Setting Robust Acceptance Criteria for Method Comparability: A Risk-Based Framework for Biologics and ATMPs
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on establishing scientifically sound and defensible acceptance criteria for analytical method comparability and equivalency studies.
Setting Robust Acceptance Criteria for Method Comparability: A Risk-Based Framework for Biologics and ATMPs
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on establishing scientifically sound and defensible acceptance criteria for analytical method comparability and equivalency studies. Covering the entire lifecycle from foundational principles to regulatory submission, it details a risk-based framework aligned with ICH Q5E and Q14. Readers will gain practical insights into statistical methods like the Two One-Sided T-test (TOST), strategies for batch selection and stability comparability, and best practices for troubleshooting and optimizing study designs to ensure robust demonstration of product quality and facilitate successful regulatory reviews.
Laying the Groundwork: Core Principles and Regulatory Expectations for Comparability
In the highly regulated pharmaceutical and biotech industries, ensuring the reliability and consistency of analytical methods is paramount. As drug development progresses and manufacturing processes evolve, scientists and regulators must frequently assess the relationship between different analytical procedures. Within this context, the terms "comparability" and "equivalency" represent distinct statistical and regulatory concepts with critical implications for product quality and regulatory compliance. While both concepts involve the assessment of methods or processes, they differ fundamentally in their stringency, statistical approaches, and regulatory consequences. Understanding this distinction is essential for designing appropriate studies, applying correct statistical methodologies, and navigating the regulatory landscape effectively throughout the analytical procedure lifecycle.
Core Definitions and Regulatory Context
Defining Comparability
Comparability refers to the evaluation of whether a modified analytical method yields results that are sufficiently similar to those of the original method to ensure consistent assessment of product quality. The objective is to demonstrate that the changes do not adversely impact the decision-making process regarding product quality attributes [1]. Comparability studies are typically employed for procedural modifications that are considered lower risk, such as optimizations within an established method's design space. These changes usually do not require prior regulatory approval before implementation, though they must be thoroughly documented and justified [1]. The statistical approach for comparability often focuses on ensuring that results are sufficiently similar and that any differences do not have a practical impact on quality decisions.
Defining Equivalency
Equivalency (or equivalence) represents a more rigorous standard, requiring a comprehensive statistical assessment to demonstrate that a new or replacement analytical procedure performs equal to or better than the original method [1]. Equivalency is necessary for high-risk changes, such as complete method replacements or changes to critical quality attributes. The key distinction lies in the regulatory burden: equivalency studies require regulatory approval prior to implementation [1]. The statistical bar is also higher, often requiring formal validation and sophisticated testing to prove that the methods are statistically interchangeable for their intended purpose.
The Regulatory Framework: ICH Q14 and Beyond
The ICH Q14 guideline on Analytical Procedure Development has formalized a structured, risk-based approach to the lifecycle management of analytical methods [1]. This framework encourages forward-thinking development where scientists define an Analytical Target Profile (ATP) and anticipate future changes. Furthermore, other regulatory documents, such as the EMA Reflection Paper on statistical methodology and the USP <1033> chapter, provide additional guidance on the appropriate statistical approaches for demonstrating comparability and equivalency [2] [3]. The recent Ph. Eur. chapter 5.27 on "Comparability of Alternative Analytical Procedures" explicitly outlines the requirement for manufacturers to demonstrate that an alternative method is comparable to a pharmacopoeial method, a process that requires authorization by the competent authority [4] [5].
Key Distinctions at a Glance
The table below summarizes the critical differences between comparability and equivalency.
| Feature | Comparability | Equivalency |
|---|---|---|
| Definition | Evaluation for "sufficiently similar" results [1] | Demonstration of "equal to or better" performance [1] |
| Regulatory Impact | Typically does not require prior approval [1] | Requires regulatory approval before implementation [1] |
| Statistical Stringency | Lower; focuses on practical similarity [1] [3] | Higher; requires formal proof of interchangeability [1] |
| Study Scope | Limited, risk-based testing [1] | Comprehensive, often full validation [1] |
| Typical Use Case | Minor method modifications, within design space changes [1] | Major method changes, method replacements [1] |
Experimental Protocols and Statistical Methodologies
Designing a Comparability Study
A comparability study is designed to show that a modified method does not yield meaningfully different results from the original. The protocol should include:
- Sample Selection: Analysis of a representative set of samples (e.g., drug product from different batches) using both the original and modified methods [1].
- Predefined Acceptance Criteria: Establishment of justified limits for the difference between method results based on the method's performance and the Critical Quality Attributes (CQAs) it measures [1].
- Data Analysis: A comparison of the results, often through descriptive statistics and graphical analysis (e.g., difference plots, correlation coefficients). The focus is on showing that all differences fall within the predefined, practically significant limits.
Designing an Equivalency Study
An equivalency study demands a more rigorous statistical approach to prove that two methods are interchangeable.
- Side-by-Side Testing: A structured study analyzing a sufficient number of samples covering the expected range of the method using both the original and new procedures [1].
- Equivalence Testing using TOST: The preferred statistical method is the Two One-Sided T-tests (TOST) procedure [2]. This approach tests the hypothesis that the difference between the two method means is less than a pre-specified, clinically or quality-relevant equivalence margin (Δ).
- The null hypotheses (H₀) are: H₀₁: μ₁ - μ₂ ≤ -Δ and H₀₂: μ₁ - μ₂ ≥ Δ.
- The alternative hypotheses (H₁) are: H₁₁: μ₁ - μ₂ > -Δ and H₁₂: μ₁ - μ₂ < Δ.
- Equivalency is concluded only if both null hypotheses are rejected, demonstrating that the true difference is conclusively within the range -Δ to +Δ [2].
- Confidence Interval Approach: Equivalency can also be demonstrated by showing that the (1-2α)% confidence interval (e.g., a 90% CI for an α=0.05) for the difference in means lies entirely within the equivalence interval (-Δ, +Δ) [2].
Setting Risk-Based Acceptance Criteria
Setting the equivalence margin (Δ) is a critical, risk-based decision. Scientific knowledge, product experience, and clinical relevance must be considered [2]. As outlined in BioPharm International, risk-based acceptance criteria can be categorized as follows [2]:
- High Risk: Allows only a small practical difference (e.g., 5-10% of the tolerance or specification range).
- Medium Risk: Allows a moderate difference (e.g., 11-25%).
- Low Risk: Allows a larger difference (e.g., 26-50%).
This ensures that the most critical methods, where a small deviation could significantly impact product quality or patient safety, are held to the most stringent standard.
Workflow and Decision Pathways
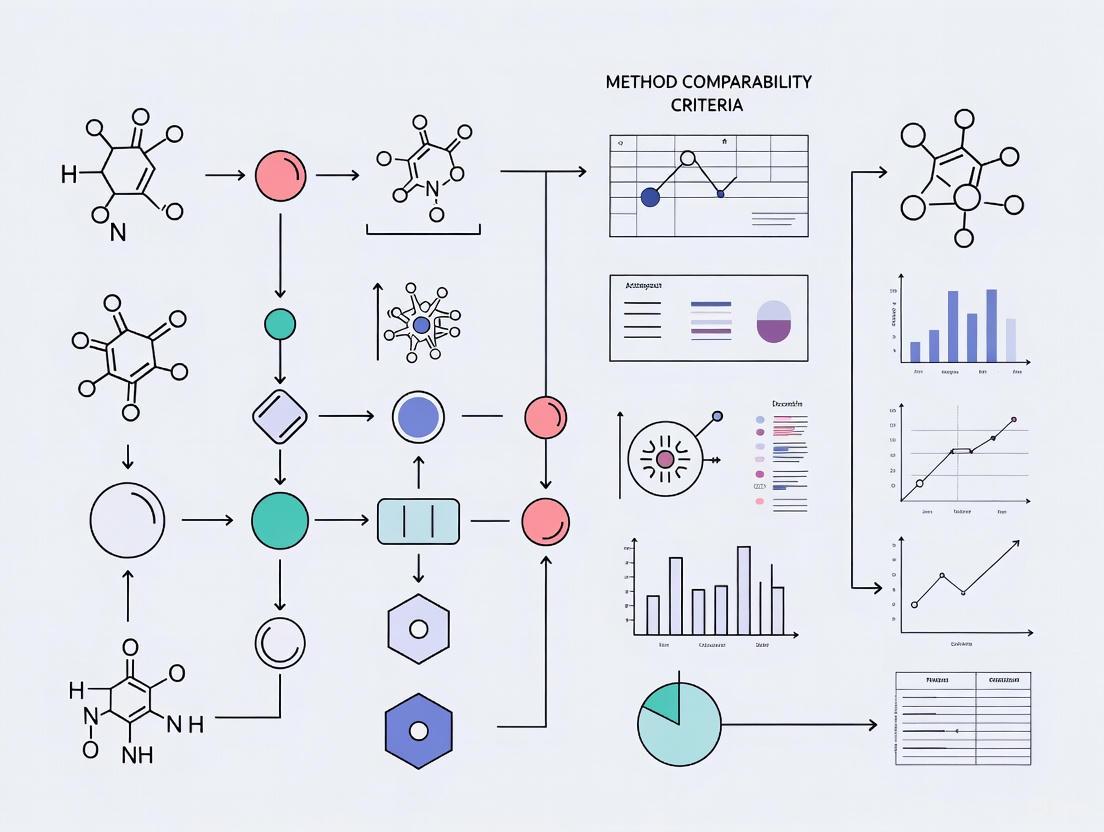
The following diagram illustrates the logical decision process for determining whether a comparability or equivalency study is required and the key steps involved in the assessment.
Decision Workflow for Method Changes
The Scientist's Toolkit: Essential Reagents and Materials
The table below details key reagents, materials, and solutions commonly required for conducting robust comparability and equivalency studies in an analytical laboratory.
| Item | Function in Comparability/Equivalency Studies |
|---|---|
| Representative Test Samples | A set of samples (e.g., drug substance, drug product from multiple batches) that accurately reflect the expected variability of the process. Essential for side-by-side testing [1]. |
| Reference Standards | Highly characterized materials with known purity and properties. Used to ensure both the original and new analytical procedures are calibrated and performing correctly [2]. |
| System Suitability Solutions | Prepared mixtures or solutions used to verify that the analytical system (e.g., HPLC, GC) is performing adequately before and during the analysis of study samples. |
| Certified Reference Materials (CRMs) | Commercially available materials with certified property values and uncertainties. Used to establish accuracy and traceability for quantitative methods. |
| Reagents and Mobile Phases | High-purity solvents, buffers, and other chemical reagents prepared according to strict standard operating procedures (SOPs) to ensure consistency and reproducibility across both methods. |
Navigating the concepts of comparability and equivalency is a fundamental requirement for successful analytical procedure lifecycle management in the pharmaceutical industry. The critical distinction lies in the regulatory and statistical burden: comparability demonstrates that methods are "sufficiently similar" for their intended purpose and is often managed internally, while equivalency demands rigorous statistical proof that methods are "interchangeable" and requires regulatory oversight. A deep understanding of these differences, coupled with the application of risk-based principles and appropriate statistical tools like equivalence testing (TOST), empowers scientists to make sound, defensible decisions. This ensures that changes to analytical methods enhance efficiency and innovation without compromising the unwavering commitment to product quality and patient safety.
This guide provides a comparative analysis of three key regulatory frameworks—ICH Q5E, FDA Comparability Protocols, and ICH Q14—that are essential for managing changes in the biopharmaceutical development lifecycle. It is designed to help researchers and scientists establish robust method comparability acceptance criteria.
Comparative Framework of Regulatory Guidelines
The table below summarizes the core focus, scope, and application of ICH Q5E, FDA Comparability Protocols, and ICH Q14.
| Guideline | Primary Focus & Objective | Regulatory Scope & Application | Key Triggers & Context of Use | Core Data Requirements |
|---|---|---|---|---|
| ICH Q5E | Assessing comparability before and after a manufacturing process change for a biologic drug substance or product [6]. | Quality and patient safety; focuses on the biologic product itself [6]. | Post-approval manufacturing changes (e.g., process scale-up, site transfer) [6]. | Extensive analytical characterization (identity, purity, potency), and often non-clinical/clinical data [6]. |
| FDA Comparability Protocols | A pre-approved plan for assessing the impact of future manufacturing changes on product quality [6]. | A submission and review tool within a BLA/IND; outlines studies for future changes [6]. | Anticipated changes (e.g., raw material supplier, equipment) [6]. | Studies defined in the pre-approved plan (e.g., side-by-side analytical testing) [6]. |
| ICH Q14 | Analytical Procedure Lifecycle Management, ensuring methods are robust and fit-for-purpose [1] [7]. | Analytical methods used to control the product; enables a structured, science-based approach [1] [7]. | Analytical method development, modification, or replacement [1]. | Analytical Target Profile (ATP), method validation data, and control strategy [8] [7]. |
Experimental Protocols for Comparability and Equivalency
This section details the methodologies for conducting key studies under these regulatory frameworks.
Protocol for Product Comparability (Aligned with ICH Q5E & FDA Protocols)
This protocol is designed to generate evidence that a manufacturing change does not adversely affect the drug product.
- 1. Hypothesis: The pre-change and post-change drug products are comparable in terms of critical quality attributes (CQAs), and the existing safety and efficacy profile is maintained.
- 2. Experimental Design & Methodology:
- Sample Preparation: Manufacture multiple lots of the drug substance and drug product using both the pre-change (reference) and post-change (test) processes [6].
- Forced Degradation Studies: Stress both reference and test samples under various conditions (e.g., light, heat, pH) to understand and compare product degradation profiles [6].
- Orthogonal Analytical Testing: Perform a comprehensive panel of analytical tests on reference and test samples to compare CQAs. This includes, but is not limited to [6]:
- Identity: Amino acid sequencing, peptide mapping.
- Purity/Impurities: Capillary electrophoresis (CE-SDS), reversed-phase liquid chromatography (RP-LC), and asymmetric flow field-flow fractionation (AF4) for aggregates [6].
- Potency: Cell-based bioassays or binding assays.
- Product Characteristics: Isoform profile, charge variants, and glycosylation pattern.
- 3. Data Analysis & Acceptance Criteria:
- Statistical Comparison: Use statistical tools (e.g., equivalence tests, t-tests) to quantitatively compare CQAs between reference and test groups [6].
- Acceptance Criteria: Predefine acceptance criteria based on process capability and historical data. The data must demonstrate that post-change product CQAs are within the qualified or validated ranges and are highly similar to the pre-change product [6].
Protocol for Analytical Method Equivalency (Aligned with ICH Q14)
This protocol is used to demonstrate that a new or modified analytical method is equivalent to or better than the original method.
- 1. Hypothesis: The new analytical procedure is equivalent to the original procedure, providing the same or superior reportable results for the same samples.
- 2. Experimental Design & Methodology:
- Sample Set Selection: Select a representative set of samples that covers the entire reportable range and includes different lots and strengths [1].
- Side-by-Side Testing: Analyze the selected sample set using both the original and new analytical methods under a pre-defined study protocol [1].
- Full Validation: Ensure the new method has undergone a full validation per ICH Q2(R2) to confirm its performance characteristics (accuracy, precision, specificity, etc.) are suitable for their intended use [1].
- 3. Data Analysis & Acceptance Criteria:
- Statistical Evaluation: Perform a statistical comparison (e.g., paired t-test, ANOVA) of the reportable results from both methods [1].
- Acceptance Criteria: Predefine equivalence margins. The study demonstrates equivalency if the results from the new method fall within the pre-defined acceptable range compared to the original method [1].
Decision Workflow for Navigating Regulatory Guidelines
The following diagram illustrates the logical decision process for determining the appropriate regulatory pathway when a change occurs during drug development.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below details key reagents and materials critical for executing the experimental protocols for comparability and equivalency.
| Item Name | Function & Role in Experimentation |
|---|---|
| Well-Characterized Reference Standards | Serves as the benchmark for assessing the quality of both pre-change and post-change products and for qualifying new analytical methods [6]. |
| Critical Quality Attribute (CQA)-Specific Assays | A panel of orthogonal assays (e.g., CE-SDS, RP-LC, qPCR) used to fully characterize the drug product's identity, purity, potency, and safety [6] [8]. |
| Stressed/Forced Degradation Samples | These samples help reveal differences in product profiles between pre-change and post-change materials that may not be visible under standard conditions [6]. |
| System Suitability Test (SST) Materials | Qualified materials used to verify that an analytical system is functioning correctly and is capable of providing valid data for each experimental run [8]. |
| ATP-Defined Analytical Procedures | Procedures developed and controlled per ICH Q14, ensuring they are fit-for-purpose and generate reliable data for comparability and equivalency decisions [8] [7]. |
In the development of biologic therapeutics, the direct linkage between Critical Quality Attributes (CQAs) and methodological rigor forms the cornerstone of a science-based quality framework. According to ICH Q8(R2), a Quality Target Product Profile (QTPP) serves as "A prospective summary of the quality characteristics of a drug product that ideally will be achieved to ensure the desired quality, taking into account safety and efficacy of the drug product" [9]. Within this framework, CQAs are defined as physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality [9]. The identification and control of CQAs are therefore paramount to patient safety and therapeutic efficacy, requiring a risk-based approach to determine the appropriate level of analytical and procedural rigor throughout the product lifecycle.
The modern paradigm of Quality by Design (QbD) emphasizes a systematic risk management approach, starting with predefined objectives for the drug product profile [9]. This involves applying scientific principles in a stage and risk-based manner to enhance product and process understanding, ensuring reliable manufacturing processes and controls for a safe and effective drug. As the industry faces increasing complexity in therapeutic modalities and manufacturing processes, the imperative to logically connect CQA criticality with study design stringency has never been more pronounced.
The Analytical Framework: From CQA Identification to Control Strategy
Systematic CQA Identification and Risk Assessment
The process of CQA identification represents the foundational step in establishing a risk-based control strategy. ICH Q9 defines risk as the combination of the probability of harm, the ability to detect it, its severity, and the uncertainty of that severity [9]. The protection of the patient by managing the risk to quality should be considered of prime importance, placing patient safety at the center of all CQA assessments.
A practical classification scheme enables development teams to identify potential critical quality attributes early in clinical development, refining this understanding as process and product knowledge matures [9]. This iterative classification typically involves:
- Prior Knowledge Assessment: Leveraging literature and platform knowledge for similar modalities to identify potential CQAs before product-specific data is available.
- Risk Ranking and Filtering: Systematically evaluating quality attributes based on their impact on safety and efficacy, often using risk assessment tools such as Failure Mode and Effects Analysis (FMEA).
- Experimental Verification: Conducting structured studies to confirm the criticality of attributes and establish appropriate ranges that ensure product quality.
The bi-directional relationship between CQA identification and process understanding creates an iterative knowledge loop, wherein information from process and product development enhances understanding of CQAs, which in turn informs further process optimization [9].
Analytical Control Stringency and Lifecycle Management
Once CQAs are identified, an Analytical Target Profile (ATP) and analytical control stringency plan must be developed [9]. The ATP, as defined in ICH Q14, consists of a description of the intended purpose of the analytical procedure, appropriate details on the product attributes to be measured, and the desired relevant performance characteristics with associated performance criteria [9]. The control stringency then determines which analytical procedures become cGMP specification tests and which are deployed for non-cGMP characterization and development studies.
The recently adopted ICH Q14 and its companion guideline ICH Q2(R2) recommend applying a lifecycle approach for analytical procedure development, validation, and monitoring [9]. This enhanced approach, while more rigorous initially, provides flexibility for continuous improvement and more efficient control strategy lifecycle management. The traditional definition of Analytical Control Strategy (ACS) has typically focused narrowly on procedural elements of an analytical method, but in the context of QbD, the scope expands significantly to include strategies for CQA identification and for when and how to apply analytical procedures based on criticality and relative abundance of product attributes [9].
Table 1: Analytical Control Stringency Application Based on CQA Criticality and Phase of Development
| CQA Criticality Level | Development Phase | Control Stringency | Typical Analytical Procedures | Data Requirements |
|---|---|---|---|---|
| High (Direct impact on safety/efficacy) | Early (Preclinical-Phase II) | High | cGMP release and stability methods | Quantitative, validated for intended purpose |
| Late (Phase III-Commercial) | Very High | cGMP specification methods with tight controls | Fully validated per ICH guidelines | |
| Medium (Potential impact on safety/efficacy) | Early | Medium | Characterization and investigation methods | Quantitative with defined performance |
| Late | High | cGMP methods with appropriate monitoring | Fully validated with defined control strategies | |
| Low (Minimal impact on safety/efficacy) | Early | Low | Development and characterization studies | Qualitative or semi-quantitative data |
| Late | Medium | Periodic monitoring or classification tests | Study-specific validation |
Experimental Protocols for Method Comparability and Equivalency
Designing Comparability Studies
In the dynamic environment of drug development, changes to analytical methods are inevitable due to technology upgrades, supplier changes, manufacturing improvements, or regulatory updates [1]. The ICH Q5E guideline requires that "the existing knowledge is sufficiently predictive to ensure that any differences in quality attributes have no adverse impact upon safety or efficacy of the drug product" [10]. Demonstrating "comparability" does not require the pre- and post-change materials to be identical, but they must be highly similar [10].
A well-designed comparability study for biologics typically comprises several key elements:
- Extended Characterization: Providing orthogonal analysis with finer-level detail than release methods, especially for CQAs.
- Forced Degradation Studies: Revealing degradation pathways through stress conditions beyond typical process ranges.
- Stability Studies: Assessing real-time and accelerated stability profiles of pre- and post-change materials.
- Statistical Analysis: Applying appropriate statistical methods to historical release data and comparability study results.
For early-phase development, when representative batches are limited and CQAs may not be fully established, it is acceptable to use single batches of pre- and post-change material with platform methods [10]. As development advances to Phase 3, extended characterization increases in complexity to include more molecule-specific methods and head-to-head testing of multiple pre- and post-change batches, ideally following the gold standard format: 3 pre-change vs. 3 post-change [10].
