Scaffold-Based 3D Spheroid Models: Enhancing Physiological Relevance in Cancer Research and Drug Development
This article provides a comprehensive overview of scaffold-based three-dimensional (3D) spheroid models, which have emerged as indispensable tools bridging the gap between traditional 2D cell cultures and in vivo models.
Scaffold-Based 3D Spheroid Models: Enhancing Physiological Relevance in Cancer Research and Drug Development
Abstract
This article provides a comprehensive overview of scaffold-based three-dimensional (3D) spheroid models, which have emerged as indispensable tools bridging the gap between traditional 2D cell cultures and in vivo models. We explore the foundational principles demonstrating how these models more accurately mimic the complex tumor microenvironment, including cell-cell and cell-matrix interactions, nutrient gradients, and drug resistance mechanisms. A detailed methodological analysis covers scaffold fabrication techniques, material choices, and specific applications across cancer types like osteosarcoma, pancreatic, and prostate cancer. The content further addresses common troubleshooting challenges and optimization strategies for generating consistent, high-quality spheroids, while presenting validation data comparing scaffold-based approaches to other 3D culture methods. This resource equips researchers and drug development professionals with the knowledge to implement and optimize these physiologically relevant models for improved preclinical screening and therapeutic development.
Why 3D Matters: The Scientific Foundation of Spheroid Models for Physiological Relevance
The Limitations of 2D Monolayers in Predicting Clinical Outcomes
In the pipeline of drug discovery and therapeutic development, preclinical testing serves as the critical gateway to human clinical trials. For decades, this testing has relied heavily on two-dimensional (2D) monolayer cultures, where cells are grown on flat, rigid plastic surfaces. While these systems have contributed fundamentally to our understanding of cellular biology, their ability to predict clinical outcomes in human patients remains profoundly limited. This discrepancy contributes significantly to the high attrition rates of candidate drugs, particularly in oncology, where the failure rate of oncology drugs in clinical development remains notably high. The fundamental issue lies in the vast physiological difference between the simplified 2D environment and the complex, three-dimensional (3D) architecture of human tissues. As research pivots toward more physiologically relevant models, 3D spheroid cultures have emerged as powerful tools that bridge the gap between traditional 2D monolayers and in vivo physiology. This review examines the core limitations of 2D monolayers and outlines how scaffold-based 3D spheroid techniques are advancing predictive accuracy in preclinical research.
Fundamental Limitations of 2D Monolayer Cultures
Altered Cell Morphology and Polarity
In vivo, cells exhibit complex 3D architectures and establish distinct apical-basal polarity, which is crucial for their specialized functions. The forced planar geometry of 2D monolayers disrupts this innate polarity, leading to aberrant cell spreading and flattened morphologies that do not reflect native tissue organization [1]. For instance, pancreatic β-cells derived from human pluripotent stem cells (hPSCs) in 2D cultures predominantly display an immature phenotype, failing to achieve the full functional maturity seen in native islets, where 3D arrangement is critical for proper cell-cell connectivity and polarity [1]. This morphological distortion subsequently alters fundamental cellular processes, including proliferation, differentiation, and apoptosis.
Loss of Native Tissue Microenvironment and Signaling
The tumor microenvironment (TME) is a critical regulator of cancer progression and therapy response, comprising complex interactions between cancer cells, stromal cells, and the extracellular matrix (ECM). 2D models largely lack this complexity, as they are devoid of essential ECM components and the heterotypic cell-cell interactions present in vivo [2]. This simplified system fails to replicate the biochemical signaling gradients of growth factors, cytokines, and metabolites that drive tumor behavior and drug resistance. Consequently, drug responses observed in 2D monolayers often show poor correlation with in vivo efficacy, as demonstrated in ovarian cancer models where carboplatin response in 2D cultures correlated with in vivo results in only 3 out of 6 cell lines [2].
Absence of Physiological Gradients
Solid tissues and tumors in vivo are characterized by the presence of nutrient, oxygen, and metabolic waste gradients that arise from limitations in diffusion. These gradients create regional variations in proliferation, metabolic activity, and cell viability. In contrast, 2D monolayers provide largely homogeneous conditions where all cells are equally exposed to nutrients, oxygen, and tested compounds [3]. This fails to model the hypoxic cores commonly found in solid tumors, which are known to contribute to chemoresistance and are a key feature replicated in 3D spheroid models [3].
Inadequate Representation of Drug Penetration and Efficacy
The compact architecture of 3D tissues presents a physical barrier to drug penetration that is entirely absent in 2D monolayers, where drugs have direct and uniform access to all cells. This discrepancy leads to systematic overestimation of compound efficacy in 2D systems [3]. In vivo, drugs must traverse multiple cell layers and ECM barriers to reach their targets, a process directly modeled in 3D spheroids but not in 2D monolayers. Furthermore, the non-physiological cell-ECM interactions in 2D cultures alter the expression of drug transporters and efflux pumps, further skewing drug response data.
Table 1: Core Limitations of 2D Monolayer Culture Systems
| Limitation Category | Specific Deficiencies | Impact on Predictive Value |
|---|---|---|
| Architectural & Morphological | Altered cell shape and polarity; Loss of native 3D structure | Disrupted cell signaling and differentiation; Poor functional maturity |
| Microenvironmental | Lack of ECM; Absence of heterotypic cell interactions; Simplified cell-ECM signaling | Fails to model TME-mediated drug resistance; Altered gene expression profiles |
| Physiological Gradients | Homogeneous nutrient/O2 distribution; No metabolic waste gradients | Does not replicate hypoxic, quiescent, or necrotic zones found in vivo |
| Pharmacological Response | Uniform drug exposure; No penetration barriers; Altered adhesion-mediated survival | Overestimates drug efficacy; Fails to predict penetration-related resistance |
Quantitative Comparisons: 2D vs. 3D Model Performance
Direct comparative studies highlight the superior predictive value of 3D models for clinical outcomes. In a systematic investigation of epithelial ovarian cancer (EOC), the correlation between carboplatin responses in various preclinical models and in vivo mouse xenografts was quantitatively assessed [2]. The results demonstrated that 2D monolayer responses correlated with in vivo results in only 50% of tested cell lines (3/6). In contrast, 3D spheroid models showed correlation in 67% of cases (4/6), while ex vivo 3D micro-dissected tumor models correlated in 83% (5/6) [2]. This clear gradient of increasing predictive accuracy from 2D to 3D models underscores the critical importance of model dimensionality.
Similar trends have been observed in nanotoxicology studies. When A549 lung cancer cells and normal PC9 cells were treated with silver nanoparticles, significant differences in cytotoxicity were observed between 2D and 3D culture systems [4]. The 3D spheroids demonstrated notably different sensitivity profiles, with the spatial-temporal structure of the 3D environment playing a "pivotal role" in the inflammatory and cytotoxic responses [4]. This confirms that the dimensional context fundamentally alters cellular responses to external stimuli.
In neurological disease modeling, the limitations of 2D systems are particularly striking. The discordance between preclinical animal studies and human clinical trials for neurological disorders like Alzheimer's disease, stroke, and traumatic brain injury has been substantial, with many drugs showing promise in 2D cultures and animal models failing in human trials [5]. This has driven the adoption of 3D brain organoids derived from induced pluripotent stem cells (iPSCs), which better recapitulate the complex cellular interactions and tissue architecture of the human brain [5].
Table 2: Correlation of Preclinical Models with In Vivo Therapeutic Response in Ovarian Cancer
| Preclinical Model Type | Correlation with In Vivo Response | Key Advantages | Key Limitations |
|---|---|---|---|
| 2D Monolayer | 50% (3/6 cell lines) [2] | Simple, cost-effective, high-throughput | Poor physiological relevance; No TME |
| 3D Spheroid | 67% (4/6 cell lines) [2] | Recapitulates some TME features; Gradient formation | Limited complexity; Variable reproducibility |
| 3D Ex Vivo Micro-dissected Tumor | 83% (5/6 cell lines) [2] | Preserves native TME and heterogeneity | Limited scalability; Technically challenging |
The Transition to Three-Dimensional Spheroid Models
Architectural and Functional Advantages of Spheroids
Spheroids are defined as spherical, self-assembled cellular aggregates that mimic key aspects of native tissue architecture. Their fundamental advantage lies in reestablishing physiological cell-cell and cell-ECM interactions that mediate tissue function and drug response [6]. Unlike 2D monolayers, spheroids develop distinct concentric zones that replicate the microenvironment of solid tumors: an outer proliferative zone, an intermediate quiescent zone, and a central necrotic or hypoxic zone [3]. This structural organization arises from the diffusion limitations of oxygen, nutrients, and metabolic waste, closely mirroring the conditions found in avascular micro-regions of tumors.
The functional consequences of this 3D architecture are particularly evident in stem cell differentiation protocols. In pancreatic β-cell generation, transitioning from 2D to 3D culture systems has proven essential for achieving functional maturity of hPSC-derived β cells [1]. The 3D environment provides the necessary cell-ECM interactions and endocrine-to-endocrine cell contacts that drive the maturation of glucose-responsive insulin-secreting cells, more closely mimicking the in vivo islet niche [1].
Enhanced Predictive Capacity for Drug Screening
The pharmacological response in 3D spheroids more accurately predicts in vivo outcomes because these models reintroduce critical drug penetration barriers and cell-ECM-mediated resistance mechanisms absent in 2D systems [3]. This is particularly valuable for screening chemotherapeutic agents, where penetration limitations significantly impact efficacy. The spatial organization of spheroids means that cells in different zones exhibit varying susceptibility to therapeutic agents, replicating the heterogeneous treatment responses observed in human tumors.
In the context of immunotherapy development, particularly for CAR-T cell research, 3D spheroid and organoid models provide a more physiologically relevant platform for evaluating efficacy [7]. Unlike 2D co-culture systems, 3D models incorporate immunosuppressive factors and stromal components of the TME that CAR-T cells must overcome in solid tumors, offering more predictive insights into clinical performance [7].
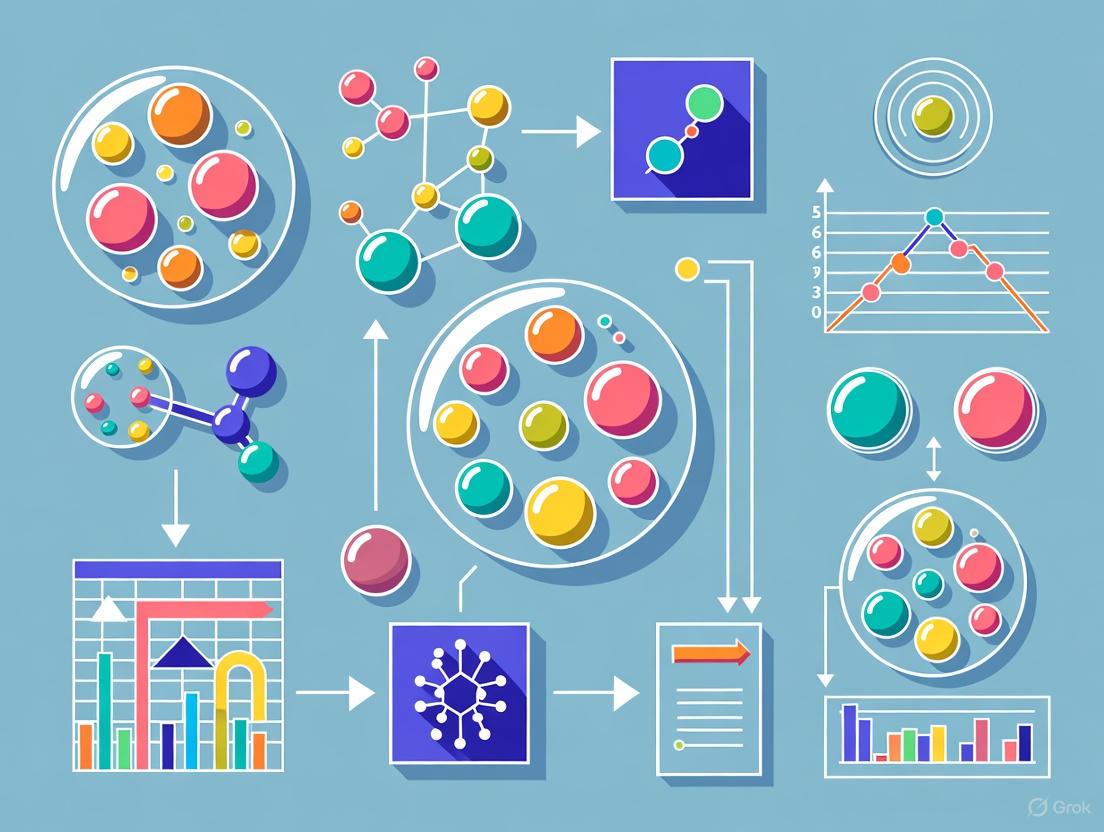
Diagram 1: Architectural and Functional Comparison Between 2D and 3D Models
Experimental Protocols for 3D Spheroid Generation and Assessment
Spheroid Formation Methodologies
Several well-established techniques enable reliable generation of 3D spheroids for research applications. The choice of methodology depends on the specific research requirements, including throughput, uniformity, and biological complexity.
Liquid-Overlay Techniques employ ultra-low attachment (ULA) plates with concave-bottom wells to promote cell aggregation by preventing adhesion to plastic surfaces. This method was utilized in ovarian cancer spheroid research, where 2,000-2,500 cells in 100 μL of complete medium were seeded per well of a 96-well ULA microplate, followed by centrifugation at 1,000 rpm for 5 minutes to encourage aggregation [2]. Spheroids formed over 48 hours of incubation, reaching approximately 500 μm in diameter [2].
Hanging Drop Methods utilize surface tension to create suspended droplets containing cell suspensions, which aggregate at the bottom of the droplet to form spheroids. While this technique produces highly uniform spheroids, it has limitations in throughput and is less amenable to long-term culture due to evaporation.
Scaffold-Based Approaches employ natural or synthetic ECM materials such as Matrigel, collagen, or alginate to provide structural support that mimics the in vivo ECM. These systems are particularly valuable for incorporating multiple cell types and studying invasion. In micro-dissected tumor production for ovarian cancer research, tumor slices were processed using a McIlwain tissue chopper to obtain 350 μm thick sections, followed by creation of sphere-like micro-dissected tissues (MDTs) using a 500 μm biopsy punch [2].
Microfluidic and Bioprinting Technologies represent advanced approaches that enable precise spatial control over cell placement and the creation of complex, multi-cellular tissue architectures with perfusable vascular networks.
Key Assessment Methodologies for Spheroid Models
Viability and Cytotoxicity Analysis in spheroids requires specialized approaches adapted to 3D structures. The alamarBlue assay protocol has been optimized for drug dose-response determination in 3D tumor spheroids, addressing the diffusion limitations that can skew results in 3D systems [4]. Similarly, live/dead assays using fluorescent staining (e.g., calcein AM for live cells, ethidium homodimer for dead cells) provide spatial information on viability within different spheroid regions.
Morphometric Analysis of spheroid size, shape, and integrity provides critical data on growth dynamics and treatment effects. Brightfield microscopy enables routine monitoring, while automated image analysis systems can quantify parameters like spheroid area and circularity over time.
Histological and Immunofluorescence Techniques adapted for spheroid sections reveal internal architecture, proliferation gradients (via Ki-67 staining), hypoxic regions (via pimonidazole or HIF-1α staining), and protein expression patterns. These require specialized processing and sectioning protocols for 3D structures.
Molecular Analysis including RNA and protein extraction from spheroids presents technical challenges due to their compact nature, often requiring specialized dissociation protocols or laser capture microdissection for regional analysis.
Table 3: Research Reagent Solutions for 3D Spheroid Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Specialized Cultureware | Ultra-Low Attachment (ULA) Plates; Hanging Drop Plates | Prevents cell adhesion; Promotes 3D aggregation |
| Scaffold Matrices | Matrigel; Collagen I; Alginate | Provides ECM mimicry; Supports complex morphology |
| Extracellular Matrix Components | Laminin; Fibronectin; Hyaluronic Acid | Enhances physiological relevance; Influences cell signaling |
| Dissociation Agents | TrypLE; Accutase; Collagenase/Hyaluronidase mixes | Gentle spheroid dissociation for downstream analysis |
| Viability Assays (3D-optimized) | AlamarBlue; PrestoBlue; CellTiter-Glo 3D | Assess metabolic activity; Account for 3D diffusion |
| Histology Processing Kits | Spheroid Gel-Embedding Kits; Specialized Fixation Buffers | Preserves 3D structure for sectioning and staining |
Diagram 2: Standardized Workflow for 3D Spheroid Drug Testing
The limitations of 2D monolayer cultures in predicting clinical outcomes are extensive and well-documented, spanning architectural, microenvironmental, and pharmacological domains. The simplified geometry of 2D systems, combined with their absence of physiological gradients and inadequate representation of drug penetration barriers, fundamentally limits their translational relevance. The compelling evidence from comparative studies indicates that 3D spheroid models offer superior predictive value for clinical responses, particularly in complex disease contexts like oncology, neurology, and metabolic disorders.
The field continues to evolve with emerging technologies that further enhance the physiological relevance of 3D models. Organ-on-a-chip systems that incorporate fluid flow and mechanical stimulation, patient-derived organoids that capture individual tumor heterogeneity, and advanced bioprinting techniques that enable precise spatial control over multiple cell types represent the next frontier in predictive preclinical modeling [7]. These technologies, used in complementary fashion with simpler 3D spheroids, promise to further bridge the gap between in vitro models and human physiology.
As the scientific community increasingly recognizes the limitations of 2D monolayers, the transition to 3D model systems represents not merely a technical enhancement but a fundamental necessity for improving the efficiency of drug development and reducing late-stage clinical failures. The ongoing standardization of 3D culture protocols and analytical methods will be crucial for maximizing the potential of these advanced models to predict clinical outcomes accurately and transform the preclinical research landscape.
The development of effective anticancer drugs remains a major challenge, with only an estimated 5-7% of new oncology molecules successfully gaining clinical approval [8] [9]. The majority of drug candidates fail due to unanticipated toxicity and poor efficacy in human trials, often resulting from the low correlation between preclinical models and human pathophysiology [8]. This translational gap is largely attributed to the inability of traditional two-dimensional (2D) cell culture systems to reproduce the complex tumor architecture and cellular crosstalk that characterize human tumors in vivo [8] [10]. Over recent years, three-dimensional (3D) cell culture models have emerged as biologically relevant platforms that more accurately mimic the tumor microenvironment (TME), bridging the gap between conventional 2D cultures and in vivo animal models [8] [3].
This technical guide examines the core principles underlying the recapitulation of the TME in 3D models, with particular focus on spheroid models and scaffold-based techniques. We will explore the key cellular and non-cellular components of the TME, detail methodologies for reconstructing these elements in 3D systems, and provide practical protocols for researchers developing these models for drug discovery applications.
The Tumor Microenvironment: Composition and Significance
The tumor microenvironment is a highly heterogeneous and dynamic ecosystem consisting of both cellular and non-cellular components that collectively influence tumor progression, metastasis, and therapeutic response [10]. The accurate reproduction of these elements in vitro is essential for creating predictive cancer models.
Cellular Components
In solid tumors, the TME contains diverse non-cancerous cells that play active roles in all stages of tumorigenesis [10]. The table below summarizes the key stromal cell types and their functions in the TME.
Table 1: Key Cellular Components of the Tumor Microenvironment
| Cell Type | Primary Functions in TME | Impact on Tumor Progression |
|---|---|---|
| Cancer-Associated Fibroblasts (CAFs) | Stimulate tumor cell proliferation via growth factor secretion; modify ECM; modulate inflammatory components [10]. | Drive tumor progression, metastasis, and angiogenesis [10]. |
| Mesenchymal Stem Cells (MSCs) | Interact with tumor cells via secretion of growth factors/cytokines; transfer mitochondria or microRNAs; form fibrovascular network [10]. | Can either promote invasion or inhibit tumor growth depending on context [10]. |
| Endothelial Cells | Form vascular network for nutrient delivery; protect tumor cells from immune system [10]. | Essential for tumor growth and metastasis; target for anti-angiogenic therapy [10]. |
| Pericytes | Stabilize blood vessel structure and permeability; serve as MSC reservoir [10]. | Influence tumor growth and metastasis through vessel stabilization [10]. |
| Immune Cells | Various functions including immune surveillance, phagocytosis, and antigen presentation [10]. | Can either inhibit or facilitate tumor growth depending on polarization [10]. |
Non-Cellular Components
The non-cellular compartment of the TME includes the extracellular matrix (ECM), which provides structural support and biochemical signals that influence tumor cell behavior [8] [10]. The ECM composition is dynamically remodeled in cancer, leading to altered stiffness and organization that promotes invasion and metastasis [10]. Additional non-cellular elements include oxygen gradients, pH variations, cytokines, growth factors, and extracellular vesicles that facilitate communication between tumor and stromal cells [10].
Core Principles of TME Recapitulation in 3D Models
Three-dimensional cancer models replicate critical features of the TME through several fundamental principles that distinguish them from traditional 2D cultures.
Architectural Organization
Unlike monolayer cultures where cells grow on flat, rigid surfaces, 3D models enable cells to establish spatial relationships and cell-cell contacts that mimic in vivo tissue organization [8] [3]. This 3D architecture influences critical cancer phenotypes including proliferation, differentiation, and drug response [8].
Gradient Formation
A defining characteristic of 3D models is their ability to establish physiochemical gradients of oxygen, nutrients, metabolites, and therapeutic agents [8] [3]. As in native tumors, these gradients create distinct microenvironments within the same structure, leading to the formation of concentric zones with different cellular states:
Stromal-Vascular Recapitulation
Advanced 3D models incorporate non-cancerous stromal cells to recreate the cellular heterogeneity of the TME [8] [10]. This includes cancer-associated fibroblasts (CAFs), mesenchymal stem cells, endothelial cells, and various immune populations. The incorporation of vascular networks represents a particular challenge but is essential for modeling larger tissue constructs and simulating drug delivery [9].
Table 2: Comparison of 2D vs 3D Cancer Models for TME Recapitulation
| Feature | 2D Models | 3D Models |
|---|---|---|
| Spatial Architecture | Monolayer; forced apical-basal polarity [8] | Three-dimensional; natural cell orientation [8] |
| Cell-Cell Interactions | Limited to peripheral contacts [8] | Extensive 3D interactions mimicking in vivo [8] [3] |
| Cell-ECM Interactions | Artificial (plastic/glass surface) [8] | Physiological with natural or engineered ECM [8] |
| Proliferation Gradient | Uniform proliferation [8] | Zonal proliferation (outer > inner) [3] |
| Oxygen/Nutrient Gradients | Uniform distribution [8] | Physiological gradients from periphery to core [8] [3] |
| Drug Penetration | Immediate and uniform access [8] | Limited penetration mimicking in vivo barriers [8] |
| Stromal Component Integration | Challenging with limited functionality [8] | More physiological co-culture possible [8] [10] |
| Hypoxic Core | Absent [8] | Present in spheroids >400-500μm [8] [3] |
| Gene Expression Profile | Often altered due to unnatural substrate [8] | More closely resembles in vivo expression [8] |
| Drug Response Prediction | Poor clinical correlation [8] | Improved clinical relevance [8] |
Technical Approaches for 3D TME Modeling
Scaffold-Free Techniques
Scaffold-free methods rely on the innate tendency of cells to aggregate and form self-assembled structures, most commonly spheroids [9].
Spheroid Formation Methods
Forced-Floating/Liquid Overlay Technique: This method employs ultra-low attachment (ULA) plates coated with hydrophilic polymers that inhibit protein adsorption and cellular attachment [9]. The ease of preparation and compatibility with high-throughput screening make this approach particularly valuable for drug discovery applications [3] [9].
Hanging Drop Method: This technique involves suspending cell droplets from the lid of a culture plate, using surface tension to maintain the suspension while gravity promotes cell aggregation at the liquid-air interface [9]. While demonstrating approximately 90% reproducibility for multicellular tumor spheroid formation, challenges remain for medium exchange and integration with functional assays [9].
Agitation-Based Methods: These approaches use dynamic suspension cultures maintained through continuous orbital shaking, spinner flasks, or rotating wall vessels to prevent cell adhesion and promote aggregation [9].
Table 3: Scaffold-Free Spheroid Formation Techniques
| Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Forced-Floating (Liquid Overlay) | Ultra-low attachment surfaces prevent adhesion [9]. | Simple; amenable to high-throughput screening; scalable [3] [9]. | Variable spheroid size/shape; reproducibility challenges [9]. |
| Hanging Drop | Gravity-induced aggregation in suspended droplets [9]. | High reproducibility (~90%); uniform spheroids [9]. | Difficult medium exchange; limited scalability for assays [9]. |
| Magnetic Levitation | Magnetic nanoparticle incorporation enables spatial manipulation [9]. | Precise spatial control; rapid aggregation [9]. | Potential nanoparticle toxicity; specialized equipment needed [9]. |
| Agitation-Based | Continuous motion prevents adhesion [9]. | Scalable for large spheroid production [9]. | Shear stress on cells; specialized equipment required [9]. |
Scaffold-Based Techniques
Scaffold-based approaches provide a biomimetic extracellular matrix (ECM) that supports 3D tissue formation and offers precise control over the biochemical and mechanical properties of the microenvironment [9].
Natural Polymer Scaffolds
Hydrogels derived from natural materials such as collagen, Matrigel, fibrin, and alginate are widely used for 3D cancer models [10]. These materials provide biological recognition sites that support cell adhesion, migration, and differentiation, closely mimicking the native ECM [10].
Synthetic and Hybrid Scaffolds
Synthetic polymers including PEG-based hydrogels and PLA/PLGA scaffolds offer enhanced tunability of mechanical properties and degradation kinetics but may lack natural cell adhesion motifs [10]. Hybrid approaches combining synthetic and natural materials provide a balance between controllability and bioactivity [10].
Vascularization Strategies
The incorporation of functional vasculature represents a significant advancement in 3D TME models, enabling the creation of larger, more physiologically relevant tissue constructs that overcome diffusion limitations [9].
Experimental Protocols for 3D TME Modeling
Protocol 1: Multicellular Spheroid Generation via Liquid Overlay Method
This protocol establishes a foundation for creating 3D tumor spheroids containing both cancer and stromal cells to model the cellular heterogeneity of the TME [3] [9].
Materials and Reagents
Table 4: Essential Research Reagents for 3D TME Modeling
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Ultra-Low Attachment Plates | ULA plates with hydrophilic polymer coatings [9]. | Prevent cell adhesion and promote 3D aggregation [9]. |
| Basal Media | DMEM, RPMI-1640 [3]. | Provide essential nutrients for cell growth and maintenance [3]. |
| Supplementation | Fetal Bovine Serum (FBS); growth factors [3]. | Support cell viability and proliferation [3]. |
| Stromal Cells | Cancer-associated fibroblasts (CAFs); mesenchymal stem cells (MSCs) [10]. | Recapitulate tumor-stromal interactions [10]. |
| Endothelial Cells | Human umbilical vein endothelial cells (HUVECs) [10]. | Model vascular components of TME [10]. |
| Immune Cells | Macrophages, T cells [10]. | Reproduce immune context of TME [10]. |
| Extracellular Matrix | Collagen, Matrigel [10]. | Provide biomechanical and biochemical cues [10]. |
Procedure
Cell Preparation: Harvest and count cancer cells and stromal cells (e.g., CAFs, endothelial cells) at the desired ratio (typically ranging from 1:1 to 10:1 cancer:stromal cells) [10] [3].
Cell Seeding: Prepare a mixed cell suspension in complete medium at a concentration of 1-5 × 10⁴ cells/mL. Seed 100-200 μL per well in 96-well ULA plates [9].
Spheroid Formation: Centrifuge plates at 300-500 × g for 5-10 minutes to promote initial cell contact. Incubate at 37°C with 5% CO₂ for 24-72 hours to allow spheroid consolidation [9].
Culture Maintenance: Carefully replace 50-70% of medium every 2-3 days without disrupting formed spheroids [9].
Quality Control: Monitor spheroid formation daily using brightfield microscopy. Well-formed spheroids should exhibit smooth, spherical morphology with compact structure [3].
Protocol 2: Vascularized 3D TME Model Using Bioprinting
This advanced protocol creates vascularized tumor models using 3D bioprinting technology, enabling the study of drug delivery and metastasis in a more physiological context [10] [9].
Materials and Reagents
- Bioink Components: Gelatin methacryloyl (GelMA), hyaluronic acid methacrylate (HAMA), or other photopolymerizable hydrogels [10]
- Vascular Cells: Human umbilical vein endothelial cells (HUVECs), human lung microvascular endothelial cells (HULEC), or induced pluripotent stem cell-derived endothelial cells (iPSC-ECs) [10]
- Support Cells: Mesenchymal stem cells or pericytes [10]
- Bioprinter: Extrusion-based or light-based bioprinting system [10]
- Photoinitiator: Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) or Irgacure 2959 for crosslinking [10]
Procedure
Bioink Preparation: Mix tumor cells with bioink material at a density of 5-20 × 10⁶ cells/mL. Prepare separate vascular bioink containing endothelial cells and support cells at 10-30 × 10⁶ cells/mL [10].
Printing Process: Using a dual-printhead system, print the tumor compartment followed by the vascular network pattern. For extrusion printing, maintain pressure (15-30 kPa) and temperature (4-22°C) optimized for cell viability and printing resolution [10].
Crosslinking: Apply appropriate crosslinking method (UV light for photopolymerizable systems, ionic crosslinking for alginate-based systems) to stabilize the printed structure [10].
Maturation Culture: Transfer constructs to perfusion bioreactors if available, or use static culture with frequent medium changes. Culture for 7-14 days to allow vascular network maturation [9].
Validation: Assess vessel formation and functionality through immunohistochemistry (CD31 staining), dextran perfusion assays, and measurement of endothelial barrier function [9].
Applications in Drug Discovery and Development
The enhanced physiological relevance of 3D TME models makes them particularly valuable for preclinical drug screening and development.
Drug Efficacy and Penetration Studies
Three-dimensional TME models enable the evaluation of drug penetration kinetics, a critical factor in anticancer drug efficacy that cannot be assessed in 2D systems [8] [3]. The presence of physiological barriers in 3D models, including compact tissue architecture and pressure gradients, more accurately predicts in vivo drug behavior [8].
Therapy Resistance Mechanisms
The zonal heterogeneity in 3D models recreates the subpopulations of tumor cells that contribute to therapy resistance in vivo [8] [3]. Quiescent cells in the intermediate zone and hypoxic cells in the core exhibit reduced sensitivity to conventional chemotherapeutics, mimicking the treatment-resistant populations observed in patient tumors [8].
High-Throughput Screening Compatibility
Adaptation of 3D models to high-throughput screening formats enables their application in large-scale drug discovery campaigns [8] [3]. Automated imaging and analysis systems allow for quantitative assessment of complex phenotypic responses in 3D contexts, providing more predictive data for lead optimization [8].
The recapitulation of the tumor microenvironment in 3D models represents a significant advancement in cancer research and drug development. By capturing the multicellular architecture, physicochemical gradients, and stromal interactions characteristic of in vivo tumors, these models provide a more physiologically relevant platform for studying tumor biology and therapeutic response. While challenges remain in standardization, vascularization, and scalability, ongoing technological innovations continue to enhance the fidelity and utility of 3D TME models. Their integration into the drug development pipeline promises to improve the predictive power of preclinical studies and ultimately increase the success rate of cancer therapeutics in clinical trials.
The evolution of three-dimensional (3D) cell culture models, particularly spheroids, represents a paradigm shift in biomedical research, offering a critical bridge between traditional two-dimensional (2D) monolayers and in vivo studies. Spheroids are spherical cellular aggregates that spontaneously self-organize, recreating cell-cell and cell-matrix interactions found in native tissues [3]. This architectural complexity enables the formation of physiological gradients—of oxygen, nutrients, and metabolic waste—that drive the emergence of heterogeneous cellular zones mirroring those in solid tumors and tissues [11]. Within these zones, proliferating cells occupy the oxygen-rich outer layer, quiescent cells reside in an intermediate zone, and necrotic or apoptotic cells form a hypoxic core [3] [11]. This recapitulation of in vivo conditions has positioned spheroid models as indispensable tools for advancing cancer biology, drug discovery, regenerative medicine, and personalized therapeutic screening.
The fundamental distinction in spheroid generation lies in the use of external supporting matrices. Scaffold-based methods utilize a three-dimensional artificial matrix that mimics the native extracellular matrix (ECM), providing mechanical support and biochemical cues to promote cell aggregation and growth [11] [12]. These scaffolds can be derived from natural materials like collagen or Matrigel, or synthetic polymers such as poly(ethylene glycol) (PEG). In contrast, scaffold-free methods rely on preventing cell-substrate adhesion, thereby forcing cells to aggregate via cell-to-cell contacts and secrete their own ECM components [12]. This forced self-assembly more closely replicates developmental processes like embryogenesis and organogenesis [12]. The choice between these approaches significantly influences spheroid properties, experimental outcomes, and translational potential, necessitating a clear understanding of their respective advantages and limitations.
Methodological Foundations: Techniques and Protocols
Scaffold-Based Spheroid Generation
Scaffold-based techniques provide a biomimetic environment that can be tailored to specific research needs. The foundational protocol involves embedding cells within a hydrogel or seeding them onto a pre-formed porous scaffold.
