing Your Mycoplasma Testing Strategy: Overcoming Common Pitfalls and Limitations
For researchers and drug development professionals, mycoplasma contamination remains a critical concern, capable of compromising experimental validity and product safety. The traditional gold standard for detection, the culture method, is hamstrung by a significant bottleneck: its prolonged turnaround time. This guide provides an objective, data-driven comparison of culture versus polymerase chain reaction (PCR) methods, framing them within the broader thesis that molecular strategies are essential for managing the inefficiencies of traditional techniques in modern, fast-paced research and development environments.
The Gold Standard's Burden: Limitations of Culture-Based Detection
Culture-based methods, as defined by pharmacopeia standards such as USP <63>, require a 28-day agar and broth cultivation process [59]. This extended timeline is fundamentally incompatible with the short shelf-life of many contemporary biologics and cellular therapies, which can be as brief as 48 to 72 hours [59]. The method's reliance on the growth of fastidious organisms in enriched media over weeks makes it impractical for timely decision-making, creating a critical bottleneck in product release and research workflows.
PCR vs. Culture: A Quantitative Performance Comparison
The following table summarizes key performance metrics, illustrating the operational advantages of PCR-based methods.
Table 1: Comparative Analysis of Mycoplasma Detection Methods
| Feature | Culture-Based Methods | PCR-Based Methods |
|---|---|---|
| Turnaround Time | Up to 28 days [59] | Same day to a few hours [38] [60] |
| Limit of Detection (LOD) | Not precisely defined (growth-dependent) | As low as 0.46 copies/µL for some commercial respiratory panels [61] |
| Sensitivity | Lower; estimates suggest 1-3 week growth [38] | High; 96.2% sensitivity reported for oropharyngeal samples [61] |
| Throughput & Automation | Low, manual processes | High, potential for full automation (e.g., Panther Fusion System) [38] |
| Primary Application | Regulatory gold standard for product release [59] | Rapid screening, high-throughput testing, diagnostics [23] [38] |
Beyond speed, PCR methods demonstrate superior analytical sensitivity. A 2023 comparative study of five commercial molecular assays found that the most sensitive PCR tests could detect Mycoplasma contamination at concentrations of 1 CFU/mL, a level not all commercial kits could achieve to meet the ≤10 CFU/mL standard set by European and Japanese pharmacopeias [59].
Experimental Insights: Validating PCR as a Viable Alternative
Key Experimental Protocol: Comparative Sensitivity Testing
A proof-of-principle study provides a template for validating PCR performance against culture methods [59].
- Objective: To evaluate the limit of detection (LOD) and repeatability of five commercial PCR assays compared to culture.
- Methodology:
- Bacterial Strains: Ten cultured Mollicutes species, including quality-control strains from pharmacopeia standards (e.g., A. laidlawii, M. pneumoniae), were used [59].
- Sample Preparation: Each organism was tested at four log-fold dilutions (1,000 CFU/mL to 1 CFU/mL) in biological duplicates with three technical replicates per condition (n=6) [59].
- Testing: The diluted samples were tested using the five commercial PCR kits and compared to culture results. Testing was also performed in the presence of a complex matrix (Tumor Infiltrating Lymphocytes) to check for inhibition [59].
- Key Findings: The Biofire Mycoplasma assay demonstrated the highest sensitivity, followed by the MycoSEQ and MycoTOOL kits. The study confirmed that not all PCR assays automatically meet the stringent ≤10 CFU/mL LOD, highlighting the need for careful assay selection and in-house validation [59].
Key Experimental Protocol: Sample Type Impact on Diagnostic PCR
The choice of sample type significantly impacts diagnostic sensitivity, a variable irrelevant to culture where the organism must grow.
- Objective: To evaluate the diagnostic performance of PCR for detecting Mycoplasma pneumoniae between nasopharyngeal (NP) and oropharyngeal (OP) swabs [61].
- Methodology: A 2025 study collected paired NP and OP swabs simultaneously from 422 children with suspected M. pneumoniae infection. Samples were tested with commercially available PCR tests and validated with RT-PCR [61].
- Key Findings: With RT-PCR as a reference, the sensitivity of a commercially available PCR test was 74.9% for NP swabs versus 96.2% for OP swabs. The study concluded that oropharyngeal samples are superior for detecting M. pneumoniae [61].
The Scientist's Toolkit: Essential Reagents for PCR-Based Mycoplasma Detection
Table 2: Key Research Reagent Solutions for PCR-Based Mycoplasma Detection
| Item | Function | Example from Literature |
|---|---|---|
| Primers & Probes | Amplify and detect unique mycoplasma DNA sequences. | Primers and probe targeting the CARDS toxin gene or the RepMp1 repetitive element [61] [38]. |
| Nucleic Acid Extraction Kit | Isolate high-quality DNA from complex samples. | QIAamp DNA Mini Kit (Qiagen) used in validation studies [61]. |
| Master Mix | Provides enzymes, dNTPs, and buffer for DNA amplification. | TaqMan Universal PCR Master Mix [38]. |
| Positive Control | Validate assay performance and for quantification. | Plasmid containing the target amplicon sequence, quantified via droplet digital PCR (ddPCR) [38]. |
| Universal Transport Media (UTM) | Preserve specimen integrity during transport and storage. | UTM Nasopharyngeal Sample Collection Kit (Copan) [61]. |
Implementing a Solution: A Workflow for Modern Mycoplasma Testing
Adopting PCR-based testing requires a strategic workflow that balances speed with regulatory compliance. The following diagram outlines a streamlined process integrating PCR for rapid results while acknowledging the place of culture methods for confirmatory testing.
Strategic Implementation in Research and Development
Integrating PCR into mycoplasma testing protocols requires more than just purchasing a kit. The following strategies are critical for success:
- Assay Validation: For product release in the US, any non-USP <63> method is considered an alternative and requires rigorous end-user validation to demonstrate equivalency, as per USP <1223> [59].
- Automation for Throughput: Platforms like the Panther Fusion System offer full automation from extraction to detection, enabling high-throughput analysis with continuous sample loading, which is vital for large-scale operations [38].
- Multi-Method Approach: In clinical diagnostics, combining NAATs with serological testing can provide a more comprehensive picture, helping to identify active infections despite the inherent limitations of each method [38].
The data and experimental evidence clearly demonstrate that PCR-based methods offer a powerful strategy for managing the protracted turnaround times of culture-based mycoplasma testing. With their superior speed, sensitivity, and potential for automation, PCR technologies are indispensable for researchers and drug development professionals working under the constraints of short product shelf-lives and aggressive development timelines. While culture methods retain their place as a regulatory gold standard, the strategic integration of validated PCR protocols is no longer a mere alternative but a necessity for efficient and innovative scientific progress.
In the context of a broader thesis on PCR versus culture methods for mycoplasma testing, molecular diagnostics face two fundamental challenges: minimizing false results and ensuring species-specific detection. False-positive and false-negative polymerase chain reaction (PCR) outcomes can significantly impact diagnostic accuracy, therapeutic decisions, and research conclusions. While culture remains the traditional gold standard for pathogen identification, PCR has emerged as a rapid, sensitive alternative with its own set of advantages and limitations [62]. This guide objectively compares the performance of these methodologies, providing supporting experimental data to help researchers, scientists, and drug development professionals navigate the complexities of mycoplasma detection and beyond.
The implications of inaccurate results are substantial. False-negative results can lead to missed diagnoses, delayed treatment, and unintended transmission of infectious agents, while false-positive results may trigger unnecessary treatments, psychological distress, and wasteful consumption of resources [63] [64]. One study analyzing COVID-19 testing found false-negative rates of approximately 9.3%, meaning nearly one in ten infected individuals might be incorrectly told they are not infected [65]. Understanding the sources of these errors and implementing robust validation protocols is therefore essential for any molecular diagnostics program.
Understanding and Preventing False-Positive PCR Results
False-positive PCR results typically occur when amplification signals are generated from non-target sources, leading to incorrect identification of a target pathogen or sequence. These errors can originate from various points in the testing process, from sample collection to data interpretation [63].
Contamination During Sampling and Processing: Aerosolization during sample collection, extraction, or amplification procedures can introduce contaminating nucleic acids. Cross-contamination from high viral titer specimens or contaminated equipment represents a frequent source of false positives [63] [64]. One investigation into false-positive SARS-CoV-2 RT-PCR tests found that contamination and issues with determining the cut-off for low viral load specimens were the two most common problems [63].
Reagent and Laboratory Supply Contamination: Manufacturing processes sometimes lead to contaminated reagents, particularly if positive controls are produced in the same facility. Contaminated consumables (pipette tips, tubes) and laboratory surfaces can also introduce target sequences into reactions [63] [64].
Cross-Reactivity with Non-Target Sequences: Primers may anneal to and amplify genetic sequences from related pathogens, commensal organisms, or host DNA, particularly if primer specificity hasn't been rigorously validated [63]. One study emphasized that primers should be designed to target genes with low levels of conservation and that are highly specific to the species of interest [64].
Data Interpretation Errors: Determining the cutoff between positive, indeterminate, and negative results, particularly with low viral loads or high cycle threshold (Ct) values, can be challenging. Software problems, data entry errors, and miscommunication of results also contribute to false-positive reporting [63].
Prevention Strategies for False Positives
Spatial Separation of PCR Steps: Establishing separate areas or rooms for pre-PCR (sample preparation, reagent setup), PCR amplification, and post-PCR analysis prevents amplicon contamination. Maintaining unidirectional workflow and dedicated equipment for each area significantly reduces false positives [64].
Stringent Laboratory Practices: Using aerosol-barrier pipette tips, fresh gloves, and dedicated lab coats for each area minimizes contamination transfer. Regular decontamination of surfaces with sodium hypochlorite, ethanol, or UV irradiation, along with autoclaving of reusable equipment, further reduces risks [64].
Technical Enhancements for Specificity: Incorporating uracil-DNA-glycosylase (UNG) into PCR reactions prevents carryover contamination by degrading previous amplification products. Hot-start PCR inhibits polymerase activity until high temperatures are reached, preventing nonspecific amplification during reaction setup. Touchdown PCR, which starts with high annealing temperatures then gradually decreases them, favors specific primer binding over non-specific binding [64].
Adequate Controls and Verification: No-template controls (NTC) containing water instead of sample DNA should be included in every run to detect reagent contamination. For low-prevalence settings or unexpected positive results in asymptomatic individuals, retesting the original sample on a different platform or obtaining a new sample for testing is recommended [63] [64].
Understanding and Preventing False-Negative PCR Results
False-negative results occur when a sample contains the target organism but fails to amplify it, potentially leading to missed diagnoses and continued disease transmission. The causes are diverse, spanning pre-analytical, analytical, and post-analytical phases.
