The Extracellular Matrix in 3D Cell Culture: From Silent Scaffold to Active Director of Cell Behavior
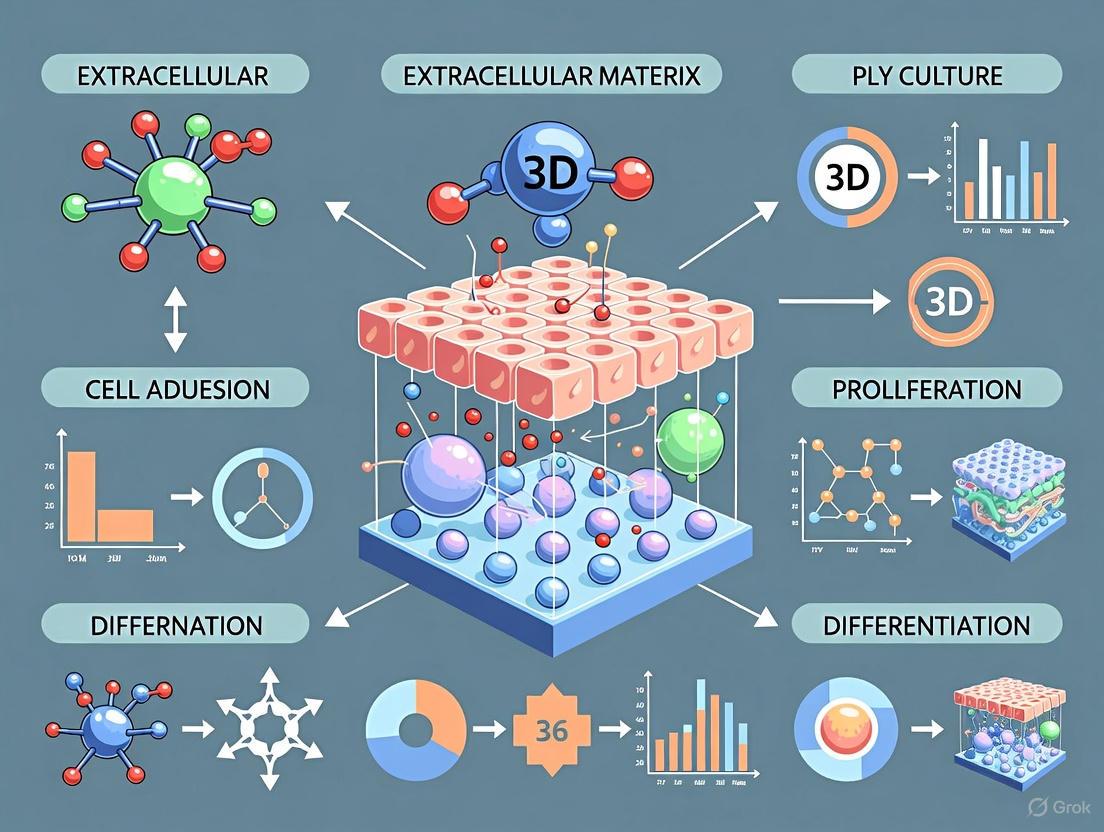
This article explores the pivotal role of the extracellular matrix (ECM) in advancing three-dimensional (3D) cell culture technologies for biomedical research and drug discovery.
The Extracellular Matrix in 3D Cell Culture: From Silent Scaffold to Active Director of Cell Behavior
Abstract
This article explores the pivotal role of the extracellular matrix (ECM) in advancing three-dimensional (3D) cell culture technologies for biomedical research and drug discovery. It covers the foundational biology of the ECM, detailing its composition and critical functions in providing structural, biochemical, and mechanical cues that direct cell fate. The review compares leading methodological approaches for creating ECM-mimicking environments, including decellularized scaffolds, hydrogels, and organoids, highlighting their applications in developing more physiologically relevant disease models. It further addresses key technical challenges and optimization strategies for these 3D systems. Finally, the article examines the compelling evidence that validates ECM-rich 3D models as superior tools for predicting drug efficacy and toxicity, ultimately discussing their transformative potential in personalized medicine and reducing reliance on animal models.
Beyond a Scaffold: Deconstructing the Multifunctional Role of the Native ECM
The extracellular matrix (ECM) is far more than a passive, structural scaffold for cells; it is a dynamic and biologically active 3D network of macromolecules that orchestrates critical aspects of cellular behavior, including proliferation, differentiation, migration, and survival. In the context of three-dimensional (3D) cell culture research, recapitulating the complex properties of the native ECM is paramount for creating physiologically relevant in vitro models. The shift from traditional two-dimensional (2D) monolayers to 3D culture systems is fundamentally centered on providing cells with an environment that mimics the in vivo ECM, thereby yielding more predictive data for drug discovery, cancer research, and regenerative medicine [1] [2]. This technical guide delves into the core composition of the ECM, its pivotal role in 3D cell culture, and the advanced methodologies used to model its complexity for biomedical research.
Core Composition and Biochemical Properties of the ECM
The ECM is a complex meshwork composed of hundreds of distinct molecules, which can be broadly categorized into a few key classes. Its specific biochemical and biophysical composition varies between tissues and is dynamically remodeled during developmental and disease processes.
Key Macromolecular Components
The primary functional components of the ECM include:
- Collagens: The most abundant proteins in the ECM, providing tensile strength and structural integrity. Collagen IV is a major component of the basement membrane [3].
- Glycosaminoglycans (GAGs) and Proteoglycans: Polysaccharide chains that attract water and ions, forming a hydrated gel that confers resistance to compressive forces and serves as a reservoir for growth factors [3].
- Glycoproteins: Multi-adhesive proteins that facilitate cell-ECM adhesion. Key examples include:
- Laminin: A major component of the basement membrane that influences cell differentiation, migration, and adhesion.
- Fibronectin: Connects cells to collagen fibers and is crucial for cell migration and wound healing.
- Vimentin: While traditionally considered an intracellular filament protein, its significant overexpression in tumor-derived ECM highlights the unique compositional shifts in disease states [3].
Table 1: Key Macromolecular Components of the Extracellular Matrix
| Component Class | Key Examples | Primary Functions |
|---|---|---|
| Fibrous Proteins | Collagen I, IV; Elastin | Structural integrity, tensile strength, and elasticity. |
| Glycosaminoglycans (GAGs) | Hyaluronic Acid, Chondroitin Sulfate | Hydration, compressive resistance, growth factor binding. |
| Glycoproteins | Laminin, Fibronectin, Vimentin | Cell adhesion, signaling, migration, and tissue organization. |
Quantitative Differences in Normal vs. Tumor ECM
The critical role of the ECM is starkly evident when comparing normal and pathological tissues. Research using Patient-Derived Scaffolds (PDS) has quantified significant alterations in tumor ECM composition and mechanics, which actively drive cancer progression.
Table 2: Quantitative Differences Between Normal and Tumor-Derived ECM (PDS)
| ECM Parameter | Normal PDS | Tumor PDS | Significance |
|---|---|---|---|
| Collagen Content | 226.71 µg/mg | 469.59 µg/mg | Increased stiffness and structural remodeling in tumors [3]. |
| GAG Content | 1.90 µg/mg | 2.99 µg/mg | Altered chemical signaling and hydration [3]. |
| Young's Modulus (Stiffness) | Significantly lower | Significantly higher | Creates a mechanobiological environment conducive to invasion [3]. |
| Key Protein Expression | Low expression of Collagen IV, Vimentin | Significant overexpression | Promotes an aggressive, invasive phenotype in cancer cells [3]. |
The Role of ECM in 3D Cell Culture Systems
In 3D cell culture, the ECM is the central element that defines the cellular microenvironment. It overcomes the limitations of 2D cultures by restoring cell-cell and cell-ECM interactions in all dimensions, leading to more authentic tissue-like structures and cellular responses [2].
Key Functions of ECM in 3D Models
- Mechanotransduction: The ECM transmits mechanical signals to cells via integrins and other adhesion receptors, influencing gene expression and cell fate. The increased stiffness of tumor PDS is a prime example of how ECM mechanics can promote invasive gene expression [3].
- Biochemical Signaling: The ECM serves as a reservoir for growth factors and cytokines, presenting them to cells in a spatially and temporally controlled manner. It also contains cryptic peptide sequences that are exposed upon proteolytic remodeling to influence cell behavior.
- Architectural Support: The 3D topography of the ECM guides tissue organization, polarity, and morphogenesis, which are essential for forming complex structures like spheroids and organoids [1] [2].
Experimental Modeling of the ECM in 3D Research
A variety of sophisticated experimental platforms have been developed to model the ECM for 3D cell culture, each with distinct advantages and applications.
Scaffold-Based Modeling Platforms
Scaffold-based systems provide a physical 3D structure that mimics the native ECM, supporting cell growth and organization.
- Natural Matrices:
- Corning Matrigel: A solubilized basement membrane preparation extracted from the Engelbreth-Holm-Swarm mouse tumor, rich in laminin, collagen IV, and growth factors. It is widely used for organoid culture and studying cell invasion [2] [4]. A key limitation is batch-to-batch variability [2].
- Fibrin and Collagen Scaffolds: Natural polymers frequently used in tissue engineering and regenerative medicine applications [1] [5].
- Synthetic and Plant-Based Scaffolds:
- Hydrogels: Tunable networks of synthetic or natural polymers (e.g., PEG-based, alginate, PeptiGels) that offer high control over stiffness, porosity, and biochemical functionality [1] [2]. Edible plant-based scaffolds are an emerging, sustainable alternative [1].
- Patient-Derived Scaffolds (PDS): Decellularized human tissues that provide the most authentic, patient-specific ECM architecture and composition for research [3].
Detailed Protocol: Establishing 3D Cultures using Patient-Derived Scaffolds (PDS)
The following methodology outlines the process for creating a highly physiologically relevant 3D culture system using decellularized human tissue [3].
Objective: To decellularize human breast tissue and utilize the resulting ECM-based PDS as a platform for 3D culture of breast cancer cells to study tumor-specific ECM effects.
Materials and Reagents:
- Tissue Samples: Surgically resected breast tumor and adjacent normal breast tissue.
- Decellularization Solution: SDS-based buffer.
- Cell Culture Reagents: Phosphate-buffered saline (PBS), cell culture media, antibiotics.
- Cell Line: MCF-7 breast cancer cells.
- Assay Kits: MTT cell viability assay, ELISA for IL-6, reagents for DNA/RNA quantification.
- Staining Solutions: Hematoxylin and Eosin (H&E), DAPI, Trichrome, Sirius Red, Alcian Blue.
Procedure:
Tissue Decellularization:
- Subject normal and tumor tissue specimens to an SDS-based decellularization protocol.
- Validate complete cell removal via H&E and DAPI staining and DNA quantification (DNA content should be drastically reduced, e.g., from 527.1 ng/µL to 7.9 ng/µL) [3].
- Confirm preservation of key ECM components through biochemical assays (e.g., for collagen and GAG content) and histological staining (e.g., Trichrome for collagen, Alcian Blue for GAGs) [3].
Scaffold Characterization:
- Perform Scanning Electron Microscopy (SEM) to verify ECM microstructure preservation and increased porosity post-decellularization.
- Conduct immunohistochemistry (IHC) for specific ECM proteins (e.g., Collagen IV, Vimentin) to confirm their overexpression in tumor PDS versus normal PDS.
- Perform a tensile test to measure the Young's modulus and confirm significantly higher stiffness in tumor PDS [3].
3D Cell Seeding and Culture:
- Seed MCF-7 breast cancer cells onto the pre-hydrated normal and tumor PDS.
- Maintain cultures in standard conditions, refreshing media as needed, for up to 15 days.
Functional Analysis:
- Cell Viability/Proliferation: Perform MTT assay on day 7 and day 15. Quantify cell nuclei directly by analyzing DAPI-stained images of the scaffolds [3].
- Gene Expression Analysis: On day 15, extract RNA from cells cultured on PDS. Use qRT-PCR to analyze the expression of hub genes associated with invasiveness (e.g., CAV1, CXCR4, CNN3, MYB, TGFB1), which are significantly upregulated in cells on tumor PDS [3].
- Cytokine Secretion: Collect conditioned media on day 15 and use an ELISA to quantify the secretion of IL-6, a cytokine correlated with tumor progression [3].
Diagram Title: 3D PDS Culture Workflow
Signaling Pathways and Downstream Functional Effects
The tumor-specific ECM induces aggressive cancer cell behavior by activating specific gene networks and signaling pathways. Bioinformatic analysis of invasive breast cancer cell lines has identified a co-expression network of hub genes associated with cell motility and migration [3].
Diagram Title: ECM-Driven Invasive Signaling
The Scientist's Toolkit: Key Research Reagent Solutions
Working with ECM in 3D cell culture requires a suite of specialized reagents and tools. The following table details essential materials and their functions in this field.
Table 3: Essential Research Reagents for ECM-Based 3D Cell Culture
| Research Reagent / Tool | Function in 3D Cell Culture |
|---|---|
| Corning Matrigel Matrix | A natural basement membrane matrix used for cultivating organoids and studying cell invasion, providing a biologically active ECM environment [2] [4]. |
| Hydrogels (Synthetic & Natural) | Tunable polymers (e.g., PeptiGels, alginate) that create a defined 3D microenvironment with controllable stiffness and porosity for tailored experiments [1] [2]. |
| Patient-Derived Scaffolds (PDS) | Decellularized human tissues that provide a native, patient-specific ECM scaffold for highly physiologically relevant disease modeling and drug testing [3]. |
| Scaffold-Free Plates (e.g., ULA, Spheroid Microplates) | Low-attachment or micro-patterned plates that promote the self-aggregation of cells into scaffold-free 3D models like spheroids [1] [4]. |
| Microfluidic Chips (Organ-on-a-Chip) | Devices that co-culture cells with ECM in perfusable channels, allowing for the precise control of the microenvironment and the creation of dynamic tissue barriers [1] [6]. |
Research Applications and Future Directions
The ability to accurately model the ECM in vitro is transforming biomedical research, with significant implications for drug development and personalized medicine.
Key Application Areas
- Cancer Research: This is the largest application segment, accounting for approximately 34% of 3D cell culture use [1]. 3D models incorporating tumor-like ECM are pivotal for studying tumor invasion, drug resistance, and for developing personalized oncology approaches using patient-derived organoids (PDOs) [1] [3] [4].
- Drug Discovery and Toxicity Testing: 3D models with relevant ECM can replicate human tissue responses more accurately, reducing clinical trial failures and saving an estimated 25% in R&D costs for pharmaceutical companies [1]. Organ-on-a-chip technologies are particularly promising for predictive toxicity testing [1].
- Regenerative Medicine: 3D cultures are critical for organoid development and tissue engineering, aiming to create functional tissues for transplantation to address the global organ shortage [1].
Emerging Technological Integration
The field is rapidly advancing with the integration of cutting-edge technologies:
- 3D Bioprinting: Enables the precise spatial deposition of cells and "bioinks" (ECM-like hydrogels) to create complex, multicellular tissue constructs for drug testing and potential transplantation [1].
- Artificial Intelligence (AI) and Machine Learning: AI is used to analyze the complex, high-content data generated from 3D cultures (e.g., imaging, omics data), optimizing culture conditions, enhancing reproducibility, and identifying novel disease mechanisms and therapeutic targets [1] [6].
The extracellular matrix is the foundational element that defines the physiological context of cellular life. A deep understanding of its complex 3D network of macromolecules is no longer a niche interest but a prerequisite for advancing modern biomedical science. By employing the sophisticated experimental models and reagents detailed in this guide—from tunable hydrogels and patient-derived scaffolds to organ-on-a-chip systems—researchers can effectively mimic the in vivo ECM. This capability is crucial for bridging the translational gap between traditional 2D cultures, animal models, and human clinical outcomes, ultimately accelerating the development of safer and more effective therapeutics.
The extracellular matrix (ECM) is not merely a structural scaffold but a dynamic, bioactive environment that critically regulates cell behavior in three-dimensional (3D) contexts. This whitepaper details the core biochemical components of the ECM—collagens, proteoglycans, and glycoproteins—focusing on their structure, function, and interplay within 3D cell culture systems. Understanding these components is essential for advancing research in tissue engineering, disease modeling, and drug development, as they directly influence cellular phenotypes, mechanotransduction, and tissue-specific responses in a way that traditional two-dimensional (2D) cultures cannot replicate.
In vivo, cells reside within a complex 3D network of extracellular matrix (ECM) that provides not only physical support but also critical biochemical and mechanical cues that direct cell fate. The shift from 2D to 3D cell culture models is driven by the recognition that cells in a 3D microenvironment exhibit more physiologically relevant behaviors, including differentiation, proliferation, migration, and drug responses [7] [8]. The ECM's core biochemical components—collagens, proteoglycans, and glycoproteins—orchestrate these cellular processes by forming a composite material with unique structural and signaling properties.
The ECM exhibits complex mechanical properties such as stiffness, nonlinear elasticity, viscoelasticity, and plasticity, all of which are sensed by cells through mechanotransduction pathways [7]. In 3D, mechanical confinement by the surrounding ECM restricts changes in cell volume and shape but allows cells to generate force on the matrix through actomyosin-based contractility and protrusions [7]. Furthermore, cell–matrix interactions are dynamic owing to constant matrix remodelling. This review will explore the fundamental roles of the core ECM components in creating a native-like 3D environment for cells.
Core Biochemical Components of the ECM
Collagens
Structure and Types
Collagens constitute the most abundant protein family in the human ECM and are the primary building blocks of connective tissues. The defining feature of collagen is a unique triple-helical structure formed by three polypeptide chains (α-chains). These chains are rich in proline and glycine and assemble into a right-handed triple helix, providing exceptional tensile strength [9]. At least 28 types of collagen have been identified, with Type I collagen being the most ubiquitous, forming large, banded fibrils that provide structural integrity to tissues like skin, tendon, and bone [7] [9]. Type IV collagen, in contrast, forms a flexible, sheet-like network that is a foundational element of the basement membrane [7].
Function in 3D Microenvironments
In 3D cell culture, collagen hydrogels are widely used as scaffolds due to their excellent biocompatibility and ability to promote cell adhesion, migration, and tissue-specific organization [9] [10]. Cells bind to collagen primarily through integrin receptors (e.g., α2β1, α1β1), triggering intracellular signaling pathways that regulate survival, proliferation, and differentiation [7]. The mechanical properties of collagen networks, such as their stiffness and degradability, play a critical role in regulating cell behavior in 3D. For instance, collagen networks exhibit strain-stiffening (nonlinear elasticity), where their resistance to deformation increases with applied strain [7].
Table 1: Key Collagen Types in the ECM and Their Functions in 3D Culture
| Collagen Type | Structural Form | Primary Tissue Distribution | Role in 3D Cell Culture |
|---|---|---|---|
| Type I | Fibrillar | Skin, tendon, bone, ligaments | Most common scaffold material; promotes cell adhesion and migration; provides structural integrity [7] [9]. |
| Type II | Fibrillar | Cartilage, vitreous body | Supports chondrogenic phenotype; maintains cartilage-specific ECM [7]. |
| Type III | Fibrillar | Skin, blood vessels, reticular fibers | Often co-distributed with Type I; contributes to ECM compliance [10]. |
| Type IV | Network-forming | Basement membrane | Provides structural support for epithelial and endothelial cells; key for polarised tissue organization [7]. |
Proteoglycans and Glycosaminoglycans (GAGs)
Structure and Classification
Proteoglycans (PGs) are a diverse family of molecules consisting of a core protein to which one or more glycosaminoglycan (GAG) chains are covalently attached [11] [12]. GAGs are long, unbranched polysaccharides made of repeating disaccharide units. Based on their localization, PGs are classified into several families:
- Intracellular PGs: (e.g., serglycin) [12].
- Cell-surface PGs: (e.g., syndecans, glypicans) [11] [12].
- Extracellular/Pericellular PGs: This group includes large, aggregating PGs like aggrecan in cartilage, and small leucine-rich proteoglycans (SLRPs) such as decorin and biglycan, which interact with collagen fibrils [7] [12].
The major GAG types include heparan sulfate (HS), chondroitin sulfate (CS), dermatan sulfate (DS), keratan sulfate (KS), and the non-sulfated hyaluronic acid (HA) [12]. The sulfation patterns of GAG chains are critical for their ability to interact with a wide range of ligands [11].
Function in 3D Microenvironments
PGs and GAGs are multifunctional components that significantly influence the 3D cellular microenvironment through:
- Water Retention and Hydration: GAGs are highly negatively charged and hydrophilic, forming hydrated gels that resist compressive forces. This is particularly important in cartilage, where aggrecan and HA create a swellable, shock-absorbing matrix [7] [11].
- Molecular Reservoirs and Co-receptor Activity: HS chains on PGs like perlecan and syndecans bind and sequester a vast array of growth factors (e.g., FGFs, VEGF), chemokines, and morphogens. This creates concentration gradients and presents these signaling molecules to their respective cell-surface receptors, modulating key developmental and homeostatic pathways [12].
- Cell Adhesion and Migration: PGs on the cell surface and in the ECM facilitate or inhibit cell adhesion and migration. For example, the endothelial glycocalyx, a PG-rich layer on blood vessels, regulates leucocyte recruitment during inflammation [11].
- Regulation of Fibrillogenesis: SLRPs like decorin and lumican bind to collagen fibrils, regulating their diameter, organization, and overall ECM architecture [12].
Table 2: Major Proteoglycans and Their Functions in the ECM
| Proteoglycan | GAG Type | Localization | Core Function in 3D Microenvironment |
|---|---|---|---|
| Aggrecan | CS/KS | Extracellular (cartilage) | Forms large aggregates with HA; provides compressive resistance by hydrating the matrix [7] [12]. |
| Decorin | CS/DS | Extracellular | Binds to collagen I fibrils, regulating fibril assembly; binds TGF-β, modulating its activity [12]. |
| Versican | CS | Extracellular/Pericellular | Regulates cell adhesion, migration, and proliferation; involved in inflammation and cancer [12]. |
| Perlecan | HS | Basement Membrane | Key structural component of basement membrane; binds and stores growth factors (e.g., FGF) [12]. |
| Syndecan-1 | HS/CS | Cell Surface | Acts as a co-receptor for growth factors and integrins; influences cell-matrix adhesion and branching morphogenesis [11] [12]. |
| Hyaluronic Acid (HA) | None (GAG only) | Extracellular | A non-sulfated GAG not attached to a protein core; interacts with CD44 and RHAMM receptors; regulates cell proliferation, migration, and mechanotransduction [7] [11]. |
Glycoproteins
Structure and Key Examples
Glycoproteins are proteins adorned with carbohydrate chains (oligosaccharides) that are typically smaller and more branched than GAGs. They play crucial roles in cell adhesion, migration, and ECM assembly. Key structural glycoproteins in the ECM include:
- Fibronectin: A large, dimeric glycoprotein that exists in soluble (plasma) and insoluble (cellular) forms. It contains multiple binding domains for other ECM components (e.g., collagen, fibrin) and for cell-surface integrins via its RGD (Arg-Gly-Asp) sequence [13].
- Laminin: A large, cross-shaped trimeric glycoprotein that is a major constituent of the basement membrane. It self-assembles into a network and binds to other ECM components like type IV collagen and to cell-surface receptors such as integrins and dystroglycan, forming a stable adhesive substrate for epithelial and endothelial cells [7] [13].
- Elastin: The core component of elastic fibers, which provide tissues like blood vessels, skin, and lungs with the ability to recoil after transient stretch. Its precursor, tropoelastin, is cross-linked into a durable, stable network.
Function in 3D Microenvironments
Glycoproteins are master organizers of the ECM and are vital for creating a functional 3D niche:
- Nucleation of ECM Assembly: Fibronectin fibrillogenesis is often an early, essential step in the assembly of other ECM components, including collagen I and III. Cells use integrins to pull on fibronectin, unfolding it and exposing cryptic binding sites that promote its assembly into fibrils and the incorporation of other molecules [13].
- Cell Adhesion and Signaling: Glycoproteins like fibronectin and laminin are primary adhesion molecules for cells. Binding to their integrin receptors initiates intracellular signaling cascades (e.g., FAK, Src) that control cell cycle progression, survival, and cytoskeletal organization [8] [13].
- Providing Tensibility: Elastic fibers, composed of an elastin core and a microfibrillar sheath (containing fibrillin etc.), allow tissues to stretch and recoil, which is crucial for dynamic tissues.
Table 3: Principal Glycoproteins and Their Roles in 3D Culture Systems
| Glycoprotein | Molecular Structure | Primary Function | Role in 3D Cell Culture |
|---|---|---|---|
| Fibronectin | Dimeric glycoprotein with RGD domain | Cell adhesion, migration, ECM assembly | Promotes initial cell attachment and spreading; nucleates collagen deposition and assembly [13]. |
| Laminin | Cross-shaped heterotrimeric glycoprotein | Basement membrane assembly; cell polarization | Supports epithelial and endothelial cell organization into polarised structures (e.g., acini, tubules) [7] [13]. |
| Elastin | Cross-linked hydrophobic polymer | Confers elasticity and recoil to tissues | Critical for engineering mechanically dynamic tissues like blood vessels and skin [8]. |
| Fibrillin | Glycoprotein forming microfibrils | Scaffold for elastin assembly; regulates TGF-β bioavailability | Provides structural framework for elastic fiber formation; mutations lead to Marfan syndrome. |
Advanced 3D Culture Models and Methodologies
Reconstituted ECM Scaffolds
A common approach to 3D culture involves using reconstituted ECM proteins to form hydrogels. Reconstituted Type I Collagen gels are a gold standard for many applications. The typical protocol involves mixing a chilled, acidic solution of collagen I with a neutralization buffer and cell suspension, then incubating at 37°C to trigger fibrillogenesis and gelation [7] [14]. Reconstituted Basement Membrane (rBM) matrices (e.g., Matrigel), derived from Engelbreth-Holm-Swarm mouse sarcoma, are a heterogeneous mixture of laminin, type IV collagen, entactin, and PGs, and are ideal for culturing epithelial cells and forming organoids [7].
Experimental Protocol: Establishing a 3D Fibroblast-Collagen Culture for ECM Deposition Analysis [14] [13]
- Scaffold Preparation: Use a solution of acid-extracted bovine or rat tail Type I collagen. Neutralize the cold collagen solution on ice with an appropriate buffer (e.g., 10× PBS) and NaOH to achieve a physiological pH (pink color of phenol red indicator).
- Cell Encapsulation: Resuspend human dermal fibroblasts (HDFs) in the neutralized collagen solution at a density of 0.5–25 × 10^6 cells/mL [15]. Pipette the cell-collagen mixture into culture wells.
- Gelation: Transfer the culture plate to a humidified incubator (37°C, 5% CO2) for 30–60 minutes to allow polymerization into a solid gel.
- Culture Maintenance: Overlay the gel with complete cell culture medium. Refresh the medium every 48–72 hours. Culture can be maintained for several weeks to study long-term ECM remodeling.
- Analysis:
- Decellularization: To analyze cell-deposited ECM, remove cellular material using extraction buffer (1% Tween-20 and 20 mM NH4OH in PBS) [13].
- Immunofluorescence Staining: Fix and stain the scaffold for deposited ECM proteins (e.g., fibronectin, collagen I, laminin) using specific primary and fluorescently-labeled secondary antibodies [13].
- Multimodal Imaging: Analyze fixed samples using confocal laser scanning fluorescence microscopy (CLSFM) for protein localization, second harmonic generation (SHG) microscopy for collagen fibril structure, and mass spectrometry imaging for molecular composition [14].
Synthetic and Biofunctionalized Scaffolds
To overcome batch-to-batch variability and immunogenicity of animal-derived materials, synthetic scaffolds and human-derived ECM are being developed. Electrospun polycaprolactone (PCL) scaffolds provide a synthetic 3D fibrous network that mimics the native collagen architecture. These scaffolds can be coated with ECM proteins to enhance cell attachment and bioactivity [13]. Human ECM-like collagen (hCol) derived from cultured mesenchymal stem cells (MSCs) is an emerging alternative. hCol exhibits a hierarchical structure and proper post-translational modifications similar to native collagen, showing excellent bioactivity for tissue engineering applications [10].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for 3D ECM Research
| Reagent / Material | Function and Application in 3D Culture |
|---|---|
| Type I Collagen (Bovine/Rat tail) | Forms the foundational hydrogel scaffold for a wide range of 3D culture models; supports fibroblast and stromal cell growth [7] [14]. |
| Reconstituted Basement Membrane (rBM) | Used for organoid generation and epithelial cell culture; provides a complex mixture of basement membrane proteins [7]. |
| Fibronectin | Coating agent or additive to promote cell adhesion and migration within scaffolds; crucial for initial ECM assembly [13]. |
| Hyaluronic Acid (HA) | Used in hydrogel formulations to mimic soft tissue environments (e.g., brain, cartilage); influences cell proliferation and mechanosensing [7] [8]. |
| Transforming Growth Factor-β1 (TGF-β1) | Cytokine used to stimulate fibroblast activation and ECM deposition (e.g., collagen, fibronectin); models fibrotic disease or CAF phenotype [13]. |
| Matrix Metalloproteinase (MMP) Inhibitors | Used to study the role of ECM degradation and remodeling in cell invasion and migration [7]. |
| PrestoBlue HS / Resazurin | Cell viability assay reagent used to monitor metabolic activity of cells proliferating in 3D microbioreactors over time [15]. |
| Decellularization Buffer (Tween-20/NH4OH) | Removes cellular material from 3D cultures to isolate and analyze the cell-secreted ECM [13]. |
Signaling Pathways and Cellular Crosstalk in 3D
The core ECM components do not function in isolation but integrate to activate key signaling pathways that dictate cell behavior in a 3D context. The following diagrams illustrate two critical pathways mediated by these components.
Diagram 1: Integrin-mediated mechanotransduction. Cells sense collagen matrix stiffness and density via integrin receptors, triggering actomyosin contractility and translocation of YAP/TAZ into the nucleus to drive transcription [7].
Diagram 2: Proteoglycan-mediated growth factor signaling. Heparan sulfate proteoglycans in the ECM bind and concentrate growth factors, presenting them to their cognate receptors on the cell surface to potentiate signaling [11] [12].
The core biochemical components of the ECM—collagens, proteoglycans, and glycoproteins—work in concert to create a sophisticated 3D microenvironment that is fundamental to in vivo-like cell behavior. Collagens provide structural integrity and mechanical cues, proteoglycans regulate hydration, growth factor signaling, and resilience, while glycoproteins orchestrate cell adhesion and ECM assembly. A deep and integrated understanding of these components, their interactions, and their roles in signaling is indispensable for the design of physiologically relevant 3D cell culture models. The continued development of advanced scaffolds, including human-derived ECM and biofunctionalized synthetic materials, coupled with multimodal analytical techniques, will further enhance our ability to model human tissues accurately, thereby accelerating drug discovery and regenerative medicine.
The Extracellular Matrix (ECM) is a dynamic, three-dimensional network that provides far more than just structural scaffolding for tissues and organs. It serves as a sophisticated signaling hub that actively regulates fundamental cellular processes including proliferation, migration, differentiation, and survival through its intricate control of growth factor bioavailability [16] [17]. The ECM achieves this regulatory function primarily through the sequestration of growth factors within its structure, creating localized reservoirs that are protected from degradation and can be released in a spatially and temporally controlled manner in response to specific physiological cues [16]. This mechanism is crucial for maintaining tissue homeostasis and orchestrating complex biological processes such as development, wound healing, and regeneration.
In the context of 3D cell culture research, understanding these ECM-growth factor dynamics is particularly critical. The native 3D microenvironment presents a more physiologically relevant context for studying cell behavior compared to traditional 2D cultures, as it better recapitulates the complex cell-ECM interactions that occur in vivo [7]. The ECM's role as a growth factor reservoir significantly influences cellular responses in 3D environments, affecting experimental outcomes and their translational relevance for drug development and tissue engineering applications.
Molecular Mechanisms of Growth Factor Sequestestration
ECM Components as Binding Reservoirs
The ECM sequesters growth factors through specific molecular interactions with its various structural components. Key among these are proteoglycans, which possess glycosaminoglycan (GAG) chains that electrostatically interact with growth factors.
