What Causes Cell Culture Contamination? A Complete Guide to Sources, Prevention, and Control
Cell culture contamination is a critical challenge that compromises experimental integrity, data reproducibility, and patient safety in biopharmaceutical production.
What Causes Cell Culture Contamination? A Complete Guide to Sources, Prevention, and Control
Abstract
Cell culture contamination is a critical challenge that compromises experimental integrity, data reproducibility, and patient safety in biopharmaceutical production. This comprehensive article explores the multifaceted causes of contamination, from common biological agents like bacteria, mycoplasma, and fungi to chemical contaminants and cross-contamination. Tailored for researchers, scientists, and drug development professionals, it provides actionable methodologies for detection, robust troubleshooting and optimization strategies for prevention, and validation frameworks to ensure culture purity and regulatory compliance across both research and Good Manufacturing Practice (GMP) environments.
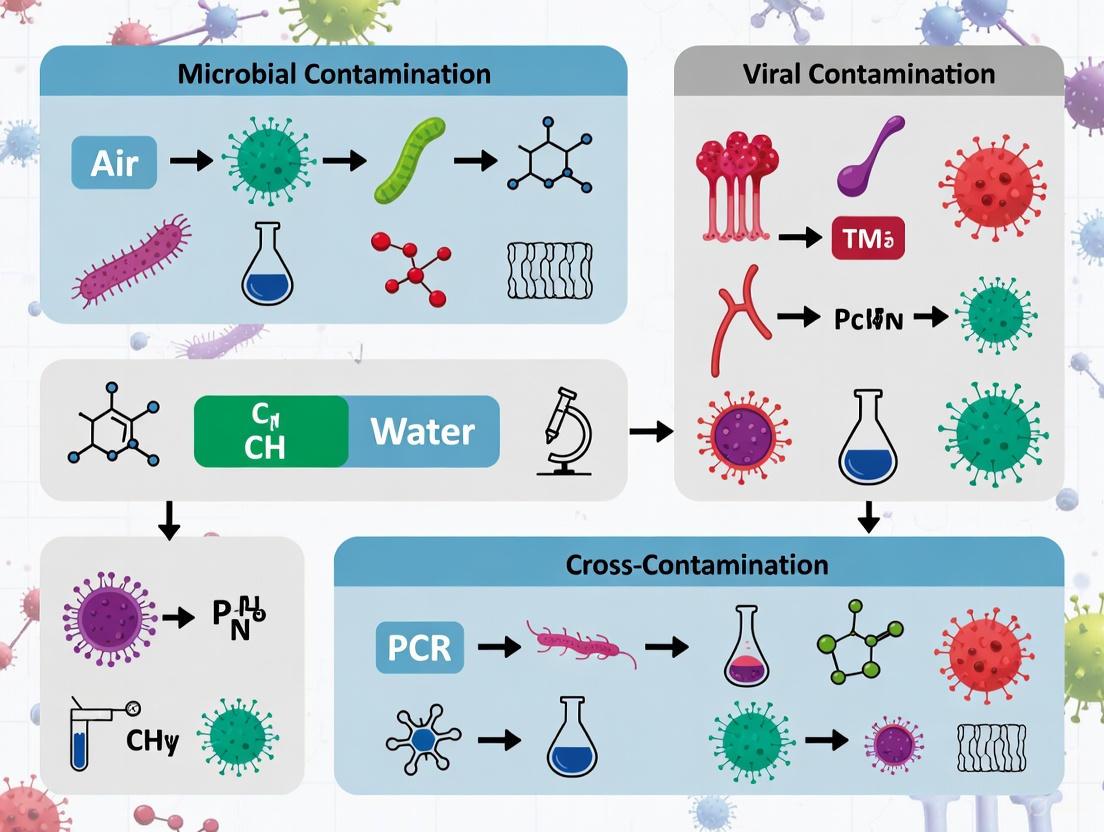
Unseen Enemies: Understanding the Spectrum of Cell Culture Contaminants
Biological contamination represents one of the most persistent and costly challenges in cellular and molecular biology research, particularly in pharmaceutical preclinical studies and biotechnological production. Microbial contaminants—including bacteria, fungi, yeast, and mold—can compromise experimental integrity, lead to irreproducible results, and jeopardize patient safety in drug development pipelines. These contaminants compete with cultured cells for nutrients, alter their microenvironment, and can introduce confounding variables that invalidate research findings. The cultivation of cells in an artificial environment removes the protective mechanisms of the immune system, leaving them vulnerable to microorganisms that are ubiquitous in laboratory settings. Consequently, understanding the sources, characteristics, and control mechanisms for these biological contaminants is fundamental to maintaining the sterility and quality assurance required for rigorous scientific research.
Within the broader context of cell culture contamination research, biological contaminants represent the most frequent and disruptive category, with estimates suggesting that problematic cell lines have contributed to approximately 16.1% of published literature [1]. The economic implications are substantial, as a single contamination event can compromise months of work and valuable reagents. More importantly, certain contaminants like mycoplasma can remain undetected while subtly interfering with cellular processes, potentially leading to false conclusions in basic research and dangerous outcomes in translational applications. This whitepaper provides an in-depth technical examination of the primary biological contaminants, their identification, experimental protocols for detection and eradication, and emerging technologies that promise to revolutionize contamination monitoring in cell culture systems.
Characteristics of Major Biological Contaminants
Biological contaminants in cell culture vary significantly in their physical characteristics, growth requirements, and effects on cultured cells. Accurate identification is crucial for implementing appropriate eradication protocols and preventing future contamination events. The most prevalent contaminants include diverse bacteria, fungi (encompassing both yeasts and molds), and mycoplasma, each with distinct morphological features and impacts on cell culture systems.
Bacterial Contamination
Bacterial contamination represents one of the most common and rapidly destructive sources of experimental compromise in cell culture laboratories. Bacteria can enter cultures through unclean surfaces, contaminated reagents, insufficiently sterilized labware, or breaches in aseptic technique. The effects are typically fast and readily noticeable to a trained eye. Under microscopic examination, bacterial contaminants appear as small (approximately 1–5 µm), motile particles that often exhibit a "quicksand-like" movement between cultured cells [2] [3]. Culture medium often turns yellowish due to a rapid drop in pH resulting from bacterial metabolic activity, and the medium may appear cloudy or turbid when contamination becomes advanced. In some cases, an unpleasant or sour odor may be detectable upon opening contaminated culture vessels [3]. Bacterial contaminants can be broadly categorized by shape—spherical (cocci), rod-shaped (bacilli), or spiral—with each type potentially introducing different challenges for eradication.
Fungal Contamination: Yeasts and Molds
Fungal contamination encompasses both yeast and filamentous molds, which pose distinct challenges in cell culture systems. These eukaryotic contaminants grow more slowly than bacteria but still significantly faster than most mammalian cell cultures, making them persistent and aggressive once established.
Yeast Contamination: Yeasts are unicellular fungi characterized by round or oval morphology, with visible budding into smaller particles observed during microscopic examination. Initially, the culture medium may remain clear, but it typically turns yellowish over time as yeast metabolic activity affects pH [2]. Yeast contamination often originates from airborne spores, poorly maintained equipment, or contaminated reagents, and can be particularly problematic due to its resilience in laboratory environments.
Mold Contamination: Filamentous molds present as multicellular structures with characteristic thread-like hyphae that form visible networks in culture. Under microscopic examination, these thin, filamentous structures may develop dense spore clusters, while the culture medium may initially appear unchanged before becoming cloudy or developing fuzzy appearances at advanced stages [2]. Mold spores are ubiquitous in laboratory environments and can survive on surfaces or in the air for extended periods, making them particularly difficult to eradicate once established in a cell culture facility.
Mycoplasma Contamination
Mycoplasma species represent a particularly insidious category of biological contaminants due to their small size (approximately 0.3 µm) and lack of a cell wall [3]. These characteristics make them resistant to many standard antibiotics that target cell wall synthesis and allow them to pass through typical filters used for sterilization. Unlike other contaminants, mycoplasma does not cause visible turbidity or produce noticeable odor, allowing it to slip past routine visual checks [2] [3]. Under microscopic examination, mycoplasma may appear as tiny black dots, but cultures typically exhibit secondary indicators such as slow cell growth, abnormal morphology, reduced transfection efficiency, and unexplained changes in metabolic activity [2]. The real damage lies in its subtle interference with cellular processes—mycoplasma can alter DNA, inhibit cell division, or modify cytokine production, often without researchers realizing it until experimental data becomes inconsistent or irreproducible.
Table 1: Characteristics of Major Biological Contaminants in Cell Culture
| Contaminant Type | Size Range | Visual Culture Indicators | Microscopic Morphology | Growth Rate |
|---|---|---|---|---|
| Bacteria | 1–5 µm | Yellowish, cloudy medium; possible odor | Spherical, rod-shaped, or spiral; motile particles | Rapid (hours) |
| Yeast | 3–10 µm | Initially clear, turns yellow over time | Round or oval cells, sometimes budding | Moderate (days) |
| Mold | Hyphae: 2–10 µm width | Initially unchanged, later cloudy or fuzzy | Thin, thread-like hyphae; dense spore clusters | Slow to moderate (days) |
| Mycoplasma | ~0.3 µm | No color change; no cloudiness | Tiny black dots; abnormal cell morphology | Slow (weeks) |
Detection and Identification Methodologies
Effective contamination control begins with reliable detection and identification methods. The optimal approach varies depending on the suspected contaminant type, available resources, and required sensitivity. The following experimental protocols represent current best practices for identifying biological contaminants in cell culture systems.
Microscopic Analysis
Direct microscopic observation serves as the first line of defense for detecting contamination in cell cultures. Regular inspection of cultures under phase-contrast microscopy should be incorporated into standard cell culture maintenance protocols.
Protocol:
- Sample Collection: Aseptically remove a small volume of cell culture medium from the vessel.
- Microscopic Examination: Observe under 100× to 400× magnification using phase-contrast microscopy.
- Bacterial Identification: Look for small, motile particles between cells exhibiting "quicksand-like" movement [2].
- Yeast Identification: Identify round or oval cells, typically 3–10 µm in diameter, with occasional budding structures [2].
- Mold Identification: Detect thin, thread-like hyphae that may form network structures; look for dense spore clusters in advanced contamination [2].
- Mycoplasma Indicators: While individual mycoplasma organisms are near the resolution limit of light microscopy, look for tiny black dots and secondary signs like granularity in the cytoplasm or abnormal cell morphology [2].
For enhanced visualization of contaminants, staining techniques such as Gram staining (for bacteria) or DNA-binding dyes like Hoechst 33258 (for mycoplasma) can be employed to improve contrast and specificity.
Culture-Based Detection Methods
Culture-based methods provide confirmatory evidence of contamination and are particularly valuable for identifying specific microbial species.
Protocol for Broth Culture Detection:
- Sample Preparation: Aseptically collect 1–2 mL of potentially contaminated cell culture supernatant.
- Inoculation: Transfer 0.5 mL of supernatant into sterile nutrient broth (for bacteria) or Sabouraud dextrose broth (for fungi).
- Incubation: Incubate inoculated broths at 37°C (for mammalian culture contaminants) and 25–30°C (for environmental fungi) for 24–72 hours.
- Assessment: Observe broths daily for turbidity (bacteria) or surface growth (fungi), which indicates positive contamination.
- Subculturing: For identification, streak positive broths onto appropriate agar plates (blood agar for bacteria, Sabouraud dextrose agar for fungi) to obtain isolated colonies.
- Analysis: Examine colony morphology, perform Gram staining, and conduct biochemical tests as needed for species identification.
Molecular Detection Methods
Molecular techniques offer superior sensitivity and specificity for detecting contaminants, particularly for challenging organisms like mycoplasma.
PCR Protocol for Mycoplasma Detection:
- DNA Extraction: Extract genomic DNA from 1–2 mL of cell culture supernatant using commercial DNA extraction kits according to manufacturer instructions.
- Primer Design: Use primers targeting conserved mycoplasma genes (e.g., 16S rRNA gene). Common sequences include:
- Forward: 5'-ACACCATGGGAGCTGGTAAT-3'
- Reverse: 5'-CTTCWTCGACTTYCAGACCCAAGGCAT-3'
- PCR Reaction Setup:
- Template DNA: 2–5 µL
- Primer mix (10 µM each): 1 µL
- PCR master mix: 12.5 µL
- Nuclease-free water to 25 µL total volume
- Amplification Parameters:
- Initial denaturation: 95°C for 5 minutes
- 35 cycles of: 95°C for 30 seconds, 55°C for 30 seconds, 72°C for 45 seconds
- Final extension: 72°C for 7 minutes
- Analysis: Separate PCR products by gel electrophoresis (1.5–2% agarose); positive detection indicated by bands of expected size (approximately 500 bp for many mycoplasma species).
Commercial mycoplasma detection kits are available that provide optimized protocols and reagents, such as the MycAway Plus Color One-Step Mycoplasma Detection Kit, which can provide results in approximately 30 minutes [2].
Emerging Detection Technologies
Advanced detection methodologies are revolutionizing contamination monitoring by enabling earlier identification through innovative approaches.
Volatile Organic Compound (VOC) Analysis: Emerging technologies utilize gas chromatography with ion mobility spectrometry (GC-IMS) to detect volatile organic compounds released by contaminating microorganisms [4]. This approach can detect as low as 10 colony-forming units (CFU) of various bacteria and mold species within just two hours post-inoculation, and mycoplasma contamination within 24 hours [4]. The methodology involves:
- Headspace Sampling: Collecting gas samples from the headspace of culture vessels.
- GC-IMS Analysis: Separating and detecting VOC profiles characteristic of specific contaminants.
- Pattern Recognition: Using machine learning algorithms to identify contamination-specific VOC signatures.
Real-Time Sensor Monitoring: Semiconductor-based sensors for total volatile organic compounds (TVOC), ammonia, and hydrogen sulfide can be implemented for real-time monitoring directly inside cell culture incubators [5]. This approach demonstrated potential for detecting bacterial contamination within a 2-hour window from onset, providing continuous sterility assurance during culture development [5].
Table 2: Detection Methods for Biological Contaminants
| Detection Method | Target Contaminants | Time to Result | Sensitivity | Special Requirements |
|---|---|---|---|---|
| Direct Microscopy | Bacteria, yeast, mold | Immediate | Low to moderate | Phase-contrast microscope |
| Culture Methods | Bacteria, fungi | 24–72 hours | Moderate | Culture media, incubators |
| PCR-Based Detection | Mycoplasma, specific bacteria | 2–4 hours | High (≤10 CFU) | Thermal cycler, specific primers |
| VOC Analysis (GC-IMS) | Bacteria, mold, mycoplasma | 20 minutes–24 hours | High (10 CFU) | Specialized instrumentation |
| Fluorescence Staining | Mycoplasma, bacteria | 1–2 hours | Moderate | Fluorescence microscope |
| ELISA | Specific pathogens | 3–5 hours | Moderate | Specific antibodies |
Eradication and Management Protocols
Once contamination is identified, appropriate response protocols are essential to minimize impact and prevent spread. The optimal approach depends on the contaminant type, value of the affected cells, and facility resources.
Bacterial Contamination Management
For Mild Bacterial Contamination:
- Washing: Gently wash cell monolayer with sterile phosphate-buffered saline (PBS) to remove loose bacteria [2].
- Antibiotic Treatment: Replace medium with fresh culture medium containing 10× penicillin/streptomycin combination [2].
- Monitoring: Observe cultures closely for 24–48 hours for signs of continued contamination.
- Passaging: If contamination appears controlled, passage cells and return to standard antibiotic-free media or maintenance-level antibiotics.
For Heavy Bacterial Contamination:
- Containment: Immediately seal contaminated vessels to prevent aerosolization.
- Disposal: Autoclave contaminated cultures before disposal.
- Decontamination: Thoroughly disinfect incubator surfaces, work areas, and water baths with appropriate sporicidal agents [2].
- Equipment Testing: Check and service biological safety cabinets to ensure proper function.
Fungal Contamination Management
Yeast Contamination:
- Recommended Approach: Discard contaminated cultures immediately—this is typically the safest option [2].
- Potential Rescue Protocol (for valuable cultures only):
- Wash cells repeatedly with sterile PBS [2].
- Replace with fresh media containing 300 µg/mL fluconazole or amphotericin B [2].
- Note that amphotericin B is toxic to mammalian cells at effective antifungal concentrations.
- If contamination is controlled after 2–3 days, reduce antifungal concentration to 150 µg/mL for maintenance through 2–3 passages [2].
Mold Contamination:
- Immediate Discarding: Discard contaminated cells immediately due to spore formation risk [2].
- Incubator Decontamination:
- Preventive Measures: Add copper sulfate to the incubator water pan to discourage future fungal growth [2].
- Environmental Monitoring: Check HEPA filters in biological safety cabinets and culture room air handling systems.
Mycoplasma Eradication
Mycoplasma contamination presents unique challenges due to its resistance to common antibiotics and intracellular localization in some cases.
Antibiotic Treatment Protocol:
- Product Selection: Use commercial mycoplasma removal agents such as MycAway Solution for Cultured Cells [2].
- Treatment Duration: Typically requires 1–2 weeks of continuous exposure.
- Monitoring: Confirm eradication using PCR or DNA staining methods at least one week post-treatment.
- Quarantine: Maintain treated cells in quarantine with regular testing for at least one month.
Alternative Approaches:
- Passage in Mice: For hybridomas and some primary cells, passage in nude mice can eliminate mycoplasma contamination.
- Antibiotic Combinations:
- Use combinations of tetracycline, quinolones, or macrolides specifically formulated for mycoplasma eradication.
- Be aware that some agents may have cytostatic effects on mammalian cells.
The following diagram illustrates the decision-making workflow for contamination identification and management:
Prevention Strategies and Best Practices
Preventing contamination requires a systematic approach addressing multiple potential introduction points throughout the cell culture workflow. The following evidence-based strategies form a comprehensive prevention framework.
Aseptic Technique Mastery
Strict aseptic technique represents the foundation of contamination prevention in cell culture laboratories.
Critical Practices:
- Personal Protective Equipment: Always wear appropriate gloves, lab coats, and sleeves to establish a barrier between the technologist and the culture environment [2] [6].
- Proper Hood Usage: Work within a certified biological safety cabinet with verified HEPA filtration, maintaining proper airflow by not blocking air inlets or outlets [6].
- Surface Decontamination: Thoroughly disinfect all work surfaces with 70% ethanol or 70% industrial methylated spirits (IMS) before and after each procedure [6].
- Reagent Handling: Use sterile pipette tips, flasks, and reagents from trusted suppliers; filter-sterilize media through 0.2 µm membranes when appropriate [3] [6].
- Movement Minimization: Avoid unnecessary movements and talking in the hood to reduce air turbulence and potential contaminant introduction [2].
Environmental Control
Maintaining a controlled laboratory environment is essential for preventing contamination, particularly from airborne sources like mold spores.
Incubator Management:
- Regular Cleaning: Decontaminate CO₂ incubators weekly—including shelves, door gaskets, and water trays—using appropriate disinfectants [6].
- Water Pan Maintenance: Replace water in incubator water pans regularly and consider adding copper sulfate or other antifungal agents to discourage microbial growth [2].
- Temperature and Humidity Monitoring: Regularly calibrate and monitor incubator conditions to ensure stability.
- Segregation: Designate separate incubators for quarantined cultures, time-lapse imaging experiments, or other higher-risk applications [6].
Laboratory Design Considerations:
- Air Quality: Ensure proper HEPA filtration in cell culture rooms and biological safety cabinets.
- Traffic Patterns: Establish unidirectional workflow patterns from "clean" to "dirty" areas.
- Surface Materials: Use non-porous, easily cleanable surfaces for benches and equipment.
Quality Control Implementation
Systematic quality control procedures provide early detection of potential contamination issues before they compromise entire experiments.
Cell Line Management:
- Quarantine Protocol: Isolate and test all new cell lines for mycoplasma and other contaminants before integrating them into main culture areas [2] [3].
- Authentication: Perform regular cell line authentication using STR profiling or other methods to detect cross-contamination [1] [3].
- Cryopreservation: Maintain early-passage master stocks to preserve valuable lines against future contamination events.
- Documentation: Implement comprehensive labeling practices including cell line name, passage number, and date to facilitate traceability [6].
Reagent Quality Assurance:
- Supplier Qualification: Source media, serum, and supplements from reliable, tested suppliers with appropriate quality certifications [2].
- Aliquoting: Divide reagents into smaller working volumes to avoid repeated freeze-thaw cycles and limit cross-contamination potential [2].
- Expiration Monitoring: Implement first-in-first-out (FIFO) inventory systems and regularly check expiration dates.
- Sterility Testing: Periodically test media and supplements for microbial contamination, particularly for long-term experiments.
The following diagram illustrates the systematic approach to contamination prevention:
The Scientist's Toolkit: Essential Reagents and Materials
Effective contamination control requires specific reagents, equipment, and materials designed to prevent, detect, and eradicate biological contaminants. The following table details key solutions used in contamination management.
Table 3: Research Reagent Solutions for Contamination Management
| Reagent/Material | Primary Function | Application Protocol | Technical Considerations |
|---|---|---|---|
| Penicillin/Streptomycin Solution | Bacterial prophylaxis and treatment | Add 1× concentration for prevention; 10× for eradication | Can mask low-level contamination; promotes antibiotic resistance with prolonged use [3] |
| Amphotericin B | Antifungal agent targeting yeasts and molds | Use at 2.5–5 µg/mL for prevention; higher concentrations (toxic to cells) for eradication | Cytotoxic to mammalian cells at concentrations needed for mold eradication [2] |
| Mycoplasma Removal Agents | Specific eradication of mycoplasma contamination | Continuous treatment for 1–2 weeks followed by confirmation testing | Multiple mechanisms of action including protein synthesis inhibition and DNA gyrase targeting [2] |
| Copper Sulfate | Fungistatic agent for incubator water pans | Add to incubator water reservoir at manufacturer-recommended concentration | Prevents fungal growth in humidified incubators without affecting cell growth [2] |
| 70% Ethanol | Surface decontamination | Spray and wipe all surfaces, gloves, and equipment entering biological safety cabinet | More effective than higher concentrations due to optimized penetration [6] |
| Mycoplasma Detection Kits | Rapid detection of mycoplasma contamination | PCR, enzymatic, or DNA staining protocols per manufacturer instructions | Some kits provide results in 30 minutes versus days for culture methods [2] |
| Benzalkonium Chloride | Strong disinfectant for equipment decontamination | Use for surface decontamination after mold contamination incidents | Effective against fungal spores; requires careful rinsing if used on culture equipment [2] |
| Filter Tips | Prevention of aerosol cross-contamination | Use for all liquid handling in cell culture procedures | Essential when working with multiple cell lines; prevents pipettor contamination [6] |
Emerging Technologies and Future Directions
The field of contamination control is rapidly evolving with advanced detection technologies and automated systems that promise to revolutionize cell culture practices.
Advanced Detection Platforms
Volatile Organic Compound (VOC) Analysis: Gas chromatography with ion mobility spectrometry (GC-IMS) represents a breakthrough in rapid contamination detection. This technology can identify bacterial contamination within 2 hours of onset and mycoplasma within 24 hours post-inoculation by analyzing signature volatile compounds [4]. The system requires minimal training, has a small laboratory footprint, and provides results in approximately 20 minutes per sample, making it ideal for integration into biomanufacturing workflows [4].
Real-Time Sensor Arrays: Semiconductor-based sensors for total volatile organic compounds (TVOC), ammonia, and hydrogen sulfide enable continuous, real-time monitoring directly within cell culture incubators [5]. Early research demonstrates the potential of TVOC sensors specifically for detecting bacterial contamination within a 2-hour window, paving the way for fully automated, non-invasive sterility assurance systems [5]. These systems could ultimately support scalability and efficiency in drug development processes without requiring human intervention for contamination monitoring.
Automated Cell Culture Systems
Automated cell culture platforms integrate multiple contamination control strategies, including:
- Closed Systems: Minimizing exposure to non-sterile environments through robotic handling in enclosed chambers.
- Continuous Monitoring: Implementing in-line sensors for real-time culture assessment.
- Algorithmic Detection: Using machine learning to identify subtle patterns indicative of early contamination.
These systems substantially reduce human-dependent variables in cell culture, potentially decreasing contamination frequency while improving reproducibility and standardization across laboratories.
Advanced Materials and Engineering Solutions
Innovative materials science approaches are contributing to contamination prevention through:
- Antimicrobial Surfaces: Incorporating copper alloys or antimicrobial polymers into incubator interiors and culture vessels.
- Smart Filtration: Developing self-sterilizing HEPA filters with photocatalytic coatings.
- Single-Use Systems: Implementing completely disposable bioreactor systems that eliminate cleaning validation and cross-contamination risks between runs.
These technological advances, combined with rigorous adherence to fundamental aseptic techniques, promise to significantly reduce the impact of biological contaminants on cell culture research and biomanufacturing in the coming years.
Mycoplasma contamination represents one of the most significant yet frequently overlooked challenges in cell culture laboratories worldwide. These minute bacteria, which lack a cell wall, surreptitiously infect cell cultures without obvious visual detection, primarily parasitizing cell surfaces and interfering with host cell functions [7]. With over 190 known species, only about 20 species of human, bovine, and porcine origin have been identified in cell culture, with eight particular species accounting for approximately 95% of all contamination incidents [8]. The sheer prevalence of this issue is staggering, with estimates suggesting that 15-35% of continuous cell cultures and at least 1% of primary cell cultures experience mycoplasma contamination [8]. The problem is particularly insidious because mycoplasma contamination often goes undetected while significantly altering cellular physiology, potentially compromising years of research and endangering the development of biopharmaceutical products [9] [10].
Within the broader context of cell culture contamination research, mycoplasma presents unique challenges that distinguish it from other contaminants. Unlike bacterial or fungal contamination, which often cause turbidity in media or noticeable pH shifts, mycoplasma contamination frequently escapes detection under standard light microscopy due to its small size (less than 300 nm) and does not cause media cloudiness [11] [12]. This stealthy nature, combined with its ability to profoundly influence virtually all aspects of cell physiology, establishes mycoplasma as a particularly dangerous "silent threat" that demands specialized detection methods and rigorous containment strategies [10] [8].
Biological Characteristics and Contamination Mechanisms
Unique Biological Features of Mycoplasma
Mycoplasma species belong to the class Mollicutes, representing the smallest self-replicating organisms known to date [12]. Their diminutive size, typically measuring less than 300 nanometers, allows them to readily pass through standard sterilizing filters with pore sizes of 0.45 μm, facilitating their unintended introduction into cell culture systems [12]. The most distinctive feature of mycoplasma is their complete lack of a cell wall, which renders them naturally resistant to common antibiotics that target cell wall synthesis, such as penicillin and its derivatives [8]. Instead, they are bounded only by a triple-layered cell membrane containing cholesterol, a characteristic more typical of eukaryotic cells than bacteria [8].
Mycoplasma possess extremely simplified genomes, which represent among the smallest of all free-living organisms [12]. This genomic reduction has resulted in limited metabolic capabilities, forcing them to become nutritional dependents on their host cells for survival [12]. Mycoplasma lack the genetic machinery to synthesize many essential nutrients and must therefore scavenge these compounds from their environment, primarily from the cell culture media and the host cells they infect [12]. This fundamental biological constraint explains their parasitic behavior in cell culture systems and their profound impact on host cell physiology.
While numerous mycoplasma species exist, only a limited subset commonly contaminates cell cultures. The eight species that account for the majority of contamination incidents include M. arginini (bovine), M. fermentans (human), M. hominis (human), M. hyorhinis (porcine), M. orale (human), M. pirum (human), M. salivarium (human), and Acholeplasma laidlawii (bovine) [8]. The species distribution of contaminants reflects common laboratory practices, with human-sourced species typically introduced through laboratory personnel and bovine-species often originating from contaminated serum supplements [8].
The primary sources and introduction routes of mycoplasma contamination in cell culture laboratories include:
- Human operators: Improper aseptic technique can transfer mycoplasma present on skin, clothing, or from airborne particles into cell cultures [12].
- Contaminated reagents: Animal sera, particularly fetal bovine serum, cell media, and other reagents can serve as contamination sources if not properly tested [8] [12].
- Cross-contamination: Already infected cell cultures can spread mycoplasma to clean cultures via shared equipment, media, or laboratory spaces [8].
- Laboratory equipment: Faulty laminar flow cabinets can disperse mycoplasma-containing dust and aerosols throughout the workspace [8].
Table 1: Major Mycoplasma Species in Cell Culture Contamination
| Species | Origin | Prevalence | Notable Characteristics |
|---|---|---|---|
| M. arginini | Bovine | High | Common in fetal bovine serum |
| M. fermentans | Human | Moderate | Can affect multiple cell functions |
| M. hominis | Human | High | Frequent human carrier |
| M. hyorhinis | Porcine | Moderate | Common in porcine-derived materials |
| M. orale | Human | High | Prevalent in human oral flora |
| M. pirum | Human | Low | Less common but impactful |
| M. salivarium | Human | Moderate | Human oral and respiratory tract |
| A. laidlawii | Bovine | High | Common serum contaminant |
Detection Methodologies: Challenges and Advanced Approaches
Limitations of Conventional Detection Methods
Traditional methods for mycoplasma detection have significant limitations that can compromise their reliability. Direct culture methods, which involve inoculating agar plates with the test culture and incubating for four to five weeks to observe characteristic "fried egg" colonies, though considered a gold standard, are prohibitively time-consuming for routine testing [8]. DNA staining techniques using fluorescent dyes like Hoechst 33258 have been widely used but often yield equivocal results, primarily detecting only heavily contaminated cultures [7]. A critical limitation of conventional DNA staining is interference from host cell DNA; degraded DNA from host cells can produce small fluorescent spots under microscopy that mimic mycoplasma, leading to false positives or difficulties in interpretation [7].
The inherent challenges with these conventional approaches have driven the development of more sophisticated detection methodologies. As noted in recent research, "Cellular DNA interferes with the results of mycoplasma elimination when using DNA staining alone," highlighting the need for more specific detection strategies [7]. Furthermore, the silent nature of mycoplasma contamination means that visible signs often appear only after significant physiological damage has occurred to the cell culture, emphasizing the need for proactive, sensitive detection methods [11].
Advanced Detection Strategies
Colocalization Approach: DNA and Membrane Staining
A novel methodological advancement addresses the limitations of standalone DNA staining by combining DNA and cell membrane fluorescent dyes. This approach leverages colocalization analysis to accurately distinguish mycoplasma contamination from background cellular DNA. The technique involves staining cells with a combination of Hoechst (DNA dye) and WGA (wheat germ agglutinin, a membrane dye), then determining mycoplasma contamination by its specific colocalization with the plasma membrane surface [7].
The key advantage of this method is its ability to differentiate true mycoplasma contamination, which localizes to the cell membrane, from cytoplasmic DNA components that can cause false positives in conventional staining [7]. Research has demonstrated that this approach "minimized interference from cytoplasmic DNA components and greatly improved the accuracy of using DNA staining alone for mycoplasma detection" [7]. This colocalization method provides a rapid, direct screening technique that facilitates early diagnosis and treatment of contaminated cultures.
PCR-Based Detection Methods
Molecular methods based on polymerase chain reaction (PCR) technology have emerged as the most reliable and efficient approach for mycoplasma detection. Modern PCR-based kits can detect over 60 species of mycoplasma, including the most common contaminants, with high sensitivity and specificity [9] [13]. These methods typically target the 16S rRNA gene in the mycoplasma genome, using universal PCR primers and specialized protocols to increase sensitivity [8] [13].
The significant advantages of PCR-based methods include:
- Rapid results: Time-to-results as short as 3 hours, compared to weeks for culture methods [13].
- High sensitivity: Detection limits of less than 10 CFU/ml for all mycoplasma species [13].
- Comprehensive coverage: Ability to detect a wide range of mycoplasma species in a single test [9].
- Regulatory compliance: Meets standards of European Pharmacopeia 2.6.7, USP <1071>, and JP G3 guidelines [8] [13].
Table 2: Comparison of Mycoplasma Detection Methods
| Method | Principle | Time to Result | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|---|
| Direct Culture | Growth on specialized agar | 4-5 weeks | High (theoretical gold standard) | Definitive identification | Extremely slow, specialized media required |
| DNA Staining | Fluorescent dye binding to DNA | 1-2 days | Low to moderate | Simple, inexpensive | Subjective, false positives from host DNA |
| Colocalization | Membrane and DNA dye combination | 1-2 days | Moderate to high | Reduces false positives, specific localization | Requires specialized analysis |
| PCR-Based | Amplification of mycoplasma-specific DNA sequences | 3 hours to 1 day | High (<10 CFU/ml) | Fast, sensitive, specific, comprehensive | Requires specialized equipment and expertise |
Experimental Protocol: Colocalization Method for Mycoplasma Detection
Principle: This protocol utilizes colocalization of DNA staining (Hoechst) and membrane staining (WGA) to accurately identify mycoplasma contamination localized to the host cell membrane, effectively mitigating false positives caused by cytoplasmic DNA [7].
Materials:
- Cell cultures (test and negative control)
- Hoechst 33258 or similar DNA-binding fluorescent dye
- WGA (wheat germ agglutinin) conjugated to a fluorescent marker with emission spectrum distinct from Hoechst
- Phosphate-buffered saline (PBS)
- Fixative (e.g., 4% paraformaldehyde)
- Permeabilization buffer (e.g., 0.1% Triton X-100 in PBS)
- Mounting medium
- Fluorescence microscope with appropriate filter sets and colocalization analysis software
Procedure:
- Culture cells on appropriate sterile glass coverslips in cell culture plates until approximately 60-70% confluence.
- Aspirate culture medium and wash cells gently with pre-warmed PBS.
- Fix cells with 4% paraformaldehyde in PBS for 15 minutes at room temperature.
- Wash fixed cells three times with PBS, 5 minutes per wash.
- Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes.
- Prepare staining solution containing both Hoechst (at manufacturer's recommended concentration) and WGA conjugate.
- Incubate cells with staining solution for 30-60 minutes at room temperature protected from light.
- Wash stained cells three times with PBS, 5 minutes per wash.
- Mount coverslips on glass slides using appropriate mounting medium.
- Visualize using fluorescence microscopy with appropriate filter sets for each dye.
- Capture images of the same field under both fluorescence channels.
- Analyze images for colocalization of DNA signal (Hoechst) with membrane signal (WGA) at the cell surface.
Interpretation: Positive mycoplasma contamination is indicated by fluorescent DNA signal that colocalizes with the membrane stain at the cell surface. Cytoplasmic or nuclear DNA without membrane association suggests absence of mycoplasma or non-specific staining.
Impact of Mycoplasma Contamination on Cellular Functions
Comprehensive Physiological Disruption
Mycoplasma contamination exerts profound effects on virtually all aspects of cellular physiology, potentially compromising experimental results and leading to erroneous conclusions. The mechanisms underlying these disruptions stem from the parasitic relationship mycoplasma establishes with host cells, competing for essential nutrients and directly interacting with cellular components [8] [12]. The primary physiological impacts include:
Metabolic interference: Mycoplasma consume essential nutrients from the culture medium, including amino acids, fatty acids, sugars, nucleic acid precursors, and choline, effectively starving host cells of these critical components [12]. This nutrient competition can lead to altered metabolic profiles and impaired cellular growth.
Genetic and epigenetic alterations: Contamination can induce chromosomal aberrations and disrupt normal nucleic acid synthesis [8]. Mycoplasma infection has been demonstrated to cause changes in gene expression profiles, potentially skewing results in transcriptomic studies and other gene expression analyses [8].
Membrane and signaling effects: The presence of mycoplasma can alter membrane antigenicity and interfere with receptor signaling pathways [8]. These changes can affect cellular communication, transport mechanisms, and response to experimental treatments.
Proliferation and viability impacts: Mycoplasma contamination frequently inhibits cell proliferation and metabolism, eventually leading to increased cell death under prolonged infection [8]. The progressive nature of these effects means that experimental results may deteriorate over time, creating inconsistencies between experiments.
Technology-specific interference: Mycoplasma infection can decrease transfection rates and adversely affect virus production in systems designed for viral vector production [8]. These technology-specific effects can undermine specialized applications and production systems.
Implications for Research and Bioprocessing
The consequences of mycoplasma-induced physiological disruptions extend throughout the research and development pipeline. In basic research, contamination can lead to misinterpretation of results, false conclusions, and irreproducible findings, potentially invalidating entire research programs [10]. One analysis noted that mycoplasma can "affect the phenotypic and functional characteristics of cells in vitro," highlighting the pervasive nature of its effects [8].
In the context of biopharmaceutical development and production, the implications are even more severe. Contamination of cell substrates used in production poses potential safety risks for patients and presents serious economic risks through batch adulteration or product recalls [9] [8]. The compromised cellular functions can alter critical quality attributes of biopharmaceutical products, affecting both efficacy and safety profiles.
Prevention and Elimination Strategies
Proactive Prevention Protocols
Preventing mycoplasma contamination requires a comprehensive approach addressing multiple potential introduction routes. Effective prevention strategies include:
Strict aseptic techniques: Proper training in aseptic techniques forms the foundation of contamination prevention. This includes maintaining uncluttered cell culture hoods, spraying items with 70% ethanol before introduction into the hood, keeping plates and bottles covered, and avoiding movements that compromise air flow [10].
Personal protective equipment (PPE): Consistently wearing proper PPE, including gloves and clean lab coats (changed at least weekly), reduces potential human-derived contamination [10] [8].
Environmental control: Regular cleaning of incubators with bleach, changing or cleaning water pans weekly, and maintaining certified vertical laminar flow hoods minimize environmental contamination risks [10] [8].
Quarantine procedures: New or previously untested cell lines should be maintained in a designated incubator separate from established cultures until confirmed mycoplasma-free through testing [10]. This practice prevents cross-contamination of valuable cell stocks.
Quality reagent sourcing: Confirming that all media, sera, and reagents come from mycoplasma-free sources safeguards cells from contamination by external materials [8]. Using sterile single-use consumables whenever possible reduces introduction risks.