Suboptimal Sample Collection and Handling: Poor-quality swabs that fail to collect adequate cellular material, inappropriate sampling sites, or improper storage conditions can all lead to false negatives. Excessive freeze-thaw cycles may degrade nucleic acids, while delays in processing can reduce target viability [64] [65]. One study noted that false negatives can occur due to "testing too early in the disease process, low analytic sensitivity, inappropriate specimen type, low viral load, or variability in viral shedding" [65].
Inhibition of PCR Amplification: Substances present in clinical specimens (hemoglobin, heparin, urea) or introduced during collection (powder from gloves, calcium alginate from swabs) can inhibit DNA polymerases, preventing amplification even when the target sequence is present [64].
Insufficient Analytical Sensitivity: No PCR assay can detect a single molecule of target DNA every time. All assays have a limit of detection (LOD), and samples with target concentrations near this LOD may occasionally test negative. Primer-probe mismatches due to genetic variations in the target organism can also reduce sensitivity [65].
Nucleic Acid Degradation: RNases and DNases present in the environment or samples can degrade target nucleic acids before amplification. Using non-sterile supplies or nuclease-free reagents can introduce these enzymes [64].
Prevention Strategies for False Negatives
Sample Collection and Handling Optimization: Using appropriate swab types (synthetic tips with plastic or metal shafts), proper collection technique, and immediate transportation under correct temperature conditions preserves target nucleic acids. Adding RNase inhibitors during RNA extraction protects labile targets [64].
Inhibition Monitoring and Elimination: Incorporating internal controls that amplify with each sample helps identify inhibition. Adding bovine serum albumin (400 ng/μL) to reaction mixes can neutralize some inhibitors. Diluting samples (1:10) may reduce inhibition enough to allow amplification while maintaining detectable target levels [64].
Proper Assay Design and Validation: Designing longer amplification targets (>100 bp as recommended by FDA) increases assay robustness. Regularly verifying primer specificity through BLAST searches ensures continued detection of circulating strains. Using high-quality reagents and properly calibrated equipment maintains assay sensitivity [64].
Comprehensive Control Systems: Internal controls (amplification of human housekeeping genes like ABL1 mRNA) verify successful nucleic acid extraction, reverse transcription, and amplification while controlling for sampling quality. One study demonstrated that using ABL1 mRNA as an internal control helped identify poor-quality samples that might otherwise yield false negatives [66]. External positive controls with known concentrations of target nucleic acid monitor assay sensitivity and detection limits [64] [66].
Species Selection for Validation Studies
Selecting appropriate species for validation studies is critical for demonstrating assay specificity, particularly for mycoplasma testing where multiple species may cause similar clinical presentations or contaminate biological products.
Method Comparison for Mycoplasma Detection
Table 1: Comparison of Culture and PCR Methods for Mycoplasma Detection
| Parameter | Culture Method | PCR Method |
|---|---|---|
| Time to Result | 7-10 days or longer [62] | 1-2 days [62] |
| Sensitivity | Variable; may miss low-level infections [67] | High; can detect low copy numbers [62] |
| Specificity | Requires subsequent speciation [62] | High with proper primer design [68] [62] |
| Viability Requirement | Requires viable organisms [62] | Detects DNA from viable and non-viable organisms |
| Multiple Species Detection | Difficult without additional testing [62] | Possible with multiplex assays [62] |
| Cost | Lower per test but labor-intensive [62] | Higher per test but less labor [62] |
| Sample Stability | Critical; reduced recovery over time [62] | Less critical; DNA is relatively stable [62] |
Relevant Species for Validation
When validating mycoplasma detection assays, particularly for bovine samples, three species are of primary importance: M. bovis, M. californicum, and M. bovigenitalium [62]. M. bovis is one of the most significant mycoplasma pathogens in cattle worldwide, causing mastitis, arthritis, and pneumonia [62]. M. californicum is the second most common cause of mycoplasma-associated disease in cattle, while M. bovigenitalium is associated with reproductive disorders [62].
For environmental monitoring or pharmaceutical testing, inclusion of Bacillus cereus is valuable due to its spore-forming nature and resistance to pasteurization, making it a concern in donor human milk and other biological products [69]. One study noted that "Bacillus cereus is a pathogen frequently found in DHM, capable of forming spores that can resist Holder pasteurization (62.5°C, 30 min)" [69].
For comprehensive validation panels, consider including:
- Species closely related to targets phylogenetically
- Organisms with genetic similarity that might cross-react
- Common environmental contaminants in the sample type
- Species causing clinically similar presentations
Experimental Design for Validation Studies
Table 2: Performance Comparison of Mycoplasma Detection Methods Across Sample Types
| Sample Type | Culture Positives | PCR Positives | Statistical Difference | Key Findings |
|---|---|---|---|---|
| Individual Milk | Not specified | Not specified | No significant difference | Both methods perform comparably [62] |
| Bulk Tank Milk | Not specified | Not specified | No significant difference | Both methods perform comparably [62] |
| Semen | Not specified | Not specified | No significant difference | Both methods perform comparably [62] |
| Swab Samples | Not specified | Not specified | Culture detected significantly more positives | Culture may be more sensitive for swabs [62] |
| All Sample Types Combined | 16/474 (3.4%) | 17/474 (3.6%) | No significant difference | PCR identified 5 samples with multiple species [62] |
A study comparing culture and multiplex PCR for detecting Mycoplasma species in bovine milk, semen, and swab samples demonstrated that while both methods detected a similar proportion of positive samples overall, PCR identified five samples with two species present, which culture with 16S-23S rRNA sequencing failed to distinguish [62]. This highlights PCR's advantage in detecting mixed infections.
Experimental Protocols and Methodologies
Multiplex PCR for Mycoplasma Species Detection
A validated protocol for detecting M. bovis, M. californicum, and M. bovigenitalium in bovine samples [62]:
Reaction Composition: 0.5 mM dNTPs, 5 mM MgCl₂, 0.5 U GoTaq polymerase, 1 μM of each primer set, 0.25 μM of each probe, 2.0 μL of 5x Buffer, and 2 μL DNA template in 10 μL final volume.
Cycling Conditions: 95°C for 60s, followed by 40 cycles of 95°C for 30s, 60°C for 30s, and 72°C for 30s.
Detection: Performed on a RotorGene 3000 RT-PCR system using green (M. bovis), yellow (M. californicum), and orange (M. bovigenitalium) channels. Data acquisition occurs during the 72°C extension step.
Controls: Each run includes no-template controls and positive controls for each target species.
Interpretation: Samples with cycle threshold (Ct) <40 are considered positive. All samples should be run in triplicate for the mycoplasma assay.
Internal Control Implementation for False-Negative Reduction
A protocol utilizing ABL1 mRNA as an internal control to reduce false negatives in SARS-CoV-2 testing [66]:
Primer Design: Forward primer in first exon, reverse primer in third exon, probe in second exon of ABL1 gene. This design spans long introns (>139,000 nucleotides), preventing amplification from genomic DNA without reverse transcription.
Reaction Composition: Three primer pairs (10 pmol each), three fluorescently labeled probes (5 pmol each), M-MLV reverse transcriptase (10 units), Taq polymerase (1 unit) in 37.5 μL final volume.
Thermal Cycling: Reverse transcription at 50°C for 15 min; 95°C for 5 min; 45 cycles of 95°C for 10s, 58°C for 10s, 72°C for 20s.
Interpretation: Only samples showing ABL1 amplification are valid. SARS-CoV-2 targets are interpreted only when the internal control is positive.
Diagram Title: PCR Workflow with Key Risk Points and Prevention Strategies
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for PCR Validation Studies
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Polymerase Enzymes | Hot-start Taq polymerase, UNG-treated master mixes | Increases specificity, prevents carryover contamination |
| Primer & Probe Sets | Species-specific primers, annealing-control primers | Target detection with reduced nonspecific binding |
| Internal Controls | ABL1 mRNA primers, human housekeeping genes | Monitors extraction efficiency, inhibition detection |
| Inhibition Reversal Agents | Bovine serum albumin (BSA) | Neutralizes PCR inhibitors in complex samples |
| Nucleic Acid Preservation | RNase inhibitors, nuclease-free buffers | Maintains target integrity before extraction |
| Quality Control Materials | Positive control plasmids, reference DNA | Verifies assay performance, standardization |
PCR methodology presents distinct advantages over culture for mycoplasma detection, particularly in speed, ability to detect multiple species simultaneously, and reduced dependence on sample viability. However, both false-positive and false-negative results remain significant challenges that require systematic approaches to mitigation. Through proper assay design, rigorous validation with relevant species, implementation of comprehensive controls, and adherence to strict laboratory practices, researchers can significantly improve the reliability of PCR-based detection systems. The choice between PCR and culture methods ultimately depends on the specific application, required turnaround time, need for viability assessment, and resources available. As molecular technologies continue to evolve, the integration of automated systems and digital PCR platforms promises to further enhance accuracy while reducing the operational variables that contribute to erroneous results.
Mycoplasma contamination represents a critical quality control challenge in biopharmaceutical production and cell culture, with the potential to compromise product safety, efficacy, and regulatory compliance. When establishing a mycoplasma testing program, research and development laboratories face a fundamental economic decision: should they invest in modern polymerase chain reaction (PCR) instrumentation with its associated recurring kit expenses, or rely on traditional culture-based methods with their different cost structures and operational requirements? This analysis objectively compares the financial and technical considerations of these approaches, drawing upon experimental data and economic studies to provide evidence-based guidance for scientists and drug development professionals making capital allocation decisions.
The global mycoplasma testing market, valued at $580 million in 2024 and projected to reach $1,049.9 million by 2032, reflects the growing importance of robust contamination screening protocols in biologics manufacturing and advanced therapy development [70]. Within this expanding market, the choice between PCR and culture methods represents not merely a technical preference but a strategic financial decision with implications for operational efficiency, regulatory compliance, and long-term testing costs.
Methodology Comparison: PCR Versus Culture
Experimental Protocols and Technical Specifications
Gold Standard Culture Method follows pharmacopeia standards (USP <63>, Ph. Eur. 2.6.7) requiring 28-day agar and broth cultivation. This labor-intensive protocol utilizes Hayflick's broth and agar or SP4 medium for fastidious species, with incubation at 35-37°C with 5% CO₂. Detection relies on metabolic activity indicators and colony observation under dissection scope (20× magnification) [59]. The method demands significant technical expertise for interpretation and requires large product volumes (approximately 15mL), making it incompatible with products having short shelf lives [59].