Table 1: Major ECM Components Involved in Growth Factor Sequestration
| ECM Component | Structure | Example Growth Factors Bound | Binding Mechanism |
|---|---|---|---|
| Heparan Sulfate Proteoglycans (HSPGs) | Protein core with heparan sulfate GAG chains | FGF2, HGF, VEGF, TGF-β | Electrostatic interactions between negatively charged sulfate groups on GAG chains and basic amino acids in growth factors [17] |
| Hyaluronic Acid (HA) | Linear polysaccharide, non-sulfated GAG | TGF-β, BMPs | Forms framework that binds proteoglycans; indirect sequestration via proteoglycan networks [17] |
| Fibrillin | Glycoprotein, forms microfibrils | TGF-β, BMPs | Latent TGF-β binding proteins (LTBPs) tether latent complexes to fibrillin in ECM [7] |
| Type IV Collagen | Network-forming collagen, basement membranes | VEGF, FGF2 | Heparin-binding domains in growth factors interact with collagen-associated HSPGs [7] |
The sequestration mechanism serves multiple biological functions: it stabilizes growth factors against proteolytic degradation, creates local concentration gradients that guide cellular responses, and prevents premature receptor activation until appropriate physiological signals trigger release [17]. For example, HS proteoglycans can facilitate fibroblast growth factor 2 (FGF2), hepatocyte growth factor (HGF), and transforming growth factor beta (TGF-β) signaling by immobilizing them via their heparin-binding domains [17].
Regulatory Dynamics of Sequestration and Release
The ECM environment dynamically regulates the equilibrium between growth factor sequestration and release through several integrated mechanisms:
Enzymatic Remodeling: Matrix metalloproteinases (MMPs) and other proteases cleave ECM components to release bound growth factors. This process is counterbalanced by tissue inhibitors of metalloproteinases (TIMPs), which maintain homeostasis [17].
Mechanical Force Application: Cellular traction forces can expose cryptic binding sites in ECM proteins like fibronectin, altering growth factor binding affinity and availability [17].
Receptor Availability Modulation: Recent research reveals that cholesterol-rich membrane domains such as caveolae can sequester growth factor receptors (e.g., TGFβR and EGFR), preventing their activation even when growth factors are present. This adds another layer of regulation to ECM-growth factor signaling [18].
Diagram 1: Growth Factor Sequestration and Release from ECM. The diagram illustrates how growth factors are sequestered in the ECM reservoir through proteoglycan binding and latent complex formation, and released via proteolytic cleavage, mechanical force, or cholesterol modulation. A critical activation barrier involves receptor sequestration in cholesterol-rich caveolae, which can be disrupted by cholesterol modulation to enable signaling.
Experimental Approaches in 3D Culture Systems
Recapitulating ECM-Growth Factor Dynamics
Advanced 3D culture models have been developed to better mimic the physiological ECM environment and study growth factor dynamics. These include:
Patient-Derived Scaffolds (PDS): Created through decellularization of human tissues, PDS preserve native ECM architecture and composition. A 2025 study decellularized human breast tissues using an SDS-based protocol that effectively removed cellular components while preserving key ECM constituents including collagen and glycosaminoglycans [3]. The resulting scaffolds maintained structural integrity and biochemical complexity, allowing researchers to demonstrate that tumor-specific ECM characteristics promote cancer cell proliferation and aggressive behavior compared to normal ECM [3].
Biomimetic Hydrogel Systems: Engineered scaffolds incorporating ECM components enable controlled study of growth factor presentation. A 2025 wound healing study developed gelatin-based hydrogels that incorporated growth factors (EGF, PDGF, VEGF) with cyclodextrins to modulate receptor accessibility [18]. These hydrogels demonstrated sustained release kinetics rather than burst release, providing more physiological growth factor delivery profiles that significantly improved healing outcomes in diabetic mouse models [18].
Methodologies for Studying Sequestered Growth Factors
Table 2: Experimental Protocols for Analyzing ECM-Growth Factor Interactions
| Method | Protocol Overview | Key Applications | Technical Considerations |
|---|---|---|---|
| Scaffold Decellularization | 1. Tissue dissection into thin sections2. SDS-based detergent treatment with agitation3. DNase/RNase enzymatic treatment4. Sterilization and storage in PBS | Preservation of native ECM architecture and endogenous growth factors; creation of physiological 3D culture environments [3] | Confirm complete DNA removal (<50 ng/mg tissue); verify retention of key ECM components (collagen, GAGs) through biochemical assays [3] |
| ECM Component Quantification | 1. Tissue digestion with proteinase K2. GAG content: dimethylmethylene blue assay3. Collagen content: hydroxyproline assay4. Sulfated GAGs: alcian blue staining | Comparative analysis of ECM composition between normal and pathological states; correlation of ECM changes with cellular behaviors [3] | Include standard curves for accurate quantification; use complementary methods (histology, biochemical assays) for validation |
| Growth Factor Release Profiling | 1. Incorporation into hydrogel systems2. ELISA-based quantification of released factors3. Assessment of bioactivity via cell-based assays4. Modulation with cholesterol-disrupting agents (e.g., MβCD) | Evaluation of release kinetics; testing therapeutic efficacy of sustained delivery systems; investigating receptor accessibility [18] | Use physiological buffers; monitor stability of released factors; include relevant biological endpoints (migration, proliferation) |
Pathophysiological Implications and Therapeutic Targeting
Dysregulation in Disease States
Disruption of normal ECM-growth factor dynamics contributes significantly to disease pathogenesis. In chronic wounds, elevated cholesterol synthesis leads to sequestration of growth factor receptors within lipid rafts, impairing their signaling capacity despite adequate growth factor presence [18]. This pathological mechanism was demonstrated through spatial analysis of human chronic wound biopsies, which revealed altered distributions of cholesterol and other lipid species compared to acute wounds [18].
In cancer progression, tumor-associated ECM remodeling creates a microenvironment that promotes aggressive behavior. Research using patient-derived scaffolds showed that breast cancer cells cultured on tumor-derived ECM significantly upregulated invasive genes (CAV1, CXCR4, CNN3, MYB, TGFB1) and secreted higher levels of IL-6 compared to those cultured on normal ECM [3]. This suggests that tumor-specific ECM alterations actively drive malignant progression rather than merely accompanying it.
Therapeutic Strategies Targeting ECM-Growth Factor Interactions
Emerging therapeutic approaches aim to restore normal ECM-growth factor dynamics:
Cholesterol Modulation: Cyclodextrins (MβCD, HβCD) extract cholesterol from cellular membranes, disrupting caveolae and releasing sequestered growth factor receptors. In diabetic wound models, this approach restored growth factor responsiveness and significantly accelerated healing [18].
ECM-Targeted Delivery Systems: Nanotechnology-based strategies and biomaterial scaffolds enable localized delivery of growth factors with controlled release kinetics, enhancing therapeutic efficacy while minimizing off-target effects [16].
Enzymatic ECM Remodeling: Targeted approaches to normalize pathological ECM composition and structure are being explored to restore physiological growth factor signaling in conditions like fibrosis and cancer [16].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying ECM-Growth Factor Dynamics
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Decellularization Agents | Sodium dodecyl sulfate (SDS), Triton X-100, DNase/RNase enzymes | Creation of patient-derived scaffolds (PDS) | Removal of cellular material while preserving native ECM structure and composition [3] |
| ECM Component Assays | Dimethylmethylene blue (GAGs), hydroxyproline assay (collagen), alcian blue staining | Quantitative and qualitative ECM analysis | Measurement of specific ECM components to characterize scaffold composition and integrity [3] |
| Cholesterol Modulators | Methyl-β-cyclodextrin (MβCD), 2-hydroxypropyl-β-cyclodextrin (HβCD) | Restoring growth factor receptor accessibility | Extraction of cholesterol from membrane lipid rafts to release sequestered growth factor receptors [18] |
| Biomaterial Scaffolds | Gelatin-based hydrogels, decellularized ECM scaffolds, synthetic polymer matrices | 3D cell culture and therapeutic delivery platforms | Providing physiological context for cell growth; enabling controlled release of bioactive factors [18] [19] |
| Protease Inhibitors | TIMP proteins, broad-spectrum protease inhibitors | Studying ECM turnover and growth factor release | Inhibition of endogenous proteases to stabilize ECM-bound factors and analyze baseline conditions [17] |
The recognition of the ECM as a dynamic signaling hub rather than a passive scaffold has fundamentally transformed our understanding of tissue regulation and cellular behavior. The controlled sequestration and regulated release of growth factors represents a crucial mechanism for spatial and temporal control of signaling in physiological and pathological processes. For researchers utilizing 3D culture systems, faithfully recapitulating these ECM dynamics is essential for generating biologically relevant data and predictive models.
Future research directions will likely focus on developing increasingly sophisticated ECM-mimetic platforms that dynamically respond to environmental cues, integrating multiple cell types to better model the complexities of tissue microenvironments, and advancing therapeutic strategies that target specific aspects of ECM-growth factor interactions for conditions ranging from chronic wounds to cancer [16] [17]. As these technologies evolve, they will continue to enhance our ability to study and manipulate the fundamental processes that govern tissue homeostasis and disease.
Diagram 2: Experimental Workflow for ECM-Growth Factor Research. The diagram outlines a systematic approach to studying ECM-growth factor dynamics, beginning with comprehensive ECM analysis, progressing through appropriate 3D model selection, testing targeted interventions, and concluding with multifaceted outcome assessment.
The extracellular matrix (ECM) is a dynamic, three-dimensional network that provides far more than just structural support to tissues; it is a rich source of biochemical and mechanical cues that fundamentally govern cellular behavior [16]. Its mechanical properties, particularly stiffness—the resistance of a material to deformation—serve as a critical regulator of cell fate, influencing processes ranging from differentiation and proliferation to migration and apoptosis [16]. The process by which cells sense and respond to these mechanical cues, known as mechanotransduction, is therefore pivotal to understanding development, homeostasis, and disease pathogenesis. This whitepaper delves into the molecular mechanisms of stiffness-directed cell fate, framed within the advancing context of 3D cell culture research, which offers more physiologically relevant environments than traditional 2D models [6]. For researchers and drug development professionals, mastering this mechanical dialogue is key to developing novel therapeutic strategies for conditions like cancer, fibrosis, and regenerative medicine [20] [16].
Fundamental Concepts: ECM Composition and Stiffness
The ECM's composition is a complex interplay of macromolecules, including collagens (providing tensile strength), elastin (conferring resilience), fibronectin (crucial for cell adhesion), and glycosaminoglycans (GAGs) (maintaining structural hydration and facilitating signaling) [16]. The specific composition and architectural organization of these components determine the matrix's mechanical properties.
Stiffness, often quantified as the Young's modulus (E), varies significantly across tissues and pathological states, providing a mechanical context that cells constantly monitor. The following table summarizes typical stiffness values for various biological contexts.
Table 1: ECM Stiffness Across Tissues and Pathological States
| Tissue or Condition | Approximate Stiffness | Biological Context |
|---|---|---|
| Brain (Soft Tissue) | < 2 kPa | Represents a soft, compliant microenvironment [16]. |
| Healthy Breast Tissue | ~0.17 kPa | Baseline soft tissue stiffness [16]. |
| Breast Cancer Tumor | ~4.0 kPa | Significant stiffening compared to healthy tissue [16]. |
| Fibrotic Lung | ~16.5 kPa | 5-10 times stiffer than healthy lung tissue [16]. |
| Bone (Hard Tissue) | 40-55 MPa | Represents a rigid, load-bearing environment [16]. |
Cells perceive these stiffness gradients through a process called durotaxis, where they actively migrate toward stiffer regions [16]. This sensing is not passive; cells probe their environment by exerting contractile forces through actin-myosin cytoskeleton and integrin-based adhesions, gauging the resistance the matrix offers [21].
Molecular Mechanisms of Mechanosensing and Transduction
The cellular response to ECM stiffness is orchestrated through an integrated network of mechanosensors and signaling pathways that convert external physical forces into biochemical signals.
Key Mechanosensors and Signaling Hubs
The mechanotransduction process involves a series of molecular players working in concert:
- Integrins: Transmembrane receptors that bind to ECM ligands externally and link to the actin cytoskeleton internally, forming focal adhesions. These structures are primary sites for force transmission [20] [16] [21].
- Piezo1 Channels: Mechanosensitive ion channels that open in response to membrane tension, allowing Ca²⁺ influx, which acts as a rapid second messenger. For instance, in Group 2 innate lymphoid cells (ILC2s), Piezo1 activation triggers calcium influx and subsequent mTOR signaling, selectively enhancing IL-13 protein production [22].
- YAP/TAZ Pathway: Transcriptional co-activators that are pivotal downstream effectors of mechanotransduction. In a soft ECM, YAP/TAZ are sequestered in the cytoplasm and degraded. On a stiff ECM, mechanical forces from the cytoskeleton promote their nuclear translocation, where they partner with transcription factors like TEAD to drive expression of genes promoting proliferation and stemness [20] [16].
The interplay between these components is summarized in the following diagram.
Diagram 1: Core mechanotransduction signaling from ECM stiffness. The diagram illustrates how stiff ECM promotes integrin-mediated force transmission, leading to YAP/TAZ nuclear localization and gene activation, and how Piezo1 channel activation triggers calcium-mTOR signaling to regulate protein translation.
The Nuclear Connection
Mechanical signals are not limited to the cytoplasm. Forces are transmitted from the cytoskeleton to the nucleus via the LINC complex, influencing nuclear architecture and gene expression [20]. This can lead to changes in chromatin organization and direct mechanical regulation of transcription. During events like cell migration across stiff matrix interfaces, this force transmission can cause nuclear deformation and even DNA damage, further influencing cell phenotype [21].
Quantitative Data: ECM Stiffness Directs Specific Cell Fates
The impact of ECM stiffness on cell lineage specification is demonstrated by quantitative experimental data across multiple cell types. The following table consolidates key findings from recent research.
Table 2: Experimental Evidence of Stiffness-Directed Cell Fate
| Cell Type | ECM Stiffness | Cell Fate / Response | Key Readouts & Quantitative Data |
|---|---|---|---|
| Hepatocellular Carcinoma (HCC) Cells [16] | 1 kPa (Soft) vs. 12 kPa (Stiff) | Proliferation | Stiffness (12 kPa) activated AKT and STAT3 pathways, promoting tumor proliferation. |
| Breast Cancer Cells (MCF-7) [3] | Tumor vs. Normal PDS | Aggressive Phenotype | Tumor PDS (stiffer) induced ~4x higher IL-6 secretion (122.91 vs. 30.23 pg/10⁶ cells) and upregulated invasiveness genes (CAV1, CXCR4, TGFB1). |
| Group 2 Innate Lymphoid Cells (ILC2s) [22] | Mechanical stress via Piezo1 | IL-13 Production | Piezo1 activation (e.g., by agonist Yoda1) selectively enhanced IL-13 protein production via Ca²⁺-mTOR axis, without affecting IL-5. |
| Invasive Breast Cancer Cells (MDA-MB-231) [21] | Dense vs. Open Collagen I Matrix | Phenotype Switching & Migration | Cells transmigrating from dense to open matrix showed increased contractility, directed migration, and misregulated nuclear mechanotransduction (YAP, emerin). |
Experimental Approaches in 3D Culture Models
Moving beyond 2D cultures is critical for replicating the in vivo mechanical microenvironment. Several advanced 3D models are now employed.
Patient-Derived Scaffolds (PDS)
This innovative technique utilizes decellularized human tissue to create a biologically and mechanically relevant ECM scaffold for cell culture [3].
- Protocol Workflow:
- Tissue Acquisition: Surgically resected breast tumor and normal healthy breast tissues are obtained.
- Decellularization: Tissues are treated with an SDS-based protocol to remove all cellular components while preserving key ECM components (collagen, GAGs). Validation includes H&E and DAPI staining showing no nuclei, and DNA quantification confirming significant reduction (e.g., from 527.1 ng/μL to 7.9 ng/μL) [3].
- Characterization: Histological staining (Trichrome, Sirius Red) and biochemical assays confirm preservation and abundance of ECM components. Tensile testing confirms higher stiffness in tumor PDS versus normal PDS [3].
- 3D Cell Culture: Cancer cell lines (e.g., MCF-7) are seeded onto the PDS and cultured. Outcomes like cell viability (MTT assay), proliferation (DAPI count), gene expression (qPCR), and cytokine secretion (ELISA) are analyzed to assess the impact of tumor-specific ECM [3].
The workflow and key outcomes of this approach are visualized below.
Diagram 2: Patient-derived scaffold workflow for 3D culture. The process involves decellularizing human tissue to create a native ECM scaffold, which is characterized and used for 3D cell culture, enabling analysis of cell behavior in a realistic microenvironment.
Engineered Collagen I Interface Model
To study metastasis, a defined matrix interface model mimicking the boundary between dense tumor tissue and softer healthy tissue has been developed [21].
- Protocol Workflow:
- Surface Coating: Glass coverslips are coated with poly(styrene-alt-maleic anhydride) (PSMA) for covalent attachment of collagen.
- Sequential Polymerization: Two collagen type I solutions of different concentrations (creating different pore sizes and densities) are polymerized sequentially on the coverslip to create a sharp, defined interface.
- Cell Embedding and Analysis: Invasive breast cancer cells (e.g., MDA-MB-231) are embedded in the dense compartment.
- Live-Cell Imaging and PIV: Particle Image Velocimetry (PIV) is used to quantify collagen network deformation and cellular traction forces during transmigration.
- Immunostaining: Cells are fixed and stained for mechanotransduction markers (e.g., YAP localization, emerin) to correlate forces with signaling outcomes [21].
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and materials used in the featured experiments for studying ECM stiffness and mechanotransduction.
Table 3: Research Reagent Solutions for Mechanotransduction Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Collagen I | Major structural ECM protein for constructing 3D matrices; concentration controls pore size and stiffness. | Engineered interface models for studying cell transmigration [21]. |
| Piezo1 Agonist (Yoda1) | Selective chemical activator of the Piezo1 channel, used to probe its function. | Studying Piezo1-mediated calcium influx and its effect on ILC2 cytokine production [22]. |
| Piezo1 Inhibitor (GsMTx4) | Selective peptide inhibitor of Piezo1, used to block mechanosensitive channel activity. | Validating the role of Piezo1 in Yoda1-induced IL-13 upregulation [22]. |
| Patient-Derived Scaffolds (PDS) | Decellularized human tissue providing a native, patient-specific ECM microenvironment. | Culturing MCF-7 cells to study the effect of tumor-specific ECM on cancer cell aggression [3]. |
| YAP/TAZ Antibodies | Immunostaining to determine the subcellular localization (nuclear vs. cytoplasmic) of YAP/TAZ. | Assessing mechanotransduction pathway activation in cells on stiff vs. soft substrates or after transmigration [21]. |
| mTOR Inhibitors | Pharmacological blockers (e.g., rapamycin) of the mTOR pathway, a key downstream signaling node. | Confirming the role of mTOR in Piezo1-mediated translational control of cytokine production [22]. |
The evidence is unequivocal: ECM stiffness is a master regulator of cell lineage and fate, operating through conserved mechanotransduction pathways like integrin signaling, Piezo1, and YAP/TAZ. The adoption of physiologically relevant 3D models, such as Patient-Derived Scaffolds and engineered matrix interfaces, is providing unprecedented insights into how mechanical cues drive both normal physiology and disease progression, particularly in cancer and fibrosis [6] [3] [21].
For the field of drug discovery, this mechanistic understanding opens up a new frontier for therapeutic intervention: mechanomedicine [20]. Future efforts will focus on developing small molecules, biologics, and nanomedicines that target key nodes in the mechanotransduction network—such as Piezo1, ROCK, or YAP/TAZ-TEAD interaction—to normalize aberrant mechanical signaling [20] [22] [16]. Furthermore, the integration of 3D bioprinting and AI-driven analysis with these advanced culture platforms promises to enhance the scalability and predictive power of mechanobiology research, accelerating the development of next-generation diagnostics and targeted therapies [6]. By continuing to decode the mechanical language of the ECM, researchers and clinicians can look forward to a future where manipulating the tissue microenvironment becomes a central pillar of precision medicine.
The extracellular matrix (ECM) undergoes profound remodeling in pathological conditions, transitioning from a regulator of tissue homeostasis to a driver of disease progression in cancer and fibrosis. This whitepaper examines the parallel mechanisms underlying ECM dysregulation in these conditions, highlighting the critical roles of increased stiffness, altered composition, and aberrant cell-ECM signaling. Through comprehensive analysis of current research models and emerging therapeutic strategies, we demonstrate how targeting the pathological ECM offers promising avenues for intervention. The content is framed within the context of 3D cell culture research, which provides essential platforms for replicating the complex biomechanical and biochemical properties of diseased tissues, thereby enabling more accurate drug screening and mechanistic studies.
The extracellular matrix constitutes a dynamic, complex network of proteins, glycoproteins, and proteoglycans that provides structural support and biochemical cues essential for tissue development, homeostasis, and repair. The ECM is broadly classified into basement membrane (BM) and interstitial matrix (IM), each with distinct compositional and functional characteristics [23] [24]. The BM, composed primarily of collagen IV and laminin, forms a specialized sheet-like structure that surrounds epithelial, endothelial, and muscle cells, providing structural support and establishing cell polarity [23]. The IM, consisting mainly of fibrillar collagens (types I, III, V), fibronectin, and elastin, confers mechanical strength and elasticity to tissues [24]. In healthy tissues, the ECM undergoes continuous, tightly regulated remodeling that maintains tensional homeostasis through balanced synthesis and degradation [25].
Pathological ECM remodeling represents a fundamental hallmark of both cancer and fibrotic diseases, characterized by excessive deposition, altered organization, and post-translational modifications of ECM components [23] [24] [25]. This remodeling creates a self-perpetuating cycle where matrix stiffness and composition drive disease progression through mechanotransduction pathways. In cancer, the tumor microenvironment (TME) becomes characterized by a fibrotic stroma that promotes malignancy through enhanced tumor cell growth, survival, migration, and treatment resistance [23] [25]. Similarly, in fibrotic diseases affecting organs such as the lung, liver, and pancreas, aberrant ECM accumulation leads to tissue scarring, loss of function, and eventual organ failure [24] [26]. The concept of "mechanoreciprocity" describes how cells tune their cytoskeletal tension in response to ECM stiffness, subsequently remodeling their ECM to reach a new tensional equilibrium that typically favors disease progression [23].
Hallmarks of Pathological ECM Remodeling
Increased Stiffness and Cross-Linking
The pathological ECM is characterized by significantly increased stiffness primarily resulting from excessive deposition of fibrillar collagens and enhanced enzymatic cross-linking [23] [25]. This process is driven primarily by activated fibroblasts and cancer-associated fibroblasts (CAFs) that secrete abundant ECM proteins while simultaneously upregulating cross-linking enzymes such as lysyl oxidases (LOX) and transglutaminases [23] [24]. Collagen cross-linking occurs through a multi-step process initiated by lysyl hydroxylases (LHs) that catalyze lysine hydroxylation, followed by LOX-mediated oxidative deamination that generates reactive aldehydes forming covalent cross-links between collagen fibrils [23]. In tumors such as breast and lung cancers, upregulation of LH2 shifts collagen cross-links from lysine aldol-derived (LCCs) to hydroxylysine aldol-derived (HLCCs), resulting in a stiffer, more organized matrix that correlates with tumor aggression and reduced patient survival [23].
The biomechanical properties of the pathological ECM exhibit non-linear elasticity and viscoelastic behavior, meaning that stiffness increases with applied strain (strain-stiffening) and exhibits both solid and liquid characteristics [23]. This enables cellular contractions to significantly increase stiffness sensed by neighboring cells hundreds of microns away, facilitating long-range mechanical communication within the tissue [23]. In pulmonary fibrosis, healthy lung tissue stiffness typically ranges between 1-5 kPa, while fibrotic tissue exceeds 10 kPa, creating a mechanically aberrant environment that perpetuates disease progression [26].
Altered Composition and Architecture
Pathological remodeling fundamentally alters ECM composition and organization. In cancer, the normally isotropic collagen organization becomes anisotropically aligned, creating tracks that facilitate cancer cell migration and invasion [23]. This aligned collagen signature (TACS3 in breast cancer) correlates with tumor aggression and reduced patient survival [23]. Similar alignment patterns are observed in pancreatic ductal adenocarcinoma (PDAC), where highly aligned stromal collagen correlates with reduced post-surgical survival [23].
The quantitative alterations in ECM components between normal and pathological states are summarized in Table 1.
Table 1: Quantitative Comparison of ECM Components in Normal vs. Pathological Conditions
| ECM Component | Normal Tissue | Pathological Tissue | Functional Consequences |
|---|---|---|---|
| Total Collagen | 186.94 μg/mg (breast) [3] | 507.35 μg/mg (breast tumor) [3] | Increased stiffness, barrier function |
| Glycosaminoglycans | 1.62 μg/mg (breast) [3] | 3.07 μg/mg (breast tumor) [3] | Enhanced water retention, growth factor binding |
| Collagen Cross-linking | Low [23] | High (HLCC predominant) [23] | Increased tensile strength, resistance to degradation |
| Fibrillar Collagen Alignment | Isotropic [23] | Anisotropic (aligned) [23] | Creation of migration tracks for invasive cells |
| MMP Expression | Homeostatic levels [27] | Elevated (e.g., MMP-16) [27] | Enhanced ECM remodeling and invasion |
The compositional changes extend to specific ECM proteins. Tumor ECM shows significant overexpression of collagen IV, vimentin, and other structural components compared to normal ECM [3]. These alterations create a dense physical barrier that restricts drug delivery while simultaneously activating pro-fibrotic and pro-tumorigenic signaling pathways [28] [25].
Key Cellular Actors and Signaling Pathways
The development of pathological ECM is driven by activated mesenchymal cells, primarily myofibroblasts and cancer-associated fibroblasts (CAFs). These cells exhibit enhanced contractility, elevated expression of α-smooth muscle actin (αSMA), and excessive production of ECM components [24]. Myofibroblast activation depends on a complex signaling network centered around the TGF-β superfamily, beginning with mechanical stress-induced release of TGF-β from its latent complex, followed by canonical SMAD signaling and transcriptional upregulation of genes encoding αSMA and ECM proteins [24].
Cells sense and respond to the mechanical properties of the pathological ECM through multiple receptor systems, including integrins, discoidin domain receptors (DDRs), and mechanosensitive ion channels such as PIEZO1 [29] [25]. DDR1-mediated collagen signaling in pancreatic cancer, for instance, exacerbates fibrotic barriers that impede macromolecular drug delivery through PI3K/AKT/mTOR pathway activation [28]. The relationship between ECM stiffness, cellular sensing, and downstream signaling creates a vicious cycle that drives disease progression, as illustrated in Figure 1.
Figure 1: Vicious Cycle of Pathological ECM Remodeling. ECM stiffness activates mechanotransduction pathways that promote myofibroblast/CAF differentiation, leading to further ECM production and disease progression in a self-reinforcing loop.
Experimental Models for Studying Pathological ECM
3D Cell Culture Systems
Traditional two-dimensional (2D) cell cultures fail to replicate the complex cell-ECM interactions present in vivo, limiting their utility for studying pathological ECM remodeling [30]. Consequently, research has shifted toward three-dimensional (3D) models that better recapitulate the dynamic cell-cell and cell-matrix interactions within native tissues [30]. These 3D systems preserve cellular physiology and molecular characteristics while enhancing translational relevance [26].
Spheroid models represent one approach for 3D culture, where cancer cells self-aggregate into spherical structures that mimic aspects of solid tumors. Studies comparing 2D versus 3D cultures of MCF-7 and MDA-MB-231 breast cancer cells revealed notable phenotypic transitions supported by differential expression of epithelial-to-mesenchymal transition (EMT) markers and matrix components, including altered expression of syndecans and matrix metalloproteinases (MMPs) [30]. These models provide a matrix-free platform for studying intrinsic cellular aggregation properties but lack the physiological ECM context of native tissues.
Scaffold-based systems incorporate biological or synthetic matrices to provide both structural and biochemical cues. Patient-derived scaffolds (PDS) obtained through decellularization of surgically resected tissues preserve the native ECM architecture and composition, offering a highly physiological microenvironment for cell culture [3]. A detailed protocol for generating and utilizing PDS is provided in Section 3.3.
Synthetic hydrogel platforms offer precise control over mechanical and biochemical properties, enabling systematic investigation of specific ECM parameters. Poly(ethylene glycol) norbornene (PEG-NB) hydrogels, for instance, allow independent tuning of stiffness, degradation kinetics, and bioactive ligand presentation [26]. These systems have been used to model pulmonary fibrosis by replicating the stiffness of healthy (∼5 kPa) and fibrotic (∼19 kPa) lung tissue, demonstrating that combined mechanical and biochemical cues drive pathogenic cellular responses resembling in vivo fibrosis [26].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for ECM and Fibrosis Research
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Hydrogel Systems | PEG-NB [26], Matrigel [30], Collagen [26] | 3D cell culture | Provide tunable mechanical support and biochemical cues |
| Decellularization Agents | SDS [3] | Patient-derived scaffolds | Remove cellular content while preserving ECM structure |
| Pro-fibrotic Cocktail | TGF-β, TNF-α, IL-13 [26] | Disease modeling | Induce fibrotic phenotypes in vitro |
| MMP Substrates | MMP-degradable peptides (e.g., VPMS↓MRGG) [26] | Biomaterial design | Enable cell-mediated hydrogel remodeling |
| Adhesive Ligands | RGD (fibronectin mimic) [26], IGSR (laminin mimic) [26] | Mechanotransduction studies | Promote cell adhesion and signaling |
| Anti-fibrotic Drugs | Nintedanib [26] | Therapeutic screening | Inhibit fibroblast activation and ECM production |
| Mechanotransduction Modulators | DDR1/2 inhibitors [28], PIEZO1 activators [29] | Pathway analysis | Target specific mechanosensing pathways |
Detailed Experimental Protocol: Patient-Derived Scaffolds for Cancer ECM Studies
The use of patient-derived scaffolds (PDS) represents a cutting-edge approach for modeling the tumor ECM in its native context. Below is a detailed methodology adapted from recent breast cancer research [3]:
1. Tissue Acquisition and Preparation
- Obtain surgically resected breast tumor and normal adjacent tissue specimens from biobanks or fresh surgical collections.
- Process tissues into uniform fragments (e.g., 5mm³ pieces) using sterile surgical tools.
- Wash thoroughly in phosphate-buffered saline (PBS) containing antimicrobial agents (100 IU/mL penicillin, 100 μg/mL streptomycin, 10 μg/mL gentamycin sulfate, and 2.5 μg/mL amphotericin B) to remove residual blood and contaminants.
2. Decellularization Protocol
- Incubate tissue fragments in 1% sodium dodecyl sulfate (SDS) solution with continuous agitation for 24-48 hours at room temperature.
- Replace SDS solution every 12 hours until tissue becomes opaque and translucent.
- Rinse extensively with deionized water to remove residual detergent (6-8 washes over 24 hours).
- Treat with DNase I (50 U/mL in PBS) for 6 hours at 37°C to remove residual DNA.
- Perform final rinses with PBS containing antimicrobial agents.
- Store decellularized scaffolds in PBS at 4°C for immediate use or freeze at -80°C for long-term storage.
3. Quality Control and Validation
- Confirm decellularization through H&E staining showing absence of nuclear material while maintaining ECM architecture.
- Quantify DNA content to verify reduction to <50 ng/mg of tissue (from >500 ng/mg in native tissue).
- Assess retention of ECM components through:
- Glycosaminoglycan quantification (e.g., Blyscan assay)
- Collagen content measurement (e.g., hydroxyproline assay)
- Histological staining (Trichrome, PAS, Sirius red, Alcian blue)
- Immunohistochemistry for specific ECM proteins (collagen IV, vimentin)
- Evaluate mechanical properties through tensile testing to determine Young's modulus.