Natural Hydrogel Protocols: For Matrigel-based cultures, cells are suspended in chilled Matrigel and dispensed into culture plates. The plate is then incubated at 37°C for 30 minutes to allow polymerization before adding culture medium [13]. This method supports extensive outgrowth; for instance, merospheres and paraspheres embedded in Matrigel migrate outward to form epithelial sheets, while holospheres remain intact as stem cell reservoirs [14] [13].
Synthetic Scaffold Systems: Synthetic polymers like PEG or polycaprolactone (PCL) offer controlled mechanical properties and avoid batch-to-batch variability. Cells are typically mixed with polymer precursors and cross-linked to form a stable 3D network [11]. Recent advances include micropatterned PEG hydrogel plates that generate highly uniform spheroid arrays for high-throughput screening [12].
Microfluidic and Specialized Systems: "Organ-on-a-chip" microfluidic platforms incorporate continuous perfusion, creating dynamic physiological environments. These systems often contain microchannels coated with hydrogels that provide scaffolding while allowing precise control over the microenvironment [12].
Scaffold-Free Spheroid Generation
Scaffold-free methods promote spheroid formation through physical means that enhance cell-cell contact while minimizing cell-surface adhesion.
Liquid Overlay Technique: This widely used method employs plates coated with non-adhesive substrates, such as agar or agarose, or commercially available ultra-low attachment (ULA) plates. Cells are seeded and gravity-mediated aggregation forms spheroids within 24-72 hours [11]. The six-well ULA format generates heterogeneous spheroid populations (holospheres, merospheres, paraspheres), while 96-well ULA plates like BIOFLOAT and Elplasia produce highly uniform spheroids ideal for screening [14] [13].
Hanging Drop Method: Cells are suspended in droplets from a plate lid, with surface tension and gravity forcing aggregation into a single spheroid per droplet. This technique produces highly uniform spheroids without specialized equipment, though it can be labor-intensive [11].
Agitation-Based Methods: Techniques using rotating wall vessels or bioreactors maintain cells in suspension through continuous stirring, preventing adhesion and promoting aggregation. While simple, these methods can produce a broad size distribution and expose cells to shear stress [11] [12].
Emerging Technologies: Magnetic levitation and 3D bioprinting represent advanced scaffold-free approaches. Bioprinting, particularly the "Kenzan" method using microneedle arrays, positions spheroids as bioink units into predetermined architectures where they fuse into cohesive tissues [15].
Table 1: Standardized Protocols for Spheroid Formation
| Method | Key Reagents/Equipment | Protocol Summary | Incubation Time | Resulting Spheroid Characteristics |
|---|---|---|---|---|
| Scaffold-Based (Matrigel) | Matrigel, chilled tips, 37°C incubator | Suspend cells in chilled Matrigel, plate, polymerize at 37°C, then add medium [13] | 30 min polymerization + 48-72h culture | Integrated spheroids with outgrowth capacity; holospheres maintain stemness |
| Scaffold-Free (Liquid Overlay - 96-well) | ULA plates (e.g., BIOFLOAT, Elplasia) | Seed cell suspension (e.g., 5,000-50,000 cells/well in 50μL), incubate undisturbed [13] | 48 hours | Highly uniform spheroids; size controlled by initial seeding density |
| Scaffold-Free (Liquid Overlay - 6-well) | 6-well ULA plates | Seed 8,000 cells in 2mL medium per well, incubate undisturbed [13] | Several days | Heterogeneous populations: holospheres (408.7 μm²), merospheres (99 μm²), paraspheres (14.1 μm²) |
| Hanging Drop | Hanging drop plates or lid | Suspend cells in droplets (20-40μL), invert, culture | 3-5 days | Highly uniform spheroids, single spheroid per droplet |
Comparative Analysis: Performance and Applications
Architectural and Functional Differences
The choice between scaffold-based and scaffold-free methods directly impacts spheroid architecture, gene expression, and drug response profiles. A head-to-head comparison of non-small cell lung cancer (NSCLC) spheroids demonstrated that scaffold-based (SB) A549 spheroids developed larger diameters and elevated deposition of extracellular matrix compared to their scaffold-free (SF) counterparts [16]. This structural difference correlated with enhanced drug resistance, showing a trend of IC₅₀ (A549-SB) > IC₅₀ (A549-SF) > IC₅₀ (A549-2D) across five chemotherapeutics [16].
Both SF and SB spheroids displayed elevated expression of epithelial-to-mesenchymal transition (EMT) markers and drug resistance-associated genes compared to 2D monolayers [16]. However, the enhanced resistance in SB spheroids was attributed not only to physiological barriers but also to the ECM acting as a physical barrier to drug penetration [16]. This highlights how the choice of spheroid production method can fundamentally influence the properties and drug responses of the resulting 3D model.
Applications Across Research Domains
Drug Screening and Development: Scaffold-free systems excel in high-throughput compound screening due to their scalability and reproducibility [3] [14]. The forced-floating and ULA plate methods predominate in this domain, with 96-well formats generating large numbers of uniform spheroids compatible with automated imaging and analysis pipelines [3] [13]. The physiological gradients in spheroids better predict drug penetration and efficacy, addressing the high failure rates of drugs that show promise in 2D models [12].
Regenerative Medicine and Tissue Engineering: Scaffold-based approaches demonstrate particular utility in regenerative applications. For skin regeneration, Matrigel-embedded epithelial spheroids enable study of re-epithelialization and stem cell potential [14] [13]. In osteochondral regeneration, scaffold-free ES-MSC spheroids cultured in a customizable chamber system fused into integrated tissue constructs that successfully repaired cartilage defects in ex vivo models [17]. For complex organ regeneration, scaffold-free stem cell spheroids serve as bioink in bioprinting strategies, leveraging tissue self-assembly to create cohesive constructs without synthetic materials [15].
Personalized Medicine and Cancer Research: Patient-derived spheroids enable therapeutic testing tailored to individual patients. The five most investigated cancer origins for spheroid seeding are breast, colon, lung, ovary, and brain cancers [3] [18]. While scaffold-based methods provide microenvironmental context, scaffold-free approaches using forced-floating methods predominate for initial drug sensitivity testing due to their reliability and versatility [18].
Table 2: Functional Comparison of Scaffold-Based vs. Scaffold-Free Spheroid Models
| Parameter | Scaffold-Based Models | Scaffold-Free Models |
|---|---|---|
| Physiological Relevance | Recapitulates cell-ECM interactions; provides biochemical and mechanical cues [11] [12] | Enhanced cell-cell contacts; self-secreted ECM; mimics developmental aggregation [12] |
| Reproducibility & Uniformity | Batch-to-batch variability in natural scaffolds (e.g., Matrigel); more challenging to achieve uniformity [12] | High reproducibility with commercial ULA plates; size control via seeding density [13] [12] |
| Drug Resistance Properties | Higher resistance (IC₅₀) due to combined physiological and ECM barriers [16] | Moderate resistance compared to 2D, but less than scaffold-based models [16] |
| Throughput Capability | Lower throughput; more suitable for mechanistic studies [14] | High-throughput compatible, especially 96-well ULA formats [3] [14] |
| Technical Complexity | Higher complexity; potential need for enzymatic digestion for spheroid recovery [12] | Simpler workflow; easily adaptable to existing lab routines [12] |
| Primary Applications | Regenerative medicine, mechanistic studies of cell-ECM interactions, migration studies [14] [13] | High-throughput drug screening, personalized medicine, fundamental tumor biology [3] [12] |
Technical Considerations and Standardization
Methodological Optimization and Enhancement
Several technical advancements have emerged to enhance spheroid formation and functionality. ROCK1 inhibition (using Y-27632) in scaffold-free keratinocyte cultures significantly enhances holosphere formation, preserves stemness markers (BMI-1+), and reduces premature differentiation [14] [13]. This treatment increases the proportion of holospheres from 11.3% to 23.8% while decreasing paraspheres from 67.9% to 49.5%, effectively shifting the population toward more stem-like spheroids with greater regenerative potential [13].
The standardization of culture conditions is critical for reproducibility. For high-throughput applications, 96-well platforms like Elplasia and BIOFLOAT generate spheroids with consistent circularity and size distribution [13]. Low-throughput six-well ULA plates produce heterogeneous populations that better reflect biological diversity but require more careful characterization [13]. Researchers must optimize cell seeding density specific to their cell type and platform, as this parameter directly determines final spheroid size and quality.
Analytical and Imaging Challenges
The 3D architecture of spheroids presents distinct challenges for analysis and imaging. Nutrient and oxygen gradients along with diffusion kinetics become significant factors as spheroid size increases, potentially creating microenvironments that differ from in vivo conditions [12]. Most traditional imaging systems and analysis protocols were designed for 2D cultures and may not adequately capture 3D complexity [12].
Advanced solutions include confocal microscopy for deep tissue imaging, high-content screening systems with 3D analysis capabilities, and computational methods for quantifying spatial heterogeneity. The development of standardized analytical pipelines remains an active area of innovation, essential for improving reproducibility and cross-study comparisons.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Spheroid Generation and Analysis
| Reagent/Equipment | Function | Application Context |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Minimize cell-surface adhesion to promote cell-cell aggregation | Scaffold-free spheroid formation; available in 6-well (for heterogeneity) and 96-well (for uniformity) formats [13] [12] |
| Matrigel | Natural basement membrane matrix providing ECM components and growth factors | Scaffold-based spheroid culture; supports stemness and outgrowth in regenerative studies [14] [13] |
| ROCK1 Inhibitor (Y-27632) | Inhibits Rho-associated kinase, reduces apoptosis, enhances stem cell survival | Improves formation and stemness preservation in scaffold-free epithelial spheroids [14] [13] |
| Elplasia 96-Well Microcavity Plates | Microcavity design guides single spheroid formation per well | High-throughput, uniform spheroid production for drug screening [13] |
| BIOFLOAT 96-Well U-Bottom Plates | Polymer-coated surface prevents cell attachment | Consistent scaffold-free spheroid formation with controlled size [13] |
| Synthetic Hydrogels (PEG-based) | Tunable synthetic polymers for customizable 3D microenvironments | Scaffold-based culture with controlled mechanical and biochemical properties [12] |
| Microfluidic Platforms | Perfused systems with microchannels for dynamic culture | "Organ-on-a-chip" applications; long-term spheroid culture with physiological flow [12] |
Visualizing Spheroid Methodology and Architecture
The following diagrams illustrate key concepts in spheroid biology and methodology, created using Graphviz with adherence to the specified color and formatting guidelines.
Figure 1: Cellular Zonation in Mature Spheroids
Figure 2: Methodological Workflow for Spheroid Generation
The strategic selection between scaffold-based and scaffold-free spheroid models must align with specific research objectives and practical constraints. Scaffold-free systems offer advantages in reproducibility, scalability, and ease of use for high-throughput applications like drug screening and personalized medicine. Conversely, scaffold-based approaches provide enhanced physiological context through engineered microenvironments, making them valuable for mechanistic studies and regenerative applications where cell-ECM interactions are paramount.
Future developments in spheroid technology will likely focus on standardization, automation, and enhanced physiological relevance. The integration of artificial intelligence for image analysis and data interpretation, advancements in bioprinting for precise spheroid positioning, and the development of more physiologically relevant synthetic matrices will address current limitations [19] [15]. Furthermore, the creation of multi-tissue systems through spheroid fusion and the incorporation of vascular networks represent critical steps toward engineering complex functional tissues [15]. As these technologies mature, spheroid models will increasingly bridge the gap between in vitro studies and clinical applications, accelerating drug development and advancing regenerative medicine.
Three-dimensional (3D) spheroid models have emerged as a transformative tool in experimental oncology and drug discovery, bridging the critical gap between traditional two-dimensional (2D) cell cultures and in vivo tumor biology. These scaffold-free cellular aggregates better replicate the complex in vivo cellular microenvironments of human tissues by promoting intricate cell-cell and cell-extracellular matrix (ECM) interactions that more accurately mimic pathological and physiological conditions [6]. The architecture of spheroids recapitulates essential tumor characteristics, including nutrient gradients, hypoxic cores, and heterogeneous cell populations, creating a more physiologically relevant system for evaluating therapeutic efficacy [20].
Within the context of scaffold-based techniques research, spheroids represent a sophisticated approach to modeling the 3D spatial organization of tumors without relying on exogenous scaffold materials. This technical guide examines the key advantages of spheroid models through the lens of three critical phenomena: drug penetration, resistance mechanisms, and cellular heterogeneity. By understanding and leveraging these aspects, researchers can design more predictive preclinical studies that ultimately enhance the translation of therapeutic candidates from bench to bedside, particularly in the field of personalized cancer medicine [18].
Key Advantage 1: Drug Penetration
The penetration of therapeutic compounds into solid tumors represents a fundamental challenge in oncology drug development. Spheroid models excel in quantifying this parameter by recreating the physical barriers and transport limitations characteristic of human tumors. Unlike monolayer cultures where cells are uniformly exposed to dissolved compounds, spheroids develop concentric zones with varying microenvironments that significantly influence drug distribution and efficacy.
Physiological Barriers to Drug Delivery
The multicellular architecture of spheroids generates diffusional limitations that closely mimic those observed in avascular tumor nodules or micrometastases. Therapeutic agents must traverse multiple cellular layers to reach the spheroid core, encountering progressively changing conditions including:
- Reduced oxygen tension and nutrient availability in central regions
- Accumulation of metabolic waste products such as lactic acid
- Altered pH gradients that can impact drug stability and activity
- Increased cell density and extracellular matrix deposition creating physical barriers to diffusion
These parameters collectively influence the pharmacokinetic profile of tested compounds in ways that cannot be captured in 2D culture systems [20]. The spatial heterogeneity of drug exposure within spheroids provides crucial information about a compound's ability to reach all target cells at effective concentrations.
Experimental Assessment Methodologies
Several established protocols enable quantitative analysis of drug penetration in spheroid models. The standardized spheroid-based drug screening protocol involves initiating spheroids, treating them with serial dilutions of therapeutic compounds, and determining analytical endpoints including spheroid integrity and cell survival [20]. Key methodological considerations include:
- Spheroid Size Standardization: Maintaining consistent spheroid diameter (typically 200-500 μm) is critical for reproducible diffusion kinetics
- Treatment Duration: Exposure times must be sufficient to allow compound penetration to the core
- Analysis Techniques: Sectioning and staining of spheroids following treatment enables visualization of spatial distribution
- Viability Assessment: Multiparametric assays measuring both overall and zone-specific cell death
For penetration studies, fluorescently tagged compounds or combination with fluorescent viability dyes allow direct visualization of distribution patterns using confocal microscopy. The acquisition of z-stack images through the entire spheroid diameter enables 3D reconstruction of penetration profiles [21].
Table 1: Experimental Approaches for Assessing Drug Penetration in Spheroid Models
| Method | Key Readouts | Technical Considerations | Compatible Assays |
|---|---|---|---|
| Confocal Microscopy with Fluorescent Tags | Spatial distribution, Penetration depth, Gradient formation | Requires fluorescent compounds or dyes; Tissue clearing may enhance resolution [21] | Live/dead staining, Compound autofluorescence |
| Sectioning and Staining | Zone-specific effects, Cellular response heterogeneity | Destructive method; Enables high-resolution histology | Immunofluorescence, H&E, TUNEL apoptosis assay |
| Multiparametric Viability Assays | Global vs. core-specific toxicity | Penetration of assay reagents must be considered | Acid phosphatase, AlamarBlue, PrestoBlue [21] |
| Mass Spectrometry Imaging | Absolute compound quantification, Metabolite distribution | Technically challenging; Provides untargeted spatial metabolomics | Matrix-assisted laser desorption/ionization (MALDI) |
Key Advantage 2: Resistance Mechanisms
Spheroid models provide unique insights into the complex mechanisms underlying drug resistance, which remains a primary challenge in clinical oncology. The 3D architecture and heterogeneous microenvironment of spheroids promote the emergence of multicellular resistance phenotypes that more accurately reflect treatment failure in patients than conventional 2D models.
Molecular Drivers of Resistance
Research using integrated single-cell and 3D spheroid platforms has elucidated key molecular pathways contributing to therapy resistance. In lung cancer models, cisplatin-resistant subclones demonstrated elevated expression of drug efflux transporters including ABCB1 (MDR-1) and ABCG2, enhancing their capacity to expel chemotherapeutic agents [22] [23]. Additionally, resistant subclones showed upregulation of cancer stem cell (CSC) markers (OCT4, SOX2, CD44, CD133) and activation of epithelial-mesenchymal transition (EMT) programs, characterized by E-cadherin downregulation and increased Vimentin, N-cadherin, and Twist expression [22].
These molecular adaptations correlate with functional phenotypes including enhanced migratory capacity and invasive potential, mirroring the aggressive behavior observed in treatment-resistant tumors. The spheroid model maintains these resistance mechanisms during in vitro culture, enabling sustained investigation of resistant cell populations [23].
Experimental Evidence from 3D Models
Comparative drug sensitivity assessments between 2D and 3D culture systems consistently demonstrate enhanced resistance phenotypes in spheroids. In lung cancer studies, chemotherapeutic agents including Docetaxel and Alimta displayed significantly higher IC₅₀ values in 3D spheroids compared to 2D cultures, suggesting that 3D models better reflect clinical dosing requirements [22] [23]. Similarly, targeted therapies such as Giotrif (afatinib) and Capmatinib exhibited subclone-specific efficacy patterns in MPE-derived spheroids, with Holoclone populations showing particular resistance profiles [23].
This resistance profile is mediated through both cell-autonomous mechanisms (e.g., efflux pump expression, CSC properties) and non-cell-autonomous factors (e.g., limited drug penetration, hypoxic core, cell-cell signaling). The convergence of these mechanisms in spheroids creates a pathophysiologically relevant system for investigating resistance and developing strategies to overcome it.
Table 2: Experimentally Demonstrated Resistance Mechanisms in Spheroid Models
| Resistance Mechanism | Key Molecular Markers | Functional Consequences | Therapeutic Implications |
|---|---|---|---|
| Drug Efflux Transport | ABCB1 (MDR-1), ABCG2 upregulated [22] | Reduced intracellular drug accumulation | Combination therapy with efflux inhibitors |
| Cancer Stem Cell Enrichment | OCT4, SOX2, CD44, CD133 elevated [22] | Enhanced self-renewal, Tumor initiation capacity | CSC-targeted agents, Differentiation therapy |
| EMT Activation | E-cadherin ↓, Vimentin ↑, N-cadherin ↑, Twist ↑ [22] | Increased invasion, metastasis, and survival | EMT pathway inhibitors, Microenvironment modulation |
| Phenotypic Plasticity | Dynamic marker expression, Non-genetic adaptation [23] | Reversible resistance states, Tumor heterogeneity | Epigenetic modifiers, Intermittent dosing strategies |
Key Advantage 3: Cellular Heterogeneity
Intratumoral heterogeneity represents a defining feature of human malignancies and a significant obstacle to effective treatment. Spheroid models uniquely capture this complexity by supporting the coexistence of multiple cellular subpopulations with distinct phenotypic and functional characteristics within a single integrated system.
Modeling Subclonal Diversity
The integration of single-cell isolation techniques with 3D spheroid culture enables precise dissection of subclonal heterogeneity and its functional consequences. In lung cancer models, researchers have isolated and characterized distinct resistant subclones—Holoclone, Meroclone, and Paraclone—derived from a common A549 parental line following cisplatin selection [23]. These subclones demonstrate stable differences in:
- Morphological appearance and growth patterns
- Gene expression profiles including resistance markers
- Drug sensitivity spectra to conventional and targeted agents
- Differentiation capacity and stem-like properties
This subclonal diversity mirrors the heterogeneity observed in patient tumors, where minor resistant populations can ultimately drive disease progression and treatment failure. Spheroid models maintain these subpopulations in physiologically relevant proportions and spatial arrangements, enabling investigation of clonal dynamics under therapeutic pressure [22].
Technical Approaches to Heterogeneity Analysis
Several methodological innovations facilitate the study of cellular heterogeneity in spheroid models:
- Single-Cell Cloning and Expansion: Microchip-based isolation enables derivation of pure subclones from heterogeneous populations [23]
- Long-Term 3D Culture: Maintenance of subclones as spheroids preserves their phenotypic characteristics during experimental manipulation
- High-Content Imaging: Multiparametric analysis of spheroid structure and composition at single-cell resolution
- Molecular Profiling: Transcriptomic and proteomic characterization of distinct spheroid regions or isolated subclones
These approaches collectively enable researchers to deconstruct the cellular complexity of spheroids and attribute specific functional capabilities to defined subpopulations. This resolution is essential for understanding how minor cell populations can dictate therapeutic outcomes.
Technical Guide: Experimental Protocols
Standardized Spheroid Formation Protocol
Consistent generation of uniform spheroids is foundational to reproducible experimental outcomes. The following protocol outlines a reliable approach for spheroid formation using low-attachment surfaces:
Cell Preparation: Harvest cells using standard trypsinization procedures and prepare a single-cell suspension in complete growth medium. Determine cell concentration using a hemocytometer or automated cell counter.
Seeding Optimization: For initial experiments, test a range of seeding densities (500-10,000 cells/well) to identify optimal conditions for your cell type. Centrifuge the plate at low speed (150 × g for 5 minutes) to promote cell aggregation [21].
Spheroid Formation: Culture cells in round-bottom, low-attachment 96-well plates to promote spontaneous aggregation. The hydrophilic polymer-coated surface of plates such as Nunclon Sphera inhibits cell attachment, forcing cells to aggregate into a single spheroid per well [21].
Culture Maintenance: For long-term cultures (≥7 days), perform half-media changes every 2-3 days by carefully tilting the plate and aspirating half the supernatant without disturbing the settled spheroids. Add fresh pre-warmed media gently along the well wall [21].
Quality Control: Monitor spheroid formation daily using brightfield microscopy. Most cell types form compact spheroids within 24-72 hours, though some may require longer periods. Exclude wells with multiple aggregates or irregular morphology from analysis.
Drug Sensitivity Assessment in 3D Models
Evaluation of compound efficacy in spheroids requires specific methodological adaptations to account for their 3D architecture:
Spheroid Maturation: Allow spheroids to form for 3-5 days prior to drug treatment, ensuring establishment of relevant microenvironmental gradients.
Drug Preparation: Prepare serial dilutions of test compounds in culture medium at 2× final concentration. Include appropriate vehicle controls.
Treatment Application: Carefully remove 50% of existing medium from each well and replace with an equal volume of 2× drug solution to achieve desired final concentration.
Exposure Duration: Typical treatment periods range from 72-144 hours, depending on compound mechanism and experimental objectives.
Viability Assessment:
- For metabolic assays (e.g., PrestoBlue, AlamarBlue), increase incubation times 2-4 fold compared to 2D protocols to allow sufficient reagent penetration [21]
- For imaging-based viability assessment, use fluorescent probes (e.g., Calcein-AM for live cells, ethidium homodimer for dead cells) with extended incubation periods
- Consider tissue clearing reagents (e.g., CytoVista) to enhance imaging depth and resolution for larger spheroids [21]
Data Analysis: Normalize treatment groups to vehicle controls and calculate IC₅₀ values using nonlinear regression models. Compare 3D results to parallel 2D experiments to identify compound-specific differences in efficacy.
Research Reagent Solutions
Successful implementation of spheroid-based research requires specialized reagents and materials optimized for 3D culture applications. The following toolkit outlines essential components for spheroid formation, maintenance, and analysis:
Table 3: Essential Research Reagents for Spheroid Models
| Reagent Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Low-Attachment Plates | Nunclon Sphera 96-well U-bottom plates [21] | Promote spontaneous spheroid formation via inhibition of cell attachment | Round-bottom geometry encourages single spheroid formation per well |
| Extracellular Matrix | Cultrex Basement Membrane Extract, Matrigel | Scaffold-based spheroid formation, Invasion assays | Lot-to-lot variability; Potential biological activity [21] |
| Viability Assays | PrestoBlue HS, AlamarBlue HS, Acid Phosphatase Assay [20] | Metabolic activity measurement in 3D structures | Require extended incubation times for penetration [21] |
| Cell Staining Reagents | CellEvent Caspase 3/7, MitoTracker Orange [21] | Apoptosis detection, Organelle-specific staining | Concentration often requires optimization for 3D (e.g., 2X for MitoTracker) [21] |
| Tissue Clearing Kits | Invitrogen CytoVista 3D Cell Culture Clearing/Staining Kit [21] | Enhance antibody and dye penetration for imaging | Enables high-resolution imaging to depths up to 1000 μm |
| Specialized Pipette Tips | Finntip wide orifice tips [21] | Spheroid transfer without structural damage | Essential for maintaining spheroid integrity during manipulation |
Signaling Pathways and Workflow Visualization
Drug Resistance Mechanisms in Spheroid Models
Diagram 1: Resistance Mechanisms in Spheroids
Integrated Single-Cell to Spheroid Workflow
Diagram 2: Single-Cell to Spheroid Workflow
Spheroid models represent a sophisticated experimental platform that recapitulates critical aspects of in vivo tumor biology, particularly in the domains of drug penetration, resistance mechanisms, and cellular heterogeneity. By incorporating these 3D systems into preclinical drug development pipelines, researchers can obtain more clinically predictive data regarding compound efficacy and identify resistance mechanisms early in the development process. The technical protocols and reagent solutions outlined in this guide provide a foundation for implementing spheroid models in diverse research settings, with particular relevance for personalized medicine approaches using patient-derived materials. As standardization and accessibility of 3D culture technologies continue to improve, spheroid models are poised to play an increasingly central role in bridging the gap between traditional in vitro assays and clinical outcomes.
Building Better Models: Techniques and Applications of Scaffold-Based Spheroids
In the field of three-dimensional (3D) cell culture, scaffold-based techniques are fundamental for advancing spheroid models that better recapitulate the in vivo microenvironment. These scaffolds, whether derived from natural sources or synthetically engineered, provide the essential 3D architecture that supports cell-cell and cell-extracellular matrix (ECM) interactions, which are crucial for maintaining cellular phenotypes and functions not possible in traditional two-dimensional (2D) cultures [24] [6]. The selection between natural polymers like Matrigel and collagen and synthetic polymers such as PLGA (poly(lactic-co-glycolic acid)) and PEG (poly(ethylene glycol)) represents a critical strategic decision in research design. This choice directly influences the biological relevance, reproducibility, mechanical stability, and experimental outcomes of spheroid studies [24] [25]. This guide provides an in-depth technical comparison of these material classes, equipping researchers with the data and methodologies needed to make informed decisions for their specific applications in cardiovascular biology, cancer research, and drug development.
Material Properties and Comparative Analysis
Natural Polymers: Matrigel and Collagen
- Matrigel: This is a basement membrane matrix extract derived from Engelbreth-Holm-Swarm (EHS) mouse sarcoma. It is a complex, biologically active mixture containing type IV collagen, laminin, entactin, and sulfated proteoglycans, along with various growth factors [26]. Its primary advantage is its high bioactivity, which promotes excellent cell adhesion, proliferation, and differentiation. However, its animal-derived origin, batch-to-batch variability, and complex composition can be significant drawbacks for standardized studies [26] [13].
- Collagen: The most abundant protein in the human ECM, type I collagen is widely used for scaffold fabrication. It is biocompatible, biodegradable, and possesses cell-binding motifs (e.g., RGD sequences) that facilitate cell attachment [26] [27]. A key limitation is its poor mechanical behavior, leading to significant compaction under cellular forces, which can be mitigated by forming composites with other materials [26].
Synthetic Polymers: PLGA and PEG
- PLGA: A copolymer of lactic acid and glycolic acid, PLGA is a cornerstone of synthetic scaffold materials. Its key advantages include precise control over degradation rate (by adjusting the lactide:glycolide ratio), proven biocompatibility, and tunable mechanical properties [28] [27]. As a polyester, it degrades by hydrolysis into metabolites that enter the body's natural metabolic pathways [27]. Its potential drawbacks include hydrophobic surfaces that may require modification for optimal cell attachment and the possibility of eliciting acidic inflammatory responses during degradation [24] [27].
- PEG: Known for its high hydrophilicity and bio-inertness, PEG is often used to create hydrogels or as a block in copolymers (e.g., PLA-PEG). Its "blank slate" nature is a double-edged sword; it resists non-specific protein adsorption and cell attachment, which allows researchers to precisely engineer cell-material interactions by incorporating specific bioactive peptides. However, it lacks inherent bioactivity [28] [29].
Quantitative Material Comparison
The following tables summarize the key properties and parameters of these scaffold materials to facilitate direct comparison.
Table 1: Qualitative Comparison of Scaffold Material Properties
| Property | Matrigel | Collagen (Type I) | PLGA | PEG |
|---|---|---|---|---|
| Origin | Natural (Murine) | Natural (Mammalian) | Synthetic | Synthetic |
| Bioactivity | High (Contains growth factors) | High (RGD motifs) | Low / Modifiable | Very Low / Engineerable |
| Mechanical Strength | Low (Soft hydrogel) | Low, prone to compaction [26] | High & Tunable [27] | Tunable |
| Degradation Rate | Enzymatic, Variable | Enzymatic, Relatively Fast | Hydrolytic, Tunable (weeks-months) [27] | Hydrolytic, Tunable |
| Batch-to-Batch Variation | High [13] | Moderate | Very Low | Very Low |
| Immunogenicity Risk | Moderate (Xenogeneic) | Low (if purified) | Low (can cause mild inflammation) [24] | Very Low |
| Key Advantage | Physiologically rich microenvironment | Excellent innate cellular recognition | Controllable properties & degradation | Precision and control over biofunctionalization |
Table 2: Quantitative Parameters for Scaffold Fabrication and Performance
| Parameter | Matrigel-Collagen Composite [26] | PLGA / PLA-PEG [28] | Ideal Scaffold Range (General) [25] |
|---|---|---|---|
| Typical Polymer Conc. | 3-10 mg/mL (Collagen) | 10-20% (w/v) for electrospinning | Varies by method and material |
| Pore Size | Porous structure observed [26] | Nano-fibrous (via electrospinning) [28] | 150 - 500 μm (for cell infiltration & vascularization) [25] |
| Degradation Time | Not specified | Sustained release over 20 days [28] | Proportional to tissue formation rate [25] |
| Mechanical Properties (Tensile/Compressive) | Enhanced vs. collagen alone [26] | Tensile Modulus: ~35 MPa [28] | Matches target tissue (Bone: 1-20 GPa; Cardiac: 30-400 kPa) [25] |
| Water Absorption | Tunable swelling behavior [26] | Varies with PEG content | High porosity (>90%) for nutrient diffusion [25] |
Experimental Protocols for Spheroid Research
Protocol 1: Forming a Matrigel-Collagen Semi-IPN Scaffold for Dynamic Cell Culture
This protocol is adapted from studies on valve interstitial cells and demonstrates the formation of a composite hydrogel to improve the mechanical properties of collagen alone [26].
- Preparation of Stock Solutions: Prepare a sterile solution of Type I collagen (e.g., from rat tail tendon) in a weak acetic acid solution (e.g., 0.1% v/v). Thaw Matrigel on ice overnight.
- Neutralization of Collagen: Mix the cold collagen solution with the appropriate volume of neutralization buffer (e.g., 10X PBS) and sodium hydroxide (NaOH) to achieve a physiological pH of 7.4. Keep everything on ice to prevent premature gelling.
- Forming the Composite Hydrogel: Rapidly mix the neutralized collagen solution with the thawed Matrigel at the desired volume ratio (e.g., 1:1 Matrigel:Collagen). Gently pipette to mix without introducing air bubbles.
- Polymerization: Transfer the mixture to the desired culture vessel (e.g., multi-well plate) and incubate at 37°C for 30-60 minutes to allow a solid hydrogel to form.
- Cell Seeding and Culture: Seed the cell suspension directly on top of the pre-formed gel for a 3D overlay culture, or mix the cells with the composite solution before polymerization for 3D embedding. Add complete culture medium after the gel has set.
- Dynamic Mechanical Stimulation: Place the cultured scaffolds in a bioreactor system capable of applying cyclic mechanical strain (e.g., cyclic stretching) that mimics in vivo conditions, such as those found in cardiovascular tissues [26].
Protocol 2: Incorporating Spheroids into a Matrigel Scaffold for Invasion/Outgrowth
This protocol, derived from skin regenerative research, is used to study spheroid behavior and stem cell potential in a matrix-rich environment [13].
- Spheroid Generation: Generate epithelial spheroids using a scaffold-free method, such as culture in ultra-low attachment (ULA) 6-well plates. This produces a heterogeneous population of spheroids (holospheres, merospheres, paraspheres) [13].
- Matrigel Bed Preparation: Thaw Matrigel on ice. Carefully coat the wells of a pre-chilled culture plate with a thin layer of pure Matrigel and incubate at 37°C for 30 min to solidify.
- Spheroid Embedding: Resuspend the harvested spheroids in a small volume of cold Matrigel solution. Gently pipette this spheroid-Matrigel suspension on top of the pre-formed gel bed.
- Polymerization and Culture: Incubate the plate at 37°C for another 30 min to solidify the embedding layer. Once set, carefully overlay with complete culture medium.