Demonstrating Method Equivalency
While comparability evaluates whether a modified method yields results sufficiently similar to the original, equivalency involves a more comprehensive assessment to demonstrate that a replacement method performs equal to or better than the original [1]. Such changes require regulatory approval prior to implementation and typically include:
- Side-by-Side Testing: Analyzing representative samples using both the original and new methods under standardized conditions.
- Statistical Evaluation: Employing appropriate statistical tools such as paired t-tests or ANOVA to quantify agreement between methods.
- Predefined Acceptance Criteria: Establishing thresholds based on method performance attributes and CQAs before study initiation.
- Risk-Based Documentation: Tailoring documentation and regulatory submissions to the criticality of the change and its potential impact on product quality.
ICH Q14 encourages a structured, risk-based approach to assessing, documenting, and justifying method changes [1]. For high-risk changes involving method replacements, a comprehensive equivalency study with full validation is often required to ensure the data used for comparison meets GMP standards.
Table 2: Experimental Design for Analytical Method Comparability and Equivalency Studies
| Study Component | Comparability Study | Equivalency Study |
|---|---|---|
| Regulatory Threshold | Typically does not require regulatory filings or commitments [1] | Requires regulatory approval prior to implementation [1] |
| Sample Requirements | Single or multiple representative batches [10] | Multiple batches (typically 3 pre-change vs. 3 post-change) [10] |
| Testing Scope | Extended characterization, forced degradation, stability [10] | Full validation plus side-by-side comparison with original method [1] |
| Statistical Rigor | Descriptive statistics, graphical comparison | Formal statistical tests (t-tests, ANOVA, equivalence testing) [1] |
| Acceptance Criteria | Qualitative and quantitative criteria for "highly similar" [10] | Predefined statistical thresholds for "equivalent or better" [1] |
| Study Duration | Medium-term (aligned with stability testing intervals) | Comprehensive, often longer-term to ensure robustness |
Visualization of the Risk-Based CQA to Study Rigor Framework
Logical Workflow for CQA-Based Study Design
The following diagram illustrates the logical relationship between CQA identification, risk assessment, and the implementation of appropriate analytical control strategies, culminating in method comparability assessments.
Extended Characterization and Forced Degradation Experimental Workflow
The following diagram details the experimental workflow for extended characterization and forced degradation studies, which are critical components of comparability assessments for biologics.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of a risk-based approach to CQA assessment and method comparability requires specialized reagents and analytical tools. The following table details key research reagent solutions essential for conducting rigorous comparability studies.
Table 3: Essential Research Reagents and Materials for CQA Assessment and Comparability Studies
| Reagent/Material | Function and Application | Critical Attributes for Comparability |
|---|---|---|
| Reference Standards | Calibrate analytical methods and serve as benchmarks for product quality attributes [9] | Well-characterized, high purity, established stability profile |
| Critical Reagents | Enable specific detection and quantification in bioassays and immunoassays | Specificity, affinity, consistency between lots |
| Cell-Based Assay Systems | Measure biological activity and potency for CQAs related to mechanism of action [11] | Relevance to mechanism of action, reproducibility, appropriate controls |
| Chromatography Columns | Separate and analyze product variants and impurities | Selectivity, resolution, retention time reproducibility |
| Mass Spectrometry Standards | Enable accurate mass determination and structural characterization | Mass accuracy, purity, compatibility with analytical system |
| Forced Degradation Reagents | Stress products to reveal degradation pathways and product vulnerabilities [10] | Purity, concentration accuracy, solution stability |
The imperative of a risk-based approach connecting CQAs to study rigor represents a fundamental principle in modern pharmaceutical development and quality assurance. By systematically linking the criticality of quality attributes to the stringency of analytical controls and comparability assessments, organizations can build robust, scientifically justified development strategies that ensure product quality while maintaining flexibility for continuous improvement.
ICH Q14 transforms how organizations approach analytical procedures, emphasizing long-term planning from the outset [1]. While cultivating a forward-thinking culture can be challenging, the benefits of a well-designed lifecycle management program are invaluable. With intelligent design, validations become seamless, and change management evolves from reactive to proactive, enabling analytical procedures to stay aligned with innovation while remaining fit-for-purpose throughout a product's lifecycle [1].
The convergence of enhanced regulatory frameworks, advanced analytical technologies, and risk-based decision-making creates an opportunity for organizations to demonstrate deeper product and process understanding. This knowledge ultimately strengthens the scientific basis for quality determinations and accelerates the development of safe, effective, and high-quality biologic therapeutics for patients.
In pharmaceutical development, demonstrating method comparability is a critical regulatory requirement. While traditional t-tests have long been used for statistical comparisons, they are fundamentally limited for proving practical equivalence. This guide examines the theoretical and practical superiority of equivalence testing, particularly the Two One-Sided Tests (TOST) procedure, for establishing method comparability. Through experimental data and regulatory context, we demonstrate why moving beyond simple significance testing is essential for robust analytical procedure lifecycle management.
The Fundamental Limitation of Traditional T-Tests
Traditional null hypothesis significance testing (NHST), such as the common t-test, poses a significant challenge for comparability studies. The standard t-test structure examines whether there is evidence to reject the null hypothesis of no difference between methods. When the p-value exceeds the significance level (typically p > 0.05), the only statistically correct conclusion is that the data do not provide sufficient evidence to detect a difference—not that no difference exists [12].
This approach creates a fundamental logical problem for comparability studies. As noted in the United States Pharmacopeia (USP) chapter <1033>, "A significance test associated with a P value > 0.05 indicates that there is insufficient evidence to conclude that the parameter is different from the target value. This is not the same as concluding that the parameter conforms to its target value" [2]. The study design may have too few replicates, or the validation data may be too variable to discover a meaningful difference from the target.
Three critical limitations of t-tests for comparability assessment include:
- High variability masking: Excessive method variability can lead to non-significant p-values even when meaningful differences exist
- Sample size dependence: With extremely large sample sizes, trivial, practically irrelevant differences can become statistically significant
- Incorrect conclusion framing: Failure to reject the null hypothesis does not provide evidence for equivalence
Equivalence Testing: A Statistically Sound Framework
Equivalence testing reverses the traditional hypothesis testing framework, making it particularly suitable for comparability assessments. The goal is to demonstrate that differences between methods are smaller than a pre-specified, clinically or analytically meaningful margin [12].
The Two One-Sided Tests (TOST) Procedure
The TOST procedure tests two simultaneous null hypotheses:
- H01: μ2 – μ1 ≤ -θ (The difference is less than or equal to the lower equivalence bound)
- H02: μ2 – μ1 ≥ θ (The difference is greater than or equal to the upper equivalence bound)
The alternative hypothesis is that the true difference lies within the equivalence interval: -θ < μ2 – μ1 < θ [13]. When both one-sided tests reject their respective null hypotheses, we conclude that the difference falls within the equivalence bounds, supporting practical equivalence.
Establishing Equivalence Boundaries
Setting appropriate equivalence boundaries (θ) is a critical, scientifically justified decision that should be based on:
- Risk to product quality: Higher risks allow only small practical differences
- Analytical method capability: The inherent variability of the method
- Clinical relevance: The impact on safety and efficacy
- Process capability: Potential impact on out-of-specification (OOS) rates [2]
Table 1: Risk-Based Equivalence Acceptance Criteria
| Risk Level | Typical Acceptance Range | Application Examples |
|---|---|---|
| High | 5-10% of tolerance | Critical quality attributes with narrow therapeutic index |
| Medium | 11-25% of tolerance | Key analytical parameters with moderate impact |
| Low | 26-50% of tolerance | Non-critical attributes with wide specifications |
Experimental Design for Method Comparability
Statistical Protocol
A robust equivalence study for analytical method comparison should include the following elements:
Sample Size Planning: Based on the formula for one-sided tests: n = (t₁₋α + t₁₋β)²(s/δ)², where s is the estimated standard deviation and δ is the equivalence margin [2]. For medium-risk applications with alpha = 0.05 and power of 80%, a minimum sample size of 13 is often appropriate, with 15 recommended for additional assurance.
Experimental Execution:
- Analyze representative samples using both original and modified methods under identical conditions
- Ensure sample selection represents the entire specification range
- Use appropriate blocking to minimize confounding factors
- Maintain full GMP documentation throughout the process
Data Analysis Workflow
Comparative Experimental Data: T-Test vs. Equivalence Testing
Case Study: HPLC Method Transfer
An experimental comparison was conducted during the transfer of a stability-indicating HPLC method from R&D to a quality control laboratory. The critical quality attribute measured was assay potency (%) for 15 samples across the specification range (90-110%).
Table 2: Method Comparison Results for Assay Potency
| Statistical Test | Result | Conclusion | Statistical Evidence | Regulatory Acceptance |
|---|---|---|---|---|
| Traditional t-test | p = 0.12 | No significant difference found | Weak (failure to reject null) | Questionable |
| TOST Procedure | p₁ = 0.03, p₂ = 0.04 | Equivalence demonstrated | Strong (rejection of both nulls) | Acceptable |
| 90% Confidence Interval | (-1.45, 1.89) within (-2.5, 2.5) | Clinical equivalence confirmed | Interval within bounds | Strongly supported |
Comparative Performance Across Multiple Attributes
Table 3: Multi-Attribute Method Comparability Assessment
| Quality Attribute | Risk Category | Equivalence Margin | Traditional t-test p-value | TOST Result | Correct Conclusion |
|---|---|---|---|---|---|
| Potency | High | ±2.5% | 0.15 | Equivalent | TOST only |
| Impurities | High | ±0.15% | 0.08 | Equivalent | TOST only |
| pH | Medium | ±0.3 units | 0.03 | Equivalent | Both methods |
| Dissolution | Medium | ±5% | 0.22 | Not equivalent | TOST only |
| Color | Low | ±2 units | 0.41 | Equivalent | TOST only |
Regulatory Framework and Implementation Guidelines
ICH Guidelines and Lifecycle Management
The introduction of ICH Q14: Analytical Procedure Development provides a formalized framework for the creation, validation, and lifecycle management of analytical methods [1]. Within this framework, demonstrating comparability or equivalency becomes essential when modifying existing procedures or adopting new ones.
Comparability vs. Equivalency Distinction:
- Comparability: Evaluates whether a modified method yields results sufficiently similar to the original, ensuring consistent product quality
- Equivalency: A more comprehensive assessment demonstrating that a replacement method performs equal to or better than the original, often requiring full validation and regulatory approval [1]
Practical Implementation Strategy
For Low-Risk Changes: A comparability evaluation with limited testing may be sufficient when a method's range of use has been defined by robustness studies.
For High-Risk Changes: A comprehensive equivalency study must show the new method performs equal to or better than the original, typically requiring:
- Full validation of the new method
- Side-by-side testing with representative samples
- Statistical evaluation using TOST or similar methodology
- Predefined acceptance criteria based on method performance attributes and Critical Quality Attributes (CQAs) [1]
Essential Research Reagent Solutions
Table 4: Key Materials for Analytical Method Equivalency Studies
| Reagent/Material | Function in Comparability Studies | Critical Specifications | Supplier Considerations |
|---|---|---|---|
| Reference Standards | Primary method calibration and system suitability | Certified purity, stability, traceability | Official compendial sources preferred |
| Chemically Defined Reagents | Mobile phase preparation, sample dilution | HPLC/GC grade, low UV absorbance, lot-to-lot consistency | Manufacturers with robust change control processes |
| Columns and Stationary Phases | Chromatographic separation | Column efficiency (N), asymmetry factor, retention reproducibility | Multiple qualified vendors to mitigate supply risk |
| Quality Control Samples | Method performance verification | Representative of product quality attributes, stability | Should span specification range (low, mid, high) |
| Forced Degradation Materials | Stress testing for stability-indicating methods | Controlled conditions (oxidative, thermal, photolytic, acidic, basic) | Scientific justification for stress levels and duration |
Logical Decision Framework for Method Changes
The transition from statistical significance to practical equivalence represents a fundamental shift in analytical science that aligns statistical methodology with scientific and regulatory needs. Equivalence testing, particularly through the TOST procedure, provides a statistically rigorous framework for demonstrating method comparability that traditional t-tests cannot offer. By implementing risk-based equivalence margins, appropriate experimental designs, and clear decision frameworks, pharmaceutical scientists can robustly demonstrate method comparability while maintaining regulatory compliance throughout the analytical procedure lifecycle.
From Theory to Practice: Designing and Executing a Comparability Study
In the highly regulated landscape of pharmaceutical development, establishing scientifically sound acceptance criteria is paramount for ensuring product quality, patient safety, and regulatory compliance. A one-size-fits-all approach to acceptance criteria is increasingly recognized as inefficient and scientifically unjustified, often leading to unnecessary resource allocation or inadequate risk control. The paradigm has decisively shifted toward risk-based approaches that tailor acceptance criteria according to the potential impact of changes on product quality, safety, and efficacy [14].
This guide frames the establishment of risk-based acceptance criteria within the broader context of method comparability research, providing a structured framework for pharmaceutical professionals to differentiate strategies for high, medium, and low-risk changes. By directly linking risk assessment to statistical confidence levels and sample sizing, organizations can make more informed decisions about which changes require rigorous testing and which can be managed with more efficient approaches [15] [14]. The fundamental principle is that the stringency of acceptance criteria should be proportional to the risk posed by the change, ensuring optimal resource allocation while maintaining robust quality standards.
Foundational Concepts: Risk Assessment and Statistical Underpinnings
Core Risk Assessment Methodology
A standardized risk assessment process forms the foundation for establishing appropriate acceptance criteria. The process typically involves these key stages [16] [17]:
- Risk Identification: Systematic brainstorming sessions with cross-functional stakeholders to identify potential risks associated with a change, categorizing them as strategic, operational, financial, or external [16].
- Risk Analysis: Evaluation of each risk's likelihood of occurrence and potential impact on project objectives, often using qualitative (High/Medium/Low) or semi-quantitative (1-5 or 1-10 scales) scoring [17].
- Risk Prioritization: Using a risk matrix to categorize risks as high, medium, or low based on their likelihood and impact scores, enabling focused resource allocation [16].
Statistical Foundation for Acceptance Criteria
Risk-based acceptance criteria are grounded in statistical sampling theory, which balances producer risk (α, probability of rejecting an acceptable lot) and consumer risk (β, probability of accepting a rejected lot) [14]. The Operating Characteristic (OC) curve visually represents this relationship, showing how a sampling plan performs across various possible quality levels [14].
Two primary sampling approaches inform acceptance criteria:
- Attribute Sampling: Uses pass/fail criteria and is simpler to implement but typically requires larger sample sizes to achieve statistical confidence [14].
- Variable Sampling: Uses quantitative measurements against numerical specifications, providing more information about lot quality and requiring fewer samples to achieve the same statistical confidence as attribute sampling [14].
Table 1: Key Statistical Parameters for Acceptance Criteria
| Parameter | Definition | Impact on Acceptance Criteria |
|---|---|---|
| Alpha (α) | Producer's risk; probability of rejecting an acceptable lot | Lower α requires more stringent acceptance criteria |
| Beta (β) | Consumer's risk; probability of accepting a rejected lot | Lower β requires more stringent acceptance criteria |
| AQL | Acceptable Quality Limit; highest defect rate considered acceptable | Sets the quality standard for routine production |
| RQL | Rejectable Quality Limit; lowest defect rate considered unacceptable | Directly tied to patient risk; drives sample size requirements |
Risk Classification Framework for Changes
Defining Risk Levels for Changes
The first step in establishing risk-based acceptance criteria is categorizing changes according to their potential impact on product quality and patient safety. This classification directly determines the appropriate statistical confidence levels and sample sizes for testing [14].
- High-Risk Changes: Changes with potential for direct impact on product quality, safety, or efficacy. Examples include changes to drug substance synthesis, formulation modifications, or changes to primary container closure systems. These require the most stringent acceptance criteria with high statistical confidence [14].
- Medium-Risk Changes: Changes with potential indirect impact on product quality attributes. Examples include certain manufacturing process parameter changes or analytical method changes. These require balanced acceptance criteria with moderate statistical confidence [14].
- Low-Risk Changes: Changes with negligible impact on product quality. Examples include documentation changes or equipment changes with proven equivalence. These require streamlined acceptance criteria with focus on efficiency [14].
Risk Assessment and Treatment Workflow
The following diagram illustrates the systematic process for assessing risk levels and selecting appropriate acceptance criteria strategies:
Strategic Approaches by Risk Level
Strategy for High-Risk Changes
High-risk changes demand the most rigorous approach to acceptance criteria, with focus on patient safety and quality assurance. The strategy should include [14]:
- Statistical Confidence: Maintain both α and β at 5% to ensure 95% confidence and power, minimizing both producer and consumer risk [14].
- RQL Focus: Set stringent RQL targets (e.g., <1%) based on severity of potential harm to patients, making this the primary driver of sample size [14].
- Sample Size: Select larger sample sizes to achieve higher AQL values while maintaining RQL targets, reducing the chance of rejecting acceptable material [14].
- Variable Sampling: Prefer variable over attribute sampling plans to maximize information obtained from each unit tested [14].
Table 2: Acceptance Criteria Strategy by Risk Level
| Strategy Element | High-Risk Changes | Medium-Risk Changes | Low-Risk Changes |
|---|---|---|---|
| Statistical Confidence | 95% (α/β = 5%) | 90-95% (α/β = 5-10%) | <90% (α/β >10%) |
| RQL Target | Low (e.g., 0.1-1%) | Medium (e.g., 1-5%) | High (e.g., 5-10%) |
| Sampling Approach | Variable preferred | Variable or attribute | Attribute typically sufficient |
| Sample Size | Larger (justified by RQL) | Moderate | Minimal |
| Documentation | Extensive, with formal rationale | Standard documentation | Basic documentation |
Experimental Protocol: Establishing Acceptance Criteria
The following protocol provides a detailed methodology for establishing statistically sound, risk-based acceptance criteria:
Define the Change Scope: Clearly document the proposed change and its potential impact on product Critical Quality Attributes (CQAs). Form a cross-functional team including quality, regulatory, manufacturing, and development experts [14].
Conduct Risk Assessment: Using a standardized risk assessment methodology (e.g., FMEA), score the change for severity, probability, and detectability. Classify as high, medium, or low risk based on predefined criteria [17].
Select Statistical Parameters: Based on risk classification, set appropriate α, β, and RQL values. For high-risk changes, maintain both α and β at 5%. Link RQL directly to the potential severity of patient harm [14].
Determine Sample Size: Using the selected RQL and β values, calculate the required sample size. For variable sampling, this typically requires 20-30 samples to achieve 5% RQL with 95% confidence. For attribute sampling, similar protection may require 59+ samples [14].
Establish Acceptance Criteria: Define specific numerical limits or pass/fail criteria based on the selected statistical approach. For variable plans, establish process capability (Cpk) or tolerance interval requirements. For attribute plans, define the maximum allowable failures [14].
Document and Justify: Formalize the complete acceptance criteria strategy in a controlled document, including the risk assessment, statistical justification, and sample size calculation. Obtain appropriate quality and regulatory approval [15].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Acceptance Criteria Studies
| Item | Function/Application | Considerations |
|---|---|---|
| Statistical Software | (e.g., JMP, Minitab, R) For OC curve generation, sample size calculation, and data analysis | Must support variable and attribute sampling plan analysis; validation required for regulated environments |
| Reference Standards | Well-characterized materials with known properties for method validation and system suitability | Certified reference materials preferred; requires proper storage and handling |
| Risk Assessment Tools | (e.g., FMEA templates, risk matrices) For standardized risk scoring and classification | Should be company-approved and aligned with ICH Q9 principles |
| Data Integrity Systems | (e.g., ELN, LES) For capturing, storing, and reporting experimental data | Must meet 21 CFR Part 11 requirements for electronic records and signatures |
| Quality Management Software | For documenting acceptance criteria, deviations, and change control | Should integrate with existing quality systems and provide audit trails |
Implementation and Compliance Considerations
Regulatory Alignment and Documentation
Successful implementation of risk-based acceptance criteria requires careful attention to regulatory expectations and documentation practices. Key considerations include [15] [14]:
- Structured Documentation: Implement formal Risk Acceptance Criteria (RAC) documents that clearly define risk thresholds, authority levels, and review processes. These should be officially documented in policy documents to ensure consistency across teams [15].
- Regulatory Compliance: Ensure acceptance criteria approaches align with relevant regulatory requirements, such as 21 CFR 820.250, which requires valid statistical techniques for sampling plans [14].
- Cross-Functional Communication: Communicate RAC across all departments (IT, Finance, Operations) to ensure consistent understanding and application. Internal audits should regularly challenge whether accepted risks remain justified [15].
Post-Implementation Strategy
After establishing and implementing risk-based acceptance criteria, ongoing monitoring is essential [15]:
- Performance Monitoring: Track actual outcomes against acceptance criteria to validate statistical assumptions and refine approaches for future changes.
- Periodic Review: Establish a regular schedule (e.g., quarterly for high-risk, annually for lower-risk) to reassess accepted risks and criteria as business conditions and threat landscapes evolve [15].
- Process Optimization: Use control charts and trend analysis to potentially reduce testing requirements post-process validation, once sufficient data demonstrates process stability [14].
Establishing risk-based acceptance criteria represents a scientifically rigorous approach to managing changes in pharmaceutical development and manufacturing. By differentiating strategies for high, medium, and low-risk changes, organizations can better allocate resources, maintain regulatory compliance, and ultimately enhance patient safety. The framework presented in this guide—connecting risk assessment to statistical confidence levels and sample sizing—provides a actionable approach for researchers, scientists, and drug development professionals engaged in method comparability studies.
As the pharmaceutical industry continues to embrace risk-based methodologies, the ability to justify acceptance criteria through statistical principles and patient-centric risk assessment becomes increasingly important. This approach not only satisfies regulatory requirements but also fosters a more efficient and science-driven quality culture within organizations.