4. 3D Cell Culture on PDS
- Seed appropriate cell lines (e.g., MCF-7 breast cancer cells at 5,000-15,000 cells per scaffold) onto sterilized PDS.
- Culture in complete medium (DMEM with 10% FBS) for up to 15 days, monitoring cell viability and proliferation regularly.
- Assess functional outcomes including:
- Gene expression of invasiveness markers (CAV1, CXCR4, CNN3, MYB, TGFB1) via qRT-PCR
- Cytokine secretion profiles (e.g., IL-6 ELISA)
- Cell morphology and distribution within scaffolds (histology, SEM)
The complete workflow for PDS generation and application is visualized in Figure 2.
Figure 2: Workflow for Patient-Derived Scaffold Generation and Application. Surgical specimens are decellularized, validated, and used as physiological substrates for 3D cell culture and disease modeling.
Therapeutic Targeting of Pathological ECM
Anti-Fibrotic Strategies
Targeting the pathological ECM represents a promising therapeutic approach for both fibrotic diseases and cancer. Nintedanib, an FDA-approved anti-fibrotic drug for idiopathic pulmonary fibrosis (IPF), has demonstrated efficacy in 3D human lung models by reducing fibroblast activation and promoting epithelial repair genes [26]. Treatment with Nintedanib downregulated key fibroblast activation markers (ACTA2, COL1A1) while upregulating transitional and alveolar type I cell markers, indicating potential restoration of epithelial repair mechanisms [26].
Emerging strategies focus on specific ECM assembly and remodeling pathways. Inhibition of collagen cross-linking through LOX or LOX-like family members can reduce tissue stiffness and decrease tumor aggression [23]. Similarly, targeting DDR1-mediated collagen signaling in pancreatic cancer enhances macromolecular drug delivery by diminishing collagen I expression in pancreatic stellate cells [28]. Isoform-specific targeting has shown that inhibiting DDR1, but not DDR2, effectively reverses fibrotic barriers through modulation of the PI3K/AKT/mTOR pathway, particularly alternative mTOR complexes involving MEAK7 and GIT1 [28].
Challenges in ECM-Targeted Therapies
Despite the promising potential of ECM-targeted therapies, several challenges remain. The complexity and heterogeneity of the ECM across tissues and disease states complicates the development of broadly effective treatments [25]. Additionally, the dense fibrotic ECM acts as a physical barrier to drug delivery, potentially limiting the efficacy of therapeutic agents [28] [25]. There is also risk of off-target effects, as ECM components play essential roles in normal tissue homeostasis and repair [25].
Successful clinical translation will require sophisticated approaches that consider disease stage, specific ECM alterations, and combination therapies that simultaneously target multiple aspects of disease pathogenesis. The development of biomarkers to stage fibrosis and monitor disease activity represents a critical component for patient stratification and treatment monitoring [24].
The pathological ECM represents more than a passive scaffold in fibrotic diseases and cancer—it actively drives disease progression through biomechanical and biochemical signaling. Understanding the parallel mechanisms underlying ECM remodeling in these conditions provides valuable insights for therapeutic development. The emergence of sophisticated 3D culture models, including patient-derived scaffolds and tunable hydrogel systems, has significantly advanced our ability to study these processes in physiologically relevant contexts.
Future research directions should focus on developing increasingly sophisticated human 3D models that better capture the cellular heterogeneity and dynamic remodeling of diseased tissues. Additionally, the discovery of novel biomarkers to stage ECM remodeling and monitor therapeutic response will be essential for clinical translation. As our understanding of the pathological ECM continues to evolve, so too will opportunities for therapeutic intervention that disrupt the vicious cycle of ECM-driven disease progression.
Engineering the Cellular Niche: Techniques for ECM-Mimetic 3D Culture
In the field of 3D cell culture research, the Extracellular Matrix (ECM) is far more than a passive scaffold; it is a dynamic, information-rich microenvironment that is fundamental to directing cell behavior, from differentiation and proliferation to tissue-specific function [31]. The transition from traditional two-dimensional (2D) culture to three-dimensional (3D) models is driven by the need to better recapitulate the physiological environment, where cell-to-cell interactions and diffusion gradients create tissue-like conditions that are impossible to achieve on a flat plastic surface [32]. Within this context, Decellularized ECM (dECM) scaffolds have emerged as a premier platform technology. They are engineered by removing the cellular components from native tissues or organs while preserving the intricate 3D architecture and biochemical composition of the original ECM [33]. This process yields a non-immunogenic biological template that provides the critical mechanical support, biochemical cues, and tissue-specific context essential for advanced 3D cell culture models, regenerative therapies, and drug screening applications [34] [35].
Fabrication of dECM Scaffolds: Methodologies and Protocols
The core objective of decellularization is the complete removal of cellular material—a source of immunogenicity—while minimizing damage to the structural and functional integrity of the native ECM. The success of a protocol depends on factors such as tissue density, lipid content, and thickness [33].
Core Decellularization Techniques
Decellularization methods are typically classified into three categories, which are often used in combination [31] [36]:
- Physical Methods: These techniques disrupt cell membranes through physical forces. Freeze-thaw cycles are common, where the formation of intracellular ice crystals causes cell lysis. Other methods include immersion and agitation, and perfusion for whole organs [33].
- Chemical Methods: This involves the use of chemical agents to lyse cells and dissolve cytoplasmic components.
- Ionic Detergents: Sodium dodecyl sulfate (SDS) is highly effective at solubilizing lipid membranes and nuclear material but can disrupt ECM structure and reduce glycosaminoglycan (GAG) content [31] [37].
- Non-ionic Detergents: Triton X-100 disrupts lipid-lipid and lipid-protein interactions but is less effective for dense tissues [31].
- Acidic/Basic Solutions: Alkaline and acid solutions can degrade nucleic acids and disrupt cell membranes [31].
- Enzymatic Methods: Enzymes like nucleases (DNase, RNase) are used to digest residual genetic material after cell lysis. Trypsin is also used to dissociate cells [38].
The workflow below illustrates the general process for creating and applying a dECM scaffold.
Experimental Protocol: Cartilage Decellularization
A 2025 study provides a detailed protocol for creating a dECM bioink for cartilage tissue engineering [37].
- Tissue Source: Native cartilage tissue.
- Decellularization Protocol:
- Physical Decellularization: Subject the tissue to multiple freeze-thaw cycles. This involves immersion in liquid nitrogen followed by thawing in a water bath to disrupt chondrocytes.
- Chemical Decellularization: Treat the tissue with an adjusted concentration of Sodium Dodecyl Sulfate (SDS) to solubilize cell membranes and remove cellular debris while minimizing collagen damage.
- dECM Preparation: The decellularized cartilage matrix is then solubilized using a urea extraction method to obtain the dECM component for bioink formulation [37].
- Validation:
- Histology: Hematoxylin and Eosin (H&E) staining confirmed the removal of chondrocytes, with only empty lacunae visible.
- Biochemical Assay: A Bradford assay demonstrated that approximately 59% of the protein content was preserved, indicating successful decellularization with substantial ECM retention [37].
Characterization of dECM Scaffolds: Quantitative and Qualitative Analysis
Rigorous characterization is essential to confirm the efficacy of decellularization and the functional properties of the resulting dECM scaffold.
Biochemical and Structural Analysis
The following table summarizes key characterization methods and typical outcomes from recent research.
Table 1: Key Characterization Methods for dECM Scaffolds
| Analysis Type | Method | Purpose & Outcome | Reference |
|---|---|---|---|
| Cellular Removal | Hematoxylin & Eosin (H&E) Staining | Visual confirmation of cell removal; presence of empty lacunae indicates success. | [37] |
| Protein Content | Bradford Assay | Quantifies total protein preservation post-decellularization. A study showed ~59% retention. | [37] |
| Rheology | Oscillatory Rheometry | Measures viscoelastic properties (Storage Modulus G', Loss Modulus G''). Essential for bioprintability. | [37] |
| Mechanical | Uniaxial Tensile Test | Determines mechanical strength, elasticity, and damping properties critical for load-bearing tissues. | [37] |
| Biocompatibility In Vitro | Live/Dead Assay & Cell Viability Test | Evaluates cytocompatibility; a dECM/Gellan Gum scaffold showed ~97% cell viability. | [37] |
| Functional Capacity | Alcian Blue Staining | Detects deposition of Glycosaminoglycans (GAGs), confirming cartilage-specific matrix production. | [37] |
Functional and Rheological Properties
For applications like 3D bioprinting, the functional performance of dECM-based bioinks is paramount.
Table 2: Functional Properties of a dECM-Gellan Gum Bioink vs. Control
| Property | Gellan Gum Bioink (GGb) Control | dECM/Gellan Gum Bioink (GG/dECMb) | Biological Significance |
|---|---|---|---|
| Cross-linking Degree | 6.65 ± 0.48% | 5.04 ± 0.79% | Lower cross-linking may enhance nutrient diffusion and cell remodeling. |
| Contact Angle (°) | Not Specified | 44.27 ± 6.0 | Indicates higher hydrophilicity, which promotes cell adhesion and spreading. |
| Shear-Thinning | Present | Present | Essential for extrudability during 3D bioprinting. |
| Mechanical Behavior | Elastic | Damping | Damping is crucial for cartilage to absorb mechanical shock. |
| Cell Viability | Lower | 97.41 ± 1.02% | High viability confirms the bioactive, pro-survival cues in dECM. |
| GAG Deposition | Lower | Enhanced | Confirms the dECM bioink's ability to promote cartilage-specific differentiation. |
The Scientist's Toolkit: Essential Reagents for dECM Research
The following table catalogs key reagents and materials used in the fabrication and evaluation of dECM scaffolds, as cited in the literature.
Table 3: Research Reagent Solutions for dECM Scaffold Development
| Reagent / Material | Function in dECM Research | Example Application |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for effective cell membrane solubilization and nuclear material removal. | Used in cartilage decellularization combined with freeze-thaw cycles [37]. |
| Triton X-100 | Non-ionic detergent for disrupting lipid-lipid and lipid-protein interactions. | Applied in the perfusion decellularization of rat pancreas [38]. |
| DNase/RNase | Enzymatic degradation of residual DNA and RNA to reduce immunogenicity. | Common final step in decellularization protocols to remove nucleic acids [38]. |
| Gellan Gum | A polysaccharide hydrogel that provides structural integrity and bioprintability. | Mixed with cartilage dECM to create a novel, printable bioink [37]. |
| Urea | A chaotropic agent used to solubilize and extract dECM proteins from tissues. | Method for preparing dECM with high GAG content for bioink formulation [37]. |
| Trypsin/EDTA | Enzymatic (Trypsin) and chelating (EDTA) agent for cell dissociation from ECM. | Often used in combination with other agents for cell removal [36]. |
Applications in 3D Cell Culture and Beyond
dECM scaffolds bridge the gap between simple 3D culture systems and the complex in vivo microenvironment.
- Physiologically Relevant 3D Models: dECM scaffolds provide the tissue-specific biochemical and biophysical cues that guide stem cell differentiation and maintain the phenotype of primary cells in culture. This is a significant advancement over synthetic scaffolds or animal-derived matrices like Matrigel [32] [36].
- Drug Screening and Disease Modeling: dECM-based 3D models are increasingly used to create more predictive platforms for drug testing and modeling human diseases. They offer a patient-specific and physiologically relevant context to study disease progression and drug responses, advancing personalized medicine [35].
- 3D Bioprinting: Solubilized dECM can be processed into bioinks for 3D bioprinting. These "tissue-inks" allow for the fabrication of complex, patient-specific constructs that mimic the native tissue microenvironment. This has been demonstrated for heart, muscle, nerve, and cartilage tissues [38] [37].
- Whole Organ Engineering: Perfusion decellularization of entire organs (e.g., heart, lung, liver, kidney) produces an intact ECM scaffold with preserved vascular networks. These can be recellularized to create bioartificial organs for transplantation research [33].
Decellularized ECM scaffolds successfully preserve nature's blueprint for tissue architecture and function, making them an indispensable tool in modern 3D cell culture research. By providing a tissue-specific microenvironment that orchestrates cell behavior, they enable the development of highly predictive in vitro models, advance the frontiers of regenerative medicine, and create new pathways for drug discovery. Future research will focus on standardizing decellularization protocols, improving the mechanical properties of dECM-based bioinks, and scaling up production to fully realize the clinical potential of this transformative technology.
The extracellular matrix (ECM) is far from a passive scaffold; it is a dynamic, instructive environment that actively regulates cell behavior and tissue function. In every tissue, ECM macromolecules provide critical biochemical, structural, and mechanical cues that guide cell fate decisions, influencing processes from embryogenesis to disease progression [31] [39]. The recognition of this fundamental role has driven the development of three-dimensional (3D) cell culture models that more faithfully replicate the in vivo microenvironment than traditional two-dimensional (2D) systems. Among these, hydrogels—water-swollen polymeric networks—have emerged as premier ECM-mimetic platforms due to their exceptional biocompatibility and highly tunable properties [39] [40].
This technical guide explores how synthetic and natural hydrogels serve as precise tools for controlling what cells "see" (biochemical and structural cues) and "feel" (mechanical and dynamic cues) in 3D cultures. Framed within the broader thesis of ECM biology, we detail how strategic hydrogel design can decode the complex language of the cellular microenvironment, offering researchers unparalleled control for fundamental discovery and therapeutic development.
What Cells "See": Biochemical and Structural Design of Hydrogels
Biochemical Composition and Ligand Presentation
The biochemical makeup of the native ECM is a complex assortment of proteins, glycosaminoglycans, and growth factors. Hydrogels recapitulate this environment through their incorporated bioactive motifs.
- Natural Hydrogels: Materials like Matrigel, collagen, and hyaluronic acid (HA) inherently present native biological signals. For instance, HA-based hydrogels have been a predominant focus in recent research due to their versatility and biocompatibility [41].
- Synthetic Hydrogels: Platforms based on polymers like poly(ethylene glycol) (PEG) offer a "blank slate." Bioactivity is introduced by conjugating specific adhesive peptides (e.g., RGD for integrin binding) or enzyme-sensitive sequences (e.g., MMP-degradable crosslinkers) [39] [42]. This allows for precise control over the identity, density, and spatial distribution of biochemical signals.
A critical advancement is the ability to preserve native ECM composition in a controlled system. The DECIPHER (DECellularized In situ Polyacrylamide Hydrogel–ECM hybRid) method stabilizes decellularized young or aged cardiac tissue within a tunable synthetic hydrogel. This platform maintains the native ligand landscape (collagen, fibronectin, laminin) while allowing independent mechanical control, enabling the discovery that a young biochemical signature can outweigh the profibrotic mechanical cues of an aged ECM in promoting cardiac fibroblast quiescence [43].
Architectural Cues and Topography
Cells "see" the physical architecture of their surroundings—the porosity, fiber alignment, and nanoscale topography. These structural features dictate cell morphology, migration, and spatial organization.
- Fiber Architecture: Native ECM is often fibrous. Hydrogels can be engineered to mimic this using techniques like electrospinning to create micro-/nano-fibrous structures that guide cell orientation [31].
- Pore Size and Mesh Size: The hydrogel mesh size (typically <20 nm) governs solute transport but is too small for cell migration. To enable 3D migration, hydrogels must be designed with cell-sized paths or be degradable, allowing cells to create their own migration routes [40]. Quantification of architectural parameters such as branch points, fractal dimension, and alignment in DECIPHER scaffolds has confirmed that key differences between young and aged ECM architectures can be preserved in hydrogel culture systems [43].
Table 1: Key Biochemical and Structural Parameters for Hydrogel Design
| Parameter | Design Consideration | Cellular Impact | Example Materials |
|---|---|---|---|
| Adhesive Ligand | Type, density, spatial patterning | Cell adhesion, spreading, survival, differentiation | RGD peptides, fibronectin, laminin [39] |
| Degradation Profile | Protease-sensitive crosslinks (MMP, aggrecanase) | Cell invasiveness, matrix remodeling, release of trapped factors | MMP-sensitive peptides (e.g., CGPQGIAGQGC) [42] |
| Architecture | Fiber formation, pore size, anisotropy | Cell polarity, migration mode, tissue morphogenesis | Electrospun fibers, decellularized ECM [31] |
| Growth Factor Delivery | Covalent immobilization, non-covalent sequestration | Stem cell differentiation, angiogenesis, inflammation | Heparin-based binding, affinity peptides [31] |
What Cells "Feel": Mechanical and Dynamic Properties of Hydrogels
Static Mechanical Properties
The mechanical stiffness of the microenvironment is a powerful regulator of cell behavior through mechanotransduction pathways. Hydrogels excel in this domain due to their highly tunable mechanical properties.
- Stiffness Tuning: By varying polymer concentration, crosslinking density, or network structure, hydrogels can be engineered to mimic tissues ranging from the soft brain (~1 kPa) to stiff bone (>10 kPa) [31] [41]. For example, in the DECIPHER system, polyacrylamide hydrogel formulations were optimized to mimic either young (~11.5 kPa) or aged (~39.6 kPa) cardiac tissue stiffness [43].
- Impact on Cell Fate: Stiffness gradients can induce durotaxis (directional migration towards stiffer regions), and matrix stiffness directly influences lineage specification—softer matrices promote neurogenesis, while stiffer matrices favor osteogenesis [31] [39].
Dynamic and "Smart" Mechanical Properties
Native tissues are not static; their mechanical properties change over time due to development, disease, or rhythmic physiological processes (e.g., heartbeat, breathing) [44]. A new generation of "smart" hydrogels is being developed to capture this dynamic complexity.
- Photo-tunable Hydrogels: Systems incorporating photoswitchable proteins like Photoactive Yellow Protein (PYP) enable rapid, reversible stiffness changes in response to blue light. Using such a platform, researchers discovered that cyclic rigidity changes at specific frequencies (e.g., 1-minute intervals) can enhance cellular traction forces and mechanotransduction beyond what is possible on statically rigid surfaces [44].
- Remote Force Application: Hydrogels embedded with near-infrared-responsive macromolecular actuators (e.g., CD-PNIPAM) allow precise mechanical stimulation of specific integrin subtypes in 3D. This technology has revealed that mechanical force parameters (magnitude, frequency, duration) can trigger specific cancer cell migration behaviors, such as a mesenchymal-to-amoeboid transition, in an integrin-dependent manner [42].
- Viscoelasticity: Unlike purely elastic synthetic hydrogels, native tissues are viscoelastic—they exhibit time-dependent mechanical responses. Advanced hybrid scaffolds, such as the DECIPHER system, successfully replicate this property, displaying loss moduli that match reported values for cardiac tissue [43].
Table 2: Key Mechanical and Dynamic Properties of Hydrogels
| Property | Definition | Hydrogel Design Strategy | Biological Relevance |
|---|---|---|---|
| Stiffness (Elastic Modulus) | Resistance to deformation | Varying crosslink density, polymer concentration | Lineage specification, durotaxis, disease modeling [31] [43] |
| Viscoelasticity | Time-dependent stress-strain response | Using dynamic covalent bonds, interpenetrating networks | Embryonic development, wound healing, cancer progression [43] |
| Stress Relaxation | Dissipation of stress under constant strain | Incorporating reversible crosslinks | Cell spreading, proliferation, and differentiation [44] |
| Dynamic Stiffness | Spatiotemporal control of rigidity | Photoswitching proteins (PYP), thermo-responsive polymers (PNIPAM) | Modeling development and disease; studying mechanosensing memory [44] [42] |
Experimental Protocols and Methodologies
Protocol: Fabrication of DECIPHER Hybrid Scaffolds
This protocol enables the creation of hydrogels with decoupled control over biochemical composition (from native ECM) and mechanical stiffness [43].
- Sample Preparation: Fix thin sections (e.g., 200 µm) of fresh or frozen young or aged murine cardiac tissue onto methacrylated coverslips.
- Hydrogel-Tissue Stabilization:
- Incubate the tissue with a solution of acrylamide/bis-acrylamide and the crosslinker N-methylolacrylamide.
- Expose to UV light to polymerize the polyacrylamide hydrogel, creating an interpenetrating network that covalently links to the tissue.
- In Situ Decellularization:
- Treat the stabilized hybrid construct with a solution of sodium deoxycholate (SDC) and deoxyribonuclease (DNase) to remove cellular material and nucleic acids.
- Validate decellularization using a PicoGreen dsDNA assay and confirm preservation of ECM composition via immunohistochemistry and sGAG/collagen quantification.
- Cell Seeding: Seed primary cells (e.g., cardiac fibroblasts) onto the surface of the acellular DECIPHER scaffold for culture and analysis.
Protocol: Assessing (CAR-)T Cell Function in 3D Hydrogels
This methodology is critical for preclinical evaluation of cell-based immunotherapies using chemically defined hydrogels [45].
- Hydrogel Preparation:
- NFC Hydrogel: Use a commercially available, chemically defined nanofibrillar cellulose hydrogel. Encapsulate cells at room temperature.
- Matrigel/BME: Thaw and handle these animal-derived matrices on ice according to standard protocols.
- 3D Cell Encapsulation:
- Mix murine CD4+ T cells or human CAR-T cells with the hydrogel precursor solution to achieve a homogeneous 3D distribution.
- For NFC, the gel forms spontaneously. For Matrigel/BME, incubate at 37°C to trigger thermal gelation.
- Culture and Activation: Culture the encapsulated T cells in appropriate media, adding soluble activation stimuli such as anti-CD3/CD28 antibodies and IL-2.
- Functional Analysis:
- Microscopy: Visually assess cell clustering and morphology after several days in culture.
- Flow Cytometry: Retrieve cells by mechanically dissociating the hydrogel (especially feasible for NFC) and analyze for viability, activation markers (e.g., CD25), and differentiation (e.g., Treg Foxp3+).
- Functional Assays: Quantify cytokine secretion (e.g., via ELISA) and, for CAR-T cells, perform cytotoxicity assays against target cancer cells.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Hydrogel-Based 3D Culture
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Matrigel / BME | Basement membrane mimic; organoid culture | Animal-derived, undefined composition, rich in ECM proteins and growth factors [45] |
| Nanofibrillar Cellulose (NFC) | Chemically defined 3D T cell culture | Synthetic, mechanically stiff, preserves (CAR-)T cell effector function [45] |
| DECIPHER Scaffold | Decoupling ECM biochemistry and mechanics | Integrates native decellularized ECM with a tunable synthetic PA hydrogel [43] |
| PYP-Crosslinked PEG Hydrogel | Dynamic, photo-tunable stiffness | 8-armed PEG-Mal crosslinked with photoactive yellow protein; reversible rigidity switching with blue light [44] |
| Dextran-MA with Molecular Actuators | Integrin-specific mechanical stimulation | Dextran-based hydrogel with embedded NIR-responsive actuators (CD-PNIPAM-Ligand) for targeted force application [42] |
| MMP-Sensitive Crosslinker (e.g., CGPQGIAGQGCR) | Enables cell-mediated hydrogel degradation | Dicysteine peptide crosslinker that allows cell invasion and matrix remodeling in 3D [42] |
Signaling Pathways and Cellular Response
Mechanical and biochemical cues from hydrogels are converted into biochemical signals inside the cell via mechanotransduction pathways. The following diagram illustrates a key pathway elucidated using dynamic hydrogels, showing how cells sense and respond to rapid changes in matrix rigidity.
Diagram 1: Mechanosignaling Accumulation in Dynamic Environments. Research using photo-tunable hydrogels revealed that while traction forces adapt in real-time to rigidity changes, phosphorylation of signaling proteins like FAK can persist. This accumulation of activated signaling molecules over multiple cycles enhances mechanotransduction beyond levels possible on static substrates [44].
The following diagram outlines the experimental workflow for applying integrin-specific mechanical forces in a 3D hydrogel platform to study cancer cell migration.
Diagram 2: Workflow for Integrin-Specific Mechanical Stimulation. This platform uses NIR-light-responsive actuators embedded in a dextran hydrogel to apply precise forces to specific integrins (e.g., via RGD or RTD ligands), enabling the study of parameters that trigger specific cancer cell migration modes like mesenchymal-to-amoeboid transition [42].
Synthetic and natural hydrogels have evolved from simple support structures into sophisticated, tunable platforms that provide unprecedented control over the cellular microenvironment. By enabling the independent manipulation of what cells "see" (biochemical and architectural cues) and "feel" (static and dynamic mechanical forces), these materials are proving indispensable for unraveling the complex biology of the ECM. The ongoing innovation in hydrogel design—from dynamic and viscoelastic systems to platforms that incorporate native ECM—is providing deeper insights into developmental biology, disease mechanisms, and regenerative medicine. As these technologies mature, they will continue to bridge the gap between traditional in vitro models and in vivo physiology, accelerating the development of more effective and personalized therapies.
The transition from traditional two-dimensional (2D) cell culture to three-dimensional (3D) models represents a paradigm shift in biomedical research, enabling more accurate representation of in vivo conditions. Spheroids and organoids, as self-organizing 3D structures, have emerged as powerful tools that better replicate the complex cellular environments found in living tissues [46]. These advanced models preserve critical aspects of tissue architecture, including cell-cell interactions, nutrient and oxygen gradients, and physiologically relevant cell-ECM dynamics that are absent in conventional 2D systems [47]. The extracellular matrix (ECM) serves not merely as a structural scaffold but as an bioactive environment that provides essential mechanical and biochemical cues guiding cell behavior, differentiation, and morphogenesis [16]. Within the context of 3D cell culture research, understanding how ECM composition, stiffness, and architecture influence the formation and function of spheroids and organoids is fundamental to harnessing their full potential in drug discovery, disease modeling, and regenerative medicine [48] [49]. This technical guide examines the core principles, methodologies, and applications of these self-organizing 3D structures within their matrix environments, providing researchers with comprehensive insights into their implementation and analysis.
Defining Spheroids and Organoids
Core Characteristics and Distinctions
While both spheroids and organoids represent three-dimensional cellular models, they differ significantly in their complexity, origin, and applications. Understanding these distinctions is crucial for selecting the appropriate model for specific research questions.
Table 1: Comparative Analysis of Spheroids and Organoids
| Feature | Spheroids | Organoids |
|---|---|---|
| Complexity | Simple cell clusters | Complex structures with organ-specific cell types |
| Self-organization | Limited | High capacity for self-organization and patterning |
| Cellular Origin | Cell lines or primary cells | Stem cells (pluripotent or adult tissue-specific) |
| ECM Dependence | Scaffold-free or scaffold-based | Typically require ECM support (e.g., Matrigel) |
| Physiological Relevance | Recapitulates some tissue features | Mimics organ microstructure and function |
| Applications | Drug screening, cancer biology, basic research | Disease modeling, personalized medicine, developmental biology |
Spheroids are defined as three-dimensional spherical cell aggregates that form through self-association of cells, typically from established cell lines or primary cells [46]. The process of spheroid formation occurs in three distinct phases: aggregation, compaction, and growth [46]. During aggregation, transmembrane receptors such as integrins facilitate initial cell-cell and cell-ECM adhesion. Compaction follows, where spheroids become more densely packed and assume a spherical shape. Finally, growth involves proliferation, differentiation, and development of internal gradients that mimic in vivo conditions [46].
Organoids represent more sophisticated 3D structures that are generated from stem cells and possess the ability to self-differentiate and exhibit organ-specific properties and functions [46]. These complex structures more closely mirror the organization and function of human organs, making them particularly valuable for studying disease mechanisms and developing personalized medicine approaches [2]. Organoids require specific ECM environments that provide the necessary biochemical and mechanical cues to guide their development and maintain their tissue-specific characteristics [4].
Structural Organization and Microenvironment
The internal architecture of spheroids exhibits distinct zoning patterns driven by diffusion limitations. As spheroids increase in size (>500 μm diameter), they develop gradients of oxygen, nutrients, and waste products, resulting in three concentric layers: an outer proliferating zone, an intermediate senescent layer, and a central necrotic core [46]. This organization mimics the nutrient and oxygen gradients found in solid tumors and other tissues, providing a more physiologically relevant model for drug penetration and efficacy studies compared to 2D cultures [2].
Organoids display more complex spatial arrangements that recapitulate organ-specific tissue organization. For instance, intestinal organoids develop crypt-villus structures, while cerebral organoids form layered cortical regions. This sophisticated patterning emerges from coordinated cell differentiation, migration, and self-organization processes guided by both intrinsic genetic programs and extrinsic ECM-derived signals [50]. The ECM serves as an instructive microenvironment for organoids, providing not only structural support but also critical biochemical and biophysical cues that direct morphogenesis and maintain tissue-specific function [16].
The Extracellular Matrix as an Instructive Microenvironment
ECM Composition and Physical Properties
The extracellular matrix is a highly dynamic, three-dimensional network that provides structural support and regulates key biological processes including cell adhesion, migration, differentiation, and signal transduction [16]. Its composition includes macromolecules such as collagens, glycosaminoglycans, elastin, and proteoglycans, which collectively determine its physical properties and signaling capabilities [16].
Table 2: ECM Physical Properties and Their Biological Significance
| Property | Definition | Biological Impact |
|---|---|---|
| Stiffness | Resistance to deformation | Influences cell proliferation, migration, differentiation, and organoid formation [16] |
| Viscoelasticity | Combination of elastic (energy storage) and viscous (energy dissipation) properties | Affects cell spreading, migration, and tissue assembly dynamics [16] |
| Topology | Spatial arrangement of fibers | Guides cell orientation, migration, and tissue patterning [48] |
| Porosity | Measure of void spaces in the material | Affects nutrient diffusion, cell migration, and network formation [48] |
The mechanical properties of ECM show significant variation across different tissue types and pathological states. For example, normal breast tissue exhibits stiffness values of approximately 0.167 kPa, while breast cancer tumors demonstrate increased stiffness up to 4.04 kPa [16]. Similarly, during pulmonary fibrosis, ECM stiffness increases 5-10 times compared to healthy tissue [16]. These mechanical alterations actively influence disease progression by modulating cellular behaviors through mechanotransduction pathways.
Matrix-Directed Morphogenesis
The ECM plays an instructive role in guiding the formation and patterning of 3D cellular structures. Recent research has elucidated how specific ECM properties direct spheroid and organoid development. Fiber diameter, architecture, and network deformability have been identified as critical parameters regulating spontaneous spheroid formation [48]. Aligned fiber networks of sufficient deformability promote spheroid formation, while larger-diameter crosshatched networks with low deformability can abrogate this process [48].
Mechanical cues from the ECM environment directly influence transcriptional programs and cellular behavior during 3D structure assembly. Transcriptomic analysis of cells forming spheroids on fibrous networks revealed striking changes in cell-cell, cell-matrix, and mechanosensing gene expression profiles concordant with spheroid assembly [48]. This genomic reprogramming highlights the profound influence of matrix mechanical properties on cellular phenotype and tissue morphogenesis.
The development of synthetic ECM-mimicking platforms has enabled precise dissection of these mechanical contributions. Engineered fibrous scaffolds with controlled architecture demonstrate that fiber orientation significantly affects cell behavior, including adhesion, formation of pseudospheroids, and differentiation marker expression under high-density conditions [51]. Random and aligned fibers elicit distinct structural patterns and molecular responses, underscoring the importance of scaffold architecture in guiding 3D cellular organization [51].
Formation Techniques and Methodologies
Scaffold-Based and Scaffold-Free Approaches
The generation of spheroids and organoids employs diverse methodologies that can be broadly categorized into scaffold-based and scaffold-free techniques, each with distinct advantages and applications.