- Analysis: Monitor spheroid behavior over time. Merospheres and paraspheres are expected to migrate outward, forming epithelial sheets, while holospheres may remain intact as stem cell reservoirs. Analyze using immunofluorescence for stemness markers (e.g., BMI-1) and imaging for migratory outgrowth [13].
Protocol 3: Fabricating a PLGA-PEG Nanostructured Scaffold for Gene Delivery
This protocol outlines the creation of a composite scaffold for sustained molecular release, such as DNA or growth factors, using electrospinning [28].
- Polymer Solution Preparation: Dissolve PLGA and a PLA-PEG block copolymer in a volatile organic solvent (e.g., hexafluoro-2-propanol, tetrahydrofuran) at a total polymer concentration of 10-20% (w/v). The ratio of PLGA to PLA-PEG can be varied (e.g., 85:15) to adjust fiber morphology and release kinetics.
- Functionalization: Add the bioactive agent (e.g., plasmid DNA) to the polymer solution and mix thoroughly to ensure a homogeneous distribution.
- Electrospinning Setup: Load the solution into a syringe with a metallic needle. Connect the syringe to a high-voltage power supply. Use a grounded collector drum or plate covered with aluminum foil to collect the fibers.
- Fabrication Process: Apply a high voltage (e.g., 15-25 kV) to the needle tip. Precisely control the flow rate of the polymer solution (e.g., 1.0 mL/h) using a syringe pump. The electrostatic forces will draw a jet of the solution towards the collector, forming solid, nano-fibrous scaffolds as the solvent evaporates.
- Post-Processing: Dry the fabricated scaffold under vacuum for 24-48 hours to remove any residual solvent.
- Release Study and Cell Culture: Sterilize the scaffold via UV irradiation. For release studies, incubate the scaffold in PBS at 37°C and collect supernatant at predetermined time points for analysis. For cell studies, seed cells directly onto the scaffold and assess transfection efficiency (if delivering DNA) and cell viability [28].
Visualizing the Scaffold Selection Workflow
The following diagram illustrates the strategic decision-making process for selecting between natural and synthetic polymers for spheroid research, based on the core experimental objectives.
The Scientist's Toolkit: Essential Research Reagents
This table lists key materials and their functions for implementing the protocols discussed in this guide.
Table 3: Essential Reagents for Scaffold-Based Spheroid Research
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Type I Collagen (e.g., Rat Tail) | Forms the primary 3D hydrogel matrix for cell culture; provides biological cues for cell adhesion and proliferation. | Natural polymer, contains RGD sequences, thermo-reversible gelation at 37°C [26]. |
| Matrigel / Basement Membrane Extract | Creates a biologically active, complex hydrogel environment; used for stem cell culture, organoid formation, and invasion assays. | Rich in ECM proteins and growth factors; promotes complex tissue-specific morphogenesis [26] [13]. |
| PLGA (Poly(lactic-co-glycolic acid)) | Synthetic polymer for fabricating durable, biodegradable scaffolds (fibrous meshes, porous foams) with controlled release properties. | Ester-linkage hydrolysis degradation; degradation rate tunable by LA:GA ratio [28] [27]. |
| PLA-PEG Block Copolymer | Used to create hydrogels or composite scaffolds; PEG enhances hydrophilicity, modulates release kinetics, and reduces protein fouling. | Amphiphilic nature; can be engineered for thermosensitive gelation (sol-gel transition) [28] [29]. |
| Ultra-Low Attachment (ULA) Plates | Generate scaffold-free spheroids for subsequent embedding in scaffolds or for comparative studies. | Covalently bonded hydrogel surface minimizes cell attachment, forcing cell aggregation into spheroids [13]. |
| ROCK Inhibitor (Y-27632) | Enhances cell survival and stemness in spheroid cultures, particularly during the initial phases of aggregation and after dissociation. | Inhibits Rho-associated kinase; reduces anoikis (detachment-induced apoptosis) [13]. |
The strategic selection of scaffold materials is a cornerstone of robust and physiologically relevant spheroid model development. Natural polymers like Matrigel and collagen offer unparalleled bioactivity and are the materials of choice for investigations demanding high biological fidelity, such as modeling complex stem cell niches or tissue-specific morphogenesis. In contrast, synthetic polymers such as PLGA and PEG provide unmatched control, reproducibility, and tunability, making them ideal for high-throughput drug screening, mechanistic studies, and applications requiring precise control over the physical and chemical environment. The emerging trend of creating composite or hybrid scaffolds (e.g., Matrigel-Collagen, PLGA-PEG) represents a powerful approach to harness the advantages of both material classes, enabling researchers to design a tailored 3D microenvironment that addresses the specific requirements of their spheroid-based research [24] [26] [28].
This technical guide provides an in-depth analysis of three core fabrication techniques advancing spheroid models in scaffold-based research: hydrogel embedding, 3D bioprinting, and co-culture systems. These methodologies bridge the critical gap between conventional two-dimensional cell cultures and in vivo models, enabling researchers to create more physiologically relevant tumor microenvironments for drug discovery and personalized medicine. By offering detailed protocols, material specifications, and experimental workflows, this whitepaper serves as a comprehensive resource for scientists and drug development professionals seeking to implement these technologies in preclinical cancer research. The integration of these approaches allows for superior recapitulation of tumor heterogeneity, cell-cell interactions, and metabolic gradients that mirror clinical pathophysiology.
The transition from traditional 2D cell cultures to three-dimensional models represents a paradigm shift in cancer research and drug development. While 2D cultures have contributed significantly to basic research, their oversimplified architecture fails to recapitulate the complex tumor microenvironment (TME), leading to poor predictive accuracy for drug efficacy and toxicity [30]. Spheroids—three-dimensional cell aggregates that mimic tissues and microtumors—have emerged as essential tools that more accurately simulate in vivo conditions by replicating critical features such as surface-exposed and deeply buried cells, proliferating and non-proliferating populations, and hypoxic centers with well-oxygenated outer layers [31]. The development of scaffold-based techniques, particularly those utilizing hydrogels, has further enhanced our ability to control the biochemical and mechanical properties of the 3D environment, enabling precise manipulation of experimental conditions for basic and translational research [30] [32].
Within the context of spheroid models, several distinct approaches have been developed, each with specific advantages and applications. Multicellular tumor spheroids (MCTS) are often generated from cancer cell lines and mimic metabolic and proliferation gradients of in vivo tumors, modeling clinically relevant resistance to chemotherapy [30]. Tumor-derived spheroids are prepared from dissociated tumor tissue and cultured in serum-free media containing growth factors that promote the expansion of cells with stem-like properties [30]. Organoids represent a more complex 3D culture system that demonstrates self-organization and self-assembly capabilities, forming structures that partially reflect the original organ in both architecture and function [30]. The table below compares key characteristics of these models against traditional approaches.
Table 1: Comparison of Preclinical Cancer Models
| Model | Advantages | Disadvantages | Best Applications |
|---|---|---|---|
| 2D Cell Culture | Reproducible, rapid growth; Low-cost and simple; High-throughput drug screening [30] | Oversimplified cancer model; Lacks tumor heterogeneity and TME; Low establishment success for some tumors [30] | Initial drug screening; Basic mechanism studies |
| Patient-Derived Xenografts (PDTX) | Recapitulates human disease including heterogeneity; Ability to study metastasis [30] | Requires immune-deficient hosts; Low implantation rates; Costly and time-consuming [30] | Validation studies; Preclinical efficacy testing |
| Spheroids | Bridges gap between 2D and in vivo; Retains tumor heterogeneity; More accurate drug responses [30] [31] | Limited TME reconstitution in some models; Standardized analysis methods still developing [30] | Drug penetration studies; Metabolic gradient research; Mid-throughput screening |
| Organoids | Recapitulates tumors histologically/genetically; Long-term culture possible; Amenable to genetic manipulation [30] | Relatively costly; Unified production methods limited; Complex TME not fully reconstituted [30] | Personalized medicine; Biobanking; Disease modeling |
Hydrogel Embedding for Spheroid Formation
Hydrogel Properties and Selection Criteria
Hydrogels are three-dimensional networks of hydrophilic polymer chains that absorb substantial amounts of water while maintaining structural integrity, making them ideal for mimicking the native extracellular matrix (ECM) [33] [32]. Their biocompatibility, tissue-like mechanical properties, and porosity facilitate nutrient diffusion and waste removal—critical factors for supporting 3D spheroid development and growth [33]. The selection of an appropriate hydrogel is paramount for experimental success and depends on multiple physicochemical and biological parameters.
Natural polymer hydrogels, such as alginate, collagen, and gelatin, typically offer superior bioactivity and cell recognition sites but may suffer from batch-to-batch variability and limited mechanical strength. Synthetic hydrogels, including polyethylene glycol (PEG) and Pluronic, provide excellent control over mechanical properties and high reproducibility but often lack inherent biological cues [33] [32]. Key properties to consider include mechanical stiffness (which influences cell differentiation and proliferation), degradation kinetics (should match tissue formation rates), porosity (affects nutrient diffusion and cell migration), and ligand density (impacts cell adhesion and signaling) [33].
Table 2: Characteristics of Common Hydrogels for Spheroid Research
| Hydrogel Material | Type | Cross-linking Method | Advantages | Disadvantages |
|---|---|---|---|---|
| Alginate | Natural | Ionic (e.g., CaCl₂) [33] | Rapid crosslinking; High cell viability post-print; Inexpensive [33] | Poor mechanical strength; Low cell recognition/adhesion; Complex biodegradability [33] |
| Collagen | Natural | Enzymatic (MMP) [33] | Highly biocompatible; Represents major ECM component; Easily degraded [33] | Poor mechanical properties; Poor cross-linking kinetics [33] |
| Gelatin Methacrylate (GelMA) | Natural-derived | Photo-crosslinking [34] | Excellent biocompatibility; Contains RGD motifs for cell adhesion; Tunable mechanical properties [34] | Requires modification for optimal gelation; Limited mechanical strength alone [34] |
| Fibrin | Natural | Enzymatic (plasmin) [33] | Encourages cellular growth; Crosslinking emulates natural clotting [33] | Liquifies at high temperatures [33] |
| Polyethylene Glycol (PEG) | Synthetic | Photo-crosslinking [33] | Easily modified chemically; Hydrophilic; Consistent properties [33] | Lacks biological cues; Photocrosslinking may affect viability; Doesn't naturally biodegrade [33] |
| Hyaluronic Acid | Natural | Enzymatic (hyaluronidase) [33] | Highly biocompatible; Native component of ECM [33] | Requires modification for gelation control [33] |
Experimental Protocol: Sodium Alginate-Gelatin Hydrogel Embedding
The following protocol has been optimized for establishing non-small cell lung cancer (NSCLC) patient-derived xenograft (PDX) cells and cancer-associated fibroblast (CAF) co-culture spheroids, but can be adapted for other cell types with appropriate modifications [35].
Materials and Reagents
- Sodium alginate (3.25%-4.0% w/v)
- Gelatin (4% w/v)
- Calcium chloride (CaCl₂) crosslinking solution (100 mM)
- Cell culture medium appropriate for your cell type
- Low-attachment multi-well plates or appropriate culture vessels
Hydrogel Preparation and Characterization
- Hydrogel Formulation: Prepare sodium alginate-gelatin (SA-GL) hydrogels by dissolving 3.25-4.0% (w/v) sodium alginate and 4% (w/v) gelatin in distilled water or culture medium. Sterilize using 0.22µm filtration.
- Rheological Characterization: Evaluate viscosity using a rheometer. Optimal formulations demonstrate shear-thinning behavior where viscosity significantly decreases with increasing shear rate, facilitating smooth extrusion during printing or pipetting [35].
- Viscoelasticity Assessment: Measure storage modulus (G') and loss modulus (G") through oscillatory frequency sweep tests. Optimal SA-GL hydrogels (3.25% SA, 4% GL) typically show G' values of approximately 104.42 Pa and G" values of 16.25 Pa at 0.1 Hz, with both moduli increasing with frequency and G' consistently higher than G", indicating solid-like behavior essential for structural stability [35].
Cell Encapsulation and Culture
- Cell Preparation: Harvest and count cells. For co-culture models, prepare cell suspensions at desired ratios (e.g., NSCLC PDX cells to CAFs at 1:1 ratio).
- Cell-Hydrogel Mixing: Gently mix cell suspension with prepared SA-GL hydrogel to achieve final cell density of 1-5×10⁶ cells/mL. Avoid bubble formation.
- Hydrogel Dispensing: Transfer cell-laden hydrogel to low-attachment plates or molds. For manual dispensing, use wide-bore tips to minimize shear stress.
- Cross-linking: Add CaCl₂ solution (100 mM) to cover hydrogel constructs for 5-10 minutes to induce ionic cross-linking of alginate chains.
- Culture Maintenance: Remove cross-linking solution and replace with appropriate culture medium. Refresh medium every 2-3 days.
- Spheroid Monitoring: Monitor spheroid formation daily using microscopy. Typically, spheroids begin forming within 24-48 hours, with mature spheroids developing over 5-15 days, reaching diameters of 50-1100 µm depending on initial cell density and culture duration [35].
Validation and Analysis
- Viability Assessment: Use live/dead staining (e.g., calcein-AM/ethidium homodimer) to quantify cell viability, which should exceed 85-90% in optimized protocols.
- Spheroid Characterization: Measure spheroid size distribution, circularity, and number using automated image analysis software.
- Functional Validation: For co-culture models, confirm functional interactions through immunostaining for markers such as vimentin, α-SMA (CAF markers), and E-cadherin (epithelial marker) to demonstrate expected phenotypic changes [35].
3D Bioprinting of Spheroid Models
Bioprinting Technologies and Bioink Design
3D bioprinting represents an advanced fabrication technique that enables precise spatial positioning of cells, biomaterials, and biological factors to create complex tissue-like structures [36]. Unlike conventional hydrogel embedding, bioprinting provides superior control over architecture and cellular organization, allowing researchers to model specific tissue geometries and heterogeneous cell distributions. The three primary bioprinting modalities used in spheroid research include microextrusion (continuous filament deposition), inkjet (droplet-based deposition), and laser-assisted printing (laser-induced forward transfer) [33] [36].
Bioink design is arguably the most critical component of successful bioprinting. An ideal bioink must balance multiple, often competing, requirements: printability (extrusion and shape fidelity), structural stability (maintenance of 3D structure), biocompatibility (supporting cell viability and function), and biomimicry (recapitulating tissue-specific properties) [37]. Advanced bioink formulations often combine multiple materials to achieve optimal properties. For example, a blend of 4% alginate, 10% carboxymethyl cellulose (CMC), and 8-16% gelatin methacrylate (GelMA) has demonstrated excellent printability, long-term mechanical stability (up to 21 days), and enhanced cell proliferation [37].
Table 3: Comparison of 3D Bioprinting Techniques for Spheroid Models
| Bioprinting Method | Mechanism | Resolution | Advantages | Limitations | Suitable Bioinks |
|---|---|---|---|---|---|
| Microextrusion | Pneumatic or mechanical dispensing of continuous filaments [36] | 100-1000 µm [36] | High cell density printing; Wide viscosity range; Multiple crosslinking methods [35] [36] | Lower resolution; Potential shear stress on cells [36] | Alginate-gelatin blends [35], GelMA [34], High-viscosity hydrogels |
| Inkjet | Thermal or piezoelectric droplet ejection [36] | 50-300 µm [36] | High printing speed; Parallel workflow possible; Good cell viability [36] | Limited bioink viscosity; Potential nozzle clogging; Droplet uniformity issues [36] | Low-viscosity alginate [33], Collagen, Fibrin |
| Laser-Assisted | Laser-induced forward transfer from ribbon [36] | 10-100 µm [36] | High resolution; No nozzle clogging; Minimal shear stress [36] | Complex setup; Higher cost; Limited material choices [36] | Matrigel [33], Alginate [33], Cell spheroids |
Experimental Protocol: Bioprinting Co-culture Spheroid Models
This protocol outlines the specific methodology for bioprinting NSCLC PDX and CAF co-culture models using SA-GL bioink, with adaptations for other cell types noted [35].
Bioink Preparation and Optimization
- Bioink Formulation: Prepare SA-GL bioink with optimal concentrations (3.25-3.5% SA, 4% GL) in sterile conditions. For other applications, GelMA-based bioinks (8-16% concentration) have demonstrated excellent properties for bone tissue engineering [34].
- Rheological Tuning: Characterize viscosity versus shear rate to confirm shear-thinning behavior. Optimal extrusion typically occurs in the viscosity range of 10-100 Pa·s at applicable shear rates (10-100 s⁻¹) [35].
- Cell Incorporation: Mix concentrated cell suspension with bioink to achieve final density of 5-10×10⁶ cells/mL. Maintain bioink-cell mixture on cooling plate (16-20°C) to prevent premature gelation.
Bioprinting Process Parameters
- Printing Setup: Use a temperature-controlled bioprinting system. Set printing temperature to 18-22°C for SA-GL bioinks [35]. For GelMA-based bioinks, maintain temperature below gelation point during printing.
- Extrusion Parameters: Optimize pressure for specific bioink formulation:
- 3.25% SA + 4% GL: ~35 kPa
- 3.5% SA + 4% GL: ~60 kPa
- Adjust based on nozzle diameter and desired printing speed [35]
- Nozzle Selection: Use nozzles with diameters of 200-400 µm depending on required resolution and cell aggregate size.
- Cross-linking Strategy: Implement immediate cross-linking after deposition using CaCl₂ (50-100 mM) for alginate-containing bioinks or UV light (with appropriate photoinitiators like LAP) for GelMA-based systems [34] [35].
Post-Printing Processing and Culture
- Cross-linking Completion: Immerse printed constructs in cross-linking solution for 5-15 minutes to ensure complete gelation.
- Culture Medium Exchange: Remove cross-linking solution and replace with appropriate culture medium.
- Long-term Maintenance: Culture printed constructs with regular medium changes every 2-3 days. Monitor structural integrity and spheroid formation over time.
- Maturation Period: Allow 7-21 days for spheroid maturation and ECM development, depending on cell type and application.
Quality Control and Validation
- Structural Fidelity: Assess printed construct architecture using microscopy and compare to digital design.
- Cell Viability: Quantify viability at 24 hours post-printing using live/dead assays. Target viability >85% for optimized protocols.
- Spheroid Formation: Monitor spheroid size distribution and morphology over time using brightfield and fluorescence microscopy.
- Functionality Assessment: Evaluate tissue-specific functions through immunostaining, gene expression analysis, or functional assays relevant to your research question.
Co-culture Systems in Spheroid Research
Designing Physiologically Relevant Co-culture Models
Co-culture systems represent a significant advancement in spheroid modeling by incorporating multiple cell types to better mimic the cellular heterogeneity and complex interactions within the tumor microenvironment [35]. These systems enable researchers to study paracrine signaling, cell-cell contacts, and stromal-epithelial interactions that drive tumor progression, drug resistance, and metastasis. The two primary approaches to co-culture include direct co-culture, where different cell types are mixed within the same hydrogel matrix, and indirect co-culture, where cells are separated by physical barriers but share soluble factors [35].
Key considerations for designing co-culture models include:
- Cell Type Selection: Choose stromal components relevant to your cancer type, such as cancer-associated fibroblasts (CAFs) for epithelial tumors [35], or macrophages for modeling immune interactions [34].
- Spatial Arrangement: Decide whether mixed (random) or patterned (organized) distribution better addresses your research question.
- Ratio Optimization: Systematically optimize cell ratios to reflect physiological conditions while maintaining viability and function.
- Medium Composition: Select culture medium that supports all cell types without preferentially expanding one population.
Experimental Protocol: Establishing Direct Co-culture Spheroids
This protocol describes the establishment of direct co-culture spheroids containing NSCLC PDX cells and CAFs, with principles applicable to other cell type combinations [35].
Cell Culture and Preparation
- Cell Source Identification: Obtain appropriate cell types. Patient-derived cells offer highest clinical relevance, while established cell lines provide consistency.
- Monoculture Expansion: Culture each cell type separately under optimal conditions to generate sufficient cell numbers.
- Cell Harvesting: Harvest cells at 70-80% confluence using standard trypsinization or non-enzymatic methods.
- Cell Counting and Ratio Determination: Count cells using hemocytometer or automated counter. Prepare co-culture mixtures at predetermined ratios (e.g., 1:1, 1:2, or 1:4 cancer:stromal cells) based on your experimental design.
Co-culture Spheroid Formation
- Hydrogel Preparation: Prepare appropriate hydrogel (SA-GL or other optimized formulation) as described in Section 2.2.
- Cell-Hydrogel Mixing: Gently mix cell suspensions at desired ratio with hydrogel matrix to achieve final density of 1-5×10⁶ total cells/mL.
- Dispensing and Cross-linking: Transfer cell-hydrogel mixture to low-attachment plates and cross-link following protocol in Section 2.2.
- Culture Maintenance: Refresh medium every 2-3 days, carefully removing and replacing to avoid disrupting developing spheroids.
Validation and Functional Analysis
- Spheroid Characterization: Monitor spheroid formation and growth using brightfield microscopy. Document size distribution and morphology.
- Cell-Type Specific Markers: Use immunocytochemistry to verify presence and distribution of different cell types within spheroids:
- For NSCLC-CAF co-cultures: Stain for E-cadherin (epithelial cells), vimentin, and α-SMA (CAFs) [35]
- Quantify expression changes over time to validate model maturity
- Functional Interactions: Assess functional evidence of cellular crosstalk through:
- Expression changes in EMT markers (loss of E-cadherin, gain of vimentin) [35]
- Altered proliferation rates compared to monocultures
- Differential drug responses relative to monoculture controls
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Spheroid Fabrication Techniques
| Reagent/Material | Function/Application | Example Formulations | Key Considerations |
|---|---|---|---|
| Sodium Alginate | Primary biopolymer for hydrogel formation; ionic cross-linking with calcium [35] | 3.25-4.0% (w/v) in combination with gelatin [35] | Concentration affects viscosity and printability; source affects purity and consistency |
| Gelatin | Provides thermoresponsive properties and improves cell adhesion [35] | 4% (w/v) with sodium alginate [35] | Gelation temperature ~29°C; can be modified (e.g., GelMA) for enhanced properties |
| Gelatin Methacrylate (GelMA) | Photocrosslinkable hydrogel with excellent biocompatibility [34] | 8-16% (w/v) with photoinitiator [37] [34] | Degree of methacrylation affects mechanical properties and cell behavior |
| Calcium Chloride (CaCl₂) | Ionic cross-linking agent for alginate-based hydrogels [35] | 50-100 mM solution for cross-linking [35] | Concentration and exposure time affect gelation degree and cell viability |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Photoinitiator for UV cross-linking of GelMA and other photopolymerizable hydrogels [34] | 0.05-0.5% (w/v) depending on application [34] | Cytocompatibility superior to some other photoinitiators (e.g., Irgacure 2959) |
| Carboxymethyl Cellulose (CMC) | Bioink additive to modify rheological properties and improve printability [37] | 10% (w/v) in alginate-GelMA composites [37] | Enhances shear-thinning behavior and structural fidelity |
| Ultra-Low Attachment Plates | Scaffold-free spheroid formation by preventing cell adhesion [31] | Round-bottom plates for uniform spheroid formation [31] | Surface coating prevents protein adsorption and cell attachment |
| Luteolin-loaded ZIF-8 Nanoparticles | Functional additive for immunomodulation and enhanced osteogenesis [34] | Incorporated in GelMA hydrogels for bone regeneration [34] | Provides sustained release of bioactive compounds; modulates macrophage polarization |
The integration of hydrogel embedding, bioprinting, and co-culture systems represents a powerful toolkit for advancing spheroid models in cancer research and drug development. These scaffold-based techniques enable researchers to create increasingly sophisticated models that bridge the critical gap between conventional 2D cultures and in vivo physiology. As these technologies continue to evolve, several emerging trends are poised to further enhance their capabilities and applications.
Future developments will likely focus on increased complexity through the incorporation of vascular networks, immune components, and neural elements to better simulate the complete tumor microenvironment. Multi-material bioprinting approaches will enable more precise spatial control over biochemical and mechanical cues within the same construct. The integration of sensing capabilities through smart biomaterials that respond to environmental changes or report on cellular activity will provide real-time monitoring of spheroid behavior and drug responses. Additionally, the adoption of standardized characterization methods and analytical pipelines will improve reproducibility and enable more meaningful cross-study comparisons.
As these technologies mature and become more accessible, they have the potential to transform drug discovery pipelines and personalized medicine approaches by providing more predictive preclinical models that better recapitulate patient-specific tumor biology.
In the context of a broader thesis on spheroid models and scaffold-based techniques, the optimization of cell seeding density and matrix concentration emerges as a fundamental prerequisite for generating physiologically relevant three-dimensional (3D) in vitro systems. Scaffold-free three-dimensional (3D) cellular spheroid cultures have demonstrated a superior capacity to replicate the in vivo cellular microenvironments of complex tissues than traditional two-dimensional (2D) cultures, primarily because they promote more intricate cell-cell and cell-extracellular matrix (ECM) interactions [6]. This is particularly critical in cardiovascular biology and pathology, cancer research, and drug development, where the accuracy of the model directly impacts the translational potential of the findings.
The shift from 2D to 3D models is driven by the need for more predictive and human-relevant systems. Within this paradigm, scaffold-based techniques provide a controlled environment for guiding spheroid formation and function. The physical and biochemical properties of the matrix, coupled with the initial number of cells, dictate critical outcome variables such as spheroid size, uniformity, viability, and metabolic activity. Therefore, this protocol deep dive is designed to provide researchers, scientists, and drug development professionals with a detailed framework for systematically optimizing these two key parameters, thereby enhancing the reproducibility and biological significance of their scaffold-based spheroid research.
Theoretical Foundations: Why Seeding Density and Matrix Concentration Matter
The interplay between cell seeding density and matrix concentration governs the self-assembly process of cells into spheroids. Seeding density directly influences the initial cell-cell contact, which is a primary driver of aggregation. Too few cells may result in failed spheroid formation or micro-aggregates, while excessive cell numbers can lead to necrotic cores due to diffusion limitations of nutrients and oxygen [6] [18].
Concurrently, the matrix concentration, often comprising materials like Matrigel, collagen, or synthetic hydrogels, defines the physical microenvironment. It provides mechanical support and biochemical cues that mimic the native extracellular matrix. The concentration of the matrix determines parameters such as stiffness, porosity, and ligand density, which in turn affect:
- Migration and Packing: The ability of cells to migrate towards each other to form a compact spheroid.
- Proliferation and Viability: The diffusion of gases, nutrients, and waste products.
- Differentiation and Function: The activation of mechanotransduction pathways and presentation of integrin-binding sites.
A systematic review of seeding methodologies underscores that forced-floating and scaffold-based methods are among the most reliable and versatile techniques for spheroid generation, highlighting the need for precise optimization of these parameters to ensure success across different cancer types, including breast, colon, lung, ovary, and brain cancers [18].
Quantitative Optimization Data and Guidelines
A critical step in protocol establishment is the empirical determination of the ideal seeding density and matrix concentration for a specific cell type and research application. The following tables summarize key quantitative considerations and provide a template for experimental data collection.
Table 1: General Starting Points for Seeding Density by Cell Type
| Cell Type / Application | Recommended Starting Density (cells/spheroid) | Key Considerations & Outcome Metrics |
|---|---|---|
| Cancer Cell Lines (e.g., MCF-7, HT-29) | 500 - 5,000 cells | Optimize for consistent size and prevent necrotic core; monitor viability with assays like WST-1 [18]. |
| Patient-Derived Cells | 1,000 - 10,000 cells | High variability; requires titration to account for viability and proliferative capacity from primary tissue. |
| Cardiovascular Progenitors | 2,000 - 7,000 cells | Aim for spheroids that support angiogenesis and cell-cell signaling in cardiac microenvironments [6]. |
| Mesenchymal Stem Cells (MSCs) | 3,000 - 8,000 cells | Density influences differentiation potential; higher densities often promote osteogenic/chondrogenic pathways. |
Table 2: Matrix Concentration Optimization Guide
| Matrix Material | Common Working Concentration Range | Impact of Low Concentration | Impact of High Concentration |
|---|---|---|---|
| Matrigel | 2 - 10 mg/mL | Poor structural integrity, irregular spheroid morphology. | High stiffness, impedes cell migration and can inhibit proliferation. |
| Collagen I | 1.5 - 3.0 mg/mL | Insufficient attachment sites, weak contraction. | Dense network limits nutrient diffusion, increases hypoxia. |
| Agarose | 1.0 - 2.0% (w/v) | Ineffective cell entrapment and aggregation. | Prevents necessary cell-cell contact for spheroid formation. |
| Synthetic PEG-based Hydrogels | 2 - 10% (w/v) | Tunable; too low may not present sufficient adhesive ligands. | Tunable; too high can be overly restrictive for cell remodeling. |
Table 3: Template for Systematic Optimization Experiment Data Recording
| Test Condition (Cell Line: XYZ) | Seeding Density (cells/well) | Matrix Conc. (mg/mL) | Avg. Spheroid Diameter (µm) @ 72h | Viability (WST-1 Absorbance) | Morphology Score (1-5) | Notes |
|---|---|---|---|---|---|---|
| Condition A | 1,000 | 2.0 | ||||
| Condition B | 1,000 | 4.0 | ||||
| Condition C | 3,000 | 2.0 | ||||
| Condition D | 3,000 | 4.0 | ||||
| Condition E | 5,000 | 2.0 | ||||
| Condition F | 5,000 | 4.0 |
Detailed Experimental Protocols
Core Protocol: Systematic Titration of Parameters
This protocol outlines the steps for a multi-factorial experiment to identify the optimal seeding density and matrix concentration.
Research Reagent Solutions & Essential Materials
| Item | Function & Brief Explanation |
|---|---|
| Basement Membrane Matrix (e.g., Matrigel) | Provides a biologically active scaffold that mimics the in vivo extracellular matrix, promoting cell adhesion and 3D organization. |
| Serum-Free Cell Culture Medium | Used to dilute the matrix and suspend cells, ensuring undefined serum components do not interfere with controlled matrix polymerization. |
| WST-1 Assay Reagent | A colorimetric method to quantitatively assess cell viability by measuring cellular metabolic activity via mitochondrial dehydrogenases [38]. |
| 96-Well U-Bottom Plates | The geometry of these wells encourages the natural aggregation of cells into a single spheroid per well through gravity. |
| Phosphate-Buffered Saline (PBS) | Used for washing cells and diluting reagents; it provides an isotonic and pH-balanced environment. |
| Centrifuge | Essential for pelleting cells during passaging and ensuring accurate cell counts for seeding. |
| Hemocytometer or Automated Cell Counter | Allows for precise quantification of cell concentration prior to seeding, which is critical for reproducibility. |
| Microplate Reader | Instrument required to measure the absorbance of the formazan dye produced in the WST-1 assay, correlating to viability [38]. |
Methodology:
- Cell Preparation:
- Harvest cells during the logarithmic growth phase using a standard method (e.g., trypsinization).
- Centrifuge the cell suspension, aspirate the supernatant, and resuspend the pellet in an appropriate volume of serum-free medium.
- Perform a viable cell count using a hemocytometer (e.g., Trypan Blue exclusion) or an automated cell counter. Accuracy at this stage is paramount.
Experimental Plate Setup:
- Prepare a stock solution of the matrix material (e.g., Matrigel) on ice to prevent premature polymerization. Dilute it to the desired starting concentration(s) using cold, serum-free medium.
- Prepare cell suspensions at varying densities based on your experimental design (e.g., 1,000, 3,000, and 5,000 cells in 50 µL of medium per well).
- In a 96-well U-bottom plate, combine the matrix and cell suspensions. For each test condition, add 50 µL of the diluted matrix solution to the well, followed immediately by 50 µL of the cell suspension. Pipette up and down gently to mix. This results in a final volume of 100 µL per well with the desired final cell number and matrix concentration.
- Include control wells: blank controls (medium and matrix only, no cells) and positive controls (cells known to form robust spheroids under set conditions).
- Centrifuge the plate at a low speed (e.g., 300 x g for 1-2 minutes) to gently pellet the cells into the bottom of the U-well, initiating contact.
- Carefully transfer the plate to a cell culture incubator (37°C, 5% CO₂) and allow the matrix to polymerize for 30-60 minutes without disturbance. After polymerization, add an additional 100 µL of complete culture medium on top of each well to prevent evaporation.
Culture and Monitoring:
- Culture the spheroids for the desired duration (typically 3-7 days), replacing 50% of the medium every 2-3 days to maintain nutrient levels.
- Monitor spheroid formation daily using an inverted microscope. Document morphology and take images for subsequent size analysis.
Assessment Protocol: Viability and Size Analysis
Spheroid Imaging and Size Quantification:
- On the day of analysis, image at least 5-10 spheroids per condition using a microscope with a calibrated digital camera.
- Use image analysis software (e.g., ImageJ) to measure the diameter (or cross-sectional area) of each spheroid. Calculate the average diameter and standard deviation for each condition.
Cell Viability Assessment (WST-1 Assay):
- Prepare the WST-1 reagent according to the manufacturer's instructions.
- Carefully remove 100 µL of spent medium from each well of the 96-well plate.
- Add 100 µL of fresh culture medium and 10 µL of WST-1 reagent directly to each well (following a 1:10 ratio of reagent to culture volume is a common guideline) [38].