Routine testing: Implementing a schedule for periodic mycoplasma testing, including testing whenever freezing new cell banks, ensures early detection of potential contamination events [10].
Elimination and Decontamination Approaches
Once mycoplasma contamination is detected, prompt action is necessary to prevent laboratory-wide spread:
Immediate quarantine: Separating contaminated cultures from vulnerable cells is the critical first step [10]. All equipment and materials exposed to the contaminated culture should be identified and properly decontaminated.
Antibiotic treatment: Specialized antibiotics effective against mycoplasma, such as Plasmocin, are typically administered at 25 μg/mL for one to two weeks [10]. Importantly, conventional antibiotics like penicillin are ineffective against mycoplasma due to their lack of a cell wall [8].
Post-treatment verification: After completing antibiotic treatment, cells must be cultured without antibiotics for one to two weeks and then re-tested to confirm elimination success [10]. This antibiotic-free period is essential as it allows low-level persistent contaminants to proliferate to detectable levels.
Decision points: If post-treatment testing remains positive, options include repeated antibiotic treatment with extended duration, trying alternative antibiotics, or discarding the culture depending on the cell line's value and persistence of contamination [10].
Comprehensive decontamination: All laboratory surfaces, incubators, and equipment exposed to the contaminated culture require thorough decontamination with appropriate sporicidal agents to prevent recurrence [11].
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Mycoplasma Detection and Prevention
| Reagent/Category | Function/Application | Examples/Specifications | Key Features |
|---|---|---|---|
| PCR Detection Kits | Rapid, sensitive detection of mycoplasma DNA | Universal Mycoplasma Detection Kit (ATCC), Venor Mycoplasma Detection (Minerva) | Detects >60 species, 3-hour protocol, sensitivity <10 CFU/ml |
| Fluorescent Stains | Visual detection via DNA binding | Hoechst 33258, DAPI | DNA-specific fluorescence, requires fluorescence microscopy |
| Membrane Stains | Cell membrane labeling for colocalization | WGA (wheat germ agglutinin) conjugates | Specific membrane binding, different fluorophore options |
| Antibiotic Treatments | Elimination of contamination | Plasmocin, Enrofloxacin | Effective against mycoplasma, different mechanisms |
| Positive Controls | Assay validation and calibration | Quantitative genomic DNA from M. hominis, M. pneumoniae | Certified reference materials, known concentrations |
| Reference Strains | Assay development and validation | Titered mycoplasma reference strains | Calculated genome copy numbers, panel of common species |
| Growth Supplements | Culture-based detection enhancement | Mycoplasma growth supplement | Enhances recovery in broth and agar media |
| Decontamination Agents | Laboratory surface purification | Bleach, specialized sporicidal agents | Effective against mycoplasma on equipment and surfaces |
Mycoplasma contamination remains a persistent and formidable challenge in cell culture laboratories, representing a silent threat that can compromise years of research and development efforts. The unique biological characteristics of these microorganisms—including their small size, lack of cell wall, and stealthy infection patterns—require specialized detection methods beyond conventional microbiological approaches. Advanced techniques such as PCR-based detection and colocalization staining provide the sensitivity and specificity needed for reliable identification, while comprehensive prevention protocols centered on rigorous aseptic technique and routine monitoring form the first line of defense.
The profound impact of mycoplasma contamination on virtually all aspects of cellular physiology underscores the critical importance of vigilant monitoring and rapid response strategies. From altered metabolic pathways and genetic expression changes to compromised experimental results and potential product safety concerns, the consequences of undetected contamination can be far-reaching. As cell culture technologies continue to advance and play increasingly important roles in biopharmaceutical development and regenerative medicine, maintaining mycoplasma-free cultures becomes ever more essential. Through implementation of the detection, prevention, and elimination strategies outlined in this review, researchers can protect their cellular models, ensure the integrity of their data, and safeguard the translation of their findings into meaningful scientific and clinical advancements.
Viral contamination represents a persistent and covert threat to the integrity of biological research and the safety of biopharmaceutical manufacturing. Unlike bacterial or fungal contamination, viral contaminants can be difficult to detect, often escaping notice until they have compromised experimental results or entire production batches [14] [11]. In cell culture systems, which are fundamental to modern biological research and therapeutic production, viral infections can alter cellular metabolism, gene expression, and viability, potentially leading to misleading scientific conclusions or dangerous therapeutic products [14].
The implications of viral contamination extend beyond scientific accuracy to encompass significant economic and health consequences. Historical incidents of viral transmission through biological products have led to patient harm, highlighting the critical importance of robust viral safety strategies [15] [16]. This technical guide examines the sources, detection methods, and prevention strategies for viral contamination, providing researchers and bioprocessing professionals with a comprehensive framework for safeguarding their work against these invisible threats.
Viral contamination in cell culture systems can originate from multiple sources, which regulatory guidelines broadly categorize into two groups: endogenous contaminants present in cell banks, and adventitious viruses introduced during production [17].
Cell Banks and Raw Materials: Master Cell Banks (MCBs) and Working Cell Banks (WCBs) can harbor endogenous viruses, particularly retroviruses, which are constitutively expressed and transmitted through sequential cell passage [17]. Raw materials of animal origin, such as bovine serum or porcine-derived trypsin, historically represent significant contamination risks [15] [16]. Although the industry has shifted toward animal-component-free media, risks persist from contaminated reagents or inadequate sterilization [18].
Production Process Introduction: Adventitious viruses can be introduced during manufacturing through handling of cell cultures, contaminated raw materials, or operator error [17] [15]. The case study of baculovirus contamination in a BEVS manufacturing process illustrates how simultaneous operations in shared facilities can lead to cross-contamination, even with spatial segregation [18]. In this incident, the same operator working on both virus harvest and media preparation activities likely facilitated the transfer of concentrated virus into host-cell media, resulting in multiple batch failures.
Environmental and Human Factors: Laboratory environments, including unfiltered air, unclean surfaces, and improper airflow control, can serve as contamination vectors [11]. Human operators remain a potential source through improper aseptic techniques, inadequate training, or failure to follow standard operating procedures [11].
Historical Context and Impact
Historical contamination events underscore the serious consequences of viral contamination:
Figure 1: Consequences of Viral Contamination and Historical Examples
Notably, before implementation of viral inactivation procedures, hepatitis C virus and human immunodeficiency virus type 1 were transmitted to patients through human-plasma-derived biological products [15]. While no infectious virus has been transmitted to patients by biopharmaceuticals derived from cell lines, contamination events have been detected in process intermediates, leading to significant economic losses and product shortages [15].
Detection and Identification of Viral Contaminants
Effective detection of viral contamination requires a multi-faceted approach, as no single method can identify all potential contaminants. The selection of detection methodologies depends on the type of virus, the stage of production, and the required sensitivity.
Established Detection Methods
Cytopathic Effects (CPE) Observation: Many viruses induce visible morphological changes in infected cells, known as cytopathic effects [14]. These can include cell rounding, syncytia formation (cell fusion), and cell lysis. For example, HSV-2 infection in A549 cells causes significant rounding and detachment from the culture surface [14]. While CPE observation provides an initial indication of contamination, many viruses, particularly latent ones, do not produce obvious cytopathic effects.
PCR-Based Assays: Polymerase chain reaction (PCR) methods, including quantitative PCR (qPCR), offer highly sensitive and specific detection of viral nucleic acids [14]. These assays can identify both active and latent viral forms, making them particularly valuable for detecting viruses like Epstein-Barr virus (EBV), which infects approximately 98% of the human population [14]. PCR is especially crucial for detecting mycoplasma contamination, which doesn't cause turbidity or other obvious signs but alters gene expression and cellular function [11].
In Vitro and In Vivo Virus Assays: Broad-specificity in vitro assays using indicator cell lines can detect a wide range of viral contaminants through observation of CPE or immunochemical staining [17]. In vivo assays, involving inoculation of samples into animals such as mice or embryonated eggs, provide a complementary approach for detecting viruses that may not grow in standard cell cultures [17].
Emerging Detection Technologies
Next-generation sequencing (NGS) enables comprehensive detection of known and unknown viral contaminants without prior knowledge of the viral sequence [17]. This untargeted approach is particularly valuable for identifying emerging contaminants or viruses not previously associated with cell culture systems. The "Blazar Platform" represents an example of rapid molecular testing methods that enable real-time decisions on in-process materials [17].
Table 1: Viral Detection Methods and Their Applications
| Method | Principle | Sensitivity | Applications | Limitations |
|---|---|---|---|---|
| Cytopathic Effect Observation | Visual identification of virus-induced morphological changes | Variable; depends on virus | Initial screening; virus identification | Insensitive to non-cytopathic viruses |
| PCR/qPCR | Amplification of viral nucleic acids | High (can detect few copies) | Specific virus detection; latency identification | Requires prior knowledge of viral sequence |
| Next-Generation Sequencing | High-throughput sequencing of all nucleic acids | High | Comprehensive detection; unknown viruses | Cost; complex data analysis |
| In Vitro Virus Assays | Infection of permissive indicator cell lines | Moderate to high | Broad virus detection | Limited by cell line permissiveness |
Prevention and Control Strategies
A comprehensive viral safety strategy employs multiple complementary approaches to prevent contamination from entering bioprocessing systems and to manage risks throughout production.
Prevention Framework
The foundational framework for viral safety involves three key elements: prevention, detection, and removal [17]. Prevention focuses on careful selection of cells and raw materials, with preference for animal-derived component-free materials wherever possible [17]. For raw materials that cannot be eliminated, sourcing from low-risk geographies or using materials treated with gamma irradiation, UV irradiation, or high-temperature short-time (HTST) pasteurization reduces contamination risk [17].
Closed Processing Systems: Implementing closed bioprocessing technologies provides a higher level of process protection than open processing by isolating the process and product from environmental contaminants [18]. Functionally closed systems, appropriately validated, can allow manufacturing in controlled, non-classified environments because the surrounding environment no longer affects the process [18].
Environmental and Personnel Controls: Strict cleanroom standards utilizing HEPA filtration, proper gowning procedures, and comprehensive environmental monitoring programs are essential for controlling contamination risks [11]. Well-trained operators following established aseptic techniques represent a critical defense against adventitious viral introduction [11].
Testing Strategy
A comprehensive testing strategy covers all aspects of the production process, from raw materials to final product. According to ICH Q5A guidance, Master Cell Bank (MCB) characterization requires broad specificity in vitro and in vivo virus assays, while Working Cell Banks (WCB) undergo more limited testing [17]. End-of-production (EOP) cells are tested extensively for viral contaminants that may be present but not detected in the MCB [17].
Figure 2: Comprehensive Viral Risk Management Framework
Viral Clearance and Inactivation Methodologies
Despite rigorous prevention efforts, the risk of viral contamination cannot be entirely eliminated, making viral clearance steps essential components of biopharmaceutical manufacturing processes. Viral clearance studies demonstrate the capability of manufacturing processes to remove or inactivate potential viral contaminants.
Viral Clearance Study Design
Viral clearance studies are performed using scaled-down models that accurately represent actual manufacturing processes [15]. To ensure validity, these scaled-down models must mimic full-scale processes in terms of buffers, linear flow rates, contact times, and other critical parameters [15]. Product and impurity profiles from scaled-down processes must reflect those from full-scale manufacturing for viral clearance data to be considered valid [15].
For early-stage clinical trials, the European Medicines Agency requires a minimum evaluation of two orthogonal steps with a retrovirus and a parvovirus [15]. As product development advances toward licensure, more comprehensive studies are performed with an extended virus panel under a range of processing conditions, including worst-case parameters [15].
Viral reduction is typically expressed in logarithmic terms (log10 reduction), calculated by comparing the amount of virus in preprocessed load material to that in post-processed samples [15]. Cumulative process reduction values are determined by summing the log reduction levels for each unit operation.
Viral Clearance Technologies
Effective viral clearance employs orthogonal methods with different mechanisms of action to ensure robust viral safety.
Low pH Treatment: Exposure to low pH (e.g., pH 3.0–3.6) is highly effective against enveloped viruses and is commonly used in monoclonal antibody purification processes following Protein A chromatography [17] [15]. This method provides robust viral reduction, typically exceeding 4.0 log10 for enveloped viruses [15].
Solvent/Detergent Treatment: Originally developed for blood products, solvent/detergent treatment using combinations such as 0.3% tri(n-butyl) phosphate/0.2% sodium cholate effectively inactivates enveloped viruses by disrupting their lipid membranes [15]. This method is robust and effective against a wide range of enveloped viruses.
Virus Filtration: Virus-retentive filters physically remove viruses based on size exclusion [17] [15]. These filters are particularly valuable for removing small, non-enveloped viruses such as parvoviruses, which are resistant to many inactivation methods [17]. Virus filtration is considered a robust clearance method when properly validated and operated within specified parameters.
Chromatography Operations: Although optimized for product purification, chromatography steps often provide incidental viral clearance through a combination of mechanisms, including binding to resin surfaces, degradation during elution, and separation from the product [15]. Anion-exchange chromatography can be optimized to provide significant viral clearance, though chromatography steps are generally less robust than dedicated viral clearance operations [15].
Table 2: Viral Clearance Methods and Their Effectiveness
| Method | Mechanism | Virus Types Affected | Typical Log Reduction | Considerations |
|---|---|---|---|---|
| Low pH Treatment | Denaturation of viral envelope proteins | Enveloped viruses | >4.0 log10 | Effectiveness depends on pH, time, temperature |
| Solvent/Detergent | Disruption of viral lipid envelope | Enveloped viruses | >4.0 log10 | Ineffective against non-enveloped viruses |
| Virus Filtration | Size-based exclusion | All viruses larger than pore size | >4.0 log10 | Filter integrity critical; fouling concerns |
| Anion-Exchange Chromatography | Binding to resin surfaces | Enveloped and non-enveloped | 2-4 log10 | Highly dependent on process conditions |
Experimental Protocols for Viral Detection and Clearance Validation
Protocol for Viral Detection in Cell Banks
This protocol outlines the standard procedure for detecting viral contaminants in cell banks using a combination of in vitro and in vivo assays, as recommended by regulatory guidelines [17].
Sample Preparation: Collect approximately 10^7 cells from the cell bank. Prepare cell lysates by freeze-thaw cycling or chemical lysis. For co-cultivation assays, prepare viable cells for co-cultivation with indicator cell lines.
In Vitro Assay: Inoculate samples onto at least three different indicator cell lines, including human and non-human primate cell lines known to support growth of a wide range of viruses. Maintain cultures for at least 14 days with at least one subculture during this period. Observe regularly for cytopathic effects. Include positive controls with known viruses to demonstrate assay sensitivity.
In Vivo Assay: Inoculate samples into at least two animal systems, typically suckling mice and embryonated eggs. Observe animals for signs of disease or mortality. Examine embryos for evidence of viral replication after appropriate incubation.
Other Virus-Specific Tests: Perform specific tests for retroviruses and other known contaminants. For retroviruses, use reverse transcriptase assays or transmission electron microscopy. For specific viruses of concern (e.g., EBV, OvHV-2), implement PCR-based assays with appropriate controls [14].
Results Interpretation: A sample is considered positive if any test system shows evidence of viral presence. Negative results across all assays provide confidence in the viral safety of the cell bank, though they do not guarantee absolute absence of viral contaminants.
Protocol for Viral Clearance Studies
This protocol describes the general approach for validating the viral clearance capability of manufacturing process steps, following regulatory expectations [15].
Scale-Down Model Qualification: Before viral clearance studies, qualify the scaled-down model by demonstrating that it accurately represents the full-scale manufacturing process. Compare critical process parameters (flow rates, contact times, buffer compositions) and performance indicators (step yield, product quality attributes) between scales.
Virus Panel Selection: Select a panel of relevant model viruses representing different virus types and characteristics. Typical panels include:
- Murine Leukemia Virus (MuLV) as a model for endogenous retroviruses
- Minute Virus of Mice (MVM) or other parvoviruses as models for small, non-enveloped viruses
- Additional viruses based on risk assessment, potentially including pseudorabies virus, bovine viral diarrhea virus, or others
Virus Spike Preparation: Prepare high-titer virus stocks in appropriate matrices. Characterize virus stocks for titer and purity. Determine the appropriate spike ratio (typically 1-10% v/v) to ensure it does not significantly alter product or process stream characteristics.
Process Step Execution: Spike the virus into the preprocessed intermediate material. Execute the process step using predetermined operating parameters. Collect samples before processing and after completion of the step.
Virus Titration: Determine virus titers in pre- and post-processing samples using appropriate assays (plaque assay, 50% tissue culture infectious dose (TCID50), or quantitative PCR). Include necessary controls to account for assay variability and toxicity.
Calculation of Viral Reduction: Calculate the log reduction value (LRV) using the formula: LRV = log10 (Vpre × Vvol.pre) - log10 (Vpost × Vvol.post), where Vpre and Vpost are virus titers in pre- and post-processing samples, and Vvol.pre and Vvol.post are sample volumes.
Data Interpretation and Reporting: Report individual LRVs for each virus and process step combination. Evaluate the overall clearance capacity of the process by summing LRVs from orthogonal steps. Discuss limitations and assumptions of the study.
The Scientist's Toolkit: Essential Reagents and Materials
Implementing effective viral safety programs requires specific reagents, materials, and systems designed to prevent, detect, or remove viral contaminants.
Table 3: Essential Research Reagent Solutions for Viral Safety
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Virus-Screened Fetal Bovine Serum | Cell culture supplement | Sourced from closed herds in low-risk geographical areas; tested for specific viruses |
| Animal-Derived Component Free Media | Cell culture medium | Eliminates risk from bovine- or porcine-derived materials; chemically defined formulations preferred |
| PCR/qPCR Kits for Virus Detection | Specific virus detection | Target common contaminants (e.g., mycoplasma, retroviruses, specific viruses of concern) |
| Indicator Cell Lines | Broad virus detection | Includes cell lines such as Vero, MRC-5, HEK293 with known susceptibility to various viruses |
| Virus Removal Filters | Physical removal of viruses | Size-based exclusion with pore sizes typically 20-50 nm; validated for specific retention ratings |
| Chromatography Resins | Product purification and virus removal | Anion-exchange resins particularly effective for virus removal under appropriate conditions |
| Solvent/Detergent Reagents | Viral inactivation | TNBP/Triton X-45 or polysorbate 80/TNBP combinations for enveloped virus inactivation |
Viral contamination remains a persistent, covert risk to both biological research and biopharmaceutical production. The complex nature of viral contaminants, combined with the potential for devastating scientific, economic, and health consequences, necessitates comprehensive viral safety strategies integrating prevention, detection, and removal approaches. Implementation of robust quality control systems, including careful raw material selection, routine testing programs, and validated clearance steps, provides multilayered protection against these invisible threats.
As bioprocessing technologies evolve to include novel modalities such as cell and gene therapies, viral safety considerations must adapt to address new risk profiles. Maintaining vigilance against viral contamination through continued research, industry collaboration, and regulatory alignment will ensure the ongoing safety and efficacy of biological products while protecting the integrity of scientific research.
Cell culture contamination represents a significant challenge in biomedical research and biopharmaceutical production, potentially compromising experimental validity, product safety, and therapeutic efficacy. While microbial contamination receives considerable attention, chemical contaminants—specifically endotoxins, detergents, and media impurities—pose equally critical yet often less apparent risks. These contaminants can induce subtle but profound alterations in cellular responses, leading to unreliable data, failed experiments, and compromised biological products. This technical guide examines the sources, mechanisms, and impacts of these chemical contaminants within the broader context of cell culture contamination research, providing researchers with comprehensive methodologies for detection, removal, and prevention. Understanding these contaminants is essential for maintaining the integrity of in vitro systems and ensuring the reliability of research outcomes in drug development and basic science.
Endotoxin Contamination
Origins and Chemical Nature
Endotoxins, structurally known as lipopolysaccharides (LPS), are complex amphiphilic molecules constituting the outer membrane of Gram-negative bacteria such as Escherichia coli, Klebsiella, and Pseudomonas [19]. Unlike exotoxins secreted by living bacteria, endotoxins are released primarily upon bacterial death and lysis, making sterilization processes potential contamination sources [20]. Structurally, LPS consists of three domains: a hydrophobic Lipid A moiety that anchors the molecule to the bacterial membrane, a core oligosaccharide, and a variable O-antigen polysaccharide chain [19]. The Lipid A component is responsible for the profound biological toxicity associated with endotoxins.
Mechanisms of Cellular Toxicity
Endotoxins exert their pathological effects primarily through activation of the innate immune system. The Lipid A component of LPS is recognized by Toll-like receptor 4 (TLR4) and its co-receptor MD-2 on immune cells such as monocytes and macrophages [19]. This recognition triggers intracellular signaling cascades leading to NF-κB activation and subsequent transcription of pro-inflammatory cytokines including TNF-α, IL-1, and IL-6 [19]. At low levels, this response may cause subtle changes in cell behavior; at higher concentrations, it can induce fever, endotoxic shock, and cell death [19] [20].
Figure 1: Endotoxin (LPS) Signaling Pathway via TLR4 Activation
Detection and Quantification Methods
Accurate detection and quantification of endotoxins are essential for quality control in cell culture and bioprocessing. The Limulus Amoebocyte Lysate (LAL) assay remains the gold standard, with several validated formats approved by regulatory agencies [19] [21].
Table 1: Endotoxin Detection Methods
| Method | Principle | Sensitivity | Applications | Regulatory Status |
|---|---|---|---|---|
| Gel-Clot LAL | Visual detection of gel formation | 0.03 EU/mL | Qualitative analysis | FDA approved [19] |
| Turbidimetric LAL | Measures turbidity increase | 0.001 EU/mL | Quantitative analysis | FDA approved [19] |
| Chromogenic LAL | Hydrolyzes chromogenic substrate | 0.005 EU/mL | Highly quantitative | FDA approved [19] |
| Rabbit Pyrogen Test | In vivo fever response | Varies | Systemic pyrogenicity | Being phased out [20] |
| Monocyte Activation Test (MAT) | Human cytokine release | 0.25 EU/mL | Detects all pyrogens | Alternative to animal testing [20] |
The Bacterial Endotoxins Test (BET) methodologies described in USP Chapter <85> and AAMI ST72 provide regulatory frameworks for testing [21]. For medical devices, endotoxin limits depend on the intended use, with more stringent requirements for devices contacting blood, cerebrospinal fluid, or other circulating fluids [20].
Removal and Control Strategies
Effective endotoxin control requires both removal from reagents and prevention of introduction. Removal techniques exploit the physicochemical properties of LPS and must be tailored to specific applications:
- Ion-Exchange Chromatography: Effective for separating negatively charged LPS from proteins [19]
- Affinity Adsorbents: Specific ligands target LPS structure [19]
- Triton X-114 Phase Separation: Exploits detergent properties to partition LPS [19]
- Sterilization Protocols: Dry heat at 250°C for >30 minutes or 180°C for 3 hours destroys endotoxins on glassware [22]
Preventive measures include using high-purity water (testing with LAL assay), selecting low-endotoxin FBS (<1ng/mL), and employing certified plasticware (<0.1 EU/mL) [22]. For organ-on-chip technologies fabricated with PDMS, oxygen plasma treatment can reduce endotoxin adsorption, though effects may diminish with hydrophobic recovery [23].
Detergent Contamination
Roles and Classifications in Cell Culture
Detergents are amphipathic molecules essential for various cell culture and protein biochemistry applications, including cell lysis, membrane protein solubilization, and preventing non-specific binding in affinity purification [24]. They are classified by the ionic character of their polar head groups:
- Ionic detergents (e.g., SDS): Charged head groups; strongly denaturing
- Non-ionic detergents (e.g., Triton X-100, NP-40): Uncharged; mild and non-denaturing
- Zwitterionic detergents (e.g., CHAPS): Both positive and negative charges; net neutral [24]
Table 2: Properties of Common Laboratory Detergents
| Detergent | Type | Critical Micelle Concentration (CMC) | Aggregation Number | Applications | Removability |
|---|---|---|---|---|---|
| SDS | Anionic | 6-8 mM (0.17-0.23%) | 62 | Strong lysis, denaturing | Difficult [24] |
| Triton X-100 | Non-ionic | 0.24 mM (0.0155%) | 140 | Mild lysis, membrane protein isolation | Dialysis/adsorption [24] |
| Tween-20 | Non-ionic | 0.06 mM (0.0074%) | - | Immunoassays, blocking | Dialysis [24] |
| CHAPS | Zwitterionic | 8-10 mM (0.5-0.6%) | 10 | Membrane protein solubilization | Dialyzable [24] |
| Octyl-glucoside | Non-ionic | 23-24 mM (~0.70%) | 27 | Protein crystallization | Highly dialyzable [24] |
Contamination Mechanisms and Impacts
Detergent contamination typically occurs through improper rinsing of laboratory ware, carryover from purification procedures, or misformulation of culture media. The impacts vary by detergent type and concentration:
- Ionic detergents like SDS denature proteins, disrupt membrane integrity, and cause complete cell lysis at low concentrations [24]
- Non-ionic detergents may interfere with receptor-ligand interactions, enzyme activities, and membrane protein functions without visible cell death [24] [25]
- Excess detergent micelles can block assay substrates, convolute analytical readings, and prevent protein crystallization [25]
Removal Techniques and Methodologies
Selecting appropriate detergent removal strategies depends on the detergent properties, sample volume, and intended downstream applications:
Figure 2: Detergent Removal Method Selection Workflow
Detailed Protocol: Styrene Bead Adsorption
- Principle: Porous polystyrene beads (e.g., Bio-Beads) adsorb detergent molecules through hydrophobic interactions [25].
- Procedure:
- Determine optimal bead-to-sample ratio empirically (typically 10-50 mg beads/100 μL sample)
- Add washed, wet beads to sample
- Incubate with gentle agitation for 2-4 hours at 4°C
- Centrifuge at 1000 × g for 2 minutes to pellet beads
- Carefully collect supernatant
- Repeat process if necessary
- Validation: Measure detergent concentration using iodine vapor staining with TLC and laser densitometry [25].
- Considerations: May co-remove essential lipids; risk of protein precipitation if detergent is over-removed [25].
Alternative Methods:
- Size-exclusion chromatography: Effective when protein and micelle sizes differ significantly [25]
- Dialysis: Suitable for detergents with high CMC; requires appropriate membrane selection [25]
- Detergent removal columns: Proprietary resins for rapid spin-column removal [25]
Media Impurities
Cell culture media contain multiple potential sources of chemical contaminants beyond endotoxins and detergents:
- Water impurities: Bacterial residues, ions, organic compounds from poorly maintained water purification systems [22]
- Serum components: High endotoxin levels in FBS, hormones, antibodies, viruses [22]
- Raw materials: Amino acid solutions with endotoxin levels as high as 50ng/mL, heavy metals, pesticides [22]
- Additives: Growth factors, cytokines, antibiotics with variable purity
- Leachables: Chemicals migrating from bioprocess containers or tubing
Impact on Cell Culture Systems
Media impurities can profoundly affect cellular responses and experimental outcomes:
- Altered growth kinetics: Subtle changes in proliferation rates without visible cytotoxicity
- Differentiation effects: Unplanned differentiation in stem cell cultures
- Gene expression changes: Modulation of inflammatory or stress response pathways
- Metabolic shifts: Altered nutrient utilization and waste production
- Morphological variations: Changes in cell shape, attachment, or organization
Detection and Quality Control
Implementing rigorous quality control measures for media and reagents is essential:
- Comprehensive testing: Beyond standard sterility testing to include endotoxin, mycoplasma, and viral contamination screens [14]
- Water quality monitoring: Regular LAL testing of water purification systems [22]
- Component qualification: Testing individual media components before full formulation
- Certified sourcing: Using manufacturers that provide comprehensive quality documentation
- In-process controls: Monitoring media throughout production and storage
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Contamination Control
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| LAL Reagents | Endotoxin detection and quantification | Choose format (gel-clot, chromogenic, turbidimetric) based on sensitivity needs [19] |
| Bio-Beads SM-2 | Hydrophobic adsorption of detergents | Optimal for Triton X-100 removal; requires ratio optimization [25] |
| Detergent Removal Columns | Rapid spin-column detergent removal | HiPPR and Pierce columns suitable for small volumes (<100μL) [25] |
| Low-Endotoxin FBS | Cell culture supplement with <1ng/mL endotoxin | Critical for sensitive cultures; premium grade available [22] |
| Certified Plasticware | Culture vessels tested for endotoxins | Typically <0.1 EU/mL; reduces introduction of contaminants [22] |
| Water for Injection (WFI) | High-purity water source | Alternative when laboratory water systems are compromised [22] |
| Recombinant Factor C (rFC) | Animal-free endotoxin testing | Eliminates horseshoe crab sourcing concerns; not yet FDA-approved [20] |
Integrated Contamination Control Strategy
Effective management of chemical contaminants requires a systematic, preventive approach rather than reactive measures. Implementation of Quality by Design (QbD) principles in research workflows helps identify critical control points for contamination prevention [21]. Key elements include:
- Comprehensive risk assessment: Evaluate all potential contamination sources from raw materials to final culture conditions
- Strategic sampling plans: Test in-process materials and finished products with dynamic sampling protocols that adapt as process knowledge increases [21]
- Process validation: Demonstrate contaminant removal capabilities of purification steps
- Environmental monitoring: Regular testing of water systems, laboratory surfaces, and air quality
- Documentation and traceability: Maintain complete records of reagents, lots, and quality control data
For medical devices and biologics, the FDA recommends developing scientifically sound sampling plans that consider the potential for contamination in raw materials, in-process materials, and finished products, adjusting these plans as confidence in contamination prevention increases [21].
Emerging Technologies and Future Directions
The field of contamination control continues to evolve with several promising developments:
- Advanced detection methods: Recombinant Factor C (rFC) assays for animal-free endotoxin testing, though not yet FDA-approved [20]
- Novel removal technologies: Affinity matrices with enhanced specificity for contaminants
- Point-of-use monitoring: Rapid tests for routine contamination screening
- Material science innovations: Low-binding surfaces and materials that resist contamination adsorption
- Microfluidic applications: Organ-on-chip platforms with integrated contamination sensors [23]
The Monocyte Activation Test (MAT) represents a particularly promising advancement, as it detects both endotoxin and non-endotoxin pyrogens using human cells, potentially replacing the rabbit pyrogen test which the European Pharmacopoeia Commission plans to eliminate by 2025 [20].
Chemical contaminants—endotoxins, detergents, and media impurities—represent significant yet often overlooked challenges in cell culture systems. Their impacts range from subtle alterations in cellular physiology to complete experimental failure, with particular concern for drug development and biological product manufacturing. Through understanding contamination sources, implementing robust detection methodologies, and applying appropriate removal strategies, researchers can significantly enhance the reliability of their cell culture systems. As technological advances provide more sensitive detection methods and more effective removal techniques, integration of comprehensive contamination control practices remains essential for research integrity and translational success.
Cell line cross-contamination represents one of the most persistent and damaging problems in biomedical research, compromising data integrity and reproducibility on a global scale. This issue traces its origins to the earliest days of cell culture, yet continues to affect modern laboratories despite increased awareness and technological advancements. Cross-contamination occurs when a fast-growing cell line inadvertently invades and overtakes another culture, typically through laboratory errors in handling or inadequate quality control procedures. The consequences extend beyond mere inconvenience—misidentified cell lines have generated invalid scientific data, wasted billions in research funding, and potentially misdirected clinical therapy development [26] [27].
The seminal case of cross-contamination involves HeLa cells, the first immortal human cell line established from cervical adenocarcinoma cells of patient Henrietta Lacks in 1951. As early as 1968, Stanley Gartler demonstrated that 18 supposedly independent human cell lines were actually HeLa contaminants, including the presumed laryngeal carcinoma HEp-2 and embryonic intestinal cell line Intestine 407 [26]. Despite this early warning, the problem has proliferated over decades, with current estimates suggesting that 15-20% of cell lines in use may not be what they are documented to be [27]. The International Cell Line Authentication Committee (ICLAC) currently maintains a register of 576 misidentified cell lines, including 531 with no known authentic stock [26].
The Scope and Impact of Cross-Contamination
Quantitative Assessment of the Problem
The prevalence and economic impact of cell line misidentification reveal a crisis affecting multiple dimensions of biomedical research.
Table 1: Prevalence of Cell Line Misidentification Across Studies
| Source | Cell Lines Tested | Misidentification Rate | Context |
|---|---|---|---|
| DSMZ Analysis [26] | 848 leukemia-lymphoma cell lines | 14-18% | Secondary sources (1990-2014) |
| DSMZ Analysis [26] | 848 leukemia-lymphoma cell lines | 6% | Primary sources (1990-2014) |
| China CCTCC [26] | 380 cell lines from 113 sources | 25% | General collection |
| China CCTCC [26] | 69 China-origin models | 85.5% | Cell lines established in China |
| ICLAC Register [26] | - | 576 total misidentified lines | Current known problematic lines |
The financial implications of this widespread misidentification are staggering. Korch and Capes-Davis calculated that approximately $990 million was spent to publish 9,894 manuscripts using just two contaminated cell lines (HEp-2 and Intestine 407) [26]. Extrapolating this to the 531 misidentified cell lines with no authentic stock suggests billions of research dollars have been wasted on studies using misidentified cell lines, not accounting for subsequent research built upon these flawed foundations [26].
Notable Case Examples
Table 2: Examples of Commonly Misidentified Cell Lines
| Supposed Cell Line | Supposed Cell Type | Actual Identity | Actual Cell Type | Status |
|---|---|---|---|---|
| HEp-2 [26] | Laryngeal carcinoma | HeLa | Cervical adenocarcinoma | Misidentified |
| Intestine 407 [26] | Embryonic intestine | HeLa | Cervical adenocarcinoma | Misidentified |
| ECV-304 [28] | Normal endothelium | T-24 | Bladder carcinoma | Misidentified |
| DAMI [28] | Megakaryocytic | HEL | Erythroleukemia | Misidentified |
| Chang Liver [28] | Liver | HeLa | Cervical adenocarcinoma | Misidentified |
| ARO [28] | Thyroid cancer | HT-29 | Colon carcinoma | Misidentified |
The scientific impact extends beyond financial waste. Research conducted with misidentified cell lines generates invalid data that can misdirect scientific understanding and clinical applications. For instance, the cell line ECV-304 was widely used as a normal endothelial model until it was identified as the bladder carcinoma line T-24, invalidating countless studies on endothelial biology [28]. Similarly, the DAMI cell line, used extensively for megakaryocyte research, was actually an erythroleukemia cell line (HEL), distorting the understanding of megakaryocyte-specific functions [28].
Causes and Mechanisms of Cross-Contamination
Pathways to Contamination
The process of cell line cross-contamination typically follows two principal pathways, each with distinct implications for detection and prevention:
Laboratory Cross-Contamination: This occurs when cell cultures are exchanged between research groups and accidental contamination happens during handling. If the contaminated sample is subsequently passed on, the contaminating population becomes established in multiple laboratories, even though some stocks of the original cell line may remain genuine [28].
Source Contamination: More seriously, contamination can occur during the initial establishment of a novel cell line, when contaminating cells are accidentally introduced into the original cultures. These aggressive contaminants eventually outgrow the desired cells, meaning the authentic cell line never truly existed or became extinct shortly after establishment. In such cases, even early testing may not reveal the contamination, and all subsequent samples represent the contaminating cells, creating what are termed "virtual cell lines" [28].
Contributing Factors
Several laboratory practices and cell biological factors contribute to the persistence of cross-contamination:
- Unequal Growth Kinetics: Fast-growing cell lines like HeLa can rapidly overtake slower-growing cultures. A single HeLa cell is sufficient to take over another cell line in culture [27].
- Inadequate Aseptic Technique: Poor practices during media changes, cell passaging, or shared equipment use facilitate accidental mixing of cell lines [29].
- Unverified Cell Sources: Obtaining cell lines from other laboratories rather than reputable cell banks increases risk. One study showed cell lines from secondary sources had 14-18% cross-contamination rates versus 6% from primary sources [26].
- Insufficient Authentication Testing: Surveys indicate more than a third of researchers obtain cells from other labs, and almost half do not perform identity testing [27].
- Inadequate Record Keeping: Poor documentation of cell stocks and freezing procedures leads to mislabeling and inability to track contamination events [27].
Detection and Authentication Methods
Comprehensive Authentication Techniques
Multiple methodological approaches have been developed for detecting cross-contamination and authenticating cell lines, each with distinct advantages and applications.
Table 3: Cell Line Authentication Methods
| Method | Principle | Applications | Advantages | Limitations |
|---|---|---|---|---|
| STR Profiling [26] [27] | PCR amplification of short tandem repeat loci | Intraspecies identification of human cell lines | High discrimination, standardized, inexpensive | May not detect intraspecies contamination |
| Karyotyping [28] [27] | Chromosome number and structure analysis | Species confirmation, genetic stability | Detects gross chromosomal abnormalities | Limited resolution, labor-intensive |
| Isoenzyme Analysis [27] | Electrophoretic mobility of enzyme variants | Species identification | Rapid, robust, multiple enzymes | Low reproducibility, limited discrimination |
| DNA Barcoding [27] | Cytochrome c oxidase (COI) sequence analysis | Species identification | High accuracy for species determination | Limited for intraspecies discrimination |
STR Profiling: The Gold Standard
Short tandem repeat (STR) profiling has emerged as the international reference standard for human cell line authentication. This technique works on the same principle as forensic DNA fingerprinting but utilizes polymerase chain reaction (PCR) to simultaneously amplify multiple polymorphic STR loci throughout the genome [27]. The American Type Culture Collection Standards Development Organization (ATCC SDO) Workgroup ASN-0002 has developed a comprehensive standard for authentication of human cell lines by STR profiling, including detailed protocols for DNA extraction, STR profiling, data analysis, and quality control [26].
The authentication workflow follows a systematic process to ensure accurate identification:
Critical to the STR authentication process is comparison with reference databases. The Cellosaurus database, a knowledge resource documenting over 102,000 human cell lines, provides STR profiles for more than 8,000 distinct human cell lines and includes the CLASTR (Cellosaurus STR similarity search tool) for comparing obtained STR profiles against this extensive database [26]. The database also flags problematic cell lines and assigns unique Research Resource Identifiers (RRIDs) to facilitate proper tracking and identification [26].