Within method comparability acceptance criteria research, establishing equivalence between two methods or processes is a frequent and critical challenge. Traditional hypothesis significance tests (NHST), which aim to detect a difference, are fundamentally unsuited for this purpose. A non-significant p-value (e.g., p > 0.05) does not allow researchers to conclude that two methods are equivalent; it may simply indicate insufficient data to detect the existing difference [12] [2]. Equivalence testing, specifically the Two One-Sided Tests (TOST) procedure, directly addresses this need by statistically validating that two means differ by less than a pre-specified, clinically or analytically meaningful amount [13] [18]. This guide provides a comparative analysis of TOST versus traditional confidence intervals, offering experimental protocols and data interpretation frameworks essential for drug development professionals.
Conceptual Framework: TOST vs. Traditional Confidence Intervals
The Logic of the Two One-Sided Tests (TOST)
The TOST procedure operates by reversing the conventional roles of null and alternative hypotheses. It formally tests whether the true difference between two population means (μ₁ and μ₂) lies entirely within a pre-defined equivalence margin (-θ, θ) [13].
- Null Hypothesis (H₀): The difference between the means is large and clinically unacceptable (i.e., μ₂ – μ₁ ≤ –θ or μ₂ – μ₁ ≥ θ).
- Alternative Hypothesis (H₁): The difference between the means is small and practically negligible (i.e., –θ < μ₂ – μ₁ < θ).
The procedure conducts two separate one-sided t-tests against the lower and upper equivalence bounds. If both tests yield a statistically significant result, the null hypothesis of non-equivalence is rejected, allowing the researcher to conclude equivalence [13] [19]. The overall p-value for the TOST is taken as the larger of the two p-values from the one-sided tests [13].
The Confidence Interval Approach
A visually intuitive and statistically equivalent method involves constructing a 1 – 2α confidence interval for the mean difference. For a standard 5% significance level, a 90% confidence interval is constructed [13] [2]. Equivalence is concluded if this entire confidence interval falls completely within the equivalence margins (-θ, θ) [13] [20]. This approach is graphically summarized in the following decision logic diagram:
Experimental Protocols for TOST
Core Workflow for a Method Comparability Study
Implementing TOST requires a structured approach, from planning to execution. The following workflow outlines the key stages in a typical method comparability study, emphasizing the critical pre-specification of the equivalence margin.
Detailed Methodology
The protocol below is adapted from a cleanability assessment case study [18] and general guidance on comparability testing [2].
1. Objective: To demonstrate that the cleanability (measured as cleaning time) of a new protein product (Product Y) is equivalent to a validated reference product (Product A).
2. Experimental Design:
- Test and Reference: Product Y (test) vs. Product A (reference).
- Measurement: Cleaning time (in minutes) from a bench-scale model using spotted coupons.
- Sample Size: 18 independent replicates per product group, determined via a power analysis to achieve sufficient power (e.g., 80-90%) given the expected variability and the chosen equivalence margin [18] [2].
3. Data Collection:
- Cleaning times are recorded for each replicate in a randomized order to avoid bias.
- Data are collected in accordance with Good Manufacturing Practices (GMP).
4. Statistical Analysis Plan:
- Equivalence Margin (θ): Justified from historical data on the reference product. For example, θ = 4.48 minutes, calculated as two times the upper 95% confidence limit for the standard deviation of Product A's cleaning times [18].
- Analysis Method: TOST with α = 0.05 (corresponding to a 90% confidence interval).
- Software: Analysis can be performed using specialized statistical software like JMP, R (with the
TOSTERpackage), or Excel add-ins like QI Macros or XLSTAT [18] [19] [21].
5. Acceptance Criterion: The two products are considered equivalent if the 90% confidence interval for the difference in mean cleaning times (Product Y - Product A) lies entirely within the interval (-4.48, 4.48) [18].
Comparative Experimental Data and Interpretation
Case Study Results and Analysis
The following table summarizes the outcomes from two real-world case studies applying the above protocol, demonstrating both successful and failed equivalence [18].
Table 1: TOST Analysis of Cleanability for Protein Products
| Product Comparison | Sample Size (each) | Mean Cleaning Time (min) | Difference (B - A) | 90% CI of Difference | Equivalence Margin (θ) | Conclusion |
|---|---|---|---|---|---|---|
| Product A vs. Product B | 18 | A: 86.21, B: 152.85 | 66.64 min | (62.91, 70.36) | ±4.48 min | Not Equivalent. The entire CI is outside the margin [18]. |
| Product A vs. Product Y | 18 | A: 86.21, Y: 85.41 | -0.80 min | (-1.55, 0.06) | ±4.48 min | Equivalent. The entire CI is within the margin [18]. |
Interpretation of Outcomes
The case studies in Table 1 illustrate how the TOST procedure provides clear, defensible conclusions.
- Product A vs. Product B: The 90% confidence interval (62.91, 70.36) is far outside the equivalence margin of ±4.48. This leads to a rejection of the alternative hypothesis of equivalence. Furthermore, since the entire interval is positive, we can conclude that Product B is significantly more difficult to clean than Product A [18].
- Product A vs. Product Y: The 90% confidence interval (-1.55, 0.06) is completely contained within the equivalence margin of ±4.48. Therefore, the null hypothesis of non-equivalence is rejected, and it is concluded that the two products are equivalent in cleanability [18].
Essential Research Reagent Solutions
Successful execution of equivalence studies requires both statistical rigor and high-quality experimental materials. The following table details key reagents and their functions in the context of a bioanalytical method comparability study.
Table 2: Key Reagents and Materials for Method Comparability Studies
| Research Reagent / Material | Function in Experiment |
|---|---|
| Reference Standard | A well-characterized material with a known property (e.g., concentration, potency) that serves as the benchmark for comparison in the equivalence test [2]. |
| Test Article / Sample | The new product, material, or method whose performance is being evaluated for equivalence against the reference standard. |
| Validated Analytical Method | The procedure (e.g., HPLC, ELISA) used to measure the critical quality attribute. It must be validated to ensure accuracy, precision, and specificity to generate reliable data [22]. |
| Control Samples | Samples with known values used to monitor the performance and stability of the analytical method throughout the experimentation process. |
Regulatory and Practical Considerations
Setting the Equivalence Margin
The single most critical step in designing an equivalence test is the prospective justification of the equivalence margin (θ). This is a scientific and risk-based decision, not a statistical one [2] [23].
- Risk-Based Approach: Higher risks to product quality, safety, or efficacy warrant tighter (smaller) equivalence margins. For example, a critical quality attribute may allow only a 5-10% shift, whereas a lower-risk parameter may allow 11-25% [2].
- Considerations for Justification:
- Clinical Relevance: What difference would have no impact on patient safety or efficacy?
- Process Capability: What shift in the mean would lead to an unacceptable increase in out-of-specification (OOS) rates? [2]
- Analytical Variation: The margin should be set relative to the measurement uncertainty or biological variability of the method [23].
- Historical Data: As in the cleanability case study, historical data from a controlled dataset can be used to set a margin that accounts for natural variability [18].
TOST in the Regulatory Landscape
Equivalence testing is firmly embedded in regulatory guidance for the pharmaceutical industry.
- The ICH E9 guideline recognizes TOST as the standard for testing equivalence [24].
- The United States Pharmacopeia (USP) explicitly recommends equivalence testing over significance testing for demonstrating conformance, stating that a non-significant p-value is not evidence of equivalence [2].
- Regulatory bodies like the FDA require equivalence testing for demonstrating bioequivalence, where the confidence interval for the ratio of means must fall within 80%-125% [23], and for assessing comparability after process changes [18] [2].
In the context of method comparability acceptance criteria research, the choice of statistical tool is paramount. Traditional hypothesis tests and their associated 95% confidence intervals are designed to find differences and are inappropriate for proving equivalence. The TOST procedure, with its dual approach of two one-sided tests or a single 90% confidence interval, provides a statistically rigorous and logically sound framework for demonstrating that differences are practically insignificant. By prospectively defining a justified equivalence margin, following a structured experimental protocol, and correctly interpreting the resulting confidence intervals, researchers and drug development professionals can generate robust, defensible evidence of comparability to meet both scientific and regulatory standards.
In the pharmaceutical industry, demonstrating comparability following a manufacturing process change is a critical regulatory requirement. The foundation of a successful comparability study lies in a scientifically sound batch selection strategy, which ensures that pre- and post-change batches are representative of their respective processes. According to ICH Q5E, comparability does not require the materials to be identical but must demonstrate they are highly similar and that differences in quality attributes have no adverse impact upon safety or efficacy [10]. The selection of an appropriate number of batches and ensuring their representativeness provides the statistical power and confidence needed to draw meaningful conclusions from comparability data. This guide objectively compares different strategic approaches, providing a framework for researchers and drug development professionals to optimize their study designs.
Regulatory and Scientific Foundations
Regulatory guidelines emphasize a risk-based approach to comparability study design. The European Medicines Agency (EMA) draft guideline on topical products recommends comparison of at least three batches of both the reference and test product, often with at least 12 replicates per batch [25]. The U.S. Food and Drug Administration (FDA) similarly recommends a population bioequivalence approach for comparing relevant physical and chemical properties in guidance for specific topical products [25].
The primary objective is to demonstrate equivalence through a structured protocol that includes defined analytical methods, a statistical study design, and predefined acceptance criteria [2]. The strategy must account for inherent process variability, distinguishing between:
- Inter-batch variability: The natural variation in quality attributes between different manufacturing batches.
- Intra-batch variability: The variation observed among individual units within a single batch [25].
Failure to adequately account for these variabilities in the batch selection strategy can lead to studies that lack the statistical power to demonstrate equivalence, potentially requiring costly study repetition or regulatory delays.
Quantitative Batch Selection Recommendations
The required number of batches and units per batch is not fixed; it depends on the specific variability of the product and the sensitivity of the quality attributes being measured. The following tables summarize data-driven recommendations.
Table 1: Sample Size Scenarios Based on Variability and Expected Difference
| Inter-Batch Variability (%) | Intra-Batch Variability (%) | Expected T/R Difference (%) | Recommended Number of Batches | Recommended Units per Batch |
|---|---|---|---|---|
| Low (<2.5) | Low (<2.5) | 0 (No difference) | 3 | 6 |
| Low to Moderate (<5) | Low to Moderate (<5) | 2.5 – 5 | 6 | 12 |
| Moderate to High (>10) | Moderate to High (>10) | 2.5 – 5 | >6 | >12 |
Table 2: Risk-Based Scenarios for Equivalence Acceptance Criteria
| Risk Level | Typical Acceptance Criteria Range (as % of tolerance) | Applicable Scenarios |
|---|---|---|
| High | 5 – 10% | Changes to drug product formulation, manufacturing process changes impacting Critical Quality Attributes (CQAs). |
| Medium | 11 – 25% | Changes in raw material suppliers, site transfers for non-sterile products. |
| Low | 26 – 50% | Changes with minimal perceived risk to safety/efficacy, such as certain analytical procedure updates. |
Experimental Protocols for Batch Comparison
Statistical Protocol for Equivalence Testing
The Two One-Sided T-test (TOST) is a widely accepted method for demonstrating comparability [2]. This protocol ensures that the difference between pre- and post-change batches is within a pre-specified "equivalence margin."
- Step 1 – Define the Equivalence Margin (∆): Set the upper and lower practical limits (UPL and LPL) based on a risk assessment, product knowledge, and clinical relevance. For a medium-risk attribute like pH with a specification of LSL=7 and USL=8, a common margin is ±0.15 (15% of the tolerance) [2].
- Step 2 – Formulate Hypotheses:
- H₀₁: Mean difference ≤ -∆ (Inferiority)
- H₀₂: Mean difference ≥ ∆ (Inferiority)
- Hₐ: -∆ < Mean difference < ∆ (Equivalence)
- Step 3 – Calculate Sample Size: Use a sample size calculator for a single mean (difference from standard). For alpha=0.1 (0.05 per one-sided test) and sufficient power (e.g., 80%), the minimum sample size can be determined. For the pH example, a minimum sample size of 13 is required, with 15 often selected [2].
- Step 4 – Execute the Experiment: Test the predetermined number of units from the selected pre- and post-change batches.
- Step 5 – Perform Statistical Analysis: Conduct two one-sided t-tests. If both tests yield p-values < 0.05, the null hypotheses are rejected, and equivalence is concluded [2].
Protocol for Extended Characterization and Forced Degradation
For biologics, a comprehensive analytical comparison is crucial. This involves head-to-head testing beyond routine release analytics [10].
- Extended Characterization: This provides an orthogonal, finer-level detail of Critical Quality Attributes (CQAs). A typical testing panel for a monoclonal antibody includes:
- Primary Structure: Peptide mapping with LC-MS, Intact mass analysis (LC-ESI-TOF MS), Sequence variant analysis (SVA)
- Higher Order Structure: Size exclusion chromatography with multi-angle light scattering (SEC-MALS), Analytical ultracentrifugation (AUC)
- Purity and Impurities: Capillary electrophoresis (CE-SDS), Ion exchange chromatography (IEC)
- Potency: Cell-based bioassay [10]
- Forced Degradation Studies: These studies "pressure-test" the molecule to uncover potential differences in degradation pathways not seen in real-time stability. Standard stress conditions include:
- Thermal Stress: Incubation at elevated temperatures (e.g., 25°C, 40°C)
- pH Stress: Exposure to acidic and basic conditions
- Oxidative Stress: Exposure to chemicals like hydrogen peroxide
- Light Stress: As per ICH guidelines [10]
- The comparability of pre- and post-change batches is assessed by comparing the trendline slopes, bands, and peak patterns of the degradation profiles.
Diagram: Batch Comparability Study Workflow. This diagram outlines the key stages in designing and executing a comparability study, from objective definition to final conclusion.
Essential Research Reagent Solutions
The following table details key materials and solutions required for the analytical characterization of batches in a comparability study.
Table 3: Key Reagents for Extended Characterization and Forced Degradation Studies
| Research Reagent / Material | Function in Comparability Study |
|---|---|
| Reference Standard / Cell Bank | Serves as a benchmark for ensuring analytical method performance and provides a baseline for comparing pre- and post-change product quality attributes [10]. |
| Characterized Pre-Change Batches | Act as the reference material for head-to-head comparison. Batches should be representative and manufactured close in time to post-change batches to avoid age-related differences [10]. |
| Trypsin/Lys-C for Peptide Mapping | Enzymes used to digest the protein for detailed primary structure analysis and identification of post-translational modifications via Liquid Chromatography-Mass Spectrometry (LC-MS) [10]. |
| Stable Cell Line | Essential for conducting cell-based bioassays that measure the biological activity (potency) of the product, a critical quality attribute [10]. |
| Hydrogen Peroxide Solution | A common oxidizing agent used in forced degradation studies to simulate oxidative stress and understand the molecule's degradation pathways [10]. |
| LC-MS Grade Solvents | High-purity solvents (water, acetonitrile, methanol) with low UV absorbance and minimal contaminants are critical for sensitive analytical techniques like LC-MS to ensure accurate results [10]. |
A scientifically rigorous batch selection strategy is the cornerstone of a successful comparability study. The data and protocols presented demonstrate that the optimal number and representativeness of pre- and post-change batches are not one-size-fits-all but must be determined through a risk-based assessment of inter- and intra-batch variability. Employing a combination of rigorous statistical methods like equivalence testing and comprehensive analytical characterization provides the highest level of confidence for demonstrating comparability. By adhering to these structured approaches, drug developers can build robust data packages that satisfy regulatory requirements and ensure the continuous supply of high-quality medicines to patients.
In pharmaceutical development, the establishment of robust acceptance criteria is fundamental for demonstrating method comparability. While specification limits define the final acceptable quality attributes of a drug substance or product, acceptance criteria for analytical methods serve a different, equally critical purpose: they provide the documented evidence that an alternative analytical procedure is comparable to a standard or pharmacopoeial method [5]. This process is not merely a regulatory checkbox but a scientific exercise in risk management. The European Pharmacopoeia chapter 5.27, which addresses the "Comparability of alternative analytical procedures," underscores that the final responsibility for demonstrating comparability lies with the user and must be documented to the satisfaction of the competent authority [5]. This guide moves beyond basic specification limits to explore the strategic definition of acceptance criteria for both quantitative and qualitative methods, providing a structured framework for researchers and drug development professionals engaged in method development, validation, and transfer activities.
Theoretical Foundations: Quantitative vs. Qualitative Research Paradigms
The approach to defining acceptance criteria is fundamentally shaped by the nature of the method—whether it is rooted in quantitative or qualitative research paradigms. Understanding this distinction is crucial for selecting appropriate comparison strategies.
- Quantitative Research deals with numbers and statistics, aiming to objectively measure variables and test hypotheses through structured, predetermined designs [26] [27]. It answers questions about "how many" or "how much" and seeks generalizable results. In an analytical context, this translates to methods that generate numerical data, such as assay potency or impurity content.
- Qualitative Research, in contrast, deals with words and meanings [26]. It is exploratory and seeks to understand concepts, thoughts, or experiences through a subjective, flexible lens [27] [28]. In a scientific context, this does not refer to subjective opinion but to methods that characterize qualities, such as the identity of a peak in a chromatogram, its morphology in microscopy, or descriptive physical attributes.
The choice between these paradigms dictates the entire approach to method comparability. Table 1 summarizes the core differences that influence how acceptance criteria are established.
Table 1: Fundamental Differences Between Quantitative and Qualitative Research Approaches Influencing Acceptance Criteria
| Aspect | Quantitative Methods | Qualitative Methods |
|---|---|---|
| Core Objective | To test and confirm; to measure variables and test hypotheses [26] [27] | To explore and understand; to explore ideas, thoughts, and experiences [26] [27] |
| Nature of Data | Numerical, statistical [28] | Textual, descriptive, informational [28] |
| Research Approach | Deductive; used for testing relationships between variables [27] | Inductive; used for exploring concepts and experiences in more detail [26] |
| Sample Design | Larger sample sizes for statistical validity [29] | Smaller, focused samples for in-depth understanding [29] |
| Outcome | Produces objective, empirical data [27] | Produces rich, detailed insights into specific contexts [27] |
Defining Acceptance Criteria in a Regulatory Context
Acceptance criteria are specific, verifiable conditions that must be met to conclude that a product, process, or, in this context, an analytical method is acceptable [30] [31]. In the framework of method comparability, they are the predefined metrics that determine whether the results and performance of an alternative analytical procedure are comparable to those of a standard procedure [5]. Their primary function is to define the boundaries of success, mitigate risks of adopting a non-comparable method, and streamline testing by providing clear "pass/fail" standards [31]. According to regulatory guidance, the definition of these criteria should be based on the entirety of process knowledge and defined prior to running the comparability study [32] [5].
The Concept of Specification-Driven Acceptance Criteria
A modern, robust approach involves developing specification-driven acceptance criteria. This methodology leverages process knowledge and data to define intermediate acceptance criteria that are explicitly linked to the probability of meeting the final drug substance or product specification limits [32]. The novelty of this approach lies in basing acceptance criteria on pre-defined out-of-specification probabilities while accounting for manufacturing variability, moving beyond conventional statistical methods that merely describe historical data [32].
Comparative Analysis: Acceptance Criteria for Quantitative versus Qualitative Methods
The strategies for setting acceptance criteria differ significantly between quantitative and qualitative methods, reflecting their underlying paradigms.
Acceptance Criteria for Quantitative Methods
Quantitative methods demand statistically derived, numerical acceptance criteria. The focus is on equivalence testing of Analytical Procedure Performance Characteristics (APPCs).
Common APPCs & Acceptance Strategies:
- Accuracy: Often evaluated through a comparison of mean results between the new and standard procedures. An equivalence approach is used, where the confidence interval of the difference must fall within predefined equivalence margins (e.g., ±1.5%) [5].
- Precision: Comparison of variance (e.g., repeatability, intermediate precision) using statistical tests like the F-test. Acceptance criteria may specify a maximum allowable ratio of variances.
- Specificity/Selectivity: Demonstration that the alternative method can discriminate the analyte in the presence of potential interferents, often by spiking studies.
Statistical Foundation: The preferred approach is equivalence testing (or "difference testing"), not just significance testing. For instance, one may decide that the confidence intervals of the mean results of two procedures differ by no more than a defined amount at an acceptable confidence level [5]. This is superior to conventional approaches like setting limits at ±3 standard deviations (3SD), which rewards poor process control and punishes good control by being solely dependent on observed variance [32].
Acceptance Criteria for Qualitative Methods
For qualitative methods, acceptance criteria are necessarily more descriptive and focus on the correct identification or characterization of attributes.
- Common APPCs & Acceptance Strategies:
- Specificity: The primary focus. Acceptance criteria define the required ability to discriminate between closely related entities (e.g., identification of a microorganism, confirmation of a polymorphic form). This is often assessed through a set of challenge samples, with criteria requiring 100% correct identification.
- Robustness: The ability of the method to remain unaffected by small, deliberate variations in method parameters. Acceptance is based on the method's consistent performance across these varied conditions.
- Comparability of "Fingerprints": For complex methods like spectroscopic identity tests, acceptance criteria may involve a direct, point-by-point comparison of spectra or chromatograms to a reference standard, requiring a match exceeding a predefined threshold (e.g., >99.0%).
Table 2 provides a direct comparison of how acceptance criteria are applied to different attributes in quantitative versus qualitative methods.
Table 2: Comparison of Acceptance Criteria Application in Quantitative vs. Qualitative Methods
| Performance Characteristic | Application in Quantitative Methods | Application in Qualitative Methods |
|---|---|---|
| Accuracy | Equivalence of means within statistical confidence intervals (e.g., 95% CI within 98.0-102.0%) [5] | Not directly applicable in a numerical sense; superseded by Specificity. |
| Precision | Statistical comparison of variance (e.g., F-test for repeatability, p > 0.05) | Consistency in achieving correct identification/result across replicates and analysts. |
| Specificity/Selectivity | Demonstrated by no interference from placebo, and ability to quantify analyte in presence of impurities/degradants. | Demonstrated by 100% correct identification from a panel of challenge samples, including near-neighbors. |
| Core Acceptance Logic | Equivalence Testing: Is the numerical output of the new method statistically equivalent to the standard method? [5] | Descriptive Matching: Does the new method correctly identify/characterize the attribute to the same conclusion as the standard method? |
Experimental Protocols for Method Comparability
A well-defined experimental protocol is the backbone of a successful comparability study. The following workflow, detailed in the diagram below, outlines the key stages from planning to conclusion.