Table 3: Comparison of 3D Culture Formation Techniques
| Method | Principle | Uniformity | Throughput | Applications |
|---|---|---|---|---|
| Hanging Drop | Gravity-mediated aggregation | Relatively uniform, depends on droplet size and cell number | Easily scalable but labor-intensive | Short-term culture, drug screening, easy imaging [47] |
| Low-Attachment Plates | Prevents cell adhesion, promotes aggregation | Forms single, uniformly sized spheroids | Compatible with multi-well formats, suitable for large-scale experiments | Mainly short-term culture, drug screening, tumor modeling [47] |
| Hydrogel Embedding | Cells suspended in ECM-mimicking hydrogels | High, depends on hydrogel consistency | Moderate to high, compatible with automation | Organoid generation, long-term culture, disease modeling [2] |
| Scaffold-Based | Cells cultured on 3D fibrous scaffolds | Variable, depends on scaffold homogeneity | Moderate | Tissue engineering, regenerative medicine, controlled microenvironments [51] |
| Microfluidic Systems | Controlled fluid flow in microchambers | High uniformity | High once established | High-throughput screening, vascularized models, precise gradient control [47] |
Scaffold-free methods include techniques such as hanging drop, low-attachment plates, and liquid overlay systems that rely on gravitational forces and prevented adhesion to facilitate cell aggregation [47]. These approaches are particularly valuable for generating spheroids with minimal external influence, allowing the study of intrinsic self-organization capabilities. The hanging drop technique, one of the simplest methods, produces relatively uniform spheroids based on droplet size and cell number, though variability may arise from manual handling [47].
Scaffold-based methods utilize natural or synthetic materials to provide structural support and biochemical cues that guide 3D organization. Natural ECM materials like Matrigel, derived from the Engelbreth-Holm-Swarm mouse tumour, are widely used for both spheroid and organoid culture [2]. However, Matrigel presents challenges including batch-to-batch variability and potential optical aberrations during imaging [2]. Synthetic hydrogels offer greater control over mechanical properties and composition, enabling tailored microenvironments for specific research applications [2] [49].
Advanced and Emerging Technologies
Recent technological advances have expanded the capabilities for generating and analyzing 3D cellular models. Microfluidic systems enable precise control over the cellular microenvironment, allowing creation of gradient systems and high-throughput screening platforms [47]. These "organ-on-a-chip" technologies facilitate the integration of fluid flow and mechanical forces that more accurately mimic in vivo conditions.
Bioprinting techniques offer unprecedented spatial control over cell placement and ECM composition, enabling creation of complex, multi-cellular tissue architectures with reproducible geometry [47]. This approach allows researchers to design and fabricate 3D tissues with specific organizational patterns that more closely resemble native tissues.
Advanced imaging and analysis methodologies have similarly evolved to address the challenges of 3D culture analysis. Label-free imaging techniques, such as LabelFreeTracker, employ machine learning to visualize nuclei and membranes in bright-field images of 3D organoids, eliminating the need for fluorescent reporter engineering and reducing phototoxicity [50]. These approaches enable long-term, high-resolution imaging of dynamic processes in 3D cultures without artificial labeling.
Experimental Protocols for 3D Model Establishment
Protocol 1: Forming Spheroids Using the Hanging Drop Method
The hanging drop technique remains a widely used approach for generating uniform spheroids, particularly for cancer research and drug screening applications.
Materials:
- Cell suspension of interest (e.g., cancer cell lines, primary cells)
- Standard cell culture medium
- Low-adhesion multi-well plates or glass slides with depression wells
- Pipettes and sterile tips
- Humidified cell culture incubator (37°C, 5% CO₂)
Procedure:
- Prepare a single-cell suspension at appropriate density (typically 1×10⁴ to 5×10⁴ cells/mL, depending on cell type and desired spheroid size).
- Pipette 20-50 μL droplets of cell suspension onto the lid of a multi-well plate or into depression wells.
- Carefully invert the lid and place it over the bottom chamber containing PBS to maintain humidity.
- Incubate for 24-72 hours to allow spheroid formation.
- Monitor aggregation daily using light microscopy.
- Carefully transfer formed spheroids to appropriate culture vessels for experimental applications.
Technical Considerations:
- Optimal cell density must be determined empirically for each cell type.
- Spheroid size increases with higher initial cell density and longer culture duration.
- Maintain strict humidity control to prevent evaporation of droplets.
- This method is ideal for short-term culture (up to 2 weeks) with viability typically >92% [47].
Protocol 2: Generating Organoids in ECM Hydrogels
This protocol describes the generation of complex organoids using ECM hydrogel scaffolds, suitable for stem cell-derived models and long-term culture.
Materials:
- Stem cells (pluripotent or organ-specific adult stem cells)
- ECM hydrogel (e.g., Matrigel, synthetic ECM alternatives)
- Organoid-specific culture medium with appropriate growth factors
- Pre-chilled pipettes and tubes
- 24-well or 48-well cell culture plates
- Water bath set to 4°C
Procedure:
- Keep ECM hydrogel on ice throughout the procedure to prevent premature polymerization.
- Harvest and count cells, centrifuging to obtain a cell pellet.
- Resuspend cell pellet in cold ECM hydrogel at appropriate density (typically 1×10³ to 1×10⁴ cells per 50 μL of hydrogel).
- Plate 20-50 μL droplets of cell-hydrogel mixture into pre-warmed culture plates.
- Incubate plates at 37°C for 20-30 minutes to allow hydrogel polymerization.
- Carefully overlay polymerized hydrogels with organoid culture medium.
- Culture for required duration, changing medium every 2-3 days.
- Monitor organoid development using microscopy.
Technical Considerations:
- ECM hydrogel composition should be optimized for specific organoid types.
- Growth factor combinations in culture medium must support desired differentiation pathways.
- For imaging and analysis, organoids can be released from hydrogel using appropriate recovery solutions.
- This method supports long-term culture (weeks to months) with proper medium optimization.
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for 3D Cell Culture
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| ECM Hydrogels | Matrigel, Collagen I, Fibrin, Synthetic PEG-based hydrogels | Provide 3D scaffold mimicking native extracellular environment [2] |
| Specialized Cultureware | Low-attachment plates, Hanging drop plates, Microfluidic chips | Facilitate cell aggregation and spheroid formation without external scaffolds [47] |
| Synthetic Polymers | Polycaprolactone (PCL) scaffolds, Polystyrene fibers | Create controlled fibrous environments for guided 3D organization [48] [51] |
| Mechanobiology Modulators | ROCK inhibitors (Y-27632), Myosin inhibitors (Blebbistatin) | Probe role of cellular contractility in spheroid/organoid formation [48] |
| Imaging Tools | LabelFreeTracker, Confocal microscopy, High-content screening systems | Enable 3D visualization and analysis of structure and function [50] |
Signaling Pathways in ECM-Guided 3D Organization
The following diagram illustrates key signaling pathways through which ECM properties influence spheroid and organoid formation and function:
ECM sensing and mechanotransduction pathways central to 3D model development. Key mechanosensors including integrins, Piezo1, and TRPV4 channel proteins detect physical ECM properties such as stiffness, fiber alignment, and viscoelasticity [16]. These signals activate downstream pathways including Rho-associated protein kinase (ROCK) and YAP/TAZ signaling, which regulate actomyosin contractility and gene expression programs essential for spheroid and organoid formation [48] [16].
Applications in Disease Modeling and Drug Development
Cancer Research and Personalized Medicine
Spheroids and organoids have transformed cancer research by providing more physiologically relevant models for studying tumor biology and therapeutic responses. Patient-derived organoid (PDO) platforms enable optimization for high-throughput pharmacotyping, allowing evaluation of drug sensitivity in patient-specific models [4]. For instance, pancreatic cancer patient-derived organoids cultured in Corning Matrigel matrix have proven valuable for defining novel therapeutic vulnerabilities and studying mechanisms of chemotherapy resistance [4].
The tumor microenvironment is particularly well-modeled using 3D systems, as they recapitulate critical features such as hypoxia, nutrient gradients, and cell-ECM interactions that influence drug penetration and efficacy. Cancer spheroids have demonstrated utility in studying invasion mechanisms, with research using 3D hydrogel/Matrigel organoid cultures to model tumor invasion processes [4]. These models more accurately predict in vivo drug responses compared to traditional 2D cultures, potentially reducing late-stage drug failure rates.
Cardiovascular and Neuroscience Applications
In cardiovascular research, 3D spheroid models have emerged as valuable tools for studying angiogenesis, modeling the cardiac microenvironment, and advancing drug development [47]. iPSC-derived cardiac spheroids and organoids in 3D culture systems are being used to advance both cardiovascular and space biosciences research [4]. These models better replicate the complex cellular interactions and mechanical forces present in cardiac tissue, providing more predictive platforms for drug toxicity and efficacy testing.
In neuroscience, 3D brain organoids have enabled unprecedented study of human-specific brain development and disease processes. Innovative platforms combining patient-derived brain organoids with AI tools are transforming neurotherapeutic discovery by modeling complex neurological diseases with improved accuracy [4]. These brain organoids faithfully recapitulate disease-relevant cell types, neural circuits, and phenotypes, serving as foundations for high-content screening and functional analysis [4].
Drug Screening and Toxicity Testing
The pharmaceutical industry has increasingly adopted 3D models for early-stage drug discovery and toxicity assessment. Spheroid-based screening platforms provide more predictive data on compound efficacy, penetration, and toxicity, potentially reducing the high attrition rates in drug development [46]. The more physiologically relevant microenvironments in 3D cultures yield drug response profiles that better correlate with in vivo outcomes compared to traditional 2D screens [47].
Advanced screening approaches now combine 3D models with high-content imaging and analysis systems to extract rich quantitative data about drug effects and mechanisms of action. These integrated platforms allow simultaneous assessment of multiple parameters including cell viability, morphology, and specific pathway activation within the context of 3D tissue-like structures [2].
Emerging Technologies and Future Directions
Advanced Imaging and Artificial Intelligence
The integration of advanced imaging technologies with artificial intelligence represents a transformative approach for extracting meaningful information from complex 3D models. Label-free imaging methods, such as LabelFreeTracker, use machine learning to visualize nuclei and membranes in bright-field images of 3D organoids, eliminating the need for fluorescent labeling and reducing phototoxicity [50]. This enables long-term, high-resolution imaging of dynamic processes in 3D cultures.
AI-powered analysis platforms are increasingly being applied to organoid models to identify subtle patterns and phenotypes that might escape conventional analysis. For example, AI-powered human brain organoid platforms are being developed for precision medicine applications, layering AI tools trained on multimodal biological data to enhance mapping of dysregulated pathways and therapeutic target prioritization [4]. These integrated systems create "clinical trials in a dish" that support more predictive and patient-relevant drug testing [4].
Biofabrication and Complex Microenvironment Engineering
Advanced biofabrication techniques including 3D bioprinting and microfluidic systems enable creation of increasingly sophisticated 3D models with precise control over architecture and composition. These technologies allow spatial patterning of multiple cell types and ECM components to better mimic native tissue organization [6]. The development of complex, multi-tissue systems through these approaches promises more comprehensive models for studying organ-level functions and systemic drug effects.
Engineered microenvironmental control extends to mechanical property manipulation, with growing capabilities to dynamically modulate ECM stiffness, viscoelasticity, and topography. These dynamic systems enable researchers to probe the temporal aspects of mechanosensing and their contributions to disease processes and therapeutic responses [16]. Lightweight, portable, and temperature-tolerant ECM hydrogels developed for point-of-care applications demonstrate the potential for translating these technologies to clinical settings [49].
Experimental Workflow for 3D Culture Analysis
The following diagram outlines a comprehensive workflow for establishing and analyzing spheroids and organoids in matrix environments:
A systematic workflow for 3D culture research. The process begins with careful method selection and optimization, considering factors such as scaffold-free versus scaffold-based approaches, cell type and density optimization, and protocol standardization [47] [46]. ECM preparation follows, with selection of appropriate natural or synthetic hydrogels and tuning of mechanical properties to match the physiological context [2] [16]. After 3D culture establishment, careful maintenance and monitoring are essential, particularly for long-term organoid cultures that require specific signaling cues for proper differentiation and maturation [46]. Endpoint analysis incorporates multiple readouts including viability assessment, morphological analysis, molecular and functional assays, and high-content imaging to comprehensively evaluate model performance and experimental outcomes [2] [50].
The extracellular matrix (ECM) is far more than a passive scaffold; it is a dynamic, signaling-active network that critically influences tumor progression, drug resistance, and cellular behavior. Traditional two-dimensional (2D) cell cultures, grown as monolayers on plastic surfaces, fail to recapitulate the three-dimensional (3D) architecture and complex cell-ECM interactions of native tissues. This limitation significantly reduces their predictive value in drug screening, contributing to the high failure rates of oncology drugs in clinical trials. The transition to three-dimensional (3D) cell cultures represents a paradigm shift in preclinical research, enabling the creation of tumor models that more faithfully mimic the tumor microenvironment (TME). These advanced models preserve essential pathophysiological features, including gradients of nutrients and oxygen, the presence of heterogeneous cell populations, and, most importantly, a biologically relevant ECM that governs cell signaling, proliferation, and survival. This article explores how 3D models that accurately incorporate the ECM are revolutionizing oncology drug screening by uncovering therapeutic vulnerabilities that remain invisible in conventional 2D assays.
Why Move to 3D Models? Limitations of Traditional Systems
Conventional drug screening has long relied on monocultures of tumor cells grown flat on a petri dish. While this approach allows for the high-throughput identification of drugs that kill fast-growing cells, it lacks the complexity of the environment that allows tumors to survive and expand within the body [52]. The table below summarizes the critical limitations of 2D cultures in modeling the TME.
Table 1: Key Differences Between 2D and 3D Cell Cultures
| Parameter | 2D Culture | 3D Culture |
|---|---|---|
| Cell Morphology | Flat, stretched | In vivo-like, often spherical |
| Cell Growth | Rapid proliferation; contact inhibition | Slower, more physiologically relevant proliferation |
| Cell Function | Functionally simplified | Closer to in vivo cell function |
| Cell Communication | Limited cell-cell communication | Robust cell-cell and cell-ECM communication |
| Cell Polarity & Differentiation | Lack of polarity; incomplete differentiation | Maintained polarity; normal differentiation [53] |
| Drug Sensitivity | Often overestimated | More clinically predictive, can show resistance [54] |
| ECM Interaction | Minimal or absent | Active, biomechanical, and biochemical signaling [55] |
The biological implications of these differences are profound. In 2D cultures, the lack of a 3D ECM leads to altered gene expression and metabolism, which are critical factors in antitumor drug sensitivity testing [53]. Furthermore, the tumor microenvironment's stroma, primarily composed of cancer-associated fibroblasts (CAFs) that secrete ECM components, creates a protective barrier that keeps chemotherapies and immune cells out [52]. This barrier effect and the associated drug resistance cannot be modeled in a simple 2D system.
3D Model Systems: Architectures for Recapitulating the TME
A variety of 3D culture technologies have been developed to bridge the gap between simple 2D cultures and complex, costly animal models. These systems can be broadly categorized into scaffold-based and scaffold-free approaches, each with distinct advantages for specific applications.
Table 2: Overview of Common 3D Cell Culture Models
| Model Type | Description | Key Advantages | Common Applications |
|---|---|---|---|
| Multicellular Spheroids | Scaffold-free 3D aggregates of cells that self-assemble into spheres. | Simple setup; mimic tumor architecture and nutrient/gradient formation. | High-throughput drug screening, studies of tumor core biology [56]. |
| Organoids | 3D structures derived from stem cells or patient tumor cells that self-organize into organ-like entities. | Retain genetic and phenotypic heterogeneity of the original tumor; can be biobanked. | Personalized medicine, disease modeling, biomarker discovery [54] [53]. |
| Organ-on-a-Chip | Microfluidic devices that culture cells in 3D channels to simulate organ-level physiology and fluid flow. | Incorporates dynamic flow (e.g., interstitial, vascular); allows for real-time monitoring. | Studying metastasis, intravasation, and vascular-tumor interactions [55]. |
| 3D Bioprinting | Use of cell-laden bioinks to fabricate complex, predefined tissue constructs layer-by-layer. | High spatial control over cell and matrix placement; customizable architecture. | Tissue engineering, creating complex multi-tumor interfaces [57] [6]. |
| Microtumors / Organotypic Cultures | Fresh tumor samples sliced and cultured to preserve the original TME's 3D structure and cell heterogeneity. | Preserves native ECM and cellular composition; highly clinically relevant. | Ex vivo drug testing, studying patient-specific tumor-stroma interactions [52]. |
A pivotal consideration for scaffold-based models (including organoids and bioprinting) is the choice of ECM material. These can be derived from natural sources (e.g., collagen, Matrigel) or synthetic polymers, each offering different advantages in terms of biochemical cues, mechanical tunability, and reproducibility [53].
Technical Guide: A Workflow for 3D Drug Screening
Implementing a robust 3D drug screening platform involves a multi-step process, from model establishment to data analysis. The following workflow and detailed methodology are based on successful implementations in recent research.
Figure 1: A generalized workflow for drug screening using 3D models that recapitulate the tumor microenvironment.
Detailed Experimental Protocol: 3D Microtumor Drug Screening
This protocol is adapted from a study that used 3D microtumors to identify novel therapeutic vulnerabilities [52].
1. Model Establishment:
- Source Tissue: Obtain fresh tumor samples from surgical resections or biopsies. Breast and pancreatic cancers are often used due to their dense, fibrous stroma.
- Microtumor Generation: Using a vibratome, slice the fresh tumor tissue into thin (200-500 µm) sections. This preserves the native TME's 3D architecture, including cancer cells, CAFs, immune cells, and the endogenous ECM.
- Culture Conditions: Maintain the microtumor slices in organotypic culture on membrane inserts with appropriate air-liquid interface media. Use a serum-free, defined medium to avoid confounding effects of serum-derived growth factors.
2. Drug Treatment:
- Compound Library: Prepare a library of compounds for screening. For kinase inhibitor studies, a panel of 32+ inhibitors is a common starting point.
- Dosing: Treat microtumors with a range of clinically relevant concentrations of the compounds. Include a DMSO vehicle control.
- Duration: The standard treatment duration is 72-96 hours, but this should be optimized for the specific tumor type and compound mechanism.
3. Endpoint Analysis:
- Viability Assay: Measure cell viability using ATP-based assays (e.g., CellTiter-Glo 3D). Normalize luminescence readings to the vehicle control to calculate percent viability.
- Histology and Imaging: Fix and paraffin-embed a subset of microtumors for H&E staining and immunohistochemistry (IHC) to assess morphology and protein expression (e.g., Ki-67 for proliferation, cleaved caspase-3 for apoptosis).
- Molecular Profiling: For hits of interest, perform RNA sequencing and proteomics on treated vs. control microtumors to identify differentially expressed genes and proteins, particularly those involved in ECM pathways.
4. Validation and Mechanism:
- Co-culture Assays: Validate findings using simplified 3D co-culture models. For example, mix pure tumor cell lines with primary CAFs in a defined 3D matrix (e.g., Matrigel/collagen) and treat with the hit compound to confirm the role of the stroma in the response.
- In Vivo Correlation: Test efficacy in mouse models. For instance, treat mice bearing patient-derived xenografts (PDX) with the identified compound and monitor tumor growth and weight over 2-4 weeks.
- Target Engagement: Use biochemical kinase assays to confirm the compound binds to its intended targets from a panel of hundreds of kinases. Follow up with RNAi knockdown of identified targets (e.g., MAPK12, DDR1/2) to confirm their functional role in the observed phenotype.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for 3D TME Research
| Reagent / Material | Function in 3D Culture | Example Use Case |
|---|---|---|
| Matrigel / Geltrex | A basement membrane extract providing a biologically active scaffold for cell growth and differentiation. | Used as a substrate for cultivating patient-derived organoids and forming tumor spheroids [56] [55]. |
| Collagen I | A major ECM protein that can be polymerized into a tunable 3D hydrogel. | Used to study cell invasion and to create defined 3D microenvironments for co-culture assays [55]. |
| Alvetex & Other Scaffolds | Synthetic, porous polystyrene scaffolds that provide a physical structure for 3D cell growth without animal-derived components. | Used for high-throughput formation and culture of 3D spheroids with high reproducibility [57]. |
| Gibco Geltrex Flex Matrix | A next-generation, recombinant hydrogel designed for consistency and control over mechanical properties. | Showcased for its utility in creating standardized and scalable 3D culture models [57]. |
| Cancer-Associated Fibroblasts (CAFs) | Primary stromal cells that are critical for secreting and remodeling the tumor ECM. | Co-cultured with tumor cells in 3D to model the pro-tumorigenic effects of the stroma and test stromal-targeting drugs [52] [56]. |
Case Study: Uncovering a Shared Vulnerability via the ECM
A landmark study demonstrates the power of this approach. Researchers from the Gujral Lab performed a drug screen comparing 2D tumor cell lines to 3D microtumors derived from breast and pancreatic cancers [52]. Surprisingly, two to three times as many drugs were predicted to be effective in the 3D models than in the 2D culture, highlighting the ability of 3D systems to reveal a broader range of therapeutic vulnerabilities.
A key finding was the drug doramapimod, a p38 MAPK inhibitor whose potential in cancer had been overlooked. In 3D microtumors with dense stroma, doramapimod significantly inhibited growth. Mechanistic investigations revealed that doramapimod does not kill cancer cells or CAFs directly. Instead, it targets the MAPK12 and DDR1/2 kinase pathways in CAFs, which converge on the GLI1 transcription factor. This signaling axis is critical for CAFs to produce and remodel the ECM. By disrupting this process, doramapimod breaks down the tumor's support structure and protective barrier.
Figure 2: Signaling pathway in Cancer-Associated Fibroblasts (CAFs) identified as a vulnerability in 3D microtumor screens. Doramapimod inhibits DDR1/2 and MAPK12, reducing GLI1-driven ECM production.
The most compelling result was that by reducing the ECM barrier with doramapimod, the efficacy of both chemotherapy and immune checkpoint inhibitors was significantly enhanced. The anti-tumor effect of these drug combinations was far greater than any agent alone, presenting a powerful strategy to overcome treatment resistance [52].
The Integrated Future: 3D Models, AI, and Personalized Medicine
The future of oncology drug screening lies in the integration of sophisticated 3D models with advanced computational technologies. Artificial intelligence (AI) and machine learning (ML) are now being deployed to deconvolve the complex signaling networks within the TME. For instance, researchers have integrated 3D screening data into machine learning platforms to computationally predict tumor responses to hundreds of kinase inhibitors, vastly expanding the potential for discovering novel drug combinations and biomarkers [52] [58].
The drive towards personalized medicine is also being accelerated by these technologies. Patient-derived tumor organoids (PDTOs) can be established from individual patients, cryopreserved to create biobanks, and used to test a panel of drugs to identify the most effective therapy for that specific patient's tumor [54] [53]. This approach moves beyond generic treatment guidelines based on tumor type alone.
Furthermore, regulatory shifts and ethical concerns are pushing the adoption of 3D models as alternatives to animal testing. Agencies are increasingly backing microphysiological systems and organoid-based testing as more human-relevant and reliable tools for drug development [57] [54]. As these technologies mature—through advancements in 3D bioprinting, organ-on-a-chip systems, and AI-driven analysis—their integration into every stage of the drug discovery pipeline will become the standard, ultimately leading to the faster development of safer and more effective therapies for cancer patients.
The extracellular matrix (ECM) is no longer considered a passive structural scaffold in biological systems. Rather, it is a dynamic, information-rich network that actively regulates cell behavior, fate, and drug response. Within the context of 3D cell culture research, recapitulating the native ECM has emerged as a critical frontier for creating physiologically relevant models. Patient-Derived Scaffolds (PDS) represent a groundbreaking advancement in this field, enabling the direct use of a patient's own tissue-specific ECM as a culture platform. This technical guide explores how PDS technology leverages the unique biochemical and biophysical properties of the native tumor ECM to drive innovations in personalized medicine, offering a more predictive platform for therapeutic testing and disease modeling.
By preserving the patient-specific ECM composition, topology, and stiffness, PDS create a physiologically relevant context that profoundly influences cancer cell behavior, drug sensitivity, and disease progression pathways in a way that synthetic matrices cannot fully replicate [3] [59]. This approach marks a significant departure from conventional 3D culture matrices, such as Matrigel, by maintaining the unique tumor microenvironment (TME) that varies between individuals and cancer types.
The Scientific Rationale for Patient-Derived Scaffolds
Limitations of Conventional 3D Culture Matrices
Traditional 3D culture systems rely on matrices of animal or synthetic origin. While valuable, these systems present significant limitations for personalized medicine applications:
- Batch-to-Batch Variability: Matrices like Matrigel, derived from mouse sarcoma, exhibit considerable variation between lots, compromising experimental reproducibility and clinical translation [59].
- Limited Tunability: Conventional matrices offer limited control over specific biochemical and mechanical properties, restricting their ability to mimic diverse human tissue environments [59].
- Simplified Composition: They lack the complex, tissue-specific composition and architecture of human ECM, which is shaped by the unique pathophysiology of a patient's disease [3] [60].
The Unique Advantages of Patient-Derived Scaffolds
PDS technology addresses these limitations by using decellularized human tissues that preserve the native ECM structure and composition. The decellularization process removes cellular components while preserving key ECM components, creating a scaffold that retains patient-specific disease signatures [3]. The biochemical and architectural cues embedded within the tumor ECM play an active role in driving aggressive disease behavior. Research demonstrates that breast cancer cells cultured on tumor PDS significantly overexpress genes associated with invasiveness (CAV1, CXCR4, CNN3, MYB, TGFB1) and secrete higher levels of pro-metastatic cytokines like IL-6 compared to those cultured on normal PDS [3]. This demonstrates that the tumor ECM actively promotes malignant phenotypes, making it a critical component for accurate drug response modeling.
Table 1: Key Characteristics of Patient-Derived Scaffolds Versus Conventional Matrices
| Characteristic | Patient-Derived Scaffolds (PDS) | Conventional Matrices (e.g., Matrigel) |
|---|---|---|
| Origin | Human patient tissue | Mouse sarcoma or synthetic sources |
| Composition | Patient-specific ECM with native complexity | Limited, defined components |
| Reproducibility | High patient-to-patient variability, but structurally consistent per sample | Batch-to-batch variability |
| Tunability | Fixed, reflects native state | Adjustable but limited |
| Clinical Relevance | High, preserves disease-specific ECM alterations | Moderate, generic cancer environment |
| Key Applications | Personalized drug testing, disease modeling, tumor ECM biology | General drug screening, basic biology |
Technical Methodology: Generating and Utilizing PDS
Tissue Decellularization and PDS Preparation
The generation of biologically active PDS requires a meticulous decellularization protocol that removes all cellular material while maximizing the preservation of native ECM structure and composition.
Experimental Protocol: SDS-Based Decellularization for PDS Creation [3]
- Tissue Acquisition: Obtain surgically resected tumor and matched normal tissue biopsies from patients. Fresh tissues should be processed immediately or stored using standardized cryopreservation methods.
- Tissue Processing: Mince tissues into small, uniform fragments (approximately 1-2 mm³) to increase surface area for decellularization.
- Decellularization Process: Incubate tissue fragments in a solution of Sodium Dodecyl Sulfate (SDS), a ionic detergent that lyses cells and solubilizes nuclear and cytoplasmic components. The concentration and duration are optimized to balance complete cell removal with ECM preservation.
- Washing and Sterilization: Thoroughly rinse the decellularized scaffolds in phosphate-buffered saline (PBS) to remove all detergent residues. Subsequently, sterilize the PDS using methods like peracetic acid treatment or antibiotic washes to ensure aseptic culture conditions.
- Quality Control Verification:
- Histology: Perform Hematoxylin and Eosin (H&E) staining to confirm the absence of cell nuclei.
- DNA Quantification: Measure DNA content to verify a significant reduction (e.g., from 527.1 ng/µL in native tissue to 7.9 ng/µL post-decellularization) [3].
- ECM Composition Analysis: Use staining techniques (e.g., Trichrome for collagen, Alcian Blue for glycosaminoglycans) and immunohistochemistry (e.g., for collagen IV, vimentin) to confirm the preservation of key ECM components.
- Mechanical Testing: Assess the Young's modulus via tensile testing to quantify scaffold stiffness, a critical mechanical property.
3D Cell Culture on PDS
Once validated, PDS serve as the biological substrate for establishing patient-specific 3D cultures.
Experimental Protocol: 3D Culture Setup for Drug Testing [61]
- Cell Seeding: Revive and expand cryopreserved primary tumor cell suspensions from the same patient. Seed these cells onto the pre-hydrated PDS in a defined geometry (e.g., single-point seeding) that promotes consistent cell distribution and spheroid formation.
- Culture Optimization: Screen different growth media to select the formulation that best supports cell viability and heterogeneity. For instance, Endothelial Cell Growth Medium 2 (ECM-2), sometimes supplemented with conditioned medium from Cancer-Associated Fibroblasts (CAFs), has been used to generate invasive aggregates in head and neck cancer models [61].
- Culture Maintenance: Maintain cultures for a period sufficient for the cells to proliferate and establish complex structures (typically 1-3 weeks), with medium changes performed regularly.
- Morphological Quantification: Analyze the developing tumoroids using imaging. A perimeter-based complexity index can be used to quantitatively assess morphology, where higher complexity often correlates with a more invasive phenotype [61].
Diagram 1: A workflow for creating and using Patient-Derived Scaffolds (PDS), from tissue acquisition to personalized drug testing.
Key Applications and Experimental Findings
Modeling the Tumor Microenvironment and Drug Response
PDS technology excels in creating clinically predictive models for oncology research. A seminal study in head and neck cancer (HNC) demonstrated that PDS co-cultured with cancer-associated fibroblasts (CAFs) generated tumoroids with invasive morphology and deposited endogenous matrix, effectively preserving tumor-stroma crosstalk [61]. This model was used for drug sensitivity testing, where tumoroids from different patients showed variable responses to cisplatin and a Notch pathway inhibitor (FLI-06), underscoring the platform's utility for personalized treatment selection [61].
Similarly, research on breast cancer PDS revealed that the tumor ECM itself drives aggressive behavior. MCF-7 breast cancer cells cultured on tumor PDS displayed significantly higher viability and proliferation over 15 days compared to those on normal PDS. Crucially, these cells also overexpressed a panel of hub genes (CAV1, CXCR4, CNN3, MYB, TGFB1) linked to invasiveness and secreted significantly more IL-6 (122.91 vs. 30.23 pg/10⁶ cells), a cytokine linked to poor prognosis [3]. This indicates that the tumor ECM actively instructs cells toward a more aggressive phenotype, which in turn modulates therapeutic response.
Quantitative Data from PDS Studies
Table 2: Experimental Outcomes from Select PDS Studies in Cancer Research
| Study Model | Key ECM Findings in Tumor vs. Normal PDS | Cell Behavior & Drug Response Outcomes |
|---|---|---|
| Breast Cancer [3] | - Collagen: 507.35 vs. 186.94 µg/mg- Glycosaminoglycans: 3.07 vs. 1.62 µg/mg- Significantly higher stiffness (Young's modulus) | - Viability & proliferation: Significantly higher on tumor PDS- IL-6 secretion: 122.91 vs. 30.23 pg/10⁶ cells- Upregulation of invasiveness genes (CAV1, CXCR4, TGFB1) |
| Head and Neck Cancer [61] | Preservation of native ECM architecture post-decellularization enabling CAF-supported culture. | - Generated invasive tumor aggregates with high complexity index.- Patient-specific drug responses: Two of three patient models were cisplatin-sensitive; all showed growth inhibition with FLI-06 Notch inhibitor. |
Essential Reagents and Research Tools
Implementing a PDS workflow requires a combination of specialized biological materials, reagents, and analytical tools. The following toolkit outlines the core components.
Table 3: The Scientist's Toolkit for PDS Research
| Category / Item | Specific Examples | Function in PDS Workflow |
|---|---|---|
| Tissue Processing | Surgical biopsy specimens, collagenase, dispase | Source of patient-specific ECM and cells; enzymatic dissociation of tissues. |
| Decellularization | Sodium Dodecyl Sulfate (SDS), Peracetic acid, Antibiotics | Removes cellular material; sterilizes the resulting scaffold. |
| Cell Culture | Primary tumor cells, Cancer-Associated Fibroblasts (CAFs), Endothelial Cell Growth Medium 2 (ECM-2) | Patient-derived cellular components; optimized media for maintaining complex cultures. |
| Matrix Supports | Matrigel (for comparative studies), Collagen I hydrogels | Conventional matrices used for protocol optimization and comparative analysis [62] [61]. |
| Analysis & QC | DNA quantification kits, H&E staining, Antibodies (Collagen IV, Vimentin) | Verifies decellularization efficiency and characterizes preserved ECM components. |
| Functional Assays | WST-8 cell viability assay, Cytokine ELISA kits (e.g., IL-6), qPCR systems | Assesses cell viability, proliferation, secretome, and gene expression in response to therapies. |
Signaling Pathways and Mechanotransduction in PDS
The ability of PDS to accurately guide cell behavior hinges on its preservation of native cell-ECM interactions. These interactions trigger critical signaling pathways that control fate decisions in tumor cells. Integrins on the cell surface bind to ECM ligands (e.g., collagen, laminin) in the PDS, initiating intracellular signaling cascades. A key pathway involves Focal Adhesion Kinase (FAK), which influences gene expression and can promote cell survival, proliferation, and migration [60] [59].