Molecular PCR Detection employs commercially available kits like MycoSEQ (Life Technologies), MycoTOOL (Roche), VenorGEM qOneStep (Minerva Biolabs), ATCC universal Mycoplasma detection kit, and BioFire Mycoplasma assay (bioMérieux). These tests typically utilize real-time PCR or digital PCR platforms with optimized primer sets targeting conserved genomic regions of Mollicutes species. Sample processing involves DNA extraction using reagents like PrepMan Ultra, followed by amplification with platform-specific master mixes [59]. The BioFire Mycoplasma assay demonstrates superior sensitivity, followed by MycoSEQ and MycoTOOL which show comparable performance [59].
Table 1: Key Methodological Comparison Between Culture and PCR Methods
| Parameter | Culture Method | PCR Method |
|---|---|---|
| Time to Result | 28 days [59] | Same day to 24 hours [59] |
| Sample Volume | ~15 mL [59] | <1 mL |
| Labor Intensity | High (multiple subcultures, media preparation) | Moderate (automation compatible) |
| Expertise Required | Specialized microbiological training | Molecular biology techniques |
| Regulatory Status | USP <63> gold standard [59] | Alternative method requiring validation [59] |
Performance Metrics: Sensitivity and Specificity
Comparative studies demonstrate that PCR methods generally offer excellent sensitivity compared to culture methods. In mycoplasma testing for cellular therapy products, the BioFire Mycoplasma assay showed the highest sensitivity, capable of detecting down to 1 CFU/mL for some Mycoplasma species [59]. Not all commercial PCR assays meet the ≤10 CFU/mL limit of detection required to replace culture-based methods according to European and Japanese pharmacopeia standards, highlighting the importance of careful assay selection [59].
In food pathogen detection (a related field), real-time PCR exhibited statistically superior detection sensitivity (p<0.05) compared to standard culture methods, particularly in samples with high background microflora where culture methods generated numerous false-negative results [50]. This enhanced sensitivity in complex matrices has relevance for mycoplasma testing in biological products containing multiple process-related impurities.
Financial Analysis: Instrumentation Versus Consumables
Cost Structure Breakdown
The financial decision between PCR and culture methods revolves around the fundamental trade-off between capital investment and recurring operational expenses. PCR systems require significant upfront instrumentation costs, with digital PCR instruments potentially exceeding $250,000 per unit, while ongoing expenses include reagents and consumables representing 55-65% of lifetime testing expenses [71]. Culture methods conversely demand lower initial equipment investment but incur substantial labor costs, media preparation expenses, and quality control requirements over time.
Table 2: Cost Structure Analysis for Mycoplasma Testing Methods
| Cost Component | PCR Method | Culture Method |
|---|---|---|
| Initial Instrument Investment | $50,000-$250,000+ [71] | $10,000-$50,000 |
| Cost Per Test (Consumables) | $50-$500 [71] [70] | $20-$100 (media and supplies) |
| Labor Cost Per Test | Lower (automation compatible) | Higher (manual processes) |
| Space/Infrastructure Requirements | Moderate (instrument footprint) | Significant (incubators, biosafety cabinets) |
| Quality Control Costs | Moderate (controls, calibration) | High (media QC, strain maintenance) |
| Training Requirements | Molecular techniques | Specialized microbiological skills |
Cost-Effectiveness and Operational Efficiency
Studies across diagnostic applications consistently demonstrate that despite higher per-test costs, PCR methods can yield significant overall savings through improved operational efficiency and better outcomes. In complicated urinary tract infections, PCR-guided treatment provided significantly better clinical outcomes (88.08% vs. 78.11%, p=0.011) with substantially shorter mean turnaround time (49.68h vs. 104.4h, p<0.001) [9]. The faster time-to-result enabled more rapid clinical decision-making, potentially reducing overall treatment costs.
For mycoplasma testing in dairy herds during mastitis outbreaks, the most cost-effective strategy involved bacterial culture, with PCR testing serving as a component of the second most cost-effective alternative [72]. The economic advantage of different testing strategies varied with herd size and disease prevalence, with larger herds benefiting from testing larger sample pools (50 or 100 samples) to improve cost-effectiveness [72]. This demonstrates the context-dependent nature of optimal testing strategy selection.
Decision Framework and Implementation Strategy
Testing Workflow and Process Integration
The selection between PCR and culture methods should follow a systematic decision-making process that accounts for specific application requirements, testing volume, and resource constraints. The following workflow outlines key decision points:
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementation of either testing methodology requires specific reagent systems and materials. The following table details essential components for establishing mycoplasma testing capabilities:
Table 3: Essential Research Reagent Solutions for Mycoplasma Testing
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Hayflick's Broth and Agar | Culture medium for mycoplasma growth | Supports diverse Mycoplasma species; color change indicates metabolic activity [59] |
| SP4 Medium with Arginine | Enhanced culture medium | For fastidious species (M. pneumoniae, M. hyorhinis) [59] |
| PCR Master Mixes | Amplification reaction components | Platform-specific formulations; contain enzymes, dNTPs, buffers |
| Sample Preparation Reagents | Nucleic acid extraction and purification | PrepMan Ultra or similar; compatible with complex matrices [50] |
| Positive Control Strains | Quality assurance and validation | M. pneumoniae, M. orale, A. laidlawii as pharmacopeia standards [59] |
| Inhibition Controls | Detection of PCR interference | Internal controls to identify matrix effects [59] |
The decision between PCR instrumentation with recurring kit expenses versus traditional culture methods for mycoplasma testing involves multifaceted technical, regulatory, and financial considerations. PCR systems offer compelling advantages in speed, sensitivity, and potential for automation, making them suitable for high-throughput laboratories with adequate capital budget. Despite higher per-test costs, the overall economic value proposition may be favorable due to reduced labor requirements and faster time-to-results that accelerate decision-making in drug development pipelines.
Culture methods retain importance as regulatory gold standards and for environments with limited testing volume or capital resources. The 28-day incubation period remains a significant limitation for products with short shelf lives, though the method provides the broadest detection of viable organisms without molecular target dependency.
Future developments in PCR technologies, including further miniaturization, reduced reagent costs through market competition, and increased automation, will continue to improve the cost-benefit equation for molecular methods. Meanwhile, emerging methodologies such as digital PCR and isothermal amplification may offer additional alternatives with different cost structures. Laboratories should regularly reassess their testing approach against evolving technological capabilities and changing operational requirements to maintain optimal economic and scientific outcomes in mycoplasma testing programs.
In cell and gene therapy (CGT) development, safeguarding the integrity of high-cell-density samples is paramount. These samples are not only irreplaceable but also highly vulnerable to degradation and contamination, with mycoplasma contamination representing a major risk that can compromise biological studies and lead to significant economic losses [11]. Effective sample management requires a robust strategy to minimize product loss, integrating stringent contamination control, precise temperature stability, and validated handling procedures [73] [74].
The selection of a mycoplasma detection method is a critical control point. This guide provides a comparative analysis of the primary detection technologies—microbial culture, enzymatic assays, DNA staining, conventional PCR, and real-time PCR—to equip researchers with the data needed to implement the most reliable and efficient testing protocol for their samples.
Comparative Analysis of Mycoplasma Detection Methods
Extensive studies have been conducted to evaluate the performance of different mycoplasma detection techniques. The table below summarizes key performance metrics from a comparative study of 30 cell lines, providing a clear, data-driven overview [11].
Table 1: Performance Metrics of Mycoplasma Detection Methods (n=30 cell lines)
| Detection Method | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive Predictive Value (%) | Negative Predictive Value (%) |
|---|---|---|---|---|---|
| Real-time PCR | 100 | 100 | 100 | 100 | 100 |
| Conventional PCR | 94.44 | 100 | 96.77 | 100 | 92.85 |
| Enzymatic (Mycoalert) | 88.89 | 92.86 | 90.32 | 94.12 | 86.67 |
| DNA Staining (DAPI) | 83.33 | 92.86 | 87.10 | 93.75 | 81.25 |
| Microbial Culture | 55.56 | 100 | 74.19 | 100 | 63.64 |
The data demonstrates the superior performance of nucleic acid amplification tests. Real-time PCR achieved perfect scores across all metrics, establishing it as the most reliable standalone method [11]. Conventional PCR also performed excellently, with high sensitivity and specificity. In contrast, the traditional gold standard, microbial culture, showed significantly lower sensitivity (55.56%), failing to detect nearly half of the contaminations that other methods identified [11].
Further supporting these findings, a 2023 study on bacterial identification in sputum samples confirmed that real-time PCR provides enhanced sensitivity and specificity over culture-based methods. This study reported that real-time PCR detected Haemophilus influenzae and Moraxella catarrhalis at rates nearly double those of culture, highlighting the risk of false negatives with less sensitive methods [75].
Detailed Experimental Protocols
To ensure reproducibility and understanding of the cited data, the experimental workflows for the two primary methods are detailed below.
Protocol for Microbial Culture Method
As the historical gold standard, microbial culture relies on growing mycoplasma in specialized media [11].
- Sample Preparation: Culture cells in an antibiotics-free medium for at least 4-5 days without exchanging the medium prior to testing.
- Inoculation: Inoculate the sample into multiple liquid and solid mycoplasma-specialized culture media (e.g., SP4 medium).
- Incubation: Incubate the media aerobically and anaerobically at 37°C for up to 28 days.
- Observation: Monitor the liquid media for color change (indicating growth) and regularly examine the solid media under a microscope for the characteristic "fried-egg" colony formation.
- Subculture: Subculture from positive liquid media onto solid media to confirm colony morphology.
This method's main limitations are the extended time-to-result (up to 28 days) and lower sensitivity, as some mycoplasma strains are non-cultivable [11] [76].
Protocol for Real-time PCR Method
Real-time PCR offers a rapid, highly sensitive, and specific alternative by detecting mycoplasma DNA [11].
- Sample Collection: Collect supernatant from the cell culture.
- Nucleic Acid Extraction: Extract DNA from the sample using a commercial kit, such as the QIAamp DNA Mini Kit.
- PCR Setup: Prepare the reaction mix using a commercial real-time PCR kit (e.g., PromoKine diagnostic kit) with primers and probes targeting a conserved region of the mycoplasma 16S rRNA gene.
- Amplification and Detection: Run the PCR in a real-time thermocycler with the following typical cycling conditions:
- Initial Denaturation: 95°C for 10 minutes.
- 40 cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 60 seconds (with fluorescence acquisition).
- Result Analysis: Analyze the amplification curve. A sample is considered positive if the fluorescence signal crosses the threshold within the defined cycle number.
Figure 1: Real-time PCR Mycoplasma Detection Workflow
Integrated Strategies for Minimizing Product Loss
Beyond detection, a holistic sample management strategy is essential for protecting valuable CGT samples from all sources of loss, including contamination and physical degradation.
Comprehensive Contamination Control
Mycoplasma testing is one component of a broader Contamination Control Strategy (CCS), as mandated by regulations like the revised EU GMP Annex 1 [73].