Protocol for a Quantitative Comparability Study (e.g., HPLC Assay)
This protocol provides a detailed methodology for comparing an alternative quantitative method against a pharmacopoeial procedure.
- 1. Study Objective: To demonstrate that the alternative HPLC assay method for Drug Substance X is comparable to the USP monograph method in terms of accuracy and precision.
- 2. Materials and Reagents:
- Drug Substance X reference standard
- Placebo formulation
- HPLC-grade solvents (acetonitrile, water)
- Two HPLC systems: one qualified for the standard method, one for the alternative method.
- 3. Experimental Design:
- Prepare a calibration curve and quality control (QC) samples at 50%, 100%, and 150% of the target concentration (n=6 for each level) using both methods.
- The samples will be a mixture of Drug Substance X and placebo to mimic the product matrix.
- A second analyst will repeat the 100% QC level (n=6) on a different day to assess intermediate precision.
- 4. Data Analysis:
- Accuracy: Calculate the mean percent recovery for each QC level for both methods. Perform an equivalence test (e.g., two one-sided t-tests, TOST) to show that the difference in mean recovery between the two methods is within ±2.0% at each level (α=0.05).
- Precision: Compare the repeatability (within-day) and intermediate precision (between-day/analyst) of the two methods at the 100% level using an F-test (α=0.05). The 90% confidence interval of the ratio of variances must be within 0.5 to 2.0.
- 5. Predefined Acceptance Criteria:
- The 90% confidence interval for the difference in mean recovery at all QC levels must be within ±2.0%.
- The 90% confidence interval for the ratio of variances (alternative/standard) for precision at 100% QC must be within 0.5 to 2.0.
Protocol for a Qualitative Comparability Study (e.g., FTIR Identity Test)
This protocol outlines the comparison for a qualitative identity method.
- 1. Study Objective: To demonstrate that the alternative FTIR identity test for Active Y is comparable to the Ph. Eur. method.
- 2. Materials and Reagents:
- Active Y reference standard
- Structurally similar compounds (potential impurities, degradants, or isomers)
- Potassium bromide (KBr) for pellet preparation or ATR crystal accessory.
- 3. Experimental Design:
- Obtain spectra of the Active Y reference standard using both the standard and alternative methods (n=5).
- Obtain spectra of five different lots of Active Y drug substance using both methods.
- Obtain spectra of three structurally related compounds using both methods as negative controls.
- 4. Data Analysis:
- Visually and algorithmically compare the spectra from the alternative method to those from the standard method.
- For the reference standard and drug substance lots, the spectral correlation coefficient (or other validated algorithm) when compared to the standard method's reference spectrum must be ≥ 0.99.
- For the structurally related compounds, the spectral correlation must be ≤ 0.90, demonstrating discrimination.
- 5. Predefined Acceptance Criteria:
- 100% of the spectra for Active Y (reference and drug substance lots) must meet the similarity threshold (≥ 0.99).
- 100% of the spectra for the structurally related compounds must fail the similarity threshold (≤ 0.90).
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials required for the experimental protocols described above, with a brief explanation of their critical function in ensuring reliable and comparable results.
Table 3: Essential Research Reagent Solutions for Method Comparability Studies
| Item | Function in Experiment |
|---|---|
| Certified Reference Standard | Provides the benchmark for identity, purity, and potency against which all measurements are traceable; its quality is non-negotiable for a valid comparison. |
| Placebo/Blank Matrix | Allows for the demonstration of method specificity/selectivity by confirming the absence of interference from non-active components in the sample. |
| Challenger Compounds (Impurities, Degradants, Isomers) | Used in specificity testing for both quantitative and qualitative methods to prove the method can distinguish the analyte from closely related species. |
| HPLC-Grade Solvents | Ensure the reproducibility of mobile phase preparation and prevent baseline noise or spurious peaks that could compromise quantitative accuracy and precision. |
| Standardized Materials for Spectroscopy (e.g., KBr) | Provide a consistent and inert medium for sample preparation in techniques like FTIR, ensuring spectral quality is comparable between methods. |
Data Presentation and Statistical Evaluation
The presentation of data from a comparability study must be clear, concise, and focused on the pre-defined acceptance criteria. The following diagram illustrates the logical flow of the statistical and decision-making process for a quantitative study, culminating in a conclusion about equivalence.
Summary of Key Statistical Outcomes: The core of a quantitative comparability study is the equivalence test. For instance, in a study comparing an alternative bioassay to a compendial one, the acceptance criteria might require that the confidence intervals of the mean results of the two procedures differ by no more than a defined amount at an acceptable confidence level [5]. When this equivalence is accepted, the alternative procedure may be considered statistically equivalent [5].
Defining acceptance criteria for analytical methods requires a nuanced approach that moves beyond simple specification limits. The paradigm—quantitative or qualitative—dictates the fundamental strategy. For quantitative methods, the emphasis is on statistical equivalence testing of performance characteristics like accuracy and precision, using predefined confidence intervals and equivalence margins. For qualitative methods, the focus shifts to descriptive and binary outcomes, such as 100% correct identification against a panel of challengers. The modern, specification-driven approach, which links intermediate acceptance criteria to the probability of meeting final product quality attributes, represents a superior and more scientifically rigorous framework [32]. By adopting these tailored, data-driven strategies, researchers and drug development professionals can robustly demonstrate method comparability, thereby ensuring product quality, patient safety, and regulatory compliance throughout the product lifecycle.
In method comparability and bioequivalence studies within drug development, achieving statistically defensible results is paramount. A cornerstone of this process is the rigorous planning of sample size and power calculations. These calculations ensure that a study is capable of reliably detecting a difference—or proving equivalence—between two methods or treatments, thereby supporting robust scientific and regulatory decisions. An underpowered study risks overlooking meaningful differences (Type II errors), while an overpowered study wastes resources and potentially exposes more subjects than necessary to experimental procedures [33] [34]. This guide objectively compares the predominant statistical approaches for sample size determination, providing experimental data and protocols to equip researchers with the tools for defensible study design.
Core Concepts: Error Types and Key Parameters
Understanding Type I and Type II Errors
Statistical hypothesis testing revolves around two potential errors. A Type I error (α), or a "false positive," occurs when a study incorrectly concludes that a difference exists. The threshold for this error (commonly α=0.05) is the significance level. Conversely, a Type II error (β), or a "false negative," happens when a study fails to detect a true difference [35] [34]. Statistical power, defined as 1-β, is the probability that the study will correctly reject the null hypothesis when there is a true effect to be found. The ideal power for a study is conventionally set at 80% or 90% [33] [35].
The Four Key Inputs for Calculation
All sample size calculations require these four essential components [34] [36]:
- Significance Level (Alpha, α): The risk of a Type I error, typically set at 0.05.
- Power (1-β): The desired probability of detecting an effect, typically 0.8 or 0.9.
- Effect Size (ES): The minimum difference or relationship the study must detect to be scientifically or clinically meaningful. This is a critical and often challenging value to define [37].
- Variability (Standard Deviation, σ): The expected standard deviation of the outcome measure, often estimated from pilot studies or previous literature [33].
The following workflow outlines the logical sequence and key relationships for determining sample size and power.
Comparative Analysis of Statistical Approaches
Different study objectives and data types necessitate distinct statistical methodologies for sample size calculation. The table below summarizes the purpose, key formula, and experimental context for the most common tests used in method comparability and clinical research.
Table 1: Comparison of Sample Size Calculation Methodologies
| Statistical Test | Primary Research Objective | Key Formula Components | Common Experimental Context |
|---|---|---|---|
| Two One-Sided Tests (TOST) | To demonstrate equivalence between two methods or formulations [38]. | Equivalence margin (Δ), alpha (α), power (1-β), standard deviation (σ) [38]. | Bioequivalence studies, analytical method comparability, demonstrating therapeutic equivalence [38]. |
| Two-Sample t-test | To detect a difference between the means of two independent groups [34]. | Alpha (α), power (1-β), effect size (difference in means, d), standard deviation (σ) [34] [36]. | Comparing the average potency of two drug batches, or the mean response of a treatment vs. control group [34]. |
| Test of Two Proportions | To detect a difference in the event rates (proportions) between two groups [35]. | Alpha (α), power (1-β), the two proportions (p1, p2) [35]. | Comparing response rates, success rates, or the proportion of subjects with an adverse event between two treatments. |
| ANOVA | To detect a difference in means across three or more independent groups [39]. | Alpha (α), power (1-β), effect size (e.g., F-statistic), number of groups, standard deviation (σ). | Comparing the effects of multiple drug doses or several different analytical methods on a continuous outcome. |
Experimental Protocols for Key Scenarios
Protocol 1: Equivalence Testing via Two One-Sided Tests (TOST)
The TOST procedure is the gold standard for demonstrating equivalence, a common goal in method comparability studies [38].
- Objective: To demonstrate that the difference between a new method (Test) and a standard method (Reference) is within a pre-defined equivalence margin (Δ).
- Hypotheses:
- H₀: True mean difference ≤ -Δ OR True mean difference ≥ Δ (The methods are not equivalent).
- H₁: -Δ < True mean difference < Δ (The methods are equivalent).
- Procedure:
- Define the Equivalence Margin (Δ): Set Δ based on regulatory guidance or scientific consensus. This is the largest difference that is considered clinically or analytically unimportant [38].
- Specify Parameters: Set α=0.05 and power=0.8 or 0.9. Estimate the expected standard deviation (σ) from prior data.
- Calculate Sample Size: Use statistical software with the exact power function for TOST, inputting Δ, σ, α, and power to determine the required sample size per group [38].
- Conduct Experiment & Analysis: Run the study, collecting measurements from both methods. Calculate the 90% confidence interval for the mean difference (Test - Reference). If the entire 90% CI falls within the range (-Δ, Δ), the two methods are declared statistically equivalent [38].
Protocol 2: Superiority/Difference Testing via Two-Sample t-test
This protocol is used when the goal is to prove that one method is superior to another, or simply to detect a statistically significant difference.
- Objective: To detect a specified difference (d) between the means of two independent groups.
- Hypotheses:
- H₀: μ₁ = μ₂ (No difference between group means).
- H₁: μ₁ ≠ μ₂ (A difference exists).
- Procedure:
- Define the Effect Size (d): Determine the minimum difference (d) that is scientifically meaningful. This requires subject-area knowledge [36] [37].
- Estimate Variability (σ): Obtain an estimate of the common standard deviation from a pilot study or previous literature [33].
- Calculate Sample Size: Use the formula for a two-sample t-test [34]:
n per group = 2 * [(Zα/2 + Zβ) * σ / d]^2, where Zα/2 is 1.96 for α=0.05 and Zβ is 0.84 for 80% power. - Conduct Experiment & Analysis: Randomly assign samples to the two groups. After data collection, perform a two-sample t-test. A p-value less than 0.05 allows rejection of H₀ in favor of H₁.
The Scientist's Toolkit: Essential Reagents for Statistical Power
Table 2: Key Research Reagents and Resources for Power Analysis
| Tool / Resource | Function | Application Example |
|---|---|---|
| Pilot Study Data | Provides preliminary estimates of the standard deviation (σ) and baseline event rates, which are critical for accurate sample size calculation [33] [34]. | Before a large bioequivalence study, a small pilot with 10-15 subjects is run to estimate the variability in pharmacokinetic parameters. |
R Package PowerTOST |
A specialized statistical software tool for performing power and sample size calculations for (bio)equivalence studies [40]. | Used to compute the exact sample size required for a TOST procedure using the methodology described in [38]. |
| Minimum Detectable Effect (MDE) | The smallest effect size that a study can detect with a given level of power and significance. It is not a universal rule but must be meaningful to stakeholders [37]. | A partner organization states they would only switch to a new manufacturing process if it increases yield by at least 5%; this 5% becomes the MDE. |
| SAS/IML & R Code | Custom statistical programming scripts that implement exact power and sample size calculations, especially for complex designs like TOST with specific allocation constraints [38]. | Used to calculate optimal sample sizes for an equivalence study where the ratio of group sizes is fixed in advance or where there is a budget constraint [38]. |
| Intra-Cluster Correlation (ICC) | A measure used in clustered study designs (e.g., patients within clinics) to account for the similarity of responses within a cluster. It directly impacts the required sample size [37]. | When randomizing by clinic in a multi-center trial, the ICC for the primary outcome is estimated from previous studies and incorporated into the sample size calculation to ensure adequate power. |
A statistically defensible study is not an accident but the result of meticulous pre-planning. As detailed in this guide, the choice of statistical approach—whether TOST for equivalence or a t-test for difference—must be driven by the explicit research objective. The calculated sample size is not a standalone number but a function of the defined alpha, power, effect size, and variability. By adopting these protocols and utilizing the outlined toolkit, researchers and drug development professionals can design method comparability studies that are not only efficient and ethical but also capable of producing compelling, defensible evidence for regulatory and scientific evaluation.
Anticipating Challenges: Risk Mitigation and Protocol Optimization
Common Pitfalls in Comparability Studies and How to Avoid Them
In the development of biological products, comparability studies are critical assessments conducted to ensure that a product remains safe, pure, and potent after a manufacturing change [41]. For researchers and drug development professionals, navigating these studies is a core component of method comparability acceptance criteria research. The fundamental goal is to demonstrate that the pre-change and post-change products are highly similar and that the manufacturing change has no adverse impact on the product's quality, safety, or efficacy [42]. Despite their importance, these studies are fraught with challenges, from strategic missteps to technical analytical failures. This guide outlines the most common pitfalls encountered and provides a structured, evidence-based framework for avoiding them, ensuring robust and defensible comparability conclusions.
Common Pitfalls and Strategic Solutions
A successful comparability exercise relies on careful planning, robust analytical tools, and a deep understanding of the product and process. The following pitfalls, if unaddressed, can jeopardize the entire study.
Pitfall 1: Inadequate Planning and Late-Stage Process Changes
One of the most significant strategic errors is a failure to plan for manufacturing changes early in the product development lifecycle.
- The Challenge: Making major changes to the manufacturing process after a pivotal clinical trial (typically Phase III) triggers the need for a complex comparability exercise [42]. For complex products like cell and gene therapies, this is especially "difficult and cumbersome" because the living, cell-based product is "not comparable by definition" [43]. This can lead to significant delays in regulatory submissions for life-saving medicines [44].
- The Solution: Plan manufacturing needs years in advance. Anticipate scale-up and process improvements to lock down the manufacturing process before initiating pivotal clinical trials [43] [42]. Whenever possible, manufacture the clinical trial material intended for the registrational study at commercial scale to minimize the need for comparability exercises prior to approval [44].
Pitfall 2: Applying a "One-Size-Fits-All" Approach
Assuming that a standard comparability protocol can be applied universally across different products and manufacturing changes is a common oversight.
- The Challenge: Comparability assessments are not hierarchical or uniform. The most appropriate strategy depends on multiple factors, including the type of molecule, the extent of the manufacturing change, and the stage of clinical development [44].
- The Solution: Adopt a risk-based approach. Design the comparability study by systematically considering the product's risk level, categorizing the type of CMC change (e.g., minor, moderate, major), and thoroughly understanding the outcome of the analytical comparability exercise [44]. This ensures that resources are focused on the most critical aspects of the product.
Pitfall 3: Misapplication of Statistical Tests
Using inappropriate statistical methods for data analysis can lead to incorrect conclusions about product comparability.
- The Challenge: Using statistical significance testing (e.g., a t-test seeking a p-value > 0.05) is not the same as demonstrating comparability. A non-significant p-value merely indicates insufficient evidence to conclude a difference; it does not provide positive evidence that the products are equivalent [2]. This can fail to detect practically meaningful differences.
- The Solution: Use equivalence testing (e.g., the Two One-Sided T-test, or TOST) to demonstrate practical significance [2]. This method proves that the difference between two products is smaller than a pre-defined, clinically relevant acceptance criterion. The acceptance criteria should be risk-based, informed by scientific knowledge and the potential impact on process capability and out-of-specification (OOS) rates [2].
Pitfall 4: Overlooking the Impact of Raw and Starting Materials
Forgetting that changes in raw materials can be as impactful as changes in the core manufacturing process itself.
- The Challenge: Changes in critical raw materials of biological origin, such as human serum or recombinant reagents, can significantly affect the quality of the final product, especially for cell-based products [43]. The inherent variability of these starting materials adds another layer of complexity [42].
- The Solution: Establish stringent specifications for raw and starting materials early in development. Justify these specifications based on manufacturing process requirements and, where possible, set wide but validated acceptance limits to accommodate natural variation without affecting final product quality [42].
Pitfall 5: Relying on Insufficient or Non-Robust Analytical Data
Basing comparability conclusions on limited analytical data or methods that are not fit-for-purpose.
- The Challenge: The analytical toolbox may be inadequate to detect subtle but meaningful differences in product attributes. Potency and mode of action assays are often the most complex yet most critical for assessing comparability [42].
- The Solution: Employ extended characterization that goes beyond routine release tests. This includes stress studies to compare degradation profiles and the use of advanced analytical methods like the Mass Spectrometry-based Multi-Attribute Method (MAM), which can simultaneously monitor multiple critical quality attributes (CQAs) such as oxidation, deamidation, and glycosylation with high specificity [45].
Experimental Protocols for Robust Comparability
A robust comparability study is built on a foundation of well-designed experiments. Below are detailed methodologies for key experiments cited in modern comparability exercises.
Equivalence Testing Protocol for Analytical Data
This protocol uses statistical equivalence testing to compare a specific quality attribute (e.g., pH, potency, concentration) between the pre-change and post-change product.
- Objective: To demonstrate with high statistical confidence that the mean value of a specific attribute in the post-change product is practically equivalent to that of the pre-change product.
- Methodology:
- Define Acceptance Criteria: Set the Upper Practical Limit (UPL) and Lower Practical Limit (LPL) based on a risk assessment. For example, for a medium-risk attribute with a specification of 7.0-8.0, the practical limits could be set at ±0.15 (15% of the tolerance) [2].
- Determine Sample Size: Use a sample size calculator for a single mean (difference from standard) to ensure the study has sufficient statistical power (typically 80-90%). For an alpha of 0.1 (0.05 for each one-sided test), a minimum sample size might be 13-15 per group [2].
- Perform the Two One-Sided T-Tests (TOST):
- Null Hypothesis 1: The true mean difference is less than or equal to the LPL.
- Null Hypothesis 2: The true mean difference is greater than or equal to the UPL.
- Reject both null hypotheses if both one-sided p-values are < 0.05.
- Analyze and Conclude: If both p-values are significant, conclude that the mean difference is statistically within the equivalence limits. Always report the confidence intervals for the difference [2].
Stress Study Protocol for Degradation Pathway Comparison
This protocol uses accelerated stability studies to uncover differences in degradation profiles that may not be apparent under normal storage conditions.
- Objective: To qualitatively and quantitatively compare the degradation rates and pathways of the pre-change and post-change products under stressed conditions.
- Methodology:
- Study Design: Conduct side-by-side testing of both products. Expose them to high-temperature stress conditions, typically 15–20 °C below the melting temperature (Tm), for durations ranging from one week to two months [45].
- Sampling and Analysis: Collect samples at multiple time points. Analyze them using a suite of orthogonal analytical methods, such as SE-HPLC for aggregates, CE-SDS for fragmentation, and IEX-HPLC for charge variants.
- Data Evaluation:
- Qualitative: Compare chromatographic and electrophoretic profiles at each time point, looking for the appearance of new peaks or changes in peak shapes [45].
- Quantitative: Plot the degradation rates for key attributes (e.g., % aggregates over time). Perform a statistical assessment (e.g., test for homogeneity of slopes) to determine if the degradation rates are comparable between the two products [45].
Population Pharmacokinetic (PopPK) Protocol for Bridging Studies
A "non-traditional" clinical pharmacology approach to streamline pharmacokinetic (PK) comparability assessments, particularly useful in expedited development programs [44].
- Objective: To use popPK modeling to compare the exposure profiles of the pre-change and post-change products without requiring a dedicated, powered bioequivalence study.
- Methodology:
- Trial Design: In a small cohort of patients (e.g., n=28), randomly assign them to treatment sequences where all patients receive both the pre-change and post-change product in different treatment cycles [44].
- Pharmacokinetic Sampling: Obtain rich or sparse PK sampling at multiple time points over the course of the study [44].
- Modeling and Analysis:
- Develop a structural popPK model using historical data from the pre-change product.
- Apply this model to the new PK data from the study comparing both products.
- The popPK model predicts whether the key PK parameters (e.g., clearance, volume of distribution) are comparable between the two products. This can be supplemented with Non-Compartmental Analysis (NCA) to show that the 90% confidence intervals for exposure metrics (e.g., AUC) fall within the 0.8-1.25 range [44].
Data Presentation: Quantitative Comparisons
The following tables summarize key quantitative data and acceptance criteria essential for designing and interpreting comparability studies.
Table 1: Risk-Based Acceptance Criteria for Equivalence Testing
| Risk Level | Typical Acceptance Criteria (as % of tolerance) | Example for a Parameter with 7.0-8.0 Specification (Tolerance=1.0) | Justification |
|---|---|---|---|
| High | 5-10% | ±0.05 to ±0.10 | Small practical differences allowed to minimize patient risk [2]. |
| Medium | 11-25% | ±0.11 to ±0.25 | Balance between risk and process capability [2]. |
| Low | 26-50% | ±0.26 to ±0.50 | Larger differences are acceptable with minimal impact on safety/efficacy [2]. |
Table 2: Comparison of Traditional vs. Non-Traditional PK Comparability Approaches
| Aspect | Traditional Powered BE Study | Non-Traditional PopPK Approach |
|---|---|---|
| Study Design | Dedicated, parallel-group or crossover study in healthy volunteers or patients [44]. | Integrated into clinical trials using sparse or rich sampling in the patient population [44]. |
| Sample Size | Large, powered to show bioequivalence [44]. | Can be smaller (e.g., dozens of patients) [44]. |
| Key Analysis | Non-Compartmental Analysis (NCA) with 90% CI for AUC and Cmax falling within 80-125% [44]. | Population PK modeling to compare parameters; often supplemented with NCA [44]. |
| Timeline Impact | Can lead to significant delays in regulatory submissions [44]. | Potentially streamlines development in expedited programs [44]. |
| Regulatory Acceptance | Well-established and widely accepted. | Gaining traction but not yet considered sufficient alone; used in case examples like dinutuximab [44]. |
Visualizing Comparability Strategy and Workflows
Diagram 1: Risk-Based Decision Framework for Comparability Assessments
This diagram visualizes a systematic, risk-based approach to planning comparability studies, as discussed in industry workshops [44].