Prevention Strategies and Quality Control
Comprehensive Prevention Framework
Effective prevention of cell line cross-contamination requires a multi-layered approach addressing both technical practices and institutional policies.
Table 4: Key Resources for Cell Line Authentication and Quality Control
| Resource Type | Specific Examples | Function and Application |
|---|---|---|
| Reference Databases | Cellosaurus, ICLAC Register of Misidentified Cell Lines | Provides STR profiles and alerts for problematic cell lines |
| Authentication Services | ATCC, DSMZ, commercial testing services | Professional STR profiling and species verification |
| Cell Banking Facilities | Liquid nitrogen storage systems, cryopreservation reagents | Secure long-term storage of authenticated stocks |
| Quality Control Kits | STR profiling kits, mycoplasma detection kits | Regular monitoring of cell line identity and purity |
| Reference Materials | Certified reference cell lines from ATCC, ECACC | Positive controls for authentication procedures |
Institutional Policies and Standards
Beyond individual laboratory practices, addressing the cross-contamination crisis requires systematic institutional and policy changes. Several scientific journals have implemented authentication requirements for manuscripts reporting cell line research [26] [27]. The International Journal of Cancer (IJC) experience with mandatory authentication revealed that at least 5% of human cell lines used in submitted manuscripts were misidentified, with about 4% of manuscripts rejected for severe cell line problems [26].
Funding organizations increasingly recognize the importance of authentication, with some proposing that cell line authentication should be conditional for grant receipt [27]. Research institutions play a critical role by implementing regular authentication schedules, staff training programs, and centralized cell banking systems to minimize cross-contamination risks.
Cell line cross-contamination remains a significant threat to research integrity decades after its initial discovery. The problem persists not due to lack of detection methods or awareness, but because of inconsistent implementation of authentication practices across the biomedical research community. Solutions require coordinated efforts among individual researchers, institutions, funding agencies, and publishers to establish and enforce authentication standards.
Emerging technologies promise enhanced detection capabilities, including real-time monitoring systems [5] and advanced molecular profiling methods. However, the most immediate impact will come from widespread adoption of existing STR profiling technologies and adherence to good cell culture practices. Only through sustained commitment to cell line authentication can the scientific community ensure the validity and reproducibility of research findings, proper stewardship of research resources, and ultimately, the advancement of reliable biomedical knowledge.
In the context of cell culture contamination research, particulate contamination represents a critical and often overlooked challenge in Good Manufacturing Practice (GMP) environments. While microbial contamination (bacteria, fungi, mycoplasma) and viral contamination typically receive significant attention due to their direct impact on cell viability, non-viable particulate contamination poses unique risks to drug product safety, quality, and regulatory compliance. These particles, which include intrinsic particles from manufacturing processes and extrinsic particles from the environment, can originate from various sources including single-use technologies, cleanroom operations, and personnel [30] [11]. Unlike viable contaminants, particles cannot replicate, but they can accumulate throughout upstream and downstream bioprocessing, making them particularly problematic for cell and gene therapies that cannot undergo final filtration without compromising the product itself [30].
The control of particulate matter is stringently regulated under guidelines such as USP 〈788〉, which defines acceptable levels of subvisible particles in injectable products [31]. With the recent revision of this standard (officially effective August 1, 2026), the title has been updated to "Subvisible Particulate Matter in Injections," emphasizing the precise characterization of this contamination type and highlighting its classification as contamination rather than merely "matter" [31]. This evolving regulatory landscape, coupled with the growing adoption of single-use technologies (SUTs) in bioprocessing, necessitates a comprehensive understanding of particulate contamination sources, detection methodologies, and control strategies to ensure the safety and efficacy of biologically derived products.
Regulatory Framework and Standards
USP 〈788〉 and International Guidelines
The United States Pharmacopeia (USP) general chapter 〈788〉 sets the foundational standards for particulate matter in injections, specifying two primary test methods: Light Obscuration Particle Count Test (Method 1) and Microscopic Particle Count Test (Method 2) [31]. The recently adopted revisions include significant changes that reflect industry evolution: the title has been modified to "Subvisible Particulate Matter in Injections," terminology has been updated (e.g., "aggregation" to "agglomeration"), and testing flexibility has been enhanced to accommodate modern biopharmaceutical products, including allowing single-unit testing and sample aliquots of 1-5 mL with justification for products with limited volume [31].
Internationally, the EU GMP Annex 1 (2022) provides complementary guidance with particular emphasis on monitoring ≥5.0 µm particles in Grade A and B cleanrooms [32]. Unlike classification activities, which establish the initial cleanroom state, Annex 1 emphasizes continuous monitoring to capture "interventions, transient events, and any system deterioration" [32]. This standard presents practical challenges, as monitoring often utilizes cubic foot measurements (rather than cubic meters), making the detection of even a single ≥5.0 µm particle potentially significant and requiring investigation [32].
Current Good Manufacturing Practice (CGMP) Requirements
Title 21 of the Code of Federal Regulations establishes the Current Good Manufacturing Practice (CGMP) requirements for finished pharmaceuticals, providing the legal framework for contamination control [33]. Key provisions relevant to particulate control include:
- §211.42 Design and construction features: Requires separate or defined areas to prevent contamination, with specific provisions for aseptic processing including "an air supply filtered through high-efficiency particulate air filters under positive pressure" and "a system for monitoring environmental conditions" [33].
- §211.46 Ventilation, air filtration: Mandates "equipment for adequate control over air pressure, micro-organisms, dust, humidity, and temperature" and requires that "air filtration systems, including prefilters and particulate matter air filters, shall be used when appropriate on air supplies to production areas" [33].
- §211.22 Responsibilities of quality control unit: Charges the quality control unit with responsibility and authority to approve or reject all components, drug product containers, closures, in-process materials, and drug products, ensuring comprehensive oversight of particulate control measures [33].
Table 1: Key Regulatory Standards for Particulate Control in GMP Manufacturing
| Regulatory Standard | Focus Area | Key Requirements | Recent Updates |
|---|---|---|---|
| USP 〈788〉 | Subvisible particulate matter in injections | • Sets limits for ≥10 µm and ≥25 µm particles• Specifies Light Obscuration and Microscopic Particle Count methods• Defines acceptance criteria for large and small volume parenterals | Title change to "Subvisible Particulate Matter in Injections" (effective Aug 2026); Allowance for single-unit testing and smaller aliquots with justification [31] |
| EU GMP Annex 1 | Cleanroom classification and monitoring | • Differentiates classification from monitoring• Emphasizes ≥5.0 µm particle monitoring in Grade A/B areas• Requires investigation of consecutive or regular counting of low-level macro particles | 2022 revision emphasizes continuous monitoring and quality risk management; Focus on particle emissions from equipment and processes [32] |
| 21 CFR Part 211 | Current Good Manufacturing Practice | • Defines facility and equipment requirements for contamination control• Establishes quality control unit responsibilities• Mandates appropriate air filtration systems | Foundational requirements with ongoing enforcement focus on contamination control [33] |
Particulate contamination in GMP manufacturing is systematically categorized based on its origin and nature. Understanding these classifications is essential for implementing effective control strategies.
Categorization by Origin
- Inherent Particles: Particles innate to a drug product, which may be considered acceptable according to its target product profile [30]. These are typically characterized and justified as part of product development.
- Intrinsic Particles: Particles introduced by the manufacturing process itself, potentially including rubber, glass, silicone, or other materials from processing equipment, single-use systems, or container-closure systems [30].
- Extrinsic Particles: Particles originating from outside the process, including hair, skin, dust, fibers, cleaning products, or other materials from personnel or the environment [30]. These represent breaches in contamination control systems.
Single-Use Technologies as a Particulate Source
The rapid adoption of single-use technologies (SUTs) in bioprocessing represents a significant particulate control challenge. While SUTs eliminate cleaning validation concerns and reduce cross-contamination risks between batches, they introduce unique particulate challenges [30]. Polymer-based solutions such as bags, tubing, transfer sets, and manifolds with overmolded designs can shed particles during assembly, shipping, or use. Unlike traditional stainless-steel systems that can be rinsed with water or air, SUTs "cannot undergo the same arduous chemical cleaning procedures" and "require more intensive protocols that involve vacuum systems and particulate traps" [30].
Environmental and Process-Generated Particles
Cleanroom operations generate particles from multiple sources, including:
- Personnel: Skin cells, hair, and clothing fibers introduced despite gowning procedures [11]
- Equipment: Wear particles from moving parts, shedding from seals and gaskets, and particles generated during maintenance interventions [11]
- Process Operations: Particles generated during component assembly, material transfers, and manipulations within the critical zone [32]
Detection and Monitoring Methodologies
Compendial Test Methods
USP 〈788〉 describes two primary methods for quantifying subvisible particles:
Method 1: Light Obscuration Particle Count Test This automated method determines particle size and concentration by measuring the light blocked by individual particles as they pass through a laser beam. The revised USP 〈788〉 allows greater flexibility in method application, including single-unit testing for both large- and small-volume parenterals and "easy sample preparation of protein products" to minimize interference from protein aggregates [31]. The method now also permits testing of sample aliquots of 1-5 mL, with justification for products that do not have a sufficient testing volume of 25 mL, and allows for the use of alternative diluents if justified [31].
Method 2: Microscopic Particle Count Test This manual method involves membrane filtration of a sample followed by microscopic examination and particle counting. The revised standard replaces "solution" with "sample" or "preparation" where appropriate, reflecting broader application beyond traditional solutions [31]. The evaluation criteria clarify that "the average number of particles in the pooled sample complies with the requirements" [31].
Table 2: Comparison of Particulate Detection Methods in GMP Manufacturing
| Method | Principle | Scope | Advantages | Limitations |
|---|---|---|---|---|
| Light Obscuration (USP 〈788〉 Method 1) | Measures light blocked by particles in a sensing zone | Subvisible particles (≥10 µm & ≥25 µm) in injections | • High-resolution, automated counting• Statistical robustness from high sample volume• Rapid analysis | • Potential interference from protein aggregates or air bubbles• Limited suitability for viscous solutions• Requires refractive index contrast |
| Microscopic Particle Count (USP 〈788〉 Method 2) | Membrane filtration and microscopic examination | Subvisible particles (≥10 µm & ≥25 µm) | • Direct visual confirmation• Suitable for colored/opaque solutions• Particle morphology characterization | • Time-consuming and labor-intensive• Lower statistical power due to smaller sample size• Subjectivity in operator interpretation |
| Environmental Monitoring | Continuous airborne particle counting | ≥0.5 µm and ≥5.0 µm particles in cleanrooms | • Real-time data on environment state• Trend analysis capability• Early warning of system deterioration | • Requires careful data interpretation to avoid false alarms• Correlation to product quality not always direct• Equipment calibration critical |
Cleanroom Monitoring Strategies
The EU GMP Annex 1 guideline emphasizes continuous monitoring of cleanrooms, particularly for ≥5.0 µm particles in Grade A and B areas [32]. This approach requires sophisticated strategies to balance sensitivity with practical operation:
- Extended Sampling Periods: Taking samples longer than one minute to reduce the multiplication factor and minimize false alarms from transient events [32]
- Rolling Averages: Responding based on a rolling average of several minutes' data rather than individual measurements [32]
- Rate of Occurrence Analysis: Focusing on the frequency of particle counts rather than single instances, similar to viable particle monitoring approaches in USP 1116 [32]
The ISPE Good Practice Guide: SMEPAC (Standardized Methodology for the Evaluation of Pharmaceutical Airborne Particle Emissions) provides a standardized framework for assessing equipment particle emissions, including complex systems such as continuous manufacturing equipment [34].
Emerging Monitoring Technologies
While not yet compendial, real-time monitoring approaches are emerging that detect volatile organic compounds (TVOC) as potential indicators of contamination events. Semiconductor-based sensors for TVOC, ammonia, and hydrogen sulfide show promise for early detection of bacterial contamination within a 2-hour window, potentially offering non-invasive, real-time monitoring capabilities [5].
Impact on Product Quality and Patient Safety
The risks posed by particulate contamination extend beyond regulatory non-compliance to potentially significant patient harm. The FDA's draft guidance on visible particulate control (December 2021) recommends establishing "a holistic, risk-based approach to visible particulate control that incorporates product development, manufacturing controls, visual inspection techniques, particulate identification, investigation, and corrective actions" [30].
For cell and gene therapies, the risk is particularly acute because "biologics-based therapies cannot be filtered, and therefore any particulates introduced to a therapy during manufacture or packaging cannot be removed" [30]. This limitation means that particles introduced during manufacturing remain in the final product, potentially leading to:
- Immunogenic reactions in patients
- Capillary occlusion from intravenous administration
- Inflammatory responses at injection sites
- Compromised therapeutic efficacy through physical interaction with cellular products
The regulatory expectation is that manufacturers should implement "more stringent limits may be more appropriate for individual products" than the general standards specified in USP 〈788〉 [31].
Mitigation Strategies and Control Systems
Comprehensive Particulate Control Program
Effective particulate control requires a systematic approach spanning the entire manufacturing lifecycle:
- Raw Material Control: SUT suppliers must "vet raw material suppliers" to understand their cleaning practices for raw materials, as many materials used in SUT fabrication are made using processes that introduce significant risk for increased extraneous particulate matter [30].
- Process Design: Implementing "one-piece flow" production approaches where multiple operators inspect each component as it is passed down the assembly line enables tighter control compared to traditional batch production processes [30].
- Facility and Equipment Controls: Using classified HEPA-filtered cleanrooms, proper gowning procedures, and environmental monitoring systems that meet or exceed ISO 14644 standards [11] [33].
- Closed Processing Systems: Implementing closed and single-use systems (SUS) to reduce contamination risks from open processing and complex cleaning validation [11].
Single-Use Technology Particulate Control
For single-use technology suppliers, comprehensive particulate control includes:
- Supply Chain Management: Regular assessment of every element of the single-use component supply chain, including raw materials received from suppliers, production facilities, and operator training [30]
- Facility Controls: Adhering to stringent cleanroom standards, often implementing ISO 5 gowning standards in ISO 7 facilities to meet customer requirements [30]
- Continuous Improvement: Establishing cross-functional teams dedicated to continuously evaluating manufacturing processes to identify areas of improvement, incorporating perspectives from manufacturing, engineering, customer-facing roles, and beyond [30]
The "Path to Zero" Initiative
Some industry leaders have adopted a "Path to Zero" initiative that takes a holistic approach to particulate control via continuous improvement techniques addressing:
- Best practices for gowning
- Monitoring environmental conditions
- Cleaning and inspection processes during production and for incoming raw materials
- Facility assessments
- Operator training programs
- Supplier management programs [30]
This approach acknowledges that while particulates can never be fully eliminated, continuous reduction is essential for advancing therapy safety.
Experimental Workflows for Particulate Control
The following workflow diagrams illustrate systematic approaches for particulate monitoring and contamination investigation in GMP manufacturing.
Particulate Monitoring and Investigation Workflow
Single-Use Technology Quality Assurance
Table 3: Research Reagent Solutions for Particulate Control Studies
| Tool/Reagent | Function | Application in Particulate Control |
|---|---|---|
| Light Obscuration Particle Counter | Quantifies size and concentration of subvisible particles | USP 〈788〉 Method 1 testing for injectable products; Environmental monitoring data collection |
| Microscopic Particle Count Setup | Membrane filtration and microscopic examination of particles | USP 〈788〉 Method 2 testing; Visual confirmation and morphological characterization of particles |
| Environmental Monitoring System | Continuous real-time monitoring of airborne particles | Cleanroom classification and monitoring per EU GMP Annex 1; Trend analysis for preventive maintenance |
| Single-Use Technology Components | Polymer-based bags, tubing, manifolds for bioprocessing | Evaluation of intrinsic particle generation; Compatibility studies with biological products |
| Reference Materials & Standards | Particle size standards for instrument calibration | Qualification and validation of particle counting equipment; Method verification |
| Quality Control Documentation | Standard Operating Procedures (SOPs), specifications | Establishing acceptance criteria; Investigation of deviations; Regulatory compliance |
Particulate contamination control represents a critical aspect of GMP manufacturing that intersects directly with cell culture contamination research. The evolving regulatory landscape, including the recently revised USP 〈788〉 and EU GMP Annex 1, emphasizes more sophisticated approaches to particle monitoring and control, particularly as advanced therapies like cell and gene treatments cannot incorporate final filtration steps [31] [30]. Effective management of non-viable particles requires a holistic, risk-based approach that encompasses raw material control, process design, environmental monitoring, and continuous improvement initiatives.
The scientific and regulatory focus has shifted from merely detecting particles to understanding their origin, preventing their introduction, and implementing robust control strategies throughout the product lifecycle. As the industry continues to advance toward more complex biological products and manufacturing technologies, the imperative for comprehensive particulate control strategies will only intensify. By integrating the methodologies, standards, and approaches outlined in this technical guide, researchers, scientists, and drug development professionals can effectively mitigate particulate contamination risks and ensure the production of safe, high-quality biological products.
Detecting the Undetectable: Methodologies for Contamination Identification and Analysis
In cell culture-based research and drug development, contamination represents one of the most persistent and costly challenges, with the potential to compromise experimental validity, product safety, and research reproducibility. Within the broader context of contamination research, visual inspection and microscopy serve as the first line of defense—the fundamental techniques that enable researchers to identify biological invaders before they jeopardize months of work. While some contaminants remain invisible to standard microscopy, many present telltale signs that, when recognized early, can prevent widespread laboratory contamination.
This technical guide provides a comprehensive framework for recognizing early contamination signs through visual inspection and microscopy, detailing the morphological characteristics of common contaminants, and presenting standardized protocols for detection and confirmation. By integrating these practices into routine cell culture maintenance, researchers can significantly reduce the risk of contaminant-driven experimental artifacts and contribute to more robust, reproducible scientific outcomes.
Recognizing Contaminants: Morphological Characteristics and Visual Cues
Bacterial Contamination
Bacterial contamination is among the most common issues in cell culture laboratories due to the ubiquity, small size, and rapid growth rate of bacterial cells [29]. Visual identification typically becomes apparent within a few days of infection.
Key identification features include:
- Macroscopic appearance: Cloudy or turbid culture medium, sometimes with a thin film on the surface [29] [3]. The medium may turn yellow due to a sudden drop in pH caused by bacterial metabolic byproducts [3] [2].
- Microscopic appearance: Under low-power microscopy, bacteria appear as tiny, moving granules between cells. Higher magnification reveals their distinct shapes—spheres (cocci), rods (bacilli), or spirals [29]. This movement between adherent cells is often described as a "shimmering" or "quicksand-like" effect [2].
Table 1: Characteristics of Bacterial Contamination
| Characteristic | Description |
|---|---|
| Medium Turbidity | Cloudy appearance within 2-3 days of contamination |
| pH Change | Sudden drop in pH (yellow color with phenol red indicator) |
| Common Shapes | Cocci (spherical), bacilli (rod-shaped), spirilla (spiral) |
| Size Range | Typically 0.5-5 μm |
| Motility | Tiny, moving particles between cells |
Fungal Contamination: Yeasts and Molds
Fungal contaminants encompass both unicellular yeasts and multicellular molds, which can enter cultures through airborne spores or contaminated surfaces [3].
Yeast contamination identification:
- Macroscopic appearance: Culture medium becomes turbid, especially in advanced stages. Unlike bacterial contamination, the pH typically remains stable initially, only increasing when contamination becomes heavy [29] [3].
- Microscopic appearance: Yeasts appear as individual ovoid or spherical particles that may bud off smaller particles as they replicate [29]. Their size ranges from a few micrometers up to 40μm [29].
Mold contamination identification:
- Macroscopic appearance: Visible floating colonies often appearing as white, green, or dark patches with a "fuzzy" or filamentous texture [3]. The medium may become cloudy as contamination progresses.
- Microscopic appearance: Mold presents with thin, wisp-like filaments called hyphae, which form a network known as mycelium. Denser clumps of spores may also be visible [29].
Table 2: Characteristics of Fungal Contamination
| Characteristic | Yeasts | Molds |
|---|---|---|
| Medium Appearance | Turbid, especially in advanced stages | Fuzzy colonies, cloudy medium |
| pH Change | Stable initially, increases later | Stable initially, increases with heavy contamination |
| Structural Features | Ovoid/spherical cells, budding | Filamentous hyphae, mycelium, spores |
| Size Range | Few μm to 40μm | Hyphae can extend hundreds of μm |
| Growth Pattern | Unicellular, budding | Multicellular, filamentous |
Mycoplasma Contamination
Mycoplasma represents one of the most insidious biological contaminants due to its small size (0.15-0.3 μm) and lack of a cell wall, making it resistant to many common antibiotics and difficult to detect with standard microscopy [35] [2].
Identification challenges and clues:
- Macroscopic appearance: No visible change in medium clarity or color, allowing contamination to persist undetected without specific testing [3] [35].
- Microscopic appearance: May appear as tiny black dots under phase contrast microscopy, but often shows no direct visual evidence [2]. Indirect signs include slowed cell growth, abnormal cell morphology, unexplained changes in metabolic activity, and reduced transfection efficiency [3] [35].
- Confirmation requires specialized testing including PCR, DNA staining, ELISA, or microbial culture techniques specifically designed for mycoplasma detection [3] [35].
Viral Contamination
Viral contamination presents unique detection challenges due to the submicroscopic size of viruses and their dependence on host cell machinery for replication [29] [14].
Identification approaches:
- Direct visualization: Not possible with standard light microscopy; requires electron microscopy [29].
- Cytopathic effects (CPE): Some viruses cause visible morphological changes in host cells, including cell rounding, detachment, syncytia formation (cell fusion), and lysis [14].
- Detection methods: PCR-based assays, immunofluorescence, ELISA, or plaque assays are typically required for definitive identification [29] [3].
Contamination Identification Workflow
The following diagram illustrates the systematic process for identifying and confirming cell culture contamination through visual inspection and subsequent testing methods:
Advanced Detection Methodologies and Experimental Protocols
Mycoplasma Detection Protocol
Mycoplasma contamination requires specialized detection methods due to its small size and lack of visual indicators. Multiple standardized approaches exist:
DNA Fluorescence Staining Method:
- Principle: DNA-binding dyes (e.g., DAPI or Hoechst) stain both mammalian and mycoplasma DNA, revealing mycoplasma as extranuclear fluorescent spots [35].
- Procedure:
- Grow cells on sterile coverslips in culture dishes until subconfluent
- Fix cells with fresh Carnoy's fixative (methanol:glacial acetic acid, 3:1) for 5 minutes
- Stain with DNA-binding dye (e.g., 1 μg/mL Hoechst 33258 in PBS) for 15-30 minutes
- Mount coverslips and examine under fluorescence microscopy with appropriate filters
- Interpretation: Uninfected cells show only nuclear fluorescence; mycoplasma-contaminated cultures display fine, particulate fluorescence throughout the cytoplasm and surrounding cells [35].
PCR-Based Detection:
- Principle: Amplifies specific mycoplasma DNA sequences using genus-specific primers [3] [35].
- Procedure:
- Collect conditioned medium from test cultures by centrifugation
- Extract DNA from pellet using standard molecular biology techniques
- Perform PCR with mycoplasma-specific primers targeting 16S rRNA genes
- Analyze amplification products by gel electrophoresis
- Advantages: High sensitivity, can detect multiple mycoplasma species, and provides rapid results [3].
Comprehensive Testing Workflow
For rigorous contamination screening, especially when working with valuable cell lines or preparing for critical experiments, follow this comprehensive testing methodology:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Contamination Detection and Prevention
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Phase Contrast Microscope | Routine examination of cell health and contamination | 100-400x magnification for detecting bacteria/fungi [29] |
| DNA-binding Dyes (DAPI/Hoechst) | Mycoplasma detection via fluorescence microscopy | Reveals extranuclear DNA staining pattern [35] |
| Mycoplasma Detection Kits | Specific detection of mycoplasma contamination | Available as PCR-based or enzyme activity assays [2] |
| Selective Culture Media | Microbial contamination identification | Supports growth of bacteria/fungi while inhibiting mammalian cells |
| Penicillin-Streptomycin Solution | Antibiotic combination to control bacterial growth | Use short-term only; can mask low-level contamination [29] |
| Amphotericin B | Antifungal agent for yeast/mold control | Use with caution due to potential cellular toxicity [2] |
| Mycoplasma Removal Agents | Treatment of confirmed mycoplasma contamination | Specific antibiotics targeting mycoplasma [2] |
| Ethanol (70%) | Surface and equipment decontamination | More effective than higher concentrations [6] |
| Bleach (10%) | Decontamination of discarded cultures | Effective against most biological contaminants [6] |
| Filter Tips | Prevention of cross-contamination during pipetting | Essential when working with multiple cell lines [6] |
Prevention and Decontamination Strategies
Aseptic Technique Fundamentals
Preventing contamination requires rigorous aseptic technique, including working in properly maintained laminar flow hoods, using personal protective equipment, and thoroughly disinfecting all surfaces and materials with 70% ethanol before use [6]. Additional critical practices include handling only one cell line at a time, using filter tips to prevent aerosol cross-contamination, and clearly labeling all vessels with cell line name, date, and passage number [3] [6].
Antibiotic Use Policy
The routine use of antibiotics in cell culture is discouraged as it can promote antibiotic-resistant strains, mask low-level contamination (particularly mycoplasma), and potentially interfere with cellular processes under investigation [29] [3]. When absolutely necessary, antibiotics should be used for short durations and removed from culture as soon as possible, with antibiotic-free cultures maintained in parallel as controls [29].
Decontamination Protocol for Irreplaceable Cultures
When facing contamination of valuable or irreplaceable cultures, this systematic decontamination approach may be attempted:
- Contaminant Identification: First, determine whether the contamination is bacterial, fungal, yeast, or mycoplasma [29]
- Culture Isolation: Immediately quarantine the contaminated culture from other cell lines [29]
- Environmental Decontamination: Thoroughly clean incubators and laminar flow hoods with laboratory disinfectants, and check HEPA filters [29]
- Toxicity Testing: Dissociate, count, and dilute cells in antibiotic-free medium, then dispense into multi-well plates with a range of antibiotic concentrations to determine toxicity thresholds [29]
- Treatment Phase: Culture cells for 2-3 passages using antibiotics at concentrations one- to two-fold lower than the toxic level [29]
- Post-Treatment Assessment: Culture cells in antibiotic-free medium for 4-6 passages to verify elimination of contamination [29]
Visual inspection and microscopy remain indispensable tools in the ongoing challenge of cell culture contamination control. While not all contaminants are visible through standard microscopy, systematic observation of both macroscopic culture characteristics and microscopic cellular morphology provides the foundation for early detection and intervention. When integrated with modern molecular detection methods and rigorous aseptic technique, these approaches form a comprehensive contamination management strategy essential for research reproducibility and experimental validity.
The rising sophistication of cell culture applications—from CRISPR-edited lines to organoid models—further underscores the necessity of robust contamination monitoring protocols. By mastering visual recognition of early contamination signs and implementing systematic detection methodologies, researchers can protect valuable experiments and contribute to the overall integrity of biomedical science.
Cell culture contamination represents a significant threat to research integrity and biopharmaceutical production. Among contaminants, mycoplasma and viruses are particularly problematic due to their small size and often cryptic nature. Mycoplasma contamination affects an estimated 15-35% of continuous cell cultures, while viral contaminants have been reported in over 25% of common cell lines [8] [36]. These contaminants can alter virtually all aspects of cell physiology, including chromosomal aberrations, disruption of nucleic acid synthesis, changes in membrane antigenicity, inhibition of cell proliferation, and altered gene expression profiles [8]. The insidious nature of these contaminants necessitates robust, sensitive detection methods that can identify contamination before experimental outcomes are compromised. Molecular techniques, particularly PCR and qPCR, have emerged as powerful tools for detecting these contaminants with the sensitivity, specificity, and speed required by modern biotechnology and pharmaceutical industries.
Mycoplasma Detection: PCR and qPCR Methodologies
Technical Approaches and Primer Design
Modern PCR-based mycoplasma detection methods leverage conserved genomic regions to achieve broad species coverage. The 16S rRNA gene and the 16S-23S rRNA intergenic spacer region serve as ideal targets due to their presence across mycoplasma species with conserved sequences suitable for primer design [37]. Recent advancements have demonstrated that a single qPCR assay can specifically detect eleven mycoplasma species relevant to pharmacopoeia standards using only two primers and two hydrolysis probes, significantly streamlining laboratory operations [38]. This comprehensive approach detects major contaminating species including M. arginini, M. fermentans, M. hominis, M. hyorhinis, M. orale, M. pirum, M. salivarium, and A. laidlawii, which account for approximately 95% of all mycoplasma contamination in cell culture [8].
While primers may exhibit cross-reactivity with bacterial species, the specificity conferred by hydrolysis probes allows for confident interpretation of qPCR results and unambiguous statement regarding mycoplasma presence in test articles [38]. This technical refinement addresses a critical need in quality control laboratories embedded in biologics production sites, which must provide results in a timely manner and contribute to root cause analysis in case of contamination.
Performance Metrics and Validation
Recent validation studies demonstrate substantial improvements in mycoplasma detection methods. Universal PCR, basic ERA (Enzymatic Recombinase Amplification), and qPCR assays targeting the 16S-23S rRNA intergenic spacer region have shown exceptional specificity, accurately identifying 16 different Mycoplasma species while exhibiting no cross-reactivity with common cell culture contaminants including bacteria, viruses, and fungi [37].
Table 1: Performance Comparison of Mycoplasma Detection Methods
| Method | Detection Limit | Detection Time | Key Advantage | Compliance |
|---|---|---|---|---|
| Direct Culture | N/A | 4-5 weeks | Gold standard, visual confirmation | Pharmacopoeia |
| Indirect Culture | N/A | 3-4 weeks | DNA staining, fluorescent detection | Pharmacopoeia |
| Conventional PCR | 10¹ copies | 1-2 hours | Broad species detection | EU Pharmacopoeia 2.6.7 |
| qPCR | 10⁻¹ copies | 1-2 hours | Quantitative, superior sensitivity | Pharmacopoeia compliant |
| ERA | 10⁰ copies | 1-2 hours | Isothermal, equipment simple | Validation in progress |
These novel methods achieved 17% (PCR), 36.8% (ERA), and 40.6% (qPCR) higher detection rates than conventional approaches while reducing testing time from several weeks to just 1-2 hours [37]. The dramatic improvement in sensitivity is particularly valuable for detecting fastidious mycoplasma species that grow poorly in vitro, addressing a significant limitation of pharmacopeial testing standards.
Viral Detection: PCR and qPCR Applications
Technical Considerations for Viral Pathogens
Viral contamination presents unique detection challenges due to the diversity of viral pathogens, their potential latency, and the absence of visual indicators in cell cultures [3]. PCR and qPCR methods for viral detection must account for RNA genomes (requiring reverse transcription), sequence variability, and potentially low copy numbers. Reverse transcription quantitative PCR (RT-qPCR) has long been the gold standard for detecting RNA viruses such as influenza A and B, respiratory syncytial virus (RSV), and SARS-CoV-2 [39]. These methods typically target conserved viral genes with primer-probe sets designed to minimize cross-reactivity while maintaining broad detection capabilities across viral strains.
Multiplex qPCR formats enable simultaneous detection of multiple viral targets in a single reaction, a critical capability during periods of co-circulation such as the 2023-2024 "tripledemic" when influenza A (H1N1 and H3N2), influenza B, RSV, and SARS-CoV-2 co-circulated, placing considerable strain on healthcare systems worldwide [39]. The ability to precisely quantify viral load provides critical insights into infection dynamics, including disease severity, transmissibility, and treatment response.
Digital PCR: Emerging Advancements
Digital PCR (dPCR) has emerged as a robust alternative to traditional qPCR, offering absolute quantification without standard curves by partitioning the PCR mixture into thousands of individual reactions [39]. Recent comparative studies demonstrate dPCR's superior accuracy, particularly for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV [39]. dPCR platforms such as droplet digital PCR (ddPCR) and nanowell-based systems (e.g., QIAcuity) offer distinct methodologies for reaction partitioning, with the latter facilitating high-throughput processing and seamless integration with automated workflows.
Table 2: Comparison of PCR-Based Viral Detection Platforms
| Platform | Quantification Method | Sensitivity | Throughput | Best Application |
|---|---|---|---|---|
| Conventional PCR | Endpoint detection | Moderate | Low | Qualitative detection |
| Real-Time RT-qPCR | Relative quantification via Ct values | High | High | Routine diagnostics, screening |
| Digital PCR | Absolute quantification by partitioning | Very High | Medium | Low viral load, precise quantification |
| Multiplex PCR | Varies by platform | High | High | Co-infections, pathogen panels |
The precision of dPCR becomes particularly valuable in co-infection scenarios where multiple viral genomes in a single sample, combined with complex respiratory matrices containing mucus and cellular debris, may differentially affect amplification efficiency in qPCR assays, resulting in inconsistent Ct values and reduced quantification reliability [39].
Experimental Protocols
Sample Preparation and Nucleic Acid Extraction
Proper sample preparation is fundamental to successful mycoplasma and viral detection. For cell culture supernatants, collect 1-2 mL and centrifuge at 13,000 × g for 10 minutes to pellet particulate matter [38] [37]. For adherent cells, include both supernatant and trypsinized cells after confirming absence of antibiotics. Nucleic acid extraction should be performed using automated systems such as the KingFisher Flex system with the MagMax Viral/Pathogen kit or the STARlet Seegene automated platform with the STARMag 96 X 4 Universal Cartridge Kit [39] [37]. Include internal extraction controls to monitor extraction efficiency and potential inhibition.
qPCR Assay Protocol for Mycoplasma Detection
The following protocol is adapted from recent pharmacopoeia-compliant approaches [38] [37]:
Reaction Setup: Prepare 20 μL reactions containing 1× master mix, 400 nM of each primer, 200 nM of each hydrolysis probe, and 5 μL of template DNA.
Thermocycling Conditions:
- Initial denaturation: 95°C for 5 minutes
- 45 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (with fluorescence acquisition)
Data Analysis: Determine cycle threshold (Ct) values. Samples with Ct values ≤ 35 are considered positive, while values between 35-40 require retesting. Include positive controls (mycoplasma genomic DNA) and negative controls (nuclease-free water) in each run.
For viral detection, incorporate a reverse transcription step prior to PCR amplification using reverse transcriptase at 50°C for 30 minutes [39].
Quality Control and Validation
Implement rigorous quality control measures including:
- Positive controls: Quantified genomic DNA from target mycoplasma or viral species
- Inhibition controls: Spike internal controls into samples to detect PCR inhibition
- Cross-reactivity testing: Validate against non-target species to ensure specificity
- Limit of detection: Establish using serial dilutions of target nucleic acids
For biologics production, validation should comply with relevant pharmacopoeia guidelines (e.g., European Pharmacopoeia 2.6.7) [38] [8].
Workflow Visualization
Contamination Prevention and Quality Control
Effective contamination management requires a comprehensive approach integrating prevention, detection, and corrective actions. Prevention strategies include strict aseptic techniques, quarantining new cell lines, using certified reagents, and avoiding routine antibiotic use which can mask low-level contamination [36] [40] [3]. Regular monitoring through PCR-based testing should be implemented at critical control points throughout production processes.
For biopharmaceutical manufacturing, the integration of PCR testing into quality systems provides a rapid method for detecting mycoplasma and viral contaminants, enabling timely intervention before products are compromised [38]. This is particularly important given that mycoplasma contamination of biologics intended for human use poses potential safety risks for patients and presents serious economic risks for manufacturers in the event of batch adulteration or product recall [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for PCR-Based Contamination Detection
| Reagent/Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Positive Controls | Mycoplasma genomic DNA (M. pneumoniae, M. hominis), Titered reference strains | Assay development, calibration, run controls | Select species relevant to contamination profile; quantify precisely |
| Nucleic Acid Extraction Kits | MagMax Viral/Pathogen kit, STARMag Universal Cartridge Kit | Nucleic acid purification, inhibitor removal | Automated compatibility; internal control inclusion |
| PCR Master Mixes | Probe-based qPCR master mixes, Multiplex PCR kits | Enzymes, buffers, nucleotides for amplification | Compatibility with platform; inhibitor resistance |
| Primer/Probe Sets | Custom designs targeting 16S-23S rRNA ISR, Commercial mycoplasma detection kits | Specific target recognition and amplification | Pharmacopoeia compliance; species coverage validation |
| Reference Materials | Quantitative genomic DNA, Certified reference materials | Assay development, standardization, quality control | Traceability to reference standards; stability documentation |
PCR and qPCR methodologies have revolutionized mycoplasma and viral detection in cell culture systems, offering unprecedented sensitivity, specificity, and speed compared to traditional culture-based methods. The development of universal detection systems capable of identifying multiple contaminant species with minimal reaction components represents a significant advancement for quality control laboratories in research and biopharmaceutical settings [38] [37]. As molecular technologies continue to evolve, with digital PCR and isothermal amplification methods offering new capabilities, the capacity to safeguard cell cultures from these insidious contaminants will further improve. Implementation of these molecular techniques within comprehensive quality management systems provides the foundation for reliable research outcomes and safe biopharmaceutical products.
Microbial Culture and Staining Methods for Bacteria and Fungi
In the context of cell culture research, microbial contamination represents a significant and persistent challenge that can compromise experimental integrity and lead to erroneous conclusions. Biological contaminants, primarily bacteria and fungi, are ubiquitous in laboratory environments and can be inadvertently introduced at any stage of the culture process. Estimates suggest that 5-30% of cell cultures are contaminated with支原体 (mycoplasma) alone, while bacterial and fungal contaminants collectively affect a substantial proportion of cultures [41]. Understanding the methods to culture and identify these microorganisms is therefore fundamental to maintaining sterile conditions and ensuring research reproducibility, particularly in pharmaceutical development where compromised cell lines can have far-reaching consequences.