- Aseptic Handling: Follow GMP principles and use sterile containers and validated cleanroom protocols during all sample manipulations [73].
- Reagent Quality: Use high-quality, tested reagents. Animal sera, for example, is a common source of mycoplasma and should be sourced from qualified vendors [11].
Ensuring Stability through Cryopreservation
Maintaining sample viability, especially for high-cell-density samples, requires precise cryopreservation.
- Cryoprotectants: Use agents like DMSO (typically at 10% concentration) in combination with appropriate media to reduce ice crystal formation and protect cell viability during freezing [73] [74].
- Controlled-Rate Freezing: Control the cooling rate at approximately -1°C/minute using validated systems to prevent rapid cellular dehydration and damage [73] [74].
- Storage Conditions: For long-term storage, maintain cells at -135°C to -196°C in the vapor phase of liquid nitrogen to halt all metabolic activity [73] [74]. Ultra-low temperature freezers (-80°C) are suitable for some materials like DNA, RNA, and proteins [73].
Robust Chain of Identity and Monitoring
- Traceability: Implement digital systems to log every transfer point with detailed metadata (sample ID, storage conditions, excursions) to ensure a full chain of custody and identity [73] [74].
- Real-Time Monitoring: Use continuous temperature monitoring with alarms for storage units and shipments to proactively intervene during temperature excursions [73] [77].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and kits are fundamental for implementing the mycoplasma detection and sample preservation strategies discussed.
Table 2: Key Reagents and Kits for Sample Management and Mycoplasma Testing
| Product Name/Type | Function | Application Context |
|---|---|---|
| Mycoalert Mycoplasma Detection Kit | Enzymatic assay that detects mycoplasma-specific enzymes, leading to a luminescent signal. | Rapid, high-throughput screening of cell cultures for mycoplasma contamination. Useful for in-process testing [11]. |
| PromoKine Real-time PCR Kit | Contains primers and probes targeting mycoplasma 16S rRNA for highly specific DNA amplification and detection. | The most sensitive and specific method for definitive mycoplasma testing, ideal for lot-release and critical quality control points [11]. |
| Dimethyl Sulfoxide (DMSO) | A cryoprotective agent (CPA) that penetrates cells to prevent intracellular ice crystal formation during freezing. | Essential for cryopreservation of cell therapies. Typically used at 5-10% concentration. Requires post-thaw washing to reduce cytotoxicity [73] [74]. |
| Liquid Nitrogen (Vapor Phase) | Provides an ultra-low temperature environment (-135°C to -196°C) for long-term storage of cells and live biologics. | The standard for preserving the viability and functionality of cell and gene therapy products for extended periods [73] [74]. |
| SERODIA MYCO-II Particle Agglutination Kit | Serological test that detects anti-mycoplasma antibodies (IgM) in patient serum. | Used for serological diagnosis of active M. pneumoniae infection in a clinical setting [76]. |
The integrity of high-cell-density samples in cell and gene therapy is protected by a multi-layered strategy. While robust cryopreservation and cold-chain management are foundational, vigilant contamination control is equally critical. The experimental data conclusively shows that real-time PCR is the superior method for mycoplasma detection, offering unmatched sensitivity, specificity, and speed compared to traditional culture-based methods.
By adopting real-time PCR as a cornerstone of their quality control protocol and integrating it into a holistic sample management framework, researchers and drug developers can significantly minimize product loss, ensure regulatory compliance, and accelerate the delivery of safe and effective therapies to patients.
Head-to-Head: A Data-Driven Comparison of PCR and Culture Method Performance
The detection of mycoplasma contamination is a critical quality control step in the biopharmaceutical industry and cell therapy production. For decades, the culture method has been the gold standard, requiring a minimum of 28 days to complete. The ≤10 colony forming units (CFU) per milliliter sensitivity standard represents the rigorous benchmark for these tests, ensuring that even low-level contaminants are detected. Polymerase Chain Reaction (PCR) technologies have emerged as rapid alternatives, but their ability to consistently meet this stringent sensitivity requirement is a subject of extensive research and validation. This guide examines the experimental evidence supporting PCR's capabilities, comparing various technologies against the ≤10 CFU/mL benchmark.
The Regulatory Standard: Understanding the ≤10 CFU/mL Requirement
International pharmacopoeias, including the European Pharmacopoeia (EP), have established a detection sensitivity of ≤10 CFU/mL for mycoplasma testing. The recent revision of EP chapter 2.6.7 recognizes Nucleic Acid Amplification Techniques (NAT) as equivalent to culture-based methods, formally accepting their use for product release testing when properly validated [16].
A key aspect of this harmonized framework is the introduction of genomic copies (GC) as a standardized unit. The requirement specifies that NAT methods must demonstrate a limit of detection comparable to <100 genomic copies per mL, acknowledging the relationship between genomic material and viable organisms [16]. This equivalence is crucial for comparing molecular methods to traditional culture-based assays.
Performance Comparison of PCR Methods
Extensive research has evaluated the performance of different PCR technologies against the ≤10 CFU/mL standard. The table below summarizes key findings from recent studies:
Table 1: Performance Comparison of Detection Methods for Various Pathogens
| Method | Target Organism | Limit of Detection (LOD) | Sensitivity | Specificity | Turnaround Time |
|---|---|---|---|---|---|
| Liquid Microarray + PCR | Salmonella PMQR genes | 5-25 CFU/mL [78] | Not specified | No positive signals for non-target strains [78] | Not specified |
| Real-time PCR (Qualified with gDNA) | Mycoplasma spp. | <10 CFU/mL equivalent [79] | Meets regulatory requirement [79] | Detects wide variety of strains [79] | Days vs. 28 days for culture [79] |
| Real-time PCR | Mycoplasma spp. | Not specified | 100% [11] | 100% [11] | Not specified |
| Real-time PCR | Avibacterium paragallinarum | 10 CFU/mL [80] | 98.2% agreement with conventional PCR [80] | No cross-reaction with close relatives [80] | Not specified |
| Real-time PCR | Listeria monocytogenes | Statistically superior to culture (p<0.05) [50] | Excellent detection sensitivity [50] | Not specified | Less time consuming than culture [50] |
| Droplet Digital PCR (ddPCR) | Sepsis pathogens | 10 CFU/mL [81] | 70.37% [81] | 55.28% [81] | 4.06 hours [81] |
| Conventional PCR | Shigella spp. | 10² CFU [82] | Lower than RTQ-PCR and ddPCR [82] | Specific amplification [82] | Not specified |
| RTQ-PCR | Shigella spp. | 10¹ CFU [82] | 10× higher than conventional PCR [82] | Specific amplification [82] | Time-consuming due to standard curve [82] |
| ddPCR | Shigella spp. | 10ⰠCFU [82] | 10× higher than RTQ-PCR [82] | Specific amplification [82] | Does not require standard curve [82] |
The data demonstrates that multiple PCR platforms, including real-time PCR and ddPCR, can achieve the requisite ≤10 CFU/mL sensitivity for various bacterial targets, including the fastidious mycoplasma organisms.
Experimental Protocols for Validating PCR Sensitivity
Protocol 1: Qualification Using Genomic DNA
A validated approach for establishing PCR sensitivity without handling live mycoplasma involves using genomic DNA (gDNA) as a reference material [79].
- Step 1: Obtain Quantified gDNA - Use genomic DNA from reference strains like M. arginini (ATCC qCRM-23838D) and M. hominis (ATCC qCRM-27545D) [79].
- Step 2: Establish Genome Copy to CFU Ratio - Apply empirically derived genome copy to CFU (GC/CFU) ratios to convert between genomic copies and the required CFU/mL values [79].
- Step 3: Serial Dilution - Dilute gDNA samples in elution buffer to concentrations spanning the expected limit of detection.
- Step 4: PCR Amplification - Perform PCR amplification using commercial kits like the MycoTOOL PCR Mycoplasma detection kit (Roche) with a modified touchdown PCR protocol [79].
- Step 5: Detection and Analysis - Visualize results by gel electrophoresis and establish the lower limit of detection (LLOD) as the lowest concentration detected in 10 out of 10 reactions [79].
Protocol 2: Direct Culture-Based Comparison
For direct comparison against culture methods, a parallel testing approach is employed:
- Step 1: Sample Preparation - Spike test samples with low concentrations of viable mycoplasma organisms (≤10 CFU/mL) in the actual product matrix [83].
- Step 2: Parallel Processing - Process identical samples using both the PCR method and the compendial culture method.
- Step 3: DNA Extraction - For PCR samples, extract DNA using kits such as the DNeasy blood and tissue kit (Qiagen), often incorporating a concentration step to compensate for small sample volumes [80] [83].
- Step 4: Amplification and Detection - Use real-time PCR systems (e.g., ABI 7500) with universal primers targeting the 16S rRNA sequence conserved across multiple mycoplasma strains [79] [11].
- Step 5: Comparability Assessment - Demonstrate that the PCR method detects the same low level of contamination as the culture method, typically requiring a 100% detection rate at the 10 CFU/mL threshold [83].
The following diagram illustrates the key decision points in the validation workflow:
Key Validation Considerations for Implementation
Sample Volume and Concentration
Most PCR methods use small sample volumes (typically <100μL) in the amplification step, creating a potential 100-fold sensitivity loss compared to culture methods that process up to 15mL. To compensate, sample concentration through centrifugation is essential prior to DNA extraction [83].
Nucleic Acid versus Viable Organism Detection
PCR detects nucleic acids rather than viable organisms, which may lead to false positives from non-viable contaminants. This can be addressed by:
- RNA-based detection targeting organisms actively undergoing protein synthesis [83]
- Quantitative DNA methods monitoring concentration increases over time, indicating replicating organisms [83]
Establishing the Nucleic Acid/CFU Ratio
Determining the relationship between genomic copies and colony forming units is critical for demonstrating equivalence. This requires:
- Using fastidious strains and actively growing cultures
- Minimizing carryover from initial inoculum
- Purified nucleic acids from representative species for spiking experiments [83]
Reagent Solutions for Compliant Testing
Table 2: Essential Research Reagent Solutions for Mycoplasma PCR Testing
| Reagent/Kit | Function | Regulatory Compliance |
|---|---|---|
| Venor Mycoplasma qPCR (Minerva Biolabs) | Quantitative real-time PCR detection of >130 mollicute species | Fully aligned with EP 2.6.7, USP <63>, JP 18 G3 [16] |
| 100GC Mycoplasma Standards | Quantitative reference material with traceable 100 genomic copies/vial | Verifies assay sensitivity in product-specific matrices [16] |
| MycoTOOL PCR (Roche) | Mycoplasma detection with touchdown PCR protocol | Approved by FDA, Health Canada, and EMA [79] |
| DNeasy Blood & Tissue Kit (Qiagen) | DNA extraction from samples | Compatible with various sample matrices [80] |
| MagMax-96 Viral RNA Isolation Kit | High-throughput nucleic acid extraction in 96-well format | Enables automated processing for high-volume testing [80] |
The experimental evidence confirms that properly validated PCR methods can indeed meet the stringent ≤10 CFU/mL sensitivity standard required for mycoplasma testing. Advanced PCR technologies, particularly real-time PCR and ddPCR, demonstrate equivalent or superior sensitivity compared to traditional culture methods while providing results in hours rather than weeks. Success depends on rigorous validation incorporating proper sample concentration, establishment of nucleic acid/CFU relationships, and use of appropriate controls and reference materials. The recent harmonization of pharmacopoeial standards provides a clear framework for implementing PCR methods that meet regulatory requirements while accelerating critical quality control processes in biopharmaceutical manufacturing and cell therapy production.