Furthermore, the mechanical properties of the PDS, such as its stiffness, are sensed by cells via mechanotransduction pathways. This can lead to the activation of the TGF-β1 pathway, a known regulator of invasion and metastasis. The diagram below illustrates how a tumor-specific PDS orchestrates these signals to drive an aggressive phenotype, including the secretion of cytokines like IL-6 and the upregulation of genes associated with cell motility and invasion [3] [59].
Diagram 2: Key signaling pathways activated by tumor-specific Patient-Derived Scaffolds (PDS), leading to an aggressive cell phenotype.
Patient-Derived Scaffolds represent a significant leap forward in the quest for physiologically relevant in vitro models. By faithfully preserving the unique biochemical and biophysical signature of a patient's native tissue ECM, PDS offer an unparalleled platform for personalized drug testing and the study of tumor-stroma interactions. The technology directly addresses the critical role of the ECM in disease progression and therapy resistance, a component largely missing from traditional models.
Future developments in this field will likely focus on enhancing reproducibility and scalability. The integration of engineered and synthetic matrices with defined compositions is a promising approach to overcome the natural variability of PDS while still capturing key aspects of human tissue mechanics and biochemistry [59]. Furthermore, combining PDS with advanced microfluidic systems and AI-driven analysis will enable higher-throughput screening and more sophisticated computational modeling of patient-specific responses [6] [1]. As these technologies mature, PDS are poised to become an indispensable tool in the translational pipeline, accelerating the development of effective, personalized therapies and strengthening the bridge between benchtop research and clinical application.
Navigating the Third Dimension: Challenges and Optimization in ECM-Based Models
In the field of 3D cell culture research, the extracellular matrix (ECM) is recognized not merely as a structural scaffold but as a dynamic, instructive microenvironment that regulates essential cell behaviors including differentiation, migration, and proliferation through mechanotransduction [7]. The biological functionality of native ECM in directing cell fate has driven the development of decellularized ECM (dECM) as a superior biological scaffold for tissue engineering and regenerative medicine. Decellularization involves the removal of cellular components from native tissues while aiming to preserve the intricate architecture and bioactivity of the underlying ECM [63] [64]. The fundamental challenge lies in navigating the inherent tension between efficient cell removal and maximal ECM preservation. Aggressive decellularization agents that effectively eliminate immunogenic cellular material often concurrently damage the structural and functional ECM components that provide mechanical support and biochemical cues [64] [65]. This technical guide examines the core principles, evaluates current protocols, and presents standardized methodologies to achieve this critical balance, thereby enabling the creation of highly bioactive dECM scaffolds that faithfully mimic the native cellular microenvironment for advanced 3D research models.
Core Principles of the Decellularization Process
The Goal: Defining Effective Decellularization
An effective decellularization protocol is quantified by specific, measurable outcomes. The widely accepted standards, as established by Crapo et al., require: (1) absence of visible nuclear material in histological stains (e.g., H&E, DAPI), (2) residual DNA content below 50 ng per mg of dry tissue weight, and (3) DNA fragment lengths less than 200 bp [65]. Beyond cell removal, success is equally defined by the preservation of key ECM components, including collagens, glycosaminoglycans (GAGs), elastin, laminin, and fibronectin, which maintain the matrix's mechanical integrity and bioactivity [66] [64]. The ultimate benchmark for a dECM scaffold is its biocompatibility and ability to support cell attachment, proliferation, and differentiation upon recellularization, confirming the retention of a functional microenvironment [63].
The Central Challenge: Agent-Driven Trade-offs
The decellularization process inherently involves trade-offs, as the mechanisms that disrupt and remove cells also risk damaging the ECM.
- Ionic Detergents: Sodium dodecyl sulfate (SDS) is highly effective at lysing cells and solubilizing DNA but is a denaturing agent that can disrupt protein-protein interactions, leading to collagen denaturation and loss of GAGs, which ultimately compromises ECM structure and mechanics [63] [64].
- Non-Ionic Detergents: Triton X-100 is less denaturing and better preserves ECM structure and growth factors but is less effective at complete cell removal and can wash out essential ECM components like GAGs and lipids [63].
- Enzymatic Agents: Trypsin cleaves peptide bonds and is effective for cell dissociation but can excessively degrade key ECM proteins like laminin and fibronectin if overused [64] [65].
Achieving balance requires careful optimization of reagent concentration, exposure time, and sequential application to maximize efficacy while minimizing collateral damage to the ECM.
Quantitative Analysis of Decellularization Outcomes
Table 1: Quantitative Evaluation of Decellularization Efficacy Across Different Protocols
| Tissue Source | Protocol Description | Residual DNA (ng/mg tissue) | Key Preserved ECM Components | Collagen Retention | GAG Retention | Reference |
|---|---|---|---|---|---|---|
| Human Umbilical Cord | Trypsin/EDTA + Triton X-100 + Sodium Deoxycholate | Not specified (Most cells eliminated) | Collagen, GAGs | Preserved (confirmed by staining) | Preserved (confirmed by staining) | [66] |
| Canine Myocardium | 1% SDS for 5 days + 1% Triton X-100 for 48 hrs | Not specified | Collagen, Essential ECM elements | Preserved architecture | Not specified | [67] |
| Human Myocardium | 1% SDS for 7 days + 1% Triton X-100 for 48 hrs | Not specified | Collagen, Essential ECM elements | Preserved architecture | Not specified | [67] |
| Rat Tibialis Anterior Muscle | Multi-step protocols (P1-P4) involving Triton, SDS, Trypsin, SDC | Quantitative data via spectrophotometry | Laminin, Collagen I | Varies by protocol | Varies by protocol | [65] |
| Human Facial Graft | 1% SDS for 216 hrs + 1% Triton X-100 for 48 hrs (Immersion) | Quantitative data via Nanodrop | Collagen, GAGs, Elastin, Growth Factors | Preserved (quantified) | Preserved (quantified) | [68] |
| Breast Tissue (PDS) | SDS-based decellularization | 7.9 ng/μL (from 527.1 in native) | Collagen, GAGs, Collagen IV, Vimentin | 469.59 μg/mg (Tumor) | 2.99 μg/mg (Tumor) | [3] |
Table 2: Impact of Decellularization on Mechanical and Functional Properties
| Tissue Source | Protocol | Mechanical Property Assessment | Key Functional Outcomes | Reference |
|---|---|---|---|---|
| Breast Tissue (Tumor PDS) | SDS-based | Young's modulus: Significantly higher in tumor vs. normal PDS | Tumor PDS enhanced cancer cell viability, proliferation, and aggressive gene expression vs. normal PDS | [3] |
| Human Facial Graft | 1% SDS + Triton X-100 (Immersion) | Mechanical strength not altered after decellularization | Scaffold allowed cell engraftment, biocompatible in vitro and in vivo | [68] |
| Canine Myocardium | Protocol II (1% SDS 5 days + Triton 48 hrs) | Not specified | Preservation of architecture and components with reduced reagent exposure | [67] |
Detailed Experimental Methodologies
A Representative Optimized Protocol: Human Umbilical Cord Decellularization
The following protocol from [66] demonstrates an effective combination strategy for a complex tissue.
- Tissue Preparation: Human umbilical cord tissue is sliced longitudinally into thin sections (5 cm × 2 cm × 0.5 cm). The sections are rinsed in ultrapure water on a shaking bed three times for 10 minutes each.
- Decellularization Steps:
- Treatment: Immersion in a solution of 0.025% w/v Trypsin-EDTA at 37°C for 1.5 hours with agitation at 120 rpm.
- Treatment: Transfer to a solution of 5% v/v Triton X-100 for 1.5 hours at 120 rpm.
- Treatment: Final immersion in 4% w/v Sodium Deoxycholate (SD) for 2 hours at 120 rpm.
- Washing and Storage: The tissue is subsequently washed thoroughly with deionized water to eliminate any residual reagents. The decellularized matrix is then dehydrated via freeze-drying for 48 hours.
This protocol, completed in a short 5-hour timeframe, successfully removed most cellular components while preserving collagen and GAGs, as confirmed by histology and biochemical assays [66].
Comparative Protocol Analysis: Canine Myocardium Decellularization
A study comparing four protocols for canine heart tissue [67] highlights the impact of reagent exposure time.
- Protocol II (Optimal): Immersion in 1% SDS for 5 days, followed by washing in distilled water overnight, and then treatment with 1% Triton X-100 for 48 hours. This protocol achieved excellent cell removal and ECM preservation.
- Protocol I (Less Optimal): Extended exposure to 1% SDS for 7 days, followed by the same Triton X-100 step. While effective, the longer SDS duration posed a greater risk to ECM integrity.
- Protocols III & IV (Suboptimal): These protocols incorporated an initial Trypsin step and freezing, which resulted in ECM retraction and the removal of essential matrix elements.
The findings underscore that reduced exposure time to harsh detergents like SDS, even when achieving similar cell removal, is critical for preserving ECM quality [67].
Workflow for Developing and Evaluating a Decellularization Protocol
The following diagram visualizes the key decision points and evaluation feedback loop essential for developing an optimized decellularization protocol.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Reagents for Decellularization and Their Functions
| Reagent Category | Specific Examples | Primary Function | Key Considerations for ECM Preservation |
|---|---|---|---|
| Ionic Detergents | Sodium Dodecyl Sulfate (SDS) | Powerful solubilization of cell membranes and nuclear material; highly effective for cell removal. | Can denature proteins, damage collagen ultrastructure, and remove GAGs; concentration and time must be tightly controlled. [63] [64] |
| Non-Ionic Detergents | Triton X-100 | Disrupts lipid-lipid and lipid-protein bonds; milder, helps preserve native protein structure. | Less effective at removing cellular material from dense tissues; can wash out GAGs and lipids. [63] [64] |
| Enzymatic Agents | Trypsin/EDTA | Cleaves peptide bonds for cell dissociation and removal; effective for breaking cell-ECM attachments. | Can degrade desirable ECM proteins (e.g., laminin, fibronectin) if not carefully limited. [64] [65] |
| Zwitterionic Detergents | CHAPS, Sulfobetaine | Possesses properties of both ionic and non-ionic detergents; can offer a balance of efficacy and preservation. | Generally milder, leading to better ECM structural maintenance but potentially incomplete cytoplasmic removal. [63] |
| Chelating Agents | EDTA, EGTA | Binds divalent cations to disrupt cell adhesion to the ECM. | Typically used in combination with other agents (e.g., Trypsin) to enhance efficacy. [63] |
| Nucleases | DNase, RNase | Degrades residual nucleic acid fragments post-cell lysis to reduce immunogenic potential. | Used in final stages to eliminate residual DNA/RNA without damaging ECM structure. [63] [65] |
The pursuit of balancing complete cell removal with optimal ECM preservation is a cornerstone of producing biologically functional scaffolds for 3D cell culture and regenerative medicine. As evidenced by the comparative data, there is no universal protocol; success depends on a methodical, tissue-specific approach that considers the unique structural and compositional properties of the source material [67] [65]. The future of decellularization lies in the continued refinement of multi-step, combinatorial protocols that leverage the strengths of individual agents while mitigating their weaknesses, such as using short, potent ionic detergent treatments followed by extensive washing and neutralizing steps [66] [68]. Standardizing quantitative assessment metrics—including residual DNA, GAG/collagen content, and mechanical properties—across the research community is critical for direct comparison and protocol optimization. By mastering this balancing act, scientists can reliably generate bioinstructive dECM scaffolds that faithfully recapitulate the native tissue microenvironment, thereby advancing the development of more physiologically relevant 3D in vitro models, personalized disease models, and effective regenerative therapies.
The extracellular matrix (ECM) is far more than a passive scaffold; it is a dynamic, instructive environment that regulates essential cell behaviors including differentiation, migration, and proliferation through mechanotransduction—the process by which cells convert mechanical cues from their microenvironment into biochemical signaling [69]. In three-dimensional (3D) cell culture, the mechanical properties of the surrounding hydrogel, particularly its stiffness and porosity, are critical determinants of cellular phenotype and function. These parameters influence diverse processes from stem cell differentiation and organoid development to the efficacy of cell-based immunotherapies [45] [70]. Consequently, fine-tuning these properties is not merely a technical exercise but a fundamental requirement for creating physiologically relevant models that can bridge the gap between conventional 2D cultures and complex in vivo environments. This guide provides a detailed framework for researchers aiming to precisely control hydrogel stiffness and porosity to mimic native tissue environments for advanced research and drug development applications.
Quantifying Hydrogel Mechanical Properties
To replicate physiological conditions, one must first be able to accurately measure the key mechanical properties of hydrogels. The following table summarizes the core properties, their physiological significance, and standard measurement techniques.
Table 1: Key Hydrogel Properties and Their Measurement
| Property | Definition | Physiological Significance | Measurement Techniques |
|---|---|---|---|
| Stiffness (Elastic Modulus, E) | Resistance to deformation under an applied force; often reported as shear modulus (G) or elastic modulus (E), with E ~ 3G for many hydrogels [71]. | Regulates cell fate, differentiation, and migration; aberrant stiffness is linked to disease states like fibrosis and cancer [69] [70]. | Atomic Force Microscopy (AFM) for 2D films; Bulk compression/tensile testing or indentation for 3D gels [71]. |
| Viscoelasticity | Combination of solid-like (elastic) and liquid-like (viscous) behavior, enabling time-dependent stress relaxation [69]. | Influences cell spreading, migration, and mechanosensing; native tissues are viscoelastic [69]. | Oscillatory rheology to measure storage modulus (G') and loss modulus (G") [45] [71]. |
| Swelling Ratio (Qm, Qv) | The amount of water or buffer absorbed by the hydrogel at equilibrium [71]. | Indicator of crosslinking density; affects nutrient flux and can create osmotic pressure on embedded cells. | Calculated from wet weight (Mw) and dry weight (Md) as Qm = Mw/Md [71]. |
| Mesh Size (ξ) | The average distance between crosslinks, defining the molecular porosity of the network [71]. | Controls diffusion of nutrients, oxygen, and biomolecules; typically smaller than 20 nm, requiring degradation for cell migration [40]. | Fluorescence Recovery After Photobleaching (FRAP), diffusion assays, or theoretical calculation [71]. |
The selection of a measurement technique depends on the hydrogel format (2D film vs. 3D bulk) and the property of interest. Rheology, for instance, is indispensable for characterizing gelation kinetics and viscoelasticity. As shown in foundational studies, the storage modulus of common hydrogels like Matrigel, Basement Membrane Extract (BME), and nanofibrillar cellulose (NFC) can range from 3 to 40 Pa, values comparable to soft tissues [45]. Furthermore, rheological amplitude sweeps can reveal how a material behaves under strain—whether it strain-stiffens like Matrigel and BME or becomes more fluid-like like NFC, which is crucial for understanding how cells will mechanically remodel their environment [45].
Strategies for Tuning Hydrogel Stiffness and Porosity
Achieving physiological relevance requires independent control over mechanical and structural properties. The table below outlines key design parameters and their effects.
Table 2: Strategies for Tuning Hydrogel Properties
| Design Parameter | Effect on Stiffness | Effect on Porosity/Mesh Size | Common Hydrogel Systems |
|---|---|---|---|
| Polymer Concentration | Increases with higher polymer concentration [71]. | Decreases mesh size with higher concentration [71]. | Nearly all systems (Collagen, Alginate, PEG). |
| Crosslinking Density | Increases with higher crosslinking density [71]. | Decreases mesh size with higher crosslinking density [71]. | Covalently crosslinked systems (PEG-diacrylate, GelMA). |
| Molecular Weight of Polymer | Variable effect, depends on system. | Higher molecular weight can lead to larger mesh sizes. | Alginate, PEG, HA. |
| Crosslink Type (Ionic vs. Covalent) | Ionic crosslinks (e.g., Ca2+ in alginate) often yield softer, more dynamic gels [72]. | Mesh size is system-dependent. | Ionic: Alginate. Covalent: PEG, GelMA. |
Material-Specific Tuning Approaches
- Natural Polymers (e.g., Collagen, Matrigel): These materials are derived from biological sources and offer innate bioactivity but often suffer from batch-to-batch variability and limited tunability. Stiffness is primarily controlled by concentration. For example, collagen gel stiffness can be adjusted by varying the acid-soluble collagen concentration before neutralization and polymerization [71]. However, as research reveals, natural matrices like Matrigel and BME contain undefined growth factors (e.g., TGF-β) that can profoundly influence cell behavior, such as driving CD4+ T cells toward a regulatory phenotype, independent of mechanical properties [45].
- Synthetic Polymers (e.g., Polyethylene Glycol - PEG): Synthetic hydrogels provide excellent control over mechanical properties and chemical definition. Stiffness and porosity are precisely tuned by varying the molecular weight of the PEG chains and the concentration or functionality of the crosslinker. This allows for the creation of highly reproducible networks devoid of confounding biological signals [71] [72].
- Functionalized Hybrids (e.g., GelMA, HA-MA): Methacrylated derivatives of natural polymers like gelatin (GelMA) or hyaluronic acid (HA-MA) combine the bioactivity of natural materials with the tunability of synthetic systems. Stiffness is powerfully controlled by the concentration of the polymer and the photoinitiator, as well as the UV light exposure time and intensity [72]. This enables the fabrication of stable, mechanically defined hydrogels that can support cell adhesion and degradation.
Experimental Protocols for Hydrogel Characterization and Cell Culture
Protocol: Oscillatory Rheology for Mechanical Characterization
This protocol is essential for quantifying hydrogel stiffness (storage modulus G') and viscoelasticity [45] [71].
- Instrument Setup: Use a rheometer with a parallel plate geometry. Set the temperature control to mimic the gelation process (e.g., a ramp from 4°C to 37°C for thermosensitive gels like collagen or Matrigel).
- Loading: Pipette the pre-gel solution onto the bottom plate and lower the top plate to a defined gap (e.g., 500 μm), trimming excess material.
- Gelation Kinetics: Perform a time/temperature sweep experiment at a fixed strain and frequency (e.g., 1% strain, 1 Hz) to monitor the evolution of G' and G" over time as the hydrogel forms.
- Frequency Sweep: Once the hydrogel is formed (G' > G" and stable), perform a frequency sweep (e.g., 0.1 to 10 Hz) at a constant strain within the linear viscoelastic region to observe the time-dependent behavior.
- Amplitude Sweep: Perform an amplitude sweep (e.g., 0.1% to 100% strain) at a fixed frequency to determine the yield point where the gel structure breaks down.
Protocol: 3D Cell Encapsulation and Functional Assessment
This general protocol can be adapted for evaluating (CAR-)T cell function, as in the cited study [45].
- Hydrogel Precursor Preparation:
- For NFC hydrogel: Suspend NFC in culture medium to the desired concentration. As a synthetic material, it can be handled at room temperature [45].
- For Matrigel/BME: Thaw the matrix on ice and keep all reagents and tips chilled to prevent premature gelation.
- Cell Mixing: Centrifuge the cell suspension (e.g., CD4+ T cells or CAR-T cells) and gently resuspend the pellet in the appropriate, cytocompatible hydrogel precursor solution. Ensure uniform distribution of cells. For photopolymerizing gels like GelMA, add a cytocompatible photoinitiator (e.g., I2959 or LAP) [71].
- Hydrogel Formation:
- NFC/Chemically crosslinked gels: Pipette the cell-polymer mixture into the desired mold (e.g., a 96-well plate). Gelation for NFC occurs rapidly upon cessation of shearing [45].
- Matrigel/BME: Pipette the cell-matrix mixture into the mold and transfer to a 37°C incubator for 15-30 minutes to trigger thermal gelation.
- GelMA: Pipette the mixture into the mold and expose to UV light (e.g., 365 nm, 5-10 mW/cm²) for a specified duration (e.g., 30-60 seconds) to crosslink.
- Culture and Analysis: After gelation, add culture medium on top of the hydrogels. Culture for the desired period (e.g., 5 days [45]).
- Viability/Phenotype: At endpoint, dissociate hydrogels using appropriate methods (e.g., enzymatic degradation with collagenase for collagen gels, or mechanical disruption for NFC [45]) and analyze retrieved cells by flow cytometry for viability (e.g., using a LIVE/DEAD stain) and phenotype markers (e.g., Foxp3/GFP for Treg cells [45]).
- Proliferation: Use dyes such as CFSE or CellTrace Violet to track cell division via flow cytometry.
- Function: Quantify cytokine secretion (e.g., IFN-γ, IL-2) in the supernatant by ELISA and assess cytotoxicity in co-culture assays with target cells.
The diagram below illustrates the mechanotransduction pathways through which the engineered hydrogel properties influence cell behavior in 3D culture.
Mechanotransduction Pathways in 3D Hydrogels
The Scientist's Toolkit: Essential Reagents and Materials
Selecting the appropriate materials is critical for successful experimental outcomes. The following table catalogs key reagents and their functions in designing 3D cultures.
Table 3: Research Reagent Solutions for 3D Hydrogel Culture
| Material/Reagent | Function and Key Characteristics | Example Applications |
|---|---|---|
| Matrigel / BME | Basement membrane extract from murine sarcoma; contains ECM proteins (laminin, collagen IV) and growth factors. Chemically undefined and variable [45]. | Organoid culture, tumor spheroid models, angiogenesis assays. |
| Nanofibrillar Cellulose (NFC) | Synthetic, chemically defined hydrogel. Mechanically stiffer than Matrigel/BME, allows room-temperature handling, and preserves (CAR-)T cell effector function [45]. | Preclinical testing of immunotherapies, 3D models requiring defined conditions. |
| Gelatin Methacryloyl (GelMA) | Methacrylated gelatin derivative; contains cell-adhesive RGD sequences and is enzymatically degradable. Stiffness is tunable via UV crosslinking [72]. | Tissue engineering, bioprinting, cell migration studies. |
| Alginate | Natural polysaccharide from brown algae; forms hydrogels via ionic crosslinking (e.g., with CaCl₂). Lacks cell adhesion sites unless modified [72]. | Cell encapsulation, drug delivery, cartilage tissue engineering. |
| Polyethylene Glycol (PEG) | Synthetic, bioinert polymer; highly tunable mechanics via chemical crosslinking. Requires functionalization with adhesion peptides (e.g., RGD) [71] [72]. | Reductionist studies of mechanotransduction, controlled drug release. |
| Decellularized ECM (dECM) | Hydrogel derived from decellularized tissues (e.g., lung, liver); retains tissue-specific biochemical composition [73]. | Disease modeling (e.g., fibrotic lung), studies of cell-ECM interactions in a native context. |
The experimental workflow for developing and validating a 3D hydrogel model is summarized below.
Hydrogel Model Development Workflow
The precise fine-tuning of hydrogel stiffness and porosity is a cornerstone of modern 3D cell culture, enabling researchers to create engineered tissues with high physiological relevance. By applying the principles and protocols outlined in this guide—from rigorous material characterization and informed selection of hydrogel systems to the implementation of robust cell-based assays—scientists can better replicate the in vivo mechanical milieu. This approach is already yielding more predictive models, as evidenced by studies showing that a chemically defined NFC hydrogel maintains CAR-T cell function where traditional matrices suppress it [45]. As the field advances, the integration of dynamic, viscoelastic materials and sophisticated fabrication techniques will further enhance our ability to deconstruct and mimic the complex mechanobiology of the extracellular matrix, ultimately accelerating discovery in basic research and therapeutic development.
Within the broader context of extracellular matrix (ECM) research in three-dimensional (3D) cell culture, the transition to high-throughput screening (HTS) presents distinct challenges that hinder its widespread adoption in drug discovery and development. Traditional two-dimensional (2D) cultures have long served as the standard for pharmaceutical testing due to their simplicity and cost-effectiveness, but they lack the physiological relevance required for accurate prediction of human responses [32]. The integration of ECM components into 3D culture systems—including scaffold-based hydrogels, decellularized tissue matrices, and complex organoid models—creates a more biologically relevant microenvironment that better mimics in vivo conditions. However, this increased physiological relevance comes with significant technical hurdles in standardization and scalability that must be overcome for effective implementation in HTS pipelines. This technical guide examines these critical challenges and presents current methodological solutions for researchers aiming to incorporate ECM-rich 3D models into high-throughput screening workflows.
Key Standardization Challenges in ECM-Based 3D Models
Reproducibility and Protocol Variability
The lack of standardized protocols for ECM-based 3D cultures presents a fundamental barrier to reproducible HTS outcomes. Unlike traditional 2D cell culture methods, which follow well-established procedures, 3D cell culture techniques vary significantly based on the type of model used, including scaffold-based, spheroid, and organoid cultures [74]. This variability leads to inconsistencies in experimental outcomes, making it difficult for researchers and industries to replicate results across different laboratories. The problem is particularly pronounced with natural ECM materials like Matrigel or decellularized tissues, which exhibit inherent batch-to-batch variability in their composition and mechanical properties.
A primary concern is the diffusional limitations and gradient formations of nutrients, gases, reagents, dyes, and antibody solutions within 3D constructs, which can lead to inaccurate results and problems with imaging [32]. This variability directly impacts the reliability of high-content screening readouts, as signal intensity may reflect diffusion efficiency rather than true biological activity. Furthermore, the difficulty in extracting cells from different biomaterial-based 3D constructs using classic dissociation techniques introduces additional variability in endpoint analyses that require single-cell suspensions [32].
Quantification and Analytical Hurdles
Accurate quantification of cellular responses within ECM-rich 3D environments presents distinctive challenges not encountered in 2D systems. The most basic of parameters—cell number—is notoriously difficult to measure precisely in 3D cultures, yet essential for normalizing data across different experimental conditions [32]. Traditional cell counting methods rely on obtaining a single-cell suspension, which is challenging with many 3D models due to the protective nature of the ECM and strong cell-cell interactions.
Advanced quantification methods have emerged to address these challenges. For instance, a novel approach combining in-situ fluorescent staining of accumulated decellularized ECM proteins with automated high-content microscopy enables quantitative assessment of ECM accumulation and organization [75]. This method demonstrated good agreement with established radiolabelled amino acid incorporation assays when testing TGFβ1 as a pro-fibrotic stimulus, while also providing valuable information about matrix fibrillar organization [75]. Similarly, fluorescently labeled collagen-binding probes have been successfully implemented to quantify total collagen content in high-throughput screens for compounds enhancing collagenous ECM production [76].
Table 1: Quantitative Comparison of ECM Detection Methods for HTS
| Method | Throughput | Sensitivity | Information Gained | Limitations |
|---|---|---|---|---|
| Radiolabelled amino acid incorporation [75] | Low | High | Quantitative matrix accumulation | Radioactive handling, no structural data |
| Immunofluorescence of specific ECM proteins [75] | Medium | Medium | Protein-specific localization and quantification | Antibody-dependent, limited multiplexing |
| Fluorescent total protein stain [75] | High | High | Total ECM protein content and organization | Non-specific protein detection |
| Collagen-binding fluorescent probes [76] | High | Medium | Specific collagen content | Limited to collagenous ECM |
Scalability Limitations and Technical Solutions
Platform Compatibility and Automation
The integration of ECM-based 3D models with automated liquid handling systems presents significant technical hurdles. Many natural ECM materials, particularly hydrogels like Matrigel or collagen, exhibit variable viscosity and gelation properties that complicate robotic dispensing. Furthermore, the structural complexity of decellularized tissue matrices can clog dispensing nozzles and create inconsistencies in scaffold distribution across wells.
Recent advancements in platform technologies show promise for overcoming these limitations. The development of a pulmonary three-dimensional (3D) floating ECM model utilizing a 384-pillar/well platform successfully addressed issues related to the aggregation and sedimentation of nanoparticles and their possible optical interference with toxicity assays [77]. This system demonstrated variable toxicities of silica nanoparticles that depended on their behavior under different conditions, unlike conventional 2D models which showed high toxicity regardless of media composition [77]. Similarly, tissue ECM arrays featuring spotted tissue matrix particles as two-dimensional arrays or incorporated with cells to generate three-dimensional cell-matrix microtissue arrays enable high-throughput screening of biological responses to tissue-specific scaffold microenvironments [78].
For organoid cultures, microfluidic systems have emerged as particularly valuable platforms. The Akura Twin microplate featuring 168 interconnected well pairs enables scalable modeling of liver fibrosis by seeding HepaRG microtissues with hepatic stellate cell (hTERT-HSC) microtissues in separate but connected compartments [79]. This platform facilitates the study of fibrosis progression through key events of the adverse outcome pathway (AOP) in a format compatible with high-throughput screening.
Imaging and Analysis Complexities
The 3D architecture of ECM-embedded cultures creates substantial challenges for high-content imaging and analysis. Light scattering and absorption within dense ECM materials reduces image quality and resolution, while the increased z-dimension requires more sophisticated imaging modalities such as confocal microscopy or light sheet fluorescence microscopy [80]. These techniques often involve longer acquisition times and generate massive datasets that strain storage capacities and computational resources.
Advanced computational approaches are being developed to address these limitations. Deep learning-based recognition systems enable automated evaluation of tumor spheroid behavior in 3D culture, dramatically improving analysis throughput and consistency [80]. Similarly, machine learning algorithms can extract multiparametric data from high-content images of 3D cultures, identifying subtle patterns in ECM organization and cell-matrix interactions that would be imperceptible through manual analysis [75].
Table 2: Market Analysis of 3D Cell Culture Technologies (2025-2035)
| Parameter | Scaffold-Based 3D Culture | Organoid Platforms | Microfluidic Systems |
|---|---|---|---|
| Market Share (2025) | 80.4% [74] | Not specified | Growing segment |
| Projected CAGR | 9.8% (overall market) [74] | Not specified | Not specified |
| Primary Applications | Cancer research, regenerative medicine [74] | Disease modeling, personalized medicine [74] | Toxicity testing, disease modeling [81] |
| Key Advantages | Reproducibility, scalability, commercial availability [74] | Physiological relevance, patient-specific modeling [74] | Dynamic flow, mechanical cues [81] |
| Standardization Challenges | Batch-to-batch variability, matrix composition control [74] | Protocol variability, structural heterogeneity [74] | System complexity, operational standardization [81] |
Experimental Protocols for ECM-Based HTS
High-Throughput ECM Quantification Assay
The following protocol adapts the methodology described by Le et al. (2015) for quantitative screening of compounds affecting collagenous ECM production [76]:
Workflow Overview:
Step-by-Step Methodology:
- Cell Seeding: Plate ATDC5 cells (or relevant cell type) in 384-well plates at optimized density (e.g., 5,000 cells/well) in appropriate growth medium.
- Compound Treatment: Add compounds from screening library (e.g., LOPAC1280) using automated liquid handling systems. Include controls: negative control (vehicle alone) and positive control (e.g., insulin for ATDC5 cells).
- Culture Period: Maintain cultures for 7-14 days with medium changes every 2-3 days to allow significant ECM accumulation.
- Decellularization:
- Remove culture medium and wash with PBS.
- Incubate with 20mM ammonium hydroxide solution for 10 minutes at room temperature.
- Wash thoroughly with PBS to remove cellular debris.
- Fluorescent Staining:
- Incubate with fluorescently labeled collagen-binding probe (1:1000 dilution in PBS) for 1 hour at room temperature.
- Wash with PBS to remove unbound probe.
- High-Content Imaging: Image plates using automated high-content microscope with appropriate filters. Acquire multiple fields per well to ensure representative sampling.