The economic and scientific costs of microbial contamination are considerable, resulting in lost time, wasted resources, and unreliable data. Different types of contaminants present distinct challenges in detection and eradication. While some cause rapid culture destruction, others, known as "cryptic contaminants," persist with minimal obvious signs while subtly altering host cell physiology and experimental outcomes [41] [42]. This guide provides comprehensive methodologies for detecting, identifying, and addressing the most common bacterial and fungal contaminants in cell culture systems.
Identification of Common Microbial Contaminants
Bacterial Contamination
Bacteria are prokaryotic, ubiquitous microorganisms typically measuring a few micrometers in diameter. In cell culture, bacterial contamination manifests through several characteristic signs:
- Visual and macroscopic indicators: Rapid turbidity (cloudiness) of the culture medium, often accompanied by a sudden drop in pH (manifested as a color change in phenol red-containing media to yellow) [42] [29].
- Microscopic appearance: Under low-power microscopy, bacteria appear as tiny, shimmering granules exhibiting Brownian motion between cultured cells. Higher magnification (1000x) reveals their distinct morphological shapes (cocci, bacilli, etc.) [29].
- Time course: Bacterial populations can expand exponentially, often reaching detectable levels within 48-72 hours post-contamination [42].
Common bacterial contaminants in cell culture include Gram-positive organisms such as Staphylococcus spp. and Bacillus spp., and Gram-negative organisms such as Escherichia coli and Pseudomonas aeruginosa [42].
Fungal Contamination
Fungal contaminants, including yeasts and molds, represent another major category of cell culture invaders:
- Yeast contamination: Unicellular fungi that appear as spherical or ovoid particles under microscopy, often observed in the process of budding (producing smaller daughter cells). Initially, the culture pH remains stable, but becomes alkaline with heavy overgrowth. The medium typically becomes turbid, similar to bacterial contamination [42] [29].
- Mold contamination: Multicellular fungi that form filamentous structures called hyphae. Under microscopy, these appear as thin, wispy, branching filaments that may form dense clumps of spores. Contamination often presents as floating fuzzy or fuzzy colonies visible to the naked eye, while the medium may remain clear initially [42] [29].
- Reproductive resilience: A significant challenge with fungal contaminants is their ability to produce spores that are resistant to harsh environmental conditions, enabling survival in dormant states until encountering favorable growth conditions [29].
Staining Methods for Microbial Detection and Identification
Bacterial Smear Preparation
Proper smear preparation is fundamental to accurate microscopic evaluation:
- Labeling: Label a clean glass slide with a wax marker [43].
- Sample application: If working with a broth culture, apply a small loopful directly to the slide. For agar cultures, place a drop of saline on the slide first, then emulsify a small amount of bacterial colony in the saline [43].
- Spreading: Spread the mixture to form a thin, even film over a small area of the slide [43].
- Air drying: Allow the smear to air dry completely at room temperature [43].
- Heat fixation: Pass the slide slowly through a Bunsen burner flame 2-3 times. This critical step kills the bacteria, adheres them to the slide, and makes them more permeable to stains. Avoid excessive heat which can distort cellular morphology [43].
Simple Staining
Simple staining employs a single basic dye to visualize microbial morphology against a contrasting background. Methylene blue is commonly used for this purpose in cell culture monitoring [43].
Protocol:
- Prepare and heat-fix a bacterial smear as described above.
- Flood the smear with methylene blue solution and incubate for the prescribed time (typically 30-60 seconds).
- Gently rinse with distilled water to remove excess stain.
- Blot dry with bibulous paper and examine under oil immersion (1000x magnification) [43].
Interpretation: This method allows for clear visualization of basic cellular shapes (cocci, bacilli) and arrangement patterns, but does not differentiate between bacterial types [43].
Gram Staining
The Gram stain remains the fundamental differential staining technique for bacterial classification, dividing bacteria into Gram-positive and Gram-negative groups based on cell wall structure differences. This distinction is valuable for identifying contamination sources and selecting appropriate decontamination strategies.
Reagents:
- Crystal violet (primary stain)
- Gram's iodine (mordant)
- Ethanol or acetone (decolorizer)
- Safranin (counterstain)
Protocol:
- Prepare and heat-fix a bacterial smear.
- Flood with crystal violet for 30-60 seconds, then rinse gently with water.
- Apply Gram's iodine for 30-60 seconds, then rinse.
- Decolorize with 95% ethanol or acetone for 5-15 seconds—this is the most critical step. Rinse immediately.
- Counterstain with safranin for 30-60 seconds, then rinse.
- Blot dry and examine under oil immersion [43].
Interpretation:
- Gram-positive bacteria: Appear purple/violet due to retention of the crystal violet-iodine complex within their thick peptidoglycan layer.
- Gram-negative bacteria: Appear pink/red as their thinner peptidoglycan layer allows decolorization, permitting uptake of the safranin counterstain.
Fungal Staining Methods
Fungal elements in cell culture can be detected using several specialized staining approaches:
Potassium Hydroxide (KOH) Preparation: KOH clears cellular material while preserving fungal structures, making it particularly useful for clinical specimens [44].
Fluorescent Staining: Fluorescent dyes such as calcofluor white or blankophor bind to fungal cell wall polymers (chitin and cellulose), producing fluorescence under UV light. This method offers high sensitivity for detecting sparse fungal elements [44].
Histochemical Stains:
- Gomori Methenamine Silver (GMS): Stains fungal cell walls black against a green background.
- Periodic Acid-Schiff (PAS): Stains fungal carbohydrates magenta [44].
For general cell culture monitoring, the same DNA-binding fluorescent dyes used for mycoplasma detection (e.g., Hoechst 33258) can reveal fungal nuclei when examined by fluorescence microscopy [41] [42].
Advanced Detection and Culture Methods
Culture-Based Detection
Culture remains the gold standard for detecting viable microorganisms despite the emergence of molecular methods:
Liquid Culture (Broth)
- Purpose: Enrichment and amplification of microbial populations.
- Methodology: Inoculate samples into nutrient broth (e.g., tryptic soy broth) and incubate at appropriate temperatures. Monitor daily for turbidity indicating microbial growth [45].
Solid Culture (Agar)
- Purpose: Isolation, quantification, and preliminary identification based on colony morphology.
- Methodology: Streak samples on nutrient agar plates (e.g., blood agar, Sabouraud dextrose agar for fungi) to obtain isolated colonies. Incubate and examine for characteristic colonies [44] [45].
For comprehensive environmental monitoring in cell culture facilities, settle plates (agar plates exposed to the air for specified periods) can assess airborne contamination levels [46] [45].
Molecular Detection Methods
Molecular techniques provide rapid, sensitive alternatives to traditional culture methods:
PCR-Based Detection:
- Amplifies species-specific DNA sequences.
- Particularly valuable for detecting fastidious organisms like mycoplasma and slow-growing fungi.
- Can identify contaminants that escape visual detection [41] [42] [47].
DNA Fluorescence Staining:
- Uses DNA-binding dyes (e.g., Hoechst 33258, DAPI) that fluoresce upon binding DNA.
- Effective for detecting mycoplasma and other epicellular contaminants.
- Stained preparations reveal characteristic particulate or filamentous fluorescence patterns outside mammalian cells when viewed by fluorescence microscopy [41] [42].
Understanding contamination sources is essential for prevention. The table below summarizes major contamination sources and corresponding control strategies.
Table: Microbial Contamination Sources and Control Strategies in Cell Culture
| Source Category | Specific Sources | Prevention and Control Strategies |
|---|---|---|
| Personnel | Skin, hair, breath, improper aseptic technique [46] [48] | Strict PPE use (lab coats, gloves, masks); thorough hand disinfection; minimal conversation in BSC [46] [47] |
| Laboratory Environment | Unfiltered air, dust, contaminated surfaces [46] [48] | HEPA filtration; regular disinfection; proper cleanroom design/maintenance [46] [45] |
| Equipment & Supplies | Non-sterile media/reagents, improperly sterilized equipment [46] [48] | Validate sterilization protocols; filter-sterilize heat-sensitive reagents; source reagents from certified suppliers [41] [45] |
| Cross-Contamination | Working with multiple cell lines simultaneously, contaminated incubators [46] [48] | Dedicated media per cell line; avoid simultaneous opening of vessels; regular incubator decontamination [46] [45] |
Visual Workflows for Contamination Identification and Management
Microbial Contamination Identification Workflow
Gram Staining Procedure Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Table: Essential Research Reagents for Microbial Detection in Cell Culture
| Reagent/Equipment | Primary Function | Application Notes |
|---|---|---|
| Microscope with 1000X magnification | Visualization of microbial contaminants | Phase contrast preferred for live observation; oil immersion required for bacterial morphology [42] [43] |
| Gram Stain Kit | Differential bacterial classification | Contains crystal violet, iodine, decolorizer, safranin; critical for identifying contamination source [43] |
| DNA Fluorescent Dyes (Hoechst/DAPI) | Detection of mycoplasma and fungal elements | Requires fluorescence microscopy; reveals extranuclear DNA patterns characteristic of epicellular contaminants [41] [42] |
| Culture Media (Broth & Agar) | Microbial amplification and isolation | Tryptic soy broth/agar for bacteria; Sabouraud dextrose for fungi; used for sterility testing [45] |
| Selective Antibiotics | Contamination control in valuable cultures | Penicillin/streptomycin for bacteria; amphotericin B for fungi; use sparingly to avoid cryptic contamination [42] [45] |
| HEPA-filtered Biological Safety Cabinet | Primary sterile working environment | Must be certified annually; proper airflow maintenance critical for protecting cultures and personnel [41] [46] |
Vigilant monitoring through appropriate microbial culture and staining techniques forms the cornerstone of effective cell culture contamination control. The integration of traditional methods (Gram staining, culture) with modern molecular approaches provides a robust defense against the diverse microorganisms that threaten research integrity. As contamination sources are multifaceted—spanning personnel, environment, equipment, and reagents—a systematic, comprehensive approach to detection and prevention is essential. For researchers in drug development and basic science, mastering these fundamental techniques ensures not only the reliability of their own findings but also contributes to the broader reproducibility of scientific research that depends on uncontaminated cellular models.
Cell culture contamination represents one of the most persistent and costly challenges in biomedical research and biopharmaceutical production, compromising data integrity, therapeutic safety, and regulatory compliance. Contaminants span multiple categories—including biological (bacteria, mycoplasma, viruses), chemical (endotoxins, media components), and physical (microplastics, particulate matter)—each requiring specialized detection approaches [11] [3]. Traditional methods like visual inspection and light microscopy offer limited sensitivity, failing to detect subvisible particles, nanoplastic fragments, or latent viral contaminants that can profoundly alter cellular function and experimental outcomes [49] [50].
Advanced analytical technologies have emerged as essential tools for comprehensive contamination identification, characterization, and source tracking. Spectroscopy, scanning electron microscopy (SEM), and specialized particle analysis platforms enable researchers to move from simple detection to sophisticated contaminant analysis, providing critical information about elemental composition, morphological features, and molecular signatures [51] [49]. These technologies are particularly valuable for investigating subtle contamination events that evade conventional screening methods yet significantly impact cell viability, differentiation potential, and genetic stability [50]. This technical guide explores the principles, applications, and methodological protocols for these advanced tools within the context of cell culture contamination research, providing researchers with a framework for implementing these technologies in quality control workflows.
Core Analytical Technologies: Principles and Applications
Scanning Electron Microscopy (SEM) with Energy-Dispersive X-ray Spectroscopy (EDS)
SEM provides high-resolution, topographical imaging of contaminants at the micro- and nanoscale, while EDS delivers simultaneous elemental composition analysis [51]. This combined approach is particularly valuable for characterizing inorganic particulates, identifying material defects in bioprocessing equipment, and detecting subvisible particles that can compromise biotherapeutic products.
The fundamental operating principle involves scanning a focused electron beam across the sample surface, generating signals including secondary electrons for topological contrast and backscattered electrons for compositional information. When the electron beam interacts with the sample, it displaces inner-shell electrons, causing outer-shell electrons to release energy as characteristic X-rays during transition to fill the vacancies [51]. EDS detects these X-rays, providing elemental identification and semi-quantitative composition data. This combined approach enables researchers to differentiate contamination sources—such as stainless steel particles from bioreactor components versus silicon fragments from tubing—based on both morphological features and elemental signatures [51].
Spectroscopic Techniques for Molecular Characterization
Spectroscopic methods analyze the interaction between matter and electromagnetic radiation to determine molecular structure and composition of contaminants. Different spectroscopic techniques provide complementary information for contaminant identification:
- Fourier Transform Infrared Spectroscopy (FTIR) identifies organic materials and polymers by detecting characteristic molecular vibrations and chemical functional groups, with different plastic polymers (e.g., polyethylene, polypropylene, polystyrene) displaying distinct infrared absorption signatures [52]. This technique has been successfully applied to characterize microplastic contamination in cell culture systems and environmental samples [52].
- Raman Spectroscopy provides molecular fingerprinting based on inelastic light scattering, effectively complementing FTIR for analyzing biological contaminants and crystalline structures [49].
- Attenuated Total Reflectance-FTIR enhances analysis of complex samples by limiting penetration depth, improving signal quality for surface contamination characterization [53].
These spectroscopic methods are particularly valuable for identifying chemical contaminants, polymer-based particulates, and organic residues that may affect cell culture systems.
Specialized Particle Analysis Systems
Advanced particle characterization systems employ multiple detection modalities to quantify and identify subvisible particles in biopharmaceutical products and cell cultures. These platforms combine Backgrounded Membrane Imaging (BMI), Fluorescence Membrane Microscopy (FMM), and Side Illumination Membrane Imaging (SIMI) to provide comprehensive particulate analysis [49].
BMI utilizes high-contrast imaging technology that first captures a background image of the membrane filter, then images the same membrane after sample filtration, and digitally subtracts the background to reveal particles with exceptional clarity [49]. When combined with FMM, which employs specific fluorescent dyes or antibodies to label biological components, researchers can distinguish protein aggregates from other particulate contaminants [49]. SIMI further enhances detection capability by identifying high-refractive-index particles like glass or plastic fragments, and light-absorbing metallic particles [49]. These integrated approaches are particularly valuable for biotherapeutic development, where regulatory standards (USP <788>) strictly limit subvisible particle counts in injectable products [49].
Quantitative Comparison of Analytical Techniques
Table 1: Technical Specifications and Applications of Advanced Analytical Tools
| Technique | Detection Principle | Size Range | Information Obtained | Primary Applications in Contamination Control |
|---|---|---|---|---|
| SEM-EDS | Electron beam-sample interaction + X-ray detection | 1 nm - 100 µm | High-resolution morphology, elemental composition | Inorganic particulate identification, material defect analysis, source tracking [51] |
| FTIR Spectroscopy | Molecular bond vibrations | >500 nm | Chemical functional groups, polymer identification | Organic contaminant characterization, microplastic detection [52] |
| Raman Spectroscopy | Inelastic light scattering | >1 µm | Molecular structure, crystallinity | Chemical contamination analysis, complementary to FTIR [49] |
| BMI/FMM/SIMI | Optical/fluorescence imaging + membrane filtration | ≥1 µm | Particle count, size distribution, composition | Subvisible particle characterization in biotherapeutics, protein aggregation analysis [49] |
| Py-GC/MS | Thermal decomposition + chromatographic separation | Cumulative detection | Polymer quantification, plastic concentration | Microplastic/nanoplastic mass quantification in tissues [53] |
| Digital PCR | Nucleic acid amplification | N/A | Pathogen detection and absolute quantification | Viral contamination screening, mycoplasma detection [54] |
Table 2: Detection Capabilities for Different Contaminant Types
| Contaminant Type | Recommended Primary Technique | Complementary Techniques | Detection Sensitivity | Key Advantages |
|---|---|---|---|---|
| Inorganic Particles | SEM-EDS | BMI/SIMI, Raman | ≥1 nm (SEM) | Elemental signature for source identification [51] |
| Microplastics/Nanoplastics | Py-GC/MS | SEM-EDS, FTIR | Varies by polymer | Mass quantification, polymer-specific detection [53] |
| Biological Particles | FMM | PCR, SEM | ≥1 µm | Distinguishes protein aggregates from other particulates [49] |
| Mycoplasma | Digital PCR | Fluorescence staining | ~0.3 µm organism size | High sensitivity, detects non-culturable contaminants [3] [54] |
| Viral Contaminants | Digital PCR | ELISA, immunofluorescence | Varies by assay | Detects latent viruses, rapid turnaround (3-6 hours) [54] |
| Chemical Contaminants | FTIR | Raman, LC-MS | Varies by compound | Molecular fingerprinting, polymer identification [52] |
Experimental Protocols for Contamination Analysis
SEM-EDS Analysis for Particulate Contamination
Sample Collection and Preparation:
- Collect representative samples using clean techniques to prevent secondary contamination. For liquid samples, use membrane filtration with appropriate pore size (typically 0.1-0.45 µm) [51].
- Transfer captured particles to SEM specimen stubs using conductive adhesive tabs to ensure proper charge dissipation.
- Sputter-coat non-conductive samples with a thin layer (5-20 nm) of gold or carbon to prevent charging under electron beam examination [51].
Imaging and Analysis:
- Load samples into SEM chamber and evacuate to appropriate vacuum level (typically 10⁻³ to 10⁻⁶ Pa).
- Acquire secondary electron images at accelerating voltages of 5-20 kV to visualize topological features of contaminants.
- Switch to backscattered electron detection mode to enhance compositional contrast between different particulate types.
- Perform EDS analysis at multiple representative sites on each particle of interest, with acquisition times of 30-60 seconds to ensure adequate signal-to-noise ratio for minor elements [51].
- Utilize EDS spectral libraries to identify elemental compositions and compare contaminant signatures against potential source materials.
Data Interpretation: Correlate morphological characteristics (size, shape, surface texture) with elemental composition to classify particulate types and identify probable contamination sources. Metallic particles typically exhibit smooth, spherical morphologies if generated through heating, or irregular shapes if from mechanical abrasion [51].
FTIR Spectroscopy for Polymer Identification
Sample Preparation:
- Isolate contaminants from cell culture media or tissues through filtration or density separation. For complex biological matrices, enzymatic digestion (e.g., with KOH) may be necessary to remove interfering organic material [53].
- For attenuated total reflectance (ATR) mode, ensure direct contact between the particle and the ATR crystal. Apply consistent pressure to maintain intimate contact during measurement.
- For microplastic analysis from tissues, transfer the KOH-insoluble pellet to infrared-transparent substrates for transmission analysis [53].
Spectral Acquisition:
- Collect background spectrum before analyzing the sample.
- Acquire spectra in the mid-infrared range (4000-400 cm⁻¹) with 4 cm⁻¹ resolution, co-adding 32-64 scans to improve signal-to-noise ratio [52].
- For heterogeneous samples, map multiple areas to account for compositional variations.
Data Analysis:
- Process spectra by applying atmospheric suppression and baseline correction algorithms.
- Compare acquired spectra against reference libraries of known polymers (polyethylene, polypropylene, polystyrene, polyethylene terephthalate, etc.) [52].
- Identify characteristic absorption bands: C-H stretching (2800-3000 cm⁻¹), carbonyl stretching (~1715 cm⁻¹ for PET), and fingerprint regions (1500-400 cm⁻¹) for definitive polymer identification.
Integrated Particle Analysis Using BMI/FMM
Sample Preparation:
- Gently mix samples to ensure homogeneous distribution without generating additional particles through agitation.
- For fluorescent labeling, incubate samples with appropriate dyes (e.g., Nile red for plastics, specific antibodies for protein aggregates) according to manufacturer protocols [49].
Image Acquisition:
- Filter 5-50 µL of sample through a membrane with appropriate pore size (typically 0.1-1 µm) using gentle vacuum or pressure.
- Acquire background image of the membrane before sample application using high-magnification optics.
- Apply sample to membrane and acquire post-filtration images using the same imaging conditions.
- For FMM, capture multiple fluorescence channels corresponding to the specific dyes employed [49].
Image Analysis:
- Subtract background image from sample image to eliminate membrane texture artifacts.
- Identify and count particles based on size, morphology, and fluorescence properties.
- Classify particles according to established criteria: fluorescent particles indicate specific biological components or plastics, while light-scattering particles suggest inorganic materials [49].
Research Reagent Solutions for Contamination Analysis
Table 3: Essential Research Reagents and Materials for Advanced Contamination Analysis
| Reagent/Material | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Conductive Adhesive Tabs | Secure non-conductive samples for SEM imaging | Particulate analysis, fiber identification | Carbon-based tabs preferred for EDS to avoid elemental interference |
| Gold/Palladium Sputtering Targets | Create conductive coating for SEM | Coating of biological specimens, plastic particles | Thinner coatings (5-10 nm) preserve fine topological details |
| ATR Crystals (Diamond, ZnSe) | Internal reflection element for FTIR | Polymer identification, chemical contamination | Diamond crystal provides durability for irregular particles |
| Fluorescent Dyes (e.g., DANS, Nile Red) | Specific staining of polymer components | Microplastic identification and quantification | Staining specificity must be validated for each polymer type [52] |
| Nucleic Acid Extraction Kits | Isolation of pathogen DNA/RNA | Viral/mycoplasma detection via dPCR | Automated systems improve reproducibility for clinical samples [54] |
| dPCR Master Mixes | Partitioned amplification of target sequences | Absolute quantification of viral contaminants | Multi-channel panels enable simultaneous pathogen detection [54] |
| Membrane Filters (Various Pore Sizes) | Particle capture for SEM/BMI analysis | Subvisible particle concentration | Material compatibility (e.g., polycarbonate) must be considered |
Workflow Integration and Experimental Design
The contamination analysis workflow begins with initial assessment through visual inspection and light microscopy to identify obvious microbial contamination [55] [3]. For biological contaminants without clear identification, digital PCR provides highly sensitive detection of viral sequences and mycoplasma with rapid turnaround times of 3-6 hours, significantly faster than traditional culture methods which can require 94+ hours [54]. When biological testing returns negative or contamination is suspected from non-biological sources, the analytical pathway diverges based on the nature of the suspected contaminant.
SEM-EDS analysis is particularly valuable for investigating inorganic particulates from equipment wear or manufacturing processes, providing both morphological and elemental composition data for source tracking [51]. FTIR and Raman spectroscopy excel at identifying organic chemical contaminants and polymer-based materials such as microplastics, which have been shown to induce inflammatory responses and cell death in human cell cultures at concentrations as low as 100 ng/mL [52]. For biopharmaceutical applications where subvisible particles in injectable products present significant safety concerns, integrated BMI/FMM/SIMI approaches provide comprehensive particulate characterization while complying with regulatory requirements [49].
Data integration from these complementary techniques enables researchers to identify contamination sources definitively and implement targeted corrective actions, such as process adjustments, equipment maintenance, or supplier changes. This systematic approach to contamination investigation helps establish robust prevention strategies that minimize future contamination risks in both research and manufacturing environments.
Emerging Technologies and Future Directions
Artificial intelligence (AI) and machine learning are transforming contamination detection and analysis through automated image recognition and predictive modeling. Convolutional neural networks (CNNs) can now analyze microscopy images to identify subtle morphological changes indicative of contamination with over 90% accuracy, often before visible signs emerge [50]. These AI-driven approaches enable real-time monitoring of critical quality attributes, including cell morphology, differentiation status, and early contamination indicators, providing researchers with proactive intervention capabilities [50].
Advanced spectroscopic techniques coupled with machine learning algorithms are enhancing detection sensitivity and automation for microplastic analysis. The integration of pyrolysis gas chromatography-mass spectrometry (Py-GC/MS) with spectroscopic methods enables robust quantification of plastic polymers in complex biological samples, with recent studies detecting polyethylene concentrations up to 4917 µg/g in human brain tissues [53]. These methodological advances are particularly relevant for cell culture research given the emerging evidence that micro- and nanoplastics can induce inflammation, alter cellular function, and potentially accumulate in biological systems [53] [52].
Future developments in contamination analysis will likely focus on increased automation, real-time monitoring capabilities, and enhanced integration of multiple analytical modalities. Sensor technologies with AI-powered analytics will enable continuous quality monitoring rather than periodic sampling, potentially revolutionizing contamination control in critical applications like stem cell manufacturing and biopharmaceutical production [50]. As these advanced analytical tools become more accessible and user-friendly, their implementation in standard cell culture workflows will significantly enhance research reproducibility and product safety across biomedical applications.
Cell line misidentification and cross-contamination represent a persistent and pervasive challenge in biomedical research, directly undermining data integrity and reproducibility. Within the context of cell culture contamination research, authentication serves as the first and most critical defense against the compromise of scientific findings. Studies have documented that between 6% and 100% of cell lines across various collections are misidentified or cross-contaminated, with HeLa cells alone contaminating at least 209 cell lines documented in the Cellosaurus database [56]. The problem persists due to mishandling and inattention to best practices in tissue culture, leading to irreproducible results, wasted resources, and misguided scientific conclusions [56] [57].
Authentication methodologies, primarily Short Tandem Repeat (STR) profiling and karyotype analysis, provide powerful tools to verify cell line identity and genomic stability. STR profiling delivers a DNA "fingerprint" unique to each cell line donor, while karyotype analysis reveals gross chromosomal abnormalities indicative of transformation or contamination. When implemented routinely, these techniques form an essential component of a comprehensive quality control framework that also includes mycoplasma testing and environmental monitoring [56] [11]. This guide provides researchers and drug development professionals with detailed technical protocols and analytical frameworks for implementing robust cell line authentication within their contamination prevention strategies.
Short Tandem Repeat (STR) Profiling: Methodology and Analysis
Principles and Historical Context
STR profiling exploits naturally occurring variations in hypervariable genomic regions containing short, repetitive DNA sequences (typically 2-6 base pairs in length) [56]. These regions are distributed throughout the genome and exhibit significant length polymorphism between individuals due to variations in the number of repeat units. The technology has evolved from early DNA fingerprinting techniques using minisatellite DNA to the current focus on microsatellite STR regions, which are more easily amplified and analyzed [56].
The application of STR profiling to cell line authentication gained urgency following seminal studies revealing widespread cross-contamination. Stanley Gartler's work in 1967-1968 demonstrated that 18 extensively used cell lines were actually derived from HeLa cells [56]. Subsequent investigations confirmed this troubling pattern, with Drexler et al. (1999) finding that 15% of hematopoietic cell lines were cross-contaminated, and more recent reports documenting misidentified lines purportedly representing breast, prostate, thyroid, and other cancers [56].
Core STR Methodology
DNA Amplification and Fragment Analysis
STR analysis employs polymerase chain reaction (PCR) amplification of multiple selected loci using fluorescently labeled primers [56]. The process involves:
- Multiplex PCR: Simultaneous amplification of typically 16-26 STR loci in a single reaction, with primers designed to produce non-overlapping amplicon size ranges for each dye channel [56].
- Capillary Electrophoresis (CE): Size-based separation of PCR products through a polymer matrix under electrical current, with smaller fragments migrating faster than larger ones [56].
- Fluorescent Detection: A laser excites fluorescent dyes as DNA fragments pass a detection window, generating signals converted to electrophoretograms showing peaks corresponding to different alleles [56].
- Allele Designation: Fragment sizes are compared to an internal size standard and allelic ladders containing common variants to determine the number of repeats at each locus [56].
Table 1: Common STR Markers in Commercial and Custom Panels
| Marker | Chromosome Location | Repeat Motif | Included in CODIS | Included in ESS |
|---|---|---|---|---|
| D7S820 | 7q21.11 | GATA | No | No |
| vWA | 12p13.31 | TCTA[TCTG]_{1-4} | Yes | Yes |
| FGA | 4q28 | CTTT | Yes | Yes |
| D8S1179 | 8q24.13 | TCTA | No | Yes |
| D21S11 | 21q21.1 | TCTA/TCTG | Yes | No |
| D18S51 | 18q21.33 | AGAA | Yes | No |
| D5S818 | 5q23.2 | AGAT | Yes | No |
| D13S317 | 13q31.1 | TATC | Yes | No |
| D16S539 | 16q24.1 | GATA | Yes | No |
| CSF1PO | 5q33.3-34 | TAGA | Yes | No |
| TPOX | 2p25.3 | AATG | Yes | No |
| TH01 | 11p15.5 | TCAT | Yes | No |
| SE33 | 6q14 | AAAG | No | No |
| D2S441 | 2p14 | TCTA | No | Yes |
| D22S1045 | 22q12.3 | ATT | No | Yes |
| D12S391 | 12p13.2 | AGAT | No | Yes |
| D1S1656 | 1q42 | TAGA | No | No |
| D10S1248 | 10q26.3 | GGAA | No | Yes |
| D19S433 | 19q12 | AAGG | No | No |
| Amelogenin | Xp22.2 / Yp11.2 | N/A (Sex marker) | Yes | Yes |
Note: CODIS = Combined DNA Index System; ESS = European Standard Set. Commercial kits often include subsets of these markers plus additional loci [58].
STR Analysis Workflow
The following diagram illustrates the complete STR profiling workflow from sample preparation to data interpretation:
STR Data Interpretation and Quality Metrics
STR genotyping produces distinct allele calls for each locus, typically represented as whole numbers corresponding to repeat counts. Microvariants (incomplete repeats) are designated with decimal extensions (e.g., 8.1, 8.2, 8.3) [56]. Authentication requires comparison to reference profiles, with match strength calculated using the match algorithm:
Match Algorithm: Percentage of alleles shared between two samples = (Number of matching alleles / Total number of alleles compared) × 100 [56].
Authentication guidelines generally require ≥80% match for confirmation of identity, with lower percentages indicating potential misidentification or contamination [56]. The following table summarizes key quality metrics in STR profiling:
Table 2: STR Profiling Quality Control Metrics and Interpretation
| Parameter | Optimal Value/Range | Significance | Troubleshooting Tips |
|---|---|---|---|
| Template DNA Quantity | 0.5-1.0 ng [59] | Below range: allele dropout; Above range: signal saturation | Quantify DNA fluorometrically; optimize dilution |
| Heterozygote Balance | ≥60% [56] | Measures relative peak heights between alleles | Values <60% may indicate mixed samples or PCR inhibition |
| Signal Intensity | 1000-6000 RFU [59] | Below range: poor detection; Above range: spectral pull-up | Adjust injection time or template concentration |
| Stutter Peaks | <15% of primary allele [56] | PCR artifacts mimicking smaller alleles | Filter using analysis software thresholds |
| Peak Morphology | Sharp, symmetric | Indicates proper electrophoresis | Check capillary condition, polymer quality, voltage settings |
| Background Noise | <50 RFU [59] | Interferes with allele calling | Purify DNA, use quality reagents, maintain equipment |
Karyotype Analysis: Chromosomal Evaluation by Flow Cytogenetics
Principles of Flow Cytogenetics
Flow cytogenetics involves the analysis and sorting of single metaphase chromosomes in suspension, providing insights into chromosome number, structure, and DNA content [60]. This methodology enables detection of deletions, translocations, and aneuploidy that may arise during cell culture and serve as indicators of transformation or contamination [60]. The technique contributed significantly to the Human Genome Project through sorting pure chromosome populations for gene mapping and library construction [60].
Flow karyograms display chromosomal distributions based on DNA content, with peak positions proportional to chromosomal DNA content and peak areas representing chromosome frequency [60]. Univariate analysis uses a single DNA stain (e.g., propidium iodide), while bivariate analysis employs two dyes with different base-pair preferences (e.g., Hoechst 33258 for A:T and Chromomycin A3 for G:C regions) to enhance resolution [60].
Chromosome Preparation and Staining Protocols
Metaphase Chromosome Isolation
The following diagram outlines the complete workflow for chromosome preparation and analysis by flow cytogenetics:
Basic Protocol 1: Mitotic Block and Cell Harvesting [60]
- Culture Preparation: Begin with exponentially growing sub-confluent monolayer cultures (e.g., two T-150 flasks at 50-60% confluency).
- Colcemid Application: Add colcemid at a concentration of 0.01-0.1 μg/ml (optimized for cell type; typically 0.1 μg/ml for Chinese hamster fibroblasts).
- Incubation: Incubate under normal growth conditions for 3-15 hours (cell type-dependent; 10-12 hours for human fibroblasts, 3 hours for faster-growing hamster cells).
- Mitotic Cell Collection: Maintain flask horizontally and sharply "slap" against hand 2-3 times to dislodge mitotic cells. Pour media into 50ml collection tube on ice.
- Centrifugation: Pellet cells at 400 × g for 5-7 minutes. Completely discard supernatant.
- Optional QC: Remove small aliquot before centrifugation, stain with 10 μM Hoechst 33342, and determine mitotic index.
Basic Protocol 2: Propidium Iodide Isolation Procedure [60]
This single-color method yields chromosomes stabilized in their typical X-shape, ideal for species with smaller numbers of chromosomes or highly variable DNA content.
- Cell Swelling: Resuspend cell pellet in 0.5 ml PI Solution A. Incubate 10 minutes at room temperature in dark.
- Quality Assessment: Place 10 μl suspension on glass slide, cover with coverslip, and examine by fluorescence microscopy. Ideal preparations show swollen cells with intact membranes (non-fluorescent).
- Membrane Permeabilization: Add 0.25 ml PI Solution B to suspension. Incubate in dark at room temperature for 3 minutes. Cells will now appear fluorescent under microscope.
- Chromosome Liberation: Gently pass suspension 4-5 times through a 22-gauge needle attached to a 3ml syringe.
- Filtration: Filter suspension through 35-60 μm mesh to remove aggregates and large debris.
- Staining Enhancement: Add 2.5 μl of 1 mg/ml RNase A and incubate 30 minutes at 37°C to reduce RNA-associated background.
- Analysis: Analyze by flow cytometry within 2-3 hours for optimal results.
Karyogram Interpretation and Aberration Detection
Normal diploid cells exhibit a characteristic pattern of peaks corresponding to their chromosome complement, while contaminated or transformed lines show distinct alterations:
Table 3: Chromosomal Aberrations Detectable by Flow Cytogenetics
| Aberration Type | Flow Karyogram Signature | Biological Significance |
|---|---|---|
| Aneuploidy | Altered peak areas and positions | Indicates gain or loss of specific chromosomes; common in transformed lines |
| Translocations | New peaks in bivariate analysis | Chromosomal rearrangements; marker of genetic instability |
| Deletions | Peak position shifts toward lower DNA content | Loss of chromosomal material; may indicate specific mutations |
| Trisomy | Increased area of specific peak | Presence of three copies of a chromosome; diagnostic for certain syndromes |
| Double Minutes | Small particles in sub-chromosomal region | Gene amplification; common in drug-resistant lines |
| Polyploidy | Uniform shift toward higher DNA content | Whole genome duplication; occurs in some established lines |
The Researcher's Toolkit: Essential Reagents and Materials
Implementation of robust authentication protocols requires specific reagents and instrumentation. The following table details essential components for establishing STR profiling and karyotype analysis capabilities:
Table 4: Essential Research Reagents and Materials for Cell Line Authentication
| Category | Specific Products/Components | Function and Application Notes |
|---|---|---|
| STR Profiling Kits | PowerPlex systems [59], GlobalFiler, Investigator kits | Multiplex PCR reagents containing primer sets, buffer components, and DNA polymerase optimized for STR amplification |
| DNA Quantitation Tools | Qubit dsDNA HS Assay, PicoGreen fluorescence assay | Fluorometric quantification for accurate template DNA measurement (0.5-1.0 ng optimal) [59] |
| Capillary Electrophoresis Systems | ABI PRISM 3500 Series, SeqStudio Genetic Analyzer | Instrumentation for fragment separation with multicolor fluorescence detection capabilities |
| Chromosome Isolation Reagents | Colcemid solution, PI Solution A (Sucrose/Tris/EDTA/KCl), PI Solution B (Sucrose/Tris/EDTA/PI) [60] | Chemical solutions for metaphase arrest, cell membrane swelling, and controlled lysis for chromosome liberation |
| DNA Staining Dyes | Propidium iodide, Hoechst 33258, Chromomycin A3, DAPI | Fluorochromes with DNA binding specificity for univariate or bivariate chromosome analysis [60] |
| Analysis Software | GeneMapper ID-X, CellProfiler, FCS Express | Applications for STR allele calling, karyogram interpretation, and data management |
| Quality Control Standards | Internal size standards, allelic ladders, positive control DNA | Reference materials for instrument calibration and assay validation |
Integrating Authentication into Contamination Prevention Strategies
Effective contamination control requires a multifaceted approach combining authentication with other quality measures. STR profiling should be performed upon cell line receipt, before freezing in cell banks, and at regular intervals during extended culture (e.g., every 3 months or 10 passages) [56] [57]. Karyotype analysis provides complementary information about genomic stability and should be conducted when establishing new lines or observing phenotypic changes.
Leading scientific journals now mandate authentication for publication, requiring details on species, sex, tissue origin, source, and authentication method [57]. The International Cell Line Authentication Committee (ICLAC) maintains a register of misidentified cell lines that researchers should consult when acquiring new lines [57].
By implementing rigorous STR profiling and karyotype analysis within a comprehensive quality framework, researchers can significantly reduce contamination-related errors, enhance data reproducibility, and accelerate meaningful scientific discoveries.
Implementing a Routine Screening Protocol for Continuous Monitoring
Cell culture contamination remains one of the most persistent and costly challenges in biological research and biopharmaceutical manufacturing. Within the broader context of contamination research, a proactive strategy of continuous monitoring is paramount, as contamination not only leads to experimental failure and wasted resources but can also compromise data integrity, patient safety, and regulatory compliance [11]. Unlike reactive approaches, a routine screening protocol is designed to detect contaminants before they can impact experimental outcomes or production batches. This is particularly crucial for insidious contaminants like mycoplasma and viruses, which can alter cellular function and metabolism without causing visible turbidity in the culture medium [11] [29]. The implementation of such a protocol is a fundamental component of Good Cell Culture Practice (GCCP) and is essential for ensuring the reproducibility and reliability of all downstream applications.
The consequences of undetected contamination vary between research and Good Manufacturing Practice (GMP) environments. In research laboratories, contamination primarily affects data integrity and reproducibility, potentially leading to misleading scientific conclusions [11]. In contrast, contamination in GMP manufacturing for biopharmaceuticals can lead to complete batch failures, significant financial losses, and serious regulatory actions [11] [61]. Furthermore, certain viral contaminants can pose a health hazard to laboratory personnel, especially when working with human or primate cells [29]. A robust, routine screening protocol is therefore the cornerstone of a successful cell culture system, mitigating these risks by ensuring early detection and intervention.