Diagram 2: Experimental Workflow for a Comprehensive Comparability Exercise
This diagram outlines the key phases and activities in a typical comparability study, from planning to reporting.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful comparability study relies on a suite of well-characterized reagents and advanced analytical instruments.
Table 3: Key Research Reagent Solutions for Comparability Studies
| Item | Function in Comparability Studies | Key Considerations |
|---|---|---|
| Reference Standard | A fully characterized sample of the pre-change material used as a benchmark for all side-by-side analyses [41] [45]. | Critical for ensuring the validity of the comparison; must be well-characterized and stable. |
| Cell-Based Potency Assay | Measures the biological activity of the product relative to its mechanism of action; often the most critical assay for assessing comparability [42]. | Must be relevant to the clinical mechanism of action and demonstrate sufficient precision and accuracy to detect meaningful differences. |
| Mass Spectrometry (MS) Reagents | Used in peptide mapping for the Multi-Attribute Method (MAM) to directly monitor multiple CQAs (e.g., oxidation, deamidation) [45]. | Requires high-purity trypsin and other enzymes, as well as LC-MS grade solvents for reproducible results. |
| Container-Closure Integrity Test Systems | Ensure the primary packaging (e.g., vials, syringes) maintains sterility and product quality after a change. Methods include headspace analysis and high-voltage leak detection [45]. | Method selection depends on the container-closure system, drug product, and specific leak concern [45]. |
| Stressed/Forced Degradation Study Materials | Used to accelerate product degradation and compare the degradation profiles of pre- and post-change products, revealing subtle differences [45]. | Requires controlled stability chambers and qualified analytical methods to monitor degradation over time. |
In pharmaceutical development, demonstrating analytical method comparability is essential for ensuring consistent product quality when method modifications become necessary. Method comparability evaluates whether a modified analytical procedure yields results sufficiently similar to the original method, ensuring consistent monitoring of drug substance and product quality attributes [1]. Conversely, non-comparability occurs when statistical or pre-defined acceptance criteria are not met, indicating that the modified method performs significantly differently from the original procedure. Such failures necessitate a structured investigation to determine the root cause and implement corrective actions, as they may impact the ability to monitor critical quality attributes (CQAs) effectively.
Establishing method comparability follows a risk-based approach where the rigor of testing aligns with the potential impact on product quality. As outlined by ICH Q14, analytical procedure modifications require assessment through either comparability or equivalency studies [1]. Comparability studies typically suffice for low-risk changes with minimal impact on product quality, while equivalency studies require more comprehensive assessment, often including full validation, to demonstrate a replacement method performs equal to or better than the original [1]. These studies are foundational to a robust control strategy and form part of the regulatory submissions requiring health authority approval prior to implementation.
Experimental Protocols for Assessing Comparability
Study Design and Statistical Approaches
A well-designed comparability study incorporates side-by-side testing of representative samples using both the original and modified analytical methods [1]. The United States Pharmacopeia (USP) <1010> provides valuable statistical tools for designing, executing, and evaluating equivalency protocols, though application requires proficient understanding of statistics [22]. For demonstrating comparability, equivalence testing is preferred over significance testing, as it confirms that differences between methods are practically insignificant rather than merely statistically undetectable [2].
The Two One-Sided T-test (TOST) approach provides a statistically rigorous framework for establishing equivalence [2]. This method tests whether the difference between two methods is significantly lower than the upper practical limit and significantly higher than the lower practical limit. The TOST approach involves:
- Setting risk-based acceptance criteria: Practical limits are established based on scientific knowledge, product experience, and clinical relevance [2]. For high-risk parameters affecting product safety and efficacy, tighter acceptance criteria (e.g., 5-10% difference) are appropriate, while medium-risk parameters may allow 11-25% differences [2].
- Calculating appropriate sample size: Adequate power (typically 80-90%) must be ensured to detect practically significant differences. Sample size calculations incorporate the acceptable difference (δ), estimated variability (s), and desired statistical power [2].
- Conducting statistical analysis: The two one-sided t-tests are performed against the pre-defined upper and lower practical limits. If both tests reject the null hypothesis (p < 0.05), the methods are considered equivalent [2].
Table 1: Risk-Based Acceptance Criteria for Equivalence Testing
| Risk Level | Typical Acceptance Criteria Range | Application Examples |
|---|---|---|
| High Risk | 5-10% | Potency, impurities with toxicological concerns |
| Medium Risk | 11-25% | Dissolution, identity tests, residual solvents |
| Low Risk | 26-50% | Physicochemical properties, appearance |
Key Reagents and Research Solutions
Successful comparability studies require carefully selected reagents and materials that ensure reliability and reproducibility. The following table outlines essential research solutions for conducting robust comparability assessments:
Table 2: Essential Research Reagent Solutions for Comparability Studies
| Research Solution | Function in Comparability Studies | Critical Quality Attributes |
|---|---|---|
| Reference Standards | Provides benchmark for method performance comparison; ensures accuracy and system suitability [2] | Certified purity, stability, traceability to primary standards |
| System Suitability Solutions | Verifies chromatographic system resolution, precision, and sensitivity before analysis | Well-characterized peak profile, stability, representative of method conditions |
| Representative Test Samples | Enables side-by-side comparison of original and modified methods [1] | Representative of actual product variability, covers specification range |
| Quality Control Materials | Monitors analytical performance throughout the study; detects analytical drift | Established acceptance criteria, long-term stability, homogeneous distribution |
Systematic Root-Cause Analysis for Non-Comparability
When comparability studies fail to demonstrate equivalence, a structured root-cause analysis (RCA) is essential to identify the underlying factors responsible for the methodological divergence. The investigation should follow a systematic workflow that progresses from analytical instrumentation to method parameters and sample-related considerations.
The following diagram illustrates the logical workflow for conducting a comprehensive root-cause analysis when faced with non-comparability:
Analytical Instrumentation Assessment
The investigation should begin with comprehensive instrument qualification and verification. This includes examining detector performance for sensitivity drift or linearity issues, pump systems for composition accuracy and flow rate precision, autosampler for injection volume accuracy and carryover, and column oven for temperature stability [22]. Performance verification should employ certified reference materials and system suitability tests that challenge the critical parameters of the method. Any deviation from established performance specifications should be documented and correlated with the observed analytical discrepancies.
Reagent and Material Investigation
Method differences may stem from variations in reagent quality, mobile phase composition, or reference standard integrity. Key considerations include supplier qualification, lot-to-lot variability testing, preparation documentation review, and storage condition verification [22]. For compendial methods, any alternative methods used must be thoroughly validated against the official method to ensure equivalent performance [22]. Reagent-related issues often manifest as changes in selectivity, baseline noise, or retention time shifts in chromatographic methods.
Method Parameter Optimization
Subtle modifications in method parameters may significantly impact method performance even when within the method's operable design region. The investigation should focus on critical method parameters identified during development, including pH adjustments, mobile phase composition, gradient profiles, temperature settings, and detection wavelengths [1]. Understanding the method operable design region (MODR) provides flexibility in method parameters while maintaining equivalent performance [22]. If the original and modified methods have no overlap in their MODR, experimental equivalence studies become necessary [22].
Sample Compatibility and Stability
Sample-related factors constitute a frequent source of non-comparability, particularly when method modifications alter the sample-solvent interaction. Investigation should address sample preparation techniques, extraction efficiency, filter compatibility, auto-sampler stability, and solution stability over the analysis timeframe. For methods with increased sensitivity, previously negligible degradation pathways may become significant, necessitating enhanced stabilization measures or modified handling procedures.
Table 3: Common Root-Causes of Non-Comparability and Investigation Approaches
| Root-Cause Category | Specific Failure Modes | Investigation Approach |
|---|---|---|
| Instrument-Related | Detector drift, pump malfunctions, column heater instability | Preventive maintenance records review, system suitability test trend analysis |
| Reagent-Related | Lot-to-lot variability, supplier changes, degradation | Side-by-side testing with different lots, certificate of analysis review |
| Method Parameter | Outside MODR, incorrect parameter transfer, unintended changes | Experimental design to map parameter effects, robustness testing data review |
| Sample-Related | Instability in new solvents, incomplete extraction, filter adsorption | Stability-indicating studies, extraction efficiency profiling, filter compatibility testing |
Protocol Refinement Strategies
After identifying root causes, protocol refinement addresses the deficiencies while maintaining methodological robustness. The refinement process should follow a structured approach that incorporates lifecycle management principles as outlined in ICH Q14 [1].
The following diagram outlines the systematic approach to refining analytical protocols after identifying root causes of non-comparability:
Method Operable Design Region (MODR) Expansion
Refining the MODR establishes proven acceptable ranges for critical method parameters that ensure robust method performance [22]. This expansion involves systematic experimentation to define parameter boundaries, edge-of-failure testing to determine operational limits, and robustness validation within the expanded ranges. A well-defined MODR provides operational flexibility while maintaining data comparability, reducing the likelihood of future non-comparability issues when minor adjustments are necessary.
Enhanced System Suitability Criteria
Strengthened system suitability requirements provide ongoing verification of method performance. Refinements may include tighter acceptance criteria for critical resolution pairs, additional tests for sensitivity or precision, system precision thresholds that account for observed variability, and reference standard verification to detect reagent degradation [22]. These enhanced controls serve as early warning indicators of potential comparability issues during routine method application.
Targeted Method Validation
Protocol refinement should include selective re-validation addressing the specific areas where non-comparability was observed. This targeted approach focuses on accuracy profiles demonstrating equivalent recovery, precision assessment under intermediate conditions, specificity verification for known interferences, and robustness testing across the MODR [1]. The validation should demonstrate that the refined method controls the previously identified failure modes while maintaining equivalent performance to the original method.
Knowledge Management and Change Control
Comprehensive documentation of the root-cause analysis and refinement process creates valuable organizational knowledge [1]. This includes revised procedures incorporating lessons learned, enhanced change control processes that address identified gaps, training materials highlighting critical method attributes, and technical transfer documentation that explicitly addresses comparability risks. Effective knowledge management prevents recurrence of similar non-comparability issues across the organization.
Handling non-comparability requires a systematic approach rooted in sound scientific principles and quality risk management. Through structured root-cause analysis followed by targeted protocol refinement, organizations can transform method failures into opportunities for enhanced method understanding and robustness. The strategies outlined—encompassing rigorous investigation, statistical equivalence testing, MODR expansion, and enhanced controls—provide a framework for restoring confidence in analytical methods while maintaining regulatory compliance. As the pharmaceutical industry continues to embrace analytical procedure lifecycle management under ICH Q14, these approaches to addressing non-comparability will become increasingly integral to sustainable method performance throughout a product's lifecycle.
Leveraging Extended Characterization and Forced Degradation Studies for Deeper Insight
In the development of biopharmaceuticals, extended characterization and forced degradation studies serve as indispensable scientific tools that provide deep molecular insights far beyond standard quality control testing. These studies intentionally expose drug substances and products to stress conditions more severe than normal storage environments, systematically generating and profiling degradation products that could impact drug safety and efficacy [46] [47]. For recombinant monoclonal antibodies and other complex biologics, even minor changes in the manufacturing process can significantly impact critical quality attributes (CQAs), making these studies essential for demonstrating comparability between pre- and post-change material as outlined in ICH Q5E guidelines [48] [10]. The forced degradation study is not designed to establish qualitative or quantitative limits for change but rather to understand degradation pathways and develop stability-indicating methods [49] [50].
The pharmaceutical industry employs forced degradation studies throughout the product lifecycle, from early candidate selection to post-approval changes [46]. When manufacturing processes change, forced degradation becomes particularly valuable for comparability assessments, revealing differences that may not be detectable through routine testing alone [48]. By applying controlled stresses such as elevated temperature, pH extremes, mechanical agitation, and light exposure, scientists can accelerate the aging process, identify vulnerable molecular sites, elucidate degradation pathways, and establish stability-indicating methodologies that ensure product quality, safety, and efficacy throughout the shelf life [46] [47].
Experimental Design and Methodologies
Strategic Approach to Forced Degradation Conditions
Designing appropriate forced degradation studies requires a systematic approach that balances sufficient stress to generate relevant degradation products without creating unrealistic degradation pathways. The International Conference on Harmonisation (ICH) guidelines provide general principles but allow significant flexibility in implementation, recognizing that optimal conditions are product-specific [49] [50]. A well-designed forced degradation study should investigate thermolytic, hydrolytic, oxidative, and photolytic degradation mechanisms using conditions that exceed those employed in accelerated stability testing [47] [49].
Industry surveys reveal that most companies employ a risk-based approach when designing forced degradation studies for comparability assessments [48]. The extent of manufacturing process changes directly influences study design, with more significant changes warranting more comprehensive forced degradation protocols. Prior knowledge about the product's stability characteristics and the critical quality attributes (CQA) assessment are the primary factors influencing the selection of specific stress conditions [48]. For early-stage development, studies may focus on platform conditions, while later-stage studies become increasingly molecule-specific.
Comprehensive Experimental Protocols
The following table summarizes the core stress conditions employed in forced degradation studies for biologics, along with their specific experimental parameters and primary degradation pathways observed:
Table 1: Comprehensive Experimental Protocols for Forced Degradation Studies
| Stress Condition | Typical Experimental Parameters | Primary Degradation Pathways | Key Influencing Factors |
|---|---|---|---|
| High Temperature | 35-50°C for up to 2 weeks; typically 15-20°C below Tm (melting temperature) [46] [45] | Aggregation (soluble/insoluble), fragmentation (hinge region), deamidation, oxidation, isomerization [46] | pH, buffer composition, protein concentration [46] |
| Freeze-Thaw | Multiple cycles (typically 3-5) between -80°C/-20°C and room temperature [46] | Non-covalent aggregation, precipitation, particle formation [46] | Cooling/warming rates, pH, excipients, protein concentration [46] |
| Agitation | Stirring (100-500 rpm) or shaking (50-200 oscillations/min) for hours to days [46] | Insoluble and soluble aggregates (covalent/non-covalent), surface-induced denaturation [46] | Headspace, interface type, presence of surfactants, container geometry [46] |
| Acid/Base Hydrolysis | pH 2-4 (acid) and pH 9-11 (base) at 25-40°C for hours to days [47] [50] | Fragmentation, deamidation, isomerization, disulfide scrambling at high pH [46] | Buffer species, ionic strength, protein concentration [47] |
| Oxidation | 0.01%-0.3% H₂O₂ at 25-40°C for several hours; metal ions; radical initiators [46] [47] | Methionine/tryptophan oxidation, cysteine modification, cross-linking [46] | Catalytic metals, light, peroxide impurities in excipients [46] |
| Photolysis | Exposure to UV (320-400 nm) and visible light per ICH Q1B guidelines [47] [49] | Tryptophan/tyrosine oxidation, disulfide bond cleavage, backbone fragmentation [46] | Container closure, solution vs. solid state, sample thickness [49] |
A progressive approach to stress level selection is recommended, beginning with moderate conditions and increasing intensity until sufficient degradation (typically 5-20%) is achieved [47] [50]. This prevents over-stressing, which can generate secondary degradation products not relevant to real-world storage conditions [47]. For biologics, a degradation level of 10-15% is generally considered adequate for method validation [49]. Studies should include multiple time points to distinguish primary from secondary degradation products and understand kinetic profiles [47] [50].
The following workflow diagram illustrates the strategic approach to designing and implementing forced degradation studies:
Figure 1: Strategic workflow for designing and implementing forced degradation studies
Analytical Toolbox for Degradation Characterization
Advanced Analytical Techniques
The analytical characterization of stressed samples requires a comprehensive suite of orthogonal techniques capable of detecting and quantifying diverse degradation products. The selection of analytical methods should be driven by the degradation pathways observed and the critical quality attributes being monitored [48]. As outlined in ICH Q5E, manufacturers should propose "stability-indicating methodologies that provide assurance that changes in the identity, purity, and potency of the product will be detected" [49].
The multi-attribute method (MAM) has emerged as a particularly powerful approach for monitoring product quality attributes. This mass spectrometry-based technique enables simultaneous monitoring of multiple degradation products, including oxidation, deamidation, fragmentation, and post-translational modifications [45]. MAM provides a scientifically superior alternative to conventional chromatographic and electrophoretic methods by offering direct attribute-specific quantification and the ability to detect novel species not present in reference standards [45].
Table 2: Analytical Techniques for Monitoring Degradation Pathways
| Analytical Technique | Key Applications in Forced Degradation | Attributes Monitored | Technology Platform |
|---|---|---|---|
| Size Exclusion Chromatography (SEC) | Quantification of soluble aggregates and fragments [46] | Size variants, aggregation, fragmentation | HPLC/UHPLC with UV/RI detection |
| Capillary Electrophoresis SDS (CE-SDS) | Size variant analysis under denaturing conditions [46] | Fragmentation, non-glycosylated heavy chain | Capillary electrophoresis with UV detection |
| Ion Exchange Chromatography (IEC) | Charge variant analysis [46] [45] | Deamidation, isomerization, sialylation, C-terminal lysine | HPLC/UHPLC with UV detection |
| Hydrophobic Interaction Chromatography (HIC) | Hydrophobicity changes due to oxidation or misfolding [46] | Oxidation, misfolded variants, hydrophobic aggregates | HPLC/UHPLC with UV detection |
| Liquid Chromatography Mass Spectrometry (LC-MS) | Peptide mapping for attribute identification [46] [45] | Oxidation, deamidation, glycosylation, sequence variants | LC-MS/MS with electrospray ionization |
| Multi-Attribute Method (MAM) | Simultaneous monitoring of multiple attributes [45] | Comprehensive quality attribute profile | LC-MS with automated data processing |
Essential Research Reagent Solutions
The execution of forced degradation studies requires carefully selected reagents and materials to ensure consistent, reproducible results. The following table outlines key research reagent solutions and their specific functions in forced degradation protocols:
Table 3: Essential Research Reagents for Forced Degradation Studies
| Research Reagent | Function in Forced Degradation Studies | Typical Working Concentrations | Key Considerations |
|---|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Oxidative stress agent to mimic peroxide exposure [46] [47] | 0.01% - 0.3% (v/v) [47] | Concentration and time-dependent effects; typically limited to 24h exposure [47] |
| Polysorbates (PS20/PS80) | Surfactants to mitigate interfacial stress [46] [45] | 0.01% - 0.1% (w/v) | Quality and peroxide content may influence oxidative degradation [45] |
| Buffer Systems (Histidine, Succinate, Phosphate) | pH control during solution stress studies [46] [47] | 10 - 50 mM | Buffer species can catalyze specific degradation reactions [46] |
| Metal Chelators (EDTA, DTPA) | Inhibit metal-catalyzed oxidation and fragmentation [46] | 0.01% - 0.1% (w/v) | Important for controlling variable metal impurities [46] |
| Radical Initiators (AIBN) | Generate radicals to study auto-oxidation pathways [47] | Concentration varies by molecule | Useful for predicting long-term oxidation potential [47] |
| Reducing Agents (DTT, TCEP) | Characterize disulfide-mediated aggregation [46] | 1 - 10 mM | Used analytically to distinguish covalent vs. non-covalent aggregates [46] |
Application in Comparability Assessments
Role in Manufacturing Process Changes
Forced degradation studies serve as an amplification tool in comparability assessments, making subtle differences between pre- and post-change products detectable through accelerated stress conditions [48]. When manufacturing processes change, even well-controlled biological products may exhibit subtle molecular differences that are not apparent under standard stability conditions but may become pronounced during storage or stress [10]. The ICH Q5E guideline explicitly recognizes the value of "accelerated and stress stability studies" as useful tools to establish degradation profiles and enable direct comparison between pre-change and post-change products [48].
The most common approach across the industry involves side-by-side testing of pre-change and post-change material under identical stress conditions [48] [45]. This methodology enables both qualitative assessment (comparing degradation profiles for new peaks or pattern changes) and quantitative assessment (comparing degradation rates) [45]. For quantitative comparison, statistical analysis of degradation rates for selected attributes evaluates homogeneity of slopes and ratios of rates between the pre-change and post-change materials [45].
Batch Selection and Study Design Considerations
Appropriate batch selection is critical for meaningful comparability conclusions. The industry standard for formal comparability studies typically involves three pre-change and three post-change batches, providing sufficient data for statistical analysis and confidence in the comparison [48] [10]. These batches should be manufactured close in time using representative processes and should have passed all release criteria to avoid the appearance of "cherry-picking" favorable results [10].
The following diagram illustrates the key decision points in designing a comparability study:
Figure 2: Decision pathway for implementing forced degradation in comparability assessments
The phase of development significantly influences the extent of forced degradation studies. During early development (Phase 1-2), limited batch availability may restrict studies to single pre- and post-change batches with platform methods [10]. As development progresses to Phase 3 and commercial filing, studies typically expand to include multiple batches (the "3×3" design) and more molecule-specific analytical methods [48] [10]. This phase-appropriate approach acknowledges that product and process knowledge increases throughout the development lifecycle.
Emerging Trends and Advanced Applications
Design of Experiments (DoE) in Forced Degradation
Traditional forced degradation studies often employ a one-factor-at-a-time (OFAT) approach, which can miss interactive effects between stress factors and lead to correlated degradation patterns that complicate data interpretation [51]. The emerging application of design of experiments (DoE) methodologies represents a significant advancement in forced degradation study design [51]. This systematic approach simultaneously investigates multiple stress factors through strategically combined experiments, creating greater variation in degradation profiles and enabling more sophisticated statistical analysis.