- Automated Quantification: Analyze images using integrated intensity measurement algorithms. Normalize data to positive controls.
Validation: This assay demonstrated Z-factor >0.5, indicating excellent suitability for HTS. The method identified tetradecylthioacetic acid (TTA) as a potent enhancer of collagenous ECM production in ATDC5 cells, with synergistic effects when combined with insulin [76].
Tissue ECM Array Fabrication
Based on the methodology described by Pouliot et al. (2015) [78]:
Workflow Overview:
Detailed Protocol:
- Tissue Processing:
- Harvest porcine tissues (spleen, intestine, bladder, bone, brain, cartilage, heart, kidney, liver, lung, adipose).
- Chemically treat tissues using combination of acid, detergent, and DNAse to remove cellular components while preserving ECM structure.
- Lyophilize processed tissues and mechanically fragment using cryomill to create tissue ECM microparticles.
Array Fabrication:
- Spot tissue ECM particles (3-mm diameter) on acrylamide-coated glass slides.
- Include a layer of purified soluble type I collagen to promote homogeneous particle binding.
- Distribute replicate spots of each tissue type evenly across the array to control for positional effects.
Cell Seeding and Culture:
- Seed cells uniformly using a confined flow device to limit seeding variability (approximately 13% coefficient of variation per row and column).
- Culture cells for predetermined time based on experimental endpoint (typically 7-14 days).
3D Microtissue Formation (Optional):
- For 3D models, create hanging droplet arrays containing 10,000-20,000 cells and ECM particles (0-10 ng/cell).
- Allow spontaneous cell-matrix assembly over 2-6 days to form compact spheroids.
This platform enables high-throughput morphological, histological, and immunohistochemical analyses of cell-ECM interactions across multiple tissue types simultaneously [78].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for ECM-Based HTS
| Category | Specific Products/Platforms | Key Applications | Technical Considerations |
|---|---|---|---|
| Scaffold Materials | Natural hydrogels (Matrigel, collagen), Synthetic hydrogels (PEG-based), Decellularized tissue matrices [78] [32] | 3D cell culture, tissue-specific microenvironment modeling | Batch variability (natural), tunability (synthetic), complexity (decellularized) |
| Specialized Platforms | 384-pillar/well plates [77], Akura Twin microplates [79], Microfluidic organ-on-chip devices [81] | High-throughput toxicity screening, disease modeling, mechanistic studies | Compatibility with automation, imaging capabilities, throughput capacity |
| Detection Reagents | Fluorescent collagen-binding probes [76], SYPRO Ruby/Flamingo fluorescent stains [75], Antibodies against specific ECM components [75] | ECM quantification, matrix organization analysis, specific protein detection | Penetration efficiency in 3D, signal-to-noise ratio, specificity |
| Analysis Tools | Deep learning-based recognition algorithms [80], High-content imaging systems, Automated image analysis pipelines [80] [75] | Quantitative assessment of 3D cultures, multiparametric analysis | Computational requirements, validation needs, standardization challenges |
Emerging Solutions and Future Perspectives
Technological Innovations Addressing Standardization
The field is rapidly evolving with new technologies specifically designed to overcome standardization challenges in ECM-based HTS. Microfluidics and organ-on-chip technologies are revolutionizing 3D cell culture by enabling the creation of lab-on-chip devices that simulate dynamic physiological conditions [74]. These systems integrate precisely controlled fluidic environments, allowing continuous nutrient supply, waste removal, and mechanical stimuli, closely mimicking in vivo conditions while improving reproducibility.
Similarly, the integration of 3D bioprinting with cell culture is emerging as a transformative trend, enabling the fabrication of complex, physiologically relevant tissue models with precise spatial arrangement of cells, biomaterials, and growth factors [74]. This approach enhances reproducibility by controlling the initial distribution of ECM components and cellular constituents, reducing the heterogeneity that plagues self-assembled 3D models.
Methodological Advances for Enhanced Scalability
Methodological innovations are progressively addressing the scalability limitations of ECM-based 3D models. Automated, interconnected multi-tissue platforms now enable the cultivation of several organ models simultaneously within a single fluidic system, facilitating the assessment of complex organ-organ interactions in a scalable format [81]. These systems maintain tissue-specific ECM environments while allowing coordinated analysis.
Advances in label-free imaging techniques and artificial intelligence-driven image analysis are overcoming the analytical bottlenecks associated with 3D HTS. These approaches enable quantitative assessment of ECM remodeling and cell-matrix interactions without extensive sample processing, thereby maintaining sample integrity for subsequent analyses and increasing throughput [80] [75].
The continued maturation of these technological and methodological approaches promises to gradually overcome the current limitations in standardization and scalability, ultimately enabling the full integration of physiologically relevant ECM-based 3D models into mainstream drug discovery and development pipelines.
The extracellular matrix (ECM) is not merely a structural scaffold but a dynamic, bioactive environment that profoundly influences cellular behavior. In the context of three-dimensional (3D) cell culture, the ECM provides critical biochemical and mechanical cues that regulate cell differentiation, proliferation, survival, and migration—processes that are central to both developmental biology and disease pathology, particularly cancer research [82] [3]. Traditional two-dimensional (2D) cultures fail to recapitulate the complex cell-ECM interactions found in vivo, leading to poor predictive accuracy in drug discovery and a limited understanding of fundamental biology [82] [83].
The shift towards 3D models, especially spheroids and organoids, is therefore a pivotal advancement. These models bridge the gap between simple 2D cultures and complex, costly animal models, offering a more physiologically relevant microenvironment [82]. This guide focuses on innovative, cost-effective methods for spheroid formation, framing them within the essential context of ECM biology. We will explore how these methods not only reduce costs but also enhance the biological fidelity of 3D models by more accurately mimicking the native ECM.
The Scientific and Economic Rationale for Advanced Spheroid Models
Limitations of Traditional 2D Culture
Traditional 2D cell cultures, while simple and inexpensive, present significant limitations. They cannot mimic the original in vivo tumor architecture and provide limited cell–cell and cell–matrix interactions [82]. Cells grown in 2D exhibit altered morphology, polarity, and gene expression profiles, which lead to:
- Overestimation of drug efficacy [83].
- Poor prediction of drug penetration and metabolic responses [82] [83].
- Lack of key tissue features such as hypoxia gradients, nutrient diffusion limitations, and cellular heterogeneity [84].
Advantages of 3D Spheroid Models
3D spheroid models replicate the structural and functional characteristics of in vivo solid tumors more effectively. By incorporating both cell–cell and cell–matrix interactions, they provide a powerful platform for studying the tumor microenvironment (TME) [82]. Spheroids develop distinct spatial organization:
- An outer layer of highly proliferative cells.
- An intermediate layer containing quiescent, less metabolic cells.
- An inner core, characterized by hypoxic and acidic conditions that can lead to necrosis [82] [84].
This cellular heterogeneity creates critical gradients of nutrients, oxygen, and signaling molecules, making spheroids an invaluable tool for studying tumor progression and drug resistance [82] [84].
Market Growth and the Drive for Cost-Effectiveness
The global organoids and spheroids market, valued at USD 1.5 billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of 20.3% [85]. This growth is driven by the increasing demand for physiologically relevant models that reduce reliance on animal testing and improve predictive accuracy in drug development. However, the high cost of specialized reagents and equipment can be a barrier to adoption [85]. This underscores the need for the innovative and cost-effective methodologies detailed in this guide, which make robust 3D models more accessible without compromising quality.
A Toolkit for Spheroid Research: Key Reagents and Materials
The following table summarizes essential materials used in the cost-effective spheroid formation methods discussed in this guide.
Table 1: Key Research Reagent Solutions for Spheroid Formation
| Item | Function in Spheroid Formation | Application Examples |
|---|---|---|
| Agarose | Creates a non-adhesive surface to promote cell aggregation and prevent attachment to the substrate. | Used in the liquid overlay technique [84] and the SpheroidSync method [86]. |
| Dispase | An enzyme that cleaves cell-ECM junctions, enabling the detachment of intact cell sheets for subsequent spheroid formation. | Central to the facile method for generating large quantities of spheroids [87]. |
| Ultra-Low Attachment (ULA) Plates | Surface-treated plates that inhibit cell attachment, forcing cells to aggregate and form spheroids in a scaffold-free manner. | Widely used for matrix-independent spheroid culture and patient-derived spheroids [82]. |
| Methylcellulose | Increases the viscosity of the medium in hanging drop cultures, enhancing droplet stability and preventing evaporation. | Used in the traditional hanging drop method to improve spheroid formation [86]. |
| Orbital Shaker | Provides shear flow that assists in the curling of cell sheets and the formation of spherical aggregates in liquid suspension. | Used in the dispase-mediated spheroid formation method [87]. |
Detailed Experimental Protocols for Cost-Effective Spheroid Formation
The SpheroidSync Method: Integrating Hanging Drop and Transfer
The SpheroidSync (SS) method is an innovative, low-cost approach that combines the hanging drop technique with a unique transfer step to produce highly uniform MCF-7 breast cancer spheroids without the need for special growth factors or supplements [86].
Table 2: Quantitative Outcomes of the SpheroidSync Method
| Parameter | Result from SpheroidSync Method | Significance |
|---|---|---|
| Viability | Sustained intracellular esterase activity over extended culture periods; superior structural integrity vs. conventional methods. | Indicates robust, healthy spheroids suitable for long-term studies [86]. |
| Stemness Markers | CD44: >40-fold increase; ALDH1: >3-fold increase; HIF-1α: >11-fold increase vs. 2D cultures. | Establishes a hypoxic core and enriches for cancer stem cells (CSCs), mimicking in vivo tumor properties [86]. |
| Cost | Very low cost, achieved by avoiding specialized growth factors and using standard lab equipment. | Enhances accessibility for high-throughput screening applications [86]. |
Detailed Protocol:
- Cell Culture: Maintain MCF-7 cells in RPMI 1640 medium supplemented with 5-10% fetal calf serum at 37°C and 5% CO₂ [86].
- Hanging Drop Preparation: Using sampler tips, place 58 µL droplets on the lid of a Petri dish. Each droplet should contain between 1,500 and 15,000 cells. Invert the lid and place it over a PBS-filled bottom dish to prevent evaporation. Culture for 24-72 hours [86].
- Innovative Transfer: Instead of pipetting, which can disrupt the formed cell sheets, the SpheroidSync method uses cut sampler tips to gently transfer the entire cell sheet from the hanging drop. This preserves its integrity [86].
- Spheroid Maturation: Transfer the cell sheets onto a non-adhesive agarose-coated surface. The sheets will self-assemble into uniform, spherical spheroids without needing viscosity-increasing agents like methylcellulose. This step effectively addresses nutrient diffusion and hypoxia, promoting a viable, stem-cell-enriched spheroid [86].
Diagram 1: The SpheroidSync workflow.
Dispase-Mediated Cell Sheet Curling for Mass Production
This facile method enables the generation of tumor spheroids in large quantities with controllable size and high uniformity, using simple Petri-dish culturing and orbital shaking [87].
Detailed Protocol:
- Sparse Seeding: Sparsely seed HCT-116 cells (or other lines like HeLa, A431) onto tissue-culture treated Petri dishes at a low density. This ensures individual cells have sufficient space to grow into separate cellular islets [87].
- Cell Sheet Growth: Culture the cells for 6-13 days, allowing them to form separated cell sheets. The size of the final spheroid can be controlled by tuning the initial cell seeding density and the duration of this growth phase [87].
- Dispase Detachment: Treat the cultures with the enzyme dispase, which specifically cleaves cell-ECM junctions without disrupting cell-cell connections. This allows the detachment of intact cell sheets while maintaining their structural integrity [87].
- Orbital Shaking for Spheroid Formation: Transfer the detached cell sheets into media doped with dispase. Place the suspension on an orbital shaker. The shear flow from shaking, combined with the inhibition of re-attachment by dispase, causes the cell sheets to curl at the edges and eventually form spherical spheroids within 24-72 hours [87].
- Size Uniformization: To achieve high uniformity, sieve the resulting spheroids through a set of home-made stainless steel meshes or commercial sieves with specific mesh sizes (e.g., 300–400 µm) to narrow the size distribution [87].
Table 3: Size Control in the Dispase-Mediated Method
| Factor | Effect on Spheroid Size | Experimental Example |
|---|---|---|
| Cell Sheet Growth Time | Longer growth time results in larger cell sheets and, consequently, larger spheroids. | Spheroid diameter increased from ~150 µm (7-day growth) to ~250 µm (13-day growth) [87]. |
| Initial Seeding Density | Lower initial cell density leads to the formation of larger individual spheroids. | Spheroids from a density of 1x10⁴ cells/dish were significantly larger than those from 4x10⁴ cells/dish [87]. |
| Shaking Duration | Extended shaking in dispase-doped media allows the curling process to complete, forming compact spheroids. | Spheroids formed spherical shapes within 72 hours of shaking [87]. |
Diagram 2: Mass production via cell sheet curling.
The Hanging Drop Method and Its Modern Iterations
The hanging drop method is a classic, scaffold-free technique for producing uniform spheroids. While it can be labor-intensive for large quantities, it remains a fundamental and cost-effective approach for many labs, forming the basis for innovations like SpheroidSync [86] [87].
Detailed Protocol:
- Droplet Preparation: Create droplets of a cell suspension (typically 20-50 µL) on the inner surface of a Petri dish lid. The number of cells per droplet determines the initial spheroid size [86] [87].
- Inversion and Incubation: Carefully invert the lid and place it over a bottom dish containing PBS or medium to maintain humidity and prevent droplet evaporation.
- Spheroid Formation: Incubate the setup for 2-5 days. Gravity causes the cells to settle at the bottom of the droplet, where they aggregate and form a single spheroid.
- Harvesting: Carefully harvest the formed spheroids by pipetting. The use of additives like methylcellulose can increase medium viscosity and improve droplet stability during this process [86].
The Central Role of the Extracellular Matrix in Spheroid Biology
The ECM's role extends far beyond passive structural support. It is a dynamic entity that engages in active mechanotransduction, relaying biochemical and mechanical signals to cells that influence their behavior [3]. In cancer, the tumor ECM undergoes significant remodeling, becoming stiffer and altering its composition of proteins like collagen and glycosaminoglycans [82] [3].
Research using Patient-Derived Scaffolds (PDS) has vividly demonstrated this effect. When breast cancer cells (MCF-7) were cultured on decellularized tumor ECM versus normal ECM, the tumor PDS led to significantly higher cell viability, proliferation, and secretion of IL-6 (122.91 vs. 30.23 pg/10⁶ cells). Critically, the tumor PDS induced the overexpression of genes associated with an aggressive phenotype (CAV1, CXCR4, CNN3), which did not occur on normal PDS [3]. This proves that the tumor-specific ECM actively promotes cancer progression.
In scaffold-free spheroid models, cells deposit their own de novo ECM, generating intricate cell-to-cell and cell-to-matrix interactions in a cell line- and culture-dependent manner [82]. This self-assembled ECM is crucial for establishing the spheroid's internal structure, including the gradients that drive the formation of proliferating, quiescent, and necrotic zones.
Diagram 3: ECM-driven aggressive phenotype.
The adoption of cost-effective spheroid formation methods, such as SpheroidSync and dispase-mediated mass production, represents a significant stride toward making physiologically relevant 3D models more accessible. These methods successfully lower the barrier to entry by reducing reliance on expensive specialized reagents and equipment, all while maintaining or even enhancing the biological fidelity of the spheroids produced.
The future of 3D cell culture lies in the integration of these robust, cost-effective models with advanced technologies. The growing integration of AI-powered image analysis and digital platforms is accelerating organoid-based diagnostics and data analysis [85] [6]. Furthermore, the expansion of patient-derived organoid and spheroid biobanks will provide genetically diverse models for large-scale research and personalized therapy screening [82] [85]. As these trends converge, the tiered approach of using 2D for initial screening, 3D spheroids for predictive modeling, and patient-derived organoids for personalization will become the standard in advanced labs, ultimately improving the success rate of drug development and deepening our understanding of disease biology.
The extracellular matrix (ECM) is not merely a passive scaffold; it is a dynamic, instructive environment that regulates essential cell behaviors including differentiation, migration, and proliferation through mechanotransduction [7]. In the context of three-dimensional (3D) cell culture, the role of the ECM becomes paramount, as cells interact with the matrix in all three dimensions, a context native to most cells in vivo [7]. However, a significant limitation of traditional 3D models is their lack of a perfusion system, which constrains their size, scalability, and physiological relevance. The diffusion limit of oxygen—typically between 100 and 200 µm—means that without a vascular network, the core of larger tissue constructs becomes hypoxic and necrotic, failing to recapitulate the intricate dynamics of living tissue [88] [89].
Integrating vascular networks within 3D cell cultures is therefore a critical step towards building models that can accurately mimic in vivo conditions for drug discovery and disease modeling. Vascularization ensures the sufficient supply of oxygen and nutrients to cells, enables the removal of metabolic wastes, and establishes the concentration gradients and endothelial barriers that are fundamental to tissue function and drug response [88]. When combined with co-culture systems that incorporate multiple cell types, vascularized 3D models can simulate the complex cell-cell and cell-ECM interactions that define human physiology and pathology. This guide details the strategies and methodologies for achieving this integration, firmly framed within the context of ECM biology.
Vascularization Strategies and Their ECM Interactions
Several advanced techniques have been developed to introduce vascular networks into 3D cell cultures. These strategies can be broadly categorized, each with a distinct relationship with the ECM.
Table 1: Comparison of Vascularization Strategies in 3D Cell Culture
| Strategy | Core Principle | Key Advantages | Limitations / Challenges | Role of/Impact on ECM |
|---|---|---|---|---|
| Scaffold-Based Strategies | Using porous biomaterials to support cell growth and guide tissue formation. | High reproducibility; amenable to high-throughput screening; provides mechanical and biochemical support [90]. | Simplified architecture; potential batch-to-batch variability (natural scaffolds) [90]. | The scaffold itself acts as a synthetic ECM, whose stiffness, porosity, and ligand density directly influence cell fate [91]. |
| Bioprinting-Based Strategies | Additive manufacturing of cells and biomaterials to create predefined structures. | Custom-made, complex architectures; ability to create physical and chemical gradients; high-throughput production potential [88] [90]. | Challenges with vascular maturation; lack of vasculature in final construct is common; technical complexity [88] [90]. | Allows precise spatial patterning of ECM-like bio-inks and living cells to recreate in vivo ECM organization. |
| Microfluidic-Assisted Systems | Using microfabricated channels to perfuse media and house endothelial cells. | In vivo-like architecture and microenvironment; dynamic flow conditions; creation of chemical and physical gradients [88] [90]. | Can be difficult to adapt to high-throughput screening; often lacks full, biological vascular integration [90]. | Dynamic flow conditions directly modulate ECM deposition and remodeling by cells, and shear stress activates crucial endothelial cell pathways [88]. |
| Sacrificial Printing | 3D printing of a sacrificial material that is later removed to leave behind a patent channel. | Creates intricate, perfusable microvascular networks within large-volume scaffolds [89]. | The periphery of channels can be composed of bulk hydrogels that hinder cell migration [89]. | The technique is defined by its interaction with the ECM-mimetic hydrogel, which must be stable enough to hold the channel yet permissive for cell invasion. |
Scaffold Internal Perfusable Network Printing (SINP)
A novel printing technique, Scaffold Internal Perfusable Vascular Network Printing (SINP), exemplifies the convergence of several strategies. This method uses crosslinkable Gelatin Methacrylate (GelMA) microspheres as a suspension bath, into which sacrificial ink is printed to create vascular patterns [89]. The process and its benefits are outlined below.
The SINP Experimental Workflow:
- Preparation of GelMA Microspheres: GelMA hydrogel microspheres are prepared using a co-flow microfluidic method. A 10% (w/v) GelMA solution is used as the aqueous phase, and mineral oil containing 2% Span80 serves as the oil phase. The formed droplets are cryogenically crosslinked into microspheres, which are then collected via centrifugation and washing [89].
- Suspension Bath and Printing: The physical crosslinked GelMA microspheres are packed into a printing reservoir to serve as a support bath. A sacrificial ink, such as Pluronic F127, is then printed into this bath to form the desired vascular network pattern [89].
- Photocrosslinking and Sacrificial Removal: The entire construct is exposed to UV light (with a photoinitiator) to permanently photocrosslink the GelMA microspheres into a cohesive, porous scaffold. Following this, the scaffold is immersed in a cell culture medium at 37°C to liquefy and remove the sacrificial ink, leaving behind hollow, perfusable channels [89].
- Cell Seeding and Culture: The lumen of the channels can be seeded with Human Umbilical Vein Endothelial Cells (HUVECs) to form an endothelial lining. The porous scaffold itself can be infiltrated with other tissue-specific cells, such as adipogenic-induced Adipose-Derived Stem Cells (ADSCs), to create a complex, vascularized tissue model [89].
Key Advantages of SINP: This technique offers three significant benefits: (1) the microsphere-based scaffold has high porosity, facilitating excellent nutrient diffusion and cell migration; (2) the sacrificial printing enables the creation of complex, perfusable vascular networks; and (3) the use of GelMA provides a biocompatible, bioactive ECM environment that supports cell adhesion and function [89].
Diagram 1: SINP fabrication workflow for vascularized constructs.
Experimental Protocols for Vascularized Co-culture Models
This section provides a detailed methodology for establishing a vascularized adipose tissue model using the SINP technique, adaptable for other tissue types.
Protocol: Creating a Vascularized Adipose Tissue Model via SINP
Objective: To fabricate a 3D vascularized adipose tissue construct by co-culturing HUVECs and pre-differentiated ADSCs within a GelMA microsphere scaffold featuring perfusable channels.
Materials:
- Cells: Human Umbilical Vein Endothelial Cells (HUVECs), Adipose-Derived Stem Cells (ADSCs).
- Reagents: GelMA (e.g., SunP Biotech, 55-65% degree of substitution), Photoinitiator (e.g., Irgacure 2959), Pluronic F127, Adipogenic induction medium, Endothelial cell growth medium (EGM-2), Span80, Mineral oil.
- Equipment: Co-flow microfluidic device (32G + 21G coaxial needle), 3D bioprinter equipped with a temperature-controlled printhead and UV light source (365-405 nm).
Methodology:
- GelMA Microsphere Fabrication:
- Prepare a 10% (w/v) GelMA solution in a sterile environment.
- Using a co-flow microfluidic device, inject the GelMA solution as the aqueous phase and mineral oil with 2% Span80 as the oil phase.
- Collect the formed droplets and cool the outflow to induce physical crosslinking into microspheres.
- Centrifuge the collected outflow to pellet the microspheres and wash thoroughly with PBS to remove residual oil [89].
Scaffold Fabrication with Sacrificial Vascular Network:
- Pack the prepared GelMA microspheres into a printing chamber to create a support bath.
- Load a sacrificial ink (e.g., 30% Pluronic F127) into a printing cartridge.
- Print the desired vascular network pattern into the GelMA microsphere bath.
- Expose the entire construct to UV light (e.g., 5-10 mW/cm² for 30-60 seconds) to photocrosslink the GelMA microspheres into a solid scaffold.
- Transfer the scaffold to a cell culture incubator (37°C) and perfuse with warm culture medium to liquefy and flush out the sacrificial ink, leaving behind hollow channels [89].
Cell Seeding and Co-culture:
- Endothelialization: Introduce a suspension of HUVECs (e.g., 5-10 million cells/mL) into the lumen of the channels and allow them to adhere under static conditions for a few hours. Subsequently, connect the construct to a perfusion system and culture with EGM-2 medium for 5-7 days to form a confluent endothelium.
- Tissue Cell Incorporation: Prior to scaffold fabrication, pre-differentiate ADSCs into adipogenic lineage using a commercial adipogenic induction medium for 7-14 days. Alternatively, mix the pre-differentiated ADSCs with the GelMA microspheres before packing the bath, or seed them into the porous scaffold after its formation.
- Co-culture Maintenance: Maintain the co-culture in a mixed medium suitable for both cell types, or under perfused conditions that provide endothelial-specific factors and adipocyte maintenance factors.
Key Assays for Validation:
- Vascular Network Assessment: Immunofluorescence staining for CD31/PECAM-1 to visualize endothelial cell junctions and confirm a continuous lumen.
- Adipogenic Differentiation: Oil Red O staining to visualize intracellular lipid droplets.
- Functionality: Permeability assays (e.g., FITC-dextran diffusion) to assess the barrier function of the engineered endothelium.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Vascularized 3D Co-culture
| Item | Function in Experiment | Specific Example(s) |
|---|---|---|
| Basement Membrane Extract | Mimics the epithelial/endothelial basement membrane; rich in ECM proteins and growth factors. | Matrigel [92] |
| Fibrillar Collagen | Provides a natural, fibrillar 3D ECM that supports cell adhesion, migration, and angiogenesis. | Type-I Collagen (Col-1) gels [7] [92] |
| Synthetic Hydrogels | Offers a defined, tunable ECM environment with controllable stiffness, degradability, and bioactivity. | Polyethylene Glycol (PEG), GelMA [91] [89] |
| Sacrificial Bioink | A temporary material used to print channels that are later removed to create perfusable vasculature. | Pluronic F127 [89] |
| Vascular Growth Media | Provides specific factors (e.g., VEGF) necessary for endothelial cell survival, proliferation, and tube formation. | Endothelial Cell Growth Medium (EGM-2) [88] |
| Magnetic Bioprinting Reagents | Enables scaffold-free spheroid and organoid formation via magnetic levitation for high-throughput assembly. | NanoShuttle-PL [93] |
The integration of co-cultures and vascularization strategies within 3D models represents the forefront of in vitro tissue engineering. By deliberately designing the ECM component—whether through the choice of natural hydrogels, the synthesis of tunable synthetic polymers, or the architectural innovation of microsphere scaffolds—researchers can now create models that more faithfully capture the complexity of native tissues. These advanced systems are poised to significantly improve the predictive power of preclinical drug screening, potentially reversing the decades-long decline in drug approval rates by providing more human-relevant efficacy and toxicity data [88].
Future developments will likely focus on standardizing these complex protocols, achieving even greater biological fidelity in the vascular networks (e.g., incorporating pericytes and smooth muscle cells), and scaling the technologies for high-throughput applications. As our understanding of cell-ECM mechanotransduction in 3D deepens [7], so too will our ability to engineer functional tissues that blur the line between in vitro model and living tissue.
Proof in Performance: Validating 3D ECM Models Against 2D and In Vivo Data
The transition from traditional two-dimensional (2D) monolayer cultures to three-dimensional (3D) models incorporating extracellular matrix (ECM) components represents a paradigm shift in preclinical drug development. While 2D cultures have served as a workhorse for decades due to their simplicity and cost-effectiveness, they fundamentally lack the physiological context that governs drug behavior in vivo [83]. The ECM, a dynamic three-dimensional network of proteins, glycoproteins, and proteoglycans, is not merely a structural scaffold but an active signaling entity that regulates key biological processes including cell adhesion, migration, differentiation, and survival via mechanotransduction pathways [16]. This whitepaper provides a comprehensive technical comparison of drug responses in 2D versus 3D ECM environments, framing the discussion within the critical context of ECM biology and its implications for predicting clinical efficacy.
The limitations of 2D models became starkly apparent when promising cancer therapies that cleared preclinical hurdles based on 2D data failed dramatically in Phase I clinical trials [83]. The root cause was often traced to the models themselves: in patients, tumors are dense, three-dimensional ecosystems, not flat sheets of cells isolated from real-world complexities. This realization has propelled the adoption of 3D culture systems that recapitulate the intricate cell-cell and cell-ECM interactions, spatial organization, and metabolic gradients characteristic of human tissues [62] [82]. Understanding these differences is not merely an academic exercise but a practical necessity for improving the predictive validity of preclinical studies and reducing the alarming attrition rates of drug candidates in clinical development.
Fundamental Differences Between 2D and 3D Culture Systems
Architectural and Microenvironmental Contrasts
The architectural divergence between 2D monolayers and 3D ECM-embedded cultures creates fundamentally different microenvironments that profoundly influence cellular phenotype and drug response.
2D Monolayers confine cells to a flat, rigid plastic surface, forcing unnatural apical-basal polarization and disrupting native cytoskeletal organization. Cells are uniformly exposed to nutrients, oxygen, and therapeutic agents, eliminating the physiological gradients found in living tissues [83]. This environment selects for rapidly proliferating cells that may not represent the heterogeneous subpopulations within a tumor. Consequently, 2D cultures often overestimate drug efficacy because they fail to model the physical barriers and heterogeneous cell states that confer protection in vivo [83] [94].
3D ECM Environments, whether using natural matrices (e.g., Matrigel, collagen), synthetic scaffolds, or scaffold-free spheroids, restore a volumetric context for cellular growth. Cells in 3D culture exhibit more physiological cell-ECM interactions, establish proper cell polarity, and self-organize into structures that mimic key aspects of native tissue architecture [62]. Critically, 3D models recapitulate the tissue-scale gradients of oxygen, nutrients, pH, and metabolic waste products that arise as substances diffuse through the cellular mass [82]. This spatial heterogeneity creates distinct cellular zones—proliferative at the periphery, quiescent in the middle, and necrotic in the core—that mirror the microenvironments of solid tumors and significantly impact drug distribution and efficacy [82].
The Extracellular Matrix as an Active Signaling Platform
Beyond providing structural support, the ECM serves as a reservoir for growth factors and a platform for mechanotransduction—the process by which cells convert mechanical cues from their environment into biochemical signals [16]. The mechanical properties of ECM, including stiffness, viscoelasticity, and topology, are crucial regulators of cell behavior. In pathological conditions like cancer and fibrosis, ECM remodeling leads to measurable changes in these physical properties [16].
For instance, breast cancer tumors are significantly stiffer (≈4 kPa) than normal breast tissue (≈0.17 kPa), and this increased stiffness activates pro-tumorigenic signaling pathways such as YAP/TAZ and AKT, enhancing cell proliferation and invasion [16]. Similarly, during pulmonary fibrosis, ECM stiffness increases 5-10 times compared to healthy tissue [16]. These biomechanical changes are not recapitulated in 2D plastic cultures but are integral to 3D ECM models, influencing drug penetration and cellular responses to therapy. The ECM's physical properties regulate drug access through control of pore size, porosity, and binding sites, while simultaneously activating mechanosensitive pathways that can alter cellular susceptibility to pharmacological intervention [16] [3].
Table 1: Comparative Analysis of 2D vs. 3D Culture Systems
| Parameter | 2D Monolayer Culture | 3D ECM-Based Culture |
|---|---|---|
| Growth Pattern | Single layer on flat surface | Volumetric expansion in all directions |
| Cell-ECM Interactions | Minimal, unnatural | Extensive, physiologically relevant |
| Spatial Organization | Homogeneous, 2D | Heterogeneous, 3D with zoning |
| Nutrient/Oxygen Gradients | Absent | Present (outer to inner core) |
| Proliferation Profile | Uniform, rapid | Heterogeneous (proliferative, quiescent) |
| Gene Expression | Often de-differentiated | Tissue-specific, more in vivo-like |
| Drug Penetration | Immediate, uniform | Gradual, diffusion-limited |
| Mechanotransduction | Limited, substrate-driven | Physiological, ECM-mediated |
| Cost & Throughput | Low cost, high-throughput | Higher cost, moderate throughput |
Quantitative Differences in Drug Response
Documented Resistance in 3D Models
Empirical evidence consistently demonstrates that cells cultured in 3D ECM environments exhibit significantly higher resistance to chemotherapeutic agents compared to their 2D counterparts. A 2024 study utilizing stimulated Raman scattering (SRS) microscopy to investigate lapatinib treatment in A549 lung cancer cells revealed that despite similar intracellular drug concentrations in both 2D and 3D cultures, the growth of 3D spheroids was less impacted, indicating intrinsic drug tolerance mechanisms in the 3D microenvironment [95]. This finding suggests that resistance in 3D models is not solely attributable to physical barriers but involves fundamental changes in cellular physiology.