Understanding the Contamination Landscape
A effective screening protocol must account for the diverse nature of potential contaminants, each requiring specific detection methodologies. The most common biological contaminants can be categorized as follows:
- Bacterial Contamination: This is a frequent issue, often resulting in rapid pH shifts (media turning yellow), cloudy or turbid media, and high cell mortality, making it relatively easily detectable by visual inspection and microscopy [11] [29].
- Fungal and Yeast Contamination: Fungal contamination may appear as visible filaments or mycelia, while yeast presents as ovoid or spherical particles that bud off smaller particles. Both can lead to increased turbidity and, in advanced stages, a rapid increase in media pH [11] [29].
- Mycoplasma Contamination: Perhaps one of the most problematic contaminants, mycoplasma is difficult to detect because it does not cause turbidity or obvious changes under standard light microscopy. Instead, it alters gene expression, metabolism, and cellular function, which can lead to profoundly misleading experimental results [11]. Its detection requires specialized techniques such as PCR, fluorescence staining, or enzymatic assays [11] [29].
- Viral Contamination: Viruses pose a unique challenge due to their small size and the fact that they often do not cause immediate visible changes in culture. Viral contamination can be introduced through contaminated raw materials like serum or host cell lines. Detection methods include electron microscopy, PCR, ELISA, and immunostaining [11] [29] [14].
- Cross-Contamination: The accidental mixing of cell lines, often by fast-growing lines like HeLa, can lead to cell line misidentification and invalid experimental outcomes [11] [29]. Regular cell line authentication is necessary to prevent this issue.
Table 1: Common Cell Culture Contaminants and Their Detection
| Contaminant Type | Common Signs of Presence | Primary Detection Methods |
|---|---|---|
| Bacteria | Cloudy (turbid) media; sudden pH drop; cell death [11] [29] | Visual inspection; light microscopy [29] |
| Yeast | Turbid media; stable then increasing pH; ovoid/spherical particles [29] | Light microscopy; microbial culture [29] |
| Mold | Visible filaments (hyphae); turbid media [29] | Light microscopy [29] |
| Mycoplasma | No turbidity; subtle changes in cell growth & metabolism [11] [29] | PCR, fluorescence staining, ELISA, microbial culture [11] [29] |
| Virus | Often no visible signs; potential cytopathic effects [29] [14] | PCR, ELISA, electron microscopy, immunostaining [11] [29] |
| Cross-Contamination | Altered growth rates or morphology [11] | STR profiling, karyotyping, isotype analysis [11] [29] |
Designing the Routine Screening Protocol
A comprehensive screening protocol is multi-layered, incorporating daily observations, regular scheduled testing, and strict quality control measures. The frequency of specific tests should be calibrated to the risk and application of the cell culture, with higher-stringency testing for cells intended for therapeutic use.
Daily and Weekly Monitoring Activities
Continuous monitoring begins with simple, non-invasive checks that can provide the first line of defense.
- Daily Visual and Microscopic Examination: Cultures should be observed daily with the naked eye and under a light microscope [62] [63]. Key indicators include a change in the color of the medium (when containing phenol red, a shift to yellow indicates acidity, while purple indicates alkalinity), increased turbidity, or unexpected changes in cell morphology [62] [29]. Any of these signs should trigger further investigation.
- Monitoring Cell Behavior: Researchers should be alert to subtle changes, such as a slow-down in cell growth, unexpected cell death, or a failure of the cells to reach confluency as expected. These can be early warning signs of contamination, particularly from mycoplasma or viruses [29] [14].
Scheduled Specific Detection Assays
While daily observation is crucial, it is insufficient for detecting all contaminants. The following assays should be implemented on a routine basis.
- Mycoplasma Testing: Given its stealthy nature, mycoplasma screening should be performed regularly, ideally every 1-2 months, or before starting new experiments or freezing down cell stocks [11]. Polymerase chain reaction (PCR) is a highly sensitive and commonly used method for this purpose [11]. Alternative methods include fluorescence staining with DNA-binding dyes like Hoechst 33258, which allows for visualization of mycoplasma DNA on the cell surface [11] [29].
- Microbial Sterility Testing: To detect bacteria and fungi, cultures should be periodically tested using microbial culture methods. This can involve inoculating samples into nutrient-rich broths (like thioglycolate medium for aerobes/anaerobes and soybean-casein digest medium) and monitoring for turbidity over 14 days [63].
- Viral Screening: For cell banks or biologics production, viral testing is critical. Methods include in vitro assays using indicator cell lines to detect cytopathic effects, and in vivo assays. PCR-based methods are also widely used for their sensitivity in detecting viral DNA or RNA [63] [14].
- Cell Line Authentication: To prevent the devastating effects of cross-contamination, cell lines should be authenticated upon receipt and at regular intervals thereafter. Short Tandem Repeat (STR) profiling is the international standard for human cell lines, while karyotyping and isoenzyme analysis are also valuable tools [29] [61].
Table 2: Recommended Screening Frequency and Methods for Key Contaminants
| Contaminant | Recommended Testing Frequency | Standard Detection Methods | Advanced / Confirmatory Methods |
|---|---|---|---|
| Bacteria & Fungi | With every medium change (visual); formally bi-monthly [63] | Visual inspection; light microscopy [29] | Microbial culture methods (14-day sterility test) [63] |
| Mycoplasma | Monthly or bi-monthly; before critical experiments & cryopreservation [11] | PCR, fluorescence staining [11] [29] | Microbial culture; ELISA [11] |
| Virus | For Master Cell Banks (MCBs); or if suspected [63] | PCR with viral primers, ELISA [29] [63] | Electron microscopy; in vivo assays [29] [63] |
| Cross-Contamination | Upon cell line receipt; every 10 passages or 3 months [61] | STR Profiling, karyotype analysis [29] [61] | Comparative Genomic Hybridization (aCGH) [61] |
The following workflow diagram outlines the logical sequence for implementing a continuous monitoring protocol:
The Researcher's Toolkit: Essential Reagents and Materials
Implementing a successful screening protocol requires access to specific reagents and equipment. The following table details key materials necessary for the routine tests described.
Table 3: Essential Research Reagent Solutions for Contamination Screening
| Reagent / Material | Function in Screening Protocol |
|---|---|
| PCR Kits (Mycoplasma) | Amplifies specific mycoplasma DNA sequences for highly sensitive detection, often considered the gold standard [11] [29]. |
| Fluorescence Stains (Hoechst 33258) | DNA-binding dyes used with fluorescence microscopy to visualize mycoplasma DNA adherent to infected cells [29]. |
| Microbial Culture Media | Nutrient broths (e.g., thioglycollate, soybean-casein digest) used to support the growth of contaminating bacteria and fungi over a 14-day period [63]. |
| STR Profiling Kits | Provides reagents for Short Tandem Repeat analysis, the definitive method for authenticating human cell lines and detecting cross-contamination [61]. |
| Viral PCR Assays | Detects the presence of specific viral DNA or RNA sequences from common contaminants like Epstein-Barr Virus (EBV) [63] [14]. |
| HEPA-Filtered Biosafety Cabinet | Provides a sterile workspace for all cell culture handling to prevent the introduction of contaminants during testing procedures [11] [40]. |
Implementing a Quality Management System for Sustainable Monitoring
For a screening protocol to be effective long-term, it must be embedded within a larger framework of quality assurance. Adopting a Quality Management System (QMS), such as ISO9001:2015, provides the structure needed for standardization and reproducibility [61]. A key component of a QMS is the use of Standard Operating Procedures (SOPs) for every aspect of cell culture and screening, from passaging cells to performing a PCR test for mycoplasma. This minimizes variation between personnel and over time [61].
Research has demonstrated that the implementation of a QMS with standardized SOPs leads to a striking improvement in the genomic stability of pluripotent stem cells in vitro, significantly reducing the prevalence of chromosomal aberrations [61]. This principle extends to contamination control; standardized, documented procedures for cleaning incubators, maintaining equipment, and screening cultures ensure that vigilance remains high and errors are minimized. Furthermore, a QMS mandates thorough documentation and batch tracking for all materials and processes, providing full traceability in the event of a contamination incident and facilitating root cause analysis [11] [61].
Implementing a routine screening protocol for continuous monitoring is not an optional luxury but a fundamental requirement for rigorous and reproducible cell culture research. By moving from a reactive to a proactive stance, researchers can safeguard their experiments against the wide array of biological contaminants that threaten data integrity. This requires a disciplined, multi-faceted approach combining daily observation, regularly scheduled assays for pathogens like mycoplasma and viruses, and periodic cell line authentication. Ultimately, the most robust strategy integrates these technical protocols into a formal Quality Management System, ensuring that "best practices" become the standardized, documented, and consistently followed norm for every member of the laboratory.
Building Your Defense: Proactive Strategies for Contamination Prevention and Control
Cell culture contamination remains one of the most persistent and costly challenges in biological research and biopharmaceutical manufacturing, directly impacting data integrity, reproducibility, and patient safety. Within the broader context of contamination research, aseptic technique emerges as the fundamental pillar for preventing the introduction and spread of contaminants throughout cell culture workflows. Mastering these techniques requires understanding that contamination can arise from multiple sources, including human handling, environmental exposure, non-sterile supplies, and contaminated reagents [11]. The consequences of failure are severe: in research settings, contamination compromises experimental results and validity, while in Good Manufacturing Practice (GMP) manufacturing, it can lead to complete batch failures, regulatory actions, and significant financial losses [11].
The distinction between aseptic and sterile techniques is crucial for proper implementation. Sterile techniques ensure a space is completely free of any microorganisms, while aseptic techniques focus on not introducing contamination to a previously sterilized environment [64]. This whitepaper examines the core principles of aseptic technique through the lens of contemporary contamination research, providing researchers and drug development professionals with evidence-based methodologies to safeguard cell integrity and experimental validity.
Effective contamination control begins with comprehensive knowledge of potential contaminants and their sources. Biological contamination represents the most frequent challenge, with bacteria, fungi, mycoplasma, viruses, and cross-contamination by other cell lines posing significant risks to culture purity [11] [29].
Biological Contaminants
- Bacterial Contamination: Characterized by rapid pH shifts and cloudy media, bacterial contamination is easily detectable through visual inspection and microscopy, where bacteria appear as tiny, moving granules between cells [11] [29].
- Fungal and Yeast Contamination: Fungal contamination often presents with visible filaments (mycelia), while yeast appears as ovoid or spherical particles that bud off smaller particles. Both cause media turbidity, though pH changes may be less immediate than with bacterial contamination [11] [29].
- Mycoplasma Contamination: Particularly problematic due to the absence of visual indicators, mycoplasma alters cellular function and gene expression without causing turbidity, requiring specialized detection methods like PCR or fluorescence-based assays [11].
- Viral Contamination: Difficult to detect without advanced methods, viral contamination often originates from contaminated raw materials and can persist without visible culture changes while compromising experimental outcomes and presenting safety hazards [11] [14].
- Cross-Contamination: The unintended mixing of cell lines, particularly with fast-growing lines like HeLa, can lead to misidentification and invalid experimental outcomes without proper authentication protocols [11] [29].
Chemical and Particulate Contaminants
Chemical contamination from residual detergents, endotoxins, or plasticizers can negatively impact cell viability and differentiation potential [11] [29]. In GMP environments, particulate contamination from equipment components or human handling presents additional challenges, with regulatory requirements mandating strict controls [11].
Table 1: Common Cell Culture Contaminants and Identification Methods
| Contaminant Type | Visual Indicators | Detection Methods | Common Sources |
|---|---|---|---|
| Bacteria | Cloudy media, rapid pH drop, thin surface film | Microscopy, pH monitoring, microbial cultures | Improper technique, contaminated reagents [11] [29] |
| Fungi/Yeast | Turbidity, visible filaments, stable pH initially | Microscopy, microbial cultures | Airborne spores, improper sterilization [11] [29] |
| Mycoplasma | No visible change, altered cell function | PCR, fluorescence assays, ELISA | Contaminated sera, human origin [11] |
| Viruses | Often no visible change, potential CPE* | PCR, ELISA, electron microscopy | Raw materials, host cell lines [11] [14] |
| Cross-Contamination | Altered growth/morphology | STR profiling, karyotyping, isotype analysis | Shared spaces, improper handling [11] [29] |
*CPE: Cytopathic Effects [14]
Core Principles of Aseptic Technique
Establishing and Maintaining a Sterile Work Area
The laboratory environment must be deliberately designed and maintained to minimize contamination risks. Laminar flow hoods (biosafety cabinets) provide the primary barrier between the environment and sterile cultures and should be positioned in low-traffic areas free from drafts [64]. Proper setup includes maintaining an uncluttered work surface containing only items required for the immediate procedure, as clutter disrupts airflow and increases contamination risk [64].
Rigorous disinfection protocols are essential. Work surfaces should be wiped with 70% ethanol before and during work, especially after any spillage [64]. Ultraviolet light can be used to sterilize the air and exposed surfaces in cell culture hoods between uses, though flaming with a Bunsen burner is generally unnecessary and not recommended within modern biosafety cabinets [64]. Equipment including incubators, refrigerators, and freezers must be cleaned and sterilized regularly according to established schedules [11].
Personal Protective Equipment and Hygiene
Personnel represent a significant contamination source, carrying microorganisms on skin, hair, and breath [65]. Proper personal protective equipment (PPE) including lab coats, gloves, masks, and hairnets creates a crucial barrier [65] [64]. Gloving technique requires particular attention, as improper donning or doffing can transfer contaminants even when gloves are worn [65].
Personal behavior directly impacts contamination risk. Researchers must avoid talking, coughing, or sneezing near open cultures and should not enter culture areas without proper attire [65]. Thorough hand washing before and after working with cultures, even when gloves are worn, provides additional protection [64].
Sterile Handling of Reagents and Cultures
Commercial reagents and media undergo strict quality control for sterility but can become contaminated during handling. Always wipe container exteriors with 70% ethanol before introducing them to the sterile work area [64]. Avoid pouring media directly from bottles or flasks; instead, use sterile pipettes for all liquid transfers [64].
Proper container management is critical. Always cap bottles and flasks when not in immediate use, and seal multi-well plates with tape or in resealable bags [64]. If a cap must be placed on the work surface, position it with the opening facing down to minimize environmental exposure [64]. Work deliberately but efficiently, minimizing the time that cultures and reagents remain open to the environment [64].
Diagram: Aseptic Technique Workflow for Contamination Prevention. This workflow outlines the critical steps for maintaining sterility during cell culture procedures.
Advanced Strategies and Quality Control
Monitoring, Detection, and Decontamination
Routine contamination screening provides essential quality control. Regular mycoplasma and microbial testing using PCR, fluorescence staining, or ELISA-based methods should be implemented, with cell lines tested prior to beginning experiments and monitored periodically throughout research activities [11]. Novel detection methods continue to emerge, including machine learning-aided UV absorbance spectroscopy that can provide contamination assessment within 30 minutes—significantly faster than traditional 14-day sterility tests [66].
When contamination occurs in irreplaceable cultures, decontamination may be attempted through targeted antibiotic or antimycotic treatments. However, these approaches require careful dose response testing to determine concentrations that eliminate contaminants without causing cellular toxicity [29]. Antibiotics should not be used routinely in cell culture, as continuous use encourages resistant strains and can mask low-level contamination [29].
Table 2: Contamination Detection Methods and Timeframes
| Detection Method | Time to Result | Contaminants Identified | Key Advantages/Limitations |
|---|---|---|---|
| Visual Inspection/Microscopy | Immediate | Bacteria, fungi, yeast | Rapid but limited sensitivity [29] |
| Traditional Sterility Testing | Up to 14 days | Broad microbial range | Gold standard but slow [66] |
| PCR-Based Methods | Several hours | Mycoplasma, specific viruses | Highly sensitive, specific targets [11] |
| Machine Learning/UV Spectroscopy | ~30 minutes | Microbial contamination | Rapid, label-free, early detection [66] |
| Microbial Cultures | 2-7 days | Bacteria, fungi | Broad detection but slow [11] |
Research vs. GMP Environments
While the fundamental principles of aseptic technique remain consistent, their implementation differs significantly between research and GMP environments. Research laboratories focus on data integrity and reproducibility, emphasizing strict aseptic handling, routine testing, and cell line authentication [11]. GMP manufacturing prioritizes patient safety and batch consistency, requiring stringent cleanroom standards, closed processing systems, comprehensive environmental monitoring, and detailed documentation for regulatory compliance [11] [67].
In both settings, the human element remains critical. Proper training, adherence to standard operating procedures, and maintaining a culture of attention to detail are essential for successful contamination control [11] [64]. Cross-contamination risks necessitate strict labeling protocols, dedicated reagents for different cell lines, and physical separation when working with multiple cultures [11] [65].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Materials and Reagents for Aseptic Cell Culture
| Item Category | Specific Examples | Function & Importance |
|---|---|---|
| Sterilization Agents | 70% Ethanol, vapor phase hydrogen peroxide (VPHP) | Surface and environmental decontamination [67] [64] |
| Sterile Consumables | Pre-sterilized pipettes, culture vessels, filters | Single-use items to prevent cross-contamination [11] [64] |
| Culture Media Components | Sera, supplements, balanced salt solutions | Cell nutrition; require sterile filtration and quality verification [11] [29] |
| Quality Testing Kits | Mycoplasma PCR kits, microbial culture tests | Regular contamination screening and verification [11] [29] |
| Personal Protective Equipment | Sterile gloves, lab coats, masks, hairnets | Create barrier between personnel and cultures [65] [64] |
Mastering aseptic technique requires integrating knowledge of contamination sources with disciplined practical application. As cell culture technologies advance and become more integral to drug development and personalized medicine, maintaining the highest standards of sterile handling becomes increasingly critical. By establishing robust protocols, implementing regular quality control measures, and fostering a culture of meticulous technique, researchers can significantly reduce contamination events, thereby enhancing experimental reliability and accelerating scientific discovery.
Biosafety Cabinets (BSCs) are engineered containment devices fundamental to modern laboratories, providing a critical barrier against biological hazards. Their primary function is to maintain a controlled and contained workspace where procedures involving potentially harmful materials can be conducted safely [68]. The core principle of a BSC is the use of controlled, HEPA- or ULPA-filtered airflow to create a protective barrier between the laboratory environment and the samples, thereby safeguarding the operator, the experimental materials, and the external environment [69] [68] [70]. Within the context of cell culture contamination research, BSCs are the first line of defense against the introduction of airborne biological contaminants, making their proper selection, installation, and maintenance a cornerstone of reliable scientific practice.
Cell culture contamination is a pervasive and costly problem that can compromise experimental integrity, lead to erroneous data, and render biological products unsafe [71] [29]. Contaminants can be chemical or biological, with the latter including bacteria, molds, yeasts, viruses, and mycoplasma [29]. These unwanted microbes primarily originate from laboratory personnel, unfiltered air, humidified incubators, contaminated media or sera, and the laboratory equipment itself, including improperly functioning BSCs [71]. The role of high-efficiency filtration within BSCs is to actively remove these airborne particulates, thus preventing them from settling into sterile media or open culture vessels and ensuring the purity of the cell cultures.
Classification of Biosafety Cabinets
Biosafety Cabinets are classified into three main categories (Class I, II, and III) based on their design, airflow patterns, and level of protection offered. Understanding these distinctions is crucial for selecting the appropriate cabinet for a specific biological risk level and application.
Class I BSCs are designed to provide personnel and environmental protection, but do not protect the product or samples from contamination [72] [73]. They operate by drawing room air (which may be contaminated) into the cabinet and passing it through a HEPA filter before exhausting it [72] [68]. This inward airflow protects the user, while the HEPA filter protects the environment. Class I cabinets are suitable for housing equipment like centrifuges or for working with low to moderate-risk agents where sample sterility is not critical [73].
Class II BSCs are the most common cabinets found in cell culture laboratories, as they provide three-way protection: for the personnel, the product, and the environment [72] [73]. They achieve this through a combination of inward airflow (inflow) that protects the user, downward HEPA-filtered laminar airflow (downflow) that protects the sample, and HEPA-filtered exhaust that protects the environment [69] [68]. Class II cabinets are further subdivided into types (e.g., A1, A2, B1, B2) based on their airflow ratios, recirculation rates, and exhaust systems [68].
Class III BSCs offer the highest level of containment and are used for working with highly infectious and hazardous agents, typically in Biosafety Level 4 (BSL-4) laboratories [72] [73]. These are totally enclosed, gas-tight cabinets where all operations are conducted through attached glove ports [72] [68]. The cabinet is maintained under negative pressure, and both supply and exhaust air are HEPA-filtered, with an optional incinerator for the exhaust [73].
Table 1: Comparison of Biosafety Cabinet Classes
| Feature | Class I | Class II | Class III |
|---|---|---|---|
| Personnel Protection | Yes | Yes | Yes (Highest Level) |
| Product Protection | No | Yes | Yes |
| Environmental Protection | Yes (via HEPA Exhaust) | Yes (via HEPA Exhaust) | Yes (via Double HEPA Exhaust) |
| Airflow Principle | Inward air drawn away from user; unfiltered air flows over work area [72] | Laminar downflow of HEPA-filtered air; inward airflow at front opening [69] [68] | Total containment; air enters and exits via HEPA filters; operations via glove ports [72] [68] |
| Typical Applications | Housing centrifuges, cleaning contaminated equipment [73] | Cell culture, microbiology, pharmaceutical compounding [72] [73] | Work with highly infectious and hazardous agents (BSL-4) [73] |
Airflow and Protection Dynamics in a Class II BSC
The following diagram illustrates the sophisticated aerodynamic balance within a Class II BSC, which is the workhorse for cell culture and other procedures requiring product protection.
High-Efficiency Filtration: HEPA and ULPA Technologies
High-efficiency particulate air (HEPA) filters are the cornerstone of biosafety cabinet functionality. These filters are composed of a mat of randomly arranged borosilicate glass fibers formed into a pleated sheet to maximize surface area [69] [74]. They are designed to capture particulates, including microorganisms, from the air, ensuring that the exhaust air and the air bathing the work surface are free of harmful pathogens [74].
Mechanisms of Particle Capture
HEPA and ULPA filters do not operate like a simple sieve. Instead, they employ a combination of four physical mechanisms to capture particles across a wide size spectrum [75] [69] [70].
- Inertial Impaction: This mechanism captures large, heavy particles (typically >0.5 µm). These particles have too much inertia to follow the curved airstream around filter fibers and instead collide with and embed themselves into the fibers [75] [69].
- Interception: Medium-sized particles (approximately 0.1 to 0.5 µm) follow the airstream but are intercepted and trapped when they come into side contact with a filter fiber [75] [69].
- Diffusion: Very small particles (<0.1 µm) are bombarded by air molecules, causing them to move in a random, zigzag pattern (Brownian motion). This erratic movement increases the probability that they will drift into and be retained by a filter fiber [75] [69] [70].
- Sieving: While a minor mechanism for sub-micron particles, sieving occurs when a particle is too large to fit through the space between two adjacent fibers [75].
The interplay of these mechanisms results in a "U-shaped" efficiency curve, where a specific particle size, known as the Most Penetrating Particle Size (MPPS), is most difficult to capture. For HEPA filters, the MPPS is approximately 0.3 micrometers, which is the particle size at which they are tested and rated [75].
HEPA vs. ULPA: A Detailed Comparison
Ultra Low Penetration Air (ULPA) filters represent a higher grade of filtration efficiency. The key differences between the two are critical for laboratory decision-making.
Table 2: HEPA vs. ULPA Filter Specifications
| Feature | HEPA Filter | ULPA Filter |
|---|---|---|
| Minimum Efficiency | 99.97% of particles ≥0.3 µm [75] [74] | 99.999% of particles ≥0.12 µm [75] |
| Test Particle Size | 0.3 micrometers [75] [74] | 0.1 - 0.2 micrometers [69] |
| Most Penetrating Particle Size (MPPS) | ~0.1 µm – 0.25 µm [75] | ~0.05 µm – 0.15 µm [75] |
| Primary Target Contaminants | Bacteria, larger viruses, fungal spores, pollen [75] | Smaller viruses, nanoparticles, ultra-fine dust [75] |
| Typical Cleanliness Class | ISO Class 5 [69] | ISO Class 3 or better [69] |
| Airflow Resistance & Energy Use | Lower resistance and energy consumption [75] [70] | Higher resistance; can consume 40-50% more power [75] |
| Filter Lifespan | 7-15 years (varies with use) [70] | 5-8 years (varies with use) [75] |
| Cost | Lower initial and operational cost [75] | 30-100% more expensive than HEPA [75] |
The "ULPA Paradox" in Biosafety Cabinets
A critical concept in BSC design is the "ULPA Paradox"—the counterintuitive scenario where installing a more efficient ULPA filter can actually compromise safety [75]. ULPA filters have a denser fiber construction, which creates significantly higher airflow resistance [75] [70]. If a BSC's motor and blower system are not specifically engineered to overcome this added resistance, the critical inflow and downflow velocities can drop below their certified safety thresholds [75]. This disrupts the aerodynamic balance, weakening the protective air barrier and potentially allowing contaminants to escape or enter the work zone. Consequently, NSF/ANSI 49, the primary standard for BSCs, mandates HEPA filters and does not require or provide for ULPA filters, as HEPA filtration has been proven sufficient for biological containment when integrated into a properly balanced system [75].
Biosafety Cabinet Installation, Maintenance, and Certification
Proper installation and rigorous maintenance are non-negotiable for ensuring a BSC continues to operate as a certified system, thereby preventing cell culture contamination.
Installation Guidelines
The performance of a BSC is highly dependent on its location within the laboratory. Key installation requirements, based on NSF/ANSI 49, include [68]:
- Placement: Cabinets must never be placed in line with doors, openable windows, or high-traffic areas. A minimum of 40 inches (1020 mm) of open space is required in front of the BSC for user access and safety.
- Clearances: A clearance of at least 6 inches (150 mm) is needed from adjacent walls or columns on the sides and rear to allow for service access. A minimum of 12 inches (300 mm) is required from the filter face to any overhead obstruction for testing purposes.
- Airflow Disturbances: Room air supply diffusers should be kept at least 1.5 meters (5 feet) away from the cabinet's front opening to prevent disruption of the inflow air curtain.
Maintenance and Cleaning Protocols
A disciplined maintenance schedule is essential for contamination control.
Table 3: Biosafety Cabinet Maintenance Schedule
| Frequency | Maintenance Task | Purpose in Contamination Control |
|---|---|---|
| Daily | Surface decontaminate work zone with appropriate disinfectant (e.g., 70% alcohol) [71] [68]. | Remove contaminants introduced during work sessions. |
| Weekly/Monthly | Clean UV lamps (if present) of dust; perform thorough decontamination of drain pan; clean exterior surfaces and sash [68]. | Maintain overall cabinet cleanliness and UV lamp effectiveness. |
| Monthly | Clean with 10% bleach or equivalent to eliminate resistant biofilms [71]. | Address tougher contamination that alcohol may not remove. |
| Yearly | Professional recertification, including filter integrity and airflow velocity testing [68] [70]. | Verify the cabinet's performance meets original safety specifications. |
Cleaning Procedure: The work surface and interior walls should be cleaned with an appropriate disinfectant, followed by soapy water. Finally, rinse with sterile water to remove any chemical residues that could contaminate cultures. Avoid using bleach on stainless steel surfaces as it can cause pitting and corrosion [68].
Certification and Performance Testing
Annual recertification is mandatory to ensure the BSC is functioning correctly. Key performance tests include [68]:
- Inflow Velocity Test: Measures the velocity of air entering the front grille to ensure it is sufficient to contain aerosols.
- Downflow Velocity Test: Measures the velocity of the vertical laminar airflow to ensure it properly protects the sample.
- Filter Integrity Test: A challenge test using an aerosol (e.g., PAO, DOP) upstream of the filter to scan for and identify any leaks in the HEPA/ULPA filter or its seals.
- Particle Count Test: Counts and sizes particles in the work zone to classify and verify the cabinet's cleanliness level (e.g., ISO Class 5).
The Scientist's Toolkit: Key Reagents and Materials
Table 4: Essential Materials for BSC Maintenance and Contamination Control
| Item | Function |
|---|---|
| 70% Ethanol | A widely used disinfectant for daily surface decontamination of the BSC work zone; effective against many bacteria and fungi [71] [68]. |
| 10% Sodium Hypochlorite (Bleach) | A potent chemical disinfectant used for monthly deep cleaning to eliminate a broader spectrum of microbes, including viruses and bacterial spores [71]. Note: should be rinsed to prevent corrosion [68]. |
| Stainless Steel Polisher (e.g., Autosol) | Used to clean stubborn stains on the stainless-steel work surface, helping to maintain a smooth, easy-to-clean finish that resides harboring contaminants [68]. |
| HEPA/ULPA Filter | The core filtration component of the BSC; it must be integrity tested annually and replaced when clogged or damaged to maintain containment and aseptic conditions [68] [74]. |
| Personal Protective Equipment (PPE) | Gloves, lab coat, and safety glasses are essential for protecting the operator during both routine work and cabinet decontamination procedures [68]. |
Within the critical context of cell culture contamination research, the Biosafety Cabinet, supported by robust HEPA filtration, is an indispensable engineering control. A thorough understanding of BSC classes, the science behind high-efficiency filtration, and a steadfast commitment to proper installation, maintenance, and certification protocols are fundamental to creating a secure and sterile working environment. By meticulously integrating these laboratory setup and environmental controls, researchers can effectively mitigate the risk of contamination, thereby safeguarding the integrity of their scientific work, the validity of their data, and the safety of both personnel and the surrounding environment.
In cell culture-based research, the integrity of reagents and media is not merely a procedural concern but a foundational aspect of experimental validity. Contamination originating from these sources represents a silent and pervasive threat that can compromise years of research, leading to irreproducible results, misleading scientific conclusions, and substantial financial losses [11] [1]. While improper aseptic technique during handling is a common culprit, this guide focuses on the often-overlooked pre-analytical phase: the sourcing, sterilization, and quality control of the materials themselves. Effective management in these areas creates a critical barrier against the introduction of biological contaminants (bacteria, fungi, mycoplasma, viruses), chemical contaminants (endotoxins, extractables), and cross-contaminants that can derail research outcomes and, in biomanufacturing, pose direct risks to patient safety [11] [76]. By framing reagent and media management within a comprehensive contamination control strategy, researchers can address a root cause of experimental failure and enhance the reliability of their scientific data.
A targeted defense requires a precise understanding of the threat. Contaminants introduced via reagents and media vary in their nature, detectability, and impact on cell cultures.
Types and Origins of Contamination
The most common contaminants introduced through reagents and media include:
- Microbial Contamination: Bacteria and fungi can be introduced through non-sterile raw materials, such as contaminated serum, or during the in-house preparation of media [11]. Bacterial contamination often leads to rapid pH shifts and cloudy media, while fungal contamination may present more gradually with visible filaments [11].
- Viral Contamination: Viruses pose a unique challenge as they are often introduced through contaminated raw materials like serum or host cell lines [11] [14]. Unlike bacteria, viral contamination does not always cause immediate visible changes, making detection difficult without specific screening methods [11] [14]. For instance, Epstein-Barr virus (EBV) and Ovine Herpesvirus 2 (OvHV-2) are gammaherpesviruses of concern that can persist latently in cell cultures used for biological production [14].
- Mycoplasma Contamination: This particularly problematic bacterial contamination does not cause turbidity or other obvious signs, but instead alters gene expression, metabolism, and cellular function, potentially leading to misleading experimental results [11]. Since mycoplasma cannot be detected using standard light microscopy, specialized testing is required [11] [77].
- Chemical Contamination: This can stem from various sources, including residual detergents from improperly cleaned glassware, endotoxins from bacterial contaminants, or extractables and leachables from plastic consumables [11]. Even trace amounts can negatively impact cell viability, differentiation potential, and introduce variability in experimental results [11].
Table 1: Common Contaminants in Cell Culture: Sources and Impacts from Reagents and Media
| Contaminant Type | Common Sources in Reagents/Media | Typical Impact on Culture | Ease of Detection |
|---|---|---|---|
| Bacteria | Non-sterile water, contaminated serum, improper in-house preparation [11] | Rapid pH shift, cloudiness, high cell mortality [11] | Relatively easy (visual, microscopy) |
| Fungi/Yeast | Non-sterile lab environment, contaminated raw materials [11] | Turbidity, slowed cell growth, visible filaments [11] | Moderate (visual, microscopy) |
| Mycoplasma | Contaminated serum, host cell lines [11] [77] | Altered cellular metabolism & gene expression; no visible cloudiness [11] | Difficult (requires PCR, fluorescence assays) [11] [77] |
| Viruses | Contaminated serum (e.g., FBS), host cell lines [11] [14] | May be latent; can alter cellular metabolism or pose safety concerns [11] [14] | Very difficult (requires specific PCR or qPCR) [14] [76] |
| Chemical | Endotoxins, extractables from plastics, residual detergents [11] | Reduced viability, altered growth and differentiation [11] | Varies (requires specific assays) |
Sourcing and Quality Control of Raw Materials
The first line of defense against contamination is the rigorous selection and qualification of raw materials. The principle is simple: starting with a contaminated or substandard material makes it impossible to achieve a clean, reliable culture.
Critical Sourcing Considerations
- Serum and Supplements: Fetal Bovine Serum (FBS) is a well-known potential source of viral and mycoplasma contamination [11] [14]. Sourcing from reputable suppliers who provide comprehensive testing certificates, including for viruses (e.g., specific panels for bovine viruses), mycoplasma, and endotoxins, is paramount.
- Water Quality: Water is a key component of culture media and reagents. The use of highly purified water (e.g., Type I ultrapure water) is non-negotiable for media preparation to avoid introducing ions, organics, and microorganisms [76]. Contaminated laboratory tap or demineralized water systems have been identified as sources of persistent, spore-forming bacterial contaminants that can survive in 70% ethanol [76].
- Chemicals and Amino Acids: Use high-purity, cell culture-grade chemicals to minimize the introduction of endotoxins and trace contaminants that can subtly influence cell behavior [11].
- Plastic Consumables: Single-use, pre-sterilized consumables (flasks, pipettes) significantly reduce the risk of contamination compared to reusable glassware [11] [64]. However, it is important to consider potential chemical contamination from extractables and leachables from the plastics themselves [11].
Incoming Quality Control (QC) Protocols
Upon receipt, a robust QC process should be implemented:
- Quarantine and Pre-screening: All new lots of critical reagents, especially new cell lines and serum, should be quarantined and tested before being integrated into routine use [77]. This prevents a single contaminated source from spreading through the entire laboratory.
- Mycoplasma Testing: Conduct thorough mycoplasma testing on new cell lines and other susceptible biologicals upon receipt. PCR-based assays are widely used for their rapid and sensitive detection [11] [77].
- Sterility Testing: Screen reagents and media for bacterial and fungal contamination by inoculating samples into nutrient-rich broths and observing for turbidity [77].
- Cell Line Authentication: To prevent cross-contamination and misidentification, authenticate human cell lines using Short Tandem Repeat (STR) profiling upon receipt [78] [77]. This generates a unique genetic fingerprint for the cell line, which should be cross-checked against reference databases [77].
Table 2: Essential Research Reagent Solutions for Contamination Control
| Item/Category | Key Function in Contamination Control | Considerations |
|---|---|---|
| Cell Culture-Grade Water | Base for media and reagent preparation; prevents introduction of ions, organics, and microbes [76]. | Use Type I ultrapure water; avoid using laboratory tap or demineralized water systems that can harbor spores [76]. |
| Pre-tested Fetal Bovine Serum | Provides essential growth factors and nutrients. | Source from suppliers that provide virus and mycoplasma testing certificates; heat-inactivation may be used for certain applications [11]. |
| Single-Use, Pre-sterilized Consumables | Provides a sterile surface for cell growth and fluid handling, eliminating risk from improper glassware cleaning [11] [64]. | Reduces need for cleaning validation; be aware of potential for extractables [11]. |
| Validated Sterilization Filters | Removes microorganisms from heat-labile solutions (e.g., media, supplements) [11]. | Use 0.2 µm pores for bacteria; 0.1 µm for mycoplasma reduction. Implement post-filtration integrity testing in GMP [11]. |
| Quality Control Kits (Mycoplasma PCR, STR Profiling) | Authenticates cell line identity and tests for silent contaminants [11] [77]. | PCR is rapid and sensitive; STR profiling is essential for confirming human cell line identity [77]. |
Sterilization and Microbial Control Methodologies
Sterilization is the process of eliminating all viable microorganisms, while microbial control aims to reduce bioburden to an acceptable level. The choice of method depends on the nature of the material and the required level of sterility assurance.
Primary Sterilization Techniques
- Gamma Irradiation: A common method for sterilizing single-use bioprocess systems (e.g., polymeric film bags, filter capsules, tubing) [79]. Gamma rays penetrate deeply and inactivate microorganisms by damaging their nucleic acids. A standard dose of 25 kGy is often used to achieve a Sterility Assurance Level (SAL) of 10⁻⁶, meaning there is a less than one in a million chance of a single viable microorganism being present [79]. This method is particularly suited for heat-sensitive materials and pre-sterilized, single-use components [11] [79].
- Steam Sterilization (Autoclaving): The use of saturated steam under pressure (e.g., 121°C for 15-20 minutes) is a highly effective and reliable method for sterilizing heat-stable solutions, glassware, and some equipment. It is the method of choice for in-house sterilization of aqueous solutions and labware that can withstand heat and moisture.
- Filtration: The only practical method for sterilizing heat-labile solutions like media containing proteins or vitamins. Filters with a pore size of 0.2 μm are standard for removing bacteria and fungi [11]. For solutions that may contain mycoplasma, which can pass through 0.2 μm filters, a 0.1 μm pore size is recommended [11]. In Good Manufacturing Practice (GMP) settings, the integrity of these filters must be validated post-use to ensure they functioned correctly during processing [11].