- Incubate the plate in the cell culture incubator for a predetermined period (e.g., 1-4 hours). Monitor the development of the orange-colored formazan dye.
- After incubation, shake the plate gently on an orbital shaker for 1 minute.
- Measure the absorbance of the solution in each well using a microplate reader. Use a test wavelength of 440–450 nm and a reference wavelength of 600–650 nm to correct for background interference [38].
- Calculate the net absorbance for each test well by subtracting the average absorbance of the blank control wells (containing matrix and medium, but no cells).
Data Analysis and Workflow Visualization
The process of optimizing spheroid formation and analyzing the results involves a logical sequence of steps, from experimental design to data-driven decision-making. The following workflow diagram outlines this process.
Diagram 1: Spheroid Optimization and Analysis Workflow
Once data is collected, the relationship between the input parameters (density, matrix) and the output metrics (size, viability) must be visualized to identify the optimal condition. The following logic diagram illustrates how to interpret these relationships.
Diagram 2: Logic of Parameter Impact on Outcomes
Troubleshooting and Best Practices
Common Challenges and Solutions:
- Irregular Spheroid Shape: This is often due to inconsistent cell seeding or an suboptimal matrix concentration. Ensure a homogeneous cell suspension and centrifuge the plate post-seeding. Re-titrate the matrix to find a concentration that supports cohesion without being too restrictive.
- Low Viability Metrics: Necrotic cores are a sign of overly large spheroids or a matrix that is too dense, impairing diffusion. Reduce the seeding density. Widespread low viability can indicate cytotoxicity of the matrix components; ensure materials are sterile and tested for cell culture use.
- High Well-to-Well Variability: This typically stems from inaccurate cell counting or pipetting errors. Use calibrated pipettes and practice consistent technique. When diluting viscous matrices, pre-chill all tips and tubes and mix thoroughly without introducing air bubbles.
Best Practices for Reproducibility:
- Standardize Cell State: Always use cells at a similar passage number and harvest during the log-phase of growth.
- Handle Matrix with Care: Keep matrix materials on ice at all times during preparation to prevent premature gelling.
- Include Adequate Controls: Each experimental plate should contain its own set of blanks (for background subtraction) and reference controls to normalize results across different experimental runs.
- Validate with Multiple Assays: While the WST-1 assay is an excellent tool for measuring metabolic activity, correlating its results with other methods, such as imaging of live/dead stains, provides a more comprehensive picture of spheroid health.
The meticulous optimization of cell seeding density and matrix concentration is not merely a preliminary step but a cornerstone of robust and reproducible scaffold-based spheroid research. By following the systematic, data-driven approach outlined in this guide—employing precise protocols, quantitative viability assays like WST-1, and rigorous morphological analysis—researchers can establish a solid foundation for their 3D models [6] [38] [18]. This optimization directly enhances the physiological relevance of spheroids, thereby strengthening their application in critical areas such as drug screening, disease modeling, and the advancement of personalized medicine. A well-optimized spheroid protocol ensures that subsequent experimental results are a true reflection of biological phenomena rather than artifacts of the culture system.
Three-dimensional (3D) spheroid models have emerged as a transformative technology in cancer research, addressing the critical limitations of traditional two-dimensional (2D) cell cultures. Unlike monolayer cultures, 3D spheroids better recapitulate the complex tumor microenvironment (TME), including intricate cell-cell interactions, cell-extracellular matrix (ECM) dynamics, and physiological nutrient and oxygen gradients [6]. These models more accurately mimic the in vivo architecture of solid tumors, providing enhanced predictive value for drug response and tumor behavior. The integration of scaffold-based and scaffold-free techniques has further expanded their application across various cancer types, enabling researchers to investigate tumor biology with unprecedented physiological relevance. This technical guide examines the application of 3D spheroid models in three distinct malignancies—osteosarcoma, pancreatic ductal adenocarcinoma (PDAC), and prostate cancer—highlighting specific methodologies, quantitative findings, and translational applications within the broader context of scaffold-based techniques research.
Osteosarcoma Spheroid Models
Model Applications and Advantages
Osteosarcoma (OS), the most common malignant primary bone tumor, presents significant therapeutic challenges, particularly in metastatic cases where outcomes remain poor [39]. Traditional 2D models and animal systems have failed to fully capture the complexity of OS biology, creating an urgent need for more physiologically relevant models. Three-dimensional OS spheroid models have successfully replicated critical tumor features including hypoxic gradients, ECM dynamics, and cellular heterogeneity [39]. These models serve multiple research applications: they facilitate studies of OS biology, enable preclinical drug screening, and support the development of precision oncology approaches through patient-derived organoid models that retain individual-specific traits [39].
Scaffold-free and scaffold-based spheroid systems have both demonstrated utility in OS research, with each approach offering distinct advantages. Scaffold-free systems typically generate compact spheroids with natural ECM production, while scaffold-based approaches provide defined mechanical and biochemical cues that can direct specific cellular behaviors. The integration of 3D bioprinting techniques has further advanced the field by allowing the development of highly structured, biomimetic OS models that better mirror the anatomical complexity of bone tumors [39].
Advanced Analytical Techniques
Multimodal mass spectrometry imaging (MSI) has emerged as a powerful analytical technique for characterizing drug responses in OS spheroid models. A 2024 study utilized desorption electrospray ionization (DESI) mass spectrometry imaging to investigate the chemotherapy drug-induced response of OS multicellular tumour spheroids (MCTS) following treatment with doxorubicin [40]. This approach revealed previously unknown doxorubicin-induced metabolite upregulation, providing insights into potential mechanisms of chemotherapeutic resistance [40].
The study complemented endogenous metabolite distributions with subcellularly resolved protein localization through the detection of metal-tagged antibodies using Imaging Mass Cytometry (IMC). This multimodal approach demonstrated specific tumor survival mechanisms characteristic of those reported for in vivo tumors, validating the value of OS spheroid models as tools to investigate drug resistance pathways [40]. The application of matrix-assisted laser desorption ionization–immunohistochemistry (MALDI-IHC) to 3D cell culture models represented a methodological advancement, enabling detailed spatial resolution of protein expression following chemotherapeutic intervention [40].
Table 1: Key Research Applications of Osteosarcoma Spheroid Models
| Application Area | Specific Utility | Model Type | References |
|---|---|---|---|
| Drug Screening | Evaluation of chemotherapeutic efficacy and resistance mechanisms | Scaffold-free & scaffold-based spheroids | [39] |
| Tumor Microenvironment Studies | Investigation of hypoxic gradients and ECM dynamics | Multicellular tumor spheroids (MCTS) | [39] [40] |
| Precision Oncology | Development of patient-specific treatment approaches | Patient-derived organoids | [39] |
| Biomarker Discovery | Identification of novel therapeutic targets and resistance markers | 3D bioprinted models | [39] |
Experimental Protocol: Osteosarcoma Spheroid Formation and Drug Treatment
Materials and Reagents:
- Osteosarcoma cell lines (e.g., MG-63, Saos-2) or patient-derived cells
- Ultra-low attachment (ULA) multiwell plates or Elplasia microcavity plates
- Complete culture medium (DMEM/F12 supplemented with FBS)
- Therapeutic agents (e.g., doxorubicin)
- Fixation reagents (paraformaldehyde)
- Staining solutions (Hoechst, viability dyes, immunohistochemistry reagents)
Methodology:
- Cell Preparation: Harvest OS cells from 2D culture using standard trypsinization procedures. Count cells and adjust concentration to 1.0-2.0 × 10^5 cells/mL in complete medium.
- Spheroid Formation: Seed cell suspension into ULA plates (100-200 μL per well). For high-throughput applications, utilize microcavity plates to ensure uniform spheroid size.
- Culture Maintenance: Incubate plates at 37°C, 5% CO2 for 48-72 hours without disturbance to allow spheroid consolidation.
- Drug Treatment: Add chemotherapeutic agents in concentration gradients after spheroid formation. Include vehicle controls.
- Endpoint Analysis: After 3-5 days of treatment, assess spheroid viability using ATP-based assays (CellTiter-Glo), image for morphological changes, and process for MSI or IMC analysis as required [39] [40].
Pancreatic Ductal Adenocarcinoma (PDAC) Spheroid Models
Clinical Relevance and Model Specifications
Pancreatic ductal adenocarcinoma (PDAC) represents the fourth leading cause of cancer-related deaths, with a nearly universal fatality rate primarily attributable to profound chemotherapy resistance [41]. The failure of numerous promising drugs in clinical trials after showing efficacy in conventional 2D models has highlighted the critical need for more physiologically relevant testing systems. PDAC spheroids have emerged as next-generation models that closely mirror aspects of pancreatic tumor biology, addressing the limitations of traditional systems through better recapitulation of the native TME [41].
These 3D models demonstrate distinct advantages over 2D systems across multiple parameters: they exhibit more physiological morphology, appropriate proliferation patterns, clinically relevant drug response profiles, and authentic protein expression signatures [41]. The dense stromal component characteristic of pancreatic tumors is particularly well-modeled in PDAC spheroid systems, enabling investigation of stromal-epithelial interactions that contribute to therapeutic resistance. Both tumor organoids and spheroids generated through various methodologies have shown significant promise for advancing PDAC research and improving drug development pipelines.
Technical Approaches and Applications
PDAC spheroid models can be generated through multiple technical approaches, each offering distinct advantages for specific research applications. The forced-floating method, which utilizes low-attachment surfaces with specialized coatings, represents one of the most common approaches for generating uniform PDAC spheroids [18]. Alternatively, scaffold-based techniques employing natural or synthetic ECM substitutes provide physiological matrix cues that influence spheroid development and drug resistance mechanisms [41].
These models have been successfully applied to multiple aspects of PDAC research: they facilitate studies of tumor-stromal interactions, enable high-throughput drug screening, support investigations of metabolic adaptations in the tumor microenvironment, and provide platforms for evaluating novel therapeutic combinations [41]. The ability to generate PDAC spheroids from patient-derived tissue further enhances their translational relevance, creating opportunities for personalized medicine approaches in a malignancy with limited treatment options.
Table 2: Quantitative Analysis of PDAC Spheroid Drug Response Compared to 2D Models
| Parameter | 2D Models | 3D Spheroid Models | Clinical Correlation |
|---|---|---|---|
| Drug IC50 Values | Significantly lower | 10-1000x higher | Better predicts clinical resistance |
| Proliferation Rate | High, uniform | Heterogeneous, gradient-dependent | Mirrors in vivo tumor growth patterns |
| Gene Expression | Altered differentiation markers | Maintains original tumor signature | Better preserves tumor biology |
| Stromal Components | Limited or absent | Includes CAFs, immune cells | Recapitulates TME complexity |
Experimental Protocol: PDAC Spheroid Formation and Drug Testing
Materials and Reagents:
- Pancreatic cancer cell lines (e.g., PANC-1, MIA PaCa-2) or patient-derived cells
- Low attachment multiwell plates (U-bottom preferred)
- Matrigel or other ECM scaffolds for scaffold-based approaches
- Serum-free or serum-reduced media optimized for pancreatic cells
- Chemotherapeutic agents (e.g., gemcitabine, abraxane)
Methodology:
- Cell Preparation: Harvest PDAC cells at 80-90% confluence. Prepare single-cell suspension at appropriate density (5,000-25,000 cells/mL depending on desired spheroid size).
- Spheroid Formation: Plate cell suspension in low-attachment plates. Centrifuge plates at low speed (100-200 × g) for 5 minutes to promote cell aggregation.
- Culture Maintenance: Incubate at 37°C with 5% CO2 for 3-5 days, monitoring spheroid formation daily. Change media carefully every 2-3 days without disrupting aggregates.
- Drug Treatment: After spheroid maturation, add chemotherapeutic agents in serial dilutions. Include appropriate vehicle controls.
- Viability Assessment: Use ATP-based assays, live/dead staining (Calcein AM/EtHD), or morphological analysis to quantify drug response [41].
Prostate Cancer Spheroid Models
Tumor Biology and In Vivo Applications
Prostate cancer (PCa) represents an ideal candidate for 3D modeling approaches due to its heterogeneous biology and dependence on complex tumor-stromal interactions. Traditional 2D PCa cultures fail to replicate the androgen receptor signaling dynamics and tumor architecture critical for therapeutic response [42]. Prostate spheroids (prostaspheres) have enabled more accurate investigation of PCa biology, particularly in studying the emergence of castration-resistant prostate cancer (CRPC) following androgen deprivation therapy (ADT) [42].
A landmark 2024 study established an orthotopic implantation technique for preformed PCa spheroids, demonstrating that the three-dimensional organization significantly impacts tumor progression and metastatic potential [43]. In this innovative approach, researchers implanted LNCaP cells into the prostate of immunodeficient SCID mice either as single cells or as preformed 3D spheroids. The results revealed that spheroid-derived tumors evolved earlier, exhibited shorter doubling times, and developed larger tumor volumes compared to tumors derived from single cells [43]. Furthermore, spheroid tumors established lung and lymph node metastases in 75% of mice, compared to only 50% in the single-cell implantation group [43].
Exercise Modulation Studies
A novel application of PCa spheroid models emerged in 2025 with a study investigating how physical activity influences cancer cell behavior. Researchers collected serum from healthy male participants before, immediately after, and 3 hours after running sessions (5 km and 10 km) [44]. This running session-conditioned human serum was then used to stimulate LNCaP and PC3 prostate cancer cells in 3D culture systems.
The findings demonstrated a significant reduction in spheroid formation capacity when cells were treated with post-exercise serum. Specifically, LNCaP cells showed reductions in spheroid number of up to 37.8% with POST-3h serum following a 5 km run [44]. Additionally, spheroid volume decreased by 42.6% (5 km) and 51.1% (10 km) with POST-3h serum in LNCaP cells [44]. The study further correlated these effects with participant characteristics, finding that higher muscle mass, cardiorespiratory fitness, and age were associated with greater reductions in spheroid number and volume [44].
Experimental Protocol: Orthotopic Implantation of Prostate Spheroids
Materials and Reagents:
- Prostate cancer cell lines (LNCaP, PC3)
- Ultra-low attachment plates for spheroid formation
- Immunodeficient SCID mice
- Anesthetic agents (isoflurane)
- Surgical instruments for microsurgery
- High-resolution ultrasound system for monitoring
Methodology:
- Spheroid Preparation: Generate LNCaP spheroids using ULA 96-well plates seeded with 25,000 cells/well. Culture for 6 days until spheroids reach approximately 1000 μm in size [43].
- Animal Preparation: Anesthetize SCID mice and place in supine position. Shave and disinfect abdominal area.
- Surgical Procedure: Make a lower midline abdominal incision to expose the prostate. Using a 20G needle, carefully implant preformed spheroids or single-cell suspensions directly into the anterior prostate lobe [43].
- Post-operative Monitoring: Monitor tumor growth weekly using high-resolution 3D ultrasonography and measure serum PSA levels every 2-4 weeks [43].
- Endpoint Analysis: After 20 weeks, sacrifice animals and analyze primary tumors and potential metastases (lung, lymph nodes) using histology (H&E) and immunohistochemistry (AMACR, AR, Ki-67) [43].
Table 3: Comparative Tumor Progression Following Orthotopic Implantation of Prostate Spheroids vs. Single Cells
| Tumor Characteristic | Single Cell Implantation | Spheroid Implantation | Significance |
|---|---|---|---|
| Tumor Formation Rate | 50% (4/8 mice) | 50% (4/8 mice) | Not significant |
| Metastasis Rate | 50% (2/4 tumors) | 75% (3/4 tumors) | Increased metastatic potential |
| Mean Tumor Volume at 14 Weeks | 55 mm³ | 766 mm³ | 14-fold increase |
| Tumor Doubling Time | Longer | Shorter | More aggressive growth |
| IHC Expression (Ki-67, AR) | Lower | Higher | Enhanced proliferation |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for 3D Spheroid Culture
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevent cell adhesion, promote 3D aggregation | General spheroid formation across cancer types [43] [13] |
| Elplasia Microcavity Plates | High-throughput uniform spheroid generation | Standardized drug screening assays [13] |
| Matrigel/ECM Scaffolds | Provide physiological matrix environment | Scaffold-based spheroid models, invasion studies [13] |
| ROCK Inhibitor (Y-27632) | Enhance stemness, reduce anoikis | Improving spheroid formation efficiency [13] |
| CellXpress.ai System | Automated 3D culture and screening | High-throughput spheroid assays, compound testing [45] |
| Hanging Drop Plates | Generate spheroids through gravity-enforced aggregation | Prostate cancer spheroid formation [18] |
Visualizing Experimental Workflows
Workflow for Automated 3D Spheroid Screening
Orthotopic Spheroid Implantation and Analysis
The case studies presented in this technical guide demonstrate the significant advances enabled by 3D spheroid models across three distinct cancer types. In osteosarcoma research, these models have facilitated the identification of novel drug resistance mechanisms through advanced analytical techniques. For PDAC, spheroid systems have provided critical insights into stromal interactions and drug resistance patterns that better correlate with clinical outcomes. In prostate cancer, sophisticated orthotopic implantation techniques have revealed the profound impact of three-dimensional organization on tumor progression and metastasis, while innovative exercise modulation studies have opened new avenues for understanding lifestyle impacts on cancer biology.
The continued refinement of scaffold-based techniques, standardization of methodologies, and integration of automated systems will further enhance the reproducibility and translational potential of 3D spheroid models. As these technologies mature, they promise to accelerate the drug development pipeline and advance personalized medicine approaches across multiple cancer types, ultimately improving patient outcomes through more physiologically relevant preclinical models.
Three-dimensional (3D) spheroid models, once primarily the domain of oncology research, have emerged as powerful tools in tissue engineering and regenerative medicine. These scaffold-free cellular aggregates better replicate the in vivo cellular microenvironments of complex tissues than traditional two-dimensional (2D) cultures by promoting more intricate cell-cell and cell-extracellular matrix (ECM) interactions [6]. In regenerative medicine, spheroids function as fundamental building blocks that can be assembled into larger, more complex tissue constructs, offering enhanced physiological relevance for both tissue repair strategies and disease modeling outside the cancer context [46]. This technical guide explores the application of spheroid technologies within scaffold-based frameworks, detailing methodologies, mechanistic insights, and quantitative data supporting their utility across multiple tissue systems.
The paradigm shift from single-cell suspensions to spheroid-based therapies addresses critical limitations in regenerative approaches. Traditionally injected as monodispersed cells, transplanted cells often exhibit rapid cell death and insufficient retention at implantation sites, severely limiting their therapeutic potential to just a few days [47]. Spheroids circumvent these issues by preserving endogenous ECM and enhancing cell-cell signaling, which collectively increase cell survival in harsh microenvironments and upregulate beneficial trophic factor secretion [47].
Table 1: Advantages of 3D Spheroids Over 2D Cultures in Regenerative Applications
| Parameter | 2D Monolayer Culture | 3D Spheroid Culture | Biological Impact |
|---|---|---|---|
| Cell-Matrix Interactions | Limited to synthetic substrate | Natural, omnidirectional ECM | Enhanced mechanotransduction and signaling |
| Cell Morphology | Flattened, stretched | Tissue-like, condensed | Restored apical-basal polarity in epithelial cells |
| Metabolic Gradients | Uniform | Hypoxic core/nutrient gradients | Mimics in vivo tissue conditions |
| Therapeutic Secretome | Reduced | Potentiated | Enhanced angiogenic and anti-inflammatory effects |
| Transplantation Survival | Poor (<10%) | Significantly improved | Longer-lasting therapeutic effects |
Spheroid Formation and Instructional Methodologies
Core Formation Techniques
The formation of spheroids relies on promoting cellular self-assembly under conditions that prevent surface adhesion. Several established methods enable researchers to generate spheroids with specific characteristics suited to different applications:
Liquid Overlay Technique: Cells are seeded on non-adherent surfaces coated with agarose or poly-HEMA to prevent attachment, forcing cellular aggregation into spheroids [48]. This approach offers simplicity and compatibility with standard multi-well plates.
Hanging Drop Method: Suspensions of cells are dispensed as droplets on the lids of culture dishes, with gravity causing cells to accumulate at the liquid-air interface and form spheroids [18]. This technique produces highly uniform spheroids without the need for specialized equipment.
Microwell Arrays: Fabricated molds containing numerous microwells constrain cell populations into defined spaces, promoting aggregation [49]. These platforms enable high-throughput spheroid production with excellent size control and are particularly valuable for screening applications.
Bioprinting Approaches: Automated deposition of cell-containing bioinks in precise spatial patterns allows the creation of complex spheroid arrangements [46]. This emerging methodology facilitates the fabrication of tissue constructs with anatomical geometry.
Microfluidic Systems: Labyrinthine channels and chambers enable controlled spheroid formation with minimal reagent consumption [18]. These platforms provide exceptional control over the cellular microenvironment during aggregation.
Instructional Strategies for Phenotypic Control
Spheroid phenotype and function can be directed through precise instructional cues applied either during formation (ex vivo) or after implantation (in situ):
Ex Vivo Instruction: Priming cells before spheroid formation or during spheroid culture through soluble factors, microenvironmental manipulation, or incorporated biomaterials. For example, hypoxic preconditioning enhances spheroid survival after transplantation into poorly vascularized sites by upregulating endogenous survival mechanisms [47]. Similarly, culture with dexamethasone and calcium/phosphate supplementation promotes osteogenic differentiation in mesenchymal stromal cell (MSC) spheroids [49].
Biomaterial Incorporation: Nano- and microparticles can be embedded within spheroids to provide instructional cues. For instance, mineral-coated microparticles loaded with bone morphogenetic protein-2 (BMP-2) induce spatially uniform osteogenic differentiation in MSC spheroids, maintaining the differentiated phenotype even after soluble cues are removed [47].
In Situ Instruction: The implantation environment itself provides biological signals that guide spheroid integration and function. Endogenous growth factors, mechanical cues from the surrounding tissue, and vascular interactions all contribute to spheroid maturation and tissue-specific differentiation post-implantation [47].
Diagram 1: Strategic framework for instructing spheroid phenotype and function through ex vivo and in situ approaches
Quantitative Analysis of Spheroid Properties
The functional capacity of spheroids in tissue engineering applications is governed by their biomechanical properties and compositional characteristics. Quantitative analysis reveals significant differences between spheroids derived from different cellular sources, impacting their fusion behavior and ultimate utility.
Mechanical Properties by Cell Type
Mechanical characterization through nanoindentation protocols demonstrates that spheroids from different cellular origins exhibit distinct biomechanical profiles. These properties critically influence spheroid fusion behavior and their subsequent maturation into functional tissues [50].
Table 2: Mechanical Properties of Spheroids from Different Cellular Sources
| Cell Type | Young's Modulus (Pa) | Apparent Surface Tension (mN/m) | Fusion Kinetics | Structural Features |
|---|---|---|---|---|
| Mesenchymal Stem Cells (L-MSCs) | 1080 ± 520 | 26 ± 3 | Slow | Abundant ECM, multiple surface layers |
| Epithelial Cells (RPE) | 470 ± 260 | 17 ± 4 | Fast | Limited ECM, single surface layer |
| MSC Monolayer | 1150 ± 510 | N/A | N/A | N/A |
| RPE Monolayer | 1090 ± 470 | N/A | N/A | N/A |
Contrary to predictions from liquid droplet fusion models, spheroids from epithelial cells with lower apparent surface tension actually fuse faster than those from mesenchymal cells with higher surface tension [50]. This discrepancy suggests that biological processes such as ECM remodeling and cell migration mechanisms significantly influence fusion beyond simple physical properties [50].
Mineralization Capacity Under Ionic Supplementation
In bone tissue engineering, the mineralization capacity of MSC spheroids in response to calcium (Ca²⁺) and phosphate (Pi) supplementation demonstrates their utility as models for skeletal regeneration. Optimization of ionic concentrations is crucial for balancing mineralization efficacy with cell viability [49].
Table 3: Mineralization Response of MSC Spheroids to Ionic Supplementation
| Culture Condition | Concentration | Mineralization Onset | Viability at 10 Days | Spheroid Size Change |
|---|---|---|---|---|
| Ca²⁺ Supplementation | 4 mM | Day 10 | Maintained | Significant increase |
| Ca²⁺ Supplementation | 6-8 mM | Not applicable | Complete loss | Not applicable |
| Pi Supplementation | 2 mM | Day 20 (with DEX) | Maintained | Moderate increase |
| Pi Supplementation | 4-8 mM | Not applicable | Complete loss | Not applicable |
| Control (OM) | N/A | After 20 days | Maintained | Minimal change |
Mineralized spheroids represent valuable in vitro models for studying small molecule perturbations and extracellular-mediated calcification events. The spheroid environment promotes an osteogenic gene expression profile through combined biophysical and inorganic signaling, requiring less calcium or phosphate to achieve mineralization compared to monolayer cultures [49].
Experimental Protocols for Spheroid Analysis
Spheroid Formation and Immunofluorescence Protocol
A standardized protocol for spheroid preparation and immunofluorescence enables detailed characterization of 3D tissue models [48]:
Spheroid Formation: Seed cells in round-bottom non-adherent tissue culture plates at optimized density (e.g., 2,000 HCT116 cells per well). Incubate at 37°C for 3-5 days until spheroid formation is complete.
Recovery: Use wide-bore ice-cold tips to recover spheroids, transferring to pre-chilled tubes pre-coated with 1% BSA/PBS to prevent adhesion. Centrifuge at 20 × g for 20 seconds at 4°C and carefully aspirate medium.
Embedding: Carefully mix spheroids with appropriate 3D scaffolding material (Matrigel, collagen, or synthetic hydrogels) using wide-bore tips. Dispense into PDL-coated imaging plates and incubate for 15 minutes at 37°C to solidify.
Fixation: Remove culture medium and wash samples three times with PBS. Add fixative (4% paraformaldehyde for 10 minutes at room temperature or chilled 100% methanol for 5 minutes at 4°C). Remove fixative and wash three times with PBS.
Antigen Retrieval (if required): For formaldehyde-fixed samples, heat-induced epitope retrieval may be necessary. Incubate spheroids in antigen retrieval buffer (Tris/EDTA pH 9.0 or sodium citrate pH 6.0) for 20 minutes at 96-98°C.
Permeabilization: Incubate with permeabilization buffer (PBS with 0.5-2% Triton X-100) for one hour at room temperature with gentle shaking.
Blocking: Apply blocking buffer (PBS with 0.1% Tween, 1% BSA, 22.52 mg/mL glycine, and 10% goat serum) overnight at room temperature with shaking.
Antibody Staining: Incubate with primary antibodies at optimized concentrations according to manufacturer protocols. Wash four times (1 hour each) with wash buffer (PBS with 0.1% Tween). Apply secondary antibodies and nuclear stains (DAPI/Hoechst) if needed, incubating overnight. Repeat washing procedure.
Imaging: Mount samples in appropriate media and image using confocal or fluorescence microscopy with optimized excitation/emission settings.
Diagram 2: Comprehensive workflow for spheroid preparation and immunofluorescence analysis
Spheroid Fusion Kinetics Assay
The fusion kinetics of tissue spheroids provides a quantitative in vitro assay for evaluating tissue maturation potential. This approach serves as a high-throughput screening platform for identifying factors that accelerate functional tissue formation [51]:
Spheroid Preparation: Generate uniformly sized spheroids using microwell arrays or hanging drop methods. For fusion analysis, spheroids should be standardized to 300-500 μm diameter.
Initial Imaging: Acquire brightfield images of individual spheroids to establish baseline morphology and dimensions. Measure cross-sectional area and perimeter for each spheroid.
Aggregate Assembly: Carefully transfer spheroids into non-adherent culture dishes in close proximity (100-200 μm spacing) or into specific fusion patterns using bioprinting or micromanipulation approaches.
Time-Lapse Monitoring: Culture assemblies under appropriate conditions while capturing time-lapse images at regular intervals (15-60 minutes) over 24-72 hours.
Fusion Quantification: Analyze image sequences to determine fusion metrics:
- Fusion Index: Calculate as 1 - (Gap Length / Initial Distance) × 100
- Area Reduction: Measure decrease in total surface area over time
- Kinetic Constants: Derive rate constants from time-course data
Maturogenic Factor Screening: Apply test compounds or conditions to spheroid assemblies and compare fusion kinetics to untreated controls. Accelerated fusion indicates enhanced tissue maturation potential.
Essential Research Reagents and Materials
Successful implementation of spheroid-based tissue engineering requires specific reagents and materials optimized for 3D culture systems. The following toolkit represents essential components for spheroid research in regenerative applications:
Table 4: Essential Research Reagent Solutions for Spheroid-Based Tissue Engineering
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Non-adherent Plates | Prevents cell attachment, forcing spheroid formation | U-bottom or V-bottom designs optimize spheroid uniformity |
| Pluronic F108 | Microwell coating to inhibit cell adhesion | Critical for scaffold-free spheroid formation in arrays |
| Basement Membrane Matrix | Provides 3D scaffolding for spheroid embedding | Matrigel preferred for its natural composition |
| Wide-Bore Pipette Tips | Enables spheroid transfer without disruption | Essential for maintaining structural integrity |
| Triton X-100 | Membrane permeabilization for antibody access | Concentration optimization critical (0.5-2%) |
| Glycine-Containing Blocking Buffer | Reduces non-specific antibody binding | Superior to BSA-alone for complex 3D structures |
| Calcein-AM | Viability staining in 3D constructs | Penetration limited in larger spheroids |
| OsteoImage | Fluorescent mineralization detection | Specific binding to hydroxyapatite crystals |
| Mineral-Coated Microparticles | Sustained growth factor delivery | Enables prolonged differentiation signaling |
Signaling Pathways in Spheroid-Medated Tissue Regeneration
Spheroid-based tissue regeneration engages multiple signaling pathways that coordinate cellular responses leading to functional tissue formation. Understanding these pathways enables more precise instructional strategies:
Diagram 3: Key signaling pathways engaged during spheroid-based tissue regeneration
The BMP and WNT signaling pathways are particularly important in MSC spheroids directed toward osteogenic differentiation [49]. These pathways are naturally enhanced in the 3D spheroid environment compared to monolayer cultures, contributing to the observed promotion of osteogenic phenotypes without exogenous stimulation [49]. Similarly, calcium signaling not only provides building blocks for mineralized matrix but also activates intracellular signaling cascades that promote osteogenic gene expression [49].
Spheroid technologies represent a paradigm shift in tissue engineering and regenerative medicine, offering enhanced physiological relevance over both traditional 2D cultures and single-cell suspensions. As building blocks for complex tissue constructs, spheroids demonstrate improved survival after transplantation, potent secretory activity, and enhanced functional differentiation compared to dissociated cells [47]. The continued refinement of instructional strategies—combining biological cues, biomaterial integration, and spatial control—will further advance their therapeutic potential.
Future developments in spheroid-based therapies will likely focus on standardizing formation protocols across different cell types, enhancing vascularization strategies for larger constructs, and developing more sophisticated in situ instructional approaches. As these technologies mature, spheroid-based treatments are poised to transition from promising preclinical models to clinically viable therapies for a range of degenerative conditions, ultimately fulfilling their potential as essential tools in the regenerative medicine arsenal.
Solving Practical Challenges: A Guide to Reproducible and High-Quality Spheroid Culture
In the realm of three-dimensional (3D) cell culture, spheroid models have become an indispensable tool for preclinical cancer research, drug discovery, and tissue engineering. These microtissues mimic the complex cellular microenvironment and avascular tumor regions more accurately than traditional two-dimensional (2D) cultures [52]. However, a significant challenge persists: controlling the uniformity of spheroids in terms of size, shape, and density. As spheroid uniformity is a critical parameter influencing the reproducibility of drug test results and experimental outcomes, developing robust strategies to achieve homogeneity is paramount [53].
This technical guide explores advanced methodologies for controlling spheroid size and shape, framed within the context of scaffold-based techniques research. We provide an in-depth analysis of surface engineering, design adaptations, and culture optimization strategies to help researchers standardize their 3D culture systems for more reliable and translatable results.
Surface Optimization Techniques
The Critical Role of Surface Engineering
The substrate surface properties profoundly influence cellular responses, particularly cell adhesion, which directly impacts the self-assembly process of spheroids [54]. Polydimethylsiloxane (PDMS) is widely used in microfluidic biochip platforms but presents challenges due to its hydrophobic nature, which promotes protein adsorption and consequent cell adhesion to the surface [53] [54]. This adhesion interferes with the cell-cell interactions necessary for homogeneous spheroid formation.
Surface Modification with Bovine Serum Albumin (BSA)
Surface modification of PDMS with bovine serum albumin (BSA) effectively suppresses cell adhesion, creating a surface that facilitates cell self-aggregation into uniform spheroids [53]. The concentration of BSA is crucial for achieving the desired cell-repellent properties:
- 10% BSA treatment: Renders PDMS surfaces hydrophilic and effectively blocks adhesive properties, leading to higher cell-cell interactions and homogeneous spheroid production [53] [54].
- 3% BSA treatment: Demonstrates cell repellent properties similar to bare PDMS surfaces, proving insufficient for optimal spheroid formation [53].
The surface optimization process involves flushing microfluidic channels with BSA solutions, followed by incubation overnight at 37°C with 5% CO₂ after cell seeding [54]. This straightforward surface treatment method successfully facilitates the production of uniform, non-scaffold-based spheroids across multiple human cell lines and co-culture models [53].