Mycoplasma contamination represents a critical quality control challenge in pharmaceutical manufacturing and biological research. These small, cell wall-less bacteria can profoundly alter cell metabolism and gene expression, compromising research validity and product safety. The regulatory requirement for mycoplasma testing in cell cultures used for pharmaceutical production necessitates rigorous detection methods. This guide objectively compares the performance of established and emerging mycoplasma detection technologies, with particular focus on analytical specificity and cross-reactivity against compendial species, providing researchers and drug development professionals with data-driven insights for method selection.
Regulatory authorities prescribe specific methods for mycoplasma testing in the biopharmaceutical industry. The European Pharmacopeia and US Code of Federal Regulations outline two primary compendial methods: the culture method and the indicator cell culture method [84]. The culture method involves inoculating cell culture supernatant into specialized broth medium, followed by periodic subculturing onto agar media and examination for characteristic 'fried egg' colonies. This process requires at least 28 days to confirm negative results [84]. The indicator cell culture method, while faster (3-5 days), involves staining Vero cell cultures with Hoechst DNA stain and examining for surface fluorescence indicating contamination [84].
In contrast, molecular methods have emerged as rapid alternatives. PCR-based assays typically target conserved regions of the 16S rRNA gene, enabling broad detection of Mollicutes while minimizing cross-reactivity with other bacterial families [84]. These methods can produce results within 2.5 to 5 hours, offering dramatic time savings for screening applications [84].
Figure 1: Experimental workflow comparison between traditional culture methods and modern PCR-based detection systems
Comparative Performance Data Analysis
Detection Sensitivity Across Methods
Multiple studies have directly compared the performance characteristics of mycoplasma detection methods. A comprehensive evaluation of 30 cell lines found significant variability in detection rates across methods [11].
Table 1: Detection Sensitivity Across Methodologies
| Detection Method | Detection Rate | Sensitivity | Specificity | Time to Result | Reference |
|---|---|---|---|---|---|
| Real-time PCR | 60% | 100% | 100% | 2.5-5 hours | [11] |
| Conventional PCR | 56.66% | 94.44% | 100% | 4-8 hours | [11] |
| Enzymatic MycoAlert | 53.33% | Not specified | Not specified | 1-2 days | [11] |
| DAPI Staining | 46.66% | Not specified | Not specified | 3-5 days | [11] |
| Microbial Culture | 33.33% | 100% | 100% | 28+ days | [11] |
The superior sensitivity of molecular methods is further demonstrated in clinical sample comparisons. A prospective study comparing PCR with culture and serological tests for Mycoplasma pneumoniae diagnosis found that all culture-positive patients were also PCR-positive, and only a combination of PCR and complement fixation test (CFT) allowed diagnosis of all cases [67].
Analytical Specificity and Cross-Reactivity Profiles
The specificity of detection methods is crucial for accurate mycoplasma identification. A multiplex probe PCR assay developed for M. bovis, M. californicum, and M. bovigenitalium demonstrated appropriate amplification for all target isolates with no cross-reactivity observed against other Mollicutes or eubacterial isolates [62]. This high specificity is achieved through careful primer design targeting genomic regions conserved within Mycoplasma species but distinct from related bacteria.
PCR assays achieve broad detection capability while maintaining specificity by targeting the 16S rRNA coding region at loci well conserved across Mollicutes but not in other bacterial species [84]. Properly designed assays can detect up to 100 mycoplasma species while minimizing false positives from non-target organisms.
Table 2: Specificity Profiles of Detection Methods
| Method Type | Cross-Reactivity Concerns | Species Coverage | False Positive Risks |
|---|---|---|---|
| Culture Methods | Difficult to distinguish from Acholeplasma species | Limited to cultivable species | Acholeplasma species due to similar colony morphology |
| PCR-Based Methods | Primarily related to primer design | Up to 100 species with pan-mycoplasma assays | Lower than culture when properly designed |
| Enzymatic Methods | Potential interference from sample components | Varies by assay design | Moderate |
| DAPI Staining | Non-specific DNA binding | All contaminating species | High without confirmatory testing |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Mycoplasma Detection
| Reagent/Kit | Function | Application Context |
|---|---|---|
| SP4 Agar & Broth | Culture medium for mycoplasma growth | Traditional culture methods for broad mycoplasma cultivation [67] |
| Hoechst DNA Stain | Fluorescent DNA binding dye | Indicator cell culture method for microscopic detection [84] |
| 16S rRNA Genus-Specific Primers | Amplification of conserved mycoplasma sequences | PCR detection of multiple mycoplasma species [11] |
| MycoAlert Reagents | Enzymatic detection of mycoplasma enzymes | Rapid, non-culture based screening [11] |
| DNA Extraction Kits (e.g., ION Force FAST) | Nucleic acid purification from complex samples | Sample preparation for PCR-based detection [85] |
| Internal Amplification Controls | Monitoring PCR inhibition | Quality control in molecular assays [67] |
Experimental Protocols for Method Comparison
Protocol 1: Culture-Based Detection (Compendial Method)
- Sample Preparation: Inoculate 50-250 μL of cell culture supernatant into 2 mL of specialized broth medium (e.g., SP4 broth supplemented with amphotericin B and colistin) [67].
- Broth Incubation: Incubate at 36°C in 5% CO₂ atmosphere, monitoring periodically for color change indicating growth [67].
- Agar Subculture: Upon color change or weekly, subculture 50-100 μL from broth onto SP4 agar plates [67].
- Colony Identification: Incubate agar plates at 36°C in 5% CO₂ for up to 4 weeks, examining regularly for characteristic 'fried egg' colonies [67] [84].
- Confirmation: Verify putative mycoplasma colonies by indirect immunofluorescence or PCR sequencing [67].
Protocol 2: Real-Time PCR Detection
- DNA Extraction: Extract nucleic acids from 200 μL of sample using commercial extraction kits following manufacturer's protocols [85].
- PCR Master Mix Preparation: Combine 5 μL of DNA template with 15 μL reaction mix containing primers targeting conserved 16S rRNA regions, probes, and PCR reagents [85] [62].
- Amplification Parameters: Program thermal cycler with conditions typically including: 95°C for 3 minutes, followed by 40 cycles of 95°C for 30 seconds, 60°C for 30 seconds, and 72°C for 30 seconds [62].
- Result Interpretation: Analyze amplification curves; samples with cycle threshold (Ct) values <40 are considered positive [62]. Include appropriate positive and negative controls in each run.
Discussion: Strategic Method Selection
The choice between mycoplasma detection methods involves balancing multiple factors including regulatory requirements, time constraints, and required sensitivity. While culture methods remain the regulatory gold standard for final product release testing, PCR-based methods offer clear advantages for screening applications and process control.
The superior sensitivity of real-time PCR (100% sensitivity and specificity in controlled studies) makes it particularly valuable for detecting low-level contaminations that might be missed by other methods [11]. Additionally, PCR enables identification of multiple species in a single sample, a capability challenging with culture methods followed by 16S-23S rRNA sequencing [62].
However, method selection may depend on sample type. One study found that while culture could detect significantly more positive swab samples, no significant differences were identified for semen, individual milk, or bulk tank milk samples when comparing culture and PCR [62]. This highlights the importance of validating methods for specific sample matrices.
For comprehensive quality control programs, a combined approach utilizing rapid PCR screening for early detection followed by confirmatory culture testing for positive results may provide optimal balance between speed and regulatory compliance.
Mycoplasma detection technology has evolved significantly, with PCR-based methods demonstrating clear advantages in speed and sensitivity while maintaining high specificity against compendial species. The analytical data presented enables researchers and drug development professionals to make evidence-based decisions regarding mycoplasma testing strategies. As regulatory acceptance of molecular methods continues to grow, the integration of these rapid detection platforms throughout the biopharmaceutical workflow will enhance product safety while streamlining development timelines.
The accurate detection of microbial contaminants is a critical pillar of quality control in biomedical research and pharmaceutical development. Among these contaminants, mycoplasma species present a particularly stealthy challenge, capable of altering cell behavior, compromising research validity, and jeopardizing biotherapeutic safety. For decades, culture methods have been regarded as the historical gold standard for mycoplasma detection due to their theoretical ability to support the growth of diverse species. However, the extended time-to-results—often requiring weeks for completion—creates significant bottlenecks in fast-paced research and development pipelines [86] [76].
In contrast, polymerase chain reaction (PCR) technologies offer a paradigm shift toward rapid, molecular-based detection. These methods target specific microbial genetic sequences, providing results in hours rather than weeks. While their adoption is growing, the comparative analytical performance of leading commercial PCR kits against traditional culture methods requires systematic evaluation. Such analysis is crucial for researchers, scientists, and drug development professionals who must balance speed, sensitivity, specificity, and regulatory compliance when selecting detection methodologies. This guide provides an objective, data-driven comparison to inform these critical decisions.
Performance Metrics: PCR Kits vs. Culture
The transition from culture-based to molecular detection methods necessitates a clear understanding of their relative capabilities. The following tables synthesize experimental data from clinical and laboratory studies to compare these methodologies across key performance metrics.