The DoE approach offers several distinct advantages: it reduces correlation structures between co-occurring modifications, enables identification of interactive effects between stress factors, and facilitates model-based data evaluation strategies such as partial least squares regression [51]. This methodology is particularly valuable for establishing structure-function relationships (SFR) by creating more diverse degradation profiles that help link specific modifications to changes in biological activity or potency [51]. By generating samples with more varied modification patterns, DoE approaches enhance the ability to correlate specific molecular attributes with changes in critical quality attributes.
Industry Perspectives and Best Practices
A recent industry-wide survey conducted by the BioPhorum Development Group provides valuable insights into current practices and trends in forced degradation studies [48]. The survey revealed that while all companies use forced degradation to support comparability, specific approaches vary significantly in terms of study design, analytical characterization strategies, and data interpretation criteria [48]. This diversity reflects the product-specific nature of forced degradation studies and the absence of prescriptive regulatory guidance on detailed implementation.
The survey identified several key considerations for successful forced degradation studies:
- Prior knowledge about the product or similar molecules is the primary factor influencing the selection of forced degradation conditions [48]
- Critical quality attribute assessment drives the analytical characterization strategy, with greater focus on attributes potentially impacted by the manufacturing change [48]
- Stage of development significantly influences study scope, with earlier phases employing more limited studies that expand as development progresses [48] [10]
- Formal comparability assessments typically employ statistical analysis with pre-defined acceptance criteria, though specific approaches vary between companies [48]
Extended characterization and forced degradation studies provide an essential scientific foundation for understanding biopharmaceutical stability and demonstrating comparability after manufacturing changes. When strategically designed and executed, these studies reveal subtle differences in degradation pathways and rates that might otherwise remain undetected until product failure or compromised patient safety [46] [10]. The continued evolution of forced degradation methodologies, including the adoption of design of experiments approaches and advanced analytical techniques like multi-attribute methods, promises to further enhance our ability to establish meaningful structure-function relationships and ensure the consistent quality of biological products throughout their lifecycle [51] [45].
As the biopharmaceutical industry continues to advance, the role of forced degradation studies continues to expand beyond regulatory compliance to become a fundamental tool for product understanding and process control. By implementing these studies early in development and applying them systematically throughout the product lifecycle, manufacturers can build a comprehensive knowledge base that supports both continuous process improvement and robust quality assurance, ultimately ensuring that patients consistently receive safe and effective biopharmaceutical products [48] [10].
In the rigorous landscape of drug development, establishing method comparability is a critical cornerstone for ensuring the reliability and validity of scientific data. Specifications—defined as a list of tests, references to analytical procedures, and appropriate acceptance criteria—form the foundation of quality standards to which a drug substance or product must conform [22]. The journey from a method's initial development to its eventual implementation is fraught with challenges, including manufacturing changes, technological discontinuation, and method modernization. These changes necessitate a robust process for demonstrating that a new or modified analytical procedure is equivalent to the originally approved method. Such equivalency studies are performed to demonstrate that results generated by different methods yield insignificant differences in accuracy and precision, ensuring the same accept/reject decisions are reached [22]. This article explores the framework for optimizing study designs through platform methods and prior knowledge, providing researchers with structured approaches for comparative evaluation within the context of method comparability acceptance criteria research.
Theoretical Framework: Foundations of Method Equivalence
Regulatory and Statistical Foundations
The concept of specification equivalence encompasses both the analytical procedure itself and the corresponding acceptance criteria. According to current regulatory and compendial guidance documents, including ICH Q2 and ICH Q14, methods included in specifications must be validated and/or verified to be fit for purpose [22]. The analytical target profile (ATP) provides the foundation for required method development and subsequent validation parameters, establishing the intended use of the method prior to initiating any work. During method development, defining the method operable design regions (MODRs) introduces a quality by design (QbD) approach, providing flexibility through larger operating ranges than standard single points [22]. When comparing methods with MODRs, theoretical comparison is only possible if there is overlap in their design space; otherwise, an experimental equivalence study becomes necessary.
The Research Continuum: From Basic Research to Implementation
A structured framework for research progression provides essential guidance for method evaluation studies. The National Center for Complementary and Integrative Health (NCCIH) outlines a multiphase research paradigm that progresses from basic research through dissemination and implementation science [52]. This framework, while developed for complementary health interventions, offers valuable principles for analytical method evaluation:
- Basic Research: Investigates the fundamental principles of an approach or intervention, aiming to determine whether biologically and/or clinically meaningful effects can be demonstrated [52].
- Mechanistic and Translational Research: Examines interactions between interventions and their targeted systems, determining if mechanistic effects can be reliably measured and translated to human applications [52].
- Intervention Refinement and Optimization: Focuses on developing, refining, and standardizing interventions to increase adherence and potential impact through determining appropriate parameters and delivery methods [52].
- Efficacy Trials: Test clinical benefit in optimized settings with high internal validity, typically requiring multisite implementation with careful selection of comparison groups [52].
- Effectiveness and Pragmatic Studies: Determine effects under "real world" conditions with broader heterogeneity in providers and participants, often resulting in smaller effect sizes [52].
- Dissemination and Implementation Science: Studies how to best spread and sustain evidence-based interventions in clinical care or other appropriate settings [52].
This phased approach ensures that method evaluation studies progress systematically from fundamental validation to practical implementation, reducing the risk of methodological flaws in comparative assessments.
Experimental Design Strategies for Method Comparison
Core Principles of Equivalency Study Design
Equivalency studies for analytical methods must demonstrate that the original and proposed methods produce equivalent results, leading to identical accept/reject decisions. The United States Pharmacopeia (USP) <1010> presents numerous methods and statistical tools for designing, executing, and evaluating equivalency protocols [22]. While this chapter serves as a valuable educational tool, it requires proficient statistical understanding for proper application. For many pharmaceutical analytical laboratories, basic statistical tools—including mean, standard deviation, pooled standard deviation, evaluation against historical data, and comparison to approved specifications—may suffice to determine method equivalency, particularly when analysts possess deep knowledge of the methods and materials being evaluated [22]. More complicated methods, such as those requiring modeling, typically necessitate more sophisticated statistical evaluation.
Incorporating Platform Methods in Comparative Evaluation
Modern experimentation platforms offer sophisticated capabilities for comparative evaluation across multiple concepts or strategies. A cross-platform optimization system enables comparative evaluation through optimization across multiple generative models, creating a coherent workflow for multi-model optimization, parallel performance simulation, and unified design and data visualization [53]. Such systems allow researchers to manage complex optimization tasks associated with different generative models, define meaningful performance evaluation functions, and conduct comparative evaluation of results from multiple optimizations [53]. This approach is particularly valuable in early-stage exploration where conventional single-model optimization tools often prove inadequate due to their narrow focus on numerical improvement within a constrained design space.
Table 1: Key Properties for Evaluating Comparative Method Performance
| Property Category | Specific Metrics | Evaluation Method | Statistical Considerations |
|---|---|---|---|
| Analytical Accuracy | Mean recovery, comparison to reference standards | Statistical comparison against known values | Confidence intervals, tolerance limits |
| Precision | Repeatability, intermediate precision, reproducibility | Multiple measurements across different conditions | Standard deviation, relative standard deviation, ANOVA |
| Capability to Capture Preferences | Ability to reflect user requirements and constraints | Questionnaire assessment of method alignment with needs [54] | Likert scales, qualitative analysis |
| Cognitive Load | Mental effort required for method implementation | Standardized questionnaires assessing perceived difficulty [54] | Between-subjects designs to avoid fatigue effects |
| Responsiveness | Sensitivity to changes in parameters or preferences | Measurement of adjustment capability to modified requirements [54] | Pre-post comparison, effect size calculation |
| User Satisfaction | Overall experience with method implementation | Post-study questionnaires on satisfaction and confidence [54] | Mixed methods approaches |
Experimental Protocols for Method Equivalence
A streamlined approach to determining specification equivalence begins with a paper-based assessment of the methods and progresses to data assessment for methods under evaluation [22]. This tiered approach conserves resources while ensuring rigorous comparison:
- Paper-Based Assessment: Initial comparative review of methodology, operating principles, and procedural steps to identify fundamental incompatibilities or theoretical differences.
- MODR Overlap Analysis: Evaluation of method operable design regions to determine if theoretical comparison is feasible or if experimental study is required.
- Experimental Design Phase: Development of a protocol that includes sample selection, measurement conditions, and statistical analysis plan based on the ATP and MODR characteristics.
- Data Collection: Execution of the protocol with sufficient replication to ensure statistical power, incorporating quality control samples and reference standards.
- Statistical Analysis: Application of appropriate statistical methods ranging from basic descriptive statistics to sophisticated modeling, depending on method complexity.
- Decision Matrix Application: Comparison of results against pre-defined acceptance criteria to determine equivalence.
Table 2: Essential Research Reagent Solutions for Method Equivalence Studies
| Reagent Category | Specific Examples | Function in Study Design | Quality Requirements |
|---|---|---|---|
| Reference Standards | USP compendial standards, certified reference materials | Provide benchmark for method accuracy and precision | Documented purity, stability, and traceability |
| Quality Control Materials | Spiked samples, pooled patient samples, manufactured controls | Monitor method performance over time and across conditions | Well-characterized, stable, representative of test samples |
| System Suitability Solutions | Tailored mixtures for chromatography, known challenge panels | Verify operational readiness of instrumental systems | Fit-for-purpose, stable, sensitive to critical parameters |
| Cross-Validation Samples | Historical samples with established values, proficiency testing materials | Bridge between original and modified methods | Commutability with both methods, documented history |
Quantitative Data Analysis and Visualization in Method Comparison
Statistical Analysis of Comparative Data
Quantitative data analysis serves as the foundation for objective method comparison, employing mathematical, statistical, and computational techniques to uncover patterns, test hypotheses, and support decision-making [55]. In method equivalence studies, both descriptive and inferential statistics play crucial roles:
- Descriptive Statistics: Summarize and describe dataset characteristics using measures of central tendency (mean, median, mode) and dispersion (range, variance, standard deviation) to provide a clear snapshot of method performance [55].
- Inferential Statistics: Use sample data to make generalizations, predictions, or decisions about method population performance through hypothesis testing, T-tests, ANOVA, regression analysis, and correlation analysis [55].
- Specialized Techniques: Cross-tabulation analyzes relationships between categorical variables; MaxDiff analysis identifies most preferred items from option sets; gap analysis compares actual performance to potential [55].
The selection of statistical approaches should align with the method's intended use and complexity, with basic methods potentially requiring only fundamental statistics while complex methods may need advanced modeling.
Data Visualization for Comparative Analysis
Effective data visualization transforms raw comparison data into understandable insights, exploiting the human visual system's capacity to recognize patterns and structures [56]. For method equivalence studies, specific visualization strategies enhance interpretability:
Best practices in data visualization for method comparison include knowing your audience and message, adapting visualization scale to the presentation medium, avoiding chartjunk (keeping it simple), using color effectively, and avoiding default settings [56]. Color selection should align with data properties: qualitative palettes for categorical data without inherent ordering, sequential palettes for numeric data with natural ordering, and diverging palettes for numeric data that diverges from a center value [56]. Streamlined design with clear interpretive headlines significantly enhances communication effectiveness [57].
Case Study: Experimental Evaluation of Interactive Methods
Methodology and Implementation
A sophisticated experimental design for comparing interactive methods based on their desirable properties offers valuable insights for method comparison studies across domains. Recent research has developed questionnaires assessing multiple desirable properties of interactive methods, including cognitive load, ability to capture preferences, responsiveness to preference changes, user satisfaction, and confidence in final solutions [54]. The experimental approach employed a between-subjects design where participants solved problems using only one method, avoiding fatigue effects and enabling comparison of more methods with deeper questionnaire items [54].
The study compared three interactive methods: E-NAUTILUS (a trade-off-free method), NIMBUS (using classification of objective functions), and RPM (using reference points with aspiration levels) [54]. This comparative approach allowed researchers to derive statistically significant conclusions about method behavior relative to the desirable properties considered.
Quantitative Results and Analysis
The experimental results revealed important differentiations between method types. Trade-off-free methods demonstrated particular suitability for exploring whole sets of Pareto optimal solutions, while classification-based methods proved more effective for fine-tuning preferences to find final solutions [54]. This finding highlights how method performance characteristics may vary depending on the specific research objective or stage of investigation.
Table 3: Experimental Results from Method Comparison Studies
| Method Category | Cognitive Load | Preference Capture | Exploration Capability | Fine-Tuning Precision | User Satisfaction |
|---|---|---|---|---|---|
| Trade-Off-Free Methods | Lower perceived cognitive demand | Moderate effectiveness | Superior for broad solution space exploration | Limited precision in final stages | Higher during exploration phases |
| Classification-Based Methods | Moderate cognitive demand | High effectiveness | Limited exploration efficiency | Superior for final solution refinement | Higher during final selection |
| Reference Point Methods | Variable cognitive demand | High effectiveness with experienced users | Balanced exploration capability | Moderate refinement precision | Dependent on user expertise |
The optimization of study designs for method comparison requires systematic approaches that leverage both platform methods and prior knowledge. Through structured frameworks incorporating phased research progression, robust experimental designs, appropriate statistical analysis, and effective data visualization, researchers can establish method comparability with greater confidence and efficiency. The integration of platform methods enables comparative evaluation across multiple concepts or strategies, while prior knowledge informs acceptance criteria and study design parameters. As methodological complexity increases and regulatory expectations evolve, continued refinement of these comparative approaches will remain essential for advancing pharmaceutical research and development while maintaining rigorous quality standards. The experimental evidence demonstrates that different method categories exhibit distinct performance characteristics across evaluation metrics, highlighting the importance of aligning method selection with specific research objectives and contexts.
Demonstrating Success: Stability, Process Performance, and Regulatory Confidence
For researchers and drug development professionals, demonstrating stability comparability is a critical component of the product lifecycle, ensuring that manufacturing changes or new formulations do not adversely impact drug product quality. Stability comparability provides evidence that a product made after a manufacturing change maintains the same safety, identity, purity, and potency as the pre-change product without needing additional clinical studies [41]. This assessment relies on two primary experimental approaches: real-time stability studies conducted at recommended storage conditions and accelerated stability studies performed under elevated stress conditions. Within the framework of method comparability acceptance criteria research, selecting the appropriate study design and statistical analysis method is paramount for generating defensible, scientifically sound data that regulatory authorities will accept.
The foundation of stability comparability lies in the comparability protocol, which includes the analytical methods, study design, representative data set, and associated acceptance criteria [2]. According to ICH Q5E, demonstrating "comparability" does not require the pre- and post-change materials to be identical, but they must be highly similar with sufficient knowledge to ensure that any differences in quality attributes have no adverse impact upon safety or efficacy [10]. The strategic application of both real-time and accelerated study designs enables scientists to build this evidence throughout the drug development lifecycle, from early-phase development to post-approval changes.
Real-Time Stability Study Designs
Fundamental Principles and Protocols
Real-time stability testing serves as the gold standard for establishing a product's shelf life under recommended storage conditions. In this design, a product is stored at recommended storage conditions and monitored until it fails specification, with the time until failure defining the product's shelf life [58]. The fundamental purpose is to directly observe degradation patterns under actual storage conditions, providing regulators with the most reliable evidence of product performance over time.
The standard experimental protocol for real-time stability studies involves several critical steps. According to regulatory requirements, studies must utilize at least three lots of material to capture lot-to-lot variation [58]. Testing should be performed at time intervals that encompass the target shelf life and continue for a period after the product degrades below specification. A typical sampling schedule for a product with a proposed 24-month shelf life includes testing at 0, 3, 6, 9, 12, 18, and 24 months, with potential extension beyond the proposed shelf life to fully characterize the degradation profile. The International Council for Harmonisation (ICH) Q1A(R2) guideline specifies that long-term testing should cover a minimum of 12 months' duration on at least three primary batches at the time of submission [59].
Data Analysis and Shelf Life Determination
The analysis of real-time stability data focuses on modeling the degradation pattern of critical quality attributes. Degradation typically follows zero-, first-, or second-order reaction kinetics [58]. For attributes degrading via a first-order reaction, the pattern can be described mathematically as:
[ Y = α \times e^{(-δ \times t)} + φ + ε ]
Where Y represents the measured attribute at time t, α is the initial potency, δ is the degradation rate, φ represents lot-to-lot variability, and ε represents random experimental error. The true degradation pattern at storage temperature can be expressed with the equation:
[ Y_{storage} = α \times e^{(-δ \times t)} ]
The shelf life determination involves identifying the time point (t_s) at which the product's critical attribute reaches a predetermined specification limit (C). The estimated time that the product remains stable is calculated as:
[ t_s = \frac{ln(\frac{C}{α})}{-δ} ]
To ensure public safety, the labeled shelf life is established as the lower confidence limit of this estimated time, not the point estimate itself [58]. This conservative approach accounts for variability and uncertainty in the estimation process, with the confidence interval width influenced by the number of lots tested, testing frequency, and analytical method variability.
Table 1: Key Parameters in Real-Time Stability Study Design
| Parameter | Typical Specification | Regulatory Basis |
|---|---|---|
| Number of batches | At least 3 | ICH Q1A(R2) |
| Study duration | Minimum 12 months for submission | ICH Q1A(R2) |
| Testing frequency | Every 3 months (year 1), every 6 months (year 2), annually thereafter | ICH Q1A(R2) |
| Storage conditions | Recommended storage conditions with temperature and humidity monitoring | ICH Q1A(R2) |
| Statistical confidence | 95% confidence limit for shelf life estimation | FDA Guidance |
Accelerated Stability Study Designs
Fundamental Principles and Protocols
Accelerated stability assessment provides an efficient approach to support drug product development and expedite regulatory procedures by subjecting products to elevated stress conditions [59]. The core principle involves using known relationships between stress factors and degradation rates to predict long-term stability under recommended storage conditions. Temperature serves as the most common acceleration factor because its relationship with degradation rate is well-characterized by the Arrhenius equation [58]:
[ k = A \times e^{(-E_a/RT)} ]
Where k is the degradation rate constant, A is the pre-exponential factor, E_a is the activation energy, R is the gas constant, and T is the absolute temperature in Kelvin. This relationship enables scientists to model degradation rates at recommended storage temperatures based on data collected at elevated temperatures.
The Accelerated Stability Assessment Program (ASAP) represents a sophisticated application of these principles, utilizing a moisture-modified Arrhenius equation and isoconversional model-free approach to provide a practical protocol for routine stability testing [59]. A typical ASAP study design for a parenteral medication might include conditions at 30°C ± 2°C/65% RH ± 5% RH for 1 month, 40°C ± 2°C/75% RH ± 5% RH for 21 days, 50°C ± 2°C/75% RH ± 5% RH for 14 days, and 60°C ± 2°C/75% RH ± 5% RH for 7 days [59]. This multi-condition approach allows for robust modeling of degradation kinetics across a range of stress conditions.
Data Analysis and Prediction Models
The analysis of accelerated stability data focuses on establishing a mathematical relationship between stress conditions and degradation rates. The acceleration factor (λ) is calculated as the ratio of the degradation rate at elevated temperature to the degradation rate at storage temperature [58]:
[ λ = \frac{k{accelerated}}{k{storage}} = e^{[\frac{Ea}{R} \times (\frac{1}{T{storage}} - \frac{1}{T_{accelerated}})]} ]
The true degradation pattern at storage temperature can then be predicted using the equation:
[ Y_{storage} = α \times e^{(-δ \times λ \times t)} ]
Research has demonstrated that various reduced models can maintain predictive reliability while accelerating stability evaluation. A 2025 study on carfilzomib parenteral drug product found that while the full ASAP model and 11 reduced models provided reliable predictions of degradation products, the three-temperature model was identified as the most appropriate for the specific medication under investigation [59]. These models showed high R² (coefficient of determination) and Q² (predictive relevance) values, indicating robust model performance and predictive accuracy when compared with actual long-term stability results.
Table 2: Typical Conditions for Accelerated Stability Studies
| Study Type | Temperature | Humidity | Duration | Application |
|---|---|---|---|---|
| Accelerated (ICH) | 40°C ± 2°C | 75% RH ± 5% | 6 months | Drug products stored at room temperature |
| Intermediate (ICH) | 30°C ± 2°C | 65% RH ± 5% | 6-12 months | When significant change occurs at accelerated conditions |
| ASAP | 30°C to 60°C (multiple levels) | Varies by design | Days to weeks | Comprehensive degradation modeling |
| Stress Studies | Elevated temperatures | Specific to product | Usually 1 month | Evaluate effect of short-term excursions |
Comparative Analysis: Applications and Limitations
Strategic Application in Product Lifecycle
Real-time and accelerated stability studies serve complementary roles in demonstrating stability comparability throughout the product lifecycle. Real-time studies provide the definitive evidence required for establishing shelf life in regulatory submissions, while accelerated studies offer efficient tools for formulation screening, manufacturing change assessment, and preliminary shelf-life estimation during development. For comparability studies following manufacturing changes, a combination of both approaches is typically employed, with accelerated studies providing early indication of comparable stability profiles and real-time studies confirming long-term equivalence [10].
The phase-appropriate application of these study designs is essential for efficient drug development. During early-phase development, when representative batches are limited and critical quality attributes may not be fully established, accelerated studies provide valuable preliminary data on stability profiles [10]. As development progresses to Phase 3 and preparation for regulatory submission, the complexity of stability studies increases to include more molecule-specific methods and head-to-head testing of multiple pre- and post-change batches, typically following the "3 pre-change vs. 3 post-change" gold standard [10]. For post-approval changes, well-designed accelerated studies can support the implementation of changes while real-time studies run in parallel to confirm the predictions.
Experimental Design and Methodological Considerations
The experimental workflow for designing and executing stability comparability studies follows a systematic approach that incorporates both accelerated and real-time elements. The process begins with thorough planning and progresses through method development, experimental execution, data analysis, and regulatory submission.