Alternative Surface Optimization Methods
Beyond BSA treatment, other surface optimization strategies include:
- Ultra-low attachment (ULA) plates: Specifically designed with hydrophilic and neutrally charged surfaces to minimize protein binding and cell adhesion [55].
- Agarose coating: Creates a non-adhesive surface through a 1.5% agarose hydrogel solution that prevents cell-substrate attachment [56] [57].
- Design adaptation: Modifying microwell geometry to cylindrical forms prevents cells from sticking to corners and promotes spheroid formation [54].
Table 1: Surface Modification Techniques for Spheroid Uniformity
| Technique | Mechanism of Action | Optimal Parameters | Cell Lines Demonstrated | Key Advantages |
|---|---|---|---|---|
| BSA Coating | Blocks cell adhesion sites on PDMS | 10% w/v in PBS [53] | Multiple human cancer cell lines [53] | Effective, reproducible, cost-efficient |
| Agarose Hydrogel | Creates non-adhesive surface | 1.5% agarose in microwells [56] | MDA-MB-231, HCT116 [56] [58] | Prevents cell-substrate attachment |
| Ultra-Low Attachment Plates | Hydrophilic, neutrally charged surface | Commercial ULA plates [55] | Ovarian cancer cells [55] | Standardized, easy to use |
| Design Adaptation | Prevents cell sticking in corners | Cylindrical microwells [54] | Various cell lines [54] | Integrated into microfluidic devices |
Scaffold-Based Design and Adaptation
Microfluidic Biochip Platforms
Advanced microfluidic devices offer precise control over the cellular microenvironment through sophisticated design features. These platforms typically consist of:
- Two PDMS layers bonded together using oxygen plasma treatment [54].
- Bottom layers containing channels with square cross-sections (e.g., 840 μm × 840 μm) and circle-bottom microwells (e.g., 840-μm-diameter) [54].
- Top layers with inlet and outlet holes for introducing cells and media [54].
The fabrication process involves creating 3D-printed molds using stereolithography-based printers, followed by soft lithography with PDMS to produce the final devices [54]. The cylindrical well design adaptation prevents cells from sticking to corners, further promoting uniform spheroid formation [54].
Innovative Scaffold-Free Mass Production
While scaffold-based techniques are valuable, some innovative scaffold-free methods also contribute significantly to spheroid uniformity. The cell sheet-based approach represents a novel method for producing large quantities of uniform spheroids:
Diagram 1: Workflow for Facile Spheroid Formation in Large Quantity
This method enables size control through multiple parameters [58]:
- Cell sheet culturing time: Extended culture periods (6-13 days) produce larger cell sheets that form larger spheroids.
- Initial cell seeding density: Lower densities produce larger spheroids due to more extensive cell sheet growth.
- Shaking duration: Longer shaking periods (up to 72 hours) allow for complete spheroid formation and compaction.
Size uniformization is achieved using stainless steel mesh sieves, which filter spheroids into highly uniform populations with controllable size ranges [58].
Nanocellulose-Based Scaffold Systems
Emerging scaffold materials like nano-fibrillated cellulose (NFC) offer promising avenues for advanced spheroid research. These scaffolds provide:
- Adjustable porosity and structural integrity mimicking natural tissue architecture [59].
- Mechanical stability necessary for cell development and tissue regeneration [59].
- Custom 3D structures fabricated through direct-ink-writing (DIW) 3D printing [59].
The protocol involves creating a specialized ink from NFC, carboxymethyl cellulose (CMC), and citric acid, followed by 3D printing, freeze-drying, and cross-linking via dehydrothermal treatment [59]. These scaffolds support cell adhesion, proliferation, and communication while providing a structural framework that can be customized for specific research needs.
Advanced Methodologies for Size and Shape Control
Co-culture Systems for Enhanced Compactness
Integrating multiple cell types in co-culture spheroids significantly influences both size and morphology. Research with ovarian cancer models demonstrates that:
- Simultaneous seeding of cancer cells and fibroblasts promotes fibroblast invasion into the spheroid core, creating more compact structures [55].
- Fibroblast ratio directly impacts spheroid size and compactness, with higher fibroblast ratios (e.g., 2:1) producing smaller, more rounded spheroids in certain cell lines [55].
- Co-culture spheroids develop more defined necrotic cores compared to mono-culture spheroids, better mimicking in vivo tumor complexity [55].
These co-culture systems more accurately represent the tumor microenvironment (TME), including cancer-associated fibroblasts (CAFs) that play crucial roles in tumor progression [55].
Mathematical Modeling for Structure Analysis
Quantitative analysis frameworks provide valuable insights into spheroid structure and growth dynamics. Mathematical models based on nutrient diffusion and consumption patterns reveal that:
- Spheroids progress through three distinct phases: (1) ubiquitous cell cycling throughout the spheroid, (2) development of a viable but cell cycle-arrested region in the center, and (3) formation of a necrotic core [52].
- The limiting structure of spheroids is primarily a function of overall size rather than initial seeding density [52].
- Analyzing spheroid structure as a function of size rather than time produces results that are relatively insensitive to variability in initial conditions [52].
This mathematical approach helps researchers distinguish between different spheroid regions (proliferating, arrested, and necrotic) and establish standardized comparison metrics independent of initial seeding variations.
Table 2: Optimization Parameters for Different Spheroid Models
| Spheroid Model Type | Key Optimization Parameters | Optimal Seeding Density | Culture Duration | Size Control Methods |
|---|---|---|---|---|
| Microfluidic Platform [54] | Surface treatment (10% BSA), microwell geometry | Varies by cell line | 4-9 days [56] | Microwell dimensions, flow control |
| Scaffold-Free Co-culture [55] | Cell ratio, sequential vs. simultaneous seeding | 1000 cells/well [57] | Up to 96 hours [55] | Cell ratio adjustment |
| Cell Sheet-Based [58] | Sheet culture time, shaking duration | Sparse seeding | 6-13 days sheet formation + 72h shaking [58] | Mechanical sieving |
| Agarose Microwell [56] | Agarose concentration, microwell size | 2×10⁶ cells/mL [56] | Up to 14 days [56] | Microwell dimensions |
Experimental Protocols for Uniform Spheroid Formation
Microfluidic Platform Protocol with Surface Optimization
Materials Needed:
- PDMS and curing agent (Sylgard 184 elastomer kit)
- 3D-printed molds
- Oxygen plasma system
- BSA (Sigma-Aldrich)
- Phosphate buffered saline (PBS)
- Ethanol (99.9%)
- Cell lines of interest
Step-by-Step Procedure:
Fabricate PDMS replicas by mixing elastomer base and curing agent in a 10:1 ratio, degassing for 1 hour, pouring into 3D-printed molds, and curing at 65°C for 2 hours [54].
Bond PDMS layers using oxygen plasma treatment (20 sccm oxygen flow, 600 mTorr pressure, 20W RF power for 20s) [54].
Sterilize and prepare devices by flushing channels with 99.9% ethanol to remove air bubbles and sterilize surfaces [54].
Apply surface modification with 10% BSA in sterile PBS by flushing channels 3-4 times with BSA solution, then incubating overnight at 37°C with 5% CO₂ after cell seeding [53] [54].
Seed cells at appropriate density for your cell line (e.g., 2×10⁶ cells/mL for MDA-MB-231 cells [56]) and culture for the required duration with periodic media changes.
Cell Sheet-Based Mass Production Protocol
Materials Needed:
- Standard tissue culture petri dishes
- Dispase enzyme solution
- Orbital shaker
- Stainless steel meshes for sieving
- Cell culture media appropriate for your cell line
Step-by-Step Procedure:
Sparsely seed cells onto petri dishes at low density to ensure separated cellular islets [58].
Culture for 6-13 days until separated cell sheets form, monitoring size regularly [58].
Detach cell sheets using dispase enzyme solution, which cleaves cell-ECM junctions while maintaining sheet integrity [58].
Transfer to orbital shaker with dispase-doped media and shake for up to 72 hours to facilitate sheet curling and spheroid formation [58].
Filter spheroids through stainless steel mesh sieves to achieve desired size uniformity [58].
Transfer to fresh media without dispase for long-term culture and experimentation [58].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Spheroid Uniformity Research
| Reagent/Material | Function | Example Application | Key Considerations |
|---|---|---|---|
| Bovine Serum Albumin (BSA) | Surface modification to prevent cell adhesion | 10% BSA for PDMS treatment [53] | Concentration critical; 10% effective, 3% ineffective [53] |
| Dispase Enzyme | Cleaves cell-ECM junctions for cell sheet detachment | Cell sheet-based spheroid formation [58] | Prevents sheet stacking during shaking; negligible cytotoxicity [58] |
| Agarose | Creates non-adhesive surfaces for spheroid formation | 1.5% agarose for microwell arrays [56] | Prevents cell-substrate attachment; promotes self-assembly |
| Nano-fibrillated Cellulose (NFC) | Scaffold material for 3D tissue architecture | 3D-printed scaffolds for tissue engineering [59] | Adjustable porosity; high biocompatibility |
| Carboxymethyl Cellulose (CMC) | Enhances hydrogel characteristics for 3D printing | Component of NFC-based bioinks [59] | Improves print quality and scaffold stability |
| Citric Acid | Cross-linking agent for scaffold stability | Component of NFC-based bioinks [59] | Increases mechanical stability and biocompatibility |
Characterization and Quality Assessment
Structural and Viability Assessment
Ensuring spheroid uniformity requires robust characterization methods:
- Histological analysis (H&E staining) reveals internal structure, zonation, and necrotic core development [56] [58].
- Immunohistochemistry (IHC) for markers like Ki-67 assesses proliferation zones within spheroids [56].
- Viability staining (e.g., live/dead assays) distinguishes between viable peripheral cells and non-viable core regions [58].
- Optical Coherence Tomography (OCT) provides 3D structural information without damaging spheroids [58].
Functional Characterization
Beyond structural analysis, functional assessments validate spheroid relevance:
- Drug sensitivity testing compares IC₅₀ values between 2D and 3D cultures, with spheroids typically showing increased resistance [56].
- Migration and invasion assays (e.g., Transwell, scratch healing) assess functional behaviors that may differ from 2D cultures [56].
- EMT marker expression (e.g., via Western blot) evaluates epithelial-to-mesenchymal transition, often enhanced in 3D models [56].
Diagram 2: Comprehensive Spheroid Characterization Workflow
Achieving uniformity in spheroid size and shape requires a multifaceted approach combining surface engineering, design optimization, and culture parameter control. The strategies outlined in this technical guide—from surface modification with BSA to microfluidic design adaptations and innovative cell sheet-based production—provide researchers with robust methodologies for generating standardized 3D culture models.
As spheroid technology continues to evolve, the integration of advanced scaffold materials like nanocellulose and the implementation of mathematical frameworks for structure analysis will further enhance our ability to control and predict spheroid characteristics. These developments will ultimately strengthen the translational relevance of spheroid models in drug discovery, disease modeling, and personalized medicine applications, enabling more accurate prediction of clinical responses and advancing our understanding of complex biological systems.
In the field of tissue engineering and regenerative medicine, three-dimensional (3D) spheroid models have emerged as a powerful in vitro tool that better replicates the in vivo cellular microenvironments of complex tissues than traditional two-dimensional (2D) cell cultures [6]. These models promote more intricate cell-cell and cell-extracellular matrix (ECM) interactions, making them invaluable for studying cardiovascular biology, cancer progression, and for advancing drug development [6] [60]. However, a significant challenge in the development and application of larger, more physiologically relevant spheroids is the prevention of central necrosis due to diffusion limitations of oxygen and nutrients [61] [62].
The absence of vascular networks in most in vitro spheroid systems means that oxygen and nutrients must reach the core via diffusion from the surrounding culture medium. When spheroids exceed a critical size, the diffusion distance becomes too great to support the core cells, leading to the formation of a necrotic region [60] [62]. This necrotic core compromises the utility and reproducibility of spheroid models and poses a major obstacle to engineering larger, clinically relevant tissue constructs. Therefore, managing these diffusion limits is paramount for successful scaffold-based techniques research.
This guide provides an in-depth technical analysis of the principles governing nutrient and oxygen diffusion in spheroids and outlines evidence-based strategies to prevent necrosis, framed within the context of advanced scaffold-based research methodologies.
The Biophysics of Diffusion in Spheroids
Fundamental Principles
In avascular spheroids, oxygen distribution is governed by a reaction-diffusion equation. Oxygen diffuses from the surrounding medium into the spheroid while being consumed by the metabolically active cells. The steady-state distribution of oxygen partial pressure is described by the following equation [62]:
[ D \nabla^2 c = Q ]
Where ( D ) is the diffusion coefficient of oxygen in the tissue, ( c ) is the oxygen concentration, and ( Q ) is the cellular oxygen consumption rate. The solution to this equation for a spherical spheroid predicts a parabolic oxygen profile, with the minimum oxygen concentration at the center.
Critical Size Thresholds
The maximum permissible spheroid radius before necrosis occurs is determined by the balance between oxygen supply and demand. Experimental and mathematical modeling studies have identified specific size thresholds for different cell types, summarized in Table 1.
Table 1: Experimentally Determined Critical Size Thresholds for Various Cell Types
| Cell Type | Critical Radius (μm) | Key Parameters | Reference/Model |
|---|---|---|---|
| HepaRG (Liver) | Maintained without necrosis for 9 days | Maximum size without necrosis | Mathematical and Experimental Model [61] |
| Human Melanoma (WM793b) | Necrotic core appears at specific radius ( R_c ) | ( R_c ), ( Q^2 ) ratio (nutrient thresholds) | Greenspan Model Application [60] |
| Normal Tissue (General) | Hypoxia then necrosis with increasing diameter | Range of diameters for hypoxic region formation | Numerical Modeling for Bioprinting [62] |
| hMSC (Cartilage) | Customizable chamber system for construct formation | 7-day maturation before implantation | Scaffold-Free Osteochondral Grafts [17] |
The seminal Greenspan mathematical model for avascular tumour spheroid growth describes three distinct phases of growth: (i) all cells proliferate; (ii) an outer proliferating layer surrounds an inner region of living but non-proliferating cells (inhibited region); and (iii) an outer proliferating layer, an intermediate inhibited region, and a central necrotic core [60]. The formation of the necrotic core is triggered when the spheroid radius exceeds a critical value ( R_c ), and the volume of the necrotic core is governed by a proportionality constant ( \gamma = \lambda/s ), where ( \lambda ) is the rate at which cell volume is lost from the necrotic core and ( s ) is the rate of cell volume production by mitosis [60].
Quantitative Methodologies for Modeling and Analysis
Mathematical Modeling Frameworks
Advanced computational approaches are essential for predicting oxygen distribution and optimizing spheroid size.
Numerical Modeling Using Function Representation (FRep) and Finite Volume Method (FVM): A novel pipeline combines FRep for geometric modeling with FVM for solving reaction-diffusion equations. This approach can model complex shapes, including spheroids with surface irregularities and fusing spheroids, providing a more realistic simulation than simple spherical models. The workflow involves [62]:
- Modeling the spheroid with FRep as a sphere
- Adding solid noise (e.g., Gardner noise) to simulate surface deformities
- Slicing the 3D model
- Constructing an STL file from the slices
- Building a mesh for numerical analysis
- Running FVM simulation on the mesh to model oxygen diffusion
Profile Likelihood Analysis for Parameter Identifiability: When using models like the Greenspan model, it is crucial to determine which parameters can be reliably estimated from experimental data. Profile likelihood analysis calculates maximum likelihood estimates (MLE) and forms confidence intervals for parameters such as the proliferation rate ( s ) and the critical radius ( R_c ). This analysis reveals that measurements of the spheroid's internal structure (necrotic and inhibited radii) provide far more information for parameter identification than outer radius measurements alone [60].
Experimental Measurement Techniques
Accurate quantification of internal spheroid structure is necessary for model validation.
Live-Dead Cell Staining: This standard method differentiates viable and necrotic regions through fluorescent markers. It provides snapshots of necrosis at specific time points but is typically endpoint or semi-quantitative [60].
Fluorescent Ubiquitination-Based Cell Cycle Indicator (FUCCI): This advanced real-time imaging technique uses transduced cell lines whose nuclei fluoresce red when cells are in the G1 phase and green during S, G2, and M phases. FUCCI powerfully reveals the inhibited region (non-proliferating but living cells) in addition to the necrotic core, providing a more complete picture of the internal spheroid structure over time—creating a 4D dataset (3D space plus time) [60].
Semi-Automated Phenotypic Analysis: Systems like the IncuCyte S3 live-cell imaging system enable automated image acquisition and processing, allowing for high-frequency, non-invasive monitoring of spheroid size and morphology. This can be combined with specific assays to quantify viability and function over time [63].
Experimental Strategies to Prevent Necrosis
Size Control and Optimization
The most direct method to prevent necrosis is to maintain spheroid size below the critical diffusion limit.
High-Throughput Uniform Spheroid Production: Using 96-well U-bottom plates (e.g., BIOFLOAT, Elplasia) enables the generation of large numbers of highly uniform spheroids. The Elplasia plate, with its microcavity design, is particularly effective for producing spheroids of consistent size and circularity, which is vital for reproducible screening applications [13]. Automated imaging and analysis pipelines (e.g., with MetaXpress Software) allow for precise quantification of spheroid number, diameter, and circularity, ensuring quality control [13].
Heterogeneous Population Studies: For fundamental studies of stemness and heterogeneity, low-throughput 6-well ultra-low attachment (ULA) plates can be used. These generate a mix of spheroid subtypes (holospheres, merospheres, and paraspheres) with distinct sizes and functional properties. The larger holospheres can act as stem cell reservoirs, but their size must be managed to avoid core necrosis [13].
Enhancing Diffusion with Scaffold-Based and Scaffold-Free Geometries
Spheroid Sheets for Thin Tissue Constructs: A innovative scaffold-free approach involves assembling pre-formed spheroids into a thin, planar sheet sandwiched between two flexible meshes held by a frame. This geometry constrains tissue thickness, guiding lateral spheroid fusion while ensuring efficient nutrient and oxygen diffusion through the thin construct. This method is highly scalable and produces tissue membranes suitable for research or therapeutic applications [64].
Customizable Closed Chamber Systems: For scaffold-free osteochondral grafts, a closed chamber system can be used to direct the fusion of mesenchymal stem cell (MSC) spheroids into a single, larger tissue construct. By controlling the chamber dimensions and culture duration (e.g., 7-day maturation), researchers can generate integrated neocartilage that expresses cartilage-specific markers without central necrosis [17].
Biochemical and Molecular Interventions
ROCK Pathway Inhibition: Treating spheroid cultures with ROCK1 inhibitor (Y-27632) enhances the formation of holospheres (larger spheroids with high stemness) by preserving stemness markers and reducing premature differentiation. This intervention can help maintain cell viability in the core of larger spheroids [13].
Tailored Differentiation Media: For engineered tissues, using specialized differentiation media is critical. For example, chondrogenic medium for hMSCs contains key components like TGF-β1, ascorbic acid, proline, and dexamethasone to support matrix production and cellular function, thereby improving the overall health of the spheroid and its resistance to stress [64].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Spheroid Culture and Analysis
| Item Name | Function/Application | Example Product/Catalog |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Promotes scaffold-free spheroid formation by minimizing cell adhesion. | Corning Elplasia 96-well plates (Cat. No. 4442); Sarstedt BIOFLOAT 96-well plates (Cat. No. 83.3925.400) [13] |
| ROCK1 Inhibitor | Enhances stemness and viability in spheroid cultures; reduces premature differentiation. | Y-27632 [13] |
| Basement Membrane Matrix | Scaffold-based culture; provides ECM cues for studying spheroid outgrowth and migration. | Matrigel [13] |
| FUCCI Vectors | Real-time, non-destructive visualization of cell cycle status (G1 vs. S/G2/M phases) in live spheroids. | (Not specified in results, but commercially available) [60] |
| Chondrogenic Differentiation Media | Directs MSC spheroids toward cartilage formation; contains essential growth factors and supplements. | Custom formulation with TGF-β1, ITS-X, ascorbic acid, proline, dexamethasone [64] |
Visualizing Experimental Workflows and Diffusion Dynamics
Workflow for 4D Spheroid Analysis
The following diagram illustrates an integrated experimental and computational pipeline for analyzing spheroid growth and internal structure, which is critical for identifying diffusion limitations.
Oxygen Diffusion and Necrotic Core Formation
This diagram depicts the relationship between spheroid size, oxygen diffusion gradient, and the emergence of distinct cellular regions, including the necrotic core.
Preventing necrosis in 3D spheroids by managing nutrient and oxygen diffusion is a foundational challenge in scaffold-based techniques research. Success hinges on a multifaceted strategy that integrates rational spheroid size control, advanced bioreactor design that enhances mass transfer, and the potential incorporation of pre-vascularization strategies. Quantitative mathematical modeling and rigorous experimental validation using techniques like FUCCI imaging are indispensable for identifying critical parameters and optimizing culture conditions. As the field progresses, the standardization of these methodologies, as demonstrated in the comparative analysis of scaffold-free and scaffold-based systems, will be crucial for enhancing reproducibility and accelerating the translation of spheroid-based models from the laboratory bench to clinical applications in drug screening and tissue regeneration.
Protocol Adaptation for Stubborn Cell Lines and Co-cultures
Within the broader thesis of scaffold-based techniques in spheroid model research, the challenge of adapting standard protocols for stubborn cell lines and complex co-cultures represents a critical frontier. Two-dimensional (2D) monolayer cultures fail to recapitulate the in vivo tissue architecture involving complex cell-cell and cell-matrix interactions [65] [66]. Three-dimensional (3D) spheroid models, particularly those utilizing scaffold-based systems, have emerged as powerful tools that more accurately reproduce the compact architecture of in vivo cell growth and can model characteristics of tissue development and disease progression such as drug resistance [66] [67].
However, protocol standardization remains challenging, as different cell lines exhibit vastly different capacities for spheroid formation [68]. This technical guide provides a structured approach to protocol adaptation within a scaffold-based research framework, offering detailed methodologies and quantitative benchmarks for developing robust spheroid models from challenging cellular systems.
Material and Reagent Solutions
The successful formation of spheroids, particularly with stubborn cell lines, often requires specific reagents to promote cell aggregation and maintain 3D structure. The table below summarizes key research reagent solutions and their functions.
Table 1: Essential Research Reagents for Spheroid Formation with Stubborn Cell Lines
| Reagent Solution | Function & Mechanism | Application Notes |
|---|---|---|
| Matrigel [68] [65] | Natural ECM polymer scaffold; provides structural support and bioactive cues. | Can be used as supplement (1-3.5%) or embedding matrix. Batch-to-batch variability requires optimization. |
| Methodel (Methylcellulose) [68] [66] | Inert, viscous polymer that discourages monolayer formation and enhances cell-cell adhesion. | Typical concentration range: 1-5 mg/mL. Water-soluble and easily washed away post-formation. |
| Collagen (Type I) [66] | Natural polymer hydrogel used for embedding spheroids in invasion assays. | Requires neutralization to pH 7.4 before use. Final concentration of 2.5 mg/mL is common. |
| Cell-Repellent Plates [66] | Surface-treated plates (e.g., U-bottom) that prevent cell attachment, forcing aggregation. | Essential for scaffold-free methods. Must be sterile and dust-free to avoid aggregation artifacts. |
Quantitative Benchmarking of Protocol Performance
Systematic comparison of different spheroid formation protocols across diverse cell lines provides critical baseline data for protocol adaptation. The following table synthesizes quantitative performance data from method comparison studies.
Table 2: Protocol Performance Across Different Cell Lines and Conditions [68]
| Cell Line | Protocol Type | Key Additives | Formation Success | Structural Features (IHC) |
|---|---|---|---|---|
| MCF-7 (Breast Cancer) | Hanging Drop | 25% Methocel | Success under almost all conditions | Uniform spheroids; Ki-67+, cPARP+, MUC-1+ |
| MCF-7 (Breast Cancer) | Liquid Overlay | Various | High success rate | Proliferative and necrotic regions present |
| MDA-MB-231 (Breast Cancer) | Liquid Overlay | 3.5% Matrigel | Successful formation under only one protocol | Requires specific matrix support |
| MDA-MB-231 (Breast Cancer) | Hanging Drop | 25% Methocel | Limited success | Inconsistent aggregation |
| SK-BR-3 (Breast Cancer) | Multiple | Various | No success under tested conditions | Requires extensive protocol adaptation |
Core Methodologies and Detailed Protocols
Optimized Liquid Overlay Technique with Matrix Supplementation
For cell lines like MDA-MB-231 that respond poorly to scaffold-free methods, the liquid overlay technique with matrix support provides a reliable alternative [68].
Detailed Protocol:
- Surface Coating: Prepare a solution of 3.5% Matrigel in cold serum-free medium. Coat each well of a 96-well plate with 50-100 µL of this solution and incubate at 37°C for 30 minutes to allow gelation.
- Cell Preparation: Trypsinize cells and neutralize with serum-containing medium. Centrifuge at 500 × g for 10 minutes and resuspend in appropriate spheroid formation medium.
- Cell Seeding: Seed cells at optimized densities (1,000-10,000 cells/well, depending on cell line) in 100-200 µL of medium supplemented with matrix components.
- Spheroid Formation: Culture at 37°C and 5% CO2 for 24-48 hours. Monitor daily for spheroid formation.
- Validation: Confirm spheroid integrity by gently pipetting medium over the spheroid; properly formed spheroids will loosen and roll, confirming their 3D structure [66].
Methyl Cellulose-Based Aggregation for Stubborn Cell Lines
The use of methyl cellulose provides a scaffold-free approach to promote aggregation for cell lines that retain some capacity for self-assembly but form inconsistent spheroids under standard conditions [66].
Detailed Protocol:
- Methyl Cellulose Preparation: Prepare a 100 mg/mL stock solution of methyl cellulose. Heat 50 mL ultrapure H2O to 80°C, add 10 g methyl cellulose powder, and agitate until dispersed. Bring to final volume with cold water and stir at 4°C until clear. Filter through a 0.45 µm filter and store at 4°C for up to 12 months.
- Spheroid Formation Medium: Dilute methyl cellulose stock to 1-5 mg/mL in appropriate culture medium immediately before use. Filter sterilize through a 0.22 µm filter.
- Cell Seeding and Aggregation: Trypsinize cells, count, and resuspend in spheroid formation medium at 1 × 10^4 cells/mL. Dispense 100 µL into each well of a 96-well U-bottom cell-repellent plate. Culture at 37°C and 5% CO2.
- Optimization: Titrate methyl cellulose and serum concentrations for each cell line to yield formation of a single spheroid per well. Cells should settle to the bottom within 6 hours and aggregate into a spheroid within 24-48 hours.
Co-culture Spheroid Formation Using Primary Cells
For primary cells with limited viability or those requiring stromal support, co-culture systems dramatically enhance viability and function [69].
Detailed Protocol:
- Cell Preparation: Isolate primary cells (e.g., hepatocytes from partial hepatectomy specimens) and supportive cells (e.g., human adipose-derived stem cells - hADSCs).
- Cell Mixing: Combine primary cells and supportive cells in a 1:1 ratio. Create a cell suspension at the appropriate density in spheroid formation medium.
- Microwell Seeding: Seed the cell mixture into concave microwells that have been pre-coated with 3% BSA to prevent attachment.
- Culture and Maturation: Culture for several days, allowing spheroid aggregation and maturation. Co-cultured spheroids typically form more compact structures more rapidly than mono-cultured spheroids.
- Functional Assessment: Assess functional improvement compared to mono-cultures through methods such as albumin secretion measurement, urea synthesis assays, or cytochrome P450 activity tests [69].
Systematic Workflow for Protocol Adaptation
The following diagram illustrates a systematic approach to adapting spheroid protocols for stubborn cell lines, integrating both scaffold-based and scaffold-free methods.
Systematic Protocol Adaptation Workflow
Co-culture Spheroid Formation Logic
For particularly challenging primary cells or those requiring specialized microenvironments, co-culture systems provide essential support. The following diagram outlines the logical pathway for establishing functional co-culture spheroids.
Co-culture Spheroid Formation Logic
Advanced Applications and Future Directions
The successful adaptation of spheroid protocols for stubborn cell lines and co-cultures enables more physiologically relevant models for drug discovery and toxicology testing. The implementation of standardized, yet flexible protocols allows for the generation of high-quality spheroids compatible with advanced applications such as high-throughput drug screening [70], nanoparticle uptake studies [65], and toxicology assessment [69] [67].
Recent technological advances, including commercial kits designed specifically for RNA sequencing from 3D spheroid models [70], highlight the growing importance of robust spheroid generation protocols. Furthermore, the combination of 3D spheroid models with high-resolution fluorescence imaging provides real-time information on how nanomaterials and therapeutic agents interact with cells in a more physiologically relevant context [65].
The continued refinement of these protocols within the scaffold-based research framework will further bridge the gap between in vitro and in vivo data, enhancing the predictive value of preclinical models in drug development and disease modeling.
Best Practices for Spheroid Handling, Media Changes, and Transfer
Three-dimensional (3D) spheroid models have emerged as indispensable tools in biomedical research, bridging the critical gap between traditional two-dimensional (2D) cell cultures and in vivo studies. These sophisticated models better replicate the complex physiological relevance of native tissues by facilitating intricate cell-cell interactions and cell-extracellular matrix (ECM) communications that mirror the architectural and functional complexities of human tumors and tissues [6] [3]. The transition from 2D to 3D culture systems represents a paradigm shift in cancer research, drug development, and regenerative medicine, offering enhanced predictive value for clinical outcomes.
Within spheroids, cells self-organize into distinct microenvironments that closely mimic the conditions found in solid tumors. This organization generates nutrient gradients and oxygen tension variations that drive the formation of three functionally unique cellular zones: an outer proliferative layer, an intermediate quiescent region, and a hypoxic, apoptotic core [3]. This zonal architecture creates physiological barriers to drug penetration and efficacy that cannot be adequately modeled in conventional 2D systems, making spheroids particularly valuable for therapeutic screening applications [20]. Furthermore, the preservation of cancer stem cell (CSC) subpopulations within spheroids provides crucial insights into tumor initiation, progression, and therapeutic resistance mechanisms [71].
The growing adoption of spheroid models across diverse research domains—including personalized medicine, drug screening, and tissue engineering—has highlighted the necessity for standardized, reproducible methodologies [3] [18]. This technical guide outlines evidence-based best practices for spheroid handling, media changes, and transfer procedures, with particular emphasis on scaffold-based techniques that maintain the structural and functional integrity of these complex 3D microtissues throughout experimental workflows.
Core Methodologies and Workflows
Spheroid Formation and Culture
Spheroid formation employs either scaffold-based or scaffold-free approaches, with the selection dependent on specific research objectives and cell type requirements. Scaffold-based systems utilize natural or synthetic extracellular matrices (such as Matrigel or collagen) to provide structural support and biochemical cues that enhance spheroid development and maturation [48] [13]. These systems particularly benefit epithelial and tumor cells that require ECM engagement for optimal growth and function. In contrast, scaffold-free methods leverage ultra-low attachment (ULA) surfaces to promote cell self-assembly into spheroids through forced aggregation, making them ideal for high-throughput screening applications [3] [18].
The initial seeding density significantly influences spheroid morphology and growth kinetics. Research analyzing over 32,000 spheroids demonstrated that densities of 6,000-7,000 cells often produce the largest diameters but may compromise structural stability, leading to potential rupture and release of necrotic regions [72]. Lower seeding densities yield smaller, more compact spheroids with enhanced structural integrity, highlighting the importance of matching seeding parameters to specific experimental goals. Furthermore, different cell types exhibit distinct growth patterns; for instance, MCF-7 spheroids typically decrease in size over time, while HCT 116 spheroids show the opposite trend [72].
Media composition represents another critical variable in spheroid culture. Studies comparing common media formulations (DMEM, DMEM/F12, and RPMI 1640) have revealed significant differences in spheroid size, shape, and viability attributable to variations in glucose and calcium concentrations [72]. Similarly, serum concentration directly impacts structural integrity, with 10-20% fetal bovine serum (FBS) producing compact, viable spheroids with distinct necrotic and proliferative zones, while serum-free conditions often result in substantial shrinkage and cell detachment [72]. Environmental factors, particularly oxygen tension, further shape spheroid development, with hypoxic conditions (3% O₂) producing decreased dimensions, reduced viability, and lower ATP content—features that may better mimic the physiological conditions of solid tumors [72].
Routine Maintenance and Media Changes
Proper media change protocols are essential for maintaining spheroid health while minimizing mechanical disruption. The semi-permeable nature of spheroids creates diffisional limitations that necessitate careful attention to nutrient replenishment and waste removal. For spheroids cultured in ULA plates, partial media changes (typically 50-70% volume replacement) every 2-3 days effectively maintain metabolic homeostasis without disturbing fragile aggregates [71] [73]. The use of wide-bore pipette tips is strongly recommended to prevent accidental aspiration or structural damage during media exchange procedures.
Research indicates that media composition should be optimized for specific cell types and experimental objectives. For cancer stem cell enrichment and tumorsphere assays, defined serum-free formulations like Tumorsphere Medium XF support serial passage while maintaining stemness characteristics and chemoresistance properties [71]. Supplementation with specific factors such as ROCK inhibitor (Y-27632) has been shown to enhance stemness marker preservation and reduce premature differentiation in epithelial spheroid systems [13]. Additionally, the incorporation of extracellular matrix components like collagen I (at 3μg/mL final concentration) dramatically improves spheroid formation efficiency and structural consistency for certain cell lines, including MDA-MB-231 [73].