Table 1: Overall Comparative Performance of Detection Methods for Mycoplasma pneumoniae
| Detection Method | Sensitivity (%) | Specificity (%) | Youden Index | Time to Result |
|---|---|---|---|---|
| Culture (Gold Standard) | (Reference) | (Reference) | (Reference) | 2-4 weeks [86] |
| Real-Time PCR (RT-PCR) | 36.6% (Positive Rate) [76] | N/A | N/A | Several hours [86] |
| MP-IgM (Particle Agglutination, PA) | 74.0% [76] | 79.7% [76] | 53.7 [76] | Several hours |
| MP-RNA (SAT) | 57.2% [76] | 97.5% [76] | 54.7 [76] | Several hours |
| Combination (MP-RNA + MP-IgM PA) | 84.2% [76] | 78.7% [76] | 62.9 [76] | Several hours |
Table 2: Performance of Specific Commercial PCR Kits for Various Pathogens
| Commercial PCR Kit | Target Pathogen | Sensitivity / Positive Agreement | Specificity / Negative Agreement | Key Findings |
|---|---|---|---|---|
| Bosphore STD Urethritis Mini Bundle Kit | Mycoplasma genitalium | 83.0% [87] | 100% [87] | Good performance for detecting non-viral STIs [87] |
| Viasure STD Real-Time PCR Kit | Mycoplasma genitalium | 68.1% [87] | 100% [87] | Missed 31.9% of positive specimens [87] |
| Smart Gene Myco (Oropharyngeal Sample) | Mycoplasma pneumoniae | 96.2% [61] | 100% [61] | Superior sensitivity compared to nasopharyngeal sampling [61] |
| Multiplex PCR (Nasopharyngeal Sample) | Mycoplasma pneumoniae | 74.9% [61] | 99.2% [61] | Inferior sensitivity compared to oropharyngeal sampling [61] |
| Doc Lab UTM 2.0 (PCR) | Uropathogens (cUTI) | Detected additional pathogens in 54.44% of cases [88] | N/A | Identified polymicrobial infections in 43.52% of cases vs. 31.95% with culture [88] |
Experimental Protocols for Method Comparison
To ensure the reliability and reproducibility of the data presented, understanding the underlying experimental methodologies is essential. The following protocols are synthesized from the cited comparative studies.
Protocol 1: Culture-Based Mycoplasma Detection
The traditional culture method is a multi-step process that relies on microbial growth.
- Sample Collection: The sample type is critical. For respiratory Mycoplasma pneumoniae, oropharyngeal swabs have demonstrated superior sensitivity over nasopharyngeal swabs [61]. Samples are collected using appropriate swabs and placed in transport media.
- Inoculation and Incubation: The sample is inoculated into specialized liquid and solid mycoplasma culture media. These media are enriched with nutrients, serum, and yeast extract to support the fastidious growth of mycoplasma species.
- Prolonged Incubation: The inoculated media are incubated aerobically at 35-37°C under humidified conditions. Because mycoplasma grows slowly, cultures must be maintained and observed for color changes (in liquid media) or colony formation (on solid media) for up to 4 weeks before a sample can be declared negative [86] [76].
- Confirmation: Suspected colonies on solid media are typically confirmed using DNA-binding fluorochromes like DAPI for microscopic observation.
Protocol 2: Real-Time PCR-Based Mycoplasma Detection
PCR methods detect pathogen-specific genetic material, drastically reducing turnaround time.
- Sample Collection and Nucleic Acid Extraction: Samples (swabs, supernatant from cell cultures, etc.) are collected. For many modern PCR kits, such as the CultureGro Clear, this step is simplified, allowing for direct sample input without separate DNA isolation [89]. For other protocols, DNA is extracted from samples using commercial kits, such as the QIAamp DNA Mini Kit, on platforms like the KingFisher [61] [88].
- PCR Setup: The extracted DNA (or direct sample) is added to a prepared PCR master mix. This mix contains all necessary components for amplification: primers and probes specific to the target mycoplasma DNA sequence (e.g., the CARDS toxin gene), DNA polymerase (e.g., TAQ), dNTPs, and buffer [61].
- Amplification and Detection (Real-Time PCR): The reaction plate or tube is placed in a real-time PCR thermocycler, such as the AriaMx Real-Time PCR System or QuantStudio systems [61] [88]. The instrument runs a programmed thermal cycling protocol. With each cycle, the target DNA is amplified, and a fluorescent probe binds to the amplified product, releasing a signal that is monitored in "real-time."
- Result Analysis: Software analyzes the fluorescence curve to determine if the target pathogen is present (qualitative) and can quantify the bacterial load (quantitative) by comparing to a standard curve. The entire process, from sample to result, can be completed in under 2 hours for some kits [89].
Workflow Visualization
The stark contrast in complexity and duration between the two methods is best understood visually. The following diagram illustrates the sequential steps for both culture and PCR workflows.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful mycoplasma testing, whether by culture or PCR, relies on a foundational set of reagents and instruments. The table below details key solutions and their functions in the featured experimental protocols.
Table 3: Key Research Reagent Solutions for Mycoplasma Detection
| Item | Function / Application | Example Products / Kits |
|---|---|---|
| DNA Extraction Kit | Purifies and isolates microbial DNA from clinical or cell culture samples for subsequent PCR amplification. | QIAamp DNA Mini Kit (Qiagen) [61] [76] |
| PCR Master Mix | A pre-mixed solution containing enzymes, dNTPs, and buffers required for the PCR amplification reaction. | TAQ 2X PCR MasterMix [89] |
| Primer & Probe Mix | Target-specific oligonucleotides that define the genetic sequence to be amplified and detected. | Pro Primer Mix [89], Custom probes for CARDS toxin gene [61] |
| Positive Control | Contains a known quantity of the target sequence; used to validate PCR kit performance and run integrity. | Included in commercial kits [89] |
| Commercial PCR Kit | All-in-one solution typically including master mix, primers/probes, controls, and reaction buffer. | MycoTOOL (Roche) [86], CultureGro Clear [89], Smart Gene Myco [61] |
| Real-Time PCR System | Instrument that performs thermal cycling and fluorescent detection for real-time PCR analysis. | AriaMx (Agilent) [61], QuantStudio 7 or 12 (Thermo Fisher) [88] |
| Culture Media | Enriched broth and agar designed to support the growth of fastidious mycoplasma organisms. | Specialized liquid and solid media [76] |
| Transport Medium | Preserves sample integrity and viability during transport from collection site to laboratory. | Universal Transport Medium (UTM) [61] |
Discussion and Concluding Analysis
The comparative data firmly establishes that modern PCR kits offer a superior alternative to culture for mycoplasma detection in most research and quality control contexts. The most significant advantage of PCR is its dramatic reduction in turnaround time, providing results within hours and enabling rapid decision-making [86]. Furthermore, studies demonstrate that PCR exhibits higher sensitivity for detecting certain pathogens, such as Mycoplasma genitalium and Mycoplasma pneumoniae, particularly when optimal sampling sites (e.g., oropharyngeal) are used [61] [87].
PCR also excels in complex diagnostic scenarios. For complicated urinary tract infections (cUTIs), PCR identified polymicrobial infections in 43.5% of cases, a rate significantly higher than the 32% detected by culture [88]. This enhanced detection capability directly impacts clinical outcomes, as failures to identify polymicrobial infections or resistance markers with culture were linked to significantly higher rates of clinical treatment failure [88].
While culture retains its place in specific scenarios requiring viable organisms, the combination of high sensitivity, speed, and reproducibility makes PCR the pragmatic choice for modern laboratories. The data supports integrating PCR-based testing as a primary method for mycoplasma testing, bolstering both research integrity and biomanufacturing safety.
In the field of pharmaceutical development and biological safety testing, alternative methods—including in vitro, in silico, and chemico approaches—are increasingly vital for replacing, reducing, and refining animal testing (the 3Rs). For researchers and drug development professionals, particularly those focused on mycoplasma testing, navigating the validation requirements of major regulatory jurisdictions is crucial for gaining acceptance of new methodologies. This guide objectively compares the validation frameworks for alternative methods in the United States, European Union, and Japan, with a specific focus on their application in the context of PCR versus traditional culture methods for mycoplasma detection.
The global regulatory environment is dynamically evolving. In the US, the FDA has launched a New Alternative Methods Program to spur the adoption of methods that can replace, reduce, and refine animal testing [90]. Similarly, the EU is progressing with a targeted revision of its Medical Device Regulation (MDR) and In Vitro Diagnostic Medical Device Regulation (IVDR) to simplify the regulatory framework while maintaining patient safety [91]. Japan's Pharmaceuticals and Medical Devices Agency (PMDA) operates under the Pharmaceuticals and Medical Devices Act (PMD Act), which has been amended to incorporate several expedited approval pathways [92]. Understanding these evolving landscapes is essential for successful method validation and regulatory acceptance.
Regulatory Framework Comparison
The validation of alternative methods for mycoplasma testing requires navigating distinct pathways across major regulatory regions. The table below summarizes the core regulatory frameworks and acceptance processes.
Table 1: Regulatory Frameworks for Alternative Methods in the US, EU, and Japan
| Region | Governing Regulations | Key Agencies | Acceptance Process | Key Guidance/Documents |
|---|---|---|---|---|
| United States | Food, Drug, and Cosmetic Act; FDA Modernization Act 2.0 | FDA (CDER, CBER, CDRH), EPA, ICCVAM | Qualification for specific Context of Use (COU) via Drug Development Tool (DDT) programs; Acceptance of OECD test guidelines | FDA's "New Alternative Methods Program" [90]; Various product-specific guidance documents [93] |
| European Union | Medical Device Regulation (MDR) 2017/745; In Vitro Diagnostic Medical Device Regulation (IVDR) 2017/746 | European Commission; Medical Device Coordination Group (MDCG); Notified Bodies | Conformity assessment by Notified Bodies; Compliance with Common Specifications; MDCG guidance documents | MDCG 2024-11: Guidance on qualification of IVDs [94]; Ongoing targeted revision to simplify framework [91] |
| Japan | Pharmaceuticals and Medical Devices Act (PMD Act) | PMDA; MHLW | Pre-market certification; Orphan Drug, Sakigake, and Conditional Early Approval pathways available | PMDA review reports; MHLW ordinances; ICH guidelines adoption [92] |
United States Regulatory Framework
In the United States, the Food and Drug Administration leads regulatory efforts through its New Alternative Methods Program, which aims to spur the adoption of alternative methods for regulatory use that can replace, reduce, and refine animal testing [90]. The program focuses on expanding processes to qualify alternative methods for regulatory use, providing clear guidelines to external stakeholders, and filling information gaps with applied research.
A central concept in the US system is qualification, which allows an alternative method to be evaluated by the FDA in advance for a specific context of use [90]. The FDA employs several qualification programs:
- Drug Development Tool Qualification Programs for drugs and biologics
- Medical Device Development Tools Program for device assessment
- ISTAND Pilot Program to expand drug development tool types
The FDA also accepts alternative methods from Organisation for Economic Cooperation and Development guidelines for some product types, such as the reconstructed human cornea-like epithelium model (OECD TG 437) which replaced rabbit tests for eye irritation for pharmaceuticals [90]. The Interagency Coordinating Committee on the Validation of Alternative Methods coordinates the development and validation of alternative methods across federal agencies [93].