Decision Framework for Sterilization vs. Microbial Control
The required level of sterility depends on the application. The following diagram outlines a logical decision-making workflow for choosing an appropriate sterilization or microbial control strategy.
Experimental Protocols for Quality Control
Implementing standardized testing protocols is essential for verifying the sterility and identity of cell culture components.
Protocol 1: Mycoplasma Detection by PCR
Mycoplasma contamination is common and can profoundly affect cell physiology without causing turbidity [11] [77]. PCR provides a rapid and sensitive detection method.
- Sample Collection: Collect supernatant from the test cell culture after it has been grown for at least 3 days without antibiotics. Include both a known positive control (e.g., a deliberately contaminated culture) and a negative control (sterile medium).
- DNA Extraction: Use a commercial DNA extraction kit to isolate DNA from 200 µL of the sample supernatant according to the manufacturer's instructions. This step concentrates the nucleic acids and removes potential PCR inhibitors.
- PCR Amplification: Prepare a PCR master mix containing primers specific for highly conserved mycoplasma genes (e.g., 16S rRNA). A common primer set is GPO-3 (5'-GGG AGC AAA CAG GAT TAG ATA CCC T-3') and MGSO (5'-TGC ACC ATC TGT CAC TCT GTT AAC CTC-3'), which produces a ~720 bp amplicon.
- Analysis: Run the PCR products on a 1.5% agarose gel. The presence of a band at the expected size in the test sample, which co-migrates with the positive control, indicates mycoplasma contamination. The test is invalid if the positive control shows no band or the negative control shows a band.
Protocol 2: Cell Line Authentication by STR Profiling
STR profiling is the international standard for authenticating human cell lines and detecting cross-contamination [77].
- DNA Isolation: Extract high-quality genomic DNA from the cell line to be tested. The sample can be a cell pellet or a section of a confluent culture flask.
- PCR Amplification: Amplify the DNA using a multiplex PCR assay that targets a standard panel of STR loci (e.g., the 16-locus kit used by the ATCC). These loci are short, repetitive sequences that are highly variable between individuals.
- Capillary Electrophoresis: Separate the fluorescently labeled PCR products by size using capillary electrophoresis. The instrument generates an electropherogram showing peaks at each STR locus.
- Data Analysis and Comparison: The software converts the peak patterns into an allelic profile—a string of numbers representing the genotype at each locus. This profile must be compared against a database of known cell line profiles (e.g., the ATCC STR database). A match of 80% or higher is typically required to confirm identity, while a lower percentage suggests cross-contamination or misidentification.
A Proactive Regimen for Ongoing Quality Management
Effective reagent and media management extends beyond one-time procedures to encompass continuous, systematic vigilance. The workflow below integrates the key procedures for maintaining ongoing quality control of cell culture reagents and media.
This workflow should be supported by additional best practices:
- Documentation and Traceability: Maintain meticulous records for all reagents, including product codes, lot numbers, expiration dates, and QC certificates. This enables full traceability in the event of a contamination incident [11] [77].
- Storage and Handling: Properly aliquot reagents to minimize repeated freeze-thaw cycles and exposure to the environment. Store all materials under specified conditions and clearly label them with preparation and expiration dates [64].
- Crisis Management: If contamination is detected, immediately quarantine the affected cultures and any reagents suspected to be the source. Decontaminate work surfaces and equipment thoroughly. For persistent or unusual contaminants, DNA sequencing can be employed to identify the organism, which is critical for implementing a targeted eradication strategy, as demonstrated with cases of human adenovirus C and Brevibacillus [76].
Reagent and media management is a critical pillar in the defense against cell culture contamination. By implementing a rigorous, multi-layered strategy that encompasses informed sourcing, validated sterilization, and relentless quality control, researchers can protect the integrity of their cellular models. This proactive approach, integrated into the daily rhythm of the laboratory, moves beyond simply reacting to contamination to systematically preventing it. In doing so, it safeguards not only individual experiments but also the very credibility and reproducibility of scientific research and the safety of biopharmaceutical products.
Maintaining laboratory equipment is a cornerstone of reproducible and reliable cell culture research. Contamination originating from improperly maintained incubators and water baths is a significant yet preventable cause of experimental failure, compromising data integrity and costing valuable time and resources. This guide provides detailed protocols to integrate the decontamination of incubators and the maintenance of water baths into a robust contamination control strategy.
The Contamination Context in Cell Culture
Cell cultures are vulnerable to a wide array of biological and chemical contaminants. Understanding these threats is the first step in appreciating the critical role of equipment maintenance.
The table below summarizes the primary contaminants that can originate from or be facilitated by poorly maintained equipment.
Table 1: Common Cell Culture Contaminants and Links to Equipment
| Contaminant Type | Key Characteristics | Potential Equipment-Related Sources |
|---|---|---|
| Bacterial | - Rapid growth [3]- Cloudy (turbid) culture medium [3] [29]- Sudden pH drop (yellowing medium) [3] [29] | - Contaminated water bath water [6] [55]- Unclean incubator surfaces [11] |
| Fungal/Yeast | - Visible filaments or "fuzzy" structures [3] [29]- Spores resistant to harsh conditions [29] | - Incubator water trays with high humidity [3]- Airborne spores in lab environment [3] |
| Mycoplasma | - No visible turbidity; hard to detect [3] [11] [29]- Alters cell metabolism and gene expression [3] [11] | - Often introduced via contaminated reagents or cell lines [3] [11] |
| Chemical | - Residual detergents, endotoxins, plasticizers [11] [29]- Can affect cell viability and differentiation [11] | - Leaching from degraded equipment components [11]- Impurities in water bath water [55] |
| Cross-Contamination | - Overgrowth by another cell line [3] [11]- Leads to misidentification and irreproducible data [3] | - Aerosols or spills in shared incubators or water baths [11] |
Incubator Decontamination: A Critical Protocol
The warm, humid environment of a CO₂ incubator is ideal for microbial growth. A rigorous and regular decontamination protocol is non-negotiable.
Decontamination Workflow
The following diagram outlines the key stages of a comprehensive incubator decontamination process.
Incubator Decontamination Workflow
Detailed Methodology
Preparation:
Cleaning and Disinfection:
- Clean removable parts: Autoclave shelves and racks if possible, or soak them in a laboratory-grade disinfectant (e.g., 10% bleach, Trigene, or Chloros) followed by a thorough rinse with sterile water [6] [29].
- Decontaminate interior surfaces: Wipe down all internal surfaces, including walls, ceiling, and the door gasket, with 70% ethanol or a disinfectant specified by the incubator manufacturer [3] [6]. Pay close attention to seams and gaskets where contaminants can accumulate.
- Replace water: Discard the old water from the humidity pan. Clean the pan thoroughly and refill it with sterile, distilled, or autoclaved water to prevent microbial growth and mineral buildup [3] [6] [80]. Adding a water bath treatment chemical can further inhibit contamination, provided it is compatible with the pan material [6].
Reassembly and Validation:
- Allow all parts and the incubator chamber to air dry completely to prevent immediate microbial growth in a moist environment [6].
- Reassemble the incubator, ensuring all components are correctly placed.
- Turn on the incubator and allow it to reach and stabilize at the desired temperature, CO₂ concentration, and humidity for several hours before returning cultures [6].
Frequency: This deep cleaning should be performed on a weekly basis, or according to the manufacturer's recommendations and the intensity of lab use [3] [6].
Water Bath Safety and Maintenance
Water baths are a common source of bacterial and fungal contamination due to their constant presence of water at ideal growth temperatures.
Maintenance and Safety Workflow
Adhering to a strict maintenance routine is essential for water bath safety and to prevent it from becoming a contamination source.
Water Bath Maintenance Regimen
Detailed Methodology and Safety Precautions
Routine Cleaning and Water Management:
- Water Quality: Use distilled or deionized water to fill the bath. This prevents the buildup of minerals and scale that can harbor bacteria and damage the heating element [81] [80] [82].
- Cleaning Frequency: Drain, clean, and refill the water bath weekly. Clean the interior with a mild detergent or a disinfectant suitable for the bath's material, rinse thoroughly, and refill with fresh distilled water [6] [80]. For labs working with sensitive cultures, more frequent changes and the use of sterile water are recommended [81] [82].
- Contamination Control: Always use a lid on the water bath. This reduces evaporation, prevents airborne contaminants from entering, and helps maintain a consistent temperature [81] [80].
Safety and Calibration:
- Electrical Safety: Ensure the power cord is dry and undamaged. Keep the power source away from the water bath to prevent electrical hazards and spills [81] [82].
- Temperature Monitoring: Regularly check the water bath's temperature with a calibrated, independent thermometer to ensure the digital display is accurate [81] [80]. Calibration should be performed every six months or according to the manufacturer's schedule [81].
- Sample Integrity: To prevent cross-contamination, ensure all sample containers (e.g., media bottles) are sealed properly before submerging them in the water bath [80] [82].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Reagents and Materials for Equipment Maintenance
| Item | Function in Maintenance |
|---|---|
| 70% Ethanol | Standard disinfectant for wiping down exterior and interior surfaces of incubators and water baths, as well as gloves and items entering the biosafety cabinet [3] [6]. |
| Laboratory Disinfectant | Used for deeper decontamination (e.g., Trigene, Chloros, 10% bleach) to eliminate persistent microbial contaminants on dismantled incubator parts [6] [29]. |
| Sterile Distilled Water | Used to refill incubator humidity pans and water baths to prevent introduction of microorganisms and chemical impurities [81] [6] [80]. |
| Water Bath Treatment | Additives specifically designed to inhibit microbial and algal growth in water baths, used according to manufacturer instructions [6]. |
| Calibrated Thermometer | An independent, certified thermometer for verifying the temperature accuracy of water baths and incubators [81] [80]. |
| Autoclave | Provides guaranteed sterilization via pressurized steam for laboratory glassware, tools, and dismantled incubator components that are heat-resistant [6] [29]. |
Integrating these detailed protocols for incubator decontamination and water bath maintenance into standard laboratory operating procedures is essential for safeguarding cell cultures. This proactive approach directly addresses major sources of contamination, thereby protecting the integrity of research data from discovery through to drug development and manufacturing.
Within the context of cell culture contamination research, antibiotics and antimycotics represent a double-edged sword. While they are crucial tools for preventing microbial contamination, their application requires careful consideration to avoid compromising experimental integrity. These agents are designed to suppress or eliminate bacterial and fungal contaminants, yet their misuse can lead to masked low-level infections, the development of resistant strains, and unintended effects on cell physiology [83] [84]. A foundational study examining over 2,700 cell lines found nearly 40% were contaminated, with mycoplasma present in 19% of cases, highlighting the pervasive nature of contamination and the temptation to rely on chemical prophylaxis [83]. This guide examines the proper use, mechanisms, and significant limitations of these supplements to help researchers make informed decisions that protect both their cultures and the validity of their scientific data.
Common Reagents and Their Mechanisms of Action
Cell culture reagents typically consist of antibiotics to combat bacteria and antimycotics to target fungal contaminants. They are often used in combination to provide broad-spectrum coverage and are available as concentrated solutions (e.g., 100X) for convenient dilution into culture media [85].
The table below summarizes the most common reagents, their mechanisms of action, and standard working concentrations.
Table 1: Common Antibiotics and Antimycotics in Cell Culture
| Reagent | Primary Target | Mechanism of Action | Common Working Concentration |
|---|---|---|---|
| Penicillin | Gram-positive bacteria | Inhibits bacterial cell wall synthesis [83]. | 100 U/mL [83] [86] |
| Streptomycin | Gram-negative bacteria | Binds to the 30S ribosomal subunit, inhibiting protein synthesis [83]. | 100 µg/mL [83] [86] |
| Gentamicin | Broad-spectrum bacteria | Protein synthesis inhibitor; offers broader Gram-negative coverage [83]. | 10–50 µg/mL [83] |
| Amphotericin B | Fungi & Yeast | Binds to ergosterol in fungal membranes, creating pores that cause cell death [83] [87]. | 0.25–2.5 µg/mL [83] [86] |
| Nystatin | Fungi & Yeast | Binds to membrane sterols, causing leakage of cellular components [87]. | As directed by manufacturer |
Antibiotic-antimycotic mixtures are popular for their convenience. A typical 100X solution contains 10,000 U/mL penicillin, 10,000 µg/mL streptomycin, and 25 µg/mL amphotericin B, providing combined protection against gram-positive/negative bacteria and fungi [83] [85]. It is critical to note that these reagents are distinct from selection antibiotics like G418 or Hygromycin B, which are used to maintain pressure on genetically modified cells and are applied at different concentrations [83].
Table 2: Research Reagent Solutions for Contamination Control
| Item | Function | Key Considerations |
|---|---|---|
| Penicillin-Streptomycin (100X) | Broad-spectrum base antibiotic for Gram-positive/negative coverage [83]. | Synergistic combo; standard in most labs; water-soluble; store at -20°C [83]. |
| Antibiotic-Antimycotic Solution (100X) | Combines Pen-Strep with Amphotericin B for fungal and bacterial protection [83] [85]. | Convenient mix; monitor for cytotoxicity in sensitive cells; light-sensitive [83]. |
| Gentamicin Sulfate | Broad-spectrum antibiotic, especially against Gram-negative strains [83]. | Can stress sensitive cell lines; dose-dependent cytotoxicity [83]. |
| Mycoplasma Removal Reagent | Targeted reagent to eliminate mycoplasma contamination [83]. | Not a standard antibiotic; required for mycoplasma as it lacks a cell wall [83]. |
Limitations and Impacts on Research Data
The routine use of antibiotics and antimycotics carries significant risks that can fundamentally compromise experimental outcomes. Key limitations include their potential to mask contamination, direct effects on cell health, and the induction of widespread molecular changes in host cells.
Masking Contamination and Promoting Resistance
Perhaps the most significant risk is the ability of these supplements to mask low-level, persistent contamination. Instead of eliminating contaminants, they often merely suppress microbial growth to a sub-visible level [83] [84]. This creates a false sense of security, allowing insidious contaminants like mycoplasma—which are unaffected by standard antibiotics due to their lack of a cell wall—to persist unnoticed and alter cellular functions [83] [3]. Furthermore, prolonged use encourages the development of antibiotic-resistant strains; one study found that over 90% of bacterial isolates from contaminated cultures were resistant to penicillin-streptomycin [83]. When the antibiotic is removed, these resistant contaminants can proliferate into a full-scale contamination.
Cytotoxic Effects
Many of these agents exhibit dose-dependent cytotoxicity against the very mammalian cells they are meant to protect. Amphotericin B is known to be toxic to mammalian cells at higher concentrations, as it can interact with cholesterol in animal cell membranes, albeit less favorably than with fungal ergosterol [83] [87]. Similarly, gentamicin can impair membrane function and slow proliferation, particularly in fragile cell types like stem cells [83]. These cytotoxic effects can lead to reduced cell viability, altered growth rates, and distorted morphological data.
Alteration of Gene Expression and Cellular Physiology
A growing body of evidence demonstrates that antibiotics can induce profound molecular changes in cell lines, posing a critical confounding variable. A landmark genome-wide study on HepG2 cells cultured with penicillin-streptomycin (PenStrep) identified 209 differentially expressed genes compared to an antibiotic-free control [88]. These included transcription factors like ATF3, which can alter the regulation of numerous downstream genes [88]. Pathway analysis revealed that PenStrep treatment significantly enriched pathways for "xenobiotic metabolism signaling" and "PXR/RXR activation," indicating that the cells were mounting a stress and drug-metabolism response to the antibiotics themselves [88]. This molecular evidence strongly suggests that the implicit assumption that antibiotics have a negligible impact on gene expression is false.
Beyond transcriptomics, antibiotics can alter the epigenetic landscape. The same study found 9,514 genomic regions with differential enrichment for the active enhancer mark H3K27ac in PenStrep-treated cells [88]. These regulatory changes were associated with genes involved in tRNA modification, regulation of nuclease activity, and response to misfolded proteins, mirroring the known mechanism of streptomycin as a protein synthesis inhibitor in bacteria [88]. Such findings indicate that antibiotic effects are not limited to gene expression but extend to fundamental regulatory mechanisms.
Antibiotic Carryover as a Confounding Factor
A very recent (2025) study highlighted a specific experimental pitfall: antibiotic carryover. Researchers investigating the antimicrobial properties of conditioned medium (CM) from various cell lines found that the observed bacteriostatic effect against penicillin-sensitive Staphylococcus aureus was not due to cell-secreted factors, but to residual penicillin released from tissue culture plastic surfaces [89]. This carryover effect was sufficient to inhibit the growth of sensitive bacteria, potentially leading to profoundly misleading conclusions about the intrinsic antimicrobial activity of CM or extracellular vesicles (EVs) [89]. This underscores the critical importance of controlling for antibiotic history in cell-based assays.
Best Practices and Experimental Guidelines
Given the significant limitations, a strategic and deliberate approach to using antibiotics and antimycotics is essential for robust and reproducible science.
When to Use and When to Avoid
Antibiotics should be a tool applied for specific scenarios, not a universal precaution. The following table outlines recommended approaches.
Table 3: Guidelines for Antibiotic and Antimycotic Use
| Scenario | Recommended Approach | Rationale |
|---|---|---|
| Thawing frozen cells | Use antibiotics | Cells are vulnerable during initial recovery [83]. |
| Primary cell culture (early passages) | Use antibiotics | Reduces risk of early loss due to contamination from source tissue [83] [86]. |
| Suspected fungal contamination | Use antibiotic-antimycotic combo | Provides targeted, short-term coverage [83]. |
| Sensitive assays (e.g., gene expression, 'omics') | Avoid antibiotics | Prevents confounding effects on transcriptomic, epigenetic, and proteomic data [83] [88]. |
| Long-term maintenance | Avoid antibiotics | Prevents masking of aseptic technique failures and development of resistance [83] [84]. |
| Stem cell or sensitive primary cell culture | Avoid antibiotics | These cell types are more susceptible to cytotoxic and off-target effects [83]. |
| Mycoplasma not ruled out | Avoid antibiotics | Standard antibiotics suppress symptoms but do not eliminate mycoplasma, delaying diagnosis [83]. |
Protocol for Decontaminating Cultures
When an irreplaceable culture becomes contaminated, a structured decontamination protocol can be attempted. The following workflow, adapted from standard guidelines, outlines this process [84].
Detailed Steps:
- Identify and Isolate: Determine the contaminant (bacteria, fungus, yeast) via microscopy and immediately isolate the culture to prevent spread [84].
- Environmental Decontamination: Thoroughly clean biosafety cabinets and incubators with a laboratory disinfectant, paying attention to water trays—a common source of fungal contamination [84] [3].
- Toxicity Test (Critical Step): Dissociate and plate cells in a multi-well plate with a range of antibiotic concentrations. Observe cells daily for signs of toxicity like sloughing, vacuole appearance, and decreased confluency. The working concentration should be one- to two-fold lower than the toxic level [84].
- Treatment and Validation: Treat cells at the determined safe concentration for 2-3 passages, then cycle through antibiotic-free and antibiotic-containing media as shown in the workflow. The final extended period in antibiotic-free medium is crucial to confirm the contamination has been fully eradicated [84].
The Primacy of Aseptic Technique
The most reliable long-term defense against contamination is not chemical supplementation, but consistent and rigorous aseptic technique [83] [86] [84]. This includes working within a properly maintained laminar flow hood, using sterile equipment, disinfecting all surfaces with 70% ethanol, and limiting the simultaneous handling of multiple cell lines to prevent cross-contamination [3]. Aseptic technique addresses the root cause of the problem, whereas antibiotics merely treat the symptom, and often poorly.
Antibiotics and antimycotics are powerful reagents with a defined but limited role in cell culture. Their ability to prevent the loss of valuable cultures during high-risk situations like primary culture establishment or thawing is undeniable. However, the evidence is clear that their routine use introduces significant and often hidden costs, including the masking of contaminants, cytotoxic effects, and the alteration of critical cellular functions at the genetic and epigenetic levels. Therefore, these agents should be used with intentionality and not out of habit. The foundation of effective cell culture contamination control must always be impeccable aseptic technique, regular contamination monitoring, and cell line authentication. By adopting a more judicious and evidence-based approach, researchers can safeguard both the health of their cultures and the integrity of their scientific data.
Decontamination Protocols for Contaminated Cultures and Equipment
Cell culture experiments are versatile tools indispensable in cellular and molecular biology, basic biomedical, and translational research [1]. However, cell lines are frequently susceptible to contamination by biological agents such as bacteria, fungi, yeast, viruses, or mycoplasma, as well as chemical contaminants and cross-contamination by other cells [1]. The cultivation of cells in a favorable artificial environment is prone to errors if not properly conducted, making the implementation of Good Cell Culture Practice (GCCP) essential for assuring reproducibility [1]. Rough estimates suggest that approximately 16.1% of published papers have used problematic cell lines, highlighting the critical need for robust decontamination protocols and quality control measures [1]. This guide addresses decontamination within the broader thesis of contamination causation by outlining systematic responses to contamination events and preventive strategies to safeguard research integrity.
Understanding Contaminants: Types and Identification
Different contaminants present unique challenges and require specific identification methods. The most common biological contaminants in cell culture include bacteria, fungi, yeast, viruses, and mycoplasma.
Table 1: Characteristics of Common Biological Contaminants
| Contaminant Type | Typical Size | Visible Signs of Contamination | pH Shift | Common Detection Methods |
|---|---|---|---|---|
| Bacteria [90] | A few micrometers | Culture appears turbid, sometimes with a thin surface film; tiny moving granules under microscope (20x) [90] | Decreases (acidic) [90] | Direct observation, smell (foul scent) [90] |
| Fungi/Yeast [90] | 3–4 μm to over 40 μm | Culture becomes turbid; appears as ovoid particles or filamentous hyphae [90] | Increases (basic) as contamination spreads [90] | Direct microscopic observation [90] |
| Mycoplasma [90] | 0.2–0.3 μm | No visible change to culture [90] | No direct change [90] | PCR, DNA staining (Hoechst dye), luciferase-based enzymatic assays (e.g., MycoAlert) [91] [90] |
| Viruses [90] | ~200 nm | No visible change to culture [90] | No direct change [90] | Electron microscopy, ELISA, immunostaining, PCR [90] |
Mycoplasma contamination is particularly problematic as it frequently goes unobserved without specific testing, can alter cellular biology and experimental outcomes, and is spread through contaminated equipment, media, and reagents [91] [90]. Experience from the National Center for Advancing Translational Sciences (NCATS) identified an initial Mycoplasma contamination rate exceeding 10% in received cell lines [91].
Decontamination Protocols for Contaminated Cultures
The appropriate response to contamination depends on the contaminant type, the value of the cell line, and the availability of clean backup stocks.
General Principle: Immediate Discard
For most bacterial and fungal contaminations, and whenever possible for Mycoplasma, the recommended protocol is immediate destruction of contaminated cultures to prevent spread [90]. Contaminated cultures should be discarded immediately and treated with bleach [90]. All frozen stocks should also be destroyed if other cryovials prove positive [91].
Salvage Protocols for Irreplaceable Cultures
For contaminated cell lines that cannot be replaced, salvage may be attempted under strict quarantine.
- Bacterial Contamination: Administration of antibiotics may be attempted [90]. Once contamination is cleared, cells must undergo quality control testing to ensure relevant properties are retained [90].
- Mycoplasma Contamination: Treatment with anti-Mycoplasma compounds like Plasmocin can be attempted in a dedicated incubator outside the main tissue culture room [91]. Studies have shown Plasmocin treatment did not alter phenotypes in immortalized monocytes or human pluripotent stem cells [91]. Resourcing clean cell lines is always preferred [91].
Systematic Testing and Response Policy
The NCATS model provides an effective framework:
- All cell lines must be certified Mycoplasma-free prior to receipt and tested upon receipt [91].
- Cell lines in regular culture must be tested at least monthly and immediately prior to high-throughput screening [91].
- Contaminated cell lines should be destroyed immediately [91].
- Cell lines with "ambiguous" test results should be quarantined and re-tested; two ambiguous tests should be considered contaminated [91].
Decontamination of Laboratory Equipment and Workspace
Proper decontamination of equipment and work areas is crucial to prevent the spread of contamination, particularly for persistent contaminants like Mycoplasma that can survive in a dried state and be spread through laboratory equipment [90].
Work Surface Decontamination
- Disinfect the work surface with 70% ethanol before and during work, especially after any spillage [64].
- Use ultraviolet light to sterilize the air and exposed work surfaces in the cell culture hood between uses [64].
- For widespread contamination issues, thoroughly clean all hoods, incubators, and equipment, potentially requiring a full lab shutdown [90].
Sterile Handling Techniques
- Always wipe gloved hands and the outside of all containers, flasks, plates, and dishes with 70% ethanol before placing them in the cell culture hood [64].
- Avoid pouring media and reagents directly from bottles or flasks; use sterile pipettes instead [64].
- Use each sterile pipette only once to avoid cross-contamination [64].
- Always cap bottles and flasks after use and seal multi-well plates with tape or in resealable bags [64].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Decontamination and Quality Control
| Reagent/Material | Function/Application | Specific Examples/Protocols |
|---|---|---|
| 70% Ethanol [64] | Surface and container decontamination; hand wiping | Wipe work surface before and during work; wipe outside of all containers entering hood [64] |
| Bleach [90] | Decontamination of liquid waste and materials before disposal | Treat contaminated cultures with bleach before discarding [90] |
| Mycoplasma Detection Kits [91] | Routine screening for Mycoplasma contamination | MycoAlert assay (Luciferase-based); PCR-based detection kits for greater sensitivity [91] [90] |
| Plasmocin [91] | Antibiotic treatment to eliminate Mycoplasma contamination from irreplaceable cell lines | Used to "cure" contaminated cultures in quarantine; follow manufacturer's protocols [91] |
| HOECHST Dye [90] | DNA staining method for Mycoplasma detection | Highlights A-T rich DNA of mycoplasma, appearing as bright extranuclear spots [90] |
| Sterile Pipettes [64] | Aseptic liquid handling to prevent cross-contamination | Use each sterile glass or disposable plastic pipette only once [64] |
Experimental Workflow for Contamination Management
The following diagram illustrates the systematic decision-making process for managing contaminated cultures, from detection to resolution.
Quality Control and Authentication in Contamination Research
Beyond microbial decontamination, cell line authentication is vital for research integrity. Cell line misidentification and cross-contamination present significant problems, with the International Cell Line Authentication Committee (ICLAC) listing 576 misidentified or cross-contaminated cell lines in its latest register [1] [91]. DNA fingerprinting by short tandem repeat (STR) profiling has become the standard tool for authenticating human cell lines, providing a genetic signature to verify identity [91] [90]. All new cell lines entering a laboratory should be considered potentially infected and kept in quarantine until contamination status is verified [90]. Master stocks of mycoplasma-free cell lines should be frozen and stored to provide a continuous supply of cells should working stocks become contaminated [90].
Effective decontamination protocols are fundamental to maintaining research integrity in cell culture. A proactive approach combining rigorous aseptic technique, systematic quality control testing, clearly defined response policies for contamination events, and comprehensive equipment decontamination provides the strongest defense against the costly and irreproducible results caused by contaminated cultures. Within the broader context of contamination causation, understanding that contaminants are introduced through improper handling, inadequate quality control, and failure to maintain sterile workspaces informs the development of these essential decontamination protocols, ensuring the reliability and reproducibility of cellular research.
From Research to GMP: Validation Frameworks and Comparative Risk Management
In the realm of pharmaceutical manufacturing and biomedical research, adherence to Good Cell Culture Practice (GCCP) and Good Manufacturing Practice (GMP) is paramount for ensuring product safety, efficacy, and data reproducibility. These quality control standards provide a systematic framework for preventing contamination, a major cause of experimental failure and product recalls. Within the context of cell culture contamination research, these guidelines establish the foundational principles for contamination control strategies, risk management, and the implementation of robust aseptic techniques. This whitepaper provides an in-depth technical examination of GCCP and GMP standards, detailing their application in modern laboratories and manufacturing facilities to mitigate contamination risks and uphold the highest standards of quality.
Good Cell Culture Practice (GCCP)
Good Cell Culture Practice (GCCP) comprises a set of guidelines that provide a benchmark for the maintenance of high standards in cell culture research. The core objective of GCCP is to promote the reproducibility and reliability of in vitro experimentation through the harmonization and standardization of laboratory practices [1]. This is particularly critical in contamination research, where the lack of standardized protocols can itself be a source of variable results. GCCP guidelines encompass critical aspects such as quality management, documentation and reporting, general safety instructions, and the authentication of cell lines to combat issues like misidentification and cross-contamination [1]. By establishing a culture of continuous quality assurance, GCCP helps researchers create a controlled environment where the sources and impacts of contamination can be studied with precision.
Good Manufacturing Practice (GMP) and Current GMP (cGMP)
Good Manufacturing Practice (GMP) refers to the system for ensuring that products are consistently produced and controlled according to quality standards appropriate for their intended use. In the pharmaceutical industry, GMP is designed to prevent instances of product contamination, mislabeling, and incorrect ingredient amounts that could pose serious risks to patient health [92]. GMP encompasses all aspects of production, from the starting materials and equipment to the training and hygiene of staff.
A critical evolution in this field is the move towards "current" Good Manufacturing Practice (cGMP). The distinction lies in the word "current," which mandates that manufacturers employ the most up-to-date technologies and systems to comply with the latest regulatory interpretations [92]. While GMP sets the minimum standard, cGMP emphasizes continuous improvement and adaptation to new scientific knowledge and technological advancements. Regulators, including the FDA and European Medicines Agency (EMA), have established legally-binding cGMP regulations, such as 21 CFR Parts 210 and 211 in the United States, which require a proactive approach to quality risk management [92] [93] [94].
The Contamination Control Strategy: A Holistic Framework
A modern Contamination Control Strategy (CCS) is a holistic, proactive system mandated under regulatory frameworks like the revised EU GMP Annex 1, which became effective in August 2023. A CCS is defined as a “planned set of controls for microorganisms, endotoxin/pyogen, and particles, derived from current product and process understanding that assures process performance and product quality” [95]. This represents a paradigm shift from reactive monitoring to integrated, risk-based contamination prevention.
The framework for a CCS is built on three critical components, arranged in order of importance:
- Design: Encompasses process, equipment, facility, and utilities considerations.
- Control: Involves personnel training, gowning, cleaning, and sanitization procedures.
- Monitoring: Includes personnel, in-process, material, environmental, and utilities monitoring, as well as aseptic process simulation [95].
This hierarchical approach underscores a fundamental principle identified in recent regulatory inspections: organizations cannot monitor or control their way out of poor design [95]. The implementation of a CCS requires comprehensive documentation that links all aspects of the manufacturing process, from raw material receipt to final product distribution, forcing a deeper understanding of potential contamination sources and control points.
Table 1: Core Components of a Contamination Control Strategy (CCS)
| Component | Key Elements | Strategic Importance |
|---|---|---|
| Design | Process, equipment, facility, and utilities design | Most critical layer; prevents contamination at the source through engineering and system design. |
| Control | Personnel training/gowning, cleaning, sanitization | Manages operational variables to maintain a state of control and aseptic conditions. |
| Monitoring | Environmental/Particle monitoring, utility testing, media fills | Provides verification and data for trend analysis and proactive intervention. |
Core Principles and Methodologies for Contamination Prevention
Aseptic Technique and Laboratory Practice
Meticulous aseptic technique is the first line of defense against cell culture contamination. Adherence to the following protocols is essential for all personnel [29] [6]:
- Personal Protective Equipment (PPE): Wear gloves and lab coats dedicated only to the cell culture lab. Gloves should be sprayed with 70% ethanol frequently, especially after touching any surface outside the cabinet.
- Proper Use of Biosafety Cabinets: Work in a certified biosafety cabinet or laminar flow hood. Ensure the airflow is not blocked by equipment and work at least several inches inside the cabinet to maintain a sterile field. Surfaces must be thoroughly disinfected with 70% ethanol or 70% industrial methylated spirits (IMS) before and after all operations [6].
- Minimizing Exposure: Limit the time cultures spend outside sterile environments (e.g., incubators, biosafety cabinets) to reduce contamination risk during handling and microscopic observation.
Sterile Reagent and Labware Management
The use of sterile materials is a basic tenet of GCCP and GMP.
- Reagents: Only use reagents certified as sterile for cell culture work. Filter-sterilizing liquids through 0.2 μm membranes can remove bacteria. Aliquoting reagents protects stock solutions from widespread contamination [6].
- Labware: Use sterile, single-use consumables whenever possible. Reusable labware must be sterilized, typically by autoclaving, with the sterility verified by color-changing indicator tapes [6].
- Equipment Maintenance: Regularly clean and maintain incubators and water baths. Water baths are a common contamination source and require frequent water changes and the use of bath treatments [6].
Quality Risk Management and Regulatory Compliance
Both GCCP and cGMP are underpinned by the principles of Quality Risk Management (QRM), as detailed in ICH Q9. This involves a systematic process for assessing, controlling, and reviewing potential risks to quality [95]. For contamination control, this means:
- Systematic Risk Assessment: Using tools like Failure Mode and Effects Analysis (FMEA) to identify potential contamination sources and their impact.
- Documentation and Traceability: Maintaining comprehensive records for all processes, from cell line authentication to batch-specific manufacturing data. This is critical for investigating deviations and executing effective recalls [92] [94].
- Continuous Improvement: cGMP requires that quality systems are not static. Manufacturers must adopt new technologies and improve processes based on data from quality reviews and trend analyses [92] [95].
Experimental Protocols for Contamination Detection
Routine Monitoring and Identification of Common Contaminants
Regular microscopic observation is the simplest method for detecting gross contamination. Different contaminants exhibit distinct morphologies [29]:
- Bacteria: Appear as tiny, shimmering granules between cells under low-power microscopy, often accompanied by culture turbidity and a rapid drop in media pH.
- Yeast: Present as individual ovoid or spherical particles that may bud off smaller particles. Turbidity is common, but pH changes may only occur in advanced stages.
- Mold: Identified by thin, filamentous mycelia that can develop into denser clumps of spores.
- Mycoplasma: Cannot be detected visually and requires specialized testing.
Table 2: Key Research Reagent Solutions for Contamination Detection
| Reagent / Kit | Primary Function | Experimental Application |
|---|---|---|
| PCR & Molecular Kits | Detection of microbial DNA (e.g., Mycoplasma, specific viruses) | Highly sensitive identification of non-visible contaminants; used for cell bank screening [96] [76]. |
| Universal 16S rRNA Primers | Amplification of conserved bacterial genomic regions | Broad-spectrum detection and identification of unknown bacterial contaminants via DNA sequencing [76]. |
| Mycoplasma Detection Kits | Specific enzymatic or DNA-based detection | Routine screening for this common, invisible cell culture contaminant [1]. |
| Selective Culture Media | Support growth of specific microbes | Used for sterility testing and isolating contaminants from cell culture samples [76]. |
Protocol for Decontamination of Irreplaceable Cultures
When a valuable culture becomes contaminated, a targeted decontamination procedure can be attempted. The following methodology is adapted from established protocols [29]:
- Identification: First, determine the type of contaminant (bacteria, fungus, yeast) using microscopy, microbial culture, or PCR.
- Isolation: Immediately quarantine the contaminated culture from all other cell lines.
- Toxicity Test:
- Dissociate, count, and dilute the cells in antibiotic-free medium.
- Dispense the cell suspension into a multi-well plate.
- Add the chosen antibiotic or antimycotic to the wells in a range of concentrations.
- Observe the cells daily for signs of toxicity (e.g., sloughing, vacuole appearance, decreased confluency, rounding).
- Decontamination Cycle:
- Culture the cells for 2-3 passages using the antibiotic at a concentration one- to two-fold lower than the determined toxic level.
- Culture the cells for one passage in antibiotic-free media.
- Repeat the antibiotic treatment cycle.
- Finally, maintain the cells in antibiotic-free medium for 4-6 passages to confirm the contamination has been eliminated.
It is critical to note that antibiotics and antimycotics should not be used routinely, as they can mask low-level infections, encourage resistant strains, and interfere with cellular processes under investigation [29].
Case Study: Investigation of Persistent Viral Contamination
A research study demonstrated the use of molecular diagnostics to identify a pervasive and persistent contamination of primary keratinocyte cultures with Human Adenovirus C (HAdV C) [76].
- Observation: Cultures showed poor confluency and cell death, with suspicious blebs and black spots. Standard mycoplasma tests were negative, and no growth was observed on blood agar plates.
- Molecular Identification:
- Genomic DNA was isolated from the infected cultures.
- A PCR was performed using universal primers (F338/1061R) targeting the V3-V6 region of the 16S rRNA gene.
- Unexpected amplicon sizes were sequenced, revealing sequences encoding HAdV C.
- Eradication: The contamination was successfully eliminated by formalin gas sterilization of the laminar flow cabinets and the removal of all infected cell lines from the biobank, as guided by specific qPCR testing [76].
Visualization of Workflows and Systems
Contamination Detection and Decision Workflow
The following diagram illustrates a logical workflow for identifying and addressing cell culture contamination, integrating both visual inspection and modern molecular techniques as described in the experimental protocols.
Diagram 1: A workflow for detecting and addressing cell culture contamination.
The Three Pillars of Contamination Control Strategy (CCS)
This diagram visualizes the hierarchical relationship between the three core components of a modern Contamination Control Strategy as required by regulatory guidelines, showing their connection to the ultimate goal of product quality and patient safety.
Diagram 2: The three-pillar hierarchy of a Contamination Control Strategy.
Adherence to the integrated principles of GCCP and GMP/cGMP is non-negotiable for ensuring the integrity of biomedical research and the safety of pharmaceutical products. The fight against cell culture contamination is multifaceted, requiring a holistic Contamination Control Strategy that prioritizes robust design, stringent operational controls, and verifiable monitoring. As the regulatory landscape evolves, with an emphasis on "current" good practices and quality risk management, the industry must continue to adapt. The implementation of advanced detection technologies, rigorous aseptic techniques, and a culture of continuous improvement provides a defensible barrier against contamination, ultimately protecting the validity of scientific data and the health of patients worldwide.