Table 1: Media Composition Optimization Guidelines
| Component | Recommended Concentration | Functional Impact | Application Examples |
|---|---|---|---|
| Fetal Bovine Serum (FBS) | 10-20% | Promotes compact, viable spheroids with distinct zones | MCF-7 spheroids for drug screening [72] [73] |
| Collagen I | 3μg/mL | Enhances spheroid formation efficiency | MDA-MB-231 breast cancer spheroids [73] |
| ROCK Inhibitor (Y-27632) | 10μM | Reduces dissociation-induced apoptosis, enhances stemness | Epithelial holosphere formation [13] |
| Physiological Oxygen | 3-5% O₂ | Mimics tumor microenvironment, reduces dimensions | Hypoxia modeling in tumor spheroids [72] |
Spheroid Handling and Transfer Techniques
The transfer of spheroids between vessels demands meticulous technique to preserve structural integrity. Gravity sedimentation represents the gentlest approach for harvesting spheroids from culture media; this involves allowing spheroids to settle by gravity for 10 minutes at room temperature before careful aspiration of supernatant, leaving approximately 200μL to prevent accidental spheroid loss [71]. For scaffold-embedded spheroids, mechanical dissociation must be performed judiciously using a P1000 pipette to break the ECM, followed by centrifugation at 1,000 × g at 4°C to pellet the spheroids [74].
The transfer of spheroids for subculturing or shipping requires additional protective measures. When preparing spheroids for transport to other laboratories, transferring them with fresh ECM to a T25 flask allows the matrix to solidify before filling the vessel completely with culture medium and securing the cap tightly [74]. This approach provides structural protection during transit and has demonstrated recovery rates of 95-100% upon receipt. For intra-laboratory transfer, resuspending spheroids in 2-4 times their volume of fresh ECM and mixing by pipetting up and down 10 times (while avoiding air bubble introduction) ensures uniform distribution before aliquoting 5-20μL of the mixture to new culture vessels [74].
Instrument selection critically influences spheroid viability during handling. Wide-bore or ice-cold tips (prepared by cutting standard tips with clean scissors) significantly reduce shear stress and adhesion during transfer procedures [48]. Pre-coating tubes with sterile 1% bovine serum albumin (BSA) in phosphate-buffered saline (PBS) overnight further minimizes spheroid attachment to plastic surfaces, thereby preserving morphological integrity [48]. For centrifugation steps, low relative centrifugal force (RCF) settings of 20 × g for 20 seconds effectively pellet spheroids without causing excessive compaction or damage [48].
Quantitative Analysis and Assessment
Spheroid Characterization and Quality Control
Comprehensive spheroid assessment requires multimodal evaluation of morphological, viability, and functional parameters. High-content image analysis using specialized software (AnaSP, ReViSP) enables quantitative measurement of critical metrics including diameter, circularity, compactness, and solidity [72]. These morphological parameters serve as important indicators of spheroid health and maturation state, with established correlations to physiological relevance. For instance, MCF-7 breast cancer spheroids typically exhibit mean diameters >150μm after 10-12 days of culture, with aggregates below 80μm generally excluded from analysis as they may not represent fully formed spheroids [71].
Viability assessment in spheroids presents unique challenges compared to 2D cultures due to diffisional limitations and zonal heterogeneity. The CellTiter-Glo 3D Cell Viability Assay provides sensitive, quantitative ATP measurements that correlate with metabolically active cell mass, while fluorescence-based approaches using dyes like calcein-AM (for live cells) and ethidium homodimer-1 (for dead cells) enable spatial visualization of viability patterns within the spheroid architecture [72] [73]. It is important to note that dye penetration limitations may affect accuracy in larger spheroids (>500μm diameter), necessitating extended incubation times or mechanical sectioning for comprehensive assessment.
The tumorsphere formation efficiency (TFE) assay offers a specialized approach for evaluating cancer stem cell frequency within heterogeneous populations. This quantitative method calculates the percentage of cells capable of forming spheres from a single cell, providing valuable insights into tumor aggressiveness and metastatic potential [71]. TFE values are determined by dividing the number of spheres formed by the total number of wells seeded and multiplying by 100, typically assessed after 7-12 days of culture under defined conditions [71].
Table 2: Spheroid Quality Control Parameters and Benchmarks
| Parameter | Measurement Method | Acceptance Criteria | Technical Considerations |
|---|---|---|---|
| Diameter | Brightfield microscopy with calibration | Cell line-specific (e.g., >150μm for MCF-7) | Size varies with seeding density and culture duration [71] [73] |
| Circularity | Automated image analysis (AnaSP, ReViSP) | >0.6 for uniform spheroids | Lower values indicate irregular morphology [13] |
| Viability | ATP quantification (CellTiter-Glo 3D) | >70% for healthy cultures | Correlates with metabolic activity [72] |
| Structural Integrity | Phase-contrast microscopy | Compact, defined borders | Necrotic cores normal in mature spheroids [72] |
| Tumorsphere Formation Efficiency (TFE) | Limiting dilution assay | Variable by cancer cell line | Indicator of cancer stem cell frequency [71] |
The Scientist's Toolkit: Essential Reagents and Materials
Successful spheroid culture requires specialized reagents and materials optimized for 3D applications. The following table summarizes critical components and their functions based on current protocols:
Table 3: Essential Research Reagent Solutions for Spheroid Culture
| Reagent/Material | Function | Example Products | Application Notes |
|---|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, promotes spheroid formation | Elplasia 96-well plates, BIOFLOAT plates, Corning ULA plates | Enables scaffold-free spheroid formation; choice depends on throughput needs [73] [13] |
| Basement Membrane Matrix | Provides ECM support for scaffold-based methods | Matrigel, Collagen I | Enhances spheroid formation efficiency; concentration affects stiffness [74] [48] [73] |
| Defined Serum-Free Media | Supports cancer stem cell maintenance | PromoCell 3D Tumorsphere Media XF | Enables serial passage while preserving stemness [71] |
| Dissociation Reagents | Gentle enzymatic dissociation for subculturing | TrypLE, Trypsin-EDTA | Preferred over mechanical dissociation for single-cell applications [71] [73] |
| Viability Assay Kits | 3D-optimized viability assessment | CellTiter-Glo 3D, LIVE/DEAD Viability/Cytotoxicity Kit | Specifically validated for dense 3D structures [72] [73] |
| ROCK Inhibitor | Reduces anoikis, enhances stem cell survival | Y-27632 | Critical for single-cell cloning efficiency in spheroid assays [13] |
Advanced Applications and Troubleshooting
Specialized Methodological Considerations
Immunofluorescence staining of spheroids presents unique challenges compared to 2D cultures, primarily due to limited antibody penetration into the core regions. A comprehensive protocol from Abcam recommends extended fixation (10 minutes in 4% paraformaldehyde at room temperature or 5 minutes in chilled 100% methanol at 4°C), followed by permeabilization with 0.5-10% Triton X-100 for one hour with constant gentle agitation [48]. For epitopes masked by formaldehyde-induced cross-linking, an additional heat-induced antigen retrieval step (20 minutes at 96-98°C in Tris/EDTA pH 9.0 or sodium citrate pH 6.0 buffer) significantly improves antibody binding efficiency [48]. All incubation steps—including blocking, antibody staining, and washing—should be performed overnight at room temperature with gentle mixing to ensure uniform reagent distribution throughout the spheroid architecture [48].
For drug screening applications, spheroids offer superior predictive value compared to 2D models but require specialized experimental design considerations. The gradient-dependent penetration of therapeutic agents creates distinct response patterns that more accurately mirror in vivo drug behavior [20]. A standardized drug screening protocol involves treating spheroids at specific developmental stages (typically when distinct zones have formed), using limited amounts of compounds to better simulate physiological drug exposure levels [20]. Endpoint analysis generally includes assessment of spheroid integrity, cell survival through enzymatic assays (such as acid phosphatase activity), and growth kinetics monitoring to determine treatment-induced delays and regrowth patterns, with typical experimental timelines extending to 14 days or longer [20].
Troubleshooting Common Challenges
Several recurrent challenges emerge in spheroid culture, each with specific corrective strategies:
- Structural Instability: Spheroid disintegration or excessive cell shedding often results from suboptimal serum concentration or mechanical disruption during handling. Increasing FBS to 10-20% promotes compact architecture, while using wide-bore tips and minimizing pipetting forces preserves structural integrity [72].
- Size Irregularity: High variability in spheroid dimensions frequently stems from inconsistent seeding densities or inadequate aggregation promotion. Centrifuging plates after seeding (290 × g for 3 minutes) enhances uniform cell aggregation, while using specialized ULA plates with microcavities (e.g., Elplasia plates) ensures consistent spheroid size and circularity [73] [13].
- Necrotic Core Expansion: While some central necrosis is expected in mature spheroids, excessively large necrotic cores may indicate overly dense cultures or insufficient nutrient exchange. Reducing seeding density or implementing more frequent partial media changes can ameliorate this issue without compromising spheroid maturity [3] [72].
- Poor Drug Penetration: Inadequate compound distribution throughout spheroids compromises screening validity. Extending treatment durations, using smaller spheroids (<300μm diameter), or incorporating penetration enhancers (subject to experimental constraints) improves core exposure to therapeutic agents [20].
Spheroid Workflow Diagram: Comprehensive experimental pipeline from design to analysis
The adoption of standardized methodologies for spheroid handling, media changes, and transfer is paramount for generating physiologically relevant, reproducible data in 3D cell culture systems. As the field continues to evolve, several key principles emerge as fundamental to success: meticulous attention to culture conditions (including media composition, oxygen tension, and serum concentration), implementation of gentle handling techniques (utilizing wide-bore tips and gravity sedimentation), and application of appropriate characterization methods (combining morphological, viability, and functional assessments). The systematic integration of these evidence-based practices across research laboratories will significantly enhance the reliability and translational impact of spheroid models in drug discovery, personalized medicine, and basic cancer biology.
Future methodological developments will likely focus on increasing throughput and standardization while preserving the physiological complexity that makes spheroid models so valuable. Emerging technologies such as automated image analysis, microfluidic platforms, and advanced bioreactor systems promise to address current limitations in scalability and reproducibility. Furthermore, the integration of patient-derived cells into standardized spheroid workflows will accelerate the implementation of these models in personalized medicine applications, ultimately enabling more predictive preclinical assessment of therapeutic efficacy and resistance mechanisms. Through continued refinement and standardization of spheroid culture methodologies, researchers can unlock the full potential of these sophisticated 3D models to bridge the gap between conventional in vitro systems and clinical reality.
The transition from traditional two-dimensional (2D) cell cultures to three-dimensional (3D) models represents a paradigm shift in biomedical research, particularly in the fields of cancer biology, drug discovery, and regenerative medicine. Unlike 2D monolayers, 3D spheroids are self-organizing cellular aggregates that better replicate the complex tissue architecture found in vivo, including critical cell-cell and cell-extracellular matrix interactions [6] [3]. These models recapitulate essential physiological features of human tissues, such as oxygen and nutrient gradients, which lead to the formation of distinct cellular zones: an outer proliferative layer, an intermediate quiescent region, and a hypoxic, sometimes necrotic, core [3]. This architectural complexity more accurately mimics the tumor microenvironment and tissue biology, making spheroids invaluable for predicting drug responses and studying disease mechanisms.
The growing adoption of 3D spheroid models is driven by their enhanced physiological relevance and improved translational potential compared to conventional 2D systems [3]. While 2D cultures remain useful for high-throughput screening due to their simplicity and cost-effectiveness, they often fail to accurately predict in vivo drug efficacy and toxicity because they lack the spatial organization and microenvironmental pressures of real tissues [3] [75]. Spheroids bridge this gap by providing a more representative platform for studying tumor biology, drug penetration, and resistance mechanisms [75]. Within the context of scaffold-based techniques, spheroids can be embedded in matrices such as Matrigel to study invasive behavior and stem cell dynamics, further enhancing their physiological relevance for regenerative medicine applications [13].
Viability Assessment in 3D Spheroid Models
Core Principles and Methodologies
Accurately determining cell viability in 3D spheroids presents unique challenges distinct from 2D cultures, primarily due to limited reagent penetration and the presence of heterogeneous cellular zones. Viability assays must account for this spatial heterogeneity and the diffusion barriers inherent to compact 3D structures. Optimized protocols are essential to generate reliable, reproducible data that truly reflects cellular health within the spheroid architecture.
Multiplexed approaches that combine multiple fluorescent dyes provide the most comprehensive assessment of spheroid viability. These assays enable simultaneous quantification of live, dead, and apoptotic cells throughout the entire spheroid structure, offering superior information content compared to single-endpoint measurements [75]. For live-cell imaging and tracking viability over time, fluorescent protein-expressing cell lines can be utilized to monitor spheroid size and intensity changes without the need for fixation or staining [75].
Standardized Viability Assay Protocols
Multiplexed Viability and Cytotoxicity Staining: The following protocol, adapted from high-content screening methodologies, enables multiparametric viability assessment in 3D spheroids [75]:
- Preparation: Culture spheroids in low-attachment U-bottom 96-well or 384-well plates to promote consistent spheroid formation.
- Treatment: Apply experimental compounds for desired duration (typically 3-7 days for drug screening), with media changes every 2-3 days.
- Staining: Prepare a dye mixture containing 2 μM calcein AM (viable cells), 3 μM ethidium homodimer-1 (EthD-1, dead cells), and 33 μM Hoechst 33342 (all nuclei) in sterile phosphate-buffered saline (PBS).
- Incubation: Add dye solution directly to culture media without aspiration. Incubate for 3 hours at 37°C to ensure adequate dye penetration into spheroid core.
- Imaging: Acquire z-stack images using automated microscopy systems. For analysis, use maximum projection images of confocal stacks.
Apoptosis Detection Using Caspase 3/7 Activation: For specific detection of apoptotic cells within spheroids [75]:
- Staining Solution: Prepare 7.5 μM CellEvent Caspase-3/7 reagent and 10 μM Hoechst nuclear dye in Hank's Balanced Salt Solution.
- Incubation: Add solution directly to spheroid culture and incubate for 2-3 hours at 37°C protected from light.
- Processing: Image without washing to prevent spheroid disruption. Compatible with subsequent fixation if required.
Metabolic Viability Assay (Pre-staining): For measurement of reactive oxygen species in live spheroids prior to fixation [76]:
- Dye Preparation: Add CellROX Green reagent to culture media for a final concentration of 5 μM.
- Incubation: Incubate for 2 hours at room temperature with gentle agitation, protected from light.
- Washing: Wash spheroids 3 times with PBS, centrifuging at 500 g for 5 minutes between washes.
- Fixation: Proceed with fixation for compatible secondary staining or image immediately for live-cell analysis.
Table 1: Viability Assay Reagents and Applications
| Assay Type | Key Reagents | Detection Method | Information Obtained |
|---|---|---|---|
| Viability/ Cytotoxicity | Calcein AM, EthD-1, Hoechst 33342 | Fluorescence microscopy | Live/dead cell quantification, spatial distribution |
| Apoptosis | CellEvent Caspase-3/7, Hoechst | Fluorescence microscopy | Early and late apoptosis activation |
| Metabolic Activity | CellROX Green | Fluorescence microscopy | Reactive oxygen species production |
| Proliferation | Click-iT EdU | Fluorescence microscopy | DNA synthesis in proliferating cells |
Staining Protocols for 3D Spheroids
Optimization Strategies for 3D Staining
The structural density of 3D spheroids presents significant challenges for staining protocols optimized for 2D cultures. Successful staining of spheroids requires specific adaptations to ensure adequate antibody penetration and uniform labeling throughout the entire structure. Key considerations include extending incubation times, using specialized buffers to enhance reagent penetration, and physically modifying protocols to prevent spheroid damage [76].
For spheroids up to 500 microns in thickness, the following adaptations are critical: cut pipette tips to widen openings and prevent shearing of spheroids during fluid handling; optimize primary antibody concentrations through titration (testing serial dilutions from 1:10 to 1:1000); and increase incubation times for both primary and secondary antibodies, typically extending to overnight incubations at room temperature with gentle agitation [76]. Thicker spheroids may require even higher antibody concentrations and longer incubation times to achieve complete penetration.
Comprehensive Immunostaining Protocol
The following detailed protocol provides a robust framework for immunostaining of 3D spheroids, incorporating critical steps to overcome penetration barriers [76]:
Fixation and Permeabilization:
- Centrifugation: Centrifuge spheroid samples at 500 g for 5 minutes. Gently remove cell culture media without disturbing the spheroid pellet.
- Washing: Wash spheroids once with cold PBS. Centrifuge at 500 g for 5 minutes and remove supernatant.
- Fixation: Add 4% paraformaldehyde in a volume approximately 10 times the volume of the spheroid tissue. Ensure complete submersion of spheroids in fixative. Fix for 1 hour at room temperature with gentle agitation.
- Permeabilization: Permeabilize spheroids by incubating with a penetration buffer (e.g., CytoVista Antibody Penetration Buffer) for 15 minutes at room temperature with gentle agitation.
- Blocking: Block samples with a specialized blocking buffer (e.g., CytoVista Blocking Buffer) for 2 hours at 37°C with gentle agitation.
Antibody Labeling:
- Primary Antibody: Incubate spheroids with primary antibodies diluted in antibody dilution buffer (e.g., CytoVista Antibody Dilution Buffer) overnight at room temperature with gentle agitation.
- Washing: Wash samples 3 times with wash buffer (e.g., CytoVista Wash Buffer), centrifuging at 500 g for 5 minutes between washes.
- Secondary Antibody: Incubate with fluorescently-labeled secondary antibodies prepared in antibody dilution buffer overnight at room temperature with gentle agitation.
- Nuclear Counterstaining: Add 1 drop of NucBlue (DAPI) per mL of sample or 300 nM DAPI solution. Incubate for 30 minutes at room temperature with gentle agitation.
- Final Washes: Wash sample 3 times with wash buffer, centrifuging at 500 g for 5 minutes between washes.
Mounting and Clearing:
- Mounting: For imaging, pipette spheroids onto a microscope slide or glass-bottom dish. Add 1-3 drops of non-curing glass mountant (e.g., SlowFade Glass).
- Clearing: For enhanced imaging clarity, especially in thicker spheroids, consider using commercial clearing reagents (e.g., CytoVista 3D Cell Culture Clearing reagents) to improve light penetration and reduce scattering.
Diagram 1: 3D spheroid staining and imaging workflow
Advanced Imaging Techniques for 3D Models
Image Acquisition Strategies
Advanced imaging approaches are essential for extracting meaningful data from 3D spheroids due to their substantial volume and optical density. Z-stack acquisition - capturing multiple focal planes at different depths through the spheroid - represents the foundational technique for comprehensive 3D imaging [75]. These z-stacks can then be processed using maximum projection algorithms that combine information from all slices into a single 2D image, facilitating efficient comparison of different spheroid phenotypes while preserving 3D structural information [75].
Both widefield and confocal microscopy systems can be effectively employed for spheroid imaging, with distinct advantages for each approach. Widefield systems offer faster acquisition times and are suitable for lower resolution screening applications, while confocal microscopy provides superior optical sectioning by eliminating out-of-focus light, resulting in clearer images of internal structures [75]. For most applications, 10x or 20x objectives provide an optimal balance between resolution and field of view, enabling capture of entire spheroids in single images while maintaining cellular-level detail. Typical z-stacks for spheroid imaging cover 100-200 μm, approximately encompassing the lower half of each spheroid [75].
Image Analysis and Data Extraction
Robust image analysis methodologies transform raw image data into quantifiable biological insights. Automated analysis pipelines can extract multiple parameters from spheroid images, including spheroid size (diameter, cross-sectional area), morphology (circularity, shape descriptors), and cellular composition (viability counts, marker expression) [75]. These multiparametric outputs enable comprehensive characterization of complex phenotypes in response to experimental treatments.
For high-content screening applications, customized analysis algorithms first identify the spheroid boundary using nuclear staining, then segment individual cells based on membrane or cytoplasmic markers [75]. This approach enables simultaneous quantification of marker-specific cell numbers, viability metrics, and spatial distribution patterns within different spheroid regions. The resulting data can be used to generate concentration-response curves and calculate IC50 values for drug compounds, providing more physiologically relevant potency measures compared to 2D cultures [75].
Table 2: Imaging Platforms and Analysis Methods for 3D Spheroids
| Imaging Platform | Optimal Magnification | Key Features | Compatible Analysis Software |
|---|---|---|---|
| Confocal Microscope | 10x, 20x | Optical sectioning, reduced out-of-focus light | MetaXpress, Celleste |
| Widefield Microscope | 4x, 10x | Faster acquisition, larger field of view | MetaXpress, ImageJ |
| High-Content Screening System | 4x, 10x, 20x | Automated multi-well imaging | MetaXpress, Custom Modules |
Diagram 2: Image analysis workflow for 3D spheroid characterization
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for 3D Spheroid Analysis
| Category | Specific Product/Kit | Manufacturer | Primary Function |
|---|---|---|---|
| Cell Culture Plates | Nunclon Sphera 96-well plates | Thermo Fisher | Scaffold-free spheroid formation |
| Cell Culture Plates | Elplasia 96-well microcavity plates | Corning | High-throughput uniform spheroid generation |
| Cell Culture Plates | BIOFLOAT 96-well U-bottom plates | Sarstedt | Scalable spheroid production |
| Fixation Reagent | 4% paraformaldehyde | Various | Tissue preservation and structural maintenance |
| Permeabilization Buffer | CytoVista Antibody Penetration Buffer | Thermo Fisher | Enhances antibody penetration into spheroids |
| Blocking Buffer | CytoVista Blocking Buffer | Thermo Fisher | Reduces non-specific antibody binding |
| Antibody Dilution | CytoVista Antibody Dilution Buffer | Thermo Fisher | Optimizes antibody performance in 3D samples |
| Wash Buffer | CytoVista Wash Buffer | Thermo Fisher | Removes unbound antibodies effectively |
| Viability Staining | LIVE/DEAD Viability/Cytotoxicity Kit | Thermo Fisher | Simultaneously labels live and dead cells |
| Apoptosis Detection | CellEvent Caspase-3/7 Reagent | Thermo Fisher | Detects activated caspase 3/7 in apoptotic cells |
| Nuclear Staining | NucBlue Fixed Cell ReadyProbes (DAPI) | Thermo Fisher | Counterstains all nuclei for spatial reference |
| Mounting Medium | SlowFade Glass Soft-set Antifade Mountant | Thermo Fisher | Preserves fluorescence during imaging |
| Clearing Reagents | CytoVista 3D Cell Culture Clearing Kit | Thermo Fisher | Enhances light penetration for improved imaging |
The optimization of viability assessment, staining protocols, and imaging techniques for 3D spheroid models is essential for generating physiologically relevant data in cancer research, drug discovery, and regenerative medicine. By implementing the standardized methodologies outlined in this technical guide - including multiplexed viability assays, enhanced immunostaining protocols with specialized buffers, and advanced 3D image acquisition techniques - researchers can overcome the unique challenges presented by these complex tissue models. The integration of scaffold-based approaches further enhances the physiological relevance of spheroid systems, particularly for studying stem cell dynamics and regenerative applications [13]. As the field continues to advance, these optimized assays will play an increasingly critical role in bridging the gap between in vitro models and in vivo physiology, ultimately accelerating the development of more effective therapeutic strategies.
Benchmarking Performance: Validating Scaffold-Based Models Against Other Platforms
The transition from traditional two-dimensional (2D) cell culture to three-dimensional (3D) models represents a paradigm shift in biomedical research, particularly in the study of cancer biology and drug development. 3D spheroid models have emerged as invaluable tools that bridge the gap between conventional monolayer cultures and in vivo systems by more accurately recapitulating the complex tissue microenvironment found in native tissues [3]. These self-organizing cellular aggregates develop critical architectural features such as nutrient and oxygen gradients, which lead to the formation of distinct cellular zones comprising proliferating, quiescent, and necrotic cells—characteristics that closely mimic the physiology of solid tumors [3].
The drive toward more physiologically relevant in vitro models is largely motivated by the stark discrepancies between preclinical drug testing results and clinical trial outcomes, which have contributed to declining drug approval rates over recent decades [9]. While 3D cell culture systems significantly advance our ability to capture crucial cell-cell and cell-extracellular matrix interactions, the lack of integrated perfusion systems remains a limitation in fully replicating the dynamic tissue microenvironment [9]. Within this context, various techniques for generating 3D spheroids have been developed, each with distinct advantages and limitations.
This technical guide provides an in-depth comparative analysis of three prominent spheroid generation techniques: scaffold-based methods, the hanging drop technique, and the use of ultra-low attachment (ULA) plates. Framed within the broader research on scaffold-based techniques, this review examines the fundamental principles, experimental protocols, and applications of each method, providing researchers with the necessary information to select the most appropriate methodology for their specific investigations in cancer research and drug discovery.
Fundamental Principles of 3D Spheroid Models
Architectural and Physiological Features of Spheroids
Spheroids are defined as spherical cellular aggregates that form through the self-assembly of cells, typically ranging in size from 100 to 500 micrometers in diameter [3]. Their significant advantage over 2D cultures lies in their ability to establish physiological gradients that mirror those found in avascular regions of solid tumors. As spheroids increase in size, they develop three distinct concentric zones that contribute to their physiological relevance:
- Proliferative Outer Layer: Composed of rapidly dividing cells with direct access to oxygen and nutrients from the culture medium [3].
- Quiescent Intermediate Layer: Consisting of viable but non-dividing cells in a state of growth arrest due to limited nutrient availability [3].
- Hypoxic/Necrotic Core: Characterized by apoptotic or necrotic cells resulting from severe oxygen and nutrient deprivation, along with accumulated waste products [3].
This zonal architecture replicates the heterogeneous microenvironment of solid tumors, which is critical for studying tumor progression, metastasis, and therapeutic resistance mechanisms [3]. The presence of these distinct cellular compartments enables more accurate modeling of drug penetration barriers and metabolic heterogeneity observed in vivo.
The Critical Role of the Extracellular Matrix
In native tissues, cells exist within a complex extracellular matrix (ECM) that provides structural support and biochemical signals crucial for cellular function. While scaffold-free methods like hanging drop and ULA plates rely on cells to secrete their own ECM components, scaffold-based approaches provide a pre-formed synthetic or natural matrix that more directly mimics this physiological environment [67].
The ECM in 3D models influences critical cellular processes including:
- Cell signaling pathways and communication
- Cell growth and proliferation patterns
- Gene and protein expression profiles
- Drug response mechanisms and resistance development [77]
Scaffold-based systems particularly excel in providing this ECM-like environment, making them especially valuable for tissue engineering applications and studies requiring enhanced structural support for larger tissue constructs [67].
Scaffold-Based Techniques
Working Principles
Scaffold-based techniques utilize three-dimensional supporting materials that mimic the native extracellular matrix (ECM), providing both structural support and biochemical cues that influence cellular behavior [67]. These systems can be broadly categorized into several types:
- Hydrogel-based scaffolds: Composed of water-swollen polymer networks, often derived from natural materials (e.g., Matrigel, alginate, collagen) or synthetic sources [67] [78]. These represent the most popular scaffold type due to their close resemblance to the native ECM.
- Biopolymer scaffolds: Made from biological polymers such as collagen or gelatin, which can be impregnated with growth factors, hormones, or drugs to enhance functionality [78].
- Hard polymer scaffolds: Constructed from synthetic materials including ceramics, glass, or metals, primarily used in tissue engineering applications [78].
These scaffolds create a synthetic microenvironment that facilitates cell-matrix interactions and enables the formation of larger tissue constructs than those achievable with scaffold-free methods [67]. The porous nature of scaffolds allows for the efficient transport of nutrients, oxygen, and signaling molecules while providing extensive surface area for cellular attachment and growth [78].
Experimental Protocol
Materials Required:
- Scaffold material (e.g., Matrigel, AlgiMatrix, collagen-based hydrogels)
- Cell culture plate (multi-well format)
- Cell suspension of interest
- Culture medium appropriate for cell type
- Pipettes and tips
Step-by-Step Procedure:
- Scaffold Preparation: For hydrogel systems, prepare the liquid scaffold material according to manufacturer specifications. For pre-formed scaffolds, hydrate according to protocol.
- Cell-Seeding:
- For hydrogels: Mix cell suspension with liquid scaffold material at desired density (e.g., 0.5-5.0 × 10⁴ cells/mL).
- For pre-formed scaffolds: Apply cell suspension directly onto the scaffold surface.
- Solidification: For temperature-sensitive hydrogels, incubate at 37°C for 30-60 minutes to promote gelation.
- Culture Maintenance: Carefully add culture medium without disrupting the scaffold matrix. Refresh medium every 2-3 days.
- Monitoring: Observe spheroid formation and growth microscopically over 3-21 days, depending on experimental requirements.
The specific scaffold composition, pore size, and mechanical properties can be tailored to match the physiological characteristics of the tissue being modeled [67].
Hanging Drop Technique
Working Principles
The hanging drop method relies on gravity to force cellular aggregation within inverted droplets of cell suspension [77]. This technique creates a confined environment where cells naturally settle to the bottom of the droplet and self-assemble into spheroids through cell-cell adhesion mechanisms. The method leverages surface tension to maintain droplet integrity while the inverted orientation prevents cell attachment to substrate surfaces.
This approach enables precise control over initial cell numbers per spheroid, resulting in highly uniform spheroid sizes and reproducible architectures [79] [77]. The hanging drop platform also facilitates direct visualization of spheroid formation and growth, allowing researchers to monitor developmental progress without disturbing the culture.
Experimental Protocol
Materials Required:
- Hanging drop plates or standard culture plates with lids
- Cell suspension
- Culture medium
- Multichannel pipette
- PBS for maintaining humidity
Step-by-Step Procedure:
- Cell Suspension Preparation: Create a cell suspension at the desired density (typically 1.0-5.0 × 10⁴ cells/mL) in appropriate culture medium.
- Droplet Generation:
- Using a multichannel pipette, deposit 15-25 µL droplets of cell suspension onto the underside of a culture plate lid.
- For standardized systems, use specialized hanging drop plates with molded wells.
- Inversion and Incubation: Carefully invert the lid and place it over a base plate containing PBS to maintain humidity.
- Spheroid Formation: Incubate plates for 48-72 hours to allow spheroid assembly.
- Spheroid Transfer: After formation, carefully transfer spheroids to ultra-low attachment plates for long-term culture using wide-bore pipette tips.
- Culture Maintenance: Refresh medium every 2-3 days, monitoring spheroid morphology and size.
The protocol has been successfully adapted for various cell types, including primary pre-adipocytes, cancer cells, and stem cells [79] [77].
Ultra-Low Attachment Plates
Working Principles
Ultra-low attachment (ULA) plates feature specially treated surfaces that prevent cellular adhesion, thereby forcing cells to aggregate and form spheroids [80]. These plates are coated with a stable, non-cytotoxic, ultra-hydrophilic polymer that is covalently bound to the well surface, creating a non-adhesive environment that minimizes protein absorption and subsequent cell attachment [80].
The U-bottom design of these plates promotes the natural self-assembly of cells into a single, centrally located spheroid per well through spontaneous aggregation [80]. This design facilitates the formation of compact, uniform spheroids with consistent roundness and circularity parameters that can be quantitatively assessed to ensure quality control.
Experimental Protocol
Materials Required:
- Ultra-low attachment plates (U-bottom design recommended)
- Cell suspension
- Culture medium
- Pipettes and tips
Step-by-Step Procedure:
- Cell Suspension Preparation: Create a single-cell suspension at the optimal density for your cell type (typically 0.5-5.0 × 10⁴ cells/mL, depending on desired spheroid size).
- Plate Seeding:
- Aliquot cell suspension into ULA plate wells (100-200 µL per well for 96-well format).
- For high-throughput applications, use automated liquid handling systems.
- Spheroid Formation:
- Centrifuge plates at low speed (100-200 × g) for 5-10 minutes to encourage initial cell contact (optional).
- Incubate plates for 24-72 hours to allow spheroid formation.
- Culture Maintenance:
- Refresh medium carefully every 2-3 days using slow pipetting to avoid disrupting spheroids.
- For long-term cultures, monitor medium pH and nutrient depletion.
- Analysis: Image spheroids directly in plates using brightfield or fluorescence microscopy.
The optimized surface chemistry of ULA plates supports long-term spheroid culture while maintaining viability and structural integrity [80].