European Union Regulatory Framework
The European Union operates under the Medical Device Regulation and In Vitro Diagnostic Medical Device Regulation, which have been applicable since May 2021 and May 2022 respectively [95]. The system is implemented through the Medical Device Coordination Group, which provides common understanding through endorsed guidance documents on how the regulations should be applied in practice [94].
Recent developments show the EU is responding to industry pressure for regulatory reform. The European Commission has initiated a targeted revision of the MDR and IVDR to address "unintended market access barriers and administrative burdens that threaten device availability and innovation" [91]. The revision aims to achieve administrative burden reduction, enhance predictability of notified body certification, and make conformity assessment requirements more proportionate, particularly for low- and medium-risk devices.
The EU framework utilizes a conformity assessment process conducted by notified bodies, with current transition periods extending to December 2027, 2028, or 2029 depending on device type and risk classification [91]. The European Parliament has called for urgent revision of the regulations, suggesting fast-track pathways for innovative technologies and specific measures to support small and medium-sized enterprises [95].
Japan Regulatory Framework
Japan's regulatory system for pharmaceuticals and medical devices is governed by the Pharmaceuticals and Medical Devices Act, implemented in 2014 [92]. The Pharmaceuticals and Medical Devices Agency conducts scientific review of marketing authorization applications, while final approval authority rests with the Ministry of Health, Labour and Welfare's Pharmaceuticals and Food Safety Bureau.
Japan offers multiple expedited pathways for innovative products:
- Sakigake Designation: For first-in-Japan innovative therapies, providing a 6-month review and dedicated PMDA liaison
- Orphan Drug Designation: For diseases affecting <50,000 people, granting extended data exclusivity (10-year reexamination)
- Conditional Early Approval: For regenerative medicine products based on early-phase data with post-market follow-up
Japan participates in international harmonization through ICH guidelines on global trials and eCTD dossiers to integrate its processes with the US and EU [92]. A unique aspect of Japan's system is the "all-case surveillance" requirement, which forces manufacturers to track safety in every patient using a new drug [92].
Validation Pathways for Alternative Methods
US Validation and Qualification Processes
The US employs a evidence-based framework for validating alternative methods. The FDA's qualification process involves evaluating an alternative method for a specific context of use, defining the boundaries within which available data adequately justify use of the tool [90]. This concept is similar to a drug or medical device's indications for use.
The ICCVAM maintains a table of validated alternative methods accepted by US agencies, which includes methods for various toxicity endpoints [93]. Recent examples of accepted methods include:
- Defined approaches for skin sensitization (OECD Guideline 497) that replace animal use
- In vitro immunotoxicity testing (IL-2 Luc assay) accepted via OECD Test Guideline 444A
- Reconstructed human epidermis method for phototoxicity (OECD Test Guideline 498)
The FDA is also developing the Collection of Alternative Methods for Regulatory Application (CAMERA), an interactive web-based database for users to find validated and qualified new approach methodologies, with a publicly available Beta version planned for Q3 2025 [93].
EU Validation and Conformity Assessment
In the European Union, validation of alternative methods follows a harmonized administrative process guided by MDCG documents. The current system faces challenges with "unpredictable certification timelines and inconsistent practices across the EU" that are "eroding the efficiency of the CE marking process" [91].
The conformity assessment process requires manufacturers to:
- Classify devices according to MDR/IVDR rules
- Prepare technical documentation demonstrating safety and performance
- Engage a notified body for higher-risk devices
- Implement post-market surveillance systems
The EU is working to enhance international cooperation opportunities, including reliance mechanisms where appropriate, to benefit the EU medical device sector [91]. The proposed revisions aim to streamline various procedures and governance arrangements across the regulatory system.
Japan's Validation and Certification System
Japan's validation system operates through the PMDA review process, which involves specialized review divisions for different therapeutic areas [92]. The typical New Drug Application is reviewed by a team from the appropriate PMDA office, with clinical/statistical overview and often "all-hands" discussions by a panel of PMDA scientists and external experts.
Japan has implemented reforms to accelerate access to new therapies, including:
- Super Parallel program: Allows concurrent filing in Japan and abroad, reducing lag
- Conditional Early Approval: Grants temporary, term-limited approval based on early-phase data
- Foreign Exceptional Approval: Allows foreign firms to seek approval without establishing a Japanese subsidiary
After marketing approval, Japan's regulatory oversight continues via mandatory postmarketing commitments, including risk-management plans, periodic reexamination reviews, and the unique "all-case surveillance" studies [92].
Case Study: PCR vs. Culture Methods for Mycoplasma Detection
Technical Comparison of Methods
In the context of mycoplasma testing, polymerase chain reaction methods represent a modern alternative to traditional culture methods. The table below compares their performance characteristics based on current evidence.
Table 2: Performance Comparison of Mycoplasma Detection Methods
| Parameter | PCR Methods | Culture Methods | Experimental Data |
|---|---|---|---|
| Sensitivity | 96.2% (OP samples) [61] | Lower than PCR; requires viable organisms | With oropharyngeal samples, Smart Gene Myco PCR showed 96.2% sensitivity [61] |
| Time to Result | Hours to 1-2 days [60] | 4-28 days for results | PCR provides results "relatively quickly, often within a few hours" [60] |
| Species Coverage | Wide range detectable [60] | Limited to cultivable species | PCR has "ability to detect a wide range of mycoplasma species" [60] |
| Sample Type Impact | Oropharyngeal superior to nasopharyngeal (96.2% vs 74.9% sensitivity) [61] | Dependent on transport conditions | Study showed "sensitivity of MP detection was significantly better in oropharyngeal samples" [61] |
| Equipment Needs | Specialized equipment required [60] | Culture facilities and media | PCR "requires specialized equipment and technical expertise" [60] |
Regulatory Considerations for Mycoplasma Testing Methods
When validating mycoplasma testing methods for regulatory submission, several factors influence acceptance across jurisdictions:
- Sample type validation: Recent research demonstrates that oropharyngeal samples provide significantly better sensitivity (96.2%) compared to nasopharyngeal samples (74.9%) for Mycoplasma pneumoniae detection using PCR [61]. This has implications for method validation protocols.
- Antimicrobial impact: Studies show a negative correlation between fluoroquinolone use and oropharyngeal DNA loads, which can affect detection sensitivity [61]. Validation studies should account for prior antimicrobial treatment.
- Reference standards: Regulatory acceptance often requires comparison against established methods, with real-time PCR testing of residual extracts serving as a reference standard in validation studies [61].
The workflow for validating a new mycoplasma detection method typically involves the process below, which illustrates the key stages from initial development through regulatory acceptance.
Essential Research Reagent Solutions
Successful validation of alternative methods requires specific research reagents and materials. The table below details essential solutions for implementing mycoplasma detection methods.
Table 3: Essential Research Reagents for Mycoplasma Detection Validation
| Reagent/Material | Function | Application Context |
|---|---|---|
| Universal Transport Medium | Preserves sample integrity during transport and storage | Used in nasopharyngeal sample collection for multiplex PCR testing [61] |
| DNA Extraction Kits | Isolate and purify nucleic acids for amplification | QIAamp DNA Mini Kit used in RT-PCR validation studies [61] |
| PCR Master Mixes | Provide enzymes, buffers, nucleotides for amplification | Contains primers, probes for CARDS toxin gene target in RT-PCR [61] |
| Specific Primers/Probes | Target unique genetic sequences for detection | Forward: 5'-TTTGGTAGCTGGTTACGGGAAT-3', Reverse: 5'-GGTCGGCACGAATTTCATATAAG-3' [61] |
| Fluorescent Dyes/Stains | Enable detection of DNA in various assay formats | DAPI (4',6-diamidino-2-phenylindole) binds A-T rich regions in DNA [60] |
| Positive Controls | Verify assay performance and sensitivity | MP reference strain M129 (ATCC 29342) used in validation [61] |
| Extraction Buffer Solutions | Lyse cells and stabilize nucleic acids | Buffer with surfactants and chaotropic salts for oropharyngeal samples [61] |
The regulatory landscapes for alternative methods in the US, EU, and Japan are evolving toward greater acceptance of modern approaches like PCR for mycoplasma detection, though through distinct pathways and requirements. The United States employs a context-of-use qualification framework through FDA programs and ICCVAM. The European Union is undergoing targeted revisions to simplify its MDR/IVDR framework while maintaining safety standards. Japan offers expedited pathways through PMDA while maintaining rigorous post-market surveillance.
For researchers validating mycoplasma testing methods, key considerations include:
- Sample type selection significantly impacts sensitivity, with oropharyngeal samples outperforming nasopharyngeal for PCR detection [61]
- Method validation must account for pre-analytical factors like antimicrobial exposure that affect DNA loads [61]
- Regulatory strategy should leverage expedited pathways where available and address region-specific documentation requirements
The continuing harmonization of international standards and mutual acceptance of validated methods will further streamline the global approval process for alternative methods, potentially reducing development timelines while maintaining rigorous safety standards.
Conclusion
The choice between PCR and culture methods for mycoplasma testing is no longer a simple binary but a strategic decision based on product shelf-life, regulatory requirements, and operational efficiency. While culture remains the recognized compendial standard, advanced PCR methodologies offer a compelling alternative with unparalleled speed, sensitivity, and suitability for short-lived cell and gene therapies. The future of mycoplasma testing lies in the continued adoption and regulatory acceptance of these rapid molecular methods, the integration of automation and high-throughput platforms, and the development of even more robust, multiplexed assays. By strategically implementing these advanced testing protocols, the biopharmaceutical industry can enhance product safety, accelerate time-to-market for critical therapies, and fortify its defenses against this persistent contaminant.