In the context of cell culture contamination research, a fundamental understanding of hazard classification and biosafety levels is paramount. Contamination events are not merely accidents; they often result from a failure to properly assess and mitigate the risks associated with the biological materials in use. This guide provides a systematic framework for classifying cell lines by hazard group and biosafety level, enabling researchers to implement appropriate containment measures that prevent contamination and protect both experimental integrity and personnel safety.
The classification of biological agents follows a graded system where risk increases with each level. Risk Groups (RG) categorize the inherent hazard of the biological agent itself, while Biosafety Levels (BSL) prescribe the specific containment procedures, facilities, and safety equipment required to work with that agent safely [97]. Proper alignment between these two systems forms the cornerstone of an effective contamination control strategy.
Understanding Risk Groups and Biosafety Levels
Risk Group (RG) Classifications
Risk Groups provide a fundamental classification of biological agents based on their inherent potential to cause disease in healthy adult humans. The U.S. National Institutes of Health (NIH) Guidelines establish a four-tier system [97].
Table: Risk Group (RG) Classifications
| Risk Group | Level of Hazard | Description |
|---|---|---|
| RG1 | Low | Agents that are NOT associated with disease in healthy adult humans or animals. |
| RG2 | Moderate | Agents associated with human disease which is rarely serious and for which preventative or therapeutic interventions are often available. |
| RG3 | High | Agents associated with serious or lethal human disease for which preventative or therapeutic interventions may be available. |
| RG4 | Severe | Agents associated with lethal human disease for which preventative or therapeutic interventions are not readily available. |
Biosafety Level (BSL) Classifications
Biosafety Levels build upon the Risk Groups by defining the specific containment and work practices required to handle agents safely. Each BSL includes the protections of the lower level and adds further requirements [98] [97]. The correspondence between Risk Groups and Biosafety Levels, while not always perfectly 1:1, provides a practical framework for risk assessment.
Table: Biosafety Level (BSL) Requirements
| BSL | Agents & Associated Risks | Safety Equipment (Primary Barriers) | Facility Design (Secondary Barriers) |
|---|---|---|---|
| BSL-1 | Low-risk microbes (e.g., non-pathogenic E. coli, chicken pox) posing minimal threat [98]. | Not required; work typically on open benches [98]. | Not isolated from general traffic; basic lab with easy-to-clean surfaces [98]. |
| BSL-2 | Moderate-risk agents (e.g., HIV, Hepatitis, Salmonella, human-derived materials) posing limited to moderate disease risk via ingestion or mucous membrane exposure [98] [97]. | Biological Safety Cabinets (BSCs) for aerosol-generating procedures; lab coats, gloves, eye protection [98] [97]. | Self-closing, lockable doors; sink and eyewash station; biohazard warning signs [98]. |
| BSL-3 | Indigenous or exotic agents (e.g., Mycobacterium tuberculosis, COVID-19) causing serious or lethal disease via inhalation [98]. | BSCs and other physical containment devices; respiratory protection as needed [98]. | Physical separation from access corridors; self-closing double-door entry; negative airflow (directional air supply) [98]. |
| BSL-4 | Dangerous/exotic agents (e.g., Ebola, Marburg) causing life-threatening disease without available treatments or vaccines [98]. | Class III BSCs or full-body, air-supplied positive pressure suits [98]. | Separate building or isolated zone; dedicated supply/exhaust, vacuum, and decontamination systems [98]. |
The following workflow outlines the logical process for classifying a cell line and determining the appropriate biosafety practices, directly linking risk assessment to actionable containment procedures.
The Critical Link to Cell Culture Contamination
A core thesis in contamination research is that improper risk classification is a primary causative factor in contamination events. Different classes of contaminants present distinct challenges, and the biosafety level dictates the rigor required to prevent them.
Microbial Contamination
- Bacteria, Fungi, and Yeast: These contaminants are often introduced through improper aseptic technique and are a primary concern in BSL-1 and BSL-2 labs. They are typically detectable through media turbidity and pH changes [99] [11]. Their prevention hinges on the standard microbial practices and personal protective equipment mandated at these levels.
- Mycoplasma: This type of bacterial contamination is of particular concern because it is invisible to the naked eye and standard light microscopy, yet it significantly alters cell metabolism and gene expression, leading to unreliable experimental data [99] [100]. Mycoplasma contamination is estimated to affect 5-30% of cell cultures [99]. Its spread is almost exclusively due to human error and cross-contamination between cell lines, underscoring the need for strict adherence to BSL-2 practices, such as using dedicated media and working on one cell line at a time [100].
Viral and Chemical Contamination
- Viral Contamination: Viruses can be introduced via contaminated raw materials like serum or host cell lines. They are difficult to detect without specialized tests and may not cause visible changes in the culture, posing a silent risk to both experiments and product safety [11]. The risk is heightened when working with human-derived materials at BSL-2.
- Chemical Contamination: This includes endotoxins, residual detergents, or extractables from plastics. These impurities can affect cell viability and function, introducing variability in results [99] [11]. Prevention relies on using high-quality, validated reagents and adhering to strict cleaning protocols, which are foundational practices across all BSLs.
Methodologies for Risk Assessment and Contamination Detection
A robust risk assessment integrates agent hazards with laboratory procedure risks. The following experimental protocols are essential for identifying and mitigating contamination.
Protocol 1: Biological Risk Assessment Procedure
The Centers for Disease Control and Prevention (CDC) recommends a systematic approach [98]:
- Identify the Agent's Hazardous Characteristics: Assess the pathogenicity, severity of disease, transmission routes, infectious dose, stability in the environment, and host range of the agent associated with the cell line.
- Identify Laboratory Procedure Hazards: Evaluate the specific techniques to be used. Consider the potential for aerosol generation, use of sharps, handling volumes, and routes of exposure (e.g., skin contact, ingestion, inhalation).
- Determine the Appropriate BSL: The final BSL determination is made by integrating the agent and procedure risks. This decision should involve the Principal Investigator, institutional biosafety professionals, and biosafety committees, and must account for all applicable safety precautions, facility safeguards, and regulatory requirements [98] [97].
Protocol 2: Mycoplasma Detection via PCR
Given the prevalence and impact of mycoplasma, regular screening is critical [99] [100].
- Principle: Polymerase Chain Reaction (PCR) uses primers specific to mycoplasma DNA to amplify target sequences, allowing for highly sensitive detection.
- Methodology:
- Sample Collection: Collect a small aliquot of cell culture supernatant from the test culture.
- DNA Extraction: Use a commercial DNA extraction kit to isolate total DNA from the sample. This typically involves cell lysis, binding DNA to a column, washing, and elution [100].
- PCR Amplification: Set up a reaction mix containing the DNA template, mycoplasma-specific primers, nucleotides, and a thermostable DNA polymerase. The reaction is run in a thermal cycler with cycles of denaturation, annealing, and extension.
- Analysis: The PCR products are analyzed by gel electrophoresis. The presence of a band of the expected size indicates mycoplasma contamination. Faster, real-time PCR kits are also available that provide results without gel electrophoresis [100].
- Advantages: This method is rapid, providing results in hours, and is highly sensitive [100].
Protocol 3: Visual and Microscopic Examination for Contamination
Daily monitoring is the first line of defense [99].
- Principle: Macroscopic and microscopic examination can quickly reveal common bacterial, fungal, and yeast contaminants.
- Methodology:
- Macroscopic Inspection: Observe the culture media for signs of turbidity (cloudiness), unexpected color changes (especially with phenol red pH indicator), or floating fungal colonies.
- Microscopic Inspection: Under a standard optical microscope, examine the cells at low and high magnification. Look for signs of cytopathology, but also for small, motile bacteria between the cells. For mycoplasma, while not directly visible, indirect signs like a general decline in cell health may be apparent.
- Staining Techniques: For more definitive detection of mycoplasma, use DNA-binding fluorescent stains like DAPI or Hoechst. After staining, mycoplasma DNA appears as fluorescent specks or filaments on the cell surface or in the background when viewed with a fluorescence microscope [99].
The Scientist's Toolkit: Essential Reagents and Materials
The following reagents and equipment are fundamental to executing the risk assessment and contamination detection protocols described in this guide.
Table: Essential Research Reagents and Materials for Risk Assessment & Contamination Control
| Item | Function & Application |
|---|---|
| Biological Safety Cabinet (BSC) | Primary containment device; provides a sterile, HEPA-filtered work environment for handling biological agents, preventing their release and protecting the user [98]. |
| Mycoplasma Detection Kit (PCR-based) | Provides optimized primers, controls, and buffers for the sensitive and specific detection of mycoplasma contamination in cell cultures via PCR [100]. |
| DNA Extraction Kit | Used to isolate high-quality DNA from cell culture supernatants for subsequent molecular detection methods like PCR [100]. |
| Fluorescent DNA Stains (DAPI/Hoechst) | Used in fluorescence microscopy to detect mycoplasma contamination, which appears as extraneous fluorescent DNA outside of the host cell nuclei [99]. |
| Class II & III BSCs | Advanced primary barriers; Class II BSCs are used in BSL-2/3 labs, while Class III sealed cabinets are mandatory for handling BSL-4 agents [98]. |
| Autoclave | Essential for decontaminating all biohazardous waste (liquid and solid) via steam sterilization before disposal, a requirement across all BSLs [98] [11]. |
| Personal Protective Equipment (PPE) | Includes lab coats, gloves, and eye protection; forms a critical barrier between the researcher and the biological hazard, with specific requirements (e.g., respirators, full-body suits) escalating with the BSL [98] [97]. |
| Validated & Virus-Screened Fetal Bovine Serum (FBS) | Critical culture medium supplement; sourcing from suppliers that provide certification for the absence of viruses and mycoplasma is a key preventative measure against introducing contamination [99] [11]. |
A rigorous and dynamic risk assessment process is the most powerful tool for preventing cell culture contamination. By correctly classifying cell lines according to Hazard Groups and implementing the corresponding Biosafety Level practices, researchers move beyond reactive decontamination to a proactive, preventative stance. This systematic approach, which integrates knowledge of contaminant types with validated detection methodologies and appropriate physical containment, is fundamental to ensuring the integrity of scientific data, the safety of laboratory personnel, and the success of both basic research and clinical drug development.
Contamination in cell culture presents a formidable challenge across the biological sciences and pharmaceutical industry, yet its implications and management differ profoundly between research laboratories and Good Manufacturing Practice (GMP) manufacturing facilities. In research settings, contamination primarily threatens data integrity and reproducibility, whereas in GMP environments, it risks patient safety, regulatory compliance, and batch consistency [11]. This comparative analysis examines the divergent contamination profiles, impacts, and control strategies across these two domains, providing a technical framework for understanding and addressing contamination challenges within a broader thesis on cell culture contamination research.
The fundamental distinction lies in the ultimate purpose of each environment. Research laboratories prioritize discovery and data generation, often working with diverse cell lines and experimental conditions. In contrast, GMP facilities operate under stringent regulatory frameworks to produce therapeutics for human use, where consistency and safety are paramount [11] [101]. This distinction shapes every aspect of contamination control, from prevention strategies to detection methodologies and response protocols.
While both environments share some contamination sources, their prevalence and significance vary considerably, as shown in Table 1.
Table 1: Comparative Analysis of Contamination Sources in Research vs. GMP Environments
| Contamination Source | Research Laboratories | GMP Manufacturing |
|---|---|---|
| Human Handling | Improper aseptic technique, inadequate training [11] | Failure to follow SOPs, improper gowning [11] |
| Environment | Unfiltered air, unclean surfaces in shared spaces [11] | Insufficient cleanroom controls, HVAC failures [11] [102] |
| Raw Materials | Contaminated serum, non-sterile reagents [11] [3] | Non-qualified suppliers, insufficient testing [11] [103] |
| Equipment | Cross-contamination from shared equipment [11] | Improperly maintained bioreactors, particle shedding [11] [102] |
| Process-Related | Inadequate technique during media changes [104] | Insufficient filtration, inadequate sterilization validation [11] |
Prevalence of Contamination Types
The types and detection rates of contaminants differ significantly between environments due to varying screening practices and material sources, as detailed in Table 2.
Table 2: Prevalence and Impact of Different Contamination Types
| Contamination Type | Research Impact | GMP Impact | Detection Methods |
|---|---|---|---|
| Bacterial | Common, usually visible via cloudiness, pH change [3] | Less common due to controls; leads to batch failure [11] | Microscopy, culture, pH monitoring [3] |
| Mycoplasma | Prevalent (up to 35% of cultures), often undetected [104] | Rare due to mandatory testing; would cause batch rejection [11] | PCR, fluorescence staining, ELISA [11] [3] |
| Viral | Concerning for data integrity, often latent [11] | Critical patient safety risk; product recall [11] [102] | qPCR, RT-PCR, immunoassays [11] [3] |
| Cross-Contamination | Common (15-20% of cell lines misidentified) [11] | Rare due to segregation procedures [11] | STR profiling, DNA barcoding [3] |
| Particulate | Minimal research impact | Major concern for injectables; regulatory action [11] [102] | USP 788 compliance testing [11] |
Mycoplasma represents a particularly challenging contaminant in research settings due to its elusive nature. As Mark White of Bio-Rad notes, "Mycoplasma is a particular challenge in cell culture contamination because it is generally too small to see with microscopes common to cell culture facilities and it does not outright kill cells, so it is frequently missed" [104]. This invisibility leads to its prevalence in research laboratories, where it can alter cellular function and compromise experimental results without obvious signs [3].
Impact Assessment: From Data Integrity to Patient Safety
Impact in Research Laboratories
In research environments, contamination primarily affects scientific validity and resource allocation. The consequences include:
Experimental Compromise: Contamination alters cell physiology, gene expression, and metabolic activity, generating misleading data. Mycoplasma contamination alone can cause significant changes in cellular metabolism and gene expression patterns, potentially leading to false conclusions [11] [3].
Resource Depletion: Contamination events waste significant time and financial resources. Archana Bhaw-Luximon notes that contamination "may result in major problems such as the loss of entire experiments, cell cultures and cell lines" [104].
Reproducibility Crisis: Undetected contaminants contribute to the scientific reproducibility problem, particularly when contaminated cell lines are shared between laboratories without proper authentication [11].
Impact in GMP Manufacturing
The implications of contamination in GMP environments extend far beyond data issues to tangible patient and product consequences:
Patient Safety Risks: Microbial contaminants in injectable products can cause severe infections. Recall databases document cases where contaminated products led to patient harm, including Burkholderia cepacia outbreaks and streptococcus-contaminated Avastin [102].
Financial Consequences: Batch failures in biopharmaceutical manufacturing can cost hundreds of thousands to millions of dollars per incident, in addition to regulatory fines and potential legal liabilities [102].
Regulatory Actions: Contamination events can trigger regulatory inspections, manufacturing suspensions, and product recalls. The Moderna COVID-19 vaccine contamination incident led to the recall and destruction of 1.63 million vials [102].
Drug Shortages: Contamination-related production halts can cause significant drug shortages, particularly when manufacturing is concentrated at single facilities, as demonstrated in the Genzyme contamination case [102].
Prevention and Control Strategies
Research Laboratory Approaches
Research laboratories typically employ fundamental contamination control strategies focused on technique and routine testing:
Aseptic Technique: Strict adherence to aseptic methods in biosafety cabinets, including surface disinfection, proper pipetting, and minimal exposure to non-sterile environments [11] [3].
Routine Screening: Regular testing for mycoplasma (every 1-2 months) and microbial contamination through PCR, fluorescence staining, or culture methods [3].
Cell Line Authentication: Implementing STR profiling and regular authentication to prevent and detect cross-contamination [11] [3].
Antibiotic Limitations: Avoiding routine antibiotic use to prevent masking low-level contamination and developing resistant organisms [3].
GMP Manufacturing Systems
GMP facilities implement comprehensive, validated systems with multiple control layers:
Strict Cleanroom Standards: Classified HEPA-filtered cleanrooms with rigorous environmental monitoring, gowning procedures, and access controls [11].
Closed Processing Systems: Utilizing single-use technologies and closed systems to minimize operator and environmental contact. Single-use bioreactors reduce cross-contamination risks between batches [11] [105].
Quality Risk Management: Implementing formal risk assessment methodologies and Contamination Control Strategies (CCS) as required by revised Annex 1 [101].
Supply Chain Control: Rigorous qualification of raw material suppliers and comprehensive testing of starting materials, particularly those of human or animal origin [103] [101].
Process Validation: Validating all critical processes, including sterilization, cleaning, and aseptic operations, with documented evidence of effectiveness [11] [106].
The Scientist's Toolkit: Essential Reagent Solutions
Table 3: Key Research Reagent Solutions for Contamination Control
| Reagent/Material | Function | Application Context |
|---|---|---|
| Mycoplasma Detection Kits (PCR-based) | Rapid detection of mycoplasma contamination | Research & GMP; replaces 28-day culture method [104] |
| HEPA-Filtered Biosafety Cabinets | Provides ISO Class 5 air for aseptic work | Essential in both environments; first line of defense [11] [3] |
| Single-Use Bioreactors | Pre-sterilized, disposable culture vessels | GMP manufacturing; eliminates cleaning validation [105] |
| GMP-Grade Ancillary Materials | Qualified reagents for cell culture media | GMP manufacturing; ensures raw material quality [101] |
| Cell Authentication Kits (STR profiling) | Verifies cell line identity and purity | Research-critical; prevents cross-contamination consequences [3] |
Detection Methodologies and Experimental Protocols
Mycoplasma Detection Protocol
Mycoplasma contamination requires specialized detection methods due to its small size and lack of cell wall. The following protocol represents the current gold-standard approach:
Principle: Mycoplasma species lack cell walls and are too small (0.3μm) for routine microscopic detection, requiring DNA-binding dyes or PCR-based methods for identification [3].
Materials:
- DNA fluorescent stain (Hoechst 33258 or DAPI)
- Mycoplasma experience culture (positive control)
- Methanol:acetic acid (3:1) fixative
- Fluorescence microscope with appropriate filters
- PCR reagents for mycoplasma-specific primers
Procedure:
- Culture test cells on sterile coverslips in culture dishes until 60-70% confluent
- Include positive and negative controls on separate coverslips
- Fix cells with methanol:acetic acid for 5 minutes
- Stain with DNA-binding fluorescent dye (0.1μg/mL in PBS) for 15-30 minutes
- Rinse with deionized water and mount on slides
- Examine under fluorescence microscopy at 400-500x magnification
- Score for characteristic cytoplasmic and membrane-associated fluorescence
Interpretation: Negative samples show fluorescence confined to nucleus. Positive samples display particulate or filamentous cytoplasmic fluorescence and membrane-associated staining [3].
Alternative PCR Method:
- Extract DNA from culture supernatant
- Amplify with mycoplasma-specific 16S rRNA primers
- Separate products by gel electrophoresis
- Compare to positive controls and molecular weight markers
The technological advancement in mycoplasma detection represents a significant improvement, as noted by Félix Montero-Julian: "The use of nucleic acid testing technologies has decreased the time to results from 28 days to just 1 or 2 hours" [104].
Microbial Monitoring Protocol for GMP Environments
GMP facilities require comprehensive environmental monitoring to demonstrate contamination control:
Principle: Active air sampling monitors viable particulate contamination in critical areas to validate cleanroom performance [11] [106].
Materials:
- Microbial air sampler (impaction or centrifugation-based)
- Soybean Casein Digest Agar plates
- Incubator (20-25°C and 30-35°C)
- Colony counting equipment
Procedure:
- Determine sampling locations based on risk assessment and classification
- Sanitize sampler before entering cleanroom
- Place agar plate in sampler according to manufacturer instructions
- Sample specified air volume (typically 1m³)
- Repeat for all predetermined locations
- Incubate plates at 20-25°C for 3-5 days followed by 30-35°C for 2-3 days
- Count colony forming units (CFU) and calculate CFU/m³
- Compare to established alert and action limits
Classification Criteria:
- Grade A: <1 CFU/m³
- Grade B: 10 CFU/m³
- Grade C: 100 CFU/m³
- Grade D: 200 CFU/m³
This monitoring provides data for trend analysis and demonstrates ongoing control of the manufacturing environment [106].
Visualization of Contamination Control Workflows
The following diagram illustrates the key differences in contamination response between research and GMP environments, highlighting the more rigorous investigative and documentation requirements in GMP settings.
Regulatory Frameworks and Future Directions
Regulatory Landscape
The regulatory framework governing contamination control differs substantially between research and GMP environments. Research laboratories primarily follow biosafety guidelines and institutional protocols, while GMP facilities operate under comprehensive regulatory systems including:
- FDA 21 CFR Parts 210 & 211: Current Good Manufacturing Practice for finished pharmaceuticals [101]
- EMA Annex 1: Manufacturing of Sterile Medicinal Products, recently revised to emphasize Contamination Control Strategies [101]
- USP 788: Particulate Matter in Injections [11]
- ICH Q7 and Q10: Quality systems and good manufacturing practice guidance [101]
The regulatory challenge extends to starting materials, where significant international discrepancies exist. As noted in a 2025 regulatory analysis, "The lack of a harmonized language for the definition of SAMS (Starting Active Materials for Synthesis), coupled with a fragmented regulatory framework, presents a challenge for infection protection in pharmaceutical manufacturing" [103].
Emerging Technologies and Future Directions
Both research and GMP environments are benefiting from technological advancements in contamination control:
Rapid Microbiological Methods: Adoption of nucleic acid testing and solid-phase cytometry reduces detection times from weeks to hours, enabling faster decision-making [104].
Single-Use Technologies: Disposable bioreactors and closed systems minimize cleaning validation and cross-contamination risks while increasing manufacturing flexibility [105].
Advanced Detection Systems: Automated, in-line monitoring systems provide real-time contamination assessment, moving from endpoint testing to continuous quality verification [104] [105].
Novel Processing Approaches: Enzyme-free cell detachment using electrochemical methods preserves cell viability while reducing animal-derived reagent use [107].
As Félix Montero-Julian notes, "Most manufacturers concerned about process efficiency, product quality and patient safety will implement contamination control strategies, based on risk analysis, adoption of new microbial detection technologies, and implementing modern environmental monitoring approaches" [104].
This comparative analysis demonstrates that while research and GMP manufacturing face similar contamination challenges, their approaches to management reflect fundamentally different priorities and consequences. Research laboratories emphasize data integrity and experimental reproducibility through aseptic technique and routine screening, while GMP facilities implement comprehensive, validated systems focused on patient safety and regulatory compliance.
The convergence of these domains occurs in advanced therapy medicinal products (ATMPs) and cell therapies, where research processes must transition to GMP-compliant manufacturing. This transition represents a significant challenge, as the "complexity of biologics, as well as the application of emerging technology, pose challenges for cGMP compliance" [101]. Future directions point toward increased automation, rapid detection technologies, and harmonized regulatory standards to address contamination challenges across both environments.
Understanding these distinctions is essential for researchers, quality professionals, and regulatory specialists working to advance biological science and therapeutic development while maintaining the highest standards of data integrity and product quality.
In the context of cell culture research, maintaining impeccable documentation and a robust deviation management system is not merely a regulatory formality; it is a fundamental defense against contamination and a cornerstone of data integrity. Contamination remains one of the most persistent challenges, leading to experimental failures, compromised data, and significant financial losses [11]. Properly maintained batch records provide the traceability necessary to trace the origin of contamination, while an effective deviation management process ensures that any unplanned event is promptly identified, investigated, and corrected. This guide details how integrating these systems creates a framework for understanding the root causes of cell culture contamination, enabling researchers and drug development professionals to implement effective preventive strategies and protect the integrity of their work.
The Role of Batch Records in Traceability and Contamination Investigation
Batch records, often referred to as batch manufacturing records (BMRs) in a GMP environment, serve as the complete history of a single cell culture process. They are a chronological, step-by-step account of all activities, materials, and observations.
Key Components of a Batch Record for Cell Culture
For cell culture processes, a comprehensive batch record should include, but is not limited to, the following elements:
- Master Formula and Raw Materials Record: A complete list of all reagents, media, supplements, and their specific lot numbers. Tracing raw material lots is critical when investigating contamination stemming from a compromised reagent [11] [108].
- Equipment and Consumables Log: Identification of the specific bioreactor, biosafety cabinet, incubator, and single-use consumables (e.g., flasks, tubing) used. This allows for the correlation of equipment malfunctions or contamination events with specific batches [11].
- Process Parameter Log: A detailed record of all critical process parameters, such as temperature, pH, dissolved oxygen, agitation speed, and feeding schedules. Deviations from established parameter ranges can indicate the early stages of microbial contamination [11] [108].
- Operator and Activity Log: Documentation of all procedures performed, including the identity of the researcher, timestamps, and aseptic techniques employed (e.g., media changes, passaging, sampling). This is vital for identifying potential human error or technique-related contamination sources [40].
- In-Process Control and Sampling Data: Records of all samples taken for quality control, including viability, cell count, and tests for microbial contamination (e.g., sterility testing, mycoplasma PCR). The results of these tests are integral to the batch record [11].
Enabling Root Cause Analysis Through Traceability
When contamination occurs, the batch record is the primary tool for the investigation. The traceability embedded within it allows researchers to perform a systematic root cause analysis (RCA). By cross-referencing the contaminated batch's records with clean batches, investigators can identify anomalies. For instance, if multiple contaminated batches share a common raw material lot, a single piece of equipment, or were handled by a single operator, the batch record provides the data needed to pinpoint the likely source. This moves the investigation beyond speculation to a data-driven conclusion, which is the basis for implementing effective corrective and preventive actions (CAPA) [109] [110].
Deviation Management: A Systematic Framework
A deviation is defined as any departure from approved processes, procedures, instructions, specifications, or established standards [110]. In cell culture, this can range from an unplanned temperature fluctuation in an incubator to the clear turbidity of a culture indicating bacterial contamination.
Categorizing Deviations Based on Risk
Deviations are categorized based on their potential impact on product quality, patient safety, and data integrity. This risk-based approach ensures that resources are allocated effectively to address the most significant events. The following table outlines a common categorization system adapted for a research and development context.
Table: Risk-Based Categorization of Deviations in Cell Culture
| Category | Impact Level | Examples in Cell Culture |
|---|---|---|
| Critical | Poses a severe risk to product quality, patient safety, or data integrity. Likely to invalidate the entire batch or study. | Contamination of a master cell bank with mycoplasma or viruses; incorrect labelling of cell lines leading to cross-contamination and misidentification; a failure of a HEPA filter in a biosafety cabinet during processing [11] [110]. |
| Major | Has a significant impact on product quality or reliability of key study data. Requires thorough investigation and corrective action. | A significant excursion of critical process parameters (e.g., pH, temperature) for a prolonged period; an equipment failure that affects cell growth and viability; failure to follow a critical step in an approved SOP [111] [110]. |
| Minor | Has a noticeable but limited impact that does not affect critical quality attributes or the overall interpretation of study data. | A minor documentation error that does not impact data integrity; a single, isolated lapse in aseptic technique with no subsequent contamination detected; a slight delay in a non-critical process step [111] [110]. |
The Deviation Management Process Workflow
A structured workflow ensures that every deviation is handled consistently, from identification to closure. The following diagram illustrates the holistic deviation management process.
Diagram: Holistic Deviation Management Process Flow
Conducting Effective Root Cause Analysis (RCA) for Contamination
A thorough investigation is required for significant deviations, particularly those involving contamination. Regulatory guidelines emphasize that investigation conclusions of "human error" are insufficient without determining the underlying process or system-based cause [109]. Effective RCA tools include:
- 5 Whys: A simple technique of repeatedly asking "Why?" to move beyond the symptomatic cause to the root cause. For example: (1) Why is the culture contaminated? → The media was contaminated. (2) Why was the media contaminated? → The bottle was not sterile. (3) Why was the bottle not sterile? → The autoclave cycle failed. (4) Why did the autoclave cycle fail? → It had not been maintained according to the preventive maintenance schedule. (5) Why was it not maintained? → The maintenance tracking system is not robust [109].
- Fishbone (Cause & Effect) Diagram: A visual tool that helps teams brainstorm and categorize all potential causes of a problem (the effect). For cell culture contamination, major categories typically include "Methods," "Materials," "Equipment," "People," "Environment," and "Measurement" [109]. The following diagram provides a template for a contamination-related investigation.
Diagram: Fishbone Diagram for Contamination Root Cause Analysis
The Scientist's Toolkit: Essential Reagents and Materials for Contamination Control
Preventing contamination requires high-quality materials and consistent techniques. The following table details key reagents and solutions used to maintain sterility and monitor cell culture health.
Table: Research Reagent Solutions for Contamination Control
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Sterile, Single-Use Consumables | Prevents contamination from reusable glassware and cross-contamination between batches. | Use pre-sterilized pipettes, flasks, and bioprocess containers. Avoid reusing single-use items [11] [40]. |
| Validated Cell Culture Media & Sera | Provides nutrients for cell growth. A common source of viral and microbial contamination. | Use reagents from qualified suppliers. Use virus-inactivated serum (e.g., gamma-irradiated) and test raw materials for endotoxins and contaminants [11]. |
| Antibiotics & Antimycotics | Suppresses the growth of low-level bacterial and fungal contaminants. | Should not be used as a substitute for aseptic technique. Their use can mask low-level contamination and lead to the development of resistant strains [11]. |
| Mycoplasma Detection Kits | Detects mycoplasma contamination, which is not visible under a standard microscope and alters cell function. | Use PCR, fluorescence staining, or ELISA-based kits for routine screening of cell stocks and cultures [11]. |
| Sterilizing Agents (e.g., 70% Ethanol) | Disinfects work surfaces, gloves, and equipment exteriors to maintain an aseptic environment in the biosafety cabinet. | Apply liberally before and after all procedures. Ensure proper contact time for effective disinfection [40]. |
| Rapid Detection Technologies | Enables real-time monitoring for contamination. | Emerging technologies, such as Total Volatile Organic Compound (TVOC) sensors, can detect bacterial contamination inside an incubator within hours of onset [5]. |
Experimental Protocols for Monitoring and Investigation
Protocol for Routine Mycoplasma Detection via PCR
Mycoplasma contamination is a frequent and problematic issue in cell culture due to its lack of visible signs. Regular screening is essential [11].
- Sample Collection: Aseptically collect 100-200 µL of cell culture supernatant from a test culture that has been without antibiotics for at least several days.
- Positive Control Preparation: Include a well-characterized mycoplasma strain as a positive control in a separate, quarantined culture.
- DNA Extraction: Use a commercial DNA extraction kit to isolate DNA from both the test sample and the positive control. Include a negative control (sterile culture media) taken through the same extraction process.
- PCR Setup: Prepare a PCR master mix containing primers specific for highly conserved mycoplasma genes (e.g., 16S rRNA). Aliquot the mix into PCR tubes and add the extracted DNA from the test sample, controls, and a no-template control (NTC) with molecular grade water.
- Amplification: Run the PCR using a standardized cycling protocol (e.g., initial denaturation at 95°C for 2 min; 35 cycles of 95°C for 30s, 55°C for 30s, 72°C for 1 min; final extension at 72°C for 5 min).
- Analysis: Separate the PCR products by gel electrophoresis. The presence of a band of the expected size in the test sample, aligning with the positive control, indicates mycoplasma contamination.
Protocol for Investigating a Contamination Deviation
This methodology outlines the steps to take when microbial contamination is suspected or confirmed.
- Immediate Containment:
- Quarantine the contaminated culture immediately. Do not open the culture vessel outside a biosafety cabinet.
- Label the vessel clearly with "CONTAMINATED," the date, and the contaminant if known.
- Initial Assessment & Categorization:
- Observe and document the culture's macroscopic appearance (turbidity, pH change, clumping) and microscopic appearance (bacteria, fungi) at different magnifications.
- Categorize the deviation based on its impact (e.g., Critical, as it compromises the batch).
- Root Cause Analysis:
- Form an investigation team with personnel from relevant areas (lab management, quality, technical staff).
- Use the Fishbone diagram and 5 Whys to brainstorm potential causes.
- Review the complete batch record for the affected culture. Cross-reference materials (media, serum lots), equipment (incubator, biosafety cabinet records), and operator activities with clean batches from the same time period.
- Corrective and Preventive Actions (CAPA):
- Corrective Action: Safely dispose of the contaminated culture by autoclaving.
- Preventive Action: Based on the root cause, implement changes. This could include retraining on aseptic technique, revising an SOP, performing maintenance on an incubator, or quarantining a specific raw material lot.
- Documentation and Reporting:
- Complete a deviation report detailing the discovery, investigation, root cause, and CAPA.
- Ensure all actions and conclusions are documented in the quality system for tracking and trend analysis.
Within the broader thesis on the causes of cell culture contamination, meticulous documentation and traceability through batch records, coupled with a rigorous deviation management system, are not secondary activities but primary scientific controls. They transform the response to contamination from a reactive, ad-hoc effort into a proactive, knowledge-driven process. By systematically recording every aspect of the cell culture process and rigorously investigating every deviation, researchers can move beyond simply observing contamination to understanding its root causes. This structured approach is fundamental to ensuring the reliability of research data, the safety of derived biologics, and the overall success and efficiency of drug development.
Particulate contamination in injectable products represents a critical risk to patient safety, making regulatory compliance not just a legal obligation but a fundamental aspect of product quality and patient care. The United States Pharmacopeia (USP) Chapter <788> and U.S. Food and Drug Administration (FDA) guidelines establish a comprehensive framework for controlling visible and subvisible particulates in parenteral drugs. Within the broader context of cell culture contamination research, controlling particulate matter extends beyond finished product testing to encompass the entire manufacturing process, including the raw materials and cell cultures used in biological drug production. Particulate matter is defined as mobile undissolved particles unintentionally present in drug product solutions, typically categorized as subvisible particles (2-100 μm in diameter) and visible particles [112].
The regulatory landscape emphasizes that meeting USP compendial standards alone does not generally satisfy current good manufacturing practice (CGMP) requirements, necessitating a more holistic, risk-based approach to particulate control [113]. This integrated perspective is particularly relevant for biologics manufactured using cell culture systems, where the integrity of the starting materials directly impacts final product quality. Effective contamination control strategies must therefore address both extrinsic particulates introduced from the environment or equipment and intrinsic particulates derived from the product itself or its container closure system.
USP <788> Requirements and Updates
Scope and Application
USP <788>, officially titled "Particulate Matter in Injections," sets the standard for monitoring subvisible particles in parenteral drug products. The chapter has recently undergone significant revisions, with an updated version officially titled "Subvisible Particulate Matter in Injections" becoming official on August 1, 2026 [31]. This updated chapter provides clarified definitions, recognizing particulate matter as contamination and offering enhanced guidance on precautions during sample preparation. The standard applies to any parenteral drug product and is harmonized with the European (EP 2.9.19) and Japanese (JP 6.07) Pharmacopeias, facilitating global drug development and manufacturing [112].
Testing Methods and Acceptance Criteria
USP <788> specifies two compendial methods for subvisible particulate testing: Light Obscuration (Method 1) and Membrane Microscopy (Method 2). The light obscuration method is generally preferred due to its ease of use and in-solution measurements, while the microscopic method serves as an alternative for products unsuitable for light obscuration analysis, such as those with high viscosity, inherent heterogeneity, or non-transparent formulation buffers [112].
Table 1: USP <788> Particulate Matter Acceptance Criteria
| Product Volume | Test Method | Particle Size ≥10 μm | Particle Size ≥25 μm |
|---|---|---|---|
| ≤100 mL per container | Light Obscuration | 6000 per container | 600 per container |
| >100 mL per container | Light Obscuration | 25 per mL | 3 per mL |
| ≤100 mL per container | Membrane Microscopy | 3000 per container | 300 per container |
| >100 mL per container | Membrane Microscopy | 12 per mL | 2 per mL |
Recent revisions to USP <788> include several important updates: allowing single-unit testing for both large- and small-volume parenterals, permitting testing of smaller sample aliquots (1-5 mL) with justification for products with limited volume, enabling the use of alternative diluents when justified, and clarifying that the average number of particles in the pooled sample must comply with requirements [31]. The revisions also replace the term "aggregation" with "agglomeration" and emphasize that more stringent limits may be appropriate for individual products based on risk assessment.
FDA Regulatory Expectations
Holistic Approach to Particulate Control
The FDA's December 2021 draft guidance, "Inspection of Injectable Products for Visible Particulates," outlines a comprehensive, risk-based approach that extends beyond simple compliance with compendial standards [113]. The guidance emphasizes that meeting USP requirements alone is generally insufficient for satisfying CGMP obligations, requiring manufacturers to implement a holistic control strategy that incorporates:
- Product development considerations designed to minimize particulate generation
- Manufacturing controls that prevent particulate introduction
- Robust visual inspection techniques capable of detecting visible particulates
- Particulate identification and investigation procedures
- Corrective and preventive actions designed to assess, correct, and prevent recurrence of particulate contamination
This comprehensive approach aligns with the FDA's current thinking on quality by design and risk-based manufacturing, where contamination control is built into the product and process rather than merely tested at the end.
CGMP Requirements
The Code of Federal Regulations (21 CFR Part 211) establishes the CGMP requirements for finished pharmaceuticals, providing the regulatory foundation for particulate control [33]. Key provisions relevant to particulate matter include:
- Quality Control Unit Responsibilities (§211.22): Mandating a quality control unit with responsibility and authority to approve or reject all components, drug product containers, closures, in-process materials, and drug products, with adequate laboratory facilities for testing.
- Personnel Qualifications (§211.25): Requiring education, training, and experience to enable personnel to perform assigned functions, with continuing CGMP training.
- Building and Facility Design (§211.42): Specifying that buildings must be of suitable size, construction, and location to facilitate cleaning, maintenance, and proper operations while preventing contamination.
- Air Quality Control (§211.46): Requiring equipment for adequate control over air pressure, microorganisms, dust, humidity, and temperature, with appropriate air filtration systems.
These regulations collectively establish the foundation for controlling particulate matter at every stage of the manufacturing process, from facility design and personnel practices to in-process controls and final product release.