Several critical methodological considerations must be addressed when designing stability comparability studies. Lot selection is essential, as batches should be representative of the pre- and post-change processes or sites and manufactured as close together as possible to avoid natural age-related differences convoluting the results [10]. Forced degradation studies conducted as part of extended characterization can reveal degradation pathways not observed in routine stability studies by subjecting products to various stress conditions including thermal, photolytic, and oxidative challenges [10]. The proper statistical approach for comparing stability profiles typically employs equivalence testing rather than significance testing, as equivalence testing demonstrates that differences are within pre-defined practical limits rather than simply showing that a difference exists [2].
Analytical Framework and Acceptance Criteria
Statistical Approaches for Comparability Assessment
The statistical framework for assessing stability comparability has evolved from simple significance testing to more appropriate equivalence testing methodologies. The United States Pharmacopeia (USP) chapter <1033> indicates a preference for equivalence testing over significance testing, noting that significance tests may detect small, practically insignificant deviations from target or may fail to detect meaningful differences due to insufficient replicates or variable data [2].
The Two One-Sided T-test (TOST) approach is commonly used to demonstrate comparability [2]. This method tests whether the difference between two groups is significantly lower than an upper practical limit and significantly higher than a lower practical limit. The TOST approach involves:
- Setting risk-based acceptance criteria for each parameter
- Performing two one-sided t-tests against the upper and lower practical limits
- Concluding equivalence if both tests reject the null hypotheses
The acceptance criteria should be justified based on scientific knowledge, product experience, and clinical relevance, with higher risks allowing only small practical differences and lower risks allowing larger differences [2]. For stability comparisons, this approach can be applied to compare degradation rates (slopes), intercepts, or specific timepoint measurements between pre-change and post-change products.
Establishing Method and Specification Equivalence
Demonstrating specification equivalence requires a comprehensive assessment of both the analytical methods and the acceptance criteria. The methodology involves a streamlined approach that begins with a paper-based assessment of the methods and progresses to experimental data assessment when necessary [22]. When comparing methods with defined Method Operable Design Regions (MODRs), a theoretical comparison is only possible if there is overlap in their MODR design spaces; otherwise, an experimental equivalence study must be performed [22].
For analytical procedure changes, it is critical to distinguish between comparability and equivalency. Comparability evaluates whether a modified method yields results sufficiently similar to the original, typically confirmed through comparability studies without requiring regulatory filings. Equivalency involves a more comprehensive assessment, often requiring full validation, to demonstrate that a replacement method performs equal to or better than the original, with such changes requiring regulatory approval prior to implementation [1]. The ICH Q14 guideline encourages a structured, risk-based approach to assessing, documenting, and justifying method changes throughout the analytical procedure lifecycle [1].
Table 3: Essential Research Reagent Solutions for Stability Comparability Studies
| Reagent/Category | Function in Stability Assessment | Application Examples |
|---|---|---|
| Reference Standards | Serve as benchmarks for analytical method performance and system suitability | Pharmacopeial standards, in-house characterized reference materials |
| Chromatography Columns | Separate and quantify drug substances and degradation products | C18 reversed-phase, ion-exchange, size-exclusion columns |
| Mobile Phase Components | Enable separation of analytes based on chemical properties | Buffers (phosphate, acetate), organic modifiers (acetonitrile, methanol) |
| Detection Reagents | Facilitate visualization and quantification of specific attributes | UV/VIS detectors, fluorescence markers, mass spectrometry interfaces |
| Forced Degradation Solutions | Intentionally stress products to reveal degradation pathways | Hydrogen peroxide (oxidative stress), acid/base solutions (hydrolytic stress) |
| Stability-Indicating Methods | Quantitatively measure active ingredients and degradation products | Validated HPLC/UHPLC methods with specificity for degradants |
The demonstration of stability comparability through accelerated and real-time study designs represents a cornerstone of pharmaceutical development and lifecycle management. Real-time stability studies provide the definitive evidence required for regulatory shelf-life establishment, while accelerated approaches like ASAP offer efficient tools for formulation screening and rapid assessment of manufacturing changes. The strategic integration of both methodologies, supported by appropriate statistical analyses such as equivalence testing, enables manufacturers to implement necessary changes while maintaining product quality and regulatory compliance.
Within the broader context of method comparability acceptance criteria research, the principles and practices outlined in this guide provide a framework for generating scientifically sound stability comparability data. As the pharmaceutical landscape continues to evolve with increased emphasis on risk-based approaches and lifecycle management, the rigorous application of these study designs will remain essential for ensuring that manufacturing changes and process improvements can be implemented efficiently without compromising product quality, safety, or efficacy. By adopting a systematic, scientifically justified approach to stability comparability, drug developers can navigate the complex regulatory landscape while continuing to bring important and improved products to market.
In the highly regulated pharmaceutical industry, comparing process performance is a critical activity that directly impacts drug quality, safety, and efficacy. The evaluation of impurity removal and intermediate quality represents a fundamental aspect of process validation and control strategy implementation. These comparisons ensure that manufacturing processes consistently produce drug substances and products that meet predefined quality standards, particularly regarding the control of organic impurities, inorganic impurities, and residual solvents that may arise during synthesis or storage.
The foundation of these comparisons rests upon well-defined acceptance criteria derived from extensive process knowledge and analytical data. As outlined in ICH Q6B, acceptance criteria are "internal (in-house) values used to assess the consistency of the process at less critical steps" [60]. Establishing scientifically sound comparison methodologies enables manufacturers to objectively evaluate different manufacturing processes, technologies, and parameter sets, thereby facilitating data-driven decisions throughout the product lifecycle. The overarching goal is to ensure that intermediate process steps consistently deliver the required quality levels to ultimately meet drug substance specifications while managing the risk to patient safety.
Analytical Methodologies for Impurity Detection and Quantification
Key Analytical Techniques
The accurate detection and quantification of impurities is foundational to any meaningful process performance comparison. Modern analytical methods must be capable of identifying and measuring contaminants at trace levels, often as low as 0.03-0.05% of the API concentration, in accordance with regulatory thresholds [61] [62]. The selection of appropriate analytical techniques depends on the nature of the impurities, the matrix complexity, and the required sensitivity.
Table 1: Key Analytical Techniques for Impurity Profiling
| Technique | Application in Impurity Analysis | Regulatory Validation Reference |
|---|---|---|
| High-Performance Liquid Chromatography (HPLC) | Primary workhorse for organic impurity separation and quantification | ICH Q2(R1) [61] |
| Gas Chromatography (GC) | Determination of residual solvents and volatile impurities | ICH Q3C [61] |
| Mass Spectroscopy (MS) | Structural elucidation of unknown impurities; hyphenated with LC systems | - |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Identification and characterization of process-related and degradation impurities | - |
| Fourier Transform Infrared Spectroscopy (FTIR) | Functional group analysis and material identification | - |
High-Performance Liquid Chromatography (HPLC) remains the most widely employed technique for organic impurity analysis due to its robust separation capabilities, versatility, and compatibility with various detection systems [61]. When coupled with mass spectrometry (LC-MS), it becomes an powerful tool for impurity identification and structural elucidation, as demonstrated in comprehensive impurity profiling studies of complex molecules like Baloxavir Marboxil, where researchers identified and characterized 5 metabolites, 12 degradation products, 14 chiral compounds, and 40 process-related impurities [63].
Method Validation and Acceptance Criteria
For analytical results to be meaningful in process comparisons, methods must be rigorously validated according to ICH Q2(R1) guidelines [61]. The establishment of appropriate method acceptance criteria should be based on the intended use and the product specification limits the method will evaluate, rather than traditional measures like % coefficient of variation or % recovery alone [64].
Table 2: Recommended Acceptance Criteria for Analytical Methods
| Validation Parameter | Recommended Acceptance Criteria | Basis for Evaluation |
|---|---|---|
| Specificity | Excellent: ≤5% of tolerance; Acceptable: ≤10% of tolerance | Percentage of specification tolerance |
| Repeatability | ≤25% of tolerance (chemical methods); ≤50% of tolerance (bioassays) | Percentage of specification tolerance |
| Bias/Accuracy | ≤10% of tolerance | Percentage of specification tolerance |
| LOD | Excellent: ≤5% of tolerance; Acceptable: ≤10% of tolerance | Percentage of specification tolerance |
| LOQ | Excellent: ≤15% of tolerance; Acceptable: ≤20% of tolerance | Percentage of specification tolerance |
| Linearity | No systematic pattern in residuals; no significant quadratic effect | Statistical evaluation of residuals |
This specification-tolerant approach ensures method performance is evaluated in the context of its impact on product quality decisions. As emphasized in regulatory guidance, "the validation target acceptance criteria should be chosen to minimize the risks inherent in making decisions from bioassay measurements" [64]. Methods with excessive error can directly impact product acceptance out-of-specification rates and provide misleading information regarding process performance comparisons.
Experimental Designs for Process Performance Comparison
Statistical Design of Experiments (DoE)
The comparison of process performance for impurity removal and intermediate quality assessment requires structured experimental approaches that yield statistically valid conclusions. Design of Experiments (DoE) methodology provides a framework for systematically evaluating the effect of multiple process parameters on critical quality attributes, enabling evidence-based comparisons between different process conditions, technologies, or unit operations.
The fundamental basis of DoE analysis is comparison, often beginning with simple statistical tests like the t-test to compare two sample means [65]. In a typical DoE application, researchers might compare the performance of a process at different factor levels:
- Low level for factor A (Alow): 67, 61, 59, 52 (Mean: 59.75, Standard Deviation: 6.18)
- High level for factor A (Ahigh): 79, 75, 90, 87 (Mean: 82.75, Standard Deviation: 6.95)
Using a t-test with pooled standard deviation, these data yield a t-score of 4.94, which with 6 degrees of freedom corresponds to a p-value of approximately 0.003, indicating a statistically significant difference between the means [65]. This fundamental comparative approach can be extended to more complex experimental designs evaluating multiple factors simultaneously.
Integrated Process Modeling
For comprehensive process performance comparisons across multiple unit operations, Integrated Process Modeling (IPM) represents an advanced methodology that links knowledge across manufacturing steps [60]. In this approach, each unit operation is described by a multilinear regression model where performance measures (e.g., impurity clearance) serve as dependent variables, with inputs from previous steps and process parameters as independent variables.
These unit operation models are concatenated, with the predicted output of one step serving as input for the subsequent operation. Using Monte Carlo simulation, random variability from process parameters can be incorporated into the modeled process, enabling prediction of out-of-specification probabilities for given parameter sets [60]. This methodology is particularly valuable for deriving specification-driven intermediate acceptance criteria that ensure predefined out-of-specification probabilities while considering manufacturing variability.
Figure 1: Integrated Process Modeling Workflow for Acceptance Criteria Derivation
Comparative Case Studies in Impurity Removal and Process Control
Chromatographic Clarification in Biologics Manufacturing
A direct comparison of process technologies for impurity removal was demonstrated in a study evaluating traditional single-use clarification versus novel chromatographic clarification for monoclonal antibody production [66]. The research compared three clarification approaches for high cell density cultures:
- Traditional single-use clarification: Using depth filtration based on size exclusion principles
- Adsorptive hybrid filters: Combining mechanical sieving with charged resin binders
- Chromatographic clarification: Employing anion exchange principles in a single-use format
The comparative analysis revealed that the chromatographic approach achieved a 16% reduction in cost per gram while demonstrating superior performance in DNA reduction (up to 99.99%) and host cell protein removal (24% reduction) compared to conventional clarification strategies [66]. This case study illustrates how systematic comparison of unit operation technologies can yield both economic and quality improvements through enhanced impurity clearance.
Specification-Driven Acceptance Criteria Implementation
A compelling case study applying the comparison of different methodologies for establishing intermediate acceptance criteria involved a monoclonal antibody production process with nine downstream unit operations [60]. Researchers compared two approaches for defining acceptance criteria for critical quality attributes:
- Conventional 3SD Approach: Using mean ± 3 standard deviations of historical data
- Integrated Process Modeling: Employing specification-driven criteria based on predefined out-of-specification probabilities
The comparison demonstrated that the IPM methodology was superior to the conventional approach, providing a solid line of reasoning for justifying acceptance criteria in audits and regulatory submissions [60]. Unlike the 3SD method, which rewards poor process control with wider limits and punishes good control with tighter limits, the specification-driven approach maintained consistent quality risk levels while considering manufacturing variability.
Regulatory Framework and Method Comparability
ICH Guidelines for Impurity Control
The comparison of process performance for impurity removal occurs within a well-defined regulatory framework established by various ICH guidelines:
- ICH Q3A (R2): Addresses impurities in new drug substances [61]
- ICH Q3B (R2): Covers impurities in new drug products [61]
- ICH Q6B: Provides guidance on specification setting for biotechnological products [60]
- ICH Q9: Establishes quality risk management principles [64]
These guidelines stipulate that impurities present at levels above 0.05% (depending on maximum daily dose) must be identified, quantified, and reported [61]. The regulatory expectation is that manufacturers implement robust control strategies based on thorough process understanding and comparative evaluations where applicable.
Emerging Regulatory Approaches for Comparability Assessment
Recent regulatory developments reflect an evolving approach to process and product comparisons, particularly in the biologics space. The U.S. Food and Drug Administration has issued new draft guidance proposing to eliminate the requirement for comparative clinical efficacy studies (CES) for many biosimilars when sufficient analytical data exists [67] [68].
This shift acknowledges that "a comparative analytical assessment (CAA) is generally more sensitive than a CES to detect differences between two products" [68], reflecting growing regulatory confidence in advanced analytical technologies for product comparison. This principle can be extended to process performance comparisons, where analytical data increasingly forms the basis for evaluating impurity removal effectiveness and intermediate quality.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Impurity Studies
| Reagent/Material | Function in Impurity Studies | Application Example |
|---|---|---|
| Ammonium acetate (HPLC grade) | Mobile phase buffer for chromatographic separation | Preparation of 10 mM buffer for impurity detection by HPLC [62] |
| Empore SDB-XC SPE disks | Solid-phase extraction for sample clean-up | Removal of interfering contaminants prior to analysis [62] |
| Oasis HLB cartridges | Mixed-mode SPE for diverse impurity capture | Extraction of pharmaceutical impurities from complex matrices [62] |
| Envi-Carb PGC cartridges | Porous graphitic carbon for polar impurity retention | Selective capture of highly polar degradation products [62] |
| Chromatographic clarification media | Anion exchange-based impurity removal | Single-use clarification for DNA and HCP reduction [66] |
| Reference standards | Method qualification and quantification | System suitability testing and impurity quantification against known standards [64] |
Figure 2: Process Performance Comparison Methodology
The comparison of process performance for impurity removal and intermediate quality assessment requires a multidisciplinary approach combining advanced analytical technologies, statistical experimental design, and regulatory science principles. Effective comparisons employ validated analytical methods with specification-tolerant acceptance criteria, structured experimental designs yielding statistically valid conclusions, and modern methodologies like Integrated Process Modeling for deriving scientifically justified acceptance criteria.
As regulatory expectations evolve toward greater reliance on analytical comparability, the pharmaceutical industry's approach to process performance evaluation continues to mature. The case studies presented demonstrate that systematic comparison of unit operations and control strategies can yield significant improvements in both product quality and manufacturing efficiency. By implementing robust comparison methodologies grounded in sound scientific principles, pharmaceutical manufacturers can establish effective control strategies that ensure consistent product quality while facilitating continuous process improvement throughout the product lifecycle.
In the biopharmaceutical industry, changes to the manufacturing process of monoclonal antibodies (mAbs) are inevitable as companies seek to improve efficiency, scale up production, or implement new technologies. Process changes must be thoroughly evaluated to demonstrate they do not adversely impact the critical quality attributes (CQAs) of the drug substance or product. This assessment requires a robust comparability exercise to provide scientific evidence that pre-change and post-change products are highly similar and that the existing safety and efficacy profile is maintained [69].
This case study examines the application of acceptance criteria for a specific mAb process change, focusing on the experimental approaches and statistical methodologies used to justify that the change has no detrimental effect on product quality. The work is framed within broader research on method comparability acceptance criteria, which is fundamental to ensuring both regulatory compliance and consistent product quality in biopharmaceutical development.
Regulatory and Scientific Background
The Comparability Paradigm
For biological products, comparability does not mean that the pre-change and post-change products are identical. Rather, it means that their physicochemical and biological properties are sufficiently similar to ensure no adverse impact on the drug's safety, purity, identity, strength, and efficacy (SQIPSE) [69]. Regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), have issued guidance documents outlining the principles for demonstrating comparability [70]. A successful comparability study is a multi-faceted exercise that relies on analytical data, with well-justified acceptance criteria forming the cornerstone of the assessment.
The Role of Acceptance Criteria
Acceptance criteria are predefined specifications or ranges that the results of the comparability study must meet to conclude that the products are comparable. The selection of appropriate acceptance criteria is one of the most challenging steps in comparability studies [69]. These criteria must be:
- Scientifically justified based on knowledge of the product and process.
- Statistically sound, often derived from historical data from the pre-change process.
- Risk-based, focusing on the CQAs most likely to be impacted by the change.
- Fit-for-purpose, ensuring they are suitable for detecting clinically meaningful differences.
Case Study: Downstream Process Optimization for a Commercial mAb
A company sought to implement a downstream process change for a commercial monoclonal antibody to improve manufacturing efficiency and reduce cost of goods. The change involved replacing a chromatography resin with a new vendor's equivalent resin, claimed to have improved pressure-flow characteristics and dynamic binding capacity. The objective of the comparability study was to demonstrate that this change did not impact the drug substance quality.
Critical Quality Attributes (CQAs) and Analytical Methods
A risk assessment was conducted to identify CQAs potentially affected by the chromatography resin change. The following attributes were deemed critical for monitoring:
- Purity and Impurity Profile: Size variant distribution (monomer, aggregates, fragments) and charge variant distribution.
- Potency: Cell-based bioactivity.
- Product-Related Variants: Glycosylation profile, oxidation, and deamidation.
The analytical methods used are standard, platform procedures for mAb characterization, as shown in the table below.
Table 1: Key Critical Quality Attributes and Analytical Methods
| Quality Attribute Category | Specific CQA | Analytical Method |
|---|---|---|
| Purity & Impurities | High Molecular Weight (HMW) Aggregates | Size Exclusion Chromatography (SEC) |
| Low Molecular Weight (LMW) Fragments | Capillary Electrophoresis-SDS (CE-SDS) | |
| Charge Heterogeneity | Acidic and Basic Variants | Cation Exchange Chromatography (CEX) |
| Glycosylation | Afucosylation, Galactosylation | Released N-Glycan Analysis |
| Potency | Biological Activity | Cell-Based Bioassay |
| Structural Integrity | Higher Order Structure (HOS) | Circular Dichroism (CD) |
Defining Acceptance Criteria for Comparability
The acceptance criteria for the side-by-side comparability study were established based on historical data from multiple pre-change commercial batches. A key statistical approach involved using a linear mixed-effects model to analyze stability data and define equivalence margins [69].
For the accelerated stability comparability study, the acceptance criterion for the difference in degradation rates (slopes) between the pre-change and post-change products was set using an equivalence test. The null hypothesis (H₀) was that the mean degradation rates differ by more than a predefined margin, Δ. The alternative hypothesis (H₁) was that the difference is within the ±Δ margin. The acceptance margin (Δ) was determined based on the variability of degradation rates from historical pre-change stability data [69].
The following DOT script defines the statistical decision process for the equivalence test.
Diagram 1: Equivalence Testing for Comparability
The specific acceptance criteria for the key CQAs in this case study are summarized in the table below.
Table 2: Predefined Acceptance Criteria for Comparability Study
| Critical Quality Attribute (CQA) | Analytical Method | Acceptance Criterion | Rationale |
|---|---|---|---|
| HMW Aggregates | SEC | NMT 0.5% absolute difference | Based on ±3 SD of historical batch data. Clinical relevance. |
| Potency | Cell-Based Bioassay | Relative potency 95% CI falls within (80%, 125%) | Standard bioassay validation criteria. |
| Main Isoform (%) | CEX | NMT 5.0% absolute difference | Based on process capability (CpK >1.33) of historical data. |
| Afucosylation (%) | Glycan Analysis | NMT 0.8% absolute difference | Based on ±3 SD of historical data, considering impact on ADCC. |
| Degradation Rate (Accelerated Stability) | Various (e.g., SEC, CEX) | 90% CI for slope difference lies within ±Δ | Δ is the equivalence margin derived from historical slope variability [69]. |
Experimental Protocol and Workflow
Study Design
The comparability study was designed as a side-by-side analysis using three consecutive pre-change commercial batches and three consecutive post-change commercial batches. Additionally, an accelerated stability study was conducted to compare the degradation profiles of the products under stressed conditions (e.g., 25°C ± 2°C / 60% ± 5% RH for 3 months) [69].
The following DOT script outlines the overall experimental workflow for the comparability study.
Diagram 2: Comparability Study Workflow
Detailed Methodology for a Key Experiment: Accelerated Stability Comparability
Objective: To demonstrate that the degradation rate of the post-change product under accelerated conditions is equivalent to that of the pre-change product.
Protocol:
- Sample Preparation: Drug substance from three pre-change and three post-change batches was placed on an accelerated stability study.
- Testing Time Points: Samples were analyzed at time 0, 1, 2, and 3 months.
- Quality Attributes Monitored: Key stability-indicating attributes like HMW aggregates, potency, and main isoform percentage.
- Data Analysis: For each attribute and each batch, a degradation rate (slope) was calculated using linear regression. A linear mixed-effects model was fitted to the stability data, treating the degradation rate as a random effect to account for lot-to-lot variability [69].
- Statistical Comparison: An equivalence test was performed to compare the mean degradation rates of the two groups (pre- vs. post-change). The 90% confidence interval for the difference in mean slopes was calculated and compared against the pre-defined equivalence margin, Δ.
Results and Data Analysis
The side-by-side comparison of CQAs demonstrated that all attributes for the post-change batches were within the predefined acceptance criteria when compared to the pre-change batches. The results for the accelerated stability study are summarized below.