Similarly, a comprehensive 2023 study on colorectal cancer (CRC) cell lines demonstrated significant differences in responsiveness to 5-fluorouracil, cisplatin, and doxorubicin between 2D and 3D cultures [94]. The 3D-cultured cells showed notably higher viability post-treatment, confirming the protective influence of the 3D microenvironment. Transcriptomic analysis further revealed that cells in 3D models differentially expressed genes involved in drug resistance, providing a molecular basis for the observed phenotypic differences [94].
Table 2: Documented Drug Resistance in 3D Models Across Cancer Types
| Cancer Type | Therapeutic Agent | Resistance in 3D | Key Findings | Source |
|---|---|---|---|---|
| Lung Adenocarcinoma | Lapatinib | Enhanced | Similar drug uptake but reduced growth inhibition in 3D | [95] |
| Colorectal Cancer | 5-Fluorouracil, Cisplatin, Doxorubicin | Enhanced | Higher viability in 3D; distinct gene expression profiles | [94] |
| Various Solid Tumors | Chemotherapeutics | Generally Enhanced | Physical barriers, altered metabolism, and hypoxia contribute | [82] |
| High-Grade Serous Ovarian Cancer | Platinum-based agents | Enhanced | 3D models show better prediction of clinical response | [96] |
Mechanisms Underlying Differential Drug Responses
The enhanced drug resistance observed in 3D cultures arises from multiple interconnected mechanisms that collectively mimic the challenges of targeting tumors in vivo:
Physical Diffusion Barriers: The dense cellular packing and ECM composition in 3D models physically impede drug penetration, creating heterogeneous drug distribution within the spheroid. The outer layers of cells are exposed to higher drug concentrations, while inner regions receive sub-therapeutic doses, allowing survival of resistant subpopulations [95] [82]. Research using SRS microscopy has visually confirmed this heterogeneous drug penetration pattern in 3D spheroids, with decreasing drug signal from the periphery toward the core [95].
Altered Cellular Physiology and Signaling: Cells in 3D environments exhibit distinct gene expression profiles compared to 2D cultures. Transcriptomic analyses reveal significant differences in the expression of thousands of genes across multiple pathways, including those involved in cell survival, proliferation, and drug metabolism [94]. For example, 3D-cultured cells often show upregulation of efflux transporters, enhanced DNA repair capacity, and altered expression of apoptosis-related proteins [82]. Additionally, pathway activation differs substantially; breast cancer cells cultured on patient-derived tumor ECM scaffolds showed significant overexpression of invasiveness hub genes (CAV1, CXCR4, CNN3, MYB, TGFB1) and secreted higher levels of IL-6 compared to cells on normal ECM scaffolds [3].
Metabolic and Microenvironmental Adaptation: The metabolic gradients within 3D spheroids create distinct cellular subpopulations with different susceptibilities to therapeutic agents. Hypoxic regions in the spheroid core activate hypoxia-inducible factors (HIFs) that promote cell survival and upregulate drug resistance mechanisms [82]. Similarly, nutrient gradients and acidic pH in the inner regions further select for resistant phenotypes and can alter the activity of pH-dependent drugs [83].
ECM-Mediated Survival Signaling: Direct engagement with ECM components activates integrin-mediated signaling pathways that promote cell survival and confer resistance to apoptosis—a phenomenon known as "cell-adhesion-mediated drug resistance" (CAM-DR) [16] [3]. The mechanical properties of the ECM, particularly increased stiffness, can further enhance survival signaling through mechanotransduction pathways involving YAP/TAZ, FAK, and Rho GTPases [16].
Diagram 1: Mechanisms of Drug Resistance in 3D Microenvironments. The complex features of 3D culture systems activate multiple cellular response mechanisms that collectively contribute to enhanced drug resistance phenotypes.
Experimental Approaches and Methodologies
Establishing Physiologically Relevant 3D Models
Creating robust and reproducible 3D cultures requires careful selection of appropriate methodology based on research objectives and cell type characteristics. The main technical approaches can be broadly categorized as scaffold-based and scaffold-free systems:
Scaffold-Based Techniques utilize natural or synthetic matrices to provide structural support and biochemical cues that mimic the native ECM. Natural matrices like Matrigel (a basement membrane extract) and collagen type I hydrogels offer rich biological cues that support cell differentiation and tissue-specific organization [62]. For instance, a 2025 study on colorectal cancer spheroids found that Matrigel and collagen type I hydrogels promoted compact spheroid formation across multiple CRC cell lines [62]. Synthetic polymers, such as polyethylene glycol (PEG) and poly(lactic-co-glycolic) acid (PLGA), provide greater control over mechanical properties and composition but may lack natural bioactive motifs [62].
Scaffold-Free Techniques promote self-assembly of cells into spheroids without exogenous matrix support. Common methods include:
- Ultra-low attachment (ULA) plates: Surface treatment prevents cell adhesion, forcing aggregation into spheroids [96] [94].
- Hanging drop technique: Cells aggregate at the bottom of droplets by gravity, forming uniform spheroids [83] [62].
- Liquid overlay method: Agarose-coated wells prevent adhesion and promote spheroid formation [62].
A comparative study of CRC cell lines demonstrated that different techniques yield spheroids with varying morphologies, from compact spheroids to loose aggregates, depending on the specific cell line and culture conditions [62]. The study also presented a novel protocol for generating compact SW48 CRC spheroids using regular multi-well plates treated with anti-adherence solution, offering a cost-effective alternative to specialized plates [62].
Advanced Analytical Techniques for Drug Response Assessment
Conventional 2D assays often fail to accurately capture drug effects in 3D cultures due to differences in cellular metabolism, proliferation rates, and spatial heterogeneity. Advanced techniques are required to deconvolute the complex responses in 3D systems:
Stimulated Raman Scattering (SRS) Microscopy enables non-invasive, label-free quantification of intracellular drug uptake and distribution in live 3D cultures. A 2024 study utilized three-band SRS imaging (C-D, C-H, and fingerprint regions) to simultaneously measure drug uptake and cellular growth inhibition in 2D and 3D A549 cultures during lapatinib treatment [95]. This approach revealed that despite similar intracellular drug levels, 3D spheroids showed reduced growth inhibition, providing direct evidence for microenvironment-induced drug tolerance independent of uptake differences [95].
Multiparametric Viability and Apoptosis Assays that account for spatial heterogeneity are essential. The CellTiter 96 Aqueous Non-Radioactive Cell Proliferation Assay (MTS) can be adapted for 3D cultures, though with modified protocols to account for different metabolic rates and diffusion kinetics [94]. Similarly, flow cytometric analysis of apoptosis using Annexin V/PI staining requires careful dissociation of 3D structures to obtain single-cell suspensions while preserving cell viability and marker integrity [94].
Transcriptomic and Epigenetic Profiling provides molecular insights into differential drug responses. RNA sequencing of 2D versus 3D cultured cells reveals significant differences in gene expression profiles involving thousands of genes across multiple pathways [94]. Furthermore, DNA methylation patterns and microRNA expression in 3D cultures more closely resemble those in patient-derived Formalin-Fixed Paraffin-Embedded (FFPE) samples compared to 2D cultures, highlighting the superior physiological relevance of 3D models at the epigenetic level [94].
Diagram 2: Experimental Workflow for Drug Testing in 3D Models. A systematic approach from model establishment through data integration ensures physiologically relevant and reproducible assessment of drug responses in 3D microenvironments.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for 3D Drug Response Studies
| Reagent/Platform | Function/Application | Examples/Specifications |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Promote spheroid formation by preventing cell adhesion | Nunclon Sphera U-bottom plates; Corning spheroid microplates |
| Basement Membrane Matrix | Scaffold for organotypic growth; provides ECM proteins and signaling factors | Matrigel (Corning); Geltrex |
| Natural Hydrogels | Biologically active scaffolds mimicking native ECM | Collagen Type I; Fibrin; Alginate |
| Synthetic Hydrogels | Defined, tunable scaffolds with controllable mechanical properties | Polyethylene Glycol (PEG); PLGA |
| Advanced Imaging Systems | Label-free drug visualization and quantification in live 3D models | Stimulated Raman Scattering (SRS) Microscopy |
| Viability/Proliferation Assays | Metabolic activity measurement in 3D structures | CellTiter 96 Aqueous MTS Assay; ATP-based assays |
| Microfluidic Platforms | Precise control over microenvironmental conditions and gradients | Organ-on-a-chip; perfusion systems |
| Patient-Derived Scaffolds (PDS) | Decellularized human tissue retaining native ECM architecture | Tumor and normal tissue-derived PDS |
The evidence overwhelmingly demonstrates that 3D ECM-based culture systems provide a more physiologically relevant platform for evaluating drug responses compared to traditional 2D monolayers. The incorporation of proper ECM context recapitulates critical aspects of the tumor microenvironment—including 3D architecture, biomechanical cues, and metabolic gradients—that significantly influence drug penetration, cellular metabolism, and signaling pathway activation. These factors collectively contribute to the enhanced drug resistance observed in 3D models, which often more accurately predicts clinical outcomes [95] [94].
The future of preclinical drug development lies in the intelligent integration of 2D and 3D approaches, leveraging the strengths of each system. A tiered strategy employing 2D cultures for initial high-throughput screening followed by 3D validation for lead compounds represents a pragmatic approach that balances efficiency with physiological relevance [83]. Furthermore, the emergence of patient-derived scaffolds (PDS) that retain the native ECM architecture and composition from human tissues offers unprecedented opportunities for personalized therapy testing and disease modeling [3].
The integration of artificial intelligence and machine learning with 3D culture data holds particular promise for predictive modeling of drug responses and identification of resistance mechanisms [6]. As these technologies mature and standardization improves, 3D ECM-based models are poised to fundamentally transform preclinical drug development, bridging the translational gap and delivering more effective therapeutics to patients.
This case study investigates the mechanisms underlying enhanced chemoresistance in cancer spheroids, with a specific focus on the role of the extracellular matrix (ECM). Three-dimensional (3D) spheroid models recapitulate key features of the tumor microenvironment (TME) that are absent in traditional two-dimensional (2D) cultures, including complex cell-ECM interactions, nutrient and oxygen gradients, and altered metabolic phenotypes. These features collectively contribute to significant reductions in treatment efficacy, mirroring clinical chemoresistance patterns. By synthesizing recent findings on ECM composition, biomechanical properties, and their interplay with cellular metabolism, this analysis provides a mechanistic framework for understanding treatment failure and outlines advanced preclinical models for improving therapeutic outcomes. The clinical correlation of these findings underscores the importance of integrating ECM-rich 3D models into drug development pipelines to better predict patient responses.
The tumor microenvironment is a dynamic ecosystem where cancer cells constantly integrate biochemical and biophysical signals from the extracellular matrix, driving metabolic reprogramming and therapeutic resistance [97]. Traditional 2D cell culture models fail to replicate the complex 3D architecture and cell-ECM interactions of solid tumors, limiting their translational relevance [30] [98]. In contrast, 3D cancer spheroids better mimic the organization, matrix interactions, and heterogeneity found in vivo, including critical processes such as ECM remodeling, signaling gradients, and cellular heterogeneity [98] [99].
Within spheroids, the ECM is not merely a structural scaffold but an active participant that dictates cellular behavior through distinct physical and chemical properties [97]. ECM remodeling in cancer is characterized by altered composition, excessive collagen deposition, cross-linking, and increased stiffness, which activate mechanotransduction pathways that significantly rewire cellular metabolism and boost glycolytic flux [97] [100]. These ECM-driven adaptations create barriers to drug penetration and efficacy, contributing to the enhanced chemoresistance observed in spheroid models that closely mirrors clinical treatment failure [99] [101]. Understanding these matrix-mediated resistance mechanisms is crucial for developing more effective therapeutic strategies and predictive preclinical models.
Quantitative Data: ECM Properties and Their Functional Consequences in Spheroids
Table 1: Biomechanical Properties of ECM Hydrogels and Their Cellular Impact
| ECM Type | Concentration (mg/mL) | Storage Modulus, G' (Pa) | Mesh Size (nm) | Observed Cellular Response |
|---|---|---|---|---|
| Collagen | 6.0 | 206.13 ± 34.47 | 34.23 ± 1.84 | Shift toward anaerobic metabolism under glucose scarcity [97] |
| 4.0 | 57.97 ± 16.78 | 52.69 ± 5.10 | Metabolic phenotype predominantly dictated by glucose availability [97] | |
| 2.5 | 9.89 ± 3.21 | 95.33 ± 10.52 | Permissive for nutrient diffusion [97] | |
| Fibrin | 5.6 | 19.57 ± 1.36 | 74.79 ± 1.69 | Induces quiescent metabolic state [97] |
| 3.9 | 5.59 ± 2.96 | 118.57 ± 21.45 | Co-regulated adaptation by matrix and glucose levels [97] | |
| 2.2 | 3.38 ± 0.40 | 134.55 ± 5.51 | Promotes metabolic rigidity in pancreatic cancer cells [97] |
Table 2: Chemoresistance Factors in 3D Spheroid Models Versus 2D Cultures
| Resistance Mechanism | 2D Culture Manifestation | 3D Spheroid Manifestation | Clinical Correlation |
|---|---|---|---|
| Drug Penetration | Uniform access | Limited diffusion; penetration barriers [101] | Reduced intratumoral drug concentrations [99] |
| Proliferation Gradient | Homogeneous proliferation | Heterogeneous proliferation; quiescent core [99] | Tumor regions with slow cycling, resistant cells [99] |
| Metabolic Adaptation | Primarily oxidative metabolism | Glycolytic shift; metabolic reprogramming [97] | Therapy-resistant persister cells [97] [102] |
| ECM-Mediated Protection | Minimal ECM interaction | Dense ECM; physical barrier to drugs [101] [100] | Desmoplastic tumors with poor drug response [101] |
| Stromal Interaction | Limited stromal crosstalk | Integrated cancer-stromal signaling [101] | Activated stroma contributing to resistance [100] |
Experimental Protocols: Methodologies for Investigating ECM-Mediated Resistance
Protocol 1: Generation of Stromal-Rich Pancreatic Cancer Spheroids
This protocol establishes a reproducible co-culture spheroid model that recapitulates key features of pancreatic ductal adenocarcinoma (PDAC), including hypoxia, fibrosis, and chemoresistance [101].
Materials:
- PANC-1 (KRASG12D mutant) or BxPC-3 (wild-type KRAS) PDAC cell lines
- Human pancreatic stellate cells (hPSCs)
- Low-attachment 96-well plates
- Complete DMEM medium supplemented with 10% FBS
- Matrigel (for PANC-1 spheroids) or collagen I (optional)
Methodology:
- Cell Preparation: Mix PDAC cells and hPSCs in a ratio appropriate for your experimental design (e.g., 1:1) in complete medium.
- Seeding: Plate the cell mixture in low-attachment 96-well plates at a density of 1,000-5,000 cells per well, depending on desired spheroid size.
- Centrifugation: Centrifuge plates at 200 × g for 5 minutes to force cell-cell contact and promote uniform spheroid formation.
- Matrix Supplementation (Line-Specific):
- For PANC-1:hPSC spheroids: Supplement medium with 2.5% Matrigel to enhance compaction and density.
- For BxPC-3:hPSC spheroids: Use Matrigel-free medium to maintain regular morphology.
- Culture: Incubate under standard conditions (37°C, 5% CO2) for 2-10 days, monitoring formation daily.
- Validation: Assess spheroid morphology, size distribution, and compaction using live-cell imaging systems like Incucyte [101].
Key Considerations: PANC-1 spheroids require Matrigel for proper compaction, while BxPC-3 spheroids form dense structures without matrix supplementation. Collagen I can be used as an alternative to Matrigel but may induce invasiveness in PANC-1 models [101].
Protocol 2: Assessing Nanocarrier Penetration in 3D Spheroids
This protocol evaluates drug delivery system efficacy by quantifying nanoparticle penetration through spheroid ECM using light sheet microscopy [101].
Materials:
- Mature spheroids (5-10 days old)
- Fluorescently labeled nanocarriers (e.g., Pluronic F127-polydopamine NCs)
- Light sheet fluorescence microscope
- Image analysis software (e.g., Fiji/ImageJ with 3D plugins)
Methodology:
- Treatment: Incubate spheroids with fluorescent nanocarriers at clinically relevant concentrations for 24-48 hours.
- Washing: Gently wash spheroids 3× with PBS to remove non-internalized nanoparticles.
- Fixation: Fix spheroids with 4% paraformaldehyde for 1 hour at room temperature.
- Imaging: Mount spheroids in clear imaging chambers and image using light sheet microscopy.
- Critical Note: Confocal microscopy is not suitable for these studies due to limited penetration and should be avoided [101].
- Quantification:
- Acquire z-stacks through entire spheroid volume
- Measure fluorescence intensity from periphery to core
- Calculate penetration efficiency as percentage of core fluorescence relative to periphery
- Analysis: Generate 3D reconstructions to visualize nanoparticle distribution patterns relative to ECM density and cellularity.
Applications: This protocol enables direct evaluation of how ECM composition and density influence therapeutic access, providing insights for designing improved delivery systems to overcome physical barriers in solid tumors [101].
Signaling Pathways: Molecular Mechanisms of ECM-Mediated Resistance
Diagram 1: ECM-Driven Chemoresistance Pathways in Cancer Spheroids
Diagram 2: Experimental Workflow for Spheroid Chemoresistance Studies
The Scientist's Toolkit: Essential Research Reagents for Spheroid-ECM Studies
Table 3: Key Research Reagents for ECM-Integrated Spheroid Research
| Reagent/Material | Function in Spheroid Research | Application Examples |
|---|---|---|
| Ultra-Low Attachment Plates | Promotes cell aggregation by preventing surface adhesion | Spheroid formation without external scaffolds [30] [98] |
| Matrigel | Basement membrane extract rich in laminin and collagen IV | Enhances spheroid compaction; PDAC model development [101] |
| Collagen I Hydrogels | Mimics collagen-rich tumor stroma; tunable stiffness | Studying ECM density effects on drug penetration [97] [100] |
| Fibrin Hydrogels | Models provisional wound healing matrices | Investigating matrix-specific metabolic adaptation [97] |
| Decellularized ECM (dECM) | Preserves tissue-specific ECM architecture | Creating physiologically relevant microenvironments [100] |
| Pluronic F127-polydopamine NCs | Nanocarriers for evaluating drug penetration | Assessing transport barriers in spheroids [101] |
| Pancreatic Stellate Cells (hPSCs) | Source of cancer-associated fibroblasts (CAFs) | Modeling stromal-rich pancreatic TME [101] |
Clinical Correlation and Future Perspectives
The enhanced chemoresistance observed in 3D spheroid models has direct clinical correlations, particularly in desmoplastic cancers like pancreatic ductal adenocarcinoma where dense ECM creates physical barriers to therapeutic delivery [101]. Patient-derived spheroids are increasingly employed in clinical precision medicine, with several trials demonstrating the successful use of biopsy-derived cells to generate spheroids for drug screening and selection of optimal patient-specific treatments [99] [101]. The ECM composition and biomechanical properties of these models more accurately predict therapeutic response than traditional 2D cultures, potentially bridging the gap between conventional preclinical models and human clinical trials.
Future directions in the field include the integration of spheroid models with advanced technologies such as 3D bioprinting for precise ECM patterning, microfluidic systems for dynamic nutrient flow, and spatial transcriptomics to map gene expression patterns within different spheroid regions [99] [102]. The development of organoid models that incorporate patient-specific ECM components represents a promising avenue for personalized therapy selection [99]. Furthermore, understanding how obesity-driven ECM remodeling influences therapeutic resistance may uncover new targets for overcoming treatment failure in associated cancers [100]. As these advanced 3D models continue to evolve, their ability to recapitulate the complex ECM-mediated resistance mechanisms of human tumors will be instrumental in redesigning therapeutic strategies and improving clinical outcomes.
The extracellular matrix (ECM) is a major component of the tumor microenvironment, providing not only structural support but also critical biochemical and mechanical cues that influence cell behavior [103]. In cancer, the ECM undergoes significant remodeling, leading to alterations in its composition, architecture, and stiffness [3] [103]. This case study utilizes a 3D patient-derived scaffold (PDS) model to demonstrate that the tumor-specific ECM alone is sufficient to drive an aggressive phenotype in breast cancer cells, underscoring its vital role in cancer progression [3] [104].
The use of 3D cell cultures has become instrumental in cancer research as they better mimic the in vivo physiology compared to traditional 2D monolayers [90] [8]. Scaffold-based 3D cultures, in particular, provide a platform to study the complex interactions between cells and their native ECM [3]. This study specifically explores how ECM derived from human breast tumor tissue influences the gene expression and secretory profile of MCF-7 breast cancer cells, offering insights with significant implications for drug discovery and therapeutic targeting [3] [90].
Experimental Findings
Tumor ECM Exhibits Altered Composition and Mechanical Properties
The decellularization protocol successfully removed cellular content (DNA content reduced from 527.1 ng/μL to 7.9 ng/μL) while preserving key ECM components, as confirmed by histological staining and biochemical assays [3] [104]. Comparative analysis revealed significant differences between tumor-derived and normal ECM.
Table 1: Characterization of Decellularized Patient-Derived Scaffolds (PDS)
| Parameter | Normal PDS | Tumor PDS | Significance/Notes |
|---|---|---|---|
| DNA Content | Significantly reduced | Significantly reduced | Post-decellularization: 7.9 ng/μL (from 527.1 ng/μL in native) |
| Glycosaminoglycans (GAG) | 1.90 µg/mg | 2.99 µg/mg | Preserved after decellularization |
| Collagen Content | 226.71 µg/mg | 469.59 µg/mg | Preserved after decellularization |
| Collagen IV | Lower expression | Significantly overexpressed | Based on IHC evaluation |
| Vimentin | Lower expression | Significantly overexpressed | Based on IHC evaluation |
| Stiffness (Young's Modulus) | Lower | Significantly higher | Confirmed by tensile test |
The tumor PDS showed a higher density and abundance of key ECM proteins and increased cross-linking, which corresponded to a significantly stiffer microenvironment compared to normal PDS [3].
Tumor ECM Enhances Cell Proliferation and Inflammatory Secretion
When MCF-7 cells were cultured on the scaffolds, those on tumor PDS exhibited markedly higher viability and proliferation over a 15-day culture period [3] [104].
Table 2: Functional Cellular Responses on Normal vs. Tumor PDS
| Cellular Response | Normal PDS | Tumor PDS | Significance/Notes |
|---|---|---|---|
| Cell Viability (MTT Assay) | Lower | Higher | Measured on day 7 and day 15 |
| Proliferation (DAPI Nuclei Count) | 6 (mean count) | 59 (mean count) | P-value = 0.016 on day 15 |
| IL-6 Secretion | 30.23 pg/10⁶ cells | 122.91 pg/10⁶ cells | P-value = 0.048 |
The stark difference in IL-6 secretion, a cytokine strongly correlated with tumor progression and metastasis, further highlights the role of the tumor ECM in promoting a more aggressive and inflammatory phenotype [3].
Tumor ECM Upregulates Genes Associated with Invasiveness
A bioinformatic analysis identified differentially expressed genes (DEGs) associated with invasiveness and migration by comparing non-metastatic MCF-7 cells with metastatic breast cancer cell lines (MDA-MB-231, HCC1937, BT549, Hs578t) using two independent gene expression datasets (GSE111653 and GSE48213) [3] [104]. Gene co-expression network analysis identified seven hub genes as significant markers of cell motility and migration.
Table 3: Hub Genes Upregulated in MCF-7 Cells Cultured on Tumor PDS
| Gene Symbol | Gene Name | Primary Function in Cancer |
|---|---|---|
| CAV1 | Caveolin 1 | Role in cell signaling, migration, and mechanoprotection |
| CXCR4 | C-X-C Chemokine Receptor Type 4 | Promotes cell migration and metastasis |
| CNN3 | Calponin 3 | Regulates cytoskeleton and cell contraction |
| MYB | Myeloblastosis Proto-Oncogene | Transcription factor involved in cell proliferation |
| TGFB1 | Transforming Growth Factor Beta 1 | Induces epithelial-mesenchymal transition (EMT) |
| CAV2 | Caveolin 2 | Associated with CAV1 function |
| ZNF518B | Zinc Finger Protein 518B | Role in transcriptional regulation |
Quantitative real-time PCR confirmed that after 15 days in culture, MCF-7 cells on tumor PDS showed significant overexpression of these hub genes compared to cells cultured on normal PDS [3]. This provides direct evidence that the tumor ECM actively reprograms cancer cells toward a more invasive state.
Experimental Protocols
Decellularization Protocol for Patient-Derived Scaffolds (PDS)
- Tissue Source: Surgically resected breast tumor and normal adjacent healthy breast tissue specimens [3] [104].
- Decellularization Agent: An SDS-based protocol is employed to lyse and remove cellular material [3].
- Process Validation:
- Histology: Hematoxylin and Eosin (H&E) staining confirms the absence of cell nuclei while revealing preserved ECM architecture [3].
- Biochemical Assays: Quantification of DNA content confirms a drastic reduction. Assays for glycosaminoglycans (GAGs) and collagen confirm these key components are retained post-decellularization [3] [104].
- Immunohistochemistry (IHC): Staining for specific ECM components (e.g., Collagen IV, Vimentin) demonstrates their preservation and allows for comparison between normal and tumor PDS [3].
- Scanning Electron Microscopy (SEM): Used to visualize the ultrastructure, porosity, and integrity of the ECM in the PDS [3].
3D Cell Culture on PDS
- Cell Line: The breast cancer cell line MCF-7 is used [3] [104].
- Seeding: Cells are seeded onto the sterilized normal and tumor PDS.
- Culture Duration: Cells are cultured for up to 15 days to allow for full interaction and phenotypic adaptation to the ECM [3].
- Culture Conditions: Standard cell culture conditions are maintained (37°C, 5% CO₂) [3].
Analysis of Cell Behavior and Gene Expression
- Cell Viability and Proliferation:
- Cytokine Secretion:
- ELISA: The concentration of IL-6 secreted into the culture media is measured after 15 days and normalized to cell number [3].
- Gene Expression Analysis:
- Bioinformatics Pipeline: Microarray data from public repositories (GSE111653, GSE48213) is analyzed to identify DEGs and construct co-expression networks to pinpoint hub genes related to invasiveness [3] [104].
- Quantitative Real-Time PCR (qRT-PCR): Used to validate the expression levels of the identified hub genes (CAV1, CXCR4, CNN3, MYB, TGFB1, etc.) in MCF-7 cells cultured on both normal and tumor PDS [3].
Signaling Pathways and Workflow
The experimental workflow and the subsequent ECM-driven signaling that promotes invasiveness can be visualized in the following diagrams.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for PDS-based 3D Culture Research
| Item | Function/Application | Specific Examples/Notes |
|---|---|---|
| SDS (Sodium Dodecyl Sulfate) | Primary detergent for decellularization protocol; lyses cells and removes cellular material from tissue. | Used in a defined protocol to ensure complete decellularization while preserving ECM structure [3]. |
| DNase/RNase Enzymes | Degrade residual nucleic acids post-decellularization to ensure complete removal of genetic material. | Often used following detergent washes to clean the scaffold [3]. |
| Patient-Derived Tissues | Source of biologically relevant, human-specific ECM for creating scaffolds. | Surgically resected breast tumor and normal adjacent tissues [3] [104]. |
| MCF-7 Cell Line | Model non-metastatic, hormone-responsive breast cancer cell line for studying ECM-induced phenotypic changes. | Well-characterized; its shift to an aggressive phenotype on tumor PDS is a key outcome measure [3] [104]. |
| Collagen & GAG Assay Kits | Quantitative biochemical assessment of key ECM components to validate scaffold composition post-decellularization. | Confirms preservation of critical ECM proteins and glycosaminoglycans [3]. |
| qRT-PCR Reagents & Probes | Quantification of gene expression changes in cells cultured on PDS. | Essential for validating the upregulation of identified hub genes (e.g., CAV1, CXCR4, TGFB1) [3] [104]. |
| IL-6 ELISA Kit | Quantification of secreted IL-6 cytokine as a marker of tumor-promoting inflammation and aggression. | Used to measure cytokine levels in conditioned media [3]. |
| Anti-Collagen IV & Anti-Vimentin Antibodies | Immunohistochemical staining to visualize and quantify specific ECM proteins in the PDS. | Critical for comparing ECM composition between normal and tumor PDS [3]. |
The transition from conventional two-dimensional (2D) to three-dimensional (3D) cell culture represents a paradigm shift in biomedical research, particularly for biomarker discovery and therapeutic target identification. Traditional 2D cultures, while simple and low-cost, fail to replicate the complex interactions present in solid tumors, as cells grown in monolayers exhibit uniform access to nutrients and therapeutic agents that do not reflect the in vivo microenvironment [32]. Three-dimensional models, including spheroids and organoids, more accurately mimic the dynamic cell–cell and cell–matrix interactions within the tumor microenvironment (TME), better resembling tumor growth and initial stages of dissemination [30] [32].
The extracellular matrix (ECM) serves as a critical component in this process, forming a complex 3D dynamic intercellular macromolecular network that provides structural support while functionally driving cell morphology, signaling, and cellular behavior [30]. Within the TME, the interplay between stromal and cancer cells creates a provisional matrix that mediates cancer cell reprogramming and induces epithelial-to-mesenchymal transition (EMT), fostering aggressive and invasive characteristics [30]. This matrix remodeling, primarily driven by enzymes like matrix metalloproteinases (MMPs), generates pathways that enable cancer cell migration and invasion [30]. The ECM also facilitates the storage and controlled presentation of signaling molecules to neighboring cells, thereby inducing pathways that influence cell fate, making it an essential element for identifying clinically relevant biomarkers and therapeutic targets [30].
Experimental Platforms for 3D Biomarker Discovery
Types of 3D Culture Systems
Three-dimensional cell culture technologies can be broadly categorized into scaffold-free and scaffold-based systems, each offering distinct advantages for biomarker discovery research:
Scaffold-free systems rely on low-adherence surfaces to encourage cell self-aggregation through techniques including hanging-drop, low-adherence round-bottom wells, and rotating cultures [32]. These cultures self-organize, produce their own ECM, and form extensive cell-to-cell contacts, making them akin to the avascular in vivo environment of organs like the heart, liver, and pancreas [32]. They represent a simple, cost-effective, and scalable approach for producing uniform spheroids for high-throughput applications [32].
Scaffold-based systems use physical networks including hydrogels and polymer scaffolds to mimic the native tissue ECM [32]. Natural hydrogels formed of proteins and ECM components such as collagen, chitosan, or Corning Matrigel matrix are biocompatible, non-immunogenic, and have been shown to enhance multiple cellular activities [4] [32]. Synthetic gels composed of materials such as poly(ethylene glycol) or polyacrylamide offer simple chemistry, robust manufacturing, and high customizability [32].
Organoid systems represent more advanced 3D models that self-organize and recreate organ physiology, accurately representing clinical diseases in remarkable detail [32]. These mini-organ cultures originate from various sources including neonatal tissues, pluripotent stem cells, and tissue biopsies, making them particularly valuable for disease modeling, drug discovery, and personalized medicine applications [32].
Experimental Workflow for 3D Biomarker Identification
The following diagram outlines a comprehensive experimental workflow for biomarker discovery using 3D culture models:
Key Methodologies and Protocols
Spheroid Formation and Maintenance
Protocol: Scaffold-free Spheroid Development using U-bottom Plates
- Cell Seeding: Harvest cells using standard trypsin-EDTA protocol and prepare single-cell suspension. Seed MCF-7 and MDA-MB-231 breast cancer cell lines at densities ranging from 5,000-15,000 cells per well in U-shape, round bottom 96-well plates with ultra-low adhesive properties (SPL Life Sciences, 911606) [30].
- Culture Conditions: Incubate cells in complete medium (DMEM with 10% FBS and antimicrobial agents) at 37°C in a humidified atmosphere of 5% CO₂, allowing for cellular self-aggregation and spheroid development [30].
- Growth Monitoring: Monitor spheroid growth through phase-contrast microscopy (e.g., Evident Scientific CKX41 with integrated digital camera) to determine optimal time points for downstream analyses. Typically, 72 hours of culture is sufficient for spheroid development [30].