Connection to Cell Culture Contamination Research
Microbial Contamination Detection Technologies
Advanced detection methods for cell culture contamination represent a critical front in the overall strategy for controlling particulate matter in biologics manufacturing. Recent research has yielded promising technologies that could transform contamination monitoring in cell therapy products and other biologics:
UV Absorbance Spectroscopy with Machine Learning: Researchers from the Singapore-MIT Alliance for Research and Technology have developed a novel method that combines UV absorbance spectroscopy with machine learning to detect microbial contamination in cell therapy products within 30 minutes [66]. This approach measures ultraviolet light absorbance of cell culture fluids and uses machine learning algorithms to recognize light absorption patterns associated with microbial contamination. The method offers significant advantages over traditional sterility testing, which requires 7-14 days, by providing a rapid, label-free, non-invasive assessment that facilitates automation of cell culture sampling with a simple workflow.
TVOC Sensor Technology: A feasibility study published in Talanta demonstrates the potential of total volatile organic compound (TVOC) sensors for real-time monitoring of bacterial contamination in cell cultures, with detection possible within 2 hours of contamination onset [5]. This approach continuously monitors bacterial emissions of volatile organic compounds directly inside cell culture incubators using semiconductor-based sensors. While measurements of ammonia and hydrogen sulfide proved inconclusive, TVOC sensors showed specificity for bacterial contamination, providing a foundation for developing non-invasive, real-time monitoring systems that ensure sterility and quality during cell culture development.
Table 2: Comparison of Contamination Detection Methods
| Detection Method | Time to Result | Key Advantages | Limitations |
|---|---|---|---|
| Traditional Sterility Testing | 7-14 days | Established regulatory acceptance; broad spectrum detection | Labor-intensive; slow results affecting patient treatment |
| Rapid Microbiological Methods (RMMs) | ~7 days | Faster than traditional methods | Complex processes; requires skilled workers; growth enrichment needed |
| UV Absorbance with Machine Learning | 30 minutes | Label-free; non-invasive; simple workflow; enables automation | Preliminary step only; requires confirmation |
| TVOC Sensor Technology | 2 hours | Real-time monitoring; non-invasive; automated systems | Early research stage; requires refinement of sensitivity/specificity |
Viral Contamination Challenges
Viral contamination presents distinct challenges in cell culture systems, particularly because some viruses lack obvious cytopathic effects and require sophisticated detection methods [14]. Epstein Barr virus (EBV) and Ovine Herpesvirus 2 (OvHV-2) represent particular concerns as gammaherpesviruses with high prevalence and worldwide distribution. The presence of their latent and active forms can be problematic for human and animal cell technology used in biological production, necessitating robust detection methodologies including PCR assays that can identify both active and latent viral forms.
Implementation Strategies
Integrated Control Strategy
Implementing an effective particulate control strategy requires an integrated approach that spans the entire product lifecycle:
- Product Development Stage: Design formulations and container closure systems to minimize particulate generation, leachables, and interactions.
- Process Development: Establish manufacturing processes with appropriate controls for filtration, mixing, and filling operations.
- Environmental Controls: Implement adequate air classification systems with regular monitoring for nonviable particulates.
- Component Controls: Establish stringent specifications and inspection procedures for components likely to contribute to particulate matter.
- In-Process Testing: Implement appropriate in-process controls and testing to monitor particulate levels throughout manufacturing.
- Final Product Inspection: Conduct 100% inspection for visible particulates complemented by subvisible particulate testing per USP <788>.
Investigation and Root Cause Analysis
When particulate matter exceeds established limits, manufacturers must conduct thorough investigations to determine root cause and implement appropriate corrective and preventive actions. Flow imaging microscopy (FIM) serves as a valuable orthogonal technique for root cause analysis, providing insight into particle morphology, type, and source that complements the compendial light obscuration and microscopic methods [112]. While not a compendial method for lot release, FIM can capture images of unexpected particles to help identify their type and source, enabling researchers to address underlying process issues before they impact product quality.
Experimental Protocols and Methodologies
Compendial Testing Procedures
USP <788> Method 1 - Light Obscuration Particle Count Test Protocol
- Apparatus Preparation: Ensure the light obscuration particle count test instrument is properly calibrated and qualified according to manufacturer specifications.
- Sample Preparation: Carefully mix the samples by gentle inversion to achieve uniform distribution without introducing air bubbles. For products requiring dilution, use appropriate particle-free diluents with proper justification.
- Instrument Priming: Rinse the instrument fluid path with particle-free water until background counts meet specifications, then prime with the specific product being tested if necessary.
- Sample Analysis: Perform multiple measurements (typically 3-5) per container, discarding the first milliliter if necessary to avoid contamination from the container closure system.
- Data Analysis: Calculate the mean particle count for each container and determine compliance with the acceptance criteria based on product volume.
USP <788> Method 2 - Microscopic Particle Count Test Protocol
- Membrane Preparation: Use a clean membrane filter apparatus with a grid-patterned membrane filter of appropriate pore size (typically 1.0 μm or less).
- Filtration Assembly: Assemble the filtration apparatus under laminar airflow conditions to prevent contamination.
- Sample Filtration: Transfer the specified volume of sample to the filtration funnel and apply vacuum filtration.
- Membrane Washing: Rinse the inner walls of the funnel with particle-free water to ensure complete transfer of particles to the membrane.
- Membrane Examination: Place the membrane in a petri dish and examine microscopically under controlled lighting conditions, counting particles ≥10 μm and ≥25 μm.
Advanced Monitoring Techniques
UV Absorbance with Machine Learning Protocol [66]
- Sample Collection: Collect cell culture fluid samples at designated intervals using automated sampling systems to minimize operator variability.
- UV Spectral Analysis: Measure ultraviolet light absorbance across relevant wavelengths without additional sample preparation or staining.
- Data Processing: Process spectral data to extract features relevant to contamination detection.
- Machine Learning Classification: Apply trained machine learning algorithms to classify samples as contaminated or uncontaminated based on UV absorption patterns.
- Result Interpretation: Provide intuitive "yes/no" contamination assessment within 30 minutes, enabling timely corrective actions.
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents and Materials for Particulate Contamination Studies
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Particle-Free Diluents | Sample preparation for light obscuration testing | Validated for low particulate background; compatible with product |
| Grid-Patterned Membrane Filters | Microscopic particle count testing | Consistent pore size (≤1.0 μm); minimal particle shedding |
| Particle Size Standards | Instrument calibration | Certified reference materials of known size and concentration |
| Microbial Reference Strains | Contamination detection validation | Representative ATCC strains for method validation |
| PCR Master Mixes | Viral contamination detection | High sensitivity and specificity for target viruses |
| Cell Culture Media | Contamination challenge studies | Serum-free options to reduce background interference |
| Particle-Free Consumables | All testing procedures | Validated containers, gloves, and utensils to prevent contamination |
Workflow and Relationship Diagrams
Particulate Control System Workflow
Advanced Contamination Detection Technologies
Meeting USP <788> and FDA guidelines for particulate matter requires a comprehensive, science-based approach that integrates robust quality systems, modern analytical technologies, and thorough process understanding. The regulatory framework emphasizes that compendial testing alone is insufficient, instead requiring a holistic control strategy that spans product development, manufacturing controls, inspection techniques, and investigation procedures. For manufacturers utilizing cell culture systems, emerging technologies for rapid contamination detection offer promising opportunities to enhance product quality and patient safety while maintaining regulatory compliance. By implementing the strategies and methodologies outlined in this guide, manufacturers can establish effective particulate control programs that satisfy regulatory requirements and protect patient health.
Contamination represents one of the most persistent and devastating challenges in cell culture laboratories, with profound implications for research integrity, drug development timelines, and biomanufacturing product quality. Despite advances in aseptic technologies, contamination events continue to compromise experimental reproducibility and validity, potentially leading to erroneous scientific conclusions and substantial financial losses. Within the broader context of contamination research, effective crisis management requires a systematic approach that moves beyond mere detection to comprehensive root cause analysis and implementation of robust corrective and preventive actions (CAPA). This technical guide provides researchers, scientists, and drug development professionals with a structured framework for managing contamination events, with emphasis on practical methodologies for investigation, data analysis, and process improvement.
The consequences of contamination extend across the research and development spectrum. In academic settings, contamination primarily affects data integrity and reproducibility, potentially invalidating months of research and compromising publication quality [11]. In Good Manufacturing Practice (GMP) environments, the stakes are significantly higher, where contamination can lead to batch failures, regulatory actions, and patient safety risks [11] [114]. A single contamination event in biopharmaceutical production can result in losses exceeding hundreds of thousands of dollars and substantial delays in therapy availability [3]. Understanding these consequences underscores the critical importance of robust contamination crisis management protocols.
Cell culture contaminants can be broadly categorized as biological, chemical, or physical, each presenting distinct challenges for detection and eradication. Biological contaminants include bacteria, fungi, mycoplasma, viruses, and cross-contaminating cell lines [29]. Unlike microbial contamination, which often produces visible signs, viral and mycoplasma contamination can persist cryptically, altering cellular functions without obvious morphological changes [14] [115]. Chemical contamination encompasses endotoxins, detergent residues, plasticizers, and media impurities, while particulate contamination presents particular concerns in GMP manufacturing of injectable biologics [11].
Contamination sources are equally diverse, originating from multiple points in the cell culture workflow:
- Personnel: Improper aseptic technique, inadequate personal protective equipment, and human error represent frequent contamination vectors [116].
- Raw materials: Contaminated sera, media, supplements, and reagents introduce contaminants directly into culture systems [117] [11].
- Equipment: Non-sterile instruments, improperly maintained incubators, and compromised filtration systems serve as contamination reservoirs [11] [116].
- Environment: Airborne microorganisms, unclean laminar flow hoods, and inadequate facility controls enable contamination ingress [117] [116].
Table 1: Major Contamination Types, Characteristics, and Detection Methods
| Contamination Type | Visual Indicators | Impact on Culture | Preferred Detection Methods |
|---|---|---|---|
| Bacterial | Cloudy/turbid medium, sudden pH drop (yellow color), odor [29] [3] | Rapid cell death, metabolic alteration [3] | Microscopy, microbial culture [29] |
| Mycoplasma | No visible signs in medium [3] | Altered metabolism, chromosomal aberrations, reduced transfection efficiency [115] | PCR, fluorescence staining, ELISA [3] [115] |
| Fungal/Yeast | Filamentous threads, fuzzy structures, visible colonies [3] | Slowed cell growth, culture overgrowth [3] | Microscopy, microbial culture [29] |
| Viral | Often no visual indicators; possible cytopathic effects [29] [3] | Altered cellular function, safety risks [14] [29] | qPCR/RT-PCR, immunofluorescence, electron microscopy [3] |
| Cross-Contamination | Unexpected changes in cell behavior/morphology [3] | Genetic and phenotypic drift, erroneous data [3] | STR profiling, karyotype analysis, isoenzyme analysis [3] |
Crisis Management Protocol: A Structured Approach
Immediate Response and Containment
Upon detection of suspected contamination, immediate action is required to prevent further spread:
- Quarantine Affected Cultures: Immediately isolate contaminated cultures from clean stocks to prevent cross-contamination [11] [29]. Clearly label quarantined materials with contamination type, date, and investigator.
- Document Initial Observations: Record contamination morphology, affected vessels, culture history, and recent experimental manipulations. Photograph contamination signs through microscopy when possible.
- Cease All Related Experiments: Discontinue use of shared reagents, media, and equipment pending investigation to prevent secondary contamination events.
- Notify Relevant Personnel: Alert laboratory management, quality assurance staff, and collaborating researchers to implement broader containment measures.
Root Cause Analysis Methodologies
Effective root cause analysis employs structured investigative approaches to identify underlying contamination sources rather than superficial symptoms:
Environmental Monitoring Assessment
Review environmental monitoring data including air quality metrics, surface microbial counts, and water system testing [117]. Compare current values against established baselines to identify deviations. In one documented case, approximately 10% of process contamination was traced to airflow issues in cleanrooms [117].
Process Mapping and Timeline Analysis
Reconstruct the entire culture history through detailed process mapping, documenting all manipulations, reagent additions, and equipment usage. Identify temporal patterns correlating with contamination emergence, paying particular attention to recent protocol changes or deviations.
Material and Reagent Traceability
Establish complete traceability for all culture components, including serum lots, media batches, and supplements. Maintain records of supplier certifications, sterilization validation, and quality control testing. Studies indicate that 5-35% of cell lines used for bioproduction contain mycoplasma contamination, highlighting the importance of rigorous material screening [117].
The following workflow outlines the comprehensive crisis management process from detection to preventive action:
Diagram 1: Contamination Crisis Management Workflow
Experimental Protocols for Contamination Investigation
Microbial Identification Protocol
For bacterial and fungal contamination characterization:
- Sample Collection: Aseptically transfer 1mL of contaminated medium to sterile microcentrifuge tube. Include samples from unaffected cultures as controls.
- Microscopic Examination:
- Prepare wet mounts of contaminated medium for direct microscopy at 100-400x magnification.
- Use Gram staining to differentiate bacterial types (Gram-positive vs. Gram-negative).
- Employ lactophenol cotton blue staining for fungal element visualization.
- Culture-Based Identification:
- Inoculate contaminated samples onto blood agar, MacConkey agar, and Sabouraud dextrose agar.
- Incubate at 25°C and 37°C for 24-72 hours under aerobic and anaerobic conditions.
- Document colony morphology, pigment production, and hemolytic patterns.
- Molecular Identification (for persistent or atypical contaminants):
- Extract microbial DNA using commercial kits validated for contamination detection.
- Perform 16S rRNA gene sequencing for bacterial identification or ITS sequencing for fungi.
- Compare sequences against databases (NCBI, RDP) for taxonomic classification.
Mycoplasma Detection Protocol
Multiple complementary methods are recommended due to the challenges in detecting mycoplasma:
DNA Fluorescence Staining:
- Culture cells on sterile coverslips in 6-well plates until 60-70% confluent.
- Fix cells with fresh Carnoy's fixative (methanol:acetic acid, 3:1) for 10 minutes.
- Stain with DNA-binding dye (Hoechst 33258 or DAPI) for 30 minutes in the dark.
- Examine under fluorescence microscopy using UV excitation.
- Positive samples show characteristic particulate or filamentous staining outside cell nuclei [115].
PCR-Based Detection:
- Extract DNA from culture supernatant and cell pellets using commercial kits.
- Use mycoplasma-specific primers targeting 16S rRNA genes (e.g., MycoSP or MycoLP systems).
- Include positive controls (known mycoplasma DNA) and negative controls (nuclease-free water).
- Amplify according to manufacturer protocols and analyze amplicons by gel electrophoresis.
- PCR assays can detect less than 10 colony-forming units (CFU) of contamination [96].
Microbiological Culture (Gold Standard):
- Inoculate samples into selective mycoplasma broth and agar media.
- Incubate aerobically and anaerobically for up to 28 days at 37°C.
- Monitor weekly for color changes in broth and colony formation on agar.
- Confirm suspicious colonies by subculture and DNA staining.
Table 2: Contamination Detection Technologies and Applications
| Detection Technology | Principles | Applications | Sensitivity | Time Requirements |
|---|---|---|---|---|
| Spectroscopy | Measures light interaction with molecules [96] | Chemical contamination, particle identification [96] | Variable by technique | Minutes to hours |
| PCR/Molecular Diagnostics | Amplification of target nucleic acid sequences [96] | Viral, mycoplasma, and microbial detection [96] [3] | High (<10 CFU for bacteria) [96] | 2-6 hours |
| Microscopy | Visual observation of morphological characteristics [29] | Bacterial, fungal, yeast contamination [29] | Limited by resolution | Immediate to 30 minutes |
| Immunoassays (ELISA) | Antigen-antibody binding with enzymatic detection [3] | Viral contamination, specific pathogen detection [3] | Moderate to high | 2-4 hours |
| Microbial Culture | Growth in selective media [29] | Bacterial and fungal contamination [29] | 1-10 CFU | 2-14 days |
Viral Screening Protocol
For comprehensive viral contamination assessment:
Cytopathic Effect (CPE) Evaluation:
Molecular Detection:
- Extract total nucleic acids from cell culture supernatants and cell pellets.
- Perform PCR or qPCR with pan-viral primers or virus-specific primers (e.g., for Epstein-Barr virus or ovine herpesvirus 2) [14] [3].
- Include appropriate controls (positive, negative, inhibition).
- For RNA viruses, incorporate reverse transcription step prior to amplification.
Electron Microscopy:
- Concentrate culture supernatant by ultracentrifugation.
- Fix pellet with glutaraldehyde and prepare thin sections.
- Stain with uranyl acetate and lead citrate.
- Examine under transmission electron microscope for viral particles.
Corrective and Preventive Actions (CAPA)
Decontamination Procedures
Following contamination identification and root cause analysis, implement targeted decontamination:
Equipment Decontamination:
- Clean incubators, biosafety cabinets, and work surfaces with sporicidal agents (e.g., hydrogen peroxide vapor, chlorine dioxide) [118].
- Validate decontamination efficacy using biological indicators (Geobacillus stearothermophilus spores).
- Replace HEPA filters in biosafety cabinets and incubators if compromised.
Culture Decontamination (for irreplaceable cell lines):
- Implement antibiotic/antimycotic treatment at determined non-toxic concentrations [29].
- Use multiple passages at 2-3x the minimum inhibitory concentration.
- Validate decontamination success through comprehensive testing after antibiotic-free culture.
Process Controls and System Improvements
Engineering and administrative controls provide sustainable contamination prevention:
- Closed Processing Systems: Implement closed bioreactor systems and single-use technologies to minimize manual interventions and environmental exposure [11] [118].
- Environmental Monitoring Enhancement: Establish continuous monitoring for non-viable particles, viable microorganisms, and air pressure differentials in critical areas [117].
- Quality Control Testing: Strengthen raw material testing protocols, particularly for high-risk components like fetal bovine serum and cell culture supplements [117] [11].
The following diagram illustrates the relationship between major contamination sources and corresponding control measures:
Diagram 2: Contamination Sources and Control Measures
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Contamination Management
| Reagent/Material | Function | Application Notes |
|---|---|---|
| HEPA-Filtered Biosafety Cabinet | Provides sterile workspace with unidirectional airflow [11] [116] | Must be certified annually; surfaces decontaminated before/after use [116] |
| PCR Master Mixes | Amplification of target microbial/viral sequences [96] [3] | Select kits validated for sensitivity to detect <10 CFU [96] |
| DNA Binding Dyes (Hoechst/DAPI) | Fluorescent staining of microbial DNA [115] | Critical for mycoplasma detection; requires fluorescence microscopy [115] |
| Selective Culture Media | Supports growth of specific contaminants [29] | Used for bacterial/fungal identification; incubation up to 14 days [29] |
| Validated Disinfectants | Surface decontamination [118] | Rotation of sporicidal and bactericidal agents prevents resistance [118] |
| Sterile Single-Use Systems | Closed processing solutions [11] | Reduces contamination risk from reusable equipment; pre-validated [11] |
| Antibiotic/Antimycotic Solutions | Suppression of microbial growth [29] | Use sparingly to avoid masking low-level contamination [29] [3] |
Documentation and Regulatory Considerations
Comprehensive documentation is essential for both regulatory compliance and continuous improvement:
- Deviation Reporting: Document contamination events through formal deviation reports including date, time, affected materials, preliminary assessment, and immediate actions [11].
- Investigation Reports: Prepare detailed investigation reports containing root cause analysis, supporting data, and CAPA implementation plans.
- CAPA Effectiveness Verification: Establish metrics to monitor CAPA effectiveness, including contamination rate trending, environmental monitoring data, and quality control test results.
- Regulatory Alignment: Ensure contamination control strategies align with current regulatory guidance including EU Annex 1, FDA aseptic processing guidelines, and pharmacopeial standards [11] [118].
In GMP environments, regulatory agencies require documented contamination control strategies based on scientific justification and quality risk management principles [118]. These strategies must include detailed assessments of facility design, equipment controls, and procedural safeguards to prevent contamination ingress into drug products.
Effective management of contamination events requires a systematic approach that integrates immediate containment, rigorous root cause analysis, and sustainable corrective actions. By implementing the protocols and frameworks outlined in this technical guide, research and development organizations can transform contamination crises from catastrophic setbacks into opportunities for process improvement and quality system enhancement. The continued evolution of contamination detection technologies, particularly rapid microbiological methods and real-time monitoring systems, promises enhanced capabilities for early detection and prevention [96]. However, technological advances must be supported by robust quality systems, comprehensive training, and a culture of transparency and continuous improvement to achieve meaningful reduction in contamination-related risks.
Conclusion
Effective management of cell culture contamination requires a holistic and proactive strategy that integrates foundational knowledge, rigorous methodological application, continuous optimization, and robust validation. Understanding the diverse sources of contamination—from biological and chemical to cross-contamination—is the first critical step. Implementing consistent aseptic techniques, coupled with regular monitoring and advanced detection methods, forms the backbone of contamination control. Furthermore, recognizing the distinct requirements and higher stakes in GMP manufacturing versus research settings is essential for applying appropriate risk management and regulatory compliance. By adopting these comprehensive practices, scientists can safeguard the integrity of their research, ensure the reproducibility of data, and uphold the safety and efficacy of biopharmaceutical products, thereby reinforcing the critical role of pure cell cultures in advancing biomedical science and clinical applications.
References
- 1. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 2. Troubleshooting Cell Culture Contamination: A Practical ... [https://www.yeasenbio.com/blogs/cell/troubleshooting-cell-culture-contamination-a-practical-solution-guide]
- 3. Cell Culture Contamination: 5 Common Sources and How ... [https://www.capricorn-scientific.com/knowledge-center/cell-culture-contamination]
- 4. VOC analysis for rapid, early detection of bacteria, mold ... [https://www.sciencedirect.com/science/article/pii/S2472555225000759]
- 5. Real-time monitoring of cell culture contamination via ... [https://www.sciencedirect.com/science/article/pii/S0039914025014493]
- 6. Preventing and Avoiding Cell Culture Contamination [https://www.technologynetworks.com/cell-science/how-to-guides/preventing-and-avoiding-cell-culture-contamination-299231]
- 7. A new method for detecting mycoplasma in cell cultures ... [https://www.sciencedirect.com/science/article/pii/S2405580825002201]
- 8. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 9. Mycoplasma Testing for Quality Control [https://www.atcc.org/microbe-products/applications/quality-control/mycoplasma-testing]
- 10. Mycoplasma Contamination: Prevention, Testing & Treatment [https://blog.cellsignal.com/mycoplasma-contamination]
- 11. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 12. How Does Mycoplasma Contamination Affect Cell Culture? [https://www.eppendorf.com/us-en/lab-academy/life-science/cell-biology/how-does-mycoplasma-contamination-affect-cell-culture/]
- 13. rapid and reliable mycoplasma detection based on PCR [https://www.rapidmicrobiology.com/news/unexplained-cell-culture-results-hidden-mycoplasma-contamination-could-be-the-cause]
- 14. Viral contamination in cell culture: analyzing the impact of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 15. Fundamental Strategies for Viral Clearance Part 2 [https://www.bioprocessintl.com/viral-clearance/fundamental-strategies-for-viral-clearance-part-2-technical-approaches]
- 16. Viral contamination in biologic manufacture and ... [https://www.nature.com/articles/s41587-020-0507-2]
- 17. Viral Safety in Bioprocessing [https://www.merckmillipore.com/RS/en/technical-documents/technical-article/pharmaceutical-and-biopharmaceutical-manufacturing/monoclonal-antibody-manufacturing/viral-safety-in-bioprocessing]
- 18. Viral Contamination of Cell Cultures [https://www.bioprocessintl.com/biochemicals-raw-materials/spontaneous-infection-did-you-leave-the-back-door-open-to-your-cultivation-suite-]
- 19. Controlling Endotoxin Contamination in Bioprocessing [https://www.genscript.com/protein-news/controlling-endotoxin-contamination-in-bioprocessing.html]
- 20. Pyrogen Testing for Medical Devices [https://namsa.com/resources/blog/pyrogen-testing-for-medical-devices/]
- 21. Guidance for Industry: Pyrogen and Endotoxins Testing [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-pyrogen-and-endotoxins-testing-questions-and-answers]
- 22. Five Easy Ways to Keep Your Cell Cultures Endotoxin-Free [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/five-easy-ways-to-keep-your-cell-cultures-endotoxin-free.html]
- 23. Controlling endotoxin contamination in PDMS-based ... [https://www.sciencedirect.com/science/article/pii/S0142941825001096]
- 24. Detergents for Cell Lysis and Protein Extraction [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/detergents-cell-lysis-protein-extraction.html]
- 25. 6 Easy Ways to Remove Excess Detergent from Membrane ... [https://bitesizebio.com/53887/remove-excess-detergent-from-membrane-proteins/]
- 26. Cell line authentication: a necessity for reproducible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9289526/]
- 27. Cell Line Cross-Contamination and Misidentification [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-cell-line-misidentification?srsltid=AfmBOoqCp16CDSAk2RCbjpGSupsGkLLKeEv13npyBZ52_WBWXXVZAdp7]
- 28. List of contaminated cell lines [https://en.wikipedia.org/wiki/List_of_contaminated_cell_lines]
- 29. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 30. Prioritizing Particulate Control for Safer Therapy Development [https://chartermedical.com/single-use-manufacturing-prioritizing-particulate-control-for-safer-therapy-development/]
- 31. <788> Particulate Contamination [https://www.usp.org/harmonization-standards/pdg/general-methods/particulate-contamination]
- 32. The EU GMP Annex 1 (2022) and the 5 µm Particles in ... [https://www.gmp-compliance.org/gmp-news/the-eu-gmp-annex-1-2022-and-the-5-um-particles-in-grade-a-b]
- 33. 21 CFR Part 211 -- Current Good Manufacturing Practice ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-211]
- 34. Good Practice Guide: SMEPAC - Standardized ... [https://ispe.org/publications/guidance-documents/good-practice-guide-smepac-standardized-methodology-evaluation-pharmaceutical-airborne]
- 35. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooLwv5D-Cayg8T2LypUw00Tg8_v6arQzWKRbCN-Y-9zI7eMC-F3]
- 36. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOoooSnSIAg4cAvNKjMbkTsXFploTz6F_tP-yRP25mddfm1b1TBNU]
- 37. Development and validation of universal PCR, basic ERA, ... [https://pubmed.ncbi.nlm.nih.gov/40339624/]
- 38. Simple, specific, rapid, and pharmacopoeia-compliant ... [https://www.sciencedirect.com/science/article/pii/S2329050125001676]
- 39. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 40. Tips and Tricks to Minimize Cell Culture Contamination [https://cellculturecompany.com/tips-and-tricks-to-minimize-cell-culture-contamination/]
- 41. 细胞培养污染故障排除 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooHMVoTtSjwuCDpxY7arNKzs2qcw6yFRkc55cWuJGBJNALzrCEg]
- 42. 实验技术(八):常见细胞污染及解决策略 [https://www.muhn.edu.cn/ecmd/info/1481/15455.htm]
- 43. 4.3: Lab Procedures- Bacterial Smear, Simple and Gram ... [https://bio.libretexts.org/Courses/North_Carolina_State_University/MB352_General_Microbiology_Laboratory_2021_(Lee)/04%3A_Staining_Techniques/4.03%3A_Lab_Procedures-_Bacterial_Smear_Simple_and_Gram_Staining]
- 44. 《CMI》发表最新综述:如何使用直接镜检法诊断真菌感染? ... [https://www.kanhuxi.com/documents/%E5%A4%B4%E6%9D%A1/6703/]
- 45. 如何最大程度地降低污染风险并保护细胞培养物| 康宁 [https://www.corning.com/cn/zh/products/life-sciences/resources/stories/at-the-bench/how-to-minimize-contamination-risk-and-protect-your-cultures.html]
- 46. 微生物实验室中的污染:来源、影响与控制策略 [https://www.hzmeizhuo.com/news/sterilization-encyclopedia/wswsyszd.html]
- 47. 原代细胞培养实战指南:三步彻底杜绝支原体污染 [https://www.uptbio.com/news/view/1228.html]
- 48. The 5 Most Common Causes of Contamination in Tissue ... [https://plantcelltechnology.com/blogs/blog/the-5-most-common-causes-of-contamination-in-tissue-culture-labs?srsltid=AfmBOordGuuE7OFjr4UqHmJ_Y9ko_0R-8bLFT5VOJRg_MSMiCDtf-h_5]
- 49. Decoding Cell Culture Contamination—An In-Depth Analysis [https://www.halolabs.com/blog/cell-culture-contamination/]
- 50. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 51. Manufacturing Contamination | SEM EDS Analysis [https://www.thermofisher.com/um/en/home/materials-science/learning-center/eds-analysis/manufacturing-contamination-tracking.html]
- 52. Micro- and nano-plastics induce inflammation and cell death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995046/]
- 53. Bioaccumulation of microplastics in decedent human brains [https://www.nature.com/articles/s41591-024-03453-1]
- 54. Comparative analysis between digital PCR and blood ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1615409/full]
- 55. Troubleshooting Common Cell Culture Contamination Issues [https://cellculturecompany.com/troubleshooting-common-cell-culture-contamination-issues/]
- 56. Authentication of Human and Mouse Cell Lines by Short ... [https://www.ncbi.nlm.nih.gov/books/NBK144066/]
- 57. Cell line authentication and validation is a key requirement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181071/]
- 58. Development and validation of a 21-plex STR panel [https://www.sciencedirect.com/science/article/abs/pii/S1875176819303403]
- 59. STR Amplification | STR Analysis | STR kits [https://www.promega.com/products/forensic-dna-analysis-ce/str-amplification/]
- 60. Mammalian chromosome analysis and sorting by flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10356183/]
- 61. Standardization of Cell Culture Conditions and Routine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9265327/]
- 62. Cell culture and maintenance protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 63. Appendix 3: Cell Culture Hygiene Practices [https://www.isscr.org/basic-research-standards/appendix-3]
- 64. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 65. The 5 Most Common Causes of Contamination in Tissue ... [https://plantcelltechnology.com/blogs/blog/the-5-most-common-causes-of-contamination-in-tissue-culture-labs?srsltid=AfmBOoolFCdOOx-XYT2xL366e_M7GauBhF5xtQ67TwBW1wf3y9QfWObj]
- 66. Novel method detects microbial contamination in cell cultures [https://news.mit.edu/2025/novel-method-detects-microbial-contamination-smart-0425]
- 67. The current state of aseptic processing & fill-finish manufacturing [https://www.crbgroup.com/insights/pharmaceuticals/aseptic-processing]
- 68. BSC Installation and Maintenance Best Practices [https://www.escolifesciences.com/news/optimizing-safety-bsc-installation-and-maintenance-best-practices]
- 69. In-Depth Comparison Between HEPA and ULPA Filters ... [https://www.escolifesciences.com/news/in-depth-comparison-between-hepa-and-ulpa-filters-in-biosafety-cabinets]
- 70. High-Efficiency Filtration: The Role of HEPA and ULPA ... [https://www.labmanager.com/high-efficiency-filtration-the-role-of-hepa-and-ulpa-filters-in-lab-safety-33870]
- 71. Cell Culture Contamination: How to Prevent Fungal, Yeast, ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/how-to-control-bacterial-contamination-and-other-unwelcome-micro.html]
- 72. Biological Safety Cabinets and Culture Hoods: Know The ... [https://bitesizebio.com/8998/biological-safety-cabinets-and-culture-hoods-know-the-difference/]
- 73. Class I vs Class II vs Class III Biological Safety Cabinets [https://www.aesenvironmental.co.uk/2025/08/29/biological-safety-cabinet-class-comparison/]
- 74. HEPA Filters in Biosafety Cabinets [Simplified Guide] [https://www.labrepco.com/2024/02/27/understanding-the-role-of-hepa-filters-in-biosafety-cabinets/?srsltid=AfmBOopaccmjfawYKPyhrMPnY9pbuI8MrlDcYAqUz35RrgjdAUxoSsF9]
- 75. ULPA filter vs HEPA filter in Biosafety Cabinets [https://unicornlifescience.com/ulpa-filter-vs-hepa-filter-guide/]
- 76. Unexpected, pervasive and persistent viral and bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7496648/]
- 77. Essential Quality Control Considerations for Cell Culture [https://absbio.com/white-papers/essential-quality-control-considerations-for-cell-culture/]
- 78. Cell Culture Quality Control: Best Practices [https://cellculturecompany.com/cell-culture-quality-control-best-practices/]
- 79. Guide to Irradiation and Sterilization Validation of Single- ... [https://www.bioprocessintl.com/single-use/guide-to-irradiation-and-sterilization-validation-of-single-use-bioprocess-systems]
- 80. Water Bath Uses in Laboratory: Working Principle, Types ... [https://www.borosilscientific.com/water-baths-oil-baths/]
- 81. Do's and Don'ts while using a Water Bath [https://labstac.com/News/Dos-and-Donts-while-using-a-Water-Bath/2023111601]
- 82. How to Use Laboratory Water Baths [https://www.mrclab.com/how-to-use-laboratory-water-baths]
- 83. Antibiotics in Cell Culture: When and How to Use Them [https://www.capricorn-scientific.com/knowledge-center/antibiotics-in-cell-culture]
- 84. Cell Culture Contamination | Thermo Fisher Scientific - ZA [https://www.thermofisher.com/za/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 85. Antibiotic-Antimycotic (100X) 100 mL | Buy Online | Gibco™ [https://www.thermofisher.com/order/catalog/product/15240062]
- 86. Antibiotics and antimycotics in cell culture: how do they ... [https://bitesizebio.com/13679/antibiotics-antimycotics-cell-culture-how-do-they-work-when-to-use-them/]
- 87. Antifungals Reagents in Cell Culture [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/antifungals?srsltid=AfmBOoqnVJKpN0Q4ZugtAOLy9n4-yf4DoWvWasifZDbDGI_nK34OC8Ik]
- 88. Use antibiotics in cell culture with caution: genome-wide ... [https://www.nature.com/articles/s41598-017-07757-w]
- 89. Antibiotic carry over is a confounding factor for cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319067/]
- 90. Bacterial Contamination - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/bacterial-contamination]
- 91. Keeping it clean: the cell culture quality control experience at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8506661/]
- 92. GMP vs cGMP: What Are The Differences? [https://www.scilife.io/blog/gmp-vs-cgmp-differences]
- 93. FDA Issues New Guidance on Current Good Manufacturing ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/01/fda-guidance-good-manufacturing-practices-for-drugs]
- 94. Guidance on good manufacturing practice and good ... [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/compliance-research-development/good-manufacturing-practice/guidance-good-manufacturing-practice-good-distribution-practice-questions-answers]
- 95. Implementation of Contamination Control Strategy [https://www.americanpharmaceuticalreview.com/Featured-Articles/619888-Implementation-of-Contamination-Control-Strategy-Regulatory-Evolution-and-Industry-Adaptation-Since-2023/]
- 96. Contamination Detection in Pharma Products Market 2025 ... [https://www.towardshealthcare.com/insights/contamination-detection-in-pharma-products-market-sizing]
- 97. Risk Groups & Working at BSL-1, BSL-2, or BSL-3 [https://ehs.virginia.edu/Biosafety/Riskgroups]
- 98. Biosafety Levels 1, 2, 3 & 4: What's the Difference? [https://consteril.com/biosafety-levels-difference/]
- 99. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOopyH6zkCKrSsJlcn5e45nuukQgyK0DVheF8HOL0Q4KyY_UiiS_6]
- 100. On the frontline of the fight against cell culture contamination [https://www.nature.com/articles/d42473-019-00306-1]
- 101. Differences, challenges and best practices for ... [https://www.polyplus-sartorius.com/differences-challenges-and-best-practices-for-manufacturing-of-biologics-under-gmp-compliance]
- 102. Contamination Trends & Proposed Solutions [https://ispe.org/pharmaceutical-engineering/march-april-2023/contamination-trends-proposed-solutions]
- 103. Preventing Microorganism Contamination in Starting Active ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298561/]
- 104. Cell culture and contamination: ask the experts [https://www.regmednet.com/cell-culture-and-contamination-ask-the-experts/]
- 105. Why Single-Use Bioreactors Are Revolutionizing Cell ... [https://cellculturecompany.com/why-single-use-bioreactors-are-revolutionizing-cell-culture-in-2025/]
- 106. The management of good manufacturing practice (GMP ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1687864/full]
- 107. An improved way to detach cells from culture surfaces [https://news.mit.edu/2025/improved-way-detach-cells-culture-surfaces-1118]
- 108. Seven Common Causes of Pharma Process Deviations [https://www.sartorius.com/en/knowledge/science-snippets/seven-common-causes-of-pharmaceutical-process-deviations-602740]
- 109. Deviation Management - Blog - PQE Group [https://blog.pqegroup.com/gxp-compliance/deviation-management]
- 110. Deviation Management Process in the Pharmaceutical ... [https://simplerqms.com/deviation-management/]
- 111. Clinical Trial Protocol Deviation [https://www.biopharmaservices.com/blog/exploring-clinical-trial-protocol-deviation-a-comprehensive-guide/]
- 112. An Overview of USP <787>, <788>, and <789> Standards [https://www.fluidimaging.com/blog/usp-787-usp-788-usp-789-standards-injectables]
- 113. Inspection of Injectable Products for Visible Particulates [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/inspection-injectable-products-visible-particulates]
- 114. WHO and UNODC release landmark report on ... [https://www.who.int/news/item/24-07-2025-who-and-unodc-release-landmark-report-on-contaminated-medicines--urging-action-to-protect-patients-from-preventable-harm]
- 115. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOopEB3ihSS8pRQrwXXSkBJMQmH_cJ7vJtSlyoUprivirivJhRE7-]
- 116. The 5 Most Common Causes of Contamination in Tissue ... [https://plantcelltechnology.com/blogs/blog/the-5-most-common-causes-of-contamination-in-tissue-culture-labs?srsltid=AfmBOoqCvifze9fuOOYqqHXSPQ0MQXEouGAl8f_lzdHS9HAC4QsVwBnJ]
- 117. Comprehensive Microbial Control Strategy [https://www.bioprocessintl.com/qa-qc/beyond-traditional-microbiology-testing-developing-a-comprehensive-strategy-for-microbial-control-and-detection]
- 118. Contamination-Control Processes [https://www.bioprocessintl.com/risk-management/what-unseen-trouble-lies-within-your-processes-]