Table 3: Results from Accelerated Stability Comparability Study
| CQA | Pre-Change Mean Slope (%/month) | Post-Change Mean Slope (%/month) | Difference in Slopes (Post-Pre) | 90% Confidence Interval | Equivalence Margin (Δ) | Conclusion |
|---|---|---|---|---|---|---|
| HMW Aggregates | +0.15 | +0.17 | +0.02 | (-0.05, +0.09) | ±0.10 | Equivalent |
| Potency | -1.05 | -1.10 | -0.05 | (-0.20, +0.10) | ±0.25 | Equivalent |
| Main Isoform | -0.45 | -0.48 | -0.03 | (-0.11, +0.05) | ±0.15 | Equivalent |
The data shows that the 90% confidence interval for the difference in degradation rates for each CQA falls entirely within the respective equivalence margin, allowing for the rejection of the null hypothesis and a conclusion of statistical equivalence for the stability profiles [69].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of a comparability study relies on high-quality, well-characterized reagents and materials. The following table details key solutions used in the analytical methods featured in this case study.
Table 4: Key Research Reagent Solutions for mAb Characterization
| Reagent / Material | Function / Purpose | Example & Justification |
|---|---|---|
| Reference Standard (RS) | Serves as a benchmark for system suitability and method performance; critical for ensuring data reliability and regulatory compliance. | A well-characterized, stable mAb sample. Using a compendial RS (e.g., from USP) can save significant cost and time compared to developing an in-house standard [71]. |
| Cell-Based Assay Kit | Measures the biological activity (potency) of the mAb by quantifying its functional response in a live cell system. | Commercially available kits with validated components (e.g., reporter cells, substrates) reduce development time and improve assay reproducibility. |
| Chromatography Resins & Columns | Used in analytical SEC, CEX, and other methods to separate and quantify mAb variants based on size, charge, etc. | Columns with consistent performance (e.g., from a single lot) are vital. The switch to a new resin in the manufacturing process was the core change investigated here. |
| Enzymes for Glycan Analysis | Cleave N-linked glycans from the mAb for subsequent labeling and analysis to characterize glycosylation patterns. | PNGase F is commonly used. High-purity, recombinant enzymes ensure complete and consistent digestion for accurate results. |
| Stability Study Buffers | Provide the necessary ionic strength and pH for formulations during accelerated and long-term stability studies. | Buffers must be prepared to precise specifications, as variations in pH or excipients can influence the degradation rate of the mAb. |
This case study demonstrates a systematic and statistically rigorous approach to applying acceptance criteria for a monoclonal antibody process change. By leveraging historical data to set scientifically justified and risk-based acceptance criteria, and by employing equivalence testing for the statistical comparison, a compelling case for comparability was established. The work underscores that a well-designed comparability protocol, centered on robust acceptance criteria, is essential for ensuring that manufacturing process changes can be implemented without compromising the quality, safety, or efficacy of a biotherapeutic product. This approach aligns with the industry's and regulators' growing emphasis on analytical data as the primary evidence for demonstrating product sameness [72] [73].
In the dynamic landscape of pharmaceutical development, change is inevitable. Whether optimizing manufacturing processes, adopting modern analytical technologies, or transitioning between production sites, sponsors must demonstrate that such changes do not adversely affect drug product quality. A well-structured comparability package serves as the foundational evidence that modified products remain equivalent to their predecessors in terms of identity, strength, quality, purity, and potency as they relate to safety and effectiveness [74]. This guide examines the core components, experimental methodologies, and analytical frameworks essential for building a robust comparability package that withstands regulatory scrutiny.
Understanding the Regulatory Framework
Defining Comparability and Equivalency
Within the pharmaceutical industry, "comparability" and "equivalency" represent distinct but related concepts with specific regulatory implications.
- Comparability evaluates whether a modified method or process yields results sufficiently similar to the original, ensuring consistent product quality. These studies typically confirm that modified procedures produce expected results and may not always require regulatory filings [1].
- Equivalency involves a more comprehensive assessment, often requiring full validation, to demonstrate that a replacement method performs equal to or better than the original. Such changes require regulatory approval prior to implementation [1].
The Comparability Protocol (CP) provides the strategic framework for these assessments—a comprehensive, prospectively written plan that evaluates the impact of proposed Chemistry, Manufacturing, and Controls (CMC) changes on product quality attributes [74].
Relevant Regulatory Guidelines
Multiple regulatory guidelines govern comparability assessments:
- ICH Q14: Provides a structured framework for analytical procedure development and lifecycle management, emphasizing science-based and risk-based approaches [1] [22].
- FDA Guidance on Comparability Protocols: Outlines requirements for assessing product or process changes that may impact safety or efficacy [2] [74].
- ICH Q2(R2): Defines validation requirements for analytical procedures [22].
- USP <1010> and <1033>: Offer statistical methods for designing and evaluating equivalency protocols [2] [22].
Core Components of a Comparability Package
A successful comparability package requires thorough documentation across several interconnected domains, summarized in the table below.
Table 1: Essential Components of a Comparability Package
| Component | Description | Key Elements |
|---|---|---|
| Administrative Information | Basic submission identifiers | • Product name and dosage form• Application type and number• Contact information |
| Description & Rationale for Change | Detailed explanation of the proposed change | • Comprehensive change description• Scientific and business rationale• Risk assessment |
| Supporting Data & Analysis | Evidence demonstrating unchanged product quality | • Side-by-side testing results• Statistical analyses• Stability data |
| Comparability Protocol | Prospective plan for assessing the change | • Study design and acceptance criteria• Testing methodologies• Statistical approaches |
| Proposed Reporting Category | Recommended regulatory reporting mechanism | • Justification for reduced reporting• Regulatory pathway |
Experimental Design and Methodologies
Statistical Approaches for Comparability
Choosing appropriate statistical methods is crucial for robust comparability conclusions.
- Equivalence Testing: Preferred over significance testing for demonstrating comparability. Unlike significance tests that seek to identify differences, equivalence testing provides assurance that means do not differ by a practically meaningful amount [2].
- Two One-Sided T-Test (TOST): Commonly used approach where two one-sided t-tests determine if the difference between groups is significantly lower than the upper practical limit and significantly higher than the lower practical limit [2].
- Risk-Based Acceptance Criteria: Practical limits for equivalence should reflect the risk associated with the change [2]:
- High risk: Allow 5-10% difference
- Medium risk: Allow 11-25% difference
- Low risk: Allow 26-50% difference
Analytical Method Equivalency
Demonstrating equivalence between analytical methods requires a structured approach:
- Method Operable Design Regions (MODR): During method development, defining MODR provides flexibility by establishing larger operating ranges than standard single points [22].
- Side-by-Side Testing: Analyzing representative samples using both original and new methods under standardized conditions [1].
- Method Validation Parameters: Assessing accuracy, precision, specificity, detection limit, quantitation limit, linearity, and range per ICH Q2(R2) [22].
Figure 1: Method Equivalency Study Workflow
Quantitative Data Analysis and Presentation
Statistical Analysis Methods
Quantitative data analysis forms the evidentiary foundation of any comparability package, employing both descriptive and inferential statistics [75].
Table 2: Statistical Methods for Comparability Assessment
| Statistical Method | Application in Comparability | Example Use Case |
|---|---|---|
| Descriptive Statistics | Summarize central tendency and variability of data | Report means, standard deviations, and ranges for critical quality attributes |
| Two One-Sided T-Tests (TOST) | Demonstrate equivalence between two groups | Show method equivalency for updated analytical procedures |
| Analysis of Variance (ANOVA) | Compare means across multiple groups | Assess product consistency across multiple manufacturing batches |
| Confidence Intervals | Estimate precision of measured differences | Report equivalence margins with statistical confidence |
| Regression Analysis | Model relationships between variables | Evaluate stability profiles between pre- and post-change products |
Data Visualization for Comparability
Effective visualization enhances regulatory understanding of comparability data:
- Box Plots: Display distributional characteristics, including median, quartiles, and outliers for comparative data sets [76].
- 2-D Dot Charts: Illustrate individual data points across comparison groups, effective for small to moderate data sets [76].
- Line Graphs: Demonstrate trends over time, particularly useful for stability data comparisons [77].
- Histograms: Show distribution shapes for large continuous data sets, helping assess normality assumptions [77].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful comparability studies require carefully selected reagents and materials to generate reliable, reproducible data.
Table 3: Essential Research Materials for Comparability Studies
| Material/Reagent | Function in Comparability Assessment | Critical Considerations |
|---|---|---|
| Reference Standards | Benchmark for qualifying analytical performance | • Well-characterized• Traceable to primary standards• Appropriate stability |
| System Suitability Materials | Verify chromatographic system performance | • Representative of test samples• Sensitive to critical parameters |
| Quality Control Samples | Monitor assay performance over time | • Cover specification range• Long-term stability |
| Biocompatibility Testing Materials | Assess safety of device materials | • Relevant biological models• Validated endpoint measurements |
| Container Closure Simulation Materials | Evaluate packaging compatibility | • Representative extraction conditions• Sensitive detection methods |
Navigating the Regulatory Submission Process
Preparing the Comparability Protocol Submission
A well-structured Comparability Protocol Submission should include [74]:
- Summary Section: Concise overview of proposed changes, methodologies, and anticipated outcomes
- Detailed Change Description: Comprehensive explanation of changes with scientific rationale
- Supporting Data: All relevant studies, analyses, and statistical evaluations
- Protocol Details: Specific methodologies, testing criteria, and acceptance criteria
- Proposed Reporting Category: Justification for reduced reporting when applicable
Submission Timing and Implementation
- Prospective Submission: Comparability Protocols should be submitted for FDA review and approval before implementing changes [74].
- Documentation: After implementation, a comprehensive report detailing outcomes, comparisons with historical data, and any observations should be submitted [74].
- Global Considerations: While comparability is recognized globally, specific requirements may vary across regulatory agencies [74].
Figure 2: Regulatory Pathway for Comparability Protocols
Common Pitfalls and Best Practices
Avoiding Common Pitfalls
- Insufficient Sample Size: Studies with inadequate power may fail to detect meaningful differences [2].
- Poorly Justified Acceptance Criteria: Limits not based on scientific rationale or risk assessment [2] [22].
- Incomplete Data Sets: Missing critical quality attributes or failure to assess worst-case conditions.
- Retrospective Criteria Adjustment: Modifying acceptance criteria post-study to achieve passing results [2].
Best Practices for Success
- Early Engagement: Consider submitting Pre-Submission requests to obtain FDA feedback on proposed approaches [78].
- Risk-Based Strategy: Identify critical method parameters early and understand their impact on method performance [1].
- Knowledge Management: Capture and leverage development data to inform modifications and troubleshooting [1].
- Robust Statistical Design: Implement appropriate statistical methods with predefined acceptance criteria [2] [22].
- Comprehensive Documentation: Maintain detailed records of all development, validation, and comparability activities [1] [74].
Building a successful comparability package requires meticulous planning, robust experimental design, and comprehensive documentation. By understanding regulatory expectations, implementing appropriate statistical approaches, and maintaining a science-based, risk-informed strategy, sponsors can effectively demonstrate that manufacturing and analytical changes do not adversely impact product quality. A well-executed comparability package not only facilitates regulatory approval but also strengthens the overall quality system, ensuring consistent delivery of safe and effective medicines to patients.
Conclusion
Establishing robust acceptance criteria for method comparability is not a one-size-fits-all exercise but a strategic, science- and risk-based endeavor fundamental to biopharmaceutical development. By integrating foundational regulatory principles with rigorous statistical methodologies like equivalence testing and a proactive approach to risk management, developers can build a compelling data package that demonstrates control over their process and product. As therapies grow more complex, the principles outlined will become even more critical. The future of comparability will likely see greater integration of advanced analytical technologies, continued regulatory alignment through guidelines like ICH Q14, and a reinforced focus on leveraging comprehensive data to ensure that manufacturing changes do not adversely impact the quality, safety, or efficacy of life-changing medicines for patients.
References
- 1. A New Era for Analytical Procedure Lifecycle Management [https://synergbiopharma.com/navigating-analytical-method-comparability-and-equivalency-under-ich-q14-a-new-era-for-analytical-procedure-lifecycle-management/]
- 2. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 3. Comparability, equivalence, similarity… How statistics can ... [https://www.a3p.org/en/comparability-equivalence-similarity-how-statistics-can-help-us-to-demonstrate-these-and-soon-the-end-of-blind-testing-for-health-authorities-and-manufacturers/]
- 4. Specification Equivalence—A Practical Approach [https://www.pharmtech.com/view/specification-equivalence-a-practical-approach]
- 5. How to Demonstrate Comparability of Analytical Procedures [https://www.gmp-compliance.org/gmp-news/how-to-demonstrate-comparability-of-analytical-procedures]
- 6. FDA IND CMC Requirements for Biologics: A 2025 ... [https://scxcmc.com/fda-ind-cmc-requirements-for-biologics/]
- 7. ICH Q14 and the Paradigm Shift in Pharmaceutical Analytics [https://www.gmp-journal.com/current-articles/details/ich-q14-and-the-paradigm-shift-in-pharmaceutical-analytics.html]
- 8. A Practical Approach to Implementing ICH Q14 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449753/]
- 9. Analytical control strategy for biologics. Part I: Foundations [https://www.sciencedirect.com/science/article/abs/pii/S0022354925002795]
- 10. Understanding comparability studies for biologics [https://mmsholdings.com/perspectives/comparability-studies-biologics-importance/]
- 11. Identifying and Measuring Critical Quality Attributes - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK475684/]
- 12. A Practical Primer for t Tests, Correlations, and Meta-Analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC5502906/]
- 13. Equivalence Testing (TOST) [https://real-statistics.com/students-t-distribution/equivalence-testing-tost/]
- 14. Considerations for Risk-Based Sampling During ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/580332-asdf/]
- 15. How to Implement Risk Acceptance Criteria (RAC) for ... [https://www.linkedin.com/posts/rameshchandranvadali_are-your-risk-acceptance-decisions-based-activity-7306895749726855168-5F0B]
- 16. Risk Assessment Matrix: Overview and Guide [https://auditboard.com/blog/what-is-a-risk-assessment-matrix]
- 17. 6 Types of Risk Assessment Methodologies + How to Choose [https://drata.com/grc-central/risk/risk-assessment-methodologies]
- 18. Statistical Equivalence Testing for Assessing Bench-Scale ... [https://www.biopharminternational.com/view/statistical-equivalence-testing-assessing-bench-scale-cleanability]
- 19. Introduction to Equivalence Testing with TOSTER [https://cran.rstudio.com/web/packages/TOSTER/vignettes/IntroductionToTOSTER.html]
- 20. ( TOST ) | Statistical Equivalence for Excel test Software [https://www.xlstat.com/solutions/features/equivalence-test-tost]
- 21. in Excel | Equivalence | Two One-Sided Test TOST Test [https://www.qimacros.com/hypothesis-testing/equivalence-test/]
- 22. Specification Equivalence: A Practical Approach to Method ... [https://www.pharmtech.com/view/specification-equivalence-a-practical-approach-to-method-and-acceptance-criteria-equivalence]
- 23. ACOMED - statistik, statistical equivalence , testing TOST [https://www.acomed-statistik.de/en-gb/equivalence-tests-TOST.html]
- 24. A Journey Through the Statistical Fundamentals of ... [https://bebpa.org/before-the-beginning-comes-the-question-a-journey-through-the-statistical-fundamentals-of-comparability/]
- 25. Influence of Inter- and Intra-Batch Variability on the Sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7760601/]
- 26. Qualitative vs. Quantitative Research | Differences, ... [https://www.scribbr.com/methodology/qualitative-quantitative-research/]
- 27. Qualitative vs Quantitative Research: What's the Difference? [https://www.simplypsychology.org/qualitative-quantitative.html]
- 28. What Is Qualitative vs. Quantitative Study? - National University [https://www.nu.edu/blog/qualitative-vs-quantitative-study/]
- 29. Types of Research Methods: Quantitative & Qualitative ... [https://paperguide.ai/blog/types-of-research-methods/]
- 30. What is Agile Acceptance Criteria? A Complete Guide [https://www.6sigma.us/six-sigma-in-focus/agile-acceptance-criteria/]
- 31. What Is Acceptance Criteria: Definition, How-Tos, And Tips [https://mambo.io/blog/acceptance-criteria]
- 32. Specification-driven acceptance criteria for validation of ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1010583/full]
- 33. Sample size estimation and power analysis for clinical research studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3409926/]
- 34. Basic concepts for sample size calculation: Critical step for any clinical trials! - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4916819/]
- 35. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 36. How to Calculate Sample Size Needed for Power - Statistics By Jim [https://statisticsbyjim.com/hypothesis-testing/sample-size-power-analysis/]
- 37. Quick guide to power calculations [https://www.povertyactionlab.org/resource/quick-guide-power-calculations]
- 38. Exact Power and Sample Size Calculations for the Two One-Sided Tests of Equivalence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5012670/]
- 39. How to calculate power (or sample size) for a multiple ... [https://communities.sas.com/t5/Statistical-Procedures/How-to-calculate-power-or-sample-size-for-a-multiple-comparison/td-p/888816]
- 40. Sample size calculations (Ep. 41) [https://teuschersolutions.com/podcast/sample-size-calculations-ep-41/]
- 41. Demonstration of Comparability of Human Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/demonstration-comparability-human-biological-products-including-therapeutic-biotechnology-derived]
- 42. Comparability: manufacturing, characterization and controls ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5422032/]
- 43. Plan ahead, avoid comparability studies says Novartis [https://www.bioprocessintl.com/therapeutic-class/cgt-cmc-plan-ahead-avoid-comparability-studies-says-novartis]
- 44. Comparability Considerations and Challenges for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7691403/]
- 45. Drug Product Comparability: Developing Criteria [https://www.bioprocessintl.com/cmc-forums/emerging-strategies-for-drug-product-comparability-and-process-validation-part-1-analytical-tools-and-drug-product-comparability]
- 46. Forced degradation of recombinant monoclonal antibodies [https://pmc.ncbi.nlm.nih.gov/articles/PMC5680805/]
- 47. Development of forced degradation and stability indicating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5761119/]
- 48. An Industry Perspective on the use of Forced Degradation ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354923005373]
- 49. Forced Degradation Studies: Regulatory Considerations ... [https://www.biopharminternational.com/view/forced-degradation-studies-regulatory-considerations-and-implementation]
- 50. Forced Degradation – A Review [https://biomedres.us/fulltexts/BJSTR.MS.ID.007492.php]
- 51. Advancing forced degradation studies: Design of ... [https://www.sciencedirect.com/science/article/pii/S093964112500164X]
- 52. Research Framework - nccIH.nih.gov [https://www.nccih.nih.gov/grants/nccih-clinical-trials-funding-opportunities/research-framework]
- 53. A Cross-Platform Optimization System for Comparative ... [https://www.sciencedirect.com/science/article/pii/S2352710225026506]
- 54. An experimental design for comparing interactive methods ... [https://link.springer.com/article/10.1007/s10479-024-05941-6]
- 55. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 56. Designing Effective Data Visualizations [https://guides.library.jhu.edu/datavisualization/design]
- 57. Quantitative Data Visualization Tips for Beginners [https://keracollective.com/blog/evaluation-research-design-data-visualization-quantitative]
- 58. Assessing Shelf Life Using Real-Time and Accelerated ... [https://www.biopharminternational.com/view/assessing-shelf-life-using-real-time-and-accelerated-stability-tests]
- 59. Accelerated Predictive Stability Testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858995/]
- 60. Specification-driven acceptance criteria for validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9537461/]
- 61. Resolving API Impurity Issues in Drug Development [https://www.pharmaguideline.com/2025/04/resolving-api-impurity-issues-in-drug-development.html]
- 62. Removal of Contaminant Peaks in Reversed-Phase ... [https://www.chromatographyonline.com/view/removal-contaminant-peaks-reversed-phase-gradient-liquid-chromatography-improved-detection-pharmac-0]
- 63. Comprehensive review on impurity profiling, control ... [https://link.springer.com/article/10.1007/s44371-025-00329-2]
- 64. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 65. The Basis of Design of Experiments is Comparison [https://accendoreliability.com/basis-design-experiments-comparison/]
- 66. Chromatographic capture of cells to achieve single stage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9286051/]
- 67. FDA Proposes To Eliminate Comparative Clinical ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-proposes-to-eliminate-biosimilar-comparative-studies]
- 68. FDA rethinks need for comparative efficacy studies ... [https://www.jdsupra.com/legalnews/fda-rethinks-need-for-comparative-8509505/]
- 69. Determination of acceptance criteria and sample sizes for ... [https://www.sciencedirect.com/science/article/abs/pii/S1045105617300891]
- 70. Considerations for Monoclonal Antibody Bioprocess and ... [https://www.pharmtech.com/view/considerations-for-monoclonal-antibody-bioprocess-and-manufacturing-validation]
- 71. mAb Therapies: Reducing Costs and Accelerating Timelines [https://www.bioprocessintl.com/monoclonal-antibodies/reducing-costs-and-accelerating-timelines-with-tools-for-physicochemical-characterization-of-mab-therapies]
- 72. Survey on the Role of Comparative Efficacy Studies ... [https://pubmed.ncbi.nlm.nih.gov/40971119/]
- 73. FDA Waives Clinical Trials for Biosimilar mAbs in the USA [https://biopharmaspec.com/blog/fda-biosimilar-regulation-changes-usa/]
- 74. New Guidance on Comparability Protocols [https://www.linkedin.com/pulse/new-guidance-comparability-protocols-edward-narke-k8kie]
- 75. Quantitative Data Analysis Methods & Techniques 101 [https://gradcoach.com/quantitative-data-analysis-methods/]
- 76. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 77. 2.3 Displaying Quantitative Data – Significant Statistics [https://pressbooks.lib.vt.edu/introstatistics/chapter/histograms-frequency-polygons-and-time-series-graphs/]
- 78. De Novo Classification Request [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/de-novo-classification-request]