References
- 1. Mycoplasma Testing Market Outlook 2027 [https://www.pharmiweb.com/press-release/2025-11-19/mycoplasma-testing-market-outlook-2027-key-developments-and-future-scope]
- 2. Mycoplasma Testing Market Size, Share [https://www.fortunebusinessinsights.com/mycoplasma-testing-market-108687]
- 3. Antimicrobial susceptibility and molecular characteristics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568347/]
- 4. Antibiotic resistance and viral co-infection in children ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-10712-0]
- 5. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 6. Comparative analysis between digital PCR and blood ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1615409/full]
- 7. Comparative diagnostic evaluation of real-time PCR and ... [https://pubmed.ncbi.nlm.nih.gov/41269024/]
- 8. Mycoplasma Testing Market Size & Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/global-mycoplasma-testing-market]
- 9. Clinical utility of PCR compared to conventional culture ... [https://www.sciencedirect.com/science/article/pii/S0732889324004255]
- 10. Mycoplasma [https://unclineberger.org/tissueculture/contaminant/mycoplasmacontam/]
- 11. Real-time PCR assay is superior to other methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4960155/]
- 12. How Does Mycoplasma Contamination Affect Cell Culture? [https://www.eppendorf.com/us-en/lab-academy/life-science/cell-biology/how-does-mycoplasma-contamination-affect-cell-culture/]
- 13. Metabolomics reveals mycoplasma contamination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6300981/]
- 14. STRATEGY FOR VALIDATION OF NEW MYCOPLASMA ... [https://journal.pda.org/content/early/2025/09/27/pdajpst.2025-000023.1]
- 15. Specifity and sensitivity of polymerase chain reaction (PCR ... [https://www.sciencedirect.com/science/article/pii/002217599390279G]
- 16. New EP 2.6.7 Revision: Compliant Mycoplasma Testing [https://www.rapidmicrobiology.com/news/ep-2-6-7-revision-compliant-mycoplasma-testing-for-biopharma-and-atmps]
- 17. Mycoplasma Testing for Quality Control [https://www.atcc.org/microbe-products/applications/quality-control/mycoplasma-testing]
- 18. Comprehensive Testing Strategies: Reliable Analytical ... [https://www.bioprocessintl.com/process-development/safeguarding-bioproduction-modalities-comprehensive-testing-strategies-require-reliable-analytical-processes-and-reference-materials]
- 19. Pharmacopoeial Standards: USP vs. EP vs. JP [https://masi.eu/en-usd/blogs/longevity-news/pharmacopoeial-standards-usp-vs-ep-vs-jp?srsltid=AfmBOorJ3_Dex8H5eBaEbVp-A9xpjuogH6_Q1j9XRM1SWd-PA0pxBosW]
- 20. An Overview of USP , , and Standards [https://www.fluidimaging.com/blog/usp-787-usp-788-usp-789-standards-injectables]
- 21. Biosafety Testing of Biologicals for Mycoplasma ... [https://www.bioprocessintl.com/analytical/biosafety-testing-of-biologicals-for-mycoplasma-contamination]
- 22. Mycoplasma In-Process and Lot Release Testing: To PCR ... [https://www.bioprocessintl.com/manufacturing/mycoplasma-in-process-and-lot-release-testing-to-pcr-or-not-to-pcr]
- 23. Rapid, season-specific PCR testing versus traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318422/]
- 24. The scope of mycoplasma contamination within ... [https://pubmed.ncbi.nlm.nih.gov/20362237/]
- 25. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 26. Mycoplasma Contamination Risks in Biomanufacturing - Mabion [https://www.mabion.eu/science-hub/articles/mycoplasma-contamination-in-biologics-manufacturing/]
- 27. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 28. Development of real-time PCR methods for quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058689/]
- 29. Cell bank system, establishment, and application in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409320/]
- 30. Why Mycoplasma Testing Is Critical for Mammalian Cell ... [https://cellculturecompany.com/why-mycoplasma-testing-is-critical-for-mammalian-cell-cultures/]
- 31. Comparison of Culture and PCR Methods for Diagnosis ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4138688/]
- 32. Comparison of PCR with the Routine Procedure for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC356878/]
- 33. Systematic review Performance of molecular tests for ... [https://www.sciencedirect.com/science/article/pii/S1198743X24005937]
- 34. PCR vs. Microbial Culture: Is it Time for a Diagnostic ... [https://www.reviewofophthalmology.com/article/pcr-vs-microbial-culture-is-it-time-for-a-diagnostic-paradigm-shift]
- 35. PCR vs. Traditional Culture Methods in Diagnosing UTIs [https://realdxlabs.com/pcr-vs-traditional-culture-methods-in-diagnosing-utis/]
- 36. PCR-based diagnostics for infectious diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC7106425/]
- 37. A new method for detecting mycoplasma in cell cultures ... [https://www.sciencedirect.com/science/article/pii/S2405580825002201]
- 38. Implementation of a Laboratory-Developed Test for the ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300490/]
- 39. A Basic Guide to Real Time PCR in Microbial Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC5288344/]
- 40. How Does qPCR Work? (Technology Basics) [https://biosistemika.com/blog/qpcr-technology-basics/]
- 41. Principles of digital PCR and its applications in current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6943456/]
- 42. Medical diagnostic value of digital PCR (dPCR) [https://www.sciencedirect.com/science/article/pii/S2667099223000221]
- 43. Absolute quantification of Mycoplasma pneumoniae in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1177273/full]
- 44. Droplet Digital PCR versus qPCR for gene expression ... [https://www.nature.com/articles/s41598-017-02217-x]
- 45. Direct qPCR is a sensitive approach to detect Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6823952/]
- 46. Basic Principles of RT-qPCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/basic-principles-rt-qpcr.html]
- 47. Automated urine culture system with reduced turnaround time [https://www.sciencedirect.com/science/article/abs/pii/S073288932500149X]
- 48. Real-time PCR assays compared to culture-based ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/21077984/]
- 49. PCR Testing Outperforms Traditional Culture Methods for ... [https://www.doclabinc.com/blog/pcr-vs-culture-uti-research/]
- 50. Comparison of Culture, Conventional and Real-time PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4662229/]
- 51. Diagnostic comparison of microbial culture and ... [https://www.sciencedirect.com/science/article/pii/S277270762500178X]
- 52. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 53. Comparison of Multiplex PCR Assay with Culture for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC387538/]
- 54. Which is a Better Lab Test, PCR or Culture? [https://americanpharmacogenomicsassociation.com/li-newsletter/pcr-or-culture/]
- 55. Molecular Diagnostic Methods Versus Conventional Urine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459428/]
- 56. Comparison of In-house PCR with Conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2615280/]
- 57. Lot Release Testing [https://www.sartorius.com/en/services/biologics-testing/lot-release-testing]
- 58. Lot Release Testing versus Process Validation Studies [https://elsmar.com/elsmarqualityforum/threads/lot-release-testing-versus-process-validation-studies.63913/]
- 59. Comparison of Five Commercial Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9945500/]
- 60. Mycoplasma Detection Kits Compared: PCR vs. ELISA ... [https://synapse.patsnap.com/article/mycoplasma-detection-kits-compared-pcr-vs-elisa-vs-dapi-staining]
- 61. PCR sensitivity for Mycoplasma pneumoniae detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345179/]
- 62. Comparison of culture and a multiplex probe PCR for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0173422]
- 63. False Positive Results With SARS-CoV-2 RT-PCR Tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7934325/]
- 64. Preventing False Positive and False Negative PCR Results [https://www.clinicallab.com/preventing-false-positive-and-false-negative-pcr-results-26261]
- 65. False negative rate of COVID-19 PCR testing: a discordant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7794619/]
- 66. How to Avoid False-Negative and False-Positive COVID-19 ... [https://www.mdpi.com/2673-8937/2/2/18]
- 67. Comparison of PCR, Culture, and Serological Tests for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC84154/]
- 68. Novel Species-Specific Primers Enable Accurate Detection ... [https://www.sciencedirect.com/science/article/pii/S0362028X25000195]
- 69. Validation of a Real-Time PCR Assay for Fully Automated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299169/]
- 70. Testing Market Size, Share and Forecast Report 2032 Mycoplasma [https://www.credenceresearch.com/report/mycoplasma-testing-market]
- 71. PCR Molecular Diagnostics Market Size Report (2025-2030) [https://www.mordorintelligence.com/industry-reports/pcr-molecular-diagnostics]
- 72. -effectiveness of diagnostic strategies using quantitative real-time... Cost [https://pubmed.ncbi.nlm.nih.gov/24485275/]
- 73. sample storage and stability for the next generation of cell ... [https://www.astoriom.com/insight/cell-and-gene-therapy-sample-storage-best-practices/]
- 74. Cell & Gene Therapy Cold Chain: Ensuring Product Integrity [https://www.cellandgene.com/topic/cell-gene-therapy-cold-chain]
- 75. Real-time PCR has advantages over culture-based methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000296/]
- 76. Comparison of different detection methods for Mycoplasma ... [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-021-02523-4]
- 77. Cell & Gene Therapies [https://www.envirotainer.com/segments/therapy-areas/cell-and-gene-therapies/]
- 78. Validation of a liquid microarray technology combined with ... [https://pubmed.ncbi.nlm.nih.gov/41206656/]
- 79. A Rapid and Sensitive Nucleic Acid Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7044503/]
- 80. Validation of a real-time PCR assay for high-throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6727126/]
- 81. Optimizing Clinical Indicators in Hematologic Malignancies ... [https://link.springer.com/article/10.1007/s40121-025-01207-1]
- 82. Comparing the performance of conventional PCR, RTQ ... [https://www.sciencedirect.com/science/article/abs/pii/S0890850819304219]
- 83. Top Ten Validation Considerations when Implementing a ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/112516-Top-Ten-Validation-Considerations-when-Implementing-a-Rapid-Mycoplasma-Test/]
- 84. Mycoplasma Detection in Cell Cultures [https://www.rapidmicrobiology.com/test-method/rapid-detection-of-mycoplasmas]
- 85. Performance Evaluation of a Commercial Real-Time PCR ... [https://www.mdpi.com/2304-8158/13/4/609]
- 86. MycoTOOL Mycoplasma Real-Time PCR Kit [https://custombiotech.roche.com/global/en/products/cb/mycotool-mycoplasma-real-time-pcr-kit-3531932.html]
- 87. Clinical evaluation of two commercial PCR kits for the ... [https://pubmed.ncbi.nlm.nih.gov/40605691/]
- 88. The Clinical Validity and Utility of PCR Compared to ... [https://www.mdpi.com/2076-2607/13/4/949]
- 89. CultureGro Clear™ – Mycoplasma Detection Kit [https://cellculturecollective.com/product/culturegro-clear-pcr-mycoplasma-detection-kit-100-reactions/?srsltid=AfmBOor1j-n_wqj-9oKUOsUT3CHUZlTVqmzmCVAzOkAchSV8E7lXMMVs]
- 90. Implementing Alternative Methods [https://www.fda.gov/science-research/advancing-alternative-methods-fda/implementing-alternative-methods]
- 91. EU progresses targeted revision of medical device rules ... [https://www.osborneclarke.com/insights/eu-progresses-targeted-revision-medical-device-rules-amid-industry-pressure]
- 92. Japan's PMDA Drug Approval: Standard & Expedited ... [https://intuitionlabs.ai/articles/pmda-regulatory-pathways-japan]
- 93. Alternative Methods Accepted by US Agencies [https://ntp.niehs.nih.gov/whatwestudy/niceatm/accept-methods]
- 94. MDCG endorsed documents and other guidance - Public Health [https://health.ec.europa.eu/medical-devices-sector/new-regulations/guidance-mdcg-endorsed-documents-and-other-guidance_en]
- 95. EU Medical Devices Legislation: What You Need To Know ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/03/eu-medical-devices-legislation-what-you-need-to-know]