Technical Comparison of Methodologies
Comparative Analysis of Key Parameters
Table 1: Technical comparison of spheroid formation methods
| Parameter | Scaffold-Based | Hanging Drop | Ultra-Low Attachment Plates |
|---|---|---|---|
| Principle | Cells embedded in or seeded on 3D matrix | Gravity-forced aggregation in inverted droplets | Spontaneous aggregation on non-adhesive surfaces |
| Spheroid Uniformity | Moderate to low | High | High |
| Throughput Capacity | Moderate | Low without automation | High |
| Ease of Use | Moderate | Low (labour-intensive) | High |
| Cost Factors | High (specialized materials) | Low to moderate | Moderate |
| Special Equipment | Possibly | Yes (special plates) | No |
| Cell Recovery | Difficult | Moderate | Easy |
| Assay Compatibility | Moderate | Low | High |
| Size Control | Moderate | High (via cell density) | High (via cell density) |
| Commercial Availability | Multiple vendors | Limited vendors | Multiple vendors |
| Reproducibility | Batch-dependent for natural scaffolds | High | High |
| Direct Imaging | Challenging | Possible | Excellent |
Quantitative Experimental Data
Table 2: Experimental performance metrics based on published studies
| Method | Optimal Spheroid Size Range | Formation Time | Reproducibility Rate | Drug Screening Compatibility |
|---|---|---|---|---|
| Scaffold-Based | 200-600 μm | 3-14 days | Variable | Moderate |
| Hanging Drop | 300-500 μm | 48-72 hours | ~90% [9] | Low to moderate |
| Ultra-Low Attachment Plates | 300-500 μm | 24-72 hours | High [80] | High |
Table 3: Experimental results from comparative drug screening study [81]
| Culture Method | IC50 Doxorubicin (μg/mL) | Cell Viability | Proliferation Rate | Metabolic Activity |
|---|---|---|---|---|
| 2D Monolayer | 0.39-0.43 | Low | High | High |
| Hanging Drop (3D) | 0.83 | High | Reduced | Reduced |
| ULA Plates (3D) | 1.00 | High | Reduced | Reduced |
Research Applications & Case Studies
Application-Specific Method Selection
Each spheroid formation technique offers distinct advantages for specific research applications:
Scaffold-Based Methods are particularly valuable for:
- Tissue engineering and regenerative medicine applications [77]
- Studies requiring enhanced ECM interactions and mechanical signaling [67]
- Long-term culture systems requiring structural support
- Modeling tissues with complex architectural organizations
Hanging Drop Technique excels in:
- Generating highly uniform spheroids for standardized assays [79]
- Co-culture systems with multiple cell types [77]
- Applications requiring precise control over initial cell numbers
- Studies where direct visualization of formation is beneficial
ULA Plates are ideal for:
- High-throughput drug screening applications [81] [80]
- Toxicology studies and compound libraries [67]
- Long-term maintenance of established spheroid cultures
- Automated imaging and analysis workflows
Case Study: Bladder Cancer Spheroids for Drug Screening
A comparative study using RT4 human bladder cancer cells demonstrated significant differences between 2D and 3D culture models, as well as between different 3D methodologies [81]. Researchers generated spheroids using both hanging drop and ULA plate methods, then evaluated their response to the chemotherapeutic agent doxorubicin.
Key findings included:
- Both 3D methods produced spheroids with smooth surfaces and round shapes within approximately 48 hours.
- Reduced cell growth and metabolism was observed in 3D cultures compared to 2D monolayers.
- The optimal spheroid diameter range of 300-500 μm was achieved using different seeding concentrations for each method.
- Enhanced drug resistance was observed in 3D spheroids, with IC50 values for doxorubicin approximately 2-2.5 times higher than in 2D cultures.
- The forced floating method using ULA plates was determined to be more suitable and straightforward for generating spheroids for drug screening applications [81].
This case study highlights how the choice of 3D culture methodology can significantly impact experimental outcomes, particularly in drug sensitivity testing.
Case Study: Adipose Spheroids for Metabolic Research
Research in metabolic diseases has benefited from 3D spheroid models, as demonstrated by a study generating adipose spheroids from human and mouse pre-adipocytes using the hanging drop method [79]. This scaffold-free approach enabled investigators to create uniform spheroids that exhibited morphological and physiological behaviors mimicking in vivo adipose tissue.
Notable outcomes included:
- Successful generation of hundreds of 3D adipose spheroids from multiple cell sources.
- Development of unilocular lipid droplets characteristic of mature white adipocytes, a feature not typically observed in 2D cultures.
- Enhanced adiponectin secretion in 3D spheroids compared to 2D cultures, indicating improved functional differentiation.
- Retention of brown adipose tissue (BAT) markers in spheroids derived from BAT sources.
- Responsiveness to environmental toxins and pro-inflammatory stimuli, demonstrating utility for metabolic disease modeling and toxicology studies [79].
This application illustrates how the hanging drop method can successfully maintain tissue-specific functionality for specialized research applications.
Research Reagent Solutions
Table 4: Essential research reagents and materials for spheroid generation
| Product Category | Specific Examples | Key Function | Application Notes |
|---|---|---|---|
| Ultra-Low Attachment Plates | Millicell ULA Plates, Corning Spheroid Microplates, Nunclon Sphera | Prevent cell attachment to promote spheroid formation | Ideal for high-throughput screening; compatible with imaging [80] |
| Hanging Drop Systems | Perfecta3D Hanging Drop Plates, InSphero GravityPLUS | Facilitate spheroid formation in inverted droplets | Excellent for uniformity; suitable for co-culture studies [79] [77] |
| Scaffold Materials | Matrigel, AlgiMatrix, Coregel | Provide 3D extracellular matrix environment | Mimic native tissue microenvironment; support complex structures [67] [78] |
| Hydrogel Systems | Corning Matrigel, ThermoFisher AlgiMatrix | Synthetic or natural polymer networks for cell embedding | Batch-to-batch variability can affect reproducibility [67] |
| Specialized Media | Pre-adipocyte differentiation media, Spheroid formation media | Support cell viability and function in 3D format | Composition varies by cell type and application [79] |
Methodological Workflows
The comparative analysis of scaffold-based, hanging drop, and ultra-low attachment plate methods for spheroid formation reveals a nuanced landscape where methodological selection must be guided by specific research objectives and practical constraints. Each technique offers distinct advantages: scaffold-based systems provide enhanced ECM mimicry and structural support for complex tissue models, the hanging drop method delivers exceptional spheroid uniformity ideal for standardized assays, and ULA plates offer high-throughput compatibility essential for drug discovery pipelines.
The growing emphasis on physiological relevance in preclinical research continues to drive adoption of 3D spheroid models across diverse applications. As the field advances, standardization of protocols and rigorous comparative validation will be essential for maximizing the translational potential of these powerful experimental platforms. Future developments in vascularization techniques, advanced biomaterials, and integrated analytical methods will further enhance the utility of spheroid models in both basic research and drug development contexts.
Three-dimensional (3D) spheroid models have revolutionized the preclinical evaluation of drug response and chemoresistance by offering a more physiologically relevant alternative to traditional two-dimensional (2D) cultures. These scaffold-free cellular aggregates better replicate the in vivo cellular microenvironments of complex tissues, promoting more intricate cell-cell and cell-extracellular matrix (ECM) interactions critical for accurate drug assessment [6]. The architectural complexity of spheroids leads to the development of nutrient, oxygen, and metabolic gradients that mimic the heterogeneous microenvironment of solid tumors, including the development of proliferative outer layers, quiescent intermediate zones, and hypoxic, apoptotic cores [3]. This physiological relevance makes spheroids invaluable for studying tumor progression, metastasis, and—most importantly—resistance to therapies, thereby addressing a critical gap in conventional drug screening approaches [3].
The transition from 2D to 3D models represents a paradigm shift in cancer research and drug development. While 2D monolayer cultures have served as the cornerstone of in vitro research for decades due to their simplicity and adaptability to high-throughput screening, they fail to replicate the complexity of the tumor microenvironment [3]. Cells grown in 2D often exhibit altered morphology, gene expression, and behavior compared to their in vivo counterparts, limiting their predictive value for clinical outcomes [3]. In contrast, 3D spheroid models provide a platform that bridges the gap between conventional cell cultures and in vivo studies, enabling more accurate predictions of drug efficacy and resistance mechanisms [82] [83].
Key Advantages of Spheroid Models for Drug Response Assessment
Physiological Relevance and Predictive Value
The enhanced biological relevance of 3D spheroids translates directly to improved predictive value in drug screening. Significant evidence demonstrates that in vitro three-dimensional tumor cell cultures more accurately reflect the complex in vivo microenvironment than simple two-dimensional cell monolayers, particularly with respect to gene expression profiles, signaling pathway activity, and drug sensitivity [82]. This fidelity enables researchers to identify differential sensitivities to targeted agents between 2D and 3D cultures, with some compounds showing enhanced potency against cell migration and invasion compared to proliferation—suggesting their preferential utility in metastatic disease [82].
The ability of spheroids to model therapeutic resistance represents one of their most valuable applications. The heterogeneous cellular zones within spheroids—including quiescent and hypoxic regions—replicate the conditions that foster chemoresistance in solid tumors [3]. This allows for the identification of new therapeutic targets and the testing of tumor microenvironment (TME)-targeted therapies that might be missed in conventional 2D screens [83]. Furthermore, the incorporation of multiple cell types, such as cancer-associated fibroblasts (CAFs), endothelial cells (ECs), immune cells, and even gut bacteria in colorectal cancer models, creates heterotypic systems that better mimic the in vivo regulation of signaling pathways and their influence on chemoresistance [83].
Technical Advancements and Standardization
Recent methodological advances have addressed previous limitations in spheroid-based assays, making them more accessible for routine preclinical studies. Standardized microplate methods now enable high-throughput capabilities with desirable characteristics including 96-well suspension culture formats, single spheroid per well centered for ease of optical imaging, high reproducibility, simple harvesting for further analysis, and fully automated imaging and quantitative analysis [82]. The utilization of ultra-low attachment (ULA) 96-well round-bottomed plates has significantly improved reproducibility, with intraplate coefficients of variation (CV) for spheroid volumes ranging from approximately 5% to 11% for various cancer cell lines [82].
Automated imaging systems, such as the Celigo cytometer, have further enhanced the utility of spheroid models by enabling rapid, routine imaging and analysis. These systems can scan a ULA 96-well plate in approximately 8 minutes, allowing fast, automated multiparametric analysis including measurements of spheroid diameter, perimeter, and area [82]. This technological advancement supports the generation of robust growth curves and facilitates dynamic monitoring of drug responses over time, significantly increasing throughput without compromising data quality.
Quantitative Parameters for Assessing Drug Response
The evaluation of drug response in spheroid models requires multidimensional assessment across various parameters that collectively provide a comprehensive picture of compound efficacy and mechanisms of action. The table below summarizes the key quantitative metrics used in these analyses.
Table 1: Key Quantitative Parameters for Assessing Drug Response in Spheroid Models
| Parameter Category | Specific Metrics | Significance in Drug Assessment |
|---|---|---|
| Spheroid Viability & Growth | Spheroid volume, diameter, area [82] | Measures overall anti-proliferative effects and growth inhibition |
| Metabolic activity (e.g., ATP levels) [82] | Assesses cellular viability and metabolic inhibition | |
| Necrotic core area/ratio [3] | Evaluates compound penetration and toxicity in inner regions | |
| Spheroid Integrity & Morphology | Spheroid compactness [82] | Indicates structural stability and cell-cell adhesion |
| Perimeter irregularity [82] | May indicate invasive potential or response to treatment | |
| Cell Fate & Death | Apoptosis markers (e.g., caspase activation) [48] | Distinguishes mechanisms of cell death |
| Proliferation markers (e.g., Ki-67) [48] | Identifies effects on cell division in specific zones | |
| Invasion & Migration | Invasion area/distance into matrix [82] | Critical for assessing anti-metastatic potential |
| Cell motility parameters [82] | Quantifies effects on migratory behavior |
These parameters can be evaluated using a combination of brightfield imaging, fluorescence-based assays, and immunohistochemical techniques. The specific choice of metrics depends on the research questions, compound mechanisms, and available analytical capabilities. The integration of multiple parameters provides a systems-level understanding of drug effects that surpasses what is possible with simple viability assays in 2D cultures.
Experimental Workflow for Drug Response Assessment
A standardized workflow for evaluating drug response in spheroid models ensures reproducibility and meaningful interpretation of results. The following diagram illustrates the key stages in this process:
Diagram 1: Experimental workflow for drug response assessment using spheroid models
Spheroid Generation and Maturation
The initial phase of spheroid generation requires careful selection of methodology based on cell type and research objectives. Among seeding methodologies, forced-floating and scaffold-based methods predominate, demonstrating reliability and versatility in spheroid generation [3] [18]. Other techniques, including microfluidics, bioprinting, hanging drop, and suspension culture also play significant roles, each with distinct advantages and limitations [3] [18]. The use of ultra-low attachment (ULA) 96-well round-bottomed plates has emerged as a particularly effective approach, as the well shape promotes the formation of single, centrally located spheroids of reproducible size without requiring additional coating steps [82].
Optimal seeding densities must be established empirically for each cell line to ensure spheroids fall within an appropriate size range (typically 300-500 μm in diameter) for initiating experimental studies [82]. The maturation period typically ranges from 3-7 days, during which spheroids develop their characteristic zonal architecture with proliferative outer layers, quiescent intermediate zones, and hypoxic cores [3]. This maturation is essential for establishing the physiological gradients that influence drug penetration and efficacy.
Drug Treatment and Incubation
Following quality control to verify appropriate size and morphology uniformity, spheroids are exposed to therapeutic compounds according to experimental design. Treatment regimens should include appropriate controls and a range of concentrations to establish dose-response relationships. The incubation period following drug exposure typically ranges from 24 to 168 hours, depending on the specific research questions and compound mechanisms [82]. During this period, maintenance protocols such as replacing 50% of the medium on days 4, 7, 10, and 12 may be implemented for longer-term studies [82].
Analytical Techniques for Functional Validation
Imaging and Morphological Analysis
Advanced imaging technologies form the cornerstone of spheroid-based drug assessment. Automated imaging systems, such as the Celigo cytometer, enable high-throughput, quantitative analysis of spheroid growth and morphology [82]. These systems utilize brightfield or fluorescent illumination to capture high-quality images that can be analyzed using specialized applications to measure parameters including spheroid diameter, perimeter, area, and circularity [82]. The implementation of such automated platforms has significantly enhanced reproducibility and throughput compared to traditional manual microscopy approaches.
For more detailed morphological assessment and protein localization, immunofluorescence staining provides critical insights into drug effects on specific cellular compartments and pathways. A comprehensive immunofluorescence protocol for spheroids involves multiple stages: fixation to preserve morphology (using 4% paraformaldehyde or chilled methanol), permeabilization to allow antibody access (with detergents like Triton X-100), blocking to reduce non-specific binding, antibody incubation, and finally imaging [48]. These techniques enable researchers to visualize and quantify the distribution of biomarkers related to proliferation, apoptosis, hypoxia, and other physiological states within different spheroid regions.
Functional Assays
Beyond morphological assessment, a suite of functional assays provides multidimensional insights into drug mechanisms:
Invasion and Migration Assays: These assays evaluate the potential of compounds to inhibit metastatic behavior by measuring the ability of cells to invade through extracellular matrix components such as Matrigel [82]. The inclusion of these functional endpoints is particularly valuable for assessing agents targeting migratory pathways.
Viability and Cytotoxicity Assays: Metabolic assays (e.g., MTT, resazurin) and membrane integrity markers provide quantitative measures of cell viability and death in response to treatment [82]. The spatial distribution of cell death within spheroids can offer insights into drug penetration limitations.
Metabolic and Hypoxic Profiling: Assessment of oxygen consumption, glycolytic activity, and hypoxic markers helps characterize the metabolic effects of treatments and their relationship to the heterogeneous spheroid microenvironment [3].
The integration of these analytical approaches creates a comprehensive picture of drug effects that encompasses both direct cytotoxic activity and more subtle functional modifications of cellular behavior.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of spheroid-based drug screening requires specific reagents and materials optimized for 3D culture systems. The following table details key components and their functions:
Table 2: Essential Research Reagents and Materials for Spheroid Drug Response Studies
| Category | Specific Items | Function & Application |
|---|---|---|
| Spheroid Formation | Ultra-low attachment (ULA) plates [82] | Prevents cell adhesion, promotes spheroid self-assembly |
| Matrigel/synthetic scaffolds [48] | Provides extracellular matrix support for structure | |
| Wide-bore pipette tips [48] | Enables gentle handling without disrupting structure | |
| Culture Maintenance | BSA-coated tubes [48] | Reduces cell adhesion during processing steps |
| Specialized 3D culture media [82] | Supports nutrient diffusion in 3D architecture | |
| Drug Treatment | Molecularly targeted inhibitors [82] | Specific pathway modulation (e.g., PI3K, HSP90) |
| Chemotherapeutic agents [83] | Standard care comparators for response studies | |
| Analysis & Staining | Paraformaldehyde/methanol [48] | Fixation for structural preservation |
| Triton X-100 [48] | Permeabilization for intracellular antibody access | |
| Blocking serum (e.g., goat serum) [48] | Reduces non-specific antibody binding | |
| Primary/secondary antibodies [48] | Target protein detection and localization | |
| Nuclear stains (DAPI, Hoechst) [48] | Cell counting and viability assessment | |
| Advanced Applications | Cancer-associated fibroblasts [83] | Models tumor-stroma interactions |
| Endothelial cells [83] | Studies angiogenesis and vascular mimicry | |
| Immune cells [83] | Immunotherapy response evaluation |
The selection of appropriate reagents should be guided by the specific research objectives, with careful consideration of compatibility with 3D culture systems. For instance, the penetration characteristics of detection antibodies and viability dyes may require optimization for larger spheroids where diffusion limitations can affect assay performance.
Data Analysis and Interpretation Framework
The complexity of spheroid-based drug response data necessitates a structured analytical framework. The following diagram outlines the key steps in transforming raw experimental data into biologically meaningful conclusions:
Diagram 2: Data analysis workflow for drug response evaluation
Critical to this analytical framework is the calculation of appropriate metrics for quantifying drug efficacy. While traditional 2D models often rely on IC50 values derived from viability assays, spheroid models benefit from additional parameters that capture spatial and temporal aspects of drug response. These include:
Growth Inhibition Metrics: Calculation of percentage growth inhibition relative to untreated controls, often presented as GIs0 (no effect), GI50 (50% growth inhibition), GI100 (total growth inhibition) [82].
Drug Penetration Assessment: Evaluation of gradient effects through spatial analysis of marker distribution (e.g., proliferation, apoptosis) from periphery to core [3].
Invasion/Migration Inhibition: Quantification of anti-metastatic effects through measurement of invasion area or distance into surrounding matrix [82].
The interpretation of results should carefully consider the limitations and advantages of the specific spheroid model employed, including the cellular composition, culture method, and analytical endpoints. Correlation with complementary models, including in vivo studies when possible, strengthens the translational relevance of findings.
Spheroid models represent a powerful platform for assessing drug response and chemoresistance, offering significant advantages over traditional 2D systems in predicting clinical outcomes. Their ability to replicate key aspects of the tumor microenvironment, including 3D architecture, nutrient and oxygen gradients, and cell-cell interactions, enables more physiologically relevant evaluation of therapeutic efficacy and resistance mechanisms [6] [3]. The ongoing standardization of methodologies and analytical approaches continues to enhance the reproducibility and translational potential of these models [3] [18].
Future developments in spheroid-based drug assessment will likely focus on increasing complexity through the incorporation of multiple cell types—including immune cells, fibroblasts, and endothelial cells—to better mimic the tumor microenvironment [83]. Additionally, technological advances in automation, high-content imaging, and computational analysis will further improve throughput and data richness. As these models continue to evolve, their integration into personalized medicine approaches, particularly through the use of patient-derived cells, holds promise for tailoring therapeutic strategies to individual patients and ultimately improving clinical outcomes in oncology.
Within the broader thesis on spheroid models and scaffold-based techniques, the phenotypic validation of marker expression and stemness represents a critical analytical step. Three-dimensional (3D) in vitro models, particularly spheroids, have revolutionized cancer research by offering a more physiologically relevant system that bridges the gap between traditional two-dimensional (2D) monolayer cultures and in vivo tumors [3]. These self-organizing cellular aggregates recapitulate key aspects of the tumor microenvironment, including intricate cell-cell interactions, nutrient gradients, and spatial organization that closely mimic in vivo conditions [6] [3]. The core hypothesis driving this field posits that the 3D architecture of spheroids provides a selective pressure that enriches for and maintains cancer stem-like cells (CSCs), a subpopulation with enhanced self-renewal capacity, differentiation potential, and resistance to therapies [84] [85]. This technical guide provides an in-depth framework for validating the phenotypic and functional characteristics of CSCs within scaffold-based 3D culture systems, with a specific focus on marker expression patterns and stemness properties.
Key Stemness Markers in 3D Spheroid Models
The validation of CSC populations in 3D models relies on the detection of specific stemness markers that are consistently upregulated in these primitive cell states. These markers encompass transcription factors, cell surface proteins, and intermediate filaments that collectively define the stem-like phenotype.
Table 1: Key Stemness Markers and Their Significance in 3D Spheroid Models
| Marker | Type | Biological Function | Detection Methods | Relevance in 3D Culture |
|---|---|---|---|---|
| CD133 (PROM1) | Cell surface transmembrane protein | Stem cell maintenance, tumor initiation | Flow cytometry, Immunostaining | Enriched in 3D spheroids; marks tumor-initiating cells [84] [85] |
| SOX2 | Transcription factor | Maintenance of self-renewal and pluripotency | qRT-PCR, Immunostaining | Upregulated in 3D spheroids; core stemness regulator [84] [85] |
| OCT4 (POU5F1) | Transcription factor | Regulation of pluripotency, cell fate determination | qRT-PCR, Immunostaining, Reporter systems (SORE6) | Highly expressed in CSCs; indicator of stemness potential [84] [85] |
| NANOG | Transcription factor | Pluripotency maintenance, self-renewal capability | qRT-PCR, Immunostaining | Elevated in 3D cultures; sustains undifferentiated state [85] |
| NESTIN | Intermediate filament protein | Progenitor cell marker, structural integrity | qRT-PCR, Immunostaining | Increased expression in 3D neural and GBM spheroids [85] |
| CD44 | Cell surface adhesion receptor | Cell-matrix interactions, homing, and migration | Flow cytometry, Immunostaining | Co-expressed with CD133; CSC population marker [84] |
The expression profiles of these markers are consistently enhanced in 3D spheroid cultures compared to traditional 2D monolayers. For instance, in glioblastoma (GBM) spheroid models, the expression of stemness markers including NESTIN, SOX2, CD133, NANOG, and OCT4 was significantly increased, particularly when grown in heterotypic cultures incorporating astrocytes and endothelial cells to better simulate the tumor microenvironment [85]. This enhanced marker expression in 3D cultures underscores their superiority in maintaining and enriching for CSCs, providing a more representative platform for studying tumor biology and therapeutic resistance.
Experimental Workflow for Phenotypic Validation
The comprehensive validation of CSC phenotypes in 3D cultures requires an integrated experimental approach that combines scaffold-based culture techniques with multiple analytical endpoints. The workflow progresses systematically from spheroid generation through functional validation, as illustrated in the following diagram:
Diagram 1: Experimental workflow for phenotypic validation of CSCs in 3D culture (87 characters)
Detailed Methodologies for Key Experiments
Agar-Based Scaffold Culture Protocol
The agar-based non-adherent 3D culture method provides an economical and effective scaffold system for CSC enrichment and has been validated across multiple cancer cell lines, including prostate, colorectal, and hepatoma models [84].
Preparation of Agar-Coated Culture Ware:
- Prepare a 0.6-4.0% solution of Noble agar in distilled water and autoclave
- Maintain agar solution at 45°C in a water bath to prevent premature solidification
- Pre-warm 2× Dulbecco's Modified Eagle's Medium/Nutrient Mixture F-12 (DMEM/F12) to 45°C
- Mix equal volumes of agar solution and 2× DMEM/F12 medium (final agar concentration: 0.3-2.0%)
- Immediately pour the DMEM/F12-agar mixture onto culture plates or dishes with gentle swirling for even coating
- Allow complete solidification for 15-30 minutes in a culture cabinet
- For storage, add 3-5 mL of serum-free medium per 10-cm dish to prevent dehydration and store at 4°C for up to one week [84]
3D Spheroid Culture and Maintenance:
- Prepare single-cell suspensions using trypsin replacement reagents (e.g., TrypLE)
- Plate cells at optimal density (1×10⁴ to 1×10⁵ cells per 6-10 mL medium for 10-cm plates) on agar-coated surfaces
- Use serum-free medium supplemented with specific growth factors:
- 20 ng/mL human epidermal growth factor (EGF)
- 20 ng/mL human basic fibroblast growth factor (bFGF)
- 4 μg/mL insulin
- 1× B-27 supplement
- 1% KnockOut serum replacement
- 1% penicillin-streptomycin [84]
- Culture for 5-7 days with half-medium changes every 2-3 days
- For serial passaging, collect spheres by gentle centrifugation, dissociate to single cells, and replate on fresh agar-coated surfaces
Multicellular Spheroid Models
For more complex microenvironment modeling, heterotypic spheroid systems incorporating stromal components provide enhanced physiological relevance:
GBM-Astrocyte-Endothelial Cell Triculture Model:
- Utilize U87-MG GBM cells, C8-D1A astrocytes, and HUVECs in defined ratios
- Pre-label different cell populations with fluorescent CellTracker dyes (e.g., CMFDA) for identification
- Seed cells in round-bottom ultra-low attachment plates at optimized ratios (e.g., 1:4:9 for GBM:astrocytes:ECs)
- Use mixed media composition (1:1:1 EMEM:DMEM:EGM-2) to support all cell types
- Centrifuge plates at 1000×g for 10 minutes to promote cell aggregation
- Culture for up to 7 days with half-medium changes every 2 days [85]
Table 2: Quantitative Analysis of Stemness Marker Enhancement in 3D vs. 2D Cultures
| Culture Model | Marker | Fold Change in 3D vs. 2D | Analytical Method | Biological Significance |
|---|---|---|---|---|
| Agar-based Prostate Cancer | CD133 | 3.5-4.2× | qRT-PCR | CSC enrichment [84] |
| Agar-based Prostate Cancer | CD44 | 2.8-3.6× | Flow Cytometry | CSC surface marker upregulation [84] |
| Agar-based Prostate Cancer | OCT4 | 4.1-5.3× | SORE6 Reporter | Pluripotency network activation [84] |
| GBM-Astrocyte Coculture (1:4) | NESTIN | 2.5-3.2× | qRT-PCR | Neural progenitor phenotype [85] |
| GBM-EC Coculture (1:9) | SOX2 | 2.8-3.5× | Immunostaining | Self-renewal capacity enhancement [85] |
| GBM Triculture (1:4:9) | NANOG | 3.2-4.1× | qRT-PCR | Pluripotency regulation [85] |
Analytical Methods for Phenotypic Validation
Molecular Analysis of Stemness Markers:
- Extract high-quality RNA from spheroids using mechanical disruption
- Perform reverse transcription quantitative PCR (RT-qPCR) with validated primer sets
- Normalize expression to housekeeping genes (GAPDH, ACTB)
- Calculate fold-change using the 2^(-ΔΔCt) method relative to 2D controls [84] [85]
Protein-Level Detection and Quantification:
- For immunofluorescence: embed, section, and stain spheroids with antibodies against target markers
- For flow cytometry: dissociate spheroids to single cells, stain with fluorophore-conjugated antibodies
- Include appropriate isotype controls and compensation standards
- Analyze using confocal microscopy or flow cytometers with advanced analysis software [84] [85]
Functional Validation of Stemness Properties:
- Self-renewal capacity: Dissociate primary spheres and reassay for secondary and tertiary sphere formation
- In vivo tumorigenicity: Perform limiting dilution xenograft assays in immunocompromised mice
- Therapeutic resistance: Compare drug sensitivity profiles between 3D spheroids and 2D monolayers [84]
Signaling Pathways in Spheroid Stemness Maintenance
The maintenance of stemness in 3D spheroid models is regulated by complex signaling networks that are activated by the 3D microenvironment and cellular interactions. The following diagram illustrates the key pathways involved:
Diagram 2: Signaling pathways regulating stemness in 3D spheroids (72 characters)
The signaling architecture demonstrates how the unique 3D spheroid microenvironment activates multiple pathways that converge on core stemness regulators. Hypoxic conditions in the spheroid core stabilize HIF-1α, which directly promotes the expression of OCT4, SOX2, and NANOG [3]. Enhanced cell-cell contact in the compact spheroid structure activates Notch signaling, known to promote stem cell maintenance in various cancer types, including glioblastoma [85]. Additionally, remodeling of the extracellular matrix and autocrine/paracrine signaling through growth factors like EGF and bFGF further sustains the self-renewal circuitry. This integrated signaling network ultimately drives the expression of CSC surface markers and confers functional stemness properties, including enhanced self-renewal, therapy resistance, and in vivo tumorigenicity.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for 3D Spheroid Validation
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Scaffold Materials | Noble Agar, Poly-HEMA, Synthetic Hydrogels | Provide non-adherent surface for sphere formation | Agar concentration 0.3-2.0%; reusable for serial passages [84] |
| Serum-Free Media Supplements | B-27 Supplement, KnockOut SR, N-2 Supplement | Replace serum while maintaining stem cell viability | Essential for CSC maintenance and expansion [84] |
| Growth Factors | EGF (20 ng/mL), bFGF (20 ng/mL) | Promote CSC proliferation and self-renewal | Critical components of serum-free media formulation [84] |
| Cell Dissociation Reagents | TrypLE, Accutase | Gentle detachment preserving cell surface markers | Prefer over traditional trypsin for CSC applications [84] |
| Fluorescent Probes | CellTracker dyes (CMFDA, etc.) | Cell lineage tracing in coculture models | Enable visualization of multiple cell populations [85] |
| CSC Surface Marker Antibodies | Anti-CD133, Anti-CD44 | Identification and sorting of CSC populations | Used in flow cytometry and immunofluorescence [84] [85] |
| Stemness Transcription Factor Assays | OCT4/SOX2/NANOG antibodies, SORE6 reporter | Detection of core pluripotency factors | Reporter systems enable live monitoring of stemness [84] |
The phenotypic validation of marker expression and stemness in 3D culture systems represents a cornerstone of modern cancer research, providing critical insights into CSC biology within microenvironmentally relevant contexts. The methodologies outlined in this technical guide—from scaffold-based culture techniques to comprehensive analytical approaches—enable robust characterization of these therapeutically resistant cell populations. The consistent demonstration of enhanced stemness marker expression in 3D spheroid models across multiple cancer types underscores their utility as physiologically relevant platforms for drug discovery, therapeutic resistance studies, and personalized medicine applications. As the field advances, standardization of these validation approaches will be essential for improving reproducibility and translational potential in cancer research.
Correlation with In Vivo Data and Patient-Derived Samples
Three-dimensional (3D) spheroid models have emerged as a critical bridge between traditional two-dimensional (2D) cell cultures and complex in vivo environments, offering a more physiologically relevant platform for biomedical research. These models better replicate the intricate cell-cell and cell-extracellular matrix (ECM) interactions found in human tissues, providing a more accurate representation of tumor biology and drug response [6]. The correlation between data generated from 3D spheroid models and clinical outcomes is paramount for enhancing the predictive value of preclinical research, particularly in drug development and personalized medicine.
This technical guide examines the methodologies for establishing and validating scaffold-based spheroid techniques against in vivo data and patient-derived samples. We provide a comprehensive framework for researchers seeking to implement these advanced models, with detailed protocols, quantitative correlation data, and essential reagent toolkits to ensure experimental rigor and reproducibility. The ability of these models to recapitulate patient-specific disease characteristics and treatment responses makes them invaluable assets for accelerating translational research.
Establishing Correlation with Clinical and In Vivo Data
Quantitative Correlation Between Spheroid Assays and Metastatic Potential
Functional assays performed on spheroid models demonstrate significant quantitative correlations with clinically relevant aggressive disease phenotypes. Research involving 307 patient-derived breast cancer samples revealed that metastatic breast cancer (MBC) samples exhibited enhanced cancer stem cell activity compared to early breast cancer (EBC) samples, as measured through mammosphere formation and tumor initiation assays [86].
Table 1: Correlation Between Spheroid Assays and Clinical Disease Progression
| Parameter | Early Breast Cancer (EBC) | Metastatic Breast Cancer (MBC) | Statistical Significance |
|---|---|---|---|
| Primary Mammosphere Formation Efficiency | 0.6% | 0.9% | p < 0.0001 |
| Tumor Initiation In Vivo | 38% | 63% | p = 0.04 |
| Correlation with Lung Metastasis In Vivo | Not Significant | Significant (p = 0.05) | p = 0.05 |
The data demonstrates that mammosphere colony formation in vitro significantly correlated with the ability of a tumor to metastasize to the lungs in vivo, suggesting that cancer stem cell activity measured in spheroid assays can predict metastatic potential [86].
Patient-Derived Xenograft (PDX) Models as a Validation Bridge
PDX models, established by implanting patient tumor samples into immunocompromised mice, serve as a crucial intermediary for validating spheroid models against in vivo data. These models maintain the genetic characteristics and histopathology of the original patient tumors, providing a robust platform for comparative studies [87] [88].