- Serum Starvation: For specific experimental applications, discard medium and culture cells following a 16-20 hour serum-free medium starvation period to synchronize cell cycles and reduce serum-induced signaling [30].
- Spheroid Collection: For molecular analyses, carefully collect spheroids using wide-bore pipette tips to prevent structural disruption. For functional assays, transfer intact spheroids to standard flat-bottom well plates to examine dissemination and migratory properties [30].
Morphological Characterization via Scanning Electron Microscopy (SEM)
Protocol: SEM Sample Preparation and Imaging
- Fixation: Once spheroids are formed, gently wash with phosphate buffer (0.2 M, pH 7.4). Fix spheroids in Karnovsky's solution [4% (w/v) PFA, 5% (v/v) glutaraldehyde, 0.04 M phosphate buffer solution] for 1 hour at room temperature to preserve cellular and structural integrity [30].
- Post-fixation: Wash fixed spheroids with 0.1% cacodylate buffer, then post-fix in 1% osmium tetroxide for enhanced membrane contrast and stabilization [30].
- Dehydration and Preparation: Dehydrate samples through a graded ethanol series (30%, 50%, 70%, 90%, 100%), followed by critical point drying to preserve 3D structure without collapse [30].
- Imaging: Mount spheroids on SEM stubs, sputter-coat with gold/palladium to approximately 10-15 nm thickness, and image using appropriate accelerating voltage (typically 5-15 kV) to visualize surface ultrastructure and cell-cell interactions [30].
Molecular Analysis of EMT and ECM Components
Protocol: RNA Extraction and Gene Expression Analysis
- RNA Extraction: Homogenize 5-10 spheroids per sample using appropriate lysis buffer. Extract total RNA using column-based purification systems, ensuring DNase treatment to remove genomic DNA contamination [30].
- cDNA Synthesis: Use 500 ng - 1 μg of total RNA for reverse transcription with oligo(dT) and random hexamer primers to ensure comprehensive cDNA representation [30].
- Quantitative PCR: Perform qPCR reactions using SYBR Green or TaqMan chemistry with primers specific to target genes. Key targets should include:
- Data Analysis: Normalize expression to appropriate housekeeping genes (GAPDH, β-actin, HPRT1) using the 2^(-ΔΔCt) method for relative quantification. Perform statistical analysis across biological replicates (n ≥ 3) [30].
Quantitative Analysis of Biomarkers in 3D Models
Differential Expression of Key Receptors and ECM Components
Table 1: Expression Profile of Therapeutic Targets in 3D Breast Cancer Models
| Target Category | Specific Marker | MCF-7 3D Expression | MDA-MB-231 3D Expression | Functional Significance |
|---|---|---|---|---|
| Hormone Receptors | ERα | Significant upregulation | Absent | Predictive of endocrine therapy response [30] |
| ERβ | Moderate expression | Significant upregulation | Potential therapeutic target in TNBC [30] | |
| Receptor Tyrosine Kinases | EGFR | Moderate | Highly upregulated | Driver of proliferation and invasion [30] |
| IGF1R | Upregulated | Significantly upregulated | Metastasis and therapy resistance [30] | |
| Syndecan Family | SDC1 | Downregulated | Upregulated | Prognostic relevance in breast cancer [30] |
| SDC4 | Significantly upregulated | Moderate upregulation | Matrix assembly and cell adhesion [30] | |
| Matrix Metalloproteinases | MMP-2 | Moderate increase | Significant upregulation | ECM remodeling and invasion [30] |
| MMP-9 | Upregulated | Highly upregulated | Metastatic potential indicator [30] | |
| MT1-MMP | Increased | Significantly upregulated | Pro-invasive microenvironment [30] |
Functional Properties in 3D Culture Systems
Table 2: Functional Characteristics of Breast Cancer Cells in 3D Models
| Functional Attribute | MCF-7 3D Model | MDA-MB-231 3D Model | Assay Method |
|---|---|---|---|
| Spheroid Formation Efficiency | 85-90% | 90-95% | Phase-contrast microscopy quantification [30] |
| Spheroid Size (72h) | 150-200μm | 200-250μm | Digital caliper measurement of SEM images [30] |
| Dissemination Potential | Low | High | Migration assay after transfer to 2D [30] |
| Invasion Capacity | Minimal | Extensive | Matrigel invasion assay [30] |
| Proliferation Rate | Moderate | High | Ki-67 staining, Alamar Blue assay [30] |
| Therapeutic Response | Tamoxifen-sensitive | Tamoxifen-resistant | Dose-response curves [30] |
| EMT Status | Epithelial characteristics maintained | Mesenchymal phenotype enhanced | Immunofluorescence, qPCR [30] |
Signaling Pathways in ECM-Mediated Biomarker Regulation
The interaction between ECM components and cellular receptors creates complex signaling networks that drive biomarker expression and represent potential therapeutic targets. The following diagram illustrates key pathways identified through 3D culture analysis:
Key Signaling Mechanisms
ER-ECM Crosstalk: 17β-estradiol (E2)-ER signaling regulates critical functional properties including cell differentiation, proliferation, EMT, migration, invasion, metastasis, and resistance to treatment [30]. The non-genomic ER-mediated E2 effects result in rapid activation of receptor tyrosine kinases and downstream signaling pathways [30]. E2-ER signaling can modulate the expression of syndecans in both ERα+ and ERα- breast cancer cells, creating a feedback loop that influences cellular responses to the microenvironment [30].
RTK-ECM Integration: EGFR and IGF1R mediate signaling pathways that regulate expression of target genes during breast cancer progression, thereby influencing cell proliferation, metabolic reprogramming, apoptotic evasion, EMT, invasion, and metastasis [30]. The coordinated actions of ERs and ECM molecules mediate matrix remodeling within the TME, with E2-ERα signaling driving MMP-2, MMP-9, and MT1-MMP upregulation, promoting ECM remodeling and thereby enhancing breast cancer cell invasion and migration [30].
Matrix-Driven EMT Regulation: ECM composition and mechanical properties regulate EMT, endowing cancer cells with invasive/migratory potential and stemness characteristics [30]. The interplay between stromal and cancer cells creates a provisional matrix that mediates cancer cell reprogramming and induces EMT, fostering aggressive and invasive characteristics [30]. Matrix remodeling, primarily driven by MMPs, generates pathways that enable cancer cells to migrate and invade the aligned and stiff ECM [30].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for 3D Biomarker Discovery
| Reagent/Category | Specific Product Examples | Research Application | Experimental Function |
|---|---|---|---|
| Ultra-Low Attachment Plates | SPL Life Sciences U-shape 96-well round bottom (911606) [30] | Spheroid formation | Prevents cell attachment, enables 3D self-assembly |
| Basement Membrane Matrix | Corning Matrigel matrix [4] | Organoid culture, invasion assays | Mimics tumor ECM, supports 3D growth |
| Hydrogel Systems | Collagen I, Synthetic PEG-based hydrogels [32] | Tunable 3D microenvironments | Customizable mechanical properties |
| Cell Lines | MCF-7 (HTB-22), MDA-MB-231 (HTB-26) from ATCC [30] | Disease modeling | Representative models of breast cancer subtypes |
| Culture Media | DMEM with 10% FBS, antimicrobial agents [30] | Cell maintenance | Supports cell growth while preventing contamination |
| Dissociation Reagents | Trypsin-EDTA 1X in PBS (LM-T1706) [30] | Cell passaging, analysis | Gentle dissociation for cell recovery |
| Fixation Reagents | Karnovsky's solution (4% PFA, 5% glutaraldehyde) [30] | SEM sample preparation | Preserves 3D ultrastructure |
| Molecular Analysis Kits | RNA extraction kits, cDNA synthesis kits [30] | Biomarker quantification | Gene expression analysis of 3D models |
Three-dimensional cell culture models represent a transformative approach for biomarker discovery and therapeutic target identification, primarily through their ability to recapitulate the crucial role of the extracellular matrix in tumor biology. The data generated from these models reveals significant differential expression of key receptors, matrix components, and EMT markers that are often missed in conventional 2D systems [30]. The integration of 3D culture with advanced technologies including artificial intelligence, high-content imaging, and bioinformatic analysis promises to further enhance the predictive value of these platforms [6]. As the field progresses, standardization of 3D culture protocols and analytical methods will be essential for translating these findings into clinically actionable biomarkers and effective therapeutic strategies for cancer patients [32].
The high failure rate of drug candidates in clinical trials, often due to inadequate efficacy or unanticipated toxicity, remains a critical challenge in pharmaceutical development. This failure is largely attributable to the poor predictive power of traditional two-dimensional (2D) cell cultures and animal models, which do not faithfully recapitulate human physiology. The integration of three-dimensional (3D) cell culture models, particularly those emphasizing the role of the extracellular matrix (ECM), represents a transformative approach for bridging this translational gap. This technical review examines how 3D models that incorporate physiologically relevant ECM components enhance the prediction of clinical efficacy and toxicity by preserving native cellular architecture, cell-ECM interactions, and mechanotransduction pathways. We provide detailed methodologies for implementing ECM-rich 3D models, quantitative data validating their superior predictive capabilities, and a strategic framework for their application across the drug development pipeline.
The extracellular matrix (ECM) is a highly dynamic, three-dimensional network that provides not only structural support but also critical biochemical and mechanical cues essential for cellular function [16]. Composed of macromolecules including collagens, glycosaminoglycans, elastin, and proteoglycans, the ECM regulates fundamental biological processes such as cell adhesion, migration, differentiation, and signal transduction [16]. In the context of drug development, the ECM's role extends beyond passive scaffolding to actively influence disease pathogenesis, drug penetration, and cellular responses to therapeutic compounds.
Traditional 2D cell cultures fail to replicate the complex 3D architecture and mechanobiological signaling present in human tissues. Cells cultured on flat, rigid plastic surfaces exhibit altered morphology, gene expression, proliferation, and metabolic activity compared to their in vivo counterparts. Similarly, animal models often poorly predict human responses due to interspecies differences in physiology and disease mechanisms. Statistics show that over 90% of drugs appearing safe and effective in animals ultimately fail in human clinical trials, often due to unanticipated safety or efficacy issues [105].
The integration of ECM-rich 3D models addresses these limitations by providing a more physiologically relevant microenvironment that enhances the predictive accuracy for both drug efficacy and toxicity. This paradigm shift is now being accelerated by regulatory evolution, including the FDA Modernization Act 2.0, which provides legal pathways for using non-animal methods in Investigational New Drug (IND) applications [105].
The ECM as a Critical Determinant in 3D Model Fidelity
ECM Composition and Mechanical Properties
The ECM's biological relevance stems from its complex composition and physical properties, which collectively influence cell behavior through mechanotransduction pathways. The mechanical properties of ECM, such as stiffness, topology, and viscoelasticity, serve as key regulators of cellular behavior in both normal and pathological conditions [16].
Table 1: Key Physical Properties of the ECM and Their Biological Significance
| Property | Definition | Physiological Range | Pathological Alterations |
|---|---|---|---|
| Stiffness | Resistance to deformation | Brain: <2 kPa [16]Bone: 40-55 MPa [16] | Breast cancer: 4.04±0.9 kPa vs. normal: 0.167±0.031 kPa [16]Pulmonary fibrosis: ~16.52 kPa (5-10x increase) [16] |
| Viscoelasticity | Combined elastic (energy storage) and viscous (energy dissipation) properties | Varies by tissue type | Increased energy dissipation in cancerous tissues enhancing aggressiveness [16] |
| Topology | Spatial arrangement and geometry of ECM fibers | Tissue-specific 3D organization | Altered fiber alignment and porosity in disease states |
These mechanical properties are sensed by cells through mechanosensitive receptors including integrins, Piezo1, TRPV4, and transduced into biochemical signals via pathways such as YAP/TAZ [16]. In pathological states, ECM dysregulation creates a self-reinforcing cycle that promotes disease progression. For example, in breast cancer, ECM stiffness activates mechanotransduction pathways that promote oncogene expression, epithelial-mesenchymal transition (EMT), and metastasis [16].
ECM Remodeling in Disease States
The ECM undergoes significant remodeling in various disease states, creating microenvironments that directly impact therapeutic efficacy. Research utilizing patient-derived scaffolds (PDS) has demonstrated that tumor-specific ECM alterations actively drive aggressive cellular behavior. In a study comparing breast tumor PDS to normal breast tissue PDS, tumor ECM showed significantly higher abundance of collagen, glycosaminoglycans, collagen IV, and vimentin [3]. When MCF-7 breast cancer cells were cultured on these scaffolds, those grown on tumor PDS exhibited significantly higher viability, proliferation, and secretion of IL-6 (122.91 vs. 30.23 pg/10⁶ cells) compared to those on normal PDS [3]. Furthermore, tumor PDS upregulated expression of invasiveness-associated genes (CAV1, CXCR4, CNN3, MYB, and TGFB1), demonstrating how the tumor ECM actively promotes malignant progression [3].
Experimental Approaches: Implementing ECM-Rich 3D Models
Patient-Derived Scaffolds (PDS) Methodology
Patient-derived scaffolds represent one of the most physiologically relevant approaches for incorporating human ECM into 3D models. The following protocol details the decellularization process for generating PDS:
Decellularization Protocol:
- Tissue Acquisition: Obtain surgically resected tumor and normal tissue specimens from consenting patients under IRB-approved protocols.
- Sample Preparation: Cut tissue into approximately 1 cm³ pieces while preserving native architecture.
- Decellularization Process:
- Incubate tissues in 1% sodium dodecyl sulfate (SDS) solution with continuous agitation for 48-72 hours.
- Replace SDS solution every 24 hours until tissue becomes opaque and translucent.
- Treat with DNase solution (100 U/mL in 1M NaCl) for 24 hours to remove residual DNA.
- Rinse extensively with phosphate-buffered saline (PBS) containing antibiotics to remove all detergent residues.
- Sterilization: Subject decellularized scaffolds to gamma irradiation or ethylene oxide treatment.
- Characterization:
- Confirm decellularization through H&E staining and DAPI staining showing absence of nuclear material.
- Quantify DNA content (<50 ng/mg dry weight indicates effective decellularization).
- Assess ECM preservation through glycosaminoglycan quantification (1.62 vs. 1.90 μg/mg in normal native vs. decellularized) and collagen content (186.94 vs. 226.71 μg/mg in normal native vs. decellularized) [3].
- Evaluate mechanical properties through tensile testing to determine Young's modulus.
This protocol successfully preserves key ECM components while removing cellular material, providing a biologically relevant scaffold for 3D cell culture that maintains disease-specific ECM alterations.
Organoid and Spheroid Models in ECM Hydrogels
While PDS offer high biological fidelity, organoids and spheroids embedded in defined ECM hydrogels provide greater standardization and scalability:
Standardized Organoid Protocol:
- Cell Sourcing: Isolate primary cells from patient tissues or use established cell lines.
- ECM Hydrogel Preparation: Prepare commercially available basement membrane extracts (e.g., Matrigel) or defined synthetic hydrogels at concentrations mimicking physiological stiffness.
- 3D Culture Setup: Suspend cells in ECM hydrogel and plate as droplets in low-attachment plates.
- Culture Maintenance: Feed with appropriate media formulations containing tissue-specific growth factors.
- Drug Testing: Expose organoids to compound libraries and assess viability, morphology, and functional endpoints.
The reproducibility of organoid models has been significantly enhanced through initiatives like the NIH's $87 million Standardized Organoid Modeling (SOM) Center, which addresses previous limitations in protocol standardization across laboratories [105].
Quantitative Assessment of Predictive Improvement
The enhanced predictive value of ECM-integrated 3D models is demonstrated through multiple studies comparing their performance to traditional models in both efficacy and toxicity assessment.
Table 2: Predictive Performance of 3D Models vs. Traditional Approaches
| Model Type | Application | Performance Metric | Result | Reference |
|---|---|---|---|---|
| Tumor PDS | Breast cancer drug response | IL-6 secretion (marker of aggression) | Tumor PDS: 122.91 pg/10⁶ cellsNormal PDS: 30.23 pg/10⁶ cells | [3] |
| Tumor PDS | Breast cancer cell proliferation | DAPI-stained nuclei count | Tumor PDS: 59 nuclei/slideNormal PDS: 6 nuclei/slide | [3] |
| Organoids | Drug-induced liver injury (DILI) prediction | Clinical concordance | Superior to animal models in predicting human DILI | [106] |
| PDX-derived models | Clinical trial outcome prediction | Correlation with patient response | 85-90% predictive accuracy for oncology drugs | [106] |
The implementation of these advanced models within drug development pipelines is yielding tangible benefits. In the first half of 2025, half of the 16 novel drugs approved by FDA's Center for Drug Evaluation and Research (CDER) were for cancer treatment, with many benefiting from more predictive preclinical models including those focusing on tumor microenvironment interactions [106].
Integrating 3D Models with Advanced Analytical Technologies
Artificial Intelligence and Machine Learning
The complex, high-dimensional data generated by 3D models creates both challenges and opportunities for analysis. Artificial intelligence (AI) and machine learning (ML) approaches are increasingly being integrated with 3D model outputs to enhance toxicity prediction and efficacy assessment [107].
AI-based toxicity prediction models are trained on large-scale public databases (e.g., ChEMBL, DrugBank, Tox21) and proprietary data from 3D model experiments to predict various toxicity endpoints including hepatotoxicity, cardiotoxicity, nephrotoxicity, and genotoxicity [107]. These models utilize diverse algorithms including Random Forest, XGBoost, Graph Neural Networks (GNNs), and Transformer-based architectures, achieving superior predictive accuracy compared to traditional methods [107].
The FDA has established a Modeling and Simulation Working Group (M&S WG) specifically to advance the use of these computational technologies, including AI/ML and Physiologically Based Pharmacokinetic (PBPK) modeling, in regulatory decision-making [105].
The Research Toolkit: Essential Reagents and Platforms
Successful implementation of ECM-rich 3D models requires specialized reagents and platforms. The following table details key components of the experimental toolkit:
Table 3: Research Reagent Solutions for ECM-Rich 3D Models
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Basement membrane extracts | Provide complex ECM microenvironment | Organoid culture, cell differentiation studies |
| Synthetic hydrogels | Defined ECM mimics with tunable properties | Mechanotransduction studies, high-throughput screening |
| Patient-derived scaffolds | Maintain disease-specific ECM architecture | Study tumor-stroma interactions, personalized therapy testing |
| Decellularization kits | Remove cellular content while preserving ECM | Creation of tissue-specific scaffolds |
| Organoid biobanks | Standardized, characterized 3D model collections | High-throughput drug screening, biomarker discovery |
| Microfluidic systems | Enable perfusion and mechanical stimulation | Organ-on-a-chip models, pharmacokinetic studies |
Regulatory and Implementation Framework
The transition toward human-relevant 3D models is being actively supported through regulatory evolution. The FDA Modernization Act 2.0 provided the critical legal foundation by authorizing the use of non-animal methods in IND applications [105]. The subsequent FDA "Roadmap to Reducing Reliance on Animal Testing in Preclinical Safety Studies" outlines a phased transition, with monoclonal antibodies (mAbs) identified as an immediate focus area [105].
The FDA is structuring internal capabilities to support this transition through the New Alternative Methods Program (NAMP) with $5 million in funding and two key working groups: the Alternative Methods Working Group (AMWG) for qualifying in vitro methods, and the Modeling and Simulation Working Group (M&S WG) for computational tools [105]. The agency's long-term goal (3-5 years) is to make animal studies the exception rather than the norm [105].
The integration of ECM-rich 3D models represents a fundamental advancement in our ability to predict clinical efficacy and toxicity during drug development. By preserving native tissue architecture, mechanical properties, and cell-ECM interactions, these models bridge the critical translational gap between traditional preclinical models and human clinical response. The experimental protocols, quantitative data, and implementation frameworks presented in this review provide researchers with practical guidance for adopting these transformative technologies. As standardization improves and regulatory acceptance grows, ECM-integrated 3D models are poised to become the default approach for preclinical testing, ultimately accelerating the development of safer, more effective therapeutics.
Diagram: Experimental Workflow for PDS-Based Drug Screening
Diagram: ECM Signaling in 3D Models
Conclusion
The integration of ECM biology into 3D cell culture is fundamentally transforming preclinical research. Evidence confirms that ECM-rich 3D models—from decellularized scaffolds to sophisticated hydrogels—far surpass traditional 2D cultures by replicating the critical biochemical and biophysical cues of the native tissue microenvironment. This enhanced physiological relevance leads to more accurate modeling of human diseases, particularly cancer, and generates drug response data that is more predictive of clinical outcomes. The future of the field lies in overcoming challenges related to standardization, scalability, and incorporating immune components. The convergence of 3D models with advanced technologies like AI-driven analysis and 3D bioprinting promises a new era of 'clinical trials in a dish,' accelerating the development of personalized and effective therapies while reducing the ethical and financial burden of animal testing.
References
- 1. 3d Cell Culture Market: Comprehensive Analysis and ... [https://www.pharmiweb.com/press-release/2025-02-12/3d-cell-culture-market-comprehensive-analysis-and-forecast-2025-2035]
- 2. Harnessing 3D cell models and high-resolution imaging to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277333/]
- 3. Tumor extracellular matrix enhances invasive gene ... [https://www.nature.com/articles/s41598-025-12196-z]
- 4. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 5. 3D Cell Culture Market Size 2024-2028 [https://www.technavio.com/report/3d-cell-culture-market-industry-analysis]
- 6. Leveraging 3D cell culture and AI technologies for next- ... [https://www.sciencedirect.com/science/article/pii/S3050562325000418]
- 7. Cell–extracellular matrix mechanotransduction in 3D - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10656994/]
- 8. Three-Dimensional in Vitro Cell Culture Models in Drug ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.00006/full]
- 9. "Collagen as extracellular matrix (ECM) for three-dimensional ... [https://tost.unise.org/pdfs/vol11/no4-2/ToST-FSMP2413-RA.html]
- 10. Human extracellular matrix (ECM)-like collagen and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10965421/]
- 11. Role of extracellular matrix proteoglycans in immune cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8961502/]
- 12. Three-Dimensional Models as a New Frontier for Studying ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.569454/full]
- 13. Identification of extracellular matrix proteins secreted by ... [https://www.nature.com/articles/s41598-021-85742-0]
- 14. Multiparametric physicochemical analysis of a type 1 ... [https://www.nature.com/articles/s41598-025-93700-3]
- 15. High-throughput Generation of Collagen Microbeads for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11566015/]
- 16. Extracellular Matrix Signaling Cues: Biological Functions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271642/]
- 17. Extracellular matrix dynamics: tracking in biological systems ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-022-00292-x]
- 18. Scaffolds with spatiotemporally controlled growth factor ... [https://www.nature.com/articles/s41536-025-00431-0]
- 19. ECM-binding properties of extracellular vesicles [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02156-5]
- 20. Emerging mechanomedicines informed by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158467/]
- 21. Matrix deformation and mechanotransduction as markers of ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01589d]
- 22. Piezo1-mediated mechanotransduction regulates the ... [https://www.nature.com/articles/s41392-025-02350-4]
- 23. Fibrosis and cancer: A strained relationship [https://pmc.ncbi.nlm.nih.gov/articles/PMC7733542/]
- 24. ECM formation and degradation during fibrosis, repair, and ... [https://www.nature.com/articles/s44324-025-00063-4]
- 25. Extracellular matrix: unlocking new avenues in cancer treatment [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00757-3]
- 26. Biomaterial-based 3D human lung models replicate ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706125005914]
- 27. Mechanisms of matrix metalloproteinase 16 in ... [https://pubmed.ncbi.nlm.nih.gov/40675518/]
- 28. Collagen Signaling via DDR1 Exacerbates Barriers to ... [https://pubmed.ncbi.nlm.nih.gov/41170605/]
- 29. PIEZO1-mediated mechanotransduction regulates ... [https://www.sciencedirect.com/science/article/pii/S174270612400744X]
- 30. Spheroid-Based 3D Models to Decode Cell Function and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606745/]
- 31. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 32. Current strategies with implementation of three- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9372643/]
- 33. Decellularized extracellular matrix scaffolds: Recent trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637010/]
- 34. Decellularized extracellular matrix biomaterials for ... [https://www.sciencedirect.com/science/article/pii/S2452199X23003006]
- 35. Decellularized extracellular matrix-based disease models ... [https://www.sciencedirect.com/science/article/pii/S2590006424003417]
- 36. Native extracellular matrix: a new scaffolding platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4058757/]
- 37. The introduction and evaluation of novel decellularized ... [https://www.nature.com/articles/s41598-025-11559-w]
- 38. Recent Advances in Decellularized Matrix-Derived Materials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10048399/]
- 39. Revisiting the biophysical aspects of extracellular-matrix ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d5bm00210a]
- 40. Hydrogel Design to Understand and Guide 3D Cell Migration [https://link.springer.com/article/10.1007/s40883-025-00395-z]
- 41. Tailoring Therapy: Hydrogels as Tunable Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469974/]
- 42. 3D hydrogel platform with macromolecular actuators for ... [https://www.nature.com/articles/s41467-025-60062-3]
- 43. Hybrid hydrogel–extracellular matrix scaffolds identify ... [https://www.nature.com/articles/s41563-025-02234-6]
- 44. Photo-tunable hydrogels reveal cellular sensing of rapid ... [https://www.sciencedirect.com/science/article/abs/pii/S193459092400359X]
- 45. Impact of 3D cell culture hydrogels derived from basement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362413/]
- 46. An Overview on Spheroid and Organoid Models in Applied ... [https://www.mdpi.com/2413-4155/7/1/27]
- 47. Three-dimensional spheroid models for cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270648/]
- 48. Mechanical cues guide the formation and patterning of 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448454/]
- 49. Extracellular Matrix (ECM) Hydrogels for Regenerative ... [https://mtec-sc.org/technology-showcase/extracellular-matrix-ecm-hydrogels-regenerative-medicine-applications]
- 50. Label-free cell imaging and tracking in 3D organoids [https://www.sciencedirect.com/science/article/pii/S2666386425001213]
- 51. Neural growth patterns: how random and aligned fibers ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1659965/full]
- 52. House of cards: therapeutic vulnerabilities in the tumor ... [https://www.fredhutch.org/en/news/spotlight/2025/11/hb-nishidi-aoki-cellrepmed.html]
- 53. Bridging the gap: the role of 3D cell cultures in mimicking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378905/]
- 54. Advancing oncology drug development: Innovative ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25002094]
- 55. Modeling Tumor Microenvironments In Vitro - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4023667/]
- 56. Modelling the complex nature of the tumor microenvironment [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-00997-9]
- 57. 3D cell culture Market is Projected to Increase at a CAGR ... [https://www.einpresswire.com/article/868865709/3d-cell-culture-market-is-projected-to-increase-at-a-cagr-of-23-4-through-2025-2032-says-coherent-market-insights]
- 58. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 59. Reproducible extracellular matrices for tumor organoid culture [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06349-x]
- 60. Scaffold-based 3D cell culture models in cancer research [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-00994-y]
- 61. A Patient-Derived Scaffold-Based 3D Culture Platform for ... [https://pubmed.ncbi.nlm.nih.gov/41090771/]
- 62. Comparative analysis of 3D-culture techniques for ... [https://www.nature.com/articles/s41598-025-13588-x]
- 63. Decellularization in Tissue Engineering and Regenerative ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.805299/full]
- 64. Decellularized extracellular matrix biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10622743/]
- 65. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11166402/]
- 66. Comparative Analysis of Decellularization Methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11276046/]
- 67. Evaluation of Different Decellularization Protocols for ... [https://www.mdpi.com/2227-9059/12/6/1190]
- 68. A New Method for Preparation of Decellularized Human ... [https://www.mdpi.com/1467-3045/47/4/275]
- 69. – Cell mechanotransduction in extracellular | Nature... matrix 3 D [https://www.nature.com/articles/s41580-023-00583-1?error=cookies_not_supported]
- 70. Dynamic hydrogel mechanics in organoid engineering [https://www.sciencedirect.com/science/article/pii/S2452199X2500427X]
- 71. A Practical Guide to Hydrogels for Cell Culture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5800304/]
- 72. Hydrogel Microspheres as Versatile Platforms for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508632/]
- 73. Distinct niches within the extracellular dictate fibroblast... matrix [https://pubmed.ncbi.nlm.nih.gov/29345200/]
- 74. 3D Cell Culture Market Size, Share & Growth 2025 to 2035 [https://www.futuremarketinsights.com/reports/3d-cell-culture-market]
- 75. Quantitative and organisational changes in mature extracellular ... [https://www.nature.com/articles/s41598-017-10298-x?error=cookies_not_supported&code=7f002483-6dac-4992-8a22-ab7d18146629]
- 76. - High Assay for the Identification of... Throughput Screening [https://cris.maastrichtuniversity.nl/en/publications/high-throughput-screening-assay-for-the-identification-of-compoun]
- 77. New approach methodologies for in vitro toxicity screening of... [https://pubmed.ncbi.nlm.nih.gov/40597321/]
- 78. Tissue matrix arrays for high throughput screening and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4666781/]
- 79. A high-throughput microphysiological system to quantify ... [https://pubmed.ncbi.nlm.nih.gov/40754287/]
- 80. 3D cell cultures toward quantitative high-throughput drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0165614722000797]
- 81. A quantitative meta-analysis comparing cell models in ... [https://www.nature.com/articles/s41598-023-35043-5]
- 82. Mimicking the Complexity of Solid Tumors: How Spheroids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11987746/]
- 83. 3D vs 2D Cell Culture: Which Model Suits Your Lab in 2025? [https://www.pharmanow.live/knowledge-hub/research/3d-vs-2d-cell-culture-comparison]
- 84. Quantitative analysis of tumour spheroid structure - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8741212/]
- 85. Organoids and Spheroids Market Trends 2025-2034 [https://www.gminsights.com/industry-analysis/organoids-and-spheroids-market]
- 86. SpheroidSync as edge cutting transfer strategy for uniform ... [https://www.nature.com/articles/s41598-025-25202-1]
- 87. Facile Tumor Spheroids Formation in Large Quantity with ... [https://www.nature.com/articles/s41598-018-25203-3]
- 88. Vascularization Strategies in 3D Cell Culture Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC9737506/]
- 89. Scaffold internal network bioprinting for vascularized tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S1359836825002938]
- 90. Three-Dimensional Cell Cultures in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5448717/]
- 91. 3D Cell Culture Methods and Applications [https://elveflow.com/microfluidic-reviews/3d-cell-culture-methods-and-applications-a-short-review/]
- 92. 3D Tissue Models: Mimicking the Extracellular Matrix [https://mimetas.com/resources/extracellular-matrix-3d-tissue-models]
- 93. Magnetic 3D Bioprinting and the Applications of 3D Cell Culture [https://focus.gbo.com/blog/3d/magnetic-3d-bioprinting-to-create-3d-cell-culture]
- 94. Comparative analysis between 2D and 3D colorectal ... [https://www.nature.com/articles/s41598-023-45144-w]
- 95. Assessing drug uptake and response differences in 2D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358159/]
- 96. Comparison of two-dimensional and three- ... [https://www.sciencedirect.com/science/article/pii/S2405580824002024]
- 97. Matrix composition and glucose availability cooperatively ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628585/]
- 98. Development, Functional Characterization, and Matrix ... [https://www.mdpi.com/2073-4409/14/17/1351]
- 99. 3D tumor cultures for drug resistance and screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927140/]
- 100. Oncogenic effects of ECM remodeling in obesity and breast ... [https://www.nature.com/articles/s41388-025-03521-x]
- 101. A 3D spheroid model for assessing nanocarrier-based ... [https://www.nature.com/articles/s44385-025-00041-x]
- 102. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 103. Extracellular matrix and its therapeutic potential for cancer ... [https://www.nature.com/articles/s41392-021-00544-0]
- 104. Tumor extracellular matrix enhances invasive gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307645/]
- 105. Human-Centric 3D Models: The NIH and FDA Push [https://insphero.com/human-centric-drug-testing/]
- 106. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 107. Recent advances in AI-based toxicity prediction for drug ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1632046/full]