Table 2: Correlation Between PDX Engraftment Success and Patient Clinical Outcomes
| PDX Characteristic | Finding | Clinical Correlation |
|---|---|---|
| Overall Engraftment Rate | 66% (23/35 BM samples) | Higher engraftment potential in aggressive disease [87] |
| Patient Survival (Engrafted vs. Non-Engrafted) | 6.1 vs. 10.8 months | p = 0.0032 [87] |
| Spontaneous Metastasis in PDX | 61% (14/23 PDX models) | Recapitulated patient dissemination patterns [87] |
| Drug Response in PDX-derived Organoids | Mirrored patient platinum sensitivity | Reliably categorized sensitive, resistant, and refractory cases [88] |
Notably, the ability of patient samples to form tumors in PDX models correlates with poorer patient survival, highlighting the clinical relevance of these models. Patients whose brain metastases successfully engrafted in mice had a significantly shorter overall survival (6.1 months) compared to those that did not engraft (10.8 months, p = 0.0032) [87]. This correlation was also observed specifically in lung cancer brain metastasis patients, further validating the prognostic value of the engraftment success [87].
Experimental Protocols for Correlation Studies
Establishing Spheroids from Patient-Derived Samples
Protocol 1: High-Throughput Spheroid Formation from Cell Lines
This protocol is optimized for generating uniform spheroids suitable for drug screening applications [13].
- Cell Preparation: Trypsinize cells, count using trypan blue exclusion, and resuspend at appropriate density.
- Platform Selection and Seeding:
- For 96-well Elplasia microcavity plates: Resuspend cells at 1.0 × 10^6 cells/mL and dispense 50 µL (5.0 × 10^4 cells) per well.
- For 96-well BIOFLOAT U-bottom plates: Resuspend cells at 1.0 × 10^5 cells/mL and dispense 50 µL (5.0 × 10^3 cells) per well.
- Incubation: Incubate plates undisturbed for 48 hours at 37°C and 5% CO₂.
- Quality Control: Image spheroids using an automated high-content imager. Analyze spheroid number, diameter, and circularity (e.g., using MetaXpress software with minimum object size 50 µm², circularity > 0.6).
Protocol 2: Cancer Cell Isolation from Malignant Ascites for Spheroid/Organoid Culture
This protocol is adapted for processing patient-derived fluid samples like malignant ascites from ovarian cancer patients [88].
- Sample Collection: Collect ascites fluid from consenting patients during standard therapeutic procedures.
- Centrifugation: Aliquot ascites into 50 mL tubes and centrifuge at 500 × g for 10 minutes at 4°C to pellet cells.
- Red Blood Cell Lysis: Resuspend the cell pellet in Ammonium Chloride Solution (e.g., STEMCELL Technologies, 07800) to lyse red blood cells.
- Spheroid Isolation: Isect cancer spheroids from the processed ascites fluid.
- Cryopreservation: Cryopreserve spheroids in freezing media (5% DMSO/95% FBS) at -80°C for future use or proceed directly to 3D culture.
Protocol 3: Low-Throughput Heterogeneous Spheroid Culture
This method generates a heterogeneous population of spheroids, useful for studying stem cell subpopulations [13].
- Seeding: Seed 8.0 × 10^3 cells in 2 mL of complete medium per well of a 6-well ultra-low attachment (ULA) plate.
- Experimental Groups: Include groups treated with compounds like ROCK1 inhibitor (Y-27632) to enhance stemness.
- Incubation: Incubate cultures undisturbed to allow for spontaneous spheroid formation.
- Classification: After several days, distinct spheroid subtypes will form: Holospheres (large, ~408.7 µm²), Merospheres (medium, ~99 µm²), and Paraspheres (small, ~14.1 µm²), which can be isolated for further analysis.
Drug Sensitivity Assays in 3D Models
Protocol 4: Standardized Spheroid-based Drug Screening
This protocol outlines a reliable method for drug testing in spheroids, with an estimated complete time of 170 hours [20].
- Spheroid Initiation: Generate uniform spheroids using high-throughput methods (Protocol 1).
- Drug Treatment: After spheroids have formed, add serial dilutions of the drug compounds to the wells.
- Long-Term Monitoring: Culture treated spheroids for ≥14 days to monitor growth kinetics, growth delay, and regrowth after treatment.
- Endpoint Analysis:
- Spheroid Integrity: Assess morphologically.
- Cell Survival: Quantify using the acid phosphatase assay or similar viability assays.
Protocol 5: Evaluating Chemotherapy Response in Patient-Derived Organoids
This protocol is used for determining platinum sensitivity in models derived from ovarian cancer patients [88].
- Model Establishment: Generate patient-derived organoids (PDOs) directly from patient samples or PDX-derived organoids (PDXOs).
- Drug Treatment: Treat organoids for 72 hours with standard chemotherapies (e.g., Paclitaxel, Carboplatin) or their combination.
- Viability Assessment: Measure organoid viability post-treatment using a validated cell viability assay (e.g., CellTiter-Glo 3D).
- Data Correlation: Compare the in vitro drug response (e.g., % reduction in viability) to the patient's clinical designation (platinum-sensitive, resistant, or refractory).
Immunofluorescence and Imaging of Spheroids
Protocol 6: Spheroid Immunofluorescence
A comprehensive protocol for staining 3D spheroids, which is critical for validating their morphology and protein expression against original patient samples [48].
- Fixation:
- Wash spheroids 3x with PBS.
- Fix with 4% PFA for 10 min at RT or chilled 100% methanol for 5 min at 4°C.
- Wash 3x with PBS.
- (Optional Antigen Retrieval): For PFA-fixed samples, heat spheroids in antigen retrieval buffer (e.g., Tris/EDTA pH 9.0) at 96-98°C for 20 min.
- Permeabilization: Incubate spheroids with permeabilization buffer (e.g., PBS with 0.5-2% Triton X-100) for 1 hour at RT on a flat shaker.
- Blocking: Incubate spheroids in blocking buffer (PBS with 0.1% Tween, 1% BSA, 22.52 mg/mL Glycine, and 10% goat serum) overnight at RT on a shaker.
- Antibody Staining:
- Primary Antibody: Incubate with primary antibody in appropriate dilution buffer overnight at RT on a shaker.
- Wash: Wash 4x with Wash Buffer (PBS + 0.1% Tween), 1 hour per wash.
- Secondary Antibody: Incubate with fluorophore-conjugated secondary antibody and nuclear stain (e.g., Hoechst) overnight.
- Wash: Wash 4x with Wash Buffer, 1 hour per wash.
- Imaging: Transfer spheroids to mounting media or storage buffer (PBS + 0.1% sodium azide) and image using confocal or high-content microscopy.
Workflow Visualization
The following diagram illustrates the integrated workflow for establishing and validating spheroid models against patient-derived samples and in vivo data.
Integrated Workflow for Spheroid Model Validation
The Scientist's Toolkit: Essential Research Reagents
Successful establishment and validation of spheroid models require specific reagents and materials. The following table details key solutions and their functions.
Table 3: Essential Reagent Solutions for Spheroid Research
| Reagent/Material | Function/Application | Example Protocols |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, forcing self-assembly into spheroids. Available in 6-well (low-throughput) and 96-well (high-throughput) formats. | High-throughput & Low-throughput Spheroid Formation [13] |
| Basement Membrane Matrix (e.g., Matrigel) | Scaffold-based culture providing ECM cues; used for embedding spheroids to study invasion, growth, and stemness. | Spheroid Immunofluorescence, Scaffold-based Studies [13] [48] |
| ROCK Inhibitor (Y-27632) | Enhances cell survival and stemness by inhibiting apoptosis in dissociated cells, improving spheroid formation efficiency. | Low-Throughput Heterogeneous Spheroid Culture [13] |
| Ammonium Chloride Solution | Lyses red blood cells in primary patient samples (e.g., ascites, pleural fluid) to enrich for cancer cells/spheroids. | Cancer Cell Isolation from Ascites [88] |
| Triton X-100 Solution | Detergent for permeabilizing spheroid cell membranes, allowing antibody penetration for intracellular target staining. | Spheroid Immunofluorescence [48] |
| Enzymatic Dissociation Kit (e.g., Miltenyi Tumor Dissociation Kit) | Digests solid patient tumor samples or spheroids into single-cell suspensions for subsequent culture or analysis. | In Vitro Sample Processing [86] |
The rigorous correlation of data from scaffold-based spheroid techniques with in vivo models and original patient samples is fundamental to establishing their predictive power in preclinical research. The protocols, validation data, and reagent toolkit provided in this guide offer a structured pathway for researchers to implement these advanced models. As the field progresses, standardizing these methodologies and demonstrating consistent correlation with clinical outcomes will be crucial for fully realizing the potential of 3D spheroid models in drug development and personalized medicine.
Standardization Efforts and Reproducibility Across Laboratories
Three-dimensional (3D) spheroid models have revolutionized in vitro cancer research by offering more physiologically relevant alternatives to traditional two-dimensional (2D) cultures, better mimicking the in vivo tumor microenvironment [3]. Their ability to recreate cell-cell and cell-matrix interactions, nutrient gradients, and spatial organization makes them indispensable tools for advancing personalized medicine and drug screening [3]. However, the growing adoption of spheroid models across laboratories has revealed significant challenges in standardization and reproducibility. The field utilizes diverse methodologies for spheroid formation, including forced-floating, scaffold-based techniques, hanging drop, microfluidics, and bioprinting, each with distinct advantages and limitations [3] [18]. This methodological heterogeneity poses a substantial barrier to comparing results across studies and institutions. Within the specific context of spheroid models scaffold-based techniques research, standardization efforts are critical for ensuring that data generated from these advanced models is reliable, reproducible, and translatable to clinical applications. This guide addresses the key challenges and provides actionable protocols and frameworks to enhance reproducibility in scaffold-based spheroid research.
Key Challenges in Reproducibility
The reproducibility of scaffold-based spheroid research is influenced by multiple variables, from cellular source to final analysis. A primary challenge is genetic intratumor heterogeneity (ITH), which is often overlooked when establishing models. Studies on colorectal cancer have demonstrated that different biopsies from the same tumor can harbor private mutations, and this heterogeneity is recapitulated in matching patient-derived spheroid cultures [89]. The concordance between original tumor biopsies and derived spheroids for coding mutations has been found to range between 40% and 70% [89]. Consequently, establishing multiple cultures from spatially distinct tumor sites is necessary to better represent the genetic landscape of the entire tumor, a critical factor for drug screening applications [89].
Furthermore, imaging and analysis present significant hurdles. Conventional microscopy is often destructive, requiring sectioning that damages the spheroid's microstructure [90]. While advanced imaging techniques like light-sheet microscopy [91] and MRI [90] offer non-invasive alternatives, the lack of a gold standard metric for comparing imaging quality, such as in the evaluation of optical clearing protocols, complicates objective analysis across platforms [92]. The selection of cell lines also introduces variability, as different lines (e.g., HT-29 vs. Caco-2) form spheroids with distinct morphological features and molecular characteristics, even when cultured using the same protocol [93].
The table below summarizes the major sources of variability and their impact on reproducibility:
Table 1: Key Challenges to Reproducibility in Spheroid Research
| Challenge Category | Specific Source of Variability | Impact on Reproducibility |
|---|---|---|
| Biological Source | Genetic intratumor heterogeneity [89] | Inconsistent genetic representation and drug response profiles. |
| Cell line-specific characteristics [93] | Differing spheroid morphology, stemness, and gene expression. | |
| Methodology | Multiple seeding techniques (e.g., forced-floating, scaffold-based) [3] [18] | Differences in spheroid structure, size, and cellular organization. |
| Scaffold material and biochemical properties | Variable cell-matrix interactions and nutrient diffusion. | |
| Analysis & Imaging | Destructive vs. non-invasive imaging [90] | Loss of structural integrity or inability to perform longitudinal studies. |
| Lack of standardized quality metrics [92] | Inability to objectively compare data between laboratories. |
Standardized Experimental Protocols
Achieving reproducibility requires the implementation of detailed and consistent experimental protocols. This section outlines standardized methodologies for scaffold-based spheroid formation and drug treatment assays.
Scaffold-Based Spheroid Formation Protocol
The following protocol is adapted from studies on colorectal cancer cell lines and can be modified for other cancer types [93].
1. Preparation of Non-Adherent Surfaces:
- Prepare a 1.2% poly-HEMA (Poly-2-hydroxyethyl methacrylate) solution by dissolving 1.2 g in 100 mL of 96% ethanol. Rotate the solution overnight to ensure complete dissolution.
- Centrifuge the solution at 400×g for 30 minutes to remove any undissolved particles. Filter the supernatant using a 0.22 µm filter.
- Coat tissue culture plates (e.g., 1.2 mL per well of a 6-well plate) with the filtered poly-HEMA solution. Allow the ethanol to evaporate completely overnight under a laminar flow hood.
- Before use, wash the coated plates with phosphate-buffered saline (PBS) to remove any residual solvent [93].
2. Cell Seeding and Spheroid Culture:
- Detach adherent cells using 0.05% trypsin/EDTA and inactivate the trypsin with complete media. Wash the resulting single-cell suspension twice with PBS and then with pre-warmed serum-free medium.
- Resuspend the cells in a defined serum-free medium. A common formulation includes:
- DMEM/F12 base medium.
- 20 ng/mL epidermal growth factor (EGF).
- 10 ng/mL basic fibroblast growth factor (bFGF).
- 2% B27 supplement.
- 1% non-essential amino acids.
- 2 mM L-glutamine.
- 1% penicillin-streptomycin.
- Seed the cell suspension onto the poly-HEMA coated plates at a density optimized for the cell line. For example, 5,000 to 10,000 cells per well for a 96-well U-bottom plate is a common starting point [93].
- Culture the cells under standard conditions (37°C, 5% CO2) for 72-96 hours, during which spheroids will self-assemble [91] [93].
Standardized Drug Treatment and Uptake Analysis
To assess drug efficacy in a reproducible manner, the following protocol for treatment and imaging can be employed, based on research with the mTOR inhibitor AZD2014 [91].
1. Drug Application:
- Prepare a stock solution of the drug candidate and dilute it to the desired working concentration in the spheroid culture medium.
- After spheroids have formed, carefully add the drug-containing medium. For a final concentration of 7 µM AZD2014, as an example, is a typical concentration used in uptake studies [91].
2. Real-Time Drug Uptake Imaging via Light-Sheet Microscopy:
- Transfer spheroids to an agarose holder housed in a glass-bottom dish compatible with the microscope stage [91].
- Place the dish onto a digital light-sheet microscope (e.g., a TCS SP8 DLS system) maintained at 37°C and 5% CO2.
- After adding the drug, acquire 3D time-lapse images. A typical setup uses a 10×/0.3 NA detection objective and a 405-nm laser for light-sheet generation.
- Acquire image stacks (e.g., 44 planes with dimensions of 780 µm × 780 µm × 300 µm) every 15 seconds for a period of 2 hours to monitor dynamic drug uptake [91]. The use of counter-propagating light sheets helps reduce image scattering and striping artifacts.
Quantitative Data and Standardization Metrics
Systematic reviews of the field reveal clear preferences and performance metrics for various spheroid formation techniques. The table below synthesizes quantitative data on the most investigated cancer types and the prevalence of different seeding methodologies, providing a benchmark for laboratory standardization.
Table 2: Systematic Analysis of Spheroid Research Focus and Methods (Based on 143 Studies)
| Parameter | Findings from Systematic Review | Implication for Standardization |
|---|---|---|
| Most Researched Cancer Types | Breast, colon, lung, ovary, and brain cancers [3] [18]. | Prioritize development of disease-specific standards for these cancers. |
| Predominant Seeding Methods | Forced-floating and scaffold-based methods are the most common [3] [18]. | These reliable methods are prime candidates for initial protocol harmonization. |
| Genetic Concordance | 40-70% concordance for coding mutations between tumor biopsies and derived spheroids [89]. | Highlights the need for multi-region sampling to capture heterogeneity. |
| Impact of Spheroid Culture on Stemness | Significant upregulation of stemness genes (SOX2, C-MYC, NANOG, OCT4) in HT-29 spheroids [93]. | Confirms the model's biological relevance but necessitates controls for stem cell enrichment. |
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting reproducible scaffold-based spheroid research, as cited in the protocols above.
Table 3: Essential Reagents for Scaffold-Based Spheroid Research
| Reagent/Material | Function in Protocol | Example from Literature |
|---|---|---|
| Poly-HEMA | Creates a non-adherent coating on cultureware to force cell aggregation into spheroids [93]. | Used to generate HT-29 and Caco-2 colonospheres [93]. |
| Serum-Free Medium (SFM) | Prevents cell differentiation and supports the proliferation of stem-like/CSC populations [93]. | DMEM/F12 supplemented with growth factors [93]. |
| Growth Factors (EGF, bFGF) | Key supplements in SFM to promote cell survival and proliferation in the absence of serum [93]. | EGF (20 ng/mL) and bFGF (10 ng/mL) in colonosphere culture [93]. |
| B27 Supplement | A defined mixture of hormones and proteins that supports neuronal and stem cell survival; commonly used in spheroid media [93]. | Added at 2% concentration to serum-free medium for spheroid formation [93]. |
| Agarose | Used to create MRI-compatible holders or micro-well supports for spheroid culture and imaging [90] [91]. | Employed in a custom 3D-printed comb to create wells for spheroid holding during light-sheet imaging [91]. |
Visualization of a Spheroid Signaling Pathway
The mTOR pathway is a critical signaling cascade often studied in spheroid models due to its role in regulating cell proliferation, metabolism, and survival. Its dysregulation is a common feature in cancer. The following diagram illustrates the mTOR pathway and the mechanism of action for a second-generation inhibitor, AZD2014, whose uptake has been visualized in spheroids [91].
The journey toward full standardization of scaffold-based spheroid techniques is ongoing, but critical progress is being made. Future efforts must focus on the dynamic refinement of standards, particularly for emerging areas like inhalation preparation packaging and nucleic acid drug carriers [94]. Furthermore, the integration of advanced computational approaches, such as Quantitative Systems Pharmacology (QSP), promises to enhance the predictive power of spheroid models. QSP uses computational modeling to bridge the gap between biology and pharmacology, helping to simulate clinical trial scenarios and optimize therapeutic strategies, thereby reducing reliance on traditional animal testing [95]. International collaboration, similar to the Sino-US Pharmacopoeia Joint Working Group mechanism for pharmaceutical packaging standards, will be vital for achieving mutual recognition of testing methods and joint research in spheroid model standardization [94]. By adopting systematic protocols, leveraging non-invasive imaging technologies, and embracing computational integration, the research community can solidify the role of spheroid models as a reproducible and translatable platform in drug development and personalized medicine.
Conclusion
Scaffold-based 3D spheroid models represent a paradigm shift in preclinical research, offering a critical bridge between simplistic 2D cultures and complex, costly in vivo models. By providing a more physiologically relevant context that recapitulates key aspects of the tumor microenvironment, these systems enable more accurate studies of tumor biology, drug penetration, and therapeutic resistance. The integration of advanced biomaterials and standardized protocols is paving the way for higher reproducibility and broader adoption. Future directions will likely focus on increasing model complexity through multi-cellular systems, incorporating patient-derived cells for personalized medicine applications, and further refining synthetic, defined scaffolds to reduce batch variability. As these models continue to evolve, they hold immense promise for improving the efficiency of drug discovery pipelines and accelerating the development of more effective cancer therapies.
References
- 1. Islets in the body are never flat: transitioning from two -dimensional... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01171-8]
- 2. Carboplatin response in preclinical models for ovarian cancer... [https://www.nature.com/articles/s41598-021-97434-w?error=cookies_not_supported&code=f845120e-e53b-4442-b181-6066c2f5e0d3]
- 3. Unlocking the Potential of Spheroids in Personalized... | Preprints.org [https://www.preprints.org/manuscript/202504.0640/v1]
- 4. between Three-Dimensional Comparison and... Spheroid [https://biot.modares.ac.ir/article_22531_en.html]
- 5. Studying Human Neurological Disorders Using Induced Pluripotent... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6705133/]
- 6. Three-Dimensional Spheroid for Cardiovascular... | CoLab Models [https://colab.ws/articles/10.1016%2Fj.mbm.2025.100144]
- 7. Frontiers | From spheroids to organoids: next-generation models for... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1626369/full]
- 8. Cell Culture Models as Recapitulators of the 3 ... D Tumor [https://pmc.ncbi.nlm.nih.gov/articles/PMC8749977/]
- 9. Vascularization Strategies in 3D Cell Culture Models : From... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9737506/]
- 10. Frontiers | Recapitulating Tumorigenesis in vitro: Opportunities and... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.682498/full]
- 11. of applying multicellular tumor Challenges in preclinical... spheroids [https://cancerci.biomedcentral.com/articles/10.1186/s12935-021-01853-8]
- 12. A New Dimension of Cell Culture: The Rise of Spheroid Culture Systems [https://cellculturedish.com/cell-culture-spheroid-culture-systems/]
- 13. Standardized Methodology of Scaffold - Free and Scaffold - Based ... [https://www.mdpi.com/2409-9279/8/5/123]
- 14. Standardized Methodology of Scaffold - Free and Scaffold - Based ... [https://pubmed.ncbi.nlm.nih.gov/41149806/]
- 15. - Scaffold Stem Cell Free in Complex Organ Bioprinti Spheroids [https://www.linkedin.com/pulse/bioprinting-functional-tissues-using-scaffold-free-stem-biradar-0qvrf]
- 16. of EMT-Related and Multi-Drug Resistant Gene... | CoLab Comparison [https://colab.ws/articles/10.3390/ijms232113306]
- 17. - Scaffold cellular free generate integrated osteochondral... spheroids [https://www.news-medical.net/news/20250814/Scaffold-free-cellular-spheroids-generate-integrated-osteochondral-grafts.aspx]
- 18. Unlocking the Potential of Spheroids in Personalized Medicine... [https://pubmed.ncbi.nlm.nih.gov/40650254/]
- 19. How Organoids And Spheroids Works — In One Simple Flow ( 2025 ) [https://www.linkedin.com/pulse/how-organoids-spheroids-works-one-simple-flow-2025-lgujf]
- 20. -based drug screen: considerations and... | Nature Spheroid Protocols [https://www.nature.com/articles/nprot.2008.226?error=cookies_not_supported&code=22da2302-c600-421d-9d21-abfb999f922e]
- 21. Cell Spheroid – Practical solutions for frequently asked... Culture [https://cellculturedish.com/spheroid-cell-culture-practical-solutions-for-frequently-asked-questions/]
- 22. Application of an Integrated Single- Cell and Three-Dimensional... [https://pubmed.ncbi.nlm.nih.gov/40004228/]
- 23. Application of an Integrated Single- Cell and... | Preprints.org [https://www.preprints.org/manuscript/202412.2142/v1]
- 24. A Comparative Review of Natural and Synthetic Biopolymer Composite Scaffolds - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8037451/]
- 25. Development of Scaffolds from Bio-Based Natural Materials for Tissue Regeneration Applications: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957409/]
- 26. Fabrication of a matrigel - collagen semi-interpenetrating scaffold for... [https://pubmed.ncbi.nlm.nih.gov/28484097/]
- 27. Bone tissue engineering scaffolding: computer-aided scaffolding techniques - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709372/]
- 28. Development of a nanostructured DNA delivery scaffold via... [https://pubmed.ncbi.nlm.nih.gov/12711456/]
- 29. Mapping the synthesis and the impact of low molecular weight... [https://link.springer.com/article/10.1007/s10965-013-0337-8]
- 30. Organoid and Spheroid Tumor Models : Techniques and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7922036/]
- 31. What are Spheroids , 3 | Molecular Devices D Spheroids Models [https://www.moleculardevices.com/applications/3d-cell-models/spheroids]
- 32. : Optimizing Your Research Methods - Elveflow 3 D Cell Culture [https://elveflow.com/microfluidic-reviews/3d-cell-culture-methods-and-applications-a-short-review/]
- 33. 3D Bioprinting Using Hydrogels : Cell Inks and Tissue Engineering... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9784738/]
- 34. 3D bioprinted biomimetic MOF-functionalized hydrogel for... scaffolds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018039/]
- 35. Characterization and printability of Sodium alginate -Gelatin hydrogel ... [https://www.nature.com/articles/s41598-019-55034-9?error=cookies_not_supported&code=7c21b85a-8c81-4e90-bb6c-3a27078ad71a]
- 36. Frontiers | Hydrogel -Based Bioinks for 3D Bioprinting in Tissue... [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2020.00076/full]
- 37. A comprehensive protocol for hydrogel -based bioink design ... [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb00737b]
- 38. WST-1 Assay: principles, protocol & best practices for cell viability [https://www.abcam.com/en-us/knowledge-center/cell-biology/wst-1-assay-principles-protocols-and-best-practices-for-cell-viability]
- 39. Three-dimensional preclinical models for Osteosarcoma : Advances... [https://pubmed.ncbi.nlm.nih.gov/40848340/]
- 40. Multimodal Mass Spectrometry Imaging of an Osteosarcoma ... [https://shura.shu.ac.uk/33834/]
- 41. A promising breakthrough in pancreatic cancer : The potential... research [https://pubmed.ncbi.nlm.nih.gov/39963557/]
- 42. Let’s Go 3D! New Generation of Models for Evaluating Drug Response... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10049142/]
- 43. Tumor promoting effect of spheroids in an orthotopic prostate ... cancer [https://www.nature.com/articles/s41598-024-59052-0?error=cookies_not_supported&code=ebbc4dc4-94df-4b82-80c2-bf58bc2faae8]
- 44. Running session-conditioned human serum lowers prostate ... cancer [https://link.springer.com/article/10.1007/s00432-025-06350-3]
- 45. 3D spheroid assays in cancer research [https://www.news-medical.net/whitepaper/20250613/High-throughput-automation-of-3D-spheroid-assays-in-cancer-research.aspx]
- 46. (PDF) Research Dynamics of Tissue as Building Blocks... Spheroids [https://www.academia.edu/92332359/Research_Dynamics_of_Tissue_Spheroids_as_Building_Blocks_A_Scientometric_Analysis]
- 47. Strategies to capitalize on cell spheroid therapeutic potential for tissue... [https://www.nature.com/articles/s41536-022-00266-z?error=cookies_not_supported&code=d00f19f0-9f23-4048-a298-16087559853c]
- 48. preparation and immunofluorescence Spheroid . | Abcam protocol [https://www.abcam.com/en-us/technical-resources/protocols/spheroid-preparation-and-immunofluorescence-protocol]
- 49. An in vitro model system based on calcium- and phosphate... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10682137/]
- 50. Cell spheroid fusion: beyond liquid drops model | Scientific Reports [https://www.nature.com/articles/s41598-020-69540-8?error=cookies_not_supported]
- 51. fusion-based in vitro screening assays for analysis of... Tissue spheroid [https://pubmed.ncbi.nlm.nih.gov/20603872/]
- 52. analysis of tumour Quantitative structure | eLife spheroid [https://elifesciences.org/articles/73020]
- 53. Surface Optimization and Design Adaptation toward Spheroid ... [https://pubmed.ncbi.nlm.nih.gov/35590879/]
- 54. Surface Optimization and Design Adaptation toward Spheroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9104470/]
- 55. Multicellular ovarian cancer spheroids : novel 3D model to mimic... [https://www.nature.com/articles/s41598-024-73680-6?error=cookies_not_supported&code=5458e351-c5bd-44c3-b881-1c5c712e3089]
- 56. Characterization of Triple-Negative Breast Cancer MDA-MB-231 Cell... [https://www.dovepress.com/characterization-of-triple-negative-breast-cancer-mda-mb-231-cell-sphe-peer-reviewed-fulltext-article-OTT]
- 57. of tumor Optimization model in mesothelioma... | Oncotarget spheroid [https://www.oncotarget.com/article/28134/text/]
- 58. Facile Tumor Spheroids Formation in Large Quantity with Controllable... [https://www.nature.com/articles/s41598-018-25203-3?error=cookies_not_supported]
- 59. Develop Cellulose- Researchers 3D Based That Mimic... Scaffolds [https://www.azolifesciences.com/news/20250409/Researchers-Develop-Cellulose-Based-3D-Scaffolds-That-Mimic-Natural-Tissue-Architecture.aspx]
- 60. Designing and interpreting 4D tumour spheroid experiments [https://www.nature.com/articles/s42003-022-03018-3?error=cookies_not_supported&code=7eb52b63-50d4-4102-a53b-337837c57141]
- 61. Mathematical and Experimental Model of Oxygen for... Diffusion [https://pubmed.ncbi.nlm.nih.gov/27165074/]
- 62. Numerical modeling of oxygen in tissue spheroids... diffusion [https://www.nature.com/articles/s41598-025-86805-2?error=cookies_not_supported&code=59ac30d8-9d74-4411-91d3-de66067fa933]
- 63. Semi-Automated Phenotypic Analysis of Functional 3D Spheroid Cell... [https://pubmed.ncbi.nlm.nih.gov/37607073/]
- 64. Sheets: A Scalable Platform for Producing Tissue Membrane... Spheroid [https://bio-protocol.org/en/bpdetail?id=5501&type=0]
- 65. Frontiers | Harnessing 3D cell models and high-resolution imaging to... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1606573/full]
- 66. An Efficient and Flexible Cell Aggregation Method for 3D Spheroid ... [https://www.jove.com/t/55544/an-efficient-flexible-cell-aggregation-method-for-3d-spheroid]
- 67. 3D Cell Culture Tools and Techniques [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/3d-cell-culture-technology]
- 68. Generation of Multicellular Breast Cancer Tumor Spheroids ... [https://pubmed.ncbi.nlm.nih.gov/27518775/]
- 69. Functional 3D Human Primary Hepatocyte Spheroids Made by... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3517565/]
- 70. Alithea Genomics Introduces MERCURIUS Spheroid -seq DRUG [https://www.iptonline.com/articles/alithea-genomics-introduces-mercurius-spheroid-drugseq]
- 71. Tumor Spheroid Formation Assay [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/3d-cell-culture/tumor-spheroid-formation-assay]
- 72. What 32,000 3D Spheroids Revealed About... - Promega Connections [https://www.promegaconnections.com/what-32000-3d-spheroids-revealed-about-culture-conditions/]
- 73. MDA-MB-231 Cell Line Spheroid ... | Thermo Fisher Scientific - JP [https://www.thermofisher.com/jp/ja/home/references/protocols/cell-culture/3-d-cell-culture-protocol/mda-mb-231-cell-line-spheroid-generation.html]
- 74. Splitting Spheroids for Sub-culturing and Shipping: A Procedure for... [https://www.jove.com/t/30057/splitting-spheroids-for-sub-culturing-shipping-procedure-for]
- 75. High-Content Assays for Characterizing the Viability and Morphology... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4556086/]
- 76. Cell Cultures for Staining | Thermo Fisher Scientific - US 3 D Imaging [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/3d-organoid-staining.html]
- 77. Advanced biomedical applications based on emerging 3D cell culturing... [https://pubs.rsc.org/en/content/articlehtml/2020/tb/d0tb01658f]
- 78. Adding Depth to Your Research: A Look at 3D Cell Culture [https://www.labx.com/resources/adding-depth-to-your-research-a-look-at-3d-cell-culture/255]
- 79. -free generation of uniform adipose spheroids for metabolism... Scaffold [https://www.nature.com/articles/s41598-017-19024-z?error=cookies_not_supported]
- 80. Millicell® Ultra - low Knowledge Center Attachment Plates [https://www.sigmaaldrich.com/BR/pt/campaigns/millicell-ultra-low-attachment-plates-knowledge-center]
- 81. Analysis of 3D Bladder Tumor Spheroids Obtained by... Comparative [https://pubmed.ncbi.nlm.nih.gov/28878686/]
- 82. Advances in establishment and analysis of three-dimensional tumor... [https://bmcbiol.biomedcentral.com/articles/10.1186/1741-7007-10-29]
- 83. Three-dimensional heterotypic colorectal cancer spheroid for... models [https://pubmed.ncbi.nlm.nih.gov/37469395/]
- 84. Development of a novel and economical agar-based non-adherent... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0987-x]
- 85. The Impact of Astrocytes and Endothelial Cells on Glioblastoma... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8630250/]
- 86. - Patient Mammosphere and Xenograft Tumour Initiation... derived [https://link.springer.com/article/10.1007/s10911-016-9361-8]
- 87. - Patient models of brain metastases recapitulate human... derived [https://pmc.ncbi.nlm.nih.gov/articles/PMC9133464/]
- 88. Organoid models established from primary tumors and patient - derived ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14811-8]
- 89. Characterization of genetic intratumor heterogeneity in colorectal... [https://pubmed.ncbi.nlm.nih.gov/29130628/]
- 90. Imaging cell spheroid clusters: An MRI protocol for non-invasive... [https://pubmed.ncbi.nlm.nih.gov/39897913/]
- 91. Imaging of Anti-Cancer Drug Uptake in Spheroids using DLS [https://www.leica-microsystems.com/science-lab/life-science/imaging-of-anti-cancer-drug-uptake-in-spheroids-using-dls/]
- 92. (PDF) A quantitative for the metric ... - Academia.edu comparative [https://www.academia.edu/106752304/A_quantitative_metric_for_the_comparative_evaluation_of_optical_clearing_protocols_for_3D_multicellular_spheroids]
- 93. Morphological and molecular characteristics of spheroid formation in... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-021-01898-9]
- 94. Innovation and significance of the pharmaceutical packaging material ... [https://www.munanglass.com/news_detail/Innovation_and_significance_of_the_pharmaceutical_packaging_material_standard_system_of_the_2025_edition_of_the_Chinese_Pharmacopoeia.html]
- 95. QSP Summit 2025 : A New Standard in the Future of Drug ... [https://www.certara.com/blog/qsp-summit-2025-a-new-standard-in-the-future-of-drug-development/]